Buy line nebivolol
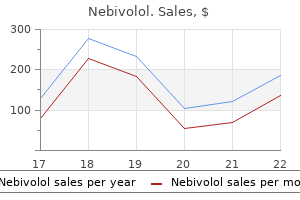
We prefer a complete total intravenous anesthetic protocol using a continuous infusion of propofol combined with either fentanyl or remifentanil blood pressure chart easy to read nebivolol 5mg otc. Inhaled agents are avoided, particularly nitrous oxide, because of their detrimental effects on motor evoked potentials. We do not use three-point cranial fixation because rigid fixation is unnecessary and could cause injury to the patient if a seizure is induced during cortical stimulation/mapping. To center the incision over the M1 region, the midpoint from nasion to inion is determined,* and a curved incision extending from approximately 1 cm behind this midpoint toward the anterior margin of the tragus is marked on the scalp before preparing and draping the surgical field. This incision allows a 5- to 6-cm craniotomy, which can be adjusted superiorly or inferiorly along the convexity to map the hand or face, respectively. Even though the craniotomy lies mainly above the superior temporal line, the superior edge of the temporalis muscle may be detached when access to the facial region of M1 is required. One may leave a cuff of temporalis fascia for reattachment of the muscle during closure. Somatosensory testing consists of placing the paddle electrode (Resume, Medtronic, Inc. The central sulcus is defined as the point at which the N20 response phase reverses polarity. The electromyogram from muscles in the upper extremity is shown after stimulation with a ball-tipped electrode in threelocationsonthedura. Typically, 7 to 10 recordings are obtained, which takes no more than 10 minutes of operative time. Electromyographic recording needles are placed in bipolar fashion in the orbicularis oculi, orbicularis oris, trapezius, deltoid, biceps, triceps, flexor carpi ulnaris, abductor pollicis brevis, first dorsal interosseus, quadriceps, tibialis anterior, and abductor hallucis muscles. Stimulation is begun at each location starting at 5 mA and increased in 1-mA steps until a motor response is elicited or the maximal stimulus of 25 mA is reached. Ice-cold saline is kept ready in the field to irrigate the dura should a seizure occur. In our experience, the mean stimulation amplitude required to generate an evoked response is 13. We reiterate the importance of anesthetic technique for successful performance of physiologic mapping. Once the location of the appropriate overlying region of dura is identified, the lead is sutured to the dura with 4-0 Neurolon. The cable exits through one of the bur holes and is tunneled ProgrammingtheImplantedDevice the implanted stimulator is activated within 24 hours of surgery. During the initial programming session we evaluate the effects of cathodal stimulation via each contact in a monopolar configuration. The use of cathodal stimulation might be questioned given that anodal stimulation administered via transcranial electrical and magnetic stimulation generates D waves and motor evoked potentials at lower intensities. Moreover, work by Hanajima and coworkers has revealed that chronic cathodal stimulation activates neurons in the motor cortex at lower stimulation intensities than does anodal stimulation. One occurred 2 days after the initial programming in a patient who also had a seizure during intraoperative mapping. The second seizure occurred in a patient with a stroke 18 months after surgery when the stimulator voltage was raised from 4. If the patient could not tolerate these settings, either contact 3 or 0 alone was used instead. In all cases, at least two contacts were activated at the initial programming session. If minimal benefit was noted from these initial settings, additional contacts were activated. Table 93-1 shows the stimulation parameters relative to the surgical implant date. For upper limb pain, care is taken to note intraoperatively which contact or contacts overlie the corresponding painful area as determined by motor mapping. The electrode configuration is determined by the contact that generates the greatest motor response at the lowest stimulus intensity intraoperatively. Stimulation frequency begins at 130 Hz, but in our experience a variety of frequencies have been tried with varied success. Patient P2 has good control of her upper extremity and face pain, but less pain control in her leg and minimal control of sensations of a "third limb. The patient with atypical head pain (P3) has experienced no relief in his scalp contralateral to the stimulation but is receiving benefit in his ipsilateral scalp region, which is not easily explained but may be related to stimulation of the trigeminal branches innervating the dura. A wide range of stimulation parameters have been used in these patients, with amplitudes ranging from 2. At the time of explantation this patient had improved approximately 50% in comparison to baseline but regressed significantly when the device was removed. In our series of patients with neuropathic pain the results are even less consistent. Despite wide variation in results, some of our patients have experienced modest success. None of the patients were able to check the devices independently and thus had no means to discover that they were depleted. Drouot and colleagues hypothesized that secondary messengers or long-term potentiation may account for the delayed response. Our experience, although quite limited, suggests that in certain cases there is long-lasting benefit that might be enhanced with additional knowledge. Effects of acute stimulation through contacts placed on the motor cortex for chronic stimulation. Control of post-stroke involuntary and voluntary movement disorders with deep brain or epidural cortical stimulation. Chronic motor cortex stimulation in the treatment of central and neuropathic pain. Motor cortex stimulation for refractory neuropathic pain: four-year outcome and predictors of efficacy. History and first results by the study group of the Italian neurosurgical society. Zerris Hundreds of thousands of people are afflicted by injuries or disorders that disrupt input-output pathways of the nervous system while sparing upper level brain areas and leaving them cognitively intact. These nervous system insults significantly reduce quality of life by interrupting the neural pathways carrying movement, auditory, and visual information. Revolutionary advances in neuroscience, biomedical engineering, and computer science have propelled the development of innovative neuroprosthetic devices that can physically restore or replace lost nervous system function. Some neuroprosthetic devices based on electrical stimulation of neural tissue, such as cochlear implants and deep brain stimulators, have demonstrated widespread clinical success. Recent developments in neurotechnology are showing promising results in restoring movement to persons with paralysis and sight to those with visual loss. By the early 1950s, stimulating and recording electrodes were placed intracranially in human cortex in the hope of alleviating psychosis. Thus, one can think of these systems in the context of two broader categories: those that interpret signals and those that create them. The physical systems that allow restoration of voluntary movement and re-creation of sensory input to the brain share an analogous set of components despite the fact that they use different signals and outputs. Upper level motor areas are frequently preserved in cases of trauma, stroke, and neurodegenerative diseases of the descending motor tracts and spinal cord. One natural source for acquiring movement information is the frontal lobe motor areas where these commands are generated. The primary motor cortex (M1), which is located roughly along the posterior half of the precentral gyrus, and the premotor cortex and supplemental motor area, which extend anteriorly from M1, give rise to the neural signals responsible for planning, initiating, and generating volitional movement.
Order cheapest nebivolol
The tumors were reasonably well circumscribed anaplastic gliomas, with some invasion of surrounding normal brain tissue heart attack jaw pain right side purchase generic nebivolol line. Although some perivascular lymphocytic cuffing was seen, there was negligible intratumoral lymphocyte infiltration. Gavin and associates described central nervous system tumors in dogs and other large animals. Ausman and colleagues reported on the implantation of choriocarcinoma in the brain of rhesus monkeys,200 as first described by Lewis and associates. Because thalidomide was originally developed as a sedative, it is already known to traverse the normal blood-brain barrier. In particular, sorafenib and bevacizumab have been shown to have clinical activity against a variety of solid tumors. Still, given the possibility that antiangiogenic therapies may actually increase invasiveness, these data must be regarded with caution. Early postoperative magnetic resonance imaging after resection of malignant glioma: objective evaluation of residual tumor and its influence on regrowth and prognosis. Development of an in vitro extracellular matrix assay for studies of brain tumor cell invasion. The in vitro motility of human gliomas increases with increasing grade of malignancy. Molecular insights into cancer invasion: strategies for prevention and intervention. Randomized, double-blind, placebocontrolled trial of marimastat in glioblastoma multiforme patients following surgery and irradiation. Analysis of the spatial characteristics of metabolic abnormalities in newly diagnosed glioma patients. The paradox of neoplastic glial cell invasion of the brain and apparent metastatic failure. Targeted therapy for metastatic renal cell carcinoma: a home run or a work in progress Invasive behaviour of human gliomas is mediated by interindividually different integrin patterns. Extracellular matrix 2: role of extracellular matrix molecules and their receptors in the nervous system. Wong the treatment of brain tumors, especially glioblastoma, is being transformed by the recent introduction of a new class of therapeutic agents: molecular-targeted, antiangiogenic drugs. He coined the term chemotherapy and described (1) specific cellular receptors, (2) the blood-brain barrier, (3) neurotoxicity of drugs, (4) rationally "designed" drugs, and (5) animal models as part of a systematic approach to drug discovery-thereby creating the foundations of experimental therapeutics in oncology. Phase I trials showed that bevacizumab was well tolerated and could be added to standard chemotherapy without exacerbating chemotherapy-induced toxicity. In 23 patients who progressed, bevacizumab was continued; changing the chemotherapy had little effect. Recurrence pattern of an increase in the volume of infiltrative growth is described. Responses noted despite patient population heavily pretreated, poor performance status, and generally ineligible for clinical trials. Survival linked to performance status, but not to age, gender, extent of surgical resection, choice of chemotherapy combination, or number of relapses before bevacizumab. Overall tumor control rate of 94%, similar to study of Norden et al6 of 93%, is remarkable compared with the meta-analysis of Wong et al. One of 12 patients with small asymptomatic hemorrhages had a significant intracranial bleed. Low-dose of bevacizumab, 4 mg/kg used with low-dose of irinotecan, 80 mg/m2, with less toxicity and comparable efficacy. Cognitive impairment (7%) and thromboembolic complications (5%) were the most serious toxicities. Retrospective, large, multicenter study confirms promising and rapid responses to bevacizumab. Results in more than 600 patients worldwide establish a new standard for treatment of malignant gliomas. We performed a meta-analysis of 605 patients with malignant gliomas from 16 reports (see Table 104-1) and found radiographic response rates of 30% to 73% (median, 50%; mean, 53%)-striking results compared with the historical controls of 9% response to cytotoxic chemotherapy for recurrent malignant gliomas. By contrast, the recent reports confirm that bevacizumab-irinotecan represents an unprecedented advance in the treatment of recurrent anaplastic gliomas and glioblastomas (see Table 104-1). Based on metabolic imaging using [18F]fluorothymidine positronemission tomography, responders had a median survival of 10. In certain series, radiographic response rates are as high as 70% when partial and complete responses are added. When stable disease is also taken into account, tumor control rates higher than 90% are achievable. Data strong for prolongation of progression-free survival, less impressive for overall survival. Minimal effects in phase I trials as a monotherapy;108 being evaluated clinically in combination with radiotherapy. Several trials are evaluating temsirolimus in combination with temozolomide and molecular targeted agents. For more than 30 years, a practical method to block this "switch" and to revert to the avascular phenotype has been a major avenue of brain tumor research, and it is currently a major focus of brain tumor therapy. In addition, some neuro-oncologists in the United States, are routinely prescribing bevacizumab as monotherapy for recurrent glioblastoma. His creative genius shaped the field of angiogenesis and angiotherapy, with profound implications for molecular oncology, cardiology, ophthalmology, and neurosurgery. Antiangiogenic therapy is truly a novel therapeutic platform on which to build innovative therapies and enhance existing ones. This approach, developed by scientists and applied by clinicians, has benefited thousands of cancer patients already receiving antiangiogenic therapy. Glioblastoma is among the most recent to receive worldwide attention as an "angiogenic disease" that can respond to "angiotherapy. In the upper panel, the patient was treated for a large, recurrent, left frontal glioblastoma (A). Six weeks after treatment (B), the tumor is much reduced, with significant resolution of the perilesional vasogenic edema and mass effect in the white matter of the left hemisphere. In the lower panel, a patient with a recurrent, left parietal anaplastic astrocytoma (C) has a tumor extending into the splenium of the corpus callosum. After 12 weeks of combined antiangiogenesis therapy (bevacizumab) and chemotherapy (irinotecan) (D), there is a significant reduction in tumor volume, contrast enhancement, and vasogenic edema. A retrospective analysis of patients with recurrent high-grade gliomas treated with bevacizumab with or without irinotecan: the Moffitt Cancer Center experience. The transformed cancer cell undergoes oncogene activation, dependence, or "addiction. Targeting tumor angiogenesis: antiangiogenic therapy for advanced malignant glioma. Analysis of the endothelium derived from gliomas, however, indicates that these cells are genetically distinct from the normal quiescent endothelium, with mutations found that resemble those characteristic of gliomas. This model provides the basis for restoring a physiologic balance of angiogenic stimulators and inhibitors. The optimal normalization window varies with each specific drug, dose intensity, duration of treatment, and duration of response. A, the vascular system normally shows a physiologic branching with arteries and arterioles (light red) each being drained by a matching system of venules and veins (light blue), adequately perfusing the zone of tissue, through a well-formed capillary bed (red and blue, center); there is a balance of endogenous proangiogenic factors (green circles) and endogenous antiangiogenic molecules (gray circles). B, Disruption of the microvasculature is induced by a tumor producing angiogenic factors. Note that the vessels are dysfunctional with significant shunting of blood to the venous system, leading to hypoxia in the tissue core. There is a balance again of inhibitors and proangiogenic factors during this period, called the normalization window. On top, there could be an excess angiosuppression resulting in reduced blood flow and impaired access of chemotherapeutic molecules, hypoxia, and radioresistance. The angiosuppressed tumor receives nutrients from preexisting vessels (co-option) or by diffusion from cerebrospinal fluid channels (compare with.
Diseases
- Hemeralopia, familial
- Thanatophoric dysplasia Glasgow variant
- Pelvic inflammatory disease
- Thalamic degeneration symmetrical infantile
- Portuguese type amyloidosis
- Bloom syndrome
- Hailey Hailey disease
- Calloso genital dysplasia
Buy nebivolol us
The jugular vein is compressed by the anesthesiologist, and any venous bleeding is identified and treated arrhythmia prognosis order generic nebivolol line. The dura is closed in watertight fashion, and the mastoid air cells are plugged with pieces of fat and fibrin glue. The neck muscles are sutured back while respecting the anatomic layers, and drains are not used. For meningiomas, it makes a difference whether the tumor originates anterior or posterior to the internal auditory canal. Anterior meningiomas must be removed between the cranial nerves, mostly between the fifth and the seventh-eighth complex. Posterior meningiomas are debulked and reduced in size until the cranial nerves are identified. The technique of dissection of the arachnoid sheath is used for nerve and vessel preparation and preservation. After a retrosigmoid craniotomy and opening of the dura, the suprameatal approach includes drilling away the petrous bone located above and anterior to the internal V. B, After dural opening, the cerebellum is retracted backward, along with the sigmoid sinus, and the temporal lobe is elevated. B, Threedimensional computed tomographic reconstruction showing bone removal at the petrous apex (arrow) for tumor resection through the retrosigmoid suprameatal approach. In our experience, transcondylar approaches with extensive condyle removal are never necessary. Epidermoid tumors may fill the entire cerebellopontine angle and even extend to the contralateral side, caudally to the foramen magnum and cranially to the middle fossa. The cerebellopontine angle is divided into four floors according to the cranial nerves: the first floor between the tentorium and the fifth nerve, the second floor between the fifth nerve and the seventh-eighth nerve complex, the third floor between the seventh-eighth nerve complex and the caudal cranial nerves, and the fourth floor below the caudal cranial nerves. The tumor is removed between these floors, mostly between the second and third floors. In 40 epidermoids in the area of the cerebellopontine angle, 75% of the tumors were removed completely, but in 25% of cases, very adherent tumor capsules could not be resected. Attempts to remove the capsule in these cases may produce severe, permanent neurological deficits. Neurinomas of the caudal cranial nerves in the region of the cerebellopontine angle extending up to the jugular foramen can also be resected with the retrosigmoid approach. A retromastoid craniectomy is then carried out to expose the transverse and sigmoid sinuses. The sigmoid sinus is mobilized from its bony groove caudally down to the jugular foramen. To extend the exposure, the posterior part of the occipital condyle may be removed, thus opening the jugular foramen dorsolaterally. Through this approach the sigmoid sinus, the jugular bulb, and the internal jugular vein are exposed. Rerouting the facial nerve is necessary only if the tumor extends to the middle ear cavity or to the carotid canal, as in cases of extensive glomus jugulare tumors. When rerouting the facial nerve, care is taken to keep the vascularized fascia and soft tissue attached to the nerve at the stylomastoid foramen to avoid a severe postoperative facial deficit. The dura may be opened Combined Intradural-Extradural Approach to the Jugular Foramen the patient is placed supine with the head turned 60 degrees to the contralateral side and slightly retroflected. The surgery involves three main steps: (1) exposure of the cervical region with vessels and nerves, (2) craniectomy and mastoidectomy, and (3) intradural exposure. After a retroauricular skin incision, a dissection plane is found between the parotid gland and the anterior border of the sternocleidomastoid muscle. The mastoid is exposed after mobilization of both the sternocleidomastoid muscle and the posterior belly of the digastric muscle. The facial nerve is identified anterior to the mastoid process at the stylomastoid foramen. The facial nerve is followed from the fallopian canal to its extracranial segments. A retroauricular incision is extended along the anterior border of the sternocleidomastoid muscle. B, After neck dissection, the posterior border of the parotid gland is separated free and retracted. After the tumor has been resected, the dura is sealed as much as possible, and a piece of muscle with fibrin glue is used for additional closure. To avoid leakage of cerebrospinal fluid, a lumbar drain is placed, and prophylactic antibiotics are given for about 1 week. Endonasal Approaches to the Skull Base Endonasal approaches to the skull base have been developed as an extension of microsurgical transsphenoidal approaches. However, a major limitation is that they permit a restricted midline exposure through a narrow surgical field. The addition of an endoscope overcomes these limitations by providing a panoramic view and the opportunity to look around the corner. The expanded endoscopic endonasal technique provides access to the entire ventral skull base, from the crista galli up to the C1 vertebra. Furthermore, early and direct exposure of the dural attachment of the tumor with early interruption of its arterial supply is possible. Therefore, when selecting the approach, a major issue is still the relationship of the lesion to the dura. For extradural lesions of the anterior skull base, the technique is safe and reliable. A growing number of papers are posterior to the sigmoid sinus and the incision extended to the jugular foramen, or it may be opened anterior to the sigmoid sinus. The cerebellopontine cistern is opened first; the cerebellum is then gently retracted medially. The extracranial portion of the tumor is usually resected first with microsurgical technique. The caudal cranial nerves are identified, and complete piecemeal tumor resection is performed. The intracranial portion of tumor is then removed through the widened jugular foramen and the suboccipital craniectomy. Schwannomas of the jugular foramen usually displace the nerves ventrally and the jugular bulb dorsally. Chemodectomas arise from the dome of the jugular bulb and extend intraluminally to the sigmoid sinus and internal jugular vein. Thus, in cases of chemodectoma, the sigmoid sinus is ligated and packed along with the internal jugular vein. A, Screenshot from the neuronavigation monitor presenting the tumor in three planes and its threedimensional reconstruction. Complete tumor removal was achieved via the endonasal approach by using a combined microscopic and endoscopic technique. This rare tumor type, although benign histologically, has a tendency for local recurrence. Therefore, both the tumor and surrounding involved bone structures have been removed. This can hardly be justified, given the need to expose the entire intact skull base and to reconstruct it at the end of the procedure. Reported rates of cerebrospinal fluid leakage remain high despite some recent advances. These, along with the relatively restricted working space and the twodimensional endoscopic view, make dissection more dangerous. Alternatively, even the largest meningiomas could be removed completely with minimal risk via the simple frontolateral approach. With lesions involving the clivus or sphenoid sinus, even if they extend intradurally, the endonasal approach provides superior exposure and the osteodural defect can be reliably reconstructed. Retrosigmoid intradural suprameatal approach: advantages and disadvantages from an anatomical perspective. Surgical management of petroclival meningiomas: factors determining the choice of approach. Anterior transpetrosal-transtentorial approach for sphenopetroclival meningiomas: surgical method and results in 10 patients.
Purchase nebivolol no prescription
Furthermore, after radiation treatment or infectious processes, it is difficult to distinguish the target of interest heart attack cover by sam tsui and chrissy costanza of atc purchase 2.5mg nebivolol visa. Simply by using a Brookwalter arm, the biopsy cannula was fixed in place as the needle was passed through into the brain under direct real-time image guidance. By maintaining visualization of the needle throughout the procedure, entry into the target lesion and avoidance of critical structures could be confirmed. However, after imaging was performed, the patient was moved away from the magnetic isocenter, beyond the 5G line. In this magnetic "fringe field," conventional surgical equipment, including drills and electrocautery, could be used. Needle-stabilizing devices were soon developed because freehand biopsies have often been criticized for being inaccurate and potentially increasing the risk for acute intracerebral hemorrhage. Stereotactic biopsy has often been used to distinguish recurrent neoplasm from postirradiation necrosis, given the similarity of these two findings on imaging scans. This is especially true for intracranial hemorrhage, which has been reported to occur in 0% to 11. Transsphenoidal Resection of Pituitary Adenomas Although the first transsphenoidal approach for pituitary adenoma removal was performed more than a century ago,44 it was relatively recently, with the development of adjuvant technologies, that it became the method of choice in the resection of pituitary tumors. Although fluoroscopy allows for rapid real-time imaging, its visualization is limited to the bony structures of the sella, and it is unable to aid in tumor detection. Finally, despite the drastic improvement that endoscopy has provided relative to the surgical microscope alone, it requires direct visualization to confirm the presence or absence of tumor and does not allow one to see beyond the surface anatomy. Given these limitations, it is not surprising that complete removal of pituitary adenomas remains a problem, with studies suggesting that this is achieved in only about 65% of macroadenoma cases. Serial updates allow the neurosurgeon to localize remnant tumor while accounting for brain shift throughout the surgery and to direct resection while preserving critical native structures. Furthermore, dynamic image sequences help distinguish normal pituitary tissue (fast contrast enhancement) from adenoma (slow contrast enhancement) and hemorrhage (heme-sensitive gradient echo). This allows the surgeon to determine on the day of surgery whether further management is required, rather than waiting the standard 2 to 3 months for artifact-free postoperative scans to decide among surveillance, radiation therapy, or secondary transcranial surgery. Consequently, it may be too early to conclude whether the reported imaging outcomes translate into truly beneficial clinical outcomes that can be compared with national statistics derived from studies with more than 10 years of follow-up. Intractable Epilepsy Although surgery has been a treatment option for pharmacoresistant epilepsy for more than 50 years, it was only recently that a randomized controlled trial53 investigated the efficacy of surgery compared with medical management. This outcome, in conjunction with other reports of increased seizure-free intervals after surgery, has continued to support this invasive treatment option over the years. Surgical techniques available for intractable epilepsy include focal cortical resection, anatomic lobectomy, lesionectomy, corticectomy, and hemispherectomy and its variants. For example, patients with epilepsy secondary to a specific seizure focus, including neoplasms and vascular malformations, undergo focal cortical resection to remove the epileptogenic lesion; alternatively, mesiotemporal lobe epilepsy patients with hippocampal sclerosis benefit from amygdalohippocampectomy or en bloc temporal lobe resection. Overall, they report the utility of intraoperative imaging at helping navigate through cortex while accommodating for brain shift as well as aiding in the detection and resection of residual epileptogenic structures or lesions. Schwartz and associates55 published similar results in a small study in which 100% of their patients were seizure free at 10 months. Because neuronavigation is based on preoperative images, brain shift during neurosurgery induces error and uncertainty in the neuronavigation system. Factors such as feasibility, safety, patient selection, and cost will play important roles in the future adaptation of this technologic advancement. Craniotomy for tumor treatment in an intraoperative magnetic resonance imaging unit. Glioma resection in a shared-resource magnetic resonance operating room after optimal image-guided frameless stereotactic resection. Intraoperative visualization of the pyramidal tract by diffusion-tensor-imaging-based fiber tracking. Magnetic resonance imaging-guided neurosurgery in the magnetic fringe fields: the next step in neuronavigation. Intraoperative diagnostic and interventional magnetic resonance imaging in neurosurgery. However, continued use of antiepileptic drugs can be necessary, and in some patients, an additional operation may be required for persistent seizure activity. In our experience, optimal control of intractable epilepsy without the use of postoperative anticonvulsants is possible when perioperative. In most cases of epilepsy, as in patients with occasional breakthrough seizures, such mapping is not needed, but complete tumor resection is. When mapping is not used and radical tumor resection (including adjacent brain) is carried out, seizures occur less frequently, but most patients continue to take antiepileptic drugs. These tumors demonstrate a slight male predominance and a biphasic age distribution, with the first peak occurring during childhood (age 6 to 12 years) and a second peak in adulthood (between the third and fifth decades). They do, however, display a tendency to reside within and extend along white matter tracts. Fifty percent to 80% of patients present with seizures as their initial symptom, with most remaining otherwise neurologically intact. These include signs and symptoms of raised intracranial pressure (headache, nausea, vomiting, lethargy, papilledema), focal neurological deficits (weakness, sensory disturbance or neglect, visual neglect, agnosia, aphasia), and impaired executive function (altered personality, disinhibition, apathy). The true extent is shown on the T2-weighted sequences, although on these sequences, tumor extent and surrounding edema are indistinguishable. Preoperatively, these techniques are also used to identify motor- or language-related regions of cortical function, but with limited specificity. Cortical stimulation, which remains the "gold standard" for monitoring brain function, is based on local circuit disruption or activation and best identifies areas that are essential to language processing. This results in a corresponding local reduction in deoxyhemoglobin because the increase in blood flow occurs in the absence of a comparable increase in oxygen extraction. This volumetric extent of resection analysis revealed that patients with greater than or equal to 90% resection had an 8-year overall survival rate of 91% and a progression-free survival rate of 43%, whereas patients with less than 90% resection had an 8-year overall survival rate of 60% and a progression-free survival rate of 21%. Nevertheless, it is likely that the timing of malignant transformation affects patient outcome, and this phenomenon may be detected by future studies that are more robust. Furthermore, extent of resection studies suggest that the natural history of malignant transformation can be altered by greater extent of resection. The only genetic alteration consistently observed in patients with low-grade astrocytomas is mutation of the p53 gene. Because this gene is essential in the regulation of apoptosis and cell cycle progression, loss of normal p53 function promotes the accelerated growth and malignant differentiation of astrocytes. Fifty percent to 60% of grade 2 and grade 3 astrocytomas exhibit p53 mutations, suggesting that inactivation of this tumor suppressor gene is an early lesion among gene alterations associated with the development of malignant gliomas. Other common alterations observed in adult low-grade astrocytomas are gain of chromosome 7 and structural abnormalities, including possessing double-minute chromosomes. Losses of chromosomes 10, 13, 15, 20, and 22 and structural rearrangements involving chromosomes 4, 11, 12, 13, 16, 18, and 21 have also been reported in patients. Because loss of 1p and 19q is not seen in astrocytic tumors (with rare exception), analysis of the presence or absence of p53, 1p, and 19q can be used to distinguish an astrocytic from an oligodendroglial genotype in cases that are difficult to distinguish histologically. Similarly, most mixed oligoastrocytomas appear to segregate genetically into astrocytic or oligodendroglial genotypes, suggesting that such mixed tumors may not be a distinct biologic entity. Additionally, reliable prognostic factors allow for the rational stratification of patients enrolled in clinical trials. In the literature, 13% to 86% of tumors initially diagnosed as low grade were observed to recur at a higher histologic grade. Nevertheless, some practitioners still advocate this extremely conservative approach for patients thought to have deep-seated lesions or lesions located in eloquent cortex for which surgery would have higher risk. Although this strategy defers treatment-related risk and treatment-related costs for patients who remain asymptomatic, it may increase the risk for tumor progression, with subsequent development of new neurological deficits or intractable seizures, as well as the risk for malignant dedifferentiation of the lesion. Furthermore, tumor growth rates can be unpredictable and are often nonlinear, leading to sudden changes in tumor size that can drastically change the surgical landscape, turning an initially resectable or radioresponsive lesion into one that is difficult to remove safely or is more resistant to adjuvant therapies. An additional drawback to this approach is the psychological stress associated with not knowing with certainty what one is dealing with, possibly resulting in increased distress and reduced quality of life for both the patient and the caregiver. Little evidence exists to support this treatment strategy, although it has not been refuted, either. In one small, retrospective case-controlled study, no difference was observed in rates of malignant transformation, overall survival, or quality of life between patients initially only observed and those undergoing immediate resection. This strategy, however, is complicated because higher grade lesions may not always show contrast enhancement in imaging studies.
Buy genuine nebivolol line
If surgery is not possible or if hydrocephalus persists following tumor resection, shunting can relieve both ventricular obstruction and intracranial hypertension prehypertension and lupus buy nebivolol 5 mg otc. It is appropriate to continue surveillance of these patients because recurrence is possible. An attempt to use chemotherapy in the treatment of these tumors has shown some modest early success. The classic finding is an intraventricular tumor in a patient with known tuberous sclerosis. These lesions are generally isointense on T1-weighted images and hyperintense on T2-weighted images. Pathology Microscopically, tumors demonstrate monomorphous, bipolar cells associated with the normal vessels of the cortex and white matter. Patients usually present with symptoms and signs related to cortical dysfunction or from related mass effect, such as hemiparesis, seizures, or personality changes. Great variability in the natural history of astroblastomas has been reported through case reports; these tumors can have a slow evolution with a relatively favorable outcome, or they can exhibit a rapidly progressive nature leading to fatality. The relative malignancy of the remaining cases may have been related to anaplastic features. Bonnin and Rubinstein10 attempted to establish clinicopathologic correlations, reinforcing the idea that astroblastomas with malignant features indicative of anaplasia are susceptible to progression to glioblastoma. In their series, those cases that displayed benign histologic features had a benign clinical course, with no postsurgical recurrences after 12 and 20 years. The specimens that displayed malignant features appeared to correlate with a rapidly fatal clinical course, with one death 10 months and the other 16 months after surgery, with pathologic evidence of tumor progression to glioblastoma and gliosarcoma. One case series has attempted to describe the imaging characteristics of these lesions. The nuclei of the tumor cells are found some distance away from the vessel, but long processes extend from the tumor cell to the vessels and end as an expanded footplate. The biologic significance of necrosis is uncertain, and it may not necessarily signify an ominous prognosis. Astroblastomas are well circumscribed and usually located in surgically accessible regions. Owing to the rarity of these tumors, the therapeutic value of radiation and chemotherapy remains uncertain. Bonnin and Rubinstein10 reported one patient who had good tumor control with a biopsy and subsequent radiotherapy. Chemotherapy was also administered in five patients in the same series, without a clear change in prognosis. Outcome is difficult to predict because these tumors can remain indolent in some patients and undergo malignant degeneration to glioblastoma in others, resulting in rapid death. These tumors occur throughout the neuraxis, with a mean age at diagnosis of 18 months. Patients present with symptoms associated with elevated intracranial pressure or mass effect of eloquent parenchyma. Generally, as for any low-grade, noninfiltrating glioma of childhood, authors advocate surgical resection if location is favorable. Most patients (70% to 80%) present with seizures followed by headache and focal location-related deficits, or evidence of increased intracranial pressure. In many cases, the tumors have been associated with chronic epilepsy, indicating an indolent course. Furthermore, their early-adult onset and histologic appearance may indicate that they are developmental in nature. These features notwithstanding, a subgroup of patients with this histologic diagnosis may experience rapid demise despite surgery and, in some cases, adjuvant radiation and chemotherapy. The tumor is usually of high to mixed intensity on T2-weighted imaging, and the cyst is typically hyperintense. Mild to moderate amounts of peritumoral edema may be seen, and calcifications are rare. Peritumoral edema may be a poor prognostic sign with this tumor, although this is not universally accepted. They typically invade the pia-arachnoid space, and up to 13% of patients have involvement of all three layers of the meninges. Close to the meninges, more prominent mesenchymal features are found, whereas more glial features are found toward the interior. These tumors rarely invade the underlying brain; normal cortex is rarely seen within tumor specimens. More specifically, these tumors are moderately cellular and pleomorphic in nature. In fact, pleomorphism can be as vast, as seen in more malignant tumors such as glioblastoma or sarcomatous tumors. Characteristically, spindle cells with elongated nuclei, akin to those seen in fibrous histiocytomas or meningiomas, are seen in streaming or storiform patterns. In other areas, round or polygonal cells are found with "groundglass" eosinophilic cytoplasm containing pleomorphic and occasionally multiple nuclei. Mitotic figures are usually rare, although a recent study linked the number of mitoses to outcome. These areas are rich in reticulin fibers that surround individual cells or small groups of cells. In many cases, areas of lymphocytic infiltrates may be seen, unrelated to necrosis. In fact, the presence of necrosis or endothelial proliferation is unusual in these tumors. Staining for synaptophysin or neuron-specific enolase may also be present in some cells. Other authors have reported these tumors in association with separate areas of ganglioglioma or cortical dysplasia. The age group and the presence of xanthomatous cells usually, although not always, distinguish these tumors from infantile desmoplastic astrocytomas and gangliogliomas. Others have demonstrated loss of chromosome 9 and gain of chromosome 7 in tumor samples. They can occur anywhere in the central nervous system but are most commonly found in the temporal lobe (up to 85%), often affecting young patients with seizure disorders (they are the most common tumor found in temporal lobe epilepsy). The most common presenting signs and symptoms are seizures (temporal lobe and other supratentorial locations), followed by headache, dizziness, ataxia (posterior fossa), and progressive weakness (spinal cord). Malignant or anaplastic gangliogliomas are even rarer and can occur as a result of malignant transformation of a preexisting lesion or de novo. Management and Outcome Because these tumors are quite rare, large series of patients are limited. Investigators found that 33% of patients who died had necrosis at presentation or recurrence, compared with only 2% of living patients. They also found statistical significance for survival based on the extent of surgical resection. For all patients, there was no difference between gross total resection and subtotal resection (91% versus 65%, P >. Analysis of patients who underwent postoperative radiotherapy revealed a trend toward improved survival with treatment, but this did not reach statistical significance. An additional retrospective series of 71 patients with a mean follow-up of 5 years revealed a similar result of overall survival rates of 81% at 5 years and 70% at 10 years, whereas recurrencefree survival rates were 71% at 5 years and 61% at 10 years. It is generally accepted that total resection in all patients should be attempted if it is possible without unacceptable deficits resulting. In some cases, a more malignant tumor may be suspected preoperatively, and frozen-section diagnosis at the time of resection may be equivocal. In these cases, when a subtotal resection is performed owing to the assumption of greater malignancy, an attempt at complete resection may be justified at the time of definitive histologic diagnosis. The data regarding adjuvant therapy for these tumors are not helpful at this time and are limited to single case reports. Patients without these negative predictors should also undergo surveillance, but perhaps at less frequent intervals. At the time of progression, in patients with favorable anatomy, repeat resection may be attempted.
Cheap 2.5mg nebivolol with visa
Complete excision decreases the risk for both postoperative chemical meningitis and tumor recurrence arrhythmia effects order 2.5mg nebivolol with mastercard. The surgeon must be cognizant of adherence of the tumor capsule to vascular and neural structures, damage to which can be devastating. As might be predicted, surgical treatment of recurrent cysts remains controversial. There is no current role for radiotherapy or chemotherapy in the treatment of these tumors. They are also clinically and biologically benign, with the main problem at initial evaluation being related to mass effect on neural structures in a tight space (intracranial or spinal). They represent a developmental malformation, with the defect in gastrulation affecting the surface ectoderm and causing a secondary disruption of neural tube closure. They tend to occur at the midline and, when extradural, may arise at the anterior fontanelle. The epithelial cell lining may be less differentiated in dermoids than in epidermoids. In one patient who had incomplete resection of a dermoid tumor, antigen levels remained high postoperatively. Gormley and coworkers noted an average age at diagnosis of 15 years for dermoid cysts versus 35 years for epidermoids. As with epidermoid cysts, there is a female preponderance, and patients may initially be seen with local neural deficits, headache, or meningitis. They have been considered part of the split notochord syndrome or split cord malformation. The neurenteric canal, a normally transient communication between the endoderm and ectoderm through the notochord, is also seen at this stage. By the third embryonic week, this neurenteric canal closes, and the notochord separates from the primitive gut. Spinal neurenteric cysts are almost pathognomonically associated with vertebral anomalies such as cleft vertebrae, hemivertebrae, spina bifida, absent or fused vertebrae, or diastematomyelia. Cyst recurrence has been reported 4 to 14 years after surgery in cases in which macroscopically complete removal was achieved. Conventional radiotherapy for residual tumor is not likely to be effective given the benign and cystic nature of the tissue. Whether there may be some role for radiosurgery in the treatment of residual neurenteric cysts remains to be seen. The cyst wall is composed of well-differentiated cuboidal, columnar, or ciliated epithelium, with or without goblet cells or microvilli. The presence of an underlying basement membrane or collagenous tissue separating the epithelial layer from neuroglial tissue is characteristic of neurenteric cysts. Wang and associates reported a patient with a neurenteric cyst that had focal malignant features. In general, the course of the disease in adults is slow and insidious; progression is more rapid in children. When a fistula persists, patients may initially be seen with recurrent meningitis. There have been reports of T1 signal changes in these tumors, probably resulting from changes in protein concentration or hemorrhage. Intracranial neurenteric cysts have been located primarily in the posterior fossa, midline fourth ventricular area, or cerebellopontine angle, although there have also been reports of parasellar cysts. Their onset is usually insidious, although any of these cysts can be accompanied by acute meningitic complaints or increased intracranial pressure as a result of cyst rupture and spillage of the irritative contents into the subarachnoid space. Epidermoid and dermoid tumors were described in a classic paper more than 70 years ago,11 and more recent series of patients have confirmed the clinical and histopathologic features. Surgical extirpation is the treatment of choice, with the goal being complete resection. However, because both these entities can grow between and around neural and vascular structures, the risk for operative damage can be high and preclude complete resection. The goal is complete resection, although this is not always feasible given the difficulty of completely removing the cyst wall at locations where it adheres to adjacent structures. Descriptions of the cyst fluid have varied, including clear and colorless, milky, yellowish, gelatinous, xanthochromic, and blackish and viscous. Unlike dermoids and epidermoids, which show a female preponderance, there is no definite sex predilection for neurenteric cysts. As with dermoids and epidermoids, spillage of the cyst contents may result in aseptic meningitis. When this occurs, as with dermoids and epidermoids, reoperation is considered because radiotherapy and chemotherapy have little to offer in treating any of these three entities. Spinal dermoid cysts originating intracranial fat drops causing obstructive hydrocephalus: case reports. Surgery of cerebellopontine angle epidermoid cysts: role of the widened retrolabyrinthine approach combined with endoscopy. Malignant transformation of intra-cranial epithelial cysts: systematic article review. Neurenteric cysts of the posterior fossa: recognition, management, and embryogenesis. Well-differentiated papillary adenocarcinoma arising in a supratentorial enterogenous cyst: case report. Love J, Kernohan J: Dermoid and epidermoid tumors (cholesteatomas) of central nervous system. Sano K: Intracranial dysembryogenetic tumors: pathogenesis and their order of malignancy. Typically, the condition arises in patients with breast, lung, and gastrointestinal tumors and melanoma and in those with poor-risk hematologic malignancies. The diagnosis is usually suspected in a cancer patient in whom multifocal, unexplained neurological symptoms develop. Longer survival rates are occasionally observed in patients with breast cancer (13% at 1 year and 6% at 2 years). Late in the disease, invasion of the brain and spinal cord parenchyma by tumor from the meninges produces edema, microinfarction, and striking neurological dysfunction. Symptoms may also result from secondary complications such as hydrocephalus and increased intracranial pressure. Most commonly, patients have altered mental status, headache, diplopia, seizures, back pain, lower extremity weakness or numbness, or other cranial neuropathies. The classic meningeal sign of nuchal rigidity has been reported in less than 20% of patients. However, most patients rapidly progress at an alarming rate and experience neurological and systemic decline despite treatment efforts. Cisternal fluid has also been proposed to be a more reliable indicator, but its acquisition may carry greater risk. Indirect signs include communicating hydrocephalus, bilateral transependymal edema, and effacement of convexity sulci. Contrast enhancement of the meninges can be associated with many non-neoplastic conditions, including prior or current infections, previous subarachnoid hemorrhage, previous lumbar puncture or intrathecal chemotherapy, prior neurosurgical procedures. Patchy nerve root enhancement, matting of nerve roots of the cauda equina, nodular deposits, and linear, continuous enhancement of the pia-arachnoid of the conus medullaris, brainstem, and cerebrum are hallmarks of the diagnosis. Patchy, asymmetric enhancement of the leptomeninges over the cerebral convexities and in the sulci, Meningeal Biopsy Occasional patients are appropriate candidates for meningeal biopsy, but most are not because of poor performance status and comorbid conditions. It should be stated that these factors have not yet been validated by multivariate analysis in controlled prospective studies. To date, no specific factors have predicted a survival benefit for these patients after therapy. Bacteria isolated from infected systems are usually Staphylococcus epidermidis or Propionibacterium, although more pathogenic organisms, including Staphylococcus aureus, Streptococcus pyogenes, and gramnegative species, can be found. In an effort to theoretically limit drug egress, some physicians have installed in-line on-off valves and, recently, programmable valves that can be set to temporarily impede shunt function. However, these manipulations carry significant risk and should be performed only by those with considerable experience in these specific techniques. Many systemically administered agents exhibit incomplete penetration of the blood-brain barrier.
Goji juice (Lycium). Nebivolol.
- Dosing considerations for Lycium.
- Are there safety concerns?
- How does Lycium work?
- Are there any interactions with medications?
- Diabetes, high blood pressure, fever, malaria, cancer, blood circulation problems, sexual problems (impotence), dizziness, ringing in the ears (tinnitus), and many other conditions.
- What is Lycium?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96984
Buy discount nebivolol 2.5mg
Anesthesia for Pregnant Women Requiring Craniotomy the multiple drugs required during craniotomy can increase the risk for developmental abnormalities if administered during the first trimester heart attack in 30s nebivolol 2.5 mg for sale. Surgery during pregnancy often increases the risk for a first- or second-trimester spontaneous abortion, but it does not seem to increase the incidence of congenital abnormalities,21 nor does surgery appear to induce premature labor. Pregnancy increases plasma volume and total blood volume with a dilutional anemia. Cardiac output is increased by 50%, and typically, anesthetic requirements are decreased by 30%. Gastric motility is decreased, and the patient is at an increased risk for vomiting and aspiration on induction of anesthesia. A reduction in Paco2 from 32 mm Hg, the normal level for pregnancy, to 25 mm Hg decreases uterine artery blood flow by 25%, but the effect may be caused by mechanical ventilation rather than simple changes in Paco2. In this case, a folded sheet can be placed under the right hip of the patient to minimize vena cava compression. However, the well-being and safety of the mother should not be jeopardized because of concerns over radiation. Obtaining a timely diagnosis that can appropriately guide the medical management of the rest of the pregnancy clearly outweighs the small risks associated with the procedures. Therefore, even with a posterior fossa approach, the park bench position should be preferred over the prone position. Several case reports of hypotension, produced by either isoflurane or nitroprusside, indicate that a mean arterial blood pressure of 40 to 50 mm Hg for up to 40 minutes does not result in injury to the fetus. Their peak incidence is in young women of childbearing age, but improvements in surgical and medical management have made it possible for an increasing number of women with such lesions to choose to become pregnant. Several factors may affect the course of pregnancy in the presence of pituitary adenomas. Because the pituitary controls the gonadotropin axis, hormonal changes related to these tumors often result in infertility in women. If infertility does not result or if bromocriptine treatment allows normal ovulatory function, pregnancy and pituitary tumors can coexist. In these cases, however, perturbed pituitary function can lead to early termination of pregnancy because of failure to maintain intrauterine implantation. Since the late 18th century, it has been noted that the pituitary gland enlarges during pregnancy as a physiologic consequence of gestation. Indeed, it has been reported that pituitary adenomas may grow more rapidly in pregnant women. In the past, delivery was postponed until after 36 to 38 weeks of pregnancy to decrease the likelihood of respiratory distress syndrome. Improvements in the use of surfactant have demonstrated that safe delivery at 32 weeks of pregnancy may be a reasonable option. If delivery and craniotomy are to be accomplished concurrently, the anesthetic management plan should be that required for a craniotomy. Rapid initiation of general anesthesia with intravenous agents, endotracheal intubation, and mild hyperventilation do not seem to have an adverse effect on the fetus. If delivery is to be accomplished before neurosurgical treatment, the presence of an intracranial lesion causing a mass effect requires a different strategy. Patients with such lesions who are ready to deliver are best anesthetized with general endotracheal anesthesia. The effect of active labor on the central nervous system of such patients is little understood, but it is unlikely to produce a positive effect. A cesarean section under general anesthesia is preferable because it is quick and safe and has minimal disadvantages to the fetus. Respiratory depression in the newborn, which is a potential problem associated with such delivery, is easily treated. Regional anesthesia should be avoided in patients with a demonstrated significant intracranial mass effect and possible shift because of the risk of loss of cerebrospinal fluid and the consequent potential risk of herniation through the foramen magnum. Regional anesthesia, specifically epidural anesthesia, is sufficient for lesions that do not exert a mass effect. B, Contrast-enhanced sagittal magnetic resonance image of the same patient in her eighth month of pregnancy (10 months after the initial study). One study showed that among 69 women who died during pregnancy, after abortion, or during the postpartum period, 12% had noninvasive microadenomas, an incidence rate similar to that found in studies conducted on a general sampling of adult autopsies. Functional adenomas secrete excessive amounts of pituitary hormones and can frequently be diagnosed when they are small-less than 5 mm in diameter. Nonfunctional adenomas are larger at the time of diagnosis and can be discerned by their direct compression of surrounding structures. Compression of surrounding structures by pituitary tumors may lead to three major consequences: pituitary insufficiency, caused by compression of the pituitary gland; compromise of the hypothalamic-hypophysial axis, caused by compression of the pituitary stalk; or visual problems such as bitemporal hemianopia, caused by compression of the optic pathways. In addition, such tumors may cause oculomotor problems and sometimes stroke by compressing the cavernous sinuses and the neurovascular structures contained in them. Headaches are commonly associated with these tumors as well because the surrounding dura mater is stretched. Patients harboring microadenomas have been shown to have a significantly smaller risk for the development of visual loss than do patients affected by adenomas greater than 1. It involves a sudden hemorrhage or ischemic or hemorrhagic infarction of the pituitary adenoma, which causes a rapid increase in intrasellar pressure. Common symptoms are sudden or violent headaches frequently accompanied by vomiting and rapid deterioration of vision or ocular motility. Emergency treatment with a decompressive surgical procedure is needed to avoid progression of the syndrome and potential death. Periodic assessment of visual performance also allows monitoring of disease evolution. Treatment Bromocriptine is highly effective in the treatment of hyperprolactinemic patients. Bromocriptine can significantly slow or even arrest the growth of a prolactin-secreting tumor and often results in restoration of normal endocrine function and a concurrent reduction in the size of the adenoma. Hyperprolactinemia also occurs in 30% to 40% of acromegalic patients,56 and bromocriptine has been shown to be effective in restoring normal ovulatory cycles in these patients as well. There are multiple reported cases of pregnancy after successful treatment of acromegaly with the somatostatin analogue octreotide. Imaging studies for evaluation of patients with pituitary tumors have improved significantly. This information is of particular importance in the preoperative evaluation of the sphenoidal bones when transsphenoidal resection is being planned. Preliminary hormonal evaluations to determine the functioning of the anterior and posterior pituitary involve the following measurements: urine volume; serum electrolytes and osmolarity; serum prolactin; early-morning cortisol level; serum gonadotropins; and thyroxine, triiodothyronine, and thyroid-stimulating hormone levels. Patients who have tumors that do not react to medical treatment, who demonstrate disease progression clinically or on imaging studies, or in whom pituitary apoplexy develops require surgical treatment. Transsphenoidal resection of the lesion is generally the safest method for intrasellar tumors. Surgical intervention can be postponed until after delivery when the pregnant woman is clinically stable and there are no changes on imaging studies and no visual deterioration. In specific cases, radiation therapy is used as an adjunctive measure after surgery to prevent recurrences; thus, it can be postponed until after delivery. The safety of continuous bromocriptine or octreotide therapy has not been fully assessed, and women should be advised to discontinue such treatment after pregnancy is confirmed. However, there is a greater than 15% risk of symptomatic enlargement of a macroprolactinoma during pregnancy, thus mandating close surveillance. Periodic assessment of visual fields every 3 months in women with microadenomas and every 6 weeks in those with macroadenomas has been recommended. Nonetheless, only a small percentage of pregnant women with pituitary adenomas require further surgical treatment before delivery. Finally, the notion that breastfeeding induces the growth of prolactin-secreting adenomas should lead to particular vigilance when managing women with larger tumors during the puerperium. Their identifying symptoms can be the result of direct destructive or irritative effects on the surrounding nervous tissue or increased intracranial pressure. Although focal neurological deficits or seizures can be clear identifying signs, symptoms resulting from elevated intracranial pressure, such as headache, drowsiness, nausea, and vomiting, are much harder to distinguish from the normal discomforts of pregnancy. In these cases, accompanying signs such as papilledema, subtle changes in mental status, cranial nerve deficits, and motor or sensory dysfunction aid in diagnosis.
Cheap nebivolol 2.5mg line
Selection of the correct treatment is more difficult in children because they are still developing and their needs may change as they grow blood pressure yoga ramdev cheap nebivolol 2.5 mg. To formulate a treatment plan one must project into the future by extrapolating the extent and severity of musculoskeletal contractures and their harmful consequences, as well as the positive effects of spontaneous psychomotor development. The second step is to measure range of motion to detect contractures that will not respond to neurosurgical treatment. The third step is to quantify the spasticity by using the Tardieu or the Ashworth scales. The final step is to grade the child on the Gross Motor Function Measure and to observe the evolution of gross motor function with time. Several effective neurosurgical treatments for spasticity can be used in children with cerebral palsy. For diffuse spasticity of the lower limbs, dorsal rhizotomy or intrathecal baclofen administration may be considered; dorsal rhizotomy is proposed when definitive action targeted to certain muscle groups is preferred. For focal spasticity, botulinum toxin injection permits delaying surgery until the child is old enough to undergo selective neurotomy. SpasticityintheLowerLimb Spasticity should be assessed every 6 or 12 months with the Gross Motor Function Measure so that future motor function can be predicted. Alsonote that the score improved significantly after dorsal rhizotomy was performed. The latter necessitates a visit every 6 months to fill the pump; accordingly, the child and family must be motivated to comply. If the spasticity is focal and involves the gastrocnemius and soleus muscles, botulinum toxin can be proposed as a complement to physiotherapy and casting. This approach enables neurosurgical treatment to be delayed until the child reaches an age appropriate for selective tibial neurotomy. When spasticity is localized to the adductors, botulinum toxin is not always sufficient to avoid obturator neurotomy, which may be necessary to prevent hip dislocation. SpasticityintheUpperLimb For upper extremity spasticity in a child, botulinum toxin injections are an effective primary treatment. The muscles of the upper limbs are small, so even if quite a few must be injected, the maximal allowable dose is rarely a limiting factor, as it may be in the legs. These injections can be considered as a definitive treatment and can be repeated every 6 or 12 months as needed. Furthermore, immunoresistance can develop and decrease the effectiveness of the treatment with time. An additional advantage of botulinum toxin injections is that they simulate the outcome of selective neurotomy, thereby allowing the patient and family to appreciate the benefit that can be achieved with ablation. The goals are to decrease "harmful spasticity," respect "useful spasticity," preserve residual motor/sensory functions, reveal masked capabilities, and improve functional ability. Peripheral selective neurotomies of the brachial plexus branches for the spastic shoulder. Long-term functional results of selective peripheral neurotomy for the treatment of spastic upper limb: prospective study in 31 patients. The rehabilitation of patients totally paralysed below waist: anterior rhizotomy for spastic paraplegia. Sectorial posterior rhizotomy, a new technique of surgical treatment for spasticity. Selective posterior rhizotomy in the dorsal root entry zone for treatment of hyperspasticity and pain in the hemiplegic upper limb. Corcos Chronic intrathecal infusion of baclofen has been extremely successful in the treatment of spasticity. This long-term commitment to treatment is similar to maintaining shunt function in hydrocephalics and may be equally rewarding or frustrating. To make proper use of this powerful tool, neurosurgeons need to understand the pharmacology and distribution of intrathecal baclofen and how pumps are used to infuse the drug. Proper selection of patients requires an understanding of the physiology of spasticity and its clinical manifestations. Other neurosurgical methods for reducing spasticity are considered elsewhere; in particular, dorsal rhizotomy for spastic cerebral palsy in children is discussed in Chapter 90. The relationship between physiologic abnormalities and motor disability is a major area of investigation and of more than academic interest. It is uncertain how or to what extent the velocity-dependent increase in stretch reflex activity interferes with movement. The primary sensory endings, which are extensions of the large, myelinated Ia afferents, attach at the noncontractile equatorial region of the intrafusal fibers. The spindle organs are attached at both ends of the muscle mass and consist of extrafusal fibers. Because the spindles are attached in this way, they undergo the same changes in length as the overall muscle and monitor changes in muscle length. If the stretch reflex operated only in conjunction with the alpha motoneuron, voluntary movements would be difficult to make because a change in alpha activity would cause contraction of the extrafusal fibers, which would shorten the muscle. As the muscle shortened, the intrafusal fibers of the muscle would slacken and would not monitor changes in length. Gamma activity prevents this problem by shortening the intrafusal fibers, which assists movement by increasing activation of alpha motoneurons through Ia feedback. When a muscle is stretched, it contracts in an attempt to regain its original length. It inhibits the motoneuron pools of antagonistic muscles through a disynaptic pathway. It facilitates, probably monosynaptically, the motoneurons of synergistic pools (not shown in. Researchers studying spasticity tend to stress definitions that emphasize abnormal reflex responses, whereas clinicians tend to stress more global definitions, primarily related to impairment of movement. To further complicate the issue, many clinical syndromes associated with spasticity are caused by injuries at multiple sites in the neuraxis, and the pathologic mechanisms producing motor dysfunction are equally varied. For the sake of clarity, a narrow physiologic definition is used in this chapter, with note made when more general meanings arise in clinical situations. According to the definition of Lance, spasticity is "a motor disorder characterized by a velocity-dependent increase in tonic stretch reflexes. In addition to hyperactive reflexes, spasticity can be associated with various symptoms that can be viewed in terms of positive and negative categories. In spasticity, an increase in deep tendon reflexes and resistance to passive stretch of the limb are positive signs. It is the negative symptoms that usually create the clinically significant problems that are disabling for the patient. Occasionally, increased muscle tone, clonus, and hyperactive reflexes can interfere with initiation and smooth completion of a movement. The text describes the sequence of events (1 through 4) that occurs in the stretch reflex arc. Excitatory synapses are represented as angle signs and inhibitory synapses as dots. A detailed discussion of these mechanisms has been presented by Pierrot-Deseilligny,11,12 Pierrot-Deseilligny and Mazieres,13 and Sehgal and McGuire. This finding of reciprocal inhibition has had a pervasive influence on our understanding of movement control. Lack of reciprocal inhibition can lead to unwanted activation of the antagonist muscle and impede movement. The Ia inhibitory interneuron receives excitatory synaptic input from numerous descending pathways, including the corticospinal tract. It has been suggested that Ia discharge is normally reduced by presynaptic inhibition and that reduced levels of presynaptic inhibition could lead to an increased stretch reflex. There is also evidence of a decrease in presynaptic inhibition in paraplegic patients but not in hemiplegic patients. Decreased Recurrent Inhibition Motor axons give off recurrent collaterals that activate Renshaw cells, which in turn inhibit alpha motoneurons,11 thereby creating a recurrent inhibitory circuit. Renshaw cells are influenced by supraspinal control, which can facilitate or inhibit them.

Buy online nebivolol
The mucosa is reflected, and the sphenoid sinus is opened with a drill or Kerrison punch arrhythmia recognition chart discount 2.5mg nebivolol with mastercard. The mucosa of the sinus is excised, and the anterior wall of the sella is removed to expose the sella dura. Anterior compression of the anterior pituitary is a common finding, and the gland may need to be divided to provide access to the tumor. The dura may then be opened over the gland and the circular sinus and anterior to the sella to provide access to the suprasellar cistern. The dural defect is closed with a graft and supported by bone or synthetic plates, with fat placed in the sphenoid and a vascularized nasal flap added for coverage of the site of surgical access from the nasopharynx. Tumor involvement in the region of the anterior cerebral complex may expose the perforating vessels to risk for injury during surgery. Direct control of intracranial neural and vascular structures is inferior when using the transsphenoidal or extended transsphenoidal approach. Suprasellar calcifications are thought to be a contraindication to the use of this approach. Although it may be more technically challenging, this approach allows wider visualization of the optic pathway and anterior circle of Willis. Proponents of the bifrontal basal interhemispheric approach cite its ability to avoid the potential blind spots encountered with unilateral approaches. This technique has also been combined with division of the anterior communicating artery in an effort to maximize removal of the retrochiasmatic portion of these tumors. Removal of the supraorbital bar may also be incorporated with the craniotomy in a single or separate step to maximize bony exposure. Once the olfactory tracts are dissected from the brain surface, the chiasmatic and interhemispheric cisterns are opened so that the optic chiasm, bilateral A2 segments of the anterior cerebral artery, and anterior communicating vessels are well visualized. The challenge of removing the tumor capsule from the vessels and neural structures is often the limiting factor, as in any approach. It may be satisfactorily used alone in the rare setting (3% to 10%) of a purely third ventricular craniopharygioma. A craniotomy is performed that is predominantly over the nondominant hemisphere but with exposure of the sagittal sinus at approximately two thirds of its length anterior and one third of its length posterior to the coronal suture, although this location may be modified after use of a neuronavigation system. The dura is reflected toward the sinus while taking great care to preserve cortical venous drainage. The ipsilateral hemisphere is gently retracted to allow dissection in the interhemispheric space down to the callosum. Care is taken to identify and preserve the pericallosal arteries on the corpus callosum. Tumor may be resected through an enlarged foramen of Monro, or the choroidal fissure can be opened to allow greater access to the third ventricle. Alternatively, an interforniceal approach with direct access to the third ventricle can be used. Internal decompression with piecemeal extirpation of tumor is favored in this location. This approach puts at risk the medial hemisphere from retraction, in addition to the pericallosal arteries and fornix, as well as the veins and floor of the third ventricle. A frontotemporal incision is made, and the temporalis muscle can be raised with the skin as a myocutaneous flap or reflected posteriorly after interfascial dissection. A frontotemporal bone flap is elevated, and the lateral aspect of the lesser wing of the sphenoid is drilled away. Frontal extension of the craniotomy is advocated by some authors to improve access. The sylvian fissure is split, and frontal and temporal retractors may be used judiciously to provide access to the tumor. Extension of craniopharyngioma into the third ventricle may be removed by opening the lamina terminalis. In the case of large retrochiasmatic or retrosellar lesions, the pterional approach offers a narrow window that may be obstructed by perforating vessels. A frontotemporal incision is made, followed by interfascial dissection to reflect the temporalis inferoposteriorly. The frontotemporal craniotomy is extended to involve the lateral orbital bar and zygoma. The dural opening and intradural procedure is then similar to the pterional approach but is extended to allow access to lesions with more vertical height. A candidate for this approach, generally in combination with a basal approach, would be a patient with hydrocephalus and craniopharyngioma extending into the third ventricle, particularly through the foramen of Monro. A linear or U-shaped flap incision is made to expose the frontal bone just anterior to the coronal suture. A neuronavigation system can be useful for planning the bone flap and to direct access to the ventricle. The dura is reflected medially and the corticectomy performed through the middle frontal gyrus. The tumor is identified and may be resected from the ventricle and followed through the foramen of Monro into the third ventricle. The size of the ventricle is important, and hence in the absence of significant hydrocephalus, this approach is unfavorable. Ipsilateral dissection of the wall of the third ventricle is also difficult with this approach. Deficiencies of four or more hormones develop in more than 75% of patients who undergo aggressive tumor resection. Hyperprolactinemia, secondary adrenal failure, and hypothyroidism were found in 41%, 32%, and 25% of patients, respectively. Preoperatively, diabetes insipidus was relatively uncommon, being clinically evident in approximately 15% of patients. Postoperatively, diabetes insipidus was common, with an incidence of 59% at 3 months. This finding is consistent with the series of Yasargil and colleagues,54 wherein permanent postoperative diabetes insipidus developed in 68% of patients. In general, it is rare to witness any improvement in endocrine status, and those with a partially deficient hypothalamic-pituitary axis frequently deteriorate. The majority of these data have been retrospective in nature and are derived from craniopharyngioma series made up predominantly of children. A battery of tests were used in this study, both preoperatively and postoperatively. No significant impairment in neuropsychological performance or quality of life could be demonstrated postoperatively. Because of the potential adherence of craniopharyngiomas to blood vessels, postoperative vascular complications have also been reported. Fusiform dilation of the carotid artery is believed to result from possible adventitial damage that occurs when craniopharyngiomas are peeled off this vessel. Patients who undergo transsphenoidal resection consistently have lower overall mortality rates than do those who undergo craniotomy. Rates of visual decline in patients treated by subtotal resection followed by radiation therapy varied from 2% in most series to as high as 30% in some series. It has been proposed as an approach to reduce the morbidity of surgery for craniopharyngioma and, with the addition of adjuvant conformal irradiation, to maintain effective disease control. These large cysts can be decompressed as either a primary or a definitive procedure. Frequently, this maneuver rapidly alleviates many of the symptoms of visual compromise, hypothalamic dysfunction, and increased intracranial pressure. It is often possible to pass a catheter through the ventricular system and into the cyst. Because most cysts reaccumulate within 2 months, definitive surgical resection is often done within 4 weeks of cyst decompression. Radiation Therapy Radiation therapy has long been used as an adjuvant treatment of craniopharyngioma after subtotal resection and as primary treatment of recurrence. Early work has shown that conventional fractionated radiotherapy appears to be beneficial when administered in doses between 45 and 55 Gy delivered to the primary tumor in fractions of 1. Pituitary dysfunction, hypothalamic dysfunction,129,130 and visual and cognitive deficits are well-recognized complications, in addition to radiation necrosis, vasculopathy, and second malignancies.
Discount 2.5mg nebivolol overnight delivery
The rationale for performing third ventriculostomy first is to do so before potential bleeding and clouding of the ventricle occur as a result of the biopsy procedure heart attack mp3 purchase nebivolol 5mg free shipping. The rationale for performing a biopsy first is that it is the main goal and should be completed before potential bleeding occurs. Endoscopic pineal tumor biopsy and third ventriculostomy with a rigid endoscope have been performed successfully through a single bur hole. The need for simultaneous biopsy of a pineal region tumor and endoscopic third ventriculostomy is the most common application for flexible neuroendoscopy. The microsurgical route to this region is well established; however, it is a long corridor that keeps the pathology at some distance from the surgeon. The walls of the third ventricle, seen from behind, form a narrow corridor where residual tumor is often perpendicular to the direction of view and hence evades direct inspection. The endoscope overcomes all these limitations and thereby allows effective endoscopically controlled surgery. With a primarily microsurgical approach to the pineal region, angled endoscopes should be used to check the walls of the resection cavity for tumor and to inspect the third ventricle for residual blood that might obstruct the aqueduct. Selected examples of anecdotal use illustrate its possibilities, which still wait to be fully explored. The applications for which it has both rationale and practical advantage are those in which the endoscope can help limit retraction and improve an otherwise restricted view. For example, during removal of an insular glioma, where the overlying opercula are extremely eloquent and cannot and should not be retracted, the endoscope can improve visualization of residual tumor. This technique can allow the surgeon to avoid expanding the corticotomy solely to improve microscopic visualization. Therefore, the sheath must be wide enough to accommodate both the endoscope and microinstruments. Introduced by otorhinolaryngologists to treat sinus disease,100 endonasal endoscopy was initially applied in neurosurgery primarily as an adjunct to the microsurgical transsphenoidal approach to the sella turcica for pituitary pathology. The remaining bright signal is the fat graft, which has shrunk down on the frontal fossa floor. A wide range of pathologies have proved accessible from this corridor, including sinonasal tumors (esthesioneuroblastomas, juvenile nasal angiofibromas), sellar pathologies (pituitary tumors, craniopharyngiomas), clival tumors (chordomas, chondrosarcomas), anterior cranial fossa dural-based tumors (meningiomas), and selected intradural tumors. Most midline and paramedian masses are highly accessible through the endonasal route in both adults and children. The inability to see behind the endoscope is mostly immaterial because the only structures affected are the walls of the nasal cavity. Knowledge of the anatomy and careful avoidance of larger vascular structures help avoid major bleeding. The two nostrils afford a surprising range of motion and, by switching between 0-degree and 30-degree endoscopes, a good range of viewing angles as well. Two surgeons working simultaneously, often a neurosurgeon and an otolaryngologist experienced in sinus endoscopy, enable a four-handed technique that not only overcomes the limitations of one-handed surgery that plague many other types of endoscopy but also actually exceeds it by allowing simultaneous use of an endoscope, a suction device, and two microsurgical instruments. In this manner, sharp dissection and bipolar electrocautery can be used on tumors just as they are under the microscope. Thorough knowledge of the anatomy of the nasal cavity, paranasal sinuses, and anterior skull base is essential for success and avoidance of complications. The surgeon should be able to identify the superior, middle, and inferior turbinates and the openings of the ostia into the maxillary and sphenoid sinuses. The middle turbinate can often be lateralized or resected to improve access to deeper structures. The cartilaginous septum can be mobilized, but it must be preserved and restored at the end of surgery to prevent nasality and whistling in speech postoperatively. The more posteriorly placed bony septum can be removed along with the face of the vomer, sphenoid, and surrounding structures as distant as the cavernous sinuses bilaterally. Having defined the normal anatomy around the tumor, its margin can be defined, and the tumor can be removed with the same techniques as used in microsurgery, including sharp dissection and electrocautery. A maxillotomy can expand this field even more if lateral structures need to be accessed. Moving anteriorly and superiorly from the face of the sella, the tuberculum sellae and planum sphenoidale can be removed to provide access to the optic chiasm and anterior communicating artery complex. At the limit of this trajectory the ostium of the frontal sinus can be accessed, but the sinus itself is frequently too anterior to work inside. However, all structures posterior to this point, from the olfactory groove back to the cervical spine, are accessible. Inferior to the sella, the entire central part of the clivus can be removed with minimal morbidity. Bone is removed sequentially with a high-speed drill or biting instruments to expose the target area. Because exposure is from below, neurovascular structures can often be separated from dural-based structures with minimal impact. Tumors ideally suited to the minimally invasive transsphenoidal or expanded transsphenoidal approach are those that are midline. The greatest advantage of the endonasal approach to the skull base is the ability to attack the tumor directly without facing intervening neurovascular structures. Meningiomas of the skull base illustrate how advantageous it is to attack a tumor directly from below. These advantages are lost if any nerve or major vessel lies between the surgeon and the tumor. Those who believe that chordomas of the clivus should be removed en bloc would be better served by using more traditional craniofacial approaches to the skull base. Although en bloc removal is possible in highly skilled hands, most lesions are removed piecemeal when an endoscope is used. Highly vascular tumors such as hemangiopericytomas create significant bleeding problems. Their removal can be very time-consuming given the constraints imposed by the relatively primitive endoscopic bipolar forceps that are available commercially. Anterior cranial fossa meningiomas can be removed extremely effectively both transcranially and endonasally. Conversely, if there is anatomic juxtaposition of the posterior margin of the tumor and large vessels or if the vessels are involuted into the tumor (as is often the case with tumors that are primarily of tuberculum sellae origin), a transcranial approach is preferred. However, this anatomic variation creates an excellent corridor to these tumors when operating from below. Expanded endonasal endoscopic techniques have been used to aid the surgeon in seeing these attachments of the tumor, thereby allowing it to be mobilized under direct vision. This lesion would be difficult to remove through a subfrontal/prechiasmatic approach. This strategy allows the ventricular extension of the tumor to be freed before it is resected from below. The main difficulty posed by more extensive skull base work is achieving appropriate closure. Even extensive removal of bone and mucosa alone usually has few serious consequences. With appropriate management, the sinuses normally mucosalize rapidly after surgery. Unlike convexity cranial approaches in which a tightly secured scalp can hold the spinal fluid and allow healing, there is no equivalent layer in the sinuses. The principles of reconstruction are to make the smallest dural defect possible, open the dura sharply, preserve the arachnoid, leave a shelf of bone on which bone or a bone substitute can rest, and cover the defect with a watertight layer, of which a vascularized mucosal flap is the best option. The addition of fat grafts, fascia lata grafts, dural substitutes, dural sealants, acellular dermis, and other adjuncts is at the discretion and experience of the treating surgeon. In other cases, an inflated Foley catheter may be used to provide a bolster for the tissue repair. The possibility of robotic instruments that could allow very fine work to be performed through a small portal has great appeal. For endoscope-assisted and endoscope-controlled surgery, major advances will be directed at allowing neurosurgeons to do microsurgical work "around the corners" under endoscopic view only. Curved instruments that allow microsurgical work to be done in these recesses and instruments that combine the functions of multiple instruments (for instance, a suction and endoscope or suction and cautery) may facilitate working with the endoscope with a single hand. New tools for sharp endoscopic dissection, primary dural closure, and control of vascular structures are needed. A sharper and brighter picture, the possibility of true three-dimensional endoscopy, flexible endoscopy with a picture equivalent to that of a rod lens endoscope, and incorporation of frameless stereotactic data onto the video image would all be welcome additions to the endoscopic armamentarium. A reality behind innovation in neuroendoscopic instrumentation is the need for enough economy of scale for instrument companies to invest in potential new developments.