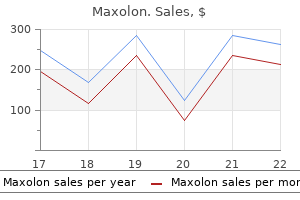
Cheap 10 mg maxolon
Lymphomas constitute 10% and the rest 5% are rhabdomyosarcoma diet while having gastritis generic maxolon 10 mg, malignant mixed salivary tumor or malignant chordoma. Other nodes include along the spinal accessory in the posterior triangle of neck and supraclavicular nodes. Distant metastases: Bone (thoracolumbar vertebrae, pelvis and femoral heads), lung and liver. In cases of strong suspicion, nasopharynx may be approached transpalatal and a strip of mucosa and submucosa from the region of fossa of Rosenmuller is taken for histology. Less weight is given to Level 1 and 2 nodes (even 6 cm nodes are considered N1 category). Coronal views assess petroclinoid fissure, foramina (lacerum, ovale, rotundum or spinosum) or cavernous sinus. Axial views evaluate retropharyngeal, paranasopharyngeal, pterygomaxillary space and infratemporal fossa. Large soft tissue density mass causing complete obliteration of nasopharyngeal lumen. Opposing lateral fields include primary tumor, upper neck and third anterior matched field irradiate lower cervical and supraclavicular nodes. Systemic chemotherapy: It may be used as palliation for distant metastases or in radiation failures. Single and combination chemotherapy (cicplatinum/5-flurouracil) have been used as an adjunct to radiation. Unilateral tumors of nasopharynx and paranasal sinuses and retro-orbital region and bilateral is caused by hyperthyroidism exophthalmos. Causes: They include Congenital and familial Trauma: Maxillofacial injuries, complication of endoscopic sinus surgery. Infection: Complications of rhinosinusitis such as subperiosteal abscess, orbital cellulitis and cavernous sinus thrombosis. Benign tumors: Inverted papilloma, ethmoidal polyps and fungus, juvenile nasopharyngeal angiofibroma and fibrous dysplasia. Malignant tumors: Carcinoma and sarcomas of nose, paranasal sinuses and nasopharynx. It is a median recess that is located in the posterior wall of the nasopharynx in the adenoid mass. Notochord, which is attached to the endoderm in the area of nasopharynx, produces this invagination pouch. Endoscopic excision of juvenile nasopharyngeal angiofibroma- a comprehensive approach. Facial translocation approach to infratemporal fossa and cranial base in extensive angiofibroma: a review of 7 cases. The management of these tumors needs a multidisciplinary team, which consists of head and neck cancer surgeon, reconstructive surgeon, speech and swallowing therapist, prosthodontist, dentist and radiation and medical oncologist. Some of the varieties are listed below: Squamous cell carcinoma: Squamous cell carcinoma is the most common variety of carcinoma. It shows various grades of differentiation: well, moderately and poorly differentiated. Minor salivary gland tumors: Minor salivary gland malignancy is mostly seen on the palate and fauces. Lymphoma: Hodgkin and non-Hodgkin arise from the tonsil and base of tongue in young adults and children. Racial-ethnic: Among men, highest rate is in blacks followed in descending order by whites (non-Hispanic), Vietnamese and native Hawaiians. Diet: Fresh fruits and vegetables may reduce the relative risk of cancer of upper aerodigestive tract. Chemotherapy Early: Throat irritation, burning sensation with acidic food, neck swelling and odynophagia. Late: Dysphagia, dysarthria or hot pota to voice, trismus, obstructive airway symptoms, deafness (serous otitis media due to Eustachian tube obstruction), and weight loss. Subtle mucosal abnormalities bleed after palpation w tumors of oropharynx Spread Local: the deeply infiltrative ulcer involves tongue musculature, epiglottis and pre-epiglottic space, tonsil and its pillars and hypopharynx. Lymphatic: Most patients (70%) have unilateral or bilateral cervical metastases (usually jugulodigastric nodes) at the time of first consultation. Biopsy and examination under general anesthesia: Examination and palpation under anesthesia provide better idea of the extent of lesion, which is usually far more extensive than it appears. Tumors, which are radiosensitive (such as anaplastic carcinoma, lymphoepithelioma or lymphoma) are usually treated with radiotherapy. T1 and T2 squamous cell carcinoma with N0 or N1 neck: Surgical excision with block dissection followed by radiotherapy if needed. Clinical features Neck swelling: Mostly patient presents with metastases in cervical nodes. Early symptoms: They are mostly ignored by the patient for a long time and include sore throat, feeling of lump in the throat and slight discomfort on swallowing. Late features: They indicate advanced diseases and include referred earache, dysphagia, bleeding from the mouth, and hot pota to voice. Deeply infiltrative ulcer with induration can be seen and palpated on base of tongue. The lesion may involve tongue musculature, epiglottis and pre-epiglottic space, tonsil and its pillars, and hypopharynx. Local: Tumor may involve soft palate and pillars, base of tongue, pharyngeal wall, parapharyngeal space, hypopharynx, pterygoid muscles or mandible. Late features are bleeding from the mouth, halitosis (fetor oris), pain and trismus (due to invasion of pterygoid muscles and mandible). Radiotherapy: For early and radiosensitive tumors irradiation includes cervical nodes. Surgical excision combined with block dissection and skin grafting: Approach may be lateral pharyngotomy with or without mandibular osteotomy. Yellowish cystic swelling visible through the oral cavity on depressing the tongue 448 parapHaryngEal tumorS (fig. Commonly seen tumors include deep lobe of parotid, neurilemmoma, carotid body chemodectoma, lipoma or aneurysm of internal carotid artery. They usually present with a bulge in lateral pharyngeal wall, which may distort the pillars and soft palate and mimic oropharyngeal neoplasm. Laterally, loss of fat planes indicates encasing of internal and external carotid arteries and approaching internal jugular vein Source: Dr Ritesh Prajapati, consultant Radiologist, anand, Gujarat Section 5 fig. Left side styloid process is thick and right side styloid process is very long Source: Dr Jayesh Patel, consultant Radiologist, anand, Gujarat Clinical Highlights 1. Forget not that the lower classes, the ignorant, the poor, the illiterate, the cobbler, the sweeper, are thy flesh and blood, thy brothers. The various subsites involved in descending order of frequency are pyriform sinus, postcricoid region and posterior pharyngeal wall. Benign tumors of laryngopharynx are very rare and include lipoma (relatively more common), papilloma, adenoma, fibroma and leiomyoma. For the detail anatomy see Chapter Anatomy and Physiology of Oral Cavity, Pharynx and Esophagus. The current trend is emerging towards the organ sparing techniques with combined chemotherapy and irradiation. Tumor invades any of the following: thyroidcricoid cartilage, hyoid bone, thyroid gland, central compartment of soft tissue such as infrahyoid strap muscles and subcutaneous tissue. Locally: Superiorly to vallecula and base of tongue Inferiorly to postcricoid region Medially to aryepiglottic folds and ventricles Laterally to thyroid cartilage, thyroid gland or soft tissue mass in the neck. Spread Pharynx and esophagus Local: Cervical esophagus, arytenoids, or recurrent laryngeal nerve at cricoarytenoid joint. Surgery Growth limited to pyriform fossa and not extending to postcricoid region: Total laryngectomy and partial pharyngectomy often combined with elective or prophylactic block dissection of lymph nodes. Growth extending to postcricoid region: Total laryngectomy and pharyngectomy with block dissection and myocutaneous flaps or stomach pull-up for pharyngoesophageal reconstruction. Inspiratory stridor in advanced tumor occurs due to pressure on larynx and bilateral recurrent laryngeal nerves involvement.
Order maxolon overnight delivery
In beginning there may be burning sensation at the back of nose gastritis diet mercola buy maxolon cheap, nasal stuffiness, rhinorrhea and sneezing. Nasal watery discharge is profuse and may become mucopurulent due to secondary bacterial invasion (Streptococcus haemolyticus, pneumococci, Staphylococcus, Haemophilus influenzae, Klebsiella pneumoniae and Morexella catarrhalis). Complications are occasional and include sinusitis, pharyngitis, tonsillitis, bronchitis, pneumonia and otitis media. In rhinitis associated with exanthemas (measles, rubella, chicken pox) secondary infection and complications are more frequent and severe. Efficient in symptom control: Decongestants, anticholinergics, and first generation antihistamines (diphenhydramine, chlorpheniramine, clemastine). Antihistamines: Symptoms can be easily controlled with antihistaminics and nasal decongestants. Antihistamines may impair psychomotor performance often without sedation or other noticeable symptoms. Nonspecific features are facial tenderness on palpation over sinuses or the maxillary teeth. Method: Middle meatus is decongested with a pledget of cotton soaked in topical decongestant. The findings may include obstruction of osteomeatal complex, polypoid changes and bony abnormalities. The recovery of bacteria in a density of at least 104 colony-forming units/ml is considered significant. Completely opaque sinuses usually (about 85%) have pus in them, while 50% sinuses that show thickened mucous membrane with central aeration have pus in them. The exudate, which is serous in beginning, becomes mucopurulent and causes destruction of mucosal lining. Ethmoidal pain, which may be aggravated by movements of the eyeball, is localized over the bridge of the nose, medial and deep to the eye. Expensive antibiotics are often prescribed when equally effective and less expensive alternatives are available. Second line of antibiotics in cases of first line failure (or severe symptoms, suspected complications and resistance). Then antibiotic based on the report of culture and sensitivity of aspirated fluid from sinus must be started. The following causes are considered in patients who fail to respond to appropriate antibiotics: Tumors, granulomatous diseases, allergic rhinitis and invasive (immunocompromised patients) and allergic fungal sinusitis. Diphtheritic rhinitis: Diphtheria, which is rare these days, may be primary or secondary to faucial diphtheria. A grayish tenacious membrane, removal of which causes bleeding, covers the inferior turbinate and the floor of nose. The symptoms may persist if nasal epithelium has been damaged and the infection supervenes. Endoscopic sinus surgeries are successfully employed in managing empyema of paranasal sinuses. It exposes the floor of frontal sinus, the bone of which is removed with a cutting drill. A plastic catheter is inserted and fixed and sinus is irrigated with normal saline two or three times daily. The patency of frontonasal duct can be determined by adding a few drops of methylene blue to the irrigating fluid and its exit can be confirmed in the nose. There occurs hyperemia and edema of mucous membrane with hypertrophy of seromucinous glands and increase in goblet cells. Infections: Viral, bacterial, fungal and parasitic infections of neighboring organs such as pharynx (tonsils and adenoids) and upper teeth. Hypersensitivity: Allergy IgE mediated and non IgE mediated hypersensitivities, aspirin hypersensitivity with asthma and polyps and vasomotor factors. Duration: Chronic rhinosinusitis is diagnosed if patients have symptoms for more than 12 weeks. Sinuscopy: Nasal endoscopy may show allergic or cobble stoned mucosa (sarcoid), presence and location of purulent discharge and polyps. The presence of just only sinus mucosal abnormalities does not mean much and is not an indication for surgery as these findings may be incidental in asymptomatic patients also (fig. Cystic fibrosis or primary ciliary dyskinesia: If the polyps are present in children then cystic fibrosis or primary ciliary dyskinesia syndrome must be ruled out. Fungal infection: In cases of very sticky, rubbery, yellow, tan or green mucus, special stains for fungus should be performed. Antibiotics and steroids usually broad-spectrum antibiotic is started immediately and then changed as per the report of culture and sensitivity. They help to keep the nose free from viscid secretions and also remove superficial infection. In cases of associated allergic fungal sinusitis, desensitization and antifungal agents may be helpful. Circumferential mucosal thickening and polyp formation in bilateral maxillary sinuses Source: Dr ritesh Prajapati, Consultant radiologist, Anand, Gujarat 304 because it may lead to rhinitis medicamentosa and affect mucociliary clearance. Massive polyps are usually not cured with antibiotics and recurrence usually occurs after surgery. With endoscopic sinus surgery, almost all the paranasal sinus lesions can be managed successfully. Maxillary Sinus (See chapter Operations of Nose and Paranasal Sinuses) Antral puncture and irrigation. A window, which provides aeration and free drainage, is made in the inferior meatus. After removing the irreversible diseases, another window is created between the antrum and inferior meatus. Frontal Sinus Intranasal drainage procedures facilitate free drainage through the frontonasal duct and include correction of deviated septum, removal of polyps or anterior part of middle turbinate, intranasal ethmoidectomy and treatment of maxillary sinusitis. In some cases it is desirable to obliterate the sinus after removing all diseased and normal mucosa of the sinus. External ethmoidectomy: Ethmoid sinuses can be approached through medial orbital incision. Depending on the course of disease it is divided in to acute (10 days to < 3 weeks), subacute (3 weeks to < 12 weeks) and chronic (> 12 weeks). The anatomic obstruction can be due to turbinate (hypertrophic or enlarged, concha bullosa or pneumatized and paradoxical bend), septum (deviation and spur), polyps, enlarged adenoids and mucosal inflammation from allergy, infection and irritation. If the symptoms of purulent discharge, facial pain, nasal obstruction and daytime cough persist longer than 10 days, a diagnosis of acute sinusitis should be considered. Surgical treatment: It is rarely needed except in cases of orbital or intracranial complications. These round or oval cysts grow concentrically and expand very slowly over 10 years or more.
Proven 10 mg maxolon
Anterior perfOiating branches from the saphenous vein may require ligation to ensure safe retraction gastritis jaw pain purchase 10 mg maxolon. The crural fascia is incised 1 em posterior to the tibia, and the fascial incision is extended proximally to the level of the semitendinosus tendon. The underlying medial head of the gastrocnemius muscle is retracted posteriorly, exposing the neurovascular bundle in the proximal aspect of the incision. More proximal exposure can be obtained by dividing the tendons of the semitendinosus, gracilis, and sartorius muscles. Exposure of the artery is facilitated by the use of vessel tapes to elevate the artery above the vein in to the incision. Because the tunnel is created blindly, the actual pathway through the musculature of the thigh can only be estimated. Care should be taken to ensure that the graft is brought between the heads of the gastrocnemius muscle at the level of the knee joint; grafts routed through this muscle tissue may be compressed during muscle co:nt:Iaction. A vertical incision is made over the fibular head and extended distally over the proximal third of the fibula. On deepening the incision, one notes the tendon ofthe biceps femoris muscle inserting on the superior aspect of the fibular head. The biceps tendon is divided, and the common peroneal nerve with its deep and superficial branches is carefully dissected and retracted anteriorly. The biceps tendon and fibular collateralligameut are divided to begin mobilization of the head of the fibula. The fibular shaft can then be transected with no shears and the bone removed from its bed. Tmnssection of the fibular shaft with rib shears is aided by elevation of the proximal fibula. To prevent kinking, grafts should be routed such that they cross the knee at the midpoint ofthe lateral femoral condyle. These disorders include popliteal entrapment syndrome, cystic adventitial disease, and traumatic intimal flaps:from posterior knee dislocations. An S-shaped incision is preferred to avoid the deforming scar contractures associated with simple vertical incisions across the posterior knee. The tibial nerve is the most superficial major midline structure, and the peroneal nerve follows the biceps femoris tendon obliquely toward the head of the fibula. Distal exposure may be enhanced at this point by retracting the two heads of the gastrocnemius muscle apart; this may require vertical division Medial sural n. The tibial and peroneal nerves are best retracted laterally, exposing the ensheathed popliteal vessels lying medial to the tibial nerve. The popliteal artery terminates in a true trifurcation approximately 3% ofthe time. The anterior tibial artery arises first, leaving a common tibioperoneal trunk that bifurcates in to the posterior tibial and peroneal arteries. Fascia tlfthe Leg A dense fascial layer, continuous with the fascia lata of the thigh, encircles the leg. Both the posterior tibial and peroneal arteries lie in the deep posterior compartment and send penetrating branches to the overlying superficial posterior compartment and to the adjacent lateral compartment. The unyielding nature of the crural fascia and its tight adherence at the knee and ankle make the closed compartmental spaces susceptible to buildup of pressure after leg injury. Such compartment syndromes can result in irreversible neuromuscular damage if not relieved by prompt fasciotamy. The gastrocnemius muscle group including the small plantaris muscle) attaches to the calcaneus through the la:rge Achilles tendon. Their tendons pass behind the medial malleolus under the flexorretinaculum lacinate ligament). The tendons of the foot evertors, the peroneus longus and brevis muscles, pass behind the lateral malleolus and are ~~~-:-Extensor cil~rum longus m. The latge tibialis anterior muscle lies adjacent to the tibia, arising from that bone and the adjacent interosseous membrane. From proximal to distal, these are the extensor digitorum longus, extensor hallucis longus, and peroneus tertius muscles. The anterior tibial vessels and deep peroneal nerve lie between these muscular columns and are directly accessible from an anterior approach. The superficial posterior compartment contains the bulky superficial gastrocnemius/soleus complex that fuses to form a common termination in the calcaneal tendon. From the apex at the fibular head, the shorter lateral fibular origin descends in a straight line down the fibula. The proximal diagonal portion originates from the soleal line of the tibia and is intenupted by the hiatus for the popliteal vessels and tibial nerve. The diagonal muscle fiber disposition of the lateral and medial origins should be used to advantage when stripping the muscle off the bone. The distal third of the peroneal artery runs within and behind the belly of the flexor hallucis longus muscle. It terminates in a variable branch perforating through the distal interosseous membrane and in calcaneal branches. Their tendons pass under the superior peroneal retinaculum posterior to the lateral malleolus. The importance of this muscle group in vascular surgery lies in the fact that it must be mobilized from the fibula to resect that bone for lateral access to the posterior compartment vessels and when simultaneous decompression of all compartments through a single incision is necessary. The bias of the muscle fibers dictates stripping upward toward the knee, whereas the dominant bias of the interosseous membiane mandates stripping in the opposite direction. Confining dissection to the periosteal plane in the distal leg prevents damage to the nearby peroneal vessels. The peroneal compartment is bounded by septa connected to the fibula, and contains the superficial peroneal nerve lying close to the bone at this level. The posterior tibial and peroneal vessels and the tibial nerve lie between the deep muscles and deep septum at the level of the calf. The small saphenous vein lies subcutaneously in the posterior midline, soon to be joined by the sural nerve, seen here deep to the fascia between the gastrocnemius bellies. The narrowed span of the deep fascia over the Achilles tendon puts the medial fusion point posterior to the tibia, allowing direct access to the deep compartment directly over the plantar flexors and posterior tibial neurovascular bundle. The tibialis posterior and flexor digitorum longus muscles are mostly tendinous in the relatively larger deep posterior compartment, whereas the flexor hallucis longus muscle remains fleshy and muscular right down to the ankle. The peroneal artery, which is beginning to diminish above the distal tibiofibular syndesmosis, lies on the interosseous membrane covered by the mass of the flexor hallucis longus muscle. The deep peroneal nerve remains in the anterior compartment with the anterior tibial artery, whereas branches of the superficial peroneal nerve have penetrated the deep fascia of the lateral compartment to lie in the subcutaneous plane. The tendon of the extensor hallucis longus muscle crosses over the anterior tibial neurovascular bundle, and the arteiy continues on to the dorsum of the foot as the dorsalis pedis artery. The tibial nerve lies posterior to the posterior tibial artery as the neurovascular bundle enters the foot. At the upper end ofthe interosseous membrane, the anterior tibial artery passes in to the anterior compartment. The tibioperoneal trunk lies on the upper part of the tibialis posterior muscle and divides in to the smaller peroneal artery laterally and the posterior tibial artery medially. Posteromedially, the posterior tibial artezy and tibial nerve lie between the flexor digitorum longus and flexor hallucis longus muscles before passing beneath the flexor retinaculum to enter the foot. The lateral plantar artery bows laterally, crosses beneath the proximal metatarsals, and joins the plantar branch of the donlalis pedis artery. In the midfoo~ the don~alis pedis artery gives off a lateral tarsal artery that anastomoses with branches of the anterior lateral malleolar artery and the more distal arcuate branch of the donlalis pedis artery, as well as with the lateral plantar artery. Small medial tarsal branches anastomose with the anterior medial malleolar and medial plantar arteries. The peroneal arte:ry sends a perforating branch through the distal interosseous membrane. There are communicating branches between vessels ofthe two arches, passing between the metatarsals proximally and distally. The relationships of the vessels of the foot to the bones of the foot are shown in.
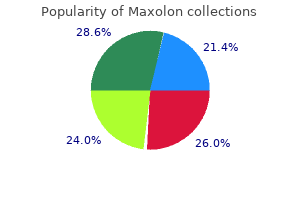
Maxolon 10 mg low price
Among postmenopausal women who had used hormones within the previous 5 years (compared to never-users) gastritis diet 800 discount 10mg maxolon fast delivery, the relative risks were 1. No significant increase in risk was noted for women who had stopped using postmenopausal hormone therapy 5 years or more previously, regardless of duration. Of note, this increase in risk was significantly higher among lean women than among obese women (who would naturally have higher levels of endogenous hormones than lean women) 281. Data on how recently a woman has used hormones and risk of breast cancer are sparse because many Epidemiology 15 earlier studies did not distinguish current from past users. Estrogen plus progestin the addition of a progestin to estrogen regimens became increasingly common from the 1980s to 2000; this addition minimizes or eliminates the increased risk of endometrial hyperplasia and endometrial cancer associated with using unopposed estrogens. The impact of added progestin on the risk of breast cancer has been evaluated rigorously only in the last 15 years; overall, the results of these studies indicate that added progestin at the doses typically used in postmenopausal hormone-replacement therapy does not have a protective effect against breast cancer 281,1616. Because widespread use of estrogen plus progestin is so recent, few data are currently available to evaluate the effect of different formulations, doses, or schedules of use of progestin on risk of breast cancer. In addition, unopposed estrogen therapy increases the risk of breast cancer, with risk augmenting with duration of use. Furthermore, this rise in risk is greatest among lean women, who have low levels of circulating estrogen due to their low body mass. Adiposity the relationship between adiposity and breast cancer depends on menopausal status: in affluent industrialized populations with high rates of breast cancer, measures of body adiposity are inversely related to risk of premenopausal breast cancer, but positively related to risk of postmenopausal breast cancer. Heavier premenopausal women, even those at the upper limits of what are considered to be healthy weights, have more irregular menstrual cycles and increased rates of anovulatory infertility 1181, suggesting that their lower risk may be due to fewer ovulatory cycles and less exposure to ovarian hormones. The lack of a stronger association has been surprising because plasma concentrations of endogenous estrogens are nearly twice as high in obese postmenopausal women as in lean women 547. Another reason for failing to appreciate a greater adverse effect of excessive weight or weight gain on risk of postmenopausal breast cancer is that the use of postmenopausal hormones obscures the variation in endogenous estrogens attributable to adiposity and elevates risk of breast cancer regardless of body weight. Weight loss in adult years and after menopause has been studied in a limited fashion, partly because few women lose weight and avoid regaining it. Women who lose 10 kg or more and maintain this weight loss have a 40% reduction in their risk of breast cancer. Most studies have focused on postmenopausal breast cancer, although there is also some evidence for a protective effect of physical activity on premenopausal disease. Recent evidence shows that the benefit of activity is independent of race or ethnicity 123. The strongest protection against breast cancer has been reported in women maintaining consistent high levels of activity from menarche through adult life 123,888. Nutrition There is some evidence of a decrease in the risk of breast cancer in individuals with healthy dietary patterns, although a recent Invasive breast carcinoma: Introduction and general features meta-analysis and large cohort studies found no evidence of increased risk of breast cancer associated with "Western" unhealthy dietary patterns 27,508,671 and high intakes of fruit and vegetables are not associated with a reduced risk of breast cancer in recent studies 156. Rapid growth and greater adult height, partly reflecting total food intake in early years, are associated with an increased risk. Similarly, a high body mass, also linked to a high total caloric intake, or intake not counterbalanced by caloric expenditure, is a risk factor for postmenopausal breast cancer. Consistent evidence suggests that higher consumption of meat, particularly red or fried/browned meat, is associated with a higher risk of breast cancer 671. Alcohol the consumption of alcohol has been consistently associated with a moderate increase in the risk of breast cancer 1345, 1386. Evidence suggests that high intake or high blood levels of folate may decrease risk 1624. Similarly, the combined data from 53 epidemiological studies showed no relationship between smoking and breast cancer among women who do not drink alcohol 538. However, substantial additional evidence has accumulated in the past decade, and a review conducted in 2009 by a Canadian task force concluded that active smoking is causally related to both preand postmenopausal breast cancer. Furthermore, this task force concluded that second-hand smoke ("passive smoking") is causally related to premenopausal breast cancer, but that the data were insufficient to allow a conclusion to be made for postmenopausal breast cancer 287. Results to date do not show any applications for these methods to either demarcate risk or offer strategies for prevention 1101. Imaging Detection Mammography is the baseline imaging method for the detection of breast cancer in women aged > 40 years. Britton cancer is most commonly manifested on mammography as an ill-defined or spiculated mass, with or without associated calcifications, but can also present as architectural distortion, focal asymmetric density or calcifications alone. Ultrasound can be added to improve sensitivity in women with mammographically dense breasts. Mammography is rarely helpful in younger women and its use in women aged < 40 years is confined to those with proven breast cancer. Ultrasound alone is the method of choice for imaging the breast in women aged < 40 years. Further assessment and staging Imaging should always be used to assess both breasts before any treatment is implemented. Mammography and ultrasound are complementary for the pretreatment assessment of the size, extent and presence of multifocality of breast cancer. The vast majority of breast cancers should be diagnosed without the need for surgical biopsy using imagingdirected needle sampling; ultrasoundguided core biopsy is the method of choice. Ultrasound is also used routinely to assess the axilla at the time of presentation, with biopsy of any abnormal lymph nodes. Rarely, breast carcinoma will present as enlargement of the axillary lymph nodes in the absence of any abnormality in the breast. All the symptoms of breast cancer may also be caused by benign breast disease, so evaluation with imaging and histological sampling with core biopsy or fine-needle aspiration cytology are indicated to establish a definitive diagnosis. The imaging workup of a breast mass should include diagnostic mammography with a marker placed over the lesion to ensure that it is visualized on the film. A spiculated mass is the classic appearance of cancer, but cancers may also be visualized as architectural distortion or well-circumscribed masses. The false-negative rate of combined mammography and ultrasound is quite low, ranging from 0% to 3% 952,1353. Unless the presence of an unequivocally benign diagnosis such as a cyst is established based on imaging, tissue sampling is M. When the results of the physical examination, mammography, and needle biopsy are all benign and concordant, the risk of malignancy is extremely low. However, if any one of these modalities is non-concordant or cannot be evaluated, surgical biopsy is indicated. A Non-specific density in the axillary tail of the right breast, undetected at screening. B 18 months later: an ill defined, high-density lobulated tumour of > 30 mm is evident and mammographically appears to be malignant. Assessment of histological grade has become more objective as the original methods by Patey & Scarff 1077 and Bloom & Richardson 151 have been modified by Elston & Ellis 377. After the adoption of these changes, many studies have demonstrated a significant association between histological grade and survival of patients with invasive breast carcinoma 1136, 1146. Grade is a powerful prognostic factor and should be included as a component of the minimum dataset for histological Table 1. Simpson reporting of breast cancer 1091 and is a key component of clinical decision-making tools such as the Nottingham Prognostic Index 146 and Adjuvant! Method of grading Three tumour characteristics are evaluated: tubule formation as an expression of glandular differentiation; nuclear pleomorphism; and mitotic counts. A numerical scoring system of 1 to 3 is used to ensure that each factor is assessed independently (Table 1. Glandular formation is assessed over the whole tumour and is a low-power assessment.
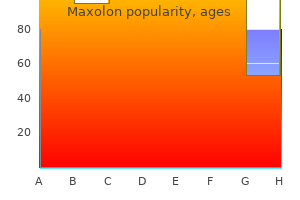
Buy discount maxolon 10 mg on line
Thumb abduction is now restored and gastritis diet options order maxolon canada, if necessary, a volar capsulodesis of a hyperextended nonarthritic metacarpophalangeal joint is performed or arthrodesis in 25 degrees of flexion is done if painful arthritis is present. After suture of the dorsal capsular flaps, the first dorsal compartment is loosely closed over the abductor pollicis longus and extensor pollicis brevis tendons. The incision is closed, with care to avoid the branches of the superficial radial nerve. The limb is kept elevated, and a thumb spica short-arm cast or thermoplastic splint is applied after 4 to 6 days and worn for 4 to 6 weeks. Guarded motion and pinch and grasp activities using various exercise devices are then started. Special considerations in reconstruction of the basal joints of the thumb include the following. Hyperextension of the metacarpophalangeal joint of the thumb contributes to the adduction tendency of the metacarpal and prevents proper abduction of the metacarpal and seating of the implant. Plication of the stretched out volar plate can be done by advancing a central portion and suturing it to the remaining intact portions or by placing a suture anchor in the bone and securing it. If the hyperextension ranges from 10 to 20 degrees, temporary fixation with a Kirschner wire is indicated; if it is greater than 20 degrees, stabilization with either palmar capsulodesis or arthrodesis is essential. Adduction of the first metacarpal, if severe and untreated, unbalances the thumb and seriously affects the result of resection arthroplasty. If the angle of abduction between the first and second metacarpals is not at least 45 degrees, the origin of the adductor pollicis muscle must be released and likely the metacarpophalangeal joint arthrodesed. Transverse skin incision over necks of metacarpal bones to expose extensor tendons. The disease process attacks the joints, ligaments, and tendons, causing painful and disabling deformities. Fortunately, developments in joint reconstruction and replacement have made it possible to restore hands deformed by crippling arthritis to a nearly normal appearance and useful function. Ideally, arthroplasty should produce a joint that is pain free, mobile, stable, and durable. Four methods of reconstruction for arthritic joints of the hand have emerged: arthrodesis, resection interposition arthroplasty, resurfacing joint replacement, and flexible implant resection arthroplasty. Arthrodesis works very well for the thumb at the metacarpophalangeal joint level and for the lesser fingers at the proximal and distal interphalangeal joint level, but lack of motion is debilitating in the lesser fingers at the metacarpophalangeal joint level and rarely used. Resection interposition arthroplasty can improve motion by shortening skeletal structures, lengthening soft parts, providing new gliding surfaces, and allowing the development of a new supportive fibrous joint capsule. The chief disadvantage of the procedure in the metacarpophalangeal joints is the unpredictability of results. Resurfacing joint replacement has proved successful in knee and hip joints, but early results in finger joints have been mixed because of dislocation, bone resorption, and implant loosening. More recently, newer designs are proving useful in patients with osteoarthritis and early rheumatoid arthritis where the soft tissue balance is still relatively normal. In flexible implant resection arthroplasty, a flexible silicone implant is used as an adjunct to resection arthroplasty. This method was devised in 1962 and has been used successfully in several hundred thousand patients. The basic concept of flexible implant resection arthroplasty can be summarized as "bone resection + implant + encapsulation = functional joint. The joint is thus rebuilt through a healing phenomenon called the "encapsulation process. Capsule and volar plate resection and release of interossei attachment to capsule and proximal phalanx. After extensive soft tissue release (including division of collateral ligaments if necessary), intramedullary canal prepared to receive implant stem using air drill with special blunt-tip burr to prevent cutting through cortex. This allows for realignment of severely dislocated and angulated joints after the significant bony and soft tissue resection needed in severe rheumatoid deformities. Postoperative mobilization is tailored to the amount of instability present after reconstruction; delay in mobilization increases stability. This is typically acceptable as the flexors greatly overpower the extensors and prolonged immobilization in extension is rapidly overcome, giving a stable, mobile grip. Soft tissue balance is key to preventing the recurrence of deformity and to implant breakage, dislocation, and failure. Flexor tendon may be drawn up (after incision of its sheath) to determine if partial synovectomy and release of sheath are indicated. If indicated, radial collateral ligament reconstructed with distally based flap composed of collateral ligament and radial half of palmar plate. In certain patients with progressive rheumatoid arthritis who have insufficient bone stock to support the implant, a simple resection arthroplasty or arthrodesis with a bone graft is preferable. Surgery is also contraindicated if postoperative hand therapy is not available or adequate. Proper staging of the reconstructive procedures is important in planning the treatment program. Procedures in the upper limbs should be delayed in patients who also need lower limb reconstruction that will necessitate the use of crutches. After hand reconstruction, patients should avoid excessive manual labor and awkward hand weight bearing when using crutches. In deformities of the metacarpophalangeal joint associated with severe wrist involvement, the wrist should be treated first. In the patient with rheumatoid arthritis, tendon repair and synovectomy of tendon sheaths must precede arthroplasty of the metacarpophalangeal joints by 6 to 8 weeks. If both metacarpophalangeal and proximal interphalangeal joints are involved, the metacarpophalangeal joint is usually treated first or simultaneously if only operating on one or two metacarpophalangeal joints. In swan-neck deformity, the metacarpophalangeal and proximal interphalangeal joints are reconstructed at the same stage. Implant arthroplasty for both the metacarpophalangeal and proximal interphalangeal joints of the same digit is usually avoided if possible. Several procedures can be performed during one operation, depending on the time available. Surgery for the thumb, proximal interphalangeal and distal interphalangeal joints, wrist, and, occasionally, the elbow joint can often be combined. A limb procedure should be limited to no more than 2 hours, and an axillary or supraclavicular block is recommended if the tourniquet time exceeds 1 1 2 hours. Small joints may also be injected with corticosteroids or other agents during surgery. Sagittal fibers of dorsal hood reefed in overlapping fashion on radial side to centralize long extensor tendon and maintain correction. With joint in extension, neither metacarpal nor proximal phalanx should impinge on implant. In the normal hand, a delicate balance exists among the muscles and tendons and the bones and joints through which they interact. The proximal transverse arch crosses the carpal area, with its center at the capitate. The distal transverse arch is formed by the metacarpal heads and is centered on the head of the third metacarpal. The digits make up the longitudinal arches, each with its apex at the metacarpophalangeal joint. The result is capsular distention, destruction of cartilage, subchondral erosions, loosening of ligamentous insertions, impaired tendon function, and, finally, joint disorganization, subluxation, and dislocation. A break in the longitudinal arch system causes collapse deformities of the multiarticular structure of the hand, disturbing the stability and balance necessary for prehension. Use of the hand in daily activities (functional adaptation) causes further deformity. This joint not only flexes and extends but also abducts and adducts; it also has some passive axial rotation. Rheumatoid arthritis commonly involves the metacarpophalangeal joints, resulting in increased ulnar deviation of the fingers, subluxation of extensor tendons, and palmar subluxation of joints (see Plate 4-21). The flexor tendons enter the fibrous sheath at an angle, exerting an ulnar and palmar pull that is resisted in the normal hand. When the rheumatoid process distends and weakens the capsule and ligaments of the metacarpophalangeal joint, the forces generated by the long flexor tendons across the sheath during flexion may elongate these supporting structures.
Generic maxolon 10mg otc
Indicators of poor outcome are following: Main guide to prognosis: Histological tumor thickness (Breslow) in mm from the granular cell layer to the deepest identifiable melanocyte gastritis daily diet proven maxolon 10 mg. Treatment: Wide surgical excision along with block dissection, if nodes are involved. It is multifocal in origin and primarily affects skin but may also be seen in the oral cavity. Abbey-Estlanderflap: It is used to reconstruct defects in cases of carcinoma of lip angle (commissure). Role of tumor thickness in carcinoma of oral tongue with clinically negative neck. Patient must be inquired about the habits of chewing paan, sopari or tobacco, smoking and alcohol. Examination Box 1 shows the methods of examination and nasopharyngeal structures, and pathological findings seen during examination and their causes. Anterior rhinoscopy: Some part of the nasopharynx can be seen in decongested nose (with vasoconstrictors); even on anterior rhinoscopy. Posterior rhinoscopy: Posterior rhinoscopy provides fragmented view of nasopharynx, which is mentally reconstituted by the examiner. Retraction of soft palate with catheters: It facilitates postnasal mirror examination in some difficult cases and requires good local or general anesthesia. In this method, a soft rubber catheter is passed through each nostril and then taken out from the mouth through the oropharynx. This method has been Pharynx and Esophagus becoming obsolete with the advent of sinuscope and flexible nasopharyngolaryngoscopy. Endoscopy: Endoscopy gives a bright and magnified view of the nose and nasopharyngeal structures. Rigid nasal endoscope (sinuscope or rhinoscope): They are available in different sizes and angles and introduced through the nose after instilling or spraying local anesthetic and decongestant. There is uniform congestion of the pillars, tonsils and pharyngeal mucosa in acute tonsillitis; however, congestion of only anterior pillars indicates chronic tonsillitis. Ulcer and proliferative growth may extend to or from the tonsil, base of tongue, and the retromolar trigone. Deviation of the uvula and soft palate occurs to the healthy side in cases of vagus palsy, which may be associated with paralysis of posterior pharyngeal wall that manifests as a "curtain effect" (the paralyzed side moves like a sliding curtain to the healthy side). Valleculae are two shallow depressions that lie between the base of tongue and the epiglottis. The traumatic causes include caustic ingestions and pill-induced ulcers (see chapter Disorders of Esophagus). Contraindications: Barium swallow is not used when aspiration is present or suspected. Malignant lesions: They show irregular narrowing of lumen along with mucosal destruction, ulceration and shouldering. Benign strictures: Smooth narrowing (may be at multiple sites) of a short or long part of esophagus. Modified Barium Swallow this procedure, which is usually conducted by radiologist in conjunction with the speech pathologist, evaluates coordination of swallow reflex and cause, and severity of laryngotracheal aspirations. The patient is given varying thickness of barium suspension, which mimics different food consistencies. Esophageal varices: Irregular filling defects (like a string of pearls) in lower portion of esophagus. Air contrast images: Double contrast study Patient is upright, and slightly left anterior oblique. It can be divided in to two types: oropharyngeal (difficulty in transferring food bolus from oropharynx to upper esophagus) and esophageal (difficulty in transporting bolus through the body of esophagus). Oropharyngeal dysphagia: It is characterized by coughing, choking and regurgitation immediately after initiation of swallowing. Neurological: Brainstem lesions (pseudobulbar palsy), multiple sclerosis, or myasthenia gravis. Esophageal dysphagia: It may occur due to mechanical obstruction or motility disorders. To confirm the diagnosis of esophageal motility disorders (achalasia or diffuse esophageal spasm) suggested by endoscopy or barium swallow. Liquids/solids: More with liquids (paralytic lesions), more with solids, and progressing to liquids (malignancy). The lesions of oral cavity and pharynx can be seen during physical examination whereas esophageal causes require investigations such as barium swallow and esophagoscopy. Sudden onset: Foreign body or impaction of food on a stricture or malignancy, and neurological lesions. Computed radiography and digital radiography: In this filmless technique, image is captured on an array of digital elements, and is read directly in to a computer. Advantages: Soft tissue differences: It can emphasize subtle soft tissue differences even if the image is suboptimally exposed. Invert image: Radiodense elements appear whiter than radiolucent elements on traditional films but computer technology can invert the image and some aspects of anatomy, and pathology can be visualized better. Barium swallow: For malignancy, cardiac achalasia, strictures, diverticulum, hiatus hernia or esophageal spasms. Ultrasound: Transesophageal echosonography can evaluate the depth of malignant ulcer, which helps in staging the disease. A pressure transducer along with a pH electrode and an open-tipped catheter are introduced in to the esophagus. Esophagoscopy (flexible or rigid): For direct examination of esophageal mucosa and biopsy. Dysphagia lusoria: this dysphagia is caused by the compression of esophagus by an abnormal right subclavian artery, which abnormally arise directly from the aorta and passes anterior or posterior to esophagus. Acute catarrhal or superficial tonsillitis is a part of generalized pharyngitis, and is mostly seen in viral infections. Child presents with fever, sore throat, and vesicular eruption surrounded by a zone of erythema on the soft palate and pillars (See Chapter: Oral Mucosal Lesions). Herpes simplex virus: It may cause exudative or nonexudative pharyngitis, which may be associated with gingivostomatitis (See Chapter: Oral Mucosal Lesions). The openings of crypts present yellowish spots of pus which may coalesce, and form a membrane on the surface of tonsil (acute membranous tonsillitis). Abdominal pain: It is due to mesenteric lymphadenitis, and simulates acute appendicitis. Tonsils red and swollen with yellowish spots of pus at the opening of crypts (acute follicular tonsillitis) which Diagnosis Characteristic feature: Petechiae at the junction of hard and soft palate. Serological tests: Monospot and Paul Bunnell or Ox-cell hemolysis test shows high titers of heterophil antibody. Leukemia: In children, acute lymphoblastic leukemia is more common (75%) than acute or chronic myelogenous (25%) leukemia. Aphthous ulcers: Small/large, single/multiple painful ulcers on any part of oral cavity or oropharynx. Clinical Features: It has insidious onset with mild fever and discomfort in throat. Diagnosis Sore throat and fever with cervical adenopathy and pharynx with exudative covering are highly suggestive of Streptococcus pyogenes. Throat culture: Swab the posterior pharynx and tonsillar area when body temperature is greater than 38. Differential Diagnoses of white Patches on Tonsils In addition to the above-mentioned causes of membranous pharyngitis-tonsillitis, certain conditions (Box 1), most of which are described in the sections of this chapter, can present with white lesions on the tonsils. Chronic/Recurrent tonsillitis due to incomplete resolution of tonsil infection, which may persist in lymphoid follicles of the tonsil like microabscesses. However, it should be kept in mind whenever any membrane is seen on the tonsils of a child (Table 1).
Diseases
- Lopes Marques de Faria syndrome
- Dementia progressive lipomembranous polycysta
- Herrmann Opitz arthrogryposis syndrome
- Hinson Pepys disease
- Nelson syndrome
- Exostoses, multiple, type 3
- Skandaitis
- 6-pyruvoyltetrahydropterin synthase deficiency
- Q fever
- Follicular ichthyosis
Buy maxolon 10mg fast delivery
For example gastritis symptoms and chest pain purchase maxolon 10mg without a prescription, an isolated fracture of the greater tuberosity without displacement would be called a one-part fracture involving the greater tuberosity or a minimally displaced fracture of the greater tuberosity. In the example shown, the displacement is superior as seen on the anteroposterior view and posterior as seen on the axillary view. This finding represents disruption of the surrounding soft tissue and tearing of the rotator cuff tissue to allow this fragment to displace. The supraspinatus, infraspinatus, and teres minor are attached to the greater tuberosity. A fracture of the greater tuberosity of this large-sized fragment will result in the ability of these rotator cuff muscles to pull the fragment superiorly and posteriorly. Surgery is required for placing the fragment in its proper location to restore proper rotator cuff strength and to avoid loss of motion due to malunion of the fragment. Malunion will cause impingement of the malunited fragment on the posterior aspect of the glenoid when attempting external rotation of the arm or impingement on the undersurface of the acromion when attempting elevation of the shoulder. Treatment of the late sequelae of a malunion is very difficult and often results in a less-than-ideal functional outcome. Early recognition of these displaced fractures is important for early surgical intervention. If an anatomic reduction is achieved with stable fixation, then healing and rehabilitation can result in normal shoulder function and no pain. In the case shown, the fracture was treated with open resection and internal fixation with heavy suture material. This technique is best used in the older patient with osteoporosis when fixation using screws may fail owing to poor fixation of the screw between the bone fragments. Suture fixation between the tendon insertions of the rotator cuff is much stronger than fixation isolated to the bone fragments. With isolated fracture of the greater tuberosity in patients with good quality bone, minimally invasive reduction under fluoroscopy and screw fixation can be done as an effective, less invasive alternative to open reduction and suture fixation (see Plate 1-24). The clinical significance is related to the additional damage caused to the articular cartilage of the humeral head, the additional trauma to the blood supply to the humeral head, and the additional trauma to the glenoid and glenohumeral ligaments. Each of these can result in additional long-term adverse clinical sequelae, specifically post-traumatic arthritis, avascular necrosis of the humeral head, glenoid arthritic changes, or instability of the joint. Each of these additional problems makes surgery necessary to manage this problem and also increases the urgency for early surgical invention. It is also difficult to see the fracture of the humeral head segment on the anteroposterior radiograph. These types of fractures are often missed in the office or emergency department setting if inadequate imaging is performed. When this occurs, early surgical invention is not performed; and in some cases the patient is treated without surgery, resulting in a very poor outcome. Late reconstructive surgery for management of the late sequelae of malunion of this fracture often results in improvement but a less than favorable outcome when compared with early fracture management. In this case of a young middle-aged and active person who fell from a horse, open surgery for an anatomic reduction of the fracture and reduction of the dislocation resulted in the ability to use minimal fixation devices because of the high-quality bone tissue 1 D E Axillary radiograph (A) of a two-part fracture dislocation. Open reduction and internal fixation with two interfragmentary cancellous and corticoid screws (D and E). The distal screw was a cortical screw for the cortical bone using overdrilling of the lateral fragment, resulting in compression at the fracture site, with the screw orientation being perpendicular to the fracture line, thus resulting in compression of the fracture. The superior screw is a partially threaded cancellous screw placed in to cancellous bone of the humeral head. The larger treads of the cancellous screw achieve better fixation in cancellous bone. The smooth part of the cancellous screw allows for the lag screw again effecting compression across the fracture site. Fracture was treated by open reduction and internal fixation using a locking plate. Percutaneous method of reduction of the humeral head fracture fragment A valgus-impacted four-part fracture is a variation of a classic four-part fracture-dislocation. In a classic fourpart fracture-dislocation the humeral head segment is completely separated from the other three segments of the proximal humerus (greater and lesser tuberosity and the humeral shaft). In many of these classic four-part fractures the humeral head segment is also dislocated from the joint and is not articulating with the glenoid. When the articular segment is separated from its blood supply (see Plates 1-16 and 1-17), there is a high incidence of avascular necrosis. In most cases these fractures occur in the elderly, and humeral head replacement using a stemmed prosthesis as shown in Plate 1-25 is the preferred treatment for reduction and fixation of the tuberosities and replacement of the avascular articular segment. The valgus-impacted four-part fracture results in rotation of the humeral head articular segment in to a horizontal position with impaction of this segment between the fractures of the greater and lesser tuberosities that become split and widened to accommodate the impacted humeral head. With this fracture, the humeral head segment is oriented with the articular surface facing superiorly toward the undersurface of the acromion. The humeral head is not in contact with the glenoid and is shrouded by the displaced tuberosities. In many of these fractures the periosteum on the medial side of the humeral shaft and humeral head segment remains intact and forms a soft tissue bridge between the two, adding to the stability of the head segment and to its blood supply. This results in a much lower incidence of avascular necrosis than that seen with classic four-part fracture-dislocations. Both the greater and lesser tuberosity fracture fragments are displaced laterally but keep an intact soft tissue attachment to the humeral shaft. As a result of these soft tissue attachments, this fracture configuration allows for keeping the humeral head and fracture in reduction and fixation rather than displacement. With traction on the arm, both the greater and lesser tuberosities are reduced by tensioning the intact soft tissues. Percutaneous placement of two cannulated cancellous screws through the greater tuberosity fracture fragment thereby completes the internal fixation using minimally invasive techniques. If the medial soft tissue hinge is present and providing some stability of the head segment, then a more minimally invasive method of fracture reduction and internal fixation can be accomplished as shown at the bottom of Plate 1-24. When there is more instability of the fragment, comminution of the segments, or poor bone quality secondary to osteoporosis, then a more formal operation with open incision with plate fixation as shown at the top of Plate 1-24 is preferred. Open reduction and internal fixation provides more rigid internal fixation but does require a larger open procedure. In this variation of the classic four-part fracture, the fracture line goes through the articular humeral head segment. As a result of the soft tissue attachments to each of the fragments, elevation of the head fragment with traction on the arm easily realigns the tuberosities under the humeral head segment. Percutaneous pinning and screw fixation provides sufficient fixation of the segments to maintain the reduction. This is not ridged fixation, and removal of the pins at 6 weeks after surgery allows for sufficient healing to begin rehabilitation. Because of the minimally invasive approach, delay in rehabilitation does not result in the vast majority of patients achieving good range of motion, assuming that the fracture fragments maintain good position. Patients treated in plate fixation generally have better fixation and can and should start rehabilitation rangeof-motion exercises soon after surgery. The fracture through the humeral head segment results in a much more difficult fracture to manage and generally requires humeral head replacement. In addition, the likelihood for post-traumatic arthritis and avascular necrosis in this fracture configuration is certain, again making humeral head replacement the treatment of choice. With humeral head replacement, the stem of the prosthetic is securely placed in to the shaft of the humerus, in most cases by the use of bone cement. One of the most difficult parts of the surgery is to place the stem in the correct height and rotation to reproduce the normal pre-fracture anatomy. When done correctly, there will be the same amount of space between the metallic humeral head and the shaft as there was before the fracture in order to place all of the fracture fragments of the greater and lesser tuberosities within this interval so that the fragments are below the metallic humeral head and above the humeral shaft. Fixation of these fragments is aided by use of the metallic stem as an internal fixation device, around which the fragments are reduced with the humeral head in place. Very heavy and strong nonresorbable sutures are placed through the humeral shaft bone and prosthetic as well as through the rotator cuff tendons that are attached to the tuberosity fragments. Despite the multiple fractures and fragments of bone, when an anatomic reduction is achieved with good fixation, long-term outcome is excellent.
Generic 10 mg maxolon overnight delivery
Paget cells contain mucin in 40% of cases 1516 and may contain melanin pigment as a result of phagocytosis gastritis diet vi discount maxolon 10 mg visa. Three histological variants are recognized: classical, bowenoid and pemphiguslike 1416. The first postulates that Paget cells originate in underlying or intraepidermal lactiferous or deeper ducts, then migrate in to the epidermis. Estrogen and progesterone receptors are expressed in about 40% and 30% of cases, respectively 217,307. A Nipple epidermis containing Paget cells with pale stained cytoplasm and large irregular nuclei with prominent nucleoli. Paget cells are genetically similar to the underlying carcinoma cells in 80% of cases 946. Differential diagnosis this includes malignant melanoma and Bowen disease of the skin. Paget cells also have to be distinguished from Toker Prognosis and predictive factors the prognosis depends on the presence or absence of an underlying carcinoma and on the stage of the disease. Primary lymphoma of the breast is often defined as a tumour limited to the breast and regional lymph nodes in a patient with no prior history of lymphoma 1425,1590. However, it has also been suggested that primary lymphoma of the breast should be defined in the same way as other extranodal lymphomas: initial presentation with the dominant mass or symptom in the extranodal site in a patient without a prior history of lymphoma elsewhere, even if distant involvement is discovered at staging 202, 609,864,893,1396. The lymphoma should be seen in close proximity to breast tissue, not confined to an intramammary lymph node. Clinical features Primary lymphomas of the breast are rare and have been estimated to comprise < 0. Most patients are postmenopausal women, although younger patients have been reported, including pregnant or lactating women presenting with massive bilateral breast swelling due to Burkitt lymphoma 864,1301. Patients usually present with a painless lump, which may be multinodular, and is bilateral in approximately 10% of cases. Treatment and prognosis depends on the specific histological type of lymphoma 883,1243. Histopathology Lymphomas of the breast most commonly appear as well-circumscribed tumours of varying size; on cut surface, the neoplastic N. Jaffe tissue is similar to that of lymphomas in other sites, fleshy tan-white, with occasional haemorrhagic or necrotic foci in higher-grade tumours. Although grossly circumscribed, the majority of breast lymphomas have an infiltrating border, with permeation around lobules and ducts. There may be preferential involvement of lobular structures, imparting a nodular or pseudofollicular appearance. A higher proportion of cases appears to have an activated B-cell phenotype than a germinal-centre B-cell phenotype, when examined by immunohistochemistry and 156 Lymphoid and haematopoietic tumours classified according to the Hans algorithm 550,1610. Prognosis and predictive factors Most patients present with unilateral disease, but there is a risk of recurrence in the opposite breast. The breast may also be a site of involvement in patients with disseminated disease 1396. Sheets of large lymphoid cells displace normal elements and surround residual duct. Inset shows atypical lymphoid cells with features of centroblasts, having peripherally-placed basophilic nucleoli. Patients are usually pregnant or lactating women, but presentation during puberty is also seen. Bilateral breast involvement may be the presenting manifestation during pregnancy and puberty. Rare cases of subcutaneous panniculitis-like T-cell lymphoma have been reported 1287, but the differential diagnosis with lupus mastitis can be challenging 697. Both silicone- and saline-filled implants have been implicated, with a higher proportion of cases involving silicone. Extension beyond the fibrous capsule with infiltration of the breast parenchyma is rare. Cytologically the neoplastic cells are large, pleomorphic cells with basophilic cytoplasm, best identified in cytological specimens obtained from the seroma fluid. The optimal therapeutic management has not yet been determined, and some patients have done well with limited local therapy, including removal of the implant with watchful waiting 1437. A Cytological examination of the seroma fluid is the optimal diagnostic method, as tissue involvement is frequently limited in extent. B the seroma cavity is frequently lined by a fibrinous exudate, with the atypical cells adherent to the wall, and embedded within the exudate. Plasma cell differentiation, sometimes with Dutcher bodies, can be seen in up to 75% of cases 1159. Architecturally, the neoplastic infiltrate is frequently associated with hyperplastic Bcell follicles, and occupies the marginal zone at the periphery of B-cell follicle mantle zone. In advanced cases, the tumour cells may overrun and colonize the reactive B-cell follicles, mimicking follicular lymphoma. Transformation in to a large B-cell lymphoma, characterized by the presence of diffuse sheets of large cells has been described 421. Most cases occur in female adults in their sixth or seventh decade of life 883,893. Clinical features the patients generally present with a unilateral solitary breast mass that can be detected either by palpation or by mammography. The tumour is composed of medium-sized lymphoid cells containing irregular nuclei with dispersed chromatin and inconspicuous nucleoli and, pale, abundant cytoplasm. The characteristic cytology of these cells is often described as "monocytoid" or "centrocyte-like. A breast core biopsy showing relatively well-circumscribed, nodular, dense lymphoid infiltrate. If plasma-cell differentiation is present immunoglobulin light-chain restriction can be demonstrated by immunohistochemistry. Most cases respond to locally directed therapy such as radiotherapy or surgical excision 883. A the infiltrate is polymorphic, containing a reactive follicle (right) and a perifollicular/marginal zone component of "monocytoid"-appearing lymphoid cells. Extranodal marginal zone lymphomas of mucosa-associated lymphoid tissue 159 Follicular lymphoma F. Clinical features Follicular lymphoma may present as primary disease in the breast, with or without involvement of axillary lymph nodes, but the percentage of cases with primary versus secondary involvement of the breast varies widely in different series. Histopathology the morphology of follicular lymphoma is comparable to nodal and other extranodal sites, with both follicular and diffuse growth patterns and a predominance of histological grade 1 or 2 over grade 3A or 3B. The neoplastic follicles show a monotonous pattern and vague borders and contain centrocytes with various proportions of centroblasts, depending on grade. A neoplastic follicle in a breast core biopsy contains many large, atypical centroblasts and centrocytes. The presence of dense collagenous tissue, especially in core biopsies, may cause an "Indian file" pattern of infiltration and raise a differential diagnosis of lobular carcinoma. The diagnosis of these cases can easily be resolved by immunohistochemical analysis. Genetics the frequency of the characteristic t(14;18)(q32;q21) translocation or other cytogenetic or molecular alterations has not been assessed systematically for primary follicular lymphoma of the breast. Prognosis and predictive factors Relapse rates, patterns of spread and clinical behaviour of primary follicular lymphoma of the breast are comparable to those of conventional nodal disease, although a worse prognosis has been reported recently 883. A the tumour shows a vaguely follicular pattern without formation of lymphoepithelial lesions. Sahin Definition Metastasis to the breast from a malignancy arising outside the breast. Common types include haematological malignancies, melanoma, carcinomas of the lung, ovary, prostate, kidney and stomach and carcinoid tumours 39,1449, 1584.
Buy maxolon 10mg amex
Early studies suggested that both breasts were at equal risk for later cancer development 53A; however gastritis diet cure buy cheap maxolon line, recent carefully conducted cohort studies show that approximately two thirds of subsequent carcinomas occur in the ipsilateral breast 881,1058. Studies that have shown a substantial rate of upgrades generally show a selection bias. Reported rates of upgrade to a worse lesion on excision vary widely due to variations in study design 1018. There is consensus that excision should be performed if there is another lesion which by itself would warrant excision or if there is pathological-mammographic discordance. They are associated with an increased risk, albeit of different magnitudes, for the subsequent development of invasive carcinoma. Some of these lesions are best considered as risk indicators whereas others are recognized as true precursors of invasive breast cancer. Clinical features the age range of women with intraductal proliferative lesions is wide, spanning seven to eight decades post-adolescence. All these lesions are extremely rare before puberty; when they do occur among infants and children, they are generally a reflection of exogenous or abnormal endogenous hormonal stimulation. Macroscopy A vast majority of intraductal proliferative lesions, particularly those detected mammographically, are not evident on macroscopic inspection of the specimen. Specimen radiography is an important component in the pathological evaluation of mammographically detected lesions. The rare lesions that develop within the lactiferous ducts may progress toward the nipple, resulting in Paget disease 1027,1028,1031. In most cases, the histopathological distinction between different types of intraductal proliferation can be made on morphological grounds alone, particularly with standardization of histopathological criteria. Those lesions lacking appreciable proliferation have been described in the past as "clinging carcinoma (monomorphic type)", "atypical cystic lobules", and "atypical columnar cell change", among other terms, and are currently categorized as "flat epithelial atypia". Progression to invasive breast cancer Clinical follow-up studies have indicated that intraductal proliferative lesions are associated with different levels of risk for subsequent development of invasive breast cancer, that range from approximately 1. Molecular analysis has started to refine and should help to improve upon the traditional classification 36,1520. Hence, the classification of intraductal proliferative lesions should be viewed as an evolving concept that may be modified as additional molecular and genetic data become available. Diagnostic reproducibility Multiple studies have assessed reproducibility in diagnosing the range of intraductal proliferative lesions, some with emphasis on the borderline lesions 153, 1064,1065,1199,1284,1338,1339. These studies have clearly indicated that interobserver agreement is poor when no standardized criteria are used 1199. Diagnostic reproducibility is improved with the use of standardized criteria 1284. In one study, consistency in diagnosis and classification did not change significantly when interpretation was confined to specific images as compared with assessment of the entire tissue section on a slide, reflecting inconsistencies secondary to differences in morphological interpretation 379. Etiology In general, the factors that are associated with the development of invasive breast carcinoma are also associated with increased risk for the development of intraductal proliferative lesions 684,736 (see Chapter 1: Epidemiology). Genetics of precursor lesions the morphological similarities between invasive and in situ carcinomas of similar grade and their intimate association within the breast suggest that these proliferations are biologically related. The distinct molecular features found in different grades of invasive carcinomas are also mirrored in pre-invasive lesions of comparable morphology 844. The other pre-invasive lesions are more difficult to position along the multistep pathways. Genetic alterations have also been identified in normal breast tissues near to and distant from invasive carcinoma 330,743. The genetic alterations have been seen independently in luminal and myoepithelial cell compartments 743, suggesting that changes may have occurred very early during the development of the breast carcinoma. Genetic and transcriptomic alterations in the mammary stroma of patients with malignancy have also been described and there is currently considerable interest in understanding the relationship between the stroma and epithelial cells in breast tumorigenesis and progression 842,934. The significance of alterations in normal breast tissues in individual patients is unclear at present but is likely to shed light on cancer development and potential preventive strategies in the future. Schnitt Definition this lesion is characterized by a solid or fenestrated proliferation of epithelial cells that often show streaming growth, particularly in the centre of involved spaces. Synonyms Intraductal hyperplasia; hyperplasia of the usual type; epitheliosis; ordinary intraductal hyperplasia; hyperplasia without atypia. The presence of secondary lumina or fenestrations is characteristic of this lesion. B High magnification showing a predominantly solid intraductal proliferation with pronounced cellular streaming. C Immunostaining for keratin 5/6 shows many positively stained cells and a few negative cells. In some cases, the proliferation has a solid pattern and no secondary lumina are present 1054. Occasionally, a micropapillary architecture may be present similar to that seen in gynaecomastia. The cells often have a streaming or syncytial pattern which is particularly evident in the centre of the proliferation. Micropapillations, when present, have a broad base and a narrow or pinched tip with hyperchromatic, almost pyknotic appearing nuclei. The nuclei of the cells surrounding the secondary lumina tend to run parallel rather than perpendicular to the spaces. The cellular population exhibits a mixed phenotype and as such stains for keratins of low and high molecular weight (keratin 5/6 or 34betaE12), the latter in a heterogeneous or mosaic pattern 154. This risk is conferred on either breast and appears to be slightly higher among those with a strong family history of breast cancer 283,357,450,1279. Usual ductal hyperplasia 85 Columnar cell lesions Columnar cell change and hyperplasia A. Synonyms Blunt duct adenosis; columnar alteration of lobules; columnar metaplasia; hyperplastic unfolded lobules; hyperplastic enlarged lobular units; enlarged lobular units with columnar alteration. Clinical features In current clinical practice, these lesions are being detected increasingly because of the presence of microcalcifications seen on screening mammography. Macroscopy Columnar cell change and hyperplasia are of microscopic size and cannot be identified on macroscopic examination. The nuclei are typically ovoid, regularly oriented perpendicular to the basement membrane, and have evenly dispersed chromatin and inconspicuous nucleoli. The myoepithelial cell layer may be prominent and the specialized stroma can be cellular. Lesions in which the epithelial-cell lining is only one or two cell layers thick are categorized as columnar cell change; those with cellular stratification or tufting more than two celllayers thick are designated columnar cell hyperplasia 1110,1285. Columnar cell change and hyperplasia are often seen in association with other benign changes, such as cysts and epithelial proliferative lesions. There is a strong association between these lesions and the presence of lobular neoplasia (lobular carcinoma in situ and atypical lobular hyperplasia) 193,222,779. Prognosis and predictive factors Recent follow-up studies have shown that columnar cell change and hyperplasia are associated with a very low risk for the subsequent development of breast. A dilated acinus is lined by a monolayer of columnar cells exhibiting apical snouting. Moreover, the risk associated with these lesions is not clearly independent of the risk associated with concomitant proliferative lesions. Synonyms Columnar cell change with atypia, columnar cell hyperplasia with atypia Clinical features In current clinical practice these lesions are being detected increasingly because of the presence of microcalcifications seen on screening mammography. Occasional cellular tufts or mounds may be seen, but well-developed arcades, bridges and micropapillary formations are absent (hence their designation as "flat"). Radiologicalpathological correlation is recommended for determining further management. A A low-power view shows a portion of a terminal-duct lobular unit with variably dilated acini containing secretory material and calcifications. B At high power, the spaces are seen to be lined by several layers of columnar epithelial cells with monomorphic nuclei. The proliferation may be solid with or without subtle microacini, cribriform with round, "punched out" spaces surrounded by polarized epithelial cells, or micropapillary with epithelial projections that are typically narrower at the base than the apex.
Buy maxolon 10mg with mastercard
However gastritis vagus nerve order genuine maxolon line, cigarette smoking and obesity are confounding variables in these associations. Each inflammatory pathway has been associated with atherogenesis and subsequent cardiovascular disease. Despite the high prevalence of overlap syndrome, only limited data are available on its pathophysiological and clinical consequences. Long-term follow-up studies are lacking on the pathophysiological and clinical consequences of overlap syndrome, although some clinical outcome studies in this area have commenced [64, 65]. The magnitude and consequences of inflammation, oxidative stress and leukocyte dysfunction in the overlapping mechanisms of overlap syndrome should be better defined in future studies. Studies in overlap patients are likely to provide insight regarding the nature and significance of these responses. Sleep profile and symptoms of sleep disorders in patients with stable mild to moderate chronic obstructive pulmonary disease. Nocturnal hypoxaemia and quality of sleep in patients with chronic obstructive lung disease. Chronic obstructive pulmonary disease and obstructive sleep apnea: overlaps in pathophysiology, systemic inflammation, and cardiovascular disease. There is no relationship between chronic obstructive pulmonary disease and obstructive sleep apnea syndrome: a population study. Relationship between overnight rostral fluid shift and obstructive sleep apnea in nonobese men. The effect of obesity on chronic respiratory diseases: pathophysiology and therapeutic strategies. Theophylline improves gas exchange during rest, exercise, and sleep in severe chronic obstructive pulmonary disease. Effects of salmeterol on sleeping oxygen saturation in chronic obstructive pulmonary disease. The overlap syndrome: obstructive sleep apnea and chronic obstructive pulmonary disease. Sleep apnea and cardiovascular disease: an American Heart Association/ American College of Cardiology foundation scientific statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing in collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health). Systemic inflammation: a key factor in the pathogenesis of cardiovascular complications in obstructive sleep apnoea syndrome Sleep apnoea as an independent risk factor for cardiovascular disease: current evidence, basic mechanisms and research priorities. Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Increased incidence of coronary artery disease in sleep apnoea: a long-term followup. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Nocturnal oxygen desaturation correlates with the severity of coronary atherosclerosis in coronary artery disease. Respiratory disturbance index: an independent predictor of mortality in coronary artery disease. Cardiovascular morbidity in obstructive sleep apnea: Oxidative stress, inflammation, and much more. Selective activation of inflammatory pathways by intermittent hypoxia in obstructive sleep apnea syndrome. Therapeutic hypercapnia reduces pulmonary and systemic injury following in vivo lung reperfusion. Outcomes in patients with chronic obstructive pulmonary disease and obstructive sleep apnea: the overlap syndrome. Numerous theoretical models have been proposed to explain this relationship, with most suggesting bidirectional and complex pathways. Appropriate use of mental health screening tools, diagnostic resources and referral pathways should be implemented for optimal management. Patients with bipolar disorders cycle between depressive and manic episodes, while those with unipolar depression never present with mania or hypomania. Depression can range in severity from short-term episodes and mild symptoms through to severe long-term clinical depression. Generalised anxiety disorder is characterised by at least 6 months of persistent and excessive anxiety and worry (table 1). Panic disorder is characterised by recurrent unexpected panic attacks about which there is persistent concern and may occur with or without agoraphobia. Social phobias are characterised by clinically significant anxiety provoked by exposure to certain types of social or performance situations, often leading to avoidance behaviour. Severity of anxiety, as with depression, is determined by both the number and the level of symptoms, as well as the degree of functional impairment [6]. The clinical course of depression and anxiety disorders is acknowledged to be variable and people can move in and out of diagnostic subtypes over time [8]. Meta-analysis has also been used to provide an estimate of depression pooled across studies. The subjects in the included studies were mostly from outpatient or inpatient settings and provided an indication of the prevalence of depression likely to be found in a respiratory clinic. Estimates for the prevalence of anxiety are also available from systematic reviews and metaanalysis. One systematic review reported the prevalence of anxiety from 19 studies as ranging from 10% up to 100% [12]. Studies that have used standard diagnostic procedures have found prevalence 145 P. Prevalence of panic attacks ranged between 8% and 37%, which is several times higher than found in the general population [17]. Anxiety-related disorders are often characterised by chronicity [18], relapses [19] and periods of disability [20]. Furthermore, depression and anxiety are often comorbid with other medical conditions, compounding disability and imposing even greater burden on the daily lives of both patients and healthcare services [21]. Respiratory symptoms, in particular dyspnoea, tend to be the most powerful predictors of symptoms of depression and anxiety [7, 15]. The odds of depression are significantly greater amongst patients who live alone or who are not married [15, 24], have limited airflow reversibility and have a greater impairment to physical functioning [24, 25]. However, there is still uncertainty about the importance of other risk factors including (younger) age, female sex, smoking and markers of socioeconomic status, with some studies reporting increased risk related to these variables and other studies reporting no difference in risk [7, 15, 16, 24, 28]. Many of these theories describe the pathogenic mechanisms associated with these relationships as bidirectional and complex. Numerous studies have concluded that depression and anxiety are risk factors for initiating tobacco smoking, often in adolescence or early adulthood [29, 30]. Smoking rates amongst those with severe mental illnesses, such as major depression, are high [31]. A large multinational study reported the existence of a diagnosis of major depression in 23. Moreover, smokers with a history of depression and/or anxiety are more likely to experience worse nicotine withdrawal and have significantly more failed cessation attempts [34, 35]. A number of studies have found that smoking cessation itself may induce depressive Table 2. A twin study suggested that shared genetic factors link smoking and depression [39]. One proposed pathogenic mechanism behind the neurological and psychiatric changes relates to oxygen insufficiency in the periventricular and subcortical regions of the brain leading to similar changes to those evident on the magnetic resonance imaging scans of depressed individuals [42], with white matter damage and vascular endothelial damage [41]. Additionally, impairments in attention and memory have been associated with abnormal blood gas results [44]. A recent review of the effects of hypoxia on cognition pointed to subcortical mild cognitive impairment, which is characterised by bradyphrenia, memory impairment, verbal language loss, attention disturbance, and emotional and psychiatric problems including apathy and depression [45]. A large study, accounting for these confounders, demonstrated significant associations between inflammatory biomarkers and depression, providing further support for the shared inflammatory pathway hypothesis [54]. Since both dyspnoea and panic are linked with hyperventilation, this model also postulates that the resulting hypocapnia will further aggravate breathlessness and anxiety.