Generic 100 mg vibramycin amex
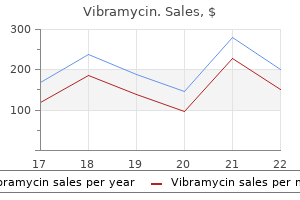
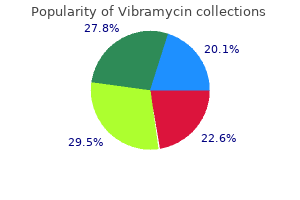
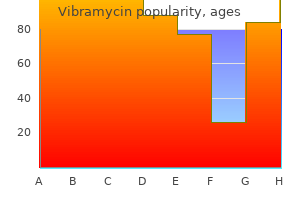
Itraconazole Isocarboxazid It is not known whether isocarboxazid crosses the placenta (it does in rats) medicine song buy vibramycin visa. Experience with isocarboxazid during lactation is also lacking, and it is not known if it enters breast milk. While evidence from cohort studies shows brief exposure to this antifungal during early pregnancy is compatible with a normal pregnancy outcome, there is evidence of doserelated toxicity and teratogenicity in animals, and other azoles are known to induce malformations in man. Reports of use, whether inadvertent or otherwise, show low risk of major congenital malformations. In newborn animals, it has been shown to cause bony defects, and for this reason, it is best avoided (fluconazole would be a better alternative). It may be used topically; other antifungals should be used if systemic administration is required. Ketoconazole passes into breast milk in small amounts (these are probably negligible when ketoconazole is used topically); moreover, absorption (which is best under acidic conditions) may be reduced by the breast milk. Omeprazole is a better studied alternative (it enters breast milk in low levels but has a known safety profile). Although there are no reports of levocetirizine use during pregnancy, it is expected that there will be similarities with cetirizine. Neither first- nor second-generation antihistamines have been found to be teratogenic. It is not known if levocetirizine enters breast milk (cetirizine is reported to do so). In general, first-generation antihistamines are preferred to newer ones due to the greater experience of use. Acute renal failure has been reported in preterm infants whose mothers received ketoprofen prior to delivery. Ketoprofen passes into breast milk in small amounts that are unlikely to affect the breastfed infant. Oligohydramnios was not seen in 45 women treated with ketorolac in a trial looking at its use as a tocolytic. Small quantities of ketorolac are found in breast milk but are unlikely to cause any problems in the breastfed infant. Poor maternal absorption (~3% of the dose only) means that it is unlikely the maternal systemic concentration will reach a level that will impact on the fetus. Again, because of poor maternal absorption, it is unlikely that the breastfed infant would receive a significant amount. While it appears to concentrate in the fetal brain, most studies reveal no evidence of teratogenicity, and rodent studies are generally reassuring. Levodopa is excreted into breast milk in small amounts that do not seem to cause problems in the breastfed infant. While it suppresses prolactin release, the suckling stimulus seems to override any inhibitory effect in most women. Levofloxacin Animal studies of several quinolones show a juvenile arthropathy, and it is this toxicity that has lead to their restricted use during pregnancy. Rodent studies with levofloxacin are reassuring, and less than 4% of levofloxacin crosses an isolated perfused human placenta, suggesting that it might be safer than 584 Maternal medication and the baby insufficient to act as hormone replacement for the breastfed hypothyroid infant. Levofloxacin passes into breast milk, but the breastfed infant receives far less than is used to treat children. It is not known whether levomepromazine crosses the placenta, and rodent teratogenicity studies have not been performed. Lisinopril Levothyroxine sodium Transplacental transfer of thyroxine is low but is sufficient to prevent the fetus without a thyroid gland from showing overt clinical hypothyroidism. In contrast, even subclinical maternal hypothyroidism in early pregnancy may increase the risk of spontaneous abortion and adversely affect neurodevelopment. While no adverse effects are reported following first trimester use, exposure during the third trimester is reported to cause fetal renal failure (which may be irreversible) and oligohydramnios. Screening for oligohydramnios may detect the affected fetus and allow cessation of lisinopril therapy. Because the drug is renally excreted, the effects may be prolonged and, in some cases, become irreversible. There are no reports of lisinopril use during lactation, nor is it known if lisinopril enters breast milk. No information is available on the use of linagliptin during breastfeeding or whether it passes into breast milk. Linagliptin is best avoided during both pregnancy and lactation until further information is available. Use of loperamide during pregnancy does not seem to be associated with an increased risk of major malformations. Because it is minimally absorbed, only extremely small amounts may be found in breast milk. Transplacental transfer of endogenous T3 occurs in low, but physiologically relevant, levels. Dose adjustment of thyroid hormones is frequently needed during pregnancy, and even subclinical hypothyroidism is best avoided. These do not cause any reported adverse effects and are It is not known whether loratadine crosses the placenta. One early study observed a prevalence of hypospadias twice that of the general population; however, this has not been confirmed. Loratadine and its active metabolite, descarboethoxyloratadine (desloratadine), pass into breast milk, but the breastfed infant receives a dose of less than 1% of the adult dose on a milligram-per-kilogram basis. They are becoming the most commonly prescribed Maternal medication and the baby laxative in pregnant women. It is not known if macrogols cross the placenta, but there is little if any systemic absorption. With the lack of systemic absorption, they are unlikely to achieve clinically relevant levels in breast milk. There is some suggestion that in utero exposure of male fetuses may double the risk of hypospadias. Abnormalities beyond the external genitalia are not noted in either humans or rodents. Although not specifically used as a galactagogue, depot medroxyprogesterone is reported to have beneficial effects on milk supply in women using the drug for contraception. Several studies suggest an increased prevalence of malformations associated with first trimester use. There was no clear evidence of teratogenicity or fetotoxicity following attempted maternal suicide when very large doses were ingested. As with many drugs during pregnancy, monotherapy and using the lowest effective dose might minimise the risks. Small amounts of meprobamate enter breast milk, but these do not pose a clinically significant risk to the breastfed infant. If mefenamic acid is to be used during the second and third trimesters, the fetus must be monitored for signs of ductal closure. Small amounts of mefenamic acid pass into breast milk and may be absorbed by the nursing infant. Although the manufacturer advises to avoid its use, in general, it is regarded as being compatible with breastfeeding. Mercaptopurine, the active metabolite of azathioprine, is a commonly used anti-neoplastic and immunomodulatory agent that may be required during pregnancy. It probably crosses the placenta and, as a result, can cause severe, but transient, neonatal pancytopenia. The effects of administration during the first trimester are mixed; some cohort studies report a higher incidence of anomalies, while others do not. Many women are exposed to more than one drug as well as to the effects of the underlying disease. Rodent studies show some evidence of teratogenicity with malformations of the jaw, limbs and gut. In general, treatment should not be withheld if medically indicated, and the risk of neonatal marrow suppression can be minimised by reducing the dose near to term. Mercaptopurine and azathioprine pass into breast milk in small amounts, and although marrow suppression may occur in the breastfed neonate, the risk is very low. Use during lactation also seems safe although diarrhoea has been reported in a few babies.
Cheapest vibramycin
Dissolve the powder in 2 ml of water for injection; the reconstituted solution can be further diluted to the volume required with 0 treatment 2nd degree heart block order vibramycin cheap. To give 5000 units/kg/hour, place 1 ml of the reconstituted solution from a 100,000 unit vial for each kilogram the baby weighs in a syringe, dilute to 10 ml with 0. Primary operative versus nonoperative therapy for pediatric empyema: a meta-analysis. Primary early thoracoscopy and reduction in length of hospital stay and additional procedures among children with complicated pneumonia: results of a multicenter retrospective cohort study. Comparison of urokinase and video-assisted thoracoscopic surgery for treatment of childhood empyema. Treatment of central venous catheter occlusions with ethanol and hydrochloric acid. It can relieve the severe itching (pruritus) that can occur in obstetric cholestasis although it does not prevent disease progression. It is less effective in dealing with the cholestasis sometimes caused by parenteral nutrition. Pharmacology Ursodeoxycholic acid is a naturally occurring bile acid originally described (ursocholeinsaure) in bile obtained from polar bears. It was later crystallised from black bear bile in Japan in 1927 by Shoda who renamed it ursodeoxycholic acid. Ursodeoxycholic acid occurs in all members of the Ursidae family, and that obtained from bears is still used in traditional Chinese medicine. Small quantities are excreted in human bile and then reabsorbed from the gastrointestinal tract (enterohepatic recirculation). It suppresses the synthesis and secretion of cholesterol by the liver and the intestinal absorption of cholesterol, and a trial in 1980 showed that it could be used to effect the slow dissolution of symptomatic cholesterol-rich gallstones in patients reluctant to undergo surgery or lithotripsy. Ursodeoxycholic acid has been used in a number of other conditions, although such use is not endorsed by the manufacturers. They do not recommend use during pregnancy, although treatment with 1 g/day is increasingly being used in patients with obstetric cholestasis. Safe use has also been reported in a patient with primary biliary cirrhosis who took the drug throughout pregnancy. Ursodeoxycholic acid does not enter human breast milk and thus poses no risk to the breastfed infant. Reports suggest that the drug is of benefit in some babies with cholestasis due to biliary atresia, alpha-1-antitrypsin deficiency, cystic fibrosis and Alagille syndrome, although it is less clear whether it delays the development of cirrhotic liver damage. Although it may sometimes reduce the serum bilirubin in babies developing cholestasis complicating prolonged parenteral nutrition, liver enzyme levels usually remain high. Side effects are uncommon, although intestinal discomfort may occur initially, and diarrhoea has occasionally been reported. A recent historical cohort review of use in neonatal cholestatic disease has suggested that the drug may not only be ineffective but harmful. Treatment In pregnancy: 500 mg twice a day has not yet been shown to slow disease progression but may help in itching. Ursodeoxycholic acid treatment in preterm infants: a pilot study for the prevention of cholestasis associated with total parenteral nutrition. Efficacy of ursodeoxycholic acid in treating intrahepatic cholestasis of pregnancy: a meta-analysis. Ursodeoxycholic acid for intrahepatic cholestasis of pregnancy: good for the mother, not bad for the baby. Assessment of stool colour in community management of prolonged jaundice in infancy. Review of historical cohort: ursodeoxycholic acid in extrahepatic biliary atresia. Ursodeoxycholic acid in neonatal hepatitis and infantile paucity of intrahepatic bile ducts: review of a historical cohort. Ursodeoxycholic acid in the treatment of cholestasis of pregnancy: a randomised double-blind study controlled with placebo. Population screening for neonatal liver disease: potential for a community-based programme. Effect of ursodeoxycholic acid on liver function in children after successful surgery for biliary atresia. Empiric use is common when nosocomial infection is suspected and the organism is not yet known, but flucloxacillin (q. Pharmacology the glycopeptide antibiotic, vancomycin, first isolated in 1953, is bactericidal to most Grampositive organisms, but is inactive against Gram-negative organisms. It is very poorly absorbed by mouth, and causes pain and tissue necrosis when given intramuscularly. This not only means that it has to be given with caution in patients with poor renal function, but that there is at least a two- to threefold difference in vancomycin clearance within the neonatal population, reflecting in part maturation and disease-related renal impairment (including that induced by other drugs) in an individual. There is no evidence of toxicity in animals, nephrotoxicity has not been seen with the product currently used, and most patients developing ototoxicity were also taking an aminoglycoside or diuretic (suggesting that damage was wrongly attributed, or that combined use increases the risk). Although vancomycin enters breast milk, poor oral absorption means it is unlikely the breast fed neonate will receive clinically relevant amounts. Giving both vancomycin and rifampicin minimises the risk of initially sensitive organisms becoming resistant, and is particularly useful in catheter and shunt-related coagulase-negative staphylococcal infection. Vancomycin is a time-dependent antibiotic, and activity is highly correlated with the duration of bacterial exposure to the antibiotic rather than being concentration dependent. If an infusion is used, it is essential to give a loading dose at the beginning otherwise it would take almost 2 days to reach a steady state concentration. Oral: Giving 15 mg/kg by mouth once every 8 hours for 7 days can reduce the risk of necrotising enterocolitis (as can an oral aminoglycoside), but might encourage the proliferation of multiresistant bacteria. Maintenance dose Post-menstrual age (weeks) <27 27 to <30 30 to <32 32 Loading dose (mg/kg) 10 10 15 15 Normal renal function* (mg/kg/day) 20 25 25 30 Impaired renal function* (mg/kg/day) 15 20 20 25 *Renal impairment suggested by serum creatinine concentration >90 mol/l. For babies older than 1 week: Maintenance dose Post-menstrual age (weeks) <27 27 to <30 30 to <32 32 Loading dose (mg/kg) 10 10 15 15 Normal renal function* (mg/kg/day) 25 30 30 35 Impaired renal function* (mg/kg/day) 20 25 25 30 *Renal impairment suggested by serum creatinine concentration >90 mol/l. References (See also relevant Cochrane reviews) Arnell K, Enblad P, Wester T, et al. Treatment of cerebrospinal fluid shunt infections in children using systemic and intraventricular antibiotic therapy in combination with externalisation of the ventricular catheter: efficacy in 34 consecutively treated infections. Vancomycin-induced nephrotoxicity: mechanism, incidence, risk factors and special populations. Prophylactic antibiotics in the prevention of catheter-associated bloodstream bacterial infection in preterm neonates: a systematic review. Continuous-infusion vancomycin therapy for preterm neonates with suspected or documented gram-positive infections: a new dosage schedule. Vancomycin during pregnancy: does it cause hearing loss or nephrotoxicity in the infant Vancomycin continuous infusion in neonates: dosing optimisation and therapeutic drug monitoring. Chickenpox during pregnancy can cause severe pulmonary disease (although selective reporting may have led to the magnitude of the risk being exaggerated). No technique has yet been developed for identifying whether the fetus has been affected or not, nor should it be assumed that exposure in the third trimester incurs no risk. Infection shortly before birth certainly exposes the baby to the risk of severe neonatal infection. These babies are at risk of multi-organ involvement and death from necrotising pneumonia. Try to delay labour for at least 3 days if the mother develops a typical rash shortly before delivery is due.
Vibramycin 100 mg discount
In 1975 medications qt prolongation purchase vibramycin with a mastercard, Jones and colleagues70 summarized the findings of an additional 40 cases subsequently reported in the literature, and 20 of their own patients. Ultrasound is a reliable noninvasive screening tool for infants during the first 6 months of life. Treatment, course, and management Although the need for surgical management of intraspinal lipomas associated with lumbosacral lipomas is controversial, it should be recognized that the development of neurologic impairment can be delayed for years. Consequently, immediate neurosurgical evaluation and long-term neurologic follow-up are required. Cutaneous findings Most patients report that lesions were present at birth or appeared in the first two decades of life. Unilateral involvement of the buttock is most common, but plaques may extend to the adjacent skin of the upper thigh or lower back. Usually lesions do not cross the midline, but bilateral involvement of opposing surfaces of the buttocks has been reported. However, new lobules may develop slowly for decades, and recurrent lesions after excision or progression may be associated with infiltration of the underlying muscle. Histopathology shows some hyperkeratosis and acanthosis of the epidermis and a marked increase in mature fat cells throughout the dermis. However, they may extend into the papillary dermis, and the distinction between the dermis and subcutaneous fat 450 27 Disorders of the Subcutaneous Tissue may be poorly defined. Although the remainder of the dermis often appears normal, other connective tissue anomalies, including thickening of collagen and elastic fibers, and increased numbers of fibroblasts and blood vessels with a perivascular mononuclear infiltrate, may also develop. Differential diagnosis the varying clinical findings explain the wide range of clinical diagnoses suspected before skin biopsy. These include pigmented nevi, supernumerary nipples, lipomas, neurofibromas, connective tissue nevi, sebaceous nevi, epidermal nevi, and warts. Consequently, treatment is not necessary, but surgical excision, particularly for small lesions, gives a good cosmetic result. Moreover, excision should be considered in lesions that demonstrate progressive growth. Papular and polypoid nodules, often contiguous to the scalp lesions, are constant features on the face of affected infants. Affected children seem to be prone to the development of benign osseous lesions, including ossifying fibromas, odontomas, osteomas, and fibrous dysplasia. Diagnosis Biopsies of the cutaneous nodules show normal epidermis overlying a dermis with irregularly shaped collagen fibers that extend into the subcutis and form large fibrous septa associated with increased amounts of fat. However, careful analysis of clinical and histologic features will help to distinguish these neurocutaneous genodermatoses. Treatment and course the care of affected children is determined by neurologic symptoms, which range from normal to global neurodevelopmental retardation, unilateral spasticity, and mental retardation. Moreover, the severity of neurologic symptoms does not seem to correlate with the extent of cutaneous involvement. Children without clinical evidence of neurologic involvement should be screened for occult spinal anomalies. Since then, a number of cases of this rare hamartomatous disorder have been reported, demonstrating the variability of clinical and histologic findings. Although scalp hair is usually normal, long curled eyelashes and thick eyebrows are typical. Extracutaneous findings Although affected children may be otherwise normal, a number of anomalies have been reported. Variable oral anomalies, including cleft lip and palate, a higharched palate, dental hypoplasia, and micrognathia, are common. Orthopedic defects such as rocker-bottom feet, metatarsus abductus, coxa valga, genu valgus, overlapping of toes, and pectus excavatum may require surgical intervention. Lesions undergo minimal change over time, though proportionate growth may be seen. Possible etiologies include a hamartomatous condition with incomplete regression of fetal tissue or a developmental defect in the plantar aponeurosis. Differential diagnosis includes piezogenic papules seen on the lateral surface of the feet in older children, fibrous hamartoma of infancy, and aponeurotic fibroma. Treatment and course Although the natural history is not fully known, lesions seem to persist over time. Van Meurs96 subsequently wrote of his experience with an infant with a lipomatous tumor in the right axilla that required four surgeries over a 2-year period before she was free of recurrence. In 1973 Chung and Enzinger97 reported a large series of lipomatous tumors in infancy and proposed that the term lipoblastoma be used to describe the well-encapsulated variant and that lipoblastomatosis be reserved for unencapsulated infiltrating lesions. Diagnosis Skin biopsies from the extremities of affected children have shown changes in the dermis consistent with nevus lipomatosus cutaneous superficialis or smooth muscle hamartoma. Treatment, course, and management Management of affected individuals depends on the presence of associated anomalies. Clinicians should look carefully for oral and orthopedic anomalies, which may require early surgical intervention. Differential diagnosis Lipoblastomatosis should be differentiated from liposarcoma, an exceedingly rare tumor in children under 10 years of age. Although extensive infiltration into local muscle and fascial structures precludes complete excision, in most cases maturation of recurrent tumor results in a favorable outcome. Lipodystrophies the lipodystrophies are a rare group of disorders characterized by complete or partial loss of fat. The congenital variants are inherited in an autosomal recessive pattern and express variable abnormalities in carbohydrate and lipid metabolism and insulin resistance. However, unusual sites, including the parotid gland, mediastinum, and tonsils, have been reported. This is supported by observations of histologic maturation of adipose cells in recurrent tumors. Diagnosis Histologically, lipoblastoma is encapsulated or well circumscribed, whereas in lipoblastomatosis the tumor infiltrates surrounding normal structures. The lobules are separated by fibrous septa Donohue and Uchida105,106 were the first to describe this rare syndrome when they reported their observations on two sisters of consanguineous parents, with intrauterine growth retardation, gnome-like facies, and severe endocrine dysfunction evidenced by emaciation, enlargement of the breasts and clitoris, and histologic changes in the ovaries, pancreas, and breasts. The incidence of this autosomal recessive disorder has been estimated at 1 in 4 million live births, and the prevalence of the carrier state as at least 1 in 1000 individuals. Etiology and pathogenesis Initially leprechaunism was identified as a primary endocrinologic disorder because of the associated cystic changes of the gonads and hyperplasia of the islet cells of the pancreas. The skin tends to become coarse, particularly in boys, and patients often develop warty fibromas on the upper half of the body. Extracutaneous features An anabolic state develops, with increased height velocity, advanced bone and dental age, muscular hypertrophy, masculine body build, acromegaloid stigmata, organomegaly, and enlarged genitals. Patients tend to be hypermetabolic with a voracious appetite, increased energy consumption, and associated hyperhidrosis and decreased heat tolerance. Cardiac muscle hypertrophy is also present at birth and may result in progressive hypertrophic cardiomyopathy with decrease in cardiac function. Diagnosis Diagnosis can be made by identifying characteristic clinical, biochemical (fasting hypoglycemia, postprandial hyperglycemia, and extreme hyperinsulism), and genetic findings. Prenatal diagnosis is possible by similar evaluation of chorionic villus biopsy specimens. Differential diagnosis Leprechaunism shares many features with congenital total lipoatrophy, including insulin resistance, absence of subcutaneous fat, acanthosis nigricans, and hyperpigmentation. Treatment and course Postnatal growth is invariably poor, and affected children are severely motor and mentally retarded. Infants rarely survive beyond the first few months of life unless they have some residual insulin receptor function. Recent data suggest 454 27 Disorders of the Subcutaneous Tissue that allow for diagnosis at birth. Metabolic features include insulin resistance, hyperinsulinemia, hypertriglyceridemia, and nonketotic diabetes. Hypertriglyceridemia varies from patient to patient, but tends to increase at puberty and with increased dietary fat consumption. In childhood, glucose and insulin levels tend to be normal except with large glucose challenges. However, at or shortly after puberty, glucose metabolism deteriorates, with the development of clinical diabetes with hyperinsulinemia, elevated serum glucose, and glycosuria. Neonatal progeroid syndrome, described in the late 1970s by Wiedemann and Rautenstrauch is inherited as an autosomal recessive disorder but the genetic marker has not yet been identified. However, investigators have suggested that a defect in biosynthesis of proteins in the nucleus may be involved.
Buy 100mg vibramycin with visa
Do not employ a less than 1 m filter symptoms 6 year molars discount vibramycin 100mg otc, expose to bright light or mix with any other drug. Add 12 ml of water for injection to obtain a solution containing 4 mg/ml and shake vigorously until the powder is completely dispersed. Remove the required volume of the suspension and dilute to a concentration of 2 mg/ml using 5% glucose. Compatibility: Do not let any of these product come into contact with any fluid other than 5% glucose. If using a pre-existing cannula, this must be flushed with 5% glucose before and after the infusion. Pharmacokinetics, outcome of treatment, and toxic effects of amphotericin B and 5-fluorocytosine in neonates. Antifungal therapy in children with invasive fungal infection: a systematic review. Liposomal amphotericin B: a review of its use in empirical therapy in febrile neutropenia and in the treatment of invasive fungal infections. Candida infection in very low birth-weight infants: outcome and nephrotoxicity of treatment with liposomal amphotericin B (AmBisome). Ampicillin is a semi-synthetic broad-spectrum aminopenicillin that crosses the placenta. A little appears in human milk, but it can safely be given to a lactating mother since the baby is known to receive less than 1% of the weight-related maternal dose. Maculo-papular drug rashes are not a sign of serious drug sensitivity and are relatively rare in the neonatal period. The drug is actively excreted in the urine and, partly as a result of this, the plasma half-life falls from about 6 to 2 hours during the first 10 days of life. Ampicillin was, for many years, the most widely used antibiotic for treating infection with Listeria, -lactamase-negative Haemophilus, enterococci, Shigella and non-penicillinase-forming Proteus species. It is also effective against streptococci, pneumococci and many coliform organisms. Ampicillin has frequently been used prophylactically to reduce the risk of infection after abdominal surgery (including caesarean delivery). Care in spontaneous preterm labour Similar prophylaxis does not delay delivery, or improve outcome, when labour threatens to start prematurely before the membranes rupture, but high-dose penicillin during delivery can reduce the risk of early-onset neonatal group B streptococcal infection. One recent study has suggested that a combination of these two strategies would result in 80% of all the babies currently dying of any bacterial infection of intrapartum origin. It means giving antibiotics to between 40 and 60 women during labour to provide optimum treatment for one baby with bacterial sepsis of intrapartum origin. Many policies treat even more patients than this, and it seems possible that this could increase the risk of late-onset infection. In other situations, a dose of 50 mg/kg is more than adequate, given (when the patient is well enough) by mouth. Oral medication can sometimes be used to complete treatment even though absorption is limited. No sugar-free oral suspension is currently available (a sugar-free oral suspension of amoxicillin is available and is a suitable alternative). Changing patterns in neonatal Escherichia coli sepsis and ampicillin resistance in the era of intrapartum antibiotic prophylaxis. Antibiotic treatment in preterm and premature rupture of membranes and neonatal morbidity: a meta-analysis. Association of intrapartum antibiotic exposure and late-onset serious bacterial infections in infants. Risk factors and opportunities for prevention of early-onset neonatal sepsis: a multicenter case-control study. Not only does this usually require sedation or anaesthesia, but it is difficult to perform and results in destruction of the peripheral retina. Ranibizumab is a smaller monoclonal antibody fragment derived from the same parent antibody as bevacizumab and is considerably more expensive. Both drugs are injected into the vitreous humour under local anaesthesia and sedation. In adult studies, there is less systemic leakage of ranibizumab and the potential for the adverse effects on other developing organs is, theoretically at least, lower. There is some evidence to suggest that these doses may be excessive; the doses above are half the doses used in adult retinopathies and are those reported to have been used in most studies. Lower doses may be as effective and have less potential for systemic effects; in adults with retinopathies, a bevacizumab dose of 1. Bevacizumab (Avastin) for retinopathy of prematurity: wrong dose, wrong drug, or both Intravitreal bevacizumab (Avastin) in the treatment of proliferative diabetic retinopathy. Short-term outcome after intravitreal ranibizumab injections for the treatment of retinopathy of prematurity. Significant treatment failure with intravitreous bevacizumab for retinopathy of prematurity. Serum concentrations of bevacizumab (avastin) and vascular endothelial growth factor in infants with retinopathy of prematurity. In some urea cycle disorders, l-arginine also facilitates nitrogen excretion, along with sodium phenylbutyrate and sodium benzoate (q. Biochemistry Arginine is a naturally occurring amino acid needed for protein synthesis. Dietary supplementation becomes essential, however, in most patients with urea cycle disorders because the enzyme defect limits arginine production, while dietary protein restriction limits arginine intake. Further supplementation also aids nitrogen excretion in citrullinaemia and argininosuccinic aciduria because excess arginine is metabolised to citrulline and argininosuccinic acid, incorporating nitrogen derived from ammonia and aspartic acid. As citrulline and argininosuccinic acid can be excreted in the urine, treatment with arginine can lower the plasma ammonia level in both these conditions. Treatment with arginine needs to be combined with a low-protein diet and supervised by a consultant experienced in the management of metabolic disease. Treatment with oral sodium phenylbutyrate and/or sodium benzoate is also usually necessary. Treatment Note: Treatment with l-arginine should be initiated only after consultation with a specialist metabolic diseases centre. Citrullinaemia and argininosuccinic aciduria: Up to 175 mg/kg of arginine four times a day can be given by mouth to promote nitrogen excretion. Hyperchloraemic acidosis can occur in patients on high-dose arginine hydrochloride: pH and plasma chloride concentrations should be monitored and bicarbonate given if necessary. High arginine levels are thought to contribute to the neurological damage in arginase deficiency, and it is recommended that plasma arginine levels should be monitored during long-term use and kept between 50 and 200 mol/l. Add 185 ml of purified water to the contents of the bottle to obtain 200 ml of a 100 mg/ml liquid which remains stable for 2 months. Arginine supplementation prevents necrotizing enterocolitis in the premature infant. Arginine, an indispensable amino acid for patients with inborn errors of urea synthesis. Enteral L-arginine supplementation for prevention of necrotizing enterocolitis in very low birth weight neonates: a double-blind randomized pilot study of efficacy and safety. Extracts of the herb Artemisia annua (sweet wormwood) have been used to treat fever in China for many centuries. The key ingredient seems to be the sesquiterpene lactone called qinghaosu (or artemisinin), which was first isolated by Chinese chemists in 1971. Artemisinin and its derivatives, artemether and artesunate, have since been shown to clear malarial parasites from the blood more rapidly than other drugs.
Diseases
- Deafness oligodontia syndrome
- Thoraco abdominal enteric duplication
- Poikilodermia alopecia retrognathism cleft palate
- Paronychia
- Human ewingii ehrlichiosis
- Renal calculi
- Cerebelloparenchymal disorder 3
Buy vibramycin overnight
In colpocentesis (culdocentesis) treatment integrity best buy for vibramycin, an aspirating syringe needle is inserted through the vaginal wall for collection of fluid from the recto-uterine cul-desac (pouch of Douglas). This pouch is the lowest site in the intraperitoneal space, and free fluids, including blood and pus, will pool there, creating a good site for diagnostic aspiration of peritoneal fluid. Partial vaginectomy includes partial excision of the vaginal wall, usually the upper or lower half. The Vagina and Other Internal Genitalia the vagina extends from the introitus of the vulva to the cervix. Rather, vaginal walls will stretch considerably during coitus, childbirth, or the insertion of a speculum during a medical exam, but otherwise are flattened tubes. Pessaries are manufactured in a number of shapes and sizes, and a pessary is selected and fitted based on lifestyle and symptoms. This may lead to urinary symptoms including urinary incontinence or to fecal incontinence. Ring pessary Pessaries used to reduce prolapse and support pelvic floor muscles Introduction Coding Atlas 57150 57155 57156 57160 57170 57180 Irrigation of vagina and/or application of medicament for treatment of bacterial, parasitic, or fungoid disease Insertion of uterine tandem and/or vaginal ovoids for clinical brachytherapy Insertion of a vaginal radiation afterloading apparatus for clinical brachytherapy Fitting and insertion of pessary or other intravaginal support device Diaphragm or cervical cap fitting with instructions Introduction of any hemostatic agent or pack for spontaneous or traumatic nonobstetrical vaginal hemorrhage (separate procedure) To treat some malignancies of the female genitalia, pelvic irradiation may be achieved using an intracavitary delivery device in a treatment known as brachytherapy. An irradiated object may be secured in the vagina or uterus so that the object delivers a constant dose of irradiation (code 57155). Another method for brachytherapy is the use of an afterloading device (code 57156). The device is secured in the vagina and then attached to an applicator that delivers a radiation source into the device. Rectocele, Enterocele Weakness in the pelvic floor and vaginal wall may cause the rectum or small intestines to bulge against the vaginal wall. In rectocele, the rectum prolapses and pushes against the posterior wall of the vagina and pelvic floor. Enterocele is a herniation in which a segment of small bowel drops into the pouch of Douglas and presses against the posterior wall of the vagina and the pelvic floor. Enteroceles may be asymptomatic or cause symptoms of vaginal discomfort and low back pain. Female Genital System 57200-57415 57287 57288 57289 57291 57292 57295 57296 Removal or revision of sling for stress incontinence (eg, fascia or synthetic) Sling operation for stress incontinence (eg, fascia or synthetic) Pereyra procedure, including anterior colporrhaphy Construction of artificial vagina; without graft with graft Revision (including removal) of prosthetic vaginal graft; vaginal approach open abdominal approach Closure of rectovaginal fistula; vaginal or transanal approach abdominal approach abdominal approach, with concomitant colostomy transperineal approach, with perineal body reconstruction, with or without levator plication Closure of urethrovaginal fistula; with bulbocavernosus transplant Closure of vesicovaginal fistula; vaginal approach transvesical and vaginal approach Vaginoplasty for intersex state Repair Coding Atlas Colpopexy (vaginopexy, culpopexy, vaginofixation) corrects prolapse of the vagina. Vaginal prolapse is most commonly seen in women who have undergone a hysterectomy or as a result of menopause or childbirth. Cystocele, Urethrocele Weakness in the pelvic floor and vaginal wall may cause the bladder or urethra to bulge against the vaginal wall. Note: Tools, implants, and/or equipment depicted in the illustration may be outdated but the procedural approach is valid. Colposcopy Colposcopy involves the use of a light and low-powered microscope to examine the vulva, vagina, and/or cervix. When the vagina or cervix is being examined, a speculum is inserted into the vagina. Urethra Bladder Fallopian tube Colposcope Uterus Rectum Speculum Cervix Endoscopy/Laparoscopy Coding Atlas 57420 57421 57423 57425 57426 Colposcopy of the entire vagina, with cervix if present; with biopsy(s) of vagina/cervix Paravaginal defect repair (including repair of cystocele, if performed), laparoscopic approach Laparoscopy, surgical, colpopexy (suspension of vaginal apex) Revision (including removal) of prosthetic vaginal graft, laparoscopic approach Laparoscopy is a technique developed to reduce risk and recovery time during abdominal or pelvic surgery. To enhance visibility, the abdomen or pelvis may be filled with gas (pneumoperitoneum) during the procedure. The Internal Female Genitalia: Sagittal View the cervix separates the uterine body from the vagina. A midline cervical canal (os) allows the passage of semen into the uterus, as well as the passage of the products of menses and of conception from the uterus into the vagina. The distal canal (external os) opens into the vagina, and the proximal canal (internal os) opens into the endometrial cavity of the uterus. Excision of the cervical stump describes the surgical removal of all or a portion of the cervix that remains following a previous subtotal hysterectomy. Female Genital System 57513-58200 57513 57520 laser ablation Conization of cervix, with or without fulguration, with or without dilation and curettage, with or without repair; cold knife or laser loop electrode excision Trachelectomy (cervicectomy), amputation of cervix (separate procedure) Radical trachelectomy, with bilateral total pelvic lymphadenectomy and para-aortic lymph node sampling biopsy, with or without removal of tube(s), with or without removal of ovary(s) Excision of cervical stump, abdominal approach; with pelvic floor repair Excision of cervical stump, vaginal approach; with anterior and/or posterior repair with repair of enterocele Dilation and curettage of cervical stump Corpus Uteri Excision Coding Atlas 57522 57530 57531 57540 57545 57550 57555 57556 57558 Total abdominal hysterectomy describes the removal of the uterus and cervix through an abdominal incision. Supracervical or subtotal hysterectomy describes the removal of most of the uterus, with the sparing of the cervix (cervical stump), using an abdominal approach. Radical hysterectomy is more extensive and includes lymphadenectomy as well as excision of mesentery associated with the uterus in addition to other surrounding tissue. The Uterus, Fallopian Tubes, and Ovaries the uterus, fallopian tubes, and ovaries lie between layers mesometrium, mesosalpinx, and mesovarium, which are the mesentery layers that help secure the uterus, tubes, and ovaries to the walls and floor of the pelvis. The mesometrium, mesosalpinx, and mesovarian are essentially a continuous fold of peritoneum and together may be referred to as the broad ligament of the uterus. Uterine Leiomyomas Uterine myomas (leiomyomas) are benign neoplasms that can arise from the smooth muscle (myometrium) of the uterus. Myomas can develop on the surface of the uterine lining (submucosal), within the uterine muscle wall (intramural or interstitial), or on the outer surface of the uterus (subserosal). Procedures for surgical excision of leiomyomas are based on the approach (abdominal, vaginal, or laparoscopic), the site (intramural or submucosal/subserosal), and, when intramural, the number and total weight of tumors excised. The sacrouterine (rectouterine) ligaments are a paired set of ligaments that arise from the base of the uterus and attach to the anterior aspect of the sacrum. A concurrent laparoscopy allows the physician to monitor the ends of the tubes for appearance of the dye. In this scenario, it would be appropriate to report the chromotubation with a diagnostic laparoscopy. Female Genital System 58541-58573 58548 Laparoscopy, surgical, with radical hysterectomy, with bilateral total pelvic lymphadenectomy and para-aortic lymph node sampling (biopsy), with removal of tube(s) and ovary(s), if performed Laparoscopy, surgical, with vaginal hysterectomy, for uterus 250 g or less; with removal of tube(s) and/or ovary(s) Laparoscopy, surgical, with vaginal hysterectomy, for uterus greater than 250 g; with removal of tube(s) and/or ovary(s) Hysteroscopy, diagnostic (separate procedure) Hysteroscopy, surgical; with sampling (biopsy) of endometrium and/or polypectomy, with or without D & C with lysis of intrauterine adhesions (any method) with division or resection of intrauterine septum (any method) with removal of leiomyomata with removal of impacted foreign body with endometrial ablation (eg, endometrial resection, electrosurgical ablation, thermoablation) with bilateral fallopian tube cannulation to induce occlusion by placement of permanent implants Laparoscopy, surgical, with total hysterectomy, for uterus 250 g or less; with removal of tube(s) and/or ovary(s) Laparoscopy, surgical, with total hysterectomy, for uterus greater than 250 g; with removal of tube(s) and/or ovary(s) Laparoscopy/Hysteroscopy Coding Atlas Laparoscopic hysterectomy procedures vary greatly, and codes have been created to describe these different circumstances. In some cases, a vaginal approach is used in combination with the laparoscopic approach. In a hysterectomy that is exclusively laparoscopic, the uterus must be morcellated before it can be removed through laparoscopy portals. The weight of the uterus plays a role in code assignment, as does whether the hysterectomy includes the entire uterus or spares the cervix (supracervical). It is also necessary to look for documentation as to whether the ovaries and fallopian tubes are excised. For open procedures, there is no coding distinction between a hysterectomy that includes removal of tubes and ovaries and one that does not. However, codes for laparoscopic hysterectomy differentiate between procedures with removal of adnexa and those without removal of adnexa. Hysteroscopy A hysteroscopy allows the physician to view the interior surface of the uterus with a scope that enters through the vagina and cervical os. The scope contains a light source and may contain an eyepiece for direct visualization of the endometrial tissue or it may contain a camera that can broadcast the image on a video screen. In some cases, media is infused into the uterus to distend the endometrial cavity for panoramic viewing. In other cases, the scope may be in contact with the endometrium for maximum magnification of a targeted site. The Fallopian Tube Each bilateral fallopian tube is between 10 cm and 12 cm in length and together are the lumen through which the ovum travels from the ovary to the uterus. Fimbriae of the fallopian tube are cilia that draw the ovum into the fallopian tube. The infundibulum of the fallopian tube is the funnel-shaped lumen that terminates at the fimbriae. The ampulla continues to narrow the lumen until it is very narrow at the isthmus, at which point it enters the uterine fundus. Intramural portion Isthmus Ampulla Fimbria Appendix vesiculosa Oviduct/Ovary Incision Coding Atlas 58615 Occlusion of fallopian tube(s) by device (eg, band, clip, Falope ring) vaginal or suprapubic approach Laparoscopy Coding Atlas Ligation or occlusion of the fallopian tubes is performed in order to prevent spermatozoa from reaching the ovum. The fallopian lumen is crimped or severed and each end is sealed, cutting off communication between the ovary and the uterus. Tubal ligation effectively sterilizes the patient without affecting her hormone secretions or requiring other medication or treatment. Codes 5860058615 are used to report tubal ligation that is achieved with an open incision into the pelvis with direct visualization of the fallopian tube. Laparoscopic ligation, reported with codes from the range 58670-58671, is the most common approach for tubal ligation or occlusion in the United States. Surgical treatment of a tubal pregnancy that requires excision of the fallopian tube is reported with code 59120. Typically, the goal in these "debulking" procedures is to remove tumors that are larger than 1 centimeter. It is done by restoring the function and patency of the fimbriae at the distal fallopian tube. Ovarian cysts are usually benign but may cause abdominal pain, interfere with bowel movements or urination, or cause symptoms related to menses.
Purchase vibramycin once a day
Suprarenal gland Suspensory (diaphragmatic) ligament Gonads Mesonephric (wolffian) duct Gubernaculum Urinary bladder Suprarenal gland Kidney Suspensory (diaphragmatic) ligament (atrophic) Testes Epididymis Gubernaculum Deep inguinal ring 8 weeks (22 symptoms juvenile rheumatoid arthritis discount vibramycin amex. Male Genital System 54700-55060 Repair Coding Atlas Epididymis Incision 54700 Incision and drainage of epididymis, testis and/or scrotal space (eg, abscess or hematoma) Excision Coding Atlas Epididymovasostomy describes the reconstruction of the spermatic duct system that has an obstruction. It is performed to restore the patency of the tubule and, in turn, restore fertility; it is most commonly done as a reversal of a vasectomy procedure. In the epididymis, immature spermatozoa are received from the testis, matured, and released into the vas deferens in preparation of ejaculation. However, if the epididymis were to be unbundled into a single tube, it would be approximately 20 feet in length. Hydrocele and Spermatocele A hydrocele is an accumulation of peritoneal fluid between the parietal and visceral layers of the tunica vaginalis within the scrotum or along the spermatic cord. A spermatocele is a benign cyst arising from the head of the epididymis and containing an accumulation of sperm. Male Genital System 55100-55450 Scrotum Incision Coding Atlas Vas Deferens Incision Coding Atlas the scrotum is a sac of skin and muscle located posterior to the penis and anterior to the anus. Involuntary contractions of the muscle fibers in the dartos fascia of the scrotum cause the scrotum to thicken and ascend closer to the perineum. Sperm production is optimal when the testes are cooler than the core body temperature. Procedures on the scrotum involve the layers of the scrotal sac or the space between the inner scrotal wall and its contents (testes, epididymis, spermatic cord). As a component of the spermatic cord, the vas deferens passes through the inguinal canal, enters the abdomen, and redirects back into the pelvic cavity where it forms the ejaculatory duct with the seminal vesicle. Usually, it is associated with injury or a postsurgical defect but may also be performed due to a congenital malformation. Vasectomy In a vasectomy, the vas deferens is severed or occluded as a form of permanent birth control, thus preventing spermatozoa from reaching the seminal vesicle during coitus. Male Genital System 55500-55725 Excision Coding Atlas Spermatic Cord Excision Coding Atlas A varicocele forms in the spermatic cord when valves inside the pampiniform venous plexus fail, causing backflow of blood, congestion, and expansion of the vein that is a component of the spermatic cord. The condition may be treated with varicocelectomy or ligation, reported using codes 55530-55540. If the varicocele is treated by embolization using transcatheter methodology, the procedure is reported using code 37241. The cyst may cause urinary symptoms and require excision if it enlarges due to fluid accumulation. The standard prostate needle biopsy can be performed under local anesthesia and may include between 6 and 12 core samples. Stereotactic guided saturation sampling is performed under general anesthesia, and between 35 and 60 core samples are collected using a transperineal approach and a template grid that organizes the collection sites systematically. Approaches to Seminal Vesicles the seminal vesicles are paired organs situated adjacent to the posterior bladder and posterior prostate. Because the seminal vesicles lie deep in the pelvis, several approaches may be considered for surgery. The Prostate, Bladder, Seminal Vesicles, and Vas (Ductus) Deferens the vas deferens and seminal vesicles sit bilaterally atop the prostate at the posterior bladder. From this position, fluids from the vas deferens and seminal vesicles flow into the ejaculatory ducts in the urethra. The prostate contributes fluid through the prostatic duct and, with the other secretions, forms semen. The proximity of the vas deferens and seminal vesicles means that surgery on the prostate may impact future sexual function and fertility. Radical Prostatectomy Radical prostatectomy describes removal of the entire prostate, seminal vesicles, and periprostatic tissues. Direct visualization of the prostate may be desired during excision of some cancers, eg, adenocarcinoma. Codes 55801-55845 are used to report open procedures that provide a more visual approach to treatment. T Female Genital System Spermatozoa travel through the vagina and cervical os into the uterus and then into the fallopian tube. Fertilization occurs in the fallopian tube, and the fertilized egg (zygote) migrates into the uterus. By this phase, the zygote has begun cell division, and the cluster of cells (blastocyst) implants itself in the nutrient-rich endometrial lining. The growing fetus is suspended in the amniotic sac, which is filled with amniotic fluid. Labor and delivery usually begin with contractions that function to open the cervix and push the fetus into the birth canal. After the neonate is born, contractions continue until the placenta is delivered (afterbirth). Within a month or two, the uterus returns to its normal size, ie, the size of a pear. Surgical encounters associated with the female genital system are often related to pregnancy or fertility, irregular menses, incontinence, hernias of the genital system, and neoplasms. Many procedures on the internal female genitalia may be performed using a vaginal or laparoscopic approach; an open surgical approach may be used when direct visualization is desired or in the case of a cesarean section. It is bordered by the mons pubis anteriorly and the rectum posteriorly and by the crease of the thigh (genitocrural fold) bilaterally. The internal genitalia include the vagina, uterus, cervix, fallopian tubes, and ovaries. The bilateral ovaries secrete two groups of sex hormones, which are estrogen and progesterone. These secretions, along with secretions from the hypothalamus and pituitary glands, regulate the menstrual cycle (consists of ovarian and uterine cycles), which is crucial to reproduction. During the follicular phase, a Graafian follicle within the ovary develops a mature egg (ovum). At the same time, the lining of the endometrium of the uterus proliferates in preparation for embryo implantation (uterine cycle). The follicle ruptures at about day 14 in the follicular phase, and an ovum is released (ovulation). During the first half of the luteal phase, the ovum is swept by fimbriae into the fallopian tube and advances into the uterus. A fertilized egg-one that has united with a sperm from the male-may embed successfully in the endometrial lining. If this does not occur, the endometrial lining begins to slough off (menstruation). The glands supply lubrication to the vaginal opening (introitus) during sexual arousal. A simple vulvectomy is the removal of skin and superficial fat and subcutaneous tissue. In a partial vulvectomy, less than 80% of the vulvar area is removed, while in a complete vulvectomy, more than 80% is removed. A radical vulvectomy involves removal of skin and deep subcutaneous tissue as well. Condyloma, papilloma, molluscum contagiosum, and herpes are usually sexually transmitted. Destruction of a lesion is therapeutic but may not be curative; the patient will no longer have the wart but may still carry the underlying virus. The Vulva, Perineum, and Introitus In its entirety, external female genitalia may be referred to as the vulva or the pudendum. In plastic repair of the introitus (introitoplasty), the vaginal opening is altered to correct a defect. In perineoplasty, the perineum between the vagina and anus, including the perineal body, is repaired or strengthened. A colposcope may also be used to examine the vagina or cervix, and codes specific to those anatomical sites should be chosen if they are the target of the exam. Dissection Exposing the Perineal Body the perineal body describes a fibromuscular convergence of pelvic floor muscles, fascia, and fibrous tissue in the medial plane of the perineum between the vagina and anus. Essential to the integrity of the pelvic floor, the perineal body may be damaged during vaginal delivery, predisposing women to prolapse involving the uterus, bladder, and/or rectum. Female Genital System 57000-57135 Excision Coding Atlas Vagina Incision Coding Atlas Colpotomy is an incision into the vaginal wall.
Cheap vibramycin online american express
Given the potential effects on the infant at a crucial stage treatment bulging disc buy 100 mg vibramycin free shipping, use is best avoided during pregnancy and lactation. Most authorities consider propylthiouracil preferable to carbimazole, especially during lactation, because of the risk of neonatal hypothyroidism. Rodent teratogenicity has not been reported except when administered at levels >7. Although the manufacturer advises avoiding use during pregnancy, two reviews consider it to be safe. Not only are small amounts absorbed systemically, but transfer of vitamin D into milk is also low and calcipotriol levels in breast milk would be expected to be negligible. Related drugs in this class cross the placenta and fetal renal effects (anuria and oligohydramnios) have been reported. There are no reports of use during lactation and it is not known if it enters breast milk. It is used for treatment of postpartum haemorrhage secondary to uterine atony after failure to respond to ergometrine and oxytocin. It is not known if carboprost enters breast milk, but it is reassuring that prostaglandins have short half-lives and that even large parenteral doses give very low plasma concentrations. Risks are greatest during the second and third trimesters through effects on the fetal kidney, causing renal failure and oligohydramnios, but teratogenesis during the first trimester is also reported. Captopril is embryocidal and causes stillbirths in a variety of animals (sheep, rabbits, rats). Captopril is excreted into breast milk at very low concentrations and is compatible with breastfeeding. Although there is no data for cefaclor, most cephalosporins pass into breast milk, and cefaclor is considered compatible with breastfeeding. Like most cephalosporins, cefadroxil is 566 Maternal medication and the baby Gardiner et al. Only small amounts of cefalexin are excreted into breast milk, and it is generally considered compatible with breastfeeding. Cefradine rapidly crosses the placenta and is found in the amniotic fluid within hours of maternal administration. Cefradine is excreted into breast milk in small amounts that are compatible with breastfeeding. Cefixime Cetirizine Cefixime can be detected in amniotic fluid after maternal treatment, so it likely crosses the placenta. Most cephalosporins are excreted into breast milk, and cefixime appears to be no exception. Like all cephalosporins, cefixime is generally considered compatible with breastfeeding. In general, first-generation antihistamines are preferred to newer ones due to the greater wealth of evidence of safety. Although not widely used in neonatal units, cefpodoxime may be used in babies as young as 15 days. In general, use should be avoided during the first trimester when risk is greatest. There are no reports of chlorambucil use during lactation; however, because of the potential adverse effects of alkylating agents on the infant, breastfeeding should be avoided. Celecoxib passes into breast milk in subclinical amounts that have not been reported to have any effects in the breastfeeding infant. First trimester exposure to some has been linked to an increased risk of anomalies. The experience with chlordiazepoxide has been reassuring with no increase in malformations or adverse effects on neurobehavioural development. Symptoms are variable and Maternal medication and the baby include sedation, hypotonia, poor suck, apnoea and cyanosis. Chlordiazepoxide enters breast milk in low concentrations, and only high maternal doses might be expected to affect the nursing infant. It is not known whether chlorhexidine enters breast milk; however, given that chlorhexidine is widely used as skin preparation in neonates, the potential for toxicity is low. Use as a disinfectant in traumatised nipples does not seem to cause problems in the infant. There is a suggestion of higher risk of stillbirth, preterm delivery and growth restriction in mothers who are treated with ciclosporin used as an immunosuppressant, but it is not clear whether this is related to the maternal disease or the treatment. Ciclosporin passes into breast milk in low amounts; however, the clearance of ciclosporin by the neonate can be quite variable. Some advise against breastfeeding; however, if breastfeeding is continued, the infant should be monitored closely (including serum ciclosporin levels) for signs of toxicity. Rodent teratogenicity studies are reassuring, but electrolyte imbalances are reported in both mother and newborn. While chlortalidone is excreted into breast milk, it is generally considered compatible with breastfeeding. Studies of the use of cimetidine during pregnancy have shown no increased risk of birth defects. Cimetidine is actively transported into breast milk; but the amounts are unlikely to cause problems in the breastfed infant. Ciprofloxacin Cholestyramine Cholestyramine has been used for the treatment of cholestasis of pregnancy. In the only randomised trial comparing it to ursodeoxycholic acid, symptom relief for the mother and pregnancy outcomes were worse for the cholestyramine group. Because cholestyramine is not systemically absorbed, it should not directly affect the fetus; however, it could interfere with the uptake of fat-soluble vitamins. Treatment of fetal mice, dogs and rabbits with other quinolones is associated with an acute arthropathy of the weight-bearing joints. Clostridium difficile pseudomembranous colitis has been reported in one breastfed infant, and discoloured teeth have been reported in infants treated with ciprofloxacin as neonates. Cisatracurium Ciclosporin Placenta transfer of ciclosporin is reported to be poor. Animal teratogenicity Cisatracurium is one of the isomers of atracurium, which has been used during fetal surgery without problems. Although small amounts of atracurium cross the placenta, use during caesarean section is not associated with neonatal sequelae. There are no published reports of use during lactation, and it is not known whether cisatracurium enters breast milk. Considering its use, cisatracurium is unlikely to affect the breastfeeding newborn. Short-term use during breastfeeding is probably safe; long-term treatment is best avoided due to the risks of tolerance in the breastfed infant. Cisplatin Although patients should be advised to avoid pregnancy during cisplatin treatment, good outcomes are possible. Cisplatin is considered to be teratogenic and embryotoxic; however, there is increasing evidence for its relative safety during gestation. Clomiphene A wide range of fetal abnormalities are reported after clomiphene-induced ovulation, but no discernable pattern has emerged. Early studies of paroxetine (but not citalopram) suggested an association with cardiovascular malformations. Overall use during pregnancy does not seem to cause problems other than during the third trimester when neonatal withdrawal syndrome has been reported. There have been two reports of excessive sleepiness in breastfed neonates, but the majority of studies report no effects. It is not known whether exposure through breast milk ameliorates the symptoms of neonatal abstinence. There are no reports of fetal abnormalities, and rodent teratogenicity studies are reassuring. Withdrawal symptoms (jitteriness, tremor and seizures) have been reported in exposed neonates. Only small trace amounts of clomipramine are found in breast milk, and these are unlikely to affect the breastfed infant. Clonidine is concentrated in breast milk (M/P ratio ~2), although neonatal effects are not usually seen.

Buy generic vibramycin 100 mg on-line
The pectinate line medicine 8162 order vibramycin paypal, also referred to as the dentate line or mucocutaneous line, is at the base of the anal columns. Although with the same pigmented color as that of the surrounding perianal skin, the verge differs in that it contains no hair, sweat glands, or sebaceous glands. Digestive System 46200-46615 Introduction Coding Atlas Excision Coding Atlas Hemorrhoidal cushions are normal anatomical structures of the anorectum, with an extensive vascular supply and high sensitivity. Hemorrhoidal cushions commonly prolapse, thrombose, itch, or cause other symptoms and are then referred to as "hemorrhoids. Hemorrhoids may be excised or treated by banding to induce ischemia and death of the hemorrhoidal tissue. Chemodenervation of the internal anal sphincter is performed by injecting botulinum toxin into the sphincter muscle to loosen the anal opening and promote healing of a fissure that has developed there. Using anoscopy and under direct visualization, the physician is able to grasp the hemorrhoid with a clamp and place a band around the base of the hemorrhoid. Hemorrhoids Hemorrhoids are swollen, symptomatic blood vessels in the rectum and anus. Internal hemorrhoids originate above the dentate line, and external hemorrhoids originate below the dentate line. An engorged hemorrhoid may clot, or thrombose, a condition that causes significant pain. A low imperforate anus will have a colon close to the skin, with a very stenotic anus or the colon ending in a blind pouch. In high imperforate anus, the colon is higher in the pelvis, with a fistula connecting the rectum to another organ. In a cloacal anomaly, the rectum, vagina, and urinary tract all form a single channel. Surfaces and Bed of the Liver the liver is in the right upper abdominal quadrant, with most of it tucked up under the rib cage. The liver has multiple segments, and each segment has its own independent blood supply and biliary branches. This may be performed as a follow-up to an abnormal test result, to evaluate a liver mass, or to evaluate the severity of a known disease, eg, alcoholic liver disease, hepatitis, or hemochromatosis. The biopsy may be performed using a cutting needle, a suction needle, or a spring-loaded needle. The most common reason for transplants in adults is cirrhosis; the most common reason in children is biliary atresia. It contains four functional surgical components: the right and left lobes; the medial lobes; the small caudate segment, which extends from the posterior side of the right lobe; and the quadrate lobe, which is inferior to the caudate segment and extends toward the gallbladder. Trisegmentectomy involves excision of the right (or, rarely, left) lobe plus the caudate and quadrate segments (medial segment). The system divides the liver into eight independent functional sections, rather than basing classification on the morphology of the organ. Abscess of the liver is usually the result of a biliary tract obstruction and infection. In a percutaneous approach, ultrasound or computed tomography guidance aids the physician in correct placement of the ablation tool through a small percutaneous incision; this is done without direct visualization. This is done by inserting a needle electrode into the site and applying high-frequency electrical current into the needle to destroy the abnormal cells. The physician manipulates the surgical tools while viewing the surgical site on a video display screen or through an eyepiece. Cryosurgery involves use of a freezing probe inserted into the malignant tissue to destroy it. Laparoscopy For many digestive procedures, laparoscopy has become the treatment of choice. It is considered less invasive, less expensive, and has a shorter recovery time than that for laparotomy. The image from the camera is projected onto a video display, and the surgeon performs the surgery while watching the video image. After infiltration of local anesthetic, Verres pneumoperitoneum needle is introduced into abdomen through small skin nick just below or above navel. Codes in the range 47552-47556 are used to report procedures in which the approach is percutaneous, ie, through a T-tube. The top of the hollow T-tube is inserted into the common bile duct, and the stem of the T-tube extends from an incision in the duct to emerge through the skin. The obstruction may be treated with a stent to maintain patency of the flow of bile or by ostomy or catheter to drain the bile to the skin surface, where it can be collected in a pouch. Several small abdominal incisions act as portals for a tiny video camera (laparoscope), light source, and surgical tools. The Gallbladder and Extrahepatic Bile Ducts the gallbladder stores and concentrates bile, which is manufactured in the liver. When the walls of the duodenum sense that the nutrients within are high in protein or fat, the duodenum signals for the release of bile from the gallbladder. Cholelithiasis occurs when the bile salts crystalize with cholesterol to form stones (calculi). In some cases, an open procedure will be required to treat stones, atresia, or a bile duct tumor. The Pancreas the pancreas is an endocrine gland that contains both endocrine and exocrine components. The head of the pancreas communicates with the duodenum through the pancreatic duct (duct of Wirsung); digestive enzymes flow through this duct to aid in duodenal digestion. The pancreas also contains islets of Langerhans, which are cell clusters that produce insulin. Some pancreas transplants are performed in patients who have already undergone kidney transplant, while a small number of patients undergo pancreatic transplant without kidney transplant. The codes used to report biopsy or excision of these tumors are based on anatomical region rather than the specific organ. In laparotomy, a midline incision is made in the abdomen so that the organs can be seen by direct visualization. The Retroperitoneum the retroperitoneum is the space within the abdominal cavity that lies behind the parietal peritoneum and is anterior to the fascia and muscle of the flank and lower back. The peritoneum is the membrane that forms the lining of the abdominal cavity, and the omentum is a peritoneal fold that connects organs to the abdominal wall. Laparoscopy Coding Atlas 49320 Laparoscopy, abdomen, peritoneum, and omentum, diagnostic, with or without collection of specimen(s) by brushing or washing (separate procedure) Laparoscopy, surgical; with biopsy (single or multiple) with aspiration of cavity or cyst (eg, ovarian cyst) (single or multiple) with drainage of lymphocele to peritoneal cavity with insertion of tunneled intraperitoneal catheter Laparoscopy is a technique developed to reduce risk and recovery time during abdominal surgery. The disruption may be a blockage, eg, esophageal malignancy, or a more generalized problem, eg, malnutrition in a severely weakened patient. The disruption can be bypassed with the creation of a communication from the lumen to the exterior of the body. A gastrostomy, duodenostomy, or jejunostomy tube may be inserted percutaneously so that nutrients can be injected, bypassing the mouth, esophagus, and/or stomach proximal to the site. This feeding tube is often referred to as a G-tube (gastrostomy tube) or J-tube (jejunostomy tube). The tube may also be placed in the duodenum for enteral feeding or in the cecum (C-tube) for bowel management in patients with fecal incontinence. The Inguinal Canal the inguinal canal is a bilateral passage in the lower anterior abdomen through which the ilioinguinal nerve and the spermatic cord passes in the male and the ilioinguinal nerve and round ligament passes in the female. Because of its composition and location, the inguinal canal can be a site through which abdominal contents can bulge in what is called an inguinal hernia. Male inguinal canals are larger than those of the female, and the frequency of inguinal hernias is higher in males. An inguinal hernia occurs in the abdomen near the groin area; an umbilical hernia occurs close to the belly button; a ventral hernia occurs at the site of a previous incision; and a femoral hernia occurs in the upper thigh near the groin. Digestive System 49585-49906 Suture 49900 Suture, secondary, of abdominal wall for evisceration or dehiscence 49585 49587 49590 49600 49605 49606 49610 49611 Repair umbilical hernia, age 5 years or older; reducible incarcerated or strangulated Repair spigelian hernia Repair of small omphalocele, with primary closure Repair of large omphalocele or gastroschisis; with or without prosthesis with removal of prosthesis, final reduction and closure, in operating room Repair of omphalocele (Gross type operation); first stage second stage Other Procedures Coding Atlas Laparoscopy 49650 49651 49652 Laparoscopy, surgical; repair initial inguinal hernia repair recurrent inguinal hernia Laparoscopy, surgical, repair, ventral, umbilical, spigelian or epigastric hernia (includes mesh insertion, when performed); reducible incarcerated or strangulated Laparoscopy, surgical, repair, incisional hernia (includes mesh insertion, when performed); reducible incarcerated or strangulated Laparoscopy, surgical, repair, recurrent incisional hernia (includes mesh insertion, when performed); reducible incarcerated or strangulated An omental pedicle flap can be key to the reconstruction of some anatomical structures. To create the flap, the physician dissects a portion of omentum and rotates the omentum to its new site. In some cases, a free flap is used, the severed omentum is secured, and its vessels anastomosed at the new site.