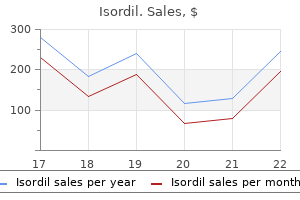
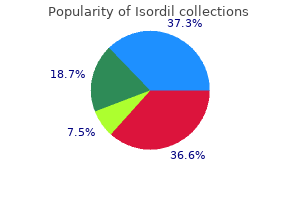
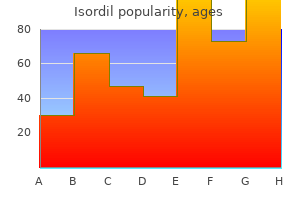
Isordil 10mg visa
Occult polymicrobial endocarditis with Haemophilus parainfluenzae in intravenous drug abusers treatment yeast infection child generic isordil 10mg otc. Short-course therapy for right-sided endocarditis due to Staphylococcus aureus in drug abusers: cloxacillin versus glycopeptides in combination with gentamycin. Effectiveness of cloxacillin with and without gentamicin in short-term therapy for right-sided 15 Right-Heart Endocarditis 221 48. Clinical practice guidelines by the infectious diseases society of America for the treatment of methicillinresistant Staphylococcus aureus infections in adults and children. Influence of vancomycin minimum inhibitory concentration on the treatment of methicillin-resistant Staphylococcus aureus bacteremia. Daptomycin versus standard therapy for bacteremia and endocarditis caused by Staphylococcus aureus. Daptomycin activity against Staphylococcus aureus following vancomycin exposure in an in vitro pharmacodynamic model with simulated endocardial vegetations. Oral antibiotic therapy for the treatment of infective endocarditis: a systematic review. Surgical management of endocarditis: the society of thoracic surgeons clinical practice guideline. Tricuspid valve replacement with bioprostheses: long-term results and causes of valve dysfunction. Current outcomes for tricuspid valve infective endocarditis surgery in North America. A novel approach to tricuspid valve replacement: the upside down stentless aortic bioprosthesis. Analysis of mortality and risk factors associated with native valve endocarditis in drug users: the importance of vegetation size. Endocarditis caused by Staphylococcus aureus: a reappraisal of the epidemiologic, clinical, 222 I. Surgical treatment of right-sided active infective endocarditis with or without involvement of the left heart: 20-year single center experience. Current profile of infective endocarditis in intravenous drug users: the prognostic relevance of the valves involved. It was Gross and Friedberg [2] in 1936 who coined the term "nonbacterial thrombotic endocarditis. These vegetations are associated neither with bacteraemia nor with destructive changes of the underlying valve [3]. The common factor is endothelial damage and subsequent exposure of the subendothelial connective tissue to the circulating platelets [4]. Factors implicated in the initiation are: (a) immune complexes, (b) hypoxia, (c) hypercoagulability, and (d) carcinomatosis [4]. It has been reported in every age group, most commonly affecting patients between the fourth and eighth decades of life with no sex predilection [7]. Lesions are thus usually clinically silent, without significant valvular dysfunction. When such dysfunction does occur, however, valvular regurgitation and, rarely, stenosis may result in heart failure and arrhythmias, such as atrial fibrillation. Symptoms often result from the underlying disease or from embolization and depend on the organ affected. Secondary infective endocarditis, although uncommon, can also complicate valvular abnormalities and can cause neurologic and systemic complications. The risk of systemic emboli is increased substantially in the presence of mitral stenosis, atrial fibrillation, or both. However, differentiation from culture-negative infective endocarditis may be 16 Non-bacterial Thrombotic Endocarditis 225 Table 16. However, the condition is not always easily recognized on echocardiographic images. Post-mortem studies described mulberry like clusters of verrucae on the ventricular surface of the posterior mitral leaflet, often with adherence of the mitral leaflet and chordae to the mural endocardium. The lesions typically consist of accumulations of immune complexes and mononuclear cells. Examination of embolic fragments after embolectomy can also help make the diagnosis. Laboratory Findings Comprehensive haematological and coagulation studies (full blood count, prothrombin time, partial thromboplastin time, fibrinogen, thrombin time, D-dimers and cross-linked fibrin degradation products) should be performed to search for a potential causes. Multiple blood cultures should be undertaken to rule out infective endocarditis, although negative blood cultures can be observed in infective endocarditis. Immunological assays for antiphospholipid syndrome (lupus anticoagulant, anticardiolipin antibodies, and anti-2-glycoprotein 1 antibodies with at least one must be positive for the diagnosis of antiphospholipid syndrome on 2 occasions 12 weeks apart) should be undertaken in patients presenting with 226 P. There is a small mobile mass (white arrow) seen at the tip of the anterior mitral valve leaflet leading to moderate mitral regurgitation (yellow arrow) recurrent systemic emboli or known systemic lupus erythematous [13]. Other features such as rheumatoid factor, antinuclear antibody and a comprehensive workup for systemic lupus erythematosus or malignancies can be indicated. They have little inflammatory reaction at the site of attachment, which make them more friable and detachable (Table 16. Following embolization, small remnants on affected valves (3 mm) may result in false negative echocardiography results. Valvular regurgitation is noted most commonly in patients with leaflet thickening, which is thought to 16 Non-bacterial Thrombotic Endocarditis 227 Table 16. Pure mitral regurgitation is the most common valvular abnormality, followed by aortic regurgitation, combined mitral stenosis and regurgitation, and combined aortic stenosis and regurgitation [19]. Prognosis the prognosis is generally poor, more because of the seriousness of predisposing disorders and associated comorbidities. The likely prevalence of secondary infective endocarditis is low, but it has not been widely reported. Potential contributing factors to infective endocarditis are connective tissue disorders connective tissue disorders such systemic lupus erythematosus, medications prescribed for these diseases, and underlying valvular abnormalities. For instance, with the introduction of steroid therapy for systemic lupus erythematosus, improved longevity of patients appears to have changed the spectrum of valvular disease. Conversely, in patients with advanced and non-curable cancers, surgery is unlikely to influence the final outcome and also not prevent recurrent embolization. If there is no contraindication, these patients should be anticoagulated with heparin/warfarin, although there is little evidence to support this strategy [21]. A trial comparing rivaroxaban (an inhibitor of factor Xa) and warfarin in patients with thrombotic antiphospholipid syndrome is currently in progress [22]. However, the risk of anticoagulation is haemorrhagic conversion of embolic events. Surgical intervention, valve debridement and/or reconstruction, is often not recommended unless the patient present recurrent thromboembolism despite well-conducted anticoagulation [23]. A rapid molecular assay for the detection of antibiotic resistance determinants in cause of infective endocarditis. Echocardiography in nonbacterial thrombotic endocarditis: from autopsy to clinical entity. Yield of transesophageal echocardiography for nonbacterial thrombotic endocarditis and other cardiac sources of embolism in cancer patients with cerebral ischemia. Cardiac valvular vegetations in cancer patients: a prospective echocardiographic study of 200 patients. Chapter 17 Infective Endocarditis in Congenital Heart Disease Joey Mike Kuijpers, Berto J. This is mainly determined by an interplay between the type of defect, its repair status, and the presence of prosthetic material used for repair or palliation. However, the risk is high in the first months after repair, due to remaining endothelial damage and the presence of foreign surfaces such as patches or closure devices that are in direct contact with blood. If residual defects remain, so will the potential for endocardial infection, as associated turbulent flow patterns will cause continued endothelial damage or hamper endothelialization of foreign surfaces.
Purchase 10mg isordil with visa
Pregnant women may be exposed to endocrine disruptors from environmental sources or medications symptoms 2dp5dt generic isordil 10 mg online, and it is crucial to study the effects of such compounds on fetoplacental steroidogenesis. The H295R/BeWo co-culture model offers the opportunity to study these interactions, by making it possible to evaluate the effects of chemical exposures on androgen and estrogen biosynthesis, as well as on various other aspects of feto-placental communication. Key words Steroidogenesis, Feto-placental unit, Estrogen, Co-culture, Trophoblast, Fetal adrenocortical 1 Introduction In the human placenta, the villous trophoblast produces large amount of estrogens, including pregnancy-specific estriol. This synthesis is dependent on precursors produced by the adrenal cortex of the mother and that of the developing fetus. We have previously shown that the H295R/BeWo co-culture is a relevant model to study estrogen biosynthesis and fulfills an essential need as research tool considering the lack of suitable in vivo or ex vivo human models. In the co-culture model, H295R cells possess fetal adrenocortical characteristics, including the ability to synthetize J. Thomas Sanderson and Cathy Vaillancourt share joint senior authorship and contributed equally to this work. The H295R/BeWo co-culture model was first characterized for its capacity to reproduce the feto-placental estrogen biosynthetic profile with interactions between the two cell types occurring in real time. In another plate, seed BeWo cells in transwell inserts at 12,500 cells/well density, 0. To the wells of the Eplate, add 100 L of either BeWo (10,000 cells/well) or H295R (20,000 cells/well) cells. To the Eplate inserts, add 50 L of BeWo (10,000 cells/insert) or H295R (20,000 cells/insert) cells. Rinse wells and inserts containing BeWo medium twice with co-culture medium, before adding the co-culture medium containing the test compound. Assemble the co-culture by placing the inserts containing BeWo cells above the H295R cells in wells or vice versa. After the treatment period (see Note 7), remove co-culture medium from the co-culture (see Note 8). Place the inserts in a 12-well plate so that the bottom of the insert is in direct contact with the well. Add 50 L/insert or 250 L/well of 54 nM [1-3H(N)] androst-4-ene-3,17-dione in uncompleted culture medium (Table 2). Table 2 Comparison of the protocol for inserts and wells Insert Volume Working solution of [1-3H(N)] androst-4-ene-3,17-dione (54 nM) Volume of supernatant + chloroform 50 L Well Dilution factor 50/40 Volume 250 L 200 L + 500 L 100 L + 100 L Dilution factor 250/200 500/200 200/100 40 L + 100 L 100/40 40/20 Volume of supernatant + dextran-coated 20 L + 20 L charcoal Volume of supernatant + scintillation cocktail Counting microplate Final dilution factor 20 L + 100 L 120/20 96 well 37. Take 40 L/insert or 200 L/well of supernatant and place in a microtube containing 100 L or 500 L chloroform, respectively (Table 2). Take 20 L/insert or 100 L/well of supernatant and place in microtubes containing 20 L or 100 L dextran-coated charcoal, respectively (Table 2). Take 20 L/insert or 100 L/well of supernatant and place in a 96-well or 24-well liquid scintillation counting microplate, respectively (Table 2). Add 10 L of 54 nM [1-3H(N)]androst-4-ene-3,17-dione in uncompleted culture medium in a well of the liquid scintillation counting microplate to determine the specific activity in the co-culture medium (Table 2). Results are either expressed as percentage of control or in pmoles of androstenedione converted/hour. This expression can be normalized to mg protein content of the well or cell number. Remove the BeWo culture medium and change to co-culture medium in the co-culture and BeWo monoculture, and place Feto-Placental Co-Culture Model 301. The longest electrode has to touch the bottom of the well, passing through the side hole of the insert. Measure 4 h after seeding the cells, directly after assembling the co-culture and every 24 h after assembly (see Note 11). Prepare and mix the solution overnight on a magnetic stir plate and mix by inverting the bottle five times before using. We recommend comparing the responses of the co-culture with those of BeWo and H295R cells in monoculture. Remove the medium from each insert as well as under the insert, where a droplet often forms, and place it in the well containing co-culture medium. In order to have an even exposure of the cells to the test compound, it should be dissolved in culture medium before treatment instead of adding the compound directly to the culture medium in the well and insert. We recommend a 24-h incubation of the co-culture, since a decrease in H295R cell proliferation is observed after 24 h under untreated circumstances [5]. To determine specificity of the tritiated water-release assay for aromatization, an irreversible inhibitor of the catalytic activity of aromatase, formestane (4-hydroxyandrostenedione), (1 M) should be used. Medium from the insert and well may be mixed together (total volume of 1 mL) or harvested separately, depending on the experimental requirements. Estrogen production by the untreated co-culture should be determined as a quality control. A synergistic production of estrogens and the presence of estriol should be observed in the co-culture compared to BeWo and H295R cells in monoculture. We consider that cells form a confluent monolayer when transepithelial resistance reaches a plateau. Processes involved in the placental transport of these nutrients are complex and tightly regulated and involve many transporters, receptors, and regulators. In this chapter, we describe the current methods to study the impact of maternal metabolic disorders on key players of human placental transfer of nutrients. Key words Placenta, Lipids, Fatty acids, Cholesterol, Transport 1 Introduction Fetal development and growth depend on the supply of nutrients from the maternal circulation through the placenta [1]. Numerous studies have shown that the deficiency of nutrients in the mother induces alterations in placental transport of nutrients during pregnancy and health problems in the offspring at birth but also during childhood and adulthood [2, 3]. Multiple factors can influence proper placental transport of nutrients including blood flow, placental size and morphology, and transporter abundance. Fatty acids and cholesterol are among the nutrients that are essential for fetal growth and development. The syncytiotrophoblast, which is the functional unit of the placenta, plays an important role in the exchange of these nutrients between the maternal and fetal circulation. It expresses several proteins involved in the placental transport of fatty acids and cholesterol. In the maternal circulation, fatty acids are found as free fatty acids or incorporated into lipoproteins. Cholesterol, which is also incorporated into Padma Murthi and Cathy Vaillancourt (eds. Horseradish peroxidase-conjugated antibody solution (anti-rabbit, anti-goat, or anti-mouse): 1:10,000 in blocking solution. Collect morphological information (weight, size, color, membrane integrity, umbilical cord, and any pathological signs such as calcification or lipid steatosis).
Discount isordil online visa
Interaction between treatment and subgroup variables will be examined in a similar fashion as above by including the relevant parameters in the model medicine 018 discount isordil 10 mg with amex. This will be done in turn for each subgroup variable and adjusted estimates presented. All tests are two-sided and results will be presented as a point estimate along with 95% confidence intervals. As such, a senior obstetric clinician who will be in ongoing communication with the research team will see them daily. Worsening preeclampsia is within the natural history of the disease and as such will not be part of discontinuation criteria. Lanoix D, Guerin P, Vaillancourt C (2012) Placental melatonin production and melatonin receptor expression are altered in preeclampsia: new insights into the role of this hormone in pregnancy. Lanoix D, Beghdadi H, Lafond J, Vaillancourt C (2008) Human placental trophoblasts synthesize melatonin and express its receptors. Okatani Y, Wakatsuki A, Shinohara K, Taniguchi K, Fukaya T (2001) Melatonin protects against oxidative mitochondrial damage induced in rat placenta by ischemia and reperfusion. Unfer V, Raffone E, Rizzo P, Buffo S (2011) Effect of a supplementation with myo-inositol plus melatonin on oocyte quality in women who failed to conceive in previous in vitro fertilization cycles for poor oocyte quality: a prospective, longitudinal, cohort study. Okatani Y, Okamoto K, Hayashi K, Wakatsuki A, Tamura S, Sagara Y (1998) Maternal-fetal transfer of melatonin in pregnant women near term. Jahnke G, Marr M, Myers C, Wilson R, Travlos G, Price C (1999) Maternal and developmental toxicity evaluation of melatonin administered orally to pregnant Sprague-Dawley rats. Hodges Abstract this chapter describes the methodologies which may be used in the development of a randomized controlled trial investigating a therapy of choice in preventing preeclampsia. Key words Preeclampsia, Melatonin, Prevention, Clinical trial, Oxidative stress 1 Introduction Preeclampsia, one of the hypertensive disorders of pregnancy, remains a leading cause of maternal death worldwide, with the majority of deaths occurring in developing countries [1]. Importantly, preeclampsia poses serious health risks for the baby, implicated in 12% of cases of fetal growth restriction, and is a known antecedent in up to 19% of preterm births [3]. There is currently no effective treatment for preeclampsia except delivery of baby, and as such it remains a significant burden of disease for both mothers and their babies worldwide. Screening for women at risk of preeclampsia is an important part of antenatal care. Once women are identified as high risk, they can be targeted for more intensive antenatal surveillance and prophylactic interventions. Most current strategies for risk assessment are based on the obstetric and medical history and clinical Padma Murthi and Cathy Vaillancourt (eds. However, there is surprisingly little reliable evidence on the actual risk associated with individual factors and how they might interact. Thrombophilia and autoimmune disease have a strong association with severe early-onset preeclampsia [8]. Obstetric factors associated with high risk are multiple pregnancy [5, 9], history of preeclampsia in a previous pregnancy especially if severe or early onset [4, 10, 11], and a current hydropic pregnancy [12]. Other factors linked with preeclampsia but associated with a somewhat lower risk include first pregnancies [5, 13], age less than 20 or more than 35 years [5], a family history of preeclampsia [14], and obesity [5, 15, 16]. Routine screening for preeclampsia is based on measurement of blood pressure and urinalysis for proteinuria. Although various physiologic and biochemical screening tests have also been developed, so far none have proved to be of good predictive value and few are used in clinical practice. Doppler ultrasound looking for increased resistance of the uterine arteries is a noninvasive imaging test to assess for abnormal blood flow to the placenta and at present holds more promise [18]. As the cause of preeclampsia is not well understood, and screening tests remain unreliable, it is difficult to develop appropriate strategies for prevention of preeclampsia. Current strategies for prevention focus on antenatal surveillance, modification of lifestyle, nutritional supplementation, and pharmacological therapy [19]. Supplementing women with melatonin (5-methoxy-Nacetyltryptamine), a potent antioxidant, may increase their resistance to oxidative stress and subsequently limit the systemic and uteroplacental endothelial damage that is observed in preeclampsia [20]. The exact pathogenesis of preeclampsia is unknown but it is likely that its evolution is multifactorial involving a complex interplay between the mother, the fetus, and the placenta (see Chapter 27). With the previously described initial abnormal placentation of preeclampsia, it is now widely accepted that resultant placental hypoperfusion can induce a state of oxidative stress [21]. Oxidative stress, coupled with an exaggerated inflammatory response, may cause the release of maternal factors that result in inappropriate endothelial cell activation and dysfunction culminating in the clinical manifestations of the disease. So while the exact pathogenesis of preeclampsia is not entirely known, it has been shown that oxidative stress is key to the origins and sequelae of the disease [22]. As described in Chapter 27, melatonin is an endogenous antioxidant hormone which has been proposed as a suitably safe Randomized Controlled Trial 349 and potentially effective drug to ameliorate the placental and/or endothelial oxidative stress response in preeclampsia. Furthermore, it may have more beneficial effects when used as a preventative therapy prior to diagnosis with preeclampsia, as opposed to an adjunct treatment in those with established disease. Following promising results from in vitro and early phase clinical trials, a randomized controlled trial would be a suitable study design to answer this research question. The population of interest involves women attending the study hospital for antenatal care and delivery. The intervention involves randomization to oral melatonin tablets 10 mg nocte or identical placebo tablet from recruitment until delivery. Randomization is achieved using computational random allocation, and both participants and researchers will be blinded to the intervention given. Calculation of the sample size takes into account that the incidence of preeclampsia is 5% in the population of interest. Side effects: any side effects or adverse events related to the intervention, intervention stopped due to side effects. Small for gestational age: defined as growth below the 10th centile or lowest centile reported. Apgar score at 5 min: low (less than 7) and very low (less than 4) or lowest reported. Neonatal morbidity: respiratory distress syndrome, chronic lung disease, sepsis, necrotizing enterocolitis, retinopathy of prematurity, and intraventricular hemorrhage. Use of hospital resources: admission to neonatal intensive care unit and duration of hospital stay after delivery. Continuous outcome measures are analyzed by linear regression with robust standard errors. Where necessary to achieve convergence, odds ratios may be considered rather than risk ratios. Caritis S, Sibai B, Hauth J, Lindheimer M, VanDorsten P, Klebanoff M, Thom E, Landon M, Paul R, Miodovnik M, Meis P, Thurnau G, Dombrowski M, McNellis D, Roberts J (1998) Predictors of pre-eclampsia in women at high risk. Rey E, Couturier A (1994) the prognosis of pregnancy in women with chronic hypertension. Iliadis S, Papageorgiou G (2012) Oxidative stress, preeclampsia and cardiovascular disease. Meher S, Duley L (2007) Nitric oxide for preventing pre-eclampsia and its complications. It can affect practically all organ systems, though the organs involved and the degree of dysfunction will vary markedly between patients. Sepsis is now officially defined as a dysregulated host response to an infection, causing life-threatening organ dysfunction [1]. This new definition, and accompanying clinical criteria, will hopefully provide a stronger, more consistent base to better inform incidence, outcomes and research. The nature of sepsis is extremely complex, and the disease course can differ markedly between patients. Diagnosis often relies upon clinician gestalt as definitive microbiological evidence of a precipitating infection is often absent. This is, in large part, due to a highly variable biological phenotype, even in patients presenting with similar clinical features. On a more positive note, our understanding of sepsis has profoundly increased, and better diagnostics are being developed to aid identification and target the dosing and timing of therapeutic interventions.
Cheap isordil 10mg with amex
Random migration across a 2D surface (chemokinesis) does not rely on the response to a directional stimulus (chemotaxis) but occurs in response to cues such as planar cell polarity and chemorepulsive signals from intercellular junctions [25] symptoms uric acid cheap 10 mg isordil amex. The most cost-effective chemokinesis assay is the scratch assay, which is performed in culture plates, meaning it can be easily adapted for large-scale analyses [19, 24]. Cell culture medium: the formulation is dependent on the cell line being cultured for the experiment. This process incorporates the movement of cells due to environmental stimuli (migration) as well as adhesion and degradation of the surrounding extracellular matrix [25]. Matrigel: Pipette 3 mL of Matrigel (stock solution 10 mg/mL; see Note 4) into a 10 mL tube containing 7 mL of serum-free culture medium to make a 3 mg/mL working solution (see Notes 5 and 6). Adhesion is closely linked with migration and invasion and is mediated by integrins (dimers of and subunits), cellular adhesion molecules, and proteoglycan receptors. Integrin engagement promotes focal adhesion formation with activation of focal adhesion kinase and recruitment of vinculin to the cytoplasmic tail of the integrin [26]. Signaling cues and deformations of the actin cytoskeleton produced by new focal adhesion formation direct planar cell polarity and ultimately the directionality of migration. One method for assessing adhesion is to examine binding capacity of cells to a variety of extracellular matrix proteins in culture [19]. A final concentration of 10 g/mL (except for vitronectin at 5 g/mL) in autoclaved water is sufficient for most cell lines. Trypan blue will differentiate live cells (clear) that can excrete the dye from dead cells (blue). Place diluted cells in trypan blue into a hemocytometer and count the clear cells in each of the four corner chambers. To calculate cell number, multiply the average count from the four chambers by 104 (as each chamber constitutes only 1/10,000th of a mL) and then by 10 for the dilution factor. Plate sufficient number of replicates (normally two to three) that will provide reliable data at each time point. Plate a standard curve of cells as well to allow for extrapolation of the results. This should be harvested on day 0 and left in fixative until the assay is stained. The next day harvest a time point of each to provide a background reading (time 0 h) that accounts for errors in pipetting and initial cell counts. Discard the wash solution, and fix the cells by pipetting 500 L of 10% (v/v) neutral buffered formalin into each well. Discard the methylene blue solution and carefully wash each well four times with 1 mL of 0. Remove all borate buffer and allow the wells to dry by turning the plate upside down on the bench for a minimum of 1 h (see Note 9). Elute the dye by pipetting 500 L of developing buffer into each well and placing the plate on a rotating platform shaker for 1 min to ensure the cells have lysed and released the methylene blue stain. Comparison of the optical densities from the test wells against the standard curve of cells will provide a means to determine absolute cell number rather than changes in relative absorbance. Grow cells in 6-well plates until 70% confluence is reached (see Note 1) and treat with vehicle or apoptosis-inducing/ inhibiting agents for the appropriate length of time. Gently suspend each cell pellet in 1 mL of solution I (see Note 11) and incubate the cells for 1 h at room temperature. Suspend the pelleted nuclei in the remaining 1 mL of solution and pass through a 70 m nylon mesh into a flow cytometry tube to remove clumps (see Note 13). Propidium iodide has a maximum excitation wavelength of 535 nm and a maximum emission wavelength of 617 nm when bound to nucleic acids. Do not gate the "debris" out of the flow analysis as much of it will represent your apoptotic populations. Apoptotic cells (filled with blue) are present in low levels in normal BeWo cells. As such, this assay can also be used in conjunction with proliferation assays to examine cell cycle blockade. Grow cells in 6-well plates until all wells have simultaneously established a confluent monolayer (see Note 1). Using a P200 pipette tip, make two horizontal and one vertical wound to the monolayer. Carefully wash the wells with 1 mL of culture medium to remove the detached cells. Make sure not to affect the integrity of the cell monolayer as it is important for the success of the assay. Normal cells show peaks for G0/G1 and G2/M (filled with red) with an intervening S-phase (filled with lines). The apoptotic cells appear as a population to the left of the G0/G1 population (filled with blue). BeWo cells grown in full culture medium (a) and under serum starvation conditions (b). Dotted lines in (b) and (c) denote the migrating front of cells in the monolayer in. Photograph the wounds immediately after creating them to establish a 0 h time point and again in the same position 24 h and 48 h post wounding. Photographing exactly the same field at 0 h and at the end of the assay is imperative to the success of the assay. Carefully pipette 3 mL of culture medium into each well taking care not to damage the Matrigel that you have just overlaid the cells with. Pipette solution over the monolayer to detach cells and add an equal volume of growth media. Incubate the cells for 30 min in a humidified cell culture incubator (see Note 18). Fix the cells by gently pipetting 500 L of 10% (v/v) neutral buffered formalin into each well and incubating for 10 min at room temperature as described in Subheading 3. Determine the number of cells that adhered to each extracellular matrix protein by staining with methylene blue as described in Subheading 3. It is suggested that proliferation assays are performed in 12-well tissue cultured-treated plates, apoptosis, migration, and invasion in 6-well plates and adhesion assays in 24-well plates. The volume of culture medium specified is specific to the size of the tissue culture plates. The minimum recommended Matrigel concentration to form a gel is 3 mg/mL, but the range of 1. Optimization may be required as individual cell lines may have a different response to the stiffness of the gel and have different abilities to produce matrix-degrading enzymes. The neutral buffered formalin can remain on the cells for up to 72 h if required depending on the length of time proliferation is being measured to allow for combined processing once all time points have been completed. The borate buffer should be nearly colorless before the remaining steps can be performed. Pay special attention to remove any methylene blue solution from the walls of each well, which may otherwise contaminate the final eluate and introduce errors into the assay.

Generic 10mg isordil with mastercard
Stress signals are neurosensory medications hair loss order line isordil, blood-borne, or mediated through limbic pathways. The response to stress varies according to the nature, duration, and intensity of the 72 N. The response to life-threatening stress is usually divided into three phases: an acute phase, an established organ dysfunction phase, and a phase of recovery. The synthesis and liberation of these hormones is aimed at maintaining an adequate blood volume, cardiac output, and tissue oxygenation as well as mobilizing reserves for the immediate production of energy. At the same time, nonessential functions such as growth or the reproductive functions are suspended. Critical illness is also associated with insulin resistance, where normal concentrations of insulin are unable to correctly regulate blood glucose levels. This state is partly explained by the effect of cytokines on insulin resistance as well as by increased gluconeogenesis. Sometime after the acute phase, during the established organ dysfunction phase, the hormonal profile alters substantially. Some endocrine changes seem to be adaptive, such as the low T3 syndrome, which may play a role in reducing energy requirements. Low T3 syndrome associates a decrease in the concentration of the T3 due to a decrease of peripheral conversion of T4 to T3 as well as an increased concentration of rT3, an inactive form of T3. These endocrine changes are somewhat induced by hormonal modifications observed during the acute phase. The recovery phase is an anabolic phase occurring up to 2 months after resolution of the acute inflammatory phase. Myocardial depression, defined by a low left ventricular ejection fraction, may occur in up to 50% of cases of septic shock [12]. Myocardial depression may occur through multiple pathways, including autonomic dysregulation, metabolic changes, mitochondrial dysfunction, as well as the consequence of increased catecholamine concentrations and possibly microvascular dysfunction [13]. Adrenergic stimulation of 5 the Endocrine System in Sepsis 73 an already failing heart increases the cardiac work and consumption of oxygen. Heart rate variability, which offers an insight into the vagal to sympathetic balance, is impaired during sepsis and may be associated with an unfavorable outcome [14, 15]. Catecholamines may promote bacterial growth and virulence, while at the same time negatively affecting the efficacy and survival of immune cells [16, 17]. Adrenergic stimulation favors insulin resistance and the associated hyperglycemia. This condition is also coined as critical illness-related corticosteroid insufficiency and may in the severest forms of sepsis affect up to 60% of patients [26, 27]. One of the most well-known causes of altered steroidogenesis occurs after necrosis or hemorrhage of both adrenal glands, also known as the Waterhouse-Friderichsen syndrome [28, 29]. Altered steroidogenesis may occur without any structural damage being done to the adrenal glands. Since cortisol storage in the adrenals is limited, adequate hormonal response to stress relies on de novo cortisol synthesis. Approximately 50% of septic shock patients exhibit decreased cortisol synthesis as well as an inadequate response to the administration of metyrapone [26]. Reduced concentration of cortisol carriers leads to increased plasma concentration of free cortisol. One of the physiological means by which patients seek to withstand severe illness might be by reducing cortisol clearance from plasma, thereby diminishing cortisol inactivation [35]. There is a general agreement that corticosteroids improve shock, organ dysfunction, and length of hospital stay. Their effects on survival and on the risk of secondary infections remain controversial. Corticosteroids participate in restoring effective blood volume, through activation of mineralocorticoid receptors in the kidney leading to sodium retention. A systematic review included the findings of 12 trials reporting the effects of corticosteroids on shock reversal by 1 week to be 1. Corticosteroids may attenuate sepsis-associated brain dysfunction by preventing a breakdown of the blood-brain barrier [48]. Corticosteroids skew T cells toward a Th2 profile, favoring the production of anti-inflammatory cytokines. Most animal models of sepsis found the administration of corticosteroids to be associated with survival benefits [49]. Current international guidelines recommend restricting the use of hydrocortisone to vasopressor-dependent septic shock [27, 50]. Vasopressin supplementation failed to improve mortality in a large multicenter randomized trial [52]. A recent trial found no improvement in the number of kidney failure-free days when comparing norepinephrine to vasopressin in septic shock, although the requirement for renal replacement therapy was lower in the vasopressin group [53]. Several trials sought to determine whether controlling blood glucose levels was associated with a better outcome. A German multicenter study, comparing intensive insulin therapy to conventional treatment, was conducted in severe sepsis. This trial was stopped prematurely because patients in the intensive therapy group suffered from more episodes of hypoglycemia [54]. Mortality rates did not differ between the intensive insulin and the conventional treatment arm although there were significantly more episodes of hypoglycemia in the intensive treatment arm. Current guidelines recommend the administration of insulin in order to control hyperglycemia during severe sepsis or septic shock aiming at obtaining a target blood glucose <180 mg/dL [50]. These modifications may be considered adaptive, aimed at sparing energy during a stressful period. There was no effect on the severity of acute renal failure, and mortality rates were 43% in T4-treated 76 N. The administration of T3 to patients undergoing coronary artery bypass surgery resulted in an increased cardiac output and lowered systemic vascular resistance without any effect on patient-centered outcome [59]. Data on other subgroups of patients and on patient-centered outcomes are still scarce. Overall the only endocrine condition during sepsis which is assessable to treatment is critical illness-related corticosteroid insufficiency which can be treated in the event of septic shock with hydrocortisone (iv bolus of 50 mg q6) combined to fludrocortisone (oral dose of 50 g per day) given for 7 days. Lehninger principles of biochemistry (9781429234146) Macmillan Learning [Internet]. Regulation of insulin synthesis and secretion and pancreatic Beta-cell dysfunction in diabetes. Interplay of somatostatin and growth hormone-releasing hormone in genesis of episodic growth hormone secretion. Experimental human endotoxemia increases cardiac regularity: results from a prospective, randomized, crossover trial. Stimulation of Staphylococcus epidermidis growth and biofilm formation by catecholamine inotropes. Epinephrine inhibits tumor necrosis factor-alpha and potentiates interleukin 10 production during human endotoxemia. Infusion of the betaadrenergic blocker esmolol attenuates myocardial dysfunction in septic rats. Effects of esmolol on systemic and pulmonary hemodynamics and on oxygenation in pigs with hypodynamic endotoxin shock. Polito A, Lorin de la Grandmaison G, Mansart A, Louiset E, Lefebvre H, Sharshar T, et al. Gilibert S, Galle-Treger L, Moreau M, Saint-Charles F, Costa S, Ballaire R, et al. Adrenocortical scavenger receptor class B type I deficiency exacerbates endotoxic shock and precipitates sepsis-induced mortality in mice. Single induction dose of etomidate versus other induction agents for endotracheal intubation in critically ill patients. Patterns of corticosteroid-binding globulin and the free cortisol index during septic shock and multitrauma. A role for corticosteroid-binding globulin in delivery of cortisol to activated neutrophils*. Local regulation of glucocorticoid activity in sites of inflammation: insights from the study of tuberculosis. Modulation of glucocorticoid receptor expression, inflammation, and cell apoptosis in septic guinea pig lungs using methylprednisolone.
Discount 10mg isordil with visa
Thromboelastography as a better indicator of hypercoagulable state after injury than prothrombin time or activated partial thromboplastin time medicine 44291 buy cheap isordil line. Utility of thromboelastography and/or thromboelastometry in adults with sepsis: a systematic review. Thromboelastometry for the assessment of coagulation abnormalities in early and established adult sepsis: a prospective cohort study. Application of the international normalized ratio in the scoring system for disseminated intravascular coagulation. Prospective validation of the international society of thrombosis and haemostasis scoring system for disseminated intravascular coagulation. The scoring system of the scientific and standardisation committee on disseminated intravascular coagulation of the International Society on thrombosis and haemostasis: a five year overview. Treatment effects of drotrecogin alfa (activated) in patients with severe sepsis with or without overt disseminated intravascular coagulation. Heparin treatment in thrombin-induced disseminated intravascular coagulation in the baboon. Diagnosis and management of disseminated intravascular coagulation: the role of heparin therapy. Prophylactic heparin in patients with severe sepsis treated with drotrecogin alfa (activated). Bioavailability of subcutaneous low-molecular-weight heparin to patients on vasopressors. Treatment effects of high-dose antithrombin without concomitant heparin in patients with severe sepsis with or without disseminated intravascular coagulation. Antithrombin and mortality in severe pneumonia patients with sepsis-associated disseminated intravascular coagulation: an observational nationwide study. Efficacy and bleeding risk of antithrombin supplementation in septic disseminated intravascular coagulation: a secondary survey. Model-based analysis of covariate effects on population pharmacokinetics of thrombomodulin alfa in patients with disseminated intravascular coagulation and normal subjects. Recombinant human soluble thrombomodulin in severe sepsis: a systematic review and meta-analysis. Non-anticoagulant heparin prevents histone-mediated cytotoxicity in vitro and improves survival in sepsis. Tumor necrosis factor-alpha inhibition protects against endotoxin-induced endothelial glycocalyx perturbation. The Endocrine System in Sepsis Nicholas Heming, Sivanthiny Sivanandamoorthy, Paris Meng, and Djillali Annane 5 5. The endocrine system maintains biological homeostasis by regulating water and electrolytes balance, metabolism, growth and development, as well as reproduction. The endocrine system is composed of glands which release hormones in response to nervous or hormonal signals. Hormones are specialized chemical compounds which are delivered through the bloodstream and bind to specialized cellular receptors, thereby modifying the cellular function of target cells. In vertebrates, endocrine glands include the pituitary, pineal, adrenal, thyroid, and parathyroid glands as well as the islets of Langerhans in the pancreas, intestinal mucosa, ovary, and testis. Apart from these specialized glands, hormones may also be produced by organs having a specific physiological role that may also exhibit secondary endocrine functions such as the heart or the kidneys. Protein hormones are usually synthesized on the endoplasmic reticulum as inactive preprohormones which are subsequently cleaved into prohormones and then hormones and N. Pineal gland Locus coeruleus Heart Liver Pancreas Intestines Adrenal gland Kidney Ovary Testis stored in vesicles until needed. Epinephrine and norepinephrine are synthesized and stored in preformed vesicles in the adrenal medulla. There is very little steroid hormone storage; however the cholesterol ester precursors are stored in cytoplasmic vesicles, ready to be rapidly mobilized. Since steroid hormones are lipophilic, steroid hormone synthesis is followed by rapid diffusion into the bloodstream. For instance, the release of catecholamines occurs seconds after a neuronal impulse, and full effect occurs within minutes. Steroids acting through the genomic pathway start having a physiological action several hours after their release into the circulation. By opposition, other hormones such as thyroid or growth hormones are fully effective after several months. Hormone production is controlled through negative feedback mechanisms where, after release of a hormone, products resulting of the cellular action of this hormone inhibit further production of the hormone. Hormone regulatory mechanisms may occur during synthesis (whether during transcription or translation) or at the time of release. For example, before ovulation, stimulation of the anterior pituitary by estrogens induces a brisk increase of luteinizing hormone, which in turn stimulates estrogen production. Hormone secretions also undergo periodic variations, induced by the diurnal cycle, the stage of development, or the onset of senescence. The amino acid tyrosine is the substrate for the biosynthesis of all catecholamines. The terminal step in catecholamine biosynthesis is catalyzed by the phenylethanolamine N-methyltransferase which converts norepinephrine to epinephrine [2]. Catecholamines do not exert negative feedback in order to downregulate its own synthesis. The pituitary gland is divided into two lobes: an anterior lobe (adenohypophysis), derived from an invagination of the oral ectoderm, and a posterior lobe (neurohypophysis), which is an extension of the hypothalamus, originating from the neuroectoderm. Hypothalamic cells are directly connected to the neurohypophysis and secrete releasing hormones in synchronous pulses, into the vessels of the pituitary stalk, which stimulate or inhibit the secretion of adenohypophysis hormones. The posterior pituitary stores and secretes neurohormones such as oxytocin, a peptide hormone produced by the paraventricular nuclei of the hypothalamus and vasopressin. The adrenal medulla is closely connected to the sympathetic system and secretes epinephrine and norepinephrine in response to sympathetic stimulation. Epinephrine and norepinephrine control cardiac output and blood pressure and stimulate glycogenesis. The adrenal cortex produces a different group of hormones called corticosteroids as well as small quantities of androgenic hormones. Corticosteroids are divided into glucocorticoids (cortisol, corticosterone) and mineralocorticoids (aldosterone). Circulating adrenocortical hormones are bound to plasma proteins (cortisol-binding globulin and albumin) and are metabolized in the liver. Aldosterone is produced in response to increased extracellular potassium concentration, while increased sodium concentration in the extracellular fluid decreases the production of aldosterone. Aldosterone promotes reabsorption of sodium and secretion of potassium at the renal tubular epithelial cells, leading to increased extracellular volume. Cortisol stimulates gluconeogenesis and mobilizes proteins and fatty acids for use in stressful situations. Cortisol also has anti-inflammatory effects as well as causes resolution of inflammation. Osmotic or hypovolemic stimuli induce vasopressin to be released into the circulation. The V2 vasopressin receptor is mainly expressed in the ascending loop and collecting duct cells of the kidney. Upon binding of vasopressin, the receptor, through coupled G-proteins, activates the adenylyl cyclase, leading to the expression of the aquaporin water channels, leading to reabsorption of free water [4]. High blood glucose concentration stimulates the beta cells to secrete insulin, whereas a low blood glucose level induces the secretion of glucagon by the pancreatic alpha cells [5]. Thyroid hormone production is composed into 80% of thyroxin (T4) and 20% of triiodothyronine (T3). In peripheral tissue, such as the liver, the less active prohormone T4 is converted to the active T3 and the metabolically inactive reverse T3 (rT3) by deiodinases, in equal quantities. Thyroid hormones are secreted in the bloodstream, where they bind to transport proteins.
Purchase isordil in united states online
Notably treatment 3 nail fungus buy genuine isordil on line, co-inhibitor blockade is associated with improved survival in multiple preclinical models of sepsis. While clinical trials examining co-inhibitory blockade in septic patients are just beginning to enroll patients, immune augmentation represents an attractive strategy in the future for sepsis. Severe sepsis in pre-hospital emergency care: analysis of incidence, care, and outcome. Developing a new definition and assessing new clinical criteria for septic shock: for the third international consensus definitions for sepsis and septic shock (sepsis-3). Application of a framework to assess the usefulness of alternative sepsis criteria. A framework for the development and interpretation of different sepsis definitions and clinical criteria. New definitions for sepsis and septic shock: continuing evolution but with much still to be done. On behalf of the Working Group on SepsisRelated Problems of the European Society of Intensive Care Medicine. Prognostic accuracy of sepsis-3 criteria for in-hospital mortality among patients with suspected infection presenting to the emergency department. Application of the third international consensus definitions for sepsis (sepsis-3) classification: a retrospective population-based cohort study. Intestine-specific deletion of microsomal triglyceride transfer protein increases mortality in aged mice. Intestine-specific Mttp deletion decreases mortality and prevents sepsis-induced intestinal injury in a murine model of Pseudomonas aeruginosa pneumonia. A critical role of leukotriene B4 in neutrophil migration to infectious focus in cecal ligation and puncture sepsis. Developing a clinically feasible personalized medicine approach to pediatric septic shock. Prospective testing and redesign of a temporal biomarker based risk model for patients with septic shock: implications for septic shock biology. The use of enrichment to reduce statistically indeterminate or negative trials in critical care. Long-term quality of life among survivors of severe sepsis: analyses of two international trials. Antimicrobial therapy for patients with severe sepsis and septic shock: an evidence-based review. Rapid diagnosis of infection in the critically Ill, a multicenter study of molecular detection in bloodstream infections, pneumonia, and sterile site infections. Impact of matrix-assisted laser desorption ionization time-of-flight mass spectrometry on the clinical management of patients with Gram-negative bacteremia: a prospective observational study. Impact of rapid organism identification via matrixassisted laser desorption/ionization time-of-flight combined with antimicrobial stewardship team intervention in adult patients with bacteremia and candidemia. Effectiveness of practices to increase timeliness of providing targeted therapy for inpatients with bloodstream infections: a laboratory medicine best practices systematic review and meta-analysis. The effect of molecular rapid diagnostic testing on clinical outcomes in bloodstream infections: a systematic review and metaanalysis. Prediction of sepsis in the intensive care unit with minimal electronic health record data: a machine learning approach. The shift of an intestinal "microbiome" to a "pathobiome" governs the course and outcome of sepsis following surgical injury. Collapse of the microbiome, emergence of the pathobiome, and the immunopathology of sepsis. Critically ill patients demonstrate large interpersonal variation in intestinal microbiota dysregulation: a pilot study. Probiotic and synbiotic therapy in critical illness: a systematic review and meta-analysis. Successful treatment of severe sepsis and diarrhea after vagotomy utilizing fecal microbiota transplantation: a case report. A prospective analysis of lymphocyte phenotype and function over the course of acute sepsis. Iron deficiency anaemia is caused by defective synthesis of haemoglobin, resulting in red cells that are smaller than normal (microcytic) and contain reduced amounts of haemoglobin (hypochromic). Absorption is helped by the presence of other reducing substances, such as hydrochloric acid and ascorbic acid. The body has the capacity to increase its iron absorption in the face of increased demand, for example, in pregnancy, lactation, growth spurts and iron deficiency (Box 1. Once absorbed from the bowel, iron is transported across the mucosal cell to the blood, where it is carried by the protein transferrin to developing red cells in the bone marrow. Iron stores comprise ferritin, a labile and readily accessible source of iron and haemosiderin, an insoluble form found predominantly in macrophages. Low (<76 fl) microcytic red cells Consider: Iron deficiency anaemia Thalassaemia Anaemia of chronic disorders History and physical examination Obvious source of blood loss On examination, several skin, nail and other epithelial changes may be seen in chronic iron deficiency. Atrophy of the skin occurs in about a third of patients and (rarely nowadays) nail changes such as koilonychia (spoon-shaped nails;. Patients may also complain of angular stomatitis, in which painful cracks appear at the angle of the mouth, sometimes accompanied by glossitis. Although uncommon, oesophageal and pharyngeal webs can be a feature of iron deficiency anaemia (consider this in middle aged women presenting with dysphagia). These changes are believed to be due to a reduction in the iron-containing enzymes in the epithelium and gastrointestinal tract. Few of these epithelial changes are seen in modern practice, and they are of limited diagnostic value. Tachycardia and cardiac failure may occur with severe anaemia irrespective of cause and, in such cases, prompt remedial action should be taken. When iron deficiency is confirmed, a full clinical history, including leading questions on possible gastrointestinal blood loss or malabsorption (as in, for example, coeliac disease), should be obtained. Menstrual losses should be assessed and the importance of dietary factors and regular blood donation should not be overlooked. These will confirm the anaemia; recognizing the indices of iron deficiency is usually straightforward (reduced haemoglobin concentration, reduced mean cell volume, reduced mean cell haemoglobin, reduced mean cell haemoglobin concentration) (Table 1. Some modern analysers will determine the percentage of hypochromic red cells, which may be high before the anaemia develops (it is worth noting that a reduction in haemoglobin concentration is a late feature of iron deficiency). Difficulties in diagnosis arise when more than one type of anaemia is present, for example, iron deficiency and folate deficiency in malabsorption, in a population where thalassaemia is present, or in pregnancy, when the interpretation of red cell indices may be difficult. Haematinic assays will demonstrate reduced serum ferritin concentration in straightforward iron deficiency. As an acute phase protein, however, the serum ferritin concentration may be normal or even raised in inflammatory or malignant disease. A prime example of this is found in rheumatoid disease, in which active disease may result in a spuriously raised serum ferritin concentration masking an underlying iron deficiency caused by gastrointestinal bleeding after non-steroidal analgesic treatment. There may also be confusion in liver disease, as the liver contains stores of ferritin that are released after hepatocellular damage, leading to raised serum ferritin concentrations. In cases where ferritin estimation is likely to be misleading, the soluble transferrin receptor (sTfR) assay may aid the diagnosis. Transferrin receptors are found on the surface of red cells in greater numbers in iron deficiency; a proportion of receptors is shed into the plasma and can be measured using commercial kits. Unlike serum ferritin, the level of sTfR does not rise in inflammatory disorders, and Table 1. Diagnostic bone marrow sampling is seldom performed in simple iron deficiency, but, if the diagnosis is in doubt, a marrow aspirate may be carried out to demonstrate absent bone marrow stores. When iron deficiency has been diagnosed, the underlying cause should be investigated and treated.
Purchase isordil 10mg free shipping
Patients are seen at a fixed interval so that comparison with baseline photographs can be made and lack of progression confirmed treatment definition isordil 10mg sale. This approach is specifically restricted to patients whose lesions have been diagnosed as probably benign, but in whom there is a small degree of uncertainty. Total body cutaneous photography the complete skin is photographed, and patients are clinically examined or re-photographed at regular intervals so that comparison can be made with baseline photographs for any new or changing lesions, which are then scrutinized more carefully. This sort of surveillance has been reported to increase early detection of melanoma in individuals at high risk who have large numbers Tools to improve in vivo diagnosis of melanoma In current clinical practice Naked eye Individual lesion / total body photography Magnifying glass Dermatoscopy In clinical research: Computer-aided dermatoscopy Multispectral imaging High-frequency ultrasound Optical coherence tomography Confocal scanning laser microscopy (a) Increasing magnification (b). There are several melanoma-specific features, including asymmetry, atypical pigment network, blue-grey veil and regression that become apparent on dermatoscopic examination. Several morphological features become apparent, including pigment architecture and blood vessel arrangement. Dermatoscopy is particularly useful at identifying certain benign lesions such as seborrhoeic keratosis and haemangioma, which have specific dermatoscopic features. Differentiating benign melanocytic naevi from melanoma is harder, and requires considerable training and experience. Diagnosing skin malignancy: assessment of predictive clinical criteria and risk factors. Tools in clinical research Several other imaging modalities that offer higher magnifications at higher resolutions are being investigated. The first site of metastasis is loco-regional in two-thirds of patients and distant in the remaining third. Immunotherapy and targeted molecular therapy may lead to improved therapeutic responses in the future. Metastatic melanoma responds poorly to chemotherapy and radiotherapy, although surgical treatment of local and lymph node metastases may still be curative. Management Primary (diagnostic) excision A lesion suspected of being melanoma must be excised completely for histopathological analysis. Punch or shave biopsies should be avoided because of possible sampling error and distortion of histological architecture compromising pathological diagnosis. A specialist dermatopathologist must report suspected melanoma, and correlation between clinical and histological findings is essential if misdiagnosis is to be avoided. This is the distance from the granular layer of the epidermis to the lower most invasive cell. Wider excision is usually curative in patients with thin melanoma (Breslow thickness < 1 mm). It predicts the risk of metastasis, and therefore the 5-year survival rate of melanoma. This is central to the successful management of melanoma, because it minimizes the risk of local and regional lymph node metastasis. For melanoma between 1 and 2 mm in thickness, margins of 2 cm are probably adequate. Most wider excision surgery takes place under local anaesthetic in the ambulatory care setting. These characteristics are used to define the American Joint Committee on Cancer staging system (Table 10. Adjuvant treatment Adjuvant treatment should eradicate micrometastases before they cause disease. Interferon-alfa, a proinflammatory cytokine, is the only licensed adjuvant treatment for melanoma, but its effect is limited to delaying metastases in some patients. Breaking the news the outlook varies enormously between patients, depending on tumour thickness and ulceration. It is therefore important to individualize prognosis when breaking bad news and to remain realistic while providing hope, reassurance and support. For example, in situ melanoma (where malignant melanocytes are confined to the epidermis) does not carry a risk of metastasis and so the patient would be strongly reassured. On the other hand, a 4-mm thick ulcerated melanoma carries a 5-year survival rate of 45%. Consequently, a specialist nurse is a vital contact for further support, advice and counselling, and should be involved as early on in the process as possible, preferably from the time the bad news is broken. The hyfrecator emits a high-frequency current producing a spark at the tip of the electrode, which burns tissue superficially. Psychosocial aspects the diagnosis of melanoma can have significant psychosocial impact, particularly because there is a widespread awareness among the public that it may be lethal. Psychosocial distress impairs ability to cope, quality of life and possibly even survival. Providing general information on coping strategies and cognitive behavioural therapy (such as relaxation training) to patients with high levels of psychosocial distress improves quality of life and general health status of melanoma patients, underpinning the need for psychological support following diagnosis. Metastatic melanoma Eighty per cent of metastases develop within 5 years of diagnosis. Surgical excision is the mainstay of treatment for metastatic disease, as systemic chemotherapy and immunotherapy have little effect. Lympho-oedema is a common post-operative complication and requires compression hosiery. Loco-regional metastases Satellite and in-transit metastases present as papules and nodules in the skin and subcutaneous tissues between the site of the original melanoma and the regional lymph nodes. Metastasis to the regional lymph nodes presents with palpable lymphadenopathy and is treated by lymph node block dissection. The prognosis from regional lymph node metastasis depends on the number of lymph nodes involved. For example, a patient with a non-ulcerated primary melanoma and a single metastatic lymph node has almost a 60% chance of cure. Surgical excision of distant metastases is central to effective palliative care, and improves survival for isolated pulmonary, cerebral or gastrointestinal metastases. Melanoma is relatively resistant to conventional chemotherapy with dacarbazine, which has been used for > 30 years and yields, at best, only a 15% response rate. Patients should have access to palliative care teams for symptomatic control of advanced disease. Follow-up Follow-up for patients with melanoma enables earlier detection of metastatic disease and of new skin cancers, so that prompt, potentially curative, surgical intervention can be provided (Box 10. Investigations at follow-up visits are usually guided by the history and physical examination. Future directions New chemotherapy agents introduced over the last 30 years have not shown any benefit over dacarbazine, even in multiple combinations, underlining the highly chemoresistant nature of melanoma. The complex molecular basis for this is becoming more apparent, and several new molecular targets have been identified with targeted agents undergoing pre-clinical and early clinical studies (Table 10. The observation that melanoma can, on rare occasions, spontaneously regress has led to significant interest in immunotherapy, Table 10. Clinical trials the inefficacy of systemic therapies for melanoma makes it important for patients at high risk of metastasis and those with advanced melanoma to be enrolled into well-designed multicentre clinical trials.