Discount 250mg terbinafine free shipping
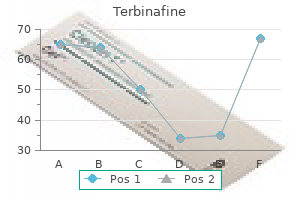
The goal is fungus under my toenail 250 mg terbinafine for sale, as the title suggests, to identify the primary, or "root," cause of the problem under analysis. One of the first users of this technique was Toyota, who famously used the "5 whys" technique. By asking "why" at least five times during the investigation of a breakdown or undesired event, quality personnel are forced to drill down layer by layer to understand progressively more fundamental causes. When applied in medicine, the root cause process begins with a multidisciplinary group assembled to evaluate every step of the process that resulted in the event in question. Attention is focused strictly on system processes and not on individual provider behavior. A causal factor chart is often created in skeleton form, with details added as each specialty adds their expertise. Although such charts are usually read from left to right, they are often created from right to left, starting with the event and using logic and time information to add relevant causal factors. Such events are called "sentinel" because they expose a dangerous "gap" in care and signal the need for immediate investigation and response. The Joint Commission also explicitly defines events that do not require focused reporting and review. These include any near miss, medication errors that do not result in death or functional loss, minor hemolysis, or death or functional loss after leaving against medical advice. Such a plan must include the action to be taken, who will implement, a time line for implementation, and strategies for measuring the result and sustaining the changes. Although reporting to the Joint Commission is voluntary, identification of such events is a key component of accreditation visits. Other patient safety organizations have suggested modifications to the Joint Commission list. Studies of action plans and implementations suggest that relatively few of these actively target true "root" causes. One highly useful outcome of the Joint Commission Sentinel Event program is their series of sentinel event alerts. To date, this program has resulted in more than 50 events including several relevant to anesthesia such as deaths due to concentrated potassium chloride solutions, ventilator-related deaths, medical gas mix-ups, transfusion errors, disruptive behavior, and magnetic resonance imaging accidents. Process flaws in care delivery may not be addressed until the event actually occurs and a patient is harmed. A process to identify and record patient allergies, for example, might fail if the interviewer is unable to accurately identify allergies, if the documentation form is difficult to read or inaccessible, or if medications sound alike. In addition to simulation and imagination, a team should use other sources to identify potential failures including sentinel event alerts, Institute for Safe Medication Practices information, and Food and Drug Administration databases and advisories. Even if most of the relevant failure modes can be identified, implementing effective change can be difficult, in part because no bad event has yet occurred. Because procedures and anesthetic strategies routinely evolve to meet changing needs, quality and safety in anesthesia present by definition a moving target. Historically, anesthesiologists have led in patient safety by being willing to embrace several practical approaches. Among these are the empiric cataloging of events, a recognition of human-machine interface errors as a significant contributor to adverse events, adoption of strategies from other highly technical fields, and early specialtywide agreement with respect to practice standards. In part because knowledge regarding care outcomes has been lacking, anesthesiologists have only recently begun to focus in the same way on care quality. Although no "magic bullet" strategy to quality improvement has yet emerged, process, structure, and outcome are all key elements in any comprehensive quality program. Finally, multiple tools exist at the departmental and institutional level for quality improvement. These tools include blueprints for local quality projects, nationally promulgated sentinel event programs, and root cause and failure mode analyses for adverse events. Taken together, numerous quality and safety tools and approaches are available to anesthesia teams interested in patient safety. With the growth and maturation of large perioperative databases, and the potential of electronic intraoperative records to shed light into the perioperative period, even more options will become available to make anesthesia practice safer and increased quality in upcoming years. What is the rationale for using process measures, structural measures, or outcome measures as a means to improve quality Ultrasound guidance versus anatomical landmarks for internal jugular vein catheterization. A study of the deaths associated with anesthesia and surgery: based on a study of 599,548 anesthesias in ten institutions 1948-1952, inclusive. Risk factors associated with ischemic optic neuropathy after spinal fusion surgery. Unexpected cardiac arrest during spinal anesthesia: a closed claims analysis of 18. Surgical site infection prevention: time to move beyond the surgical care improvement program. Timing of surgical antibiotic prophylaxis and the risk of surgical site infection. Surgical Care Improvement Project measure for postoperative glucose control should not be used as a measure of quality after cardiac surgery. Early intravenous then oral metoprolol in 45,852 patients with acute myocardial infarction: randomised placebo-controlled trial. Public reporting of antibiotic timing in patients with pneumonia: lessons from a flawed performance measure. Variability in practice and factors predictive of total crystalloid administration during abdominal surgery: retrospective two-centre analysis. Variability in anesthetic care for total knee arthroplasty: an analysis from the anesthesia quality institute. Variability in data: the Society of Thoracic Surgeons National Adult Cardiac Surgery Database. Validation of a risk stratification index and risk quantification index for predicting patient outcomes: in-hospital mortality, 30-day mortality, 1-year mortality, and length-of-stay. Association of hospital participation in a surgical outcomes monitoring program with inpatient complications and mortality. Association of hospital participation in a quality reporting program with surgical outcomes and expenditures for Medicare beneficiaries. Analysis of unintended events in hospitals: inter-rater reliability of constructing causal trees and classifying root causes. Palliative care, with its emphasis on goal setting and symptom management, attempts to improve care for these patients and their families. Many palliative care skills can be used in a variety of settings, and concepts such as shared decision making and a biopsychosocial-spiritual approach should not be reserved only for seriously ill patients. Modern palliative care started with the hospice movement in the 1960s and has spread to many health systems worldwide. In the United States, at least two thirds of hospitals have palliative care teams,4 and hospice services are widely available. Despite their common roots, hospice and palliative care are not necessarily interchangeable terms. The meaning of hospice and the services offered vary by country, though hospices generally focus on later-stage illnesses. In the United States, hospice refers to an insurance benefit for patients with a life expectancy of less than 6 months. Palliative care is a more inclusive term that is appropriate "at any age and any stage in a serious illness, and can be provided together with curative treatment. It means talking to patients and families, eliciting their values and goals, and making medical recommendations and decisions based on those values and goals. This concept acknowledges that part of the pain a patient feels may be, in part, due to existential or spiritual suffering. Medical advances and an aging population have led to an increase in the number of patients with serious illnesses. The beneficiaries using the most Medicare dollars include those in the last year of life, even though many people say they do not want to die in a hospital. In 2010, benefits to the most costly 5% of members accounted for 39% of Medicare spending.
Cheap terbinafine online amex
Type of surgery is also predictive fungus gnats on skin purchase terbinafine 250mg mastercard, with urinary retention occurring most commonly in anorectal and joint replacement surgery. Commonly used perioperative medications such as anticholinergics, -blockers, and narcotics also contribute to urinary retention. Diagnosis can be made by clinical examination, bladder catheterization, or ultrasound assessment. Bladder volumes measured by ultrasound imaging correlate well with volumes obtained by urinary catheterization, an uncomfortable procedure that can be complicated by catheter-related infections and urethral trauma. Bladder ultrasound is an efficient and accurate method to evaluate patients at risk for oliguria. Clinical postoperative urinary retention is defined as the inability to void despite a 686 the most common cause of oliguria in the immediate postoperative period is a decrease of intravascular volume. An intravascular fluid challenge (500 to 1000 mL of crystalloid) is usually effective in restoring urine output. The hematocrit should be measured when surgical blood loss is suspected and repeated intravascular boluses of fluid are required to maintain urine output. Resuscitation by intravenous administration of fluids to maximize renal perfusion is particularly important in order to prevent ongoing ischemic injury and the development of acute tubular necrosis. If an intravascular fluid challenge is contraindicated or oliguria persists, assessment of intravascular volume or cardiac function is indicated to differentiate hypovolemia from sepsis and low cardiac output states. Fractional excretion of sodium can be useful in determining the adequacy of renal perfusion (assuming that diuretics have not been given), but the diagnosis of prerenal azotemia Chapter 39 Postanesthesia Recovery will not differentiate between hypovolemia, congestive heart failure, or hepatorenal syndrome. In these cases evaluation with central venous monitoring or echocardiography may facilitate the diagnosis. Mucomyst can be given and is a relatively inexpensive and easily administered medication (single oral dose before and after procedure) that may also provide renal protection. Abdominal compartment syndrome is defined as sustained intra-abdominal pressure higher than 20 mm Hg that is associated with new organ dysfunction or failure. Intra-abdominal pressure should be measured (via bladder pressure) in patients in whom intra-abdominal hypertension is suspected so that prompt intervention can be initiated to relieve intra-abdominal pressure and restore renal perfusion. The incidence of postoperative shivering may be as high as 65% (range 5% to 65%) after general anesthesia and 33% after epidural anesthesia. Identified risk factors include male gender and the choice of drug for induction of anesthesia. Although thermoregulatory mechanisms can explain shivering in a hypothermic patient, a separate mechanism has been proposed to explain shivering in normothermic patients. The proposed mechanism is based on the observation that the brain and spinal cord do not recover simultaneously from general anesthesia. The more rapid recovery of spinal cord function results in uninhibited spinal reflexes manifested as clonic activity. Rhabdomyolysis Rhabdomyolysis is a possible cause of postoperative renal insufficiency in patients who have suffered major crush or thermal injury as well as with patients undergoing elective surgery. The incidence is increased in morbidly obese patients, particularly those having bariatric surgery. Severe postoperative pain is characteristic of myonecrosis and rhabdomyolysis, often in the areas of contact with the operating room table such as the gluteal, lumbar, and shoulder muscles. Treatment Intervention includes the identification and treatment of hypothermia if present. Shivering also increases oxygen consumption and is potentially detrimental in the postoperative patient with history of cardiac disease or limited reserve. Accurate core body temperatures can be most quickly and easily obtained using a temporal artery thermometer. V Contrast Nephropathy Angiography with intravascular stent placement is replacing open procedures to treat carotid stenosis, aortic aneurysms, and peripheral vascular disease. Patients undergoing these procedures often have chronic renal insufficiency and are at risk for developing renal failure secondary to intravenous contrast infusion. Although aggressive hydration with normal saline provides the single most effective protection against contrast nephropathy, alkalinization with bicarbonate has been shown to provide additional protection. Anesthesiarelated factors include the use of volatile anesthetics or nitrous oxide and the administration of large doses of neostigmine and perioperative opioids. A single intervention in a patient with four risk factors will result in an absolute risk reduction of 21% compared with a 3% risk reduction in a patient with an initial risk of only 10%. Strategies to reduce baseline risk include avoidance of general anesthesia by the use of regional anesthesia, preferential use of propofol infusions, avoidance of nitrous oxide and volatile anesthetics, minimization of giving postoperative opioids, and adequate hydration. When choosing an antiemetic for these patients, both the class of drug and the timing of administration are important factors (Box 39. Requiring patients to urinate before discharge should not be part of a routine discharge protocol and may be necessary only in selected patients. The demonstrated ability to drink and retain clear fluids should not be part of a routine discharge protocol but may be appropriate for selected patients. Patients should be observed until they are no longer at increased risk for cardiorespiratory depression. Monitoring with pulse oximetry and analysis of arterial blood gases should be used to rule out hypoxemia and hypoventilation. Additional studies may be indicated to evaluate possible electrolyte derangements, metabolic disturbances, and hypoglycemia. Rarely, computed tomographic imaging is indicated to rule out an acute intracerebral event. Physostigmine may be effective in reversing the central nervous system sedative effects of anticholinergic drugs (especially scopolamine). Flumazenil is a specific antagonist for the residual depressant effects of benzodiazepines. This is the case even when the decision to discharge the patient is made by the bedside nurse in accordance with the hospital-sanctioned discharge criteria or scoring system. If discharge scoring systems are to be used in this way, they must first be approved by the department of anesthesia and the hospital medical staff. What steps can be taken to determine the presence of significant upper airway edema prior to extubation What monitoring should be done to evaluate for postoperative myocardial ischemia or infarction Practice guidelines for postanesthetic care: an updated report by the American Society of Anesthesiologists Task Force on Postanesthetic Care. Intermediate acting non-depolarizing neuromuscular blocking agents and risk of postoperative respiratory complications: prospective propensity score matched cohort study. Effects of neostigmine reversal of nondepolarizing neuromuscular blocking agents on postoperative respiratory outcomes: a prospective study. Cuff-leak test for predicting postextubation airway complications: a systematic review. Meta-analysis of the association between obstructive sleep apnoea and postoperative outcome. Obstructive sleep apnea syndrome and perioperative complications: a systematic review of the literature. Continuous positive airway pressure for treatment of postoperative hypoxemia: a randomized controlled trial. Characteristics and short-term prognosis of perioperative myocardial infarction in patients undergoing noncardiac surgery: a cohort study. Myocardial injury after noncardiac surgery: a large, international, prospective cohort study establishing diagnostic criteria, characteristics, predictors, and 30-day outcomes. Incidence, predictors, and outcomes associated with postoperative Postanesthesia Recovery 33. Intra-abdominal hypertension and the abdominal compartment syndrome: updated consensus definitions and clinical practice guidelines from the World Society of the abdominal compartment syndrome. Temperature measurement in patients undergoing colorectal surgery and gynecology surgery: a comparison of esophageal core, temporal artery, and oral methods. The effect of short time periods of pre-operative warming in the prevention of perioperative hypothermia.
Order discount terbinafine on line
It is important for students of medical microbiology and infectious disease to understand the role of the microbiota because of its significance both as a defense mechanism against infection and as a source of potentially pathogenic organisms antifungal shoes buy terbinafine from india. In addition, it is important for physicians to know the typical composition of the microbiota at various sites to avoid confusion when interpreting laboratory culture results. He was influenced by an article in Scientific American about the flora of the skin. For creatures your size I offer a free choice of habitat, so settle yourselves in the zone that suits you best, in the pools of my pores or the tropical forests of arm-pit and crotch, in the deserts of my fore-arms, or the cool woods of my scalp. Subsequently, as the infant is exposed to a broader range of organisms, those best adapted to colonize particular sites become predominant. Thereafter, the flora generally resembles that of other individuals in the same age group and cultural milieu. Local physiologic and ecologic conditions determine the microbial makeup of the flora. These conditions are sometimes highly complex, differing from site to site, and sometimes with age. Many bacteria have adhesin-mediated affinity for receptors on specific types of epithelial cells; this facilitates colonization and multiplication and prevents removal by the flushing effects of surface fluids and peristalsis. Various microbial interactions also determine their relative prevalence in the flora. These interactions include competition for nutrients and inhibition by the metabolic products of other organisms. M Blood, Body Fluids, and Tissues In health, the blood, body fluids, and tissues are sterile. Occasional organisms may be displaced across epithelial barriers as a result of trauma or during childbirth; they may be briefly recoverable from the bloodstream before they are filtered out in the pulmonary capillaries or removed by cells of the reticuloendothelial system. Such transient bacteremia may be the source of infection when structures such as damaged heart valves and foreign bodies (prostheses) are in the bloodstream. Tissues and body fluids such as blood are sterile in health Transient bacteremia can result from trauma M Skin the skin provides a dry, slightly acidic, aerobic environment. Propionibacteria and staphylococci are dominant bacteria Skin flora is not easily removed Conjunctiva resembles skin of sebaceous and sweat glands. The flora is more abundant on moist skin areas (axillae, perineum, and between toes). Staphylococci and members of the Propionibacterium genus occur all over the skin, and facultative diphtheroids (corynebacteria) are found in moist areas. Propionibacteria are slim, anaerobic, or microaerophilic Gram-positive rods that grow in subsurface sebum and break down skin lipids to fatty acids. Thus, they are most numerous in the ducts of hair follicles and of the sebaceous glands that drain into them. Even with antiseptic scrubbing, it is difficult to eliminate bacteria from skin sites, particularly those bearing pilosebaceous units. Organisms of the skin flora are resistant to the bactericidal effects of skin lipids and fatty acids, which inhibit or kill many extraneous bacteria. The low bacterial count is maintained by the high lysozyme content of lachrymal secretions and by the flushing effect of tears. M Intestinal Tract the mouth and pharynx contain large numbers of facultative and anaerobic bacteria. Different species of streptococci predominate on the buccal and tongue mucosa because of different specific adherence characteristics. Gram-negative diplococci of the genus Neisseria and coccobacillary Moraxella make up the balance of the most commonly isolated organisms. Strict anaerobes and microaerophilic organisms of the oral cavity have their niches in the depths of the gingival crevices surrounding the teeth and in sites such as tonsillar crypts, where anaerobic conditions can develop readily. The total number of organisms in the oral cavity is very high, and it varies from site to site. Saliva usually contains a mixed flora of about 108 organisms per milliliter, derived mostly from the various epithelial colonization sites. The stomach contains few, if any, resident organisms in health because of the lethal action of gastric hydrochloric acid and peptic enzymes on bacteria. The small intestine has a scanty resident flora, except in the lower ileum, where it begins to resemble that of the colon. Vaginal Gram smear showing budding yeast (long arrow), epithelial cells (short arrow) and a mixture of other bacterial morphologies. In the adult, feces are 25% or more bacteria by weight (about 1010 organisms per gram). More than 90% are anaerobes, predominantly members of the genera Bacteroides, Fusobacterium, Eubacterium, and Clostridium. The remainder of the flora is composed of facultative organisms such as Escherichia coli, enterococci, yeasts, and numerous other species. There are considerable differences in adult flora depending on the diet of the host. Those whose diets include substantial amounts of meat have more Bacteroides and other anaerobic Gram-negative rods in their stools than those on a predominantly vegetable or fish diet. Recent studies have suggested the composition of the colonic microbiota could play a role in obesity. Adult colonic flora is abundant and predominantly anaerobic Diet affects species composition M Respiratory Tract the external 1 cm of the anterior nares has a flora similar to that of the skin. Approximately 25% to 30% of healthy people carry this organism as either resident or transient flora at any given time. The nasopharynx has a flora similar to that of the mouth; however, it is often the site of carriage of potentially pathogenic organisms such as pneumococci, meningococci, and Haemophilus species. The respiratory tract below the level of the larynx is protected in health by the action of the epithelial cilia and by the movement of the mucociliary blanket; thus, only transient inhaled organisms are encountered in the trachea and larger bronchi. The accessory sinuses are normally sterile and are protected in a similar fashion, as is the middle ear by the epithelium of the eustachian tubes. The vagina has a flora that varies according to hormonal influences at different ages. Before puberty and after menopause, it is mixed, nonspecific, and relatively scanty, and it contains organisms derived from the flora of the skin and colon. These conditions develop because glycogen is deposited in vaginal epithelial cells under the influence of estrogenic hormones and metabolized to lactic acid by lactobacilli. This process results in a vaginal pH of 4 to 5, which is optimal for growth and survival of the lactobacilli, but inhibits many other organisms. Perforation of the colon from a ruptured diverticulum or a penetrating abdominal wound releases feces into the peritoneal cavity; this contamination may be followed by peritonitis or intraabdominal abscesses caused by the more opportunistic members of the flora. Reduced innate defenses or immunologic responses can result in local invasion and disease by normal floral organisms. Caries and periodontal disease are caused by organisms that are members of the oral microbiota (see Chapter 41). M Exclusionary Effect Competing with pathogens has a protective effect Antibiotic therapy may provide a competitive advantage for pathogens Balancing the prospect of opportunistic infection is the tendency of the resident microbiota to produce conditions that compete with extraneous pathogens and, thus, reduce their ability to establish a niche in the host. The microbiota in the colon of the breastfed infant produces an environment inimical to colonization by enteric pathogens, as does a vaginal flora dominated by lactobacilli. The benefit of this exclusionary effect has been demonstrated by what happens when it is removed. Antibiotic therapy, particularly with broad-spectrum agents, may so alter the microbiota of the gastrointestinal tract that antibiotic-resistant organisms multiply in the ecologic vacuum. Under these conditions, the spore-forming Clostridium difficile has a selective advantage that allows it to survive, proliferate, and produce a toxic colitis. M Priming of Immune System Sterile animals have little immunity to microbial infection Low exposure correlates with asthma risk Organisms of the microbiota play an important role in the development of immunologic competence.
Order genuine terbinafine on line
When glycogen stores are depleted hepatic gluconeogenesis from substrates such as lactate fungus between thighs cheap terbinafine 250 mg on line, glycerol, and certain amino acids restores blood glucose levels. Prolonged elimination half-times for morphine, alfentanil, diazepam, lidocaine, pancuronium, and vecuronium occur in patients with cirrhosis of the liver. Likewise, chronic drug therapy can inhibit hepatic enzymes and inhibit metabolism of anesthetic drugs leading to higher circulating blood levels. Conversely, enzyme induction, particularly of cytochrome P isoforms, can also occur as a response to chronic therapy with drugs such as phenytoin, isoniazid, and rifampin or as a result of alcohol abuse. Induction of hepatic enzymes can increase metabolism of administered anesthetic and therapeutic drugs, thereby reducing plasma levels. Heme Metabolism Although fetal erythrocyte production occurs exclusively in the liver, hepatic hematopoiesis accounts for only 20% of adult heme synthesis with the remainder produced in the bone marrow. Heme degradation, primarily by the reticuloendothelial system, results in formation of bilirubin as an end product. Formed bilirubin is then bound to plasma albumin for transport to the liver, where it is extracted and conjugated for secretion into canalicular bile. The majority of bilirubin excretion occurs in the gut, although a small portion is recirculated to the liver via the enterohepatic circulation. Impaired laboratory studies reflect significant hepatic dysfunction because most coagulation factors maintain function at up to 20% to 30% of their normal levels. In addition, the liver synthesizes free fatty acids from glucose, lipids, and protein. The liver also plays an important role in regulation of cholesterol uptake, metabolism, and transport. Bile salts, the end product of cholesterol synthesis, serve as regulators of lipid metabolism. Elimination of cholesterol is achieved by biliary secretion and by excretion of bile acids. Drug Metabolism Hepatic drug metabolism is characterized by the conversion of lipid-soluble drugs to more water-soluble forms to facilitate renal excretion, transformation to pharmacologically less active substances, and excretion in bile. Phase 1 metabolism involves an increase in polarity of drugs via cytochrome P and mixed function oxidases. Phase 2 metabolism involves conjugation of metabolites to water-soluble substrates. Chronic liver disease may interfere with the metabolism of drugs because of the decreased number of enzyme-containing hepatocytes or the decreased hepatic blood flow that Protein Metabolism the liver plays a vital role in protein metabolism. Numerous biologically active proteins including albumin, cytokines, hormones, and coagulation factors are manufactured in the liver. In addition, nonessential amino acid synthesis can also occur in hepatocytes when necessary. The urea (Krebs) cycle is utilized by hepatocytes to convert the end products of amino acid degradation, such as ammonia and other nitrogenous waste products, to urea, which is readily excreted by the kidney. Nevertheless, these patients are at increased risk for acute right-sided heart failure if physiologic conditions that increase pulmonary vascular resistance (acidosis, arterial hypoxemia, hypercapnia) occur during anesthesia. Hepatic hydrothorax, defined as pleural effusions occurring in the absence of cardiopulmonary disease, can also occur in up to 10% of cirrhotic patients. In some patients, the pleural effusions from hepatic hydrothorax are large enough to impair oxygenation. Hepatic Encephalopathy Pathophysiology of End-Stage Liver Disease Cardiovascular Complications Severe parenchymal disease that has advanced to the point of cirrhosis usually results in a hyperdynamic circulation. Hemodynamic measurements generally reveal normal to low systemic blood pressure, increased cardiac output, and decreased systemic vascular resistance. Decreased systemic vascular resistance is a result of vasodilation and abnormal anatomic and physiologic shunting. Physiologic shunting is the passage of blood from the arterial to the venous side of the circulation without effectively traversing a capillary bed. Abnormal blood vessels, such as those seen in the skin as spider angiomas, represent an anatomic shunt. Vessels draining the esophagus, stomach, spleen, and intestines dilate and hypertrophy, which leads to the development of splenomegaly and esophageal, gastric, and intra-abdominal varices. Pulmonary Complications Altered mental state is a frequent complication of both acute and chronic liver failure with a clinically variable presentation ranging from minor changes in brain function to deep coma. The serum concentrations of many chemicals, which are normally filtered by the healthy liver and are present in higher concentrations with hepatic dysfunction, likely play an important role. Other etiologic factors include disruption of the blood-brain barrier, increased central nervous system inhibitory neurotransmission, and altered cerebral energy metabolism. It is also important to rule out other causes of altered mental status in the patient with liver disease, such as intracranial bleeding or masses, hypoglycemia, or a postictal state. Typically, neomycin (to reduce ammonia production by urease-producing bacteria) and the administration of lactulose (to reduce ammonia absorption) are employed. Hepatopulmonary syndrome develops as a result of intrapulmonary arteriovenous communications that are not ventilated, impairment of hypoxic pulmonary vasoconstriction, atelectasis, and restrictive pulmonary disease secondary to ascites and pleural effusion. Arterial hypoxemia, secondary to the hepatopulmonary syndrome, may improve somewhat with supplemental oxygen in the early stages of the disease, but oxygen may not be effective with disease progression. Portopulmonary hypertension is an increase in intrapulmonary vascular pressure in patients with portal hypertension. This syndrome occurs in less than 5% of patients, including the 492 When liver disease is so severe that albumin production is decreased, fewer sites are available for drug binding. This limited availability can increase levels of the unbound, pharmacologically active fraction of drugs, such as thiopental and alfentanil. Increased drug sensitivity as a result of decreased protein binding is most likely to be manifested when plasma albumin concentrations are lower than 2. Ascites Ascites is a common complication of cirrhosis affecting up to 50% of cirrhotic patients. The development of ascites is associated with significant morbidity and heralds the end stages of cirrhosis. Complications associated with ascites include marked abdominal distention (leading to atelectasis and restrictive pulmonary disease), Chapter 28 Renal, Liver, and Biliary Tract Disease spontaneous bacterial peritonitis, and circulatory instability due to compression of the inferior vena cava and right atrium. Although the exact mechanism of ascites is unclear, excess sodium retention by the kidney, decreased oncotic pressure due to hypoalbuminemia, and portal hypertension appear to play a central role. Initial therapy includes restriction of fluid administration, reduction of sodium intake, and administration of diuretics. In severe cases, abdominal paracentesis can be effective at transiently reducing abdominal distention and restoring hemodynamic stability. Renal Dysfunction and Hepatorenal Syndrome Renal dysfunction can develop in a significant portion of patients with cirrhosis. A variety of etiologic factors including diuretic therapy, reduced intravascular volume secondary to ascites or gastrointestinal hemorrhage, nephrotoxic drugs, and sepsis can provoke acute renal failure and ultimately acute tubular necrosis in cirrhotic patients. A mild form occurs in up to 20% of patients and is associated with minimal sequelae. Risk factors for development of this condition include prior exposure to halothane, age older than 40 years, obesity, and female gender. Isoflurane and desflurane are also capable of causing hepatic dysfunction, but the incidence of hepatitis after exposure to these volatile anesthetics is extremely rare, mainly because of the decreased magnitude of metabolism in comparison to halothane. These changes reflect drug- or technique-induced effects on hepatic perfusion pressure or splanchnic vascular resistance, or both. For example, reduced hepatic blood flow from volatile anesthetics, as well as regional anesthesia (T5 sensory level), is likely due to decreased hepatic perfusion pressure. Autoregulation (increased hepatic artery blood flow offsetting decreases in portal vein blood flow) of hepatic blood flow may be best maintained with isoflurane. However, hepatic blood flow during the administration of desflurane and sevoflurane is maintained by a similar mechanism. Postoperative liver dysfunction is more likely in the presence of coexisting liver disease. Furthermore, the large reserve of the liver means that considerable hepatic damage can be present before liver function test results become altered. It may take additional stressors, such as anesthesia and surgery, to reveal the underlying liver disease.
Discount 250mg terbinafine otc
In this case antifungal baby powder discount terbinafine online mastercard, productive (lytic) infection takes place in permissive cells (mucoepithelial cells), whereas latent infection occurs in nonpermissive cells (neurons). In some persistent infections, acute infection causes initial disease, which is followed by a chronic infection in which a low level of infectious virus is continuously produced with little or no damage to the target tissue. Initially, the immune system controls the infection by bringing the viral load lower than seen in acute infection; however, the immune system is unable to eliminate the infection during the acute phase. During chronicity, the virus is maintained via several mechanisms, such as infection of nonpermissive cells, spread to other cell types, antigenic variation, and inability of the immune response to completely eliminate the virus. Acute infection followed by latent infection and periodic reactivation Time Levels of infection by virus C. In these line diagrams, various patterns of viral infection are shown, including: A. Slow chronic infection Time Some unconventional infectious agents cause slow, chronic infection without acute symptoms Some unconventional infectious agents cause slow, chronic infection without acute infection such as caused by prions. This process is called viral transformation, and these viruses are oncogenic viruses. Viruses that can either cause tumors in their natural hosts or other species or can transform cells in vitro are considered to have oncogenic potential. Specifically, a tumor is an abnormal growth of cells and is classified as benign or malignant-depending on whether it remains localized or has a tendency to invade or spread by metastasis. When grown in tissue culture in the laboratory, these tumor cells exhibit a series of properties that correlate with the uncontrolled growth potential associated with the tumor in the organism. They have altered cell morphology and fail to grow in the organized patterns found for normal cells. In addition, they grow to a much higher cell density than do normal cells under conditions of unlimited nutrients and can lose contact inhibition and the requirement for growth on a solid substrate; therefore, they appear unable to enter the resting G0 state. Furthermore, they have lower nutritional and serum requirements than normal cells and are able to grow indefinitely in cell culture. These transformed or tumor cells often are used as cell lines for the culture or propagation of viruses in the laboratory. In addition to the listed properties, viral transformation usually, but not always, endows the cells with the capacity to form a tumor when introduced into the appropriate animal. Although the original use of the term transformation referred to the changes occurring in cells grown in the laboratory, current usage often includes the initial events in the animal that lead to the development of a tumor. In recent years, it has become increasingly clear that some, but not all, of these viruses cause cancers in the host species from which they were isolated. For some viruses, transformation or tumor formation has been observed only in species other than their natural host. Apparently, infections of cells from the natural host are so cytocidal that no survivor cells remain to be transformed. In addition, some viruses have been implicated in human tumors without any indication that they can transform cells in culture. In nearly all cases that have been characterized, viral transformation is the result of the continual expression of one or more viral genes that are directly responsible for the loss of growth control. Yes Yes Yes No Yes Yes No Yes Yes No Yes Yes Yes Yes Yes "Yes" means that at least one member of the group is oncogenic. Adenoviruses, papillomaviruses, and simian virus 40 all code for either one or two proteins that interact with the tumor suppressor proteins known as p53 and Rb (for retinoblastoma protein) to block their normal function, which is to exert a tight control over cell-cycle progression. In many respects, transformation is analogous to lysogenic conversion and requires that the viral genes be incorporated into the cell as inheritable elements. Unlike some of the temperate bacteriophages that code for the enzymes necessary for integration, papillomaviruses, polyomaviruses, and adenoviruses integrate by nonhomologous recombination using enzymes present in the host cell. It follows that for transformation to be successful, the insertional recombination must not disrupt a viral gene required for transformation. In summation, two events appear to be necessary for viral transformation: a persistent association of viral genes with the cell, and the expression of certain viral "transforming" proteins. First, many animal retroviruses have acquired transforming genes called oncogenes. These retroviruses require a helper virus as the insertion of the oncogene replaces a viral gene. More than 30 such oncogenes have now been found since the original oncogene was identified in Rous sarcoma virus (called v-src, where the v stands for viral). Because these transforming viruses carry cellular genes, they are sometimes referred to as transducing retroviruses. Most of the viral oncogenes have suffered one or more mutations that make them different from the cellular protooncogenes. These changes presumably alter the protein products such that they cause transformation. Although the mechanisms of oncogenesis are not completely understood, it appears that transformation results from inappropriate production of an abnormal protein that interferes with normal signaling processes within the cell. Because tumor formation in vitro by retroviruses carrying an oncogene is efficient and rapid, these viruses are often referred to as acute transforming viruses. Although common in some animal species, this mechanism has not yet been recognized as a cause of any human cancers. The second mechanism is called insertional mutagenesis and is not dependent on continued production of a viral gene product. Instead, the presence of the viral promoter or enhancer is sufficient to cause the inappropriate expression of a cellular gene residing in the immediate vicinity of the integrated provirus. This mechanism was first recognized in avian B-cell lymphomas caused by an avian leukosis virus, a disease characterized by a very long latent period. The site of the provirus insertion was found to be next to a cellular protooncogene called c-myc. In this case, transformation occurs not because the c-myc gene is altered by mutation, but because the viral promoter adjacent to the gene turns on its expression continuously and the gene product is overproduced. After such an integration event does occur, however, cell proliferation is rapid and a tumor develops. No human tumors are known for certain to result from insertional mutagenesis caused by a retrovirus; however, human cancers are known in which a chromosome translocation has placed an active cellular promoter next to a cellular protooncogene (Burkitt lymphoma and chronic myelogenous leukemia). In addition, a few retroviral gene therapy trials were stopped because of the induction of leukemia likely due to retroviral insertion near a protooncogene. This observation indicates that the tumor is a clone derived from a single cell; however, the sites of integration in tumors from different individuals are different. The resulting cellular proteins cooperate to cause uncontrolled cell proliferation. The tax gene is therefore different from the oncogenes of the acute transforming retroviruses in that it is a viral gene rather than a gene derived from a cellular proto-oncogene. It is thought that the constant inflammation and regeneration of hepatocytes leads to the eventual induction of the tumor and is, therefore, considered indirect oncogenesis. Several viral infections have repeatedly shown a variable range of outcomes from asymptomatic to symptomatic infections and even fatal disease is some cases. Furthermore, host factors probably play an important role in reversion of some of the live attenuated vaccines to a virulent state. Several of the host factors, including immune status, genetic background, age, and nutrition, play important roles in determining the outcome of viral infection. Several innate immune responses (interferons and, natural killer cells, mucocilliary responses, and others) and adaptive immune responses (antibody and T-cell responses) influence the outcome of viral infections. Individuals with weak immune systems or those who are immunocompromised or immunosuppressed often have more severe outcomes. Host genetics is one of the most important factors that influence the outcome of viral infections. The 32 homozygous allele is found in 1% of Caucasians, predominantly in Northern European populations. Age-related correlation between the host and several viral infections has been observed. It appears that age-related increased resistance to viral infections might reflect the maturity of the immune system and other defense mechanisms. For example, polio, hepatitis A, B, and E, and poxviruses are more severe during pregnancy, suggesting that hormones may influence viral pathogenesis. Nutritional state and personal habits of the hosts can also have an effect on viral pathogenesis.
Atractylis ovata (Atractylodes). Terbinafine.
- What is Atractylodes?
- Are there safety concerns?
- How does Atractylodes work?
- Dosing considerations for Atractylodes.
- Indigestion, stomach ache, bloating, edema, diarrhea, loss of appetite, rheumatism, and other conditions.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=97043
Buy terbinafine 250 mg without a prescription
The use of warmed fluids should be considered to avoid hypothermia with administration of large amounts of intravascular volume replacement anti fungal wash buy terbinafine 250mg with mastercard. Lactated Ringer solution and Plasma-Lyte A are the most commonly used isotonic solutions in pediatric patients. Administration of 5% albumin is the most common colloid used in pediatric patients, but disagreement exists as to the efficacy of this therapy versus isotonic crystalloid administration. Replacement of Preoperative Fluid Deficits the hourly maintenance rate should be calculated using the "4-2-1 rule" and should be administered in the form of isotonic solution throughout the case. Ongoing Fluid Losses Ongoing losses can be characterized as whole blood loss, third-space loss, and evaporation. Monitoring of urine output or central venous pressure can provide other information about intravascular Fluid Requirements Basis for Replacement Maintenance Weight (kg) <10 11-20 >20 Replacement of Ongoing Lossesa Type of surgery Noninvasive. If hypovolemia is suspected, a 10 to 20 mL/ kg bolus of crystalloid or colloid can be given. Glucose Administration Glucose-containing solutions should not be used routinely in pediatric patients intraoperatively. In children older than 1 year of age, the stress and catecholamine release associated with surgery usually prevent hypoglycemia. Glucose is commonly given to patients who are younger than 1 year of age or less than 10 kg. Pediatric patients at greater risk for developing hypoglycemia include premature and term neonates and any patient who is critically ill or who has hepatic dysfunction. Patients receiving total parenteral nutrition with high dextrose concentrations preoperatively can either be continued on a reduced rate of the same infusion or can be converted to a 5% or 10% dextrose-containing infusion to maintain the administration of glucose. An infusion pump should be used for high-concentration dextrose solutions to avoid bolus administration. Blood glucose concentration should be monitored closely in patients with risk of glucose instability. Irradiation of blood products is necessary to reduce the risk of transfusion-associated graft-versus-host disease, a potentially fatal condition in which transfused lymphocytes engraft and proliferate in the bone marrow of the recipient. Administration of 5 to 10 mL/kg of platelet concentrate should increase the platelet count by 50,000/dL to 100,000/dL. Indications for platelet transfusion are dependent on platelet number, function, and the presence or absence of bleeding. Fresh Frozen Plasma Initial treatment for blood loss is to maintain intravascular volume by administering crystalloid or colloid solution. Prothrombin complex concentrates are derived from human plasma and contain vitamin K-dependent coagulation factors. This reduces the waste of a residual unit when only 60 mL, for example, is required for transfusion. It also 594 Cryoprecipitate and fibrinogen concentrate are sources of fibrinogen for replacement. It is ideal for administration to infants because of high levels of these factors in a small volume. Administration of 1 unit (10 to 20 mL) for every 5 kg to a maximum of 4 units is usually adequate for correcting coagulopathy due to insufficient fibrinogen. It is increasingly being used for fibrinogen replacement in pediatric cardiac surgery and other complex pediatric surgeries, including Chapter 34 Pediatrics craniosynostosis and scoliosis repair. These drugs can decrease bleeding and the transfusion requirements during pediatric cardiac, spine, and cranial reconstructive surgery. Aprotinin is not available for use at this time owing to concerns about adverse effects in adults. Over the last 10 years, there have been multiple reports of off-label use of the drug in nonhemophiliac pediatric patients in a variety of situations including postcardiopulmonary bypass bleeding and trauma with a reduction in transfusion of blood products and normalization of coagulation studies. Care should be taken to inspect for micrognathia, midface hypoplasia, limited mouth opening or cervical mobility, and other craniofacial anomalies that can predict difficult laryngoscopy. The patient and parents should be questioned about the presence of loose teeth or orthodontic appliances that may be dislodged or broken during airway manipulation (also see Chapter 16). An appropriately sized mask should be selected, and care should be taken to optimally position the patient to avoid airway obstruction. If obstruction is encountered, continuous positive airway pressure of 5 to 10 cm H2O or an oral airway can be introduced to restore airway patency. They can also be used with pressure control mechanical ventilation safely in children. A 2014 meta-analysis found that the use of the laryngeal mask during pediatric anesthesia was associated with a decreased incidence of respiratory complications including desaturation, laryngospasm, cough, and breathholding compared with tracheal intubation. Historically, uncuffed tubes were the standard of care in children younger than 8 years of age because of concerns about subglottic stenosis and postextubation stridor. As a result of innovation in material and design, cuffs are now very thin and do not enlarge the outer diameter of the tube, and downsizing the inner diameter tube size to compensate for the bulk of the cuff is no longer recommended. A difficult airway should be anticipated in patients with craniofacial abnormalities or syndromes including Pierre Robin, Treacher Collins, and Goldenhar syndromes. Infants and young children have larger craniums and thus it is unnecessary to place a pillow under the occiput to achieve the "sniffing position" for airway management. The tongue is often relatively large in young infants and can more easily obstruct the airway. The cricoid ring is the narrowest part of the airway of the infant and young child, instead of the laryngeal aperture at the vocal cords as in adults. A history of sleep-disordered breathing (obstructive sleep apnea), heralded by obstructed breathing or loud snoring during sleep, may be associated with difficult face mask ventilation and higher sensitivity to opioid-induced respiratory depression. A review of systems should be performed, and any pertinent positive findings should be explored. The patient and parent should be questioned about the presence or recent history of congestion, cough, fever, vomiting, or diarrhea, which may impact the decision to proceed with an elective procedure. Vital signs, including heart rate, respiratory rate, temperature, and arterial blood pressure, should be measured. Use of a pulse oximeter can be used to screen for occult cardiac or pulmonary disease. The airway should be examined as thoroughly as possible with attention to craniofacial abnormalities, presence of micrognathia, and tonsillar size. The heart and lungs should be auscultated to evaluate for murmurs and wheezing or decreased breath sounds. The patient should be examined for any signs of infectious process including rhinorrhea, tonsillar exudate, fever, and cough. Drugs are commonly dosed based on weight, and accuracy is critical to avoid under- and overdosage. A history of prematurity is important, including the gestational age at which the patient was delivered and any sequelae of prematurity such as cerebral palsy, chronic lung disease and apnea, and bradycardia. If the child has a genetic or dysmorphic syndrome, distinguishing features should be reviewed for potential impact on the anesthetic including craniofacial or cervical spine abnormalities that may lead to a difficult endotracheal intubation. However, preoperative testing may be indicated in children with organ system dysfunction. Hemoglobin should be measured in former premature infants at risk for anemia having procedures associated with significant blood loss. If echocardiogram results or subspecialist notes are available, they should also be reviewed. Adolescent females are unlikely to admit that they are sexually active or if there is a chance that they Chapter 34 Pediatrics might be pregnant. Asking the parent and child about the possibility of pregnancy can be uncomfortable for all parties. There must also be a process for revealing the results to the patient and parents and for counseling, based on local institutional considerations and individual state law. Still, there is a slightly increased risk of airway hyperreactivity with associated bronchospasm, laryngospasm, and postoperative arterial desaturation due to atelectasis. The patient should be examined for nasal congestion, cough, wheezing, and fever, and if a decision is made to proceed with the anesthetic, care should be taken to minimize risk of an adverse respiratory event.
Discount terbinafine 250mg with visa
Affected individuals develop an axonal antifungal research buy terbinafine paypal, distal neuropathy with onset in the second decade. The rate of progression varies within families, with some developing proximal weakness early in the disease and others showing little progression [84]. Affected individuals present with a length-dependent mixed motor and sensory neuropathy between the ages of 26 and 42 and remain ambulant in later life [87]. Nerve conduction studies demonstrate a patchy demyelinating neuropathy, although nerve conduction velocities are often in the axonal range in affected females. It is an episodic disorder characterised by recurrent, painless motor and sensory entrapment neuropathies often preceded by minimal trauma. The cardinal neurophysiological finding is the presence of a more generalized neuropathy outside of the clinically affected nerves. The age of onset may vary from the first to the sixth decade and it is often slowly progressive with no loss of ambulation [95]. Additional clinical features include neutropenia, cataracts, ptosis, and ophthalmoplegia [93,96]. Affected individuals developed features of a neuropathy in the 1st and 2 decade (range 5 -28 years) and end stage renal failure by 21 years of age (range 12 to 47). It is also important to convey to the patient the degree of certainty that any novel mutation is pathogenic. Whilst this option may seem attractive, it is associated with reduced rates of conception and is not universally available. Whilst there are many theories about the aetiology of pes cavus, the disorder is still incompletely understood. Fusions Triple arthrodesis is the mainstay of treatment for a severely affected rigid cavovarus foot deformity. It is an option of last resort, however, and commonly results in accelerated arthritic change in the foot. Proposed therapeutic strategies have included ascorbic acid, curcumin, neurotrophin 3, progesterone antagonists, and histone deacetylase inhibitors. Transfer of the peroneus longus tendon to the peroneus brevis muscle may also be performed to correct forefoot cavus deformity. Secondly, the action of the stronger peroneus longus muscle on the everting peroneus brevis muscle insertion reduces the hindfoot varus (inversion) deformity. Clinically distinct codon 69 mutations in major myelin protein zero in demyelinating neuropathies. Discussions around family planning, and the option of prenatal genetic testing, should be approached early so that patients have time to make an informed decision. Relative quantification of 40 nucleic acid sequences by multiplex ligation-dependent probe amplification. Peripheral myelin protein 22 and protein zero: a novel association in peripheral nervous system myelin. Autosomal recessive hereditary motor and sensory neuropathy with focally folded myelin sheaths: clinical, electrophysiologic, and genetic aspects of a large family. Gene mapping in Gypsies identifies a novel demyelinating neuropathy on chromosome 8q24. Genes for hereditary sensory and autonomic neuropathies: a genotype-phenotype correlation. Curcumin treatment abrogates endoplasmic reticulum retention and aggregation-induced apoptosis associated with neuropathy-causing myelin protein zero-truncating mutants. Hallmark features comprise progressive distal sensory loss, nail changes, painless injuries, and chronic skin ulcers which are frequently complicated by spontaneous fractures and neuropathic arthropathy that often lead to amputations of distal or even proximal parts of the limbs. De novo mutations at S331 have been reported in four unrelated patients and displayed an unusually severe syndromic phenotype characterized by congenital onset with severe growth retardation, hand tremor, hypotonia, juvenile cataracts and vocal cord paralysis [20,25a,25b]. The I504F mutation occurred de novo in a patient presenting with an early onset sensorimotor neuropathy, complicated by ulcerations and osteomyelitis. The two other mutations (V359M and I504F) are located on the surface of the protein. The clinical phenotype is characterized by severe sensory disturbances affecting all senses, foot ulcers, and amputations. There was no intellectual impairment, but both affected individuals had mild muscle weakness. Nerve conduction studies showed slightly reduced motor and sensory nerve conduction velocities but normal amplitudes. Hyperhidrosis and gastrointestinal dysfunction were observed in both, suggesting autonomic involvement. The gain-of-function mechanism that underlies this channelopathy suggested an alternative way to modulate pain perception. Screening a large cohort of 115 patients detected the same mutation (Y192C) in a second family exhibiting a similar phenotype with distal sensory loss in the lower limbs, reduced tendon reflexes, and acromutilations. Additional features included throat clearing, hoarse voice, cough syncope, and sensorineural hearing loss.
Best order for terbinafine
The predominant symptom in each is myotonia antifungal rinse for mouth cheap 250mg terbinafine with amex, although variable muscle weakness or paralysis can additionally occur (see Table 31. The exact incidence is unknown but estimates range from 1 in 100 000 to 7 in 100 000 [39]. Symptoms are generally noted by the patient themselves within their first decade [41,42], often when they attend primary school. Characteristic symptoms are myotonia, especially of the hand and facial muscles, that is exacerbated by a cold environment or by repetitive muscle action. Conversely a warm environment often alleviates the myotonia and there is frequently a seasonal variation to the severity of the disease. A common story is struggling to change clothes in a cold changing room Treatment of acute attacks of paralysis Total body potassium during an attack of muscle weakness is normal but the distribution is displaced. Facial muscles may be lower limbs more than lower limbs involved None or minimal Present Absent Absent Uncommon Yes-often dramatic Absent Present Absent Variable-ranging from none to severe May be present May be present May be present. This is re-used with permission from: the non-dystrophic myotonias: molecular pathogenesis, diagnosis and treatment. The sodium channel myotonias this can be the hardest group of the non-dystrophic myotonias to characterize. These include the potassium-aggravated myotonias (acetazolamide-responsive myotonia congenita [43,44], myotonia fluctuans [45,46], and myotonia permanens [47,48]). The myotonia itself displays overlapping features of paramyotonia congenita and myotonia congenita in that it can be paradoxical or display warm up. Myotonia congenita the age of onset of myotonia congenita is commonly also in the first decade, although it can be a few years later than paramyotonia congenita [42]. It is important to enquire about physical activity because the significance of a muscular physique may be overlooked in young patients if it is assumed that it reflects an active lifestyle. A transient muscle weakness can also occur after a period of rest and for unknown reasons this also improves with activity. Myotonia congenita is the only skeletal muscle channelopathy that can be inherited in either a dominant (Thomson disease [52]) or recessive manner (Becker disease [53]), both involving the voltage-gated chloride channel ClC-1. Transient weakness is often absent in dominant cases and it can be very difficult to differentiate this clinically from sodium channel myotonia. A more formal timed 10-m walk can be performed, but in practice this is usually reserved for clinical trials. There are a number of general points to consider when examining a patient displaying myotonia: In paramyotonia congenita the myotonia is paradoxical and will worsen with repetitive muscle action. In myotonia congenita the myotonia will display a warm-up phenomenon and improve with repetitive muscle action. In sodium channel myotonia the myotonia may be paradoxical or show warm up or display both features. If a cold environment is volunteered as a severe precipitating factor for the myotonia this suggests paramyotonia congenita. Investigations Blood tests In general blood tests have no specific role in the investigation of non-dystrophic myotonia. If present each muscle action should be repeated two or three times at least to establish if the myotonia is improving (warm up) with repetition or worsening. Another useful way of assessing this is to ask the patient to rise from a chair, walk across the clinic room, sit down, and then repeat the exercise. More advanced neurophysiological techniques include the short and long exercise tests. However, if either of these conditions is suspected and gene sequencing of one gene is negative the other gene should be screened. These are useful techniques but are not always readily available outside of specialist centres. Also these are the patterns seen in typical examples of each subgroup but there can be significant overlap and variability so they are not diagnostic in isolation. Myotonia congenita is the only skeletal muscle channelopathy to be inherited in either an autosomal dominant or autosomal recessive fashion. Although there is a lack of trial evidence, benefit from both flecainide and propafenone has been described in case studies [62,63]. Even in Canada, however, there is a risk that manufacture may cease in the future. There are small series and case reports describing benefit from the carbonic anhydrase inhibitor acetazolamide [43,66] which is widely used as a treatment for periodic paralysis. This is not generally the first choice for the non-dystrophic myotonias but may be tried if other therapies are ineffective or if antiarrhythmics are contraindicated. Historical treatments have included quinine, procainamide, prednisolone, phenytoin, and lignocaine but none of these are currently recommended. Tocainide, a lignocaine derivative, seemed a promising therapy but was withdrawn from the market following reports of potentially fatal agranulocytosis [39]. The most significant includes a fatal case that involved myotonia of the respiratory muscles with the infant ultimately dying from respiratory failure [68]. Overall, labour in skeletal muscle channelopathy should be considered of relatively high risk and managed in a centre that has appropriate senior obstetric, paediatric, and anaesthetic services available. This may be sufficiently mild that the patient is not functionally limited and it is only evident on clinical examination, or severe enough for a wheelchair and home modification to be required. Pain may occur with myotonia or in isolation, but as at least some of the pain is usually linked to myotonia it is likely that this aspect will respond to mexiletine therapy although there is no trial evidence currently available to support this. Development of future therapies Several possibilities for newer therapies are on the horizon. The skeletal muscle channelopathies themselves have no adverse effect on fetal development, although some consideration may be given to the risk of injury should an attack of muscle paralysis or myotonia provoke a fall. Fatal dysrhythmia following potassium replacement for hypokalemic periodic paralysis. Sodium channel mutations in acetazolamide-responsive myotonia congenita, paramyotonia Practical issues are often also overlooked. Cold is such a severe exacerbator of symptoms in paramyotonia congenita that some patients dread the winter months and have their central heating on for the majority of the time. A Korean family of hypokalemic periodic paralysis with mutation in a voltage-gated calcium channel (R1239G). Spinal anesthesia for a patient with a calcium channel mutation causing hypokalemic periodic paralysis. Tonische Krampfe in willkurlich beweglichen Muskeln in Folge von ererbter psychischer Disposition. A new case of autosomal dominant myotonia associated with the V1589M missense mutation in the muscle sodium channel gene and its phenotypic classification. Data from similar autoimmune diseases support the hypothesis that these conditions result from chronic immune activation after exposure to environmental risk factors in individuals with a predisposing genetic background [20,21]. At the time of referral she was barely able to climb stairs and she fell frequently. Three months prior to referral she was diagnosed with breast cancer, for which she underwent surgery followed by radiotherapy and chemotherapy. On examination she was found to have characteristic skin changes, including heliotrope erythema in the face, Gottron papules. She had a dropped head due to weakness of the neck extensor muscle, and in addition the neck flexors and proximal muscles of the arms and legs were affected (varying from Medical Research Council grade 2 to 4). Since the dermatological features were characteristic we refrained from ancillary investigations and a diagnosis of dermatomyositis was established. Prednisone, 100 mg per day, was prescribed for 6 weeks and subsequently the medication was tapered. She came quickly into remission and did not relapse when the prednisone was further tapered.