Buy tizanidine toronto
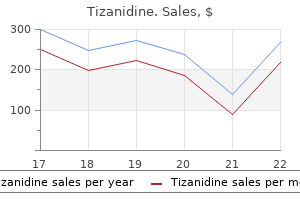
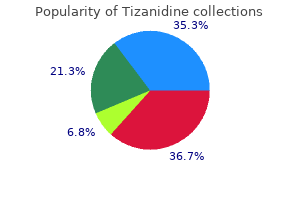
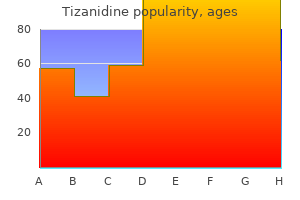
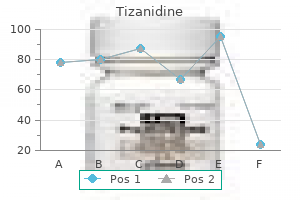
The cerebrospinal fluid culture was negative but Proteus mirabilis was cultured from the abscess hip pain treatment uk buy tizanidine 2mg with amex. Needle aspiration is useful not only for initial diagnosis and drainage but also for determining antibiotic levels in the abscess cavity. Open surgical drainage is the most definitive therapeutic approach for brain abscess. Careful serial brain imaging should be performed to ensure that the lesion (or lesions) is (are) not worsening. This 5-week-old infant had focal seizures, Proteus sepsis, and a complicated congenital cardiac lesion, including an atrioventricular canal defect. On the parasagittal view (B) extensive areas of increased echogenicity are seen adjacent to the round area of relative echolucency. The coronal magnetic resonance images, T2-weighted sequence (C), confirm the large left-sided abscess. This category of nonbacterial disease is discussed here rather than in Chapter 34 because the clinical features often mimic those of bacterial sepsis and the neuropathological features are similar to those of bacterial meningitis and brain abscess. The presence of gram-positive, small, oval, budding yeast cells and sometimes hyphae with budding yeast cells attached along their length is typical. With subacute lesions, a more granulomatous appearance Like bacterial sepsis, systemic candidiasis does not produce a distinct clinical syndrome. A subdural empyema was reported in a preterm infant who had a malpositioned central venous catheter such that the tip of the catheter migrated into the epidural space. Cranial ultrasound (A) shows severe, diffuse echogenicity throughout the white matter. They are usually not seen in the first days of candidemia but rather within a week after onset of the infection. Note the echogenic ependyma (arrowheads) and the intraventricular septa (arrow), both consistent with ventriculitis. This should include ophthalmological examination, echocardiography, abdominal ultrasound, and urine analysis. The outcome is not entirely clear because of the relatively recent advent of prompt diagnosis and therapy. Characteristic unilateral or bilateral, yellow-white, fluffy retinal or vitreal balls with frequent hemorrhage or inflammatory vitreous haze may be seen on indirect fundoscopy. Systemic antifungal therapy for such endophthalmitis usually results in a good visual outcome but there may be some subsequent decrease in visual acuity. Microabscesses are apparent as small foci of echogenicity with both imaging techniques. In one study, prophylactic fluconazole was targeted to infants administered broad-spectrum antibiotics for more than 3 days; the incidence of invasive fungal infection was 6. The major adverse effect in newborns is renal toxicity; hepatic toxicity is much less common in infants than in older patients. Serial monitoring of serum potassium and magnesium levels and of renal, liver, and bone marrow function is required. More recent reports, however, suggest no added therapeutic benefit when 5-fluorocytosine is combined with amphotericin B. The umbilical cord has usually been cut at the time of birth with an unsterile instrument and occasionally has even been smeared with a variety of unsterile foreign materials. Any degree of passive transfer of immunity to the infant during gestation is rare. In an older series of 54 affected infants reported from the United States, only 3 of the mothers had any form of tetanus toxoid immunization. The proteolytic action of the tetanus neurotoxin on this vesicle-associated membrane protein releases the latter into the cytosol and prevents docking and thereby release of the neurotransmitter-containing vesicles. The synaptic release of inhibitory transmitters, particularly glycine and gamma-aminobutyric acid, is affected. The synapses are those of interneurons of polysynaptic pathways, especially in spinal cord and brain stem. Once fixed at the presynaptic membrane site, the toxin cannot be neutralized by antitoxin, and clinical recovery depends on the slow process of membrane turnover and synthesis of vesicle-associated membrane protein. The enhanced excitatory activity that characterizes the neurological features of neonatal tetanus presumably relates to an impairment of the normal balance between inhibitory and excitatory influences on the lower motor neurons in the brain stem and spinal cord. In a careful study conducted in a town in Sudan, 1 in every 110 infants died of neonatal tetanus. The earlier the onset, the more severe the clinical features and the greater the risk of death. Diminished sucking or refusal to suck, impaired feeding, excessive crying, irritability, and rigid abdomen are the initial features. Supportive care is paramount in the management of neonatal tetanus, and maintenance of adequate. Cultures of the umbilical stump, even when handled carefully for anaerobic organisms, are usually negative. Electromyographic findings of increased insertional activity in the form of trains of motor unit discharges can be helpful in diagnosing the difficult case. The setting of birth at home, inadequate management of the umbilical stump, nonimmunized mother, and characteristic neurological features should raise the suspicion of the diagnosis of tetanus. Initially, nuchal rigidity may suggest meningeal irritation and hence meningitis or intracranial hemorrhage. Moreover, the spasms are readily mistaken for convulsions and therefore a variety of cerebral conditions. These disorders should be ruled out because more specific therapy may be needed urgently. The trismus impairs feeding, and the infant exhibits certain features particularly characteristic of neonatal tetanus. The generalized rigidity is usually accompanied by a characteristic, persistent flexion of the toes. The spasms are exacerbated by stimulation, may occur many times an hour, and may be mistaken for seizures. Indeed, respiratory failure resulting from repeated spasms is the most common cause of mortality and morbidity in this disease. The usual duration of disease in the patient with a moderate to severe case and who is effectively supported therapeutically is 3 to 5 weeks. This goal has been accomplished to a major degree in many countries by the widespread active immunization of the population, such that transplacental transfer of antitoxin is adequate. Immunization of women during pregnancy has proved highly effective in preventing the occurrence of disease in the infant. In settings with critical care facilities, younger age, lower weight, delay in admission, and leukocytosis were independent risk factors of a poor outcome. In a systemic review and meta-analysis, low-birth-weight showed a significantly increased risk of mortality. In a cumulative series of 138 infants, 19 (14%) exhibited mental retardation or an intelligence quotient lower than 80 on long-term follow-up. In a recent study, a 66% reduction in mortality was achieved by the introduction of a new management regimen including antibiotic therapy, muscle relaxation, and invasive monitoring. Invasive blood pressure monitoring enabled early detection of autonomic nervous system dysfunction and timely intervention. The umbilical infection does not usually require local surgical therapy, but penicillin G is administered intravenously in a dose of 10,000 units/kg per day for 10 days. A controlled study demonstrated equivalent benefit for human tetanus immune globulin, 500 units, and equine tetanus antitoxin, 10,000 units. Nasotracheal intubation (rather than tracheostomy), mechanical ventilation, and a degree of muscular paralysis sufficient to allow smooth ventilatory control have been shown to be highly effective. These various measures are designed to prevent the respiratory failure, pulmonary disease, hyperpyrexia, pneumonia, and dehydration, which may result in death. The sedative drugs chosen to alleviate the muscular spasms most commonly have included primarily phenobarbital, chlorpromazine, and diazepam.
Syndromes
- Go to the dentist every year for an exam and cleaning.
- General anesthesia
- Joint dislocation
- Fatigue
- Frontal bossing and a prominent jaw
- Complete blood count (CBC) may show a high number of white blood cells and reduced number of red blood cells.
- Tests to screen for chlamydia and gonorrhea (urethral smear)
- Chest pain
- Mood changes
Purchase cheapest tizanidine and tizanidine
By far the most frequent of these infections is neonatal bacterial meningitis opioid treatment guidelines journal of pain proven 2mg tizanidine, and this chapter deals with this disorder in detail. Because most of these bacterial diseases are exceedingly rare, and one (botulism) is discussed in Chapter 32, only brain abscess and neonatal tetanus are discussed in this chapter. Systemic candidiasis, a disseminated fungal infection, is also discussed briefly (rather than in Chapter 34) because the manifestations thereof, which include meningitis and brain abscess, are related more closely to the subject matter of this chapter. The major bacterial causes of early- versus late-onset sepsis are shown in Table 35. These organisms are part of the normal skin and mucosal flora and induce infection in the presence of prolonged indwelling vascular catheters and related features of neonatal intensive care, especially of very premature infants. Pseudomonas and related gram-negative organisms that contaminate moist ventilatory equipment also become prominent in late-onset sepsis. Escherichia coli and Klebsiella species account for 20% to 25% of both early-onset and late-onset cases. In the ensuing discussion, the etiology, pathogenesis, neuropathology, clinical features, diagnostic aspects, prognosis, and management of neonatal bacterial meningitis are reviewed. Where relevant, the discussion centers on specific aspects related to a particular organism, but in general the features of neonatal bacterial meningitis caused by most organisms exhibit more similarities than differences. Coagulase-negative staphylococci are particularly common etiologies in very-low-birth-weight infants with late-onset meningitis. More common in cases with onset after 30 days, especially in low-birth-weight infants. Acquisition is principally by parturitional exposure or, less commonly, ascending infection. Thus, it is not surprising that important factors predisposing to sepsis and meningitis include a variety of complications of labor and delivery (especially fetal distress, obstetrical trauma, and placental abnormalities), maternal peripartum infection (especially of the genital or urinary tracts), prolonged rupture of membranes, and chorioamnionitis (Table 35. In the majority of cases of early-onset neonatal listeriosis, a maternal history of flu-like syndrome, unexplained fever, or urinary tract symptoms in the several days to weeks before delivery can be elicited. Studies of T cells in cord blood demonstrate qualitative and quantitative differences in immune responses compared with adult T cells, and these differences are diminished only gradually during infancy. Deficiencies of specific humoral immunity have involved the immunoglobulin M (IgM) and immunoglobulin G (IgG) classes of antibodies. IgM antibodies include several antibody types that are important in the defense against gram-negative bacteria; deficiency of these antibodies in the newborn infant may play a role in the susceptibility to gram-negative bacteria. Age-dependent adaptations of innate immunity include the following: impaired leukocyte chemotaxis, phagocytosis, and bactericidal activity; defective neutrophilic metabolic responses after phagocytosis. In early life, immunity is characterized by age-dependent adaptations of both innate and adaptive immune responses. The first-line host defense is formed by innate immune cells recognizing pathogens by unique molecular patterns with pathogen recognition receptors. Innate immune responses include opsonization, complement activation, secretion of inflammatory mediators, and induction of apoptosis. These data suggest that this IgG antibody is important in protecting the infant and that passive transfer across the placenta did not occur because of maternal failure to synthesize the antibody. The propensity oo ks of both immaturity of the antibody-producing B cells and plasma cells and diminished T-cell help for antibody production. The deficiency in immune globulins has led to clinical trials of the use of intravenous immune globulin in the prophylaxis and treatment of bacterial infection in newborns, especially premature newborns. Neonates are heavily dependent on innate immune responses for protection against infections. The brain microglial cell, which is derived from monocytes (see Chapter 13), is an important part of this defense. Activation of innate immune cells occurs by way of specific cell-surface receptors. Thus nosocomial infection rates of up to 40% have been reported, particularly in medical centers where high rates of newborns are already colonized at birth (by vertical transmission from the mother) and where high daily census rates are reported, thereby favoring cross-contamination of infants by nursery personnel. Arachnoiditis is discussed first because it is the dominant feature of bacterial meningitis. The hallmark of bacterial meningitis is infiltration of the arachnoid with inflammatory cells. The evolution of this inflammatory response is well described by Berman and Banker. Moreover, certain additional histological features are particularly characteristic of infection with specific organisms; these features are discussed separately. The likelihood that capsular polysaccharides reflect, to a considerable degree, an intrinsic virulence of these organisms is suggested by in vivo and in vitro observations. Acute Arachnoiditis Ventriculitis: choroid plexitis Vasculitis Cerebral edema Infarction Associated encephalopathy (cortical neuronal necrosis, periventricular leukomalacia) Chronic Hydrocephalus Multicystic encephalomalacia porencephaly Cerebral cortical and white matter atrophy Cerebral cortical developmental (organizational) defects ( This left lateral view of the cerebrum shows thick arachnoidal exudate, especially prominent in the region of the sylvian fissure. Bacteria are visible, free, and within polymorphonuclear leukocytes and macrophages. The inflammatory exudate is particularly prominent around blood vessels and extends into the brain parenchyma along the Virchow-Robin space. Although precise, controlled data are not available, ventriculitis appears to be more common in neonatal meningitis than in meningitis at later ages. In the second and third weeks of the disease course, the ventricular exudate is associated with active ependymitis, characterized by disruption of the ependymal lining and projections of glial tufts into the ventricular lumen. Less commonly, septations in the lateral ventricle may produce a multiloculated state that is similar to abscess formation. The multiple ventricular obstructions, in fact, may isolate portions of the lateral ventricles or the fourth ventricle, cause disproportionate and severe dilation of the affected ventricle, and present a difficult therapeutic problem. Lymphocytes and plasma cells are present in relatively small numbers, and this paucity is a characteristic feature of neonatal meningitis. Whether this apparent deficiency of cells involved in the immunological response plays a role in the relative tenacity of neonatal bacterial meningitis remains to be determined but seems plausible. After approximately 3 weeks, the exudate decreases in amount and consists of mononuclear cells. Thick strands of collagen become apparent as arachnoidal fibrosis begins to develop. The characteristics of the arachnoiditis caused by different bacteria vary little. The lateral ventricle contains a mass of protein-rich cellular exudate and necrotic debris organized into layers. Gilles and co-workers146 have presented considerable data to support this view, including the high glycogen content of the neonatal choroid plexus, which provides an excellent medium for bacteria. Moreover, an age-related effect is suggested by the postnatal decrease in glycogen content of plexus epithelial cells. These observations further support the notion that the initial events in the genesis of bacterial meningitis are bacteremia and infection of the choroid plexus and lateral ventricles. The therapeutic implications of these data concerning ventriculitis are important and are discussed later, in the section on management. Stain for glial fibers shows the formation of glial bridges that have narrowed and partially occluded the aqueduct. The arteritis is manifested particularly by inflammatory cells in the adventitia; however, involvement of the intima is not uncommon. Involvement of veins is severe and includes arachnoidal, cortical, and subependymal veins. Multiple fibrin thrombi of adjacent veins are often observed in association with areas of hemorrhagic infarction (see the section on infarction later). The vasculitic changes are apparent in the first days of meningitis and become particularly prominent by the second and third weeks. More similarities than differences exist among various bacteria with regard to the nature and severity of the vascular changes with meningitis. Note the diffusely swollen appearance of the cerebral parenchyma, resulting in flattened gyri and small, slit-like ventricles.
Buy discount tizanidine on line
Strong desmin expression in a congenital desmoplastic infantile ganglioglioma mimicking pleomorphic rhadomyosarcoma: a case report including ultrastructural and cytogenetic evaluation and review of the literature low back pain treatment video order tizanidine online. Diffusion imaging for tumor grading of supratentorial brain tumors in the first year of life. Extracerebral neural tissue mass in the middle cranial fossa extending into the oropharynx in a neonate. Intracranial tumors in infants: long-term functional outcome, survival, and its predictors. Brain tumors in children under 1 year of age: emphasis on the relationship of prognostic factors. Neurosurgical treatment of brain tumors in the first 6 months of life: longterm follow-up of a single consecutive institutional series of 30 patients. Successful treatment of hemorrhagic congenital intracranial immature teratoma with neoadjuvant chemotherapy and surgery. Quality of long-term survival following irradiation for intracranial tumors in children under the age of two. Late effects of central nervous system treatment of childhood acute lymphoblastic leukemia are sex-dependent. Role of stereotactic radiosurgery with a linear accelerator in treatment of intracranial arteriovenous malformations and tumors in children. Arteriovenous malformation of the vein of Galen in three neonates: emphasis on associated early ischaemic brain damage. Hemodynamic disturbances associated with endovascular embolization in newborn infants with vein of Galen malformation. Clinical course and medical management of neonates with severe cardiac failure related to vein of Galen malformation. Recent improvement in outcome using transcatheter embolization techniques for neonatal aneurysmal malformations of the vein of Galen. Colour Doppler imaging of arteriovenous malformation of the vein of Galen in a newborn. Intracranial arachnoid cysts in children: a review of pathogenesis, clinical features, and management. The direct effects of a drug on the developing brain will vary depending on the type of drug, the gestational timing of exposure, dose, the extent of drug distribution, and the number of drugs. The developmental stage of the fetus at the time of exposure as well as the sensitivity of different brain regions to different chemical agents also likely play a role. A distinction can also be made between drugs that are associated with congenital malformations in the newborn infant co. In the broadest sense, drugs may disturb specific developmental events in the brain and, in turn, produce teratogenic effects. In addition, maternal ingestion of certain drugs can result in passive addiction of the fetus, and postnatally lead to a neonatal withdrawal or abstinence syndrome. The capacity for teratogenicity was first recognized in the late 1950s and early 1960s with the recognition of the adverse effects of thalidomide. Believed to be safe, thalidomide was prescribed to large numbers of pregnant women as a treatment for morning sickness but was later found to result in a number of birth defects. The most notable of these was phocomelia, in which the bones of the arms and, in some cases, other limbs were extremely shortened or absent. These effects vary in severity, from profound effects on morphological structure to more subtle, but nonetheless clinically significant, neurological effects. Further, few of these effects are transient, with most persisting in some form into childhood and adolescence. Multiple systems are often affected spanning cognition, motor function, language, and behavior. In addition to these direct effects, drugs can have indirect effects on fetal brain development via their impact on other organ and physiological systems. For example, cocaine impairs fetal oxygen and nutrient transfer via profound vasoconstriction of the umbilical vein. Acutely, these alterations may contribute to cerebral infarction and intracranial hemorrhage. Chronically, these perturbations may contribute to the documented impact of cocaine on cortical neuronal migration and differentiation. Functional polymorphisms in alcohol metabolism may best exemplify this phenomenon. The offspring of individuals with normal metabolism experience long-term impacts from in utero alcohol exposure, whereas the offspring of rapid metabolizers avoid these effects. Finally, there is also growing evidence to suggest epigenetic influences on outcome. In addition to these drug- and infant-related factors, several other maternal and environmental factors may play a role in determining the clinical presentation of an infant and are therefore important to consider. Comorbid physical and mental health conditions in the mother, combined with the underlying disease state, may complicate the interpretation of prenatal drug effects and exacerbate risks for the infant. In addition, maternal life style factors, such as pregnancy, nutrition, and social disadvantage, which are correlated with substance use, may also contribute to later risks, including poor growth and neurodevelopmental impairment. The accurate estimation of these rates is hindered by a number of methodological problems. Finally, one of the most affected regions of the world is Africa, where binge drinking is reported by around one in four women, and in some cases half of all pregnant women. It is important to note that these rates are widely regarded to underestimate the extent of this problem for the methodological reasons listed previously, as well as difficulties with both misdiagnosis and underdiagnosis. Two children: one (A) in the newborn period and (B) at the age of 6 months, and (C) the other at the age of 16 months. Note the short palpebral fissures, especially prominent in the newborn (A), and the low nasal bridge with short, upturned nose, epicanthal folds, long, hypoplastic philtrum, and convex upper lip with narrow vermilion border. Executive deficits include problems with planning and organization, cognitive flexibility/ set shifting, working memory, and behavioral inhibition, with parents reporting the greatest difficulty with inhibitory control and problem solving. These include (1) the extent of prenatal alcohol exposure (dose, timing) and the severity of the condition. The most disabling of these subsequent problems are the intellectual and behavioral impairments. At birth, infants have a distinct pattern of growth restriction, with length often affected more than weight, which is a pattern different from that expected with intrauterine undernutrition. This poor growth persists postnatally, but weight gain is more disturbed than linear growth. As with all recreational drugs, it is also important to clarify the extent of prenatal exposure to other drugs, such as tobacco, illicit substances, and any prescribed medications. For example, a variety of limb anomalies can be observed in around one-half of these infants. Cardiac lesions occur in approximately one-half, but these lesions are usually not severe and mostly consist of septal defects, with atrial defects more common than ventricular defects. Minor ear anomalies occur in approximately one-fourth of the children, and hearing loss, primarily conductive and of a mild nature, occurs in 75% of infants. Optic nerve hypoplasia affects 75% of infants, but disturbances of visual acuity are not marked. Other less common anomalies include strabismus, ptosis, micrognathia, cleft palate, railroad track ears (prominent horizontal crus of the helix with prominent and parallel inferior crus of the antihelix), decreased elbow pronation/supination, joint contractures (most commonly incomplete extension of one or more digits), and palmar crease abnormalities. These diagnoses may be needed to ensure that a child receives ongoing developmental surveillance in view of high rates of neurodevelopmental impairment in children exposed to alcohol in utero. Common difficulties include word comprehension, naming ability, phonological processing, speech production, and articulation errors, resulting in poorer performance on tests of both receptive and expressive language development. Note that nearly all of the left hemisphere is covered by a massive sheet of tissue that crosses the midline and extends onto the superior and medial aspects of the right frontal lobe. Extending through a break in the pial surface (upper left of cortex) is the heterotopic sheet of tissue composed of neuronal, glial, and pial elements that have covered the true cortex. The most striking additional abnormalities reported appear to involve neuronal and glial migration. Longer-term substance abuse and mood disorders, such as anxiety and depression, are also common. Aberrations of brain stem and cerebellar development, in large part related to faulty migration, also have been particularly frequent. However, it is important to note that almost all studies have been conducted in older children, thus limiting information about structural and functional brain abnormalities during infancy, or the way in which prenatal alcohol exposure affects the developing brain over time and age. Abnormalities include partial or complete agenesis, underdevelopment, and corpus callosal thinning, particularly in the splenium which is involved in communication between the parietal and temporal lobes.
Purchase tizanidine 2 mg fast delivery
Lymphocytic choriomeningitis virus infection of the developing brain: critical role of host age kidney pain treatment buy tizanidine in united states online. Lymphocytic choriomeningitis virus: an underrecognized cause of neurologic disease in the fetus, child, and adult. Birth outcomes following West Nile Virus infection of pregnant women in the United States: 2003-2004. Intrauterine Zika virus infection and microcephaly: perinatal imaging correlations with 3D virtual physical models. Epidemiology of congenital cytomegalovirus infection: maternal risk factors and molecular analysis of cytomegalovirus strains. Sequelae of acquired cytomegalovirus infection in premature and sick term infants. Postnatally acquired cytomegalovirus infection in preterm infants: a prospective study on risk factors and cranial ultrasound findings. Predictors of severity for postnatal cytomegalovirus infection in preterm infants and implications for treatment. Postnatal human cytomegalovirus infection in preterm infants has long-term neuropsychological sequelae. Symptomatic congenital cytomegalovirus infection in infants born to mothers with preexisting immunity to cytomegalovirus. Controversies in the natural history of congenital human cytomegalovirus infection: the paradox of infection and disease in offspring of women with immunity prior to pregnancy. New estimates of the prevalence of neurological and sensory sequelae and mortality associated with congenital cytomegalovirus infection. Antiviral antibody responses in mothers and their newborn infants with clinical and subclinical congenital cytomegalovirus infections. Hearing loss in children with congenital cytomegalovirus infection in relation to the maternal trimester in which the maternal primary infection occurred. Cerebral involvement with advanced periventricular calcification in generalized cytomegalic inclusion disease in the newborn; a clinicopathological report of a case diagnosed during life. The correlation of maternal cytomegalovirus infection during varying stages in gestation with neonatal involvement. Congenital cytomegalovirus infection after recurrent infection: case reports and review of the literature. Intrauterine transmission of cytomegalovirus to infants of women with preconceptional immunity. Sequelae following postnatally acquired cytomegalovirus infection in very low-birth-weight neonates: back to the future. Severe postnatally acquired cytomegalovirus infection presenting with colitis, pneumonitis and sepsis-like syndrome in an extremely low birthweight infant. Epidemiology of transmission of cytomegalovirus from mother to preterm infant by breastfeeding. Cytomegalovirus transmission from breast milk in premature babies: does it matter Cytomegalovirus transmission to extremely low-birthweight infants through breast milk. Case-control study of symptoms and neonatal outcome of human milktransmitted cytomegalovirus infection in premature infants. Postnatally acquired cytomegalovirus infection via breast milk: effects on hearing and development in preterm infants. Human cytomegalovirus nucleic acids in tissues from congenitally infected infants. Outcome of pregnancies with vertical transmission of primary cytomegalovirus infection. Fetal cytomegalovirus infection of the brain: the spectrum of sonographic findings. Focal sonographic periventricular pattern associated with mild ventriculomegaly in foetal cytomegalic infection revealing cytomegalic encephalitis in the third trimester of pregnancy. Retrospective diagnosis of congenital cytomegalovirus infection and cortical maldevelopment. Disordered migration and loss of virus-infected neuronal cells in developing mouse brains infected with murine cytomegalovirus. Congenital cytomegalovirus infection of the brain: imaging analysis and embryologic considerations. Neuro-imaging findings in infants with congenital cytomegalovirus infection: relation to trimester of infection. Letter: bilateral eventration of the diaphragm in a neonate with congenital cytomegalic inclusion disease. Magnetic resonance imaging of the brain in congenital rubella virus and cytomegalovirus infections. Clinical, biochemical, and neuroimaging findings predict long-term neurodevelopmental outcome in symptomatic congenital cytomegalovirus infection. Neuroradiographic findings in the newborn period and long-term outcome in children with symptomatic congenital cytomegalovirus infection. Newborn hearing screening: will children with hearing loss caused by congenital cytomegalovirus infection be missed A prospective study of maternal cytomegalovirus infection and its effect on the fetus. Progressive hearing loss in infants with asymptomatic congenital cytomegalovirus infection. Diabetes insipidus associated with symptomatic congenital cytomegalovirus infection. Progressive neurological disease associated with chronic cytomegalovirus infection. Progressive postnatal subependymal necrosis in an infant with congenital cytomegalovirus infection. Predictors of hearing loss in children with symptomatic congenital cytomegalovirus infection. Hearing loss in children with congenital cytomegalovirus infection born to mothers with preexisting immunity. Specific cell-mediated immunity and the natural history of congenital infection with cytomegalovirus. Congenital cytomegalovirus infection: recent advances in the diagnosis of maternal infection. Low total IgM values and high cytomegalovirus loads in the blood of newborns with symptomatic congenital cytomegalovirus infection. Secondary cytomegalovirus infection can cause severe fetal sequelae despite maternal preconceptional immunity. Comparative study of diagnostic procedures for congenital cytomegalovirus infection. Retrospective diagnosis of congenital cytomegalovirus infection using umbilical cord. Urine viral load and correlation with disease severity in infants with congenital or postnatal cytomegalovirus infection. Ganciclovir therapy for symptomatic congenital cytomegalovirus infection in infants: a two-regimen experience. Cysts of the subependymal germinal matrix: sonographic demonstration with pathologic correlation. Intracranial lesions of congenital cytomegalovirus infection detected by ultrasound scanning. Echogenic vasculature in the basal ganglia of neonates: a sonographic sign of vasculopathy. Linear areas of echogenicity in the thalami and basal ganglia of neonates: an expanded association. New pattern of hyperechogenicity in thalamus and basal ganglia studied by color Doppler flow imaging. Brain magnetic resonance findings in symptomatic congenital cytomegalovirus infection. Risk of cytomegalovirusassociated sequelae in relation to time of infection and findings on prenatal imaging. Effect of ganciclovir therapy on hearing in symptomatic congenital cytomegalovirus disease involving the central nervous system: a randomized, controlled trial. Cytomegalovirus shedding and delayed sensorineural hearing loss: results from longitudinal follow-up of children with congenital infection.
Order tizanidine 2 mg otc
Rarely pain treatment for dogs with cancer discount 2mg tizanidine mastercard, the transverse sinus is severely hypoplastic and the contralateral transverse sinus is absent. In such cases, the superior sagittal and straight sinuses can both drain via an enlarged occipital sinus into the superior jugular bulbs. In the latter case, the superior sagittal sinus continued as a large occipital sinus that joined the marginal sinus and then the distal transverse sinuses at the jugular foramina. Hoople31 found that the jugular foramen usually was contracted and the sigmoid sinus was reduced or absent when this occurred. Knott22 described two instances of complete absence of the right transverse sinus with only a small venous channel terminating through the mastoid foramen. A case was reported in which the sigmoid sinus ended in a blind pouch and drained through the large mastoid foramen. Furstenberg34 described a variation in the "lateral sinus" in which it was located in the soft tissues completely outside the skull. Overlapping lambdoidal sutures in infants may result in septation of the transverse sinus, usually at the proximal end. Occasionally, the affected side is associated with the absence of the transverse sinus, sigmoid sinus, or both. To prevent intracranial hemorrhage, a combination of arterial and venous surgery, 44 Anatomy, Imaging and Surgery of the Intracranial Dural Venous Sinuses be accessed, the transverse or sigmoid sinus often is ligated. Venograms have been reviewed to identify relative tumor locations and the drainage patterns of the confluence of sinuses. Stimulation of the superior surface of the transverse sinus resulted in orbital and supraorbital pain. Considering that the width of the proximal transverse sinus is 6 mm on average, the first and most superior burr hole in the midline infratentorial supracerebellar approach can be placed safely approximately 1 cm below the inferior nuchal line. Longitudinal changes in the ductus venosus, cerebral transverse sinus and cardiotocogram in fetal growth restriction. Color Doppler study of the venous circulation in the fetal brain and hemodynamic study of the cerebral transverse sinus. Cerebral dural arteriovenous fistulas: clinical and angiographic correlation with a revised classification of venous drainage. Early rebleeding from intracranial dural arteriovenous fistulas: report of 20 cases and review of the literature. Intraarterial and intravenous treatment of transverse/sigmoid sinus dural arteriovenous fistulas. Comparison of the infratentorial and transtentorial approaches to the pineal region. Quantitative anatomy of the occiput and the biomechanics of occipital screw fixation. Inconstant veins that drain into the sigmoid sinus include veins from the pons and medulla oblongata. The sigmoid sinus has anastomoses with the mastoid emissary and condylar emissary veins routinely. This probably is attributable to the difference in cranial size base between the sexes. When comparing either side, regardless of cranial width, the sigmoid sinus on the right side protrudes deeper, covering a greater cross-sectional area, and is situated more laterally. The asterion is the convergence point of the lambdoid, occipitomastoid, and parietomastoid sutures and is used because it overlays the region of the transverse-sigmoid junction. However, many authors have found that the asterion is not a useful landmark because of its anatomic variability as well as the difficulty of identifying it. Of note, when reading the older literature, some writers use the term lateral sinus to describe the combined sigmoid and transverse sinuses. At the very beginning of the fetal stage, when the embryo is still 40 mm, changes occur in the configuration of the sinuses that establish many of the morphologic features that are present in the adult brain. By the 60-mm and 80-mm stages, with the development of the cerebral hemispheres and the subsequent caudal swing of the transverse sinus, the caudal end of the tentorial sinus migrates cranially and ventrally toward the junction between the sigmoid and transverse sinuses. Note the relationships of the jugular foramen as well as the sigmoid and inferior petrosal sinuses. Its original course is across the cavum epiptericum, but as the epiptericum decreases in size, it attaches to the margin of the tentorium cerebelli. This has been reported in association with the underdevelopment of the petrous part of the temporal bone. These luminal outpouches may lead to erosion into the internal acoustic meatus and cause tinnitus and sensorineural hearing loss. This occurs through the formation of two channels separated by a bony ridge or fibrous septum. Some modalities are more useful than are others depending on 54 Anatomy, Imaging and Surgery of the Intracranial Dural Venous Sinuses Wang et al. These two have been found to be the main culprits in pulsatile tinnitus, which occurs secondary to malformation of the vascular structures near the ear. These vibrations can resonate with the adjacent mastoid air cells and then be transmitted to the ear. A diverticulum of the sigmoid sinus forms when the sinus erodes into the adjacent mastoid cells. A sigmoid sinus wall dehiscence is a defect of the mastoid part of the temporal bone at the area covering the sigmoid sinus, in which the mastoid cells enclose and constrict the sinus. The increased prevalence in women was attributed to a change in their hormonal balance as they age. Typically, these tumors are attached to the dura and composed of a sheetlike growth pattern circumscribed well, prominent nucleoli, and potentially, psammoma bodies. Psammoma bodies are concentric lamellated calcifications that may be present in some, but not all, meningiomas. Streeter20 speculated that this disease may have been secondary to the enlargement of intradural arteriovenous shunts that may have occurred during embryonic development. In each of the patients, all that remained of the sinus postsurgery was a small stump on the retrosigmoid sinus portion. They also stated that development might be secondary to late sinus hypertension following resection of the sigmoid sinus. Lastly, with skull base fractures, involvement of the sigmoid sinus can result in subcutaneous bleeding over the mastoid region, i. Second, the soft tissue is dissected by incising the deep cervical fascia and nuchal musculature to expose the cranium better. Each surgeon has his or her own preferred technique for drilling during a craniotomy. Sundt and Piepgras24 stated that the air drill should be held at a 30-degree angle vertical to the bone, as it allows better visualization. Once the sinus is exposed, and adequate hemostasis is achieved, the sinus can be ligated. Once this is accomplished, the medial part of the sinus can be closed with a running suture. The surgical technique described in their study involved obliteration of the draining vein with bipolar cauterization or clip ligation. Before transecting the sinus, the sinus pressure is assessed by clamping it to evaluate contralateral venous drainage. If the pressure is greater than 10 mm Hg after it has been clamped for 30 min, then the sinus should not be ligated. By drilling between these two landmarks, one can expose the entire lateral border of the sigmoid better and decrease the risk of damaging the sinus wall. A craniectomy should be considered for complex lesions, such as those with significant dural and osseous feeders. When a meningioma occludes a venous sinus completely, a gross, total resection of the intravascular portion usually is the technique preferred.
Strophanthi Kombe Semen (Strophanthus). Tizanidine.
- Are there safety concerns?
- Artery disease, heart problems, high blood pressure, and stomach problems.
- How does Strophanthus work?
- Are there any interactions with medications?
- What is Strophanthus?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96254
Cheap tizanidine 2 mg on line
The technique for placement of shaped highly cohesive gel devices depends on the ability to place the device with correct orientation into the tissue pocket treatment guidelines for neuropathic pain order tizanidine 2mg. After initial placement, orientation is confirmed with the aid of a fiberoptic retractor. The specific technique is dependent on the exact device used and the aids for orientation present. The device is then vertically lowered into the tissue pocket, confirmed by sitting the patient at 45- and 80-degree positions. Once the correct vertical position of the device is confirmed, the orientation is reconfirmed. This must be balanced with strict avoidance of any degree of overdissection of the implant pocket, particularly at the area of the inframammary fold, since repair of such an error may not be possible using a transaxillary incision. Shaped implants should not be used unless there is a strong comfort level in the ability to create a precise tissue pocket with the transaxillary endoscopic approach. Additionally, important device differences exist in the thickness of the highly cohesive gel between manufacturers that may make some devices more likely to rupture during placement using this technique. The inframammary folds are reinforced using two layers of one-inch foam tape, followed by a pressure dressing (Video 9. This pressure dressing is used to hold the implants in place and to maintain a pressure effect over the axillary incision areas and the superior aspect of the tissue tunnels used for implant placement on either side. This dressing is maintained for 1 to 2 days, and is then replaced with a bra, often in combination with an elastic wrap, to maintain implant position in the early postoperative phase. The important difference with the transaxillary approach, when compared with the inframammary approach, is that pressure must be maintained in the upper pole over the breast implant to prevent early movement of the implants into the tissue tunnel used for device placement. This is the issue that can lead to superior device malposition despite a correctly created tissue pocket. Subsequent management is essentially that of any postoperative breast augmentation patient. The technique shown in this patient entailed an angled incision, the inframammary fold was lowered, and high-profile smooth silicone gel implants were used. Additional information about the technique and its most recent modifications can also be found in the recent literature. The procedure for placement of silicone gel implants using a transaxillary endoscopic approach is shown in Videos 9. Transaxillary breast augmentation - Live Surgery Video, 49th Annual Baker Gordon Symposium on Cosmetic Surgery. Technical nuance in transaxillary breast augmentation with textured implantsLecture Video, 49th Annual Baker Gordon Symposium on Cosmetic Surgery. The ptosis is treated with periareolar ressection of the skin, providing the final scar around the areola in an upper position. The goal of this approach is to choose the minor ptosis and explain to the patient the possibility of a lower pole overprojection instead of extense scars. Round block suture is important to maintain the scar and the areolar with the better result aesthetically. Periareolar and vertical techniques for mastopexy were developed to minimize scars in minor ptosis cases. The site must not be arbitrarily based on the preferences of the surgeon and the patient, but must ensure adequate tissue covering, thus minimizing short- and long-term risks. Circumareolar incisions in breast augmentation surgery can center slightly low areolas on the breast mound and treat minor to moderate ptosis. This maneuver, however, is limited to moderate cases because it does not achieve huge lifting of the breast. The conflicting goals of mastopexy and breast augmentation, one that reduces and one that fills it up, lead to additional risks of breast augmentation and mastopexy and magnifies them. Periareolar mastopexy is mostly indicated to younger patients with good skin thickness and elasticity. The best candidates for mastopexy and augmentation are the worst candidates for mastopexy or breast reduction alone because the shape is discoid and the skin is very loose and distensible. Footprint of breast tissue is marked all over the breast to settle undermine limits. The ideal size and shape of the female breast is inherently subjective and relates to both personal preference and to cultural norms. The distance from the sternal notch to the nipple should be in a range of 17 to 19 cm and it is influenced by height, breast, and body type. Thereafter, dissection of breast tissue is initiated in the lower half area between the skin and the areola, parallel to lactiferous ducts avoiding to cut them, toward until the chest wall. A round incision is made, followed by de-epithelization of a pre-marked donut-shape area. It should be noted, however, that the eye perceives percentage differences in volume, so that even by adding the same volume to both breasts, the perceived postoperative asymmetry will be less. If a larger implant is used, one should be very conservative, because switching the side that is larger will be more noticeable to the patient. The pocket is irrigated with an antibiotic solution (saline, gentamicin, cefazoline), as well as implant inside its box. Surgeon changes gloves and washes them with antibiotic solution before touching the implants. Passing through the deep dermis of the outer skin and the areolar deep tissue, the suture takes small amount 124 10. In secondary mammaplasty, all skin markings are as in primary mammaplasty, aiming to remove excess skin and ptosis. At the procedure, after periareolar de-epithelization, we undermine until anterior implant capsule and then above it, as far as implant limits. Capsular 125 Periareolar Mastopexy Augmentation implant is opening and implant is removing, with anterior capsule resection. New implant pocket is undermined under posterior capsule, keeping some pectoralis major muscle fibers attached to it, and it reaches breast footprints made before surgery, passing through capsular contracture limits. The implant is placed into the pocket after rigorous hemostasis and antibiotic solution instillation. This pocket is not completely closed to avoid implant flatness and loss of projection. It is sutured to breast tissue to obtain coverage and to avoid subglandular implant migration. In submuscular secondary mammaplasty cases with capsular contracture, a new subfascial pocket is created to change implant placement. A periareolar technique is the first choice to avoid bigger scars in the first- and second-degree breast ptosis since implant will elevate the breast, resulting in less excess skin. In cases with surplus lax skin, it is necessary to do vertical or T-inverted incisions, even in revision cases which ideal results were not achieved. A mastopexy or reduction without an augmentation often lacks projection and desired volume and does not tend to hold its shape over time. By employing an implant when performing a mastopexy and augmentation, a predictable and safe result, with a minimized risk, can be achieved. The shape of the skin to be excised is typically not perfectly round and concentric but may be more oval and excentric so as to lift the nipple and not overly narrow the width of the breast. It is important to do the areola tattooing in cardinal points before the incision. This way, proper parameters are maintained and suitable areola spread is achieved in the end of the surgery. Round block suture with nonabsorbable stitches (colorless nylon because Gore-Tex is not available in Brazil) is done as Denis Hammond technique. Eight cardinal points guide areola spread and the suture take greater amounts of tissue at external border just in marked points and lesser bites of tissue between marked points in the areola edge. The round, block suture starts and ends at lateral-lower part of the areola, leaving the notch always at the same spot. When patient complains about feeling the suture, after 1 year it is removed at the office with local anesthesia.
Purchase online tizanidine
Other complications specifically of the graft such as infection and even its cost must be considered swedish edmonds pain treatment center order tizanidine 2 mg line. Technically, it is easy to place the graft too tight if it is sewn in without a sizer under it; however, with the sizer under it, it is often difficult to see where to put the sutures, and even the sizer can be easily damaged. Pearls Because the graft material is expensive, it is tempting to order a smaller piece. But be sure to have larger pieces on hand in case the muscle is pulled higher than you had anticipated preoperatively. Document clearly preoperatively that the patient understands that there will remain some postoperative animation and that she preferred this to creation of a submammary pocket. Some surgeons prefer a smooth implant that will be malleable and mobile underneath the contracting muscle. Others prefer a textured implant, particularly a highly cohesive one with an aggressively textured surface, so that it stays in place and mostly resists the deforming effects of muscle contracture. Bilateral medial and lateral capsular flaps were performed in this patient with Galaflex supporting the medial, lateral and inframammary folds. Strock Summary the concept of breast augmentation as a Process is helpful both as a means to present breast augmentation to patients and as a guide for management to optimize results. The Process of breast augmentation is the most powerful concept in the specialty to practice this discipline at its highest level. All patients must understand that participation in postoperative routines is a critical element for a successful outcome, as each postoperative visit is an opportunity for refinement and improvement of a result. The authors found that most patients appreciate that breast augmentation is presented in this way, as the passion for great results and teamwork needed to get there are readily apparent. It is also important to keep in mind that this is the fourth and final subprocess for the process of breast augmentation. Postoperative regimen and ultimately the patient experience can be virtually fully defined through the first three subprocesses (patient education, tissue-based planning, and refined surgical technique with fast-track 24-hour recovery) with the actual postoperative management occurring in seemingly passive fashion. Discussing postoperative management in general can be a difficult task, as there are many different concepts used in the postoperative management of a breast augmentation patient. Nevertheless, certain concepts hold true of all postoperative management regimens regardless of the details. This article offers suggested routines for the procedure types detailed in Chapters 7 through 10. The regimen discussed herein has been utilized by multiple surgeons with verifiable, peer-reviewed published outcome data. Use 191 Postoperative Management of postoperative drains is certainly surgeon dependent; however, with use of the techniques described in this book, including a precise bloodless dissection, postoperative drains have not been found to be necessary in primary augmentation, and it is universally known that patients despise having drains. Therefore, avoiding drains postoperatively has been a major benefit in the overall patient experience. Patients should not use special bras, straps, drains, pain pumps, or any other device or tactic to decrease pain, as these tend to slow recovery. In multiple peer-reviewed published series, narcotics have been eliminated from the routine postoperative phase with excellent results. Pain pumps have been developed; however, these have not been found to add an additional level of analgesia but certainly add cost and a hassle factor to the recovery phase. Exparel (liposomal bound bupivacaine) has proven effective for postoperative pain control; however, it is quite expensive and given the process for fast-track 24-hour recovery it is not cost-effective for breast augmentation. Patients are instructed to avoid sedentary behavior the first 2 to 3 days postoperatively. It is recommended that patients go out shopping and to dinner on the day of surgery, and this is important to prevent patients from not being active during window of recovery that lasts for approximately 6 to 8 hours after a breast augmentation. Following a breast augmentation, patients have 6 to 8 hours to resume normal light activities of daily living before they become extremely stiff and sore and it becomes excessively hard to get back to these activities. For this reason, the instructions to resume light activities with specific light arm raises immediately following the surgery are extremely useful to maintain the patient in this window of recovery. It is also important to have at least one phone call postoperatively to make sure the patient is following the instructions and has no questions. The timing of this call should be following the 2-hour nap and should ensure that the patient is on a normal course. Scar massage to follow up to 1 y postoperatively Not required, provided and may be used per patient preference. On arrival home, 2-h nap and then out of bed into hot shower for 20 min and get dressed. Prescribed arm raises completed five times every hour while awake for the next 5 days Commence aerobic activity at 2 wk; Noon chest weights at 4 wk; chest sit-ups at 6 wk Bra Activity Exercise 192 14. Other postoperative management points include the use of a bra, which has been found to be optional. With an atraumatic precise pocket dissection as described in preceding chapters, a bra may be worn if the patient desires. A tight-fitting bra may be useful in the cases where an overdissection of the pocket has been identified. Implant 195 Postoperative Management displacement would not be recommended for textured devices, most notably shaped implants. The follow-up intervals are also defined and should be fairly frequent for the first year postoperatively. Most problems with breast augmentation may be identified within the first year postoperatively, and it is important to closely monitor and address these problems should they arise. Scar therapy routines include use of silicone back strips, Band-Aid gel strips, Mepiform, and scar massage. The concepts for postoperative care following this procedure have much in common with those listed previously for the inframammary approach. A critical difference, however, between the transaxillary and inframammary approaches is that the transaxillary approach creates a space from the axilla to the upper edge of the breast implant, used for dissection access and implant placement, that is not needed after the implant is placed. This issue is routinely addressed by placement of a tight dressing intraoperatively that maintains pressure on the axillary access and upper pole areas, and serves to stabilize implant position. This dressing is removed at the initial postoperative visit, 1 or 2 days after the procedure. Following removal of the pressure dressing, the patient is placed in a flexible bra to maintain some support of the inframammary fold area, in addition to an elastic wrap to maintain light pressure on the axillary and upper pole areas. The patient is then fitted with an under-wire bra that provides tight support of the inframammary fold area and minimizes early implant movement. This bra is worn in daytime hours at all times, with continuation of the flexible bra when sleeping at night, until 8 weeks postoperatively. Pressure dressing applied intraoperatively, removed 1 to 2 d following procedure Patient placed in combination of flexible bra and elastic wrap for a period between 2 to 3 d and 2 wk. Patient is then fitted with tight-fitting bra that is used daily, with the initial flexible bra used at night when sleeping, until 8 wk postoperatively. Specific instructions for bra support with exercise are given at the 2-wk postoperative visit Patient is encouraged to minimize significant upper arm and shoulder movement for 5 days, with ice applied to the inferior lateral breast areas as needed. Aerobic exercise with limited arm movement such as recumbent bike is allowed after 7 d. Full activity is encouraged after 2 wk, except for major arm/shoulderbased weight lifting, which is discouraged until after 3 wk postoperatively. The authors suggest that major upper arm and shoulder movements are minimized until after the initial 5-day period. The patient may go out to dinner as tolerated during the first day or two after surgery. After 1 week, they are encouraged to resume specific aerobic activities such as a recumbent bike, where there is limited impact or major arm motion. After a second week, patients may resume all activities but are discouraged from resumption of heavy lifting or upper arm/shoulder-based weight lifting until after the third week. As discussed earlier, an important issue that contributes to quick surgical recovery and early resumption of normal activity relates to precise surgical technique that minimizes the need for narcotics following the procedure. The limitation of blunt dissection and use of nonsteroidal anti-inflammatory agents both immediately preoperatively and postoperatively have also helped greatly lessen the need for narcotic pain medications.
Buy tizanidine 2 mg
For detecting salt pain treatment for osteoporosis order 2mg tizanidine mastercard, sensory cells with a sodium channel depolarize when sodium enters them. The positively charged protons cause membrane depolarization when they enter the cell and set off an action potential. Smell the sense of smell, known as olfaction, is enormously important to animals- not just for enjoying food, but also for warning of danger and even selecting mates. It occurs as a result of the binding of odorant molecules to olfactory receptor cells in the nasal cavity. A second one is located where the roof of the mouth connects the throat to the nose. Chewing food releases odorants that can travel the second path to the olfactory receptors. Mucus-a viscous fluid full of glycoproteins called mucins-covers the lining of the nose, the nasal epithelium, and serves as both a solvent for odorant molecules and an important protection against infection, because nasal neurons connect directly to the brain. But each receptor can bind several different odorants-some weakly and others more tightly. A particular odorant may bind more than one kind of receptor, again with different affinities. These combinations give humans the ability to distinguish many more than 350 smells. In fact, a 2014 study put the number of smells humans can tell apart at one trillion. Lecture 23 the Biochemistry of Our Senses 237 Mammals have about 1000 to 1500 olfactory receptor genes. In humans, only about 350 of them make active receptors, but rats have almost 1500 genes that make active olfactory receptors. The sense of smell may play a role in the choice of sexual partners, even in humans. Children of such couples might have a more robust immune system, which would give them an evolutionary advantage. Vision the detection of light and the ability to distinguish detail by our eyes involves an amazing convergence of optics, lightsensitive proteins, nerve signaling, and brain processing. About 130 million photoreceptors in the retina absorb light and transmit visual signals to the brain. The anatomy of the eye is such that light passes through the cornea, pupil, and lens, where it is refracted and focused onto the retina at the back of the eyeball. The retina is the location of photoreceptor cells, which contain proteins called opsins that detect light. This is similar to the taste receptors for sweet, bitter, and umami; the distinctive feature of opsins is that they hold a molecule of vitamin A that gets altered when exposed to light. Biochemistry and Molecular Biology Thanks to opsins, photoreceptor cells detect light and pass signals on to other neurons, called ganglion cells. The axons of the ganglion cells are bundled into the optic nerve, which ultimately routes the information back to the visual cortex in the brain to process the signals and tell us what we are seeing. There are 2 types of retinal photoreceptor cells involved in light detection: rods and cones. They provide little color information, because they are optimized to detect things in very dim light. But what rod cells lose in color detection, they gain in sensitivity; a rod cell can detect a single photon of light. Humans have 3 types of cone cells, each specialized to absorb wavelengths corresponding to red, green, or blue. Though damage to any of the sets of cones is possible, the most common type of color blindness is redgreen color blindness, and it results from the lack of either a red or a green opsin. Lecture 23 the Biochemistry of Our Senses 239 Genes encoding the opsins are on the X chromosome. Human males have only one X chromosome, while females have 2, so the loss of coding for an opsin on its single X is a bigger deal for men than for women. People with normal hearing can detect sounds of pitches, or frequencies, between 20 and 20,000 hertz. Normal, everyday speech has a mix of low and highfrequency sounds that is generally in the 250 to 6000 hertz range. The length of time it takes our nervous system to respond to a sound signal is on the order of tens of microseconds. Sound detection occurs when tiny hair cells called stereocilia move on the membrane of an ear structure called the cochlea. Each of the stereocilia is attached to an adjacent one by a filament that controls the opening of an ion channel. And when this happens, the upanddown motion of the basilar membrane sets up sidetoside movement of the fluid between the basilar membrane and the tectorial membrane. The sensitivity of the mechanism is astounding: Movements as small as 1/2 the diameter of an atom can be detected. Hearing loss is complex, but one thing that commonly happens is damage to the hair cells of the inner ear-whether due to age, infection, or exposure to loud noises. Cells responding to high frequencies are located in the lower cochlea and are among the most easily damaged, thus explaining why highfrequency hearing loss is A 2016 report shows that men usually the first to occur. Touch stimuli can be mechanical signals, where lowthreshold mechanoreceptors sense contact with the skin. Lowthreshold mechanoreceptors detect pressure, vibration, stretching of the skin, and movement of hair follicles in the skin. These receptors respond by triggering action potentials and communicate with sensory neurons to send information to the brain. For example, the "taste" of a meal is actually made by combining information from smell receptors, taste buds, and even texture or touch. Lecture 23 the Biochemistry of Our Senses 241 Although you might not expect it, the sense of touch is responsible for your ability to "taste" spicy foods One of the prime functions of the sense of touch is to help us distinguish innocuous stimuli from harmful ones. Pain receptors that detect dangerous stimuli and signal the spinal cord and brain are called nociceptors, related to the word noxious. These pain receptors respond to mechanical, thermal, or chemical stimuli that are outside the range that is innocuous and alert the brain to tissue damage. Nociceptors for temperature are activated by dangerous heat or cold conditions with separate sensing cells for each. These are abnormal situations, and the ion channels involved signal the abnormality by opening and causing membranes to depolarize. How does this reconcile with what you learned previously about reactive oxygen species There is a whole world of examples where your biochemical knowledge can help you understand what is going on below the surface. And researchers are constantly uncovering new mechanisms and molecular events that impact our lives and enrich our views of the natural world. These are accessible to you now that you have a wide understanding of biochemistry. Caffeine When you wake up in the morning, your body has already been preparing for the day. Levels of your fastacting stress hormones epinephrine and norepinephrine are rising, your sloweracting cortisol is getting into the act, and your body is getting primed for action. So, you grab a cup of coffee, and your cells set in motion the pathway that will result in glycogen breakdown and release of glucose. While the buzz from caffeine is fairly innocuous, the buzz from other foods and drinks-especially items containing highfructose corn syrup-is not. There are 2 issues to keep in mind: the overconsumption of sugar in general and the effects of high levels of fructose on the metabolism of sugars. It has the same number of calories as glucose, and phosphorylated forms of them get interconverted in glycolysis and gluconeogenesis. The first difference between the metabolism of glucose and fructose is in the tissues that metabolize them. So, if glucose is converted to fructose 6phosphate in glycolysis, how could fructose be a problem The answer is that fructose has an alternate entry pathway to glycolysis in the liver. Regardless of whether these molecules were made from glucose or fructose, they will, beyond this point, be broken down to pyruvate, which will feed the citric acid cycle. So, the alternate fructose pathway is bypassing 2 of the steps controlling glycolysis.

Order tizanidine 2mg line
Post-contrast T1-weighted magnetic resonance imaging showing a large pineal germinoma compressing the dorsal midbrain arizona pain treatment center phoenix az cheap 2 mg tizanidine with mastercard. Features of the dorsal midbrain syndrome can be present in certain neurodegenerative diseases. While the presence of hydrocephalus is a clear indicator of shunt malfunction, its absence does not exclude it; a dorsal midbrain syndrome can sometimes occur without hydrocephalus in the setting of shunt malfunction. Neuro-ophthalmic complications of raised intracranial pressure, hydrocephalus, and shunt malfunction. Rapid sequence magnetic resonance imaging in the assessment of children with hydrocephalus. Summary the process of breast augmentation is the key to optimizing outcome in breast augmentation. For many years, surgeons have thought about breast augmentation as a surgical procedure of putting an implant into the pocket; however, this encompasses only a part of the procedure. The process of breast augmentation practiced at the highest level incorporates the following four main steps: patient education, tissue-based preoperative planning, refined surgical technique with fast-track 24-hour recovery, and defined postoperative care. Unlike many other areas of surgery, the practice of breast augmentation has suffered from a lack of a defined process for patient management. This analysis has resulted in a redefinition of this procedure to a much broader process beyond the actual surgical placement of the implant. This concept of the process has also been powerful for surgeons, as they refine their execution of the procedure. The essential components include comprehensive patient education that enhances informed consent, tissue-based preoperative planning, refined surgical technique/rapid fast-track 24-hour recovery, and defined postoperative patient planning. Although each component may exist individually, the combination of these steps in succession has resulted in enhanced outcomes for patients that are far better than any one component practiced in isolation. In recent years, as key components of this process have been elucidated, it has been demonstrated that this concept and process approach is transferable and reproducible. Patients were required to complete documents prior to their education consult, which was performed either over the phone or in person by a patient education specialist, and for an average duration of 45 to 60 minutes. During the education consult, all concepts, issues, and nuances are directly addressed and discussed with the patient. The surgeon consultation is performed only after successful completion of the education consult. The tissue evaluation is based on previously published techniques (High Five), and more recently using the next-generation implant-specific selector tissue-based system following similar principles. Implant size, which is based on the predicted tissue-based optimal fill volume of the breast. In the past 5 years, the author has found that all patients except true body builders do exceptionally well with a properly performed dual-plane pocket. The implant size is based on a breast width and breast type (envelope compliance and preoperative fill). The implant type is based on discussion with the patient as well as simulation with three-dimensional (3D) imaging. The surgeon will emphasize the reality that the postoperative breasts will not "match," discuss the limitations of cleavage based on current intermammary distance, rationale for recommended pocket plane, and likelihood of implant palpability, particularly in the inferior and lateral parts of the breast. The author has found 3D imaging technology comprehensive consultation tool that has improved the consultation and communication. Sizers are not used and only two implants (and one back-up) are ordered for the case. All cases are performed under general anesthesia with short-acting full muscle paralysis, and patients are premedicated with celecoxib 400 mg. Implant pocket planes are created under direct vision with no blunt dissection using techniques to minimize tissue trauma. These are reinforced prior to the day of surgery and on the day of surgery, and verification of compliance as well as the ability of the patient to resume normal activities is determined following discharge of the patient home after surgery. The average implant size was 289 cm3 for the entire cohort and 302 and 276 cm3 for the saline and form-stable cohesive gel subcohorts, respectively. Follow-up, patient outcomes/reoperations, and complications are reported in Table 1. The educational component cannot be overemphasized, as this remains the most critical yet often neglected part of the process. Educate the patient on the practice philosophy and have the patient assume mutual responsibility that the implant will be selected based on her chosen preferences and in accordance with her breast dimensions and tissue or alternative methods recognizing the trade-offs. The tissue-based preoperative planning allows the surgeon to get "on base" and prevents the patient from striking out on her first try. The High Five process is one of two published and peer-reviewed tissue-based systems in the literature. Also cogent is the artist versus the engineer issue, and who should pick the breast implant size, the patient or the doctor. No doubt much of plastic 7 the Process of Breast Augmentation surgery is both art and science; however, art in itself is truly unstructured and without definable boundaries. The notion that instituting a process-oriented approach will obstruct the "skills of the artist" is a misconception. Formerly the surgical technique was often the only part of a breast augmentation that many surgeons considered. Surgical advances have currently not only enhanced the actual surgical procedure but clearly defined the importance of the educational and tissue-based planning portion of the process, as these allow surgeons to make nearly every decision before entering the operating room. This not only allows surgeons to make better decisions than have historically been made in the operating room (particularly implant size) but also allows the surgical procedure to proceed as efficiently as possible. The concept of a very precise, atraumatic dissection with prospective hemostasis (identifying/controlling vessels/perforators under direct vision before they bleed) allows for both breast pockets to be typically dissected in a total time of typically less than 10 minutes. Not only does this immensely reduce the amount of tissue trauma but also the use of intraoperative narcotics, additional paralytics, and need for reversing agents, all of which slow postoperative recovery. Although the use of an appropriate breast pocket irrigation has been widely accepted,8,11,12 surgeons often inadvertently ignore other potential points of periprosthetic contamination, including handling implants without clean gloves or contact of the implant with the surgical site components. These practices do not fit with this refined surgical process and should be avoided to minimize complications, including capsular contracture and reoperation. Interestingly, a fringe benefit/by-product of this refined surgical process is recovery, the second best indicator of the quality of the procedure delivered (reoperation rate being the first). In fact, the recovery benefit is truly a favorable by-product of the whole process. This report and others have documented full return to normal activities within 24 hours using this process. We have also demonstrated this process and fast-track/24-hour recovery in eight live surgeries from 2008 to 2016. Surgeons/patients and medical personnel are often skeptical about the feasibility of fast-track/24-hour recovery. The process is often modified based on personal biases of various surgeons, but as discussed earlier, a process functions only if it is completed in proper order and procedure. Other adjuncts added to the process such as injectables, drains, pain pumps, straps, special bras, narcotics, and limitation of arm movements all detract from the goal of speeding the recovery. There were no patients who underwent a reoperation in either cohort for request for size exchange.
Purchase 2 mg tizanidine visa
Spectrum of disease and outcome in children with symptomatic congenital cytomegalovirus infection pacific pain treatment center victoria bc buy tizanidine 2 mg with amex. Outcome of symptomatic congenital cytomegalovirus infection: results of long-term longitudinal follow-up. Ten-year clinical, developmental, and intellectual follow-up of children with congenital cytomegalovirus infection without neurologic symptoms at one year of age. Congenital and postnatally acquired cytomegalovirus infections: long-term follow-up. Auditory and visual defects resulting from symptomatic and subclinical congenital cytomegaloviral and toxoplasma infections. Intellectual development in school-aged children with asymptomatic congenital cytomegalovirus infection. Progressive and fluctuating sensorineural hearing loss in children with asymptomatic congenital cytomegalovirus infection. The outcome of congenital cytomegalovirus infection in relation to maternal antibody status. Prenatal diagnosis of human cytomegalovirus by culture and polymerase chain reaction: 98 pregnancies leading to congenital infection. Development of a vaccine against mental retardation caused by cytomegalovirus infection in utero. Prevention of congenital cytomegalovirus complications by maternal and neonatal treatments: a systematic review. Early treatment with ganciclovir to prevent cytomegalovirus disease after allogeneic bone marrow transplantation. Mortality in patients with the acquired immunodeficiency syndrome treated with either foscarnet or ganciclovir for cytomegalovirus retinitis. Selecting neonates with congenital cytomegalovirus infection for ganciclovir therapy. Effect on hearing of ganciclovir therapy for asymptomatic congenital cytomegalovirus infection: four to 10 year follow up. Feasibility of neonatal screening for toxoplasma infection in the absence of prenatal treatment. Neonatal serologic screening and early treatment for congenital Toxoplasma gondii infection. Cord blood screening for congenital toxoplasmosis in northwestern Switzerland, 1982-1999. Mother-to-child transmission of toxoplasmosis: risk estimates for clinical counselling. Congenital toxoplasma infection: monthly prenatal screening decreases transmission rate and improves clinical outcome at age 3 years. Fetal toxoplasmosis: outcome of preganancy and infant follow-up after in utero treatment. Association between congenital toxoplasmosis and preterm birth, low birthweight and small for gestational age birth. Development of adverse sequelae in children born with subclinical congenital Toxoplasma infection. Repeated isolation of toxoplasma from the cerebrospinal fluid and from the blood, and the antibody response in four cases of congenital toxoplasmosis. Accuracy of real-time polymerase chain reaction for Toxoplasma gondii in amniotic fluid. Polymerase chain reaction in cerebrospinal fluid for the diagnosis of congenital toxoplasmosis. Diagnosis of congenital toxoplasmosis in the neonatal period: a multicenter evaluation. Recognition of different Toxoplasma antigens by IgM and IgG antibodies in mothers and their congenitally infected newborns. Usefulness of Western blot in serological follow-up of newborns suspected of congenital toxoplasmosis. Evaluation of a commercial IgG/ IgM Western blot assay for early postnatal diagnosis of congenital toxoplasmosis. Intellectual deficits in children born with subclinical congenital toxoplasmosis: a preliminary report. Detection of congenital toxoplasmosis by chorionic villus sampling and early amniocentesis. Prenatal diagnosis of congenital toxoplasmosis: a multicenter evaluation of different diagnostic parameters. Outcome of treatment for congenital toxoplasmosis, 1981-2004: the National Collaborative Chicago-Based, Congenital Toxoplasmosis Study. Synergistic effect of sulfadiazine and daraprim against experimental toxoplasmosis in the mouse. Effect of pyrimethamine and sulfadiazine on the fine structure and multiplication of Toxoplasma gondii in cell cultures. Report on missed opportunities and failed prevention policies among women of childbearing age. Global progress toward rubella and congenital rubella syndrome control and elimination-2000-2014. Congenital rubella syndrome: correlation of gestational age at time of maternal rubella with type of defect. Retardation of the myelo- and cytoarchitectonic maturation of the brain in the congenital rubella syndrome. Central auditory imperception: a significant factor in congenital rubella deafness. Final report of a prospective study of children whose mothers had rubella in early pregnancy. Lenticulostriate vasculopathy in infants with infections of the central nervous system sonographic and Doppler findings. The health and educational status of adolescents with congenital rubella syndrome. Growth in congenital rubella syndrome and correlation with clinical manifestations. Chronic progressive panencephalitis due to rubella virus simulating subacute sclerosing panencephalitis. Progress toward control of rubella and prevention of congenital rubella syndrome- worldwide, 2009. Neonatal herpes simplex virus infections in Canada: results of a 3-year national prospective study. Plasma and cerebrospinal fluid herpes simplex virus levels at diagnosis and outcome of neonatal infection. Effect of serologic status and cesarean delivery on transmission rates of herpes simplex virus from mother to infant. Trends in herpes simplex virus type 1 and type 2 seroprevalence in the United States. Seroprevalence of herpes simplex virus types 1 and 2 in pregnant women in the United States. Epidemiology, clinical presentation, and antibody response to primary infection with herpes simplex virus type 1 and type 2 in young women. Neonatal herpes simplex virus infection in relation to asymptomatic maternal infection at the time of labor. Neonatal herpes simplex meningoencephalitis associated with fetal monitor scalp electrodes. Neonatal herpes simplex: clinical findings and outcome in relation to type of maternal infection. Neonatal herpes simplex virus infection introduced by fetal-monitor scalp electrodes. Low risk of herpes simplex virus infections in neonates exposed to the virus at the time of vaginal delivery to mothers with recurrent genital herpes simplex virus infections. Congenital malformation of the central nervous system associated with genital type (type 2) herpesvirus. A report of three cases and review of intrauterine herpes simplex virus infection. Postnatal acquisition of herpes simplex virus by the newborn infant: a review of the literature.