Generic accutane 10mg with visa
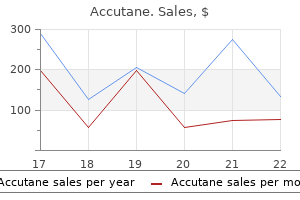
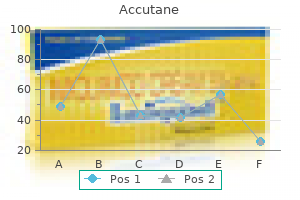
Chemical poisonings are the most common form of acute fatal poisonings and are summarized in Table 34-2 skin care questions buy accutane. Poisonings There are many natural and manufactured substances that may cause poisoning, fatal or nonfatal (Table 34-2). In forensic medicine, it is important to determine whether fatal overdoses of drugs are accidental, homicidal or suicidal. Heroin (synthetic acetyl morphine) is an opioid that does not occur in nature and is the prototype for intravenous drug abuse. These substances cause constriction of blood vessels, especially in the cerebral circulation, leading to anoxic brain injury. Talc is a noninfectious contaminant frequently introduced through illicit intravenous drugs. Rarely, ingestion of poisonous plants may be fatal in sufficient dose, especially with babies or children who may be unaware of the danger and for whom a smaller dose may be fatal. Biotoxins created by bacteria and fungi are responsible for gastrointestinal poisonings, causing fatal dehydration in circumstances where advanced medical care is not available. Other toxins cause Electrical Injury and Lightning Strikes Exposure to household voltage, or high voltage, often in an occupational setting or during storms that cause downed electrical lines, may be fatal but leave barely perceptible evidence. Where the current exits the body, there may be a trace of thermal injury on the surface of the skin, which has a dry, leathery appearance (as observed in postmortem wounds, see below). Usually, a fatal electrical shock is instantaneous, as the victim will let go or fall away from the source. When voltages are very high and contact is prolonged, there tends to be more extensive injury owing to the heat generated by resistance to the current in the body. Over a period of hours, the medical examiner relies on algor mortis (body temperature), livor mortis (postmortem lividity) and rigor mortis (postmortem rigidity), all of which are influenced by environmental temperature and other factors. Decomposition itself also presents a competition over time between desiccation and decay/putrefaction. In a very hot, arid environment, such as the sands of Egypt, a body may actually dry out before internal bacteria can bring about decomposition. Once a body is desiccated, it does not provide a fertile medium for bacterial growth, and the body becomes preserved, potentially for long periods of time. The ancient "secret" of Egyptian mummification lay in the removal of internal organs that harbored bacteria, together with exposing the body to desiccation. As decomposition ensues, postmortem blood presents a fertile medium for bacterial growth. Wherever tissues are injured, bacterial decomposition is accelerated by the presence of blood in the wounds. Initially, below the skin, discoloration occurs along the distributions of blood vessels, as bacteria metabolize respiratory pigments to variously colored chemicals, appearing blue-green, yellow and purple-black. Another product of postmortem bacterial metabolism is the generation of decomposition gases, which accumulate under the skin. These expand areas of subdermal connective tissues, especially in the areolar looser tissues around the eyes, face and torso. These gases may also expel decomposition fluids (which may appear "bloody") from body orifices. Body Temperature After death, normal body temperature falls at a predictable rate, if one takes into account the size of the body and the external temperature. The ability to retain heat by the body generally varies directly with increasing size, as the surface area of the body, through which heat is lost, is proportional to the square of the height. The mass or weight of the body, in which heat is retained, varies as the cube of the height. Factors that increase body temperature at the time of death require recalibration in estimating the time since death, for example, in people dying with a fever or from acute cocaine intoxication. Lividity Postmortem lividity results from passive pooling of blood into dependent areas owing to the effects of gravity. It presents as a distinctive red-purplish discoloration, unlike anything seen in life. The pattern of lividity indicates the position of the dead body and, depending on the presence of shifting patterns, whether a body was moved at certain intervals after death. Rigor Postmortem rigidity (rigor mortis) is the result of a chemical reaction whereby muscle tissues irreversibly go through a process of contraction, causing the body and appendages to become stiff. Over several more hours, rigidity begins to pass away again and the body becomes lax. Since it is a chemical process, it is accelerated by higher temperatures and retarded by lower ones. Rigor mortis starts from the top down-that is, it extends from the head and neck down to the arms and then the legs. Disarticulation As soft tissues decompose, after a period of weeks or months (depending upon seasonality, environmental temperatures and exposures) the skeleton becomes exposed to decay. Although the skeletal elements are usually preserved (and eventually over time the mineralized matrix becomes fossilized), there is a pattern by which skeletal elements become disarticulated from one another after soft tissues have disintegrated. Glossary of infection control terms Additional (transmission based) precautions Infection control precautions required when the standard precautions may not be sufficient to prevent transmission of infection. These are used for patients known or suspected to be infected or colonized with pathogens that can be transmitted by airborne, droplet, or contact routes. Additional precautions are transmission-based precautions and should be used in addition to standard precautions. Airborne transmission Transmission of infectious agents by either airborne nuclei or particles of <5 mm in size. Antimicrobial A chemical agent that, on application to living tissue or by systemic administration, will selectively kill or prevent the growth of susceptible organisms. This definition includes antibacterials, antivirals, antiprotozoals, antifungals, antiseptics, and disinfectants. Antisepsis the destruction or inhibition of microorganisms on living tissues, having the effect of limiting or preventing the harmful results of infection. Antiseptic A chemical agent which, when applied to living tissue, will destroy or inhibit the reproduction of microorganisms. Asepsis the prevention of microbial contamination of living tissues or sterile materials by removal, exclusion, or destruction of microorganisms. Aseptic technique A technique in which the instruments, drapes, and the gloved hands of the health care worker are sterile when performing surgery or invasive procedures. Asymptomatic infection Infection which does not display any clinical signs/ symptoms, but may still be capable of transmitting disease or microorganisms. Bacteriuria the presence of bacteria in the urine, with or without consequent urinary tract infection. Carrier A person (host) who harbours a microorganism (agent) but does not necessarily display clinical signs/symptoms of disease. Carriers may shed organisms into the environment intermittently or continuously and therefore act as a potential reservoir or source of infection. Chemoprophylaxis the administration of antimicrobial agents to prevent the development of an infection or the progression of an infection to active manifest disease. Colonization the presence of microorganisms at a body site(s) without the presence of symptoms or clinical manifestations of illness or infection. Commensal A microorganism resident in or on a body site without causing clinical infection. Community-acquired infection this is an infection which was present, or incubating, at the time the patient was admitted to hospital. It is possible that the infection may only become apparent after the patient has been admitted. Contact An exposed individual who might have been infected through transmission from another host or the environment. Contamination the presence of microorganisms on a surface or in a fluid or material. Cross-infection An infection transmitted from one patient to another, or from a member of staff, or from the environment, to another patient. Decontamination A process which removes or destroys contamination and thereby prevents microorganisms or other contaminants from reaching a susceptible site in sufficient quantities to initiate infection or any other harmful response. Disinfectant A chemical agent which, under defined conditions, is capable of disinfection.
Diseases
- Polycystic kidney disease, type 2
- Albinism, minimal pigment type
- Carnosinase deficiency
- Campylobacteriosis
- Ankle defects short stature
- Microinfarct
- Hennekam Van der Horst syndrome
Order accutane overnight delivery
They can also show mild nuclear atypia acne zip back jeans discount accutane 10mg without prescription, and as such, can be mistaken for a low-grade chondrosarcoma. The key to avoiding this diagnostic pitfall is to recognize the fact that increased cellularity and slight nuclear atypia in this site represents a normal variation. In addition, correlation with imaging features can be very reassuring that one is dealing with a benign process. Again, the radiologic features are helpful, as these are sharply demarcated lesions that do not invade the underlying cortex. Periosteal chondromas occur most commonly on the surface of the long bones and tend to be well marginated. In these types of specimens, the architectural pattern, alluded to earlier, will be completely unrecognizable. Individual chondrocytes should appear relatively small and innocuous in appearance. Lack of conspicuous atypia and pleomorphism is a reassuring sign, but does not absolutely exclude a diagnosis of welldifferentiated chondrosarcoma. In this instance, the best approach to diagnosis is careful correlation with the imaging features of the lesion. In the absence of atypical imaging features, a diagnosis of "low-grade chondroid neoplasm, consistent with enchondroma" is acceptable. Aspirates and small core biopsies of a chondroblastic variant of osteosarcoma can sometimes appear as benign cartilage. This should be suspected if the sample is from a very young patient, the imaging features suggest an aggressive neoplasm, and there is clinical concern for a malignant process. Within the lesion is a pattern of "rings and arcs," which corresponds to lobules of cartilage with peripheral calcification. It is important to note that this lesion is always in contiguity with the underlying bone and marrow cavity, a feature that helps distinguish osteochondroma from some of its mimics. Osteochondromas are most often solitary, but can occur as multiple lesions as well. The solitary form of osteochondroma is relatively common and is thought to represent up to 35% of all bone tumors. These lesions are often asymptomatic and are frequently incidental findings on imaging studies performed for an unrelated reason. Occasionally a solitary osteochondroma will cause symptoms, usually pain in relation to impingement on adjacent structures. Most cases of osteochondroma present in young individuals within the first three decades of life. Frequent sites of osteochondroma include the metaphyseal regions of the long bones, particularly the distal femur, proximal tibia or fibula, and the humerus. Occasionally they arise in the flat bones, with either the pelvis or scapula being common sites. Individuals with multiple osteochondromas or exostoses are at an elevated risk of malignant transformation (into chondrosarcoma) with a low but significant risk (between 5% and 25%). Solitary osteochondromas are also at risk, but this complication is seen very rarely (estimated at up to 3%). Cross-sectional imaging usually shows continuity with the adjacent host bone marrow space. In addition, cross-sectional imaging is useful for determining the size of the cartilaginous cap. Cap width exceeding 2 cm is associated with a higher incidence of malignant transformation. As such, a thick or irregular-appearing cartilaginous cap, a soft tissue mass, or irregular calcification of the cartilage should raise suspicion for an associated chondrosarcoma. This lesion occasionally causes diagnostic difficulty because the relationship to the host bone is less clear and there may be some histologic atypia. The cortical bone and marrow space should be in continuity with the host bone, although this feature is difficult to determine on histologic sections (and should prompt review of imaging studies). Marrow space is identifiable between the cortical bone of the stalk, and it is often filled with fat and hematopoietic elements. Examination of the cartilaginous cap is the most critical part of histopathologic assessment of osteochondroma. In general, older individuals (and older osteochondromatous lesions) have smaller cartilaginous caps than younger lesions. It tends to be more hypercelluar with less organization of the cartilaginous component. The bone and marrow spaces are often less well formed and may show striking hypercellularity and mitotic activity. They may recur after excision, but this should not prompt a diagnosis of malignancy. The latter, in particular, can often lead to a misdiagnosis of malignancy based on isolated cytologic atypia. Likewise, assessment of the cartilaginous cap (for either benign features or evidence of malignant transformation) by fine needle aspiration is not recommended. Occasional cases have been documented in the flat bones of the pelvis and shoulder (scapula). Chondroblastoma is a lesion that is most frequently diagnosed in younger individuals still undergoing active bone growth (open epiphyses). In an older adult patient population, alternative diagnoses such as giant cell tumor or clear cell chondrosarcoma should be considered. Patients usually complain of gradually increasing pain and tenderness in the affected region. On imaging, chondroblastomas are frequently lucent or lytic lesions with sclerotic borders. Occasionally, punctate calcifications can be identified in the lesion, but this is not a consistent finding. Chondroblastomas are benign lesions of bone and curettage with packing or grafting is often the treatment of choice. Recurrences are rare except in sites where it may be difficult to achieve a complete resection. These are not as frequent, large, or prominent as the giant cells of giant cell tumor, a lesion that chondroblastoma can be mistaken for. The latter should not be confused with the irregular calcification pattern of osteoid identified in association with osteosarcoma. The combination of location, patient age, and histologic findings of this lesion are usually sufficient for a definitive diagnosis of chondroblastoma. The major pitfall in diagnosis is confusing chondroblastoma with clear cell chondrosarcoma. These two lesions bear a superficial histologic and radiographic resemblance, occur in the same location of the bone (epiphysis). These are small cells with abundant cytoplasm and are fairly uniform in size and shape. In the background, there may be numerous mitotic figures, but atypical forms of mitoses should not be identified. Fragments of matrix material are infrequently aspirated, but are often identified on touch preparations of needle core biopsy specimens. Unlike the giant cells of giant cell tumor, chondroblastoma giant cells are less common and contain fewer nuclei. The chondroblastoma osteoclast-like giant cells usually contain 10 to 30 nuclei (whereas giant cell tumor giant cells contain up to 100 nuclei per cell). The chondroblast population is dispersed in the background, as single cells or in small clusters. Longitudinal coffee bean-type grooves are often identified as well as other types of nuclear irregularity. Chondroblastoma is one of only a handful of tumors that is located in the epiphysis. These giant cells tend to be smaller and more sparsely distributed than the giant cells associated with a giant cell tumor. On very close inspection, the nuclear indentations or grooves can be identified in some of the individual chondroblasts. It affects a wide age range of individuals, but there is a peak incidence between 10 and 30 years of age. About 25% of cases occur in the flat bones, including those of the pelvis as well as skull, ribs, and vertebral column.
Order accutane 30 mg without a prescription
The nostrils are closed by gently pressing the sides of the nose together; this will spread the ointment throughout the nares acne out biotrade buy accutane on line amex. A prolonged course (>7 days) or repeated courses (>two courses per hospital admission) should be avoided to prevent the emergence of mupirocin resistance. Success with low-level resistance strains is about 80% but with highlevel resistance strains is only about 27%. Naseptin contains peanut oil and is contraindicated in persons with peanut allergy. Throat: chlorhexidine gluconate spray or gargle for pharyngeal carriage may be added but its efficacy is not known. Topical nasal applications are not effective in clearing throat or sputum colonization. Eradication of throat colonization by use of systematic antimicrobial therapy is not part of routine decolonization therapy but if considered essential, then this can be given on the advice of a medical practitioner on an individual patient basis. A combination of any two oral antibiotics from fusidic acid, rifampicin, trimethoprim, and doxycycline or co-trimoxazole can be prescribed for 7 days based on the antibiotic sensitivity testing. Body bathing: Shower: the antiseptic body wash should be applied directly to the skin, paying particular attention to the hair, around the nostrils, under the arms, between the legs (groin, perineum, and buttock area), feet, and working downwards. For an antiseptic to be effective, recommended contact time on skin must be followed. All antiseptic should be used with care in patients with dermatitis and broken skin and must be discontinued if skin irritation develops. Body bathing or bed bathing: patients confined to bed can be washed with an antiseptic solution. Wet the skin and apply the antiseptic preparation directly onto the skin using a disposable clean cloth; alternatively use pre-soaked antiseptic disposable towel. Mupirocin ointment should be applied three times a day to small lesions for 5 days in selected cases only. Antiseptic powder: 1% chlorhexidine dusting powder can be used to treat carrier sites and should be applied to intact skin such as the perineum, buttocks, flexures, and axillae three times daily for 5 days. The screening swabs should be taken from the nose, perineum/groin, operative and wound sites, abnormal or damaged skin, invasive devices, catheter urine samples, and sputum, if expectorating. Direct culture methods: swab can be plated directly on to selective chromogenic agar. Broth enrichment culture: swabs are placed in enrichment broth and subsequently plated on to selective chromogenic agar. This method is more sensitive then the direct culture method but it can take up to 48 hours to get the confirmation. The result is usually available within 3 hours but it has has not been widely adopted. This is because the test is very expensive and has reduced sensitivity for samples other than nasal swabs. It addition, the swab has to be inoculated on culture medium for final confirmation and antibiotic sensitivity testing, which is required for treatment of patients and typing which is essential for epidemiology purpose. Of the factors examined, throat colonization, mupirocin resistance and age greater than 80 years were significantly associated with failure of decolonization (Gilpin et al. Those who are no longer colonized or infected and those in whom the site/s of colonization or infection does not pose a risk of infection to others, may be transported without the need for any additional infection control precautions. The following infection control measures should be taken for patients who are colonized or infected in one or more sites which cannot be covered with an occlusive dressing are liable to present a risk of cross-infection to other patients: the patient should be given clean clothing before transport. Physically clean hands can be disinfected with an alcoholic hand rub after contact with the patient or the environment. Blankets and pillow cases should be placed in an appropriate bag for laundering according to local protocol. The vehicle should be thoroughly cleaned with detergent and disinfected with freshly prepared hypochlorite solution (1000 ppm av Cl2). Because of its resistance patterns, they are more difficult to treat if infection occurs and they also have a high propensity to become endemic due to better survival in the environment. It is commonly found in patients who had been treated with broad-spectrum antibiotics and have received vancomycin. Based on the local surveillance, selective screening should be considered for high-risk patients in identifying colonized individuals. In an outbreak situation, screening swabs for culture from multiple body sites, i. Since the most frequent site of colonization is the large bowel, a faecal sample is the most useful screening specimen. It is important to emphasize that stool carriage may persist for months or years and oral antibiotic therapy to eradicate the carriage is not successful. Patients can remain colonized for a long time after discharge from hospital therefore an alert system for re-admission of these patients is required so that these patients can be promptly identified and placed in a single room with en suite toilet and isolation precautions. It also poses problems to health care facilities as numerous outbreaks have been reported worldwide. These organisms can develop resistance during treatment against third-generation cephalosporins (cefotaxime, ceftriaxone, and ceftazidime) due to the induction of chromosomal AmpC beta-lactamases. Non-fermenters: Pseudomonas aeruginosa, Acinetobacter baumannii, Stenotrophomonas maltophia, etc. Although newer agents are available, they are not as effective as older agents and their side effects and clinical efficacy for treatment of various infections is not fully evaluated. Most of the patients from the community are colonized in the urinary tract and wound sites. Early identification by taking screening swabs and prompt isolation is essential, especially if the patients are being admitted to a high-risk unit. Since Gram-negative bacteria mainly survive in wet environments, it is essential that the environment be kept clean and dry. Make sure that bedpan washer disinfector, or macerators are in good condition and in working order. If a bedpan washer disinfector breaks down, it should be repaired as an emergency. Bedpans and urinals should be disinfected using heat treatment, if possible, or disposable bedpans and urinals can be used, if available. Communal equipment (especially if wet) may act as a source for these organisms, therefore ward equipment must be stored dry. Urine drainage bags must be emptied by the tap, for which single-use disposable gloves should be used and hands must be washed after the procedure. A separate jug or container should be used for each patient when emptying urinary drainage bags. Extended-spectrum beta-lactamases Many soil microorganisms are capable of producing beta-lactamases as part of defence mechanisms to protect themselves. These organisms have a propensity to spread from patient to patient and represent a major threat as several outbreaks have been reported worldwide due to spread of mobile genetic element plasmids or transposons and the dispersion of specific clones. Recent emergence of metallo-beta-lactamases has compromised the clinical utility of this class of antibiotics. In addition, resistance to carbapenems may also be induced as a result of increased production of either AmpC beta-lactamases coupled with increased efflux of the drug. Most of the carbapenamases are either intrinsic to some species as in Acinetobacter and Stenotrophomonas while others are plasmid mediated. Beta-lactamase enzymes can be broadly divided into: 1) serine beta-lactamases which use a serine amino acid in their active site to hydrolyse -lactams, and 2) metallobeta-lactamases, which use Zn++ cations to disrupt the beta-lactam ring. Classification of selected beta-lactamase of Gram-negative bacteria are summarized in Table 10. There are over 30 species and the organism is found in soil, sewage, and water and is occasionally a cause of food spoilage. Various species colonize the human skin and they may be readily recovered from the forearm, forehead, and toe webs of healthy volunteers. However, it is has become a major cause of hospital-acquired infections because of its remarkable ability to survive and spread in the hospital environment and to rapidly acquire resistance determinants to a wide range of antibiotics.
Buy cheap accutane 5 mg
Both facilities were tertiary care acne wipes effective accutane 5 mg, academic medical centers within the same metropolitan area (Chicago, Illinois). Other organisms recovered included Acinetobacter baumanii, Escherichia coli, and Proteus mirabilis, with sensitivities of 50, 36. The gold standard comparator in this study was the culture of clinical specimens within 30 days of the surveillance culture. In the largest controlled study of active surveillance, nearly 22,000 patients at a Swiss teaching hospital were split into two arms. No differences were observed in patient characteristics between the two arms of the study. This finding alone is important from an ethical standpoint, because patients under contact isolation precautions receive fewer visits from healthcare providers, have less contact time with clinicians during their hospital stay, and, as a consequence, may suffer both clinically and psychologically (Knowles, 1992; Kirkland and Weinstein, 1999; Evans et al. This seek and destroy approach has been successful in a multitude of facilities; however, the key "Counterpoint" to this principle, presented by Dr Diekema, is practices that do not include active surveillance. The Role of the Clinical Microbiology Laboratory in Surveillance and Infection Control the most important role of the clinical microbiology laboratory as part of the infection control team is to promptly and accurately detect nosocomial pathogens and their antimicrobial resistance patterns (Barenfanger et al. It is also important for the laboratory to work with both the infection control and information technology departments to determine how best to deliver microbiology laboratory results in a streamlined fashion, so that outbreaks and clustered increases in prevalence can be quickly identified and acted upon. The microbiology laboratory can provide online culture information about individual patients, outbreaks of infection, and antibiotic susceptibility patterns of pathogens in periodic antibiotic susceptibility summary reports. The laboratory also can assist with surveillance cultures and the facilitation of molecular typing of isolates during outbreak investigations. If microbiology laboratory work is not performed on-site, it is imperative to assure that the services needed to support an effective infection control program will be available. Finally, the microbiology laboratory is under increasing pressure to provide rapid test results. As hospital lengths of stay decrease, the window of clinical relevance and clinically actionable results becomes smaller and smaller (Peleg and Hooper, 2010). Rapid diagnostic testing of clinical specimens for the identification of respiratory, gastrointestinal tract, and central nervous system viruses, as well as Bordetella pertussis, is particularly important for facilities that care for pediatric patients. The knowledge gained as part of an active hospitalbased surveillance program can continue to inform better infection control and antimicrobial stewardship practices. It is over this key premise that laboratories find themselves at a rate-limiting step. Because of consistent reductions in reimbursement from governmental healthcare payers since the mid-1990s, most hospitals and medical centers are unwilling or unable to dedicate the necessary personnel and financial resources to establishing an aggressive infection control program that includes active surveillance of important nosocomial pathogens (Peterson et al. Peterson and Noskin (2001), in a study that showed a 23% reduction in healthcare-associated infections using an integrated infection control program that included on-site molecular typing of nosocomial pathogens to determine clonality, suggested that hospitalbased clinical microbiology laboratories should be offered easily obtainable annual federal grants to enhance their laboratory support for infection control purposes. Whilst specific laboratory methods are outside the scope of this chapter, there are general administrative decisions that must be made when the clinical microbiology laboratory is preparing to engage in active surveillance. Fundamental knowledge, usually from historical analysis of antimicrobial susceptibility testing results, is necessary to understand the endemicity of certain prevalent organisms in the healthcare facility. For all other scenarios, standard infection control practices should be the prevailing approach-those so-called "horizontal" approaches to infection prevention that apply to all at-risk patient populations and are designed to prevent infections due to all pathogens. A risk assessment is the most appropriate course of action in order to determine how best to utilize precious laboratory resources; and of course, these decisions should be made in collaboration with the infection control team. Concluding Remarks One school of thought for determining the feasibility of implementing an active surveillance program was put forth by Harris et al. These authors propose the need for understanding the following: (i) the performance of available screening methods for organisms of interest. Hospitals must develop an infection control plan that outlines the scope of the infection control program, and defines the specific goals of the program as well as the metrics to be used for assessment of progress toward those goals. The infection control team should conduct an annual risk assessment, and the findings should be incorporated in the infection control plan for the upcoming year. Increasing healthcare costs and concomitant decreases in reimbursement have created enormous financial pressures on healthcare facilities. This truth introduces an economic incentive for hospitals to focus on quality medical care. Additionally, emerging infectious diseases and the threat of bioterrorism require a quick response from infection control programs in order to protect both patients and healthcare workers, and to prevent disease transmission. Lastly, but perhaps most importantly, infection control teams must demonstrate that their policies and practices are grounded in evidencedbased medicine. Critical evaluation of the literature is required of the infection control team in order that evidenced-based protocols are implemented. The clinical microbiology laboratorian, as a central pillar of the infection control team, is well suited to providing guidance and consultation on each of these challenges. In the current fiscal climate, in which microbiology laboratories are being asked to do more sophisticated testing, while still keeping their budgets in line, it is this laboratorian who can critically evaluate the literature to provide informed recommendations for testing based on in-depth knowledge of both medical and laboratory science, and make decisions, in conjunction with the entire infection control team, to provide the most appropriate course of action for his or her facility. Hospital infection control: recent progress and opportunities under prospective payment. Active Surveillance and the Prevention of Healthcare-acquired Infections 103 10 the Role of the Antibiogram in Antibiotic Stewardship Gary V. When crafted appropriately and distributed wisely, the information contained in cumulative antibiograms can serve as a valuable tool for optimizing antimicrobial therapy in patients with infection, an extremely useful information resource for active antimicrobial stewardship programs, and, ultimately, a vehicle for diminishing the burden of antimicrobial resistance in many different healthcare settings. These authors examined the results of antibiograms crafted in the laboratory with and without prior careful clinical assessment of patients with infection. Eliminate duplicate isolates It is also very important when crafting cumulative antibiograms to avoid the inclusion of susceptibility test results that have been obtained from what are essentially multiple isolates of the same organism from the same patient (Shannon and French, 2002; Horvat et al. Especially in care areas where patients reside for prolonged periods of time and where chronic infections often occur. For the purpose of crafting a cumulative antibiogram, these should only be counted once (Shannon and French, 2002; Horvat et al. The inclusion of results obtained with nonclinically significant isolates can lead to erroneous and potentially clinically misleading information, and should be avoided. A simple way of accomplishing this is to include only the first isolate of a given organism from an individual patient. Capturing only the first isolate of a particular organism from each patient potentially violates one of the most basic precepts of antimicrobial susceptibility testing, namely, when in doubt, err on the side of being conservative. That is, it is better to include rather than to exclude organisms that are resistant. A simple way to avoid missing important resistant organisms is to do the following. In addition to tabulating the first isolate of a given organism from an individual patient over a 1 year period (irrespective of the number of hospitalizations), also include any secondary isolates of that organism that may arise that are characterized by a more resistant susceptibility profile. Defining exactly what constitutes a definitive change with respect to resistance can be challenging. However, with careful consideration in consultation with infectious disease physicians and clinical pharmacology staff, guidelines can readily be developed that identify new organisms that have emerged as resistant. Having created such guidelines, rules-based algorithms can be programmed into laboratory information systems that allow for easy and reliable identification of these organisms for inclusion in the antibiogram. Only agents that can reliably be tested in the laboratory against specific organisms are candidates for inclusion in cumulative antibiograms. With this as a starting point, additional criteria for selecting which antimicrobial test results should be provided in cumulative antibiograms include the demonstrated clinical value of agents in the treatment of infections due to a specific pathogen, practice patterns in individual institutions, and lastly, formulary composition. Final decisions as to which susceptibility test results should be included in antibiograms should always be made in consultation with infectious diseases physicians, as well as the clinical pharmacy. Please note that for the purpose of facilitating use of the information, various types of Gram-positive and Gram-negative bacteria are separated. Yeast and anaerobic organisms are often presented in separate antibiograms if those isolates routinely have their susceptibility testing performed within the institution. Compiling susceptibility test results and composing antibiograms Today, the requisite information for compiling antibiograms can typically be easily accessed either from laboratory information systems or directly from the instrumentation that is used to perform antimicrobial susceptibility tests. For the purposes of a cumulative antibiogram, the percentage of isolates determined to be susceptible should be tallied. Information on the percentage of intermediate or resistant isolates or the results of the Role of the Antibiogram in Antibiotic Stewardship 105 Trimethoprim/ Sulfamethoxazole Organism (number tested) Enterobacteriaceae Citrobacter freundii group (97) C. High-dose or extended infusions of piperacillin/tazobactam and other -lactam antibiotics should be considered.
Japanese Ashitaba (Ashitaba). Accutane.
- Dosing considerations for Ashitaba.
- Are there safety concerns?
- Acid reflux, peptic ulcers, high blood pressure, high cholesterol, gout, constipation, allergies, cancer, smallpox, food poisoning, and other conditions.
- What is Ashitaba?
- How does Ashitaba work?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=97078
Order discount accutane on-line
Laboratory diagnosis Screening and treatment of asymptomatic patients is not necessary acne off discount 10mg accutane overnight delivery. Once the diagnosis has been confirmed, repeat specimens for clearance should not be taken unless there is a relapse following treatment. Persistently positive test results at the end of treatment are not predictive of a C. Cytotoxicity assay: the cell cytotoxicity assay (detects the cytopathic effect of toxin B on cultured cell lines), is considered the gold-standard clinical laboratory assay for the diagnosis; however, this facility is not available in most diagnostic C. The main disadvantage of this assay is it lacks both sensitivity and specificity compared to cell cytotoxicity assays. It can be used as initial screen as the test result are available within 2 hours and some studies have reported a good negative predictive value. However, stool culture are required in an outbreak situation for epidemiological investigations and are necessary for ribotyping. The capacity to form spores enables the organism to persist and survive in the environment for months. Environmental contamination can be heavy, especially if the diarrhoea is severe or accompanied by incontinence. Asymptomatic patients after infection may continue to shed organisms in their stools and serve as a source of contamination. The following infection control precautions should be taken: Promptly diagnosis and isolate all patients with C. In a cohort area, mixing of patients carrying 027 strain and non-027 should be avoided. To prevent spread, transfer of patients between wards/units and health care facilities should be restricted unless considered essential. Hands can become contaminated by direct contact with patients colonized/infected with C. Therefore, strict hand washing with soap and water before and after contact with patients and environmental surfaces is the most effective control measure to prevent cross-infection. Prompt isolation of patients as soon as possible in a single room with en suite toilet. Use of non-sterile single-use gloves and a plastic apron for patient care activity. Mop heads should be disposable or laundered after each use and single-use disposable cloths must be used. If the patient is discharged or transferred to another hospital or long-stay health care facility, appropriate personnel at the receiving health care facility must be informed. Avoid antiperistaltic medication: diarrhoea is the response of the infected host to expel pathogens/toxins responsible for enterocolitis. Use of opiates and antiperistaltic drugs results in the retention of pathogen/toxin, probably worsens enterocolitis-associated necrosis of the colonic mucosa, and increases the risk of toxic megacolon. Vancomycin should not be prescribed as a first-line therapy because of cost and problem of emergence of vancomycin-resistant enterococci. This is given as retention enema using 18 gauge Foley catheter with 30-mL balloon inserted per rectum and then instilling vancomycin. It is important to remember that monitoring severity of disease by the number of stools passed each day by patients using Bristol stool chart may be an unreliable indicator of severity of disease; other parameters must also be monitored on a daily basis to assess the severity. Although diarrhoea and vomiting may be caused by infectious and non-infectious agents all cases of gastroenteritis should be regarded as infectious unless good evidence suggests otherwise. Diarrhoea is defined as three or more loose/watery bowel movements that take up the shape of their container (which are unusual or different for the patient) in a 24-hour period. Infected individuals with gastroenteritis are classified into four risk groups that pose an increased risk of spreading infection (see Box 11. It is particularly important to assess infected people who belong to one of the four groups of persons for whom special action should be considered. A liquid stool is more likely than a formed stool to contaminate hands and the environment, and is consequently at greater risk of spreading faecal pathogens. Formed stools voided by asymptomatic infected people, or people who have recovered from illness, may contain pathogens and are less likely to transmit infection provided good personal hygiene can be achieved. Viral gastroenteritis Clinical and epidemiological features of gastroenteritis viruses are summarized in Table 11. Outbreaks of gastroenteritis caused by viruses are more common in health care settings, cruise ships, hotels and restaurants, day care centres and nurseries. Compared to bacteria, the viruses have a much lower infective dose, with many viral infections being largely asymptomatic or subclinical in healthy adults. Contamination of fomites from enteric viruses can also originate from aerosolized vomit which can spread over a very wide area resulting in contamination of both the environment and people in the vicinity. Enterotoxin causes epithelial necrosis in colon which can lead to pseudomembranous colitis and toxic mega colon and death; common with 027 strain Treat with metrinodazole or vancomycin, if symptomatic Can be endogenous. In certain circumstances, food handlers will need to be temporarily excluded from work or restricted to non-food handling duties to reduce the risk of spreading infection via food. The decision to exclude or restrict any food handler should be based on individual risk assessment. In addition, viruses aerosolized from flushing the toilet can remain airborne long enough to contaminate surfaces and items present in the bathroom. Therefore, it is advisable that the lid of the toilet should be closed before flushing. Enteric viruses have been detected in carpets, curtains, and lockers, which can serve as a reservoir. In addition, norovirus, adenovirus, and rotavirus have all been isolated from naturally-contaminated fomites. Adenovirus has been isolated on drinking glasses from bars and coffee shops, and rotavirus was detected on up to 30% of fomites in day care centres. Spread of all infectious diseases, both enteric and respiratory, is very common amongst children in nursery and day care centres. It has been observed that a small child puts his fingers in his mouth once every 3 min, and in children up to 6 years an average hand-to-mouth frequency of 9. Norovirus gastroenteritis Norovirus belongs to the family of Caliciviridae viruses.
Cheap accutane master card
There is cortical thinning and a single focus of probable cortical breakthrough (arrow) skin care lines for estheticians buy accutane. The matrix material begins to assume a more myxoid appearance and there is increased cellularity and nuclear irregularity. It represents about 2% of all cases of chondrosarcoma and has a strong tendency to occur in the epiphysis (or occasionally the apophysis) of long bones. A wide age range of individuals is affected, but there is a peak incidence in young adulthood. The margin of the lesion is often sclerotic, giving a false impression of a benign neoplasm. Some of the cells have abundant pale pink cartilage and can easily be confused with the chondroblasts of chondroblastoma. This imparts a "crowded" look to this neoplasm that sometimes invokes a differential diagnosis of metastatic carcinoma. Individual cells tend to appear more clear and epithelioid than regular chondrocytes, even when associated with hyaline cartilage. Aspirates are moderately cellular, usually with at least some extracellular chondromyxoid matrix material present, but less so than in conventional chondrosarcoma. In Giemsa-stained preps, they often have very foamy cytoplasm and occasionally a plasmacytoid appearance. Although the "clear cell" features are not always well identified in smears or touch preps, they are easily identifiable in cell block materials prepared by conventional methods. Imaging findings include a lytic lesion centered on the medullary cavity of the bone. The radiographic differential diagnosis usually includes osteomyelitis and Ewing sarcoma. Treatment options include simple observation, lesional curettage, or L corticosteroid injection. To date, cytogenetic studies have shown recurrent abnormalities of chromosomes 1, 9, and 22. The Langerhans cells are admixed with a variety of other inflammatory cells including numerous histiocytes, plasma cells, neutrophils, and eosinophils. In addition, occasional multinucleate, osteoclast-like giant cells are admixed in the lesion. This inflammatory infiltrate often tends to overshadow the true Langerhans cell, which is the pathognomonic feature of this disorder. Likewise, pleomorphism is largely confined to the Langerhans cell population and aside from the strange coffee bean appearance, is usually minimal. This is due in large part to the distinctive appearance of the Langerhans cells on cytologic preparations. Of note, Giemsa-based stains, commonly used for immediate assessment, often fail to highlight the nuclear details (longitudinal indentations) that are so characteristic of the Langerhans cells. They often have irregular nuclear configurations, often with longitudinal grooves similar to those of coffee beans. In this example, there is an osteoclast-type giant cell, inflammation, and histiocytes, some featuring irregular nuclear grooves. Giant cell reparative granuloma is the preferred term for lesions of the craniofacial bones. The metacarpal and metatarsal bones are more commonly affected than carpal or tarsal bones. Patients present with symptoms of pain and swelling in the tumor region and may often have an associated pathologic fracture. The bone cortex is most often thin but intact, and a periosteal reaction is usually absent. On cross sectional imaging, there may be evidence of internal septation and cystic cavity formation. Individual or focal collections of foamy macrophages are another frequent finding. The pathognomonic finding is the presence of multinucleate, osteoclast-like giant cells. Reactive bone may be present and is particularly prominent in the lesions that have undergone pathologic fracture. Brown tumor should be in the differential diagnosis of any giant cell-rich neoplasm located in an unusual site. This entity can be quickly confirmed or eliminated by serum measurements of parathyroid hormone, calcium, and phosphorus. The distal femur and proximal tibia are the most common sites, with other common locations including the distal radius and the sacrum. Patients often notice pain and swelling of the affected bone or often present with a pathologic fracture through the lesion. There may be thinning or destruction of the adjacent cortex, with extension into adjacent soft tissue. As mentioned previously, a subset of patients, about 25%, experience one or more local recurrences after surgery. These usually develop in the soft tissues adjacent to the previous excision site and occur relatively quickly, within 1 or 2 years of the original tumor removal. This phenomenon is thought to represent vascular displacement of tumor rather than true malignant metastatic potential. The latter concept is supported by the slow-growing nature of the "metastatic" foci. At least some of these seem to have followed radiation treatment for a benign precursor lesion. The individual, single cells in the background have nuclei that resemble those of the osteoclastic cells. They are usually round to oval with open chromatin and one or more prominent nuclei. In addition, small fragments of osteoid or bone are frequently found, particularly after fracture or biopsy. This latter finding can often cause diagnostic confusion and should not be interpreted as a sign of a malignant lesion such as osteosarcoma. This feature does not appear to correlate with a tendency to more aggressive behavior. This feature is also commonly identified in resections of pulmonary "implants" or "metastases" of giant cell tumor. These are usually single or loosely adherent to a background population of ovoid to spindled stromal cells. Of note, the nuclear features of the background cells are very similar to those of the multinucleate giant cells. Likewise, pigment, a feature present in aspirates of other types of giant cell tumors, is absent as well. This is one of the few bone tumors that typically extends to the articular surface. The number of mitotic figures does not correlate with the probability of recurrence or other aggressive behavior. The nuclei of the giant cells are identical in appearance to those of the mononuclear cell population in the background. This lesion tends to occur in children and younger individuals with a peak incidence between 5 and 20 years of age. Individuals with the polyostotic form of disease tend to present at a younger age, usually before 10 years. The polyostotic form of the disease has two distinctive presentations: a monomelic variant confined to one extremity and ipsilateral pelvis or the polymelic variant, which tends to involve several different bones. Monostotic lesions are frequently asymptomatic and are often incidental findings on imaging studies performed for other reasons. Symptomatic lesions can present with localized pain or, occasionally, pathologic fracture. Often there is a distinct rim of reactive bone surrounding an area of hazy lucency. There may be extensive distortion of the normal bone architecture due to stress on the weakened bone. Asymptomatic lesions that are not at risk for fracture can simply be followed by imaging.
Buy accutane 40 mg amex
When continuous renal replacement therapy is utilized in critically ill patients skin care untuk jerawat best buy for accutane, the type of filter, run time, flow rate, and ability of the drug to be removed by the system must be considered when adjusting doses. Davis frequency adjustment performed to maintain adequate drug concentrations (Roberts and Lipman, 2009). Therapeutic drug monitoring, when possible, is recommended to ensure adequate drug concentrations. Volume of distribution Patients who are experiencing severe acute illness are typically given extreme fluid volume resuscitation with normal saline to return their blood pressure to normal values. However, in the acute phase, patients may be experiencing fluid shifts caused by the systemic inflammatory process. Fluid shifts from the intracellular space to the extracellular space, otherwise known as third spacing, can drastically change drug behavior. Hydrophilic antimicrobials, such as -lactams, aminoglycosides, and linezolid, will have a much larger Vd than in a healthy patient, whereas, hydrophobic antimicrobials, such as fluoroquinolones, macrolides, and clindamycin, will not see much change in their Vd. Because of this concept, the net increase in body weight secondary to fluid resuscitation should be added to the total Vd to provide adequate antimicrobial concentration within tissues and plasma. As the Vd increases, the half-life of the antimicrobial will also increase, providing the patient with active drug for longer periods of time. Clinicians must also consider the ability of antimicrobials to penetrate to the site of action. In particular, hydrophilic antimicrobials tend to have lower interstitial penetration, while hydrophobic antimicrobials are largely unaffected and retain their interstitial penetration. Additionally, most of the fluid given during resuscitation distributes to the tissues, subsequently diluting the concentration of the antimicrobial within the site of action, despite its higher distribution. Protein binding Hypoalbuminemia is a problem in critically ill patients as drug pharmacokinetic and pharmacodynamic properties can be severely altered, requiring dose and frequency adjustment. For example, as the level of albumin and other systemic proteins decrease, the Vd of highly bound drugs increases, making more unbound, active drug available. Aminoglycosides have a larger Vd, in part from fluid resuscitation and hypoalbuminemia, and would require a larger dose to compensate for the expanded Vd, despite more free drug being available. Decreased protein binding of acidic and basic drugs also allows for the increased clearance of antimicrobials. However, as these patients improve and reach clinical stability, they may no longer have contraindications to oral therapy and may be considered for conversion. Patients recovering from critical illness may continue to require nutrition provided through enteral feeding tubes. There are some challenges with the administration of antimicrobials through these tubes, such as the concurrent administration of enteral feeding and the antimicrobial, and binding to the enteral tube. Electronic medical records with clinical decision support can be used to identify patients meeting criteria, and generate alerts and reminders to pharmacists, or Switching from Intravenous to Oral Administration 261 Table 22. Administration recommendations Duodenum Hold tube feed to administer medication then restart Hold tube feed to administer medication then restart Primary absorption site Break in feeding required Other considerations Suspension contains small amount of sorbitol (<7. In systems without this technology, the antimicrobial stewardship program may elect to use other screening methods to identify patients, and then intervene in person. Policies may also include language to delegate authority to clinical pharmacists to facilitate the ordering and monitoring of oral antimicrobials in patients meeting the prespecified criteria. This will aid not only in designing computer-generated alerts for qualified patients, but also in designing the necessary educational programs to accompany policy implementation. It is a common misconception that insurance providers and other payers will not reimburse for hospital stay in patients on oral therapy. Indeed, if no other medical issues remain to be managed, antimicrobial conversion to oral therapy should be used to facilitate discharge or transfer. However, if other comorbid conditions necessitate longer hospital stay, receipt of an oral antimicrobial should not preclude a patient from remaining hospitalized. This might include prospective audit with intervention and feedback, patient-specific education materials, nursing and physician education materials, and physician reminders to assess further need for antimicrobial therapy. Key stakeholders should be included in the program planning and rollout, including opinion leaders from infectious diseases, nursing, case management, hospitalists (specialists in the practice of hospital medicine), and others. Employing a multifaceted, interdisciplinary approach supports the successful alteration of prescriber behavior and long-term success. It is also recommended that compliance with the policy be monitored routinely with the dissemination of results to all participating individuals. This will also provide evidence of clinical and economic benefit for continued justification of the program. Switching from Intravenous to Oral Administration 265 23 the Role of Pharmacists in Antimicrobial Stewardship Haley J. As antimicrobial stewardship inherently involves the appropriate selection, dosing, route of administration and duration of antimicrobial drug therapy, there is a direct link to the roles and responsibilities of the pharmacist. In fact, hospital pharmacists have been involved in practices to improve antimicrobial use, such as recommending antimicrobial dose adjustments for organ dysfunction and managing antimicrobial formularies, long before any formal recommendations for antimicrobial stewardship existed. These types of achievements have placed pharmacists in the forefront of antimicrobial stewardship. It is the responsibility of both the physician and pharmacist leaders to act as "antimicrobial stewardship champions," taking ownership over the mission for building the program and overseeing and advocating for antimicrobial stewardship throughout the hospital (Septimus and Owens, 2011). The main points from these documents on the role of hospital pharmacists in antimicrobial stewardship are summarized in Table 23. Additionally, the chapter describes formal and non-formal training opportunities for pharmacists practicing antimicrobial stewardship. Encouraging multidisciplinary collaboration to ensure that the prophylactic, empiric, and therapeutic use of antimicrobials result in optimal patient outcomes within the institution. Making recommendations to improve the selection, dosing, timely initiation, proper monitoring and de-escalation of antimicrobials. Assisting the Pharmacy and Therapeutics Committee to ensure that the antimicrobials available are appropriate for the patient population served and in developing restricted antimicrobial use procedures, therapeutic interchange, treatment guidelines, and care plans. Collecting and analyzing antimicrobial use data and performing clinical and economic outcome analyses. Collaborating with microbiology to ensure appropriate and timely antimicrobial susceptibility testing. Using information technology to streamline antimicrobial resistance surveillance, antimicrobial use and clinical outcome reporting, and the development of clinical decision support tools. Using efficient and effective systems to reduce the risk of adverse drug events and medication errors to promote safe antimicrobial management practices. Participating in efforts to prevent the transmission of infections among patients, healthcare workers, and others within the hospital. Educating multidisciplinary health professionals, other pharmacists and pharmacists in training, patients, and the public in antimicrobial stewardship and infection. Directors of pharmacy continuously interact with hospital administrators and other department heads. Therefore, pharmacy directors may also be involved in the decisions of hiring antimicrobial stewardship personnel, in particular the antimicrobial stewardship pharmacist leader. Pharmacist time that is devoted to the program is essential to its success, as is the cooperation of the pharmacy staff that works with the antimicrobial stewardship pharmacist leader. Hospital pharmacists All pharmacists are trained to be medication experts and are highly educated in a wide variety of pharmacotherapy issues, so they have an inherent responsibility to ensure that all patients at their institution are receiving the optimal antimicrobial therapy. Nonetheless, there are many different roles for pharmacists in hospitals, such as medication processing and dispensing, the optimization of medication therapy, and providing drug information and education. Additionally, there are many different specialized or clinical coordinator pharmacist positions available at many hospitals, and there are often student and resident pharmacists in training as well. The structure of pharmacy departments itself may differ from one institution to another, with some institutions having centralized and some decentralized pharmacies. Despite differences in job duties and pharmacy structure, all of the pharmacists involved can meaningfully contribute to antimicrobial stewardship, although the specific roles that each will play may differ. It is important to note that all recommendations made by hospital pharmacists should align with those of the antimicrobial stewardship team. To facilitate parallel recommendations, there should be regular communication between the two parties. Due to their role in processing medication orders and familiarity with the hospital formulary, pharmacists whose primary responsibility is in processing and dispensing may meaningfully contribute to antimicrobial stewardship. These pharmacists may serve as "gatekeepers" for restricted antimicrobials by notifying prescribers that authorization is required for their use. Pharmacists can also assure that the right dose of an antimicrobial is ordered, and that the ordered antimicrobial can be safely used in the patient.
40 mg accutane
If it is necessary to raise collection bag above bladder level for a short period skin care physicians purchase accutane 10 mg with mastercard, drainage tube must be clamped temporarily Empty bag every 8 h or earlier, if full Do not hold bag upside down when emptying 4. Urethral catheterization is considered as a minor surgical procedure therefore the catheter must be inserted using an aseptic technique and sterile equipment. Before the procedure, check the expiry dates, integrity of containers/packages and the correct amount of sterile water required to be inserted if the device has a balloon. Lay out the sterile field on top of the trolley, making sure all items required are open and accessible. Sterile gloves must be worn for the procedure and an aseptic non-touch technique should be used. In a female, separate the labia and cleanse the vulva using a front-to-back technique. Insert the catheter and advance it by holding the inner sterile sleeve, avoiding contact with the non-sterile surface. The aseptic non-touch technique should be used, in which the operator has no contact with the sterile shaft of the catheter. Hang the drainage bag below the level of the bladder to stop reflux or apply the leg bag with the support. The bag must be supported in the drainage stand to allow free flow of urine and to prevent the bag from touching the floor. There is no evidence that they decrease symptomatic infections and therefore they should not be used routinely. However, their use should be considered in reducing bacteriuria in catheterized patients, especially in those patients at highest risk of either bacteriuria or complications associated with bacteriuria. Larger diameter catheters block the urethral gland and put pressure on the urethral mucosa, which may result in ischaemic necrosis. They are also resistant to bending and are more likely to cause pressure necrosis, especially in males. In general, the smallest diameter catheter (with a 10-mL balloon) that allows free flow of urine is the most desirable. The smallest size/gauge catheter is also less likely to be associated with leakage. Urological patients may require larger diameter catheters and these must be used on the advice of the urologist. Long-term antibiotic prophylaxis is ineffective and predisposes to infection with resistant microorganisms and fungi and is not recommended. Consideration after catheterization Maintenance of catheter: after insertion, regular inspection of the catheter and drainage system must be attended to and documented at least daily. The date and time of catheter changes should be documented either in nursing or medical notes. Meatal care: meatal cleansing should be performed at intervals appropriate for keeping the meatus free of encrustations and contamination. Daily routine bathing or showering is all that is needed to maintain meatal hygiene. If faecal incontinence occurs, the perineum must be cleaned and the catheter changed without delay. Therefore it is important that the sterile drainage bags should be positioned in a way that prevents back-flow of urine. The urinary drainage bags should be put on a holder attached to the bed frame or a stand to prevent contact with the floor. The bag and tubing must at all times be below the level of the bladder so that flow can be continuously maintained by gravity. The spout from the tap must be completely emptied to minimize a build-up of microorganisms in the stagnant urine. Extreme care must be taken when emptying the drainage bag to prevent crossinfection. Hands must be disinfected and non-sterile, single-use gloves should be worn before emptying each bag. Alcohol impregnated swabs may be used to decontaminate the outlet (inside and outside) before and after emptying the bag. When emptying the drainage bag, use a separate container for each patient and avoid contact between the urinary drainage tap and the container. For the purposes of measuring urinary output, an integral measuring device is necessary. After emptying the receptacle, non-sterile, single-use gloves should be discarded in a clinical waste bag and hands washed and dried thoroughly. The introduction of such agents causes erosion of the bladder mucosa and promotes the emergence of resistant microorganisms. If the catheter becomes obstructed and can be kept open only by frequent irrigation, the catheter should be changed, as it is likely that the catheter itself is contributing to obstruction. However, continuous or intermittent bladder irrigation may be indicated during urological surgery or to manage catheter obstruction and should only be undertaken on the advice of an urologist. Condom use for 24-hour periods should also be avoided and other methods, such as napkins or absorbent pads, used at night. Specimen collection: closed drainage bag should not be disconnected to obtain a sample as this causes interruption to the closed system and may pose a risk of infection to the patient. If a sample of urine is required for bacteriological examination, it should be obtained from a sampling port using an aseptic technique. The sampling port must first be disinfected by wiping with a 70% isopropyl alcohol impregnated swab. The sample may then be aspirated using a sterile small bore needle and syringe and transferred into a sterile container. Removal of catheter: the optimal time limit for replacing catheters depends upon individual circumstances and the type of catheter used. However, urinary catheters should not be changed as long as they are functioning well. A catheter that requires frequent irrigation for recurrent obstruction should be changed and replaced. The routine administration of prophylactic antibiotic at the time of catheter removal is not recommended. Culturing of urine sampled after catheter removal is indicated only for patients where there is a high degree of suspicion or symptoms suggestive of infection. Management of patients with bacteriuria and infections Asymptomatic bacteriuria the treatment of asymptomatic bacteriuria. In addition, the use of an antibiotic in the presence of the catheter often results in infection with a more resistant strain of bacteria. After the catheter is removed, in most patients the bacteriuria spontaneously resolves. If treatment is indicated, it is only for those cases in which the bacteriuria has persisted after catheter removal and in which there are no underlying anatomical or physiological barriers to eradication of the bacteriuria. Routine administration of prophylactic antibiotic at the time of catheter removal is not recommended. Symptomatic patients Febrile episodes are found in less than 10% of catheterized patients living in a longterm facility. Management of candiduria While it is clear that symptomatic candiduria requires treatment, it is controversial whether asymptomatic candiduria requires treatment. In the case of candiduria associated with urinary symptoms or if candiduria is secondary to systemic infection, parenteral therapy with an antifungal is indicated. However, the presence of Candida in a urine sample may reflect local infection elsewhere. Diabetes predisposes to the development of candiduria as glycosuria enhances urinary growth of Candida spp. In addition, diabetes also impairs host defences, particularly phagocytosis, and the development of a neurogenic bladder allows for urinary stasis and increases the likelihood of the urinary tract infections.
Discount accutane 10mg with amex
Resources are designed to enable students to prepare for interactive sessions to compare standard patient vignettes with their own clinical experience acne vulgaris treatments order accutane toronto. The interactive discussion sessions focus on learning prudent antibiotic prescribing through reflective practice. Prepared materials (in a PowerPoint format) in relation to structure and content for each interactive session are available for tutors to use. These resources include patient histories, clinical signs, investigations, and questions on diagnosis, assessing severity, appropriate prescribing, public health issues, and patient management. In addition, guideline answers to the questions with feedback are provided, including inappropriate responses and the corresponding reasons for them being inappropriate. Strong political support is necessary for a curriculum program to be successfully implemented. Conclusion For over 30 years antibiotic policymakers have been trying to curb antibiotic resistance. The bulk of the efforts have mainly been conducted at the adult public and professional postgraduate level, aiming to change behavior. Worldwide, only minimal investment has been put in antimicrobial stewardship education in undergraduate and fellowship training. It seems obvious that antimicrobial stewardship is likely to be more successful when the teaching is started much earlier, at the time when the knowledge, attitudes, and behavior of professionals are being shaped. There is a need for an undergraduate medical/professional curriculum that covers the principles of microbiology, infectious diseases, and clinical pharmacology, with emphasis on the principles of prudent prescribing in an adequate format. Appropriate curricula on antimicrobial stewardship are a joint responsibility of academia and the national ministries of Health and Education. Alberta Health Services and the British Columbia Centre for Disease Control, Canada. European Commission (2013) Special Eurobarometer 407 Antimicrobial Resistance: Report. The White House (2015) National Action Plan for Combating Antibiotic-resistant Bacteria. This distinguishes them from antiseptics, for example, which often work by more general mechanisms and therefore have a greater potential for toxicity to human cells. Mechanisms by which bacteria develop resistance to antibacterial agents may be specific for the mechanism of action of that agent, or applicable to a range of antimicrobial classes. In this chapter, I will endeavor to detail the variety of resistance mechanisms commonly found in human pathogenic bacteria. For clarity, I will delineate mechanisms by antimicrobial class, although a breakdown by species would also be informative. Aminoglycoside resistance is attributable to three mechanisms: (i) efflux pumps; (ii) target (ribosome) alterations; or (iii) enzymatic inactivation. In Escherichia coli, aminoglycosides are effluxed by the one-protein AcrD multidrug efflux transporter (Aires and Nikaido, 2005). Aminoglycosides the aminoglycosides (amikacin, gentamicin, kanamycin, neomycin, netilmicin, paromomycin, streptomycin, and tobramycin) are hydrophilic antibiotics that are particularly active against aerobic, Gramnegative rods and their antimicrobial activity is concentration dependent. Their principal target is the 30S subunit of the ribosome, the binding of which prevents the elongation of the growing peptide *E-mail: lrice@lifespan. Rice covalently modify specific amino or hydroxyl groups, resulting in aminoglycosides that bind poorly (higher Km, less affinity) to the ribosome. Both can be located on plasmids and other mobile elements, and have been found in a wide variety of species. Both are also highly efficient enzymes whose expression confers very high levels of resistance to ampicillin. Mutations at critical amino acids "extend the spectrum" of these enzymes and allow the hydrolysis of extended-spectrum cephalosporins (Phillipon et al. They disrupt the amide bond of a -lactam, thus permanently inactivating the antibiotic. Class A carbapenemases are becoming increasingly common, especially in Klebsiella pneumoniae (Pitout et al. These isolates are highly resistant to penicillins, cephalosporins, and commonly used -lactam/-lactamase inhibitor combinations, and show reduced susceptibility to carbapenems. With few exceptions (see below), class B -lactamases confer resistance to a wide range of -lactam compounds, including cephamycins and carbapenems, and are resistant to inactivation by clavulanate, sulbactam, and tazobactam. AmpC (ampicillin C hydrolyzing) enzymes, which are chromosomally encoded through the ampC gene, are particularly important in clinical isolates of C. Class C -lactamases hydrolyze cephalosporins more effectively than they do penicillins, but their activity against penicillins is sufficient to confer clinically significant levels of resistance. Most class C enzymes are resistant to inhibition by clavulanate, sulbactam, and tazobactam, but are inhibited by the recently approved -lactamase inhibitor avibactam. Increases in ampC expression may result from the action of some -lactam antibiotics (cefoxitin, clavulanic acid, and imipenem are specific examples) (Sanders and Sanders, 1988). Under these circumstances (induction), -lactamase is produced for only as long as the antibiotic is present in the medium. Constitutive high-level production of AmpC -lactamase most commonly results from a mutation in the ampD gene, reducing the quantity of (or eliminating) AmpD (cytosolic amidase) from the cytoplasm. Plasmid-mediated class C -lactamases have been described in many Gram-negative organisms. The loss of porin proteins in clinical isolates with plasmid-encoded AmpC enzymes may result in resistance to carbapenems (Bradford et al. Chloramphenicol Chloramphenicol acts by binding to the ribosome and inhibiting bacterial protein synthesis. Resistance to daptomycin in the clinical setting may arise associated with prolonged therapy. The precise mechanisms of resistance have not been defined, but overexpression of genes associated with increasing the positive charge of the cytoplasmic membrane and a disordering of phospholipids have been implicated (Mishra et al. Glycopeptides are only active against Gram-positive bacteria because their size precludes entry through the outer membrane porins of Gram-negative bacteria. Most glycopeptide resistance occurs through the acquisition of operons that encode the formation of altered peptidoglycan precursors. To date, several varieties of enterococcal glycopeptide resistance have been described (VanA through VanE, and VanG, VanM, and VanN). VanA enterococci are phenotypically resistant to vancomycin and teicoplanin, whereas VanB strains are resistant to vancomycin but appear susceptible to teicoplanin. This susceptibility results from the fact that teicoplanin does not induce expression of resistance (Evers and Courvalin, 1996). Gram-negative bacteria also express efflux genes specific for both chloramphenicol and florfenicol (floPp, floSt) that are often reported from animal-derived E. The ultimate outcome is a pentapeptide precursor terminating in d-alanine-d-lactate, in which the binding affinity of vancomycin to its target is reduced roughly 1000-fold (Hughes, 2003). Clonal complex 17 strains are now found worldwide and are characterized by their resistance to ampicillin and by the fact that they frequently harbor putative virulence determinants such as espEfm and hylEfm (Leavis et al. The VanC operon is intrinsic to the cell wall synthesis machinery of the minor enterococcal species E. However, within these cultures are smaller populations of cells that express higher levels of resistance. The resistance phenotype is characterized by a thickened cell wall, which may decrease glycopeptide susceptibility by providing an excess of false targets for glycopeptide binding. Resistance to linezolid has been described in both enterococci and staphylococci, but overall rates remain very low more than a decade after the first clinical use of this agent (Jones et al. As the 23S subunit genes exist as multiple copies, more than one copy must be mutated to confer resistance, with strains that have a higher percentage of mutated 23S genes expressing greater levels of resistance (Marshall et al.