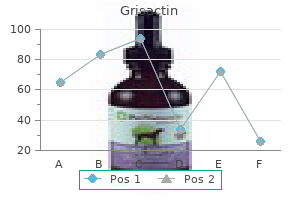
Generic grisactin 250 mg amex
A 53-year-old postmenopausal female with newly diagnosed atypical ductal hyperplasia presents to your office to discuss the role of chemoprevention medications via ng tube order grisactin pills in toronto. She asks you about the evidence available on the use of these agents for breast cancer prevention. She is very concerned and wants to do everything to reduce the risk of developing cancer. A 55-year-old female was found on screening mammogram to have suspicious microcalcifications in the right breast measuring approximately 1. Risk/benefit discussion of chemoprevention with either tamoxifen or an aromatase inhibitor 9. Which of the following statements regarding pleomorphic lobular carcinoma in situ is correct Pleomorphic lobular carcinoma in situ is, in most cases, hormone receptor negative. A 46-year-old healthy premenopausal female undergoes a screening mammogram and is found to have a cluster of microcalcifications in the right upper outer quadrant, for which biopsy is recommended. A 60-year-old woman who was diagnosed 9 years ago with ductal carcinoma in situ of the left breast, status postlumpectomy, radiation, and 5 years of tamoxifen relocated from a different state. Her physical exam is unremarkable, except for mild breast asymmetry and the presence of a surgical scar from her previous left lumpectomy. She brings her most recent mammogram done 2 days ago, which reveals a few small areas of microcalcifications at the lumpectomy site. Reassure the patient that her physical exam is unremarkable and that her mammogram is benign B. Ensure that previous mammograms are obtained in a timely fashion for proper comparison and definitive plan of care C. Obtain computerized tomography scans of the chest, abdomen, and pelvis, plus bone scan E. Recommend that she undergo a left breast mastectomy 92 Breast Cancer pain and discomfort after lumpectomy, requiring narcotics. She presents to you for a second opinion to discuss whether she needs additional treatment as her "margins were close. Re-excision in order to obtain more widely negative margins, followed by postlumpectomy whole breast radiation and consideration of subsequent endocrine therapy C. Postlumpectomy whole breast radiation and consideration of subsequent endocrine therapy E. A 37-year-old premenopausal African American woman presents with a lump in her right breast. Subsequent right breast ultrasound is unremarkable; however, there are several enlarged lymph nodes in the right axilla, with the largest measuring 3 cm. A biopsy performed under stereotactic guidance reveals proliferation of abnormal epithelial cells within the mammary ductal system. These cells are large, pleomorphic with frequent mitotic figures, and many of them had multiple prominent nucleoli. There is no evidence of invasion into the surrounding stroma on routine light microscopic examination. Right lumpectomy with right sentinel lymph node biopsy followed by postlumpectomy radiation B. Right lumpectomy without right sentinel lymph node biopsy followed by postlumpectomy radiation C. She presents to your office 4 weeks after mastectomy for postsurgical treatment planning and consideration of additional treatments. Pathology revealed ductal carcinoma in situ, cribiform pattern, intermediate to high nuclear grade, with associated necrosis, measuring approximately 2. A 60-year-old postmenopausal woman who is a current smoker presents for a second opinion after being unable to tolerate anastrozole, letrozole, or exemestane due to severe hot flashes and disabling join pains. Her medical history is significant for hypertension since the age of 50, requiring three antihypertensive agents, saddle pulmonary embolism 8 years ago, and major depression with a previous suicidal attempt at the age of 35. Estrogen and progesterone receptors were positive in greater than 90% of the cells. C the number of separate foci of atypical hyperplasia (with greater numbers of foci associated with a higher risk) and the extent of normal regression (involution) of background lobular units stratifies risk amongst women with atypical hyperplasia. Regarding answer A, women who have had a benign breast biopsy that demonstrates atypical hyperplasia are at a substantially increased risk for developing breast cancer-approximately 4 times that of the reference population. In terms of answer B, atypical hyperplasia is associated with a generalized increased risk of ipsilateral and contralateral breast cancer. Examples of proliferative lesions without atypia include moderate or florid ductal hyperplasia of the usual type, sclerosing adenosis, radial scar, and intraductal papilloma or papillomatosis. In both subsets, chemoprevention reduced the risk of developing breast cancer by more than 50%. While surveillance is an appropriate option, this patient expresses a desire to do everything she can to reduce her risk of developing breast cancer; thus answer C is the most appropriate recommendation for this patient. High-grade lesions are composed of solid nests of neoplastic cells without evidence of gland formation, and typically exhibit aneuploidy and lack estrogen and progesterone receptors (answer C). Margins less than 2 mm are associated with a higher risk of local recurrence (answer E). It is also used when a comparison with prior mammograms is needed for a definitive report. Since the nonspecific abnormalities could still represent invasive or noninvasive disease, the request for previous films and proper comparison should happen within a matter of days. It would be inappropriate to reassure patient and obtain the next mammogram in 6 or 12 months (answer A), or to go straight to biopsy (answer C). Systemic staging with imaging would be appropriate if the patient had a diagnosis of locally advanced invasive breast cancer (answer D). Similar to what is seen in invasive disease, lumpectomy as compared with mastectomy is associated with a higher risk of local recurrence, even when combined with radiation therapy. If the patient is treated with lumpectomy, it is most appropriate to postpone sentinel lymph node biopsy and only do it if invasive carcinoma is 8. Adjuvant chemotherapy is not indicated, since the risk of systemic recurrence is extremely low (answer D). However, a recent study evaluating outcomes of the 16,887 breast cancer survivors, in which 8099 used antidepressants, there was no statistically significant increased risk of subsequent recurrence in women who concurrently used paroxetine or fluoxetine and tamoxifen. Tamoxifen increases the risk of thromboembolic events, in particular in women older than 55 years old, smokers, overweight/ obese, hypertensive, and with family history of coronary artery disease. Right mastectomy would be potentially appropriate if the patient were interested in maximal risk reduction, even if this led to additional surgery. Unilateral mastectomy would decrease the risk of in-breast recurrence to approximately 2% (answer B). Neither unilateral nor bilateral mastectomy has been shown to impact Category 5 Highly suggestive of malignancy Known biopsy proven malignancy Category 6 seen. Endocrine therapy can be discussed after the definitive surgery (answers D and E). Therefore postmastectomy clinical follow-up typically includes history, physical examination, and routine mammogram. Aromatase inhibitor is not an appropriate treatment option for premenopausal patients (answer D). Adjuvant chemotherapy is not indicated, since the risk of systemic recurrence is extremely low (answer C). Screening breast magnetic resonance imaging in women with atypia or lobular carcinoma in situ. First International Consensus Conference on lesions of uncertain malignant potential in the breast (B3 lesions). The 2-mm margin minimizes the risk of ipsilateral breast tumor recurrence compared with smaller negative margins. More widely clear margins do not significantly decrease ipsilateral breast tumor recurrence compared with the 2-mm margins. Thus, in this case, next steps would include radiation and consideration of endocrine therapy for secondary chemoprevention. Subsequent breast cancer events included ipsilateral or contralateral in-situ or invasive breast cancers.
Crataegi Flos (Hawthorn). Grisactin.
- Dosing considerations for Hawthorn.
- Decreased heart function, blood circulation problems, heart disease, abnormal heartbeat rhythms (arrhythmias), high blood pressure, low blood pressure, high cholesterol, muscle spasms, anxiety, sedation, and other conditions.
- What other names is Hawthorn known by?
- Treating heart failure symptoms when a standard form (LI132 Faros or WS 1442 Crataegutt) is used.
- Are there safety concerns?
- How does Hawthorn work?
- Are there any interactions with medications?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96529
250mg grisactin amex
The ventricular function curves are shifted upward by positive inotropic interventions and downward by those impairing inotropic activity symptoms joint pain discount grisactin 250mg with amex. Afterload also may significantly influence the elevation or decline of the ventricular function curve. Both ventricular volume and pressure must be measured simultaneously to compute the compliance value. The slope of the compliance curve is called stiffness, which is the inverse of compliance. Compliance tends to decrease in chronic conditions involving myocardial hypertrophy, restrictive cardiomyopathy, or other infiltrative processes. Artifacts of pressure waveforms should be identified to avoid confusion with true pathophysiologic responses. Reversible cardiac failure during angina pectoris: Hemodynamic effects of atrial pacing in coronary artery disease. The spiral arrangement of the layers surrounding and forming the thicker muscular left ven tricle covered by the thinner right ventricle makes con traction a wiring out movement more than a simple inward movement. The result is that complex vortices are generated as the ventricular chamber shortens and thickens, ejecting their contents into the great vessels. Ventricular interaction coupled with septal contractile mechanisms plays a major role in the appearance of indi vidual ventricular pressure waveforms. Moreover, differ ences in compliance between the two ventricles and the timing of activation (conduction) produce interesting hemodynamic records which are reflections of the myo cardial diseases affecting one side more than the other. Rarely do cardiologists review simultaneous right and left ven tricular pressures during routine hemodynamic studies. As part of many training programs, a comparison of simultaneous right and left ventricular pressures during combined complete hemodynamic studies is routinely performed. The waveforms of constrictive and restrictive physiology are described elsewhere [7]. The characteristic configuration and significance of the diastolic ventricular pressure tracings in such patients will be reviewed here. Although fluidfilled systems provide clinically useful hemodynamic tracing, highfidelity micromanometer tipped catheters (or highfidelity pressure sensor guide wires) are needed to identify small pressure differences or quantitative contraction/relaxation. Right and Left Ventricular Pressures in a Patient with Hypertension A 65yearold man with hypertension had routine diag nostic study for dyspnea and atypical chest pain. Cardiac catheterization was performed from the femoral approach as described earlier [8]. Rightheart hemodynamics revealed a mean right atrial pressure of 8 mm Hg, right ventricular pressure of 65/12 mm Hg, mean pulmonary capillary wedge pressure of 20 mm Hg, and pulmonary artery pressure of 65/22 mm Hg. In assessing the ventricular pressures, examine four features: (i) the A waves; (ii) the rates of systolic pres sure rise; (iii) the position of the right ventricular pressure within the left ventricular tracing; and (iv) the rate of diastolic pressure decline and middiastolic upslope. Recall that these pressures were obtained immediately prior to left ventriculography, which demonstrated global hypokinesis and moderate mitral regurgitation. The left ventricular compliance is reflected by both the height of the A wave and the diastolic upslope. Note that both findings are lower in the right ventricle compared Hemodynamic Measurement Technique Simultaneous right and left ventricular pressures are eas ily measured during pullback of the balloontipped cath eter from the pulmonary artery to the right ventricle Hemodynamic Rounds: Interpretation of Cardiac Pathophysiology from Pressure Waveform Analysis, Fourth Edition. The left ventricular diastolic pressure has a steep upsloping diastolic filling period. The right ventricular pressure tracing is contained (that is, the upstroke and downstroke occur) equally spaced within the left ventricular pressure wave form. This normal pattern is seen with patients who have normal electrocardiographic conduction and generally normal biventricular function. Despite pulmonary hyper tension, the normal diastolic pressure upslope and dimin utive A wave suggest that right ventricular compliance is nearly normal. Note the shift of the right ventricular upstroke to the left earlier under the left ventricular pressure upstroke. The review of the A waves, diastolic upstroke, and rates of pressure rises reveals normal values with low right and left ventricular enddiastolic pressures. Wiggers over half a century ago using firstgeneration electromechanical pressure manometers [10]. Similar findings have been observed more recently with highfidelity micromanom etertipped transducers to identify the precise timing, force of contraction, and differences in contractile func tion between the two ventricles [9]. Right and left ventricular pressures were obtained during a routine catheterization. The electrocardiogram was normal, but the downstroke of the right ventricular pressure overlies that of the left ventricle on several beats (arrows). When the tip of the catheter is occluded by the septal wall, the pressure pattern falls directly with left ventricular pressure. The subsequent beats have a normal spacing of the right ventricle pres sure upstroke within the left ventricular pressure tracing and a normal spacing during early diastolic relaxation. These tracings are otherwise remarkable for findings of poor left ventricular compliance (large A wave, high minimum diastolic pressure and diastolic upstroke) and the strikingly low right ventricular filling pattern (negative overshoot in early diastole, small A wave, flat diastolic slope). Wiggers of simultaneous right and left ventricular pressures in a dog, showing the effect of a premature systole and subsequent temporary alternation on left and right ventricular pressure curves. Observe the precedence of left over right ventricular contraction in premature beat. Intermittent hypotension and Wenckebach arrhythmia were noted during the pro cedure. In the catheterization laboratory, mean right atrial pressure was 25 mm Hg and mean pulmonary cap illary wedge pressure was 22 mm Hg. An acute inferior myocar dial infarction with right ventricular involvement is responsible for elevation and near equilibration of dias tolic pressures, especially evident on beat #5. The com pliance of the ventricles is obscured by the constrictive/ restrictive diastolic dip and plateau patterns. When examining patients with abnormal right ventricular pressures, the concordance (matching) of diastolic waveforms should be placed in the clinical context. Low but matched dias tolic pressures may separate after rapid volume adminis tration, indicating normal function, whereas in restrictive myopathy, the diastolic pressure concordance may persist [5]. Beat #3 is a fusion beat with normalized 52 Left and Right Ventricular Pressure conduction (note the P and T waves). The right ventricu lar pressure on this beat is different, with the upstroke and downstroke occurring earlier inside the left ventri cular pressure. Pacemaker Pressure Responses Ventricular pacemaker activation and left bundle branch block may also produce unusual patterns of right and left ventricular pressure waves. The compliance of both ventricles was thought to be similar, with absent "a" waves (due to ven tricular pacing) and a normal diastolic upslope. A delayed rate of pressure rise and delayed relaxation of the right ventricular pressure waveform can be seen, with the later part of the right ventricular pressure (arrow) falling out side the left ventricular pressure curve. In addition, the slow upstroke reflects abnormal right ventricular systolic function. A delay of the right ventricular pressure rise could be caused by damping within the right ventricular catheter, but the resonant frequency of the pressure responses seems to be within the normal range (consider the sinusoidal variations dur ing the peak systolic and early diastolic periods). This unusual timing relationship of right and left ventricular pressures is a result of left bundle branch block and a pacemaker in a patient with ventricular dysfunction. The small right ventricular dP/dt peak precedes the onset of the rise of left ventricular dP/dt, which is delayed. A secondary rapid rise of right ventricular dP/dt occurs after the onset of left ventricular dP/dt and is followed by an unusually slow decline. This pattern reflects the contractile function and interaction between the ventricular chambers. Consider the hemodynamic tracings obtained in a 42yearold woman with mitral stenosis. Diastolic filling rates (slopes) differ between ventricles during long pauses (beat #3).
Buy grisactin canada
The reptilase time is useful in diagnosing a dysfibrinogenemia but is not helpful in monitoring patients on dabigatran medications used to treat migraines purchase grisactin pills in toronto. The dilute thrombin time is able to accurately predict therapeutic and subtherapeutic dabigatran serum concentrations over a wide range in a linear fashion. Other factors that decrease the risk for recurrence include female gender, absence of an underlying malignancy, and younger age. Heterozygosity for the prothrombin mutation does not appear to be a risk factor for recurrent thrombosis. As such, the patient should be managed with short-term anticoagulation with enoxaparin followed by warfarin. Warfarin alone would be unacceptable, as the duration to anticoagulation with warfarin is several days, and warfarin will deplete protein C before it exerts its full anticoagulant effect. Rivaroxaban has not been adequately studied in the primary prevention of thrombosis in patients with asymptomatic antiphospholipid antibodies. In pregnant women known to be homozygous for the factor V Leiden or prothrombin 20210 mutation with a family history of thrombosis, antepartum prophylaxis with postpartum prophylaxis or intermediate dose anticoagulation has been recommended (choices B and E). Treatment doses of anticoagulation antepartum and postpartum are generally not recommended in the absence of prior thrombosis (choice D). B the choice of a proper anticoagulant is very complex and depends on patient factors, patient preferences, as well as health care and social constraints. Warfarin use would be difficult with his poor diet and frequent antibiotic use (choice A). Thus in this patient who requests discharge as soon as possible, neither of these agents would be the best choice (choices C and D). In addition, dabigatran has significant renal clearance and therefore would again not be the best choice. Fondaparinux is an injectable agent and is also cleared renally, so would not be the best choice in this case (choice E). There is no indication for continuing with warfarin or transitioning to another anticoagulant. C In general, there is a very limited utility in performing thrombophilia evaluations, particularly in the in-patient and acute setting. However, there are particular instances where a deliberate evaluation for underlying thrombophilia may be useful. Specifically, in a patient with an abdominal vein thrombosis in the absence of other overt provocative events (surgery, injury, malignancy, etc. Patients with this mutation may have modest elevations in serum homocysteine levels. Metaanalyses show no correlation with thrombosis in United States patients where grains are supplemented with folate. Although B vitamin and folate supplementation may lower serum homocysteine levels, there is little evidence that such supplementation will lower the risk for thrombosis. C Classification criteria for the antiphospholipid antibody syndrome include both clinical and laboratory criteria. An underlying disorder can be identified in over 80% of the cases of Budd-Chiari syndrome. The women presented in this vignette had microcytosis in the setting of an elevated hemoglobin/ hematocrit, platelet count, and white count making previously undiagnosed polycythemia very likely. C the American College of Physicians has produced evidence-based guidelines for anticoagulation in many clinical situations, including for pregnant women with thrombophilia, but no prior thrombotic history. In pregnant women with a weak thrombophilic mutation, such as heterozygosity for the prothrombin gene mutation, and no prior or family history, only clinical surveillance is recommended (choice A). In pregnant women with no prior Coagulation thrombotic manifestations to precede the development of polycythemia or thrombocytosis. The other hypercoagulable states are much less frequently associated with the Budd-Chiari syndrome and can be falsely positive if the patient is on anticoagulation or has just had a recent thrombosis. A While the use of unfractionated heparin would be acceptable, concurrent administration with antiplatelet therapy is not indicated. Since the patient is without any objective finding of either hemodynamic compromise or severe limb dysfunction, the use of thrombolytics is not warranted. As for the placement of a filter, there is no contraindication to anticoagulation. A While it is unclear if this was truly a case of heparininduced thrombocytopenia, given the lack of reported thrombosis, only 4 weeks of anticoagulation is recommended, with 3 months in total if there was a thrombosis. As such, the patient has received more than an adequate course of anticoagulation. For this reason there is no indication to either continue or transition to a higher target/ range of warfarin, regardless of what type of valve he is to receive, especially as this will have to stopped prior to surgery. The use of any direct oral anticoagulant is contraindicated in patients with mechanical heart valves. Therefore the postoperative use of heparin or enoxaparin would not be recommended. E While the direct oral anticoagulants are characterized by the lack of need of monitoring their anticoagulant effect, nonetheless, all of these agents exert an effect on many tests of hemostasis. Even though a lupus anticoagulant is "present," (1) the presence of rivaroxaban confounds this diagnosis, and (2) the presence of an antiphospholipid antibody, 283 such as a lupus anticoagulant, must be present after 12 weeks. However, this would not account for the elevated protein C and S levels, and as noted previously, it is far more likely that an effect from rivaroxaban is being observed. A Among the many changes that occur in pregnancy, it is well established that protein S activity levels fall below normal by the first trimester, with the majority of pregnant patients having below normal levels by the third trimester. Thus there are no indications to provide any additional anticoagulation now or in the postpartum period. She had a line-associated superficial vein thrombosis that does not require further anticoagulation, either therapeutically or prophylactically. A this is the standard recommendation for postoperative thromboprophylaxis following a total knee replacement. The patient has a lupus anticoagulant, as there is (1) the prolongation of a phospholipid dependent clotting assay; (2) this is not overcome with mixing; (3) it shows phospholipid dependence; and (4) there is no specific factor inhibitor. As such, the empiric initiation of any treatment, be it an anticoagulant, antithrombotic, or antirheumatic therapy, is not indicated. C the abnormal thrombin time is indicative of either a thrombin inhibitor (such as heparin or dabigatran, not the oral Xa-inhibitors such as apixaban) or a disorder of fibrinogen. In the case of a patient with both thrombotic and hemorrhagic manifestations, the presence of a dysfibrinogenemia should be suspected. Reptilase is snake venom that is insensitive to the presence of heparin, and the reptilase time is abnormal in the setting of a dysfibrinogenemia. If the reptilase assay is abnormal, this is highly suggestive of a dysfibrinogenemia, following which a fibrinogen antigen:activity ratio should be obtained. Furthermore, there are no known F8 sequence changes that are associated with elevated levels. Performing a lupus anticoagulant evaluation, as well as clot-based protein C and S assays, are bound to be confounded by the presence of apixaban, and should not be performed. However, it is widely felt that there is no relation of this polymorphism to cardiovascular events, is not associated with venous thrombosis, and that supplementation with folate/B6 compounds does nothing to alter future events. Her thrombosis was distal and provoked, which provides no justification for prolonged anticoagulation. The patient does not have protein S or protein C deficiency; rather, she has low protein C and protein S activities, as expected on warfarin therapy. This highlights the fact that if thrombophilia testing is undertaken, clinicians must be aware of scenarios in which thrombophilia results may be inaccurate or misleading. At the same time, he is undergoing a colonoscopy, which has a low risk of bleeding. Until recently, most patients in this scenario were thought to benefit from bridging anticoagulation perioperatively by minimizing the risk of thromboembolism without increasing the risk of perioperative bleeding. However, this practice is not supported by high-level evidence, is costly, and is potentially harmful to the patient. Furthermore, although these filters are inserted for temporary prophylaxis in this setting, the filter is seldom removed in these patients. The only indication for inferior vena cava filters that has received universal agreement by leading medical professional societies is for patients with acute venous thromboembolism and contraindication to anticoagulation. D this patient is on the anticoagulant apixaban, a direct oral factor Xa inhibitor.
Order grisactin 250 mg with amex
Effect of multifocality and multicentricity on outcome in early stage breast cancer: a systematic review and meta-analysis treatment warts order 250 mg grisactin free shipping. Breast cancer diagnosed during pregnancy adapting recent advances in breast cancer care for pregnant patients. Trends in inflammatory breast carcinoma incidence and survival: the surveillance, epidemiology, and end results program at the National Cancer Institute. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. American Society of Clinical Oncology guideline recommendations for sentinel lymph node biopsy in early-stage breast cancer. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: American Society of Clinical Oncology Clinical Practice Guideline Update on Ovarian Suppression. Adjuvant aromatase inhibitors for early breast cancer after chemotherapy-induced amenorrhoea: caution and suggested guidelines. Growing use of contralateral prophylactic mastectomy despite no improvement in long-term survival for invasive breast cancer. Meta-analysis of breast cancer outcomes in adjuvant trials of aromatase inhibitors versus tamoxifen. American Cancer Society/American Society of Clinical Oncology Breast Cancer Survivorship Care Guideline. Increased risk of recurrence after hormone replacement therapy in breast cancer survivors. Preoperative treatment of postmenopausal breast cancer patients with letrozole: a randomized double-blind multicenter study. High risk of recurrence for patients with breast cancer who have human epidermal growth factor receptor 2-positive, node-negative tumors 1 cm or smaller. Estrogen-receptor status and outcomes of modern chemotherapy for patients with node-positive breast cancer. Prognosis after ipsilateral breast tumor recurrence and locoregional recurrences in five National Surgical Adjuvant Breast and Bowel Project node-positive adjuvant breast cancer trials. Tumor characteristics and clinical outcome of tubular and mucinous breast carcinomas. Clinical-pathologic features and long-term outcomes of tubular carcinoma of the breast compared with invasive ductal carcinoma treated with breast conservation therapy. Tubular carcinoma of the breast: further evidence to supports its excellent prognosis. Multidisciplinary meeting on male breast cancer: summary and research recommendations. Comparisons between different polychemotherapy regimens for early breast cancer: meta-analyses of long-term outcome among 100,000 women in 123 randomised trials. Adjuvant therapy with tamoxifen compared to aromatase inhibitors for 257 male breast cancer patients. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Management of papillary breast lesions diagnosed on core-needle biopsy: clinical pathologic and radiologic analysis of 276 cases with surgical follow-up. A 68-year-old woman was referred to your office for evaluation of a newly diagnosed left breast cancer. A core biopsy of the left axilla also showed involvement by invasive ductal carcinoma. She reports experiencing fatigue, anorexia, and abdominal pain in the epigastric area. She undergoes a biopsy of one of the liver lesions, and it is consistent with her breast primary. Docetaxel, trastuzumab, and pertuzumab Paclitaxel and trastuzumab Anastrozole and trastuzumab Letrozole and lapatinib Ado-trastuzumab emtansine 2. Agree with your colleague, reassure the patient she needs treatment, and proceed immediately with palliative chemotherapy B. Restaging of her extracranial disease shows an increase in the size of the pulmonary and liver lesions. After completing 6 weeks of therapy, she traveled to visit her family in another state. The patient is doing very well, and in great spirits, with a performance status of 1. Navelbine loading dose 50 mg/m2 and trastuzumab loading dose 4 mg/kg followed by 2 mg/kg weekly thereafter C. Navelbine 25 mg/m2 and trastuzumab loading dose 4 mg/kg followed by 2 mg/kg weekly thereafter 7. A healthy 40-year-old female presents with a 1-week history of headaches, nausea, and dizziness. She underwent lumpectomy, sentinel lymph node biopsy, radiation, and anthracycline/taxane-based adjuvant chemotherapy. Refer to a neurosurgeon for consideration of resection of the brain lesion to then be followed by irradiation D. She developed a skin rash and stomatitis, which has persisted since the second month of therapy. She describes a new progressive dry cough associated with increasing shortness of breath when going upstairs at home. This first manifested 10 days ago, and she tells you she has not been upstairs for the past 3 days. A 49-year-old woman with metastatic breast cancer is referred to you for a second opinion. She underwent lumpectomy, sentinel lymph node biopsy, and received radiation therapy to the breast and four cycles of adjuvant chemotherapy with docetaxel and cyclophosphamide. Eighteen months ago, she was diagnosed with biopsy-proven metastatic disease involving the lungs and liver. She received weekly paclitaxel and experienced a partial response lasting 12 months. Restaging studies after four cycles of liposomal doxorubicin chemotherapy showed stable disease. During her consultation with you, she reports no trouble doing most of her daily activities. No pulmonary abnormalities are detected, and the lymph nodes and liver are not enlarged. Follow-up computed tomography shows tumor progression, with an increase in the size and number of liver metastases and pulmonary nodules. Scans reveal progression of disease in the lungs and sclerotic lesions in the bones without evidence of fracture. Start palbociclib at the same time as radiation to the hip, and switch letrozole for anastrozole D. A 52-year-old woman presents to you with a history of metastatic breast cancer initially diagnosed 5 years ago. When she presented at that time, she had a mass in the right breast, right axillary lymph node, and pulmonary nodules. She received initial therapy with docetaxel, pertuzumab, and trastuzumab for six cycles and achieved a partial response. Breast Cancer also noticed increasing fatigue after work and a few days of temperature between 99. Prescribe a course of amoxicillin and clavulanate; continue treatment with exemestane and everolimus B. Refer the patient to immunologist for seasonal allergies treatment optimization C. Stop exemestane and send labs containing complete blood count and blood cultures D. Order a high-resolution computed tomography scan of the chest; draw labs including complete blood count and blood cultures; send pulmonary consultation and hold everolimus 9.
Cheap 250 mg grisactin with mastercard
In the sixth intercostal space along the ante rior axillary line medicine side effects discount grisactin line, the apical impulse was enlarged and associated with a soft S3 gallop. Cardiac catheterization showed significant (>80%) lesions in both the left anterior descending and right coronary arteries. Left ventriculography demonstrated an enlarged chamber with a calculated left ventricular ejection fraction (by area length method) of 16%. Interestingly, the left ventricular waveform on the "weak" beats differs by its reduced peak and time to peak pressure, as well as a subtle alteration of the rapid phase of relaxation. The left ventricular relaxation pattern of weak beats shows a subtle delay and an altered waveform (arrow). The time to peak systolic pressure is also prolonged in the weaker beats of right sided pressures, consistent with the hypothesized mech anism of alternating diminished contractility. Right ventricular pulsus alternans may occur independently, concordantly or discordantly with left ventricular alternans [22, 23]. This patient demonstrated pulsus alternans by both clinical and hemodynamic criteria. Physical findings associated with pulsus alternans included alternating intensity of heart sounds and an S3 gallop. Pulsus alternans may be augmented by maneuvers which decrease venous return, such as head tilting, standing, or administration of nitroglycerin. Pulsus alternans must be differentiated from condi tions with similar physical examination characteristics. Pulsus paradoxus is the decrease in pulse amplitude during the inspiratory phase of respiration. In this condition, when a patient has a rapid respiratory rate that is equal to half the pulse rate, the physical findings may resemble pulsus alter nans, with an apparent decrease in pulse amplitude every other beat. When the aerobic limit of the myocardium was exceeded, myocardial per formance declined, with resultant pulsus alternans [25]. Pulsus alternans is thought to be primarily due to decreased myocardial contractility on alternate beats, with relatively less effect produced by changes in preload, afterload, or diastolic relaxation [16, 18, 26]. Decreased contractility is attributed to deletion of the number of myocardial cells contracting on alternate beats. This reduction in the contractile cell population is thought to be caused by intracellular calcium cycling involving the sarcoplasmic reticulum, leading to localized electrical mechanical dissociation [27]. However, measured diastolic volumes in patient studies [19] suggest that the earlier mechanism may play a more predominant role. A 62yearold patient with congestive failure under went cardiac catheterization for mitral regurgitation and continuing left ventricular dysfunction. Note the differences in the height of the V and A waves during sinus rhythm on the oddnumbered beats. The alternation of V waves was consistent with the pulsus alternans produced in the systemic pressure. The left atrial filling curve (compliance) was appropriately influenced with a greater degree of mitral regurgitation (a larger V wave) for greater systolic ejection (regurgitant pressure). The theory of pressure generation and alternation of contractility on a beattobeat basis with unimpaired diastolic parameters was reported by Bashore et al. Pulsus alternans was induced by preload reduction with balloon occlusion of the inferior vena cava, performed during measurements of left ventricular function. Reduction in preload in 11 patients with nonischemic cardiomyopathy produced sustained pulsus alternans in 5 patients. The weak beats demonstrated a reduction in peak systolic pres sure, fractional shortening, and peak positive dP/dt. Left ventricular enddias tolic wall stress differed somewhat between baseline beats and weak beats, but not strong beats. These data were consistent with an augmentation and deletion of intrinsic contractile forces in association with an alternation in preload on a beattobeat basis during pulsus alternans. Of the many associations of pulsus alternans, myocar dial ischemia appears to contribute to both the alterna tion and attenuation of the pressure waveforms. Pulsus alternans observed prior to coronary angiography in a patient with severe cardiomyopathy was significantly attenuated during contrast injection [21]. Pulsus alter nans may also disappear after administration of digitalis [29] and during continued deterioration of left ventricu lar function [30]. Both the new appearance of pulsus alternans and the disappearance of pulsus alternans should alert the clinician to possible deteriorating myo cardial function. Nitroglycerin and Ventricular Unloading Effects of Nitroglycerin Nitroglycerin is the most commonly used medication in the cardiac catheterization laboratory [31]. The hemody namic effects of systemic and coronary vasodilation are often striking and, in general, are therapeutic. Nitroglycerin is routinely administered sublingually, intravenously, or intraarterially during coronary and left ventricular angiography. However, the varied hemody namic influences of nitroglycerin reported during myo cardial ischemia [34, 35] may not be readily apparent from routine responses observed in stable patients. This section will review the hemodynamic effects of nitro glycerin with particular reference to ventricular unload ing and acute ischemia. The case examples illustrate the systemic and coronary influence of this potent, short lived, and important medication. A 72yearold woman with severe triple vessel coro nary artery disease and hypertension had intermittent chest pain preceding the diagnostic coronary angiogram. What is the upper limit of left ventricular enddiastolic pressure (above which the risk of problems increases) for patients undergoing left ventriculography Based on the pressure tracing and clinical presentation, would this patient likely have a problem during or following left ventricu lography Subtle baseline concordant right and left ventricular alternans is dramatically accentuated during inferior vena caval balloon occlusion. The mild baseline pulsus alternans shown is accentuated following the postextrasystolic accentuation of the pressure. The concordance of right and left ventricular pulsus alternans is again demonstrated. Nitroglycerin reduced the systolic pressure from 200 mm Hg to 155 mm Hg and enddiastolic pressure to approxi mately 2 mm Hg. It should be obvious from this typical hemodynamic tracing that sublingual nitroglycerin produced a marked reduction in left ventricular preload, dropping the left ventricular filling pressure from 22 mm Hg to 2 mm Hg, with a corresponding reduction in the left ventricular systolic pressure. This is a characteristic response to sub lingual nitroglycerin, especially evident in patients with high left ventricular enddiastolic pressure. During the ischemic stress of supine exercise, systemic nitroglycerin also demonstrates a significant reduction in enddias tolic pressures and left ventricular endsystolic volume in comparison to intracoronary nitrates [38]. These find ings support the systemic effects of preload reduction more than coronary dilation as predominantly responsi ble for the antiischemic effects of nitroglycerin [33, 35]. Patients with elevated left ventricular enddiastolic pressure may have ongoing ischemia that does not become symptomatic until after left ventriculography. High left ventricular enddiastolic pressures (>30 mm Hg) have been associated in the catheterization labora tory with the development of accelerated angina and congestive heart failure in some patients [39, 40]. Nitroglycerin should be routinely administered (either sublingually or systemically) for left ventricular end diastolic pressures greater than 20 mm Hg. Depending on the volume status of the individual, preload reduction with small doses of nitroglycerin can result in a signifi cant decrease in filling pressures, as demonstrated in this patient. Patients with hypertension and high left ventric ular enddiastolic pressure, especially those with coro nary artery disease and hypertrophy, have an increased potential for subclinical ischemia and generally respond favorably to prophylactic nitroglycerin. To maintain a satisfactory systemic pressure after ven triculography should hypotension occur due to a marked vasodilatory effect of radiographic contrast media, we infuse fluids to increase the left ventricular enddiastolic pressure by between 5 mm Hg and 10 mm Hg. It is not routinely necessary to administer volume after nitroglyc erin, but the hemodynamic effect of nitroglycerin can be used as an indicator of the volume status to prevent hypotension, either following contrastinduced vasodila tation or later in the postcatheterization period in which contrastinduced diuresis may further deplete the mar ginal volume status of such individuals. A 61yearold woman with unstable angina was admit ted to the hospital for cardiac catheterization. In the catheterization laboratory, routine right and leftheart hemodynamic measurements were obtained before cor onary angiography and ventriculography. During these measurements, the patient complained of her typical chest pain while resting during the midportion of the study.
Purchase cheapest grisactin
Femoral artery pressure did not match left ventricular pressure during simultaneous measurements (first and second lower panels) medicine xarelto order grisactin 250 mg mastercard. Reflushing after initial pressures produced satisfactory measurements, with both pressures returning to zero (right edge, bottom middle panel). Note the delay in femoral artery pressure and marked overshoot of the peripheral pressure. Prior to pullback from left ventricle to aorta, there is again drift of the aortic pressure, and on pullback the disparity between peripheral arterial pressure and aortic pressure can be seen. The disparity between pressures is evident on both phasic and mean differences of pressure, despite an accurate "zero" of both transducers. This tracing demonstrates the differences in sensitivity of pressures due to a faulty transducer, which was replaced. Femoral or peripheral arterial pressure is not, and usually should not be, equal to central aortic pressure. The overshoot of femoral artery pressure is due to summation of the pressure wave reflections generated by the expansion and recoil characteristics of the central aortic and large artery elasticity. The peripheral or femoral artery pressure is almost always higher than the central aortic pressure. Recalibrate both transducers with a mercury manometer as a standard to identify a faulty transducer. A damped arterial sheath pressure can be due to (i) pressure artifact with damping within the sheath; (ii) significant arterial disease with aortic coarctation or iliac or femoral arterial disease; or (iii) inadequate pressure transmission outside the sheath. In this patient with peripheral vascular disease and no clinical or echocardiographic signs of aortic stenosis other than an ejection murmur, a second arterial catheter insertion was not performed. However, if there is a major discrepancy between the femoral artery and central aortic pressure tracings after all steps to insure good pressures are taken, introduction of a second arterial catheter to the central aortic position for precise transvalvular gradient measures should be performed. In contrast, some situations resulting in a high, noninvasively measured gradient do not require valve surgery. Case Examples of Hemodynamics across a Prosthetic Aortic Valve A 68yearold woman with coronary bypass surgery in 1991 developed heart failure symptoms due to severe aortic valve stenosis with aneurysmal dilatation of the ascending aorta. She remained mildly symptomatic for two years and then developed progressive and severe dyspnea on exertion with atypical chest pain. A transthoracic echocardiogram demonstrated normal systolic function with concentric left ventricular hypertrophy and a normal mitral valve. The continuouswave Doppler evaluation revealed a peak instantaneous gradient of 55 mm Hg and a mean gradient of 32 mm Hg across the aortic prosthesis. These values were substantially higher than anticipated; the reported expected parameters for this size and type of valve include a peak instantaneous gradient of 25 mm Hg and a mean gradient of 17 mm Hg, yielding an effective orifice area of 1. Aortography showed no regurgitation and left ventriculography confirmed normal left ventricular function. Coronary angiography showed no luminal obstruction except for severe proximal disease of the left anterior descending artery, which was bypassed with a widely patent left internal mammary artery graft. Chamber Pressure (in mm Hg) Right atrium Right ventricle Pulmonary artery Pulmonary capillary wedge Aorta Left ventricle a = 17, v = 16, mean = 13 83/17 83/28, mean = 50 a = 22, v = 20, mean = 18 138/64, mean = 93 163/18 Thermodilution cardiac output = 4. An exhaustive search for the cause of her pulmonary hypertension was unrevealing and she was prescribed medical therapy with sildenafil, with some symptomatic improvement. He developed congestive heart failure four years later and was found to have severe aortic regurgitation and depressed left ventricular function. The aortic prosthesis appeared to function normally, but continuouswave Doppler interrogation recorded a peak instantaneous gradient of 80 mm Hg and a mean gradient of 50 mm Hg. He was treated with diuretics and an angiotensin receptor blocker, with improvement in symptoms. Jude aortic prosthesis confirmed normal opening and closing and aortography showed no regurgitation. A right heart and transseptal catheterization was performed, both to assess the transvalvular hemodynamics and to perform left ventriculography. The aortic pressure waveform exhibited a delayed upstroke consistent with severe obstruction. The left ventricular pressure was obtained via a transseptal approach; the aortic pressure was obtained from a pigtail catheter placed at about the aortic arch. Note the delayed upstroke of the aortic pressure wave and the large (60 mmHg peak to peak) transvalvular gradient. Chamber Pressure (in mm Hg) 100 Right atrium Right ventricle Pulmonary artery Pulmonary capillary wedge Aorta Left ventricle a = 13, v = 13, mean = 8 36/11 36/19, mean = 26 a = 14, v = 12, mean = 11 118/67, mean = 87 187/15 0 e Thermodilution cardiac output = 9. The aortic pigtail catheter was repositioned 2 cm above the aortic prosthetic valve. The pigtail catheter was positioned 2 cm above the aortic prosthesis in the ascending aorta. A duallumen multipurpose catheter was then positioned in the ascending aorta, with the distal tip placed above the valve and the proximal port just distal to the radiolucent ridge seen on the aortogram. The distal port of the catheter recorded pressure in the aorta directly above the aortic valve prosthesis (arrow); the proximal port recorded pressure at the arch of the aorta just distal to the translucent ridge. Based on these findings, optimal relief of outflow tract obstruction would necessitate not only a repeat aortic valve replacement using a larger prosthesis, but also surgical repair of the acquired supravalvular aortic stenosis, a procedure with a much greater surgical risk. Prosthetic Valve Hemodynamics: Invasive versus Noninvasive Methods Following valve surgery, the function of a prosthetic valve is usually assessed noninvasively by Doppler echocardiography. Normally functioning prosthetic valves obstruct blood flow to some degree, usually resulting in a transvalvular gradient. In addition, there may be highvelocity jets around the complex orifices associated with some prostheses, resulting in turbulence and localized gradients. The challenge facing a clinician lies in determining whether the observed Doppler gradient is entirely normal and represents a wellfunctioning prosthesis, or is due to prosthetic valve malfunction. In general, Doppler gradients across aortic prosthetic valves exceed catheter gradients, particularly in St. In addition to the fact that catheter techniques report gradients differently than Doppler techniques. It is important to note that for both Doppler and a catheterbased technique, the magnitude of the gradient depends not only on the type and size of the prosthetic valve, but also on the flow across the valve. Therefore, although there are published "normal values" for Doppler indices of prosthetic valve function based on the type and size of the prosthesis [24], these data may not reconcile with an individual patient existing at either extreme of blood flow across the valve. The flow across the valve is not known when Doppler methods are employed, but is readily available during invasive techniques. Invasive interrogation of a prosthetic valve offers greater accuracy, but requires several considerations. As exemplified by patient #1, a bioprosthetic aortic valve (but not mechanical) can be crossed with a catheter and the transvalvular pressure gradient assessed similar to a native aortic valve. A mechanical prosthesis should not be crossed with a catheter, since entrapment or severe regurgitation may result, with catastrophic consequences [25]. Alternative catheterization techniques involve the placement of a catheter in the aorta above the valve and another catheter in the left ventricle via a transseptal catheterization. Direct apical puncture is another method of accessing the left ventricle, used exclusively when there is also a mechanical valve in the mitral position [26]. A recently described, easy, and safe method to measure left ventricular pressure in the presence of a mechanical aortic valve involves the use of a pressure wire [27, 28]. The main limitation of this technique is that it does not allow for ventriculography; for this reason, a transseptal catheterization was chosen for patient #2 instead of the pressurewire technique.
Syndromes
- Vulcanized butyl rubber
- Bad reactions to medicines
- Get medical attention.
- Creams and ointment for the skin
- Taking drugs like ibuprofen and naproxen to help reduce swelling and pain
- Ureteroscopy may be used for stones in the lower urinary tract.
- After a bone fracture
Cheap grisactin 250 mg otc
However treatment for pneumonia discount grisactin online visa, an inattentive operator may take several seconds to react promptly to limit asystole and hypotension. Mechanisms of Ventricularization the mechanisms of coronary pressure damping have been studied by Pacold et al. Variable degrees of intracoronary pressure changes upon cannulation of diseased left main coronary arteries were observed in 20 consecutive patients with ventricularization of coronary pressure. Confirmation of these pressure waveforms was obtained in an animal model by inserting a balloon tipped catheter and producing partial degrees of occlusion of the left main coronary artery. The ventricularized pressure wave is derived from aortic pressure, which is altered by its transmission across the narrowed left main coronary artery. Advancing a catheter into the ostium of a narrowed coronary artery reduces both systolic and diastolic pressures, as well as causing a steep decline of the pressure in diastole. A characteristic increase in pressure at enddiastole with a presystolic positive deflection was thought to be related to atrial contraction. The degree of pressure drop between the ascending aorta and a stenosed left main coronary artery is variable, depending on the degree of stenosis. Pressures from small right coronary arteries and stenosed proximal vein grafts may also demonstrate this phenomenon. The concept that ventricularization may occur by an unfavorable position of the catheter tip against an arterial wall without stenosis does not appear to be supported by the demonstration of Pacold et al. Ventricularization remains a critical observation related to left main coronary artery stenosis. Appropriate special techniques to obtain safe angiograms for this situation should be employed [81]. A lowvolume, digital subtraction ventriculogram may be a helpful "onetest" study for immediate surgical consultation. In patients with critical left main stenosis, insertion of an intraaortic balloon pump and rapid transfer for emergency cardiac surgery may be required. Pressure Damping Due to Catheter Tip Abutment against the Arterial Wall Pressure damping due to true left main stenosis must be differentiated from damping due to the tip of the catheter set flush against the vessel wall. Catheter withdrawal, repositioning, reangulation, and cusp injection should be performed. Patient management will differ according to the laboratory experience and training of the operators. Recognition and appreciation of abnormal coronary pressure waveforms may directly affect the life and death of these patients. Key Points 1) Measurements of coronary pressure and flow in the catheterization laboratory are now used in daily clinical practice and associated with improved clinical outcomes for percutaneous coronary intervention decisionmaking. Noninvasive assessment of coronary stenoses by myocardial perfusion imaging during pharmacologic coronary vasodilation: Physiologic basis and experimental validation. Fluid dynamics of a partially collapsible stenosis in a flow model of the coronary circulation. Coronary physiology revisited: Practical insights from the cardiac catheterization laboratory. Fractional flow reserve: A useful index to evaluate the influence of an epicardial coronary stenosis on myocardial blood flow. Simultaneous coronary pressure and flow velocity measurements in humans: Feasibility, reproducibility and hemodynamic dependence of coronary flow velocity reserve, hyperemic flow versus pressure slope index and fractional flow reserve. Diagnostic classification of the instantaneous wavefree ratio is equivalent to fractional flow reserve and is not improved with adenosine administration. Measurement of fractional flow reserve to assess the functional severity of coronaryartery stenoses. Metaanalysis of fractional flow reserve versus quantitative coronary angiography and noninvasive imaging for evaluation of myocardial ischemia. Variations in normal coronary vasodilatory reserve stratified by artery, gender, heart transplantation and coronary artery disease. Relation between myocardial fractional flow reserve calculated from coronary pressure measurements and exerciseinduced myocardial ischemia. Comparison of exercise electrocardiography and dobutamine echocardiography with invasively assessed myocardial fractional flow reserve in evaluation of severity of coronary arterial narrowing. Fractional flow reserve, absolute and relative coronary blood flow velocity reserve in relation to the results of technetium99 m sestamibi singlephoton emission computed tomography in patients with twovessel coronary artery disease. Use of fractional myocardial flow reserve to asses the functional significance of intermediate coronary stenosis. Clinical potential of intravascular ultrasound for physiological assessment of coronary stenosis: Relationship between quantitative ultrasound tomography and pressurederived fractional flow reserve. Intravascular ultrasound criteria for the assessment of the functional significance of intermediate coronary artery stenoses and comparison with fractional flow reserve. Morphometric assessment of coronary stenosis relevance with optical coherence tomography: A comparison with fractional flow reserve and intravascular ultrasound. Percutaneous 346 Coronary Hemodynamics 26 27 28 29 30 31 32 33 34 35 coronary intervention of functionally nonsignificant stenoses: 5 year followup of the Defer study. Comparison between angiography and fractional flow reserve versus singlephoton emission computed tomographic myocardial perfusion imaging for determining lesion significance in patients with multivessel coronary disease. Usefulness of fractional flow reserve for risk stratification of patients with multivessel coronary artery disease and an intermediate stenosis. Longterm clinical outcome after fractional flow reserveguided percutaneous coronary intervention in patients with multivessel disease. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. Longterm clinical outcome after fractional flow reserveguided treatment in patients with angiographically equivocal left main coronary artery stenosis. Fractional flow reserve assessment of left main stenosis in the presence of downstream coronary stenoses. The impact of downstream coronary stenosis on fractional flow reserve assessment of intermediate left main coronary artery disease: Human validation. Coronary pressure measurement to assess the hemodynamic significance of serial stenoses within one coronary artery validation in humans. Pressurederived fractional flow reserve to assess serial epicardial stenoses: Theoretical basis and animal validation. Abnormal epicardial coronary resistance in patients with diffuse atherosclerosis but "normal" coronary angiography. Physiologic assessment of jailed side branch lesions using fractional flow reserve. Lack of relationship between imaging and physiology in ostial coronary artery narrowings. Fractional flow reserve for the assessment of nonculprit coronary artery stenoses in patients with acute myocardial infarction. Fractional flow reserve of infarct related arteries identifies reversible defects on noninvasive myocardial perfusion imaging early after myocardial infarction. Effects of microvascular dysfunction on myocardial fractional flow reserve after percutaneous coronary intervention in patients with acute myocardial infarction. Outcome of patients with acute coronary syndromes and moderate lesions undergoing deferral of revascularization based on fractional flow reserve assessment. In vivo validation of a thermodilution method to determine regional left ventricular blood flow in patients with coronary disease. Transluminal, subselective measurement of coronary artery blood flow velocity and vasodilator reserve in man. Impaired coronary vasodilatory reserve in the immediate postcoronary angioplasty period: Analysis of coronary arterial velocity flow indices and regional cardiac venous efflux. Limitations of cough in maintaining blood flow during asystole: Assessment by two dimensional and Doppler echocardiography. Effect of abruptly increased intrathoracic pressure on coronary blood flow velocity in patients. Pulmonary inflation reflex: Its lack of physiological significance in coronary circulation of humans. Ventricular arrhythmia due to intracoronary papaverine: Analysis of clinical and hemodynamic data with coronary vasodilatory reserve.
Grisactin 250 mg with amex
In this context 7 medications that cause incontinence order grisactin 250mg with amex, the results are reasonably consistent with those previously reported by Astley et al. These composite samples were tested using uniaxial deformation testing for stretching the strips in the wet state (typically 95% water by weight). Mechanical properties of vascular tissue have been a topic of interest given the creep behavior of blood vessel walls and have been reported extensively [110,111]. However, blood vessels are able to maintain their stability and contain the pressure and flow of blood under a variety of physiological conditions. Cerebral blood vessels form part of the composite structure of the brain and, because of their relative stiffness in comparison with brain tissue, play an important role in the overall response of the brain to loading [112]. Previous studies of the mechanical properties of cerebral arteries have revealed some of the fundamental characteristics of these vessels, including observations that they are stiffer in both the axial [113,114] and circumferential [113,115] directions than most extracranial arteries and are stiffer than cerebral veins [115]. Additionally, the elastic match with blood vessel tissue will also ensure the required compliance of vessel walls during healing around the cerebral aneurysm orifice. However, the same indentation load produced different maximum penetration depths; this is a consequence of some residual elastic deformation that can be sensed when the next indentation is performed within a short difference in time. The observed residual elastic straining effect is well-known in several biological tissues like cartilage, tendons, and ligaments [117] and in blood vessels. Normal loading-unloading nanoindentation tests were performed through a Berkovich indenter by using a multimodule mechanical tester (Micro Materials Ltd. A Berkovich diamond indenter was used in this experiment, for which the contact area as a function of indenting depth was calibrated using fused silica and tungsten reference samples at room temperature. Right panel: (top) a typical nanoindentation profile showing the source of both creep data and thermal drift rate. Surface treatment of metallic biomaterials in contact with blood to enhance hemocompatibility 315 11. The creep deformation profile is extracted from the dwell period at the peak load; dwell period may affect the creep data. A number of dwell periods were tried, and a dwell period of 20 s was decided based on convergence in the measurements. In the case of highly viscoelastic polymers and porous hydrogels, plastic or inelastic deformation under nanoindentation creep is controlled by shear slipping events between both fibers and/or particles that are characterized by a horizontal constant load line on the P-h (load-depth) curve. In this case, holding the load below the shear slipping critical value during prolonged time will lead to indentation creep. Therefore, the creep investigations have to be performed at different peak indentation loads. The modulus and hardness were calculated using the well-known Oliver-Pharr method [118,119]. Surface treatment of metallic biomaterials in contact with blood to enhance hemocompatibility 317 with ~ 65. Subscripts i and s represent the indenter tip and specimen (for the diamond tip, i = 0. However, the elastic modulus calculated in this way can be highly affected by creep [121,122] especially when the material is soft (such as the case for cellulose-based structural materials), the holding time is short, the unloading rate is slow, or the peak load is large [122]. For our experiments, constant load was applied in the load-holding period, so Ph is zero in this case. Besides the creep behavior of veins, they also suffer a residual stress and strain effect that is typically reflected in that they are known to retract both longitudinally and circumferentially after excision. Circumferential retraction of medium-caliber blood vessels, such as the carotid, iliac, and brachial arteries, can exceed 70% following reduction of internal blood pressure to zero. In that sense, it is reasonable to assume that blood vessels are in a nearly stress-free state when they are fully retracted and free of external loads. This work was performed by ultrasonically determining systolic and diastolic pressures for diameter and wall thickness for several peripheral vessels as a function of age and to calculate mechanical parameters, including circumferential stiffness. For all arteries examined, the physiological parameters were observed to generally increase as a function of increasing age. This confirms that increasing the deformation of the blood vessels with time (age), leads to the decay of velocity or rate trends with time as is typically reflected in any creep curve. Indentation creep experiments with typical holding times of 500 s are used to characterize such creep deformation. Nanoscale investigations of creep deformation can also provide important insights into achieving control of creep in materials such as soft hierarchical nanocellulose matter studied here. The model found to correspond most closely was composed of a log-time function, two Kelvin elements, and a viscous flow element. This is identical to the model that was found to provide the best fit to extension of tomato fruit epidermis [129], pea leaves [130], tomato leaf rachis, wheat seed coats, and sunflower hypocotyls. Retardation and relaxation times are often interpreted as being specific to a particular type of process, with shorter times being associated with smaller scale events such as rotation of polymer segments relative to one another and longer times associated with larger-scale events such as relative movement of polymer chains. In particular, for metals, numerous chemical, physical, and biological elements combine to dictate the fate of tissue regeneration and reconstruction. Understanding the efficacy of candidate Surface treatment of metallic biomaterials in contact with blood to enhance hemocompatibility 319 metallic materials for novel biomedical devices designed as prosthetics, orthopedics, sensors, actuators, or local drug-eluting systems all must contend with the complex response of the local hemodynamic and immune response of the tissue. Simulating this process in order to provide in situ and pseudo in vivo characterization involves understanding the specific process to be simulated and the specific performance attribute to be examined. The holistic response of the body when presented by an initial wound and introduction of a foreign body is designed to provide localized selfhealing processes coded in our genes. Understanding blood-material interactions can help elucidate novel biomedical device interfaces that can work together with the body in complementing healing and in some cases even accelerating the same. Hemodynamic flow, hemostasis, and local self-healing can be successfully studied and intervened by correlating the immune response pathways with the bioactive design of metallic biomaterials that enable tissue regenerative pathways. Oreffo, Bone and metal: an orthopaedic perspective on osseointegration of metals, Acta Biomater. Hieda, Development of new metallic alloys for biomedical applications, Acta Biomater. Wessely, Evolution of coronary stents: from bare-metal stents to fully biodegradable, drug-eluting stents, Comb. Stangl, Bone-implant interface shear modulus and ultimate stress in a transcortical rabbit model of open-pore Ti6Al4V implants, J. Zhu, Similarities and differences in coatings for magnesium-based stents and orthopaedic implants, J. Witte, Reprint of: the history of biodegradable magnesium implants: a review, Acta Biomater. Stanciu, Evolution of novel bioresorbable iron-manganese implant surfaces and their degradation behaviors in vitro, J. Hansen, Metal corrosion in the human body: the ultimate bio-corrosion scenario, Electrochem. Baker, Prevention of coronary in-stent restenosis and vein graft failure: does vascular gene therapy have a role Pavlov, Extensive metallosis and necrosis in failed prostheses with cemented titanium-alloy stems and ceramic heads, J. Zeisler, Investigations of the corrosive deposition of components of metal implants and of the behaviour of biological trace elements in metallosis tissue by means of instrumental multi-element activation analysis, J.
Generic grisactin 250 mg with amex
Yet they remain within a niche market due to the longer crossclamp times and increased technical difficulty to implant surgically medicine 6 clinic grisactin 250mg with mastercard. The common components of the technology are comprised of pericardial leaflets sutured onto a collapsible stent and a delivery catheter to facilitate percutaneous valve Valve related complications and their impact on hemocompatibility Table 15. This may occur if valves are inadequately expanded, non-uniformity of calcific annulus or mal-positioning (Cao et al. Incorrect positioning of the valve can occur through either poor commissural alignment or poor annular seating (Webb et al. Wear from the occluder on cloth covered sewing rings and struts (Schottenfeld et al. Valve occluder wear from constant rubbing against the valve housing (Edgett et al. Calcification commonly occurs with glutaraldehyde treated bioprosthetic valves leading to leaflet thickening, stiffness and stenosis (Vesely, 2003). Strut fracture can occur due to malpositioning or poor sizing, subjecting the housing to increased stress (Blot et al. Occluder can become immobilized secondary to other complications such as strut fractures (Edgett et al. Obstruction to flow can occur due to the presence of the annular sewing ring or through thrombus formation (Roudaut et al. The technology has progressed rapidly from being initially limited to high-risk elderly patients denied conventional surgical valve replacement towards implantation in low and intermediate risk patients and continues to make strides in state-of-the-art valve technologies [100]. The long-term freedom from thromboembolism in pericardial valves in the absence of anticoagulant treatment is considered to be a significant benefit [76,101,102]. In a study of 1751 patients receiving aortic valve replacement with a mean follow up period of 3. However, both types of bioprosthesis have a high propensity for calcification, reducing their durability and making them unsuitable in younger patients. Calcification can be intrinsic (calcific nodules forming on the surface of an intact leaflet) or extrinsic (calcification formed Improving the hemocompatibility of heart valves 405 at site of lesion or crack on surface of leaflet). Conversely, tearing can be caused by localized calcific nodules on the surface of the leaflet. Apart from leading to structural degradation, leaflet tears can lead to hemolysis due to the increased shearing of blood through these gaps [104]. This has promoted a drive for alternative fixation methods to reduce leaflet calcification. Polymeric heart valves have also been prone to thrombogenicity and calcification [105,111]. Significant advancements in material science have improved polymer resistance to hydrolysis and oxidation. The surface properties of polymeric heart valves can be modified to increase their resistance to platelet attachment. It is influenced through a range of factors including inadequate anticoagulation treatment, valve material, blood-surface interactions, and prosthetic valve hemodynamics. The design considerations for improving valve hemocompatibility are discussed in depth below. It is applied as a thick coating over a suitable substrate using fluidized bed chemical vapor deposition. Substrates of graphite or titanium or cobalt-chromium alloys can be used and could be machined off afterwards to leave a monolithic substrate. The Debakey Surgitool was the first valve to utilize this material for their ball occluder although the superior toughness of the ball contributed to strut fracture [116]. Feng and Andrade hypothesized four stages for protein surface conditioning: diffusion of protein (collision with the surface), adsorption (mainly albumin, as it is the most abundant), denaturation (adsorbed protein denatures and a protective film of protein forms), and modification (the film prevents activation of the coagulation cascade) [121]. This may suggest that the active state of the protein adsorbed rather than its affinity is the contributing factor for surface passivation [118]. It is possible that the design and highly polished surface of these valves rather than their pure carbon content is the contributing factor to its increased hemocompatibility. In addition, their brittle nature makes them prone to Improving the hemocompatibility of heart valves 407 fracturing. Both the surface energy and semiconductivity of these coatings play a vital role in improving the hemocompatibility of heart valves. This made it more difficult to transfer charge from the protein to the surface, inhibiting the decomposition of Fng [134]. Improved hemocompatibility has also been observed through this reduction in the work function (the energy required to move an electron from the highest Fermi level of a solid to a vacuum) of Ti2+ and Ti3+ in TiO2 coatings [132]. Their classification include tetrahedral amorphous carbon (ta-C), hydrogenated amorphous carbon (a-C:H), and nonhydrogenated amorphous carbon (a-C). The improved blood compatibility of titanium incorporated a-C:H films compared to TiN and (titanium carbide) TiC coatings was shown to be due to their increased hydrophobicity [139]. In addition, the adhesion between the coating and the substrate can be poor due to high intrinsic compressive stresses [148]. This has shown reduced environmental Improving the hemocompatibility of heart valves 409 and thermal effects, reduced internal stresses, stabile sp3 bonds, and inhibited sp2 hybridization [148]. This has created a cascade of surface treatments through the application of anticoagulant coatings or by modifying the surface energy and roughness. One of the first studies on anticoagulant coated surfaces used a cationic surface active agent to bond heparin to graphite, demonstrating freedom from coagulation in the 10 h time limit of the study compared to rinsed heparin treated graphite which experienced coagulation within an hour [151]. Following this, rings of heparin bound graphite reported little to no sign of thrombosis following implantation studies after a year. Heparin coatings have also found antithrombogenic potential with tissue valves using a heparin-vascular endothelial growth factor multilayer film [153]. The durability of immobilized heparin following exposure to plasma at a high shear rate however remains an issue, with studies showing a shearing of the top layer of the coating in combination with a loss of heparin conjugate and some plasma deposition [153,154]. In addition, there has been some indication of heparin adsorption into the blood stream which may limit its anticoagulant potential with time [151]. Hirudin is a small protein with thrombin inhibition properties which has also been examined for use as a potential antithrombogenic coating. Covalent binding of hirudin on the surface of Dacron, for sewing rings, was found to reduce the rate of platelet adhesion and activation as well as a reduced conformational change to Fng [155]. A low surface tension was associated with an increased dynamic clotting time and a weak adherence of protein, allowing 410 Hemocompatibility of Biomaterials for Clinical Applications any attached platelets to wash away with the shearing rate of blood. For example, the surface tension of the Stellite 21 struts of the Starr-Edwards ball-valves was reduced through a coating of Teflon. Conversely, a high surface tension would promote a strong cellular attachment, forming a protective biological barrier. Surface modification of polymeric heart valves have shown some reduction in platelet adhesion. The higher polar component of its surface energy created a low affinity for proteins adsorption, thereby reducing thrombus formation [82]. The success of developing a confluent layer depends on the surface type and roughness. These disturbances lead to high shear stresses which contribute to hemolysis, platelet activation, and thrombus formation. High wall shear stresses can also damage the endothelium of surrounding structures, promoting thrombus and calcific plaque formation [163]. The impact of valve design on flow and accordingly the hemocompatibility was highly evident when Improving the hemocompatibility of heart valves 411 120 80 (mm Hg) 0 0. Images (A,B) are of the pressure across valve, (C,D) of their velocity profiles-a wake can be observed downstream of the ball and cage valve, and (E,F) their flow streamlines.
Order 250mg grisactin visa
Precapillary pulmonary hypertension reflects primary abnormalities of the pulmonary arterial 7 bed resulting from thromboembolic disease medications on airline flights discount grisactin 250 mg with mastercard, primary pulmonary hypertension, or occasionally extrinsic mass obstruction of the major pulmonary arteries from medi astinal tumors. Primary intrapulmonary processes include the broad range of primary obstructive or restric tive lung diseases. Biventricular diastolic dysfunc tion contributes to hemodynamic compromise in 25% of cases overall. The normal pericardium more tightly constrains the ventricles and therefore enhances such interactions. Even in the absence of the pericardium, pressure or volume overload of one ventricle influences the compliance and filling of the contralateral ventricle. The pericardium envelopes the cardiac chambers and under physiological conditions exerts mechanical effects that enhance normal ventricular interactions, balancing left and right cardiac outputs. Because the pericardium is noncompliant, con ditions that cause intrapericardial crowding. This is the case in any patient with significant pulmonary hypertension, regard less of the cause. Backward Heart Failure Elevated pulmonary capillary pressure leads to elevated pulmonary vascular resistance and ultimately pulmo nary congestion. Fundamentals of RightHeart Hemodynamics Hemodynamics of Abnormal Cardiac Rhythms One of the most common pitfalls in the interpretation of hemodynamic data is the failure to appreciate abnormal ities in cardiac rhythms, which often account for the alteration and, at times, misinterpretation of pressure waveforms [8, 9]. Let us examine the rightheart hemo dynamics in a patient undergoing evaluation for short ness of breath. During pac ing, the pulmonary artery pressure has a larger respiratory variation and is higher than pressures obtained during normal sinus rhythm. How does one explain the large pointed waveforms at the left side in contrast to the smaller, broader waveforms demon strated at the right Compare the effects on the cardiac rhythm of the generation of right ventricular pressure. As the atrial time delay permits normal sinus mechanisms to intervene, the waveform changes into a sinustype rhythm with a larger A wave and a small V wave. The rhythm changes explain the wide variations in right atrial and ventricular pressure waveforms, and should be important functional clues in the evaluation of hemodynamics for such individuals. Examine the pressure waves and consider the following: What is the etiology of the large, spiked waves (C) This occurs when atrial contraction falls out of sequence with normal ventricular systole and the atria contract against a tricuspid valve closed by the increased right ventricular pressure during ejection. The size of the C wave is dependent on the timing of atrial contraction relative to ventricular filling (and the position of the tri cuspid valve). When the atrial contraction precedes ven tricular contraction in its normal synchronous mode, normal A waves are generated (beats #6 and 7). These cannon waves can be observed on bedside physical examination in the jugular venous pulse and should be differentiated from systolic tricuspid regurgitant waves (to be identified below). Iatrogenic induced (pacemaker) or spontaneous abnormalities of conduction also can produce similar types of cannon waves of atrial activity out of synchrony with ventricular contraction. The pressure tracing demonstrates brief, sharp peaked waves, less prominent than the atrial contraction waves of the previous tracing. The dyssynchronous ventricular pace maker timing relative to atrial dissociated contraction appears to be responsible. The high pressure spike of very narrow width also suggests artifact from catheter impaction, but the timing sequence also is highly consistent with "cannon"type waves. Sometimes, transmission of the regurgitant wave can be detected beyond the vena cava. However, it is uncommon to observe chang ing waveforms in the inferior vena cava compared to those in the right atrium. A 61yearold woman had tricuspid regurgitation of unknown etiology which was associated with mild pul monary hypertension and dyspnea. Left ventriculography demonstrated mild global hypokinesis with an ejection fraction of 55%. Aortic pressure was 125/70 mm Hg, left ventricular pres sure was 125/12 mm Hg, and pulmonary capillary wedge pressure was 20 mm Hg with normal A and V wave con figurations. The effects of tricuspid regurgitation on the right atrium and inferior vena cava were assessed by measuring two pressures simultaneously, one from each of the two lumens of a balloontipped pulmonary artery catheter. The systolic wave of regurgitation could be appreciated in both the right atrium and inferior vena cava. The inferior vena cava pressure was measured approximately 10 cm below the inferior border of the right atrium. The waveform of the inferior vena cava is slower in upstroke and downstroke, with reduced velocity. The blunted waveform is due, in part, to the considerably higher capacity and compliance of the vena cava com pared to those of the right atrium. Inferior vena cava flow in most cases parallels that of superior vena cava flow and thus large V waves in the jugular vein on clinical examination can reflect either significant tricuspid regurgitation or functional regurgi tation during cardiac arrhythmias [14]. The jugular pulse closely reflects events in right atrial pressure and also parallels changes observed in the vena cava [15, 16]. However, one must remember that the change in pressure within the right atrium is reflected principally by a change in volume for the venous system. It is thought that the pulse wave transmission from the right atrium to the jugular veins has the least disparity for pressure waves which are positive and are thought to be conducted more rapidly compared to negative pres sure waves [17]. The venous pulse A and C waves have an average delay from right atrial pressures of approxi mately 60 msec, the V wave 80 msec, the Y trough 90 msec, and the X trough 110 msec [17]. It requires 60 msec for the right atrial A wave to reach the right ven tricle and cause a positive defection in this chamber. These delays should be considered when examining the jugular venous pulse, as well as inferior vena caval pres sure waves as a reflection of right atrial pressure [11]. Jugular vein pulsations may occur from an induced artifact of transmitted carotid arterial pressure waves. This artifact can be recognized by an irregular pulsation often obscuring the X descent. The irregular wave shows a carotidlike contour, with the dichrotic notch recog nized in the middle of the X descent [11]. Tavel [14] notes that tricuspid insufficiency often produces a prominent V wave, beginning early and tending to obliterate the X descent. In severe tricuspid regurgitation, the V wave corresponds and begins with the C wave and shows a broad plateau terminating in a steep Y descent. In the setting of atrial fibrillation, nearly complete obliteration of the X descent is required before making the diagnosis of tricuspid insufficiency from a venous pulse wave. In patients with normal sinus rhythm, changes in the venous pulse suggesting tricuspid regurgitation may demonstrate only slight decrease in the X descent equal to or above the level of the Y trough. In some patients, a separate systolic wave may appear on the V wave ascent and may be an obscured clue to the presence of tricuspid regurgitation [13]. In addition, in tricuspid regurgitation there may be a relatively normal venous pulse wave; hence the diagnostic accuracy of the waveform is helpful, in that a normal curve cannot be used to exclude tricus pid disease. The characteristic pulse waves may be absent at rest but brought on by inspiratory maneuvers or increasing heart rate [13]. Identical matching of the right atrial and right ventricular diastolic pressures is the norm. The A wave (atrial contraction) of the right atrial pressure cor responds to the A wave of the right ventricle. Note that pressure immediately after the A wave, called the X descent, falls and does not begin to increase until late in systole. As right ventricular pressure falls below right atrial pres sure, the tricuspid valve opens, releasing atrial pressure (the Y descent of the V wave).