Generic valtrex 500mg on-line
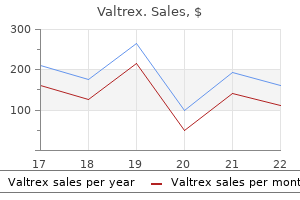
Pneumonia Pneumonia is usually due to infection affecting distal airways and alveoli antiviral vitamin c order valtrex with american express, with the formation of an inflammatory exudate. It occurs most commonly in old age, in infancy and in patients with debilitating diseases, such as cancer, cardiac failure, chronic renal failure or cerebrovascular accidents. Bronchopneumonia may also occur in patients with acute bronchitis, chronic obstructive airways disease or cystic fibrosis. Failure to clear respiratory secretions, such as is common in the postoperative period, also predisposes to the development of bronchopneumonia. Acute bronchitis may be caused by direct chemical injury from air pollutants, such as smoke, sulphur dioxide and chlorine. Chronic bronchitis is a clinical term defined as cough and sputum for 3 months in 2 consecutive years; it is discussed below under diffuse obstructive airways disease (p. Episodes of acute bronchitis are common in chronic obstructive airways disease, and cause a sudden deterioration in pulmonary function with cough and the production of purulent sputum. Most cases resolve within a few days, although a minority may develop secondary pneumonia or complications such as obliterative bronchiolitis (see p. Note the patchy areas of consolidation and pus-filled bronchi (arrowed) in this lung, which also shows upper lobe emphysema. Patients often become septicaemic and toxic, with fever and reduced consciousness. Histology shows typical acute inflammation with exudation in the bronchi and adjacent alveolar spaces. With antibiotics and physiotherapy, the inflammatory process may undergo resolution but death or healing by organisation may occur. Acute pleuritic chest pain on deep inspiration reflects inflammation of the pleura (pleurisy). The pathology of lobar pneumonia is a classic example of acute inflammation, involving four stages: 1. This first stage lasts for about 24 hours and represents the outpouring of a protein-rich exudate into alveolar spaces, with venous congestion. In this second stage, which lasts for a few days, there is massive accumulation in the alveolar spaces of polymorphs, together with some lymphocytes and macrophages. Histology shows interstitial inflammation consisting of lymphocytes, macrophages and plasma cells. Secondary bacterial infection is, however, common and may be severe, for example staphylococcal pneumonia complicating flu. Mycoplasma pneumonia tends to cause a more low-grade pneumonia, with interstitial inflammation and less exudation. It is caused by a bacillus, Legionella pneumophila, transmitted in water droplets from contaminated air humidifiers and water cisterns. Patients may be previously well, although a proportion have an underlying chronic illness, such as heart failure or carcinoma. Symptoms include cough, dyspnoea and chest pain, together with more systemic features, such as myalgia, headache, confusion, nausea, vomiting and diarrhoea. An entire lobe, paler than the other, has become consolidated due to accumulation of acute inflammatory exudate within the alveoli. Most lung infections in these patients are with organisms similar to those seen in the general population. Patients with severe immunosuppression are, however, prone to infection with unusual organisms that are usually non-pathogenic in other individuals. In any immunosuppressed patient, the onset of fever, shortness of breath and cough, together with pulmonary infiltrates, is an ominous event. These may be subclassified into those occurring in nonimmunosuppressed hosts and those occurring in immunosuppressed hosts. Chronic eosinophilic pneumonia is less frequently associated with a peripheral eosinophilia. The lung shows extensive infiltration with eosinophils and the presence of organising exudates which may go on to give rise to fibrosis. The aetiology is often unclear but can be the result of allergic-type reaction to drugs, environmental agents or parasitic infections. Pulmonary tuberculosis Viruses Viral infection may produce diffuse alveolar damage and areas of lung necrosis. Aspiration pneumonia Aspiration pneumonia occurs when fluid or food is aspirated into the lung, resulting in secondary inflammation and consolidation. Clinical situations where patients are at risk include sedation, operations, coma, stupor, laryngeal and oesophageal carcinoma, and severe debility. Often, such areas of aspiration pneumonia contain anaerobic organisms, and a lung abscess containing foul material may ensue. Lipid pneumonia Lipid pneumonia may be endogenous, associated with airway obstruction causing distal collections of foamy macrophages and giant cells. Alternatively, lipid pneumonia may be exogenous, due to aspiration of material containing a high concentration of lipid. Disease, however, occurs in only about 10% of cases of infection, when the balance between host resistance and the pathogenicity of the bacteria tips in favour of the latter. Before the advent of antituberculous treatment, therapy was aimed at improving host resistance using special diets and bed rest together with a change in socio-economic factors such as improved living conditions. Now, therapy is aimed at killing the organism using combination antibacterial chemotherapy. Public health measures including improved housing, nutrition and vaccination are also important in controlling the disease. Sensitivity can be assessed by the intradermal injection of tuberculin protein (Mantoux or Heaf tests). Primary tuberculosis the lungs are usually the initial site of contact between tubercle bacilli and humans. The pulmonary lesion is usually about 10 mm in diameter, and consists of an area of granulomatous inflammation with a central zone of caseous necrosis surrounded by palisaded epithelioid histiocytes, occasional Langhans giant cells and lymphocytes. Similar granulomas are seen in lymph nodes that drain the affected portion of the lung. In a few cases the infection may progress with systemic spread and in some cases death. In most cases, however, the primary lesion will organise and heal as the immune reaction to the organism develops, leaving a fibrocalcific nodule in the lung, and there will be no clinical sequelae. However, tubercle bacilli may still be present within such scarred foci and may persist as viable organisms for years. Histologically, granulomas are seen, most having central zones of caseous necrosis. Progression of the disease depends on the balance between host sensitivity and organism virulence. Most lesions are converted to fibrocalcific scars, a frequent finding in the lungs of elderly people at autopsy. The disease becomes widely disseminated, resulting in numerous small granulomas in many organs. Lesions are commonly found in the lungs, meninges, kidneys, bone marrow and liver, but no organ is exempt. The granulomas often contain numerous mycobacteria, and the Mantoux test is frequently negative. This is an acute medical emergency, necessitating prompt treatment with antituberculous chemotherapy if a fatal outcome is to be averted. Lung at autopsy showing cavitation and scarring at the apex of the right upper lobe. Symptoms are usually a chronic cough with expectoration of large quantities of foul-smelling sputum, sometimes flecked with blood. Recurrent respiratory tract infections result from the inability of the patient to clear pooled secretions.
Diseases
- Macias Flores Garcia Cruz Rivera syndrome
- Trichoodontoonychial dysplasia
- Arachindonic acid, absence of
- Marphanoid syndrome type De Silva
- Quadriplegia
- DiGeorge syndrome
- Late onset dominant cone dystrophy
- Viljoen Kallis Voges syndrome
- Thalamic degenerescence infantile
- Chromosome 5, trisomy 5p
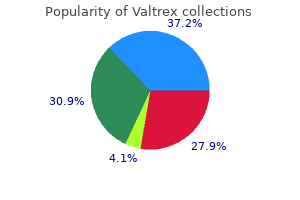
Order valtrex 1000 mg on-line
They are stellate fibrous structures with foci of ductal epithelial proliferation hiv infection transmission purchase valtrex us. There are conflicting data regarding the relationship between radial scar and development of malignancy, though where development of malignancy is described this is usually in the lowgrade spectrum of lesions. Lesions in men: gynaecomastia the breast tissue in men contains only ductular structures with no evidence of acini; it is similar in appearance to the prepubertal female breast. The breast may resemble that of a young adolescent female in appearance and consistency, or there may be a firm, mobile disc beneath the nipple. Male breast in which the ducts are lined by an increased number of cells, and are surrounded by loose connective tissue. In both of these groups it is probably due to some hormonal effects relating to oestrogens, pos sibly a result of endocrine disturbances such as hyperthy roidism, pituitary disorders and tumours of the adrenals and testis. In the older age group, diethylstilbestrol therapy of prostatic carcinoma can cause gynaecomastia. Fibroadenoma Commonesttypeofbenigntumour,mainlyinyoung frequently become fibrotic postmenopausally and may develop coarse calcification, which is detected on screening mammograms. The peak incidence is in the third decade, and whilst usually solitary they can be multiple. Fibroadenomas arise from the breast lobule, and involve proliferation of both the connective tissue stroma and the glands. Fibroadenomas may undergo hormonally induced changes such as lactational change during pregnancy. Fibroadenoma does not progress to malignancy, although very occasionally a tumour, such as lobular carcinoma, will involve a fibroadenoma. About 80% of patients present with a discharge, which is often bloodstained, and a mass can often be felt. They appear either as an elongated structure extending along a duct, or as a spheroid which causes distension of the duct, making it cystlike. The tumours have soft, pink or white outgrowths, which may be altered by haemorrhage. Solitary duct papillomas are not premalignant; there is no increased risk of carcinoma. There is a rare condition in which multiple ductal papil lomas occur, but these arise in the smaller ducts, away from the nipple, and so present as a mass rather than as nipple discharge. These tend to occur in a younger age group than do solitary papillomas and there is an increased risk of car cinoma developing. Tubular adenomas are wellcircumscribed tumours between 10 and 40 mm in diameter, occurring mainly in women in their early twenties. They are composed of closely packed, uniform tubular structures with little connective tissue in between; hence the only tumorous component is the glands. Lactating adenomas are tubular adenomas that undergo secretory changes during pregnancy. Nipple adenomas occur as a nodule under the nipple, usually less than 15 mm in diameter, in women of any age. They are well circumscribed, and contain small and larger ducts filled with masses of cells and surrounded by a dense stroma. Connective tissue tumours Lipomas and haemangiomas can occur in the breast, but are often hamartomas. Leiomyomas may occur deep in the breast or in the nipple, arising from the smooth muscle that is abundant there. A duct containing finger-like projections covered by a layer of epithelial and underlying myoepithelial cells, with a fibrous core. In North America, northwest Europe and Australia, breast cancer is the commonest type of malignancy in women. It is estimated, in the highrisk areas, that any individual woman has a 1 in 8 chance of developing the disease in her lifetime. An understanding of these can help in the develop ment of programmes directed towards the prevention of breast cancer. Schemes aimed at the early detection of breast cancer have been introduced in several countries. Femalesexandage Only 1% of breast cancers occur in men, so being female is an important risk factor. Ageatmenarcheandmenopause There is a significantly higher risk of developing breast cancer among women with an early age at menarche, whilst women whose natural menopause occurs before 45 years have only half the breast cancer risk of those whose meno pause occurs after 55 years. Ageatfirstfull-termpregnancy Nulliparous women have an increased risk of developing breast cancer. However, among parous women protection is related to early age for the first fullterm pregnancy. If the first birth is delayed to the mid or late thirties, the woman is at a greater risk of developing breast cancer than is a nul liparous woman. However, women aged 60 or over whose weight is increased have a higher cancer risk. Diet, obviously, can be a determinant for weight and some studies suggest that a highfat diet may be a risk factor, but the evidence is not as clear as it is for weight. It is of interest that the difference in incidence between high and lowincidence countries is mostly accounted for by a surplus of oestrogenpositive breast cancer. Benignbreastdisease As discussed previously, benign proliferative disease increases risk of breast cancer, particularly in the presence of atypical change. Twin studies suggest the level of breast density is an inherited characteristic, though it is modifiable by age, pregnancy and exogenous hormones. This risk is further increased if the relative was <50 years at the time of developing breast cancer, or if multiple first degree relatives are affected. Mutation in these genes is associated with a lifetime risk of breast cancer of 65% and 45%, respectively. Both also are associated with an increased risk of ovarian, and to a lesser extent, other cancers. Whereas these gene mutations are high penetrance and very significantly increase the risk of breast cancer, they account for only about 25% of familial risk. Biological studies are now underway to understand the function of such variants that should shed further light on breast cancer aetiology. Oestrogen activity appears to be important, with overex posure to oestrogens and underexposure to progesterone being significant. Early menarche and late menopause will result in a higher number of menstrual cycles, with repeated surges of oestrogen having a stimulatory effect on breast epithelium. The beneficial effect of early fullterm pregnancy could be due to the high concentrations of progesterone and/or prolactin protecting the breast cells against oestro gens in the long term. The risks associated with obesity may be partly due to the ability of fat cells to synthesise oestro gens, or to altered levels of sex hormonebinding protein. Geographicvariation There is a marked variation in breast cancer rates between different countries. The highest rates are in North America, northwest Europe, Australia and New Zealand, with the lowest in SouthEast Asia and Africa. Several factors prob ably contribute to this difference: age at menarche, age at first fullterm pregnancy, age at menopause and postmeno pausal weight. Combined oestrogen and progesterone hormone replacement therapy increases the relative risk of developing breast cancer for current users by twofold, and is greater the longer the duration of treatment. Oestrogen receptors can be detected in varying amounts in about 75% of breast cancers. The progesterone receptor, which can normally be formed only when the oestrogen receptor is present and active, is present in about 50% of tumours, and women whose tumours contain both types of receptor are more likely to respond to some form of hormone manipulation therapy. This suggests that hor mones are important in the growth and maintenance of these carcinomas. It can present as a palpable mass, especially if exten sive and associated with fibrosis. The disease can be found inci dentally in surgical biopsies or be detected by mammogra phy screening due to the presence of calcification. Pure ductal carcinoma in situ accounts for about 5% of breast carcinomas that present clinically, though up to 20% of cases in the screening setting. The size of the area involved in the breast can range from 10 to 100 mm in length.
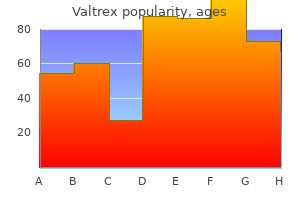
Buy generic valtrex from india
In this location hiv infection white blood cells buy 500 mg valtrex amex, the bacterium is protected from the acidic gastric juice by a thick layer of mucus in addition to its capability to neutralise hydrogen ions by urease and ammonia production. The organism can be seen on the surface on haematoxylin and eosinstained tissue sections. Chronic infection leads to mucosal atrophy, intestinal metaplasia and a 3- to 6-fold increased risk of developing gastric adenocarcinoma. Chemicalgastritis Chemical gastritis, also known as reactive gastritis, bile reflux gastritis or type C gastritis, is characterised by epithelial cell loss, compensatory hyperplasia of the gastric foveolae, vasodilatation and oedema of the lamina propria with no significant inflammatory cell infiltrates. These nonspecific reactive changes are most commonly related to reflux of alkaline duodenal contents after partial distal gastrectomy, secondary motility disturbances in patients with gallstones and after cholecystectomy, and primary disturbance of antro-duodenal motility coordination. Reflux gastritis may present with bilious vomiting or less severe dyspeptic symptoms; repeated damage to the mucosa may lead to the development of a gastric ulcer. Other forms of gastritis In lymphocytic gastritis the main histological feature is the presence of numerous mature T-lymphocytes within the surface epithelium. Alcohol Direct injury Disruption of the mucus layer Degranulation of mast cells Histological findings Glandular atrophy in body mucosa Intestinal metaplasia Clinical consequences Pernicious anaemia Bacterial infection (H. Eosinophilic gastritis is a rare disease characterised by oedema and a large number of eosinophils in the inflammatory cell infiltrate in the absence of intestinal parasites. There seems to be an association between eosinophilic gastritis and a history of atopy or connective tissue disease (scleroderma, systemic lupus erythematosus) in some patients. Gastric and duodenal ulcers differ in their epidemiology, incidence and pathogenesis (Table 15. Histological section through the ulcer revealing a deep breach of the main muscle layers and haemorrhage around an artery (arrowed) in the ulcer base. The patient presented with profuse haematemesis (vomiting blood) and underwent emergency partial gastrectomy. Microscopically, the base consists of necrotic tissue and polymorph exudate overlying inflamed granulation tissue which merges with mature fibrous (scar) tissue. Arteries within this fibrous base often show extreme narrowing of their lumina by intimal proliferation (endarteritis obliterans). Shrinkage of the fibrous tissue (cicatrisation) may lead to pyloric stenosis or a central narrowing of the stomach with outflow obstruction, the so-called hour-glass deformity. It can either be neoplastic or form as a result of an excessive reparative or regenerative process. The commonest form of polyp involves simple elongation of the gastric pits separated by fibrous tissue or mildly inflamed lamina propria. These are hyperplastic or regenerative polyps and are generally found against a background of H. A similar variety is seen in body-type mucosa, but in this instance, the main feature is enlargement by cystic dilatation of the specialised oxyntic glands. A further rare cause of a polypoid mass in the stomach is heterotopic pancreas, i. Tubular adenomas (adenomatous polyps) are benign neoplastic epithelial lesions with dysplasia most commonly located in the antrum. They are relatively more common in countries with high prevalence of gastric cancer. Malignant transformation has been reported in up to 75% of these polyps, in particular in lesions over 2 cm in diameter. There are two main benign mesenchymal tumours, the leiomyoma and the schwannoma or nerve sheath tumour. This suggests that ulceration is most likely to occur where acid and pepsin first come into contact with a susceptible mucosa. Pathogenesis the pathogenesis of gastric and duodenal peptic ulcer is still under intense debate. Excessive acid production on its own cannot fully explain the occurrence of peptic ulcers and a combination of several factors appears to be more likely, as peptic ulcers can develop in patients with normal or low levels of acid. Accelerated gastric emptying together with slower than usual neutralisation of the gastric juice in the duodenal bulb due to decreased biliary, pancreatic and duodenal secretion and impaired mucosa defences have all been implicated in peptic duodenal ulcer. Breakdown of mucosal defence mechanisms due to inhibition of prostaglandin synthesis after taking non-steroidal anti-inflammatory drugs and mucosal damage due to bile and pancreatic juice reflux appear to be more important than excessive acid production in the pathogenesis of peptic gastric ulcer. However, while some of these mutations are consistent with exogenous chemical carcinogens or exposure to endogenous free-radical injury, the nature of the mutational agent cannot be deduced from the genetic lesions with any certainty. Early gastric cancer is defined as cancer limited to the mucosa (intramucosal carcinoma) or Despite a steady worldwide decline in gastric cancer incidence, gastric cancer is still the fourth most common cancer in the world, with 1 million people newly diagnosed per year. Age-standardised incidence rates of gastric cancer are twice as high in males as in females and show prominent geographical variation ranging from 3. Gastric cancer is the second leading cause of cancer death in both sexes worldwide, accounting for around 10% of all cancer deaths. The prominent geographic variation in gastric cancer incidence suggests that environmental factors such as diet might play an important aetiological role. However, evidence for all areas such as fruit and vegetable consumption, dietary supplementation with antioxidants such as vitamin C and dietary salt and nitroso compounds is still conflicting. Smoking, obesity and previous gastric surgery for benign disease have all been implicated in gastric carcinogenesis. Early gastric cancer Intramucosal Submucosal Into the muscularis propria Advanced gastric cancer Through the muscularis propria into subserosa Penetrates through the serosa (peritoneum) Invades into adjacent structures, This classification is independent of the presence or absence of lymph node metastases. Locally advanced gastric cancer invades the main muscle coats (muscularis propria) or beyond. Ninety per cent of patients with intramucosal gastric cancer survive for more than 5 years, whereas only 16% of patients with locally advanced cancers survive 5 years or longer. Depending upon the site of the tumour, direct spread can also occur into the pancreas, transverse colon, liver and spleen. Lymphatic tumour spread is initially to regional lymph nodes along both curvatures of the stomach, then to lymph nodes along the right and left gastric, coeliac and splenic arteries. Spread to non-regional lymph nodes such as retro-pancreatic, mesenteric and paraaortic groups is considered to be distant metastasis (M1). Rarely, spread to even more distant nodes is encountered, like the classical involvement of left supraclavicular nodes (Virchow node). Morphology Foci of high-grade dysplasia and intramucosal carcinoma may be endoscopically visible as slightly elevated plaques or shallow depressions. Histologically, it can sometimes be difficult to distinguish between high-grade dysplasia and intramucosal cancer, the latter being characterised by definitive invasion of the lamina propria. Depending on size and tumour type, endoscopic resection is the method of choice for high-grade dysplasia and intramucosal cancer. With increasing size, the elevated lesions develop into polypoid and later into fungating carcinomas, while the depressed areas present an excavated ulcerated appearance mimicking that seen in chronic peptic ulcer. The distinction between carcinoma and chronic peptic ulcer cannot be made with certainty on clinical, endoscopic or radiological grounds alone, so that all gastric ulcers should be subjected to multiple biopsies both before and after therapy. Carcinomas of the stomach are almost exclusively adenocarcinomas and are graded according to their degree of differentiation into well-, moderately and poorly differentiated carcinomas. Sixty to seventy per cent of gastric cancers are intestinal-type carcinomas, showing glandular or papillary structures, and often originate from areas with intestinal metaplasia. Thirty to forty per cent of gastric cancers are diffuse-type carcinomas, consisting of chains of poorly cohesive, single cells infiltrating the wall with a poorly demarcated invasive margin. Intestinal-type gastric carcinomas carry a better prognosis than the diffuse type, but this is largely explained by the more advanced stage of diffuse-type carcinomas at the time of diagnosis. Interestingly, intestinal-type gastric cancers predominate in high-incidence countries and have a strong association with H. Carcinomas spread directly to involve the serosa, which can lead to peritoneal dissemination. This can result in the formation of a malignant effusion (ascites) or involvement of other organs by transcoelomic spread, of which Other malignant tumours Adenocarcinomas comprise over 90% of all gastric malignancies.
Order 500mg valtrex with amex
As in inflammation elsewhere hiv infection and stages purchase valtrex 1000mg without prescription, injury is mediated by many factors, including enzymes and reactive oxygen species released by neutrophils, production of proinflammatory and pro-fibrotic cytokines by macrophages, and platelet-derived prostaglandins and cytokines. Glomerular inflammation is potentially reversible if the trigger is self-limiting, such as in post-streptococcal glomerulonephritis. However, persistent antibody deposition within glomeruli results in chronic injury with irreversible glomerulosclerosis. The precise site of glomerular deposits depends on the size and charge of their constituents, and determines the type of glomerular lesion and the clinical features. Thus, deposits within the mesangium or subendothelial area tend to elicit a proliferative reaction and an active nephritis with haematuria. In contrast, subepithelial deposits are sequestered from the circulation by the basement membrane and, despite complement activation, there is typically no inflammatory reaction; an example of this pattern is membranous glomerulonephritis. Endogenous glomerular cells participate in immunemediated injury and consequently contribute to the development of the lesion and the fate of the glomerulus. These cells produce a variety of cytokines, influence the coagulation cascade and elaborate new matrix. In membranous glomerulonephritis, epithelial cells overlying subepithelial deposits are stimulated to produce basement membrane material. This results in an abnormal, thickened basement membrane that initially separates and then envelops the deposits. Activated endothelial cells promote platelet and leucocyte adhesion and further damage. Mesangial cells proliferate and synthesise extracellular matrix material, contributing to the development of glomerulosclerosis. Mechanisms of glomerular injury Glomeruli can be damaged by immunological or nonimmunological mechanisms. Immuneglomerularinjury Immunological damage underlies most types of glomerulonephritis. Injury may be mediated by antibodies, activation of complement by the alternative pathway in the absence of antibodies, and less commonly T-cell-mediated mechanisms. The proteinuria is typically massive, abrupt in onset and selective, with urinary loss of albumin but not larger globulins. Over 90% of patients respond to steroid therapy, although relapses of nephrotic syndrome following discontinuation of therapy are common. Some patients become steroid-dependent but progression to chronic renal failure is very infrequent, and those that do progress usually suffer from focal segmental glomerulosclerosis, the diagnostic lesions being absent in the original biopsy. There is some experimental evidence that it results from a T-cell-derived factor but the identity of the molecule is unknown. Proximal tubules show resorption droplets of proteins and lipids that are present in the glomerular filtrate. The extent of foot process effacement matches the severity of proteinuria; clinical response to steroid therapy is accompanied by resolution of the podocyte changes. These changes produce further endothelial and epithelial injury, increased permeability to proteins and progressive sclerosis. Definitions vary from involving most (> 50%) of a glomerular tuft for cellular lesions, or the entire glomerular tuft (100%) for sclerosing lesions. Definitions vary from involving <50% of a glomerulus for cellular lesions, or < 100% of a glomerulus for sclerosing lesions. IgA nephropathy, lupus nephritis, vasculitic glomerulonephritis) and is also associated with hyperfiltration injury to glomeruli. However, as a diagnosis, it also refers to conditions in which the primary injury is to the podocyte, the podocytopathies. There is, however, experimental evidence for a plasma factor that induces greater permeability of the glomerular filtration barrier to macromolecules. It is associated with non-selective proteinuria and is the commonest cause of the nephrotic syndrome in adults. The clinical course is variable; approximately one-third of patients show spontaneous partial or complete remission, in one-third there is long-term proteinuria with preserved renal function, and one-third progress to chronic renal failure. The most common autoantibody, detected in 70% of patients, is anti-phospholipase A2 receptor. Antibodies to tumour-associated antigens have been detected in patients with malignancies, and to microbial antigens when there is an associated chronic infection. Antibody deposition results in podocyte injury and loss of foot processes, in the absence of inflammation. Later, the deposits become embedded in a thickened membrane, producing a chain-link appearance on silver stain. Lupus nephritis Renal involvement is common in systemic lupus erythematosus and is the major cause of serious morbidity in this condition. Clinical features: Proteinuria is consistently present in patients with lupus nephritis and may be nephrotic range. In those patients who do not respond to immunosuppressive therapy there is persistent proteinuria, reflecting ongoing glomerular inflammation, and progression to chronic renal failure. These result in complement-mediated activation and injury of mesangial, endothelial or epithelial cells, the pattern of injury depending on the location of the immune deposits. Morphology: Lupus nephritis produces various histological changes, reflecting the different locations of immune deposits and resulting in the diverse clinical manifestations. Mesangial hypercellularity with focal or diffuse endocapillary proliferation are the commonest patterns, but membranous or membranoproliferative disease may also be seen. Clinical features: the commonest manifestation of renal amyloidosis is proteinuria, frequently with the nephrotic syndrome. When renal deposits are extensive there is impaired renal function, and in some patients renal failure is the main presenting feature. There may be symptoms secondary to involvement of other organs, such as cardiac arrhythmias and hepatosplenomegaly. Prognosis is generally poor with frequent progression to end-stage renal disease and a high mortality. Pathogenesis: Amyloid fibrils are formed from aggregates of misfolded proteins, bound to other proteins, including serum amyloid P component, and proteoglycans. The development of amyloid fibrils may result from high levels of a normally soluble protein, or production of an abnormal protein that has a tendency to form aggregates. Morphology: Amorphous eosinophilic deposits are present within glomeruli and vessel walls. The amyloid stains pink with Congo red stain, producing anomalous colours (red/orange/green) under polarised light. Diabetic nephropathy Diabetic nephropathy is a manifestation of diabetic microvascular disease, involving the renal arterioles and glomeruli. With progression, there is more severe proteinuria that may be nephrotic range, and chronic renal impairment. Pathogenesis: A number of factors contribute to the development of diabetic nephropathy. These accumulate in the tissues by cross-linking with collagen and modulate changes in cytokine signalling. In addition, hyperglycaemia stimulates mesangial cell proliferation and matrix production. Glomerular hyperperfusion and hyperfiltration result from defective autoregulation and potentiate albumin leakage. Morphology: Hyperfiltration with renal enlargement are the first manifestations of diabetic renal disease. The earliest Monoclonal immunoglobulin deposition disease Lymphoproliferative disorders, including multiple myeloma, may be associated with production of monoclonal proteins. Free light chains are detectable in the urine and a monoclonal paraprotein is present on serum electrophoresis. Renal prognosis depends on treatment of the underlying lymphoproliferative disease. Morphology: the commonest pattern of glomerular disease is nodular glomerulosclerosis.
Aspalathus contaminatus (Red Bush Tea). Valtrex.
- How does Red Bush Tea work?
- What is Red Bush Tea?
- Are there safety concerns?
- Dosing considerations for Red Bush Tea.
- Suppressing HIV infections, preventing cancer, and preventing aging in the brain.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96183
Generic valtrex 1000mg overnight delivery
The distribution of involved lymph nodes is usually contiguous and the pattern of spread via lymphatics predictable hiv infection japan purchase valtrex without a prescription, unlike other lymphomas which may involve multiple lymph nodes with an apparently random distribution. Involvement of the liver and bone marrow is rarely seen in the absence of splenic involvement and thus the spleen seems crucial to dissemination via the blood stream. Alcohol-induced pain, for which the biological mechanism is uncertain, may also occur. Disseminated involvement of one or more extralymphatic organs such as liver, lung and bone marrow, with or without lymph node involvement. Various haematological and biochemical abnormalities may also occur, including anaemia, lymphocytopenia, raised erythrocyte sedimentation rate and low serum albumin concentration, which predict reduced survival. Morphology Classical Hodgkin lymphoma is principally a disease of lymph nodes and the diagnosis is usually established by lymph node biopsy. Classical Hodgkin lymphoma, unlike many other lymphomas, rarely breaches the lymph node capsule, accounting for the clinical finding of discrete and mobile palpable enlarged lymph nodes. This is so named because it appears to sit in a space (lacuna), caused by partial retraction of its abundant cytoplasm during tissue processing for histology. Note that the capsule (upper border of tissue in each photomicrograph) is intact and sharply demarcated in both cases. Compare this with the infiltration of surrounding fat in follicular lymphoma shown in figure 22. Treatmentrelated causes of secondary illnesses and death are becoming increasingly important. Second epithelial malignancies and cardiovascular disease (the latter arising predominantly due to mediastinal radiotherapy) now rival mortality from the lymphoma itself. Non-Hodgkin lymphomas represent a spectrum of disease from slowly progressive neoplasms to rapidly growing and destructive tumours. Diversity in clinical behaviour is reflected in a wide range of histological appearances. Within this system, precursor lymphoid cells are processed in the thymus (T cells) and bursa-equivalent tissue (B cells) into mature lymphoid cells that populate peripheral sites such as lymph nodes, spleen and mucosa-associated lymphoid tissue. They may be of T- or B-cell lineage and express the nuclear protein TdT (terminal deoxynucleotidyl transferase; an enzyme involved in creating antigen receptor diversity) as evidence of functional immaturity. These neoplasms form a spectrum of disease and are referred to as lymphoblastic lymphomas or lymphoblastic leukaemias, depending on whether they show a greater tendency for solid tumour formation (lymphoma) or dissemination through the blood stream (leukaemia). Affected lymph nodes are enlarged and usually smoothsurfaced, with homogeneous white cut surfaces. Normal nodal architecture is replaced by a diffuse infiltrate of monomorphic small lymphocytes plus scattered larger cells (prolymphocytes or paraimmunoblasts) which may form vaguely nodular aggregates (pseudofollicles or proliferation centres). The disease is almost invariably disseminated, with a high frequency of splenic, liver and bone marrow infiltration even in patients who present with localised lymphadenopathy. In many, it runs an indolent course with patients dying from unrelated causes but there is clinical and biological heterogeneity. Approximately 50% of cases are associated with immunoglobulin gene hypermutation and a good prognosis but disease lacking hypermutation is more aggressive. Patients frequently have hypogammaglobulinaemia and are particularly susceptible to bacterial infections. Cut surfaces are homogeneous and grey/ white, with occasional areas of haemorrhage and necrosis; a faintly nodular pattern may be visible. Precursor T-cell neoplasms often present as mediastinal tumours in adolescent boys. The immunophenotype of a lymphoid cell represents its distinctive expression pattern of antigenic molecules, representing its origin and state of maturation or functional activation. The relative proportions of centroblasts and centrocytes within neoplastic follicles provide the basis of grading these lymphomas; tumours containing larger numbers of centroblasts have a worse prognosis. Splenic involvement may be minimal or cause splenomegaly; the latter may be massive, with hypersplenism. They replace and expand these so that cut surfaces of the organ may appear studded with numerous discrete white nodules separated by red pulp. Follicular lymphoma is an indolent disease but it has been regarded as incurable when disseminated, and the majority of patients, until recently, have died as a direct result of their lymphoma. The exact mode of death may be difficult to determine but, in at least 30% of patients, the disease transforms into a diffuse large B-cell lymphoma, which behaves aggressively and is usually refractory to treatment. Important roles for microenvironmental components in determining biological behaviour are also increasingly recognised in other lymphomas. It is derived from, or differentiates to resemble, the mantle zone cells of germinal centres. Note extension of neoplastic follicles through the lymph node capsule (arrow) into adjacent connective tissue. Mantle cell lymphoma arises as a result of a distinctive chromosomal translocation, t(11;14) (q13;q32). The disease usually presents with lymphadenopathy but a distinctive pattern is seen in the gastrointestinal tract, where it forms multiple mucosal polyps and is termed lymphomatous polyposis. It may arise de novo or by 544 transformation of a low-grade B-cell lymphoma (usually follicular lymphoma). Diffuse large B-cell lymphoma is usually a disease of adults but may occur in childhood. Small cells with darkly stained nuclei in the background are mainly reactive t cells. It involves extranodal sites, particularly the jaw, gastrointestinal tract and gonads. Histology is distinctive with tightly packed, medium-sized lymphoid cells interspersed with large, highly phagocytic macrophages. Morphology is not a good indicator of clinical behaviour in these neoplasms, which form a heterogeneous group. Better subclassification may emerge as their molecular genetic characterisation advances. Systemic involvement is a bad prognostic feature, associated with a median survival of only 2. Patients usually present with widespread lymphadenopathy, systemic symptoms, skin rashes, polyclonal hypergammaglobulinaemia and immunosuppression. Neoplastic T cells in involved nodes are typically larger than normal, with pale cytoplasm, and tend to cluster. Neoplastic cells may fail to express lineage-associated markers but they are genotypically T cell in origin. The disease is usually nodal but there is frequently extranodal involvement as well. A complex mixture of reactive and neoplastic cells is present; the larger cells with pale or clear cytoplasm represent the neoplastic t-cell population. Note the suggestion of pallor surrounding the epithelial structures, reflecting marked monocytoid differentiation by infiltrating lymphocytes (making them larger, with pale cytoplasm). Extranodallymphomas Extranodal lymphoid tissue is widely distributed in the body, as described earlier. Most of these sites normally lack lymphoid tissue, and acquisition of reactive lymphoid tissue, as the result of an autoimmune. Helicobacter gastritis) process, is an essential forerunner to the development of lymphoma. Histologically, they are characterised by reactive germinal centres surrounded or colonised by neoplastic B cells. The latter resemble normal marginal zone B cells and they infiltrate epithelial structures to form lymphoepithelial lesions. These lymphomas often also show abundant plasma cell differentiation, usually adjacent to the mucosal surface. The former tend to remain localised for long periods and have an indolent clinical course, often with a very good prognosis.
Cheap valtrex online mastercard
Whereas caecum to proximal transverse colon are supplied by branches of the superior mesenteric artery antiviral garlic valtrex 1000mg low price, the distal transverse to the upper rectum are supplied by branches of the inferior mesenteric artery and the remainder of the rectum is supplied by the middle and inferior rectal arteries. Knowledge of the patterns of blood supply is important in order to determine the likely affected sites of ischaemia and, because lymphatic drainage follows similar patterns, to predict the likely distribution of lymph node metastases from the site of a tumour. Nerve supply the intestine has a complex nerve network comprising autonomic motor and sensory neurones and a separate enteric nervous system. The sympathetic supply originates from ganglia outside the gut in the coeliac and mesenteric plexuses. Stimulation of parasympathetic nerves increases muscular contraction, blood supply and secretory activity; stimulation of the sympathetic supply has the opposite effects. The enteric nervous system has sensory receptors in the mucosa and bowel wall that respond to changes in volume and composition of the bowel contents, and through neuronal connections elicits the appropriate response in the effector system mediated by a wide variety of neurotransmitters, such as vasoactive intestinal polypeptide, cholecystokinin and somatostatin. Defects arising in the course of this complex intrauterine developmental process are relatively common. Atresia and stenosis Atresia refers to the complete occlusion of the intestinal lumen, whereas stenosis implies incomplete obstruction. Both lesions are most commonly found in the duodenum or small intestine and rarely in the colon. They are diagnosed on the basis of persistent vomiting of bile-containing fluid and failure to pass meconium. Jejuno-ileal atresia commonly appears to be the result of an intrauterine accident, such as incarceration of the midgut in the physiological umbilical hernia or some other form of vascular occlusion. Duplications (enteric cysts) Duplications of the bowel are most commonly seen in the ileum and may either present as a tubular double-barrelled appearance or form a cyst in the mesentery. These anomalies can produce an abdominal mass, cause intestinal obstruction, or initiate a volvulus (p. Histologically, it is a true diverticulum consisting of all three layers of bowel. The diverticulum is usually lined by small intestinal mucosa, but heterotopic gastric acid-secreting epithelium or pancreatic tissue may be seen in up to 50% of cases. Meconium ileus the term meconium ileus refers to small intestinal obstruction resulting from thickening and desiccation (inspissation) of the viscid meconium produced by neonates with cystic fibrosis (Ch. It is seen in about 15% of affected neonates and may be complicated by perforation, secondary atresia or volvulus. Under normal circumstances the parasympathetic tone, which controls the contraction of the circular muscle coat, is modulated at the ganglia by the sympathetic innervation. However, in the absence of the myenteric ganglia, the intact extramural parasympathetic supply is unchecked by sympathetic modulation and results in spasm of the circular muscle, leading to intestinal obstruction. Histologically, there is a complete lack of ganglion cells in the submucosal and myenteric plexuses, and proliferation of cholinergic nerves in the narrowed bowel segment. The effects of the aganglionosis vary from life-threatening total obstruction to mild cases causing chronic constipation. Incidence and clinical manifestations Coeliac disease is much more common in Northern Europe and is rare in Africa and Asia. It presents most frequently in either early childhood or in the third or fourth decades with a slight preponderance in females. Aetiology and pathogenesis the toxic components of gluten are gliadin and glutenin, but the mechanism by which they induce tissue damage remains uncertain. Although these toxic peptides have direct effects on intestinal permeability through the disruption of tight junctions between enterocytes, it seems increasingly likely that tissue injury is more a consequence of the immune response than a direct effect. Serum anti-transglutaminase, anti-gliadin and anti-endomysial antibodies are found in 90% of patients; however, their role in the pathogenesis of the disease remains to be established. Morphology Whilst the histological changes described here are characteristic for coeliac disease, they are not diagnostic. Anorectal anomalies A large variety of malformations that affect the termination of the large bowel have been described. Moderately accelerated cell loss can be compensated for by increased cell proliferation. Fully developed coeliac disease is therefore characterised by a total malabsorption affecting sugars, fatty acids, monoglycerides, amino acids, water and electrolytes. The lesion is more severe in the proximal small intestine (duodenum and proximal jejunum) and there may be secondary reduction in pancreatic secretion and bile flow as a result of reduced production or release of the intestinal hormones pancreozymin, secretin and cholecystokinin. B Salmonella Food poisoning by Salmonella organisms (salmonellosis) is a common and increasing problem in many countries. In some patients Salmonella infection results in vomiting and profuse watery diarrhoea, usually with colicky, periumbilical pain suggesting predominantly gastric and small intestinal involvement. In others, the symptoms relate to the large intestine, with frequent, small volume, bloody motions, teems and tenderness over the sigmoid colon. In contrast to the gastroenteritis caused by most other Salmonella species, typhoid fever is not a typical diarrhoeal disease and the intestinal pathology is characterised by a macrophage, not a polymorph, infiltrate. Patients usually present with prolonged fever, headache, abdominal discomfort and general debility. After penetration through the epithelium, Salmonella are ingested by macrophages which probably facilitate the systemic spread of the bacteria as Salmonella-infected macrophages can survive for several hours. In this way, infected cells pass into the liver and spleen and can be found also in bone marrow and blood. However, some patients may become refractory to gluten-free diet many years later. Patients with coeliac disease have a slightly increased risk of developing chronic ulcerative jejunoileitis, primary enteropathy associated T-cell lymphoma as well as adenocarcinoma of the small bowel. Tropical sprue Tropical sprue is a chronic and progressive malabsorption syndrome seen in patients who live or have lived in the tropics. The condition is thought to be secondary to bacterial contamination of the small bowel, and Escherichia coli, Klebsiella and Enterobacter have all been implicated. The histological appearances resemble those of coeliac disease; however, the findings are usually more severe in the jejunum and ileum, whereas coeliac disease involves the proximal duodenum and spares the ileum. The prognosis is excellent as long as the correct diagnosis is made, and patients are usually treated with tetracycline and folate for 6 months. Patients present with sudden onset of severe diarrhoea, accompanied by shock and dehydration. There is widespread superficial ulceration predominantly affecting the small intestine. Microscopically, there is acute inflammation of the mucosa with intense congestion and widespread necrosis. The surface of the mucosa is covered by an exudate containing numerous staphylococci. Campylobacter colitis Since the early 1900s Campylobacter organisms have been known to cause dysentery and abortion in cattle and domestic animals, but recognition of their role in human disease is relatively recent. The histological changes seen in rectal biopsies are non-specific, and are similar to those seen in other forms of infective colitis. Gonococcal proctitis Gonococcal proctitis (inflammation of the rectum) is an acute exudative inflammatory condition which develops by genitoanal spread in females, and results from anal intercourse in males. The histological changes are non-specific, but the demonstration of numerous Gram-negative diplococci in the exudate leads to a presumptive diagnosis. As with other forms of infective colitis, definitive diagnosis depends on culture of the organisms. Cholera Cholera is a form of secretory diarrhoea resulting from infection with Vibrio cholerae. The cholera toxin binds to a specific receptor on epithelial cells which leads to increased adenylate cyclase activity. The affected enterocytes secrete large amounts of fluid and sodium ions, and the ensuing watery diarrhoea can be extreme, with overwhelming fluid loss and a rapidly fatal outcome. Because the effects are mediated by an exotoxin and there is no bacterial invasion of host tissues, the histological changes are remarkably slight; the mucosa shows mild oedema and goblet cell depletion. In primary infection, an inconspicuous intestinal lesion is accompanied by gross enlargement of mesenteric nodes. Secondary tuberculous enteritis is a complication of extensive pulmonary tuberculosis which results from the swallowing of infected sputum.
Buy generic valtrex 500mg on line
Dermatomyositis is a microangiopathy affecting skin and muscle hiv infection chance buy discount valtrex on-line, where complement deposition causes capillary lysis and muscle ischaemia. Histology shows muscle fibre necrosis with phagocytosis of degenerate fibres by macrophages. Evidence of muscle fibre regeneration can usually be found, and fibre atrophy may be a striking feature in some cases, particularly in the perifascicular fibres in cases of childhood dermatomyositis. This uncommon, dominantly inherited disorder results in an abnormal sensitivity to certain anaesthetic agents, Subacute alcoholic myopathy occurs in chronic alcoholics, and presents with proximal muscle weakness and wasting. Biopsy shows selective atrophy of type 2b fibres, which is reversible in the early stages. Inclusionbodymyositis Inclusion body myositis is most frequent in elderly patients and clinically resembles polymyositis. Its aetiology is unknown, but affected muscles show inflammation and fibre necrosis associated with small filamentous intracellular inclusions and vacuoles. Over 90% of patients have antibodies against acetylcholine receptor proteins that bind to the postsynaptic receptor and block neurotransmission; anti-striated muscle antibodies are present in a smaller proportion of patients. The thymus is hyperplastic in over 50% of patients, and a thymoma is present in a further 15%. Acetylcholine release from motor nerve terminals is impaired by the binding of an abnormal IgG-class antibody to presynaptic calcium ion channels. Diagram shows cornea (1), anterior chamber (2), iris (3), ciliary body (4), lens (5), vitreous humour (6), retina (7), macula (8), choroid (9), optic disc (10), optic nerve (11) and sclera (12). Retinal ischaemia usually occurs due to the occlusion of a supplying blood vessel by atheroma, giant cell arteritis, thrombosis or embolism. If the central retinal artery is involved, the inner two-thirds of the retina will undergo ischaemic degeneration; occlusion of the posterior ciliary artery damages the photoreceptor cells in the outer retinal layers. Direct injuries to the eye are the most important clinically and may be classified according to the site and nature of the damage; in the perforating injuries, the sclera is only partially torn, but complete rupture occurs in penetrating injuries. Penetrating and perforating injuries result in the most severe form of traumatic damage to the eye. The immediate complications of penetrating injuries include disruption of the globe, with haemorrhage and detachment of the lens and retina. Infection is a common complication, particularly if the missile is composed of organic material. The cellular reactions to infection in the eye are similar to those elsewhere in the body. Inflammation of the uvea and ciliary body leads to exudation of protein and inflammatory cells into the posterior cornea, which can be detected on fundoscopy. Local inflammatory changes can result in adhesions within the anterior chamber, causing glaucoma (see below). Two main patterns of haemorrhage are seen on fundoscopy: ring when the ophthalmic division of the trigeminal nerve is involved in shingles. The organism infects the conjunctival and corneal epithelium, and can be identified as intracytoplasmic inclusions on conjunctival smears. Parasitic infections Acanthamoeba Acanthamoeba is a free-living protozoan in mains water supplies. It can cause a corneal infection (keratitis) and may invade the eye, particularly in contact lens wearers. Antibiotic therapy is usually effective, although invasive infections are difficult to eradicate. Toxoplasmosis In congenital infections with the protozoan Toxoplasma gondii, the organism spreads to numerous sites in the body. Retinal involvement takes the form of chorioretinitis with extensive tissue destruction and microphthalmos in severe cases. Toxocara canis Toxocara canis infection is usually acquired in childhood from contact with ova from infected dogs. Ingestion of the ova is followed by liberation of larvae in the stomach and duodenum; the larvae migrate through the body but do not usually mature. A granuloma can develop in the retina around a dead larva, causing visual obstruction that clinically may mimic an intraocular neoplasm. Neovascularisation Neovascularisation is an important response to retinal ischaemia and haemorrhage, resulting in proliferation of small vessels around the edge of the lesion. These small vessels may also penetrate the vitreous fluid, where the lack of supporting tissue renders them prone to rupture and haemorrhage. Autoimmune diseases these uncommon disorders usually arise as a consequence of ocular injury, particularly perforating wounds. Prompt clinical attention to such injuries has greatly reduced the incidence of these complications. Glaucoma denotes a group of common disorders in which the intraocular pressure is increased to a level that impedes blood supply to the retina, resulting in optic nerve cupping on fundoscopy and ultimately in blindness. The increase in intraocular pressure is usually caused by obstruction to the outflow of aqueous fluid, Lens-induceduveitis Release of lens protein into the anterior chamber or vitreous occasionally causes a giant cell granulomatous reaction involving the lens and uvea, resulting from a delayed hypersensitivity reaction to lens antigens. Closed-angle glaucoma Closure of the irideocorneal angle, thus obstructing the drainage of aqueous humour from the anterior chamber, can occur when the iris is in mid dilatation, particularly in middle-aged or elderly individuals. Sympatheticophthalmitis Trauma to one eye with damage to the iris or ciliary body may cause a delayed hypersensitivity reaction following sensitisation to uveal and retinal antigens. This results in a giant cell granulomatous inflammatory response in either the damaged eye or the second eye. Open-angle glaucoma Open-angle glaucoma can occur as a primary degenerative condition in the elderly, when a progressive accumulation of collagen within the trabeculae and extracellular space of the outflow system increases resistance to the flow of aqueous fluid. This causes a slow increase in intraocular pressure that often presents as a central visual field defect. Open-angle glaucoma may also occur due to mechanical obstruction of the outflow system by inflammatory cells, haemorrhage or tumour infiltration. Cataracts result from the formation of opaque proteins within the lens, which usually also results in a loss of lens elasticity. Mature cataracts can cause severe visual loss, but this can be treated surgically by removal of the affected lens and insertion of a synthetic plastic substitute. Cataracts occasionally cause glaucoma due to mechanical obstruction of the anterior chamber angle, or lens dislocation. Macular degeneration occurs in 30% of adults aged over 75 years and is commoner in females. Naevi and malignant melanoma Naevi and malignant melanoma occur most frequently in adults, and derive from the melanocytes of the uveal tract. Malignant melanomas occur as a solitary mass in one eye, usually arising in the posterior choroid. The aqueous outflow at the anterior chamber angle (arrow) is obstructed by a mass of fibrovascular tissue containing numerous capillaries [A] in contrast to a normal control [B]. The resulting increase in intraocular pressure caused glaucoma, which eventually necessitated removal of the eye. Macular damage occurs as a result of ingrowth of fragile new blood vessels beneath the retina that are prone to leak and haemorrhage.
Purchase on line valtrex
Without successful treatment of the aplasia hiv infection rate by country cheap valtrex online amex, severe forms are fatal within months. The exceptions are children and younger adults who have an appropriate stem cell donor in whom stem cell transplantation can be curative with an associated low transplant-related mortality. However, anaemia due to acute blood loss and the pancytopenia of hypersplenism are also included. A fall in haemoglobin of much greater than 10 g/L per week must indicate the presence of haemorrhage or haemolysis, as complete cessation of erythropoiesis would result in a rate of fall of no more than 10 g/L per week. An exception is the rapid fall in haematocrit due to infusion of cellfree fluids in a dehydrated subject. Acute blood loss anaemia Chronic haemorrhage, usually gastrointestinal, causes anaemia by depletion of iron stores. Acute blood loss may result initially in a state of cardiovascular collapse, as described in an earlier section. Following adjustment to the plasma volume over a period up to 48 hours, anaemia will be apparent. The blood picture is normocytic and normochromic, and an increased number of polychromatic erythrocytes and reticulocytes in the days following a brisk haemorrhage reflects increased haemopoiesis. In carcinomatosis, numerous other factors are likely to be contributory to the anaemia, such as bleeding from carcinoma of the gastrointestinal tract, folate deficiency and chemotherapy. Fibrosis of the marrow is also a feature of other myeloproliferative disorders and some other malignant marrow infiltrates. The haemolytic anaemias are those in which a major feature is a reduction in red cell lifespan. In severe haemolysis, red cell survival may be reduced from the normal 120 days to less than 1 day. Although erythropoiesis will increase, anaemia is inevitable under such circumstances. Even in the presence of normal marrow function and adequate supplies of haematinics, the maximum potential increase in red cell production is some six times the normal rate. In the presence of a defect of red cell production, as in folate deficiency or thalassaemia major, the severity of the anaemia is increased in relation to the degree of shortening of red cell survival. Worldwide, however, thalassaemia, sickle cell disease and malaria are of major importance. Abnormalities of each of these components can be a cause of chronic haemolytic anaemia. Defectsoftheredcellmembrane Hereditary spherocytosis and hereditary elliptocytosis include several disorders in which diminished red cell survival is due to a defect in one of the structural proteins of the erythrocyte membrane such as spectrin. Spherocytes are not confined to hereditary spherocytosis however; they are also present in the blood film in immune haemolytic anaemia (p. In hereditary spherocytosis, biconcave erythrocytes are released from the marrow but they rapidly lose membrane and therefore assume a spherical shape. Spherocytes are of reduced deformability, which impedes their traverse through the splenic microcirculation. They become metabolically stressed by glucose lack and acidosis, and are eventually prematurely phagocytosed. The abnormal red cells in these disorders are more sensitive than normal to lysis under osmotic stress. The clinical features are variable and are those of chronic extravascular haemolysis. Occasionally, transient red cell aplasia secondary to erythrovirus infection can develop, when several family members may be affected by aplasia simultaneously. Removal of the spleen results in resolution of the anaemia, confirming the role of the spleen in the haemolytic process. Consequencesofhaemolysis In addition to the particular pathological and clinical features of the various haemolytic diseases, certain consequences of the haemolytic process and the response to it are common to all types of haemolytic disorder. Red cell destruction occurs predominantly in the reticuloendothelial tissues of the spleen and liver. Splenomegaly is therefore common in chronic haemolytic anaemias, and hepatomegaly may also be present. Within the spleen there is congestion within the cords and deposition of haemosiderin. Particular features of intravascular haemolysis are the presence of free haemoglobin in plasma and urine (haemoglobinaemia, haemoglobinuria), of methaemalbumin in plasma (oxidised haem bound to albumin) and of haemosiderin in urine (in shed renal tubular cells that have reabsorbed haemoglobin from the tubular contents; the haem is incorporated into haemosiderin). The generation of reduced glutathione by the metabolic activity of the red cell normally inactivates oxidants. Deficiency of several of the enzymes involved in these reactions has been identified. Only two are of pathological and major clinical significance: glucose-6-phosphate dehydrogenase deficiency and pyruvate kinase deficiency. Reduced glutathione protects haemoglobin and red cell membrane from oxidative damage. It is a sex-linked disorder: female heterozygotes are usually asymptomatic and may have some protection from falciparum malaria; this probably explains the high prevalence of the disorder in many parts of the world. Type A differs from type B by a single amino acid substitution and is functionally normal. Type A-minus has an additional amino acid substitution resulting in decreased red cell enzyme activity and disease. Typically, there is a tendency to the development of an acute haemolytic episode associated with the ingestion of an oxidant drug (for example, some antimalarials and antibiotics) and with other stresses such as surgery or infection. A further variant is found in Mediterranean populations and is associated with the acute haemolytic tendency known as favism, where ingestion of the fava (broad) bean results in acute haemolysis. Oxidised, denatured haemoglobin is seen as red cell inclusions (Heinz bodies) attached to the cell membrane, when blood is stained supravitally as in the reticulocyte preparation. Treatment consists essentially of avoidance of known precipitating factors for haemolysis. This situation results in reduced oxygen affinity of haemoglobin and increased oxygen delivery to the tissues; the anaemia is thus less symptomatic than would be expected from its severity. Haemoglobinopathies(abnormalhaemoglobins) Abnormal haemoglobins are caused by a single point mutation in the genetic code resulting in an amino acid substitution in the alpha or beta globin chain of haemoglobin A. Several hundred variant haemoglobins have been identified but few are clinically significant and almost all of those involve beta chain substitutions. HbS, causing haemolysis and microvascular occlusion an unstable haemoglobin, causing chronic haemolysis with Heinz bodies (red cell inclusions composed of denatured haemoglobin) a haemoglobin of increased oxygen affinity, causing polycythaemia a haemoglobin that tends to the oxidised state (methaemoglobin), causing cyanosis. Substitution of valine for glutamic acid in position 6 in the beta chain of globin results in a haemoglobin (HbS) that undergoes aggregation and polymerisation at low oxygen tensions. The consequence of this distortion and the predominant features of sickle cell disease are a chronic haemolytic anaemia and microvascular occlusion, causing ischaemic tissue damage. The gene for HbS is common in the West and Central African populations, the Mediterranean, Middle East and some parts of the Indian subcontinent. The heterozygous state, or sickle cell trait, results in less than 40% HbS, the remainder being mostly normal HbA. Two major bands are therefore present on electrophoresis of haemoglobin: one corresponding to HbS and one to HbA. The carrier is clinically and haematologically essentially normal, sickling occurring only very uncommonly and only under conditions of severe hypoxia. Haematuria is an occasional feature, due to renal papillary necrosis from focal sickling in the renal medulla. Extramedullary erythropoiesis in the liver and, occasionally, other sites is a minor feature. Vascular occlusion with resultant ischaemia causes severe pain, often in the long bones, abdomen or chest. There is convincing evidence that transcranial arterial Doppler ultrasonography can identify children at increased risk of stroke manifested by increased Doppler flow rates. Acute sequestration of sickle cells in the liver or (in children) spleen may cause pain and acute exacerbation of anaemia. As in pyruvate kinase deficiency, oxygen affinity of the haemoglobin is low and symptoms of anaemia mild, due to the relatively enhanced O2 delivery to tissues.
Purchase valtrex in india
Over millions of years risk hiv infection kissing order valtrex with mastercard, a ribozyme eventually evolved with the ability to catalyze the formation of peptide bonds and to synthesize proteins. Proteins eventually supplanted ribozymes as catalysts for most other biochemical reactions. Each of these events is improbable, and their combined probability is exceedingly remote, even with a vast number of chemical "experiments" over hundreds of millions of years. Some steps in prebiotic evolution might have occurred in thermal vents deep in the ocean or in hot springs on volcanic islands where conditions were favorable for some of the reactions. Conditions for prebiotic synthesis were probably favorable beginning approximately 4 billion years ago, but the geologic record has not preserved convincing microscopic fossils or traces of biosynthesis older than 3. Another mystery is how L-amino acids and D-sugars (see Chapter 3) were selected over their stereoisomers for biological macromolecules. For example, mixtures of nucleotides composed of L- and D-ribose cannot basepair well enough for template-guided replication of nucleic acids. In the laboratory, particular amino acid stereoisomers (that could have come from meteorites) can bias the synthesis of D-sugars. The situation is obscure, because none of these primitive organisms survived and they left behind few traces. All contemporary organisms have diverged equally far in time from their common ancestor. These events inevitably produce genetic diversity through divergence of sequences or creation of novel combinations of domains. For example, a typical human genome differs at hundreds of thousands of sites from the the so-called reference genome (see Chapter 7). Many mutations are neutral, but others may confer a reproductive advantage that favors persistence via natural selection. As these sister genes acquire random point mutations, insertions, or deletions, their structures inevitably diverge, which allows A. Divergence of originally identical genes from different mutations in sister lineages Ancestral gene Two species diverge B. The terms ortholog and paralog describe the relationship of homologous genes in terms of how their most recent common ancestor was separated. To illustrate this point, let us say that gene A is duplicated within a species, forming paralogous genes A1 and A2. If these genes are separated by a speciation event, so that species 1 has genes sp1A1 and sp1A2 and species 2 has genes sp2A1 and sp2A2, it is proper to say that genes sp1A1 and sp2A1 are orthologs and genes sp1A1 and sp1A2 are paralogs, but genes sp1A1 and sp2A2 are also paralogs because their most recent common ancestor was the gene that duplicated. Vertebrates also lost many genes that had been maintained for more than 2 billion years in earlier forms of life. For instance, humans lack the enzymes to synthesize certain essential amino acids, which must be supplied in our diets. Evolution of Prokaryotes Bacteria and Archaea dominate the earth in terms of numbers, variety of species, and range of habitats. They share many features, including a single cytoplasmic compartment with both transcription and translation, basic metabolic enzymes and flagella powered by rotary motors in the plasma membrane. Both divisions of prokaryotes are diverse with respect to size, shape, nutrient sources, and environmental tolerances, so these features cannot be used for classification, which relies instead on analysis of their genomes. Abetted by rapid proliferation and large populations, natural selection allowed prokaryotes to explore many biochemical solutions to life on the earth. Other Bacteria and Archaea can use energy sources such as hydrogen, sulfate, or methane that are useless to eukaryotes. Far less than 1% of Bacteria and Archaea have been grown successfully in the laboratory, so many varieties escaped detection by traditional means. Only a very small proportion of bacterial species and no Archaea cause human disease. Chlorophyll-based photosynthesis originated in Bacteria around 3 billion years ago. Multiple rounds of gene duplication and divergence can create huge families of genes encoding related but specialized proteins, such as membrane carrier proteins. Such lateral transfers explain how highly divergent prokaryotes came to share some common genes and regulatory sequences. For example, all the major branching events among Archaea appear to be associated with lateral transfers of genes from Bacteria. Massive lateral transfer occurred twice in eukaryotes when they acquired two different symbiotic bacteria that eventually adapted to form mitochondria and chloroplasts. Lateral transfer continues to this day between pairs of prokaryotes, between pairs of protists, and even between prokaryotes and eukaryotes (such as between pathogenic bacteria and plants). The genetic innovations created by these processes produce phenotypic changes that are acted on by natural selection. The process depends on tolerance of organisms to change, a feature called "evolvability. Approximately 3 billion years ago, a momentous lateral transfer event brought the genes for the two photosystems together in cyanobacteria, arguably the most important organisms in the history of the earth. Cyanobacteria (formerly misnamed blue-green algae) use an enzyme containing manganese to split water into oxygen, electrons, and protons. This form of oxygenic photosynthesis derives energy from sunlight to synthesize the organic compounds that many other forms of life depend on for energy. Together, they had a reliable energy supply for processes such as biosynthesis, regulation of the internal ionic environment, and cellular motility. This massive lateral transfer of genes into the new organism was one of the defining events in the origin of eukaryotes. This pivotal transfer on the proteobacterial genome to the original eukaryote seems to have occurred just once! The two prokaryotes may have fused, but more likely an entire bacterium entered into the cytoplasm of its host allowing the two cells to establish a mutually beneficial symbiotic relationship. All traces of the original eukaryote have disappeared except for the genes donated to its progeny. Microscopic, single-celled eukaryotes called protists have been numerous and heterogeneous throughout evolution, but no existing protist appears to be a good model for the ancestral eukaryote. Origin of Eukaryotes Divergence from the common ancestor explains the evolution of prokaryotes but not the origin of eukaryotes, which inherited genes from both Archaea and Bacteria. A contemporary archaeon called Lokiarchaeota has these genes and is the closest known living relative of the ancient archaeon that became the eukaryote. The bacterial ancestor of mitochondria was an -proteobacterium related to modern-day pathogenic Rickettsias. Evolution of the Mitochondrion the mitochondrial progenitor brought along approximately 2000 genes, most of which eventually moved (by a still mysterious process) to the host cell nucleus or were lost. Bacterial genes migrate to host genome as bacteria evolves into mitochondria and intercellular digestive system forms in early eukaryote A. Mitochondria maintain the capacity to synthesize proteins and a few genes for mitochondrial components. The transfer of bacterial genes to the nucleus sealed the dependence of the organelle on its eukaryotic host. Even though acquisition of mitochondria was an early event in eukaryotic evolution, some eukaryotes, including the anaerobic protozoans Giardia lamblia and Entamoeba histolytica (both causes of diarrhea), lack fully functional mitochondria. These lineages lost many mitochondrial genes and functions through "reductive evolution" in certain environments that did not favor natural selection for respiration. These reduced organelles have two membranes like mitochondria, but vary considerably in other functions. Evolution of Membrane-Bounded Organelles Compartmentalization of the cytoplasm into membrane-bounded organelles is one feature of eukaryotes that is generally lacking in prokaryotes. Endoplasmic reticulum, Golgi apparatus, lysosomes, and endocytic compartments arose by different mechanisms. Compartmentalization allowed ancestral eukaryotes to increase in size, to capture energy more efficiently, and to regulate gene expression in more complex ways.