Buy generic ropinirole line
Imaging studies that define the pathology should be present in the operative suite to define anatomy and symptoms zinc deficiency cheap ropinirole online master card, in conjunction with preoperative site marking, minimize the risk of wrong-side surgery. Angiography, embolization, and stent placement are not routine for laparoscopic renal surgery but may be undertaken in preparation for specific pathologies or procedures. The well-documented advantages of laparoscopy compared with open surgery including reduced postoperative pain, decreased analgesic requirements, and more rapid convalescence are particularly welcome in elderly patients who are often at higher risk of perioperative complications. Limited nutritional, pulmonary, and cardiovascular reserve relative to younger patients gives rapid convalescence particular importance in this patient population. Minimization of narcotic use, early mobilization, and physical therapy (when warranted) are important management principles in this patient population. Each approach can have discrete advantages and limitations depending on the patient factors, pathology and clinical situation, and surgeon familiarity with each approach. To date, no studies have shown a definitive recuperative advantage of any one of these approaches. Potential differences in cosmesis may exist, but have also not been consistently demonstrated thus far. The pneumoperitoneum can affect patients with severe cardiopulmonary disease by compromising ventilation and venous return (Arthure, 1970; Hodgson et al, 1970; Nunn, 1987; Lew et al, 1992). Patients with chronic pulmonary disease may not be able to compensate for the pneumoperitoneum-induced hypercarbia and may require working at lower pressures, use of helium as an insufflant, specialized laparoscopic trocars minimizing carbon dioxide reabsorption, or open conversion (Monk and Weldon, 1992; Wolf et al, 1996; Makarov et al, 2007; Herati et al, 2009, 2011). TransperitonealApproach the transperitoneal approach is the traditional and most widely used laparoscopic method of addressing renal pathology. It provides the largest working space, facilitates orientation by providing readily identifiable anatomic landmarks, affords greater versatility in angles and location of laparoscopic trocars and instruments, and can result in the smallest size and number of ports used. The equipment is mature and techniques are well defined, but as with any approach, it requires significant expertise in instrument manipulation and suturing. A urinary drainage catheter and an orogastric tube are placed for decompression of the bladder and stomach during insufflation, trocar placement, and dissection. Sequential compression stockings are placed for deep venous thrombosis prophylaxis. Care is taken to pad all pressure points to minimize risk of nerve injury and reduce the incidence of tissue breakdown and rhabdomyolysis. The patient is secured to the operating table to allow lateral tilting of the table. Tilting the table away from the affected kidney will help move bowel out of the operative field. There is no need ConsiderationsinObesePatients Obesity is not a contraindication to laparoscopic surgery but can make retraction and identification of anatomic structures more challenging. It is for these reasons that laparoscopy in obese patients is associated with an increased risk of open conversion when compared with nonobese patients (Fazeli-Matin et al, 1999). In addition, although complication rates for laparoscopy in obese patients are higher when compared with laparoscopy in the general population (Mendoza et al, 1996; Aboumarzouk et al, 2012), pulmonary and wound complications are lower with laparoscopy when compared with an open approach (Kapoor et al, 2004; Montgomery et al, 2005). Other factors to account for in the obese population include the increased distance to the operative field, which calls for modifying trocar location and number, as well as the use of longer instrumentation (Doublet and Belair, 2000; Jacobs et al, 2000). Consideration must also be given to the weight of the pannus, which may raise the intra-abdominal pressure and further limit working space. The potential for rhabdomyolysis, a rare but devastating complication in the obese as well as very muscular individuals undergoing prolonged procedures, must also be considered (Troppmann and Perez, 2003; Glassman et al, 2007). Thelowerarmisplacedonapadded arm rest, and the other arm is flexed at the elbow and rested over thechest. The equipment in the operating room is situated to maximize the use of space and allow all members of the surgical team to view the procedure. The entire flank and abdomen are included in the field of skin preparation and draping, in case conversion to an open procedure is required. Once a pneumoperitoneum is established, three to five trocars are initially placed to complete the dissection. A variety of trocar configurations are effective for each type of renal procedure. A 12-mm trocar is placed in the anterior axillary line at the level of the umbilicus. This trocar is used for instrumentation and the passage of sutures, bulldog clamps, or staplers to secure and divide hilar vessels. In shorter patients, this may be placed in the midline, halfway between the umbilicus and pubis. A 10-mm trocar is placed at the umbilicus for camera manipulation, and a 5- or 10-mm port is inserted in the midline 2 cm below the xiphoid process. Additional trocars for retraction may be needed for visualization or assistance with organ entrapment. Additional low midline 10- or 12-mm trocars can be used for assistants to retract or use clamps or stapler devices. This low midline port site can be extended at the end of the case as a low midline extraction site. Anesthesia Monitor Surgeon Monitor Assistant Tech RetroperitonealApproach the retroperitoneal approach mimics open surgery because the peritoneal cavity is avoided. Mayo Patient Positioning and Trocar Placement With this approach, patients are placed in a full-flank position. Thescrub technician (Tech) is positioned to easily assist with instrument passageandexchange. B,Inright-sidedprocedures,theliverand bowel can be retracted through a 3- or 5-mm trocar placed in the midline. An axillary roll is required, and great care is taken in securing the patient to the bed. A 15-mm transverse incision is made in the posterior axillary line, midway between the tip of the 12th rib and the iliac crest. After the dissection is deepened downward through the lumbodorsal fascia, the retroperitoneum is entered, and a working space may be developed using blunt dissection with the tip of a finger in the space between the psoas muscle and the kidney. An alternative entry approach involves entry with the 0-degree lens and visual obturator through the initial incision. Entry into the retroperitoneum may be confirmed by the appearance of the characteristic yellow retroperitoneal fat; insufflation is initiated, and blunt dissection using only the laparoscope is performed to develop a working space. Becauseofitslowprofile,itwillnotobstructthe view or take up useful space in the retroperitoneum. Once the working space has been established through either approach, pertinent structures may be identified for orientation and additional trocar placement. Typically, a 5-mm trocar is placed just off the tip of the 12th rib, and a 12-mm trocar is placed posteriorly and superiorly relative to the camera port, both under laparoscopic visualization. The greatest limitations of the retroperitoneal approach are the limited working space and more subtle anatomic landmarks. Also, with the area of surgical dissection much closer to the lens, frequent smudging of the laparoscope tip may occur. If additional space is needed during the procedure, initial retroperitoneal access can be expanded to a transperitoneal approach by opening the peritoneum under direct vision. Despite these limitations, the retroperitoneal approach may be preferred in some cases, and with adequate experience a wide variety of laparoscopic renal surgical procedures may be performed via this approach. ModificationsforHand-AssistedLaparoscopy Hand assistance offers a bridge between open surgery and pure laparoscopy (Nakada et al, 1997). An incision large enough for the hand must be created and can also be used as an extraction site at the culmination of the case. This technique may be advantageous for the novice laparoscopist and in treating patients with significant scarring around the kidney or in cases for which a difficult dissection is anticipated. Thecameraisplacedseveral centimeters lateral to the edge of the actual hand-assisted device (nottheedgeoftheincision). Patient Positioning and Trocar Placement the patient positioning is similar to that for transperitoneal laparoscopic kidney surgery. The initial incision for the hand port is made through the skin and fascia and into the peritoneal cavity.
Buy ropinirole 0.25mg lowest price
Indeed medications 10325 discount 2mg ropinirole visa, in the last decade, washout of contrast enhancement has become a routine technique to differentiate lipid-poor adenomas from other adrenal lesions (Korobkin et al, 1998; Szolar and Kammerhuber, 1998; Szolar et al, 2005). The high diagnostic accuracy provided by biochemical evaluation and cross-sectional radiographic imaging of adrenal incidentalomas limits the indications for the routine use of functional imaging. However, functional adrenal imaging can provide valuable information when the origin of the adrenal tumor is unclear or when malignancy is highly suspected but has not been confirmed with other diagnostic modalities (Avram et al, 2006; Gross et al, 2009). Another radiotracer used to identify tumors of adrenocortical origin is carbon-11 (11C)-metomidate. Metomidate is an inhibitor of 11-hydroxylase and aldosterone synthase that is preferentially taken up by adrenocortical cells. The role of functional imaging for the diagnosis of pheochromocytoma is limited, given that most pheochromocytomas can be accurately diagnosed with cross-sectional imaging and metabolic evaluation for catecholamines and their metabolites. Rapid loss of contrast enhancement can differentiate even lipid-poor adenomas (approximately 30% of adenomas) from other lesions. In a prospectively followed multi-institutional Swedish cohort (N = 229, median follow-up 25 months), 7. All patients who underwent resection because of an increase in lesion size exhibited benign pathology (Libe et al, 2002). Similarly, an earlier review of the literature (N = 873) revealed that at a mean follow-up of 3 years, 9% of adrenal incidentalomas grew over 1 cm in diameter and a smaller number decreased in size. The authors concluded that the rate of malignant transformation of adrenal incidentalomas is approximately 1 in 1000 (Barzon et al, 2003). Reimaging at 6, 12, and, as possible, 24 months is currently recommended to verify oncologic indolence (Grumbach et al, 2003; Young, 2007b). Suspicious and unusual tumors may require imaging at earlier or more frequent intervals, whereas small (<2 cm) homogeneous, wellcircumscribed, nonfunctional lesions can be followed less closely (Young, 2007b). A rather arbitrary criterion of 1 cm of growth has been proposed as an indication for resection; however, the patient must be counseled that the chance of malignancy is low if growth kinetics are flat (Young, 2007b). Nevertheless, at presentation the median radiographic diameter of an adrenal incidentaloma is approximately 3 cm (Mantero et al, 2000). A relationship does exist between the size of an adrenal lesion and its malignant potential, with larger masses more likely to exhibit adverse clinical and pathologic features (Angeli et al, 1997). Masses smaller than 4 cm are considered to possess low malignant potential (2% are adrenal carcinomas) and, if nonfunctional, can be observed safely (Grumbach et al, 2003; Cicala et al, 2008). Masses that exceed 6 cm should be considered malignant until proven benign, which usually requires definitive resection. In this intermediate size range, the rate of malignancy is estimated to be only 6% (Cicala et al, 2008). Nonetheless, in otherwise healthy individuals with acceptable perioperative risk profile, most experts recommend 4 cm as the cutoff diameter that warrants resection (Barry et al, 1998; Mantero et al, 2000; Young, 2000; Thompson and Young, 2003; Young, 2007b). In the largest adrenal incidentaloma series to date (N = 1004), Mantero and colleagues (2000) reported that the 4-cm cutoff afforded a 93% sensitivity and 42% specificity for detecting malignancy. Sensitivity dropped to 74% and specificity rose to 73% when a 6-cm cutoff was applied. It is important to note that the relationship between the radiographic and pathologic size of an adrenal lesion is imperfect, with pathologic assessment usually resulting in a larger measurement (Cerfolio et al, 1993; Kouriefs et al, 2001). The urologic oncologist must remember that the incidence of benign adrenal adenomas increases with age; therefore adrenal lesions in younger patients, even those smaller than 4 cm, must be managed with greater caution than similar lesions in an older patient. Likewise, lesions larger than 4 cm in older patients with significant comorbidities may be better served with observation than resection (Young, 2007b). In the absence of level 1 evidence, large population-based reports must be integrated with sound clinical judgment. Although management of masses between 4 cm and 6 cm is controversial, thought leaders in the field advise that in otherwise healthy individuals, masses 4 cm or larger should be resected. The current recommendation is to resect masses that grow over 1 cm; however, incidence of malignancy among these patients is low. BiopsyofAdrenalMasses Overview the role of adrenal biopsy has been limited for the following reasons: (1) modern imaging in the context of clinical characteristics affords superb diagnostic capabilities, (2) histologically, adenomas cannot be reliably differentiated from adrenal carcinomas, and (3) adrenal biopsy is not without risk (Thompson and Young, 2003; Young, 2007b). Nevertheless, it is useful to review data that are available with regard to safety and diagnostic usefulness of adrenal biopsy, and the procedure can occasionally be a useful tool in the diagnostic armamentarium of the adrenal surgeon. Test Characteristics of Biopsy Welch and colleagues (1994) reported on 277 percutaneous biopsies performed at the Mayo Clinic. Most biopsies in the series were performed in patients with a known nonadrenal malignancy. Larger biopsy needles (18 or 19 gauge) resulted in better diagnostic yield and equivalent complication rates when compared with biopsies performed with smaller needles. The reported positive predictive value of adrenal biopsy is high, meaning that a positive biopsy for malignancy has a high correlation on final pathology. This is especially relevant in patients with a history of an unrelated primary malignancy and in whom an adrenal metastasis is suspected (Silverman et al, 1993; Harisinghani et al, 2002). The authors reported the negative predictive value of these negative biopsy findings based on lack of tumor growth at follow-up, autopsy findings, or a rebiopsy result of 100%, although selection and research biases may have existed (Harisinghani et al, 2002). In skilled hands, nondiagnostic biopsies appear infrequent when the majority of sampling is performed with 18-gauge needles (Paulsen et al, 2004). In contrast, an adrenal mass in a patient without a previous history of malignancy and without evidence of a synchronous nonadrenal mass is highly unlikely to be present as a metastasis (Lutz et al, 2000). Instead, other criteria, such as radiographic morphology and size, must be used to characterize adrenal masses in such patients (Thompson and Young, 2003; Mazzaglia and Monchik, 2009). No Does benefit of biopsy justify risks including possibility of making laparoscopic adrenalectomy more difficult Yes Yes No role for biopsy No Yes Complications of Biopsy the complication rates of adrenal biopsies in some large series are as low as 2. Bleeding is the most common postbiopsy issue, with pneumothoraces and hemothoraces also being reported (Silverman et al, 1993; Welch et al, 1994; Quayle et al, 2007). Surgically, there has been a suggestion that biopsy, especially if followed by hemorrhage, can complicate or even prevent laparoscopic resection (Quayle et al, 2007). It is interesting to note that inadvertent biopsy of pheochromocytomas has resulted in no ill effects in some patients (Quayle et al, 2007); however, in real-world practice, due diligence to rule out pheochromocytoma before biopsy is prudent (Mazzaglia and Monchik, 2009). Algorithm summarizing decision making regarding whether to subject the patient to an adrenal biopsy. Clinical Usefulness of Biopsy Despite the fact that adrenal biopsies-when used to differentiate benign from metastatic disease-afford favorable accuracy, some clinicians argue that most adrenal biopsies performed today are unnecessary (Quayle et al, 2007; Mazzaglia and Monchik, 2009). For instance, Quayle and colleagues retrospectively reviewed their experience with patients who were sent to their tertiary referral center after an adrenal biopsy performed in the community. The researchers concluded that in no case did the biopsy affect the clinical management of these patients. Moreover, these and other investigators have raised the issue of radiology reports recommending adrenal biopsies or stating that the lesions are "amenable" to biopsy. The authors suggested that such language in radiology reports must be strongly discouraged, because it leads to unnecessary and, at times, deleterious procedures by physicians who are not familiar with standard management of the adrenal mass (Quayle et al, 2007; Mazzaglia and Monchik, 2009). In conclusion, adrenal biopsy should be pursued only when limitations of imaging have been reached and when the physician and patient are certain that the result of biopsy will influence management. Indeed, perhaps the biggest role for adrenal mass biopsy is in patients with primary malignancies that have potentially recurred in the adrenal gland and whose management will be affected by the biopsy results. This recommendation is supported by the observation that more than 10% of adrenal incidentalomas are metabolically active (see Table 65-15). Current practice is to test all new adrenal masses for cortisol and catecholamine hypersecretion. In patients with a history of hypertension, aldosterone hypersecretion should also assessed (Grumbach et al, 2003; Young, 2007b). Despite this recommendation as a standard of care, routine clinical practice remains inadequate in this domain, whereas it is estimated that more than 80% of adrenal masses do not receive appropriate evaluation (Eldeiry and Garber, 2008). Testing for Cortisol Hypersecretion A systematic review of the literature reveals that 5% to 8% of adrenal incidentalomas produce excessive glucocorticoids (Young, 2000; Barzon et al, 2003). The section on Cushing syndrome reviews the physiologic rationale for both first-line testing discussed here and other testing that may be necessary.
Buy ropinirole with mastercard
The system erroneously assumes that the sacral spinal cord is the primary reflex center for micturition medicine logo discount 0.5 mg ropinirole fast delivery. The term is used in an analogy to efferent somatic nerve fibers such as those of the pudendal nerve, which originate in the same sacral cord segment but terminate directly on pelvic floor striated musculature without the interposition of ganglia. This type of lesion is characterized by involuntary bladder contraction during filling. Involuntary bladder contraction occurs during filling, but a residual urine volume of greater than 20% of the bladder capacity is left after bladder contraction, implying obstruction in the area of the bladder outlet during the involuntary detrusor contraction. This obstruction is generally due to striated sphincter dyssynergia, typically occurring in patients who are paraplegic or quadriplegic with lesions between the cervical and the sacral spinal cord. Smooth sphincter dyssynergia may be seen as well in patients with lesions above the level of T6, usually associated with autonomic hyperreflexia (see Chapter 75). Detrusor areflexia results, and whatever measures the patient may use to increase intravesical pressure during attempted voiding are insufficient to decrease residual urine to less than 10% of bladder capacity. This classification system applies best to spinal cord injury patients with complete neurologic lesions after spinal shock has passed. It is difficult to apply to patients with multicentric neurologic disease and cannot be used at all for patients with non-neurologic disease. The system fails to reconcile the clinical and urodynamic variability exhibited by patients who, by neurologic examination alone, seem to have similar lesions. The period of spinal shock that immediately follows severe cord injury is generally associated with bladder areflexia, whatever the status of the sacral somatic reflexes. Finally, although the terms balanced and imbalanced are helpful, in that they describe the presence or absence of a certain relative percentage of residual urine, they do not imply the true functional significance of a lesion, which depends on the potential for damage to the lower or upper urinary tracts and on the social and vocational disability that results. A muscular lesion can involve the detrusor itself, the smooth sphincter, or any portion, or all, of the striated sphincter. Detrusor dysfunction is the most common and generally results from decompensation following long-standing bladder outlet obstruction. Loop 1 consists of neuronal connections between the cerebral cortex and the pontine mesencephalic micturition center; this coordinates voluntary control of the detrusor reflex. Loop 1 lesions are seen in conditions such as brain tumor, cerebrovascular accident or disease, and cerebral atrophy with dementia. Loop 2 includes the intraspinal pathway of detrusor muscle afferents to the brainstem micturition center and the motor impulses from this center to the sacral spinal cord. Loop 2 is thought to coordinate and provide for a detrusor reflex of adequate temporal duration to allow complete voiding. Partial interruption by spinal cord injury results in a detrusor reflex of low threshold and in poor emptying with residual urine. Spinal cord transection of loop 2 acutely produces detrusor areflexia and urinary retention-spinal shock. Loop 3 consists of the peripheral detrusor afferent axons and their pathways in the spinal cord; these terminate by synapsing on pudendal motor neurons that ultimately innervate periurethral striated muscle. Loop 3 was thought to provide a neurologic substrate for coordinated reciprocal action of the bladder and striated sphincter. Loop 3 dysfunction could be responsible for detrusor striated dyssynergia or involuntary sphincter relaxation. Loop 4A is the suprasacral afferent and efferent innervation of the pudendal motor neurons to the periurethral striated musculature. Loop 4B consists of afferent fibers from the periurethral striated musculature that synapse on pudendal motor neurons in Onuf nucleus-the segmental innervation of the periurethral striated muscle. Bradley conceptualized that, in contrast to the stimulation of detrusor afferent fibers, which produced inhibitory postsynaptic potentials in pudendal motor neurons through loop 3, pudendal nerve afferents produced excitatory postsynaptic potentials in those motor neurons through loop 4B. These provided for contraction of the periurethral striated muscle during bladder filling and urine storage. The related sensory impulses arise from muscle spindles and tendon organs in the pelvic floor musculature. Abnormalities of the suprasacral portion result in abnormal responses of the pudendal motor neurons to bladder filling and emptying, manifested as detrusor striated sphincter dyssynergia and/or loss of the ability to contract the striated sphincter voluntarily. The Bradley system is sophisticated and reflects the ingenuity and neurophysiologic expertise of its originator, himself a neurologist. For neurologists, this method may be an excellent way to conceptualize the neurophysiology involved, assuming that there is agreement on the existence and significance of all four loops-a big assumption. Urodynamically, it may be extremely difficult to test the intactness of each loop system, and multicentric and partial lesions are difficult to describe. Hald-BradleyClassification Hald and Bradley (1982) described what they termed a simple neurotopographic classification (Box 70-9). A supraspinal lesion is characterized by synergy between detrusor contraction and the smooth and striated sphincters, but defective inhibition of the voiding reflex exists. Involuntary bladder contraction generally occurs, and sensation is usually preserved. However, depending on the site of the lesion, detrusor areflexia and defective sensation may be seen. Report from the standardization subcommittee of the International Continence Society. Physiological and pathological regulation of the autonomic control of urinary bladder contractility. Pharmacology of the lower urinary tract: basis for current and future treatments of urinary incontinence. Morphological and physiological characteristics of urethral circular and longitudinal smooth muscle. Neurophysiology of micturition and its modifications in animal models of human disease. Additionally, incontinence creates a tremendous cost to the individual and to society. Hu and colleagues (2004) estimated that the evaluation and management of incontinence and productivity lost as a result of the condition resulted in a $19. The decrease was speculated to be due to various factors, including decreased hospital stays and adjusted methods of assessing nursing home stays, routine care product use, and prevalence data. Other reports have demonstrated that medical expenditures for incontinence in the female Medicare population nearly doubled between 1992 and 1998, the result primarily of increased outpatient expenditure from 9. Milsom and colleagues (2014) reported a cost of $66 billion per year for urinary urgency incontinence in 2007, and Ganz and coworkers (2010) projected a total annual cost of $76. The importance of evidence-based medicine and meticulous follow-up of patients is driving improvement in the science on which advancements in this subspecialty of urology are being made. The purpose of evaluation of patients with urinary incontinence includes documentation and characterization of the incontinence, consideration of the differential diagnosis, prognostication and facilitation of treatment selection (Dmochowski et al, 2010). The type of incontinence affecting an individual must be defined and quantified to guide proper treatment planning. Transient or unrelated conditions that can cause leakage should be identified before proceeding with definitive therapy. The terminology continues to adjust to reflect the evolving understanding of the condition. The importance of this flexibility has been realized and acknowledged by leaders in the subspecialty of pelvic floor medicine (Chapple, 2009). Simply put, anterior compartment prolapse (cystocele) generally involves descent of the bladder toward the vaginal lumen, posterior prolapse (rectocele) involves the rectum compressing the posterior vaginal wall into the vagina, and apical prolapse is associated with descent of the uterus (uterine procidentia) and/or the bowel (enterocele) at the top of the vagina. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-Committee of the International Continence Society. Past Medical and Surgical History Past medical and surgical histories are vital to the assessment of incontinence insofar as medical conditions and surgeries can affect urinary tract function. Childhood and adult urologic history should be obtained, as should a neurologic history. In women, the gynecologic and obstetric history, including gravity, parity, and hormonal status is important. Determination of whether the patient is premenopausal, perimenopausal, or postmenopausal and whether she has used any exogenous hormones such as oral contraceptives or local or systemic hormone replacement therapy can be helpful in her overall assessment. Similarly, a history of prostate surgery can give rise to voiding or leakage complaints in men. Abdominoperineal resection can result in neurologic injury that can affect the function of either the bladder or the sphincter (Petrelli et al, 1993), and back surgery can cause a variety of symptoms depending on the level affected.
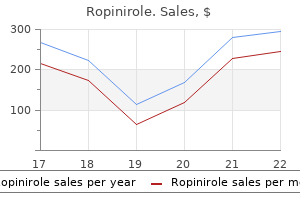
| Comparative prices of Ropinirole | ||
| # | Retailer | Average price |
| 1 | Wal-Mart | 354 |
| 2 | Lowe's | 226 |
| 3 | Subway | 404 |
| 4 | Dick's Sporting Goods | 839 |
| 5 | Office Depot | 133 |
| 6 | Kohl's | 312 |
Order cheap ropinirole on-line
Immunity to nerve growth factor prevents afferent plasticity following urinary bladder hypertrophy treatment 02 bournemouth generic 0.5mg ropinirole mastercard. Nerve growth factor in the urinary bladder of the adult regulates neuronal form and function. M(3)receptor knockout mice: muscarinic receptor function in atria, stomach fundus, urinary bladder, and trachea. Effect of partial outlet obstruction on rabbit urinary bladder smooth muscle function. Influence of hypertension on lower urinary tract symptoms in benign prostatic hyperplasia. The central neural pathways involved in micturi tion in the neonatal rat as revealed by the injection of pseudorabies virus into the urinary bladder. Upregulation of P2X3 receptor during stretch of bladder urothelial cells from patients with interstitial cystitis. A new look at detrusor underactivity: impaired contractility versus afferent dysfunction. Resiniferatoxin and its analogs provide novel insights into the pharmacology of the vanilloid (capsaicin) receptor. After a decade of intravesical vanilloid therapy: still more questions than answers. Effect of capsaicin, resiniferatoxin and piperine on ethanol induced gastric ulcer of the rat. Gap junction channel activity in shortterm cul tured human detrusor myocyte cell pairs: gating and unitary conduc tances. Expression of smooth muscle myosin isoforms in urinary bladder smooth muscle during hypertrophy and regression. The effects of changing urinary composition on silent afferents in the rat bladder. Role of alpha1 and alpha2 adrenocep tors in the sympathetic control of the proximal urethra. Treatment with oral piperazine oestrone sul phate for genuine stress incontinence in postmenopausal women. Bladder dysfunction in Parkinsonism: mechanisms, prevalence, symptoms, and management. The ultrastucture of bladder lamina propria nerves in healthy subjects and patients with detrusor hyperreflexia. Over expression of stem cell homing cytokines in urogenital organs following vaginal distention. Effect of pH on myofilament Ca(2+)sensitivity in alphatoxin permeabilized guinea pig detrusor muscle. In vitro binding of type 1fimbriated Escherichia coli to uroplakins Ia and Ib: relation to urinary tract infections. Characterization of mouse lumbar splanchnic and pelvic nerve urinary bladder mechanosensory afferents. Functional contribution of autonomic innervation to urethral striated sphincter: studies with parasympathomimetic, para sympatholytic and alpha adrenergic blocking agents in spinal cord injury and control male subjects. Contribution of tachykinin receptor sub types to micturition reflex in guinea pigs. Colonic irritation in the rat sensitizes urinary bladder afferents to mechanical and chemical stimuli: an afferent origin of pelvic organ crosssensitization. Contractile and cytoskeletal proteins in detrusor muscle from obstructed rat and human bladder. Collagen content in the rat urinary bladder sub jected to infravesical outflow obstruction. Enhancement of detrusor reflex activity by naloxone in patients with chronic neurogenic bladder dysfunction. Transneuronal labeling from the rat distal colon: anatomic evidence for regulation of distal colon function by a pontine corticotropinreleasing factor system. Duloxetine versus placebo in the treat ment of European and Canadian women with stress urinary incontinence. Alterations in neuropeptide expression in lumbosacral bladder pathways following chronic cystitis. Increased expression of neuronal nitric oxide synthase in bladder afferent pathways following chronic bladder irrita tion. Urinary incontinence in postmenopausal women treated with oestrogens: a double blind clinical trial. Role of spinal alpha(1)adrenergic mecha nisms in the control of lower urinary tract in the rat. Agerelated differential susceptibility to calcium channel blocker and low calcium medium in rat detrusor muscle: response to field stimulation. Sensitization of pelvic afferent nerves in the in vitro rat urinary bladderpelvic nerve preparation by purinergic agonists and cyclo phosphamide pretreatment. Mechanotransduction and chemosensi tivity of two major classes of bladder afferents with endings in the vicinity to the urothelium. Voiding function and dysfunction: relevant anatomy, physiology, pharmacology and molecular biology. Multiple P2X receptors on guineapig pelvic gan glion neurons exhibit novel pharmacological properties. Exogenous overexpression of nerve growth factor in the urinary bladder produces bladder overactivity and altered micturition circuitry in the lumbosacral spinal cord. Threedimensional distribution of sub stance Plike immunoreactivity in the urinary bladder of rat. Age related changes in the functional, biochemi cal and molecular properties of alpha1adrenoceptors in the rat genito urinary tract. Effects of age and hypertension on alpha1 adrenoceptors in the major source arteries of the rat bladder and penis. Agerelated changes in cholinergic and puriner gic neurotransmission in human isolated bladder smooth muscles. Bladder afferent pathway and spinal cord injury: possible mechanisms inducing hyperreflexia of the urinary bladder. Bladder overactivity and hyperexcitability of bladder afferent neurons after intrathecal delivery of nerve growth factor in rats. Increased excitability of afferent neurons inner vating rat urinary bladder after chronic bladder inflammation. Nitric oxide modulates Ca(2+) channels in dorsal root ganglion neurons innervating rat urinary bladder. Supraspinal and spinal alphaamino3 hydroxy5methylisoxazole4propionic acid and NmethylDaspartate 70 Pathophysiology and Classification of Lower Urinary Tract Dysfunction: Overview Alan J. For the purposes of description and teaching, the micturition cycle is best divided into two relatively discrete phases: bladder filling/urine storage and bladder emptying/voiding. The micturition cycle normally displays these two modes of operation in a simple on-off fashion. The cycle involves switching from inhibition of the voiding reflex and activation of the storage reflexes to inhibition of the storage reflexes and activation of the voiding reflex and back again. A simple way of looking at the pathophysiology of all types of voiding dysfunction is then presented, followed by a discussion of various systems of classification and categorization. Consistent with my own philosophy and prior attempts to make the understanding, evaluation, and management of voiding dysfunction as logical and simple as possible (Wein, 1981; Wein and Barrett, 1988; Wein, 2002), a functional and practical approach is favored. As an apology and explanation to significant contributors to the field whose works have not been specifically referenced by name as frequently as they could have been, citations have been chosen primarily because of their comprehensive review or informational content and not because of originality or initial publication on a particular subject except where noted. The first is that the micturition cycle involves two relatively discrete processes: (1) bladder filling and urine storage and (2) bladder emptying or voiding. The second is that, whatever the details involved, one can succinctly summarize these processes from a conceptual point of view as follows: Bladder filling and urine storage require: Accommodation of increasing volumes of urine at a low detrusor pressure (normal compliance) and with appropriate sensation. A bladder outlet that is closed at rest and remains so during increases in intra-abdominal pressure.
Order ropinirole 0.25 mg on-line
Aging and overactive bladder may be associ ated with loss of urethral sensation in women medicine used for uti generic 1mg ropinirole with visa. Tolterodine causes measurable restoration of urethral sensation in women with urge urinary incontinence. Functional brain imaging and the bladder: new insights into cerebral control over micturition. Action potentials and net membrane currents of isolated smooth muscle cells (urinary bladder of the guineapig). The autonomic innervation of the human urinary bladder, bladder neck and urethra: a histochemical study. Plateletderived growth factor receptor cells in mouse urinary bladder: a new class of interstitial cells. Immunohistochemical study on the localiza tion of serotonin fibers and terminals in the spinal cord of the monkey (Macaca fuscata). Urinary retention associated with a unilateral lesion in the dorsolateral tegmentum of the rostral pons. Characterization of changes in urodynamic variables 12 months after retropubic and transobturator midurethral sling surgery and effect on surgical outcomes. Influence of spinal cord injury on the morphology of bladder afferent and efferent neurons. Spinal pathways mediate coordinated bladder/ urethral sphincter activity during reflex micturition in decerebrate and spinalized neonatal rats. Pontine control of the urinary bladder and external urethral sphincter in the rat. Effects of imatinib mesylate (Glivec) as a ckit tyrosine kinase inhibitor in the guineapig urinary bladder. Motor and inflammatory effect of hyperosmolar solutions on the rat urinary bladder in relation to capsaicinsensitive sensory nerves. Further studies on the mechanisms of the tachykinininduced activation of micturition reflex in rats: evidence for the involvement of the capsaicinsensitive bladder mechanoreceptors. Differential effects of intravesical resiniferatoxin on excitability of bladder spinal neurons upon colonbladder cross sensitization. Urinary retention in bilateral pontine tumour: evidence for a pontine micturition centre in humans. Forebrain projections to the periaqueductal gray in the monkey, with observations in the cat and rat. A randomized doubleblind placebo controlled phase 2 doseranging study of onabotulinumtoxinA in men with benign prostatic hyperplasia. Gating of maxi K+ channels studied by Ca2+ concentration jumps in excised insideout multichannel patches (myo cytes from guinea pig urinary bladder). Identification of central nervous system neurons that innervate the bladder body, bladder base, or external urethral sphincter of female rats: a transneuronal tracing study using pseudorabies virus. Central nervous system innervation of the penis, prostate, and perineal muscles: a transneuronal tracing study. Inhibitory roles of peripheral nitrergic mechanisms in capsaicininduced detrusor overactivity in the rat. Mice lacking M2 and M3 muscarinic acetyl choline receptors are devoid of cholinergic smooth muscle contractions but still viable. Contribution of opioid and metabotropic gluta mate receptor mechanisms to inhibition of bladder overactivity by tibial nerve stimulation. Adrenoceptors and cholinoceptors con trolling noradrenaline release from adrenergic nerves in the urethra of rabbit and man. Control of reflex detrusor activity in normal and spinal injured nonhuman primates. Regulation of acetylcholine release from guineapig bladder urothelial cells-potential role in bladder filling sen sations. Impact of parturition on chemokine homing factor expression in the vaginal distention model of stress urinary incontinence. Focal hypoxia of the obstructed rabbit bladder wall correlates with intermediate decompensation. Estrogeninduced alterations in the autonomic responses of the rabbit urinary bladder. Structural changes in the aging submucosa: new mor phologic criteria for the evaluation of the unstable human bladder. Increased urine and serum nerve growth factor levels in interstitial cystitis suggest chronic inflammation is involved in the patho genesis of disease. Urinary nerve growth factor level is increased in patients with interstitial cystitis/bladder pain syndrome and decreased in responders to treatment. Increased nerve growth factor levels in the urinary bladder of women with idiopathic sensory urgency and interstitial cystitis. Anatomical basis for nervesparing radical hys terectomy: immunohistochemical study of the pelvic autonomic nerves. Interrelationships of bladder compliance with age, detrusor instability, and obstruction in elderly men with lower urinary tract symptoms. The dual, sensory and efferent function of the capsaicinsensitive primary sensory nerves in the bladder and urethra. The influence of afferent inputs from skin and viscera on the activity of the bladder and the skeletal muscle surrounding the urethra in the rat. Localization of M2 and M3 muscarinic receptors in human bladder disorders and their clinical correlations. Increased cannabinoid receptor 1immunoreactive nerve fibers in overactive and painful bladder disorders and their correla tion with symptoms. Induction and evasion of host defenses by type 1piliated uropathogenic Escherichia coli. Threedimensional arrangement of collagen and elastin fibers in the human urinary bladder: a scanning electron microscopic study. Cyclophosphamide induced cystitis alters neuro trophin and receptor tyrosine kinase expression in pelvic ganglia and bladder. A randomized crossover study to evaluate Ro 1151240, a selective alpha1A/1Ladrenoceptor partial agonist in women with stress urinary incontinence. Location and morphology of parasympa thetic preganglionic neurons in the sacral spinal cord of the cat revealed by retrograde axonal transport of horseradish peroxidase. Central nervous system neurons labelled follow ing the injection of pseudorabies virus into the rat urinary bladder. Early molecularlevel changes in rat bladder wall tissue following spinal cord injury. Detrusor smooth muscle cells of the guineapig are functionally coupled via gap junctions in situ and in cell culture. Agedependent alterations in betaadrenergic responsiveness of rat detrusor smooth muscle. Comparison of two alpha1adrenoceptor antago nists, naftopidil and tamsulosin hydrochloride, in the treatment of lower urinary tract symptoms with benign prostatic hyperplasia: a randomized crossover study. A model for the study of visceral pain states: chronic inflammation of the chronic decerebrate rat urinary bladder by irritant chemicals. Brain stem influences on the parasympathetic supply to the urinary bladder of the cat. Alpha1, alpha2 and betaadrenoceptors in the urinary bladder, urethra and prostate. Microvascular architecture of the human urinary bladder wall: a corrosion casting study. Effect of duloxetine, a norepinephrine and sero tonin reuptake inhibitor, on sneezeinduced urethral continence reflex in rats. Herpes simplex virus vectormediated gene delivery of glutamic acid decarboxylase reduces detrusor overactivity in spinal cordinjured rats. The segmental detailed topographical distribution of mono aminergic terminals and their pathways in the spinal cord of the cat.
Ropinirole 0.25mg discount
Opening time: the elapsed time from original rise in detrusor pressure to onset of flow medicine bow wyoming cheap ropinirole 0.25 mg without a prescription. Pressure at maximum flow: the lowest pressure recorded at maximum measured flow rate. Flow delay: the time delay between a change in bladder pressure and the corresponding change in measured flow rate. Good urodynamic practices: uroflowmetry, filling, cystometry, and pressure-flow studies. Uroflow curve interpretation is somewhat subjective because of difficultly in qualitatively judging a pattern (Boone and Kim, 1998). When the flow rate is reduced or the pattern is altered, this could indicate bladder (underactivity) or bladder outlet (anatomic or functional obstruction) dysfunction. The filling phase starts when filling commences and ends when the patient and urodynamicist decide that permission to void has been given (maximum cystometric capacity). Urethral pressure is defined as the fluid pressure needed to just open a closed urethra. Pressure-flow studies of voiding are the method by which the relationship between Pdet and urine flow rate is measured during bladder emptying (voiding). Pdet is measured as described previously with the simultaneous measurement of flow rate by uroflowmeter. The voiding phase starts when permission to void is given, or when uncontrollable voiding begins, and ends when the patient considers voiding has finished. However, it is recommended that, when choosing a system, the patient population and spectrum of diseases frequently encountered, space, convenience of operation (if a factor), and the need for data storage and processing be considered. In addition it is recommended that a multichannel system be used where channels are available to measure Pves, Pabd (and subtracted Pdet), and flow rate. However, despite all the advances, the clinician performing the study remains the most important constant in data collection and interpretation. Adding this capability is costly, but it allows the most comprehensive study possible. C,Interruptedorstrainingpattern, which can be seen with impaired bladder contractility, obstruction, or voiding with or by abdominalstraining. In addition to the necessary urodynamic hardware and software, a fluoroscopy unit and room of adequate size are required. External strain gauge transducers located between the patient and the urodynamic machine have been popular for years. Pressurized tubing (to avoid damping or dissipating the pressure) extends from the pressure transducer to the catheters placed in the patient. An electronic cable or wireless transmission brings the signal from the transducer to the urodynamic machine. Traditionally a water-filled system was used in which the entire system from transducer to patient is filled with water. Because this system depends on the transmission of pressure through fluid (water), it is crucial that there are no air bubbles in the transducer or tubing. The pressurized tubing transmission lines should be lucent to allow for easy recognition of air in the line. Air-charged catheters use a miniature air-filled balloon placed circumferentially around a polyethylene catheter. External forces on the balloon of the catheter are transmitted to the air-filled catheter lumen and communicated to an external semiconductor transducer. Air-charged catheters have several practical advantages over fluid-filled pressure lines because there is no fluid connection between the patient and the urodynamic equipment, just air. This means there is no hydrostatic pressure effect to account for, so there is no need to position anything at the level of the symphysis pubis and no need to flush the system through to exclude air (essential when using a fluid-filled system) Also, there are no artifactual fluctuations in pressure produced when the patient moves. There is comparative evidence for the use of air-charged catheters to measure urethral pressure and Valsalva leak point pressure, with one study showing comparable performance between air-charged and microtip catheters (Pollak et al, 2004) and one study concluding that they cannot be used interchangeably, because air-charged catheters showed systematically higher readings (Zehnder et al, 2008). Cooper and colleagues (2011), in an experimental model, showed that air-charged and water-filled catheters respond to pressure changes in dramatically different ways. Aircharged catheters acted as an overdamped system and attenuated signals at frequencies higher than 3. They demonstrated significantly less motion and hydrostatic artifacts than waterfilled catheters. Addingintra-abdominalpressuremonitoring gives a better representation of the true detrusor pressure (Pdet). The electronic dipstick flowmeter measures the electrical capacitance of a dipstick mounted in a collecting chamber. The output of the signal is proportional to the accumulated volume, and the volumetric flow rate is determined by differentiation. The weight transducer method is simple, reliable, and accurate, regardless of the site of stream impact, but requires that the density of urine must be set. The rotating disc method is also reliable and accurate and provides a direct measurement without need for differentiation of volume with respect to time. Electronic flowmeters provide a range of electronically read flow parameters with graphic depiction of the uroflow and have sufficient precision for clinical use with error rates of 1% to 8% in voided volume and 4% to 15% in flow rate (Susset, 1983). Most systems allow for calibrations for various fluids such as radiographic contrast agent. Electromyography Muscle depolarization must be detected by an electrode placed in or near the muscle. Surface electrodes are self-adhesive skin patch electrodes that are applied over the skin of the anal sphincter (Barrett, 1980). Surface electrodes have a significant advantage compared with the needle electrode regarding patient convenience and comfort. However, the surface electrodes provide an inferior signal source and must be precisely placed to provide an adequate signal source. Compared with the surface electrode, placement of the needle electrode has the disadvantage of being uncomfortable for the patient, especially if more than one attempt at placement of the electrode is required to obtain an adequate signal. Also, the needle electrode is easily dislodged and may require replacement during the study. Patients typically have a low tolerance for replacement of the needle electrode during urodynamic studies (Brucker et al, 2012). However, urodynamic signals can have frequency components greater than 3 Hz, particularly when using rapidly changing signals, such as coughs. The authors concluded that "knowledge of the characteristics of the pressure-measuring system is essential to finding the best match for a specific application. Thus it is recommended that investigators planning to use air-charged catheters for intravesical and intraabdominal pressure monitoring check for themselves that they have an equivalent performance to their current system for measuring pressure (Rosier et al, 2013). Finally, a microtip or fiberoptic system can be used to process pressure transmission. These catheters are quite expensive and reusable and must be sterilized before each use. The intention should be that the information that may be obtained could be used to guide patient treatment. Uroflowmeters Urine flow rate, or uroflow, can be determined by a number of different types of devices or uroflowmeters. Modern uroflowmeters use weight, electrical capacitance, or a rotating disc to determine urinary flow rates. The two most common techniques today are the weight transducer or load cell method and the rotating disc method. With the load cell the voided weight is measured and then differentiated with respect to time to determine the flow rate. This allows for ease of classification of voiding dysfunction according to the functional classification system mentioned previously. This is especially important when rises in Pdet are small or when they are accompanied by changes in Pabd. It can measure filling pressure, sensation, involuntary contractions, compliance, and capacity. Some treatments are thought to have a specific influence on sensation (de Wachter et al, 2011; Heeringa et al, 2011). NormalFillingandStorage Normally, the bladder should store urine at a low pressure and not contract involuntarily. Once capacity is reached or voluntary voiding is desired, intravesical pressure will increase (voluntary detrusor contraction).
Buy discount ropinirole 0.25mg on line
Five- and 10-year outcomes show oncologic equivalence to open radical nephrectomy in treatment of renal cancer medications xarelto ropinirole 2mg lowest price. Median follow-up was 54 months, and recurrence-free survival rates were 91% and 92%, respectively, for the two groups at 5 years. The 5-year cancer-specific survival was 98% for the laparoscopic cohort and 92% for the open cohort. Most important, the calculated disease-free survival rates for laparoscopic and open radical nephrectomy were 95% and 89%, respectively, at 10 years. The actuarial survival rates for laparoscopic and open radical nephrectomy were 87% and 75%, Transperitoneal Procedure Access and trocar placement are similar to what has been described for simple nephrectomy. With larger masses, caval involvement, or organ invasion, additional trocars or a hand port may be needed. The main distinguishing feature is that the Gerota fascia and fat are left intact during dissection. To aid in this, the renal vein is taken medial to the take-off of the adrenal vein. In adrenal-sparing surgery, the fascia is opened over the upper medial aspect of the kidney. Suspect lymph nodes may be removed, and a full hilar or retroperitoneal dissection can be carried out if deemed necessary based on preoperative imaging, tumor location, and histologic subtype if known based on preoperative biopsy, prior surgery pathology, or hereditary predisposition. Recurrence-free, cancer-specific, and overall survival rates were 86%, 92%, and 65%, respectively, at 10 years postnephrectomy (Berger et al, 2009). Although outcomes in this study were not compared with an open radical nephrectomy cohort, results are quite comparable to those for open surgery. Perioperative outcomes in contemporary groups undergoing laparoscopic and open radical nephrectomy have also been extensively studied. In a report comparing minimally invasive radical nephrectomy with open radical nephrectomy in the National Surgical Quality Improvement Program database, 5459 radical nephrectomy cases were identified. Significantly lower operative times, need for blood transfusion, length of hospitalization, and postoperative complications were noted in the laparoscopic patient cohort (Liu et al, 2014a). Similarly, in a well-matched cohort comparing laparoscopic with open radical nephrectomy, the laparoscopic approach was shown to have less blood loss, shorter hospital course, lower analgesic requirement, and shorter return to convalescence (Gill et al, 2000). Consistently, similar findings have been reported by multiple authors over the past three decades (Kerbl et al, 1994a; McDougall et al, 1996; Hemal et al, 2007). Hand-Assisted Procedure the patient is positioned, and the hand port and trocars are placed as previously described. To incise the white line of Toldt, the nondominant hand retracts the colon medially while the dominant hand uses laparoscopic scissors to divide the attachments. The irrigator-aspirator is then used to help identify and dissect the correct plane posterior to the large bowel mesentery and anterior to the Gerota fascia. For a left-sided renal procedure, the hand may also be used to gently retract the spleen and pancreas medially while the lienorenal attachments are divided. Similarly, on the right, the hand is used to retract the liver anteriorly, exposing the upper pole and facilitating its dissection. After the colon is sufficiently mobilized, the psoas muscle is identified, which will allow the ureter to be elevated. On the left the gonadal vein is typically elevated in the packet along with the ureter, but on the right the gonadal vein is reflected medially. With the ureter elevated, the hand can bluntly dissect and elevate the entire kidney off the psoas muscle, and the ureter is then followed up to the renal hilum. The fingers are then used to place anterolateral traction on the kidney while the thumb pushes the bowel and mesentery medially. The hilum should begin to come into view at this point, and the irrigator-aspirator can be used to gently dissect the overlying connective tissue while the hand is used to keep the vessels on stretch. Once the vessels are sufficiently skeletonized, the endovascular stapler or clips are used to ligate and divide the artery Retroperitoneal Procedure the patient is positioned, and trocars are placed for retroperitoneal access as described earlier in the chapter. After identification of the psoas muscle and tendon, medial dissection in this plane will reveal the ureter. Elevation of the ureter will allow visualization and subsequent elevation of the lower pole of the kidney. The arterial pulsation may be indirectly visualized through overlying connective tissue, and just as with the transperitoneal approach, gentle layer-by-layer dissection with the suction-irrigator will allow the renal vessels to come more directly into view. Use of the rightangle dissector will allow the artery to be circumferentially freed from the surrounding tissue, and the endovascular stapler or clips are used to divide the artery and vein sequentially. During surgery on the left kidney, a lumbar vein will typically require dissection, ligation, and division to allow unencumbered access to the main hilum. Care must be taken to continuously reorient to anatomic relationships to ensure that the inferior vena cava is not mistakenly identified as the renal vein. A randomized study comparing transperitoneal and retroperitoneal laparoscopic approaches was performed in 102 patients (52 transperitoneal, 50 retroperitoneal) with a mean tumor size of 5 cm (Desai et al, 2005). No difference was seen in blood loss, narcotic requirement, hospital stay, or complication rate. However, there was a significant difference noted in operative time, which favored the retroperitoneal approach (150 vs. A second randomized study of 40 patients compared the number and size of trocars, pathologic stage, blood loss, operative time, complication rate, and hospital stay (Nambirajan et al, 2004). No statistical difference was noted in any of these outcomes, including operative time. The inserted hand can also facilitate closure of trocar sites greater than 10 mm with a suture-passing device. Wound complications such as hernias and infections have been reported at the hand-port site, with hernias typically manifesting 3 months or more after surgery and with an overall 4% incidence (Okeke et al, 2002; Wolf, 2005). Care must be taken to copiously irrigate and close the handport incision, ideally closing the peritoneum separately from the fascia to minimize the chance of injuring intraperitoneal structures and hernia formation. Results Most outcomes are comparable between pure laparoscopy and the hand-assisted technique, including efficacy, operative times, complication rates, narcotic requirements, length of hospital stay, and return to convalescence. Some comparative studies between laparoscopic and hand-assisted techniques have demonstrated that the hand-assisted procedures can require shorter operative times, but patients had more abdominal pain and wound complications (Nelson and Wolf, 2002). Patients were grouped into those with tumors larger than 7 cm and those with tumors smaller than 7 cm. Short-term outcomes at mean follow-up of 12 months were not different between the two groups, including positive margin rate, local recurrence, and metastasis. A SpecialConsiderations Large Tumors Experience with laparoscopy for large tumors (>7 cm) has grown substantially as confidence with renal laparoscopy has increased (Steinberg et al, 2004; Hemal et al, 2007; Berger et al, 2008; Rosoff et al, 2009; Luciani et al, 2013). The bulk of the mass can decrease working space and alter normal anatomic landmarks. This can result in disorientation with potentially higher risk of injury to surrounding structures. Continuous intraoperative reference to preoperative imaging as well as use of intraoperative ultrasonography is helpful. Flexible endoscopes may be used to better visualize portions of the surgical field that would otherwise not be visible via a conventional rigid laparoscope. The weight of large tumors may cause the surgeon to apply additional force for manipulation, potentially resulting in tumor rupture. It may be beneficial to use a hand port or additional trocars in these instances to allow for more widely distributed retraction of the kidney. Consideration may also be given to lymphadenectomy with larger, higher-stage tumors. The lateral and superior attachments may then be divided, using a LigaSure device or Harmonic scalpel (Ethicon) while the hand keeps them on traction. The hand should not be used to bluntly dissect the adrenal gland free from the upper pole of the kidney, because this will typically result in bleeding. Ultrasonic energy, LigaSure, or bipolar cautery may be used to divide the fragile attachments between the kidney and the adrenal gland, just as with pure laparoscopy. A rolled laparotomy sponge is often placed through the hand port at the beginning of the procedure to assist with retraction, absorb blood, and allow the surgeon to hold pressure if needed. In addition, the tip of the irrigator-aspirator can be placed into the compressed sponge to facilitate suction when needed. The previously made hand-port incision allows rapid removal of sponge and the intact specimen.

Buy ropinirole 2 mg with visa
They found a marked decrease in the volume at which various filling sensations occurred and that the electrical threshold decreased after after drug administration medicine to help you sleep discount 1 mg ropinirole free shipping. De Wachter and colleagues (2003) treated 18 women with impaired detrusor contraction with subcutaneous bethanechol (5 mg four times daily) for 10 days. They also found that in these women the sensation of filling and the electrical sensitivity were significantly increased compared with before treatment. The authors suggested that patients likely to respond to bethanechol can be identified by determination of the bladder electrical perception threshold. Riedl and colleagues (2000) performed a clinical study in 45 patients with detrusor areflexia. The patients were tested with electromotive administration of intravesical bethanechol. Bethanechol 25 mg given orally once daily was then prescribed for 15 patients, and voiding control was assessed after 6 weeks of therapy. A mean pressure increase of 34 cm H2O during the electromotive administration of bethanechol was found in 24 of 26 patients with areflexia and neurologic disease compared with only 3 cm H2O in 3 of 11 with a history of chronic bladder dilation. Oral bethanechol restored spontaneous voiding in 9 of 11 patients who had had a positive response to the electromotive administration of bethanechol, whereas all 4 without a pressure increase during the electromotive administration of bethanechol did not void spontaneously. The researchers concluded that electromotive administration of intravesical bethanechol can identify patients with an atonic bladder and adequate residual detrusor muscle function who are candidates for restorative measures, such as oral bethanechol and intravesical electrostimulation. Those who do not respond to the electromotive administration of bethanechol do not benefit from oral bethanechol and are candidates for catheterization. No agreement exists as to whether cholinergic stimulation produces an increase in urethral resistance (Wein et al, 1980a, 1980b). As to whether cholinergic agonists can be combined with agents to decrease outlet resistance to facilitate emptying and achieve an additive or synergistic effect, our own experience with such therapy, using even 200 mg (50 mg qid) of oral bethanechol daily, has been disappointing. Certainly, most clinicians would agree that a total divided daily dose of 50 to 100 mg rarely affects any urodynamic parameter at all. The question of whether bethanechol may be efficacious in a particular patient can be answered by a brief urodynamically controlled trial in which institution of therapy is the only variable. In the laboratory, a functioning micturition reflex is an absolute requirement for the production of a sustained bladder contraction by a subcutaneous injection of the drug (Downie, 1984). Patients with incomplete lower motoneuron lesions constitute the most reasonable group for a trial of bethanechol (Awad, 1985), although subcutaneous administration may be required. It is generally agreed that, at least in a "denervated" bladder, an oral dose of 200 mg is required to produce the same urodynamic effects as a subcutaneous dose of 5 mg (Diokno and Lapides, 1977). The potential side effects of cholinomimetic drugs include flushing, nausea, vomiting, diarrhea, gastrointestinal cramps, bronchospasm, headache, salivation, sweating, and difficulty with visual accommodation (Brown and Taylor, 2006). Intramuscular and intravenous use can precipitate acute and severe side effects, resulting in acute circulatory failure and cardiac arrest, and are therefore prohibited. One potential avenue of increasing bladder contractility is cholinergic enhancement or augmentation. Such an action might be useful alone or in combination with a parasympathomimetic agent. Metoclopramide is a dopamine-receptor antagonist with cholinergic properties (Pasricha et al, 2006). Nineteen patients with detrusor underactivity (17 men and 2 women) were eligible and randomized to one of two treatments. A second group of 10 patients received a once-weekly instillation of saline together with placebo tablets, again for 6 weeks. The authors did not recommend this treatment as routine but suggested that it may be considered for the occasional treatment of a patient with detrusor underactivity. There has been little recent activity in this area, a fact that usually means that clinicians have lost interest or that the initial optimistic results have not been confirmed. Prostaglandins have a relatively short half-life, and it is difficult to understand how any effects after a single application can last up to several months. If such does occur, it must be the result of a "triggering effect" on some as yet unknown physiologic or metabolic mechanism. Because of the number of conflicting positive and negative reports with various intravesical preparations, double-blind, placebocontrolled studies would obviously be helpful to see whether there are circumstances in which prostaglandin use can reproducibly facilitate emptying or treat postoperative retention. Potential systemic side effects of prostaglandin use include vomiting, diarrhea, pyrexia, hypertension, and hypotension (Campbell and Halushka, 1996). Some data from dogs suggest that this agent can increase detrusor contractility (Mitchell and Venable, 1985), but there are no controlled studies documenting a useful clinical effect in the treatment of detrusor underactivity. Cisapride is a substituted piperidinyl benzamide with a number of different pharmacologic activities, including a possible direct stimulation of smooth muscle (Pasricha, 2006). Until recently it was commonly used as a prokinetic agent, particularly for gastroesophageal reflux and gastroparesis. It was also suggested that it could improve bladder contractility (Binnie et al, 1988; Carone et al, 1993; Steele et al, 2001). However, there was never any particularly convincing data that the drug improved voiding function, and it is no longer available in the United States because of its potential to induce serious and occasional cardiac arrhythmias (Pasricha, 2006). The concept, however, of cholinergic enhancement or augmentation remains attractive but awaits the development of a bladder-selective compound. Prostaglandins the reported use of prostaglandins to facilitate emptying is based on hypotheses that these substances contribute to the maintenance of bladder tone and bladder contractile activity (see Chapter 69 and Andersson, 1993; Zderic et al, 1995; Andersson, 1999a, 1999b, 1999c; Andersson and Wein, 2004 for a complete discussion). Prostanoids may affect bladder activity directly by effects on the smooth muscle or indirectly through effects on neurotransmission. Twenty of 36 patients showed a strongly positive immediate response, and 6 showed a weakly positive one. Fourteen patients were reported to show prolonged beneficial effects, all but 1 of whom had shown a strongly positive immediate response. Stratification of the data revealed that an intact sacral reflex arc was a prerequisite for any type of positive response. The drug was administered in 50 mL of saline solution as a single dose and retained for 2 hours. However, in these "successfully" treated patients, the average maximum flow rate was 10. The maximum effect occurred within 1 to 2 minutes after intravenous injection and was gone by 5 minutes. Galeano and colleagues (1986) reported that although naloxone increased bladder contractility in cats with chronic spinal injury, it also aggravated striated sphincter dyssynergia and spasticity- a potential problem in the treatment of emptying failure. Although an intriguing area, the concept of reversing an inhibitory opioid influence to stimulate reflex bladder activity is of little practical use at present. It is difficult to find reproducible urodynamic data that support a recommendation for the use of oral bethanechol chloride in any specific category of patients, despite its pharmacologic characteristics as a cholinergic agonist. It is possible that bethanechol, by increasing static intravesical pressure, may cause afferent stimulation at a lower bladder volume than usual, prompting detrusor contraction at a more favorable bladder volume. Initial reports of the use of intravesical prostanoids producing lasting favorable clinical effects have not been confirmed. Decreasing Outlet Resistance at the Level of the Smooth Sphincter -Adrenoceptor Antagonists. Furthermore, they hypothesized that some obstructions at this level during bladder contraction are a result of inadequate opening of the bladder neck and/or of an inadequate decrease in resistance in the area of the proximal urethra. Successful results, usually defined as an increase in flow rate, a decrease in residual urine, and an improvement in upper tract appearance (where pathologic), could often be correlated with an objective decrease in urethral profile closure pressure. One would expect success with such therapy to be most evident in patients without detrusor striated sphincter dyssynergia, as reported by Hachen (1980). Scott and Morrow (1978), on the other hand, noted excellent results with phenoxybenzamine therapy in 9 of 10 patients with a flaccid bladder and a flaccid external sphincter and in a single patient with an upper motor neuron bladder with intact sympathetic innervation, but in only 8 of 21 patients with hyperreflexia and autonomic dysreflexia, and in none of 6 patients with an upper motor neuron bladder and sympathetic denervation (lesion between T10 and L2). One cannot tell by pressure tracings alone whether decreased resistance in this area of the urethra is secondary to a decrease in smooth or striated muscle activity. They concluded (1) that the effect of phentolamine was from smooth muscle relaxation alone; (2) that the effect of clonidine, and possibly phenoxybenzamine, was elicited mostly through centrally induced changes in striated urethral sphincter tonus; and (3) that these agents also had an effect on the smooth muscle component of urethral pressure. None of the three drugs, however, affected the reflex rise in either urethral pressure or electromyographic activity seen during bladder filling, and none decreased the urethral pressure or electromyographic activity response to voluntary contraction of the pelvic floor striated musculature. Thind and colleagues (1992) reported on the effects of prazosin on static urethral sphincter function in 10 healthy women. Decreased bladder compliance is a common clinical problem in such patients, and this, along with a fixed urethral sphincter tone, results in the paradoxic occurrence of both storage and emptying failure.