Discount lincocin 500mg with mastercard
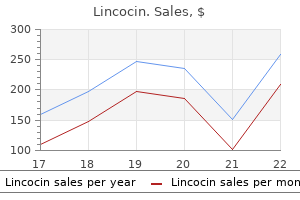
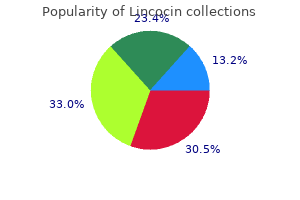
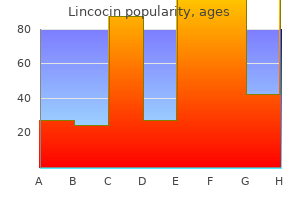
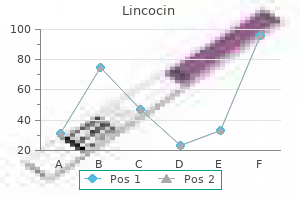
Acrodermatitis continua demonstrating acral pustule formation and subungual lakes of pus with destruction of the nail plate medicine zebra lincocin 500 mg mastercard. Potent or superpotent topical steroids, preferentially under occlusion, are useful in blocking pustulation. The therapeutic result lasts as long as the drugs are given, and relapses occur after withdrawal. The disease may remain confined to the original site, sometimes up to several years, but more often it spreads proximally to cover the hand, dorsum of forearm, or foot. Acrodermatitis continua may be associated with generalized pustular psoriasis of the Zumbusch type (see Chapter 18). The main histopathologic feature of acrodermatitis continua is a subcorneal cavity filled with neutrophils. Epidermal cell necrosis and spongiosis does not occur, but the roof and shoulder zones adjacent to the pustule show aggregated leukocytes between the epidermal cells, forming spongiform pustules. There is a moderate lymphohistiocytic infiltrate in the upper dermis, together with focal edema. Lesions of long duration show severe atrophy of the papillary dermis and thinning of the epidermis. Systemic abnormalities are absent, and laboratory tests are usually within normal ranges. In advanced cases, X-ray may reveal atrophy of the distal phalanx and arthropathy of the interphalangeal joints. Michaelsson G et al: the psoriasis variant palmoplantar pustulosis can be improved after cessation of smoking. Koshiba S et al: Tonsillar crypt epithelium of palmoplantar pustulosis secretes interleukin-6 to support B-cell development via p63/p73 transcription factors. Dermatology 220:154-158, 2010 4 Chapter 22 Chapter 22:: Seborrheic Dermatitis:: Chris D. It is characterized by sharply demarcated, yellow to red to brown, greasy or bran-like scaling patches and plaques. Flares occur when sebaceous glands are most active (first few months of life, and post puberty). The etiology is unclear but there are associations with Malassezia yeasts, sebum secretion and composition, and certain drugs. Severe forms are also seen with immunosupression in premature infants and congestive heart failure patients. A higher incidence of seborrheic dermatitis is also seen in patients with alcoholism and endocrinologic diseases that lead to obesity. It is characteristically found in regions of the body with high concentrations of sebaceous follicles and active sebaceous glands including the face, scalp, ears, upper trunk, and flexures (inguinal, inframammary, and axillary). A male predominance is seen in all ages, without any racial predilection, or horizontal transmission. On the other hand, some patients with elevated sebum levels may not have seborrheic dermatitis either. Both Malassezia species and the resident flora Propionobacterium acnes have lipase activity resulting in transformation of triglycerides into free fatty acids. The free fatty acids and reactive oxygen radicals produced in turn have antibacterial activity that alters the normal skin flora. Some authors believe this disturbance in flora, lipase activity, and free oxygen radicals may be more closely linked to seborrheic dermatitis than an altered immune response. Although some patients may have cultures showing Candida albicans, Staphylococcus aureus, Propionobacterium acnes, and other aerobic bacteria, none have been linked to the pathogenesis of seborrheic dermatitis. The pathogenic role of Malassezia furfur (previously known as Pityrosporum ovale) is also controversial. The number of yeasts on the skin does not directly correlate with the severity of seborrheic dermatitis also. Patients with both dandruff and seborrheic dermatitis generally have abundant yeast counts when compared to controls supporting the role of yeast in the disease. A higher rate of seborrheic dermatitis is also seen in patients with Pityrosporum folliculitis and tinea versicolor. Malassezia species also play a role in the inflammatory response with stimulation of the alternative complement pathway. Malassezia can lead to inflammation on the skin from metabolic products produced and complement activation via the direct and alternative pathways. The presence or imbalance of microbial number of different cytostatic medications such as azeleic acid. There is no evidence to suggest infants with seborrheic dermatitis will have disease as adults. Patients with zinc deficiency (acrodermatitis enteropathica, and acrodermatitis enteropathica like conditions) may have an eruption that appears similar to seborrheic dermatitis and improves with zinc supplementation, while seborrheic dermatitis patients do not improve with zinc supplementation. But again, biotin supplementation has not been substantiated to improve seborrheic dermatitis. Lesions can be seen on the face, neck and can be disseminated to the trunk and extremities with inflammatory glistening plaques in intertriginous sites such as the axillae and groin. A differential diagnosis should be undertaken in any infant with a widespread form of seborrheic dermatitis (Box 22-1). Atopic dermatitis patients tend to have lesions on the forearms and shins, while sparing the axillae. This Israeli Jewish Moroccan family presented with an autosomal dominant seborrhea-like dermatosis. It tends to localize to the scalp, face, and presternal chest as seen with seborrheic dermatitis. However, the margins tend to be better defined, more erythematous and with thicker scales than those seen with seborrheic dermatitis. The biopsy can be indistinguishable from psoriasis, similar to the chronic form of seborrheic dermatitis. Widespread pattern of seborrheic dermatitis with psoriasiform lesions on the trunk and groin. Some authors believe that infantile seborrheic dermatitis is actually a variant of atopic dermatitis rather than a separate entity. Extensive involvement plus lesions on the palms and soles with severe pruritis suggests scabies. Infantile psoriasis can also be extensive, with erythematous plaques and scale, with less scale in intertriginous sites. The adult form on the other hand, tends to be chronic and can persist from the fourth through the seventh decades of life, with a peak at age 40. Other sites commonly involved include retroauricular regions, external auditory canal, auricle, and conchae bowl. Intertriginous sites such as axillary and inguinal regions show less scale and mimic intertrigo. Erythema and pruritis are common, as well as burning or tingling sensitivity reported as well, particularly on the scalp. Pityrosporum folliculitis can be seen as well with diffuse monomorphic tiny pustules and papules with peripheral erythema on the trunk. Prepubertal patients tend to not get seborrheic dermatitis because of this lack of androgen stimulation of sebaceous glands, and have also not been shown to have excessive colonization of Malessezia species. The hereditary form has been associated with deficiencies of complement C3, C5, and phagocyte malfunction therefore resulting in defective opsonization of bacteria. Patients with the hereditary form may necessitate treatment with fresh frozen plasma and whole blood to supplement these complement deficiencies. Pityriasis amiantacea was first described by Alibert in 1832, and is also known as asbestos scalp, tinea asbestina, keratosis follicularis amiantacea, and porrigo 263 4 plex chronicus can have patches of pityriasis amiantacea as well. Alopecia may result and is nonscarring unless secondary scalp infection occurs with Streptococcus or Staphylococcus and should be treated appropriately. Staphylococcal isolates in the matted hairs can be found in up to 96% of patients.
Diseases
- PHACE association
- Langer Nishino Yamaguchi syndrome
- Wiedemann-Rautenstrauch syndrome
- Microcephalic
- Aqueductal stenosis, X linked
- Retroperitoneal fibrosis
Buy generic lincocin online
Laboratory tests for the diagnosis of tuberculosis are histopathologic examination treatment narcissistic personality disorder cheap 500 mg lincocin free shipping, cultures, and a tuberculin skin test. Therapy consists of systemic antituberculous drugs and is best left to the specialist physician. Lupus Vulgaris rapidly coalesce and become necrotic, forming large, irregular vegetating, granulating, or ulcerating lesions. The differential diagnosis includes squamous cell carcinoma, lymphoma, systemic mycoses, and other granulomatous diseases. Histopathologic examination is essential in establishing the final diagnosis, along with radiographs. Leprosy Lupus vulgaris is the most common form of secondary tuberculosis of the skin. It is usually observed in persons with a moderate or high degree of tuberculin sensitivity. The skin lesions usually appear most frequently on the head and neck, followed by the extremities. The oral mucosa is rarely affected, either through extension of facial lesions or through lymphatic or hematogenous spread. Clinically, oral lesions begin as a collection of small red nodules that Leprosy is a chronic, contagious, systemic granulomatous disease, caused by Mycobacterium leprae. The disease is transmitted from person to person and has a long incubation period, ranging from 2 to 6 years. Leprosy involves mainly the peripheral nerves, the skin, the mucosa of the upper respiratory tract, and such other tissues as bones and viscera. Leprosy, by clinical, bacteriologic, immunologic, and histopathologic criteria, is classified as tuberculoid, lepromatous, borderline, and indeterminate. Oral manifestations appear usually in lepromatous leprosy and occur in 20 to 60 % of the cases. Clinically, oral lesions are manifested as multiple nodules (lepromas) that progress to necrosis and ulceration. The lesions are usually found on the soft and hard palate, uvula, dorsum of the tongue, lips, and gingiva. The differential diagnosis of oral lesions includes tertiary syphilis, cicatricial pemphigoid, lethal lymphomas, systemic midline granuloma, mycoses, traumatic lesions, and malignant neoplasms. Laboratory tests helpful in establishing the diagnosis are bacteriologic and histopathologic examinations, and the lepromin skin test. Dapsone is the cornerstone of therapy, but other medications, such as rifampin and clofazimine, are also useful. As the lesion progresses, multiple abscesses and draining sinuses form, usually on the skin of the face and upper neck. Yellow purulent material that represents colonies of Actinomyces (sulfur granules) may discharge from these sinuses. As the disease becomes chronic, healing of old lesions results in scar formation, but new abscesses and sinuses develop. Mandibular or maxillary involvement may be severe and usually is associated with trismus. The differential diagnosis includes tuberculosis, systemic mycoses, nocardiosis, dental and periodontal abscess, and other nonspecific infections. Laboratory tests to establish the diagnosis are direct bacteriologic examination and culture. Penicillin is the drug of choice, but erythromycin or tetracycline may be utilized in sensitive patients. Actinomycosis Actinomycosis is a chronic granulomatous infectious disease caused by the anaerobic Gram-positive bacterium Actinomyces israelii. There are three clinical forms of the disease: cervicofacial, thoracic, and abdominal. Cervicofacial actinomycosis is the most common form of the disease and oral manifestations are part of this form. It is assumed that oral actinomycosis occurs as an endogenous infection and that trauma in the oral cavity, such as wounds of the oral mucosa, tooth extraction, and fractures, is necessary to initiate the disease. In addition, open necrotic dental pulp may be the site of entrance of the bacterium. Fungal Infections Candidosis Candidosis is the most frequent fungal infection and is caused by Candida albicans, a fungus that is part of the normal oral flora in 20% to 50% of healthy persons. Recently a novel cofactor implicated in the pathogenesis of oral candidosis has been the host blood group secretor status. It has been recently suggested that oral candidosis should be classified as primary, comprising infections exclusively localized to the oral and perioral area, and secondary, comprising oral lesions of systemic mucocutaneous disease. Primary Oral Candidosis Primary oral candidosis includes the following clinical varieties. Pseudomembranous Candidosis Pseudomembranous candidosis is the most common form of the disease and is usually acute, but the chronic type may also occur. Clinically it is characterized by creamy white or whitish-yellow, slightly elevated spots or plaques, which usually can be easily detached, leaving a raw underlying reddish or normal surface. These lesions may be localized or generalized and may appear at any oral site, but more frequently on the buccal mucosa, the tongue, and the soft and hard palate. Erythematous Candidosis Papillary Hyperplasia of the Palate Erythematous (atrophic) candidosis is also classified as acute or chronic. Clinically, there are erythematous patches which have a predilection for the dorsal surface of the tongue. Nodular Candidosis Papillary hyperplasia of the palate is a rare chronic form of candidosis that usually affects persons with a high-arched palate who do not wear dentures. Clinically, multiple small spherical nodules appear on the palate, which is usually red. This lesion should not be confused with denture stomatitis, which appears in persons wearing dentures. Candida-associated Lesions Nodular candidosis (chronic hyperplastic/Candida leukoplakia) is a chronic form of candidosis that is characterized by deep infiltration of the oral tissues by fungal hyphae. Clinically, it is characterized by white, firm, and raised plaques occasionally surrounded by erythema. The lesions my persist for years, do not detach, and are usually located on the retrocommissural area, the dorsum of the tongue, the buccal mucosa, and rarely in other areas. It has been suggested that nodular candidosis predisposes to squamous cell carcinoma and is therefore a precancerous lesion. In this category three lesions are included: angular cheilitis, median rhomboid glossitis, and denture stomatitis. Angular cheilitis is a disease of multifactorial etiology, which may be infective or noninfective. Angular cheilitis is often associated with denture stomatitis, which is common among denture wearers. Clinically, it manifests as red, fissured crusts with or without erosion, occasionally covered by whitish-yellow spots or plaques. Clinically, it appears as a reddish smooth or nodular surface located on the midline of the dorsum of the tongue anterior to the circumvallate papillae. Denture stomatitis is usually associated with Candida infection and was referred to in the past as chronic atrophic candidosis. Clinically, it is characterized by a diffuse erythema and slight edema of the mucosa underneath the denture. Secondary Oral Candidosis Secondary oral candidosis includes the following two clinical varieties. Chronic Mucocutaneous Candidosis this form of candidosis is a heterogeneous group of clinical syndromes that are characterized by chronic lesions of the skin, nails, and mucosae. It usually appears in childhood and is often associated with numerous immunologic abnormalities, predominantly of cell-mediated immunity and rarely of humoral immunity. Clinically, the early oral lesions are similar to those seen in pseudomembranous candidosis, but later they are similar to the lesions of chronic hyperplastic (nodular) candidosis. Characteristically, the lesions are generalized, with a predilection for the buccal mucosa, commissures, tongue, palate, and lips, and may extend to the oropharynx and esophagus. Cutaneous and nail involvement in varying degrees of severity are associated with the oral lesions.
Purchase lincocin on line amex
It probably originates from primitive mesenchymal cells medicine 524 purchase 500mg lincocin with amex, such as endothelial cells. The clinical course of this form is indolent, but sometimes can be very aggressive, involving the viscera, but rarely the oral mucosa. The classic form is frequently located on the skin and seldom in other mucosae and internal organs. It affects men more often than women (ratio about 8: 1) 50 to 70 years of age and progresses slowly. Clinically, the skin lesions are characterized by multiple macules, plaques, nodules, and tumor lesions of purplish or dark blue color. The oral mucosa is occasionally affected, usually after the skin, but, although rarely, the disease can start from the mouth. Clinically, the oral lesions present as multiple or solitary red, brownreddish, soft, or ulcerated elevated plaques or tumors. They most frequently develop on the palate and gingiva, followed by the tongue, lips, and buccal mucosa. The differential diagnosis includes pyogenic granuloma, peripheral giant cell granuloma, hemangioma, hemangiopericytoma, hemangioendothelioma, pigmented nevi, and malignant melanoma. Radiotherapy, interferon-A, and chemotherapy or surgical excision in small localized lesions. Polymorphous Low-Grade Adenocarcinoma Polymorphous low-grade adenocarcinoma of minor salivary glands, or terminal duct carcinoma, is a form of adenocarcinoma, locally persistent, with a relatively indolent course. The mean age at onset is 50 years and women are affected more frequently than men. In the great majority of cases the lesion occurs on the palate (frequently at the junction of soft and hard palates), followed by the buccal mucosa, lips, retromolar region, and other areas. Clinically, it appears as a painless, firm swelling or an elevated nodule that is rarely ulcerated. The size varies from 1 to several centimeters in diameter and the prognosis is favorable. The differential diagnosis should include pleomorphic adenoma, other malignant minor salivary gland tumors, and lymphomas. Fibrosarcoma Fibrosarcoma of oral soft tissues is an extremely rare malignant tumor of mesenchymal origin. Clinically, the tumor appears as an exophytic mass, soft or semihard on palpation, with or without ulceration. Malignant Fibrous Histiocytoma Malignant fibrous histiocytoma is one of the most common soft tissue sarcomas of late adult life. Approximately 60 cases have been described so far, and the majority appear in the jaw bones. Clinically, the tumor presents as a quickly developing exophytic painless mass, of reddish-brown color, with or without ulceration. The differential diagnosis includes postextraction granuloma, peripheral giant cell granuloma, and other malignant tumors of mesenchymal origin. Hemangiopericytoma Hemangioendothelioma Hemangioendothelioma is a rare malignant neoplasm that originates from blood vessel endothelial cells. It is rare in the oral cavity, where the tongue, palate, gingiva, and lips may be involved. Clinically, it presents as an elevated firm tumor with characteristic deep red color. The differential diagnosis includes hemangioma, pyogenic granuloma, peripheral giant cell Hemangiopericytoma is a rare neoplasm originating from blood vessel wall pericytes. It affects equally both sexes, usually before the age of 50 years, and is extremely rare in the oral mucosa. Clinically, it presents as a well-circumscribed, firm, painless tumor of red or normal color. Malignant Neoplasms Chondrosarcoma Chondrosarcoma is a relatively common malignant neoplasm characterized by the formation of aberrant cartilage tissue. Chondrosarcoma is subclassified as primary when it arises de novo and secondary when it arises from a preexisting benign cartilage tumor. Clinically, the tumor presents as a painless, hard swelling that progressively enlarges, causing extensive bone destruction with pain and loosening of the teeth. Occasionally, a large, erythematous, lobulated, and ulcerated mass may present in the oral cavity. Mesenchymal chondrosarcoma is a rare histologically distinct variant of chondrosarcoma that may also occur in the maxillofacial area. The differential diagnosis includes osteosarcoma, fibrosarcoma, chondroma, central and peripheral giant cell granuloma. Malignant Melanoma Malignant melanoma occurs primarily in the skin and originates from melanocytes. The tumor may develop de novo or in association with a preexisting melanocytic lesion. Malignant melanoma of the oral mucosa affects equally both sexes, usually after 40 years of age. The great majority of the lesions (about 70 to 80%) occur on the palate, upper gingiva, and alveolar mucosa. The rest appear on the lower gingiva, buccal mucosa, tongue, floor of the mouth, and lips. According to clinical and histopathologic criteria, malignant melanoma is classified in 3 forms: nodular melanoma, which clinically presents as an elevated black or reddish-brown nodule that frequently grows quickly, hemorrhages easily, may become ulcerated, and has a poor prognosis. It affects males more than females and usually occurs between 10 and 20 years of age. The jaws are affected in 6 to 7% of the cases, the mandible and maxilla equally often. The tumor usually appears about 10 years later than a primary tumor elsewhere in the skeleton. Clinically, the lesion presents as a rapidly growing hard swelling of the jaw bone that progressively produces facial deformity. The differential diagnosis includes mainly chondrosarcoma, fibrosarcoma and rarely odontogenic tumors. Laboratory test to confirm the diagnosis is histopathologic and X-ray examination. Metastatic Tumors Metastases in the jaws or oral mucosa represent approximately 1 to 2% of all oral cancers. Metastases may arise from carcinomas of the gastrointestinal tract, lung, prostate, breast, kidney, etc. Metastatic tumors of the oral mucosa are usually located on the tongue, gingiva, and palate, where they appear as asymptomatic nodules, frequently ulcerated, without specific clinical features. The differential diagnosis includes pyogenic granuloma, peripheral giant cell granuloma, fibroma, traumatic ulcer, squamous cell carcinoma, etc. Investigation for the primary site of involvement may be necessary if not already apparent. Treatment is related to the type of neoplasia and the therapy of the primary tumor. Osteosarcoma of the mandible presenting as a hard swelling at the angle of the mandible. Malignancies of the Hematopoietic and Lymphatic Tissues Leukemias Leukemias are a heterogeneous group of malignant neoplastic disorder of the blood-forming tissues characterized by defects in the maturation and proliferation of leukocytes. The disorder leads to infiltration of the bone marrow by abnormal white cell clones, abnormalities in the white cell count in peripheral blood, systemic manifestations, infections, anemia, abnormalities in the i mmune responses, and bleeding disorders. Depending on the clinical course and the degree of maturation of the cells, the leukemias are subdivided into acute and chronic forms. Leukemias are also classified according to the abnormal cell clones that predominate and the cell type of origin of these clones, such as lymphocytic leukemia, myelocytic leukemia, myelomonocytic leukemia, eosinophilic leukemia, etc. All types of leukemia may exhibit oral manifestations during their course, but characteristic alterations of the oral lesions occur more often in acute leukemias, irrespectively of the cell type. On light and electron microscopy and cytochemical criteria, acute leukemias are classified into three major types: myelogenous, lymphocytic, and undifferentiated.
Cheap lincocin 500mg mastercard
In individuals of African descent medicine names generic lincocin 500 mg fast delivery, the melanosomes are typically large and dispersed singly in the keratinocytes. Structural or functional differences in white versus nonwhite human skin beyond those related to photoprotection19 and pigmentary alterations are not known. Conflicting data have been presented on variations in lipid content, sebum content, and the number of stratum corneum layers and compaction. Whether there are genetically determined functional differences of the skin associated with skin color is the subject of study and debate. It is largely determined by melanin amount, type (ratio of black/brown eumelanin to red/yellow pheomelanin), and intracellular distribution and location within the layers of the skin. The number of melanocytes in a given area of skin is similar among all individuals. It is genotypically and phenotypically variable, representing mixtures of European (largely Spanish), African, and Central and South American Native origins. Perhaps because of these challenges, genetic determinants of Hispanic skin color remain virtually unstudied. To date, most studies have focused on African hair, which presents the greatest array of clinical disorders. The biochemical composition of hair in people from different geographic regions and racial groups has been shown to be virtually identical in terms of keratin and amino acid content,32,33 despite significant differences in tensile strength, combability, and moisture content. In contrast, numerous studies have described the physical differences in hair from people of different races. There are nevertheless differences in hair morphology and physical properties that contribute to the unique features of the hair fiber, response to hair treatments, and development of disease processes in different groups. However, three-dimensional computeraided reconstructions of scalp biopsy cross-sections suggest that the shape of the hair follicles (helical or curved in Africans vs. In vitro experiments comparing the growth of curly and straight hair found that follicles producing curled hairs, when dissected out of the scalp and placed in culture, continue to grow curled hair shafts. These data suggest that most of the African hair collected from combing in this study was broken and not shed. In a review of tensile strength tests obtained from four different private laboratories, two showed no difference between African hair and that of Caucasian and Asian hair and the other two found African hair to be weaker. Others found a lower tensile strength of both wet and dry curly African hair compared to wet and dry Caucasian hair. The strength of hair has been shown to be dependent upon the integrity of its sulfur-rich proteins and disulfide bonds. It is unclear whether the lack of symmetry of the African hair bulb increases the tendency to mechanical damage, but it is likely that the shape of African hair makes it susceptible to physical damage as a result of certain grooming practices. In addition, intraracial variation in the degree of curl may influence mechanical properties. In a comparative study of African-American hair with different degrees of curl, from a loose to a tight curl pattern, mechanical fragility of hair increased with a tighter curl pattern. Although hair from individuals of European descent has been observed to grow an average of 1 cm a month,48 African hair grows an average of 0. Possible contributors to the differences in hair length, other than a slower growth rate, could include a significantly shorter anagen phase of the hair cycle or perhaps repeated breakage of African hair. In the same comparative study of African, European, and Asian hair, the African hair appeared as a tightly coiled spring-like structure. The teeth of a comb and method of combing can influence the extent of resulting damage. Broken hairs from combing are more numerous and of shorter length in curly African-American hair compared to straight Caucasian and Asian hair. Knots or trichonodes that are commonly seen in tightly curled hair are sites especially susceptible to damage by comb teeth. The relative "dryness" of African-American hair is worsened by the cumulative effect of environmental forces. Features of such weathering include a damaged cuticle, longitudinal fissures known as "split ends," and transverse fissures resembling the nodes of trichorrhexis nodosa. When combing untreated curly hair, a highly negative electrostatic charge develops, in contrast to the low positive electrostatic charge for untreated straight hair. The highly negative charge on African-American hair may be the result of decreased moisture content and increased pulling force from combing. Also, the higher electrostatic charges in African-American hair can produce "flyaway" hair and can lead to difficulty in styling. Hypopigmentation may similarly be more common and more apparent in skin of darker color. Treatment of skin disorders may also affect pigmentation, either positively or negatively. Hypertrophic scarring and keloids are more frequent in black and Asian skin than white skin, a major problem for which the pathogenesis remains unknown. There are also some variations in the prevalence and presentation of certain skin diseases in patients with skin of color (Table 9-5). Not all of these can be attributed to pigmentation differences, but other contributing factors are as yet unidentified. For example, topical corticosteroids may produce unwanted hypopigmentation in treated skin but may also speed resolution of postinflammatory hyperpigmentation. Cryotherapy, which preferentially damages melanocytes, may produce striking and/or irreversible pigment loss. Conversely, the irritation associated with many topical therapies and dermatologic procedures may produce unwanted hyperpigmentation. Awareness of these possibilities, careful choice of therapies and detailed patient education can avoid these iatrogenic problems. Lesions are more often of the acral or subungual subtype than the more common superficial spreading type seen in whites and present at more advanced stages. Public education and melanoma screening campaigns typically target Caucasians and often do not provide relevant information or convey the risk to those with skin of color, and in fact may even provide false reassurance. Development of education campaigns directed toward skin of color may aid in improving detection and prognosis, but until then individualized patient counseling and education remain important. The cosmetic procedure literature has focused primarily on white skin, and often does not discuss outcomes in dark-skinned patients. However, this is changing as greater numbers of patients with skin of color seek cosmetic and procedural treatments. Dermal pigmentation retained in melanophages is not affected by topical therapies and is highly resistant to all treatment modalities. However, increased epidermal melanin can often be improved with topical therapy that reduces melanogenetic stimulation, tyrosinase activity, or melanin transfer to keratinocytes (Table 9-6). Topical therapies generally produce slow and subtle improvements, and treatment expectations should be discussed with patients. Hence, sun protection is recommended for optimal prevention of age-associated changes, regardless of skin color. However, dyschromia (irregular pigmentation) unrelated to photoaging is perhaps the most frequent complaint for patients with skin of color. Prevention and minimization of postinflammatory pigmentary changes due to trauma and irritation, whenever possible, are paramount. These and the many other marketed formulations must be judged by the user on the basis of esthetics, cost, and other factors of importance to the individual. Referral to a professional makeup artist or camouflage makeup therapist for application demonstration and education regarding proper use can provide significant benefit. Inadvertent absorption of laser energy by epidermal melanin can lead to scarring and dyspigmentation. Complexities of racial and ethnic contributors to disease susceptibility, clinical presentation, and therapeutic response are still poorly understood. The welcome movement toward considering skin types as a continuous spectrum rather than dichotomously as white and nonwhite may one day render obsolete the term "skin of color. Microdermabrasion is appropriate for all skin types, is often used for acne and other types of facial scarring, and is a good option for those unable to tolerate peels or extensive recovery times.
BARLEY BRAN (Barley). Lincocin.
- High cholesterol.
- Are there any interactions with medications?
- Preventing cancer of the colon (bowels) or rectum.
- Dosing considerations for Barley.
- What other names is Barley known by?
- Are there safety concerns?
- How does Barley work?
- Bronchitis, cancer prevention, diarrhea, swelling (inflammation) of the stomach or bowel, boils, increasing strength and energy, weight loss, and other conditions.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96777
Purchase cheap lincocin
Photosensitivity affects about 50% symptoms when pregnant order lincocin 500mg with amex, hypothyroidism occurs in about 6% and hyperthyroidism in 1 - 2%. Patients should also be counselled regarding risk of liver impairment and pulmonary fibrosis. In extreme clinical emergency, amiodarone may be given as a slow injection of 150 300 mg in 10 - 20 ml 5% glucose over a minimum of 3 minutes. Patients should be advised of the long-term risk of side-effects such as thyroid and liver dysfunction and phototoxicity. Sotalol (Beta-Cardone, Sotacor) is a -blocker which is very useful for supraventricular arrhythmias and occasionally ventricular arrhythmias. Flecainide (Tambocor) is very useful for supraventricular arrhythmias, particularly paroxysmal atrial fibrillation and re-entry tachycardias. Flecainide injection can be given in an emergency or for rapid effect by a slow injection of 2 mg/kg over not less than 10 minutes, or in divided doses. If preferred, the dose may be diluted with 5% glucose and given as a mini-infusion. In patients with severe renal impairment, each of the above dosage recommendations should be reduced by half. Propafenone (Arythmol) is useful for supraventricular arrhythmias, especially paroxysmal atrial fibrillation. A sufficient period of time should be allowed to enable a slow circulation to carry the drug to the site of action. No more than 200 to 300 mg of lidocaine should be administered during a one hour period. If an infusion is indicated, give 4 mg/min for 30 minutes, 2 mg/min for 2 hours, then 1 mg/min for a maximum of 24 hours. Subsequent doses: 1 mg = 1 ml of 1 mg/1 ml dilution to be given over 30 seconds at 2 minute intervals if required as per main protocol. If more rapid reversal is required, protamine sulphate can be employed (1 mg for each 100 U of heparin given in the previous 4 hours). If > 30 minutes has passed since the infusion was discontinued, reduce the dose of protamine sulphate by 50%. Ensure you are familiar with how to refer to the anticoagulant outpatient service. In the absence of contraindications, all patients should receive 75 mg/day, after an initial dose of 300 mg. For those with apparent aspirin allergy, many patients can be successfully desensitised over half a day employing the following algorithm: Doses are administered every 30 minutes employing aspirin dissolved in water. The onset of action is significantly quicker with prasugrel compared to clopidogrel. Prasugrel is administered as a loading dose of 60 mg followed by 10 mg daily (for up to 12 months). Particular benefit is apparent in patients with diabetes and those under the age of 75. In renal failure (creatinine clearance < 30 ml/min), the dosage of Aggrastat should be reduced by 50%. Best infused into a large vein or centrally as extravasation can cause tissue necrosis. A syringe with a fine hypodermic needle should be used to liberally infiltrate the ischaemic area as soon as extravasation is noted. Adverse effects: the most frequently reported include ectopic beats, tachycardia, anginal pain, palpitations, dyspnoea, nausea, vomiting, hypotension and peripheral vasoconstriction. In higher therapeutic doses, -adrenergic receptors are stimulated and the net effect of the drug is the result of -adrenergic, 1-adrenergic, and dopaminergic stimulation. In low doses, cardiac stimulation and renal vascular dilation occur and in larger doses vasoconstriction occurs. If given peripherally, use a large vein and a dilution of 200 mg in 50 ml (= 4 mg/ml). New chapters and illustrations have been included and the text of the first edition has been modified on several occasions. Sixty-four illustrations of lesions and clinical entities affecting the oral cavity, not published in the first edition, are now included. Nineteen new illustrations of diseases published in the first edition have been added to broaden the spectrum of clinical presentation of these entities. Twenty-three illustrations have been replaced by new, higher quality, more representative ones. I hope that the revised and enlarged second edition of the Atlas is an improvement, and that it will be as useful as the first edition to all of those who are involved in the field of oral medicine. To achieve the optimum goals, oral medical clinicians have to broaden their knowledge bases and practice their clinical skills. When 1 first started to work in this field 20 years ago, I could not imagine the variety of disorders that affect the oral cavity, including genetic diseases, infections, cancers, blood diseases, skin diseases, endocrine and metabolic disorders, autoimmune and rheumatologic diseases, local lesions, to name a few. Fortunately, the oral cavity is accessible to visual examination, and I have attempted to record oral lesions in color slides. During my career as a stomatologist, I have collected more than 25,000 clinical color slides that encompass a broad spectrum of common and rare oral diseases. The most representative and educationally useful illustrations have been used in this Atlas. This book is the distillation of my clinical experience and is intended to aid primarily the practicing dentist, the specialist in oral medicine, the oral pathologist and surgeon, the dermatologist, and otorhinolaryngologist to solve the diagnostic problems posed by oral diseases. It can also be valuable to dental and medical students, general internists, pediatricians, and other medical specialists. This book is not a complete reference work of oral medicine and should be used in conjunction with current textbooks and articles regarding recommendations on treatment and new diagnostic techniques that are beyond its scope. Each entity is accompanied by color plates and a description of the clinical features, differential diagnosis, helpful laboratory tests, and a brief statement on treatment. I hope that the Atlas will serve as a comprehensive pictorial guide for diagnostic problems in the mouth and it will find its way in the places where the battle against oral diseases is waged daily, that is dental schools, hospitals, and private practice offices. My gratitude is extended to the late Professor of Dermatology, John Capetanakis, and the current Professor of Dermatology and Head of the Department of Dermatology, University of Athens, "A. Syngros" Hospital, John Stratigos, for their constant encouragement in my endeavors. I am also indebted to Associate Professor of Dermatology Antony Vareltzidis, who has greatly helped me to broaden my knowledge in the field of dermatology. Syngros" Hospital, Department of Dermatology, University of Athens, for their willing and prompt help during the 23 years of our cooperation. My deepest gratitude is due to Professor Crispian Scully, Department of Oral Medicine and Surgery, University of Bristol, England, and Professor Gerald Shklar, Department of Oral Medicine and Pathology, Harvard School of Den- tal Medicine, United States, both of whom read the manuscript of the first edition. Their suggestions and criticisms have been gratefully received and indeed improved the text considerably.
Discount generic lincocin uk
Bacterial Infections Atrophic Glossitis Congenital Syphilis Congenital (prenatal) syphilis is transmitted by the mother to the fetus in utero symptoms 2 months pregnant buy lincocin 500 mg free shipping. It is classified as early if the disease manifests before age 2 years, late if it becomes apparent after age 2 years, and stigmata, which are developmental changes without active infection. Clinically, the upper central permanent incisors are widely spaced and shorter than the lateral incisors. They are conical or barrel-shaped and at the biting surfaces are usually smaller than at the gingival margins. Similar changes may exist in the lateral incisors (although to a lesser degree), and the teeth may be irregularly spaced. Affected teeth are narrower on their occlusal surfaces and have supernumerary cusps. Clinically, there is atrophy of the filiform and fungiform papillae, and the dorsum becomes smooth and atrophic. Vasculitis finally ending in an obliterative endarteritis is the process underlying these changes. Atrophic syphilitic glossitis may lead to the development of leukoplakia and squamous cell carcinoma. The differential diagnosis includes atrophic lichen planus and Plummer-Vinson syndrome. I nterstitial Glossitis Late syphilis of the tongue may occur either as a solitary gumma or most commonly as a diffuse gummatous infiltration, which heals spontaneously, leading to interstitial glossitis. This is the result of contracture of the lingual musculature after the healing of gummas. The schedules and dosages are internationally established and depend on the stage of the disease. Bacterial Infections Gonococcal Stomatitis Gonorrhea is a common venereal disease caused by the Gram-negative diplococcus Neisseria gonorrhoeae. Gonorrhea is sexually transmitted and involves the genitals, the anal canal, the pharynx, and rarely the oral cavity. Gonococcal stomatitis and pharyngitis are the result of fellatio and are more common in prostitutes and homosexual men. The oral mucosa is red, inflamed, and the patient complains of itching and burning. Gonococcal pharyngitis is more frequent and can be manifested as a sore throat or as a diffuse or patchy erythema and edema with or without tiny pustules on the tonsillar pillars and uvula. The differential diagnosis includes streptococcal stomatitis, herpeticinfection, and candidosis. Penicillin, tetracycline, amoxicillin, and ampicillin in different regimens may eradicate the disease. Chancroid Chancroid is an acute venereal disease caused by Hemophilus ducreyi, a Gram-negative bacillus. The disease is rare in Europe and the United States and occurs most frequently in underdeveloped countries, especially in communities with poor hygiene. After an incubation period of 2 to 5 days, the disease begins as a small red papule or macule that soon becomes pustular and finally ulcerates. The ulcer is round or oval, 1 mm to 2 cm in diameter with slightly raised border and a soft base. The differential diagnosis includes aphthous ulcer, traumatic ulcer, primary and secondary syphilis. Laboratory tests that are helpful in establishing the diagnosis include bacteriologic stains of smears and culture. In addition, the combination of sulfamethoxazole and trimethoprim or other antibiotics are effective. The surface of the ulcer is vegetating and usually covered by a gray-yellowish exudate. The dorsal surface of the tongue is most commonly affected, followed by the palate, buccal mucosa, and lips. Rarely, a tuberculous ulcer of the oral cavity may be the only manifestation of an otherwise silent tuberculosis. Tuberculous osteomyelitis of the jaws and periapical tuberculous granuloma may also occur. Fungal Infections Candida-Endocrinopathy Syndrome this syndrome is a unique form of chronic mucocutaneous candidosis that is accompanied by endocrinopathies, such as hypoparathyroidism, hypoadrenalism, hypothyroidism, or pancreatic and ovarian hypofunction. Oral candidosis begins at the age of 4 to 6 years or later, whereas the endocrinopathy may be delayed in onset. Clinically, the oral, skin, and nail lesions are similar to those seen in chronic mucocutaneous candidosis. The differential diagnosis of candidosis includes chemical burns, traumatic lesions, white spongue nevus, leukoplakia, hairy leukoplakia, lichen planus, and mucous patches of secondary syphilis. Laboratory test useful in establishing the diagnosis is direct microscopic examination of smears. Ketoconazole, amphotericin B, fluconazole, and intraconazole are used systemically with success in generalized forms of the disease. Oral lesions occur in about 35 to 45% of the cases and are clinically characterized by indurated painful ulceration or verrucous, nodular, or granulomatous lesions. The palate, tongue, buccal mucosa, gingiva, and lips are the preferred sites of localization. Histopathologic examination of biopsy specimens, direct examination of smears and culture are helpful in establishing the diagnosis. North American Blastomycosis Blastomycosis is a chronic fungal infection caused by Blastomyces dermatitidis and usually occurs in North America and Africa. The disease mainly involves the lungs and the skin, rarely the bones, the genital tract, and other organs. Clinically, oral lesion is usually present as an ulcer with a slightly verrucous surface and thin borders or as a raised vegetating plaque. The differential diagnosis includes squamous cell carcinoma, tuberculosis, tertiary syphilis, and other systemic fungal infections. Histopathologic examination, direct smear examination, and culture are helpful in establishing the diagnosis. Histoplasmosis Histoplasmosis is a systemic fungal disease caused by the organism Histoplasma capsulatum. The disease is endemic in the United States in the Mississippi and Ohio River Valleys, where about 80% of the adult population show positive histoplasmin skin test reaction. Three forms of histoplasmosis have been recognized: acute primary, chronic cavitary, and progressive disseminated. The acute primary form, which is more common, is characterized by constitutional symptoms (low-grade fever, malaise, chills, myalgias, etc. The chronic cavitary form is characterized exclusively by pulmonary signs and symptoms. Clinically, it is characterized by constitutional symptoms and hepatosplenomegaly, lymphadenopathy, bone marrow involvement, pulmonary radiologic findings, gastrointestinal disorders, adrenal insufficiency, and oral and pharyngeal manifestations. Fungal Infections Paracoccidioidomycosis Paracoccidioidomycosis (South American blastomycosis) is a chronic granulomatous disease and is caused by Paracoccidioides brasiliensis. The disease is particularly restricted to Brazil and other countries of South and Central America. Three forms of the disease are recognized: pulmonary, disseminated, and mucocutaneous. Clinically, paracoccidioidomycosis is characterized by weight loss, fever, dyspnea, cough, lymph node enlargement, draining lesion of the skin and genital area, and ulcers of the nose, larynx, oropharynx, and oral cavity. Clinical, oral lesions usually present as a chronic irregular ulcer with a granular surface. Clinically, the disease is characterized by lowgrade fever, headache, malaise, sinus pain, bloody nasal discharge, periorbital or perinasal swelling and edema, ptosis of the eyelid, extraocular muscle paresis, and progressive lethargy. Tissue necrosis of nasal and paranasal sinuses may result in perforation of the palate.
Generic lincocin 500mg with amex
Adolescent with multiple erythematous papules and crusted lesions in various stages of evolution symptoms 12 dpo purchase lincocin 500 mg online. The presence of lesions in various stages of evolution imparts a polymorphous appearance that is characteristic of pityriasis lichenoides. Large necrotic eschar with halo erythema developing in febrile patient with antecedent pityriasis lichenoides et varioliformis acuta. As with the morphology of the clinical lesions, pityriasis lichenoides can exhibit a range of histopathologic features encompassing acute, chronic, and intermediate lesional variants. All cases of pityriasis lichenoides contain an interface dermatitis that is denser and more wedge shaped in the acute lesions. The infiltrate is composed mainly of lymphocytes with a variable admixture of neutrophils and histiocytes. Epidermal damage ranges from intercellular and extracellular edema in less severe cases to extensive keratinocyte necrosis, vesicles, pustules, and ulcers. The acute variants can exhibit lymphocytic vasculitis with fibrinoid degeneration of blood vessel walls. Ulcerated papule with epidermal necrosis, hemorrhage, and superficial and deep perivascular lymphocytic infiltrate. Most of them can be excluded based on history and typical clinicopathologic features. A few, such as secondary syphilis and virus-associated lesions, can also be excluded based on serologic tests. Parakeratosis, spongiosis, and a predominant mononuclear cell infiltrate in the epidermis and dermis with papillary edema. Systemic antibiotics in the tetracycline and erythromycin families are used primarily for their antiinflammatory rather than antibiotic effects. Topical and systemic antibiotics may be needed to treat secondary infections complicating ulcerated skin lesions. These agents are often selected initially to cover Gram-positive pathogens, but subsequent use should be guided by culture results. The disorder may resolve spontaneously within a few months or, less commonly, persist for years. Although the conclusion was not confirmed by subsequent investigation, one report suggested that the duration of pityriasis lichenoides in children correlated better with its clinical distribution than with the relative abundance of acute and chronic lesions, which often coexisted. Vakeva L et al: A retrospective study of the probability of the evolution of parapsoriasis en plaques into mycosis fungoides. Ersoy-Evans S et al: Pityriasis lichenoides in childhood: A retrospective review of 124 patients. Sotiriou E et al: Febrile ulceronecrotic Mucha-Habermann disease: A case report and review of the literature. Acta Derm Venereol 88(4):350-355, 2008 296 Section 4:: Inflammatory Disorders Based on T-Cell Reactivity and Dysregulation Chapter 26:: Lichen Planus:: Mazen S. Lesions: Symmetric, grouped, erythematous to violaceous, flat-topped, polygonal papules. Pathology: Basal epidermal keratinocyte damage and lichenoid interface lymphocytic reaction. The term lichenoid reaction1 is the histologic description used to capsulize the pathologic characteristics of skin diseases resembling lichen planus. The four Ps-(1) purple, (2) polygonal, (3) pruritic, and (4) papule-is the mnemonic device often used to recall the constellation of symptoms and skin findings that characterize lichen planus. Females are usually affected in their 50s and 60s, whereas males develop lichen planus at a somewhat earlier age. The development of lichen planus may be affected by seasonal or environmental factors. The familial form tends to be more protracted and severe and presents in erosive, linear, or ulcerative patterns or with atypical features affecting young adults and children. Lichen planus (Greek leichen, "tree moss"; Latin planus, "flat") is a unique, common inflammatory disorder that affects the skin, mucous membranes, nails, and hair. The appearance of lichen planus-like lichenoid dermatoses has been likened to the scurfy, finely furrowed, dry excrescences of the symbiotic vegetation known as lichen. Although this morphologic comparison may be antiquated, lichen planus is a distinctive entity with prototypic "lichenoid" papules that show distinctive color and morphology, develop in typical locations, and manifest characteristic patterns of evolution. T-cell mediated pathologic alterations involving proinflammatory and counterregulatory mechanisms function in the pathogenesis of lichen planus. Cell-mediated immunity, on the other hand, plays the major role in triggering the clinical expression of the disease. These cells are considered responsible for the development of the most characteristic change observed in the lichenoid reaction, namely, apoptosis. Contact sensitizers such as metals could act as haptens and elicit an immunologic response. Enhanced lymphocyte reactivity to inorganic mercury, a component of dental amalgam, has been found in patients with oral lichenoid reactions. Low-grade chronic exposure to mercury, and possibly to other metals such as gold, may stimulate a lymphocytic reaction that manifests as lichen planus. A list of contact chemicals and drugs that can elicit lichenoid reactions is discussed in Section "Drug-Induced Lichen Planus. The balance between lymphocytic activation and down regulation determines the clinical behavior of the disease. Theoretically, the antigen may be an autoreactive peptide, thus classifying lichen planus as an autoimmune disease. Alternatively, it may represent an exogenous antigen such as an altered protein, drug, contact allergen, viral or infectious agent, or an unidentified immunogenic target. Intercellular adhesion molecule-1 is a ligand for the 2-integrin, leukocyte function-associated antigen-1, on the surface of lymphocytes, which further enhances the interaction of these lymphocytes with the antigenpresenting cells. This close interaction between lymphocytes and basement membrane targets metalloproteinases produced by lymphocytes to alter extracellular matrix proteins and integrins, and the process eventuates in apoptosis, basement membrane disruption, reduplication, and subepidermal cleft formation (see Section "Pathology"). These cytokines further activate tissue macrophages and peripheral blood mononuclear cells and upregulate expression of cell surface adhesion molecules and migration activity. Keratinocyte-produced cytokines also upregulate expression of specific keratin genes. Keratin (K)17, usually restricted to adnexal structures, is variably expressed in the basal and suprabasal layers of the interfollicular epithelium of affected epidermis. K4 and K13 are reduced in the suprabasal compartment in areas with orthokeratosis, associated with increased production of K1 and K10. Various other environmental, behavioral, or infectious factors have been observed on occasion to be associated with the development or exacerbation of lichen planus. However, no well-established association has been documented between emotional stress, tobacco use, or oral or gastrointestinal candidiasis and development of lichen planus. Recent studies using microarray technologies to examine and characterize in greater detail various inflammatory and immune-mediated skin diseases have provided considerable new insights into mechanisms mediating-specific inflammatory responses, including lichen planus, oral lichen planus, lichen planopilaris as well as lichenoid eruptions, and interface dermatitis. Lichen planus was distinguished from atopic dermatitis, psoriasis, and healthy skin by elevated expression of type I interferon-induced genes and a specific cytokine expression pattern. In lichen planus, granzyme B predominates in lesional epidermis versus perforin in graft-versus-host disease. Caspase 3 is frequently found to be elevated in both cutaneous and oral lichen planus lesional skin. Fine, whitish puncta or reticulated networks referred to as Wick-ham striae are present over the surface of many well-developed papules. The surface alteration may result from localized thickening of the keratohyalin-containing cell layers of the stratum granulosum, although a focal increase in the activity of lichen planus may account for the morphologic alteration of Wickham striae. Sometimes multiple lesions develop rapidly with dissemination following the initial appearance. The lesions are usually distributed symmetrically and bilaterally over the extremities. Small, flat-topped violaceous papules, some grouped, some disseminated, becoming confluent on the trunk. Lichen planus tends to be quite pruritic, although some patients are completely asymptomatic.
Order lincocin with mastercard
The selectins bind their respective carbohydrate ligands located on protein scaffolds and thus mediate the transient binding or "rolling" of leukocytes on endothelial cells treatment modality definition buy lincocin 500 mg low price. A vast array of data suggest that the binding of chemokines to leukocyte chemokine receptors plays a critical role in activating both b1 and b2 integrins. Integrin activation via chemokine-mediated signals appears to be more complex in T cells, which appear to use multiple chemokine receptors, and is described in more detail below. Leukocytes, pushed by the blood stream, first transiently bind or "roll" on the surface of activated endothelial cells via rapid interactions with P-, E-, or L-selectin. Chemokines are secreted by endothelial cells and bind to proteoglycans that present the chemokine molecules to chemokine receptors on the surface of the leukocyte. After chemokine receptor ligation, intracellular signaling events lead to a change in the conformation of integrins and changes in their distribution on the plasma membrane resulting in "Integrin Activation. In several different systems, inhibition of specific chemokines produced by endothelial cells or chemokine receptors found on T cells dramatically influences T cell arrest in vivo and in vitro. All three of these chemokines are distinguished from other chemokines by being highly upregulated by interferon-g. Just as Th1 and Th2 (T cell) subsets have different functional roles, it might have been predicted that these two subsets of T cells would express different chemokine receptors. Keratinocytes from patients with distinctive skin diseases appear to express unique chemokine expression profiles. The inflammatory infiltrate of psoriatic skin is predominantly composed of Th1- and Th17-polarized memory T cells, as well as neutrophils, macrophages, and increased numbers of dendritic cells. This may lead to the formation of the long tortuous capillary blood vessels in the papillary dermis that are characteristic of psoriasis. It has been proposed that they act by displacing growth factors from proteoglycans. Tumors, including melanoma, have long been known to secrete chemokines that can attract a variety of leukocytes. While chemokines secreted by tumor cells do lead to recruitment of immune cells, this does not necessarily lead to increased clearance of the tumor. With skin cancers such as melanoma, there is a propensity for specific sites such as brain, lung, and liver, as well as distant skin sites. The discovery of nodal metastasis often portends a poor prognosis for the patient. In fact, the presence of nodal metastases is one of the most powerful negative predictors of survival in melanoma. Broad expression of this receptor may be due to its regulation by hypoxia, a condition common to growing tumors, via the hypoxia inducible factor-1a transcription factor. Thus, a limited number of specific chemokine receptors appear to play distinct, nonredundant roles in facilitating cancer progression and metastasis (summarized in. In fact, there is an association of less severe autoimmune diseases in patients with these mutations. Chemokines not only orchestrate the migration of inflammatory cells but also play roles in angiogenesis, cancer metastasis, and cellular proliferation. Signaling pathways are just beginning to be understood, and further work needs to be done to understand the regulation of these receptors, the specificity of intracellular activities, and the mechanism by which chemokine receptors work in the face of multiple chemokines present in many inflammatory sites. Zlotnik A, Yoshie O: Chemokines: A new classification system and their role in immunity. J Clin Invest 119(8): 2317-2329, 2009 151 4 Chapter 13:: Allergic Contact Dermatitis:: Mari Paz Castanedo-Tardan & Kathryn A. The acute phase is characterized by pruritus, erythema, edema, and vesicles usually confined to the area of direct exposure. Recurrent contact to the allergen in a sensitized individual will result in chronic disease, characterized by lichenified erythematous plaques with variable hyperkeratosis and fissuring that may spread beyond the areas of direct exposure. Appropriate allergen identification through proper epicutaneous patch testing has been demonstrated to improve quality of life as measured by standard tools,3 as it allows for appropriate avoidance of the inciting allergen and possibly sustained remission of this potentially debilitating condition. In 2007, Thyssen and colleagues4 performed a retrospective study that reviewed the main findings from previously published epidemiological studies on contact allergy in unselected populations including all age groups and most publishing countries (mainly North America and Western Europe). Based on these heterogeneous published data collected between 1966 and 2007, the median prevalence of contact allergy to at least one allergen in the general population was 21. Additionally, the study found that the most prevalent contact allergens in the general population were nickel, thimerosal, and fragrance mix. Importantly, the prevalence of contact allergy to specific allergens differs between various countries5,6 and the prevalence to a specific allergen is not necessarily static, as it is influenced by changes and developments in the regional environment, exposure patterns, regulatory standards, and societal customs and values. On a final note about epidemiology, contact allergy caused by ingredients found in personal care products (cosmetics, toiletries) is a well-known problem, with approximately 6% of the general population estimated to have a cosmetic-related contact allergy. Educating patients about avoidance of the allergen and its potentially related substances, and providing suitable alternatives are crucial to a good outcome. As the largest organ in the human body, the skin is a complex and dynamic organ that serves among many other purposes, the function of maintaining a physical and immunologic barrier to the environment. Therefore, the skin is the first line of defense after exposure to a variety of chemicals. When the human repeat-insult patch testing method was used to assess induction rates for ten common allergens, women were more often sensitized to seven of the ten allergens studied. When looking specifically at nickel sensitivity, the same study showed that the prevalence was much higher among women than men (17. This might be due to the fact that numerous studies have demonstrated that pierced ears are a significant risk factor for development of nickel allergy. However, the edema and papules/vesicles are usually obvious and palpable; therefore palpation of the patch-test site can help to detect allergic reactions in patients with darker skin types. Finally, the darker the skin, the more difficult it is to mark the patch-test site after removal. Such immunological reaction, results from exposure and subsequent sensitization of a genetically susceptible host, to an environmental allergen, which on reexposure triggers a complex inflammatory reaction. The resulting clinical picture is that of erythema, edema, and papulo-vesiculation, usually in the distribution of contact with the instigating allergen, and with pruritus as a major symptom. Mast cells appear to be pivotal in determining the magnitude of the inflammatory reaction. Such rechallenge can occur via multiple routes, including transepidermal, subcutaneous, intravenous, intramuscular, inhalation, and oral ingestion. Additionally, one must also consider contact allergy in patients with other types of dermatitis. This localized proinflammatory state results in the classical clinical picture of spongiotic inflammation (redness, edema, papules and vesicles, and warmth). History taking should begin with a discussion of the present illness focusing on the site of onset of the problem and the topical agents used to treat the problem (including over the counter and prescription medications). A past history of skin disease, atopy, and general health should be routinely investigated. This is followed by a detailed history of the usage of personal care products (soap, shampoo, conditioner, deodorant, lotions, creams, medications, hair styling products, etc. The occupation should be ascertained as well, and if it appears contributory, or there are potential allergenic exposures, then a thorough occupational history should be taken. Occupations requiring frequent hand washing, glove use, or frequent chemical exposure should be prime suspects, among others. Geometric or linear patterns or involvement of focal skin areas, may also be suggestive of an exogenous etiology. Occasionally, the actual sensitizing substance in these plants, an oleoresin named urushiol may be aerolized when the plants are burned, leading to a more generalized and severe eruption on exposed areas such as the face and arms. Transfer of the resin from sources other than directly from the plant (such as clothes, pets, or hands) may result in rashes on unexpected sites.

Cheap lincocin 500mg without prescription
If one mutated and one wild-type allele is inherited by the offspring symptoms 0f ovarian cancer buy 500 mg lincocin with visa, the child will be an unaffected carrier, similar to the parents. If both wild-type alleles are transmitted, the child will be genotypically and phenotypically normal with respect to an affected individual. If the mutations from both parents are the same, the individual is referred to as a homozygote, but if different parental mutations within a gene have been inherited, the individual is termed a compound heterozygote. For someone who has an autosomal recessive condition, be it a homozygote or compound heterozygote, all offspring will be carriers of one of the mutated alleles but will be unaffected because of inheritance of a wildtype allele from the other, clinically and genetically unaffected, parent. Although this is usually the case in nonconsanguineous relationships, it may not hold true in first-cousin marriages or other circumstances where there is a familial interrelationship. For example, if the partner of an individual with an autosomal recessive disorder is also a carrier of the same mutation, albeit clinically unaffected, then there is a 50% chance of the offspring inheriting two mutant alleles and therefore also inheriting the same autosomal recessive disorder. In X-linked dominant inheritance, both males and females are affected, and the pedigree pattern may resemble that of autosomal dominant inheritance. An affected male transmits the disorder to all his daughters and to none of his sons. Key observations include: the disorder affects both males and females; there are mutations on both inherited copies of the gene; the parents of an affected individual are both heterozygous carriers and are usually clinically unaffected; autosomal recessive disorders are more common in consanguineous families. Filled circle indicates affected female; half-filled circles/ squares represent clinically unaffected heterozygous carriers of the mutation; unfilled circles/squares represent unaffected individuals. Key observations include: affected individuals are either hemizygous males or heterozygous females; affected males will transmit the disorder to their daughters but not to their sons (no male-to-male transmission); affected females will transmit the disorder to half their daughters and half their sons; some disorders of this type are lethal in hemizygous males and only heterozygous females survive. Filled circles indicate affected females; filled squares indicate affected males; unfilled circles/squares represent unaffected individuals. Key observations include: usually affects only males but females can show some features because of lyonization (X-chromosome inactivation); transmitted through female carriers, with no male-to-male transmission; for affected males, all daughters will be heterozygous carriers; female carrier will transmit the disorder to half her sons, and half her daughters will be heterozygous carriers. Dots within circles indicate heterozygous carrier females who may or may not display some phenotypic abnormalities; filled squares indicate affected males; unfilled circles/squares represent unaffected individuals. X-linked recessive conditions occur almost exclusively in males, but the gene is transmitted by carrier females, who have the mutated gene only on one X chromosome (heterozygous state). The sons of an affected male will all be normal (because their single X chromosome comes from their clinically unaffected mother). However, the daughters of an affected male will all be carriers (because all had to have received the single X chromosome from their father that carries the mutant copy of the gene). Some females show clinical abnormalities as evidence of the carrier state (such as in hypohidrotic ectodermal dysplasia; see Chapter 142); the variable extent of phenotypic expression can be explained by lyonization, the normally random process that inactivates either the wild-type or mutated X chromosome in each cell during the first weeks of gestation and all progeny cells. They occur in about 6% of all conceptions, although most of these lead to miscarriage, and the frequency of chro- mosomal abnormalities in live births is about 0. Approximately two-thirds of these involve abnormalities in either the number of sex chromosomes or the number of autosomes; the remainder is chromosomal rearrangements. The most common numerical abnormality is trisomy, the presence of an extra chromosome. This occurs because of nondisjunction, when pairs of homologous chromosomes fail to separate during meiosis, leading to gametes with an additional chromosome. Loss of a complete chromosome, monosomy, can affect the X chromosome but is rarely seen in autosomes because of nonviability. A number of chromosomal disorders are also associated with skin abnormalities, as detailed in Table 8-2. Structural aberrations (fragility breaks) in chromosomes may be random, although some chromosomal regions appear more vulnerable. If the deletion leads to loss of neighboring genes this may result in a contiguous gene disorder, such as a deletion on the X chromosome giving rise to X-linked ichthyosis (see Chapter 49) and Kallman syndrome. If two chromosomes break, the detached fragments may be exchanged, known as reciprocal translocation. Other structural aberrations include duplication of sections of chromosomes, two breaks within one chromosome leading to inversion, and fusion of the ends of two broken chromosomal arms, leading to joining of the ends and formation of a ring chromosome. Array-based cytogenetic tools do not rely on cell division and are very sensitive in detecting unbalanced lesions as well as copy number-neutral loss of heterozygosity. A further possible chromosomal abnormality is the inheritance of both copies of a chromosome pair from just one parent (paternal or maternal), known as uniparental disomy. For certain chromosomes, uniparental disomy can also result in distinct phenotypes depending on the parental origin of the chromosomes, a phenomenon known as genomic imprinting. Three phenotype abnormalities commonly associated with uniparental disomy for chromosomes with imprinting are (1) intrauterine growth retardation, (2) developmental delay, and (3) reduced stature. Mitochondrial mutations can induce, or be induced by, reactive oxygen species, and may be found in, or contribute to , both chronologic aging and photoaging. Indeed, currently there is little understanding of the interplay between the nuclear and mitochondrial genomes in both health and disease. Nevertheless, it is evident that the genes encoded by the mitochondrial genome have multiple biologic functions linked to energy production, cell proliferation, and apoptosis. By contrast, for complex traits, such as psoriasis and atopic dermatitis, these traditional approaches have been largely unsuccessful in mapping genes influencing the disease risk or phenotype because of low statistical power and other factors. To dissect out genes that contribute and influence susceptibility to complex traits, several stages may be necessary, including establishing a genetic basis for the disease in one or more populations; measuring the distribution of gene effects; studying statistical power using models; and carrying out marker-based mapping studies using linkage or association. It is possible to establish quantitative genetic models to estimate the heritability of a complex trait, as well as to predict the distribution of gene effects and to test whether one or more quantitative trait loci exist. These models can predict the power of different mapping approaches, but often only provide approximate predictions. Moreover, low power often limits other strategies such as transmission analyses, association studies, and familybased association tests. Another potential pitfall of association studies is that they can generate spurious associations due to population admixture. To counter this, alternative strategies for association mapping include the use of recent founder populations or unique isolated populations that are genetically homogeneous, and the use of unlinked markers (so-called genomic controls) to assign different regions of the genome of an admixed individual to particular source populations. In addition, and relevant to several studies on psoriasis, linkage disequilibrium observed in a sample of unrelated affected and normal individuals can also be used to fine-map a disease susceptibility locus in a candidate region. Normally, 2,000 or more cases are required versus 3,000 ethnically matched random population controls. The P values are plotted along each chromosome ("Manhattan plot") and where disease susceptibility loci exist, there are clusters of strong association. Typically, P values of 10-10 or lower are indicative of a true locus, although this generally has to be replicated in a number of other case-control sets for confirmation. Furthermore, across the entire field of complex trait genetics, relatively few causative genes have emerged (the role of the filaggrin gene in atopic dermatitis, below, being a notable exception). However, recently, a conventional genetics approach has revealed fascinating new insight into the pathophysiology of one particular complex trait, namely atopic dermatitis (eczema). This finding emanated from the discovery that the disorder ichthyosis vulgaris was due to loss-of-function mutations in the gene encoding the skin barrier protein filaggrin (see Chapters 14 and 49). Therefore, Mendelian disorders may be useful in the molecular dissection of more complex traits. There are several different types of mosaicism, including single gene, chromosomal, functional, and revertant mosaicism. The earlier this occurs, the more likely it is that there will be clinical expression of a disease phenotype as well as involvement of gonadal tissue (gonosomal mosaicism); for example, when individuals with 86 segmental neurofibromatosis subsequently have offspring with full-blown neurofibromatosis (see Chapter 141). However, in general, if the mutation occurs after generation of cells committed to gonad formation, then the mosaicism will not involve the germ line, and the reproductive risk of transmission is negligible. Gonosomal mosaicism refers to involvement of both gonads and somatic tissue, but mosaicism can occur exclusively in gonadal tissue, referred to as gonadal mosaicism. The lines of Blaschko were delineated over 100 years ago; the pattern is attributed to the lines of migration and proliferation of epidermal cells during embryogenesis. Monoallelic expression on autosomes (with random inactivation of either the maternal or paternal allele) is also feasible, and probably underdocumented.