Generic lasix 40 mg
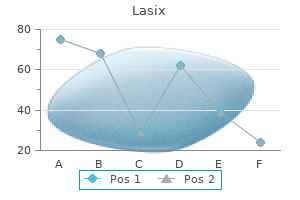
The blow to the eye that causes us to "see" a flash of light is another example of labeled line coding pulse pressure and stroke volume relationship order 100 mg lasix mastercard. The sensory regions of the cerebrum are highly organized with respect to incoming signals, and input from adjacent sensory receptors is processed in adjacent regions of the cortex. This arrangement preserves the topographical organization of receptors on the skin, eye, or other regions in the processing centers of the brain. For example, touch receptors in the hand project to a specific area of the cerebral cortex. Experimental stimulation of that area of the cortex during brain surgery is interpreted as a touch to the hand, even though there is no contact. Similarly, one type of the phantom limb pain reported by amputees occurs when secondary sensory neurons in the spinal cord become hyperactive, resulting in the sensation of pain in a limb that is no longer there. Neurons in the ears are sensitive to different frequencies of sound, but they have no receptive fields and their activation provides no information about the location of the sound. A sound originating directly in front of a person reaches both ears simultaneously. A sound originating on one side reaches the closer ear several milliseconds before it reaches the other ear. Lateral inhibition, which increases the contrast between activated receptive fields and their inactive neighbors, is another way of isolating the location of a stimulus. A pin pushing on the skin activates three primary sensory neurons, each of which releases neurotransmitters onto its corresponding secondary neuron. The secondary neuron closest to the stimulus (neuron B) suppresses the response of the secondary neurons lateral to it. The inhibition of neurons farther from the stimulus enhances the contrast between the center and the sides of the receptive field, making the sensation more easily localized. Intensity of the Stimulus the intensity of a stimulus cannot be directly calculated from a single sensory neuron action potential because a single action potential is "all-or-none. Population coding for intensity occurs because the threshold for the preferred stimulus is not the same for all receptors. Only the most sensitive receptors (those with the lowest thresholds) respond to a low-intensity stimulus. Once stimulus intensity exceeds threshold, the primary sensory neuron begins to fire action potentials. Duration of the Stimulus the duration of a stimulus is coded by the duration of action potentials in the sensory neuron. In general, a longer stimulus generates a longer series of action potentials in the primary sensory neuron. Receptors fall into one of two classes, depending on how they adapt to continuous stimulation. Tonic receptors are slowly adapting receptors that fire rapidly when first activated, then slow and maintain their firing Left Signals coming from the right reach the brain first. The responses of primary sensory neurons A, B, and C are proportional to the intensity of the stimulus in each receptor field. Secondary sensory neuron B inhibits secondary neurons A and C, creating greater contrast between B and its neighbors. Pressure-sensitive baroreceptors, irritant receptors, and some tactile receptors and proprioceptors fall into this category. In general, the stimuli that activate tonic receptors are parameters that must be monitored continuously by the body. Once a stimulus reaches a steady intensity, phasic receptors adapt to the new steady state and turn off. This type of response allows the body to ignore information that has been evaluated and found not to threaten homeostasis or well-being. For example, you can smell your cologne when you put it on in the morning, but as the day goes on your olfactory receptors adapt and are no longer stimulated by the cologne molecules. Adaptation of phasic receptors allows us to filter out extraneous sensory information and concentrate on what is new, different, or essential. In general, once adaptation of a phasic receptor has occurred, the only way to create a new signal is to either increase the intensity of the excitatory stimulus or remove the stimulus entirely and allow the receptor to reset. The molecular mechanism for sensory receptor adaptation depends on the receptor type. In some receptors, K+ channels in the receptor membrane open, causing the membrane to repolarize and stopping the signal. Accessory structures may also decrease the amount of stimulus reaching the receptor. In the ear, for example, tiny muscles contract and dampen the vibration of small bones in response to loud noises, thus decreasing the sound signal before it reaches auditory receptors. To summarize, the specificity of sensory pathways is established in several ways: 1. Stimulus location and modality are coded according to which receptors are activated or (in the case of sound) by the timing of receptor activation. Each sensory pathway projects to a specific region of the cerebral cortex dedicated to a particular receptive field. Receptor activation triggers action potentials in the associated primary sensory neuron. Primary sensory neurons in the peripheral nervous system are pseudounipolar neurons [p. What is the adaptive significance of irritant receptors that are tonic instead of phasic Stimulus Stimulus (b) Phasic receptors rapidly adapt to a constant stimulus and turn off. Stimulus Receptor Receptor potential Axon of sensory neuron Action potentials in sensory neuron Time Time Neurons associated with receptors for nociception, temperature, and coarse touch synapse onto their secondary neurons shortly after entering the spinal cord. In contrast, most fine touch, vibration, and proprioceptive neurons have very long axons that project up the spinal cord all the way to the medulla. All secondary sensory neurons cross the midline of the body at some point, so that sensations from the left side of the body are processed in the right hemisphere of the brain and vice versa. The secondary neurons for nociception, temperature, and coarse touch cross the midline in the spinal cord, then ascend to the brain. Fine touch, vibration, and proprioceptive neurons cross the midline in the medulla. In the thalamus, all secondary sensory neurons synapse onto tertiary sensory neurons, which in turn project to the somatosensory region of the cerebral cortex. In addition, many sensory pathways send branches to the cerebellum so that it can use the information to coordinate balance and movement. Within the cortical region for a particular body part, columns of neurons are devoted to particular types of receptors. For example, a cortical column activated by cold receptors in the left hand may be found next to a column activated by pressure receptors in the skin of the left hand. This columnar arrangement creates a highly organized structure that maintains the association between specific receptors and the sensory modality they transmit. Some of the most interesting research about the somatosensory cortex has been done on patients during brain surgery for epilepsy. Because the brain has no pain fibers, this type of surgery can be performed with the patient awake under local anesthesia. The surgeon stimulates a particular region of the brain and asks the patient about sensations that occur. The ability of the patient to communicate with the surgeon during this process has expanded our knowledge of brain regions tremendously. Experiments can also be done on nonhuman animals by stimulating peripheral receptors and monitoring electrical activity in the cortex. We have learned from these experiments that the more sensitive a region of the body is to touch and other stimuli, the larger the corresponding region in the cortex. If a particular body part is used more extensively, its topographical region in the cortex will expand. For example, people who are visually handicapped and learn to read Braille with their fingertips develop an enlarged region of the somatosensory cortex devoted to the fingertips. In contrast, if a person loses a finger or limb, the portion of the somatosensory cortex devoted to the missing structure begins to be taken over by sensory fields of adjacent structures. Reorganization of the somatosensory cortex "map" is an example of the remarkable plasticity [p. Unfortunately, sometimes the reorganization is not perfect and can result in sensory sensations, including pain, that the brain interprets as being located in the missing limb (phantom limb pain).
Cheap lasix 40mg overnight delivery
The activated lymphocytes undergo clonal expansion hypertension management buy lasix toronto, with cell division creating new effector cells. Some of these effector cells differentiate into plasma cells, which lose the B cell receptors on their membranes. Plasma cells synthesize and secrete antibody molecules to create humoral immunity, the soluble antibodies of the plasma. Antibody production in the primary immune response is slower and lower in magnitude because the body has not encountered the antigen previously. After the pathogen has been successfully repulsed, most of the short-lived plasma cells die off-it could be dangerous to have them secreting a lot of antibody after the antigen is gone. A few Antigen-Presenting Cells Bridge Innate and Adaptive Responses Digestion of pathogens by phagocytes is a critical step that links the nonspecific innate immune response to antigen-specific adaptive responses. Dendritic cells with antigen migrate to secondary lymphoid tissues, such as lymph nodes, where they present the antigen to lymphocytes to activate them. Some of the activated B cells become memory B cells that also stay alive, waiting for the next exposure to the same antigen. Clonal expansion is enhanced by lymphocytes that carry a molecular memory of the first exposure to the antigen, so antibody production begins sooner, goes faster (at incredible rates, estimated to be as high as 2000 molecules per second! Why should the parent be particularly alert when the child is stung a second time In most instances, the antibody binds first to the antigen, forming an antibody-antigen complex, also known as an immune complex. This creates clumping of antigens, which facilitates their recognition and destruction by the immune system. Additional functions of antibodies include the following: 2 Inactivate bacterial toxins. Natural immunity to diphtheria occurs when the host produces antibodies that disable the toxin. As mentioned earlier, some bacteria are not recognized as pathogens by phagocytes. Coating the bacteria with antibody allows phagocyte receptors to bind the stem end of the antibody, triggering phagocytosis of the entire immune complex. One example is during infection by Corynebacterium diphtheria, the bacterium that causes diphtheria, an upper respiratory infection. Plasma cells Clonal expansion Short-lived effector cells carry out the immediate response. These proteins assist with the innate response, including mast cell degranulation. Once antigen binds to B cell recep- tors, B cells activate and differentiate into plasma cells that secrete more antibodies. Active and Passive Immunity Adaptive immunity due to antibodies can be subdivided into passive immunity and active immunity. The transfer of antibodies from mother to fetus across the placenta is one example. Travelers going abroad may be injected with gamma globulin (antibodies extracted from donated human plasma), but this passive immunity lasts only about three months as the injected proteins degrade and are cleared from the circulation. Active immunity occurs when the body is exposed to a pathogen and produces its own antibodies, as just discussed. The existence of a secondary immune response is what allows vaccinations to be an effective protection from disease. A vaccine contains an altered pathogen that no longer harms the host but that can be recognized as foreign by immune cells. The altered pathogen in the vaccine triggers creation of memory cells specific to that particular pathogen. If a vaccinated person is later infected by the pathogen, the memory cells produce a stronger and more rapid secondary immune response. For example, to develop a vaccine against Corynebacterium diphtheria, researchers created an inactivated C. When administered to a person, the vaccine triggers antibody production without causing any symptoms of the disease. Trigger degranulation Antibody-dependent cell-mediated cytotoxicity Kills pathogen Releases histamine and cytokines Bacteria 2. Act as opsonins to tag antigens for phagocytosis Activated complement Pathogen Antibody molecules 1 Encapsulated bacteria are coated with antibody. Activate B lymphocytes Secrete antibodies Plasma cells 2 Antibodies bind to phagocyte receptors, triggering phagocytosis. Cytotoxic T Cells the role of cytotoxic T lymphocytes is to defend the body against intracellular pathogens. Once a pathogen gets inside a host cell, antibodies are no longer effective because they can only bind to soluble or exposed antigens. Although this destruction may seem to be an extreme response, it prevents the reproduction of intracellular invaders such as viruses, some parasites, and some bacteria. First, they can release a cytotoxic pore-forming molecule called perforin along with granzymes, enzymes related to the digestive enzymes trypsin and chymotrypsin. When granzymes enter the target cell through perforin channels, they activate an enzyme cascade that induces the cell to commit suicide (apoptosis). Alternatively, cytotoxic T cells can instruct target cells to undergo apoptosis by activating Fas, a "death receptor" protein on the target cell membrane that is linked to the apoptosis enzyme cascade. Treg activation suppresses immune cell function to help prevent excessive immune responses. The details depend on the particular challenge, but the basic pattern is the same. The innate response starts first, and it is reinforced by the more specific adaptive response. The two pathways are interconnected, so cooperation and communication are essential. There they may cause an inflammatory T lymphocytes have T cell receptors into their cell membranes. If bacteria enter the lymph, infectionfighting takes place in lymph nodes as well. Products of the complement cascade: act as opsonins to enhance phagocytosis, cause degranulation of mast cells with histamine release that promotes inflammation, are chemotaxins that attract leukocytes from the circulation, and form membrane attack complex molecules that insert themselves into the wall of unencapsulated bacteria, creating an influx of ions and water that lyses the bacteria. If the bacteria are encapsulated, opsonins must coat the capsule before the bacteria can be identified and ingested by phagocytes. In this figure, we have assumed prior exposure to the virus and the presence of preexisting antibodies in the circulation. Antibodies from longlived plasma cells can play an important defensive role in the early extracellular stages of a viral infection. However, once the virus is inside host cells, antibodies are no longer as effective. Macrophages also secrete a variety of cytokines to initiate the inflammatory response. They produce interferon-a, which causes host cells to make antiviral proteins that keep viruses 24 from replicating. If antibodies against the bacteria are already present, they enhance the innate response by acting as opsonins and neutralizing bacterial toxins. This second exposure to the virus activates the memory cells and promotes development of plasma cells, resulting in additional antibody production. Once the bacteria are removed by the immune response, the injured site is repaired under the control of growth factors and other cytokines. Perforin molecules insert pores into the host cell membrane so that granzymes can enter the cell, inducing it to commit suicide and undergo apoptosis. Destruction of infected host cells is a key step in halting the replication of invading viruses. Viral Infections Require Intracellular Defense What happens when viruses invade the body
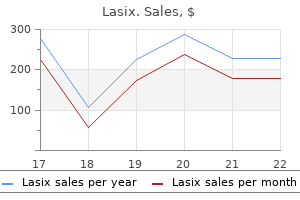
40 mg lasix mastercard
The most important metabolic effect of cortisol is its protective effect against hypoglycemia heart attack sam tsui discount lasix online visa. When blood glucose decreases, the normal response is secretion of pancreatic glucagon, which promotes gluconeogenesis and glycogen breakdown [p. In the absence of cortisol, however, glucagon is unable to respond adequately to a hypoglycemic challenge. Because cortisol is required for full glucagon and catecholamine activity, it is said to have a permissive effect on those hormones [p. Cortisol receptors are found in every tissue of the body, but for many targets we do not fully understand the physiological actions of cortisol. However, we can speculate on these actions based on tissue responses to high levels (pharmacological doses) of cortisol administered for therapeutic reasons or associated with hypersecretion. Some glucose produced in the liver is released into the blood, and the rest is stored as glycogen. Cortisol causes the breakdown of skeletal muscle proteins to provide a substrate for gluconeogenesis. Cortisol enhances lipolysis so that fatty acids are available to peripheral tissues for energy use. In addition, cortisol is catabolic in bone tissue, causing net breakdown of calcified bone matrix. As a result, people who take therapeutic cortisol for extended periods have a higher-than-normal incidence of broken bones. States of cortisol excess or deficiency cause mood changes as well as memory and learning alterations. You are mountain-biking in Canada and encounter a bear, which chases you up a tree. The illegal use of anabolic steroids by bodybuilders and athletes periodically receives much attention. Iatrogenic (physician-caused) hypercortisolism occurs secondary to cortisol therapy for some other condition. In some of these inherited disorders, excess androgens are secreted because substrate that cannot be made into cortisol or aldosterone is converted to androgens. In newborn girls, excess androgens cause masculinization of the external genitalia, a condition called adrenogenital syndrome. Cortisol Is a Useful Therapeutic Drug Cortisol suppresses the immune system by preventing cytokine release and antibody production by white blood cells. It also inhibits the inflammatory response by decreasing leukocyte mobility and migration. These immunosuppressant effects of cortisol make it a useful drug for treating a variety of conditions, including bee stings, poison ivy, and pollen allergies. However, glucocorticoids also have potentially serious side effects because of their metabolic actions. For this reason, it is essential that patients taking steroids taper their dose gradually, giving the pituitary and adrenal glands a chance to recover, rather than stopping the drug abruptly. It can arise from hormone-secreting tumors or from exogenous administration of the hormone. Most signs of hypercortisolism can be predicted from the normal actions of the hormone. Paradoxically, excess cortisol deposits extra fat in the trunk and face, perhaps in part because of increased appetite and food intake. Both peptides are now known to belong to larger families of related molecules, with multiple receptor types found in numerous tissues. Melanocytes contain pigments called melanins that influence skin color in humans and coat color in mice. Of more interest to physiologists, however, is the fact that agouti mice overeat and develop adult-onset obesity, hyperglycemia, and insulin resistance-in other words, these mice are a model for obesity-related type 2 diabetes. The link between melanocortin receptors, eating behavior, and diabetes has opened up a new area of research on treatments to prevent type 2 diabetes. The thyroid gland has two distinct endocrine cell types: C ("clear") cells, which secrete a calcium-regulating hormone called calcitonin, and follicular cells, which secrete thyroid hormone. Thyroid Hormones Contain Iodine Thyroid hormones, like glucocorticoids, have long-term effects on metabolism. Unlike glucocorticoids, however, thyroid hormones are not essential for life: adults can live, although not comfortably, without thyroid hormone or a thyroid gland. Thyroid hormones are essential for normal growth and development in children, however, and infants born with thyroid deficiency will be developmentally delayed unless treated promptly. Because of the importance of thyroid hormones in children, the United States and Canada test all newborns for thyroid deficiency. Protein synthesis 2 Enzymes, Thyroglobulin T3 T4 - Na + T3 T4 6 T3 T4 Free T3 and T4 enter the circulation. Tyrosine Follicular cells Pendrin 4 Thyroglobulin is taken back into the cell in vesicles. Calcium-based kidney stones occur when calcium phosphate or calcium oxalate crystals form and aggregate with organic material in the lumen of the kidney tubule. Use what you have learned about filtration at the glomerulus to speculate on why some plasma Ca 2+ cannot filter [p. The hollow center of each follicle is filled with a sticky glycoprotein mixture called colloid. These proteins are packaged into vesicles, then secreted into the center of the follicle. As I- enters the colloid, the enzyme thyroid peroxidase removes an electron from the iodide ion and adds iodine to tyrosine on the thyroglobulin molecule 3. There intracellular enzymes free the hormones T3 and T4 from the thyroglobulin protein 5. For many years, scientists believed that the lipophilic nature of T3 and T4 allowed the hormones to diffuse out of the follicular cells and into the plasma, but current evidence indicates that the thyroid hormones also move across cell membranes by protein carriers 6. T3 and T4 have limited solubility in plasma because they are lipophilic molecules. Target tissue uptake transporters for thyroid hormones vary from tissue to tissue. For years it was thought that T4 was the active hormone but we now know that T3 is three to five times more active biologically, and that T3 is the active hormone in target cells. Target cells make about 85% of active T3 by using enzymes called deiodinases to remove an iodine from T4. Target tissue activation of the hormone adds another layer of control because individual target tissues can alter their exposure to active thyroid hormone by regulating their tissue deiodinase synthesis. Hormone binding initiates transcription, translation, and synthesis of new proteins. The thyroid hormones normally act as a negative feedback signal to prevent oversecretion. The main function of thyroid hormones in adults is to provide substrates for oxidative metabolism. Thyroid hormones also interact with other hormones in a complex and tissuespecific fashion to modulate protein, carbohydrate, and fat metabolism. In children, thyroid hormones are necessary for full expression of growth hormone, which means thyroid function is essential for normal growth and development, especially of the nervous system. In the first few years after birth, myelin and synapse formation requires T3 and T4. Cytological studies suggest that thyroid hormones regulate microtubule assembly, which is an essential part of neuronal growth. The actions of thyroid hormones are most observable in people who secrete too much or too little hormone. Physiological effects that are subtle in people with normal hormone secretion often become exaggerated in patients with endocrine disorders. Patients with thyroid excess or deficiency may experience decreased tolerance to heat or cold and mood disturbances, in addition to other symptoms. Simply knowing that someone has a goiter does not tell you what the pathology is, however. Hyperthyroidism A person whose thyroid gland secretes too much hormone suffers from hyperthyroidism.
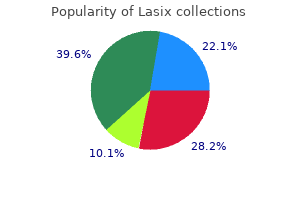
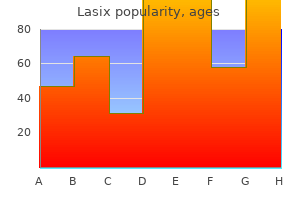
Order generic lasix from india
The final concentration of urine depends on the water permeability of the collecting duct ulterior motive meaning purchase lasix 40mg with mastercard. The hypothalamic hormone vasopressin controls collecting duct permeability to water in a graded fashion. Vasopressin causes distal nephron cells to insert aquaporin water pores in their apical membrane. Blood pressure and blood volume are sensed by receptors in the carotid and aortic bodies, and in the atria, respectively. The loop of Henle is a countercurrent multiplier that creates high osmolarity in the medullary interstitial fluid by actively transporting Na+, Cl -, and K+ out of the nephron. This high medullary osmolarity is necessary for formation of concentrated urine as filtrate flows through the collecting duct. The vasa recta capillaries form a countercurrent exchanger that carries away water leaving the tubule so that the water does not dilute the medullary interstitium. Hyperkalemia and hypokalemia cause problems with excitable tissues, especially the heart. Homeostatic compensations for changes in salt and water balance follow the law of mass balance. Fluid and solute added to the body must be removed, and fluid and solute lost from the body must be replaced. Intercalated cells in the collecting duct are responsible for the fine regulation of acid-base balance. Type A intercalated cells are active in acidosis and type B cells active in alkalosis. List five organs and four hormones important in maintaining fluid and electrolyte balance. Compare the routes by which water enters the body with the routes by which the body loses water. List the receptors that regulate osmolarity, blood volume, blood pressure, ventilation, and pH. Where are they located, what stimulates them, and what compensatory mechanisms are triggered by them What happens to the resting membrane potential of excitable cells when plasma K+ concentrations decrease Appetite for which two substances is important in regulating fluid volume and osmolarity For each transporter, tell (a) which section(s) of the nephron contain(s) the transporter; (b) whether the transporter is on the apical membrane only, on the basolateral membrane only, or on both; (c) whether it participates in reabsorption only, in secretion only, or in both. Concept map: Map the homeostatic reflexes that occur in response to each of the following situations: a. Explain how the loop of Henle and vasa recta work together to create dilute renal filtrate. Make a table that specifies the following for each substance listed: hormone or enzyme Name the four main compensatory mechanisms for restoring low blood pressure to normal. Why do you think there are so many homeostatic pathways for raising low blood pressure The interstitial fluid in contact with the basolateral side of collecting duct cells has an extremely high osmolarity, and yet the cells do not shrivel up. A 45-year-old man visiting from out of town arrives at the emergency room having an asthma attack caused by pollen. A year ago his family doctor diagnosed chronic obstructive pulmonary disease (emphysema). Food and Drug Administration has now approved a new class of drugs called vasopressin receptor antagonists. Predict the effect these drugs would have on renal function and describe some clinical situations or diseases in which these drugs might be useful. When the doctor sees her, her weight is 89 lb and her respiration rate is 6 breaths/min (normal 12). Hannah, a 31-year-old woman, decided to have colonic irrigation, a procedure during which large volumes of distilled water were infused into her rectum. About 12 hours later, her roommate found her in convulsions and took her to the emergency room. Her blood pressure was 140/90, her plasma Na+ concentration was 106 mEq/L (normal: 135 mEq/L), and her plasma osmolarity was 270 mOsM. In a concept map or flowchart, diagram all the homeostatic responses her body was using to attempt compensation for the changes in blood pressure and osmolarity. Assuming that dehydration causes maximal vasopressin secretion and allows the urine to concentrate to 1200 mOsM, how much additional urine does this diabetic patient excrete in a day Osmotic diuresis refers to the loss of additional water in urine as a result of unreabsorbed solutes. To see what difference unreabsorbed solutes make, calculate the volumes of filtrate that would be needed for excretion of 150 milliosmoles of NaCl. Then repeat the calculation for a diabetic who is excreting the same 150 mosmol NaCl plus 200 mosmol unreabsorbed glucose. If the minimum amount of waste solute that a person must excrete daily is about 600 milliosmoles, what is the minimum urine volume that is excreted in one day Positive feedback and feedforward control Biomolecules Micelles Microvilli Cell junctions Transporting epithelia Apical and basolateral membranes Endocrine and exocrine glands Enzymes Protein synthesis and storage Secondary active transport Exocytosis and transcytosis Smooth muscle Portal systems Lymphatics Renal transport Acidification of urine 21. Martin narrowly escaped death when a gun discharged 3 feet from him, tearing open his chest and abdomen and leaving a hole in his stomach wall. The gaping wound over the stomach failed to heal properly, leaving a fistula, or opening, into the lumen. Martin even agreed to "obey, suffer, and comply with all reasonable and proper experiments of the said William [Beaumont] in relation to . Like physicians of old who tasted urine when making a diagnosis, Beaumont tasted the mucous lining of the stomach and the gastric juices. He described them both as "saltish," but mucus was not at all acidic, and gastric fluid was very acidic. Beaumont collected copious amounts of gastric fluid through the fistula, and in controlled experiments he confirmed that gastric fluid digested meat, using a combination of hydrochloric acid and another active factor now known to be the enzyme pepsin. These observations and others about motility and digestion in the stomach became the foundation of what we know about digestive physiology. Although research today is conducted more at the cellular and molecular level, researchers still create surgical fistulas in experimental animals to observe and sample the contents of the digestive tract. Why is the digestive system-also referred to as the gastrointestinal system intestinus, internal-of such great interest The reason is that gastrointestinal diseases today account for nearly 10% of the money spent on health care. Many of these conditions, such as heartburn, indigestion, gas, and constipation, are troublesome rather than major health risks, but their significance should not be underestimated. Go into any drugstore and look at the number of over-the-counter medications for digestive disorders to get a feel for the impact digestive diseases have on our society. Digestion, the chemical and mechanical breakdown of food, 21 takes place primarily in the lumen of the gut. Along the way, secretions are added to ingested food by secretory epithelial cells and by accessory glandular organs that include salivary glands, the liver, the gallbladder, and the pancreas. At intervals along the tract, rings of muscle function as sphincters to separate the tube into segments with distinct functions. The products of digestion are absorbed across the intestinal epithelium and pass into the interstitial fluid. From there, they move into the blood or lymph for distribution throughout the body. Because the digestive system opens to the outside world, the tract lumen and its contents are actually part of the external environment. The arrangement is usually described as a commensal relationship, in which the bacteria benefit from having a home and food supply, while the human body is not affected. However, we are discovering ways in which the body does benefit from its bacterial companions. The relationship between humans and their bacterial microbiome is a hot topic in physiology today, and you will learn more about it at the end of the chapter.
Buy lasix without a prescription
When she exhales all the air she can blood pressure medication ziac purchase generic lasix on line, the volume of air left in her lungs is the. Cigarette smoke paralyzes the cilia that sweep debris and mucus out of the airways. Normal passive expiration depends on elastic recoil of muscles and elastic tissue in the lungs. Forceful expiration involves the internal intercostal muscles and the abdominal muscles. Like blood flow, air flow is bulk flow that requires a pump to create a pressure gradient and that encounters resistance, primarily from changes in the diameter of the tubes through which it flows. The mechanical properties of the pleural sacs and elastic recoil in the chest wall and lung tissue are essential for normal ventilation. Gas exchange requires a large, thin, moist exchange surface; a pump to move air; and a circulatory system to transport gases to the cells. Respiratory system functions include gas exchange, pH regulation, vocalization, and protection from foreign substances. External respiration is the exchange of gases between the atmosphere and cells of the body. It includes ventilation, gas exchange at the lung and cells, and transport of gases in the blood. The respiratory system consists of anatomical structures involved in ventilation and gas exchange. The lower respiratory tract includes the trachea, bronchi, bronchioles, and exchange surfaces of the alveoli. Each lung is contained within a double-membrane pleural sac that contains a small quantity of pleural fluid. Each primary bronchus divides into progressively smaller bronchi and finally into collapsible bronchioles. Bulk flow of air occurs down pressure gradients, as does the movement of any individual gas making up the air. A single respiratory cycle consists of one inspiration followed by one expiration. Air flow in the respiratory system is directly proportional to the pressure gradient, and inversely related to the resistance to air flow offered by the airways. Active expiration requires contraction of the internal intercostal and abdominal muscles. Intrapleural pressures are subatmospheric because the pleural cavity is a sealed compartment. Elastance is the ability of a lung to resist stretching or to return to its unstretched state. Reduced surface tension prevents smaller alveoli from collapsing and also makes it easier to inflate the lungs. The diameter of the bronchioles determines how much resistance they offer to air flow. Parasympathetic neurons cause bronchoconstriction in response to irritant stimuli. There is no significant sympathetic innervation of bronchioles, but epinephrine causes bronchodilation. What kind(s) of muscles are the different respiratory muscles (skeletal, cardiac, or smooth) Name the anatomical structures that an oxygen molecule passes on its way from the atmosphere to the blood. What is a typical arterial blood pressure for the pulmonary circuit, and how does this pressure compare with that of the systemic circulation What happens to inspired air as it is conditioned during its passage through the airways During inspiration, most of the thoracic volume change is the result of movement of the. Describe the changes in alveolar and intrapleural pressure during one respiratory cycle. List the major paracrines and neurotransmitters that cause bronchoconstriction and bronchodilation. Use up arrows, down arrows, greater than symbols (7), and less than symbols (6) as modifiers. Decide whether each of the following parameters will increase, decrease, or not change in the situations given. Of the three factors that contribute to the resistance of air flow through a tube, which plays the largest role in changing resistance in the human respiratory system Define the following terms: pneumothorax, spirometer, auscultation, hypoventilation, bronchoconstriction, minute volume, partial pressure of a gas. The cartoon coyote is blowing up a balloon in another attempt to catch the roadrunner. He first breathes in as much air as he can, then blows out all he can into the balloon. This volume can be measured directly by measuring the balloon volume or by adding which respiratory volumes together In 10 years, when the coyote is still chasing the roadrunner, will he still be able to put as much air into the balloon in one breath In the absence of other changes, would the following parameters increase, decrease, or not change as compliance decreases Assume a normal female has a resting tidal volume of 400 mL, a respiratory rate of 13 breaths/min, and an anatomic dead space of 125 mL. When she exercises, which of the following scenarios would be most efficient for increasing her oxygen delivery to the lungs A container of gas with a movable piston has a volume of 500 mL and a pressure of 60 mm Hg. You have a mixture of gases in dry air, with an atmospheric pressure of 760 mm Hg. Calculate the partial pressure of each gas if the composition of the air includes: a. Li is a tiny woman, with a tidal volume of 400 mL and a respiratory rate of 12 breaths per minute at rest. Just before a physiology exam, her ventilation increases to 18 breaths per minute from nervousness. Assuming her anatomic dead space is 120 mL, what is her alveolar ventilation in each case A spirometer with a volume of 1 liter (V1) is filled with a mixture of oxygen and helium, with the helium concentration being 4 g/L (C 1). Helium does not move from the lungs into the blood or from the blood into the lungs. He then puts the spirometer tube in his mouth and breathes quietly for several breaths. A student breathes at a rate of 20 breaths/min, with a tidal volume of 300 mL/breath. If his anatomic dead space is 130 mL, calculate his total pulmonary ventilation rate and his alveolar ventilation rate. Over the years, she has found that she can breathe better if she sleeps sitting nearly upright. If oxygen moves out of the lungs into the body, why is there more oxygen in the expired air In which condition does the lung have higher compliance, or is compliance the same in the two situations Lung Volume (L) Vital capacity Total lung capacity Functional residual capacity Subject Men Women Men Women Men Women Men Women Formula (0. Everest, climbers must pass through the "death zone" located at about 8000 meters (over 26,000 ft. Of the thousands of people who have attempted the summit, only about 2000 have been successful, and more than 185 have died. The mechanics of breathing include the events that create bulk flow of air into and out of the lungs. In this article, we focus on the two gases most significant to human physiology, oxygen and carbon dioxide, and look at how they move between alveolar air spaces and the cells of the body. The process can be divided into two components: the exchange of gases between compartments, which requires diffusion across cell membranes, and the transport of gases in the blood.
Discount lasix 40mg overnight delivery
Glucagon and insulin cycle according to food intake heart attack 38 years old cost of lasix, but both hormones are always present in some amount. So it appears that the ratio rather than an absolute amount of hormone determines the direction of metabolism. Diet-induced thermogenesis-heat generated by digestive and anabolic reactions during the absorptive state. Chylomicrons-lipoprotein complexes assembled in intestinal epithelium and absorbed into lymphatic system. Cholesterol-steroid component of cell membranes and precursor to steroid hormones. Convective heat loss-upward movement of warm air and its replacement by cooler air. If a person ingests a pure protein meal and only insulin is released, blood glucose concentrations might fall too low. Some other neurotransmitter besides acetylcholine (which binds to muscarinic receptors) is involved in the vasodilation reflex. The medulla secretes catecholamines (epinephrine, norepinephrine), and cortex secretes aldosterone, glucocorticoids, and sex hormones. Testosterone is anabolic for skeletal muscle, which might give an athlete a strength advantage. This immediate stress response is too rapid to be mediated by cortisol and must be a fight-or-flight response mediated by the sympathetic nervous system and catecholamines. If the stress is a physical one caused by an injury, the endogenous opioid b@endorphin can decrease pain and help the person continue functioning. In peripheral tissues, T4 is converted to T3, which is the more active form of the hormone. Normal growth and development require growth hormone, thyroid hormone, insulin, and insulin-like growth factors. Hypercalcemia hyperpolarizes the membrane potential, which makes it harder for the neuron to fire an action potential. A baby born with deficient 21-hydroxylase would have low aldosterone and cortisol levels and an excess of sex steroids, particularly androgens. Functions: blood clotting, cardiac muscle excitability and contraction, skeletal and smooth muscle contraction, second messenger systems, exocytosis, tight junctions, strength of bones and teeth. In the thyroid gland, tyrosine and iodine combine on thyroglobulin to make thyroid hormones. However, effects on metabolic rate are apparent within a few minutes and are thought to be related to changes in ion transport across cell and mitochondrial membranes. Zona glomerulosa (aldosterone), zona fasciculata (glucocorticoids), zona reticularis (sex steroids, primarily androgens). Conditions: adequate diet, absence of chronic stress, and adequate amounts of thyroid and growth hormones. Physiological stress stimulates secretion of cortisol, which increases blood glucose. Patient B: Dexamethasone decreases cortisol, suggesting that the problem is in the pituitary. Variables: season when blood collected, age group, and percent of people with vitamin D insufficiency. Days are shorter in the winter and the sun is at a more oblique angle and its rays are weaker. Also, at northern latitudes like Boston, people spend less time outside during the winter. Fewer than half the people tested were deficient, however, suggesting that most people consumed enough vitamin D. Osteopetrosis is characterized by excessive bone formation due to loss of osteoclast function. This can close up the normal holes (foramena) in bone and compress nerves running through the openings, causing changes in vision and hearing. Bone growth can also fill in the central marrow space of bones, leading to decreased production of red and white blood cells and platelets. Graph A: x@axis = plasma parathyroid hormone concentration, hormone concentration, y@axis = plasma Ca2+concentration. Graph B: x@axis = plasma Ca2+concentration, y@axis = plasma parathyroid hormone concentration. When capillary permeability increases, proteins move from plasma to interstitial fluid. This decreases the colloid osmotic force opposing capillary filtration, and additional fluid accumulates in the interstitial space (swelling or edema). Memory-immune cells remember prior exposure to an antigen and create a stronger immune response. Protect the body against foreign pathogens; remove dead or damaged tissues and cells; recognize and remove abnormal "self " cells. Detect the pathogen, recognize it as foreign, organize a response, and recruit assistance from other cells. When blood cells are exposed to an antibody, an antibodyantigen reaction may cause the blood cells to agglutinate. They are all names given to specialized tissue macrophages before scientists recognized that they were the same cell type. It consists of monocytes and macrophages, which ingest and destroy invaders and abnormal cells 8. Antibodies can be moved across cells by transcytosis or released from cells by exocytosis. The child developed antibodies to bee venom on first exposure, so if the child will have a severe allergic reaction to bee venom, it will occur on the second exposure. After the first bee sting, IgE antibodies secreted in response to the venom are bound to the surface of mast cells. At the second exposure, bee venom binding to the IgE causes the mast cells to degranulate, resulting in an allergic reaction that may be severe enough to cause anaphylaxis. Occurs because T lymphocytes that react with "self " cells are eliminated by clonal deletion. If self-tolerance fails, the body makes antibodies against itself (autoimmune disease). General adaptation syndrome-stress response that includes activation of the adrenal glands (fight-orflight response by adrenal medulla and cortisol secretion by the cortex). When lymph nodes trap bacteria, activated immune cells create a localized inflammatory response with swelling and cytokine activation of nociceptors that create the pain sensation. Antigens-substances that trigger an immune response and react with products of the response. Inflammation-nonspecific response to cell damage or invaders, including nonpathogens such as a splinter. Opsonins-proteins that coat and tag foreign material so that it can be recognized by the immune system. Delayed-may take several days to develop; mediated by helper T cells and macrophages. Baby received an O gene from Maxie, and could have received the other O gene from Snidely. Also likely that students are spending more time inside and having closer contact with fellow students. Autoimmune diseases often begin in association with an infection and are thought to represent cross-reactivity of antibodies that developed because of the infection.
Lasix 100mg cheap
Among these are acetylcholine hypertension treatment guidelines 2013 buy on line lasix, histamine, substance P (a neuropeptide), and leukotrienes secreted by mast cells, macrophages, and eosinophils. Leukotrienes are lipidlike bronchoconstrictors that are released during the inflammatory response. Asthma is treated with inhaled and oral medications that include b2@adrenergic agonists, anti-inflammatory drugs, and leukotriene antagonists. Restrictive Lung Disease Pathological conditions in which lung compliance is reduced are called restrictive lung diseases. A decrease in lung compliance affects ventilation because respiratory muscles must work harder to stretch a stiff lung. In restrictive lung disease the energy expenditure can far exceed the normal work of breathing. Two common causes of decreased compliance are inelastic scar tissue formed in fibrotic lung diseases, and inadequate alveolar production of surfactant, the chemical that facilitates lung expansion. Pulmonary fibrosis is characterized by the development of stiff, fibrous scar tissue that restricts lung inflation. Other forms of fibrotic lung disease result from chronic inhalation of fine particulate matter, such as asbestos and silicon, that escapes the mucus lining the airways and reaches the alveoli. If the particles are organic, the macrophages can digest them with lysosomal enzymes. However, if the particles cannot be digested or if they accumulate in large numbers, an inflammatory process ensues. Forced Vital Capacity Test A forced vital capacity test with a spirometer allows the clinician to assess respiratory system function as well as static lung volumes. In this test, the subject takes in as much air as possible, then blows it all out as fast as possible. The Auscultation and Spirometry Assess Pulmonary Function Most pulmonary function tests are relatively simple to perform. Auscultation of breath sounds is an important diagnostic technique in pulmonary medicine, just as auscultation of heart sounds is an important technique in cardiovascular diagnosis [p. Breath sounds are more complicated to interpret than heart sounds, however, because breath sounds have a wider range of normal variation. Normally, breath sounds are distributed evenly over the lungs and resemble a quiet "whoosh" made by flowing air. When air flow is reduced, such as in pneumothorax, breath sounds may be either diminished or absent. Abnormal sounds include various squeaks, pops, wheezes, and bubbling sounds caused by fluid and secretions in the airways or alveoli. Inflammation of the pleural membrane results in a crackling or grating sound known as a friction rub. It is caused by swollen, inflamed pleural membranes rubbing against each other, and it disappears when fluid again separates them. Auscultation and pulmonary function tests, described earlier, are non-invasive tests that allow quick assessment of lung function. They can also be used to differentiate between two major types of lung disease, obstructive and restrictive. Obstructive Lung Disease Diseases in which air flow is diminished because of increased airway resistance are known as obstructive lung diseases. When patients with obstructive lower airway diseases are asked to exhale forcefully, air whistling through the narrowed airways creates a wheezing sound that can be heard even without a stethoscope. Depending on the severity of the disease, the bronchioles may even collapse and close off before a forced expiration is completed, reducing both the amount and rate of air flow as measured by a spirometer. Obstructive lung diseases include asthma, obstructive sleep apnea, emphysema, and chronic bronchitis. Obstructive sleep apnea apnoia, breathless results from obstruction of the upper airway during sleep, often due to abnormal relaxation of the muscles of the pharynx and tongue that increases airway resistance during inspiration. Asthma is considered an obstructive lung disease because inflammation of the airways, often associated with allergies, results in bronchoconstriction and airway edema. Asthma can be triggered by exercise (exercise-induced asthma) or by rapid changes in the temperature or humidity of inspired air. How will inspiratory reserve volume change in patients with a restrictive lung disease Chronic obstructive lung disease causes patients to lose the ability to exhale fully. Next, we shift focus from the bulk flow of air to the diffusion and transport of oxygen and carbon dioxide as they travel between the air spaces of the alveoli and the cells of the body. Now check your understanding of the physiology in the problem by comparing your answers with those in the following table. Edna leaves the office with prescriptions for a mucus-thinning drug, a bronchodilator, and anti-inflammatory drugs to keep her airways as open as possible. She has agreed to try to stop smoking once more and also has a prescription and brochures for that. According to the American Question Facts Integration and Analysis Q1: What does narrowing of the airways the relationship between tube radius and When resistance increases, the body do to the resistance airways offer to air resistance is the same for air flow as for must use more energy to create air flow Q2: Why do people with chronic bronchitis have a higher-than-normal rate of respiratory infections Q4: When Edna fills her lungs maximally, the volume of air in her lungs is known as the capacity. If the diffusion of gases between alveoli and blood is significantly impaired, or if oxygen transport in the blood is inadequate, hypoxia (a state of too little oxygen) results. These two conditions are clinical signs, not diseases, and clinicians must gather additional information to pinpoint their cause. To avoid hypoxia and hypercapnia, the body uses sensors that monitor arterial blood composition. Recall that diffusion is movement of a molecule from a region of higher concentration to one of lower concentration [p. When we think of concentrations of solutions, units such as moles/liter and milliosmoles/liter come to mind. However, respiratory physiologists commonly express plasma gas concentrations in partial pressures to establish whether there is a concentration gradient between the alveoli and the blood. Gases move from regions of higher partial pressure to regions of lower partial pressure. The purpose of the expedition was to study human physiology at extreme altitudes, starting with the base camp at 5400 m (18,000 ft) and continuing on to the summit at 8850 m (over 29,000 ft). From the work of these scientists and others, we now have a good picture of the physiology of high-altitude acclimatization [p. If nitrogen is 78% of atmospheric air, what is the partial pressure of this gas when the dry atmospheric pressure is 720 mm Hg Oxygen therefore diffuses down its partial pressure (concentration) gradient from the alveoli into the capillaries. There can also be problems with the transfer of gases between the alveoli and pulmonary capillaries. If something impairs blood flow to the lung, then the body is unable to acquire the oxygen it needs. Composition of the Inspired Air the first requirement for adequate oxygen delivery to the tissues is adequate oxygen intake from the atmosphere. The partial pressure of oxygen in air decreases along with total atmospheric pressure as you move from sea level (where normal atmospheric pressure is 760 mm Hg) to higher altitudes. High altitude is considered anything above 1500 m (5000 ft), but most pathological responses to altitude occur above 2500 m (about 8000 ft). By one estimate, 25% of people arriving at 2500 m will experience some form of altitude sickness. Diffusion Problems Cause Hypoxia If hypoxia is not caused by hypoventilation, then the problem usually lies with some aspect of gas exchange between alveoli and blood. The exchange of oxygen and carbon dioxide across this diffusion barrier obeys the same rules as simple diffusion across a membrane [p. The diffusion rate is directly proportional to the available surface area, the concentration gradient of the gas, and the permeability of the barrier: Diffusion rate surface area * concentration gradient * barrier permeability For example, Denver, 1609 m above sea level, has an atmospheric pressure of about 628 mm Hg.
Buy online lasix
During atrial filling blood pressure home remedies discount lasix 100mg overnight delivery, is pressure in the atrium higher or lower than pressure in the venae cavae Which chamber-atrium or ventricle-has higher pressure during the following phases of the cardiac cycle Murmurs are abnormal heart sounds caused either by blood forced through a narrowed valve opening or by backward flow (regurgitation) through a valve that has not closed completely. Valvular stenosis stenos, narrow may be an inherited condition or may result from inflammation or other disease processes. Today, however, it is usually performed by listening through a stethoscope placed against the chest and the back. Two additional heart sounds can be recorded with very sensitive electronic stethoscopes. The third heart sound is caused by turbulent blood flow into the ventricles during ventricular filling, and the fourth sound is associated with turbulence during atrial contraction. In certain abnormal conditions, these latter two sounds may become audible through a regular stethoscope. They are called gallops because their timing puts them close to one of the normal heart sounds: "lub-dup-dup," or "lub-lub-dup. This figure represents the changes in volume (x-axis) and pressure (y-axis) that occur during one cardiac cycle. Recall that the flow of blood through the heart is governed by the same principle that governs the flow of all liquids and gases: Flow proceeds from areas of higher pressure to areas of lower pressure. When the heart contracts, the pressure increases and blood flows out of the heart into areas of lower pressure. The left side of the heart creates higher pressures than the right side, which sends blood through the shorter pulmonary circuit. The ventricle has completed a contraction and contains the minimum amount of blood that it will hold during the cycle. Atrial blood now flows into the ventricle, increasing its volume (point A to point B). As blood flows in, the relaxing ventricle expands to accommodate the entering blood. Consequently, the volume of the ventricle increases, but the pressure in the ventricle goes up very little. During periods of very high heart rate, for instance, when the ventricle does not have time to fill completely between beats, the end-diastolic value may be less than 135 mL. Once ventricular pressure exceeds the pressure in the aorta, the aortic valve opens (point C). Pressure continues to increase as the ventricle contracts further, but ventricular volume decreases as blood is pushed out into the aorta (C S D). Once pressure in the ventricle falls below aortic pressure, the semilunar valve closes, and the ventricle again becomes a sealed chamber. When ventricular pressure finally falls to the point at which atrial pressure exceeds ventricular pressure, the mitral valve opens and the cycle begins again. Why does it decrease during the initial part of ventricular systole, then increase Because all blood that leaves the heart flows through the tissues, cardiac output is an indicator of total blood flow through the body. However, cardiac output does not tell us how blood is distributed to various tissues. This means that, at rest, one side of the heart pumps all the blood in the body through it in only 1 minute! However, if one side of the heart begins to fail for some reason and is unable to pump efficiently, cardiac output becomes mismatched. In that situation, blood pools in the circulation behind the weaker side of the heart. Homeostatic changes in cardiac output are accomplished by varying the heart rate, the stroke volume, or both. Both local and reflex mechanisms can alter cardiac output, as Play Interactive Physiology 2. For the average contraction in a person at rest: 135 mL - 65 mL = 70 mL, the normal stroke volume (10) Concept Check 31. If the stroke volume of the left ventricle is 250 mL/beat and the stroke volume of the right ventricle is 251 mL/beat, what happens to the relative distribution of blood between the systemic and pulmonary circulation after 10 beats This means the ventricle is ejecting 52% of the blood that was in it at the end of relaxation and filling. Stroke volume is not constant and will increase as contraction force of the ventricles increases. For example, if stroke volume increases to 100 mL during exercise, the ejection fraction increases to 100 mL/135 mL, or 74%. Stroke volume, like heart rate, is regulated by mechanisms we discuss later in this chapter. The Autonomic Division Modulates Heart Rate An average resting heart rate in an adult is about 70 beats per minute (bpm). Trained athletes may have resting heart rates of 50 bpm or less, while someone who is excited or anxious may have a rate of 125 bpm or higher. Parasympathetic activity slows heart rate, while sympathetic activity speeds it up. Normal Parasympathetic stimulation (e) Sympathetic stimulation and epinephrine depolarize the autorhythmic cell and speed up the pacemaker potential, increasing the heart rate. Normal Sympathetic stimulation Membrane potential (mV) 0 Membrane potential (mV) 20 20 0 -20 -40 -60 -60 Hyperpolarized 0. Decreased Ca2+ permeability slows the rate at which the pacemaker potential depolarizes. The combination of the two effects causes the cell to take longer to reach threshold, delaying the onset of the action potential in the pacemaker and slowing the heart rate. The catecholamines norepinephrine (from sympathetic neurons) and epinephrine (from the adrenal medulla) increase ion flow through both If and Ca2+ channels. Catecholamines exert their effect by binding to and activating b1@adrenergic receptors on the autorhythmic cells. Increased permeability to Na+ and Ca2+ during the pacemaker potential phase speeds up depolarization and heart rate. Tonic Control Normally, tonic control of heart rate is dominated by the parasympathetic branch. This control can be shown experimentally by blocking all autonomic input to the heart. To achieve a resting heart rate of 70 beats per minute, tonic parasympathetic activity must slow the intrinsic rate down from 90 bpm. Norepinephrine (or epinephrine) on b1@receptors speeds up the depolarization rate of the autorhythmic cells and increases heart rate. In the isolated heart, the force of ventricular contraction is affected by two parameters: the length of muscle fibers at the beginning of contraction and the contractility of the heart. The volume of blood in the ventricle at the beginning of contraction (the end-diastolic volume) determines the length of the muscle. Contractility is the intrinsic ability of a cardiac muscle fiber to contract at any given fiber length and is a function of Ca2+ interaction with the contractile filaments. Length-Tension Relationships In striated muscles, the force created by a muscle fiber is directly related to the length of the sarcomere, as indicated by the initial length of the muscle fiber [p. If additional blood flows into the ventricles, the muscle fibers stretch, then contract more forcefully, ejecting more blood. The degree of myocardial stretch before contraction begins is called the preload on the heart because this stretch represents the load placed on cardiac muscles before they contract. The Frank-Starling Law of the Heart the relationship between stretch and force in the intact heart was first described by a German physiologist, Otto Frank. Starling attached an isolated heart-lung preparation from a dog to a reservoir so that he could regulate the amount of blood returning to the heart.