Discount 50 mg cytoxan mastercard
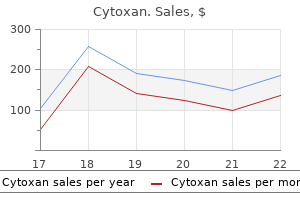
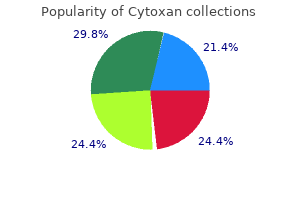
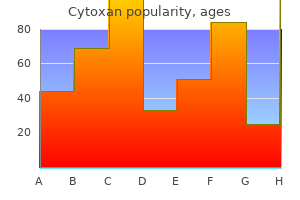
The combination of pirfenidone with food caused a reduction and delay in the absorption of the drug and a reduced plasma concentration of both drug and metabolites symptoms 9 weeks pregnancy buy cytoxan cheap online. It has been largely demonstrated that alterations of the Wnt signaling transduction pathway have clinical relevance in the pathogenesis of cancer. It is interesting that the same compound has already been used with success in an animal model of lung fibrosis. This pathway is involved in the regulation of cell growth, proliferation, and survival. It transmits chemical signals from outside the cell, through the cell membrane toward the cytoplasm, and then into the nucleus. Tyrosine kinase is an enzyme that acts as a sort of "on" or "off" switch that regulates many cellular functions. Mutations can turn tyrosine kinases in a nonstop functional state that, under specific circumstances, may lead to the initiation or progression of cancer. More recently this pathway has also been studied in the context of the wound healing process and fibrosis. It was able to inhibit fibroblast proliferation and collagen deposition in vitro and in vivo, but when it was evaluated in a clinical trial, no benefit in slowing disease progression was found. It was found to attenuate fibrosis by reducing the expression of profibrotic factors and by decreasing collagen deposition. The safety profile of the explored drug is already known so that the risk of adverse events is reduced. In addition, the mechanism of action of a repositioned drug is known and can be used in those diseases where a similar mechanism is involved. Today, computational strategies are available to explore the mechanisms of action of approved drugs and to match them with cellular and/or molecular targets involved in the pathogenesis of virtually any disease. The secondary endpoints were represented by the time to the first exacerbation and the change in total St. This analysis also demonstrated a positive trend toward a reduction in risk for all-cause and respiratory mortality. This metabolite is eliminated through the liver and feces, while the excretion in the urine is minimal. In the pooled data analysis, diarrhea was the most frequent adverse event in the nintedanib group (61. In general, adverse events are reversible with reducing the dose of nintedanib or stopping the treatment, without clinically significant consequences. The pathophysiologic mechanism of drug-induced diarrhea is still not completely understood, but some studies conducted for oncologic tyrosine kinase inhibitors could be helpful to understand the molecular mechanisms through which 31 diarrhea develops. Sometimes the addition of loperamide is indicated as a useful treatment to decrease intestinal motility. It is well known that the trial failed, showing an increase in the number of deaths and hospitalizations in the group treated with the triple therapy. Some of these mechanisms are obscure, some others are partially clear, and some of them are well understood and are being used to develop new therapeutic strategies. All of them are obviously inspired by the new pathogenic knowledge that comes every day from the research field. The drug was well tolerated, and just transient skin reactions were observed as adverse events. Cell-based therapies represent an innovative possibility to treat patients with lung fibrosis because transplanted cells could be potentially able to proliferate and differentiate into alveolar cells replacing the damaged epithelial alveolar cells and some benefits could be obtained from the paracrine properties of the newly administered cells. Different routes of cell administration were tested, intravenously or through intraperitoneal or intratracheal 34 Interstitial Lung Disease For these reasons, during the last few years the scientific attention has focused on some steps of the fibrogenic process, characterized by the activation of multiple and different pathways that may represent specific therapeutic targets. The current approach to treatment is based on sequential therapy, so that one of the two approved drugs is started and when it is believed to be ineffective or side effects due to the drug are severe, it is possible to switch to the alternative drug. Similar to cancer, for the first time exists the possibility to have a first-line and, as alternative, a second-line of treatment. Two different clinical trials are currently under way exploring the safety of the association of pirfenidone and nintedanib, and hopefully, as in other diseases, there will be the possibility to use in the same patients a combination of drugs. The mechanisms of action of the two drugs seem different, so it is reasonable to think of a possible increase in their efficacy without necessarily having a sum of side effects. Other issues are unsolved such as the effective cell dose equivalent for cell therapy, defined as the minimum cell number required to have a significant result. Safety and tolerability are the most important issues because of the risk of teratoma and other risks associated with isolation, culture, and storage of cells. The most commonly used cells are mesenchymal cells, which are characterized by low immunogenicity and low risk of teratoma. The future development of cell therapy is fascinating and possibly realistic using bioengineering approaches that according to recent studies will make it possible to use decellularized whole lungs as a scaffold for subsequent cellular implantation. Genetic predisposition and aging play a fundamental role in altering the response of epithelial cells to chronic damage. The final result of all this is the activation of fibroblasts, and their recruitment, proliferation, and differentiation into myofibroblasts, resulting in scar formation and loss of lung function. Relationship of alveolar epithelial injury and repair to the induction of pulmonary fibrosis. Pirfenidone suppresses tumor necrosis factor-alpha, enhances interleukin-10 and protects mice from endotoxic shock. Effects of pirfenidone on transforming growth factor-beta gene expression at the transcriptional level in bleomycin hamster model of lung fibrosis. Collagen synthesis by normal and fibrotic human lung fibroblasts and the effect of transforming growth factor-beta. Pirfenidone for idiopathic pulmonary fibrosis: analysis of pooled data from three multinational phase 3 trials. Safety of pirfenidone in patients with idiopathic pulmonary fibrosis: integrated analysis of cumulative data from 5 clinical trials. Ameliorative effects of mosapride or Rikkunshi-to on the suppression of gastrointestinal motility by pirfenidone in rats. Effect of food and antiacids on the pharmacokinetics of pirfenidone in older healthy adults. Pirfenidone in idiopathic pulmonary fibrosis: expert panel discussion on the management of drug-related adverse events. Photosafety assessments on pirfenidone: photochemical, photobiological, and pharmacokinetic characterization. Pharmacokinetics, safety and tolerability of pirfenidone and its major metabolite after single and multiple oral doses in healthy Chinese subjects under fed conditions. Pharmacokinetic evaluation of tissue distribution of pirfenidone and its metabolites for idiopathic pulmonary fibrosis therapy. Antifibrotic effects of nintedanib in lung fibroblasts derived from patients with idiopathic pulmonary fibrosis. Anti fibrotic and antiinflammatory activity of the tyrosine kinase inhibitor nintedanib in experimental models of lung fibrosis. Reducing lung function decline in patients with idiopathic pulmonary fibrosis: potential of nintedanib. Phosphatidylinositol 3-kinase mediates the inhibitory effect of epidermal growth factor on calcium-dependent chloride secretion. Practical management of patients with chronic myeloid leukemia receiving imatinib. Intracellular glutathione and bronchoalveolar cells in fibrosing alveolitis: effects of N-acetylcysteine. Efficacy of inhaled N-acetylcysteine monotherapy in patients with early stage idiopathic pulmonary fibrosis. Effect of inhaled N-acetylcysteine monotherapy on lung function and redox balance in idiopathic pulmonary fibrosis. Expression of suppressor of cytokine signalling 1 in the peripheral blood of patient with idiopathic pulmonary fibrosis. The role of tyrosine kinases in the pathogenesis of idiopathic pulmonary fibrosis. Inhibition of plateletderived growth factor signalling attenuates pulmonary fibrosis.
Syndromes
- Prevent cardiovascular disease
- Caffeine may lead to painful, lumpy breasts (fibrocystic disease).
- Stupor (lack of alertness)
- Ultrasounds, including an ultrasound of the working heart (echocardiogram) and of the kidneys
- Convulsions
- Anxiety
- Chemicals
Order cytoxan american express
There are many known fibronectin-binding proteins medicine games purchase generic cytoxan from india, but each is expressed and distributed in a particular group of M-serotype organisms and is involved in adhesion and invasion. Streptococci express two major classes-M- and T-antigen-and two minor classes-R- and F-antigen. It binds to serum H-factor, destroys C3 convertase, and prevents opsonization by C3. However, plasma B-cells can generate antibodies against M-protein, which further helps in opsonization and destruction of the organisms by macrophages and neutrophils. M-protein is typespecific and is resistant to heat and acid but sensitive to trypsin. T-antigens are the non-virulent factor and are resistant to heat, acid, and trypsin. Migratory polyarthritis occurs for between a few days and a few weeks and resolves completely; 3) Sydenham chorea, involuntary, purposeless, jerky movements of the hands and arms, shoulders, feet, legs, face, and trunk, along with hypotonia and weakness, which disappear during sleep; 4) subcutaneous nodules, commonly noticed over the occiput, elbows, knees, ankles, and Achilles tendons. On microscopic examination, these nodules show central fibrinoid degeneration of the collagen surrounded by chronic mononuclear inflammatory cell infiltrate; 5) erythema marginatum, less commonly found, these present as a pink, non-pruritic skin rash present over the upper parts of the arms or trunk but not on the face. The rash generally occurs early or late in the course of the disease and extends centrifugally with a clear center. Pathophysiology includes the deposition of immune complexes on joints causing non-destructive synovitis and non-destructive reactions in the basal ganglia, whereas the development of autoimmune cytotoxic reactions destroys the heart valves, causing a severe form of cardiac involvement. An accurate description is as follows: "rheumatic fever licks the joint, but bites the heart. The mitral valve is the most commonly involved valve, seen in approximately 90% of cases, followed by the aortic and other valves in decreasing order of frequency. The inflammatory process in the valve and the heart is mainly due to the cross-reactivity of streptococcal 36 the pathophysiology of mitral stenosis cell wall proteins and enzymes against the heart valve tissue. The main protein involved in this cross-reactivity is the streptococcal M-protein with the cardiac myosin. Many studies have supported this mechanism and the culture report studied in all these valves was negative for any pathogens unless if there was any superadded secondary infection. Studies have shown that the risk of acute rheumatic fever is six times higher in monozygotic twins when compared with that of dizygotic twins. This may indicate the association of different strains of streptococcus in different regions of the world. Some authors have documented that the majority of these genes were found to be involved in the regulation of the immune system. Interleukins produced by inflammatory cells further activate other inflammatory cells and their adhesion molecules. Autoimmunity is a primarily adaptive immune response driven by T and B lymphocytes. The M-protein of the streptococcal antigen shares structural homology with cardiac myosin, tropomyosin, laminin, and vimentin. Hence, infection with streptococcal pyogenes triggers the autoimmunity responsible for pathological changes in the heart, joints, and central nervous system. Antibodies produced against N-acetylglucosamine cross-react with laminin in the heart valves. These mechanisms have been studied by many researchers who had demonstrated the presence of gamma globulin in the myocardium of rheumatic atrial appendage, valvulitis, and myocarditis. It has been demonstrated that antistreptococcal antibodies were cytotoxic for cultured endothelial cells, valvular endothelial cells, and the underlying basement membrane in humans. These autoreactive T-lymphocytes further activate the B-cells to produce more self-specific antibodies, further enhancing the inflammatory process. This is the mechanism of humoral-mediated antibody production in the initiation of cardiac inflammation via cellular immune response. Studies have also described the presence of peripheral and cardiac T-cells, which are capable of cross-reacting with streptococcal M5 protein and cardiac myosin, laminin, and tropomyosin. A final explanation for the mechanism is by an increased number of peripheral antigen-specific T-cells migrating to the heart because of antigenic mimicry. These cells expand locally and become capable of recognizing new selfantigens by the epitope spreading mechanism. The frequency of valvular involvement in descending order is as follows: mitral valve, aortic valve, tricuspid valve, and pulmonary valve (pulmonary valve involvement is very rare). In the acute stage, the affected valves are edematous and opaque and lose their normal transparency. They are firm in consistency and contain fibrinoid necrosis of the valve collagen surrounded by few histiocytic cells. They are characteristically present on the atrial surface in case of mitral valves and ventricular surface in case of semilunar valves. Rheumatic vegetations are formed mainly due to endothelial injury as a result of hemodynamic turbulence. Endothelial injury causes exposure of the subendothelial collagen and elastin to the flowing blood, which is highly thrombogenic and causes deposition of fibrin and platelets on the damaged site. The inflammatory infiltrate usually consists of lymphocytes, histiocytes, a few polymorphs, and eosinophils. Antischkow cells and Aschoff cells may also be seen; 3) myocardium: on gross examination, the heart becomes soft and flabby in acute myocarditis along with the dilatation of all chambers, especially the ventricles. Microscopic examination reveals presence of non-specific interstitial inflammation along with the presence of Aschoff bodies in the interstitium. In the chronic stage, heart valves show dense fibrosis, commissural fusion, calcification, and scarring of the valve components resulting in severe stenosis and other deformities. Fibrosis may involve the valve leaflets, chordae tendineae, and papillary muscles. This results in characterized morphological deformities like a "funnel shaped valve," "fish mouth," and "button hole," depending upon the severity. Fibrosis is extending into the papillary muscles with fusion and shortening of the chordae tendineae (dotted line). The severity of inflammation varies depending upon the disease status and activity. The inflammatory infiltrate usually consists of lymphocytes, histiocytes, and plasma cells. Sometimes, when there is superadded infection/inflammation, polymorphonuclear neutrophils and eosinophils may also be present. Fibrosis is mainly due to the deposition of varying amounts of collagen in the valve substance, which is nothing but the sequelae of any chronic inflammation. Fibrosis of the valve leads to fusion of the valve commissures, leading to stenosis. This finding is a characteristic feature of chronic inflammatory/ rheumatic valve disease. Fibrosis involving the chordae tendineae and papillary muscles may cause shortening and thickening, leading to valve regurgitation. Macrophages are the first cells to migrate and aggregate around the degenerated collagen and fibrinoid necrosis at the site of injury. These cells secrete various cytokines that will attract the T-lymphocytes followed by B-lymphocytes. These nodules may occasionally be encountered in the pericardium and adventitia of the aorta. The mononuclear cardiac histiocytes in the Aschoff nodule are called Antischkow cells. The same cell in transverse section shows central chromatin with surrounding clear halo, which is also known as an "owl-eyed" nucleus. Sometimes, multinucleated giant cells are also present, known as Aschoff giant cells. Silver and Stollerman defined three developmental stages of Aschoff nodules: stage 1) central fibrinoid necrosis, edema, and infiltration by histiocytes, lymphocytes, and plasma cells (exudative and degenerative phase); stage 2) a specific granulomatous phase with accumulation of characteristic Aschoff giant cells and Antischkow cells; and stage 3) a late stage with diminution of the cellular infiltrate and replacement by scar tissue. Normally, valves are avascular and may show the presence of a few capillaries near their attachment at the base.
Cytoxan 50 mg visa
In addition medicine gif order cytoxan uk, patients should avoid the sun several weeks prior and after the laser procedure to prevent side effects of dyschromia. The provider and the Melasma 273 patient should use appropriate eye protection depending on the wavelength of the laser. Various modalities have been used to treat melasma, but recurrences are common, making it difficult to cure. Lasers that have been studied for the treatment of melasma include Q-switched lasers (alexandrite, ruby, and neodymium-doped yttrium aluminum garnet) and fractional lasers. Two regions on each patient were assessed 4 weeks following the last treatment and showed statistically significant lightening of the skin and decrease in the melanin index of the melasma lesions. By delivering repetitive energy with a subtherapeutic fluence, it is thought that melanin granules are fragmented and dispersed into cytoplasm without causing cellular damage or cell death. This method has been shown to be effective for lightening both epidermal and dermal melasma. However, due to the frequency of recurrence with melasma, prevention with broad-spectrum sunscreens and topical tyrosinase inhibitors following laser therapies is recommended. Serious complications justifying suspension of treatment include mottling hypopigmentation, leukoderma, severe urticarial, severe acneiform eruption, and herpes simplex activation. Although initial results demonstrated significant improvement in melasma, recurrence was noted after discontinuation of treatment. Although success has been shown with some laser therapies, the risk versus benefit must be addressed when considering such treatment options for patients. Due to the high recurrence rates, combined topical therapy is recommended to help maintain laser treatment results. Although these lesions are benign, it is important to differentiate them from other pigmented lesions such as melanoma. Solar lentigines are flat brown to dark brown macules ranging from millimeters to centimeters in diameter. They are most frequently found on chronic sunexposed areas (face, dorsum of hands, forearms) and are more common after age 50. They cause tissue destruction purely by photothermolysis, whereas Q-switched lasers cause both photothermal and photomechanical effects due to their short burst of high energy radiation. Melanin has a strong affinity for 532-nm green light, whereas the 1064-nm wavelength penetrates skin more deeply but with a lower melanin absorption coefficient. Efficacy has been reported with one treatment, and higher fluences have been noted to produce higher clearance rates. However, lower doses and pulsed modes have been used to help reduce these complications. Although all three methods proved to be effective in lightening or clearing solar lentigines, cryotherapy was shown to be the most effective. However, grading of improvement was not standardized and was subject to variation in the judgments of the observers grading the photographs of the lesions treated. This lesion occurs mainly in darker skin types, especially Asians, and predominantly in women. In cases where nevus of ota involves the eye, there have been reports of glaucoma and uveal melanoma. Q-switch lasers produce very short pulses of energy in nanoseconds,7 and this short pulse duration limits thermal damage to the surrounding tissues and selectively destroys the target tissue of melanin within the dermal melanocytes. As nevus of ota usually occurs in patients with darker skin types, lower fluences are used to prevent complications of dyschromia. The average age of the patients was 30 years, most were women, and there was a favorable response by 1 year of treatment. The number of treatments depended on the color of the nevus of ota, with blue-green lesions requiring more treatments than brown lesions. The patients in this study were mainly women ranging in age from 7 months to 60 years, and after 3 years of follow-up, there were no reports of erythema, textural change, scarring, or dyschromia. However, this laser has less absorption of melanin and high fluences are required, which can cause more pain and potential for scarring. In addition, arachidonic acid and other inflammatory markers are thought to stimulate melanin synthesis in the epidermis. It is also necessary to treat the underlying inflammatory skin condition that caused the dyschromia to prevent further worsening of the dyschromia. Improved quality of life with effective treatment of facial melasma: the pigment trial. Selective photothermolysis: Precise microsurgery by selective absorption of pulsed radiation of pulsed radiation. Fractional photothermolysis: A new concept of cutaneous remodeling using microscopic patterns of thermal injury. A randomized, split-face clinical trial of low-fluence Q-switched neodymium-doped yttrium aluminum garnet (1,064 nm) laser versus low-fluence Q-switched alexandrite laser (755 nm) for the treatment of facial melasma. Ineffective treatment of refractory melasma and postinflammatory hyperpigmentation by Q-switched ruby laser. Treatment of melasma using fractional photothermolysis: A report of eight cases with long-term follow-up. Treatment of melasma in Asian skin using a fractional 1,550-nm laser: An open clinical study. Split-face study of melasma patients treated with non-ablative fractionated photothermolysis (1540 nm). Is non-ablative 1550-nm fractional photothermolysis an effective modality to treat melasma Nonablative 1550-nm fractional laser therapy versus triple topical therapy for the treatment of melasma: A randomized controlled pilot study. Nonablative 1,550 nm fractional laser therapy versus triple topical therapy for the treatment of melasma: A randomized controlled split-face study. Low-fluence Q-switched neodymium-doped yttrium aluminum garnet laser for melasma with pre- or posttreatment triple combination cream. Irradiation of pigmented melanoma cells with high intensity pulsed radiation generates acoustic waves and kill cells. A comparison of Q-switched and long-pulsed alexandrite laser for the treatment of freckles and lentigines in oriental patients. Response of naevus of Ota to Q-switched ruby laser treatment according to lesion colour. A retrospective study looking at the long-term complications of Q-switched ruby laser in the treatment of nevus of Ota. Fractional photothermolysis for the treatment of postinflammatory hyperpigmentation. Multiple endogenous chromophores, including melanin, water, and hemoglobin, exhibit characteristic preferred absorption wavelengths. For example, melanin absorbs light continuously over a broad spectrum with peak absorptions at lower wavelengths. Conversely, shorter wavelengths are used to target more superficial targets while preserving and avoiding damaging deeper skin parts such as the dermis. Multiple protocols have been described and studied in a variety of these pigmented lesions (Table 35. Melasma Melasma is an acquired disorder of hyperpigmentation appearing on sun-exposed areas that mostly involve the centrofacial region; histologically, one may see increased melanin, melanosomes, as well as melanocytes. Melasma is multifactorial, and pathogenesis may include genetic predisposition, pregnancy, cosmetics, medications, hormone therapies, phototoxic drugs, and ultraviolet radiation. Additionally, certain populations, such as African Americans, Asians, and Hispanics, have been noted to be particularly susceptible to melasma. Melasma can be classified histologically, with treatment implications, into three patterns based on the location of melanin deposition: epidermal, dermal, and mixed pattern. There is no universal efficacious treatment, and thus a combination approach is often undertaken.
Order cytoxan 50 mg
Nothing much has been added in the literature regarding preventive aspects of the disease in recent years medications you can give dogs order cytoxan 50mg free shipping. Fifty percent of those with positive rheumatic history had negative auricular biopsy. So, there are cases where there is neither clinical nor biopsy evidence of rheumatic process. Importantly, in this series, the number of rheumatic attacks did not appear to increase the incidence of mitral stenosis. A good echocardiographic examination has ruled out typical congenital morphologies. There are certain echocardiographic features which are suggestive of rheumatic etiology. The mitral leaflets are typically pliable, with restricted mobility of the leaflet tips, which results in doming and a "hockey-stick" appearance of the anterior mitral leaflet in diastole in parasternal long-axis view. On parasternal short-axis examination, there is a typical fishmouth appearance because of commissural fusion. Carditis is one component of it and rheumatic fever can be diagnosed even in the absence of clinical carditis if other major/minor criteria are present. Rheumatic fever may occur without clinical carditis (heart failure, new-onset murmur, pericardial friction rub, etc. Subclinical carditis is the term given to those cases of rheumatic fever where carditis is diagnosed by echocardiography and there is no clinical evidence of carditis. Patients with subclinical carditis suffer the same fate as that of manifest carditis. Since all cases of rheumatic fever (with or without carditis) need to get penicillin prophylaxis, the therapeutic significance of subclinical carditis lies in the duration of penicillin prophylaxis. Paul Wood11 states that the average duration between rheumatic fever and critical mitral stenosis is 19 years. The inference from the West is supported by echocardiography-based longitudinal studies that have estimated the average decline in valve area to be as low as 0. This picture was described as "musculare lungencirhose" of mitral stenosis by Davidson in 1905. A high percentage of minute orifices are encountered at surgery in this age group. The small left atrium in this age group is attributed to rapid progression of the disease. There is no time for left-atrial distension and the brunt of back pressure falls on the pulmonary vasculatures. Valve morphology Six types of valve morphologies encountered during surgery were described by Paul. According to Paul these valves are occasionally seen in early adult cases and are possibly due to early disease. These are present in 25% of cases and the valve is button hole, densely sclerotic with fibrous tissue that resembles cartilage in consistency. This was impossible to fracture with Sex ratio Boys are affected more often than females, with a ratio of 1. This is quite unlike the 3:1 or 4:1 female preponderance noted in all adult series. Paul theorized the influence of sex hormones on the female preponderance after puberty as both the sexes are equally exposed to rheumatic infection. This dense sclerotic cartilaginous valve had no counterpart in the adult series of 700 patients of the same author. The patients with severe pulmonary vascular obstruction have a dusky look owing to a combination of extreme pallor and slight cyanosis. Paul Wood11 conferred the term mitral facies for a group of patients who had extreme pulmonary vascular resistance (>10 wood units), decreased cardiac output, and reduced arterial oxygen saturation of less than 90%. We should also recognize that symptoms in young children may be predominantly respiratory limited to tachypnea, dyspnea, or failure to thrive (Table 15. This conclusion was extremely relevant in the pre-echocardiography era as the patients were sent for surgery on the basis of clinical findings alone. Echocardiography in juvenile mitral stenosis 247 hypokinesia as well as regional wall motion abnormalities. They attributed it to rheumatic myocardial damage, subvalvular fibrosis, or secondary to rightventricular volume overload. A number of theories have been proposed to explain this rapid progression of pulmonary vascular disease. Hypersensitive reaction of pulmonary vasculature to a fulminating rheumatic process1 2. This may be the reason for decreased incidence of atrial fibrillation and absence of left-atrial thrombus in this patient population. Right-atrial and right-ventricular dilatation may be present because of significant pulmonary hypertension. Right-ventricular systolic pressures as measured by tricuspid regurgitation jet velocity may be suprasystemic. Unfortunately, there are no validated thresholds for interventions in this group of patients on the basis of large series. We should also recognize that symptoms in young children may be limited to tachypnea, dyspnea, or failure to thrive. Prior correction of anemia, infection, and heart failure stabilization is advisable. However, a critically ill child may need intervention on an urgent/emergent basis. Rarely, if the child is extremely uncooperative, the procedure may require general anesthesia. Most often, the procedure is performed under local anesthesia with conscious sedation. Transseptal puncture should ideally be performed with a pediatric transseptal set in the usual manner under fluoroscopic guidance. The differences between the adult and pediatric transseptal set are summarized in Table 15. The length and shaft diameter of the Inoue and Accura balloon are 70 and 80 cm, and 12F and 11F, respectively. A stepwise inflation technique is recommended, beginning with the smallest volume and progressively increasing by 0. To overcome this, the double-loop technique27 or over-the-wire technique28 can be tried. Replacement of the diseased mitral valve with the prosthesis is associated with the risks of anticoagulation, suboptimal preservation of ventricular function, and reduced survival. Children who have small prostheses implanted are at an increased risk of restrictive hemodynamics and the certainty that the child will outgrow the prosthesis. Actuarial freedom from thrombotic, embolic, and hemorrhagic events at 10 and 14 years is 63% and 45%, respectively. In the Gamra series32 the better results in juvenile patients were attributed to small left-atrial dimensions and more pliable valves. This probably results from the aggressive nature of the disease in this group leading to severe subvalular deformity. This may be due to smoldering rheumatic activity or the recurrence of rheumatic fever in this age group. The rates of restenosis ranged from 16% at intermediate follow-up (mean followup: 34 months) to 26% on long-term follow-up (mean follow-up: 8. Optimal immediate and long-term results are seen in children and young adults with favorable valve morphology.
Cytoxan 50 mg sale
In such a situation treatment depression cytoxan 50 mg low price, the 14F septal dilator should be repositioned across the false track to seal the rent temporarily. Technically, it is possible to close the stitch percutaneously by means of an atrial septal occluder. Subtle signs such as yawning may be a pointer to the development of pericardial effusion. Another important clue is the observation of reduced pulsations of the left cardiac border on fluoroscopy. It must be remembered that even a small pericardial effusion can lead to tamponade. Autotransfusion should be initiated as it is likely that the collection will reappear repeatedly, leading to the loss of a considerable volume of blood. The former will almost always need surgical intervention while the latter may seal off with conservative management. Removal of the dilator will lead to a dramatic increase in pericardial effusion and hemodynamic deterioration. Through a contralateral venous access, the procedure can be completed, preferably by a more experienced operator. This will reduce the cardiopulmonary bypass time as well as postoperative complications. Recurrent appearance of pericardial effusion after pericardiocentesis is an indicator for surgery. The pigtail guidewire was removed and so was the pigtail in the pericardial cavity. A vascular sheath was left in the pericardial space for any delayed fluid accumulation (see Videos 13. The usual presentation is the development of hypotension due to reduced forward output. Hypotensive patients will need inotropic support and insertion of an intra-aortic balloon pump. Those in pulmonary edema need intravenous diuretics, morphine, and ventilatory support (noninvasive/invasive) as they await surgery. Embolic material may be clot (old, organized or freshly formed), air, or calcified valve material. Intravenous or intraarterial thrombolytic therapy is recommended for cardioembolic ischemic stroke. Recently, many trials have shown the superiority of mechanical thrombectomy (using stent retrievers) over intravenous thrombolytic therapy for ischemic stroke. Mechanical thrombectomy using stent retrievers is the indicated option in those in whom thrombolysis is contraindicated or has failed. This is also an option when the embolus is an organized clot or calcific material wherein thrombolytic therapy is ineffective. Finally, the question arises as to when to imitate anticoagulation in a patient who has had an ischemic stroke. After two balloon inflations, the patient became nonresponsive and had developed right hemiplegia. Intrarterial urokinase at a dose of 1 lakh unit was given every five minutes to a total of 3 lakh units. Within 15 minutes, patient started talking coherently and her power in the left upper and lower limbs had become Grade 3. It has been shown that the Accura balloon can be safely reused six times and the Inoue balloon five times. It is good practice to examine the guidewire outside the body for any kinks or excessive undulations. As such the retrieval device also needs to be large enough to accommodate the loop. The loop could be increased or decreased by fixing one free end and pushing or pulling the other free end into the multipurpose catheter. The broken pigtail guidewire could be snared within minutes as the loop formed by the snare was large enough. As such, the whole unit (Mullins sheath, multipurpose catheter, indigenous snare, captured pigtail guidewire) must be removed en bloc. Note the large loop of the snare; (c,d) fracture guidewire caught by the indigenous snare and the assembly removed via femoral sheath (see Videos 13. It can be catastrophic if the fully inflated balloon continues to straddle the mitral valve, obstructing forward blood flow. Finally, any kink in the balloon shaft (from excessive twisting) may also lead to deflation failure. First, it has a vent tube that is meant for deairing the Inoue balloon during preparation. In the event of deflation failure, the accumulated contrast material can slowly escape, causing the balloon to collapse over time. The dilution of contrast may be increased (nine parts saline and one part contrast, rather than fourfold if an ionic dye is used). The balloon should be checked for integrity outside the body with smooth inflation and deflation. There should be no undue resistance when the balloon is slenderized over the metal tube. In the case of the Inoue balloon, opening the vent tube may allow the contrast to flow out. Further, the two tiny holes provided in the Inoue balloon may allow slow seepage of contrast from the balloon. If a kink is suspected, straightening the balloon shaft with the stainless steel pigtail guidewire can be tried. If this fails to straighten the kink, an attempt to pass the stretching tube may be tried. There would be a risk of air embolism if complete deairing had not been performed prior to balloon insertion. Through another venous access, a Mullins catheter was advanced, through which a Brockenbrough needle was passed. Attempts to overinflate the balloon have been tried, but run the risk of air and balloon material embolization. Further, removal of the slenderized balloon from the femoral vein is atraumatic and smooth. This often occurs if the correct sequence of stretching the balloon is not followed (the correct sequence is to lock the stainless-steel tube to the gold metal tube first, and then advance the two as a whole to lock into the plastic hub. The calcified lateral commisure does not yield, the noncalcified medial commissure splits on serial graded, guided inflation. Note that the first septal dilator is almost at the posterior border of the right atrium indicating that the first septal puncture was at an inappropriate site. The Indian experience of percutaneous transvenous mitral commissurotomy: Comparison of the triple lumen (Inoue) and double lumen (Accura) variable sized single balloon with regard to procedural outcome and cost savings. Comparative study on safety, efficacy, and midterm results of balloon mitral valvotomy performed with triple lumen and double lumen mitral valvotomy catheters. Atrial septal puncture technique in percutaneous transvenous mitral commissurotomy: Mitral valvuloplasty using the Inoue balloon catheter technique. Impossibility to cross a stenotic mitral valve with the Inoue balloon: Success with a modified technique. Percutaneous transvenous mitral commissurotomy-A modified over-the-wire technique for difficult left ventricle entry. Retrograde non trans-septal balloon mitral valvotomy in mitral stenosis with interrupted inferior vena cava, left superior vena cava, and hugely dilated coronary sinus. Safety of Inoue balloon mitral commissurotomy in patients with left atrial appendage thrombi. Balloon mitral valvotomy in patients with mitral stenosis and left atrial thrombus.
Common Alder (Black Alder). Cytoxan.
- Sore throat, pharyngitis, and bleeding in the intestines.
- What is Black Alder?
- Dosing considerations for Black Alder.
- How does Black Alder work?
- Are there safety concerns?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96585
Buy cheap cytoxan 50mg line
Valvular dysfunction mainly results from chronic inflammation symptoms graves disease buy cheap cytoxan line, fibrosis, and calcification. Acute rheumatic fever Rheumatic fever is an inflammatory disease that usually affects children and young adults aged between 1 and 19 years. Approximately two-thirds of rheumatic fever patients progress to rheumatic carditis and only a portion of them suffer from severe cardiac manifestations. However, studies have shown evidence of an epitope-spreading phenomenon (molecular mimicry) and the development of a long-lasting cellular immune response that are responsible for the cardiovascular damage. Group A streptococcus pyogenes is an important pathogenic bacterium that causes a wide variety of clinical conditions ranging from pharyngitis to 34 the pathophysiology of mitral stenosis severe invasive infections and necrotizing fasciitis. The most common mode of disease transmission is by direct contact of mucus droplets from an infected person. According to the Lancefield classification, they are categorized as group A because they display antigen A on their cell wall. The outer layer of streptococcus pyogenes is covered by a hyaluronic acid capsule that is chemically similar to the host connective tissue; therefore, it is non-antigenic. The cytoplasmic membrane has antigens similar to human cardiac, skeletal, and smooth muscle cells. C-Carbohydrates: Protect the streptococcus from being dissolved by the lysosomal defense mechanisms of the host. Lipoteichoic acid: Enables streptococcus pyogenes to adhere to the epithelial cells in the skin or respiratory mucosa. M-protein: A fibrillary surface projection that contributes to the virulence of the organism by resisting phagocytosis and improving adherence. Hyaluronic acid: Also found in human tissue; hence, it does not provoke an immune response from the host. Its amount and distribution vary in different cases and depend on the duration of the disease. Sometimes, the valve may show extensive calcification with surrounding foreign body giant cell reaction to the deposited calcium. Repetitive trauma due to changes in hemodynamic stress and the chronic inflammatory process of the valve tissue leads to the formation of vegetations on the mitral valve surface near the line of closure. These are usually fibrin-rich vegetations without any organisms (aseptic vegetations). Sometimes, repetitive trauma may also be the precedent factor for superadded secondary infections, leading to secondary infective vegetations. Due to the obstruction in the normal blood flow, there will be an increased transmitral pressure gradient in the left atrium. This will lead to decreased filling in the left ventricle, which further causes a decrease in blood volume and decreased stroke volume resulting in a decrease in cardiac output. Commonly associated adaptive changes include hypertrophy of the atrial muscle fibers and interstitial fibrosis due to the deposition of collagen between the cardiac myocytes, which leads to geometric remodeling and dilatation of the left atrium. These changes are known to cause the development of atrial fibrillations and intra-atrial luminal thrombus. This is mainly because of the transmission of back pressure from the left atrium to the pulmonary veins and subsequently to the pulmonary capillaries and arteries. A constant increase in back pressure leads to histopathological alterations in the pulmonary vasculature. Quantitative pulmonary parenchymal and vascular changes are usually seen consistently in almost all cases, with more severity in younger individuals. Anatomy of the mitral valve: Understanding the mitral valve complex in mitral regurgitation. Lung parenchyma may show accumulation of proteinaceous fluid and red blood cells in the alveolar interstitium and lumen due to pulmonary edema. The interstitial space may show congestion of the septal capillaries and areas of hemorrhage because of the rupture of small-caliber vessels due to increased luminal pressure. In chronic stages, the extravasated red blood cells will be degraded by the alveolar macrophages, which in turn form hemosiderin-laden macrophages. Etiopathogenesis includes the chronic inflammatory disease process affecting the heart valves due to cross-reactivity of streptococcal antigens with the cardiac myosin. Although Aschoff nodules are rarely seen in histopathological specimens, they are a pathognomonic feature of rheumatic valvular heart disease. The number of Aschoff nodules may vary but their presence does not indicate the activity of the disease process. Spectrum of congenital mitral valve abnormalities associated with solitary undifferentiated papillary muscle in adults. Congenital uni-leaflet mitral valve with severe stenosis: A case report with literature review. Accessory mitral valve leaflet causing severe left ventricular outflow tract obstruction in a preterm neonate with a partial atrioventricular septal defect. The infant with aortic arch hypoplasia and small left heart structures: Echocardiographic indices of mitral and aortic hypoplasia predicting successful biventricular repair. Association of triglyceride-related genetic variants with mitral annular calcification. Special Writing Group of the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease of the Council on Cardiovascular Disease in the Young of the American Heart Association. A description of six grades of structural changes in the pulmonary arteries with special reference to congenital cardiac septal defects. In combined valve diseases, the clinical features are often modified by the severity of other associated valvular lesions. Typically, there is a latent period from the occurrence of rheumatic fever to the onset of symptoms. In less developed countries, where incidence of rheumatic fever is as high as 50/100,000, patients may present with symptoms as early as the second, and the vast majority present in the third to fourth, decade of life. Whether this difference is explained by a more aggressive form of disease progression after an episode of rheumatic carditis, or due to repeated subclinical carditis in highly endemic areas with rheumatic fever, is debatable. This may be attributed to better awareness and early medical attention and treatment of all acute rheumatic fever cases, resulting in the survival of all patients with acute rheumatic fever-mitral incompetence being the major residual lesion in almost all of them. The diastolic transvalvular pressure gradient for any given valve area is a function of the square of the transvalvular flow rate. Similarly, to maintain the same forward stroke output, the transmitral gradient increases proportionately, as a function of the square of decrease in cross-sectional valve area. Stated simply, doubling transmitral flow quadruples the gradient; halving the valve area quadruples the gradient. This happens due to the fusion of the anterior and posterior mitral leaflets along the closure line extending from the mitral annulus, along the posteromedial and anterolateral commissures towards the center, resulting in a central oval stenotic orifice. Degenerative changes like fibrosis and Symptom progression 49 pulmonary regurgitation. Right-heart failure leads to hepatic congestion, elevated jugular venous pressure, ascites, and bilateral pedal edema. Rupture of the pulmonary veins from elevated hydrostatic pressure can result in hemoptysis. Although left-ventricular end-diastolic pressure and cardiac output remains within the normal range in the early stages of the disease, cardiac output falls over time, leading to a state of low cardiac output. However, the life expectancy of such patients is still low as expected for the age due to the related complications of the disease. Mild symptoms on accustomed effort will be present once the valve area falls below 2 cm2. However, this may not be forthcoming from the history, as most patients will scale down their physical activity to avoid the unpleasant sensation of dyspnea. Following the onset of mild effort limitation and dyspnea, it takes around 7 to 9 years to develop severe complications. However, factors such as severe anemia, fever, thyrotoxicosis, exercise, pregnancy, or excitement may trigger an attack of dyspnea. As the stenosis worsens, symptoms of dyspnea on exertion, paroxysmal nocturnal dyspnea, or orthopnea develop.
Generic 50mg cytoxan otc
A less painful parenteral alternative is benzathine penicillin in combination with procaine penicillin treatment trichomoniasis cheap 50 mg cytoxan otc. Other -lactams, including semisynthetic derivatives of penicillin and the cephalosporins, are at least as effective as penicillin for treating streptococcal pharyngitis. The broader spectrum of the cephalosporins and their higher cost relegate them to second-line status. The decreased dosing frequency of amoxicillin and some cephalosporins may improve patient adherence. Patients who are allergic to penicillin can receive a cephalosporin if they have not had an immediate hypersensitivity reaction. Erythromycin or another non-lactam antibiotic, such as clarithromycin, azithromycin, or clindamycin, can be used. Of note, both macrolide and clindamycin resistance are more common in Canada than in the United States. Fever, dysphagia, drooling, stridor, extension of the neck, and a mass in the posterior pharyngeal wall may be noted. The markedly swollen and tender anterior cervical nodes that result can suppurate. Additional parapharyngeal suppurative infections that may mimic streptococcal disease are noted in Table 1. Oropharyngeal torticollis lasts less than 2 weeks and is not associated with abnormal neurologic signs or pain over the spinous process. In addition, an association between streptococcal infection and neuropsychiatric disorders such as tic disorder, obsessivecompulsive disorder, and Tourette syndrome has been postulated. The reason for the near disappearance of rheumatogenic types in the United States is unknown. The left tonsil is asymmetrically inflamed and swollen; there is displacement of the uvula to the opposite side. The supratonsillar space (arrow) is also swollen; this is the usual site of the surgical incision for drainage. A, Lateral soft tissue neck radiograph reveals extensive soft tissue swelling displacing the airway anteriorly from the skull base to C6 (arrow). B, Sagittal reconstructed contrast-enhanced computed tomography confirms thickened, enhancing retropharyngeal soft tissues indicating cellulitis. Region of hypoattenuating fluid is concerning for retropharyngeal abscess (asterisk). In infants the retropharyngeal space is usually less than one width of the adjacent vertebral body. In addition, under normal circumstances, the retrotracheal space does not exceed 22 mm in adolescents when measured from the anterior aspect of C6 to the trachea. Dotted lines depict the "thumbprint" sign, noted on a lateral neck radiograph, made by a swollen epiglottis. This causes considerable consternation among affected patients and their families. A few such patients are symptomatic and are characterized as having clinical treatment failure. Re-infection with the same strain or a different strain is possible, as is intercurrent viral pharyngitis. There is no easy way to identify chronic carriers prospectively among patients with symptoms of acute pharyngitis. Available treatment options for the physician faced with a chronic streptococcal carrier include the following: 1. Acute rheumatic fever is not a sequela to these infections but acute glomerulonephritis has been documented in rare cases after epidemic group C and group G streptococcal pharyngitis. The first option is simple, as safe as amoxicillin and penicillin, and appropriate for most patients. Amoxicillin-clavulanate (40 mg amoxicillin/kg/day up to 2000 mg amoxicillin/day divided tid for 10 days) has also been used. Approximately 80% of cases of Lemierre syndrome are due to this bacterium, but the proportion of patients infected or colonized with F. Patients present initially with fever, sore throat, exudative pharyngitis, and/or peritonsillar abscess. The symptoms persist, severe neck pain and swelling develop, and the patient appears toxic. Septic shock may ensue along with metastatic complications, especially septic pulmonary emboli. Diagnosis is confirmed by computed tomography or magnetic resonance imaging of the neck and isolation of the organism on anaerobic blood culture. Many expert clinicians use metronidazole, clindamycin, a -lactam in combination with a -lactamase inhibitor (such as ampicillin-sulbactam), or a carbapenem. The septic thrombophlebitis of Lemierre syndrome can be polymicrobial; combination antibiotic therapy may be beneficial. In contrast to chronic carriers, appropriate antibiotic treatment of each episode results in eradication of the organism. The role of tonsillectomy in the management of patients with multiple episodes of streptococcal pharyngitis is controversial. Fewer episodes of sore throat were reported among patients treated with tonsillectomy (in contrast to patients treated without surgery) during the first 2 years after operation. By 2 years after tonsillectomy there was no difference between the groups in the frequency of pharyngitis. Tonsillectomy cannot be recommended for treatment of recurrent pharyngitis except in unusual circumstances. Obtaining follow-up throat specimens for culture can help distinguish recurrent pharyngitis from chronic carriage but is unnecessary in most instances. Well-documented epidemics of food-borne group C and group G streptococcal pharyngitis have been reported in young adults. In these situations, a high percentage of individuals who had ingested the contaminated food promptly developed acute pharyngitis, and throat cultures yielded virtually pure growth of the epidemiologically linked organism. However, the role of non-A streptococcal organisms as etiologic agents of acute pharyngitis in endemic circumstances has been difficult to establish. Group C and group G streptococci may be responsible for acute pharyngitis, particularly in adolescents. However, the exact role of these agents, most of which are carried asymptomatically in the pharynx of some children and young adults, remains to be fully characterized. Detecting this agent requires special methods for culture, and it has not routinely been sought in patients with scarlet fever or pharyngitis. The rash is erythematous and blanches; it may be pruritic and demonstrate minimal desquamation. A, Axial contrast enhanced computed tomography image shows low-attenuation retropharyngeal fluid (asterisk). B, Magnetic resonance imaging 2 days later, performed because of acute left arm weakness, confirms lack of left internal jugular vein patency on magnetic resonance venogram. C, Diffusion-weighted image of the brain reveals multiple small foci of bright signal infarction secondary to emboli from thrombophelebitis, vasospasm, or both. Historically, it was an infection in 1-4 year-old children caused by Haemophilus influenzae type b. Management depends on establishing a secure airway by intubation and treating with antibiotics. When epiglottitis is suspected, the oropharynx should not be visualized or manipulated except in a controlled environment (intensive care unit or operating room) by someone with expertise in management of the airway who is prepared to immediately intubate the patient. Bacterial tracheitis (bacterial croup, bacterial laryngotracheitis) is a rare complication of viral croup. Patients have a history of prolonged croup symptoms that become dramatically worse with fever and signs of airway obstruction. While sore throat may have been present at the onset of croup, it is not a prominent complaint once bacterial infection of the airway occurs. The clinical appearance of patients with bacterial tracheitis may mimic that of patients with epiglottitis. It has become very rare in the United States and other developed countries as a result of immunization.
Purchase 50 mg cytoxan visa
Because the virus is endemic to human beings medications quizlet order cytoxan online from canada, the disease is highly contagious and is transmitted through respiratory secretions. Before widespread rubella immunization, this viral infection usually occurred in childhood, although it also affected adults. Epidemiology of Rubella Three strains of live, attenuated rubella vaccine virus were developed and first licensed for use in the United States in 1969. Before widespread rubella immunization in the United States and Canada, rubella infections occurred in epidemic proportion at 6- to 9-year intervals. In 1964 more than 20,000 cases of congenital rubella syndrome and an unknown number of stillbirths occurred in the United States as the result of an epidemic that year. Costa Rica, Honduras, Brazil, and Chile, as well as the member countries of the Caribbean, have rubella elimination initiatives under way. In countries where vaccination is uncommon, the incidence of rubella infection is high and epidemics are common. However, pockets of unvaccinated children appear to have fueled the 2014 to 2015 measles outbreak traced back to Disneyland in California. Because measles is so contagious, a high level of vaccination coverage is necessary to prevent outbreaks. In the case of the Disney outbreak, the vaccination rates of the exposed population may be as low as 50% but no higher than 86%. Herd immunity occurs when most of a population has been vaccinated for an infectious disease. This provides some protection for people who are not vaccinated, but if herd immunity erodes, the most contagious diseases emerge first. Many cases of rubella infection have been unrecognized or unreported because these cases are mild or subclinical. Contracting the infection and vaccinating against rubella are the only routes to developing immunity. Individuals should be immune to rubella if they have a dated record of rubella vaccination on or after their first birthday, or if they have demonstrable rubella antibody. Even when antibody titers fall to relatively low levels, previous infection or successful vaccination appears to confer permanent immunity to rubella, except in cases of congenital rubella. The only proof of immunity is a positive serologic screening test result for rubella antibody. A history of rubella infection, even if verified by a physician, is not acceptable evidence of immunity. It is critical to continue to determine the rubella immune status of women of childbearing age and to vaccinate those who are not immune. If the patient is not rubella-immune, she should be cautioned to avoid exposure to rubella infection. Vaccination is contraindicated in pregnant women; however, a woman should be vaccinated immediately after termination of the pregnancy. The Institute of Medicine has determined that a causal relationship exists between rubella vaccine and acute arthritis in adult females. There is weak but consistent evidence for a causal relationship between rubella vaccine and chronic arthritis in adult women. Incidence rates are estimated to average 13% to 15% in adult women after vaccination. Much lower levels of arthritic adverse reactions were noted in children, adolescents, and adult males. Reliable estimates of excess risk of chronic arthritis after rubella vaccination are not available. Signs and Symptoms of Rubella Infection A diagnosis of acquired rubella is not based solely on clinical manifestations. The signs and symptoms of rubella vary widely from person to person and may not be recognized in some cases, especially if the characteristic rash is light or absent, as may occur in a substantial number of cases. Rubella infection also may resemble other disorders, such as infectious mononucleosis and drug-induced rashes. Acquired Rubella Infection the incubation period of acquired rubella infection varies from 10 to 21 days, and 12 to 14 days is typical. Infected persons are usually contagious for 12 to 15 days, beginning 5 to 7 days before the appearance (if present) of a rash. Acute rubella infection lasts from 3 to 5 days and generally requires minimal treatment. Congenital Rubella Infection Rubella infection is usually a mild, self-limiting disease with only rare complications in children and adults. In utero infection can result in fetal death or manifest as rubella syndrome, a spectrum of congenital defects. Some infants manifest almost all the defects associated with rubella, whereas others exhibit few, if any, consequences of infection. Clinical evidence of congenital rubella infection may not be recognized for months or even years after birth. In addition to stillbirth, fetal abnormalities associated with maternal rubella infection include encephalitis, hepatomegaly, bone defects, mental retardation, cataracts, thrombocytopenic purpura, cardiovascular defects, splenomegaly, and microcephaly. Severely affected children are likely to have multiple defects in different organ systems. In neonates with congenital rubella syndrome, low birth weight and failure to thrive are common. In late childhood, however, about one third of these patients lose antibody and become susceptible to acquired rubella. Children with congenital rubella should be screened for rubella immunity in late childhood and vaccinated if necessary. Immunologic Manifestations Acquired Rubella Infection In a patient with primary rubella infection, the appearance of both immunoglobulin G (IgG) and immunoglobulin M (IgM) antibodies is associated with the appearance of clinical signs and symptoms, when present. These antibodies persist but rapidly diminish in concentration over the next 4 to 5 weeks, until antibody is no longer clinically detectable. The presence of IgM antibody in a single specimen suggests that the patient has recently experienced a rubella infection. Production of IgG is also associated with the appearance of clinical signs and symptoms. Antibody levels increase rapidly for the next 7 to 21 days and then level off or even decrease in strength. Detection of IgG antibody is a useful indicator of rubella infection only when the acute and convalescent blood specimens are drawn several weeks apart. Optimum timing for paired testing in the diagnosis of a recent infection is 2 or more weeks apart, with the first (acute) specimen taken before or at the time signs and symptoms appear, or within 2 weeks of exposure. In these cases, either the patient was previously immunized or the acute sample was taken after the antibody had already reached maximum levels. Demonstration of an unequivocal increase in IgG antibody concentration between the acute and convalescent specimens suggests a recent primary infection or a secondary (anamnestic) antibody response to rubella in an immune individual. In cases of an anamnestic response, IgM antibodies are not demonstrable, but IgG production begins quickly. If both IgM and IgG test results are negative, the patient has never had rubella infection or been vaccinated. If no IgM is demonstrable but IgG is present in paired specimens, the patient is immune.
Purchase 50 mg cytoxan with mastercard
In a few instances medications routes purchase cheapest cytoxan, where the atrial septal defect is restrictive and mitral stenosis is severe, transatrial pressure gradients exist throughout the cardiac cycle. The continuous murmur is best heard at the lowerright sternal border and corresponds to the site of the right atrium. A continuous murmur at this site has few differentials: Ruptured sinus of Valsalva to the right atrium and coronary cameral fistula to the right atrium. While the former is distinguished by its loud and harsh quality, the continuous murmur of a coronary cameral fistula draining to the right atrium is accentuated during systole. Left-atrial enlargement and pulmonary venous congestion serve to distinguish a patient of mitral stenosis with Lutembacher syndrome. Enlargement of the right heart and pulmonary artery is 268 Lutembacher syndrome common to both. Pulmonary plethora reflects increased pulmonary blood flow from the pretricuspid shunt. Pulmonary venous congestion may be less conspicuous as compared to a patient with isolated mitral stenosis. Transmitral gradients are underestimated and cannot be used to assess the severity of mitral stenosis. The degree of pulmonary hypertension and orifice area help in assessing the severity of mitral stenosis. The atrial septal defect should be profiled on two-dimensional echocardiography and color Doppler that shows left-to-right shunt, dilated right-sided chambers, and pulmonary hypertension. On rare occasions, sinus venosus defects have been associated with mitral stenosis. Cardiac catheterization is not performed to make a diagnosis, as the requisite information to diagnose and manage the condition is obtained on echocardiography. However, if transcatheter management is contemplated, several interesting features may be noted. Equalization of a- and v-wave amplitudes are demonstrated in rightatrial pressure tracings due to the large, non-restrictive atrial septal defect. The left- and right-atrial pressures are equal and usually not high, unless there is severe pulmonary hypertension. The increased pulmonary diastolic pressure would then translate into elevated right-ventricular end-diastolic and atrial pressures. Simultaneous pressure tracings of the left ventricle and left atrium should be obtained after the mitral valve has been crossed. Crossing the mitral valve may be difficult due to the lack of support for an Inoue catheter system at the level of interatrial septum, especially if the atrioventricular or inferior venacaval rim is deficient. We may have to resort to an over-the-wire technique to track the balloon across the valve. It is our practice to refer them for surgery, as device closure would preclude future transcatheter procedures for mitral restenosis. The dictum is not to close the atrial septal defect, unless the mitral stenosis has been relieved and has been followed up for gradual progression over several years. This is especially important in patients who have undergone percutaneous transmitral commissurotomy in the second decade of life, as there is a chance of progression and restenosis over subsequent years, necessitating a repeat procedure for mitral stenosis. A new concept of mitral valve disease and left to right shunt at the atrial level. Coexistent mitral valve disease with left to right shunt at atrial level: Clinical profile, hemodynamics and surgical considerations in 67 consecutive patients. Atrial septal defect associated with mitral stenosis: the Lutembacher syndrome revisited. Transcatheter treatment of Lutembacher syndrome: Combined balloon mitral valvuloplasty and percutaneous atrial septal defect closure. These patients are at increased risk of thromboembolism and stroke, as well as complications of long term anticoagulation. Rheumatic inflammatory activity also contributes to myocardial disarray and fibrosis. In severe cases, extensive areas of sarcoplasmic vacuolation and presence of myelin figures and mitochondrial aggregates were seen. Local and global conduction abnormalities in the form of fractionated electrograms, double potentials, and increased conduction time are present. On electrical stimulation, these patients have a higher tendency to develop atrial fibrillation. Not uncommonly, a persistent high ventricular rate may lead to tachycardiomyopathy and heart failure. The variable conduction produces the characteristic "irregularly irregular" pulse. Heart rate needs to be controlled and conversion to sinus rhythm in some selected patients is a reasonable option. This effect might have been caused by a reduction in sudden death and myocardial infarction. Although exercise tolerance was better with rhythm control, there were more frequent hospital admissions and an increase in non-cardiovascular mortality in the rhythm control group. However, 280 Atrial fibrillation and other arrhythmias these interventions may lead to a higher rate of successful cardioversion and maintenance of sinus rhythm. Alternatively, after ruling out the presence of atrial thrombus on transesophageal echocardiography, immediate cardioversion can be carried out after intravenous heparin anticoagulation. Though the pharmacological approach appears satisfactory in short-term studies, the result may not be sustained in long term. Therefore, the conventional full maze procedure carries a potential risk of postoperative complications, such as bleeding, lowoutput syndrome, and sick sinus syndrome. The substitution of conventional incisions by sutureless techniques such as cryoablation or radiofrequency ablation has significantly decreased the bypass time and helped in preserving the mechanical function of the atria. Atrial flutter and atrial tachycardias were treated on the basis of activation and entrainment mapping. While the efficacy of a single procedure was 35%, nearly three-quarters of patients were in sinus rhythm at 2 years after repeat procedure(s). A reasonable Holter definition of heart rate during normal activity should be 80 bpm and certainly none of the hour-averaging rates 90 bpm. Intravenous diltiazem, verapamil, or -blockers are effective in controlling heart rate more rapidly and are used in severely symptomatic patients. Rate control Adequate ventricular rate control ameliorates the negative hemodynamic effect of fast heart rate. Prolonged periods of rapid ventricular rate can lead to tachyarrhythmic 282 Atrial fibrillation and other arrhythmias 5. Prevalence and predictors of atrial fibrillation in rheumatic valvular heart disease. Factors associated with the development of atrial fibrillation in patients with rheumatic mitral stenosis. Prevention of systemic arterial embolism in chronic rheumatic heart disease by means of protracted anticoagulant therapy. Atrial fibrillation in mitral stenosis: Histologic, hemodynamic and metabolic factors. Clinical, echocardiographic, and hemodynamic characteristics of rheumatic mitral valve stenosis and atrial fibrillation. Factors associated with atrial fibrillation in patients with mitral stenosis: A cardiac catheterization study. Two-dimensional atrial systolic strain imaging predicts atrial fibrillation at 4-year follow-up in asymptomatic rheumatic mitral stenosis. Prediction of atrial fibrillation in patients with severe mitral stenosis: Role of atrial contribution to ventricular filling. Angiographic and histomorphometric study of pulmonary veins in rheumatic heart disease. Angiographic study of pulmonary venous anatomy in patients with rheumatic heart disease with mitral stenosis undergoing balloon mitral valvotomy. Light and electron microscopic features of surgically excised left atrial appendage in rheumatic heart disease patients with atrial fibrillation and sinus rhythm.
Buy 50mg cytoxan visa
Pelech Most heart murmurs are normal or innocent treatment sinus infection buy discount cytoxan line, and must be distinguished from pathologic murmurs of congenital or acquired cardiac diseases. Whereas less than 1% of the population has structural congenital cardiac disease, as many as 85% of the population has a heart murmur sometime during childhood. The causes of cardiac murmurs are often influenced by the age of the patient at presentation (Table 8. The causes of congenital heart disease are varied and include genetic disorders, syndrome complexes (Table 8. The causes of acquired heart diseases in children include rheumatic fever, endocarditis, and cardiac injury caused by systemic illnesses. It is important to understand the timing of events in the cardiac cycle as a prerequisite to understanding heart murmurs. The cardiac cycle begins with atrial systole, the sequential activation and contraction of the 2 thin-walled upper chambers. Atrial systole is followed by the delayed contraction of the more powerful lower chambers, termed ventricular systole. Isovolumic contraction: the short period of early contraction when the pressure builds within the ventricle but has yet to rise sufficiently to permit ejection 2. Ventricular ejection: when the ventricles eject blood to the body (via the aorta) and to the lungs (via the pulmonary artery) 3. Isovolumic relaxation: the period of ventricular relaxation when ejection ceases and pressure falls within the ventricles During ventricular contraction, the atria relax (atrial diastole) and receive venous return from both the body and the lungs. Then, in ventricular diastole, the lower chambers relax, allowing initial passive filling of the thick-walled ventricles and emptying of the atria. This atrial systole augments ventricular filling just before the onset of the next ventricular contraction. The relationship of blood volume, pressure, and flow determines opening and closing of heart valves and generates characteristic heart sounds and murmurs. The right atrium and right ventricle are located anteriorly, immediately beneath the sternum. The outflow tract of the right ventricle, which contains the pulmonary valve, rises to the left of the sternum. The parts of the left side of the heart that are close to the chest wall include the left ventricular apex and the ascending aorta as it passes up to the right of the sternum. The amount of pressure that forces the valve closure influences the intensity of a heart sound. Other mechanical factors such as valve stiffness, thickness, and excursion have less effect on sound intensity. The amount of turbulence and consequently the intensity of a cardiac murmur is directly proportional to both the pressure difference or gradient across a narrowing or defect and the blood flow or volume moving across the site. As sound radiates from its source, sound intensity diminishes with the square of the distance. Sound passage through the body is affected by the transmission characteristics of the tissues. Fat has a more pronounced dampening effect on higher frequencies than does more dense tissue such as bone. If the difference in tissue density is significant-for example, between the heart and lungs-more sound energy is lost. Only the loudest sounds may be heard when lung tissue is positioned between the heart and chest wall. In contrast to intensity, the frequency of a cardiac murmur is proportional to pressure difference or gradient across a narrowing alone. The majority of significant structural congenital heart disease is recognized in the first few weeks of life. The age at recognition or referral often dictates the nature of the cardiac anomaly and the urgency with which assessment is necessary. Preferentially, flow is directed across the foramen ovale to enter the left atrium and, subsequently, the left ventricle. Other and more complex lesions (forms of heterotaxy) together represent 5-10% of all lesions. The pressures within both ventricles are essentially equal, inasmuch as both chambers pump to the systemic circulation. However, in utero, the right ventricle does the majority of the work, pumping 66% of the combined cardiac output. Through mechanical and chemical mechanisms, the ductus arteriosus begins to close. Intermittent right-to-left atrial level shunting through the foramen ovale may occur, particularly if pulmonary vascular resistance fails to drop. In addition, structural cardiac abnormalities necessitating patency of the ductus arteriosus for maintenance of either pulmonary blood flow (pulmonary atresia) or systemic blood flow (hypoplastic left heart syndrome) most often manifest within the first few days of life. Thus, the time when a pediatric patient presents for evaluation is influenced by the spectrum of heart diseases. Ductusdependent abnormalities, such as pulmonary atresia, transposition of the great arteries, coarctation of the aorta, hypoplastic left heart syndrome, or significant outflow obstructions. Pressure in the great vessels during systole is identical to that in the corresponding ventricles. Resistance to blood flow in the vascular bed determines the diastolic pressures in the great arteries. The thin-walled atria generate much lower pressures than do the ventricles, both during the phase of passive atrial filling (v wave) and during atrial contraction (a wave). During ventricular relaxation, the diastolic pressures are lower than those in the atria, enabling filling. Knowledge of the cardiac cycle is important in understanding the more complicated hemodynamics and flow patterns of specific cardiac abnormalities. An index of exercise or play capacity should be sought, as should an assessment of growth and development. The presence of congenital abnormalities of other major organ systems is associated with structural cardiac problems in as many as 25% of patients. Structural heart disease is frequently seen in association with recognizable syndromes (see Table 8. Family history of sudden unexplained death, rheumatic fever, sudden infant death syndrome, or a structural cardiac abnormality in a first-degree relative may be relevant. Hypertrophic cardiomyopathy in a first-degree relative is associated with a high incidence of inheritance, and this condition is sufficiently subtle that echocardiographic screening is mandatory. A maternal history of gestational diabetes mellitus may be associated with a transient hypertrophic cardiomyopathy in as many as 30% of infants of these mothers, as well as with definable congenital structural abnormalities. Unexplained fever, lethargy, a history of intravenous drug use, or additional symptoms arising after recent dental work should arouse suspicion of possible endocarditis. Particularly relevant are the rate of growth, development, and history of past illnesses. Although symptoms of failure to thrive are nonspecific, patterns of growth reflect duration and severity of the disease and effectiveness of treatment (see Chapter 9). In an infant, feeding difficulties are often the first evidence of congestive heart failure. Feeding problems are common manifestations of cardiac disease and may be evidenced as disinterest, excessive fatigue, long feeding duration, diaphoresis, tachypnea, dyspnea, or a change in the pattern of respiration. It is important to obtain a measure of caloric intake by quantitating the number and/or volume of feedings. Some index of exertional tolerance should be sought in all children as an index of cardiovascular fitness and a sign of functional capability. This index should be age relevant and, in an infant, might include assessment of the vigor and duration of feeding and the time period of interactive play. In a toddler, the index might include ability to keep up with peers, climb stairs, or walk for extended periods. In an older child, a comparison with peer sporting interactions, level of function in physical education, and an index of aerobic ability should be sought.