Discount 200mg viramune otc
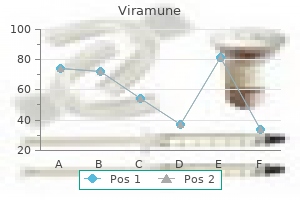
For example treatment group cheap 200 mg viramune free shipping, when a person becomes excited for any reason or during states of anxiety, the sympathetic system becomes excessively stimulated, peripheral vasoconstriction occurs everywhere in the body, and acute hypertension ensues. Another type of acute neurogenic hypertension occurs when the nerves leading from the baroreceptors are cut or when the tractus solitarius is destroyed in each side of the medulla oblongata. These are the areas where the nerves from the carotid and aortic baroreceptors connect in the brain stem. The sudden cessation of normal nerve signals from the baroreceptors has the same effect on the nervous pressure control mechanisms as a sudden reduction of the arterial pressure in the aorta and carotid arteries. That is, loss of the normal inhibitory effect on the vasomotor center caused by normal baroreceptor nervous signals allows the vasomotor center suddenly to become extremely active and the mean arterial pressure to increase from 100 mm Hg to as high as 160 mm Hg. The pressure returns to nearly normal within about 2 days because the response of the vasomotor center to the absent baroreceptor signal fades away, which is called central resetting of the baroreceptor pressure control mechanism. Therefore, the neurogenic hypertension caused by sectioning the baroreceptor nerves is mainly an acute type of hypertension, not a chronic type. The sympathetic nervous system also plays an important role in some forms of chronic hypertension, in large part by activation of the renal sympathetic nerves. For example, excess weight gain and obesity often lead to activation of the sympathetic nervous system, which in turn stimulates the renal sympathetic nerves, impairs renal pressure natriuresis, and causes chronic hypertension. These abnormalities appear to play a major role in a large percentage of patients with primary (essential) hypertension, as discussed later. Spontaneous hereditary hypertension has been observed in several strains of animals, including different strains of rats and rabbits and at least one strain of dogs. In the strain of rats that has been studied to the greatest extent, the Okamoto spontaneously hypertensive rat, there is evidence that in early development of the hypertension, the sympathetic nervous system is considerably more active than in normal rats. In the later stages of this type of hypertension, structural changes have been observed in the nephrons of the kidneys: (1) increased preglomerular renal arterial resistance; and (2) decreased permeability of the glomerular membranes. These structural changes could also contribute to the long-term continuance of the hypertension. In other strains of hypertensive rats, impaired renal function also has been observed. In humans, several different gene mutations have been identified that can cause hypertension. These forms of hypertension are called monogenic hypertension because they are caused by mutation of a single gene. An interesting feature of these genetic disorders is that they all cause impaired kidney function, either by increased resistance of the renal arterioles or by excessive salt and water reabsorption by the renal tubules. In some cases, the increased reabsorption is due to gene mutations that directly increase the transport of sodium or chloride in the renal tubular epithelial cells. In other cases, the gene mutations cause increased synthesis or activity of hormones that stimulate renal tubular salt and water reabsorption. Thus, in all monogenic hypertensive disorders discovered thus far, the final common pathway to hypertension appears to be impaired kidney function. Monogenic hypertension, however, is rare, and all the known forms together account for less than 1% of cases of human hypertension. These terms simply mean that the hypertension is of unknown origin, in contrast to the forms of hypertension that are secondary to known causes, such as renal artery stenosis or monogenic forms of hypertension. In most patients, excess weight gain and a sedentary lifestyle appear to play a major role in causing primary hypertension. Most patients with hypertension are overweight, and studies of different populations have suggested that excess adiposity may account for as much as 65% to 75% of the risk for developing primary hypertension. Clinical studies have clearly shown the value of weight loss for reducing blood pressure in most patients with hypertension, and clinical guidelines for treating hypertension recommend increased physical activity and weight loss as a first step in treating most patients with hypertension. The following characteristics of primary hypertension, among others, are caused by excess weight gain and obesity: 1. Cardiac output is increased in part because of the additional blood flow required for the extra adipose tissue. However, blood flow in the heart, kidneys, gastrointestinal tract, and skeletal muscle also increases with weight gain because of increased metabolic rate and growth of the organs and tissues in response to their increased metabolic demands. Sympathetic nerve activity, especially in the kidneys, is increased in overweight patients. The causes of increased sympathetic activity in obese persons are not fully understood, but studies have suggested that hormones such as leptin that are released from fat cells may directly stimulate multiple regions of the hypothalamus, which in turn have an excitatory influence on the vasomotor centers of the brain medulla. There is also evidence for reduced sensitivity of arterial baroreceptors in buffering increases in arterial pressure, as well as activation of chemoreceptors in obese persons, especially in those who also have obstructive sleep apnea. The renal-pressure natriuresis mechanism is impaired, and the kidneys will not excrete adequate amounts of salt and water unless the arterial pressure is high or kidney function is somehow improved. If mean arterial pressure in the essential hypertensive person is 150 mm Hg, acute reduction of mean arterial pressure to the normal value of 100 mm Hg (but without otherwise altering renal function except for the decreased pressure) will cause almost total anuria. The person will then retain salt and water until the pressure rises back to the elevated value of 150 mm Hg. Chronic reductions in arterial pressure with effective antihypertensive therapies, however, usually do not cause marked salt and water retention by the kidneys because these therapies also improve renal pressure natriuresis, as discussed later. However, if hypertension is not effectively treated, there may also be vascular damage in the kidneys that can reduce glomerular filtration rate and increase the severity of hypertension. Eventually, uncontrolled hypertension associated with obesity and associated metabolic disorders can lead to severe vascular injury and complete loss of kidney function. Analysis of arterial pressure regulation in (1) saltinsensitive essential hypertension and (2) salt-sensitive essential hypertension. The curves of this figure are called 242 sodium-loading renal function curves because the arterial pressure in each case is increased very slowly, over many days or weeks, by gradually increasing the level of sodium intake. The sodium-loading type of curve can be determined by increasing the level of sodium intake to a new level every few days and then waiting for the renal output of sodium to come into balance with the intake and, at the same time, recording the changes in arterial pressure. Note in both cases that the curves are shifted to the right, to a higher pressure level than for people with normal arterial pressure. In the case of the person with salt-insensitive essential hypertension, the arterial pressure does not increase significantly when changing from a normal salt intake to a high salt intake. However, in patients who have salt-sensitive essential hypertension, the high salt intake significantly exacerbates the hypertension. First, salt sensitivity of blood pressure is not an all-or-none finding-it is quantitative, with some individuals being more salt-sensitive than others. Second, salt sensitivity of blood pressure is not a fixed characteristic; instead, blood pressure usually becomes more salt sensitive as a person ages, especially after 50 or 60 years of age, when the number of functions units (nephrons) in the kidneys begins to decrease gradually. The reason for the difference between salt-insensitive essential hypertension and salt-sensitive hypertension is presumably related to structural or functional differences in the kidneys of these two types of hypertensive patients. For example, salt-sensitive hypertension may occur with different types of chronic renal disease because of the Chapter 19 Role of the Kidneys in Long-Term Control of Arterial Pressure and in Hypertension Maximum feedback gain at optimal pressure Acute change in pressure at this time Treatment of Essential Hypertension. As a first step, current guidelines for treating hypertension recommend lifestyle modifications aimed at increasing physical activity and weight loss in most patients. Unfortunately, many patients are unable to lose weight, and pharmacological treatment with antihypertensive drugs must be initiated. Two general classes of drugs are used to treat hypertension: (1) vasodilator drugs, which increase renal blood flow and glomerular filtration rate; and (2) natriuretic or diuretic drugs, which decrease tubular reabsorption of salt and water. Vasodilator drugs usually cause vasodilation in many other tissues of the body, as well as in the kidneys. Different vasodilators act in one of the following ways: (1) by inhibiting sympathetic nervous signals to the kidneys or by blocking the action of the sympathetic transmitter substance on the renal vasculature and renal tubules; (2) by directly relaxing the smooth muscle of the renal vasculature; or (3) by blocking the action of the reninangiotensin-aldosterone system on the renal vasculature or renal tubules. Drugs that reduce the reabsorption of salt and water by the renal tubules include, in particular, drugs that block active transport of sodium through the tubular wall; this blockage in turn also prevents the reabsorption of water, as explained earlier in the chapter. These natriuretic or diuretic drugs are discussed in greater detail in Chapter 32. Abnormal function of the renin-angiotensin system can also cause arterial pressure to become salt-sensitive, as discussed previously in this chapter. Approximate potency of various arterial pressure control mechanisms at different time intervals after the onset of a disturbance to the arterial pressure. These mechanisms can be divided into three groups: (1) those that react rapidly, within seconds or minutes; (2) those that respond over an intermediate time period-that is, minutes or hours; and (3) those that provide long-term arterial pressure regulation for days, months, and years. For example, when a person bleeds so severely that the pressure falls suddenly, two problems confront the pressure control system. The first is survival; the arterial pressure must be rapidly returned to a high enough level that the person can live through the acute episode.
Purchase viramune on line amex
Therefore symptoms 0f ovarian cancer cheap viramune 200 mg online, they play key roles in causing airway obstruction in allergic asthma; this is especially true of the slow reactive substance of anaphylaxis. The same irritants that cause parasympathetic constrictor reflexes of the airways-smoke, dust, sulfur dioxide, and some of the acidic elements in smog-may also act directly on the lung tissues to initiate local, non-nervous reactions that cause obstructive constriction of the airways. Direct All the respiratory passages, from the nose to the terminal bronchioles, are kept moist by a layer of mucus that coats the entire surface. The mucus is secreted partly by individual mucous goblet cells in the epithelial lining of the passages and partly by small submucosal glands. In addition to keeping the surfaces moist, the mucus traps small particles out of the inspired air and keeps most of these particles from ever reaching the alveoli. The entire surface of the respiratory passages, in the nose and the lower passages, down as far as the terminal bronchioles, is lined with ciliated epithelium, with about 200 cilia on each epithelial cell. These cilia beat continually at a rate of 10 to 20 times/sec by the mechanism explained in Chapter 2, and the direction of their "power stroke" is always toward the pharynx. That is, the cilia in the lungs beat upward, whereas those in the nose beat downward. This continual beating causes the coat of mucus to flow slowly, at a velocity of a few millimeters per minute, toward the pharynx. Then the mucus and its entrapped particles are swallowed or coughed to the exterior. Cough Reflex A few parasympathetic nerve fibers derived from the vagus nerves penetrate the lung parenchyma. These nerves secrete acetylcholine and, when activated, cause mild to moderate constriction of the bronchioles. When a disease process such as asthma has already caused some bronchiolar constriction, superimposed parasympathetic nervous stimulation often worsens the condition. When this situation occurs, administration of drugs that block the effects of acetylcholine, such as atropine, can sometimes relax the respiratory passages enough to relieve the obstruction. Sometimes the parasympathetic nerves are also activated by reflexes that originate in the lungs. Most of these reflexes begin with irritation of the epithelial membrane of the respiratory passageways, initiated by noxious gases, dust, cigarette smoke, or bronchial infection. Also, a bronchiolar constrictor reflex often occurs when microemboli occlude small pulmonary arteries. The bronchi and trachea are so sensitive to light touch that slight amounts of foreign matter or other causes of irritation initiate the cough reflex. The larynx and carina (the point where the trachea divides into the bronchi) are especially sensitive, and the terminal bronchioles and even the alveoli are sensitive to corrosive chemical stimuli such as sulfur dioxide gas or chlorine gas. Afferent nerve impulses pass from the respiratory passages mainly through the vagus nerves to the medulla of the brain. There, an automatic sequence of events is triggered by the neuronal circuits of the medulla, causing the following effects. The epiglottis closes, and the vocal cords shut tightly to entrap the air within the lungs. The abdominal muscles contract forcefully, pushing against the diaphragm while other expiratory muscles, such as the internal intercostals, also contract forcefully. Consequently, the pressure in the lungs rises rapidly, to as much as 100 mm Hg or more. The vocal cords and epiglottis suddenly open widely, so that air under this high pressure in the lungs explodes outward. Almost none of these particles are precipitated in the respiratory passageways before they reach the alveoli. Unfortunately, up to one-third of them do precipitate in the alveoli by the diffusion process, with the balance remaining suspended and expelled in the expired air. Many of the particles that become entrapped in the alveoli are removed by alveolar macrophages, as explained in Chapter 34, and others are carried away by the lung lymphatics. An excess of particles can cause growth of fibrous tissue in the alveolar septa, leading to permanent debility. Vocalization Importantly, the strong compression of the lungs collapses the bronchi and trachea by causing their noncartilaginous parts to invaginate inward, so the exploding air actually passes through bronchial and tracheal slits. The rapidly moving air usually carries with it any foreign matter that is present in the bronchi or trachea. Sneeze Reflex the sneeze reflex is very much like the cough reflex, except that it applies to the nasal passageways instead of the lower respiratory passages. The initiating stimulus of the sneeze reflex is irritation in the nasal passageways; the afferent impulses pass in the fifth cranial nerve to the medulla, where the reflex is triggered. A series of reactions similar to those for the cough reflex takes place, but the uvula is depressed, so large amounts of air pass rapidly through the nose, thus helping clear the nasal passages of foreign matter. These functions together are called the air-conditioning function of the upper respiratory passageways. When a person breathes air through a tube directly into the trachea (as through a tracheostomy), the cooling and especially the drying effect in the lower lung can lead to serious lung crusting and infection. The hairs at the entrance to the nostrils are important for filtering out large particles. Much more important, though, is the removal of particles by turbulent precipitation. That is, the air passing through the nasal passageways hits many obstructing vanes-the conchae (also called turbinates, because they cause turbulence of the air), the septum, and the pharyngeal wall. Each time air hits one of these obstructions, it must change its direction of movement. The particles suspended in the air, having far more mass and momentum than air, cannot change their direction of travel as rapidly as the air can. Therefore, they continue forward, striking the surfaces of the obstructions, and are entrapped in the mucous coating and transported by the cilia to the pharynx to be swallowed. The nasal turbulence mechanism for removing particles from air is so effective that almost no particles larger than 6 micrometers in diameter enter the lungs through the nose. Of the remaining particles, many that are between 1 and 5 micrometers settle in the smaller bronchioles as a result of gravitational precipitation. For example, terminal bronchiolar disease is common in coal miners because of settled dust particles. Some of the still smaller particles (<1 micrometer in diameter) diffuse against the walls of the alveoli and adhere to the alveolar fluid. For Speech involves not only the respiratory system but also the following: (1) specific speech nervous control centers in the cerebral cortex, discussed in Chapter 58; (2) respiratory control centers of the brain; and (3) the articulation and resonance structures of mouth and nasal cavities. Speech is composed of two mechanical functions: (1) phonation, which is achieved by the larynx; and (2) articulation, which is achieved by the structures of the mouth. The vocal cords protrude from the lateral walls of the larynx toward the center of the glottis; they are stretched and positioned by several specific muscles of the larynx itself. During phonation, the cords move together so that passage of air between them will cause vibration. The pitch of the vibration is determined mainly by the degree of stretch of the cords, but also by how tightly the cords are approximated to one another and by the mass of their edges. Immediately inside each cord is a strong elastic ligament called the vocal ligament. Posteriorly, the vocal ligament is attached to the vocal processes of two arytenoid cartilages. The vocal cords can be stretched by forward rotation of the thyroid cartilage or posterior rotation of the arytenoid cartilages, activated by muscles stretching from the thyroid cartilage and arytenoid cartilages to the cricoid cartilage. Muscles located in the vocal cords lateral to the vocal ligaments, the thyroarytenoid muscles, can pull the arytenoid cartilages toward the thyroid cartilage and, therefore, loosen the vocal cords. Also, slips of these muscles in the vocal cords can change the shapes and masses of the vocal cord edges, sharpening them to emit high-pitched sounds and blunting them for the more bass sounds. B, Laryngeal function in phonation, showing the positions of the vocal cords during different types of phonation. They need not be discussed in detail here because we are all familiar with their movements during speech and other vocalizations. The resonators include the mouth, the nose and associated nasal sinuses, the pharynx, and even the chest cavity. For example, the function of the nasal resonators is demonstrated by the change in voice quality when a person has a severe cold that blocks the air passages to these resonators.
| Comparative prices of Viramune | ||
| # | Retailer | Average price |
| 1 | Kroger | 209 |
| 2 | SUPERVALU | 469 |
| 3 | Limited Brands | 961 |
| 4 | McDonald's | 493 |
| 5 | Darden Restaurants | 497 |
| 6 | 7-Eleven | 219 |
| 7 | YUM! Brands | 847 |
| 8 | Best Buy | 216 |
Purchase 200mg viramune free shipping
Such intense damage can cause extreme headache pain referred over the entire head symptoms narcolepsy buy viramune american express. Removing as little as 20 milliliters of fluid from the spinal canal, particularly if the person remains in an upright position, often causes intense intracranial headache. Removing this quantity of fluid removes part of the flotation for the brain that is normally provided by the cerebrospinal fluid. The weight of the brain stretches and otherwise distorts the various dural surfaces and thereby elicits the pain that causes the headache. Migraine headache is a special type of headache that may result from abnormal vascular function, although the exact mechanism is unknown. Migraine headaches often begin with various prodromal sensations, such as nausea, loss of vision in part of the field of vision, visual aura, and other types of sensory hallucinations. Ordinarily, the prodromal symptoms begin 30 to 60 minutes before the beginning of the headache. Any theory that explains migraine headache must also explain the prodromal symptoms. One theory of migraine headaches is that prolonged emotion or tension causes reflex vasospasm of some of the arteries of the head, including arteries that supply the brain. The vasospasm theoretically produces ischemia of portions of the brain, which is responsible for the prodromal symptoms. Then, as a result of the intense ischemia, something happens to the vascular walls, perhaps exhaustion of smooth muscle contraction, to allow the blood vessels to become flaccid and incapable of maintaining normal vascular tone for 24 to 48 hours. The blood pressure in the vessels causes them to dilate and pulsate intensely, and it is postulated that the excessive stretching of the walls of the arteries-including some extracranial arteries, such as the temporal artery-causes the actual pain of migraine headaches. Other theories about the cause of migraine headaches include spreading cortical depression, psychological abnormalities, and vasospasm caused by excess local potassium in the cerebral extracellular fluid. There may be a genetic predisposition to migraine headaches because a positive family history for migraine has been reported in 65% to 90% of cases. As many people have experienced, a headache often follows excessive alcohol consumption. It is likely that alcohol, because it is toxic to tissues, directly irritates the meninges and causes the intracranial pain. Dehydration may also play a role in the hangover that follows an alcoholic binge; hydration usually attenuates but does not abolish headache and other symptoms of hangover. Discharge frequencies at different skin temperatures of a cold pain fiber, a cold fiber, a warmth fiber, and a heat pain fiber. Emotional tension often causes many of the muscles of the head, especially the muscles attached to the scalp and the neck muscles attached to the occiput, to become spastic; this mechanism is postulated as a common cause of headache. The pain of the spastic head muscles supposedly is referred to the overlying areas of the head and gives one the same type of headache as do intracranial lesions. The mucous membranes of the nose and nasal sinuses are sensitive to pain, but not intensely so. Also, pain from the lower sinuses, such as from the maxillary sinuses, can be felt in the face. Even though these muscles are extremely small, their tonic contraction is believed to cause retro-orbital headache. Also, excessive attempts to focus the eyes can result in reflex spasm in various facial and extraocular muscles, which is a possible cause of headache. A second type of headache that originates in the eyes occurs when the eyes are exposed to excessive irradiation by light rays, especially ultraviolet light. Looking at the sun or the arc of an arc welder for even a few seconds may result in headache that lasts from 24 to 48 hours. The headache sometimes results from "actinic" irritation of the conjunctivae, and the pain is referred to the surface of the head or retro-orbitally. However, focusing intense light from an arc or the sun on the retina can also burn the retina, which could be the cause of the headache. Thermal gradations are discriminated by at least three types of sensory receptors-cold receptors, warmth receptors, and pain receptors. The pain receptors are stimulated only by extreme degrees of heat or cold and are responsible, along with the cold and warmth receptors, for "freezing cold" and "burning hot" sensations. The cold and warmth receptors are located immediately under the skin at discrete separated spots. Most areas of the body have 3 to 10 times as many cold spots as warmth spots; the number in different areas of the body varies from 15 to 25 cold spots/cm2 in the lips to 3 to 5 cold spots/cm2 in the finger to less than 1 cold spot/cm2 in some broad surface areas of the trunk. Warmth receptors are believed to be free nerve endings because warmth signals are transmitted mainly over unmyelinated type C nerve fibers at transmission velocities of only 0. It is a special, small, type A myelinated nerve ending that branches several times, the tips of which protrude into the bottom surfaces of basal epidermal cells. Signals are transmitted from these receptors via thinly myelinated type A nerve fibers at velocities of about 20 m/ sec. Some cold sensations are believed to be transmitted in type C nerve fibers as well, which suggests that some free nerve endings also might function as cold receptors. Stimulation of Thermal Receptors-Sensations of Cold, Cool, Indifferent, Warm, and Hot. Note especially that these fibers respond differently at different levels of temperature. For example, in the very cold region, only the cold pain fibers are stimulated (if the skin becomes even colder so that it nearly freezes or actually does freeze, these fibers cannot be stimulated). One can also understand why extreme degrees of both cold and heat can be painful and why both these sensations, when intense enough, may give almost the same quality of sensation-that is, freezing cold and burning hot sensations feel almost alike. Pain, Headache, and Thermal Sensations Stimulatory Effects of Rising and Falling Temperature-Adaptation of Thermal Receptors. When a cold receptor is suddenly subjected to an abrupt fall in temperature, it becomes strongly stimulated at first, but this stimulation fades rapidly during the first few seconds and progressively more slowly during the next 30 minutes or more. Thus, it is evident that the thermal senses respond markedly to changes in temperature in addition to being able to respond to steady states of temperature. This means that when the temperature of the skin is actively falling, a person feels much colder than when the temperature remains cold at the same level. Conversely, if the temperature is actively rising, the person feels much warmer than he or she would at the same temperature if it were constant. The response to changes in temperature explains the extreme degree of heat one feels on first entering a tub of hot water and the extreme degree of cold felt on going from a heated room to outdoors on a cold day. A few thermal signals are also relayed to the cerebral somatic sensory cortex from the ventrobasal complex. Occasionally, a neuron in cortical somatic sensory area I has been found by microelectrode studies to be directly responsive to either cold or warm stimuli on a specific area of the skin. However, removal of the entire cortical postcentral gyrus in a person reduces but does not abolish the ability to distinguish gradations of temperature. In other words, thermal detection probably results not from direct physical effects of heat or cold on the nerve endings but from chemical stimulation of the endings as modified by temperature. Because the number of cold or warmth endings in any one surface area of the body is slight, it is difficult to judge gradations of temperature when small skin areas are stimulated. However, when a large skin area is stimulated all at once, the thermal signals from the entire area are cumulative. Conversely, temperature changes 100 times as great often will not be detected when the affected skin area is only 1 square centimeter in size. A brief review of these physical principles is presented in this chapter, followed by discussion of the optics of the eye. Light rays ratio of the two refractive indices of the two transparent media; and (2) the degree of angulation between the interface and the entering wave front. The light rays passing through the center of the lens strike the lens exactly perpendicular to the lens surface and, therefore, pass through the lens without being refracted.
Discount generic viramune canada
Therefore 1950s medications cheap 200 mg viramune, hyperbaric oxygenation of the tissues can frequently stop the infectious process entirely and thus convert a condition that formerly was almost 100% fatal into one that is cured in most cases by early treatment with hyperbaric therapy. Other conditions in which hyperbaric O2 therapy has been either valuable or possibly valuable include decompression sickness, arterial gas embolism, carbon monoxide poisoning, osteomyelitis, and myocardial infarction. Castellini M: Life under water: physiological adaptations to diving and living at sea. Hyperbaric Oxygen Therapy the intense oxidizing properties of high-pressure O2 (hyperbaric oxygen) can have valuable therapeutic effects in several important clinical conditions. Therefore, large pressure tanks are now available in many medical centers into which patients can be placed and treated with hyperbaric O2. The O2 is usually administered at Po2 values of 2 to 3 atm pressure through a mask or intratracheal tube, whereas the gas around the body is normal air compressed to the same high-pressure level. The same oxidizing free radicals responsible for O2 toxicity are also believed to be responsible for at least some of the therapeutic benefits. Some of the conditions in which hyperbaric O2 therapy has been especially beneficial are described next. Each minute it receives literally millions of bits of information from the different sensory nerves and sensory organs and then integrates all these to determine responses to be made by the body. Before beginning this discussion of the nervous system, the reader should review Chapters 5 and 7, which present the principles of membrane potentials and transmission of signals in nerves and through neuromuscular junctions. These sensory experiences can either cause immediate reactions from the brain, or memories of the experiences can be stored in the brain for minutes, weeks, or years and determine bodily reactions at some future date. This information enters the central nervous system through peripheral nerves and is conducted immediately to multiple sensory areas in (1) the spinal cord at all levels; (2) the reticular substance of the medulla, pons, and mesencephalon of the brain; (3) the cerebellum; (4) the thalamus; and (5) areas of the cerebral cortex. Incoming signals enter this neuron through synapses located mostly on the neuronal dendrites, but also on the cell body. For different types of neurons, there may be only a few hundred or as many as 200,000 such synaptic connections from input fibers. Then, this axon may have many separate branches to other parts of the nervous system or peripheral body. A special feature of most synapses is that the signal normally passes only in the forward direction, from the axon of a preceding neuron to dendrites on cell membranes of subsequent neurons. This feature forces the signal to travel in required directions to perform specific nervous functions. This task is achieved by controlling (1) contraction of appropriate skeletal muscles throughout the body; (2) contraction of smooth muscle in the internal organs; and (3) secretion of active chemical substances by both exocrine and endocrine glands in many parts of the body. These activities are collectively called motor functions of the nervous system, and the muscles and glands are called effectors because they are the actual anatomical structures that perform the functions dictated by the nerve signals. Operating parallel to this axis is another system, called the autonomic nervous system, for controlling smooth muscles, glands, and other internal bodily systems; this system is discussed in Chapter 61. Thus, if a person places a hand on a hot stove, the desired instantaneous response is to lift the hand. Other associated responses follow, such as moving the entire body away from the stove and perhaps even shouting with pain. However, it is important to note here that synapses determine the directions that the nervous signals will spread through the nervous system. Some synapses transmit signals from one neuron to the next with ease, whereas others transmit signals only with difficulty. Also, facilitatory and inhibitory signals from other areas in the nervous system can control synaptic transmission, sometimes opening the synapses for transmission and, at other times, closing them. In addition, some postsynaptic neurons respond with large numbers of output impulses, and others respond with only a few. Thus, the synapses perform a selective action, often blocking weak signals while allowing strong signals to pass but, at other times, selecting and amplifying certain weak signals and often channeling these signals in many directions rather than in only one direction. More than 99% of all sensory information is discarded by the brain as irrelevant and unimportant. For example, one is ordinarily unaware of the parts of the body that are in contact with clothing, as well as the seat pressure when sitting. However, when important sensory information excites the mind, it is immediately channeled into proper integrative and motor regions of the brain to cause desired responses. This channeling and processing of information 570 Chapter 46 Organization of the Nervous System, Basic Functions of Synapses, and Neurotransmitters Motor area Motor nerve to muscles Caudate nucleus Once memories have been stored in the nervous system, they become part of the brain processing mechanism for future "thinking. From this heritage, three major levels of the central nervous system have specific functional characteristics: (1) the spinal cord level; (2) the lower brain or subcortical level; and (3) the higher brain or cortical level. However, much of the information is stored for future control of motor activities and for use in the thinking processes. Most storage occurs in the cerebral cortex, but even the basal regions of the brain and the spinal cord can store small amounts of information. The storage of information is the process we call memory, which is also a function of the synapses. Each time certain types of sensory signals pass through sequences of synapses, these synapses become more capable of transmitting the same type of signal the next time, a process called facilitation. After the sensory signals have passed through the synapses a large number of times, the synapses become so facilitated that signals generated within the brain itself can also cause transmission of impulses through the same sequences of synapses, even when the sensory input is not excited. This process gives the person a perception of experiencing the original sensations, although the perceptions are only memories of the sensations. The precise mechanisms whereby long-term facilitation of synapses occurs in the memory process are still uncertain, but what is known about this and other details of the sensory memory process are discussed in Chapter 58. We often think of the spinal cord as being only a conduit for signals from the periphery of the body to the brain or in the opposite direction from the brain back to the body. Even after the spinal cord has been cut in the high neck region, many highly organized spinal cord functions still occur. For example, neuronal circuits in the cord can cause (1) walking movements; (2) reflexes that withdraw portions of the body away from painful objects; (3) reflexes that stiffen the legs to support the body against gravity; and (4) reflexes that control local blood vessels, gastrointestinal movements, or urinary excretion. In fact, the upper levels of the nervous system often operate not by sending signals directly to the periphery of the body, but by sending signals to the control centers of the cord, simply "commanding" the cord centers to perform their functions. For example, subconscious control of arterial pressure and respiration is achieved mainly in the medulla and pons. Control of equilibrium is a combined function of the older portions of the cerebellum and the reticular substance of the medulla, pons, and mesencephalon. Feeding reflexes, such as salivation and licking the lips in response to the taste of food, are controlled by areas in the medulla, pons, mesencephalon, amygdala, and hypothalamus. In addition, many emotional patterns, such as anger, excitement, sexual response, reaction to pain, and reaction to pleasure, can still occur after destruction of much of the cerebral cortex. The cortex never functions alone but always in association with lower centers of the nervous system. Without the cerebral cortex, the functions of the lower brain centers are often imprecise. The vast storehouse of cortical information usually converts these functions to determinative and precise operations. Finally, the cerebral cortex is essential for most of our thought processes, but it cannot function by itself. In fact, it is the lower brain centers, not the cortex, that initiate wakefulness in the cerebral cortex, thereby opening its bank of memories to the thinking machinery of the brain. Thus, each portion of the nervous system performs specific functions, but it is the cortex that opens a world of stored information for use by the mind. Block diagram of a general-purpose computer showing the basic components and their interrelations. However, each impulse (1) may be blocked in its transmission from one neuron to the next; (2) may be changed from a single impulse into repetitive impulses; or (3) may be integrated with impulses from other neurons to cause highly intricate patterns of impulses in successive neurons. First, all computers have input circuits that can be compared with the sensory portion of the nervous system, as well as output circuits that are analogous to the motor portion of the nervous system. In simple computers, the output signals are controlled directly by the input signals, operating in a manner similar to that of simple reflexes of the spinal cord. In more complex computers, the output is determined by input signals and by information that has already been stored in memory in the computer, which is analogous to the more complex reflex and processing mechanisms of the human higher nervous system. Furthermore, as computers become even more complex, it is necessary to add still another unit, called the central processing unit, which determines the sequence of all operations. Even a rapid study of this diagram demonstrates its similarity to the nervous system. The fact that the basic components of the general purpose computer are analogous to those of the human nervous system demonstrates that the brain has many features of a computer, continuously collecting sensory information and using this, along with stored information, to compute the daily course of bodily activity.
Buy 200 mg viramune visa
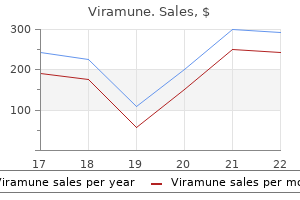
Indeed symptoms carpal tunnel order viramune 200 mg without prescription, an increase in arterial pressure in the human of only a few millimeters of Hg can double the renal output of water, a phenomenon called pressure diuresis, as well as double the output of salt, called pressure natriuresis. However, through the stages of evolution, multiple refinements have been added to make this system much more precise in its control. An especially important refinement, as discussed later, has been the addition of the reninangiotensin mechanism. If blood volume increases and vascular capacitance is not altered, arterial pressure will also increase. The rising pressure, in turn, causes the kidneys to excrete the excess volume, thus returning the pressure back toward normal. This animal has a low arterial pressure, only 8 to 14 mm Hg, and this pressure increases almost directly in proportion to its blood volume. The hagfish continually drinks sea water, which is absorbed into its blood, increasing the blood volume and blood pressure. However, when the pressure rises too high, the kidney excretes the excess volume into the urine and relieves the pressure. Therefore, because the hagfish continues to drink, extracellular fluid volume, blood volume, and pressure all build up again to the higher levels. This primitive mechanism of pressure control has survived throughout the ages, but with the addition of multiple nervous system, hormones, and local control systems that also contribute to the regulation of salt and water excretion. The curve in this figure is called a renal urinary output curve or a renal function curve. In humans, at an arterial pressure of 50 mm Hg, the urine output is essentially zero. Furthermore, not only does increasing the arterial pressure increase urine volume output, but it also causes an approximately equal increase in sodium output, which is the phenomenon of pressure natriuresis. Then, the arterial pressure was suddenly elevated by infusing about 400 ml of blood intravenously. The equilibrium point A describes the level to which the arterial pressure will be regulated if intake is not altered. Shown by the middle curve is the effect of this increased arterial pressure on urine output, which increased 12-fold. Along with this tremendous loss of fluid in the urine, both the cardiac output and arterial pressure returned to normal during the subsequent hour. Thus, one sees an extreme capability of the kidneys to eliminate excess fluid volume from the body in response to high arterial pressure and, in so doing, to return the arterial pressure back to normal. Increases in cardiac output, urinary output, and arterial pressure caused by increased blood volume in dogs whose nervous pressure control mechanisms had been blocked. This figure shows return of arterial pressure to normal after about 1 hour of fluid loss into the urine. Let us see what happens if the arterial pressure increases above or decreases below the equilibrium point. At this level, the renal output of water and salt is almost three times as great as intake. Therefore, the body loses fluid, the blood volume decreases, and the arterial pressure decreases. Furthermore, this negative balance of fluid will not cease until the pressure falls all the way back exactly to the equilibrium level. Even when the arterial pressure is only a few mm Hg greater than the equilibrium level, there still is slightly more loss of water and salt than intake, so the pressure continues to fall that last few mm Hg until the pressure eventually returns to the equilibrium point. If the arterial pressure falls below the equilibrium point, the intake of water and salt is greater than the 230 output. Therefore, body fluid volume increases, blood volume increases, and the arterial pressure rises until once again it returns to the equilibrium point. Furthermore, there are only two ways in which the pressure of this equilibrium point can be changed from the 100 mm Hg level. One is by shifting the pressure level of the renal output curve for salt and water, and the other is by changing the level of the water and salt intake line. Therefore, expressed simply, the two primary determinants of the long-term arterial pressure level are as follows: 1. Under steadystate conditions, the renal output of salt and water is equal to intake of salt and water. Points A and B represent the equilibrium points for long-term regulation of arterial pressure when salt intake is normal or six times normal, respectively. Because of the steepness of the chronic renal output curve, increased salt intake normally causes only small changes in arterial pressure. In persons with impaired kidney function, the steepness of the renal output curve may be reduced, similar to the acute curve, resulting in increased sensitivity of arterial pressure to changes in salt intake. A, By shifting the renal output curve in the right-hand direction toward a higher pressure level or by increasing the intake level of salt and water (B). Therefore, one can state that if the renal output curve shifts to a new pressure level, the arterial pressure will follow to this new pressure level within a few days. In this case, the intake level has increased fourfold, and the equilibrium point has shifted to a pressure level of 160 mm Hg, 60 mm Hg above the normal level. Thus, it is impossible to change the long-term mean arterial pressure level to a new value without changing one or both of the two basic determinants of long-term arterial pressure, either (1) the level of salt and water intake or (2) the degree of shift of the renal function curve along the pressure axis. However, if either of these is changed, one finds the arterial pressure thereafter to be regulated at a new pressure level, the arterial pressure at which the two new curves intersect. Thus, when the kidneys are functioning normally, the chronic renal output curve is much steeper than the acute curve. The powerful effects of chronic increases in arterial pressure on urine output occur because increased pressure not only has direct hemodynamic effects on the kidney to increase excretion, but also has indirect effects mediated by nervous and hormonal changes that occur when blood pressure is increased. Reduced activity of these antinatriuretic systems therefore amplifies the effectiveness of pressure natriuresis and diuresis in raising salt and water excretion during chronic increases in arterial pressure (see Chapters 28 and 30 for further discussion). Conversely, when blood pressure is reduced, the sympathetic nervous system is activated, and formation of antinatriuretic hormones is increased, adding to the direct effects of reduced pressure to decrease renal output of salt and water. This combination of direct effects of pressure on the kidneys and indirect effects of pressure on the sympathetic nervous system and various hormone systems make pressure natriuresis and diuresis extremely powerful factors for long-term control of arterial pressure and body fluid volumes. The importance of neural and hormonal influences on pressure natriuresis is especially evident during chronic changes in sodium intake. Note that the blood pressure equilibrium point B on the curve is nearly the same as point A, the equilibrium point at normal salt intake. Conversely, decreases in salt and water intake to as low as one-sixth normal typically have little effect on arterial pressure. Thus, many persons are said to be salt-insensitive because large variations in salt intake do not change blood pressure more than a few mm Hg. In these cases, even moderate increases in salt intake may cause significant increases in arterial pressure. For example, surgical reduction of kidney mass or injury to the kidney due to hypertension, diabetes, or various kidney diseases all cause blood pressure to be more sensitive to changes in salt intake. In these cases, greater than normal increases in arterial pressure are required to raise renal output sufficiently to maintain a balance between the intake and output of salt and water. There is evidence that long-term high salt intake, lasting for several years, may actually damage the kidneys and eventually makes blood pressure more salt-sensitive. We will discuss salt sensitivity of blood pressure in patients with hypertension later in this chapter.
Syndromes
- Infant botulism
- Sore throat
- Intolerance to cold
- Shortness of breath
- Hematoma (blood collecting under the skin)
- A mass that can be felt on a physical exam
- Vascular ultrasound
- Breathing problems
- Rheumatoid arthritis
- Diabetes
Buy discount viramune online
Most of the clotting factors listed in Table 37-1 are designated by Roman numerals medicine gustav klimt buy genuine viramune on line. Extrinsic Pathway for Initiating Clotting the extrinsic pathway for initiating the formation of prothrombin activator begins with a traumatized vascular wall or traumatized extravascular tissues that come in contact with the blood. Traumatized tissue releases a complex of several factors called tissue factor or tissue thromboplastin. This factor is composed especially of phospholipids from the membranes of the tissue plus a lipoprotein complex that functions mainly as a proteolytic enzyme. These mechanisms are set into play by the following: (1) trauma to the vascular wall and adjacent tissues; (2) trauma to the blood; or (3) contact of the blood with damaged endothelial cells or with collagen and other tissue elements outside the blood vessel. In each case, this leads to the formation of prothrombin activator, which then causes prothrombin conversion to thrombin and all the subsequent clotting steps. The activated factor X combines immediately with tissue phospholipids that are part of tissue factors or with additional phospholipids released from platelets, as well as with factor V, to form the complex called prothrombin activator. Within a few seconds, in the presence of Ca2+, prothrombin is split to form thrombin, and the clotting process proceeds as already explained. At first, the factor V in the prothrombin activator complex is inactive, but once clotting begins and thrombin begins to form, the proteolytic action of thrombin activates factor V. This activation then becomes an additional strong accelerator of prothrombin activation. Thus, in the final prothrombin activator complex, activated factor X is the actual protease that causes splitting of prothrombin to form thrombin. Activated factor V greatly accelerates this protease activity, and platelet phospholipids act as a vehicle that further accelerates the process. Note especially the positive feedback effect of thrombin, acting through factor V, to accelerate the entire process once it begins. Intrinsic Pathway for Initiating Clotting the second mechanism for initiating formation of prothrombin activator, and therefore for initiating clotting, begins with trauma to the blood or exposure of the blood to collagen from a traumatized blood vessel wall. Simultaneously, the blood trauma also damages the platelets because of adherence to collagen or to a wettable surface (or by damage in other ways); this releases platelet phospholipids that contain the lipoprotein called platelet factor 3, which also plays a role in subsequent clotting reactions. This reaction also requires high-molecularweight kininogen and is accelerated by prekallikrein. Platelets are the clotting factor that is lacking in the bleeding disease called thrombocytopenia. This step in the intrinsic pathway is the same as the last step in the extrinsic pathway. That is, activated factor X combines with factor V and platelet or tissue phospholipids to form the complex called prothrombin activator. The prothrombin activator, in turn, initiates the cleavage of prothrombin to form thrombin within seconds, thereby setting into motion the final clotting process, as described earlier. The intrinsic pathway is much slower to proceed, usually requiring 1 to 6 minutes to cause clotting. Intravascular Anticoagulants Prevent Blood Clotting in the Normal Vascular System Endothelial Surface Factors. Therefore, in the absence of calcium ions, blood clotting by either pathway does not occur. In the living body, the calcium ion concentration seldom falls low enough to affect blood-clotting kinetics significantly. However, when blood is removed from someone, it can be prevented from clotting by reducing the calcium ion concentration below the threshold level for clotting by deionizing the calcium by causing it to react with substances such as citrate ion or by precipitating the calcium with substances such as oxalate ion. Interaction Between Extrinsic and Intrinsic Pathways-Summary of BloodClotting Initiation It is clear from the schemas of the intrinsic and extrinsic systems that after blood vessels rupture, clotting occurs by both pathways simultaneously. While a clot is forming, about 85% to 90% of the thrombin formed from the prothrombin becomes adsorbed to the fibrin fibers as they develop. This adsorption helps prevent the spread of thrombin into the remaining blood and, therefore, prevents excessive spread of the clot. This further blocks the effect of thrombin on the fibrinogen and then also inactivates thrombin itself during the next 12 to 20 minutes. Heparin is another powerful anticoagulant but, because its concentration in the blood is normally low, it has significant anticoagulant effects only under special physiological conditions. However, heparin is used widely as a pharmacological agent in medical practice in much higher concentrations to prevent intravascular clotting. Heparin is produced by many different cells of the body, but the largest quantities are formed by the basophilic mast cells located in the pericapillary connective tissue throughout the body. These cells continually secrete small quantities of heparin that diffuse into the circulatory system. The basophil cells of the blood, which are functionally almost identical to the mast cells, release small quantities of heparin into the plasma. Mast cells are abundant in tissue surrounding the capillaries of the lungs and, to a lesser extent, capillaries of the liver. It is easy to understand why large quantities of heparin might be needed in these areas because the capillaries of the lungs and liver receive many embolic clots that have formed in slowly flowing venous blood; sufficient production of heparin prevents further growth of the clots. In fact, many small blood vessels in which blood flow has been blocked by clots are reopened by this mechanism. Thus, an especially important function of the plasmin system is to remove minute clots from millions of tiny peripheral vessels that eventually would become occluded were there no way to clear them. Three particular types of bleeding tendencies that have been studied to the greatest extent are discussed here-bleeding caused by (1) vitamin K deficiency, (2) hemophilia, and (3) thrombocytopenia (platelet deficiency). Therefore, diseases of the liver such as hepatitis, cirrhosis, and acute yellow atrophy (degeneration of the liver caused by toxins, infections, or other agents) can sometimes depress the clotting system so much that the patient develops a severe tendency to bleed. Another cause of depressed formation of clotting factors by the liver is vitamin K deficiency. On adding the carboxyl group to glutamic acid residues on the immature clotting factors, vitamin K is oxidized and becomes inactive. In the absence of active vitamin K, subsequent insufficiency of these coagulation factors in the blood can lead to serious bleeding tendencies. Vitamin K is continually synthesized in the intestinal tract by bacteria, so vitamin K deficiency seldom occurs in healthy persons as a result of the absence of vitamin K from the diet (except in neonates, before they establish their intestinal bacterial flora). However, in persons with gastrointestinal disease, vitamin K deficiency often occurs as a result of poor absorption of fats from the gastrointestinal tract because vitamin K is fat-soluble and is ordinarily absorbed into the blood along with the fats. One of the most prevalent causes of vitamin K deficiency is failure of the liver to secrete bile into the gastrointestinal tract, which occurs as a result of obstruction of the bile ducts or of liver disease. Plasmin is a proteolytic enzyme that resembles trypsin, the most important proteolytic digestive enzyme of pancreatic secretion. Therefore, whenever plasmin is formed, it can cause lysis of a clot by destroying many of the clotting factors, thereby sometimes even causing hypocoagulability of the blood. When a clot is formed, a large amount of plas- minogen is trapped in the clot, along with other plasma proteins. Thus, liver disease often causes decreased production of prothrombin and some other clotting factors because of poor vitamin K absorption and because of the diseased liver cells. As a result, vitamin K is injected into surgical patients with liver disease or with obstructed bile ducts before the surgical procedure is performed. Ordinarily, if vitamin K is given to a deficient patient 4 to 8 hours before the operation and the liver parenchymal cells are at least halfnormal in function, sufficient clotting factors will be produced to prevent excessive bleeding during the operation. Both these clotting factors are now available as recombinant proteins, although they are expensive and their half-lives are relatively short; therefore, these products are not readily available for many patients with hemophilia, especially in economically disadvantaged countries. Both these factors are transmitted genetically by way of the female (X) chromosome and are recessive in their inheritance. Therefore, a woman will rarely have hemophilia because at least one of her two X chromosomes will have the appropriate genes. If one of her X chromosomes is deficient, she will be a hemophilia carrier; her male offspring will have a 50% chance of inheriting the illness, and her female offspring will have a 50% chance of inheriting the carrier status. Although female carriers have one normal allele and usually do not develop symptomatic hemophilia, some may experience a mild bleeding trait. It is also possible for female carriers to develop mild hemophilia due to loss of part or all of the normal X chromosome (as in Turner syndrome) or inactivation (lyonization) of the X-chromosomes.
Order viramune 200 mg otc
Indeed symptoms zika virus buy 200mg viramune overnight delivery, this reflex is so strong that if an animal whose spinal cord has been transected for several months-after the reflexes have become exaggerated-is placed on its feet, the reflex often stiffens the limbs sufficiently to support the weight of the body. The positive supportive reaction involves a complex circuit in the interneurons similar to the circuits responsible for the flexor and crossed extensor reflexes. The locus of the pressure on the pad of the foot determines the direction in which the limb will extend; pressure on one side causes extension in that direction, an effect called the magnet reaction. When a spinal animal is laid on its side, it will make uncoordinated movements to try to raise itself to the standing position. Such a reflex demonstrates that some relatively complex reflexes associated with posture are integrated in the spinal cord. Motor and Integrative Neurophysiology a well-healed transected thoracic cord between the levels for forelimb and hindlimb innervation can right itself from the lying position and even walk using its hindlimbs in addition to its forelimbs. In the case of an opossum with a similar transection of the thoracic cord, the walking movements of the hindlimbs are hardly different from those in a normal opossum, except that the hindlimb walking movements are not synchronized with those of the forelimbs. Rhythmical stepping movements are frequently observed in the limbs of spinal animals. Indeed, even when the lumbar portion of the spinal cord is separated from the remainder of the cord and a longitudinal section is made down the center of the cord to block neuronal connections between the two sides of the cord and between the two limbs, each hindlimb can still perform individual stepping functions. Forward flexion of the limb is followed a second or so later by backward extension. This oscillation back and forth between flexor and extensor muscles can occur even after the sensory nerves have been cut, and it seems to result mainly from mutually reciprocal inhibition circuits within the matrix of the cord, oscillating between the neurons controlling agonist and antagonist muscles. The sensory signals from the footpads and from the position sensors around the joints play a strong role in controlling foot pressure and frequency of stepping when the foot is allowed to walk along a surface. For instance, if the top of the foot encounters an obstruction during forward thrust, the forward thrust will stop temporarily; then, in rapid sequence, the foot will be lifted higher and proceed forward to be placed over the obstruction. If the lum- An especially important cord reflex in some animals is the scratch reflex, which is initiated by an itch or tickle sensation. This reflex involves two functions: (1) a position sense that allows the paw to find the exact point of irritation on the surface of the body; and (2) a to-and-fro scratching movement. If a flea is crawling as far forward as the shoulder of a spinal animal, the hind paw can still find its position, even though 19 muscles in the limb must be contracted simultaneously in a precise pattern to bring the paw to the position of the crawling flea. To make the reflex even more complicated, when the flea crosses the midline, the first paw stops scratching and the opposite paw begins the to-and-fro motion and eventually finds the flea. The to-and-fro movement, like the stepping movements of locomotion, involves reciprocal innervation circuits that cause oscillation. Spinal Cord Reflexes That Cause Muscle Spasm In human beings, local muscle spasm is often observed. One type of clinically important spasm occurs in muscles that surround a broken bone. The spasm results from pain impulses initiated from the broken edges of the bone, which cause the muscles that surround the area to contract tonically. Pain relief obtained by injecting a local anesthetic at the broken edges of the bone relieves the spasm; a deep general anesthetic of the entire body, such as ether anesthesia, also relieves the spasm. If a well-healed spinal animal (with spinal tran- section in the neck above the forelimb area of the cord) is held up from the floor and its legs are allowed to dangle, the stretch on the limbs occasionally elicits stepping reflexes that involve all four limbs. This diagonal response is another manifestation of reciprocal innervation, this time occurring the entire dis694 Another type of local spasm caused by cord reflexes is abdominal spasm resulting from irritation of the parietal peritoneum by peritonitis. Here again, relief of the pain caused by the peritonitis allows the spastic muscle to relax. The same type of spasm often occurs during surgical operations; for instance, during abdominal operations, pain impulses from the parietal peritoneum often cause the abdominal muscles to contract extensively, sometimes extruding the intestines through the surgical wound. For this reason, deep anesthesia is usually required for intraabdominal operations. Any local irritating factor or metabolic abnormality of a muscle, such as severe cold, lack of blood flow, or overexercise, can elicit pain or other sensory signals transmitted from the muscle to the spinal cord, which in turn cause reflex feedback muscle contraction. The contraction is believed to stimulate the same sensory receptors even more, which causes the spinal cord to increase the intensity of contraction. Thus, positive feedback develops, so a small amount of initial irritation causes more and more contraction until a full-blown muscle cramp ensues. Chapter 55 Spinal Cord Motor Functions; the Cord Reflexes Autonomic Reflexes in the Spinal Cord Many types of segmental autonomic reflexes are integrated in the spinal cord, most of which are discussed in other chapters. Briefly, these reflexes include (1) changes in vascular tone resulting from changes in local skin heat (see Chapter 74); (2) sweating, which results from localized heat on the surface of the body (see Chapter 74); (3) intestinointestinal reflexes that control some motor functions of the gut (see Chapter 63); (4) peritoneointestinal reflexes that inhibit gastrointestinal motility in response to peritoneal irritation (see Chapter 67); and (5) evacuation reflexes for emptying the full bladder (see Chapter 26) or the colon (see Chapter 64). In addition, all the segmental reflexes can at times be elicited simultaneously in the form of the so-called mass reflex, described next. In a spinal animal or person, sometimes the spinal cord suddenly becomes excessively active, causing massive discharge in large portions of the cord. The usual stimulus that causes this excess activity is a strong pain stimulus to the skin or excessive filling of a viscus, such as overdistention of the bladder or the gut. Regardless of the type of stimulus, the resulting reflex, called the mass reflex, involves large portions or even all of the cord. Because the mass reflex can last for minutes, it presumably results from activation of large numbers of reverberating circuits that excite large areas of the cord at once. This mechanism is similar to the mechanism of epileptic seizures, which involve reverberating circuits that occur in the brain instead of in the cord. Spinal Cord Transection and Spinal Shock nervous system activity becomes blocked almost to extinction. All skeletal muscle reflexes integrated in the spinal cord are blocked during the initial stages of shock. In lower animals, a few hours to a few days are required for these reflexes to return to normal; in humans, 2 weeks to several months are sometimes required. In both animals and humans, some reflexes may eventually become hyperexcitable, particularly if a few facilitatory pathways remain intact between the brain and the cord while the remainder of the spinal cord is transected. The first reflexes to return are the stretch reflexes, followed in order by the progressively more complex reflexes: flexor reflexes, postural antigravity reflexes, and remnants of stepping reflexes. The sacral reflexes for control of bladder and colon evacuation are suppressed in people for the first few weeks after cord transection, but in most cases they eventually return. Duysens J, Clarac F, Cruse H: Load-regulating mechanisms in gait and posture: comparative aspects. Frigon A: the neural control of interlimb coordination during mammalian locomotion. Jankowska E, Hammar I: Interactions between spinal interneurons and ventral spinocerebellar tract neurons. Marchand-Pauvert V, Iglesias C: Properties of human spinal interneurones: normal and dystonic control. When the spinal cord is suddenly transected in the upper neck, essentially all cord functions, including the cord reflexes, immediately become depressed to the point of total silence, a reaction called spinal shock. The reason for this reaction is that normal activity of the cord neurons depends to a great extent on continual tonic excitation by the discharge of nerve fibers entering the cord from higher centers, particularly discharge transmitted through the reticulospinal tracts, vestibulospinal tracts, and corticospinal tracts. After a few hours to a few weeks, the spinal neurons gradually regain their excitability. This phenomenon seems to be a natural characteristic of neurons everywhere in the nervous system; after they lose their source of facilitatory impulses, they increase their own natural degree of excitability to make up at least partially for the loss. In most nonprimates, excitability of the cord centers returns essentially to normal within a few hours to a day or so, but in people, the return is often delayed for several weeks and occasionally is never complete; conversely, sometimes recovery is excessive, with resultant hyperexcitability of some or all cord functions. Some of the spinal functions specifically affected during or after spinal shock are the following: 1. For a few types of movements, however, the cortex has almost a direct pathway to the anterior motor neurons of the cord, bypassing some motor centers on the way. This is especially true for control of the fine dexterous movements of the fingers and hands. This article and Chapter 57 explain the interplay among the different motor areas of the brain and spinal cord to provide overall synthesis of voluntary motor function. This mapping was done by electrically stimulating the different areas of the motor cortex in human beings were undergoing neurosurgery. Note that more than half of the entire primary motor cortex is concerned with controlling the muscles of the hands and the muscles of speech. Point stimulation in these hand and speech motor areas on rare occasion causes contraction of a single muscle, but most often, stimulation contracts a group of muscles.
Cheap viramune 200 mg online
All the fac- body are equally damaged by shock because some tissues have better blood supplies than others medicine university buy discount viramune on-line. For example, the cells adjacent to the arterial ends of capillaries receive better nutrition than cells adjacent to the venous ends of the same capillaries. Therefore, more nutritive deficiency occurs around the venous ends of capillaries than elsewhere. Similar punctate lesions occur in heart muscle, although here a definite repetitive pattern, such as occurs in the liver, cannot be demonstrated. Nevertheless, the cardiac lesions play an important role in leading to the final irreversible stage of shock. Deteriorative lesions also occur in the kidneys, especially in the epithelium of the kidney tubules, leading to kidney failure and occasionally uremic death several days later. Deterioration of the lungs also often leads to respiratory distress and death several days later, called the shock lung syndrome. Metabolic derangements that oc- tors just discussed that can lead to further progression of shock are types of positive feedback-that is, each increase in the degree of shock causes a further increase in the shock. In mild degrees of shock, the negative feedback mechanisms of the circulation, including sympathetic reflexes, reverse stress-relaxation mechanism of the blood reservoirs, and absorption of fluid into the blood from the interstitial spaces, can easily overcome the positive feedback influences and, therefore, cause recovery. In severe shock, however, the deteriorative feedback mechanisms become more and more powerful, leading to such rapid deterioration of the circulation that all the normal negative feedback systems of circulatory control acting together cannot return the cardiac output to normal. Considering once again the principles of positive feedback and vicious cycles discussed in Chapter 1, one can readily understand why there is a critical cardiac output level above which a person in shock recovers and below which a person enters a vicious cycle of circulatory deterioration that proceeds until death. Ironically, even in this irreversible stage, therapy can, on rare occasions, return the arterial pressure and even the cardiac output to normal or near normal for short periods, but the circulatory system nevertheless continues to deteriorate, and death ensues in another few minutes to few hours. However, the cardiac output soon begins to fall again, and subsequent transfusions have less and less effect. Progressive stage Transfusion cur in shocked tissue can lead to acidosis throughout the body. This results from poor delivery of oxygen to the tissues, which greatly diminishes oxidative metabolism of the foodstuffs. When this occurs, the cells obtain most of their energy by the anaerobic process of glycolysis, which leads to excess lactic acid in the blood. In addition, poor blood flow through tissues prevents normal removal of carbon dioxide. The carbon dioxide reacts locally in the cells with water to form high concentrations of intracellular carbonic acid, which, in turn, reacts with various tissue chemicals to form additional intracellular acidic substances. Thus, another deteriorative effect of shock is generalized and local tissue acidosis, leading to further progression of the shock. Beyond a certain point, so much tissue damage has occurred, so many destructive enzymes have been released into the body fluids, so much acidosis has developed, and so many other destructive factors are now in progress that even a normal cardiac output for a few minutes cannot reverse the continuing deterioration. Therefore, in severe shock, a stage is eventually reached at which the person will die, even though vigorous therapy might still return the cardiac output to normal for short periods. The high-energy phos- phate reserves in the tissues of the body, especially in the liver and heart, are greatly diminished in severe shock. Essentially all the creatine phosphate has been degraded, and almost all the adenosine triphosphate has downgraded to adenosine diphosphate, adenosine monophosphate and, eventually, adenosine. Much of this adenosine then diffuses out of the cells into the circulating blood and is converted into uric acid, a substance that cannot re-enter the cells to reconstitute the adenosine phosphate system. New adenosine can be synthesized at a rate of only about 2% of the normal cellular amount an hour, meaning that once the high-energy phosphate stores of the cells are depleted, they are difficult to replenish. Thus, one of the most devastating end results in shock, and the one that is perhaps most significant for development of the final state of irreversibility, is cellular depletion of these high-energy compounds. Loss of fluid from all fluid compartments of the body is called dehydration; this condition can also reduce the blood volume and cause hypovolemic shock similar to that resulting from hemorrhage. Some of the causes of this type of shock are the following: (1) excessive sweating; (2) fluid loss in severe diarrhea or vomiting; (3) excess loss of fluid by the kidneys; (4) inadequate intake of fluid and electrolytes; or (5) destruction of the adrenal cortices, with loss of aldosterone secretion and consequent failure of the kidneys to reabsorb sodium, chloride, and water, which occurs in the absence of the adrenocortical hormone aldosterone. Often, the shock results simply from hemorrhage caused by the trauma, but it can also occur even without hemorrhage because extensive contusion of the body can damage the capillaries sufficiently to allow excessive loss of plasma into the tissues. This phenomenon results in greatly reduced plasma volume, with resultant hypovolemic shock. Various attempts have been made to implicate toxic factors released by the traumatized tissues as one of the causes of shock after trauma. However, cross-transfusion experiments with normal animals have failed to show significant toxic elements. Traumatic shock, therefore, seems to result mainly from hypovolemia, although there might also be a moderate degree of concomitant neurogenic shock caused by loss of vasomotor tone, as discussed next. Distention of the intestine in intestinal obstruction partly blocks venous blood flow in the intestinal walls, which increases intestinal capillary pressure, causing fluid to leak from the capillaries into the intestinal walls and intestinal lumen. Because the lost fluid has high protein content, the result is reduced total blood plasma protein, as well as reduced plasma volume. Severe burns or other denuding conditions of the skin cause loss of plasma through the denuded skin areas so that the plasma volume becomes markedly reduced. Instead, the vascular capacity increases so much that even the normal amount of blood is incapable of filling the circulatory system adequately. One of the major causes of this condition is sudden loss of vasomotor tone throughout the body, resulting especially in massive dilation of the veins. The role of vascular capacity in helping regulate circulatory function was discussed in Chapter 15, where it was noted that an increase in vascular capacity or a decrease in blood volume reduces the mean systemic filling pressure, which reduces venous return to the heart. Diminished venous return caused by vascular dilation is called venous pooling of blood. Some neurogenic factors that can cause loss of vasomotor tone include the following: 1. Deep general anesthesia often depresses the vasomotor center enough to cause vasomotor paralysis, with resulting neurogenic shock. Spinal anesthesia, especially when this extends all the way up the spinal cord, blocks the sympathetic nervous outflow from the nervous system and can be a potent cause of neurogenic shock. Many patients who have had a brain concussion or contusion of the basal regions of the brain experience profound neurogenic shock. Septic shock is extremely important to the clinician because, other than cardiogenic shock, septic shock is currently the most frequent cause of shock-related death in the hospital. Peritonitis caused by spread of infection from the uterus and fallopian tubes, sometimes resulting from an instrumental abortion performed under unsterile conditions 2. Peritonitis resulting from rupture of the gastrointestinal system, sometimes caused by intestinal disease or by wounds 3. Generalized bodily infection resulting from spread of a skin infection such as streptococcal or staphylococcal infection 4. Generalized gangrenous infection resulting specifically from gas gangrene bacilli, spreading first through peripheral tissues and finally via the blood to the internal organs, especially the liver 5. Infection spreading into the blood from the kidney or urinary tract, often caused by colon bacilli. It results primarily from an antigen-antibody reaction that rapidly occurs after an antigen to which the person is sensitive enters the circulation. One of the principal effects is to cause the basophils in the blood and mast cells in the pericapillary tissues to release histamine or a histamine-like substance. The histamine causes the following: (1) an increase in vascular capacity because of venous dilation, thus causing a marked decrease in venous return; (2) dilation of the arterioles, resulting in greatly reduced arterial pressure; and (3) greatly increased capillary permeability, with rapid loss of fluid and protein into the tissue spaces. The net effect is a great reduction in venous return and, sometimes, such serious shock that the person may die within minutes. Intravenous injection of large amounts of histamine causes histamine shock, which has characteristics almost identical to those of anaphylactic shock. There are many varieties of septic shock because of the many types of bacterial infections that can cause it, and because infection in different parts of the body produces different effects. Most cases of septic shock, however, are caused by Gram-positive bacteria, followed by endotoxin-producing Gram-negative bacteria. Often marked vasodilation throughout the body, especially in the infected tissues 3. High cardiac output in perhaps half of patients, caused by arteriolar dilation in the infected tissues and by high metabolic rate and vasodilation elsewhere in the body, resulting from bacterial toxin stimulation of cellular metabolism and from a high body temperature 4.
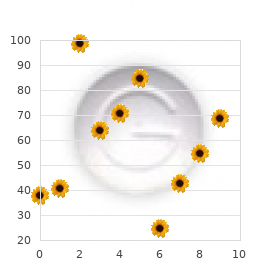
Cheap viramune 200 mg otc
This is because fluid usually enters the body through the gut and must be transported by the blood to all tissues before complete osmotic equilibrium can occur professional english medicine discount viramune 200 mg on-line. Effect of adding isotonic (A), hypertonic (B), and hypotonic solutions (A) to the extracellular fluid after osmotic equilibrium. The normal state is indicated by the solid lines, and the shifts from normal are shown by the shaded areas. The volumes of intracellular and extracellular fluid compartments are shown in the abscissa of each diagram, and the osmolarities of these compartments are shown on the ordinates. Add Hypertonic NaCl It usually takes about 30 minutes to achieve osmotic equilibrium everywhere in the body after drinking water. Effect of Adding Saline Solution to the Extracellular Fluid If isotonic saline is added to the extracellular fluid compartment, the osmolarity of the extracellular fluid does not change. The sodium and chloride largely remain in the extracellular fluid because the cell membrane behaves as though it were virtually impermeable to the sodium chloride. Again, almost all the added sodium chloride remains in the extracellular compartment, and fluid diffuses from the cells into the extracellular space to achieve osmotic equilibrium. The net effect is an increase in extracellular volume (greater than the volume of fluid added), a decrease in intracellular volume, and a rise in osmolarity in both compartments. Both the intracellular and extracellular volumes are increased by the addition of hypotonic fluid, although the intracellular volume increases to a greater extent. Calculation of Fluid Shifts and Osmolarities After Infusion of Hypertonic Saline Solution. The changes in intracellular and extracellular fluid volumes and the types of therapy that should be instituted can be calculated if the following basic principles are kept in mind: 1. Water moves rapidly across cell membranes; therefore, the osmolarities of intracellular and extracellular fluids remain almost exactly equal to each other, except for a few minutes after a change in one of the compartments. Cell membranes are almost completely impermeable to many solutes, such as sodium and chloride; therefore, the number of osmoles in the extracellular or intracellular fluid generally remains relatively constant unless solutes are added to or lost from the extracellular compartment. With these basic principles in mind, we can analyze the effects of different abnormal fluid conditions on extracellular and intracellular fluid volumes and osmolarities. The first step is to calculate the initial conditions, including the volume, concentration, and total milliosmoles in each compartment. Assuming that extracellular fluid volume is 20% of body weight, and intracellular fluid volume is 40% of body weight, the following volumes and concentrations can be calculated. Initial Conditions Volume (liters) Extracellular fluid Intracellular fluid Total body fluid 14 28 42 Concentration (mOsm/L) 280 280 280 Total (mOsm) 3920 7840 11,760 Next, we calculate the total milliosmoles added to the extracellular fluid in 2 liters of 3. Because 1 mole of sodium chloride is equal to approximately 2 osmoles (sodium chloride has two osmotically active particles per mole), the net effect of adding 2 liters of this solution is to add 2051 milliosmoles of sodium chloride to the extracellular fluid. In step 2, we calculate the instantaneous effect of adding 2051 milliosmoles of sodium chloride to the extracellular fluid along with 2 liters of volume. There would be no change in the intracellular fluid concentration or volume, and there would be no osmotic equilibrium. In the extracellular fluid, however, there would be an additional 2051 milliosmoles of total solute, yielding a total of 5971 milliosmoles. Because the extracellular compartment now has 16 liters of volume, the concentration can be calculated by dividing 5971 milliosmoles by 16 liters to yield a concentration of about 373 mOsm/L. In this case, the concentrations in the intracellular and extracellular fluid compartments would be equal and can be calculated by dividing the total milliosmoles in the body, 13,811, by the total volume, which is now 44 liters. Therefore, all the body fluid compartments will have this same concentration after osmotic equilibrium. Assuming that no solute or water has been lost from the body, and that there is no movement of sodium chloride into or out of the cells, we then calculate the volumes of the intracellular and extracellular compartments. The intracellular fluid volume is calculated by dividing the total milliosmoles in the intracellular fluid (7840) by the concentration (313. Extracellular fluid volume is calculated by dividing the total milliosmoles in extracellular fluid (5971) by the concentration (313. Again, these calculations are based on the assumption that the sodium chloride added to the extracellular fluid remains there and does not move into the cells. This method of calculating changes in intracellular and extracellular fluid volumes and osmolarities can be applied to virtually any clinical problem of fluid volume regulation. The reader should be familiar with such calculations because an understanding of the mathematical aspects of osmotic equilibrium between intracellular and extracellular fluid compartments is essential for understanding almost all fluid abnormalities of the body and their treatment. Glucose solutions are widely used; amino acid and homogenized fat solutions are used to a lesser extent. After the glucose or other nutrients are metabolized, an excess of water often remains, especially if additional fluid is ingested. A 5% glucose solution, which is nearly isosmotic, is often used to treat dehydration. Because the solution is osmotic, it can be infused intravenously without causing red blood cell swelling, as would occur with an infusion of pure water. Therefore, infusion of a 5% glucose solution reduces extracellular fluid osmolarity and therefore helps correct the increase in extracellular fluid osmolarity associated with dehydration. Conditions that can cause hyponatremia as a result of the loss of sodium include diarrhea and vomiting. Overuse of diuretics that inhibit the ability of the kidneys to conserve sodium and certain types of sodium-wasting kidney diseases can also cause modest degrees of hyponatremia. Addison disease, which results from decreased secretion of the hormone aldosterone, impairs the ability of the kidneys to reabsorb sodium and can cause a modest degree of hyponatremia. Hyponatremia can also be associated with excess water retention, which dilutes the sodium in the extracellular fluid, a condition referred to as hyponatremiaoverhydration. Plasma osmolarity is not routinely measured but, because sodium and its associated anions (mainly chloride) account for more than 90% of the solute in the extracellular fluid, plasma sodium concentration is a reasonable indicator of plasma osmolarity under many conditions. When plasma sodium concentration is reduced more than a few milliequivalents below normal (about 142 mEq/L), a person is said to have hyponatremia. When plasma sodium concentration is elevated above normal, a person is said to have hypernatremia. Hyponatremia Causes Cell Edema Rapid changes in cell volume as a result of hyponatremia can have profound effects on tissue and organ function, especially the brain. A rapid reduction in plasma sodium concentration, for example, can cause brain cell edema and neurological symptoms, including headache, nausea, lethargy, and disorientation. If plasma sodium concentration rapidly falls below 115 to 120 mmol/L, brain swelling may lead to seizures, coma, permanent brain damage, and death. Because the skull is rigid, the brain cannot increase its volume by more than about 10% without it being forced down the neck (herniation), which can lead to permanent brain injury and death. When hyponatremia evolves more slowly, over several days, the brain and other tissues respond by transporting sodium, chloride, potassium, and organic solutes, such as glutamate, from the cells into the extracellular compartment. Transport of solutes from the cells during slowly developing hyponatremia, however, can make the brain vulnerable to injury if the hyponatremia is corrected too rapidly. K+, Na+ Organic solutes H2O Causes of Hypernatremia: Water Loss or Excess Sodium An increased plasma sodium concentration, which also causes increased osmolarity, can be due to loss of water from the extracellular fluid, which concentrates the sodium ions, or excess sodium in the extracellular fluid. Primary loss of water from the extracellular fluid results in hypernatremia and dehydration. A more common cause of hypernatremia associated with decreased extracellular fluid volume is simple dehydration caused by water intake that is less than water loss, as can occur with sweating during prolonged heavy exercise. Hypernatremia can also occur when excessive sodium chloride is added to the extracellular fluid. This often results in hypernatremia-overhydration because excess extracellular sodium chloride is also usually associated with at least some degree of water retention by the kidneys. For example, excessive secretion of the sodiumretaining hormone aldosterone can cause a mild degree of hypernatremia and overhydration. Thus, in analyzing abnormalities of plasma sodium concentration and deciding on proper therapy, one should first determine whether the abnormality is caused by a primary loss or gain of sodium or a primary loss or gain of water. During acute hyponatremia, caused by loss of Na+ or excess H2O, there is diffusion of H2O into the cells (1) and swelling of the brain tissue (indicated by the dashed lines). This process stimulates transport of Na+, K+, and organic solutes out of the cells (2), which then causes water diffusion out of the cells (3). With chronic hyponatremia, the brain swelling is attenuated by transport of solutes from the cells.
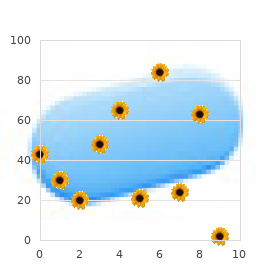
Purchase viramune 200 mg mastercard
The released adenosine is believed to be one of the substances that causes dilation of the coronary arterioles during coronary hypoxia symptoms 9 weeks pregnancy discount 200 mg viramune mastercard, as discussed earlier. Within as little as 30 minutes of severe coronary ischemia, as occurs after a myocardial infarct, about half of the adenine base can be lost from the affected cardiac muscle cells. Furthermore, this loss can be replaced by new synthesis of adenine at a rate of only 2%/hour. Therefore, once a serious bout of coronary ischemia has persisted for 30 minutes or longer, relief of the ischemia may be too late to prevent injury and death of the cardiac cells. This is almost certainly one of the major causes of cardiac cellular death during myocardial ischemia. About 35% of people in the United States aged 65 years and older die of this cause. Some deaths occur suddenly as a result of acute coronary occlusion or fibrillation of the heart, whereas other deaths occur slowly over a period of weeks to years as a result of progressive weakening of the heart pumping process. In this articler, we discuss acute coronary ischemia caused by acute coronary occlusion and myocardial infarction. In Chapter 22, we discuss congestive heart failure, which is frequently caused by slowly increasing coronary ischemia and weakening of the cardiac muscle. Most importantly, under resting conditions, cardiac muscle normally consumes more fatty acids than carbohydrates to supply its energy (70% of the energy is derived from fatty acids). However, as is also true of other tissues, under anaerobic or ischemic conditions, cardiac metabolism must call on anaerobic glycolysis mechanisms for energy. However, glycolysis consumes large quantities of the blood glucose and, at the same time, forms large 264 flow is atherosclerosis. The atherosclerotic process is discussed in connection with lipid metabolism in Chapter 69. Briefly, in people who have a genetic predisposition to atherosclerosis, who are overweight or obese and have a sedentary lifestyle, or who have high blood pressure and damage to the endothelial cells of the coronary blood vessels, large quantities of cholesterol gradually become deposited beneath the endothelium at many points in arteries throughout the body. Gradually, these areas of deposit are invaded by fibrous tissue and frequently become calcified. The net result is the development of atherosclerotic plaques, which actually protrude into the vessel lumens Chapter 21 Muscle Blood Flow and Cardiac Output During Exercise and block or partially block blood flow. A common site for development of atherosclerotic plaques is the first few centimeters of the major coronary arteries. The atherosclerotic plaque can cause a local blood clot called a thrombus that occludes the artery. The thrombus usually occurs where the arteriosclerotic plaque has broken through the endothelium, thus coming into direct contact with the flowing blood. Because the plaque presents an unsmooth surface, blood platelets adhere to it, fibrin is deposited, and red blood cells become trapped to form a blood clot that grows until it occludes the vessel. Occasionally, the clot breaks away from its attachment on the atherosclerotic plaque and flows to a more peripheral branch of the coronary arterial tree, where it blocks the artery at that point. A thrombus that flows along the artery in this way and occludes the vessel more distally is called a coronary embolus. Many clinicians believe that local muscular spasm of a coronary artery also can occur. The spasm might result from direct irritation of the smooth muscle of the arterial wall by the edges of an arteriosclerotic plaque, or it might result from local nervous reflexes that cause excess coronary vascular wall contraction. In a normal heart, almost no large communications exist among the larger coronary arteries. When a sudden occlusion occurs in one of the larger coronary arteries, the small anastomoses begin to dilate within seconds. However, the blood flow through these minute collaterals is usually less than half of that needed to keep most of the cardiac muscle alive that they now supply. The diameters of the collateral vessels do not enlarge much more for the next 8 to 24 hours. Then, however, collateral flow begins to increase, doubling by the second or third day and often reaching normal or almost normal coronary flow within about 1 month. Because of these developing collateral channels, many patients recover almost completely from various degrees of coronary occlusion when the area of muscle involved is not too large. When atherosclerosis constricts the coronary arteries slowly over a period of many years, rather than suddenly, collateral vessels can develop at the same time, while the atherosclerosis becomes more and more severe. Therefore, the person may never experience an acute episode of cardiac dysfunction. Eventually, however, the sclerotic process develops beyond the limits of even the collateral blood supply to provide the needed blood flow, and sometimes, the collateral blood vessels themselves develop atherosclerosis. When this occurs, the heart muscle becomes severely limited in its work output, and the heart cannot pump even normally required amounts of blood flow. Myocardial Infarction Immediately after an acute coronary occlusion, blood flow ceases in the coronary vessels beyond the occlusion, except for small amounts of collateral flow from surrounding vessels. The area of muscle that has zero flow or so little flow that it cannot sustain cardiac muscle function is said to be infarcted. Soon after the onset of the infarction, small amounts of collateral blood begin to infiltrate the infarcted area, which, combined with progressive dilation of local blood vessels, causes the area to become overfilled with stagnant blood. Simultaneously the muscle fibers use the last bits of the oxygen in the blood, causing the hemoglobin to become totally deoxygenated. Therefore, the infarcted area takes on a bluish-brown hue, and the blood vessels of the area appear to be engorged, despite lack of blood flow. In comparison, about 8 ml oxygen/100 g are delivered to the normal resting left ventricle each minute. Therefore, if there is even 15% to 30% of normal resting coronary blood flow, the muscle will not die. In the central portion of a large infarct, however, where there is almost no collateral blood flow, the muscle does die. The subendocardial mus- Normal contraction Nonfunctional muscle cle frequently becomes infarcted, even when there is no evidence of infarction in the outer surface portions of the heart. This occurs because the subendocardial muscle has a higher oxygen consumption and extra difficulty obtaining adequate blood flow because the blood vessels in the subendocardium are intensely compressed by systolic contraction of the heart, as explained earlier. Therefore, any condition that compromises blood flow to any area of the heart usually causes damage first in the subendocardial regions, and the damage then spreads outward toward the epicardium. When some of the cardiac muscle fibers more than 40% of the left ventricle is infarcted, and death occurs in more than 70% of patients once cardiac shock develops. That is, when the normal portions of the ventricular muscle contract, the ischemic portion of the muscle, whether it is dead or simply nonfunctional, instead of contracting is forced outward by the pressure that develops inside the ventricle. Therefore, much of the pumping force of the ventricle is dissipated by bulging of the area of nonfunctional cardiac muscle. When the heart becomes incapable of contracting with sufficient force to pump enough blood into the peripheral arterial tree, cardiac failure and death of peripheral tissues ensue as a result of peripheral ischemia. This condition, called coronary shock, cardiogenic shock, cardiac shock, or low cardiac output failure, is discussed more fully in the next chapter. Cardiac shock almost always occurs when 266 When the heart is not pumping blood forward, it must be damming blood in the atria and in the blood vessels of the lungs or in the systemic circulation. Damming of blood in the veins often causes little difficulty during the first few hours after a myocardial infarction. Instead, symptoms develop a few days later because the acutely diminished cardiac output leads to diminished blood flow to the kidneys. Then, for reasons discussed in Chapter 22, the kidneys fail to excrete enough urine. This adds progressively to the total blood volume and, therefore, leads to congestive symptoms. Consequently, many patients who seemingly are getting along well during the first few days after the onset of heart failure will suddenly experience acute pulmonary edema and often will die within a few hours after the appearance of the initial pulmonary symptoms. In many people who die of coronary occlusion, death occurs because of sudden ventricular fibrillation. The tendency for fibrillation to develop is especially great after a large infarction, but fibrillation can sometimes occur after small occlusions as well. Some patients with chronic coronary insufficiency die suddenly of fibrillation without having any acute infarction. Chapter 21 Muscle Blood Flow and Cardiac Output During Exercise Fibrillation is most likely to occur during two especially dangerous periods after coronary infarction. Then, there is a short period of relative safety, followed by a second period of cardiac irritability beginning 1 hour or so later and lasting for another few hours.