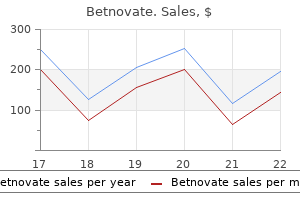
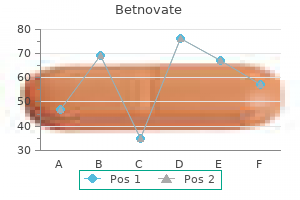
Betnovate 20gm sale
Laboratory diagnosis is mandatory since only 50% of dystrophic nails are due to dermatophytosis skin care 60 discount betnovate 20gm amex. Periodic acid Schiff stain of a histologic section of the nail plate will also demonstrate the fungus readily. Each technique is positive in only 50% of cases so several different tests may need to be performed. Onychomycosis is difficult to treat because of the long duration of therapy required and the frequency of recur rences. For toenails, treatment is indicated for patients with discomfort, inability to exercise, diabetes, and immune compromise. Although historically topical therapy has had limited value, efinaconazole 10% has been approved as a topical therapy; preliminary evidence suggests that it per forms better than prior topical treatment options. Tavaborole 5% solution has also been approved for the treatment of onychomycosis, but its clearance rates do not appear to be as good as those of efinaconazole. Adjunctive value of surgical procedures is unproven, and the efficacy of laser treatments is lacking, especially with regard to long-term cures. Fingernails can virtually always be cured, and toenails are cured 35-50% of the time and are clinically improved about 75% of the time. The costs of the various treatment options should be known and the most cost effective treatment chosen. Ketoconazole, due to its higher risk for hepato toxicity, is not recommended to treat any form of ony chomycosis. For fingernails, ultramicronized griseofulvin 250 mg orally three times daily for 6 months can be effec tive. Differential Diag nosis Onychomycosis may cause nail changes identical to those seen in psoriasis. Careful examination for more characteris tic lesions elsewhere on the body is essential to the diagnosis of the nail disorders. Cancer should be suspected (eg, Bowen disease or squamous cell carcinoma) as the cause of any persistent solitary subungual or periungual lesion. Off-label use of fluconazole, 400 mg once weekly for 6 months, can also be effective, but there is limited evidence for this option. Liver function tests and a complete blood count with plate lets are performed monthly during treatment. Pulse oral itraconazole 200 mg twice daily for l week per month for 3 months is inferior to standard terbinafine treatments, but it is an acceptable alternative for those unable to take terbinafine. The courses of terbinafine or itraconazole may need to be repeated 6 months after the first treatment cycle if fungal cultures of the nail are still positive. Pharmacogenetic testing is becoming increas ingly utilized to predict who is at risk for and therefore should avoid certain medication exposures. Simple drug erup tions involve an exanthem, usually appear in the second week of medication therapy, and have no associated consti tutional or laboratory findings. Antibiotics, including the penicillins and quinolones, are the most common causes. These may include fevers, chills, hematologic abnormalities (especially eosinophilia), and abnormal liver or kidney function. Table 6-3 summarizes the types of skin reactions, their appearance and distribution, and the common offenders in each case. Laboratory Findings Routinely ordered blood work is of no value in the diagno sis of simple drug eruptions. Constitutional sym ptoms (ma laise, a rthra lgia, headache, and fever) may be present. General Considerations Only a minority of cutaneous drug reactions result from allergy. Rashes are among the most common adverse reac tions to medications and occur in 2-3% of hospitalized patients. Calcium channel blockers are a common cause of pruritus and eczemas in the elderly. Differential Diag nosis Observation after discontinuation, which may be a slow process, helps establish the diagnosis. Rechallenge, though of theoretical value, may pose a danger to the patient and is best avoided. Complications Some cutaneous drug reactions may be associated with visceral involvement. Most common is an infectious mononucleosis-like illness and hepatitis associated with administration of anticonvulsants. Myo carditis may be a serious complication of drug-induced hypersensitivity syndrome. Reaction Appearance Distribution and Comments Common Offenders Drug exa nthem Morbill iform, maculopapular, exa nthematous reactions. Other morphologies include u rticaria that lasts over 24 hours, vesicles, bul lae, or necrotic ulcers. Exposed skin of the face, the neck, and the backs of the hands and, i n women, the lower legs. Di ltiazem, eta nercept, hyd rochloroth iazide, infl iximab, lisi nopril, terbi nafine. Pruritic, erythematous to violaceous polygonal papules that coalesce or expand to form plaques. Urticaria Red, itchy wheals that va ry in size from less than 1 em to many centi meters. Di ltiazem causes facial hyperpig mentation that may be d ifficult to d isti nguish from melasma. Pityriasis rosea-like eruptions Oval, red, slig htly raised patches with central sca le. Barbitu rates, bism uth, ca ptopril, clonidi ne, methopromazi n e, metoprolol, metronidazole, and tripelennamine. General Measures Systemic manifestations are treated as they arise (eg, anemia, icterus, purpura). Severe cutaneous adverse reactions: impact of immunology, genetics, and pharmacology. Prognosis Drug rash usually disappears upon withdrawal of the medication and proper treatment. Use of a pinhole will overcome most refractive errors and thus allows their identification as a cause of reduced visual acuity. Reduction of Rate of Progression of Nearsightedness Topical atropine and pirenzepine, a selective muscarinic antagonist; rigid contact lens wear during sleep (orthokera tology); and various types of soft contact lenses and spectacles reduce the rate of progression of nearsightedness but their long-term efficacy and safety are uncertain. Drug-eluting lenses are used to treat diseases of the cornea, conjunctiva, or lids. The major risk from contact lens wear is bacterial, amebic, or fungal corneal infection, potentially a blinding condition. Such infections occur more commonly with soft lenses, particularly extended wear, for which there is at least a fivefold increase in risk of corneal ulceration com pared with daily wear. Contact lens wearers, especially those using lenses for cosmesis, should be made aware of the risks they face and ways to minimize them, such as avoiding overnight wear or use of lenses past their replace ment date and maintaining meticulous lens hygiene, including not using tap water or saliva for lens cleaning. Surgery Various surgical techniques are available to reduce refrac tive errors, particularly nearsightedness. Laser corneal refractive surgery reshapes the middle layer (stroma) of the cornea with an excimer laser. When to Refer Any contact lens wearer with an acute painful red eye must be referred emergently to an ophthalmologist. Internal hordeolum is a meibomian gland abscess that usually points onto the con junctival surface of the lid; external hordeolum or sty usu ally is smaller and on the margin. Chalazion Chalazion is a common granulomatous inflammation of a meibomian gland that may follow an internal hordeolum. It is characterized by a hard, nontender swelling on the upper or lower lid with redness and swelling of the adjacent conjunctiva. Treatment is usually by incision and curettage but corticosteroid injection may also be effective.
Buy generic betnovate canada
Pain due to cervical or thoracic disk disease involves the outer or dorsal aspect of the arm and the thumb and index fingers rather than the ring and little fingers acne during pregnancy cheap betnovate generic. Reflux esophagitis, peptic ulcer, chronic cholecystitis, esophageal spasm, and functional gastrointestinal disease may produce pain suggestive of angina pectoris. The pic ture may be especially confusing because ischemic pain may also be associated with upper gastrointestinal symp toms, and esophageal motility disorders may be improved by nitrates and calcium channel blockers. Degenerative and inflammatory lesions of the left shoulder and thoracic outlet syndromes may cause chest pain due to nerve irritation or muscular compression; the symptoms are usually precipitated by movement of the arm and shoulder and are associated with paresthesias. Pneumonia, pulmonary embolism, and spontaneous pneumothorax may cause chest pain as well as dyspnea. Dissection of the thoracic aorta can cause severe chest pain that is commonly felt in the back; it is sudden in onset, reaches maximum intensity immediately, and may be asso ciated with changes in pulses. The main limitation to long-term nitrate therapy is tolerance, which can be limited by using a regimen that includes a minimum 8- to 10-hour period per day without nitrates. Isosorbide dini trate can be given three times daily, with the last dose after dinner, or longer-acting isosorbide mononitrate once daily. Treatment Sublingual nitroglycerin is the drug of choice for acute management; it acts in about 1-2 minutes. As soon as the Beta-blockers are the only antianginal agents that have been demonstrated to prolong life in patients with coro nary disease (post-myocardial infarction). Dieta ry su pplement niacin must not be used as a substitute for prescription niacin. The pharmacology and side effects of the beta-blockers are discussed in Chapter 1 1 (see Table 1 1 -6). The major contraindications are severe bronchospastic disease, brady arrhythmias, and decompensated heart failure. It has been shown to reduce angina in patients with chronic stable angina and is approved in Europe. Alternative and Combination Therapies Ranolazine is indicated as first-line use for chronic angina. It also decreases occurrence of atrial fibrillation and results in a small decrease in HbA1. Ranolazine does not improve out comes of patients who do not get complete coronary revascularization. Calcium Channel Blocking Agents Patients who do not respond to one class of antianginal medication often respond to another. It may, therefore, be worthwhile to use an alternative agent before progressing to combinations. The stable ischemic heart disease guide lines recommend starting with a beta-blocker as initial therapy, followed by calcium channel blockers, long-acting nitrates, or ranolazine. Platelet-Inhibiting Agents Unlike the beta-blockers, calcium channel blockers have not been shown to reduce mortality postinfarction and in some cases have increased ischemia and mortality rates. Meta-analyses have suggested that short-act ing nifedipine in moderate to high doses causes an increase in mortality. It is uncertain whether these findings are rel evant to longer-acting dihydropyridines. Nevertheless, considering the uncertainties and the lack of demonstrated favorable effect on outcomes, calcium channel blockers should be considered third-line anti-ischemic drugs in the postinfarction patient. The pharmacologic effects and side effects of the cal cium channel blockers are discussed in Chapter 1 1 and summarized in Table 1 1 -8. Diltiazem, amlodipine, and verapamil are preferable because they produce less reflex tachycardia and because the former, at least, may cause fewer side effects. Isradipine, felodipine, and nisoldipine are not approved for angina but probably are as effective as the other dihydropyridines. Several studies have demonstrated the benefit of antiplate let drugs for patients with stable and unstable vascular disease. Therefore, unless contraindicated, aspirin (81-325 mg orally daily) should be prescribed for all patients with angina. Clopidogrel, 75 mg orally daily, reduces vascular events in patients with stable vascular disease (as an alter native to aspirin) and in patients with acute coronary syn dromes (in addition to aspirin). However, it might be reasonable to use combination clopidogrel and aspirin for certain high-risk patients with established coronary disease. Specifically, prolonged used of dual antiplatelet therapy with aspirin and clopidogrel may be beneficial in patients post-percutaneous stenting with drug-eluting stents. Ticagrelor, a P2Y12 inhibitor, has been shown to reduce cardiovascular events in patients with acute coronary syn dromes. Additionally, in patients with prior myocardial infarction, long-term treatment with ticagrelor plus aspirin reduced cardiovascular events compared to aspirin alone. It is contraindicated for patients with a history of stroke or transient ischemic attack due to increased risk of intracranial hemorrhage. Risk Reduction Patients with coronary disease should undergo aggressive risk factor modification. For patients with diabe tes and cardiovascular disease, there is uncertainty about the optimal target blood sugar control. Therefore, tight blood sugar control should be avoided particularly in patients with a history of severe hypoglycemia, long-standing diabetes, and advanced vas cular disease. Indications- There is general agreement that otherwise healthy patients in the following groups should undergo revascularization: (1) Patients with unacceptable symp toms despite medical therapy to its tolerable limits. Experienced operators are able to successfully dilate more than 90% of lesions attempted. The major early complication is intimal dissection with vessel occlu sion, although this is rare with coronary stenting. The definition of a periprocedural infarc tion has been debated, with many experts advocating for a clinical definition that incorporates different enzyme cut points, angiographic findings, and electrocardiographic evidence. Factors associated with higher restenosis rates include diabetes, small luminal diameter, longer and more complex lesions, and lesions at coronary ostia or in the left anterior descending coronary artery. Drug-eluting stents that elute antiproliferative agents, such as sirolimus, evero limus, zotarolimus, or paclitaxel, have substantially reduced restenosis. In -stent restenosis is often treated with restent ing with drug-eluting stents, and rarely with brachytherapy. Coronary stenting, with either bare metal stents or drug-eluting stents, has substantially reduced restenosis. However, it should be noted that less than 20% of patients with multivessel disease meet the entry criteria for the clinical trials, so these results cannot be generalized to all multivessel disease patients. Grafts using one or both internal mammary arteries (usually to the left anterior descending artery or its branches) provide the best long-term results in terms of patency and flow. Segments of the saphenous vein (or, less optimally, other veins) or the radial artery interposed between the aorta and the coronary arteries distal to the obstructions are also used. They are more technically demanding, usually not suitable for more than two grafts, and do not have established durability. Bypass surgery can be performed both on circulatory support (on-pump) and without direct circulatory support (off pump). Randomized trial data have not shown a benefit with off-pump bypass surgery but minimally invasive surgical techniques allow earlier postoperative mobiliza tion and discharge. Patients over 70 years of age, patients undergoing repeat procedures, or those with important noncardiac disease (especially chronic kidney disease and diabetes) or poor general health also have higher operative mortality and morbidity rates, and full recovery is slow. Early (1 -6 months) graft patency rates average 85-90% (higher for internal mammary grafts), and subsequent graft closure rates are about 4% annually. Early graft failure is common in vessels with poor distal flow, while late closure is more frequent in patients who continue smoking and those with untreated hyperlipidemia. Smoking cessation and vigor ous treatment of blood lipid abnormalities (particularly with statins) are necessary. Repeat revascularization may be necessitated because of recurrent symptoms due to pro gressive native vessel disease and graft occlusions. Reop eration is technically demanding and less often fully - successful than the initial operation. Mechanical Extracorporeal Counterpulsation Extracorporeal counterpulsation entails repetitive inflation of a high-pressure chamber surrounding the lower half of the body during the diastolic phase of the cardiac cycle for daily 1 -hour sessions over a period of 7 weeks.
Cheap betnovate 20gm with visa
Magnesium hydroxide acne 6 weeks postpartum purchase betnovate 20 gm with amex, nondigestible carbohy drates (sorbitol, lactulose), and polyethylene glycol are all efficacious and safe for treating acute and chronic cases. Magnesium-containing saline laxatives should not be given to patients with chronic renal insufficiency. Polyethylene glycol 3350 (Miralax) is a component of solutions traditionally used for colonic lavage prior to colonoscopy and does not cause flatulence. When used in conventional doses, the onset of action of these osmotic agents is generally within 24 hours. For more rapid treatment of acute constipation, purgative laxatives may be used, such as magnesium citrate. These agents stimulate fluid secre tion and colonic contraction, resulting in a bowel movement within 6 - 1 2 hours after oral ingestion or 1 5-60 minutes after rectal administration. In multicenter controlled trials, patients treated with lubiprostone 24 meg orally twice daily or lina clotide 145 meg once daily increased the number of bowel movements compared with patients treated with placebo. Because these agents are expensive, they should be reserved for patients who have suboptimal response or side effects with less expensive agents. Patients with alarm symptoms or who are over age 50 should be referred for colonoscopy. Rarely, surgery (subtotal colectomy) is required for patients with severe colonic inertia. American Gastroenterological Association medical position statement on constipation. Validation of the balloon evacuation test: reproducibility and agreement with findings from anorectal manometry and electromyography. A randomized, placebo-controlled trial of lubi prostone for opioid-induced constipation in chronic noncancer pain. Belching is a normal reflex and does not itself denote gastrointestinal dysfunction. With each swallow, 2-5 mL of air is ingested, and exces sive amounts may result in distention, flatulence, and abdom ina! This may occur with rapid eating, gum chewing, smoking, and the ingestion of carbonated beverages. Evalua tion should be restricted to patients with other complaints such as dysphagia, heartburn, early satiety, or vomiting. Chronic excessive belching is almost always caused by supragastric belching (voluntary diaphragmatic contraction, followed by upper esophageal relaxation with air inflow to the esophagus) or true air swallowing (aerophagia), both of which are behavioral disorders that are more common in patients with anxiety or psychiatric disorders. However, many patients have impaired small bowel gas propulsion or enhanced visceral sensitivity to gas distention. Many of these patients have an underlying functional gastrointestinal disorder such as irritable bowel syndrome or functional dyspepsia. Rifaximin, 400 mg twice daily, a nonabsorbable oral antibi otic with high activity against enteric bacteria, has been shown to reduce abdominal bloating and flatulence in approximately 40% of treated patients compared with 20% of controls. Symptom improvement may be attributable to suppression of gas-producing colonic bacteria; however, relapse commonly occurs within days after stopping the antibiotic. Further trials are needed to clarify the role of nonabsorbable antibiotics in symptom management. Many patients report reduced flatus production with use of pro biotics, although there has been limited controlled study of these agents for this purpose. Patients interested in com plementary medical therapies may be offered a trial of 4-8 ounces daily of Kefir, a commercially available fermented milk drink containing multiple probiotics. Anal gas evacuation and colonic microbiota in patients with flatulence: effect of diet. Flatus is derived from two sources: swallowed air (primarily nitrogen) and bacterial fermenta tion of undigested carbohydrate (which produces H 2, C0 2, and methane). These include lactose (dairy products); fructose (fruits, corn syrups, and some sweeteners); polypols (stone-fruits, mushrooms, and some sweeteners); and fructans (legumes, cruciferous vegetables, pasta, and whole grains). Abnormal gas production may be caused by increased ingestion of these carbohydrates or, less commonly, by disorders of malabsorption. Foul odor may be caused by garlic, onion, eggplant, mushrooms, and certain herbs and spices. Patients with a long-standing history of flatu lence and no other symptoms or signs of malabsorption disorders can be treated conservatively. Lactose intolerance may be assessed by a 2-week trial of a lactose-free diet or by a hydrogen breath test. The colon absorbs most of the remaining fluid, with less than 200 mL lost in the stool. Although diarrhea sometimes is defined as a stool weight of more than 200-300 g/24 h, quan tification of stool weight is necessary only in some patients with chronic diarrhea. In clinical practice, it is helpful to distinguish acute from chronic diarrhea, as the evaluation and treatment are entirely different (Tables 1 5-5 and 1 5-6). Noninflammatory Diarrhea Viral Noroviruses Rotavirus Protozoa l Giardia Iamblia Cryptosporidium Cyclospora Bacterial 1. Preformed enterotoxin prod uction Staphylococcus au reus Bacillus cereus Clostridium perfringens 2. Parasites: Giardia Iamblia, Entamoeba histolytica, Strongyloidiasis stercora/is, Capillaria philippinensis 2. Etiology & Clinical Findings Diarrhea acute in onset and persisting for less than 2 weeks is most commonly caused by infectious agents, bacterial toxins (either preformed or produced in the gut), or medi cations. Community outbreaks (including nursing homes, schools, cruise ships) suggest a viral etiology or a common food source. Day care attendance or exposure to unpurified water (camp ing, swimming) may result in infection with Giardia or Cryptosporidium. Antibiotic administration within the preceding several weeks increases the likelihood of C difficile colitis. The nature of the diarrhea helps distinguish among dif ferent infectious causes (Table 1 5-5). Infectious dysentery must be distinguished from acute ulcerative colitis, which may also present acutely with fever, abdominal pain, and bloody diarrhea. Diarrhea that per sists for more than 1 4 days is not attributable to bacterial pathogens (except for C diff i cile) and should be evaluated as chronic diarrhea. Evaluation In over 90% of patients with acute noninflammatory diar rhea, the illness is mild and self-limited, responding within 5 days to simple rehydration therapy or antidiarrheal agents; diagnostic investigation is unnecessary. The isolation rate of bacterial pathogens from stool cultures in patients with acute noninflammatory diarrhea is under 3%. Thus, the goal of initial evaluation is to distin guish patients with mild disease from those with more serious illness. If diarrhea worsens or persists for more than 7 days, stool should be sent for fecal leukocyte or lactoferrin determination, ovum and parasite evaluation, and bacterial culture. Hospitalization is required in patients with severe dehydration, organ failure, marked abdominal pain, or altered mental status. For bloody stools, the laboratory should be directed to perform serotyping for Shiga-toxin-producing E coli. In patients who are hospitalized or who have a history of antibiotic exposure, a stool sample should be tested for C difficile toxin. In patients with diarrhea that persists for more than 10 days, who have a history of travel to areas where amebia sis is endemic, or who engage in oral-anal sexual practices, three stool examinations for ova and parasites should also be performed. The stool antigen detection tests for both Giardia and Entamoeba histolytica are more sensitive than stool microscopy for detection of these organisms. Although typically mild, the diarrhea (which originates in the small intestine) can be voluminous and result in dehydration with hypokalemia and metabolic acidosis (eg, cholera). Because these organisms predominantly involve the colon, the diar rhea is small in volume (less than 1 L! Fecal leukocytes or lactoferrin usually are present in infec tions with invasive organisms. E coli 0 1 57:H7 is a Shiga toxin-producing noninvasive organism most commonly acquired from contaminated meat that has resulted in sev eral outbreaks of an acute, often severe hemorrhagic colitis. Fluids should be given at rates of 50-200 mL/kg/24 h depending on the hydration status. Intravenous fluids (lac tated Ringer injection) are preferred in patients with severe dehydration. Diet Most mild diarrhea will not lead to dehydration provided the patient takes adequate oral fluids containing carbohydrates and electrolytes. Patients find it more comfortable to rest the bowel by avoiding high-fiber foods, fats, milk products, caf feine, and alcohol.

Purchase 20 gm betnovate with mastercard
If symptoms improve and cessation of therapy leads to symptoms again skin care summer betnovate 20gm sale, then a proton pump inhibitor is resumed at the lowest dose effective for remission, usually daily but at times on a demand basis. Although H 2 -receptor antagonists are an alternative to proton pump inhibitors, they are generally both less clinically effective and less cost-effective. Twenty-four-hour pH monitoring of the pharynx should best document laryngopharyngeal reflux and is advocated by some as the initial management step, but it is costly, more difficult, and less available than lower esophageal monitoring alone. Double pH probe (proximal and distal esophageal probes) testing is the best option for evaluation, since lower esophageal pH monitoring alone does not cor relate well with laryngopharyngeal reflux symptoms. Oro pharyngeal pH probe testing is available, but its ability to predict response to reflux treatment in patients with laryn gopharyngeal reflux is not known. The challenge of protocols for reflux disease: a review and development of a critical pathway. Repeated laser vaporizations or cold knife resec tions via operative laryngoscopy are the mainstay of treat ment. Severe cases can cause airway compromise even in adults and may require treatment as often as every 6 weeks to maintain airway patency. Tracheotomy should be avoided, if pos sible, since it introduces an additional squamociliary junc tion for which papillomas appear to have an affinity. Interferon treatment has been under investigation for many years but is only indicated in severe cases with pul monary involvement. Rarely, cases of malignant transfor mation have been reported (often in smokers), but recurrent respiratory papillomatosis should generally be thought of as a benign condition. Cidofovir (a cytosine nucleotide analog in use to treat cytomegalovirus retinitis) has been used with success as intralesional therapy for recurrent respiratory papillomatosis. Because cidofovir causes adenocarcinomas in laboratory animals, its poten tial for carcinogenesis is being monitored. Recurrent respiratory papillomatosis: a com plex defect in immune responsiveness to human papillomavi rus-6 and - 1 1. Prognostic factors of recurrent respiratory papillomatosis from a registry of 72 patients. Trau matic Lesions of the Voca l Folds Vocal fold nodules are smooth, paired lesions that form at the junction of the anterior one-third and posterior two thirds of the vocal folds. While nearly all true nodules will resolve with behavior modification, recalcitrant nodules may require surgical excision. Vocal fold polyps are unilateral masses that form within the superficial lamina propria of the vocal fold. They are related to vocal trauma and seem to follow resolu tion of vocal fold hemorrhage. Small, sessile polyps may resolve with conservative measures, such as voice rest and corticosteroids, but larger polyps are often irreversible and require operative removal to restore normal voice. Vocal fold cysts are also considered traumatic lesions of the vocal folds and are either true cysts with an epithelial lining or pseudocysts. They typically form from mucus secreting glands on the inferior aspect of the vocal folds. Cysts may fluctuate in size from week to week and cause a variable degree of hoarseness. They rarely, if ever, resolve completely and may leave behind a sulcus, or vocal fold scar, if they decompress or are marsupialized. Polypoid corditis is different from vocal fold polyps and may form from loss of elastin fibers and loosening of the intracellular junctions within the lamina propria. This loss allows swelling of the gelatinous matrix of the superfi cial lamina propria (called Reinke edema). These changes in the vocal folds are strongly associated with smoking, but also with vocal abuse, chemical industrial irritants, and hypothyroidism. While this problem is common in both male and female smokers, women seem more troubled by the characteristic decline in modal pitch caused by the increased mass of the vocal folds. If the patient stops smok ing or the lesions cause stridor and airway obstruction, surgical resection of the hyperplastic vocal fold mucosa may be indicated to improve the voice or airway, or both. A common but often unrecognized cause of hoarseness and odynophonia are contact ulcers or their close relatives, granulomas. Both lesions form on the vocal processes of the arytenoid cartilages, and patients often can correctly inform the clinician which side is affected. The cause of these ulcers and granulomas is disputed, but they are clearly related to trauma and may be related to exposure of the underlying perichondrium. Epiglottitis Epiglottitis (or, more correctly, supraglottitis) should be suspected when a patient presents with a rapidly develop ing sore throat or when odynophagia (pain on swallowing) is out of proportion to apparently minimal oropharyngeal findings on examination. Rarely in the era of H influenzae type b vaccine is this bacterium isolated in adults. Unlike in children, indirect laryngoscopy is generally safe and may demonstrate a swollen, erythema tous epiglottis. Lateral plain radiographs may demonstrate an enlarged epiglottis (the epiglottis "thumb sign"). Initial treatment is hospitalization for intravenous antibiotics eg, ceftizoxime, 1-2 g intravenously every 8 - 1 2 hours; or cefuroxime, 750- 1 500 mg intravenously every 8 hours; and dexamethasone, usually 4- 1 0 mg as initial bolus, then 4 mg intravenously every 6 hours-and observation of the air way. Similarly, substitution of oral antibiotics may be appropriate to complete a 10-day course. Chronic ulceration or granuloma formation has been asso ciated with gastroesophageal reflux but is also common in patients with muscle tension dysphonia. Treatment is often multimodal, and an inhaled corticosteroid (eg, fluticasone 440 meg twice daily) may be the most effective pharmaco logic therapy. Adjunct treatment measures include proton pump inhibitor therapy (omeprazole 40 mg orally twice daily, or equivalent) and voice therapy with special atten tion to vocal hygiene. Laryngeal cancer is very treatable and early detection is the key to maximizing posttreatment voice, swallowing, and breathing function. Symptoms and Signs A change in voice quality is most often the presenting com plaint, although throat or ear pain, hemoptysis, dysphagia, weight loss, and airway compromise may occur. B ecause of their early impact on vocal quality, glottic cancers are among the smallest detectable human malignancies and treatment success is very high with early lesions. Neck metastases are not common in early glottic (true vocal fold) cancer in which the vocal folds are mobile, but a third of patients in whom there is impaired fold mobility will also have involved lymph nodes at neck dissection. Supra glottic carcinoma (false vocal folds, aryepiglottic folds, epiglottis), on the other hand, often metastasizes to both sides of the neck early in the disease. Complete head and neck examination, including laryngoscopy, by an experi enced clinician is mandated for any person with the con cerning symptoms listed under Essentials of Diagnosis. La ryngeal Leu koplakia Leukoplakia of the vocal folds is commonly found in asso ciation with hoarseness in smokers. In some cases, invasive squamous cell carcinoma is present in the initial biopsy specimen. Some patients-estimated to be less than 5% of those with mild dysplasia and about 35-60% of those with severe dysplasia-will subsequently develop squamous cell carci noma. Treatment options include close follow-up with laryngovideostroboscopy, serial resection, and external beam radiation therapy. Despite their cost and the lack of any evidence for their use in the treatment of leukoplakia, proton pump inhibitors have become the mainstay of treat ment for these lesions. Imaging evaluates neck nodes, tumor volume, and cartilage sclerosis or destruction. Formal cardio pulmonary evaluation may be indicated, especially if partial laryngeal surgery is being considered. All partial laryngectomy candidates should have good to excellent lung function and exercise tolerance because chronic microaspiration may be expected following the procedure. Biopsy Diagnosis is made by biopsy at the time of laryngoscopy when true fold mobility and arytenoid fixation, as well as surface tumor extent, can be evaluated. Most otolaryngolo gists recommend esophagoscopy and bronchoscopy at the same time to exclude synchronous primary tumor. General Considerations Squamous cell carcinoma of the larynx, the most common malignancy of the larynx, o ccurs almost exclusively in patients with a history of significant tobacco use. In addition to the late complications, clinicians have noted that the over all success in the treatment of larynx cancer has declined in parallel with the increase in organ preservation chemora diation therapy over the past 20 years.

Diseases
- Apraxia, ocular motor, Cogan type
- Irritable bowel syndrome
- Ulbright Hodes syndrome
- Woolly hair hypotrichosis everted lower lip outstanding ears
- Yellow nail syndrome
- Psittacosis
- Vestibulocochlear dysfunction progressive familial
- Yersiniosis
20 gm betnovate free shipping
Anaerobic pneumonia and lung abscess can occur in both hospital and community settings and warrant separate consideration acne 9dpo generic 20 gm betnovate with mastercard. Treatment Constrictive bronchiolitis is relatively unresponsive to corticosteroids and is frequently progressive. Corticoste roids are effective in two-thirds of patients with prolifera tive bronchiolitis, and improvement can be prompt. The dose is then tapered slowly to 20-40 mg/day, depending on the response, and weaned over the subsequent 3-6 months as tolerated. Relapses are common if corticosteroids are stopped prematurely or tapered too quickly. Fever or hypothermia, tachypnea, cough with or without sputum, dyspnea, chest d iscomfort, sweats or rigors (or both). It is the deadliest infectious disease in the United States and the eighth leading cause of death. Sputum examination may be helpful in selected patients but 40% of patients cannot produce an evaluable sputum sample and Gram stain and culture lack sensitivity for the most common causes of pneumonia. Budesonide/forrnoterol for bronchiolitis obliter ans after hematopoietic stern cell transplantation. Clin ical Setting Com plications Organism; Appearance on Smear of Sputum Streptococcus pneumoniae (pneumo coccus). Such treatment improves initial antibiotic coverage, reduces unnecessary hospitalization, and appears to improve 30-day survival. It may also be diagnosed in a pre viously ambulatory patient within 48 hours after admission to the hospital. Pulmonary defense mechanisms (cough reflex, mucocili ary clearance system, immune responses) normally prevent the development of lower respiratory tract infections follow ing aspiration of oropharyngeal secretions containing bacte ria or inhalation of infected aerosols. C pneumoniae, S aureus, Neisseria meningitidis, M catarrhalis, Klebsiella pneumoniae, other gram-negative rods, and Legio nella species. A detailed assessment of epidemiologic risk fac tors may aid in diagnosing pneumonias due to the following uncommon causes: Chlamydophila psittaci (psittacosis), Coxiella burnetii (Q fever), Francisella tularensis (tularemia), endemic fungi (Blastomyces, Coccidioides, Histoplasma), and sin nombre virus (hantavirus pulmonary syndrome). A macrolide (clarithromycin, 500 mg ora l ly twice a day; or azithromycin, 500 mg orally as a fi rst dose and then 250 mg orally daily for 4 days, or 500 mg orally daily for 3 days), or b. A respiratory fl uoroquinolone (moxifloxacin, 400 mg ora l ly daily; gem ifloxacin, 320 mg orally dai ly; levofloxacin, 750 mg orally daily) or b. For i ntravenous thera py, moxifloxacin, 400 mg dai ly; l evofloxacin, 750 mg dai ly; ciprofloxacin, 400 mg every 8- 1 2 hours or 2. Other common symptoms include sweats, chills, rigors, chest discomfort, pleurisy, hemoptysis, fatigue, myalgias, anorexia, headache, and abdominal pain. Common physical findings include fever or hypother mia, tachypnea, tachycardia, and arterial oxygen desatura tion. Dullness to percussion may be observed if lobar consolidation or a parapneumonic pleural effusion is pres ent. In ambulatory outpa tients whose presentation (travel history, exposure) sug gests an etiology not covered by standard therapy (eg, Coccidioides) or public health concerns (eg, Mycobacterium tuberculosis, influenza), diagnostic testing is appropriate. Diagnostic testing results are used to guide initial anti biotic therapy, permit adjustment of empirically chosen therapy to a specific infectious cause or resistance pattern, and facilitate epidemiologic analysis. There are three widely available, rapid point -of-care diagnostic tests that may guide initial therapy: the sputum Gram stain, urinary antigen tests for S pneumonia and Legionella species, and rapid antigen detection tests for influenza. Urinary anti gen assays for Legionella pneumophilia and S pneumoniae are at least as sensitive and specific as sputum Gram stain and culture. Results are available immediately and are not affected by early initiation of antibiotic therapy. Patients with cavitary opacities should have sputum fungal and mycobacterial cultures. Sputum induction and fiberoptic bronchoscopy to obtain samples of lower respiratory secretions are indicated in patients who cannot provide expectorated sputum samples or who may have Pneumocystis jirovecii or M tuberculosis pneumonia. Serologic assays, polymerase chain reaction tests, special ized culture tests, and other diagnostic tests for organisms such as viruses, Legionella, M pneumoniae, and C pneumoniae may be performed when these diagnoses are suspected. Positive tests may reduce unnecessary antibacterial use and direct isolation of hospitalized patients. The yield of blood and sputum cultures is low; however, false-positive results are common, and the impact of culture results on patient outcomes is small. Their role is to allow narrowing of initial empiric antibiotic coverage, adjustment of coverage based on spe cific antibiotic resistance patterns, to identify unsuspected pathogens not covered by initial therapy, and to provide information for epidemiologic analysis. Apart from microbiologic testing, hospitalized patients should undergo complete blood count with differential and a chemistry panel (including serum glucose, electrolytes, urea nitrogen, creatinine, bilirubin, and liver enzymes). Differential Diag nosis the differential diagnosis of lower respiratory tract infec tion is extensive and includes upper respiratory tract infec tions, reactive airway diseases, heart failure, cryptogenic organizing pneumonitis, lung cancer, pulmonary vasculi tis, pulmonary thromboembolic disease, and atelectasis. In patients who require specific diagnostic evaluation, sputum and blood culture specimens should be obtained prior to initiation of antibiotics. Since early administration of antibiotics to acutely ill patients is associated with improved outcomes, obtaining other diagnostic specimens or test results should not delay the initial dose of antibiotics. Optimal antibiotic therapy would be pathogen directed, but a definitive microbiologic diagnosis is rarely available on or within 6 hours of presentation. Prior treatment with one antibiotic in a pharmacologic class (eg, beta-lactam, macrolide, fluoroquinolone) predis poses the emergence of drug-resistant S pneumoniae, with resistance developing against that class of antibiotics to which the pathogen was previously exposed. Definitions of resistance have shifted based on observations of continued clinical efficacy at achievable serum levels. Mac rolide resistance has increased; approximately one-third of S pneumoniae isolates now show in vitro resistance to mac rolides. Radiographic findings range from patchy airspace opacities to lobar consolidation with air bronchograms to diffuse alveolar or interstitial opacities. No pattern of radiographic abnor malities is pathognomonic of any infectious cause. Progression of pulmonary opacities during antibiotic therapy or lack of radiographic improve ment over time are poor prognostic signs and also raise concerns about secondary or alternative pulmonary pro cesses. Clearance is usually quickest in younger patients, nonsmokers, and those with only single-lobe involvement. S pneumoniae resistant to fluoroquinolones is rare in the United States (1 % to levo floxacin, 2% to ciprofloxacin) but is increasing. For previously healthy patients with no recent (90 days) use of antibiotics, the recommended treatment is a macrolide (clarithromycin or azithromycin) or doxycycline. In patients at risk for drug resistance (antibiotic therapy within the past 90 days, age greater than 65 years, comor bid illness, immunosuppression, exposure to a child in daycare), the recommended treatment is a respiratory fluo roquinolone (moxifloxacin, gemifloxacin, or levofloxacin) or a macrolide plus a beta-lactam (high-dose amoxicillin and amoxicillin-clavulanate are preferred to cefpodoxime and cefuroxime). In regions where there is a high incidence of macrolide resistant S pneumoniae, initial therapy in patients with no comorbidities may include a respiratory fluoroquinolone or the combination of a beta -lactam added to a macrolide. The decision should be influenced by the severity of illness, etiologic pathogen, response to therapy, other medical problems, and complications. Most experts recommend administering a minimum of 5 days of therapy and continuing antibiotics until the patient is afe brile for 48-72 hours. In patients at risk for Pseudomonas infection, one of two following regi mens can be used: an antipneumococcal, antipseudomonal beta-lactam (piperacillin-tazobactam, cefepime, imipenem, meropenem) plus ciprofloxacin or levofloxacin or the above antipneumococcal beta-lactam plus an aminoglycoside (gentamicin, tobramycin, amikacin) plus either azithromy cin or a respiratory fluoroquinolone (moxifloxacin, gemi floxacin, or levofloxacin). Prevention Pneumococcal vaccines have the potential to prevent or lessen the severity of pneumococcal infections in immuno competent patients. Two pneumococcal vaccines for adults are available and approved for use in the United States: one containing capsular polysaccharide antigens of 23 common strains of S pneumoniae in use for many years (Pneumovax 23) and a conjugate vaccine containing 13 common strains approved for adult use in 20 1 1 (Prevnar- 13). Current recom mendations are for sequential administration of the two vaccines in those age 65 years or older and in immunocom promised persons. Immunocompromised patients and those at highest risk for fatal pneumococcal infections should receive a single revaccination of the 23-valent vaccine 6 years after the first vaccination regardless of age. Immuno competent persons 65 years of age or older should receive a second dose of the 23-valent vaccine if the patient first received the vaccine 6 or more years previously and was under 65 years old at the time of first vaccination. The seasonal influenza vaccine is effective in preventing severe disease due to influenza virus with a resulting posi tive impact on both primary influenza pneumonia and secondary bacterial pneumonias. The seasonal influenza vaccine is administered annually to persons at risk for complications of influenza infection (age 65 years or older, residents of long-term care facilities, patients with pulmo nary or cardiovascular disorders, patients recently hospi talized with chronic metabolic disorders) as well as health care workers and others who are able to transmit influenza to high-risk patients. Hospitalized patients who would benefit from pneumo coccal and influenza vaccines should be vaccinated during hospitalization.
Purchase generic betnovate on line
There is usually bilateral disease with copious watery dis charge acne forum buy betnovate without prescription, often with marked foreign body sensation, and a follicular conjunctivitis. Epidemic keratoconjunctivitis, which may result in visual loss due to corneal subepithelial infil trates, is usually caused by adenovirus types 8, 19, and 37. Infection with adenovirus types 3, 4, 7, and 1 1 is typically associated with pharyngitis, fever, malaise, and preauricular adenopathy (pharyngo conjunctival fever). Cold compresses reduce discomfort and topical sulfonamides (or oral antibiotics) can be prescribed to prevent secondary bacterial infection. The value of weak topical corticosteroids or topical cyclosporine for corneal infiltrates due to adenoviral infection is uncertain. Trachoma-Trachoma is the most common infectious cause of blindness worldwide, with approximately 40 million people affected and 1. Recurrent episodes of infection in childhood manifest as bilateral follicular conjunctivitis, epithelial keratitis, and corneal vascularization (pannus). Scarring (cicatrization) of the tarsal conjunctiva leads to entropion and trichiasis in adulthood, with secondary central corneal scarring. Immunologic tests or polymerase chain reaction on conjunctival samples will confirm the diagnosis but treat ment should be started on the basis of clinical findings. A single 1 -g dose of oral azithromycin is the preferred drug for mass treatment campaigns, but improvements in hygiene and living conditions probably have contributed more to the marked reduction in the prevalence of tra choma during the past 25 years. Surgical treatment includes correction of eyelid deformities and corneal transplantation. In severe (hyperpurulent) cases, examination of stained con junctival scrapings and cultures is recommended, particu larly to identify gonococcal infection. A topical sulfonamide or oral antibiotic will usually clear the infection in 2-3 days. Except in special circumstances, the use of topical fluoro quinolones is rarely justified for treatment of a generally self-limiting, benign infection. Inclusion conjunctivitis Inclusion conjunctivitis is usually associated with genital infection, the eye being involved following contact with genital secretions. Diagnosis can be rapidly confirmed by immunologic tests or polymerase chain reaction on conjunctival samples. B efore treatment, all cases should be assessed for genital tract infection and other sexually transmitted diseases. Gonococcal Conjunctivitis Gonococcal conjunctivitis, usually acquired through con tact with infected genital secretions, typically causes copi ous purulent discharge. It is an ophthalmologic emergency because corneal involvement may rapidly lead to perfora tion. Conjunctival infection with Chlamydia trachomatis in sexual partners of patients with adult inclusion conjunctivitis. D ry Eyes (Keratoconj unctivitis Sicca) this is a common disorder, affecting around 50% of older women. Hypofunction of the lacrimal glands, causing loss of the aqueous component of tears, may be due to aging, hereditary disorders, systemic disease (eg, Sjogren syndrome), or systemic drugs. Excessive evaporation of tears may be due to environmental factors (eg, a hot, dry, or windy cli mate) or abnormalities of the lipid component of the tear film, as in blepharitis. Mucin deficiency may be due to vitamin A deficiency, or conjunctival scarring from tra choma, Stevens-Johnson syndrome and related conditions, mucous membrane pemphigoid, burns, or topical drugs or their preservatives. Clin ical Findings the patient complains of dryness, redness, or foreign body sensation. In severe cases, there is persistent marked dis comfort, with photophobia, difficulty in moving the eye lids, and often excessive mucus secretion. In many cases, inspection reveals no abnormality, but on slit-lamp exami nation there are subtle abnormalities of tear film stability and reduced volume of the tear film meniscus along the lower lid. In more severe cases, damaged corneal and conjunctival cells stain with 1% rose bengal. In the most severe cases, there is marked conjunctival inj ection, loss of the normal conjunctival and corneal luster, epithelial keratitis that may progress to frank ulceration, and mucous strands. The Schirmer test, which measures the rate of production of the aqueous component of tears, may be helpful. Allergic Eye Disease Allergic eye disease is common and takes a number of dif ferent forms but all are expressions of atopy, which may also manifest as atopic asthma, atopic dermatitis, or allergic rhinitis. Clin ical Findings Symptoms include itching, tearing, redness, stringy dis charge, and occasionally, photophobia and visual loss. Allergic conjunctivitis is a benign disease, occurring usually in late childhood and early adulthood. It may be seasonal (hay fever), developing usually during the spring or summer, or perennial. Clinical signs are limited to con junctival hyperemia and edema (chemosis), the latter at times being marked and sudden in onset. Vernal kerato conjunctivitis also tends to occur in late childhood and early adulthood. Both the upper and the lower tarsal conjunctivas exhibit a fine papillary conjuncti vitis with fibrosis, resulting in forniceal shortening and entropion with trichiasis. Corneal involvement, including refractory ulceration, is frequent during exacerbations of both vernal and atopic keratoconjunctivitis. Treatment Aqueous deficiency can be treated with various types of artificial tears. More prolonged duration of action can be achieved with drop preparations containing a mucomimetic such as methylcellulose, polyvinyl alcohol, or polyacrylic acid (car homers), or by using petrolatum ointment or a hydroxy propyl cellulose (Lacrisert) insert. If there is tenacious mucus, mucolytic agents (eg, acetylcysteine 1 0% or 20%, one drop six times daily) may be helpful. However, preservatives included in some preparations to maintain sterility are potentially toxic and allergenic and may cause keratitis and cicatriz ing conjunctivitis in frequent users. The development of such reactions may be misinterpreted as a worsening of the dry eye state requiring more frequent use of the artificial tears and leading in turn to further deterioration, rather than being recognized as a need to change to a preservative-free preparation. Disease modification can be achieved with topical anti inflammatory agents such as corticosteroids, of which loteprednol (Lotemax) is favored because of its low risk of intraocular adverse effects, or calcineurin inhibitors, of which cyclosporine 0. Diquafosol eye drops, which also promote water transfer, and rebamipide eye drops increase mucin secretion. Increased dietary intake of omega-3 fatty acids has been reported to be beneficial. Mild and Moderately Severe Allergic Eye Disease Topical treatments include emedastine and levocabastine, which are antihistamines; cromolyn, lodoxamide, nedocro mil, and pemirolast, which are mast cell stabilizers; alcafta dine, azelastine, bepotastine, epinastine, ketotifen, and olopatadine, which are combined antihistamines and mast cell stabilizers; and bromfenac, diclofenac, flurbiprofen, indomethacin, ketorolac, and nepafenac, which are nonste roidal anti-inflammatory drugs (Table 7-2). Mast cell sta bilization takes longer to act than antihistamine and nonsteroidal anti-inflammatory effects but is useful for prophylaxis. Topical vasoconstrictors such as ephedrine, naphazoline, tetrahydrozoline, and phenylephrine, alone or in combination with antihistamines such as antazoline and pheniramine, are available as over-the-counter medi cations but are of limited efficacy in allergic eye disease and may produce rebound hyperemia and follicular conjunctivitis. Delayed or ineffective treatment of corneal ulceration may lead to devastating consequences with corneal scarring or intraocular infection. The eye is red, with predominantly circum corneal inj ection, and there may be purulent or watery discharge. In vernal keratoconjunctivitis, a cooler climate often pro vides significant benefit. Acute Exacerbations and Severe Allergic Eye Disease Topical corticosteroids (Table 7-2) are essential to control acute exacerbations of both vernal and atopic keratocon junctivitis. Corticosteroid-induced side effects, including cataracts, glaucoma, and exacerbation of herpes simplex keratitis, are maj or problems but may be attenuated by the ester corticosteroid, loteprednol. Systemic corticosteroid or other immunosuppressant therapy and even plasmaphere sis may be required in severe atopic keratoconjunctivitis. Topical antihistamines and mast cell stabilisers for treating seasonal and perennial allergic conjunctivitis. When to Refer Any patient with an acute painful red eye and corneal abnormality should be referred emergently to an ophthalmologist. Pteryg ium is a fleshy, triangular encroachment of the conjunctiva onto the nasal side of the cornea and is usually associated with prolonged exposure to wind, sun, sand, and dust.
Discount betnovate master card
Visual acuity and red-green color vision tests are recommended before initiation of ethambu tol and serum uric acid before starting pyrazinamide acne keloidalis nuchae pictures purchase 20 gm betnovate with visa. Routine monitoring of laboratory tests for evidence of medication toxicity during therapy is not recommended, unless baseline results are abnormal or liver disease is sus pected. Patients should be educated about com mon side effects of antituberculous medications and instructed to seek medical attention should these symp toms occur. Monthly follow-up of outpatients is recom mended, including sputum smear and culture for M tuberculosis, until cultures convert to negative. Patients with negative sputum cultures after 2 months of treatment should have at least one additional sputum smear and cul ture performed at the end of therapy. Patients with drug resistant isolates should have sputum cultures performed monthly during the entire course of treatment. A chest radiograph at the end of therapy provides a useful baseline for any future films. Patients whose cultures do not become negative or whose symptoms do not resolve despite 3 months of ther apy should be evaluated for nonadherence to the regimen and for drug-resistant organisms. The clinician should seek expert assistance if drug resistance is newly found, if the patient remains symptomatic, or if smears or cultures remain positive. Patients with only a clinical diagnosis of pulmonary tuberculosis (smears and cultures negative for M tuberculosis) whose symptoms and radiographic abnormalities are unchanged after 3 months of treatment usually either have another process or have had tuberculosis in the past. Treatment of Latent Tuberculosis Treatment of latent tuberculous infection is essential to controlling and eliminating tuberculosis. Treatment of latent tuberculous infection substantially reduces the risk that infection will progress to active disease. Targeted test ing with the tuberculin skin test or interferon gamma release assays is used to identify persons who are at high risk for tuberculosis and who stand to benefit from treat ment of latent infection. Table 9 - 1 4 gives the tuberculin skin test criteria for treatment of latent tuberculous infec tion. In general, patients with a positive tuberculin skin test or interferon gamma release assay who are at increased risk for exposure or disease are treated. It is essential that each person who meets the criteria for treatment of latent tuber culous infection undergo a careful assessment to exclude active disease. A history of past treatment for tuberculosis and contraindications to treatment should be sought. Patients suspected of having tuberculosis should receive one of the recommended multidrug regimens for active disease until the diagnosis is confirmed or excluded. Vaccination of health care workers should be considered on an individual basis in settings in which a high percentage of tuberculosis patients are infected with strains resistant to both isoniazid and rifampin, in which transmission of such drug-resistant M tuberculosis and subsequent infection are likely, and in which comprehensive tuberculous infection-control precau tions have been implemented but have not been successful. Some close contacts of persons with active tuberculosis should be evaluated for treatment of latent tuberculous infection despite a negative tuberculin skin test reaction (less than 5 mm induration). These include immunosup pressed persons and those who may develop disease quickly after tuberculous infection. Close contacts who have a negative tuberculin skin test reaction on initial test ing should be retested 1 0 - 1 2 weeks later. Contacts of persons with isoniazid-resistant, rifampin sensitive tuberculosis should receive a 2-month regimen of rifampin and pyrazinamide or a 4-month regimen of daily rifampin alone. Contacts of persons with drug-resistant tuberculosis should receive two drugs to which the infect ing organism has demonstrated susceptibility. All contacts of persons with multidrug-resistant tuberculosis or extensively drug-resistant tuberculosis should have 2 years of follow-up regardless of treatment. Persons with a positive tuberculin skin test (5 mm or more of induration) and fibrotic lesions suggestive of old tuberculosis on chest radiographs who have no evidence of active disease and no history of treatment for tuberculosis should receive 9 months of isoniazid or 4 months of rifampin (with or without isoniazid). Patients receiving treat ment for latent tuberculous infection should be evaluated once a month to assess for symptoms and signs of active tuberculosis and hepatitis and for adherence to their treat ment regimen. Routine laboratory testing during treatment is indicated for those with abnormal baseline laboratory tests and for those at risk for developing liver disease. Prognosis Almost all properly treated immunocompetent patients with tuberculosis can be cured. Chronic cough, sputum production, and fatigue; less common ly: malaise, dyspnea, fever, hemopty sis, and weight loss. Parenchymal opacities on chest radiograph, most often thin-wal led cavities or multiple small nod ules associated with bronchiectasis. These organisms are not considered communicable from person to person, have distinct laboratory characteristics, and are often resistant to most antituberculous medications (Chapter 33). Bronchial washings are considered to be more sensitive than expectorated spu tum samples; however, their specificity for clinical disease is not known. Diagnostic criteria in immunocompetent per sons include the following: positive culture results from at least two separate expectorated sputum samples; or posi tive culture from at least one bronchial wash; or a positive culture from pleural fluid or any other normally sterile site. Diagnostic criteria are less stringent for patients with severe immunosuppression. Less com mon symptoms include malaise, dyspnea, fever, hemopty sis, and weight loss. Imaging Chest radiographic findings include infiltrates that are progressive or persist for at least 2 months, cavitary lesions, and multiple nodular densities. Progression of pulmonary infiltrates during therapy or lack of radiographic improvement over time are poor prognos tic signs and also raise concerns about secondary or alter native pulmonary processes. First, clinical disease may never develop in some patients, particularly asymptomatic patients with few organisms isolated from single speci mens. Second, the spectrum of clinical disease severity is very wide; in patients with mild or slowly progressive symptoms, traditional chemotherapeutic regimens using a combination of agents may lead to drug-induced side effects worse than the disease itself. The investigators monitored the participants after screening for an average of 12 years. Invasive diagnostic evaluations were uncommon and were associated with a low complication rate (1. Since the groups were ran domized and well matched, lung cancer incidence should have been identical. Many, perhaps most, of these lung cancers will never cause clinical disease and represent overdiagnosis. There is no evidence of benefit in a mixed population screened with chest radiography. For patients with severe fibrocavitary disease, streptomycin or amikacin is added for the first 2 months. The optimal duration of treat ment is unknown, but therapy should be continued for 1 2 months after sputum conversion. Medical treatment is initially successful in about two-thirds of cases, but relapses after treatment are common; long-term benefit is demon strated in about half of all patients. Surgical resection is an alternative for the patient with pro gressive disease that responds poorly to chemotherapy; the success rate with surgical therapy is good. A daily regi men of rifampin, isoniazid, and ethambutol for at least 18 months with a minimum of 12 months of negative cul tures is usually successful. Rapidly growing mycobacteria (M abscessus, M fortuitum, M chelonae) are generally resis tant to standard antituberculous therapy. When to Refer Patients with rapidly growing mycobacteria infection should be referred for expert management. Epidemiology of human pulmonary infection with nontuberculous mycobacteria: a review. Benign lesions tend to have dense calcification in a central or laminated pattern. Malignant lesions are associated with sparser calcification that is typically stippled or eccentric. Cavitary lesions with thick (greater than 16 mm) walls are much more likely to be malignant. Treatment Based on clinical and radiologic data, the clinician should assign a specific probability of malignancy to the lesion. The prob abilities in parentheses below represent guidelines only and should not be interpreted as prescriptive. In the case of solitary pulmonary nodules, a continuous probability function may be grouped into three categories. In patients with a low probability (less than 5%) of malig nancy (eg, age under 30, lesions stable for more than 2 years, characteristic pattern of benign calcification), watchful waiting is appropriate. Patients with a high probability (greater than 60%) of malignancy should proceed directly to resection following staging, provided the surgical risk is acceptable.
Betnovate 20 gm without a prescription
Limitations to intravenous prostacyclins (epoprostenol acne vulgaris cause buy 20gm betnovate free shipping, treprostinil) include short medication half life requiring a reliable continuous infusion, difficulty in titration, and high cost of therapy. Inhaled prostanoids (iloprost, treprostinil) and subcutaneous prostanoids (treprostinil) are available for patients unable to tolerate continuous intravenous infusion. One oral formulation of prostacyclin analogs has been approved for Group 1 dis ease based on a clinical trial that demonstrated a small increase in 6-minute walk distance. Treatment of patients with Group 2 pulmonary hyper tension (secondary to left heart failure) is discussed in Chapter 10. The main goal is to decrease pulmonary venous pressure by treating heart failure and volume overload. Patients with Group 3 pulmonary hypertension (due to lung disease) and hypoxemia at rest or with physical activ ity should receive supplemental oxygen. For patients with Group 1 pulmonary hypertension and Group 4 pulmonary hypertension (due to thromboembolic disease), long-term anticoagulation is recommended and generally accepted, based solely on observational studies suggesting improvement in survival. Only patients with surgically accessible lesions and acceptable perioperative risk should undergo this procedure. Lung transplantation is a treatment option for selected patients with pulmonary hypertension when medical ther apy is no longer effective. Double-lung transplant is the preferred method, although single-lung transplant is rou tinely done as well. Prog nosis the prognosis of idiopathic (some Group l) pulmonary hypertension is poor and is not affected by therapies pri marily used to treat symptoms. Conversely, the prognosis for patients with secondary pulmonary hypertension (some Group 1 and Groups 2-5) depends on the underly ing disease and its response to treatment. In all cases, right ventricular function is one of the most important prognos tic factors. The presence of cor pulmonale carries a poor survival outcome regardless of the underlying cause. When to Refer Patients with pulmonary arterial hypertension and symp toms of dyspnea, fatigue, chest pain, or near syncope should be referred to a pulmonologist or cardiologist at a specialized center for expert management. When to Adm it Patients with pulmonary hypertension, severe symp toms, and evidence of decompensated right heart fail ure with volume overload should be admitted to the hospital for aggressive diuresis. Advances in therapeutic interventions for patients with pulmonary arterial hypertension. Chronic sinusitis, arthralgias, fever, skin rash, and weight loss are frequent presenting symptoms. The most common sign of lung disease is nodular pulmonary infiltrates, often with cavitation, seen on chest radiography. The diag nosis is most often based on serologic testing and biopsy of lung, sinus tissue, or kidney with demonstration of necro tizing granulomatous vasculitis (Chapter 20). Eosinophilic granulomatosis with polyangiitis (for merly referred to as Churg-Strauss syndrome) is an idio pathic multisystem vasculitis of small and medium-sized arteries that occurs in patients with asthma. The skin and lungs are most often involved, but other organs, including the paranasal sinuses, the heart, gastrointestinal tract, liver, and peripheral nerves, may also be affected. Abnormalities on chest radiographs range from tran sient opacities to multiple nodules. The diag nosis requires demonstration of histologic features, includ ing fibrinoid necrotizing epithelioid and eosinophilic granulomas. Treatment Treatment of pulmonary vasculitis usually requires corti costeroids and cyclophosphamide. Oral prednisone (1 mg/ kg ideal body weight per day initially, tapering slowly to alternate-day therapy over 3-6 months) is the corticoste roid of choice; in granulomatosis with polyangiitis, some clinicians may use cyclophosphamide alone. For fulminant vasculitis, therapy may be initiated with intravenous meth ylprednisolone (up to 1 g intravenously per day) for several days. Cyclophosphamide (1 -2 mg/kg ideal body weight orally per day initially, with dosage adjustments to avoid neutropenia) is given until complete remission is obtained and then is slowly tapered, and often replaced with metho trexate or azathioprine for maintenance therapy. Prognosis Five-year survival rates in patients with these vasculitis syn dromes have been improved by combination therapy. Com plete remission can be achieved in over 90% of patients with granulomatosis with polyangiitis. The addition of trime thoprim-sulfamethoxazole (one double-strength tablet by Diffuse alveolar hemorrhage may occur in a variety of immune and nonimmune disorders. Hemoptysis, alveolar infiltrates on chest radiograph, anemia, dyspnea, and occa sionally fever are characteristic. Rapid clearing of diffuse lung infiltrates within 2 days is a clue to the diagnosis of diffuse alveolar hemorrhage. Causes of immune alveolar hemorrhage have been classified as anti-basement membrane antibody disease (Goodpasture syndrome), vasculitis and collagen vascular disease (systemic lupus erythematosus, granulomatosis with polyangiitis, systemic necrotizing vasculitis, and oth ers), and pulmonary capillaritis associated with idiopathic rapidly progressive glomerulonephritis. Nonimmune causes of diffuse hemorrhage include coagulopathy, mitral stenosis, necrotizing pulmonary infection, drugs (penicil lamine), toxins (trimellitic anhydride), and idiopathic pul monary hemosiderosis. Goodpasture syndrome is idiopathic recurrent alveo lar hemorrhage and rapidly progressive glomerulonephri tis. Hemoptysis is the usual presenting symptom, but pulmonary hemorrhage may be occult. Dyspnea, cough, hypoxemia, and diffuse bilateral alveolar infiltrates are typical features. The diagnosis is based on characteristic linear IgG deposits detected by immunofluorescence in glomeruli or alveoli and on the presence of anti-glomerular basement membrane antibody in serum. Combinations of immuno suppressive drugs (initially methylprednisolone, 30 mg/kg intravenously over 20 minutes every other day for three doses, followed by daily oral prednisone, 1 mg/kg/ day, with cyclophosphamide, 2 mg/kg orally per day) and plasma pheresis have yielded excellent results. Idiopathic pulmonary hemosiderosis is a disease of children or young adults characterized by recurrent pul monary hemorrhage; in contrast to Goodpasture syn drome, renal involvement and anti-glomerular basement membrane antibodies are absent, but iron deficiency is typical. Recurrent episodes of pulmonary hemor rhage may result in interstitial fibrosis and pulmonary failure. Diffuse alveolar hemorrhage in immunocompe tent patients: etiologies and prognosis revisited. As many as one-third of patients admitted to burn treatment units have pulmonary injury from smoke inhalation. Morbidity and mortality due to smoke inhalation may exceed those attributed to the burns themselves. The death rate of patients with both severe burns and smoke inhalation exceeds 50%. All patients in whom significant smoke inhalation is suspected must be assessed for three consequences of smoke inhalation: impaired tissue oxygenation, thermal injury to the upper airway, and injury to the lower airways and lung parenchyma. Impaired tissue oxygenation may result from inhalation of a hypoxemia gas mixture, carbon monoxide or cyanide, or from alterations in V/ Q matching, and is an immediate threat to life. The management of patients with carbon monoxide and cyanide poisoning is discussed in Chapter 38. The clinician must recognize that patients with carbon monoxide poisoning display a normal partial pressure of oxygen in arterial blood (Pao 2) but have a low measured (ie, not oximetric) hemoglobin saturation (Sao 2). Treatment with 100% oxygen should be continued until the measured carboxyhemoglobin level falls to less than 10% and concomitant metabolic acidosis has resolved. Thermal injury to the mucosal surfaces of the upper airway occurs from inhalation of super-heated gases. Com plications, including mucosal edema, upper airway obstruction, and impaired ability to clear oral secretions, usually become evident by 1 8-24 hours and produce inspi ratory stridor. Early management (Chapter 37) includes the use of a high humidity face mask with supplemental oxygen, gentle suctioning to evacuate oral secretions, elevation of the head 30 degrees to promote clearing of secretions, and topical epinephrine to reduce edema of the oropharyngeal mucous membrane. Helium-oxygen gas mixtures (Heliox) may reduce labored breathing due to critical upper airway nar rowing. Examination of the upper airway with a fiberoptic laryngoscope or bronchoscope is superior to routine physical examination. Endotracheal intubation is often necessary to establish airway patency and is likely to be necessary in patients with deep facial burns or oropharyngeal or laryngeal edema. Tracheotomy should be avoided if possible because of an increased risk of pneumonia and death from sepsis. Injury to the lower airways and lung parenchyma results from inhalation of toxic gases and products of combustion, including aldehydes and organic acids. The site of lung injury depends on the solubility of the gases inhaled, the duration of exposure, and the size of inhaled particles that transport noxious gases to distal lung units. Bronchorrhea and bronchospasm are seen early after expo sure along with dyspnea, tachypnea, and tachycardia.


