Quality 10 mg glucotrol xl
The goal is not usually total excision blood glucose unit of measure order discount glucotrol xl line, as part of the cyst wall is commonly adherent to the spinal cord. Syringomyelia Syrinx cavities measure larger than 2 mm in axial diameter and tend to be eccentric. These dilated residual central canals are believed to have a stable nonprogressive natural history over time. Syringomyelia refers to cavities of the spinal cord parenchyma that may be lined by glial cells outside of the central canal. A majority of syrinx cavities associated with Chiari I malformations remain stable or resolve after Chiari decompression surgery. Although caudal displacement of cerebellar tonsils 5 mm below the level of the foramen magnum is the radiographic criteria for Chiari I malformation, this may not be clinically significant in isolation without symptoms. This concurrent diagnosis appears to be more common in clinically symptomatic patients. Syringomyelia symptoms are related to the level, size, and location of the syrinx and affected spinal cord parenchyma. Scoliosis in association with syringomyelia is thought to result from lateralized anterior horn compression manifesting as inequality in paravertebral muscle strength. Patients with underlying syringomyelia with scoliosis often present with scoliosis at a young age with an atypical curve, show rapid curve progression, and experience back pain symptoms. There are no prospective randomized controlled studies or large-scale long-term prospective studies to date for syringomyelia. At present, a combination of clinical judgment and data from many case series are used for clinical decision support. Patients with asymptomatic Chiari I malformation do not necessarily require surgical intervention, whereas those with symptoms directly attributable to the Chiari I malformation have a favorable response to decompression. The presence of a syrinx in association with Chiari I malformation is typically surgically treated. The syrinx is thought to be likely to progress in size and in clinical symptoms if left untreated. In the setting of scoliosis, surgical management of scoliosis with an unrecognized syrinx is associated with the risk of neurologic complications. Intervention on syringomyelia with scoliotic curves less than 30 degrees has a more favorable prognosis in terms of avoiding future surgery and fusion. The primary treatment of choice for Chiari I malformation with or without syringomyelia at a majority of pediatric centers is posterior fossa decompression. There is no consensus on optimal operative technique for posterior fossa decompression. There may be persistent blockage at the foramen magnum with bone-only decompression in a subset of patients, which would necessitate further surgery with intradural exploration. Dural opening, duraplasty, or cerebellar tonsillar shrinkage may be added at the initial surgery or at reexploration. The arachnoid may be left intact, or there may further intradural exploration with lysis of adhesions (such as arachnoid veils or webs at the foramen of Magendie). Use of intraoperative ultrasonography to ascertain adequate decompression and movement of the cerebellar tonsils with each cardiac cycle may aid in determining the type of decompression. Management of symptomatic syringomyelia is approached by identifying and treating the etiology of the syrinx. Other important considerations include addressing hydrocephalus first, if present, prior to other corrective surgery for Chiari malformation or syringomyelia. In cases with concomitant craniocervical bony abnormalities or anterior compression of the brainstem, consideration is given to posterior occipital cervical fusion at the time of posterior fossa decompression, with or without anterior decompression, as neurologic compromise or progression has been reported in posterior fossa decompression alone. It is thought that these patients harbor chronic instability at the craniocervical junction. Regardless of the presenting symptoms, treatment of hydrocephalus and patency of any existing shunt system need to be addressed first. If surgery is done for well-selected Chiari I malformation patients with appropriate targeting of the syrinx etiology, a majority of patients respond well symptomatically and demonstrate clinical and radiographic improvement or resolution of the syrinx. Persistent syringomyelia or persistent symptomatic Chiari I malformation is thought to be due to inadequate decompression or arachnoid scarring. Shunting of the syrinx can be directed to the subarachnoid space or to more distant termini such as the pleural or peritoneal space. The cause of this lesion is distinct from that of the cervical, Chiari-related syrinx,119 or acquired syringes from tumor or trauma. A terminal syrinx is most frequently associated with tethered cord syndrome associated with low-lying filum, anorectal abnormality, meningocele manque, diastematomyelia, or lipomyelomeningocele. Syringomyelia is suspected if delayed deterioration in function occurs in a patient with occult spinal dysraphism. Syringes may not resolve with surgical intervention or may persist and recur in the setting of re-tethering. In these cases, stenting or shunting of the syrinx cavity to the subarachnoid space may result in clinical and radiographic improvement. Conclusion Congenital anomalies of the thoracic and thoracolumbar spine encompass a wide range of disorders related to errors in embryological development, resulting in bony deformity to intradural pathology. Prompt recognition, thoughtful management, and long-term follow-up are all necessary for successful treatment of this patient population. Magnetic resonance imaging in the evaluation of spinal cord injury without radiographic abnormality in children. Traumatic paraplegia in children without contiguous spinal fracture or dislocation. The anterior spinal artery: the main arterial supply of the human spinal cord-a preliminary anatomic study. Safety of spinal angiography: complication rate analysis in 302 diagnostic angiograms. Preoperative spinal artery localization and its relationship to postoperative neurologic complications. Preoperative selective intercostal angiography in patients undergoing thoracoabdominal aneurysm repair. Secondary neurulation: Fate-mapping and gene manipulation of the neural tube in tail bud. Secondary neurulation of human embryos: morphological changes and the expression of neuronal antigens. Enumeration and interrelationships in staged human embryos, and implications for neural tube defects. Ossification of the vertebral column in human foetuses: histological and computed tomography studies. Progressive congenital kyphosis: report of five cases and review of the literature. A review of 94 patients age 5 years or older, with 2 years or more follow-up in 77 patients. Its natural history and treatment as observed in a study of one hundred and thirty patients. The classic: a case of absence of cervical vertebrae with the thoracic cage rising to the base of the cranium (cervical thoracic cage). Incidence of neural tube defects in the least-developed area of India: a population-based study. Infected lumbar dermoid cyst mimicking intramedullary spinal cord tumor: Observations and outcomes. Urodynamic findings in the tethered spinal cord syndrome: does surgical release improve bladder function Occult spinal dysraphism: clinical and urodynamic outcome after division of the filum terminale. Treatment of the occult tethered spinal cord for neuropathic bladder: results of sectioning the filum terminale. Intracranial neurenteric cyst with recurrence and extensive craniospinal dissemination. Spinal arachnoid cysts in the pediatric population: report of 31 cases and a review of the literature. Spinal intramedullary ependymal cysts: a case report and review of the literature.
Discount glucotrol xl 10 mg amex
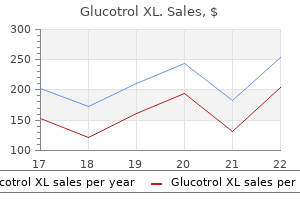
Fluoroscopy is still required diabetic ketoacidosis symptoms order glucotrol xl paypal, however, for the cement injection phase, when most radiation exposure is utilized. Once the patient is comfortably placed in the prone position, the fracture site is identified with fluoroscopy. Usual measures to ensure correct localization are taken, particularly in the thoracic spine. The pedicle of interest is marked on the skin, and local anesthetic is infiltrated along the planned track all the way to the periosteum. We have preferred the latter, aiming for a starting point slightly inferior and lateral to the pedicle, so as to enable a more centered position of the needle tip within the vertebral body. Perfect positioning of the cement is thus achieved with a unilateral injection; other surgeons, particularly if utilizing a transpedicular approach, may opt for a bilateral approach. The inferomedial quadrant of the pedicle should be avoided at all costs as it jeopardizes the exiting nerve root. Choice of Technique: Vertebroplasty Versus Kyphoplasty the fundamental principle of cement augmentation for thoracolumbar fractures is the same for both techniques. Restoration of height has been demonstrated on the order of 2 to 4 mm initially, losing 1 mm in the first year. Either a biplanar fluoroscopy (b) or navigation with O-arm (c) setup may be utilized. At this stage, additional local anesthetic can be injected through the needle if desired. Typically, immediately upon insertion, the needle tip touches the trans- verse process; it is then slowly moved caudally until it reaches the ideal insertion point. The needle is advanced into the vertebra, and biplanar fluoroscopy is utilized to ensure that the tip is advanced medial to the pedicle only after it is anterior to the posterior wall of the vertebral body. A parapedicular trajectory immediately lateral and inferior to the pedicle avoids the nerve root and enables the central positioning of cement. The Jamshidi trocar is removed, and a biopsy may be performed if neoplastic disease is suspected. We utilize a highly viscous polymethylmethacrylate cement preparation to minimize the risk of embolization or extravasation. Less complex setups may be utilized with syringes, but injection has to proceed at a slower pace to allow some settling of cement. The needle may be retracted a centimeter around the midpoint of cement injection, to enable a slightly posterior filling of the vertebral body. Kyphoplasty differs in that is has one additional step: Once the needles are positioned inside the vertebral body, the balloons are inserted and inflated gradually. The balloons are filled with contrast medium, so this process may be followed radiographically. A pressure gauge is attached to the system, and pressure during inflation should never exceed 220 psi. The injection was interrupted, and the patient did not have any clinical consequences. Cement in injected into the cavity via a cement-filled cannula and its plunger; each cannula contains ~ 1. The literature evidence overwhelmingly supports this surgical option for the treatment of neoplastic and refractory osteoporotic vertebral compression fractures. The patient is then examined to assess the symptomatology; an emergency laminectomy is performed with the patient under local anesthesia if there is any sign of neurologic compromise. We have not encountered either problem in our practice, but we include the phrase "possible emergency 744 V Lumbar and Lumbosacral Spine References 1. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. Twelve-months follow-up in forty-nine patients with acute/semiacute osteoporotic vertebral fractures treated conservatively or with percutaneous vertebroplasty: a clinical randomized study. Impact of sham-controlled vertebroplasty trials on referral patterns at two academic medical centers. Pre-existing fractures and bone mass predict vertebral fracture incidence in women. Prevalent vertebral deformities predict hip fractures and new vertebral deformities but not wrist fractures. Balloon kyphoplasty versus non-surgical fracture management for treatment of painful vertebral body compression fractures in patients with cancer: a multicentre, randomised controlled trial. Vertebroplasty and kyphoplasty for treatment of painful osteoporotic compression fractures. Effects of a new spinal orthosis on posture, trunk strength, and quality of life in women with postmenopausal osteoporosis: a randomized trial. Conservative management of patients with an osteoporotic vertebral fracture: a review of the literature. Meta-analysis of vertebral augmentation compared with conservative treatment for osteoporotic spinal fractures. Effectiveness of vertebroplasty using individual patient data from two randomised placebo controlled trials: meta-analysis. Vertebroplasty: about sense and nonsense of uncontrolled "controlled randomized prospective trials". Metastatic odontoid fracture management by anterior screw fixation and kyphoplasty. Direct anterolateral balloon kyphoplasty for a painful C-2 osteolytic malignant lesion. Percutaneous anterolateral balloon kyphoplasty for metastatic lytic lesions of the cervical spine. Percutaneous techniques in the treatment of spine tumors: what are the diagnostic and therapeutic indications and outcomes A randomized trial comparing 2 techniques of balloon kyphoplasty and curette use for obtaining vertebral body height restoration and angular-deformity correction in vertebral compression fractures due to osteoporosis. Intraoperative three-dimensional fluoroscopy-based computerized tomography guidance for percutaneous kyphoplasty. New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Balloon kyphoplasty for the treatment of acute vertebral compression fractures: 2-year results from a randomized trial. Effect of vertebroplasty on pain relief, quality of life, and the incidence of new vertebral fractures: a 12month randomized follow-up, controlled trial. This chapter discusses the classification, presentation, and management of lipomas arising from the conus. Lipomas of the conus medullaris have received the greatest amount of attention as they are the most common, making up as high as 86% of spinal lipomas,2 and are the most challenging to treat. Children with lumbosacral lipomas typically have normal neurologic function at birth and then gradually develop deficits over time. There remains considerable controversy as to the natural history of lumbosacral lipomas, which has resulted in disagreement on the management of asymptomatic patients. The caudal subtype, also known as the terminal lipoma, is joined to the caudal aspect of the conus and may enter into the central canal. These lipomas may replace the filum entirely or may be separated from the conus by a short thickened filum terminale. The dorsal type arises from the dorsal aspect of the lumbar spine, always sparing the distal conus. The lipoma extends from the neural placode through a dural defect to join extradural fat. Although the distal conus is not involved, it is often associated with a thickened or fatty filum terminale. However, unlike the dorsal variant, the transitional lipomas continue caudally to involve the conus.
Diseases
- Keratosis palmoplantar-periodontopathy
- Treft Sanborn Carey syndrome
- Subcortical laminar heterotopia
- Diethylstilbestrol antenatal infection
- Arrhinia
- Dentin dysplasia sclerotic bones
Order glucotrol xl 10mg with amex
Echo-rich areas with typical postacoustic shadowing are seen within the common bile duct diabetes medications in the pipeline cheap glucotrol xl 10mg without a prescription. Ultimately, the choice of modality should be based on clinical suspicion, availability of resources, experience, and cost. The appearance is that of a hyperechoic structure within the gallbladder, sometimes associated with an acoustic shadow. In approximately 20% of patients with acute pancreatitis, the cause is not established by history, physical examination, routine laboratory testing, or abdominal imaging. Recent studies suggest that microlithiasis may account for an unexplained attack of acute pancreatitis in as many as 75% of patients with a gallbladder in situ. Sphincter of Oddi dysfunction is most prevalent in patients with recurrent attacks who have previously undergone cholecystectomy. A, the crystals appear as floating hyperechoic foci that move when abdominal pressure is applied to the right upper quadrant and as layering material representing sludge. Cholangiography Cholangiography can be performed either invasively or noninvasively. Multifaceted cholesterol stones are retrieved at endoscopic retrograde cholangiopancreatography. Hemorrhagic cholecystitis is a form of acute cholecystitis often seen in the absence of gallstones. Hemorrhage is identified by the characteristic appearance of hemoglobin breakdown products within the wall or lumen of the gallbladder. Percutaneous Transhepatic Cholangiography ducts, anticipated need for therapeutic maneuvers (stone removal and stenting), or hypersensitivity to contrast agents and if percutaneous routes have failed. Intraductal shock wave lithotripsy offers a therapeutic option that may be effective despite the difficulties of a large, impacted stone that cannot be captured by a basket or a stricture that prohibits delivery of a stone beyond it. The overall risk of the procedure in patients with suspected gallstones is 2% to 7% for diagnostic Box 39. Gallstone Treatments Indications for cholecystectomy (open or laparoscopic) Symptomatic cholelithiasis (with or without complications) Asymptomatic cholelithiasis in patients who are at increased risk for gallbladder carcinoma or gallstone complications Acalculous cholecystitis Gallbladder polyps >0. It is almost uniformly successful in patients with dilated ducts and in 75% to 95% of those with nondilated ducts. The overall risk, including death, sepsis, bile leaks, and intraperitoneal bleeding, is 3% to 8%. Condition Intravenous ceftriaxone therapy Mimics of Biliary Colic Comments May lead to formation of crystalline biliary precipitates of drug Ceftriaxone crystals can induce all potential complications of small bile duct stones, including biliary colic and pancreatitis Manifests as syndrome of pain, fever, and cholestatic hepatitis, mimicking acute cholecystitis Eliciting antibiotic history during evaluation of symptoms is important Consistent history and associated eosinophilia may help identify syndrome Weil syndrome (characterized by fever, jaundice, azotemia, and right upper quadrant pain) mimics acute bacterial cholangitis Clues to diagnosis include history of exposure risk, myalgias, ocular pain, photophobia, azotemia, and abnormal urinalysis findings same hospital admission if possible and no later than 2 to 4 weeks after discharge for patients with a gallbladder in situ. Krawczyk M, Lutjohann D, Schirin-Sokhan R, Villarroel L, Nervi F, Pimentel F, et al. Risks include death, pancreatitis, infection, sedation or cardiovascular events, hemorrhage, and perforation. Although data are lacking to support the practice of endoscopic sphincterotomy in the absence of choledocholithiasis at the time of the procedure, the practice is a reasonable therapeutic option. The normal amylase is spurious and artificially suppressed by the hypertriglyceridemia, which is the likely cause of pancreatitis c. The normal amylase and elevated lipase levels reflect the earlier return of total amylase values to the reference range, which accommodates amylase from multiple sources. The patient in the previous question has elevated liver enzyme levels and a history of hepatitis A several years ago. Her liver test results were normal on a general blood chemistry panel during an annual physical examination in the past year. Abdominal ultrasonography now shows only modest sludge in the gallbladder and bowel gas obscuring the pancreas. The elevated transaminases most likely represent steatohepatitis related to her hypertriglyceridemia b. The transaminase elevations, if new, reflect acute bile duct obstruction and are highly specific for a biliary cause of pancreatitis c. The absence of stones in the gallbladder makes a biliary source of pancreatitis unlikely d. A 59-year-old male attorney is admitted through the emergency department with severe abdominal pain, nausea, and vomiting. The patient in the previous question is admitted to a general ward for initial management of his pancreatitis. Analgesia (fentanyl 50 mcg hourly) and hydration (normal saline 175 mL hourly) should be continued aggressively over the first 24 hours. The patient should receive nothing by mouth for now, and the route and rate of nutritional supplementation should be further considered after 3 to 4 days, when the duration of his course becomes clearer d. Parenteral antibiotics are not indicated in acute pancreatitis, but oral selective bowel decontamination should be considered if the course will be prolonged. On day 3, the condition of the patient in the previous question deteriorates, and he has increasing respiratory difficulty, a low-grade fever, a pulse of 110 beats per minute, and a blood pressure of 92/60 mm Hg. The serum level of IgG4 is normal, and he has no evidence of involvement of any other organ. A 20-year-old woman has had bouts of pancreatitis twice a year for the past 5 years. She has a strong family history of pancreatitis; her older brother, father, and paternal grandfather also have had pancreatitis. Mutation in which of these genes would be the most likely cause of her chronic pancreatitis He smokes 1 pack of cigarettes daily and drinks 2 or 3 glasses of wine on weekends. Pancreas and Biliary Tree side branches of the pancreatic duct, and small shadowing calculi in the main pancreatic duct. Which of the following features definitively confirms diagnosis of chronic pancreatitis in this patient A 32-year-old diabetic woman (22 weeks pregnant) has had 4 episodes of biliary colic over the preceding month and now presents with sustained right upper quadrant abdominal pain, fever, and leukocytosis. An 18-year-old patient who has cystic fibrosis and had recent total parenteral nutrition has frequent epigastric discomfort. Transabdominal ultrasonography shows multiple, mobile 4to 5-mm filling defects in the common bile duct. A 40-year-old alcoholic man received a diagnosis of chronic calcific pancreatitis 5 years ago. He continues to have bouts of pancreatitis that require hospitalization for 7 to 10 days. Between episodes, he has postprandial discomfort that is often disabling for a few hours. The patient should be managed conservatively since he will soon develop a painless "burnout" of chronic pancreatitis b. Longitudinal pancreaticojejunostomy will provide lasting relief from pain and pancreatitis c. A 65-year-old woman with an unremarkable medical history complains of vague, infrequent right upper quadrant discomfort. Transabdominal ultrasonography shows a 19-mm, fixed, hyperechoic lesion protruding into the lumen of the gallbladder without an acoustic shadow. In acute pancreatitis, elevated serum amylase values decrease to the reference range much faster than serum lipase values, because total serum amylase includes amylase contributed by multiple sources. Lipase is more specific to the pancreas; hence, lipase levels reflect pancreatic pathology with greater sensitivity. The other answer choices are incorrect for the following reasons: the elevated lipase level makes the diagnosis in the appropriate clinical setting. Spuriously low amylase levels are seen with much higher triglyceride levels, and only levels above 1,000 U/L are reliably incriminated as the cause of acute pancreatitis. Macroamylasemia causes spurious elevations in amylase levels without underlying pancreatitis. Four weeks previously, a 24-year-old man had his first episode of uncomplicated acute pancreatitis due to an alcohol binge and required a 3-day hospital stay. The other answer choices are incorrect for the following reasons: A patient with steatohepatitis would be expected to have long-term enzyme abnormalities without pain. Biliary sludge is a marker for stone-forming physiology and can cause biliary pancreatitis on occasion.
Generic glucotrol xl 10mg on line
Minimally invasive facet screws avoid the morbidity of an extensive exposure while offering an attractive adjunct to interbody fusion techniques of the lumbosacral spine diabetes test kit case discount glucotrol xl 10mg free shipping. However, those who are opposed to or do not qualify for general anesthesia may have conscious sedation with a controlled dose of fentanyl and midazolam during the procedure. A single intraoperative dose of either cefazolin or clindamycin is given 1 hour before incision. Once anesthesia has been induced, the patient is placed in the prone position on a padded radiolucent table. The bony imaging must be reviewed preoperatively to plan the screw trajectory and verify the feasibility of fixation across the center of the zygapophyseal joint via a percutaneous approach. The lateral view is used to ensure that the trajectory passes through the facet joint and into the pedicle of the inferior lever. The usual trajectory results in about 15 degrees of lateral angulation relative to the spinous process in the axial plane and about 30 degrees of angulation relative to the intervertebral disk in the sagittal plane. A Jamshidi needle is then advanced to engage the superior level of fixation at the defined entry points cited above. A mallet is then used to advance a Kirschner wire (K-wire) across the facet and into the inferolateral aspect of the pedicle of the inferior level of fixation. Percutaneous Translaminar Facet Screw the translaminar transfacet technique by was first described Magerl3 and has been modified to accommodate minimally invasive placement. The ipsilateral facet screw with the tip in the junction of the pedicle and vertebral body (b). The initial technique required special equipment that was not readily available, and therefore the technique was not universally adopted. Minimally invasive placement of translaminar screws using intraoperative imaging and readily available equipment has since been described by several authors (Table 108. A defining characteristic of translaminar facet screws is the ability to be placed at more rostral levels, higher than L3-L4, where an ipsilateral facet screw trajectory is obstructed by the spinous process. However, there is also greater risk of breaching the canal and subsequent neural injury. As with any procedure, the imaging must be critically studied preoperatively to ensure that placement of percutaneous tranlaminar facet screws is possible. Once the patient is positioned, the area is prepped and draped in the standard fashion. This line is continued to the skin, and the distance from the midline is then measured and marked in the operating room. The point where this line intersects the previously marked line denoting the axial plane is the site of the skin incision. A small opening is made in the fascia with Bovie cautery, and the Jamshidi needle is introduced. A K-wire is then intro- duced and advanced under fluoroscopy through the lamina, facet joint, and finally to the superolateral quadrant of the opposite pedicle. The K-wire is removed, and the same procedure can then be repeated for the opposite side. Potential Complications and Precautions As with all minimally invasive techniques, a limited exposure reduces the potential for related problems such as infection and wound breakdown. Injury to neural structures typically occurs while passing the K-wire, with inadvertent violation of the spinal canal or foramina. Also, the surgeon must ensure that the wire does not pass anterior to the spine, thereby preventing injury to vascular or visceral structures. This can be avoided by advancing slowly and repeatedly verifying the K-wire position. If the posterior elements are compromised, a percutaneous pedicle screw may be placed or the surgeon may prefer to convert to an open procedure if there is concern about neural compression. This distance is then used in the operating room to draw a paramedian line that will intersect with the line of the caudal trajectory and therein mark the site of incision. Lumbosacral fusion using the Boucher technique in combination with a posterolateral bone graft. Clinical efficacy of lumbar and lumbosacral fusion using the Boucher facet screw fixation technique. Transfacet screws with lumbar interbody reconstruction: biomechanical study of motion segment stiffness. Mini-open or percutaneous bilateral lumbar transfacet pedicle screw fixation: a technical note. Minimally invasive lumbar transfacet screw fixation in the lateral decubitus position after extreme lateral interbody fusion: a technique and feasibility study. Clinical analysis of percutaneous facet screw fixation after anterior lumbar interbody fusion. Fluoroscopically assisted percutaneous translaminar facet screw fixation following anterior lumbar interbody fusion: technical report. Efficacy of translaminar facet screw fixation in circumferential interbody fusions as compared to pedicle screw fixation. An anatomic and radiographic study of lumbar facets relevant to percutaneous transfacet fixation. Conclusion Facet fixation is a well-described technique with over 50 years of use. Now with minimally invasive techniques, percutaneous facet screws can be placed fluoroscopically with minimal exposure and relative ease. Multiple biomechanical and clinical studies have demonstrated that percutaneous facet screws are a suitable alternative to pedicle fixation as an adjunct to interbody fusion. By understanding the indications, goals, relative anatomy, and potential complications, the surgeon can ensure that this is a safe and effective intervention for patients. Stabilization of the lower thoracic and lumbar spine with external skeletal fixation. A biomechanical comparison of facet screw fixation and pedicle screw fixation: effects of short-term and long-term repetitive cycling. Tobler the transsacral (or presacral) approach is a minimally invasive surgical technique to achieve lumbar interbody fusion at L5-S1, or both L4-L5 and L5-S1. Access to the L5-S1 disk is achieved by crossing through the space anterior to the sacrum. The transsacral approach is distinct from any other interbody surgical fusions in its approach, instrumentation, and biomechanics of fixation. Benefits offered by the transsacral approach are most notable for minimizing injury to muscular, neural, ligamentous, and vascular structures. Anterior or posterior approaches entail more technical challenges in trying to expose the spine through deeper layers of soft tissues in obesity. Specifically, access is safe; the distance from the tip of the coccyx/entry point to the L5-S1 disk space does not adversely increase and the typically large presacral fat pad displaces the rectum away from the sacrum. Advantages Compared with other lumbar fusions at L5-S1, the presacral technique is unique in its approach, mechanism of discectomy, biomechanics, and suitability in cases of obesity. First, the anatomic corridor provides access to the spine previously not used for other interbody fusions. The presacral approach requires neither patient repositioning nor the assistance of an access surgeon. Second, interspace preparation uses looped/flat cutters to remove the disk, without direct visualization of the interbody space by the surgeon. Specifically, patients with a spondylolisthesis and high pelvic incidence face a high risk of construct failure because of the strong shear-force vector acting against the fixation of spinal fusion. Most interbody devices are wedged into the disc space and do not provide resistance against such forces. However, careful technique and evaluation of the anatomy of the rectum before and after the approach have reduced the risk of unrecognized bowel perforation to very low rates.
Discount glucotrol xl 10mg line
If no omovertebral bone is detected on X-rays reverse diabetes symptoms dr quillin best 10 mg glucotrol xl, then an ultrasound exam may be useful for detecting a fibrous or cartilaginous structure. What is known is that these deformities can be severe and of such a magnitude as to require operative treatment. Theiss et al,22 in their series of 120 patients with Klippel-Feil syndrome of whom 65 had scoliosis, found that no particular fusion pattern put the patient at risk for neurologic symptoms, and that neither the number of vertebrae fused nor the levels fused were predictive of symptomatology. Clinically, the most relevant of these deformities for the present discussion is cervicothoracic scoliosis. The curve may have a congenital component or it may be a compensatory curve above another curve. Outwardly, this deformity may be manifested by uneven shoulder heights, rotation of the upper thorax, and torticollis. Ideally, these deformities should be addressed early because cosmetic improvement is often a challenge. Bracing has been shown to be ineffective in controlling congenital spinal deformities, especially in the cervicothoracic region, and spinal arthrodesis is often the only option. The cardiopulmonary tree is a common site for anomalous development, with reports of pulmonary aplasia and hypoplasia and pulmonary stenosis. Signs of heart failure can include cyanosis, dyspnea, short stature, and fingernail clubbing. A baseline electrocardiogram is warranted for all patients with a known fusion in the cervical spine, and an echocardiogram if surgical intervention is planned. Genitourinary Defects the prevalence of genitourinary defects in patients with KlippelFeil syndrome has ranged from 2 to 64%. The second most commonly seen anomaly is malrotation of a normally functioning kidney. Renal pelvic and ureteral duplication occurs 25 times more frequently in these patients than in the general population. Pelvic renal ectopia is usually unilateral and involves a normally functioning kidney. Renal dysgenesis occurs 40 times more often in patients with Klippel-Feil syndrome than in the general population and may predispose these patients to uremia. All patients with Klippel-Feil syndrome should have an ultrasound evaluation of the renal system. An intravenous pyelogram need only be done if abnormalities are found on the sonogram or if the study is inconclusive. Sagittal Plane Deformities of the Cervical Spine Congenital osseous anomalies of the cervical spine can also create lordosis and kyphosis in the sagittal plane. Iniencephaly is characterized by a short immobile neck with a hyperextension deformity of the head. For curves less than 50 degrees, posterior spinal arthrodesis in situ is usually sufficient, and the potential exists for continued correction with growth if anterior growth centers exist. Larger deformities are best treated with combined anterior and posterior arthrodesis. Other Congenital Musculoskeletal Anomalies Other congenital musculoskeletal anomalies have been described, but with less frequency. Cardiopulmonary Defects Congenital anomalies of the cardiovascular system are said to occur in 4. If there is a question about whether two levels are fused, the flexion and extension views will demonstrate a change in the distance between the spinous processes. Standing posteroanterior and lateral radiographs of the thoracolumbosacral spine should be done to determine the presence of any other congenital spinal deformity. The vertebrae may assume a wasp-waist appearance, with the anterior and posterior cortices concave toward the center of the vertebral body. The neural foramina should be inspected for osteophytes, which may be present in older individuals with degenerative changes. However, in young children, careful attention should be paid to the laminae and posterior elements because these areas may ossify before the intervertebral spaces. Magnetic Resonance Imaging It is important to remember that any congenital spine deformity can be associated with a high incidence of spinal dysraphism, ranging from a tethered cord to a Chiari malformation with associated syringomyelia. For this reason, the spinal axis (spinal cord and brainstem) needs to be evaluated in all patients with a congenital spine deformity. Intraspinal lesions such as syringomyelia, meningioma, and lipoma are clearly identified. In the series of Guille et al,8 degenerative changes of the disks were seen in all of the patients, as demonstrated by a low-intensity signal on the T2-weighted images. Four cord abnormalities were seen in three patients: one hydromyelia, one Arnold-Chiari I malformation, and two diplomyelia. Ten of the 24 patients (42%) had cervical spondylosis, most commonly seen in the lower cervical spine, or disk herniation. Five patients had cervical cord dysraphism or diastematomyelia and two patients had an Arnold-Chiari type I malformation. Evaluation of Stenosis and Instability Different authors have used different criteria to evaluate spinal canal stenosis and vertebral instability. These measurements are notoriously difficult to make secondary to the congenitally dysplastic vertebrae and, unfortunately, assumptions or extrapolations are often made. The sagittal diameter of the canal is measured on the neutral lateral view, from the midpoint of the posterior aspect of the vertebral body to the nearest point on the line representing the junction of the laminae and spinous process. Normal values vary according to the age of the patient, vertebral level, and target distance. The Torg-Pavlov ratio, which is the ratio of the spinal canal to the vertebral body, is another method to evaluate spinal stenosis. Torg et al37 noted an association between neuropraxia of the cervical spinal cord in football players with congenital fusion and a decreased anteroposterior diameter of the bony canal. They recommend that players with stenosis and a congenital anomaly should be treated and counseled on an individual basis because no guidelines have been established for this subset of patients. Spinal Stenosis and Instability Spinal stenosis and instability of the cervical spine in individuals with Klippel-Feil syndrome is a debated issue. First, it must be determined if the stenosis is congenital and part of the syndrome or secondary to degenerative changes. Some authors believe that primary spinal stenosis in this patient population is uncommon, and some authors have even found the canal to be enlarged. They also found evidence of vertebral subluxation > 5 mm on the radiographs in five of their 20 patients. What is known is that coexisting spinal stenosis and vertebral subluxation are an unfortunate combination. Note that the disk is approaching the cord, but there is no bony stenosis of the cervical canal. Anterior or posterior translation of one vertebral body relative to another of greater than 5 mm may signify instability, especially if associated with neurologic findings. Flexion and extension of the cervical spine may exacerbate this relationship between the vertebrae. The combination of radiographic findings and neurologic signs makes the diagnosis easier to make. It is difficult to determine what to do with an individual with radiographic findings alone. Prediction of future neurologic risk based on positive radiographic findings in an asymptomatic patient is important, yet difficult to perform. Neurologic Problems No specific symptoms can be attributed directly to congenital fusions in the cervical spine. Patients may have nonspecific complaints such as headaches, syncope, weakness, and numbness. Radiculopathies are usually the result of nerve root irritation or impingement from osteophytes at the hypermobile segments adjacent to the fused vertebrae.
Syndromes
- Commonly has imaginary playmates
- Waking up early in the morning
- General feeling of being ill
- Stiff neck or severe weakness
- Mild microcephaly
- Bleeding
- Ulcers
- Blood clots
Discount glucotrol xl 10mg amex
Further supple mentation using intravenous or oral medication may be required to prevent worsening withdrawal symptoms diabetic herbs buy 10 mg glucotrol xl visa. Subcutaneous Fluid and Seroma Fluid may collect within the abdominal pocket or under the lum bar incision. In cases in which the effusion persists despite these measures, infection or a problem with the catheter should be suspected. X-rays of the thoracolumbar spine and abdomen may show evidence of catheter disconnection, fracture, or puncture. Catheter Tip Granuloma the incidence of a granulomatous inflammatory mass develop ing at the catheter tip is approximately 3%, and occurs most often in patients receiving intrathecal opioid therapy. The gran uloma can cause catheter occlusion that can lead to decreased therapeutic effect or even withdrawal symptoms, or the mass may cause cord compression, resulting in neurologic deficits. With discontinuation of the intrathe cal infusion, the granuloma may resolve over the next several months. Drug Overdose A malfunctioning pump or a transiently kinked catheter may deliver excessive medication, resulting in overdose symptoms (Table 117. Interrogation of the pump can confirm pump status and screen for any mechanical errors. The programmed dose may be decreased to minimum, and the cath eter port of the pump can be accessed to aspirate medication out of the catheter. Although some reversal is possible, supportive care including mechanical ventilation if necessary may be re quired to treat overdose. Prevalence of breakthrough cancer pain: a systematic review and a pooled analysis of published literature. A pump stall or fail ure can usually be identified through interrogation of the device. Compre hensive consensus based guidelines on intrathecal drug delivery systems in the treatment of pain caused by cancer pain. Polyanalgesic Consensus Conference 2012: recommendations for the management of pain by intrathecal (intraspi nal) drug delivery: report of an interdisciplinary expert panel. Prospective study of 3-year follow-up of low-dose intrathecal opioids in the management of chronic nonmalig nant pain. Polyanalgesic Consensus Conference- 2012: recommendations on trialing for intrathecal (intraspinal) drug delivery: report of an interdisciplinary expert panel. Intrathecal baclofen therapy in children with intractable spastic cerebral palsy: a cost-effectiveness analysis. Satisfaction of individuals treated longterm with continuous infusion of intrathecal baclofen by implanted pro grammable pump. Infectious complications of intrathe cal baclofen pump devices in a pediatric population. Polyanalgesic Consensus Conference- 2012: consensus on diagnosis, detection, and treatment of catheter-tip granulomas (inflammatory masses). Management of intrathecal catheter-tip inflammatory masses: an updated 2007 consensus state ment from an expert panel. Natural History, Nonoperative Management and Patient Selection Percutaneous cement augmentation was originally described for the treatment of symptomatic vertebral body hemangioma; this indication accounts for a minority of cases treated today. Black et al16 determined that the presence of kyphosis from pre- 738 vious fractures is independently associated with a fivefold increase in the risk of developing new fractures. Osseous metastases are a common complication associated with many types of solid tumors, occurring in 30 to 95% of patients with breast, prostate, lung, bladder, and thyroid cancers. Different forms of radiation therapy may also contribute to cause osteonecrosis, further weakening the bone matrix. Traditional conservative treatment includes analgesia and bed rest; however, these measures accelerate bone loss and increase the risk of developing deep venous thrombosis and pulmonary complications, with important negative impact on the patient. It should be sufficiently lightweight to ensure patient compliance, should be easy to wear and remove, and should prevent respiratory impairment. Except for the study of Rousing et al,5 they are all thought to be wellcontrolled for confusion variables. The only routinely observed complication was occurrence of a new fracture, but that was divided evenly among treatment and nontreatment groups, with three studies favoring each. Catastrophic complications of cement augmentation were not seen, and only one neurological adverse event was observed among the more than 500 patients who received intervention in these trials-severe radiculopathy due to a cement leak that required a laminectomy. However, for those patients with continued pain, particularly if it results in continued hospital admissions for pain control, cement augmentation is a safe and effective option that produces durable results. Most studies were case series, but then the pivotal Cancer Patient Fracture Evaluation trial was published in 2011 by Berenson et al. As with most studies of cement augmentation, crossover to the intervention group was significant; at 1 year of follow-up, 80% of the patients still being followed who had been assigned to nonoperative treatment had crossed over. For an accurate assessment of risks, the combined data of the randomized trials is an excellent reference, showing one symptomatic extravasation in over 500 patients. Particular attention is directed to the integrity of the posterior wall of the vertebral body; although not an absolute contraindication, a more careful and slow cement injection may be required if the posterior wall is not intact. Finally, standing radiographs may be useful to assess alignment but these are frequently not feasible. The ability to interact with the patient and perform a neurologic exam also provides an invaluable form of "neuromonitoring" while avoiding issues related to positive-pressure ventilation. In the interest of minimizing radiation exposure to the surgeon and staff, utilization of navigation during the insertion phase of the procedure has been described. The irregular nature and large size of these lipomas can make it extremely difficult to define the anatomy, which inhibits safe resection. The name is derived from the variable nature of the anatomy and the indistinct relationship among the neural placode, roots, and lipoma. The neural tube is then open posteriorly and mesenchymal cells are able to enter the abnormal cleft. The mesodermal elements mature into fat that often connects the subcutaneous space to the distal spinal cord. Caudal lipomas, also referred to as terminal lipomas, are a result of an error in secondary rather than primary neurulation. Therefore, the lumbar and upper sacral nerve roots in addition to the dura and dorsal structures that are formed during primary neurulation are never affected. Often these lesions are found to have disorganized neural elements that suggest that they are due to incomplete or failed apoptosis. The lipoma may result in deviation or asymmetry of the upper portion of the gluteal crease; if the mass is subtle, an asymmetric crease may be the only external finding. However, as impairment progresses, the child may develop repeated urinary tract infections, incomplete voiding, or complete incontinence. Although the majority of patients with a midline lipoma are intact at birth, those patients with an asymmetric mass have a greater risk of neurologic impairment in the lower extremity ipsilateral to the lesion. Patients who have clinical findings typically show progressive asymmetric weakness with patchy sensory loss in the lower extremities. Clubfoot, with equinovarus and clawing of the toes, was the most common deformity. Multiple authors have reported arrested progression and even reversal of scoliosis after untethering. The patient may complain of low back pain and asymmetric pain in the legs that changes with time; occasionally, a Lhermitte sign is seen.
Cheap glucotrol xl 10 mg otc
If the implants or autografts are placed as struts at the open side managing diabetes diastolic heart failure afib buy glucotrol xl 10mg amex, the placement at every other lamina. Can be easily combined with foraminotomy the newly formed spinal canal is structurally stable compared with double open-door laminoplasty. Reclosure of the elevated laminae can occur if some kind of materials are not placed. Double Open-Door Laminoplasty After standard exposure of the laminae and medial aspects of the facet joints, the spinous processes from C4 to C7 (C6) are cut at the height of the C3 spinous process. A trough is made with a 2-mm diamond bur at the center of the spinous process until the inner cortex of the lamina is sufficiently thin. The division of the spinous processes at the midline is confirmed by the movement of the lamina given sufficient thinning. Bilateral troughs are subsequently made with a 3-mm diamond bur at the junction of the laminae and lateral mass. After the springiness of the halved lamina is confirmed to be equivalent between the right and left sides, the bisected lamia is opened bilaterally. Bone grafts made from resected spinous processes or ceramic spacers are inserted between the opened laminae and secured in place with nonabsorbable sutures. Other Modifications to Preserve the Muscles Attached to C2 and C7 the preservation of the muscles attached to C2 and C7 is reported to reduce postoperative axial pain and kyphotic deformity progression. Laminectomy of C3 and laminoplasty from C4 to C7: In cases of degenerative cervical spine, the C2 and C3 laminae often overlap. In such cases, partial resection of the semispinalis muscle attached to C2 is required to elevate the C3 lamina. Laminectomy of C3 combined with laminoplasty at lower levels has been reported to minimize the resection of the semispinalis muscle. Midline division of the laminae enables symmetrical expansion of the canal, though the clinical significance is unclear. Although the problems of axial neck pain and segmental motor palsy remain, several modified techniques are expected to reduce their incidences. Nevertheless, additional well-designed randomized controlled studies are required to confirm the superiority of laminoplasty over laminectomy, anterior cervical decompression and fusion, and laminectomy and fusion. Surgeons must choose the optimal procedure depending on the etiology of each case while keeping in mind the benefits and drawback of each. In cases in which the divided spinous processes are thin, the ceramic spacers can migrate with the resorption of the tip of the spinous process. Technical improvements and results of laminoplasty for compressive myelopathy in the cervical spine. A new method of stabilising the elevated laminae in open-door laminoplasty using an anchor system. Spinous process-splitting laminoplasty using hydroxyapatite spinous process spacer. Expansive laminoplasty with reattachment of spinous process and extensor musculature for cervical myelopathy. Expansive midline T-saw laminoplasty (modified spinous process-splitting) for the management of cervical myelopathy. Indication and clinical results of laminoplasty for cervical myelopathy caused by disc herniation with developmental canal stenosis. Expansive laminoplasty for cervical radiculomyelopathy due to soft disc herniation. Local kyphosis reduces surgical outcomes of expansive open-door laminoplasty for cervical spondylotic myelopathy. Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: Part 1: Clinical results and limitations of laminoplasty. Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: Part 2: Advantages of anterior decompression and fusion over laminoplasty. A new concept for making decisions regarding the surgical approach for cervical ossification of the posterior longitudinal ligament: the K-line. Cervical active range-of-motion exercises and isometric exercises are encouraged when pain is manageable. Axial neck pain is not specific to laminoplasty but common in cervical posterior surgery. The preservation of muscles attached to C2 or C7 may reduce the incidence and severity of this complication. Segmental motor palsy (commonly C5 and rarely C6 and C7) occurs in ~ 5% of laminoplasties. The effect of prophylactic foraminotomy at bilateral C4-C5 for reducing the incidence of C5 palsy has been reported in a retrospective comparative study, but its effectiveness is inconclusive. The use of miniplate fixation when severe instability of the elevated laminae occurs secures the construct and may minimize the incidence of subsequent neurologic complications. Conclusion Cervical laminoplasty is well indicated for multilevel spinal cord compression without kyphotic alignment and severe anterior compression of the cord. The major advantages of laminoplasty are that the procedure is not technically difficult, multiple seg- 18. A comparison of anterior cervical fusion, cervical laminectomy, and cervical laminoplasty for the surgical management of multiple level spondylotic radiculopathy. C5 palsy after decompression surgery for cervical myelopathy: review of the literature. A prospective randomized study of clinical outcomes in patients with cervical compressive myelopathy treated with open-door or French-door laminoplasty. Comparative effectiveness of opendoor laminoplasty versus French-door laminoplasty in cervical compressive myelopathy. Results of cervical laminoplasty and a comparison between single and double trap-door techniques. Comparison of enlargement of the spinal canal after cervical laminoplasty: open-door type and double-door type. C3-6 laminoplasty takes over C3-7 laminoplasty with significantly lower incidence of axial neck pain. Axial symptoms after cervical laminoplasty with C3 laminectomy compared with conventional C3-C7 laminoplasty: a modified laminoplasty preserving the semispinalis cervicis inserted into axis. Postoperative displacement of hydroxyapatite spacers implanted during double-door laminoplasty. Two-year clinical and radiological outcomes of open-door cervical laminoplasty with prophylactic bilateral C4-C5 foraminotomy in a prospective study. Smith the traumatic process of the inferior facet of the superior ver tebrae moving anterior to the superior facet of the inferior vertebrae has been referred to as a dislocated, perched, jumped, or locked facet. Bilateral facet dis locations occur when hyperflexion forces extend anteriorly, whereas unilateral facet dislocations often include an addi tional rotational force around one of the facet joints during flexion. Anterior displacement of the more cranial vertebral body exceeding 50% of the anteroposterior diameter of the cau dal vertebral body usually results in bilateral facet dislocations.
Cheap glucotrol xl 10mg overnight delivery
After this does diabetes in dogs cause blindness generic glucotrol xl 10 mg without prescription, curettes are used to osteotomize the vertebral body medially, laterally, cranially, and caudally. The cortical shell of the vertebral body is left intact to protect neural elements and epidural vessels. Temporary fixation should be achieved with a temporary rod before a substantial portion of the body is removed, to prevent neurologic injury due to sudden translation of the spine. After decancellation has been completed in the posterior aspect of the vertebra extending from lateral wall to lateral wall, the posterior vertebral body wall is then "green-sticked" with a reverse-angle curette, pushing the bone anteriorly into the body. The lateral wall is resected in a wedge shape using a Leksell rongeur working toward the anterior aspect of the spine. This will produce a symmetric closure of the osteotomy site, correcting the sagittal deformity. The anterior cortex must be maintained to prevent subluxation of the spine during closure. Separate rods secured to the fixation points proximal and distal to the osteotomy may be connected through dominoes. In this manner, "construct-to-construct" compression may be performed and this may reduce the likelihood of fixation failure. It is recommended to widely open the canal centrally at the osteotomy site to be able to inspect the dura for buckling and to probe the neural foramina with a Woodson elevator to ensure the absence of any neural compression. We prefer to use iliac screws to protect against S1 pedicle screw pullout or failure in long constructs extending above L2. This can be performed to address sagittal imbalance with a coexistent coronal deformity. More bone along the lateral wall of the vertebral body is resected on the side of the convexity compared with the amount of bone resected along the concavity. This not only enables the restoration of sagittal alignment but also helps to restore coronal alignment. Curves with a sharp angle might be best corrected by a resection of a single vertebral body, whereas curves that are broad and sweep- ing may require a resection of multiple vertebral bodies at the apex to minimize stretching of the neural elements. Once completed, the spinal column can be shortened and the combined sagittal and coronal deformity corrected via a combination of translation and compression. A metal cage, structural autograft, or allograft may be used to reconstruct the vertebral column after correction of the deformity to bridge the defect left by resection of the vertebral body. Because this procedure circumferentially disconnects the spinal column, obtaining a fusion at this level is paramount. Following positioning of the patient as described above appropriate posterior exposure of the spine is obtained. Complete exposure should be done to both transverse processes to facilitate the removal of the vertebral bodies. Complete removal of the posterior components (spinous processes, lamina, and facet joints) should be performed to the level of the segments that need to be removed, which is often the apex of the deformity. In the thoracic spine, one may elect to sacrifice one or both exiting nerve roots to provide increased exposure for the removal of the vertebral body. The remainder of the cancellous portion of the vertebra is completely removed to the end plates of the adjacent disks above and below. Once the rib is removed, a temporary rod is placed opposite the working side to stabilize the spine and protect the neural elements. This can be done later but should be performed before removing a substantial part of the vertebral body. We prefer placing a temporary rod after completing the osteotomy on the first side and before working from the contralateral side. A careful subperiosteal dissection of the soft tissue is performed along the lateral wall of the vertebral body using a small Cobb elevator, as mentioned earlier. The importance of remaining in the subperiosteal plane cannot be overemphasized, because if the segmentals vessels are injured, the bleeding can be massive. It can be controlled by electric cauterization or hemostatic agents such as Surgicel, Gelfoam, and cottonoid. The pedicles are identified bilaterally and are resected with a Leksell rongeur following by piecemeal resection of the vertebral body and the disks above and below without interfering with the posterior vertebral wall, which is kept intact until the end to protect the thecal sac. This can be performed using the decancellation technique or osteotomies, as mentioned earlier. Bone resection should be wedged in the sagittal plane and may be asymmetric or symmetric in the coronal plane to correct kyphosis and also the scoliosis component. The bone should be removed completely to ensure that anterior cortical breakage occurs. It is usually necessary to place an anterior structural cage within the defect before complete closure to avoid shortening the spine excessively. The temporary rods are replaced with definitive rods, and the correction is gradually achieved with a combination of cantilevering and compression to correct the deformity. Sometimes in a patient with an unexplained deficit with a large deformity correction, the correction may have to be reversed in the absence of any obvious cause. The use of thromboembolic stockings and sequential compression devices should be continued throughout the recovery period. Physical therapy, including ambulation training and mobilization, should be started as soon as possible. The use of nonsteroidal anti-inflammatory drugs is avoided early in the postoperative period. Potential Complications and Precautions Lumbar osteotomies are technically challenging procedures that require extensive training and experience and can be associated with significant complications. A thorough and multidisciplinary preoperative evaluation, careful surgical planning, sound judgment, meticulous operative techniques, and early postoperative mobilization can reduce the potential complications associated with lumbar osteotomies. Application and development of minimally invasive osteotomy techniques may reduce the risk of the complications associated with open deformity surgery. Rod fracture is not uncommon following three-column osteotomies and can be seen in up to 22. We prefer using vancomycin powder during open posterior spinal instrumentation to reduce the risk of wound infection, as has been shown recently in several studies. Muscle and fascia are closed tightly in separate layers, followed by the subcutaneous layer and stapling of the skin. Postoperative Care Patients can be extubated right after the surgery or the next day, depending on the intraoperative course, the hemodynamic status, and anesthesia concerns. Thorough immediate neurologic evaluation should be performed as soon as possible, and evidence of any new neurologic deficit should be appropriately investigated. New neurologic deficits can vary from nerve root palsy to dense spinal cord level paralysis. Surgical treatment of pathological loss of lumbar lordosis (flatback) in patients with normal sagittal vertical axis achieves similar clinical improvement as surgical treatment of elevated sagittal vertical axis: clinical article. Clinical and radiographic outcomes of thoracic and lumbar pedicle subtraction osteotomy for fixed sagittal imbalance. Polysegmental lumbar osteotomies and transpedicled fixation for correction of long-curved kyphotic deformities in ankylosing spondylitis. Complications and intercenter variability of three-column osteotomies for spinal deformity surgery: a retrospective review of 423 patients. Complications in adult spinal deformity surgery: an analysis of minimally invasive, hybrid, and open surgical techniques. Prospective multicenter assessment of risk factors for rod fracture following surgery for adult spinal deformity. Comparison of standard 2-rod constructs to multiple-rod constructs for fixation across 3-column spinal osteotomies. Neurologic complications of lumbar pedicle subtraction osteotomy: a 10-year assessment. Time to development, clinical and radiographic characteristics, and management of proximal junctional kyphosis following adult thoracolumbar instrumented fusion for spinal deformity.
Cheap 10mg glucotrol xl with mastercard
The filum terminale is cauterized above and below the tumor and divided diabetes type 1 gene therapy buy glucotrol xl from india, and the tumor is carefully rotated out of the canal. It is often not possible to achieve en-bloc resec- 72 Intradural Extramedullary Tumor Resection 465 a b c. The filum is differentiated from the surrounding cauda equina nerve roots by its white color and vascularity. For example, the tumor may lack sufficient internal integrity and fall apart with even gentle manipulation. The tumor may also be too large to tease out without putting unacceptable amounts of traction on overlying nerve roots. Functional roots may appear to course directly through the substance of the tumor. Safe resection can be impossible in these cases because the lack of supportive connective tissue matrix. Potential Complications and Precautions Most complications relate to the wound and thromboembolic events. Delayed pseudomeningoceles without skin drainage can be followed conservatively for many weeks in patients with no significant symptoms because they often spontaneously resolve. A small dural defect can usually be identified as the cause of the persistent leak and can be primarily repaired with suture and a small muscle graft. Postoperative Care If a watertight dural closure is achieved, a subarachnoid lumbar spinal drain is unnecessary. The patient is kept flat in bed for 48 with sequential compression devices and a Foley catheter. If a spinal drain has been placed, it is generally clamped and removed prior to mobilizing the patient. Timely diagnosis and early treatment in symptomatic patients utilizing contemporary neurosurgical techniques lead to favorable clinical outcomes for most patients. Spinal meningiomas in patients younger than 50 years of age: a 21-year experience. Midline ventral intradural schwannoma of the cervical spinal cord resected via anterior corpectomy with reconstruction: technical case report and review of the literature. Minimally invasive removal of thoracic and lumbar spinal tumors using a nonexpandable tubular retractor. McCormick Surgery represents the most effective treatment of benign wellcircumscribed tumors, which constitute the majority of intramedullary neoplasms. Patient Selection the predominant benefit of surgery for an intramedullary tumor is prophylactic. Preservation, rather than restoration, of neurologic function is the most likely outcome after successful surgical treatment. In fact, significant improvement of a severe or long-standing preoperative neurologic deficit rarely occurs after a technically successful surgical excision. Surgical morbidity is also greater in patients with more significant preoperative deficits. This creates a therapeutic irony in which the risk of surgery is actually lower in patients with minimal or no objective neurologic deficit. Thus, early clinical diagnosis and, if possible, definitive initial treatment are critical to successful clinical management of most intramedullary tumors. A therapeutic dilemma arises, however, in the asymptomatic patient in whom an incidental intramedullary spinal cord lesion has been discovered. A posterior column deficit is a common consequence of a dorsal median myelotomy; thus, some degree of morbidity often accompanies even the most successful surgical removal. Although some benign astrocytomas are well circumscribed and are suitable for gross total resection, most exhibit variable infiltration into the surrounding spinal cord. This is often reflected in a gradual transition zone between the tumor and spinal cord. Thus, whereas gross total resection may be achieved in some cases, the extent of removal is uncertain and poorly defined in most cases. Furthermore, more peripheral dissection beyond what is clearly tumor tissue risks loss of neurologic function from the resection of infiltrated, yet functionally viable, spinal cord parenchyma. Specifically, a correlation between the extent of resection and tumor control has not been definitively established. Diffusely infiltrative tumors without a definite mass are biopsied, whereas gross total resection may be possible in well-circumscribed examples. Choice of Operative Approach the vast majority of intramedullary tumors are accessed through a standard laminectomy and midline myelotomy through the posterior median septum with the patient in the prone position. Minimally invasive techniques for intramedullary tumor removal have been described but are currently limited because the morbidity of these procedures resection is related to the intramedullary tumor resection, not the initial spinal exposure. More recently, lateral and ventral approaches have been described in selected patients with more ventrally located intramedullary tumors. This interface can be assessed accurately only through an adequate myelotomy, which extends over the entire rostrocaudal extent of the tumor. Ependymomas are usually symmetrically located and exhibit uniform tumor enhancement, whereas astrocytomas are associated with a more variable appearance with respect to tumor margins and enhancement patterns. Hemangioblastomas usually appear as intensely enhancing eccentric masses or nodules. There is often diffuse spinal cord enlargement that may extend a considerable distance from the tumor. A Mayfield skull clamp is used for cervical and upper thoracic lesions above the T6 level. The acquired data, however, rarely influence the surgical technique or the surgical objective. A midline incision and subperiosteal bony dissection are made, and a standard laminectomy is performed. This should extend to at least one segment above and one segment below the solid tumor component. Delayed instability rarely occurs after laminectomy for intramedullary tumor removal in adults. Oxidized cellulose (Surgicel) is generously spread over the lateral gutters to prevent contamination of the operative field with blood. The dura mater is opened in the midline and tented laterally to the muscles with sutures. The arachnoid is opened separately, and the spinal cord is inspected for any surface abnormality. Occasionally, the overlying spinal cord may be thinned or even transparent secondary to a large or eccentrically located tumor or polar cyst. Ultrasonography is useful for tumor localization and for ensuring adequate bony exposure. Rarely, an exophytic component of a benign glial tumor may extend into the subarachnoid space through a nerve root entry zone. Malignant neoplasms may replace surface spinal cord tissue or fungate through the pia into the subarachnoid space. Most hemangioblastomas arise from the dorsal half of the spinal cord with a visible pial attachment. Exposure of most intramedullary glial neoplasms is through a dorsal midline myelotomy. Eccentrically located tumors that abut the pia may be exposed via an off-midline myelotomy that extends longitudinally from both ends of the visible tumor. The dorsal midline septum is identified as the midpoint between corresponding dorsal root entry zones.
Discount glucotrol xl uk
Gallbladder agenesis is rare diabetes in dogs hereditary 10mg glucotrol xl overnight delivery, is of no clinical significance, and is associated with choledocholithiasis and duodenal atresia. A wandering gallbladder has either a long mesentery or no firm attachment to the liver and is at risk for torsion. However, the clinical significance of radiographic osseous abnormalities was not described until 1939 by Chamberlain2 and subsequently by Carl List in 1941. It was List who pointed out that cranial skeletal traction could reduce longstanding cervical dislocation. However, for patients with irreducible lesions with ventral cervicomedullary compression, there was considerable morbidity and mortality associated with such treatment. Eosinophilic granuloma Fibrous dysplasia Chordoma Chondroma Chondrosarcoma Plasmacytoma Secondary Neoplastic 1. Aneurysmal bone cyst Plasmacytoma Chordoma Giant cell tumor Osteoblastoma Chondroma 1. A rapid neurologic progression occurs in rare instances and may be followed by 1 Abnormalities of the Craniovertebral Junction 5 Box 1. Traumatic atlantoaxial odontoideum dislocation; os bone associated Congenital abnormalities and malformations of the craniovertebral junction A. Often, an antecedent history of minor trauma triggers a pattern of symptoms and signs that may progress at a rapid pace (Box 1. To achieve this, maneuvers such as flexion, extension, traction, disimpaction, and reduction distraction are utilized. In regard to the direction of encroachment on neural structures, the lesion is either ventral to the cervicomedullary junction or dorsal and may be superior as well as lateral in location to the foramen magnum. Note the atlantoaxial dislocation, possible os odontoideum and the anterior atlantal arch sliding forward in extension. There is an atlantoaxial dislocation with bifid anterior and posterior arches to the atlas, as well as an os odontoideum. The anterior arch of C1 is not visible, and the odontoid process is well above a line joining the hard palate and the posterior rim of the foramen magnum. There is significant decompression of the pons and medulla as well as the hindbrain herniation. Radiographs should include a lateral view of the skull showing the spine, and the anterior open-mouth view and oblique views of the cervical spine. These studies can be done with the patient in the flexed and extended position to demonstrate the biomechanics. With all imaging techniques, dynamic studies are necessary to assess the stability and the osseous-angular relationships to the neural structures. There is a secondary basilar invagination (basilar impression) with a pontomedullary flexure of less than 90 degrees. The clivus and upper cervical articulation is acute in angulation, indenting the pontomedullary junction. The vertical height of the posterior fossa is reduced by an upward invagination of the squamous-occipital bone. Note the acquired hindbrain herniation with cerebellar tonsils at the C3 vertebral level. There is an invagination of the upper cervical spine and skull base into the cranium. However, there is a fixed atlantoaxial dislocation with an upward migration of the body of C2 indenting into the ventral cervicomedullary junction. Note the atlantoaxial dislocation with the absence of the anterior atlantal arch components. In individuals with atlas assimilation and basilar invagination, a rotary subluxation of the atlas on the axis vertebrae can result in vertebral artery distortion, and occlusions are common. Imaging to determine the position of these critical vessels and the possible distortion that may occur with position change should be done prior to surgical treatment. Treatment Strategy Neurodiagnostic imaging17 should be done to demonstrate the direction and mechanics of compression and associated abnormalities as well as to define the reducibility of the lesion. Ligamentous reducible pathology such as with inflammatory states or recent trauma should be given a trial of immobilization. A treatment algorithm for problems in this region was first published by the senior author in 1980 and was recently updated by Dlouhy and Menezes. This 13-year-old boy with Down syndrome underwent a dorsal atlantoaxial arthrodesis a year previously that failed. We have utilized screw-and-rod constructs as well as custom contoured threaded titanium loops for occipitocervical fixation with autologous rib graft for the osseous construct. A variety of skull base approaches have expanded from the basic anterior, lateral, and posterior routes to the foramen magnum. Irreducible dorsal or lateral encroachment is approached dorsally or laterally, respectively. In either circumstance, if instability is present, posterior instrumentation with fixation and fusion is often necessary. Basilar impression (platybasia): a bizarre developmental anomaly of the occipital bone and upper cervical spine with striking and misleading neurologic manifestations. Craniovertebral junction database analysis: incidence, classification, presentation, and treatment algorithms. Primary craniovertebral anomalies and the hindbrain herniation syndrome (Chiari I): data base analysis. All 19 patients were either untreated or managed conservatively in a cervical collar. These studies and others strongly suggest that, once cervical myelopathy is established in patients with rheumatoid cervical spine disease, the natural history without surgical intervention is grave, and mortality is more common than previously believed. Additionally, the incidence of cervical myelopathy and therefore mortality from myelopathy is likely underestimated in rheumatoid patients. Progressive pain, immobility, and weakness are often attributed to exacerbation of the systemic disease process rather than to neural compression. A history of corticosteroid use, seropositivity for rheumatoid factor, the finding of rheumatoid subcutaneous nodules, and the presence of mutilating peripheral articular disease are all predictive of greater progression of cervical instability and neurologic injury. In a metaanalysis of 1,749 patients in the published literature, Casey and Crockard4 found that 32% (range, 5. Over half of those affected in this analysis (17%) had neurologic symptoms or signs. Joints that ultimately develop severe destruction usually become symptomatic within the first year of disease onset. Additional neurologic involvement not referable to the cervical spine includes compression neuropathies such as carpal tunnel syndrome, diffuse sensorimotor neuropathies, and mononeuritis multiplex. These changes are due to the same host of inflammatory cells and mediators that causes destruction of the joints in the appendicular skeleton. Although the inciting cause of inflammation is unclear, the inflammatory process itself is well described. Lymphokines, secreted by mononuclear cells, stimulate antibody production and the release of additional degradative products. The influx of combined fluid and inflammatory mediators produces the pain, swelling, and erythema that characterize rheumatoid synovitis. Granulation tissue known as rheumatoid pannus then forms in the affected joint as a result of proliferating fibroblasts and inflammatory cells. The pannus produces collagenase and other proteolytic enzymes, resulting in damage to adjacent cartilage, tendons, and bone. The ensuing destruction leads to cartilage loss, bony erosions, cranial settling, tendon ruptures, and ligamentous laxity. Subsequent neurologic injury secondary to compression of the spinal cord, nerve roots, or vertebral arteries can result from direct impingement by the proliferating synovitic pannus or from repetitive bony compression due to vertebral subluxation and instability. As opposed to osteoarthritis, in the rheumatoid process, lesions from the joints of Luschka extend into the disk spaces and vertebral bodies without osteophytosis. Because there is a strong correlation between the severity of cervical disease and that of peripheral erosive disease, cervical subluxation is more likely in those patients with progressive peripheral periarticular erosions.