Discount phenytoin american express
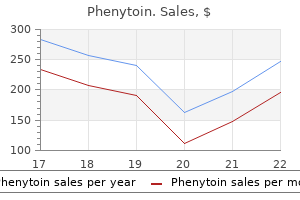
The brightness of the adventitia can be used as a gauge to discriminate predominantly fatty from fibrous plaque: an area of plaque that appears darker than the adventitia is considered fatty medications 2016 buy cheap phenytoin on line. False channels within the plaque can give a similar appearance, and occasionally, shadowing from an adjacent calcified or fibrous region can mimic the appearance of a lipid pool. When combined with automated pullback and border detection techniques, these systems can provide a quantitative assessment of each tissue category over a three-dimensional coronary artery volume. Intravascular Ultrasound Combined With Near-Infrared Spectroscopy Spectroscopy determines chemical compositions based on the analysis of spectra induced by interaction of light with tissue materials. Unlike other light-based imaging techniques, this system does not require removal of blood from the imaging field. The current system is specifically designed for the detection of lipid-rich plaque, which is exhibited yellow on the chemogram, and a color scale from red to yellow indicates increasing algorithm probability of a lipid component of the vessel wall. Classification of tissue is made based on the degree of similarity between the sample and a reference frequency spectrum. A color scale from red to yellow indicates increasing algorithm probability of lipid content. The x-axis represents millimeters of pullback in the artery, and the y-axis represents degrees of rotation. Injection of contrast in this setting can demonstrate free fluid flow behind the flap to better define the extent of tear. The severity of a dissection can be quantified according to depth (intimal, medial, or adventitial) and extent (circumferential and longitudinal). Intrastent dissection is another type of dissection, characterized as separation of neointimal hyperplasia from stent struts. True aneurysm is defined as having an intact vessel wall and a maximum lumen area 50% larger than the proximal reference. In contrast, pseudoaneurysm shows a loss of vessel wall integrity and damage to adventitia or perivascular tissue. Acute thrombus may appear as a relatively echodense mass with speckling or scintillation, whereas old organized thrombus often has a darker ultrasound appearance. Thrombus is also more likely than soft plaque to have the appearance of blood flow in microchannels. Injection of contrast or saline may disperse the stagnant flow from the lumen, often allowing differentiation of stasis from thrombus. Ruptured plaques are often eccentric, less calcified, large in plaque burden, positively remodeled, and associated with thrombus. However, lumen compromise and clinical symptoms likely depend on the severity of the original or coexisting stenosis or on thrombus formation, not solely on plaque rupture. Extensive positive remodeling has also been shown to correlate with unstable plaque. The patient developed an acute coronary syndrome 5 months after deferral of intervention for an intermediate lesion in the left anterior descending artery, based on fractional flow reserve calculated as 0. The use of automated pullback is mandatory for accurate axial registration of analysis segments. A certain length of untreated coronary segment (typically 30 to 50 mm) is preselected for serial analyses using anatomic landmarks such as major side branches. Volume data are often normalized by pullback length (expressed as mean area) or by vessel size (expressed as percent volume) for comparative analysis. Relying on angiographic assessment alone for accurate evaluation of disease progression or regression is extremely challenging, particularly with a diffuse extent of disease and a variable degree of arterial remodeling. Although several clinical trials suggest a significant association, a discrepancy between the imaging end point and clinical outcome has also been implied in some studies. The combination of plaque and carina shift after balloon dilatation or stenting may cause severe narrowing or occlusion of a side branch, particularly in the presence of preexisting ostial disease. Conversely, the ostium of a jailed side branch can falsely appear stenosed on coronary angiography. This "pseudo" sidebranch encroachment is caused by spasm, flow disturbance, or dye streaming due to jailing of the branch orifice by the stent. Several physiologic studies have demonstrated that a considerable number of intermediate lesions referred for elective interventions are in fact hemodynamically insignificant and can be successfully managed with medical treatment alone. In this study, cardiac death and eventfree survival were both comparable in the deferred versus the revascularized group over a 2-year follow-up period. The new stenosis at the proximal stent margin was primarily caused by plaque proliferation despite minimal neointimal hyperplasia observed inside the stent (lower images). Baseline intravascular ultrasound shows a significant residual plaque at the corresponding uncovered segment (upper images). After balloon angioplasty, dissections are often observed at the junction of calcified and noncalcified plaque, where shear forces from dilation are high. For lesions with extensive superficial calcium, plaque modification through the use of rotational atherectomy may be required before balloon dilation or stent implantation. These observations led to the concept of the high-pressure stent deployment technique currently used. These tears have been attributed both to shear forces created at the junction between the metal edge of the stent and the adjacent, more compliant tissue, and to the effect of balloon expansion beyond the edge of the stent (the "dog-bone" phenomenon). Side branches may provide another clue as they should communicate with the true but not with the false lumen. Optimization of Stent Expansion There is compelling evidence that procedure-related factors are important contributors to the development of both restenosis and thrombosis after stent implantation, regardless of stent type. Preinterventional intravascular ultrasound (upper images) revealed significant stent underexpansion at the midsegment with only a small amount of focal neointimal hyperplasia. In contrast, late loss in stented lesions is primarily caused by neointimal proliferation rather than by chronic stent recoil. However, this aggressive optimization strategy has been associated with several clinical issues and may not be feasible in every case. With regard to vessel remodeling, incompletely apposed struts are seen primarily in eccentric plaques, and the gaps develop mainly on the disease-free side of the vessel wall. A significant gap or aneurysm formation can also reduce local blood flow, promoting platelet adhesion and the coagulation cascade. In addition, the irregular edge of the fractured struts may chronically stimulate the vessel wall during cardiac movement. Conversely, deployment of long and rigid stents in angulated lesions with hinge motion can lead to significant alteration of local physiology, so that the strut fracture may help to restore the original dynamic state, at least in some cases. The exact incidence and clinical implications of strut fractures remain to be further investigated in large clinical studies. By angiography, strut fracture is diagnosed as complete or partial separation of the stent at follow-up where there had been contiguity of the stent at baseline. However, in this particular case, the stent fracture (complete separation type) was not associated with increased intimal hyperplasia. By intravascular ultrasound, strut fracture is defined as longitudinal strut discontinuity and can be categorized on the basis of its morphologic characteristics. Blue and red arrows represent stent fracture and resulting movement of the stent segments, respectively. Closely adjacent struts may also be difficult to identify separately because of sidelobe artifacts from the neighboring struts. Potential synergy of different technologies may also include a combination of two diagnostic modalities. Although these new technologies are yet to mature, the advances of diagnostic modalities will enable us to better understand the pathophysiology of cardiovascular disease and could help to realize the ultimate goal of delivering the most effective treatment to individual patients with truly low rates of complications. Nearinfrared spectroscopy predicts cardiovascular outcome in patients with coronary artery disease. Predictors of subacute stent thrombosis: results of a systematic intravascular ultrasound study. Long-term safety of intravascular ultrasound in nontransplant, nonintervened, atherosclerotic coronary arteries. Repeated intravascular ultrasound imaging in cardiac transplant recipients does not accelerate transplant coronary artery disease.
Order phenytoin paypal
Example: If an average of 20 platelets were observed per 1003 oil immersion field treatment yellow jacket sting buy phenytoin no prescription, the platelet estimate is 400,000/mL or mm3 (400 3 109/L). A platelet estimation factor should be determined and validated for each microscope in use (see Box 16. The average number of platelets per oil immersion field multiplied by 20,000 approximates the platelet count per microliter or cubic millimeter. For example, 12 to 16 platelets per oil immersion field equals about 280,000 platelets/mL or mm3 (280 3 109/L) and is considered adequate. Regardless of whether an "official" estimate is made, verification of the instrument platelet count should be included in the overall examination for internal quality control purposes. Blood film examination also includes an assessment of the morphology of the platelets, including size as well as granularity and overall appearance. If slides are taken to another microscope for review, oil should be wiped off first. In phase 1 the numbers and descriptions generated by the testing are summarized using appropriate terminology. This summary provides a verbal picture of the numbers that is easy to communicate to the physician, other health care provider, or another laboratorian. It is much more convenient to be able to say, "The patient has a microcytic anemia" than to say, "The hemoglobin was low, and the mean cell volume was also low. Phase 2 of the interpretation is the essence of the remaining chapters of this book on various hematologic conditions or other metabolic conditions that have an impact on the hematologic system. Generally all the parameters interpreted together provide the best information, so a complete summary of the results should be generated. Assessing Hematology Results Relative to Reference Intervals Proper performance of the phase 1 summary of test results requires comparison of the patient values with the reference intervals. It is important to select the appropriate set of reference intervals in hematology for the gender and age of the patient. Now that the testing for the component parts has been described, interpretation of the results for the total panel can be discussed. First, if the results are very far from the reference interval, it is more likely that they are truly outside the interval and represent a pathologic process. Second, if two or more diagnostically related parameters are slightly or moderately outside the interval in the same direction (both high or both low), this suggests that the results are clinically significant and associated with some pathologic process. Because some healthy individuals always have results slightly outside the reference interval, the best comparison for their results is not the reference interval but their own results from a prior time when they were known to be healthy. Then it is described using appropriate terminology, such as a relative neutrophilia, which is an increase in neutrophils, or a relative lymphopenia, which is a decrease in lymphocytes. The terms used for increases and decreases of each cell type are provided in Table 13. If the proportion of one of the cell types increases, then the proportion of others must decrease because the proportions are relative to one another. Step 3 Examine the relative differential counts for a preliminary assessment of which cell lines are affected. In this case the cells are all within reference intervals relative to one another. They typically are grouped together with the mature neutrophils in judging whether neutrophilia is present. For example, look at the following differential and the reference intervals provided in parentheses: White blood cells 10. The total of the two, 83 (65% 1 18%), exceeds the upper limit of neutrophilic cells even when the two intervals are combined, 80 (70% 1 10%), so these results would be described as a neutrophilia even though the neutrophil value itself is within the reference interval. A graphical representation was made, and the fewer the segments, the farther left was the median-hence left shift. This was called the Arneth count or ArnethSchilling count and was abandoned around the time Arneth died in 1955, but the term left shift lived on to describe increased numbers of immature cells as an indicator of infection. Some laboratories do not report the absolute counts, so being able to calculate them is important. As will be evident in later chapters, the findings in this example point toward a bacterial infection. However, the clinical utility of band counts has been called into question, and most laboratories no longer perform routine band counts. For neutrophilic cells, there is a unique term that refers to the presence of increased numbers of bands or cells younger than bands in the peripheral blood: left shift or shift to the left (Box 13. When young lymphocytic or monocytic cells are present, they can be reported in the differential as prolymphocytes, lymphoblasts, promonocytes, or monoblasts. When observed, young eosinophils and basophils are typically just called immature and are not specifically staged. Step 6 Any abnormalities of appearance are reported in the morphology section of the report. Morphology Step 1 Examine the hemoglobin (or hematocrit) for anemia or polycythemia. Hemoglobin concentration is a more direct indicator of the ability of the blood to carry oxygen. Therefore the hemoglobin is slightly more concentrated than usual, and the cells look darker with no central pallor. If the volumes are variable (more small cells, more large cells, or both), the histogram becomes wider. The blood film also serves as quality control, because the morphologic characteristics seen through the microscope. If everything in the morphology is normal, by convention, no notation regarding morphology is included. One of the major challenges is in determining when the amount or degree of an abnormality is worth noting at all. All laboratories must have good standardized morphology criteria and competent staff whose evaluations are consistent with one another and with the standardized criteria used in that facility. Generally, a semiquantitative method is used that employs terms such as slight, moderate, and marked or the numbers 11, 21, and 31. Numerical ranges representing the reporting unit are defined; for example, three to six spherocytes per oil immersion field might be reported as 21 spherocytes. Although this practice has been followed for many years, this semiquantitative method may not best serve the needs of medical staff, and many laboratories are moving toward simplifying their reports to state present for morphologic abnormalities. A better way to assess replacement erythropoiesis is with the reticulocyte count and subsequent calculation of the reticulocyte production index, if appropriate. Morphology B 2 10 20 30 fL Step 1 the platelet count should be examined for increases (thrombocytosis) or decreases (thrombocytopenia) outside the established reference interval. A patient who has unexplained bruising or bleeding may have a decreased platelet count. Pancytopenia is clinically significant because it can indicate a possible developing acute leukemia (Chapter 31) or aplastic anemia (Chapter 19). Pancytosis frequently is associated with a diagnosis of polycythemia vera (Chapter 32). Additional morphologic descriptors include terms for reporting granularity, which is most important if missing, and in this case the platelets are described as "hypogranular" or "agranular. Although the relative differential values are all within the reference intervals, calculation of absolute counts indicates an absolute neutropenia and lymphopenia. Step 5: Make note of immature cells in any cell line reported in the differential that should not appear in normal peripheral blood. Step 6: Make note of any morphologic abnormalities and correlate film findings with the numerical values. This problem must be recognized through blood film examinations and the proper course of action followed to produce accurate results. The basic technique can be modified as needed to accommodate specimens from patients with very high or very low hematocrits. A laboratory science student consistently makes wedgetechnique blood films that are too long and thin. A stained blood film is held up to the light and observed to be bluer than normal. Which of the following values most closely correlates with the estimate per microliter Which of the following is the best area to review or perform a differential on a stained blood film Usefulness of fully automated measurement of reticulated platelets using whole blood.
Discount phenytoin 100mg with visa
Transcatheter or surgical aortic valve replacement in patients with prior coronary artery bypass grafting symptoms 2016 flu order 100mg phenytoin with visa. Long-term health benefit of transcatheter aortic valve replacement in patients with chronic lung disease. Comprehensive echocardiographic assessment of normal transcatheter valve function. Prosthesis-patient mismatch in high-risk patients with severe aortic stenosis: a randomized trial of a self-expanding prosthesis. The impact of transcatheter aortic valve implantation and surgical aortic valve replacement on left ventricular remodeling. Effects of transcatheter aortic valve implantation on left ventricular and left atrial morphology and function. Early recovery of left ventricular systolic function after corevalve transcatheter aortic valve replacement. Immediate improvement of left ventricular mechanics following transcatheter aortic valve replacement. Differences in left ventricular remodelling in patients with aortic stenosis treated with transcatheter aortic valve replacement with corevalve prostheses compared to surgery with porcine or bovine biological prostheses. Health status after transcatheter aortic valve replacement in patients at extreme surgical risk: results from the CoreValve U. First direct aortic retrievable transcatheter aortic valve implantation in humans. Multicentre clinical study evaluating a novel resheathable annular functioning selfexpanding transcatheter aortic valve system: safety and performance results at 30 days with the Portico system. Thirty-day outcomes in 100 consecutive patients undergoing transfemoral aortic valve replacement with the portico valve on an all-comer basis. Implantation and 30day follow-up on all 4 valve sizes within the Portico transcatheter aortic bioprosthetic family. Transcatheter aortic valve replacement with the Portico valve: one-year results of the early Canadian experience. Portico at 1 year: "There is Nothing Like First-Hand Evidence"-Sir Arthur Conan Doyle. Feasibility and safety of transfemoral sheathless Portico aortic valve implantation: preliminary results in a single center experience. A three-dimensional echocardiographic study on aortic-mitral coupling in transcatheter aortic valve replacement. Transcatheter aortic valve replacement using the Portico system: 10 things to remember. Transcatheter aortic valve replacement with new-generation devices: a systematic review and meta-analysis. Early clinical outcomes of a novel self-expanding transapical transcatheter aortic valve bioprosthesis. Multicenter comparison of novel self-expanding versus balloon-expandable transcatheter heart valves. Transfemoral implantation of the acurate neo for the treatment of aortic regurgitation. Portico sheathless transcatheter aortic valve implantation via distal axillary artery. Sequential transcatheter aortic valve implantation due to valve dislodgement-a Portico 212. The average time from implant to valve-in-valve procedures has been approximately 8 years. Biologic prosthetic valves, fashioned from animal or human tissue, do not require long-term anticoagulation and have thus been increasingly chosen by implanting cardiac surgeons and patients. In the United States, bioprostheses accounted for 79% of all surgical aortic implants between 2002 and 2010, with the highest rates in older, higher-risk patients. The reported incidence of aortic or mitral valve deterioration requiring reintervention is high: 20% to 30% at 10 years and over 50% at 15 years. Although the outcomes associated with redo surgery continue to improve, surgical mortality remains between 3% and 23% in various series,7,8 and morbidity remains substantial. Stented surgical heart valves consist of (1) a stent frame composed of metal alloys or polymers; (2) a sewing ring allowing fixation within the valve annulus or above it (supra-annular); and (3) three valve leaflets, which are sewn to the stent frame (either internally or externally). Stented "sutureless" surgical heart valves, modeled on transcatheter valve platforms, have recently been introduced. Stentless valves eliminate the reduction in the annular area caused by a stent frame, thus increasing the effective orifice area. Unfortunately the labeling of surgical heart valves lacks standardization across manufacturers13; frequently valves labeled as being of the same size will have different internal and external dimensions. Generally labeled valve sizes refer to the external dimension of the valve frame and/or sewing ring, whereas internal dimensions are 1 to 4 mm smaller. A ViV smartphone application will list a large range of commonly used surgical and transcatheter valves-with descriptions, images, dimensions, photographic and fluoroscopic images-along with guidance on sizing and positioning. The model and its labeled size should routinely be obtained from an operative report. A useful technique is to find the fluoroscopic projection that (1) is perpendicular to the plane of the surgical valve and (2) superimposes the two valve posts (purposely positioned by the surgeon) on either side of the left coronary ostium. This work added tremendously to the understanding of the possibilities and limitations of the procedure. Patients with failing bioprosthetic aortic valves frequently have multiple comorbidities, and attention to detail in the initial assessment can help to avoid potential pitfalls. The surgical report and history can provide necessary information such as the specifics of the surgical valve implanted (manufacturer, model, size), concomitant surgery (root replacement, coronary reimplantation, bypass grafts), and procedural complications. The angulation of the surgical bioprosthetic valve is also important; tilting of the surgical valve toward the coronary ostium may cause occlusion even if there is a spacious aortic root. The question then becomes whether to reconsider other options, such as redo surgery or medical management, or to mitigate the risks of coronary obstruction. Various approaches may be considered to either reduce the risk of coronary occlusion or manage coronary occlusion should this occur. Should coronary obstruction occur, options might include emergent stenting or surgical bypass, often requiring cardiopulmonary support. Although this can be helpful in establishing coronary patency, the durability of aorto ostial stenting in the presence of an obstructive bioprosthetic leaflet is questionable. Recent years have seen a strong trend toward the use of sedation and local anesthesia. It is important to note that the sewing ring may or may not be radio-opaque and that the relationship between the sewing ring and a radio-opaque valve stent varies, particularly for annular and supra-annular surgical valves. Although this observation is speculative, low implantation resulting in intra-annular constrained leaflets may predispose to leaflet thrombosis or reduced durability. Ex vivo studies demonstrate that most currently implanted bioprosthetic valves yield at 8 to 26 atm. Jude Trifecta bioprosthetic valves, which typically do not fracture at achievable pressures. Small case series have demonstrated the feasibility of dilating Mitroflow, Perimount, Magna and Magna Ease, Biocor Epic and Epic Supra, and Mosaic surgical valves. To date complications have been infrequent, with most patients experiencing a marked reduction in transvalvular gradients. Initially, patients undergoing ViV were at high risk of surgical reintervention, with multiple comorbidities. Malpositioning and/or valve embolization has been more common in ViV cases2 and may be related to regurgitation as the mode of surgical valve failure, radiolucent surgical valves, and inexperience. Transseptal procedures are performed using femoral venous access and a transseptal puncture with antegrade access to the mitral valve. Transapical procedures are performed through a small lateral thoracotomy and direct apical puncture. Although apical access may provide a more straightforward route to the mitral valve, the trade-off is the morbidity associated with a thoracotomy and apical injury.
Order phenytoin 100mg fast delivery
The injection catheter dimensions may be influenced by whether contrast or saline is imaged within the catheter tip and by the type of material used in catheter construction treatment enlarged prostate purchase generic phenytoin line. As high-flow injection catheters have been developed, more quantitative angiographic systems have been using contrast-filled injection catheters for image calibration. Biologic Variability Studies that include a wide range of vessel sizes have more biologic variability in vessel diameter (reflected in the standard deviation of the measurements) than those that are more restrictive in their inclusion criteria. A diameter function profile curve (insert) shows the diameters of the vessel along the length of the analysis segment. Transient maximum coronary vasodilation may be achieved with intracoronary (50 to 200 g), intravenous (>10 g/ min), or sublingual (0. Acquisition Variability Acquisition factors that affect variability include cardiac and respiratory motion artifact, vessel foreshortening, inadequate filling of the coronary artery. Out-of-plane magnification and pincushion distortion may also contribute to small errors in angiographic imaging. For sequential studies, use of the identical angiographic imaging laboratory allows replication of the x-ray generator, tube, and image intensifier parameters. Quantitative angiographic analysis of bifurcation lesions is complicated by the difficulty in identifying the minimal lumen diameter at the site of vessel branching. The first is conventional quantitative angiography separately applied to each branch (A, before intervention; B, after intervention). The second method is application of the edge algorithm to both branches (C, before intervention; D, after intervention). The third method is beginning analysis at the ostium of the branch (E, before intervention; F, after intervention). From these measurements, the minimal lumen diameters within the stent (stent segment) and within the region of analysis (analysis segment) are identified. Measurement Variability Analysis of two or more orthogonal projections permits a more accurate assessment of the physiologic significance of lesion severity, although a second, technically suitable projection in many cases is unavailable due to vessel foreshortening, overlap, and poor image quality. If orthogonal projections are not available, analyses of the worst-view projection may provide sufficiently accurate information for clinical studies. After radiation brachytherapy, the proximal and distal portion of the radiation injury are identified (solid lines). A 5-mm proximal and distal edge of the radiation zone is also analyzed (shaded boxes) to identify the edge effect. From these measurements, the minimal lumen diameters within the segment of balloon injury (injury segment), the segment of radiation injury (radiation segment), and the region of analysis (analysis segment) are identified. The shaded portion in the diameter function profile curve (insert) represents the region of the artery that was treated with radiation but was not injured with the balloon. When direct digital angiography is performed and random errors associated with noise in the cine-video pathway are eliminated, frame selection may be a much more important contributor to overall measurement variability. Frame selection has been associated with substantial interobserver variability, and the frame demonstrating the sharpest and tightest view of the stenosis should be used. Core laboratory reproducibility of various angiographic parameters may affect sample size calculations for various studies. Edge-detection algorithms that identify the arterial edge using a 50% weighted threshold of the first- and second-derivative extrema may produce systematically larger reference and obstruction diameters than those using a 75% weighted value (weighted toward the first-derivative extremum) or the first-derivative extremum itself. These systematic differences may also affect the accuracy and reproducibility of the absolute and relative angiographic measurements. Binary angiographic restenosis is best defined as a 50% diameter stenosis at follow-up, although other dichotomous criteria have been used. Power transformation improved the reliability of the estimate in the sirolimus arm (predicted 3. Coronary stents provide a superior residual lumen compared with balloon angioplasty, but they may result in higher amounts of late intimal hyperplasia and late lumen loss than is seen after balloon angioplasty. With the advent of coronary stents and the determination that stent thrombosis is associated with a suboptimal initial angiographic result, a more contemporary definition of angiographic stenting success is attainment of a less than 20% residual diameter stenosis within the stent, although higher (up to 30%) inflow or outflow diameter stenosis may exist due to residual plaque at the stent margins. Whereas late loss as a surrogate was dependent on vessel size, percent diameter stenosis was independent of vessel size. Compensatory arterial dilation occurs during the early stages of coronary atherosclerosis, resulting in a preserved coronary lumen despite significant coronary atherosclerosis. Routine coronary angiography can accurately measure the arterial lumen but is relatively insensitive for the detection of arterial wall atherosclerosis, circumferential plaque distribution, vessel wall calcification, and lumen dimensions after stent implantation. Coronary angiography is limited to a lesser extent by radiographic factors, such as cardiac motion, pincushion distortion, and quantum mottling. Newer methods incorporating adaptive simultaneous coronary border detection have been developed to more accurately assess smaller vessel dimensions. Interpretation of 2D angiographic views can be affected by foreshortening and overlapping of vessels, leading to inaccurate measurements, particularly in tortuous vessels. Comparison of Mayo Clinic risk score and American College of Cardiology/American Heart Association lesion classification in the prediction of adverse cardiovascular outcome following percutaneous coronary interventions. A statistical analysis of intravascular ultrasound and coronary angiography in 1155 lesions. Shortcoming of the Medina classification as a preferred classification for coronary artery bifurcation lesions in comparison to the Movahed classification. Angioplasty guidewire velocity: a new simple method to calculate absolute coronary blood velocity and flow. Robustness of late lumen loss in discriminating drug-eluting stents across variable observational and randomized trials. Importance of stenosis morphology in the estimation of restenosis risk after elective percutaneous transluminal coronary angioplasty. Predicting major adverse cardiac events after percutaneous coronary intervention: the Texas Heart Institute risk score. Cyphering the complexity of coronary artery disease using the syntax score to predict clinical outcome in patients with three-vessel lumen obstruction undergoing percutaneous coronary intervention. Prognostic value of the Syntax score in patients undergoing coronary artery bypass grafting for three-vessel coronary artery disease. Reliability and limitations of angiography in the diagnosis of coronary plaque rupture: an intravascular ultrasound study. Development and validation of a stent thrombosis risk score in patients with acute coronary syndromes. Angiographic geometric changes of the lumen arterial wall after bioresorbable vascular scaffolds and metallic platform stents at 1-year follow-up. Stent deployment in calcified lesions: can we overcome calcific restraint with high-pressure balloon inflations Impact of lesion calcification on clinical and angiographic outcome after sirolimuseluting stent implantation in real-world patients. Predictors of target lesion revascularization and documented stent thrombosis beyond 30 days after sirolimus-eluting stent implantation: retrospective analysis in consecutive 1,070 angiographic follow-up lesions. Prognostic implications of coronary calcification in patients with obstructive coronary artery disease treated by percutaneous coronary intervention: a patient-level pooled analysis of 7 contemporary stent trials. Incidence, location, magnitude, and clinical correlates of saphenous vein graft calcification: an intravascular ultrasound and angiographic study. Angiographic features of vein grafts versus ungrafted coronary arteries in patients with unstable angina and previous bypass surgery. Early outcome of treatment of ostial de novo left anterior descending coronary artery lesions with drug-eluting stents. Effectiveness of the stent pull-back technique for nonaorto-ostial coronary narrowings. Quantitative assessment of angiographic restenosis after sirolimus-eluting stent implantation in native coronary arteries. Periprocedural and late consequences of overlapping Cypher sirolimus-eluting stents: pooled analysis of five clinical trials. Incidence and predictors of restenosis after coronary stenting in 10,004 patients with surveillance angiography. The determinants of side branch compromise after main vessel stenting in coronary bifurcation lesions. Stenting of bifurcation lesions using the Bestent: a prospective dual-center study.
Buy discount phenytoin 100mg online
Upper extremity deep venous thrombosis and its impact on morbidity and mortality rates in a hospital-based population treatment dry macular degeneration cheap phenytoin 100 mg mastercard. Color Doppler sonographic imaging in the assessment of upper-extremity deep venous thrombosis. Deep vein thrombosis of the axillary-subclavian veins: epidemiologic data, effects of different types of treatment and late sequelae. Circumferential venolysis and paraclavicular thoracic outlet decompression for "effort thrombosis" of the subclavian vein. Spectrum of upper-extremity deep venous thrombosis in a community teaching hospital. Subclavian vein thrombosis in patients treated with infusion chemotherapy for advanced malignancy. Venous thrombosis and stenosis after implantation of pacemakers and defibrillators. Early operative intervention after thrombolytic therapy for primary subclavian vein thrombosis: an effective treatment approach. Deep vein thrombosis and pulmonary embolism in two cohorts: the longitudinal investigation of thromboembolism etiology. Validation of the Canadian clinical probability model for acute venous thrombosis. Effects of a low-molecular-weight heparin on thrombus regression and recurrent thromboembolism in patients with deep-vein thrombosis. Endovascular treatment options in the management of lower limb deep venous thrombosis. Percutaneous mechanical thrombectomy combined with catheter-directed thrombolysis in the treatment of symptomatic lower extremity deep venous thrombosis. Iliofemoral deep venous thrombosis: aggressive therapy with catheter-directed thrombolysis. Midterm followup after pharmacomechanical thrombolysis for lower extremity deep venous thrombosis. Pharmacomechanical thrombectomy for iliofemoral deep vein thrombosis: an alternative in patients with contraindications to thrombolysis. Ultrasound-accelerated thrombolysis for the treatment of deep vein thrombosis: initial clinical experience. Ultrasound-assisted versus conventional catheter-directed thrombolysis for acute iliofemoral deep vein thrombosis. Post-thrombotic syndrome after catheter-directed thrombolysis for deep vein thrombosis (CaVenT): 5-year follow-up results of an open-label, randomised controlled trial. The potential for serious neurologic complications during such procedures places a premium on careful studies documenting the overall clinical efficacy of intervention compared with medical therapy. The technique has proven to be equivalent to carotid endarterectomy in high-risk patients. There remains debate on the interpretation of randomized trial data for carotid stenting and on Medicare reimbursement in normal-risk patients. Intervention at this site is straightforward and safe but has not proven to be superior to medical therapy alone. Based on dramatic technological advances and increased operator expertise, these procedures can currently be performed with a high rate of technical success. However, because of the potential for serious neurologic complications from endovascular intervention in the cerebrovascular circulation, clear documentation of the safety of these procedures and their overall clinical efficacy is of paramount importance. These considerations have raised the bar for cerebrovascular intervention compared with other peripheral vascular procedures. In the field of cerebrovascular intervention, carotid bifurcation intervention is unique in that the natural history of carotid artery bifurcation disease has been well defined and large randomized trials have previously documented the clinical effectiveness of surgical revascularization for this disease. There is already a large evidence base supporting carotid intervention in specific patient subgroups, and several randomized trials are ongoing in the remaining patient populations. In contrast, endovascular intervention in the cerebrovascular circulation outside of the carotid bifurcation has been hampered by two important considerations: the natural history of noncarotid bifurcation cerebrovascular disease is less well defined, and there is a notable absence of randomized data documenting the benefit of revascularization compared with medical therapy alone. However, despite these obstacles, dramatic advances in the technical aspects of these interventions have been made, and there is an increased recognition of the need for well-designed clinical studies that address these deficiencies. What is often underappreciated is that noncarotid bifurcation cerebrovascular disease is responsible for at least the same number of ischemic strokes as carotid bifurcation disease and represents an equally important target for stroke prevention. The emerging role of intracranial intervention in acute stroke management is also introduced. This plaque is similar to that found at other sites throughout the arterial system in that it contains a dense cap of connective tissue with embedded smooth muscle cells and an underlying core of lipid and necrotic debris. The dominant mechanism of stroke is believed to result from distal thromboembolism to the anterior cerebral circulation. However, a number of considerations, such as the size and composition of the embolus, the presence of contralateral disease, the anatomy of the circle of Willis, and the activity of fibrinolytic pathways, may attenuate or accentuate the clinical consequence of the pathologic event. Consequently, the same pathologic event may result in a reversible neurologic deficit. Symptomatic lesions of the carotid bifurcation are associated with a high risk of recurrent ischemic stroke. By contrast, asymptomatic lesions of the carotid bifurcation are associated with a much lower risk of ischemic stroke. Among asymptomatic patients, the association between stenosis severity and risk of subsequent stroke has been inconsistent. Currently there are more sophisticated models to predict the risk of stroke in patients with carotid disease, particularly for symptomatic patients. However, these models have yet to be incorporated into patient selection criteria in randomized trials to more fully establish their clinical relevance. These data are extremely important in any discussion of endovascular therapy for carotid bifurcation disease because they form the cornerstone justifying revascularization in certain subsets of patients. In addition, the crossover of the eventfree curves occurred very early in the patient cohort with 70% to 99% stenoses (1 to 2 months) compared with the patient cohort with 50% to 69% stenosis (1 year). These studies were performed in the late 1980s and early to mid-1990s; therefore the only stipulated medical therapy in the nonsurgical arm was aspirin. If the life expectancy of the patient is less than 5 years, then significant benefit should not be anticipated. In addition, participation in these trials involving patients with asymptomatic carotid stenoses required documentation of a perioperative stroke and death rate of less than 3% at the investigation site, and the generalization of these findings is predicated on reproducing similar procedural outcomes. The first rigorous clinical testing of percutaneous carotid revascularization began in the mid-1990s. The Glidewire is exchanged for a superstiff Amplatz or SupraCore wire, and then the diagnostic catheter is removed. Although this standard approach is sufficient for approximately 70% of cases, a number of variations to the technique may be necessary, depending on the specific anatomic features of the individual patient. Overall, these anatomic features allow the operator to more accurately determine the procedural risk and facilitate the planning of appropriate technique for procedural success. We administer a heparin bolus of 25 mg/kg before any diagnostic cerebrovascular procedure in an effort to minimize the risk of thrombotic complications. A variety of catheter types are used to perform angiography, depending on the personal preference of the operator and the anatomy of the aortic arch and great vessels. These systems allow continued antegrade flow during carotid intervention-an important consideration for patients with compromised collateral flow to the ipsilateral carotid territory. Manufacturer Medtronic Boston Scientific Cordis Abbott Laboratories ev3 Abbott Laboratories Medtronic Diameter (mm) 4. With the exception of the EmboShield and Spider devices, the filter is fixed to the wire. The success of such systems is predicated on adequate collateral circulation from the circle of Willis to maintain cerebral perfusion. Although these results are encouraging, a direct comparison of proximal versus distal embolic protection in a randomized trial with hard clinical outcomes is needed. Attempts to deliver the stent without predilation have been associated with a greater amount of atheroembolism, likely related to increased trauma to the lesion with forcible passage of the stent across a tight stenosis. Initial attempts at carotid stenting using relatively inflexible stainless steel balloon-expandable stents. However, their use was abandoned owing to the subsequent development of stent crushing, likely related to compression of the superficially located carotid stent from neck movements.
XueZhiKang (Red Yeast). Phenytoin.
- How does Red Yeast work?
- What is Red Yeast?
- High cholesterol.
- Are there any interactions with medications?
- Indigestion, diarrhea, improving blood circulation, spleen and stomach problems, and other conditions.
- High cholesterol and triglyceride levels caused by human immunodeficiency virus (HIV) disease (AIDS).
- Dosing considerations for Red Yeast.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96889
Purchase phenytoin from india
Although medium-term follow-up was limited treatment 2011 buy phenytoin 100 mg cheap, no patient had evidence of moderate or severe pulmonary regurgitation at 1 or 2 years of follow-up. At 1-year follow-up, there were two patients who required surgical conduit replacement, no patients who required catheter-based reintervention, and no pulmonary insufficiency worse than mild. Importantly, long-term results of a prospectively enrolled cohort have been reported. It is recommended that the patient be anticoagulated, most commonly with heparin, throughout the procedure. Variations on the technique described here, particularly prestenting of a stenotic conduit before Melody valve implantation, have become widespread. Results After an initial report on the first 34 patients, McElhinney and colleagues reported the short- and medium-term follow-up results from the expanded U. Currently, a decade in, outcomes data demonstrate excellent effectiveness and low complication rates, with sustained relief of pulmonary stenosis and pulmonary insufficiency. Balloon aortic valvuloplasty: results of the valvuloplasty and angioplasty of congenital anomalies registry. Balloon angioplasty for branch pulmonary artery stenosis: results from the valvuloplasty and angioplasty of congenital anomalies registry. Implantation of balloon-expandable intravascular grafts by catheterization in pulmonary arteries and systemic veins. Balloon angioplasty and stenting of branch pulmonary arteries: adverse events and procedural characteristics. Early results and mediumterm follow-up of stent implantation for residual aortic coarctation. Erosion of Amplatzer septal occluder device after closure of secundum atrial septal defects: review of registry of complications and recommendations to minimize future risk. Improved right ventricular function following late pulmonary valve replacement for residual pulmonary insufficiency or stenosis. Rotation angiogram in right ventricle following right pulmonary artery stent placement. Percutaneous pulmonary valvuloplasty in an octogenarian with calcific pulmonary stenosis. Effectiveness of percutaneous balloon valvuloplasty in adults with pulmonic valve stenosis. Late results of pulmonary balloon valvuloplasty in adults using double balloon technique. Percutaneous balloon valvuloplasty of the pulmonary valve: role of right to left shunting through a patent foramen ovale. Percutaneous balloon valvuloplasty for pulmonary stenosis in adolescents and adults. Outcomes for balloon pulmonary valvuloplasty in adults: comparison with a concurrent pediatric cohort. Intermediateterm outcome after pulmonary balloon valvuloplasty: comparison to a matched surgical control group. Long-term pulmonary regurgitation following balloon valvuloplasty for pulmonary stenosis. Long-term results of percutaneous balloon valvuloplasty in pulmonary valve stenosis in the pediatric population. Hemodynamic determinants of the peak systolic pressure gradient in children with valvar aortic stenosis. Balloon dilation of the aortic valve: studies in normal lambs and in children with aortic stenosis. Rapid ventricular pacing for catheter interventions in congenital aortic stenosis and coarctation: effectiveness, safety, and rate titration for optimal results. Carotid artery approach for balloon dilation of aortic valve stenosis in the neonate: a preliminary report. Follow-up results of balloon aortic valvuloplasty in children with special reference to causes of late aortic insufficiency. Percutaneous balloon valvuloplasty: a new method for treatment of congenital pulmonary-valve stenosis. Balloon angioplasty in the treatment of pulmonary valve stenosis and coarctation of the aorta. Percutaneous balloon valvotomy of congenital pulmonary stenosis using oversized balloons. Morphologic changes induced by dilation of the pulmonary valve annulus with overlarge balloons in normal newborn lambs. Percutaneous transluminal balloon valvuloplasty of congenital pulmonary valve stenosis, with a special report on infants and neonates. Critical pulmonary valve stenosis in patients less than 1 year of age: treatment with percutaneous gradational balloon pulmonary valvuloplasty. Determinants of successful balloon valvotomy in infants with critical pulmonary stenosis or membranous pulmonary atresia with intact ventricular septum. Balloon dilation of critical valvar pulmonary stenosis in the first month of life. Balloon pulmonary valvuloplasty: results of the valvuloplasty and angioplasty of congenital anomalies registry. Percutaneous balloon valvuloplasty for treatment of congenital pulmonary valvular stenosis in children. Immediate, short, intermediate and long-term results of balloon valvuloplasty in congenital pulmonary valve stenosis. Left heart growth, function, and reintervention after balloon aortic valvuloplasty for neonatal aortic stenosis. Balloon dilation of congenital aortic valve stenosis: results and influences of technical and morphological features on outcome. Balloon valvuloplasty for recurrent aortic stenosis after surgical valvotomy in childhood: immediate and follow-up studies. Balloon dilatation of congenital aortic valve stenosis in infants and children: short and intermediate term results. Independent predictors of immediate results of percutaneous balloon aortic valvotomy in childhood. Effectiveness of balloon valvuloplasty in the young adult with congenital aortic stenosis. Influence of balloon size on aortic regurgitation in neonates undergoing balloon aortic valvuloplasty: a retrospective study over an 11-year period. Aortic valve reinterventions after balloon aortic valvuloplasty for congenital aortic stenosis intermediate and late follow-up. Twenty-five year experience with balloon aortic valvuloplasty for congenital aortic stenosis. Aortic valve morphology is associated with outcomes following balloon valvuloplasty for congenital aortic stenosis. Balloon aortic valvoplasty in paediatric patients: progressive aortic regurgitation is common. Clinical and hemodynamic follow-up after percutaneous aortic valvuloplasty in the elderly. Early restenosis following successful percutaneous balloon valvuloplasty for calcific valvular aortic stenosis. Balloon dilation of calcific aortic stenosis in elderly patients: postmortem, intraoperative, and percutaneous valvuloplasty studies. Pathology of aortic valvuloplasty: findings after postmortem successful and failed dilatations. Balloon valvuloplasty versus transventricular dilation for neonatal critical aortic stenosis. Are outcomes of surgical versus transcatheter balloon valvotomy equivalent in neonatal critical aortic stenosis. Balloon dilation of severe aortic stenosis in the neonate: comparison of anterograde and 973. Intermediate-term effectiveness of balloon valvuloplasty for congenital aortic stenosis: a prospective follow-up study. Surgical valvuloplasty versus balloon aortic dilation for congenital aortic stenosis: are evidence-based outcomes relevant Repeat balloon aortic valvuloplasty effectively delays surgical intervention in children with recurrent aortic stenosis. Exercise function of children with congenital aortic stenosis following aortic valvuloplasty during early infancy.
Syndromes
- Take the drugs your doctor told you to take with a small sip of water.
- Bloating of the abdomen
- CT scans
- Heat the end of the paper clip over an open flame until it is red hot. Use a pair of pliers to hold the paper clip. While it is still very hot, touch the tip of the paper clip to the injured fingernail. Touch the nail over where the blood is collected. This is not a painful procedure for most people.The heat of the clip will burn a small hole in the fingernail. It is not necessary to press hard on the fingernail to burn the hole.
- Brain tumor or other growth (mass)
- You have had life-threatening bouts of ventricular tachycardia (VT) or ventricular fibrillation (VF).
- Bloating
- Separation from parents (perceived abandonment)
- Scaling
- A child between 3 months and 1 year has a fever that lasts more than 24 hours.
Order discount phenytoin line
Hemolysis is extravascular and is mediated by macrophages predominantly in the spleen medicine to increase appetite order phenytoin visa. Several authors have suggested that all drug-induced immune hemolysis is explained by a single mechanism, known as the unifying theory. The antibodies activate complement and trigger acute intravascular hemolysis that may progress to renal failure. Hemolysis is extravascular, mediated by macrophages predominantly in the spleen, usually with a gradual onset of anemia. Anemia varies from mild to severe, and characteristic morphologic features on the peripheral blood film are polychromasia and spherocytes. The most important finding in the diagnostic investigation of a suspected autoimmune hemolytic anemia is: a. It is due to an anamnestic response after repeat exposure to a blood group antigen d. A 63-year-old man is being evaluated because of a decrease in hemoglobin of 5 g/dL after a second cycle of fludarabine for treatment of chronic lymphocytic leukemia. Classification and therapeutic approaches in autoimmune hemolytic anemia: an update. Treatment options for primary autoimmune hemolytic anemia: a short comprehensive review. Efficacy and safety of rituximab in autoimmune hemolytic anemia: a metaanalysis of 21 studies. Primary chronic cold agglutinin disease: an update on pathogenesis, clinical features and therapy. Primary chronic cold agglutinin disease: a population based clinical study of 86 patients. High response rate and durable remissions following fludarabine and rituximab combination therapy for chronic cold agglutinin disease. A case study of a child with chronic hemolytic anemia due to a Donath-Landsteiner positive, IgM anti-I autoantibody. Autoimmune haemolysis: an 18 year study of 865 cases referred to a regional transfusion centre. Mixed-type autoimmune hemolytic anemia: differential diagnosis and critical review of reported cases. Techniques of intrauterine fetal transfusion for women with red-cell isoimmunisation for improving health outcomes. Anti-Ge3 causes late-onset hemolytic disease of the newborn: the fourth case in three Hispanic families. Prolonged anemia in an intrauterine-transfused neonate with Rh-negative hemolytic disease: no evidence for anti-D-related suppression of erythropoiesis in vitro. Exchange transfusion of least incompatible blood for severe hemolytic disease of the newborn due to anti-Rh17. Drugs that have been shown to cause drug-induced immune hemolytic anemia or positive direct antiglobulin tests: some interesting findings since 2007. Trimethoprim-induced immune hemolytic anemia in a pediatric oncology patient presenting as an acute hemolytic transfusion reaction. Positive direct and indirect antiglobulin tests associated with oxaliplatin can be due to drug antibody and/or drug-induced nonimmunologic protein adsorption. Select confirmatory tests that should be performed and describe the expected results. Describe the characteristic red blood cell morphology on the peripheral blood film. Based on the electrophoresis and red blood cell morphology results, what diagnosis is suggested Hemoglobinopathy refers to a disease state (opathy) involving the hemoglobin (Hb) molecule. The genes that are mutated can code for either proteins that make up the hemoglobin molecule (globin or polypeptide chains) or proteins involved in synthesizing or regulating synthesis of the globin chains. Regardless of the mutation encountered, all hemoglobinopathies affect hemoglobin synthesis in one of two ways: qualitatively or quantitatively. In qualitative hemoglobinopathies, hemoglobin synthesis occurs at a normal or near-normal rate, but the hemoglobin molecule has an altered amino acid sequence within the globin chains. This change in amino acid sequence can alter the structure of the hemoglobin molecule (structural defect) and its function (qualitative defect). In contrast, thalassemias result in a reduced rate of hemoglobin synthesis (quantitative) but do not affect the amino acid sequence of the affected globin chains. A reduction in the amount of hemoglobin synthesized produces an anemia and stimulates the production of other hemoglobins not affected by the mutation in an attempt to compensate for the anemia. Based on this distinction, hematologists divide hemoglobinopathies into two categories: structural defects (qualitative) and thalassemias (quantitative). To add confusion to the classification scheme, many hematologists also refer to only the structural defects as hemoglobinopathies. This article describes the structural or qualitative defects that are referred to as hemoglobinopathies; the quantitative defects (thalassemias) are described in Chapter 25. Two of the globin genes, a and z, are located on chromosome 16 and are referred to as a-like genes. The remaining four globin genes, b, g, d, and e, are located on chromosome 11 and are referred to as b-like genes. In the human genome there is one copy of each globin gene per chromatid, for a total of two genes per diploid nucleus, with the exception of a and g. There are two copies of the a and g genes per chromatid, for a total of four genes per diploid nucleus. During the first 3 months of embryonic life, only one a-like gene (z) and one b-like gene (e) are activated, which results in the production of z- and e-globin chains that pair to form hemoglobin Gower-1 (z2e2). Shortly thereafter, a and g chain synthesis begins, which leads to the production of Hb Gower-2 (a2e2) and Hb Portland (z2g2). Later in fetal development, z and e synthesis ceases; this leaves a and g chains, which pair to produce Hb F (a2g2), also known as fetal hemoglobin. During the 6 months after birth, g chain synthesis gradually decreases and is replaced by b chain synthesis so that Hb A (a2b2), also known as adult hemoglobin, is produced. Some of these changes alter the molecular structure of the hemoglobin molecule, ultimately affecting hemoglobin function. The types of genetic mutations that occur in the hemoglobinopathies include point mutations, deletions, insertions, and fusions involving one or more of the adult globin genes, namely, a, b, g, and d. Point mutation is the replacement of one original nucleotide in the normal gene with a different nucleotide. Because one nucleotide is replaced by one nucleotide, the codon triplet remains intact, and the reading frame is unaltered. This results in the substitution of one amino acid in the globin chain product at the position corresponding to the codon containing the point mutation. It also is possible to have two point mutations occurring in the same globin gene, which results in two amino acid substitutions within the same globin chain. Usually deletions and insertions are not divisible by three and disrupt the reading frame, which leads to the nullification of synthesis of the corresponding globin chain. In hemoglobinopathies, the reading frame usually remains intact, however; the result is the addition or deletion of one or more amino acids in the globin chain product, which sometimes affects the structure and function of the hemoglobin molecule. Significant globin chain extensions usually result in degradation of the globin chain and a quantitative defect. If the extension of the globin chain is insufficient to produce significant degradation, however, the defect is qualitative and is classified as a hemoglobinopathy. Hemoglobin molecules with extended globin chains fold inappropriately, which affects hemoglobin structure and function. Gene fusions occur when two normal genes break between nucleotides, switch positions, and anneal to the opposite gene. For example, if a b-globin gene and a d-globin gene break in similar locations, switch positions, and reanneal, the resultant genes would be bd and db fusion genes in which the head of the fusion gene is from one original gene and the tail is from the other. The fusion chains fold differently, however, and affect the corresponding hemoglobin function. Generally there is a level of severity associated with each normal gene that is mutated and used to synthesize the globin chain product. For the normal adult globin genes, there are four copies of the a and g genes and two copies of the b and d genes.
Generic phenytoin 100 mg on-line
Successful stenting in infants with complex aortic arch obstruction after the Norwood operation for hypoplastic left heart syndrome has also been described medications used for adhd order phenytoin now. In particular, aortic wall injury was significantly greater on follow-up imaging in the angioplasty group (21. Stent patients were more likely to require a planned reintervention, primarily for stent redilation as part of a staged approach or secondary to patient somatic growth. There was no difference in unplanned reinterventions between the treatment groups. Although these results must be interpreted with some caution given the nonrandomized nature of the study, the findings suggest that stent therapy may be the lowest-risk intervention available to this patient population. The authors identified an increased risk of aortic wall pathology in follow-up if the ratio of balloon diameter to coarctation diameter exceeded 3. Patients identified as high risk included those with a nearly atretic descending aorta, genetic syndromes associated with aortic wall weakening, or advanced age of 60 years or older. The remaining patients had minor endoleaks which did not require additional intervention. Serious adverse events occurred in 8% with access site complications occurring most frequently. Data on long-term outcomes of stent implantation for aortic coarctation are limited, with the longest reported follow-up being 15 years. Recoarctation occurred as a result of neointimal hyperplasia, somatic growth, or stent fracture. Three of 15 of these patients underwent staged redilation due to the severity of the initial lesion, and this may have contributed to the earlier time at reintervention in this group. Independent risk factors for reintervention included complex lesions, use of a balloon smaller than 14 mm in diameter for initial stent delivery, and an immediate poststent residual gradient of more than 10 mm Hg. Stent fracture was more common in the bare-metal group (5%), and the majority of these patients required reintervention due to restenosis. Somatic growth as a cause of reintervention was significantly associated with age younger than 15 years and use of a balloon diameter smaller than 14 mm at initial stent implantation. Another long-term issue with patients after coarctation repair is systemic hypertension. Many studies have found that patients with coarctation continue to exhibit elevated blood pressure after their initial intervention or develop hypertension over time, even in the setting of a good anatomic result of intervention. Twenty-three percent of patients continued to have systolic blood pressure greater than the 95th percentile, 9% had an upper-to-lower limb blood pressure gradient greater than 20 mm Hg, and 32% were taking antihypertensive medications. Sinus venosus defects result from abnormal development of either the superior or inferior horns of the sinus venosus and are located superiorly or inferiorly along the posterior margin of the atrial septum. Superior sinus venosus defects frequently have associated anomalous drainage of the right upper pulmonary vein. These defects, usually in the region of the fossa ovalis, may be extensive in size, varied in shape, and often multiple in number (fenestrated atrial septum). It is secundum type defects, often with substantial peridefect margins and positioned some distance from other vital structures, that lend themselves well to percutaneous device closure. With persistence of atrial level shunting, the right atrial and ventricular end-diastolic volumes are chronically increased, and both atrial and ventricular dimensions increase accordingly. Ultimately, Eisenmenger type physiology will prevail, at which point shunt flow will be right to left, and the patient will become cyanotic. Conclusions and Recommendations Coarctation stenting is an effective approach to native and postoperative recurrent coarctation of the aorta. Most pediatric interventionalists limit stent implantation for coarctation to large children and adolescents to avoid the need for aortic stent redilation after somatic growth in a smaller child. Stent implantation is a promising intervention for more difficult variations on coarctation anatomy, particularly transverse arch hypoplasia, arch obstruction after the Norwood operation, and mild degrees of coarctation that have not warranted surgery in the past. In older adults in whom the aortic wall is friable, covered stents may provide a safer alternative because of the increased risk of aortic wall injury with coarctation dilation. Longer-term follow-up studies are necessary to more precisely define the late risks of stent restenosis, aortic aneurysm formation, the safety of late stent redilation after somatic growth in children, and blood pressure response to exercise in the face of a rigid, stented aortic segment. Diagnosis is most often made after detection of a murmur, indistinguishable from that of pulmonary valve stenosis, or with auscultation of a fixed split-second heart sound. The exact position of the defect is determined by the specific area that fails to develop and is traditionally described in anatomic terms. In short-axis views, that dilation may again be noted, especially in the region of the infundibulum. These views allow for complete evaluation of the total septal length and provide excellent visualization of the defect margins. This is more likely in the adult patient, in the presence of obesity, or with chronic lung disease. After deployment, both devices are designed to have two discs separated by a central core or waist. One disc is positioned on the left atrial side of the defect, with the core or waist straddling the defect, and the other disc opposed to the atrial membrane from the right atrial side of the atrial septum. The devices have intrinsic recoil that opposes both discs to each other, holding the devices in place on the atrial septum. However, most operators continue to rely on balloon sizing of the defect before choosing a particular sized device. As soon as color flow across the defect is arrested, no further inflation occurs, and an angiographic measurement of that balloon waist size is used to choose the appropriately sized closure device. The left atrial disc is initially deployed and the device retracted back onto the atrial septum with both fluoroscopic and echocardiographic guidance. The remainder of the device is then deployed within the right atrium, so that the waist or core of the device straddles the defect. To ensure adequate device deployment, echocardiographic imaging is used in addition to fluoroscopy. Whichever echocardiographic modality is used, it is imperative to ensure that atrial septal tissue is noted to be present between the left and right atrial device discs in all different plains to ensure proper and safe device deployment prior to release from the delivery cable. In this photograph, the tethering cable, covered by the delivery sheath, remains attached to the device. Closure rates are comparable to surgery over similar time periods (97% to 99% at 12 months), but procedural morbidity is considerably lower. However, fluoroscopy times are typically brief, and low dose adjustments can be used. The risk of device embolization is also small and, in most cases, related to operator inexperience. Thrombus formation on the device, with distal embolization is of great concern, justifying the recommendation for aspirin therapy until device endothelialization has occurred. In addition, oversizing of the device or placement of a device that is too large to be accommodated by the total septal length could cause part of the superior margin of the left atrial disc to abut against the roof of the left atrium. Continuous rocking motion of the device against either the aorta or the atrial wall may result in erosion. If any of these findings become apparent either during device deployment or after complete deployment, the device should be withdrawn, and attempts to reposition or resize the device should be made. The device is composed of a nickeltitanium wire with a patch of microporous expanded polytetrafluoroethylene attached along its length. The elastic properties of the wire form the device into two equal-size opposing disks that reside on either side of the atrial septum after deployment, thus occluding the defect. The indentations on the balloon (white arrows) indicate the stretched margin of the atrial septal defect. That diameter is measured, and an appropriately sized septal occluder is chosen accordingly. After device implantation, patients should remain on aspirin for at least 6 months, during which time complete device endothelialization occurs. Bacterial endocarditis prophylaxis prophylaxis is also recommended during that period and should be continued if residual atrial level shunting is apparent at the time of the 6-month echocardiogram. After that, follow-up should be at least on an annual basis, with echocardiography obtained during those visits. The right atrial and ventricular dimensions return to normal within 6 months if no significant atrial level shunting remains. Although some degree of anatomic variation does occur (such as with a right aortic arch, when the ductus arises from the base of the left innominate artery), the relationship is generally consistent. At birth, with an increase in arterial oxygen content and a decrease in circulating prostaglandins, the ductus arteriosus spasms and later becomes fibrotic with permanent closure. This occurs usually by 5 to 7 days in full-term infants but may not occur until 3 weeks.
100mg phenytoin with amex
Platelets rapidly adhere to the surfaces of damaged blood vessels medications bad for your liver order 100mg phenytoin otc, form aggregates with neighboring platelets to plug the vessels, and secrete proteins and small molecules that trigger thrombosis, or clot formation. Platelets are the major cells that control hemostasis, a series of cellular and plasma-based mechanisms that seal wounds, repair vessel walls, and maintain vascular patency (unimpeded blood flow) (Chapter 35). Their small size makes them appear insignificant, but they are essential to life and are extensively studied for their complex physiology. Uncontrolled platelet and hemostatic activation is responsible for deep vein thrombosis, pulmonary emboli, acute myocardial infarctions (heart attacks), cerebrovascular accidents (strokes), peripheral artery disease, and repeated spontaneous abortions (miscarriages) (Chapter 39). Owing to their small volume, platelets are hard to distinguish visually in a hemacytometer, and phase microscopy provides for easier identification. Automated blood cell analyzers have largely replaced visual platelet counting and provide greater accuracy (Chapter 12). The specimen must be tested or prepared for storage within the appropriate time frame to ensure accurate analysis (Chapter 2) and must be accurately registered in the work list, a process known as specimen accession. Accession may be automated, relying on bar code or radiofrequency identification technology, thus reducing instances of identification error. When one of the results from the blood cell analyzer is abnormal, the instrument provides an indication of this, sometimes called a flag. However, physicians may request a blood film examination on the basis of clinical suspicion even when the analyzer results fall within their respective reference intervals. Increasingly refined laboratory methods are becoming available to assay and characterize the secretions of these important cells. Platelets are a key component of hemostasis, as previously described; plasma coagulation is the second component (Chapter 35). The coagulation system employs a complex sequence of plasma proteins, some enzymes, and some enzyme cofactors to produce clot formation after blood vessel injury. Another six to eight enzymes exert control over the coagulation mechanism, and a third system of enzymes and cofactors digests clots to restore vessel patency, a process called fibrinolysis. Bleeding (Chapters 36 to 38) and clotting (Chapter 39) disorders are numerous and complex, and the coagulation section of the hematology laboratory provides a series of plasma-based and whole blood laboratory assays that assess these plasma proteins and their interactions with hematologic cells. The medical laboratory professional focuses especially on blood specimen integrity for the coagulation laboratory, because minor blood specimen defects, including clots, hemolysis, lipemia, plasma bilirubin, and short draws, render the specimen useless (Chapter 41). The prothrombin time and partial thromboplastin time are particularly high-volume assays used in screening profiles. These tests assess each portion of the coagulation pathway for deficiencies and are used to monitor anticoagulant therapy (Chapter 40). Another 30 to 40 moderate-volume assays, mostly clot-based, are available in specialized or tertiary care facilities. The specialized or tertiary care coagulation laboratory with its interpretive complexities attracts advanced medical laboratory scientists with specialized knowledge and communication skills. Medical laboratory professionals pride themselves on their technical and analytical skills in performing the blood film examination and differential count. Performing these tests may require advanced preparation or particular dedication by medical laboratory scientists with a desire to specialize. Bone marrow aspirates and biopsy specimens are collected and stained to analyze nucleated cells that are the immature precursors to blood cells (Chapter 4). Medical laboratory scientists, clinical pathologists, and hematologists review Wright-stained aspirate smears for morphologic abnormalities, high or low bone marrow cell concentration, and inappropriate cell line distributions. The biopsy specimen, enhanced by hematoxylin and eosin (H&E) staining, may reveal abnormalities in bone marrow architecture indicating leukemia, bone marrow failure, or one of a host of additional hematologic disorders. In the bone marrow laboratory, cytochemical stains may occasionally be employed to differentiate abnormal myeloid, erythroid, and lymphoid cells. These stains include myeloperoxidase, Sudan black B, nonspecific and specific esterase, periodic acid-Schiff, tartrate-resistant acid phosphatase, and alkaline phosphatase (Chapters 31 and 32). The cytochemical stains are time-honored tests that in most laboratories have been replaced by flow cytometry immunophenotyping, molecular diagnostic, and cytogenetic techniques (Chapters 28 to 30). Since 1980, however, immunostaining methods have enabled identification of cell lines by detecting lineage-specific antigens on the surface or in the cytoplasm of leukemia and lymphoma cells. Flow cytometers may be quantitative, such as clinical flow cytometers that have grown from the original Coulter principle, or qualitative, including laser-based instruments that have migrated from research applications to the clinical laboratory (Chapters 12 and 28). Qualitative laser-based flow cytometers are mechanically simpler but technically more demanding. Both qualitative and quantitative flow cytometers are employed to analyze cell populations by measuring the effects of individual cells on laser light, such as forward-angle fluorescent light scatter and right-angle fluorescent light scatter, and by immunophenotyping for cell membrane epitopes using monoclonal antibodies labeled with fluorescent dyes. The qualitative flow cytometry laboratory is indispensable to leukemia and lymphoma diagnosis. Cytogenetics (Chapter 30), a time-honored form of chromosome analysis, is employed in bone marrow aspirate examination to find gross genetic errors such as the Philadelphia chromosome, a reciprocal translocation between chromosomes 9 and 22 that is diagnostic in chronic myeloid leukemia, and t(15;17), a translocation between chromosomes 15 and 17 diagnostic in acute promyelocytic leukemia. Cytogenetic analysis remains essential to the diagnosis and treatment of leukemia. Molecular diagnostic techniques (Chapter 29), the fastestgrowing area of laboratory medicine, enhance and even replace some of the advanced hematologic methods. The sickle cell solubility screening assay and its follow-up tests, hemoglobin electrophoresis and high-performance liquid chromatography, are used to detect and diagnose sickle cell anemia and other inherited qualitative hemoglobin abnormalities and thalassemias (Chapters 24 and 25). One of the oldest hematology tests, the erythrocyte sedimentation rate, detects inflammation and roughly estimates its intensity (Chapter 11). Finally, the medical laboratory professional reviews the cellular counts, distribution, and morphology in body fluids other than blood (Chapter 15). Analysis of nonblood body fluids is always performed with a rapid turnaround, because cells in these environments rapidly lose their integrity. Because of the unavailability of weighed standards, the measurement of cells and biological systems defies chemical standardization and requires elaborate calibration, validation, matrix effect examination, linearity, and reference interval determinations. An internal standard methodology known as the moving average also supports hematology laboratory applications. As in most branches of laboratory science, the hematology laboratory places an enormous responsibility for accuracy, integrity, judgment, and timeliness on the medical laboratory professional. Observations on the use of the Coulter model D electronic cell counter in clinical haematology. Spectrophotometric determination of hemoglobin oxygen saturation: the method of Drabkin & Schmidt as modified for its use in clinical routine analysis. Describe the procedures to validate and document a new or modified laboratory assay. Compare a new or modified assay to a reference using statistical tests to establish accuracy. Select appropriate statistical tests for a given application and interpret the results. Define and compute precision using standard deviation and coefficient of variation. Describe a quality assurance plan to control for preanalytical and postanalytical variables. Can you continue to analyze specimens as long as you subtract 2 g/dL from the results What aspect of the assay should you first investigate in troubleshooting this problem Inform physician about laboratory test availability and ways to avoid unnecessary orders. Is adequate diagnostic, treatment, and patient preparation information provided to assist the laboratory staff to appropriately test and interpret results Do turnaround time expectations match clinical necessity and ensure that stat orders are reserved for medical emergencies Is the patient correctly identified, prepared, and available for specimen collection Test request forms In medical laboratory science, quality implies the ability to provide accurate, reproducible assay results that offer clinically useful information. Of the terms quality control and quality assurance, quality assurance is the broader concept, encompassing preanalytical, analytical, and postanalytical variables (Box 2. Quality assurance further encompasses laboratory assay utilization and physician test ordering patterns, nicknamed "pre-pre" analytical variables, and the appropriate application of laboratory assay results, sometimes called "postpost" analytical variables. Does the laboratory staff conduct in-service education to support test result interpretation