Order lioresal 10 mg with visa
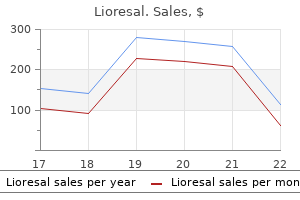
Electrocautery or argon beam device is used to coagulate the cortical aspects of the defect spasms on left side of abdomen discount 10 mg lioresal overnight delivery. The defect in the renal parenchyma is closed, and the tumor is removed intact in an entrapment bag. At present there is no difference in complication rates between open and laparoscopic partial nephrectomy. The most common postoperative complications are bleeding and urine leak (urinoma). In situations where postoperative bleeding is suspected, the patient should be managed with serial complete blood counts, bed rest, and blood transfusions as needed. Conservative measures are often adequate when the bleeding is modest, but interventions such as selective arterial embolization or surgical reexploration may sometimes be required. Urine leakage can result from inadequate intraoperative closure of a collecting system defect or ureteral obstruction from a blood clot, which increases backflow pressure. A surgical drain should therefore be used when the renal collecting system has been violated to monitor for postoperative leak. In addition, the patient should retain a Foley catheter to ensure bladder decompression and low upper tract pressure. Urine leaks are usually transient and heal without intervention; however, a persistent leak may require the placement of a ureteral stent to facilitate drainage and healing. In addition to bleeding and urine leak, other potential complications include wound infection, ileus, pneumonia, injury to adjacent organs, and transient renal insufficiency. Renal tumor ablative techniques, however, are relatively new developments with increasing application. Such techniques were initially indicated in patients with multiple renal tumors, a solitary kidney, or significant comorbidities that precluded higher risk surgery. The renal fascia is opened and the perinephric fat carefully removed to expose the tumor, which is further characterized using laparoscopic ultrasound. At present, the clinically viable ablation technologies include cryoablation and radiofrequency ablation. In cryoablation, the cryoprobe needles are cooled to very low temperatures, which induces tissue necrosis. At present, such cooling is achieved by delivering pressurized argon gas to the tips of the cryoprobes. As argon gas passes through the restricted tips of the probes and then expands, it undergoes rapid cooling (a phenomenon known as the Joule-Thomson effect) and forms an iceball over the tumor. Therefore, the iceball must involve a margin of normal tissue to ensure complete tumor destruction. Following the freeze cycle, an active thaw phase is initiated, and then a second freeze-thaw cycle is performed to further increase cell death. The cryoprobes are placed in to the tumor under direct vision, and laparoscopic ultrasound is used to confirm that their tips extend past the internal border of the tumor. Freezing continues until the ice ball extends at least one centimeter beyond the gross tumor margins. The ice ball is allowed to thaw prior to initiation of the second freeze-thaw cycle. After the second freeze-thaw cycle, the cryoprobes are removed, and surgical hemostatic pharmaceutical is applied to the insertion sites. In a laparoscopic ablation, the tumor can be directly visualized, and the ablation process can be monitored in real time. The tumor can be accessed from either a transperitoneal or retroperitoneal approach, depending on its location. In the transperitoneal approach, the colon is mobilized medially to expose the renal fascia, which is mobilized from its attachments to surrounding structures, such as the liver or spleen. Next, the renal fascia is entered over the area of the renal mass, which is targeted using preoperative imaging and intraoperative ultrasound. Once the tumor has been adequately visualized, multiple core biopsies are acquired using a percutaneous biopsy device. Finally, ablation probes are inserted through the skin and in to the tumor under direct vision. The probes should enter the tumor at a right angle, and laparoscopic ultrasound should be performed to ensure the probe tips are beyond the internal margin of the tumor. During cryoablation, laparoscopic ultrasound can be used to monitor the iceball as it forms, ensuring that it completely engulfs the mass and a 1-cm rim of normal parenchyma. To minimize the chance of bleeding, probe extraction should not be attempted until the probes are loose enough to freely twist within the tumor. Alternatively, some clinicians deploy temperature probes at selected sites around the tumor to monitor the ablation process. After the ablation process is completed, the lesion is monitored for hemorrhage, and minor bleeding is controlled using topical hemostatic agents and gentle pressure. After hemostasis has been confirmed at reduced pneumoperitoneum, the trocars are removed. Percutaneous ablation offers numerous advantages over a laparoscopic procedure, including avoidance of general anesthesia, reduced complication rate, diminished postoperative pain, and expedited convalescence. The major disadvantages, however, include the lack of direct visualization during the ablation process, as well as the inability to assess for immediate postablation bleeding. A semipermeable targeting template is positioned over the ipsilateral flank, and imaging is performed to correlate the template with the renal anatomy. An access sheath is then deployed at the Permeable targeting template placed on flank Left Right Area sterilized and draped Access sheath placed Left Right First cryoprobe is placed within sheath; second cryoprobe is placed directly through skin. Freezing in progress marked site, and its position in the kidney is confirmed and readjusted if necessary using imaging. Subsequent probes are placed directly through the skin, with additional imaging performed to confirm proper positioning. Once completed, a final image series is acquired using a half dose of intravenous contrast to confirm successful tumor ablation. Nonetheless, they carry a risk of some major complications, including bleeding from the tumor, injured intraabdominal vessels, or skin; pain at the trocar or probe sites; urinary tract infection; intraabdominal abscess; ileus; injury to adjacent organs; and tumor persistence or recurrence after treatment. The different kinds of transplanted tissue include an autograft (tissue from the recipient), an isograft (tissue from an individual with the same genotype, such as a monozygotic twin), an allograft (tissue from a genetically disparate individual from the same species), and a xenograft (tissue from a different species). As early as 1916, Little and Tyzzer articulated the important differences between these graft types, stating "isografts succeed; allografts are rejected. Nonetheless, the introduction of modern immunosuppression drugs has led to dramatic improvements in allograft outcomes. Unfortunately, only a small minority of the patients that would benefit from a kidney transplant ever receive one. There is an ever-growing waiting list-84,355 patients in the United States in 2010-that far exceeds the number of annual procedures. In 2009, 16,830 kidney transplants were performed: 10,442 from a deceased donor, and 6388 from a living donor. Despite the growing need for organs, the number of deceased organ donors per year has been stagnant. Much of this growth has been fueled by an increase in live donors, in large part because of substantial improvements in the organ harvesting process, such as the introduction of minimally invasive techniques. Those who can tolerate the surgical and anesthetic risks, and who can safely be immunosuppressed after the transplant, are potential candidates. Before transplantation, the donor and recipient must be confirmed to have compatible blood types. Recipient serum must be tested against donor lymphocytes to ensure the recipient does not have preformed antibodies to donor proteins. A positive crossmatch predicts a high likelihood of hyperacute or early rejection. Moreover, acute rejection episodes that do occur can usually be effectively treated. Kidney transplants from living donors result in superior outcomes compared with those where the kidney has been obtained from a deceased donor.
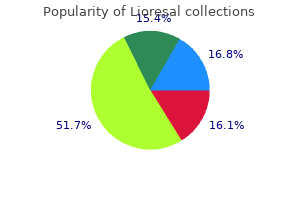
Generic lioresal 10 mg on-line
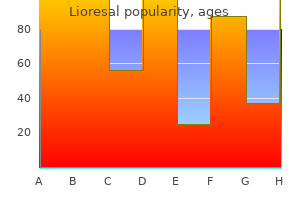
As development proceeds spasms and spasticity buy lioresal uk, however, mesoderm invades the cranial aspect of the cloacal membrane, interposing itself between the ectoderm and endoderm. This mesoderm, which now occupies the infraumbilical space, fuses in the midline and gives rise to the infraumbilical abdominal wall, pubic rami, and anterior surface of the detrusor muscle. In the meantime, the cloaca undergoes septation in to an anterior urogenital sinus and posterior rectum, the orifices of which become exposed following apoptosis of the cloacal membrane. If the cloacal membrane does not permit mesodermal invasion, midline fusion of the mesodermal structures is not possible, resulting in midline defects of the abdominal wall and pelvis. In cloacal exstrophy, this defect is hypothesized to occur in conjunction with abnormal cloacal septation. As a result, both the bladder and hindgut become exposed through the abdominal wall defect following apoptosis of the cloacal membrane. In addition, the cloacal membrane prevents fusion of the genital folds, causing the genitalia to appear bifid. Meanwhile, in both bladder exstrophy and epispadias, impaired mesodermal invasion occurs in conjunction with normal septation of the cloacal membrane. As a result, the abdominal wall defect exposes either the urethra alone or both the urethra and bladder, depending on its size. In either case, it appears that the genital folds fuse to a large extent at the level of the urorectal septum, caudal to the urogenital sinus. In males, this arrangement would explain the presence of the urethra on the anterior surface of the undivided penis. The major findings include poor visualization of the bladder, a lower abdominal bulge, small genitalia (in males), a low-set umbilicus, and a pubic bone diastasis. If the diagnosis is not established before birth, it is readily apparent upon delivery. Likewise, a sheet of plastic wrap should be used to cover the anterior abdominal defect and protect the bladder mucosa from abrasion by towels, diapers, and clothing. A thorough physical and radiologic assessment should be performed to assess for the presence of other anomalies. The relative merits of a single or staged repair of the exstrophy, epispadias, abnormal ureterovesical junctions, and abnormal bladder neck have yet to be determined; however, it is clear that the sooner the exstrophied bladder is closed and the bladder neck and sphincter are reapproximated, the better the chance for a functional bladder and long-term urinary continence. The timing of the initial closure depends on a number of variables, including the size of the bladder, the size of the penis in the male patient, the length and depth of the urethral groove, the width of the pubic diastasis, and the presence or absence of other associated anomalies. At the time of the Bifid clitoris Vagina Exstrophy of bladder in female initial closure, many patients also undergo pelvic osteotomy in which the ilia and ischia are cut to facilitate reapproximation of the pubic symphysis. This procedure can reduce tension on the abdominal wall closure, and it reapproximates the pelvic floor musculature in the midline to improve later continence. With current reconstructive strategies, most patients achieve urinary continence (albeit with clean intermittent catheterization in a significant proportion) and can lead satisfying personal and professional lives. Long-term management, however, must address the psychological effects of this condition, possible sexual dysfunction (especially in women), and later complications, such as vaginal and rectal prolapse in women. In either duplication or septation, division of the bladder may be complete or incomplete, and it may occur in the coronal or sagittal plane. In duplication, each half of the divided bladder receives its own ureter and possesses its own fullthickness wall. In incomplete duplication, the two halves typically unite above the level of the bladder neck and then drain together in to a single urethra. In complete duplication, the two halves remain separate to the level of the bladder neck and can even drain in to two independent urethras, each with its own external meatus. In some cases, however, one of the bladder halves lacks a urethral component, resulting in outlet obstruction and ipsilateral renal abnormalities. In septation, a fibromuscular wall divides the bladder in to separate compartments. In contrast to duplication, septation produces two compartments that share a common wall. Like duplication, septation can be incomplete or complete, depending on how far the wall extends toward the bladder neck. Septation, however, is not associated with duplication of the urethra, and thus both compartments must be in open communication with the urethra. In some cases, however, fusion of the septum with the bladder neck causes one compartment to lose access to the urethra, resulting in obstruction. Bladder duplication and septation are frequently associated with other anomalies, especially in the genitourinary system. For example, vesicoureteral reflux may be seen on one or both sides, resulting in hydronephrosis if severe. Likewise, one or both of the bladder components may lack a normal continence mechanism. If there is complete duplication of the bladder, concurrent duplication of the external genitalia may be seen as well. Less often, duplication may also occur in the lower gastrointestinal tract or spine. It is possible that complete duplication of the bladder and adjacent organ systems reflects partial twinning of the embryonic tail early in gestation. In contrast, isolated defects of the bladder may reflect abnormalities during cloacal septation (see Plate 2-4). The left half does not communicate with the urethra and is thus obstructed, with associated renal abnormalities. The right-sided ureter exhibits vesicoureteral reflux, with associated hydroureteronephrosis. Partial septation of bladder the timing of diagnosis depends on the nature and extent of the malformation. If there is external evidence of duplication-such as in the genitals or spine-the patient is likely to undergo comprehensive evaluation early in life, during which the bladder abnormality will be discovered. Once the diagnosis has been established, further evaluation should include a renal scan to assess kidney function, as well as video-urodynamic studies to examine voiding from each bladder compartment and to determine if vesicoureteral reflux is present. If an obstruction is present, it should be excised as soon as possible so as to reduce the risk of further infection and preserve renal function. If incontinence, vesicoureteral reflux, external duplication, and/or other anomalies are present, a more complex intervention will be required, the specifics of which must be tailored to each individual patient. The urogenital sinus, which gives rise to the bladder, is initially continuous with the allantois, a tube that extends in to the connecting stalk (see Plate 2-4 for an illustration). As the bladder matures and descends in to the pelvis, however, the allantois narrows to form a thick, epithelial-lined tube known as the urachus. Normally the urachus regresses in to a fibrous cord, known as the median umbilical ligament. For uncertain reasons, however, this normal regression process sometimes fails, resulting in a persistent urachus that is either partially or completely patent. Because many urachal anomalies are undiagnosed, their overall incidence is unknown. It typically presents during the neonatal period as dribbling of fluid from the umbilicus. The fluid leakage may increase in response to bladder contraction during either purposeful voiding or other increases in intraabdominal pressure, such as during crying or straining. A patent area at the distal end of the urachus, which communicates with the umbilicus, is known as a superior urachal sinus (or umbilical-urachal sinus) and accounts for 15% of urachal anomalies. Like a patent urachus, a superior sinus causes umbilical discharge during the neonatal period, although the fluid is not as copious. A patent area in the middle of the urachus, which communicates with neither the umbilicus nor bladder, is known as a urachal cyst and accounts for about 30% of urachal anomalies. It may be noted as an incidental finding during laparotomy; as a palpable midline mass; or as a site of infection, usually with Staphylococcus aureus, with associated pain and erythema. Finally, a patency in the proximal end of the urachus, which communicates with the apex of the bladder, is known as an inferior sinus (or vesicourachal diverticulum) and accounts for 5% of urachal anomalies. It usually does not cause symptoms because it is has a large opening in to the bladder lumen and does not communicate with other structures. In rare instances, Inferior urachal sinus (vesicourachal diverticulum) Urachal cyst Urachal adenocarcinoma: computed tomography (contrast enhanced) Rectus abdominis muscles Urachal adenocarcinoma Bladder however, it may act as a site of calculus formation or lower urinary tract infection. It is essential to remove all abnormal urachal tissue because there is a small risk of later malignant transformation.
Buy generic lioresal online
Tinea corporis can be easily diagnosed with a microscopic evaluation of a small scraping of the skin muscle relaxant 16 buy cheap lioresal 10mg on line. Widespread tinea is almost always associated with onychomycosis, and it is more commonly seen in patients who are taking chronic immunosuppressive agents or using topical steroids. Any patient who has pityriasis rosea that affects the palms and or soles should be tested for syphilis. On healing, postinflammatory hyperpigmentation or hypopigmentation may result and may persist for several months. Generalized thin oval patches the palms and soles are typically unaffected in Secondary syphillis are distributed on the trunk pityriasis rosea. Varying amounts of extravasated red blood cells are appreciated within the upper dermis. Pathogenesis: Many attempts to isolate a viral or a bacterial element in patients with pityriasis rosea have been met with frustration. The use of oral erythromycin, twice a day for 2 weeks, was shown to decrease the duration of the rash. Patients with pityriasis rubra pilaris often have erythroderma with a few islands of sparing. There are several clinical variations of the condition, and it has a characteristic histological pattern, although this pattern is not always seen on microscopic examination. These islands of completely normal skin are usually small, a few centimeters in diameter, but they can be much larger. The islands typically have an angulated shape, and they are rarely perfectly round or oval. Fissuring is very common within the keratoderma and can be a source of pain and a site for secondary infection. They typically run a chronic clinical course, with most cases spontaneously resolving a few years after onset. Skin biopsy and clinical pathological correlation help the clinician make a firm diagnosis. This pattern is not always present, and sometimes it can be seen only with close inspection. Topical corticosteroid wet wraps, oral retinoids, and ultraviolet therapy have long been used as first-line agents. The retinoids are considered first-line therapy, and both isotretinoin and acitretin have been used. Cut section reveals organizing infarcts and thrombosed aneuysms in corticomedullary region. More often, it is a multisystem disease, with the skin being affected along with other organ systems. Many other organ system may be involved, and the skin features may be the presenting sign of the disease. Excisional skin biopsies of cutaneous lesions of polyarteritis nodosa show the characteristic necrotizing vasculitis of medium vessels within the deep reticular dermis. The cutaneous diagnosis of polyarteritis nodosa should alert the clinician to the possibility of systemic disease, and appropriate testing should be undertaken to evaluate for widespread disease. Most cases of polyarteritis nodosa are idiopathic, but this condition can be seen in association with viral infections, malignancy, or autoimmune disease. Coinfection with the hepatitis B virus is the most classic and most frequent association with polyarteritis nodosa. Clinical Findings: the primary cutaneous manifestation of polyarteritis nodosa is palpable purpura. The cutaneous findings tend to be spread over wide areas of the body and are not found entirely in dependent regions, as is the case with leukocytoclastic vasculitis. The patient may develop livedo reticularis of the extremities, and secondary ulcerations may form as the vasculitis progresses and causes necrosis of the overlying skin. The diagnosis of the type of vasculitis is difficult to make from clinical examination alone. Tissue sampling is needed to determine the type of vessel affected by the inflammatory vasculitis. Polyarteritis nodosa has also been shown to have nonspecific findings, such as red macules and papules, that mimic drug eruptions or viral infections. If the only organ system involved is the integumentary system, the prognosis is good, and the disease typically follows a chronic, treatable course. Once the diagnosis of cutaneous polyarteritis nodosa has been made, a systemic evaluation must be undertaken to pursue potential life-threatening involvement. If other organ systems are involved, the patient will need to undergo systemic therapy, and a multidisciplinary approach is required. This leads to a peripheral neuropathy, and it is cited as the most common extracutaneous finding in polyarteritis nodosa. The kidneys, heart, and gastrointestinal tract are also routinely affected, and any of these can lead to life-threatening complications. Renal artery aneurysms can form along the branches of the renal artery and can become thrombosed. This leads to wedge-shaped infarcts in the kidney with varying amounts of kidney function loss. Gastrointestinal arterial infarcts can also cause bowel ischemia and symptoms of an acute abdomen. The central nervous system and the musculoskeletal system are also frequently affected. Pathogenesis: the pathomechanisms that incite polyarteritis nodosa are poorly understood. Hepatitisinduced polyarteritis is believed to be partially caused by viral disruption of arterial endothelial cells as a result of circulating antigen-antibody complexes. Inflammatory cell infiltration and fibrinoid necrosis of walls of small arteries lead to infarction in various organs or tissues. Mononeuritis multiplex with polyarteritis nodosa Pattern of diverse, asymmetric nerve involvement (nonsimultaneous in onset) Unilateral ulnar nerve Unilateral radial nerve Unilateral femoral nerve Unilateral tibial nerve Bilateral peroneal nerves (Lower limb more commonly affected) Sudden occurrence of foot drop while walking (peroneal nerve) Sudden buckling of knee while going downstairs (femoral nerve) Histology: Necrotizing vasculitis of medium and small arteries in the deep reticular dermis is the hallmark of polyarteritis nodosa. The inflammatory infiltrate is predominantly made up of neutrophils with an admixture of other leukocytes. Depending on the type of skin lesion biopsied, varying amounts of skin necrosis are seen. The use of steroid-sparing agents early in the course of the disease may help decrease steroidinduced side effects. Therapy for polyarteritis nodosa induced by hepatitis B virus infection is targeted at the replicating viral particles. It has been shown to have no bearing on pregnancy outcome or on the fetus or newborn. Those patients with onset after delivery typically have a shorter course, with 1 week of severe itching followed by remission soon afterward. Prurigo gestationis has no primary lesions and manifests as diffuse itching with excoriations. Scabies infection can also be highly pruritic and can be considered in the differential diagnosis. Scabies is easily diagnosed with a scraping and microscopic evaluation of a burrow. Scabies can have its onset at any time during a pregnancy, and urticarial papules and plaques within striae are not typically seen. Herpes gestationis, also known as pemphigoid gestationis or bullous pemphigoid of pregnancy, is the most severe of all the pregnancy-associated rashes. It can begin as urticarial red plaques on the abdomen and then spread to other regions. The biggest differentiating point is that the rash of herpes gestationis will begin to blister: Small vesicles form and quickly coalesce in to larger bullae. Herpes gestationis is caused by maternal antibody formation against hemidesmosomal antigens.
Discount lioresal
Renal revascularization may be considered if blood pressure is refractory to treatment with multiple agents spasms right side of stomach lioresal 10mg on-line, or if patients have bilateral stenosis or stenosis of a solitary kidney. In the latter group, revascularization offers the most benefit if there is no intrinsic renal disease and renal function is either intact or only mildly impaired. The resistive index, measured on ultrasound, provides some indication of the degree of renal parenchymal fibrosis, and it has been shown to predict the degree of benefit following intervention. When revascularization is being considered, preoperative assessment depends on the cause of the vascular lesion. Patients with atherosclerosis, in contrast, are likely to have disease elsewhere in the vasculature and are thus at increased risk for postoperative myocardial infarction and/or cerebrovascular accident. Therefore, such patients should undergo thorough preoperative evaluation, which may include cardiac stress testing and/or carotid ultrasound. Open surgical repair, in contrast, is typically reserved for patients who have failed endovascular repair, who have comorbidities such as aortic or renal artery aneurysms, or who have large and complex lesions. The femoral or radial artery is catheterized using the classic or modified Seldinger technique. Under fluoroscopic guidance, with occasional injections of contrast material to opacify the vasculature, a flexible guidewire is advanced across the stenotic segment of the renal artery. A balloon catheter is then selected that is approximately equal to the diameter of the nonstenotic portion of the renal artery. The balloon is placed over the wire to the level of the lesion and then inflated to a high pressure. A postdilation angiogram is performed to assess the results and determine the presence of any complications, such as injury to the vessel wall. Stents are especially useful in the treatment of atherosclerotic stenoses, which tend to be rigid and may recoil after balloon dilation. Surgical revascularization consists of bypass of the stenotic lesion or, less commonly, removal of the obstructing plaque (endarterectomy). Aortorenal bypass is often performed with an autologous graft, such as the saphenous vein. In patients with severe abdominal aortic disease, in whom aortorenal bypass would be challenging or even dangerous, alternatives include splenorenal or hepatorenal bypass. If both the abdominal aorta and celiac artery have severe stenosis, the lower thoracic aorta may sometimes be used instead. Simultaneous renal revascularization and replacement of the abdominal aorta should not be attempted unless there is another indication for aortic replacement, such as a large aneurysm. Following either endovascular or surgical treatment, success is defined as elimination of the stenotic lesion on postprocedure angiogram or a postoperative blood pressure of less than 140/90. Many patients show improvements in blood pressure but do not become completely normotensive. To reduce the probability of this complication, patients should receive adequate hydration both before and after the procedure. Other complications of endovascular repair include hematoma formation near the puncture site, thrombosis of the renal artery secondary to balloon trauma or to inadequate anticoagulation following stent deployment, and restenosis of the repaired lesion. After surgical revascularization, complications include persistent stenosis, graft thrombosis, and restenosis of the repaired lesion. Patients who have recurrent stenosis after endovascular repair often require surgical revascularization. The surgical approach may be more challenging because of perivascular inflammation associated with the initial endovascular procedure; however, this difference does not appear to lower the probability of a successful outcome. Patients with recurrent stenosis after an initial surgical revascularization may undergo another surgical procedure with an alternative bypass route. Possible indications include chronic pyelonephritis, chronic renal obstruction, extensive untreated nephrolithiasis, trauma, and ischemic nephropathy secondary to renal artery stenosis. Radical nephrectomy, meanwhile, refers to the surgical removal of the kidney along with the perinephric fat, renal fascia, ipsilateral suprarenal gland, and ipsilateral retroperitoneal lymph nodes. Radical nephrectomy is the treatment of choice for patients with renal malignancies. Both simple and radical nephrectomy may be performed using either an open or laparoscopic technique. In many cases, the surgeon will approach a simple nephrectomy with the same surgical strategy as a radical nephrectomy. Simple nephrectomies, however, may be technically more difficult because of the tissue fibrosis that commonly occurs secondary to chronic inflammation. The anterior subcostal and chevron incisions are the standard incisions for the transperitoneal approach. For both, the patient is placed in supine position, and an incision is made approximately two fingerbreadths below the costal margin. The incision extends from the anterior axillary line either to the xiphoid process (anterior subcostal incision) or to the opposite anterior axillary line (chevron incision). The dissection is carried down through the flank musculature (latissimus dorsi, external oblique, internal oblique, transversus abdominis), anterior rectus fascia, and rectus abdominis muscles. The colon is mobilized medially, and then the plane between the colonic mesentery and renal fascia is developed. The renal hilum is approached anteriorly, and the vessels are ligated using a combination of silk suture and surgical clips. A midline transperitoneal incision may be used for patients undergoing exploratory laparotomy for trauma, during which an indication for nephrectomy may be discovered. It is not a common incision in planned surgeries on the kidney, however, because the surgeon is often forced to operate caudal to the kidney. Such an approach can make it difficult to achieve control of the hilar vessels, especially in obese patients. A thoracoabdominal incision is used when radical nephrectomy is required in a patient with a large, rightsided upper pole tumor. The incision begins in the eighth or ninth right intercostal space near the angle of the rib and is carried medially to the midpoint of the left rectus muscle. The dissection is carried down to the pleura and diaphragm, which are circumferentially incised to expose the liver. After the kidney is removed, the diaphragm must be sutured, a chest tube placed, and the pleura repaired. This approach is associated with a considerable risk of injury to the lung, and there is also significant postoperative morbidity associated with the use of a chest tube. Therefore, this approach should be reserved only for large, right-sided upper pole tumors that cannot be safely removed with an anterior subcostal or chevron incision. The major advantages to transperitoneal open access include the excellent exposure to the renal hilum and a large surgical field, whereas the disadvantages include the risk of adjacent organ injury and of prolonged ileus. The patient is placed in the lateral position after induction of anesthesia, with the table flexed at the level of the twelfth rib to maximize the space between the costal margin and the iliac crest. An incision is made directly over the eleventh or twelfth rib starting posteriorly at the lateral edge of the erector spinae muscles. The rib chosen for dissection and possible removal is the one nearest the hilum, which can be determined most accurately on cross-sectional imaging. The transversus abdominis muscle and tendon of origin, as well as the thoracolumbar and transversalis fascia, are then incised to expose the paranephric fat. The peritoneum is identified and swept medially with manual dissection to separate it from the paranephric fat, which is then dissected to expose the renal fascia. Peritoneum and contents reflected Perinephric fat Paranephric fat Renal fascia (capsule of Gerota) D. The kidney is pulled laterally to reveal the renal vessels and ureter, which are ligated. A dorsal lumbotomy incision can be used when retroperitoneal access to the kidney is desired in patients who have fibrosis associated with prior abdominal or flank incisions. The incision is started over the erector spinae muscles at the level of the twelfth rib, then continued downward and laterally toward the iliac crest. The thoracolumbar fascia is incised lateral to the quadratus lumborum and erector spinae muscles, which are retracted medially. An advantage of this approach is that it avoids transection of the abdominal muscles; however, it provides limited access to the hilum, making it difficult to control vascular complications. The colon is reflected from the peritoneal wall and the anterior surface of the renal fascia. The cranial end of the renal fascia is freed from the stomach, spleen, and tail of the pancreas. The kidney is put on lateral tension to facilitate identification of the gonadal vein and ureter.
Cheap 25mg lioresal
The natriuretic effect of this action spasms near liver cheap lioresal 10mg on line, however, is largely offset by upregulation of distal Na+ reabsorption sites, such as the thick ascending limb, that possess proton-independent Na+ transport mechanisms. Moreover, the increased solute load delivered to the macula densa stimulates afferent arteriolar vasoconstriction, reducing the glomerular filtration rate. This response improves tissue oxygenation but is limited by the ensuing respiratory alkalosis. Finally, the increased urine flow through the distal nephron promotes K+ secretion through flow-sensitive maxi-K channels. Such kaliuresis, however, rarely leads to hypokalemia because metabolic acidosis stimulates K+ efflux from cells in exchange for H+ influx. Such reabsorption is essential for the maintenance of a high medullary interstitial solute gradient, which permits urine concentration in the collecting duct (see Plate 3-15). Because the distal nephron is unable to reabsorb the large sodium load rejected from the thick ascending limb, the diuresis associated with these drugs is profound. In addition, loop diuretics also have weak diuretic effects elsewhere in the nephron. In the proximal tubule, for example, some loop diuretics weakly inhibit carbonic anhydrase. In addition, loop diuretics both increase uric acid reabsorption (by promoting fluid losses, which enhances proximal uric acid reabsorption) and decrease uric acid secretion (by competing with it at the organic anion secretion pathway). Second, the increased urine flow through the cortical collecting duct upregulates flow-sensitive maxi-K channels. As a result, there is chronic dilation of the afferent arteriole despite high flow rates through the nephron, which enhances fluid losses. In addition, there is chronic secretion of renin, which leads to increased synthesis of angiotensin and aldosterone. The result is a further increase in K+ secretion, which contributes to the development of hypokalemia, and an increase in H+ secretion, which can result in metabolic alkalosis. The efficacy of loop diuretics can become limited over repeated doses for several reasons. In part, this effect occurs because the distal nephron increases its reabsorptive capacity, blunting the efficacy of loop diuretics and markedly increasing salt retention between doses. Because the vast majority of Na+ reabsorption occurs in earlier nephron segments, particularly the proximal tubule and thick ascending limb, thiazides induce only a modest degree of natriuresis. Some agents, however, are also weak carbonic anhydrase inhibitors (see Plate 10-2) and thus partially inhibit Na+ reabsorption in the proximal tubule. Second, the increased urine flow through the cortical collecting duct up-regulates apical maxi-K channels. Finally, volume losses lead to aldosterone release, which further increases distal K+ (and H+) secretion. Second, volume losses stimulate reabsorption of Na+ and Cl- in the proximal tubule, enhancing the gradient for paracellular calcium reabsorption. Like the loop diuretics, thiazides likely exert this effect by increasing proximal tubular reabsorption (secondary to fluid depletion) and decreasing proximal tubular secretion (by competing with uric acid on the organic cation secretion pathway). By inhibiting solute reabsorption in the distal nephron, thiazides prevent maximal urine dilution. In addition, significant fluid losses can trigger release of antidiuretic hormone (see Plate 3-17). Second, increased flow rates through the distal nephron stimulate K+ secretion through apical maxi-K channels. Most diuretics-including carbonic anhydrase inhibitors, loop diuretics, and thiazide diuretics-upregulate distal K+ secretion through several mechanisms. First, these agents interfere with Na+ reabsorption in more proximal portions of the nephron, which increases the load that reaches the distal nephron. Second, these agents cause volume loss, which activates the renin-angiotensin-aldosterone system. Finally, diuretics increase urine flow rates through the distal nephron, which stimulates K+ secretion through apical maxi-K channels. Meanwhile, aldosterone receptor blockers remain in the plasma to act at the basolateral surface of principal cells. Nonetheless, they can be useful in combination with other classes of diuretics because of their effects on potassium homeostasis. They can also help offset the increase in distal sodium reabsorption that occurs with the use of other diuretics. Through the same mechanisms used to reduce K+ secretion, these agents also reduce H+ secretion in to the distal nephron. In brief, renin is released from juxtaglomerular cells in response to decreased renal tubular flow, sympathetic input, or decreased stretch of afferent arterioles. These agents are powerful antihypertensive medications, but they are also capable of slowing the progression of renal disease. The mechanism by which these agents protect the kidneys is not fully known, but it likely relates in part to their effects on glomerular hemodynamics. Although this response allows the kidneys to temporarily maintain high levels of filtration function, it is ultimately maladaptive because the high intraglomerular pressure causes capillary wall damage, leading to worsening proteinuria and glomerulosclerosis. By relieving constriction of the efferent arterioles, these drugs lower intraglomerular pressure, reducing proteinuria and protecting the glomerular capillary walls. For example, they also inhibit the metabolism of bradykinins, which promote vasodilation and upregulate prostaglandin synthesis. First, because they do not interfere with bradykinin metabolism, these agents are associated with a much smaller risk of cough and angioedema. Because many renal diseases have essentially indistinguishable clinical findings, renal biopsy is often crucial for establishing the correct diagnosis and devising an effective treatment plan. The procedure is generally uncomplicated and, in most cases, can safely be performed by a nephrologist at the bedside. In patients with mild proteinuria (1 to 2 g/day) that has no obvious cause, such as diabetes mellitus, a renal biopsy may be performed to establish a definitive diagnosis. The exact threshold for biopsy differs across practitioners and depends on individual clinical judgment. Although tubulointerstitial disease commonly causes mild proteinuria, a biopsy is generally not required to establish the diagnosis. If, however, the patient has a diagnosed systemic illness that is known to cause nephrotic syndrome, a renal biopsy is typically not required. Examples include patients with long-standing diabetes mellitus and concurrent diabetic retinopathy, or patients with amyloidosis seen on a biopsy of another affected organ system. In patients with gross or microscopic hematuria, the initial workup should focus on urologic abnormalities, such as nephrolithiasis, neoplasm, or infection. The presence of dysmorphic red cells, proteinuria, and renal insufficiency, however, strongly points toward glomerular disease. Many renal diseases are associated with microscopic hematuria, including essential hematuria, acute interstitial nephritis, IgA nephropathy, membranoproliferative glomerulonephritis, postinfectious glomerulonephritis, lupus nephritis, Structure of typical spring-loaded biopsy needle Various biopsy devices are available with different needle widths and lengths. A kidney biopsy is essential for establishing the correct diagnosis and determining an optimal treatment plan. The differential diagnosis for such patients includes thin basement membrane disease, mild IgA nephropathy, and hereditary nephritis. A kidney biopsy is typically not performed, however, because treatment is not instituted unless there is significant proteinuria or renal insufficiency. Patients who have undergone renal transplant and subsequently develop renal failure should have a biopsy if their renal function does not improve after provision of intravenous fluids. Some centers also routinely take biopsies from transplanted kidneys at predetermined time points, even in the absence of overt dysfunction because some renal disease may initially be clinically silent. Ultrasound is used to locate kidney and determine optimal site and angle of needle insertion.
Herba Verbenae (Verbena). Lioresal.
- What other names is Verbena known by?
- Are there safety concerns?
- Sore throat, asthma, whooping cough, chest pain, abscesses, burns, colds, arthritis, itching, and other conditions.
- How does Verbena work?
- What is Verbena?
- Treating sinusitis when taken as a combination product containing gentian root, elderflower, cowslip flower, and sorrel.
- Dosing considerations for Verbena.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96132
Cheap lioresal master card
With time spasms posterior knee lioresal 25mg without prescription, the production of hair pigment decreases, and the hair becomes dull gray or white. This process is unpredictable in a given individual, and even those within the same family may show striking differences in hair color change. Terminal hair is thick hair that is present on the scalp, axilla, and groin and in the beard region in men. Vellus hair is the fine, thin, lightly pigmented hair that can be found in most areas of the body where terminal hair is not present. Lanugo hair is present during fetal development and is predominantly seen in premature infants. Reversion of vellus hair and terminal hair back to lanugo hair is a sign of anorexia nervosa. This growth phase is followed by the catagen phase, which is a short (2 week) transition period during which the hair follicle transforms from a growing, functioning hair in to a club hair. This is followed by the telogen phase, which lasts approximately 2 months and ends with shedding of the club hair. Anagen hairs have a floppy, pigmented end that is easily distinguished from the telogen hair. Telogen hair is termed club hair because of its depigmented bulb at the proximal end. Catagen hairs are almost impossible to identify because they appear somewhere in the spectrum between anagen and telogen hair. The length of the anagen phase is responsible for the overall length of the hair: the longer the anagen phase, the longer the hair can grow. This Outer root sheath Hair bulb Papilla Fibrous root sheath Outer root sheath Inner root sheath Eosinophilic cuticle Cortex of the hair Hair follicle Sebaceous duct Sebaceous gland External root sheath Dermis Arrector pili muscle Epidermis Light micrograph of a hair and its follicle near the epidermis in transverse section* Light micrograph of thin skin close to the epidermis* *Micrographs reprinted with permission from Ovalle W, Nahirney P. The hair follicle is remarkably capable of regeneration after the hair has entered in to telogen phase. An unknown signal causes the hair follicle stem cells, which are located in the bulge region, to differentiate and begin producing another hair, restarting the anagen phase. The bulge region is an area found in approximation to the insertion of the arrector pili muscle in to the hair follicle. Histological examination of a cross section of a terminal hair shaft reveals a complex architecture. The hair follicle undergoes trichohyalin keratinization, which is different from the keratohyalin keratinization of the epidermis. All 20 nails have the same chemical makeup; the only difference is in the size of the nail. The nail matrix is the portion of the nail unit that is responsible for production of the nail plate. The matrix lies a few millimeters behind the proximal nail fold, which ends as the cuticle (eponychium), and extends under the nail bed. Under the proximal nail bed, the nail matrix can often be appreciated as a half-circle termed the lunula. Any damage to the nail matrix can potentially cause a temporary or permanent nail dystrophy. The distal nail matrix is responsible for producing the ventral portion of the nail plate. The proximal nail matrix is responsible for producing the dorsal surface of the nail plate. It is theorized to be protective to the underlying nail matrix and distal phalanx, as well as being helpful with grasping and dexterity of the fingertips. The nail plate is firmly attached to the underlying nail bed via tiny, vertically arranged interdigitations. The nail plate is an avascular structure, and the underlying nail bed is highly vascular. The nail bed is attached to the epidermis via the proximal nail fold and the cuticle, as well as the lateral nail folds on either side of the nail. Damage to the cuticle, whether by accident or during manicures or pedicures, can increase the risk of bacterial or fungal infection within the nail or the skin of the nail folds. Improper trimming of the lateral aspects of the nail plate may lead to an ingrown toenail (onychocryptosis). Damage to this portion of the nail unit may allow for bacterial or fungal infections to take hold under or within the nail plate. Fingernails grow on average 3 mm per month, and toenails grow a bit more slowly, on average 1 mm per month. Both hair keratin and skin keratin types have been described to comprise the various portions of the nail unit. The hair keratin Ha1 and the skin keratins K5, K6, K16, and K17 make up the majority of the keratin types found in the adult nail. The rounded shape of the free edge of the nails is dictated by the shape of the lunula. After avulsion of a nail, the free edge of the new nail grows parallel to the lunula. These disorders are most often seen in isolation, with no underlying systemic abnormalities. All skin examinations should include evaluation of the nails, because many systemic diseases can manifest with nail findings, and these clinical signs may be the first signs of underlying disease. Clinical Findings: Telogen effluvium is a form of nonscarring alopecia that can result in dramatic thinning of the scalp hair but rarely causes total hair loss. It has been found to be induced by a number of stressors that cause the anagen hairs to abruptly turn in to telogen hairs. This results in an abnormal number of hairs in the telogen phase and an increase in hair shedding. Anagen effluvium is a specific form of alopecia that is typically induced by chemotherapeutic agents. Alkylating agents such as busulfan and cisplatin and the antitumor antibiotics (bleomycin and actinomycin D) are frequently responsible. Other agents have been implicated, including the antimetabolites, topoisomerase inhibitors, and vinca alkaloids. The anagen phase hair is particularly sensitive to these chemotherapy agents, which inhibit proliferation of rapidly dividing cells. This form of hair loss is easier to diagnosis, because a history of taking one of the implicated chemotherapeutic agents is critical in making the diagnosis. The presence of scarring, the form of inflammation, and the ratio of anagen to telogen hairs are evaluated. In telogen effluvium, a normal number of hairs are present without evidence of miniaturization. The ratio of telogen to anagen hairs is increased from the normal 5 to 10 telogen hairs per 100 anagen hairs to more than 20 per 100. Biopsies of anagen effluvium show a normal ratio of anagen to telogen hairs, but the anagen hairs exhibit some evidence of abnormality, either broken shafts or apoptosis of the hair. Many medications have been reported to induce telogen effluvium, and the clinician should evaluate all medications taken. Dietary habits, especially crash dieting and anorexia nervosa, may lead to telogen effluvium. The hair follicles are not scarred and eventually grow back after the stressors have been resolved. Because the beginning of hair loss may be delayed after the stressful event, by 3 to 4 months on average, the patient may not realize the relationship. Treatment: the treatment of telogen effluvium consists of determining the etiology and educating the patient. Once this has been accomplished, patients need to be educated and reassured that telogen effluvium almost always resolves within 6 to 8 months, and they may expect full regrowth. Supplemental vitamins and topical minoxidil have not been vigorously tested as therapies for telogen effluvium, and their use cannot be scientifically advocated. Referral to a psychological counselor may be appropriate in situations such as eating disorders. Telogen hair Club hair with minimal pigment in the bulb Telogen effluvium has a broad range of etiological causes. Anagen effluvium is related to the use of chemotherapeutic agents to treat systemic cancer.
Syndromes
- Warm, moist compresses to reduce inflammation and pain
- Latex rubber
- Joint pain
- Multiple endocrine neoplasia (MEN) II
- Fluid buildup in the knee joint
- After 24 hours, slowly return to your regular activities.
- Complete blood count
- Paralysis or weakness in the muscles of the face
- Pens, pocketknives, and eyeglasses may fly across the room.
- Fungal infection
Order lioresal 25mg online
Thus if amyloidosis is strongly suspected based on clinical history muscle relaxant with least side effects cheap 25mg lioresal with visa, these superficial biopsies may be performed before renal biopsy. In chronic infections, eradication of the focus of infection with appropriate measures, including antimicrobial agents, should be the focus. An example of this approach is the compound eprodisate, which attaches to the glycosaminoglycan binding sites of amyloid fibrils in tissues, leading to fibril destabilization. It is predominantly a disease of young women, with a female to male ratio of roughly 10: 1. It also varies by race and ethnicity, being more common in African Americans, African Caribbeans, and Asians than in Caucasians. These racial differences are likely attributable to both genetic and environmental factors. Factors associated with increased risk of renal disease include a younger age, male gender, and non-Caucasian race. It appears that a confluence of genetic, hormonal, and environmental factors promotes the development of autoantibodies. These antibodies form pathologic immune complexes that trigger complement fixation and inflammation, leading to tissue damage. A major event in the pathogenesis of this disease is thought to be prolonged, inappropriate exposure of self-antigens to the immune system. This sensitization process is thought to occur in the context of dysregulated apoptosis or impaired phagocytic clearance of apoptotic/necrotic cells. Subsequent failure to silence autoreactive lymphocytes allows ongoing production of antibodies that bind these self-antigens. Renal disorder is defined as the presence of either proteinuria (>500 mg/24 hr or 3+ protein on dipstick) or cellular casts. For research purposes, 4 of 11 criteria are required to make the diagnosis; however, in clinical practice, many patients are diagnosed with a lupus-spectrum disease without meeting this threshold. For example, it is unclear if the autoantibodies cross-react with glomerular antigens, or if they first form circulating antigen-antibody complexes that subsequently deposit in the glomerulus. In either case, the presence of the immune complexes leads to ongoing glomerular inflammation. Among affected patients, nearly 100% will have proteinuria, 80% will have microscopic hematuria, 45% to 65% will have the full nephrotic syndrome, and 40% to 80% will have reduced renal function. Once the presence of lupus nephritis is clinically evident, proper management often requires further characterization of the glomerular lesion. Although the clinical signs sometimes correlate with the nature and extent of glomerular disease, these associations are unreliable. For example, a given level of azotemia may reflect either active, reversible proliferative nephritis, or a burnt-out, sclerosed kidney without active disease. In the former, aggressive immunosuppression may markedly ameliorate kidney function; in the latter, it will impart no benefit and subject the patient to needless risk. Thus a kidney biopsy is often essential to clarify the disease process and guide management. The major indications for this procedure include abnormal or increasing proteinuria (>500 mg/24 hr), an active urinary sediment, or renal insufficiency. It is defined as positive staining for three immunoglobulins (IgG, IgM, and IgA) in addition to complement components C3 and C1q. Although a few isolated subepithelial or subendothelial immune deposits may be visible by immunofluorescence or electron microscopy, none should be present on light microscopy. Active lesions are those with evidence of ongoing inflammation, such as hypercellularity, karyorrhexis, fibrinoid necrosis, and cellular crescents. In contrast, chronic lesions consist of tissue that has generally undergone irreversible scarring, with features such as glomerulosclerosis, fibrous adhesions, and fibrous crescents. In addition, there is often a more diffuse distribution of the subendothelial immune deposits. When the subendothelial deposits are prominent enough to be seen by light microscopy, they impart a classic "wire-loop" appearance to the glomerular capillaries. Because the subepithelium is a major component of the protein diffusion barrier, patients with type V disease usually have more severe proteinuria than those with the other disease classes. Frank nephrotic syndrome is common and increases the risk of thromboembolic disease. Though active immune damage is no longer occurring, prior inflammation has irreparably damaged nearly every functioning nephron. Patients will invariably have significantly impaired renal function that will not benefit from immunosuppression. The relative frequency of these classes varies across studies based on geographic location, patient makeup, and local biopsy practices. Hyperlipidemia should also be treated if present, which may require the use of a statin drug. The use of nonsteroidal antiinflammatory drugs should be assessed and, if present, limited. Prolonged or unprotected exposure to sunlight should be rigorously avoided because it can trigger lupus flares. The two drugs best studied for induction therapy are pulse cyclophosphamide and mycophenolate. The preponderance of data from clinical trials suggests that the two regimens are equivalent in achieving remission, usually at rates of 60% to 80%. Immunosuppressive regimens involving corticosteroids in conjunction with cyclophosphamide, cyclosporine, or mycophenolate have all been tried with varying results. In addition, a significant number of patients will be unable to tolerate treatment, suffer serious adverse events from immunosuppression, or have disease that is refractory to therapy. These plasma cell clones hypersecrete monoclonal (M) proteins, which can be either intact immunoglobulins, usually of the IgG or IgA type, or free or light chains (known as BenceJones proteins). The disease is generally diagnosed during the sixth decade of life, and up to half of patients will experience renal complications. Renal disease typically occurs as a result of the hypersecretion of free light chains, which have a direct toxic effect on the kidneys; however, urate nephropathy and direct plasma cell infiltration of the renal parenchyma can occur as well. These proteins are filtered at the glomerulus, and the majority are reabsorbed by proximal tubular cells and subsequently catabolized. In multiple myeloma, light chains may be present in such overwhelming excess that they overcome the reabsorptive capacity of the nephrons. The high concentrations of light chains in the tubular lumina may in turn lead to a phenomenon known as "cast nephropathy. First, light chains form obstructive casts that can cause acute or chronic renal failure. Second, light chains accumulate in proximal tubule cells because of resistance to degradation, which leads to tubular epithelial cell injury (and, in turn, impaired proximal light chain reabsorption and increased delivery to the distal tubule). Second, the light chains must bind to Tamm-Horsfall protein, normally produced in the thick ascending limb. Light chain casts are thus usually found in the distal tubule because of the increased light chain concentration in this segment (secondary to fluid reabsorption in more proximal segments), as well as the presence of Tamm-Horsfall protein. Likewise, diarrheal illness, hypercalcemia, and diuretics are precipitants that likely act by causing volume depletion. Less commonly, the M proteins may deposit in the glomerulus, where they disrupt the protein filtration barrier. In addition, the light chains may sometimes cause extensive damage to the proximal tubule, resulting in more generalized reabsorption defects (renal Fanconi syndrome). A typical presentation in a patient without known myeloma is several weeks of oliguria, weakness, fatigue, lethargy, and lower extremity edema with newly diagnosed severe renal insufficiency. In contrast, a patient with a known myeloma diagnosis will often be noted to have an asymptomatic rise in creatinine on routine laboratory evaluation. Some of the known precipitants, listed previously, may be noted in the recent clinical history. The dipstick measurement of proteinuria is generally unremarkable because it detects only albumin, whereas these patients excrete large quantities of light chains. Photometry of a urine specimen after the addition of a precipitant such as sulfosalicylic acid or trichloroacetic acid, however, will reveal the presence of all urine proteins. More than a gram of protein on a quantitative photometric urine specimen with a negative dipstick for albumin is suggestive of paraproteinuria. Immunofixation electrophoresis of serum and urine should be performed to confirm and identify the paraproteins.
Buy genuine lioresal
Many different chemical peels and dermabrasion techniques have been used to help decrease the appearance of lentigines spasms and spasticity order lioresal amex. With the proliferation of medical laser devices in dermatology, lasers with unique wavelengths have been developed to target the melanin in lentigines. These laser devices have shown promise in lightening and removing solar lentigines. The name "sebaceous cyst" has been used to describe these cysts, although this is a misnomer, because epidermal inclusion cysts are not derived from sebaceous epithelium. The cysts can occur anywhere on the body except the palms, soles, glans, and vermilion border. Clinical Findings: Most epidermal inclusion cysts are subcutaneous nodules that vary in size from 5 mm to more than 5 cm. From this punctum, drainage of white, cheese-like material, which represents a buildup of macerated keratin debris, can occur. Most small epidermal inclusion cysts are asymptomatic, and they rarely cause a problem. When the cyst contents enter the dermis, the keratin sets off a massive inflammatory reaction, which manifests clinically as edema, redness, and pain. The main differential diagnosis for a ruptured epidermal inclusion cyst is a boil or furuncle. Ruptured epidermal inclusion cysts are almost never infected, although infection can occur within a long-standing ruptured cyst that has not been treated. The main differential diagnosis of an unruptured, noninflamed epidermal inclusion cyst is a pilar cyst. Pilar cysts do not have an overlying central punctum, and this is the easiest means of differentiating the two cyst types. Histology: the epidermal inclusion cyst is a true cyst with an epithelial lining of stratified squamous epithelium and an associated granular cell layer. Pathogenesis: the epidermal inclusion cyst is derived from the infundibulum of the hair follicle. Epidermal inclusion cysts occur as the result of direct implantation of epidermis in to the underlying dermis; from there, the epidermal component continues to grow in to the cyst lining. Many researchers have looked at the roles of ultraviolet light and human papillomavirus infection in the etiology, but no definitive conclusions on either have been drawn. Such trauma could cause rupture of the cyst wall and set off an inflammatory reaction. Small cysts can be cured by a complete elliptical excision, making sure to remove the Suprabulbar Isthmus Bulge area. The cyst lining is formed by stratified squamous epithelium, which contains a granular cell layer. Inflamed cysts should be treated initially with an incision and drainage technique. The resulting cheesy-white macerated keratin debris is removed with lateral pressure, and a curette is used to break apart internal loculations. The resulting cyst cavity can be packed or left open until the patient returns in 2 to 3 weeks for definitive removal of the cyst lining by excision. Intralesional triamcinolone is very effective in decreasing the inflammation and pain in these inflamed cysts. Long-standing cysts should be cultured and the patient given the appropriate antibiotic therapy based on the culture results. Clinical Findings: the epidermal nevus typically manifests in childhood as a solitary linear plaque. Epidermal nevi do not have a race predilection, and they can be found equally in males and females. This type of nevus is not melanocytic in nature; rather, it is composed of a proliferation of keratinocytes. The nevus initially has a smooth surface and develops a mamillated or verrucal surface over time. Epidermal nevi appear to occur most commonly on the head and neck region but can occur anywhere. If found on the scalp, an epidermal nevus can mimic a nevus sebaceus and can be associated with hair loss, but more commonly it does not cause alopecia. Some are large, encompassing the entire length of an extremity, and still others cover a large percentage of the body surface area. These larger epidermal nevi are more likely to be associated with systemic findings, such as underlying bone abnormalities. The epidermal nevus syndrome is a rare disorder associated with a large or widespread epidermal nevus and many systemic findings. These children often present with neurological deficits, including seizures, and developmental delay. The finding of a widespread epidermal nevus in an infant should alert the clinician to the possibility of this syndrome and the need for a multidisciplinary approach to patient care. Pathogenesis: the epidermal nevus is a hamartomatous proliferation of the epidermal components. These lesions are believed to be caused by a developmental abnormality of the ectoderm. The epidermal nevus syndrome has not been shown to have any appreciable inheritance pattern and is believed to be sporadic in nature. The exact genetic defect is unknown; it is most likely a result of genetic mosaicism. The involvement of fibroblast growth factor has been studied, but no firm conclusions have been made. A variable degree of pigmentation is seen in the involved keratinocytes, but this is not a disorder of melanocytes, and the number of melanocytes is normal. Hyperkeratosis, acanthosis, papillomatosis, and basilar hyperpigmentation are prominent. The same architecture as an epidermal nevus is seen; however, prominent vacuolar changes are seen within the epidermis. Treatment: Small, isolated epidermal nevi can be removed with shave removal technique. They have a high rate of recurrence with this technique, but recurrence may take many years. The advantages of this technique are that it is relatively easy, noninvasive, and quick, and it provides an opportunity to histopathologically evaluate the tissue for any evidence of epidermolytic hyperkeratosis. The disadvantage of shave removal is that it is appropriate only for small epidermal nevi. Cryotherapy with liquid nitrogen has been used successfully, but it may leave unsightly hypopigmentation in darker-skinned individuals and should be used with caution. Laser resurfacing, dermabrasion, and chemical peels have been used to help smooth out the appearance of epidermal nevi. They are derived from the hair follicle epithelium and show a unique mantle differentiation. Clinical Findings: these tumors, when seen, are often solitary skin growths on the head and neck. The main differential diagnosis clinically includes compound nevus, basal cell carcinoma, fibrous papule, and other types of adnexal tumor. Solitary fibrofolliculomas are usually found incidentally on routine skin examination. Some patients present with a slightly enlarging new papule, often expressing concern for or fear of skin cancer. Other cutaneous constellations of this autosomal dominantly inherited syndrome include trichodiscomas and skin tags. The most important aspect of diagnosing this syndrome early is to screen patients for the possibility of renal tumors, both benign and malignant. Renal oncocytomas are the most common malignant renal tumor seen in this syndrome. Another rare renal cancer, the chromophobe renal cell carcinoma, also may be seen.
Buy lioresal online now
Unique risks of intralesional steroids for periocular hemangiomas include central retinal artery occlusion or iris depigmentation back spasms 7 weeks pregnant discount generic lioresal canada. Although many hepatic hemangiomas are asymptomatic, a subset carries a high morbidity and mortality rate. They may be solitary or multiple and may be seen in association with cutaneous hemangiomatosis or be an isolated finding. Ulcerating Lesions Hemangiomas in mucosal (perineum, lip) or intertriginous areas or at pressure points. Other required therapies may be intralesional or systemic steroids or flashlamp pulsed dye laser. Simple but helpful measures to comfort the infant with a painful ulcerating hemangioma include twice-daily sitz baths, air drying, and construction of foam rubber cushions with custom-designed cutout areas to relieve direct pressure on the painful area. In addition to therapy directed toward the primary tumor, antifibrinolytic agents, antiplatelet agents, and heparin are helpful. Consensus guidelines have been established for management of hereditary hemorrhagic telangiectasia, including bleeding problems. Nonhepatic hemangiomas, prone to develop a high-flow component, include those involving the parotid gland, upper arm, chest wall, scalp, and (rarely) upper lip. These findings should alert the treating physician to monitor the hemodynamic status of these patients by careful physical examination and frequent follow-up evaluation. Overall, a minority of patients develop high cardiac output states requiring intervention, including diuretics, inotropic agents, or an embolization procedure. The normal physiological changes of pregnancy include increased plasma volume and cardiac output, increased venous pressure, leg edema, and venous stasis. This is also an issue when oral contraceptives are considered to treat dysmenorrhea or other gynecological problems. Preliminary data suggest that the risk of obstetric complications, especially preeclampsia and thrombotic events, is higher in women with vascular anomalies of the lower extremities. Psychosocial Issues Despite the benign clinical course of infantile hemangiomas in the majority of patients, and the tendency of these lesions to naturally involute, families of patients frequently undergo stress related to social interactions and medical care. However, support from extended family appeared to be an important factor in coping. Oster studied mother-infant interactions, comparing facial expressions in infants with facial anomalies (including vascular anomalies) and controls, showing that affected infants were capable of effective emotional communication by showing a wide range of facial expressions. Many families were dissatisfied with medical care for two reasons: (1) imprecise treatment plans, which are inherent with the nature of many hemangiomas, and (2) what the parents perceived as insensitivity on the part of physicians. The results suggested that the families, rather than the infants, experienced emotional and psychological distress. In this sense, local family support groups organized at some medical centers, as well as national support networks and meetings, are increasingly providing the necessary stability for families and patients. The Internet has played an enormous role in assisting the exchange of information, as well as enabling families and physicians to connect with one another (Table 64-5). As the field becomes more familiar, older patients who had hemangiomas as infants and children are becoming role models, publishing their experiences and speaking at meetings-further enforcing the optimistic outcome. Furthermore, adult patients with vascular malformations are networking with younger patients. Orthopedic Concerns Orthopedic issues associated with vascular anomalies involve those relating to limb-dimension discrepancies. Limb-length discrepancies may be associated with quadriceps fatigue, hip and lower back pain, or secondary scoliosis. Serial assessment of limb-length data and bone ages at regular intervals is recommended. Interventions include shoe lifts or epiphyseodesis (surgical growth plate closure) for more modest discrepancies; however, for discrepancies predicted to be greater than 5 cm, or in patients who have already reached skeletal maturity, limb shortening and lengthening are the only options to equalize limb lengths. Therapeutic options include custom shoes, ray or digital resection for macrodactyly of the fingers or toes, debulking procedures, and amputation for severe and otherwise unmanageable cases of hypertrophy. Patients with vascular anomalies can also develop joint contractures due to a mass effect from the lesion. Physical therapy with stretching exercises may be adequate to relieve symptoms; however, direct sclerotherapy plus or minus surgical excision may be required. Gynecological Issues in Patients with Vascular Malformations Some women with vascular anomalies have such severe menorrhagia that they undergo hysterectomy. Various reviews and guidelines for treatment are available in the medical literature. Via selective photothermolysis, flashlamp pulsed dye laser selectively destroys superficial dermal vessels while sparing surrounding tissue. Further information regarding laser therapy of subglottic hemangiomas is discussed later. Previously, corticosteroids were the most common medication for proliferating hemangiomas necessitating medical intervention. An immediate improvement in the hemangiomas led to a pilot study that confirmed this perceptive observation. This has revolutionized therapy for infantile hemangioma warranting treatment, and since then several papers have been published, the majority documenting its efficacy. Topical or systemic antibiotics may be warranted for superinfected ulcerated hemangiomas. Thyroid adenoma, thyroid carcinoma, angiosarcoma, or breast cancer may arise in patients who received radiation therapy (an outdated treatment) for cutaneous hemangiomas of infancy. Concomitant cutaneous hemangiomatosis with hepatic type 2 infantile hepatic hemangioendothelioma (angiosarcoma) has been reported. More severe bleeding from the genitourinary tract may require a combined approach with angiography-guided embolization, laser, or sclerotherapy. Large symptomatic thromboses may require anticoagulation, as might the coagulopathy associated with severe cases. Quiescent vascular anomalies may become more problematic secondary to local trauma, infections, or hormonal fluctuations such as puberty, menstruation, and pregnancy. These changes usually manifest as increased fullness of the malformation as well as pain. Use of hormonal birth control can elicit undesirable thromboses and/ or pain, thus alternative means of contraception are advised. Evaluation of patients with lymphedema involves physical examination and radiological studies including lymphoscintigraphy for extremity involvement. Lymphatic abnormalities involving the mouth and gastrointestinal tract are prone to infection, so patients with lymphatic malformation in these sites benefit from diligent oral hygiene and, occasionally, rotating prophylactic antibiotic regimens. Microcystic lymphatic malformations of the head and neck may respond well to sclerotherapy (doxycycline, bleomycin, picibanil) or surgery, or a combined approach. A multicenter prospective nonrandomized trial demonstrated the efficacy of picibanil in the treatment of macrocystic cervicofacial lymphatic malformations, and the results were corroborated by further reports. Liposuction for lymphedema has been successful in selected patients with recalcitrant disease. Interferon alpha was used in the 1990s, with improvement of endangering hemangiomas, but use of this agent has fallen out of favor, primarily because of concerns about potential neurotoxicity. Some surgeons prefer to defer surgery until the hemangioma has undergone substantial involution, with the rationale that the surgery will be less complex and esthetically more favorable. Other surgeons advocate early intervention to possibly prevent medical complications or avert psychological stresses on the patient and/or family. In any case, a well-planned strategy with medical, laser, and surgical management decisions discussed amongst multidisciplinary physicians can provide excellent results. The developmental interactions between mesoderm and ectoderm ultimately determine the nature of human skin. Interestingly, neural tissue and epidermal tissue are both derived from the ectoderm. It is believed that calcium signaling is critical in determining the fate of the ectoderm and its differentiation in to either epidermis or neural tissue. At approximately 4 weeks after conception, a single layer of ectoderm is present, surrounding a thicker layer of mesoderm. Two weeks later, this ectodermal layer has separated in to two different components: an outer periderm and an inner basal layer, which is connected to the underlying mesoderm.