Buy cheap malegra fxt 140 mg on-line
Hypertrophy An increase in cell size that is coupled with an increase in the amount of functioning tissue mass erectile dysfunction lotions purchase generic malegra fxt line. Hyperventilation Increased alveolar ventilation in excess of carbon dioxide production as a result of an increased rate and/or depth of breathing. Hypnogram A summary of time spent in each stage of sleep; also called a sleep histogram. Hypnopompic hallucination A vivid dreamlike hallucination that occurs on awakening. Hypochromia Condition in which red blood cells are pale in color because of a deficit of hemoglobin. Iatrogenic the etiology of conditions that are caused unintentionally by a treatment or diagnostic procedure or an error caused by a healthcare provider. Iatrogenic hypothermia the inadvertent heat loss associated with anesthesia, convective air flow, or evaporation of solutions from the skin during treatments; also called nosocomial hypothermia. Idiopathic interstitial pneumonia A classification of interstitial lung disease that includes all related disorders for which no cause has been identified, such as idiopathic pulmonary fibrosis. Idiopathic pulmonary fibrosis A respiratory disease of unknown cause in which pulmonary tissue becomes stiff and noncompliant, leading to decreased oxygenation and decreased perfusion of lungs. This is how the body recognizes and defends against bacteria and viruses along with both foreign and harmful substances. Immunodeficiency A weakened immune response as a result of a defect in one or more components of the immune system. Immunologically ignorant A form of self-tolerance in which reactive lymphocytes and their target antigen are both detectable in an individual, yet no autoimmune attack occurs. Impetigo A highly contagious superficial skin infection that is initially seen as red pimples and fluid-filled blisters, and later changes to yellow crusted lesion. Impingement syndrome An injury in which tendons of the shoulder muscles are trapped under the acromion. Inadvertent hypothermia Unintended heat loss that occurs in homes or institutional settings and often involving vulnerable infants, ill individuals, or those with impaired thermoregulation. Incidence the number of new cases of a disease or condition that occur during a specified period of time in a population that is at risk for developing the disease or condition. Incubation period the elapsed time between exposure to an infectious agent and the appearance of signs or symptoms of illness or disease. Industrial hygiene the science related to anticipating, recognizing, controlling, and evaluating hazards that arise in or from the workplace that may affect the health and well-being of workers and members of the community. Infectious disease A disorder caused by invasion of a host organism by a pathogen. Infertility the inability to achieve clinical pregnancy after 12 or more months of regular unprotected sexual intercourse. Influenza A highly contagious viral infection that sweeps through a geographic region as an epidemic that lasts 6 to 8 weeks during the winter months. Initiation the first step in the carcinogenesis model in which irreversible changes occur in the genotype of the cell, resulting in malignancy. Innate (natural) immune system A system of antigen-nonspecific defense mechanisms that respond quickly after exposure to an infectious agent; this is the immunity one is born with and is the initial response by the body to prevent infection. Insulin resistance the inability of insulin to achieve its expected biological response as the cells fail to respond to the normal actions of insulin. Intervertebral disc degeneration A health problem caused by drying out or degeneration of the pads between the vertebrae. Ionizing radiation Radiation that has enough energy to eject electrons that are tightly bound to atoms, producing positively and negatively charged ions. Iron deficiency anemia Anemia that occurs when blood lacks adequate healthy red blood cells owing to a lack of iron. Ischemia A restriction of blood supply in the tissues that causes a shortage of oxygen and glucose needed for cellular metabolism. Isotonic Property of solutions in which the concentration of sodium in fluid is equally to the concentration of sodium in the cell; results in a situation in which cells neither swell nor shrink. Jaundice A yellowish discoloration of the whites of the eyes, skin, or mucous membranes caused by the bile salts in the tissues. Jefferson fracture A fracture of all four rings of C1 that results from axial loading onto the spinal column. Karnofsky Performance Status Scale A tool that allows patients to be classified according to their functional impairment and can be used to compare effectiveness of different therapies and to assess the prognosis in individual patients. Karyotyping A test used to examine the visual appearance of chromosome structure and number. Glossary Keloid An overgrowth of collagenous scar tissue at the site of a skin injury, particularly a wound or surgical incision. Keratinization A process by which epithelial cells lose their moisture and are replaced by horny tissue. Ketogenesis the production of ketones, which are important sources of energy for peripheral tissues such as muscle. They increase blood flow, promote repair of damaged tissue, stimulate pain receptors, and enhance the ability of fluids to pass through small vessels. Kussmaul respirations Deep labored breathing often associated with diabetic ketoacidosis. Laceration A cut or tear in skin tissue, usually extending deeper than the superficial layer of the skin. Laminin A glycoprotein in the basement membrane that provides adhesion of cells above and below it. Latent viral state A condition in which a virus is not eliminated from the body but remains present in an inactive form that, under certain conditions, can be reactivated and cause illness. Left-sided heart failure A condition in which the left side of the heart is unable to pump enough blood to meet the needs of the body. Leg ulcers Sores on the skin caused by chronic venous insufficiency that persist for more than 6 weeks. Leiomyomas Benign tumors, also known as uterine fibroids, that develop from an overgrowth of smooth muscle and connective tissue in the uterus. Lethal triad of trauma the developing of hypothermia, acidosis, and coagulopathy resulting from traumatic injury. Leukotrienes A type of eicosanoid mediators produced by leukocytes and usually accompanied by the production of histamine and prostaglandin. One of their major roles is triggering contraction of the smooth muscle lining of the bronchioles, which is associated with asthma. Life-threatening injury An injury that is likely to result in death, permanent disfigurement, or permanent loss of function or impairment of function to a body part or mental ability. Lipofuscin A granular yellow-brown pigment composed of lipid containing residues of lysosomal digestion. Lipolysis the process through which triglycerides are hydrolyzed to fatty acids and glycerol. Lipoma Common, benign lumps that grow under normal skin in subcutaneous tissues G-13 Livor mortis the purple-red discoloration that occurs after death when the heart is no longer pumping blood throughout the body and so blood settles in dependent parts of the body. Loss of heterozygosity A common event in the development of inherited cancer that occurs with loss of the somatic wild-type allele. Lipoproteins that are the primary Lower back pain A common health problem that causes stiffness, mobility changes, and possible long-term health problems. Macrocytic Form of anemia characterized by large erythrocytes, defined as greater than 100 fL. Macrovascular disease Disease of large vasculature; diabetic macrovascular disease includes coronary artery disease, peripheral arterial disease, and stroke. Macular degeneration A condition in with the macula (the central part of the retina) degenerates resulting in distortion or loss of central vision; also called age-related macular degeneration. Major depressive episode A clinical syndrome involving a depressed mood (anhedonia) that lasts for 2 weeks in addition to other symptoms. Malignant Aberrant, uncontrolled invasive cell growth with the potential to become life threatening. Malignant hyperthermia A rare genetic condition associated with uncontrolled heat production caused by a mutation in a type of ryanodine receptor that causes intracellular Ca2+ release channels in skeletal muscle to react when a susceptible individual receives inhalation anesthetics or depolarizing muscle relaxants. Mallory bodies Damaged filaments found in the liver, most commonly associated with alcoholic liver disease.
Cheap malegra fxt amex
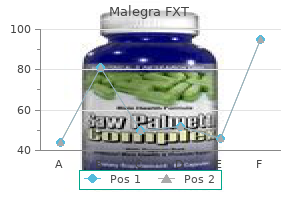
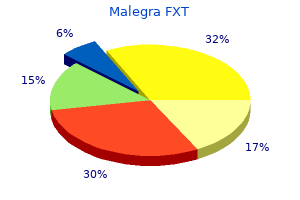
The prevalence of Clostridium difficile and toxin in a nursery population: a comparison between patients with necrotizing enterocolitis and an asymptomatic group erectile dysfunction in a young male quality malegra fxt 140mg. The spectrum of spontaneous and iatrogenic esophageal injury: perforations, Mallory-Weiss tears, and hematomas. Schonlein-henoch purpura in children and adults: diagnosis, pathophysiology and management. Relationship between upper gastrointestinal bleeding and non steroidal anti-inflammatory drugs in children. Frequency, significance and therapy of the Mallory-Weiss syndrome in patients with portal hypertension. Screening and surveillance recommendations for pediatric gastrointestinal polyposis syndromes. Clinical presentation of and outcome for solitary rectal ulcer syndrome in children. Healing of a bleeding solitary rectal ulcer with multiple sessions of argon plasma. Hemobilia in a child due to right hepatic artery pseudoaneurysm: multidetector-row computed tomography demonstration. Intramural hematomas of the gastrointestinal system: a 5-year single center experience. Unusual upper gastrointestinal bleeding: ruptured superior mesenteric artery aneurysm in rheumatoid arthritis. A case of a jejunal ectopic pancreas presenting as obscure gastrointestinal bleeding. Ectopic varices: anatomical classification, hemodynamic classification, and hemodynamic-based management. Defining eosinophilic colitis in children: insights from a retrospective case series. Cytomegalovirus colitis in patients without inflammatory bowel disease: a single center study. Overlap, common features, and essential differences in pediatric granulomatous inflammatory bowel disease. Gastrointestinal presentation of Langerhans cell histiocytosis in a child with perianal skin tags: a case report. Three years old child with juvenile hyaline fibromatosis presenting with rectal bleeding. The prevalence of childhood obesity has nearly tripled over the last 20 years, with 17% of children now considered obese. Currently there are no broadly accepted standards for body fatness for either adults or children. Although skin-fold thickness measurement is predictive of total body fat in children,17 it is not recommended for routine use due to lack of readily available reference data, training involved in performing, and measurement error between operators. These cut-offs were originally created arbitrarily and for clinically practical reasons. An early nadir and increase, occurring before 5 years of age, is associated with increased risk of hypertension and obesity in adulthood, primarily due to increased fat, rather than lean muscle deposition. Bouchard elegantly outlined a model of this epidemic and its main contributors, grouped into four areas: built environment, social environment, behavior, and biology. Attempts are frequently made to isolate a small number of significant contributors to the obesity epidemic, but much like the biologic control of appetite (see subsequent text), this is a complex problem. Changes in the social environment are represented by the increase in energy-dense foods and drinks, easily available in large portions and at low prices. Changes in family structure, including single-parent households and dual-career couples, have led to increased use of high-calorie, high-fat convenience foods. In developed or industrialized countries, much of the obesity epidemic is thought to result from food insecurity, where a person or family is at risk of being unable to provide food. Video games, television, computers/Internet, and even cell phone use have led to increasing hours of sedentary activity in children (averaging more than 21 hours a week), which has been clearly associated with obesity. During the period 1971 to 1974, the prevalence of overweight among children and adolescents ages 2 to 19 years was 15. The acute rise in obesity prevalence, cardiovascular disease, and other Chapter 14 - Obesity 157 this review also found that increased access to open green areas, in both urban and rural areas, was associated with increased physical activity in children. Active commuting to school and other activities was associated with traffic safety, pedestrian infrastructure, and lower crime threat. Obesity was found to be associated with distance to fast food restaurants, presence and density of convenience stores, distance to playgrounds, and perceived access to gardens, playgrounds, parks, and shops. Perceived neighborhood safety was associated with some forms of physical activity; however, including screen time in the model negated this association. In summary, obvious changes in the nutritional and activity (sedentary and physical) environments of children, possibly mediated by changes in families and socioeconomic status, have contributed significantly to this epidemic. Next is the family, with influences of the parent being the most immediate, as well as issues of socioeconomic status and role modeling. Broader influences, such as the community and general culture, can have profound effects on obesity risk, even though they may be indirect and more difficult to determine. Eating behaviors such as those described in the following text are thought to contribute more to excess energy consumption than to absolute weight status. Recent research has highlighted several of these behaviors and their relationship with childhood obesity. The apparent paradox of this evidence suggests other perhaps more important drivers of childhood obesity. Physical activity or exercise is thought to be beneficial for prevention of obesity as well as weight loss. A recent systematic review of the literature concluded that, although some of the more recent studies have found an inverse relationship between physical activity and weight status, many studies found no relationship between the two. Including parents in any obesity intervention or treatment plan is critical;75 effective long-term obesity studies identify that intense parental involvement and parenting skills are key to their success. Furthermore, a paradigm shift occurred in how adiposity, and more specifically the adipocyte, is viewed. No longer seen as a storage cell for excess calories, visceral adipose cells are categorized as independent endocrine cells with important roles in metabolism, inflammation, and cardiovascular disease (Table 14-2). The gastrointestinal, central nervous, and adipose/storage systems are the primary areas involved in the short- and long-term balance of energy and weight. Despite the elegance of this network, it is still influenced greatly by environmental stimuli. As an example, initiation of meals is influenced to a greater degree by environmental signals, whereas meal size and termination may be influenced to a greater degree by biologic signals. In all, more than 600 genes have been associated with human and animal models of obesity. Although described in two severely obese cousins with undetectable serum leptin levels, leptin deficiency has been identified in very few individuals. Endocannabinoids are anabolic regulators of metabolism, increasing energy intake, promoting energy storage, and decreasing energy expenditure. There are also genetic mutations associated with taste, meal size, and food selection that are tied to obesity. Although it appears that individuals may be predisposed to weight gain, it is within the context of an obesogenic environment, with many modifiers, both known. Asking questions about the amount of time spent outside, involvement in sports programs outside of school, and "fun" activities or hobbies can be a good proxy for activity in younger children. Two recent reviews of exergaming have found that this practice may not be as detrimental as other types of screen time, and may even be helpful in increasing physical activity levels in children and adults. Certain racial/ethnic groups (Native American) are at particularly high risk given the high prevalence rates in both adults and children. Obesity and family history of hypertension are independent risk factors for the development of hypertension in children. A 24-hour recall, intake diary, or food frequency questionnaire can be helpful; each has its own advantages and disadvantages.
Buy 140 mg malegra fxt visa
Once the acute phase is over impotence cures purchase malegra fxt 140mg mastercard, the serum level will decrease promptly, whereas the serum bilirubin will remain increased. Ammonia Ammonia, a by-product of protein metabolism, is formed from bacterial action in the intestine and from metabolizing tissues. Most of the ammonia is absorbed into the portal circulation and is converted in the liver to urea. With severe liver decompensation or when blood flow to the liver is altered, the plasma ammonia level remains elevated. Its concentration is low in the blood except when there is cellular injury, and then large amounts are released into circulation. More helpful when viewed in contrast to other laboratory values to aid in distinguishing possible source of inflammation. Increased or decreased Increased values indicate biliary obstruction or tissue damage. Decreased values can reflect liver damage or issues with nutritional absorption and malnutrition. Expected Abnormality Used to Diagnose Increased or decreased Increased values indicate damage to the liver. The serum level will rise early and will remain elevated as long as cellular damage persists. Expected Abnormality Used to Diagnose Increased Increased values of isoenzymes 4 and 5 indicate liver damage. Increased Increased values aid in determining the presence of biliary duct disorders or obstruction. Red Blood Cell Measures Bilirubin Bilirubin is formed from the breakdown of hemoglobin by the reticuloendothelial system and is carried in the plasma to the liver, where it is conjugated (directly) to form bilirubin diglucuronide and is excreted in the bile. There are two forms of bilirubin in the body: the conjugated, or direct-reacting (soluble), and the unconjugated, or indirect-reacting (protein bound). If the total bilirubin level is within normal range, direct and indirect bilirubin levels do not need to be analyzed. Prothrombin is converted to thrombin by the action of thromboplastin, which is needed to form a blood clot. Low Anemia 1076 Chapter 43 Disorders of the Exocrine Pancreatic and Hepatobiliary Systems commonly diagnosed cancer, liver cancer is the second most common cause of death worldwide in men. Rates of intrahepatic cholangiocarcinoma, the second most common type of liver cancer, are also increasing. Other risk factors related to lifestyle are excess alcohol consumption, coffee consumption, exposure to aflatoxins, obesity, and oral contraceptive use. Hepatitis is one such chronic liver disorder, known to cause liver cancer in up to 85% of patients with hepatocellular carcinoma. In the United States, hepatitis C is responsible for the increased rates and incidence of liver cancer and mortality in recent years. Asia and Africa have the highest incidence; Europe, Latin America, and the Caribbean have the lowest rates. Important considerations for cellular senescence of the older adult are how cumulative life events have contributed to inflammation and other potential sources of tissue damage, leading to an increased risk of metastatic liver cancer. The dark color of the feces is from the bilirubin; when bilirubin is absent, the stools are often clay colored. Lipase, from the pancreas, assists with fat digestion to produce fatty acids and glycerol from triglycerides. An increased total bilirubin in the newborn can be attributed to either hemolysis that is occurring faster than normal or the liver of the newborn being slower to conjugate the bilirubin. The liver of the newborn takes longer to remove the bilirubin from the blood because it takes a few days to produce glucuronyl transferase, an enzyme needed to convert unconjugated bilirubin to conjugated bilirubin. Another factor contributing to newborn physiologic jaundice is that intestinal flora in newborns is slower to convert bilirubin to urobilinogen, thus putting bilirubin back into the circulation. Because of these physical changes, about 60% of full-term newborns experience physiologic jaundice starting 24 hours after birth. Abdominal pain and indigestion are early, vague symptoms that are easily ignored or dismissed by the patient. When more serious symptoms appear, such as jaundice or ascites, the liver disorder is often at an advanced stage, often making the prognosis and outcome less favorable. Etiology and Pathogenesis Primary tumors of the liver are not as common as metastatic tumors. The liver is vascular; therefore, it is affected by the spread of diseases and disorders, including cancer, from other organs and tissues. A liver biopsy is often needed to help distinguish and confirm primary from metastatic liver cancer. Cirrhosis remains one of the major risk factors for hepatocellular carcinoma because the constant tissue necrosis and damage to the hepatocytes leave the cells damaged and at risk for mutations. The liver scan shows a single large mass with irregular borders, and a biopsy is performed to make the definitive diagnosis. Why is it important to obtain an occupational history from patients even if they are healthy Weakness, weight loss, and bloating are signs that people often ignore until later, when more serious symptoms appear that prompt medical attention. This type of pain stems from tissue stretching with the beginning of abdominal ascites and liver enlargement. Dark-skinned patients will show the change initially in the inner canthus of the eye or the mucous membranes of the hard palate. Assessment of jaundice also includes the palms of the hands and the plantar surfaces of the feet. The discoloration of the skin and sclera of the eye result from the increased unconjugated bilirubin. Hypoprothrombinemia might be noted as a result of the lack of bile salts that contribute to emulsification of fat-soluble vitamins, such as vitamin K, and their absorption in the intestine. Without sufficient vitamin K in the bloodstream, the liver cannot make enough prothrombin, which is needed for blood clotting. Linking Pathophysiology to Diagnosis and Treatment the blood flow to the liver helps to support the many functions that occur in this organ. The blood supply comes from both the portal circulation and a direct extension off the aorta. Because of this, the liver is exposed to many pathogens, drugs, toxins, and malignant cells that cause changes to the microenvironment as well as damage in the form of hypoxia, inflammation, or oxidative stress, which set the stage for carcinogenesis and tumor initiation. Liver cancer is believed to be caused by both infiltration of immune cells and oxidative stress. The release of cytokines and chemokines from Kupffer cells contributes to the inflammatory process in the liver as well as the deregulation of liver cell proliferation. Insulin resistance causes increased levels of pro-inflammatory cytokine (tumor necrosis factor and interleukin 6) that contribute to hepatic steatosis and inflammation. Also, high levels of insulin upregulate insulin-like growth factor 1, a protein that stimulates mechanisms of cellular proliferation and inhibits other mechanisms of programmed cellular death. Malfunction in this isoenzyme renders the body less able to detoxify toxins and carcinogens that may contribute to carcinogenesis. Birkland tells the primary healthcare provider that he works for a grain elevator company that purchases and stores corn and soybeans. He has worked at this job for over 35 years, and it often involves loading moldy grain that has been stored before shipment. The laboratory test results show the presence of abnormally high levels of alpha-fetoprotein. The liver scan is the initial diagnostic test, and results indicate an abnormally large liver mass with uneven contour in the abdomen.
Buy 140mg malegra fxt
Herbal products such as tea tree oils erectile dysfunction natural remedies diabetes cheap malegra fxt online american express, Echinacea, pomegranate, and garlic are timehonored treatments but should be used with the consultation of a healthcare provider. Herbal products can depress the immune system if used for an extended period of time or too often. Breastfed infants can also contract thrush and then pass it to their mother, so both mother and baby should be treated. Older adults who use disposable briefs are highly prone to candidiasis, especially if the garments are not changed as often as they should be. Severe cases of candidiasis from the moisture of disposable briefs may benefit from leaving the brief open on top of a waterproof pad. Dentures that are not properly cleaned and soaked can be another root of candidiasis in older adults. Etiology and Pathogenesis Tinea infections are highly contagious and are spread by direct contact, most often when an individual touches another person who is infected. It can spread on moist surfaces, such as floors of locker rooms and public showers, and through pets. Sweating, weak immune system, oily skin or hair, and shared clothing, linen, towels, or hairbrushes can facilitate the spread of the fungus. These dermatophytes infect the superficial layers of the skin, and there is a 1- to 3-week incubation period, after which the dermatophytes invade peripherally. With tinea corporis, the same symptoms appear, but as new patches emerge, the center of the older patches will clear up. Slight itching, dry and brittle hair, and bald patches will be seen in tinea capitis. In some cases, just a physical examination is needed to determine the type of infection. Tinea is also known as ringworm because it sometimes takes on a circular pattern that resembles a worm chasing its tail; however, worms are not involved in any of these infections. This type is more common in teens and young adults and is the only form that is not contagious. Stronger oral prescriptions that may work faster and are administered less often include griseofulvin, terbinafine, itraconazole, and fluconazole. Occasionally, selenium sulfide shampoo for tinea capitis, and corticosteroids (prednisone) may be recommended. In what circumstances does Candida, part of the normal flora of the skin, become problematic What types of diagnostic testing are done to confirm fungal infections of the skin Urticaria and lichen planus are skin disorders that are often caused by an autoimmune response. The most classic symptoms of most of skin inflammation are erythema, lesions, and itchy skin. The focus of this section is on contact dermatitis, seborrheic dermatitis, exfoliative dermatitis, urticaria, and lichen planus. The latest concern in healthcare is allergy to latex, which can cause a contact dermatitis. In irritant contact dermatitis, a red rash appears immediately, and the skin may be more painful than itchy. The hands and legs are the most common part of the body affected, but any part of the body can be affected. Symptoms include vomiting, shortness of breath, drop in blood pressure, elevated heart rate, and airway edema. If these physical reactions are severe, the combination may be life threatening and require immediate medical care to support respiratory and cardiovascular function. Thus for any suspected allergic condition, an assessment should be made to rule out anaphylaxis. Contact Dermatitis Contact dermatitis is inflammation and irritation of the skin caused by contact with an irritant or allergen. The irritant may be plants (poison ivy, poison oak, or poison sumac), drugs, corrosives, acids, alkalis, latex, soaps, perfumes, deodorants, materials (tape, elastic, latex), or innocuous compounds (hair dye, metals, rubber, cosmetics). Some individuals have hypersensitivity to many agents and materials that can cause contact dermatitis. Contact dermatitis is usually easily remedied, but recurrent exposure or the lack of identifying the cause can cause relapsing dermatitis. How bad the dermatitis can be may depend on the allergen or the dose of an irritant. The second exposure triggers the immune reaction and is due to a cellular-mediated response by T lymphocytes. The initial response is a release of IgE, which releases histamine, serotonin, and heparin. She is not having any shortness of breath or palpitations, she swallows well, and no swelling is 992 Chapter 40 Acute Skin Disorders noted except on her hands. While in the emergency department, she begins to show slight signs of a rash on both hands. May is allergic to latex and refers her to an allergist to have testing done for allergies. It typically involves the scalp, eyebrows, eyelids, ear canals, nasolabial folds, axillae, or trunk. A small amount of a household agent is applied to the skin far from the original area affected. The patch test is usually given by an allergy specialist to try to reproduce the eruption. Treatment should be sought if the symptoms do not go away, symptoms worsen, or the rash becomes more widespread or affects the face or genitals. If signs of infection occur, a visit to a healthcare provider is definitely needed. Steroid creams, anti-itch ointments, diphenhydramine cream or oral pill, and calamine lotions may help with some of the symptoms. Other options are applying cool, moist cloths; soaking in lukewarm water with a baking soda or oatmeal bath product; trimming nails to avoid scratching; and covering the area with a bandage to avoid scratching. The healthcare provider may order systemic corticosteroids for 2 weeks, topical immunomodulators, medicated shampoo, topical calcineurin inhibitors such as pimecrolimus and tacrolimus, and antibiotics if an infection occurs. Teaching should include good hand hygiene, avoiding dry, cracked skin from harsh soap. Emollients to avoid dryness are also recommended if frequent hand washing is required where the patient works. Exfoliative dermatitis is widespread erythema and scaling of the skin and affects at least 90% of the body surface area. The pathogenesis varies with the underlying disorder, but common to all conditions is an increased rate of skin turnover. May is sent home from the emergency department with instructions to take diphenhydramine and is given a prescription for a 5-day steroid pack. She stays home from work for 2 days, after which her hands are no longer red, itching, or swollen. May shows a severe reaction to latex and is informed that she should avoid using any products with latex. A list of products with latex are given to her, and she is prescribed an epinephrine autoinjector to carry with her at all times. She notifies her supervisor at work and asks whether she will be able to return to work. Since the skin barrier function is already impaired, the other pathogenesis is increased blood flow, which causes insensible fluid loss. Therefore, the exfoliated scales contain material that the skin normally retains (proteins, amino acids, and nucleic acids), and the result may be a negative nitrogen balance.
Buy on line malegra fxt
Primary brain injury occurs when the brain is initially injured on impact erectile dysfunction treatment mn cheapest malegra fxt, usually by blunt or penetrating trauma. The resulting damage to the brain tissues and structures is known as the primary injury. Secondary brain injury occurs as the injured brain cells begin to swell and reduce the available blood supply to the cells, robbing vital brain cells of life-saving oxygen, causing secondary cellular brain death. To understand these pressure variations in the brain, an understanding of the Monro-Kellie hypothesis is paramount. The Monro-Kellie hypothesis states that the total volume of the intracranial contents remains constant. Because the cranial vault is composed of hard fused bones, the cranial vault is a closed system. Inside this vault lie three major components: brain mass, intracerebral spinal fluid, and blood volume. For homeostasis to be maintained within the brain, all three components must be adequately perfused with oxygen-rich blood, and stable pressures must exist within the cranial vault. If any of the contents of the cranial vault swell or diminish, pressures in the other two components will change to compensate. Lung sounds are significantly decreased over the injured side when compared to the opposite side. D-Disability: Neurologic Assessment A rapid neurologic assessment is performed as part of the primary survey. It is important to note that this is only one aspect of the neurologic exam and is meant to be used as a quick indicator of gross brain injury. To understand the concept of secondary brain injury, an understanding of the three pressure systems is necessary. Adequate perfusion to the brain cells must be maintained to avoid brain cell death. Although mortality rates for these patients are very low, long-term disabilities among this group can be as high as 50%. Mortality rates among this group are as high as 40%, and fewer than 10% of these patients will make even a moderate recovery. Linear and comminuted fractures are isolated fractures involving a break in the skull that either follows a straight line or involves multiple fractures in the same area. Once the cellular energy stores are exhausted, normal cellular metabolism is compromised, and the cells go into a crisis state. As a result, there is an influx of sodium and water that leads to cellular edema, cellular acidosis, and an influx of calcium. When the brain cells are reperfused, cellular damage is accelerated, resulting in a reperfusion injury. Oxygen free radicals produce oxidative stress, causing further damage to the already compromised brain cells. When cells begin to die, the body naturally releases cytokines to the area of damage. There are four major types of brain herniation: uncal transtentorial, central transtentorial, cerebellotonsillar, and upward posterior fossa. These herniations occur when the swelling in the brain causes such severe pressure that brain tissues press on the fossa in the brain, causing the brain to extend outside its normal boundary and herniate, usually in a downward fashion. Because the skull is fixed at the superior aspect of the brain and prevents the brain from moving upward, the brain has only one place to expand: inferiorly toward the foramen magnum. Of these four types of brain herniations, the most common is the uncal transtentorial herniation, which leads to a compression of the third cranial nerve (oculomotor), causing an ipsilateral fixed and dilated pupil. As the herniation progresses, the pyramidal tract is compressed, leading to contralateral motor paralysis. Cerebellotonsillar herniation occurs when the cerebellar tonsils herniate through the foramen magnum, causing pinpoint pupils, flaccid paralysis, and sudden death. The fourth type of brain herniation, upward posterior fossa herniation, occurs from a posterior fossa lesion and results in a conjugate downward gaze with absence of vertical eye movements, pinpoint pupils, and rapid death. A cerebral contusion occurs when the brain matter directly below the injured skull is bruised. Depending on its severity, a cerebral contusion can result in a full range of brain injuries from a mild concussion to severe injury to the axons of the brain cells causing severe brain injury. Because this intracerebral hemorrhage may take hours or days to reveal itself, patients are often discharged home before the final extent of the brain injury is known. When the subarachnoid vessels are injured and bleed, blood leaks into the subarachnoid space, causing a traumatic subarachnoid hemorrhage. Patients will often complain of photophobia (eyes irritated by light) and mild meningeal signs such as headache. When a traumatic subarachnoid hemorrhage occurs, the patient has a dramatically increased likelihood of death and disability. Most epidural hematomas occur from a blunt trauma to the temporal or temporoparietal area and are often associated with a skull fracture and middle meningeal arterial disruption. The hallmark sign of an epidural hematoma is a blunt head injury resulting in a brief loss of consciousness followed by a lucid period and then unconsciousness. Because an epidural hematoma is caused by an arterial bleed, brain herniation can occur within hours and must be diagnosed and treated early if secondary brain injury is to be prevented. When the brain injury is severe enough to cause the brain to bounce around the skull, a tearing or shearing of the bridging veins often occurs, resulting in formation of a blood clot between the dura and the arachnoid mater. Because this is a venous bleed, the bleeding is slower, and it may take days or weeks for the full extent of the injury to be revealed. Treatment depends on the degree of secondary brain injury and the signs and symptoms displayed by the patient. There are three reasons for this: With aging, the brain atrophies, leaving more room for slow venous bleeding to occur and less tamponading of slow bleeds. Older adults also have friable bridging veins and small vessels, which tend to shear more easily and bleed. Older adults are also more likely to be taking anticoagulant medications, putting them at greater risk for bleeding into the brain. Warm blankets should be applied and warm fluids should be initiated to prevent hypothermia, which would further exacerbate shock. Once the primary survey has been completed and all life-threatening injuries have been identified, a more thorough secondary survey is conducted. Stone also has ecchymosis to her right parietal area and chin, along with bleeding from her left tympanic membrane. When the trauma team exposes the rest of her body, the only other injury they discover is pale, mottled feet bilaterally. In assessing the airway of a trauma patient, what other structure must be considered at the same time How do mean arterial pressure, cerebral perfusion pressure, and intracranial pressure relate to the Monro-Kellie hypothesis The healthcare provider must be careful to go back and conduct the primary survey every few minutes throughout the secondary survey to ensure that no life-threatening complications arise. E: Exposure/Environment During this final stage of the primary survey, the patient is exposed so that all areas of the body can be observed for other hidden injuries such as bruises, lacerations, impaled Head Injury Etiology and Pathogenesis Diffuse Axonal Injury. A diagnosis of mild traumatic brain injury, commonly known as concussion, is made when any alteration in cerebral function is caused by a traumatic injury to the head and results in one of the following: a brief loss of consciousness, light-headedness, vertigo, headache, nausea, vomiting, photophobia, cognitive and memory dysfunction, tinnitus, blurred vision, difficulty concentrating, amnesia, fatigue, personality change, or a balance disturbance. Approximately 50% of patients with a concussion will experience some symptoms at least 3 months after the injury, and approximately 20% will experience symptoms for 6 months or more. Patients with severe symptoms or symptoms lasting more than a few days should be referred to a neurologist for long-term care. Penetrating injuries to the neck most often result from a stab wound, gunshot wound, or sharp instrument. Blunt neck trauma is rare because the head, shoulders, and chest offer protection to the neck. Some blunt neck injuries are attributed to hyperextension, hyperflexion, rotation, and direct blows to the neck.
Buy malegra fxt 140mg amex
Chronic trichomoniasis can involve large amounts of discharge consistent with the above characteristics but slight to no vaginal mucosal inflammation erectile dysfunction instrumental order line malegra fxt. Chronic trichomoniasis is less likely to involve dyspareunia, a strawberry cervix, and postcoital bleeding. A male infected with Trichomonas vaginalis can be an asymptomatic carrier, may have mild symptomatic disease, or may have acute trichomoniasis. These three categories span the symptoms from asymptomatic to severe urethritis complicated by prostatitis. If there are symptoms, they will include some or all of the following: purulent discharge, mucoid discharge, dysuria, urethritis, testicular pain, and lower abdominal pain. Most symptomatic infections in males are intermittent and self-limiting; however, a male partner should always be treated, owing to the high likelihood of being an asymptomatic carrier. Linking Pathophysiology to Diagnosis and Treatment the history and physical examination of a woman with trichomoniasis might involve a foul, watery discharge, which is likely to be green in color and possibly frothy, and a strawberry cervix. However, because many cases of trichomoniasis have mild or nonspecific symptoms or are asymptomatic, the physical examination and history will not necessarily provide conclusive evidence of infection. The diagnosis of trichomoniasis is generally made by placing a small amount of vaginal drainage (wet mount) on a microscope slide and then examining the slide under a microscope. The key feature is microscopic identification of gyrating motile protozoan parasites. These are generally identifiable by ameboid-type movement, four flagella protruding from one side of the round or pear-shaped body of the protozoan, and one single undulating membrane extending backward from the four flagella. Again, this is not conclusive of trichomoniasis, as bacterial vaginosis also has this characteristic. A standard culture Clinical Manifestations Trichomonal infection is asymptomatic in roughly 50% of female patients and nearly 90% of male patients. The standard culture is highly sensitive but costlier and takes longer to complete than the traditional saline wet mount. Without concurrent treatment, the patient will likely be reinfected even after one event of sexual contact. The second-line treatment includes a higher dose and/or longer treatment duration of metronidazole or use of other 5-nitroimidazole medications such as tinidazole and clotrimazole. It is important to teach safe sexual practices and to instruct the patient to avoid sexual intercourse until the treatment regimen has been completed. Pediculosis Pubis Pediculosis pubis, also known as Pthirus pubis, louse (singular) or lice (plural), or the street term "crabs," is an ectoparasite (parasite that live on the outside of the body) that is spread through sexual contact, sharing of undergarments, or living in very close quarters with many other individuals, especially in unsanitary conditions. Etiology and Pathogenesis Individuals who practice safe sex with condoms are not safe from infestation with pubic lice, as condoms do not stop the spread of the parasite. However, the lice cannot be spread by a toilet seat, as is a common myth, as they cannot live for a long time without a warm human host body, and they have trouble moving along flat, smooth surfaces because of their anatomy. The Pthirus pubis is whitish-gray and oval-shaped, with a short broad body and large front claws, which contribute to the street name of "crabs. The nits (eggs) of the louse attach to hair shafts and/or the fibers of clothing and bed linens with a strong, durable, insoluble cement, which contributes to failures in treatment and reinfestation in individuals. Much like trichomoniasis, pediculosis pubis is not a reportable disease, so accurate numbers are difficult to obtain. Another clinical finding in patients with a pubic louse infection is the presence of maculae ceruleae, which are pathognomonic for pubic lice. A maculae ceruleae is a bluish-gray macule that signifies a bite from the louse on the skin. Crusts and pinpoint blood staining of the underwear can also be noted, with or without the presence of maculae ceruleae. Other, less common signs and symptoms include inguinal lymphadenopathy and axillary lymphadenopathy. It is important to note that the microscopy of nits is not diagnostic of an active infestation; however, if nits are found in or near a hairy region on the patient, active infestation is likely. Cellulose tape can be applied over an infested area to pick up lice and nits for microscopic examination. A Wood light examination can be done on infested areas to illuminate lice and nits, which will glow a yellow-green color. Permethrin is highly effective against live lice; however, it will not penetrate unhatched nits. A second treatment with permethrin is recommended roughly 9 days after the first treatment to kill any newly hatched nits to prevent another life cycle. Delaying or omitting this second treatment can lead to the new lice laying more nits, which will contribute to reinfestation. Usually, the pruritus or spotting of the parasite or nits (eggs) is the principal reason for a patient to seek healthcare advice and treatment. Excoriations commonly accompany the 1216 Chapter 49 Sexually Transmitted Infections stray lice. Any items that cannot be washed need to be disposed of or placed in a garbage bag for a period of no less than 2 weeks. Genital manifestations include small vesicles located in the genital area, often accompanied by pain. A common diagnostic measure for chlamydia is the evaluation of a urine sample; the primary means of treatment is providing a single dose of azithromycin or doxycycline for 1 week. Neisseria gonorrhoeae has surface pili that prevent the organism from being phagocytized by neutrophils. Treatment guidelines for gonorrhea recommend the use of two antibiotics: an intramuscular injection of ceftriaxone and an oral dose of azithromycin. The spirochete Treponema, in particular Treponema pallidum, causes infection as a result of contact with open lesions known as chancres. Review Questions 1217 Without appropriate intervention, syphilis will progress through four stages: primary, secondary, latent, and tertiary. Pharmacologic treatment remains the main approach, intramuscular penicillin being the antibiotic of choice. Pediculosis pubis, also known as Pthirus pubis, louse (singular) or lice (plural), or the street term "crabs," is an ectoparasite (parasite that live on the outside of the body) that is spread through sexual contact, sharing of undergarments, or living in very close quarters with many other individuals, especially in unsanitary conditions. Clinical manifestations of pediculosis pubis are similar in males and females, the predominant symptom being pruritus in the affected area or areas. Typically, pediculosis pubis can be treated with overthe-counter permethrin (usually 1%) lotion and sometimes a mousse-type application with a combination of medications. Trichomonal infection is often asymptomatic, so laboratory tests are needed to confirm diagnosis. A 37-year-old woman who is pregnant for the first time comes to the clinic for her regular checkup. She is informed about the need for routine testing for sexually transmitted infections. A bacterial infection of columnar epithelial cells of the urinary tract causing dysuria c. A spirochete that penetrates the central nervous system and results in chancres d. An ectoparasite that is whitish-gray and oval-shaped with a short, broad body and large front claws 3. A 23-year-old woman presents to the clinic with complaints of pain with urination and intercourse and discharge coming from her vagina. A 76-year-old man presents to the clinic and is diagnosed with secondary syphilis. Fever, alopecia, arthralgia, lymphadenopathy, and rash on the palms of the hands 5. How would you prepare her, in terms of education and follow-up, to monitor for the potential complications of this condition She will require follow-up in 6 months to screen for the possible development of genital malignancies. She will need to monitor for eruption of small vesicles around the genital area that are painful. She will require follow-up in 1 year to assess for the presence of chancres and meningitis. He states that the previous week, he experienced a fever, headache, and general muscle aches for a few days before the eruption of the vesicles. What is the most appropriate information for you to provide as part of the education about his treatment
Malegra fxt 140 mg visa
Wounds may also be described as partial or full thickness on the basis of the depth of the injury reasons erectile dysfunction young age generic malegra fxt 140 mg amex. A partial thickness wound is one in which damage extends through the epidermis while all or a portion the dermis remains intact. Partial thickness wounds are predominantly repaired by reepithelialization, a process whereby epithelial cells migrate to the area and replicate by mitosis. A full thickness wound is one involving extension of damage through the epidermis and the entire thickness of the dermis, with possible extension into subcutaneous tissue, muscle, and bone. The phenomenon of wound healing, also referred to as tissue repair, is a dynamic and complex yet somewhat predictable process. Because most organs in the body are capable of tissue repair in a manner similar to that in the skin, cutaneous wound healing is used as the prototype in this chapter. Each phase of the process is directed by cells that secrete chemical mediators that direct the healing process. These cells include neutrophils, macrophages, lymphocytes, platelets, keratinocytes, fibroblasts, and endothelial cells. The chemical mediators include a significant number of growth factors and cytokines, substances secreted by cells that help cells to communicate with each other and coordinate the healing process. The profile of cell types and chemical mediators at the site of injury changes as the healing processes unfolds. Although many wounds heal without complications, a variety of local and systemic factors can impede wound healing. Nutritional deficits and inadequate hydration status place an individual at risk through the loss of skin turgor and necessary vitamins necessary for proper wound healing. Increased pressure in these areas restricts blood flow, resulting in ischemic damage and tissue necrosis, manifesting as pressure injuries. A lack of adequate perfusion to distal extremities can cause arterial or venous ulceration. Furthermore, wounds sometimes result in a lack of skin integrity, placing the individual at risk for development of infection, which can complicate the healing process. Case Studies To reinforce important clinical concepts regarding tissue and wound healing, the following cases will be addressed throughout the chapter to assist in application of chapter content to clinical situations involving wound healing. Helen Baker: Introduction Helen Baker is 80 years old and lives in a nursing home. Baker has a history of dementia as well as Crohn disease and is taking prednisone. Within the past 3 days, her activity has been declining, and she is staying in bed. While providing incontinence care, the healthcare provider notes a dressing over Mrs. Maria King: Introduction Maria King, age 56, was diagnosed with a large polyp in her descending colon that showed severe dysplasia on biopsy. King is 5 feet 3 inches tall, weighs 220 pounds, and was diagnosed with type 2 diabetes mellitus 3 years ago. After surgery, she had a midline incision approximated with staples and a drain placed in the inferior portion of the incision. King had moderate serosanguineous output from the drain, which decreased significantly by the third postoperative day. On auscultation of the chest immediately after surgery and for the first 2 days postoperatively, Ms. King had coarse crackles in both lung fields that cleared with vigorous coughing, hourly use of an incentive spirometer, and frequent reminders and coaching by the nurses. At that time, her drain had been removed, and she had minimal incisional drainage. However, the discharge nurse noted redness around the lower two thirds of the incision and a superficial 2-cm-long separation of her incision at midpoint. On inspection of the incision, the surgeon notes several areas of what appear to be partial dermal separation. On removal of the staples, dehiscence of the wound is apparent in the lower half of the incision, and a large amount of dark serosanguineous drainage is expressed. The entire lower half of the incision is opened down to the fascial layer, which is found to be intact. Explain the differences between a partial thickness wound and a full thickness wound. It contains receptors for somatic sensations, including touch, pain, and temperature. It participates in the metabolism and activation of the vitamin D in the skin when exposed to ultraviolet light. Skin in different regions of the body varies in thickness, pigment, and distribution. For example, the skin is very thick in areas of the body that are exposed to high levels of friction, such as the soles of the feet. The layers are separated by a thin layer of connective tissue called the basement membrane. Stratum corneum Stratum lucidum Stratum granulosum the Epidermis the epidermis is the visible, upper layer of skin. It is composed of multiple layers of stratified squamous epithelial cells called keratinocytes. Other cells that are present in the epidermis, but in much smaller numbers, are melanocytes, T lymphocytes, dendritic (Langerhans) cells, and tactile (Merkel) cells these cells have important specialized functions that contribute to epidermal homeostasis and repair. As they migrate from the basal layer to the skin surface, keratinocytes synthesize large amounts of keratin, a water-insoluble protein. By the time they reach the surface, all the cytoplasm has been replaced by keratin, and the cells are dry, scaly, and dead. Keratinization gives the outer layers of the epidermis a tough, horny quality that provides protection for the underlying basal layers, which contain the stem cells needed for keratinocyte regeneration. The epidermis comprises three to five layers: the stratum basale, stratum spinosum, stratum granulosum, stratum lucidum, and stratum corneum. The number varies because thick skin (such as the soles of the feet) has more layers than thin skin. It consists of a single row of stem cells that will replace keratinocytes lost on the skin surface. However, as the new cells migrate farther from the stratum basale, they receive less nourishment, resulting in cellular death. Because the skin is continually exposed to environmental stressors, the epidermis must be constantly regenerated by keratinocyte stem cells in the stratum basale. The stratum basale contains three types of cells: keratinocytes, melanocytes, and tactile (Merkel) cells. Melanocytes produce a dark pigment called melanin that is phagocytized by the keratinocytes, where it provides protection from ultraviolet rays from the sun. Light-skinned and dark-skinned individuals have the same number of melanocytes, but in darker skin and freckles, each melanocyte produces more melanin. As new keratinocytes move into the stratum spinosum, they lose their ability to divide. As the cells migrate toward the surface layers of skin, their shape changes as they flatten. Dendritic (Langerhans) cells are present in both the stratum spinosum and the stratum granulosum. These cells are types of macrophages that engulf pathogenic microorganisms entering from the skin surface. In the stratum granulosum, keratinohyalin granules dehydrate and break up the nucleus, causing the cells undergo an orderly, genetically programmed death called apoptosis. These granules contain substances that combine with components of the cytoskeleton of the keratinocyte and convert them to keratin.
Buy malegra fxt us
Maintenance of a pool of bile acids is essential to normal fat absorption and bile secretion impotence tumblr buy genuine malegra fxt. For adults and children beyond infancy, newly synthesized bile acids account for approximately 20% to 25% of the total bile acid pool. Once synthesized by hepatocytes, bile acids are excreted into the canalicular lumen. In addition to bile acids, a sodium ion is excreted, which creates a gradient to passively draw water into the biliary canaliculi. Although bile acids make up the major solute of bile, other components include phospholipids, organic anions, inorganic anions (especially chloride), and cholesterol. In the proximal small bowel, bile acids form mixed micelles with dietary lipolytic products, fatty acids, and monoglycerides. Cholesterol, phospholipids, and fat-soluble vitamins are also solubilized in a similar manner. The lipolytic products are absorbed in the proximal small intestine with reabsorption of bile acids in the distal intestine. Bile acids may be reabsorbed by either passive nonionic diffusion along the length of the gastrointestinal tract or by a sodium-dependent mechanism in the ileum. The synthesis of these acids occurs through a tightly regulated enzymatic cascade within hepatocytes involving at least 14 different enzymes. Both pathways work to convert a hydrophobic cholesterol molecule into hydrophilic primary bile acids. The neutral pathway of bile acid biosynthesis involves the formation of a cholic acid-to-chenodeoxycholic acid ratio of approximately 1:1. Although the neutral pathway is believed to be the quantitatively more important pathway of bile acid synthesis, the alternative pathway is likely more functional early in life, and alterations in this pathway may have devastating consequences. On initial entry into the small intestines, bile acids have a net negative charge. As the bile acids pass through the more distal small intestine, they are deconjugated by the colonized bacteria. This deconjugation confers a neutral charge on the bile acids and thus permits rapid uptake by intestinal endothelial cells via passive diffusion. Primary bile acids synthesized in liver from cholesterol, and the secondary bile acids produced by bacterial 7-dehydroxylation. With each of the 8 to 12 enterohepatic cycles every day, there is a loss of approximately 3% to 5% of the pool of bile acids with each cycle, largely due to efficient absorption by the combination of passive and active transport systems in the intestine. A fraction of bile acids in the pool escapes reabsorption in the small intestine and is delivered to the large intestine where bacterial transformation of the bile acids occurs. Although the amount varies by diet and individual, in the adult, up to 30 g of bile acids are reabsorbed by the intestines, with 0. The bile acids lost in the stool are replaced by newly synthesized bile acids in the liver through a tightly controlled negative feedback system. This feedback inhibition mechanism ensures that the bile acid pool remains constant in healthy humans, with adequate bile acids to promote bile flow, micelle formation, and cholesterol excretion. Bile acids enter the portal venous system through absorption by intestinal endothelial cells. These bile acids are bound to albumin and other proteins as they are transported in the portal vein to the liver. Most of the reuptake is performed by periportal hepatocytes, which then secrete the bile acids into the canalicular space, the rate-limiting step of bile acid transport. A small fraction of the circulating bile acids in the portal blood escapes removal by the hepatocytes and spills over into the systemic circulation. Small arrows indicate passive intestinal absorption, whereas the large arrow in the ileum represents the active uptake of bile acids. A small fraction of the bile acids spills over into the systemic circulation and is excreted by the kidneys. The postprandial rise of bile acids serves as a reasonable indicator that the enterohepatic circulation is intact. The serum bile acids undergo filtration by the kidney and can be either excreted in the urine or reabsorbed in the renal tubules for transport back to the liver. A maturation process occurs within the fetal liver and continues throughout the first year of life; this process effectively increases the amount of bile acids available for digestion. These "atypical" bile acids have additional sites of hydroxylation, which may be important in the pathogenesis of cholestatic liver disease in the neonate. When corrected for differences in body surface area, both term and preterm normal newborn infants have reduced rates of cholate synthesis and a reduced bile acid pool size compared to normal adults. For preterm infants younger than 33 weeks of gestation, the gallbladder contraction index may be nonexistent to less than 50%. Over the first months of life, the bile acid synthetic rate increases and the pool expands, with concurrent increase in intraluminal bile acid concentrations. In fact, the serum bile acid concentration during the first 6 months of life is as high as in adults who have clinical cholestasis. An improvement in the hepatic uptake of bile acids occurs over the first year of life and corresponds to a decrease in the peripheral serum bile acid concentration. Levels of serum bile acids in infants decrease into the normal range by approximately 10 months of age. The secondary bile acids, lithocholic acid and deoxycholic acid, appear in both the serum and bile of infants undergoing intestinal microflora colonization. Alterations may occur at the level of primary bile acid synthesis, in the transport of bile acids across the hepatocyte, at the level of secondary bile acid synthesis, or in ileal transport and the recirculation of bile acids. Secondary metabolic defects that affect primary bile acid synthesis include peroxisomal disorders such as cerebrohepatorenal syndrome of Zellweger and related disorders, and SmithLemli-Opitz syndrome. These signature metabolites are generally not detected by the routine or classic methods for bile acid measurement, and mass spectrometric techniques presently provide the most appropriate means of characterizing defects in bile acid synthesis. Characteristic features of the disease in adults include progressive neurologic dysfunction, dementia, ataxia, cataracts, and xanthomata in the brain and tendons, and in infants includes neonatal cholestasis (K. Biochemically, the disease can be distinguished from other conditions involving xanthomata by the following: (1) significantly reduced primary bile acid synthesis; (2) elevations in biliary, urinary, and fecal excretion of bile alcohol glucuronides; (3) low plasma cholesterol concentration, with deposition of cholesterol and cholestanol in the tissues; and (4) marked elevations in cholestanol. The liver histopathologic findings in these young patients are similar to those observed in idiopathic neonatal hepatitis. The liver histologic findings are those of hepatitis, the presence of giant cells, and cholestasis. Although the earliest cases were identified in infants, increasingly, idiopathic late-onset chronic cholestasis has been explained by this disorder. In such patients, liver disease is not always evident initially, and patients may have fat-soluble vitamin malabsorption and rickets, which are corrected with vitamin supplementation. Serum liver enzymes that are often normal in the early stages of the disease later show progressive increases with evidence of progressive hepatic fibrosis. Infants with 4-3-oxosteroid 5-reductase deficiency tend to have more severe liver disease with rapid progression to cirrhosis and death without intervention. The 4-3oxosteroid 5-reductase deficiency has since been found in a number of patients presenting with neonatal hemochromatosis. Liver histologic and ultrastructural pathology findings include marked lobular disarray as a result of giant cell and pseudoacinar transformation of hepatocytes, hepatocellular and canalicular bile stasis, and extramedullary hematopoiesis with small bile canaliculi that are sometimes slitlike in appearance and show few or 3-Hydroxy-C27-Steroid Oxidoreductase Deficiency this was the first metabolic defect to be described involving an early step in the bile acid biosynthetic pathway; 7-hydroxycholesterol is converted to 7-hydroxy-4cholesten-3-one, a reaction catalyzed by a 3-hydroxyC27-steroid oxidoreductase. The liver injury in this defect is presumed to be the consequence of the diminished primary bile acid synthesis and the hepatotoxicity of the accumulated 4-3-oxo bile acids. The lack of canalicular secretion can be explained by the relative insolubility of oxo-bile acids and the cholestatic effects of the taurine conjugate of 7-dihydroxy-3-oxo-4-cholenoic acid. In the first infant described with the 2-methylacylCoA racemase deficiency, the liver from a 5 1 2 -month-old sibling, who 2 years previously had died from an intracranial bleed. In addition, dietary restriction of phytanic acid and pristanic acids is likely to be necessary in the long term for such patients to prevent neurotoxicity from accumulation of these fatty acids in the brain. Oxysterol 7-Hydroxylase Deficiency the recent discovery of a genetic defect in oxysterol 7-hydroxylase31 establishes the acidic pathway as a quantitatively important pathway for bile acid synthesis in early life. In humans, oxysterol 7-hydroxylase may be more important than cholesterol 7-hydroxylase for bile acid synthesis in early life. This defect has been reported in a 10-week-old boy, whose parents were first cousins, who presented with severe progressive cholestasis, hepatosplenomegaly, cirrhosis, and liver synthetic failure from early infancy. Liver biopsy findings included cholestasis, bridging fibrosis, extensive giant cell transformation, and proliferating bile ductules. The patient subsequently died after orthotopic liver transplantation at age 4 1 2 months. The accumulating monohydroxy bile acids with the 3-hydroxy-5 structure have been shown previously to be extremely cholestatic.