Discount 15 mg actos fast delivery
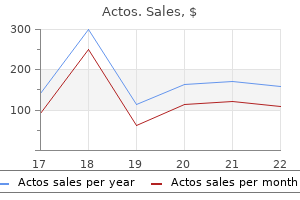
The components of potential energy are intravascular pressure (P) and gravitational potential energy diabetes food list discount actos 15 mg on line. The factors contributing to intravascular pressure are described in the preceding text. Gravitational potential energy represents the ability of a volume of blood to do work because of its height above a specific reference level. The formula for gravitational potential energy is the same as that for hydrostatic pressure (see Eq. Because the gravitational potential energy and hydrostatic pressure usually cancel each other out and the static filling pressure is relatively low, the predominant component of potential energy is the dynamic pressure produced by cardiac contraction. Potential energy can be expressed as follows: Kinetic energy represents the ability of blood to do work on the basis [Equation 5. It is proportional to the specific gravity of blood and the square of blood velocity, in centimeters per second: By combining Eqs. In a converging tube, the opposite would occur; a pressure drop and increase in velocity would result in potential energy being converted to kinetic energy. While pressure increases, total fluid energy remains constant as a result of a decrease in velocity. The fluid energy lost in moving blood through the arterial circulation is dissipated mainly in the form of heat. The term viscosity describes the resistance to flow that arises because of the intermolecular attractions between fluid layers. The coefficient of viscosity is defined as the ratio of shear stress to shear rate (D): Shear stress is proportional to the energy loss resulting from friction [Equation 5. Fluids with particularly strong intermolecular attractions offer a high resistance to flow and have high coefficients of viscosity For example, motor oil has. Because it is difficult to measure viscosity directly relative viscosity, is often used to relate the viscosity of a fluid to that of water. Because viscosity increases exponentially with increases in hematocrit, the concentration of red blood cells is the most important factor affecting the viscosity of whole blood. The viscosity of plasma is determined largely by the concentration of plasma proteins. Blood viscosity increases rapidly at low shear rates but approaches a constant value at higher shear rates. In most of the arterial circulation, the prevailing shear rates place the blood viscosity on the asymptotic portion of the curve. Thus, for arteries with diameters greater than approximately 1mm, human blood resembles a constant-viscosity or Newtonian fluid. Energy losses owing to inertial effects often exceed viscous energy losses, particularly in the presence of arterial disease. Inertial Energy Losses Energy losses related to inertia (E) are proportional to a constant (K), the specific gravity of blood, and the square of blood velocity: Because velocity is the only independent variable in this equation, [Equation 5. When the pressure drop across an arterial segment is measured at varying flow rates, the experimental data fit a line with both linear (viscous) and squared (inertial) terms. The experimental data line (solid) has both linear and squared terms, corresponding to viscous and inertial energy losses. These additional energy losses are related to inertial effects and are proportional to . For a wide range of flow rates, the pressure drop is negligible until the radius is reduced to approximately 0. The arterioles and capillaries are responsible for more than 60% of the total resistance, whereas the large- and medium-sized arteries account for only about 15%. While the velocity within each lamina remains constant, the velocity is lowest adjacent to the tube wall and increases toward the center of the tube. As discussed previously the energy expended in moving one lamina of fluid, over another is proportional to viscosity. The center laminae move more rapidly than those near the periphery, and the flow profile is parabolic. Although turbulent flow is uncommon in normal arteries, the arterial flow pattern is often disturbed. It is a transient perturbation in the laminar streamlines that disappears as the flow proceeds downstream. When turbulence is the result of a stenotic arterial lesion, it generally occurs immediately downstream from the stenosis and may be present only over the systolic portion of the cardiac cycle when the velocities are highest. Because of the random velocity changes, energy losses are greater for a turbulent or disturbed flow state than for a laminar flow state. Boundary Layer Separation In fluid flowing through a tube, the portion of fluid adjacent to the tube wall is referred to as the boundary layer. This layer is subject to both frictional interactions with the tube wall and viscous forces generated by the more rapidly moving fluid toward the center of the tube. When the tube geometry changes suddenly as at points of curvature, branching, or variations in lumen diameter, small pressure gradients are created that cause the boundary layer to stop or reverse direction. This change results in a complex, localized flow pattern known as an area of boundary layer separation or flow separation. An area of flow separation has formed along the outer wall of the carotid bulb that includes helical flow patterns and flow reversal. The region of the carotid bulb adjacent to the separation zone is subject to relatively low shear stresses. Distal to the bulb, in the internal carotid artery, flow reattachment occurs and a more laminar flow pattern is present. Rapid flow is associated with high shear stress, whereas the slower flow of the separation zone produces a region of low shear. These spectral characteristics are consistent with the presence of flow separation and are considered to be a normal finding, particularly in young individuals. The clinical importance of boundary layer separation is that these localized flow disturbances may contribute to the formation of atherosclerotic plaques. Pulsatile Flow In a pulsatile system, pressure and flow vary continuously with time and the velocity profile changes throughout the cardiac cycle. The hemodynamic principles already discussed are based on steady flow, and they are not adequate for a precise description of pulsatile flow in the arterial circulation; however, as previously stated, they can be used to determine the minimum energy losses occurring in a specific flow system. The term vascular impedance is used to describe the resistance or opposition offered by a peripheral vascular bed to pulsatile blood flow. For example, when a kidney is perfused by steady flow instead of pulsatile flow, a reduction in urine volume and sodium excretion occurs. Although the exact mechanism is unknown, transcapillary exchange, arteriolar tone, and lymphatic flow are all influenced by the pulsatile nature of blood flow. Bifurcations and Branches the branches of the arterial system produce sudden changes in the flow pattern that are potential sources of energy loss. However, the effect of branching on the total pressure drop in normal arterial flow is relatively small. Flow patterns in a bifurcation are determined mainly by the area ratio and the branch angle. The area ratio is defined as the combined area of the secondary branches divided by the area of the primary artery. If the combined area of the branches equals the area of the primary artery the area ratio is 1. This mechanism may play a role in the localization of atherosclerosis and aneurysms in this arterial segment. As blood flows around a curve, the high-velocity portion of the stream is subjected to the greatest centrifugal force; rapidly moving fluid in the center of the vessel tends to flow outward and be replaced by the slower fluid originally located near the arterial wall. This can result in complex helical flow patterns, such as those observed in the carotid bifurcation. The average angle between the human iliac arteries is 54 degrees; however, with diseased or tortuous iliac arteries, this angle can approach 180 degrees. Tangential Stress and Tension the tangential stress within the wall of a fluid-filled cylindrical tube can be expressed as follows: where P is the pressure exerted by the fluid (in dynes per square [Equation 5. Stress has the dimensions of force per unit area of tube wall (dynes per square centimeter).
Discount actos 45mg line
A median sternotomy with or without extension into the abdomen provides access to the pericardium which should be opened diabetic diet 1500 calorie actos 45mg cheap. For the portion of the vena cava below the pericardial sac, the central tendon of the diaphragm can be incised and retracted if needed. The hepatic flexure of the colon and the first and second portions of the duodenum are retracted caudally whereas the liver is, retracted cephalad. Usually within the hepaticoduodenal ligament, the bile duct runs, anterior to the portal vein and hepatic artery with the hepatic artery to the left of the portal vein. The hepaticoduodenal ligament should be opened on its right, posterior side to directly expose the portal vein. The superior mesenteric vein is exposed in a similar manner as the distal superior mesenteric artery the transverse mesocolon is elevated, and the middle colic vessels are. The splenic vein runs along the posterior surface of the pancreas, with multiple small branches directly draining the pancreas. Using a midline or left subcostal incision, one approaches the splenic vein through the lesser sac by developing a plane along the inferior edge of the pancreas. As the body of the pancreas is rotated superiorly the small, pancreatic veins must be carefully ligated. Exposure of Common Femoral Artery the common femoral artery is the extension of the external iliac artery below the inguinal ligament. The artery exits the abdomen just medial to the midpoint of the inguinal ligament, with the common femoral vein medial and the femoral nerve lateral to the artery the artery and vein cross under the inguinal ligament deep to the fascia lata, with. The common femoral artery varies in length between 1 and 10cm and is between usually between 8 and 10mm in diameter. Exposure of the common femoral artery is usually carried out with a vertical groin incision just medial to the midpoint of the inguinal ligament or two fingerbreadths lateral to the pubic tubercle. An oblique incision parallel to and a fingerbreadth below the inguinal ligament can also be used if a limited section of the artery needs to be exposed. Multiple small arteries, including the superficial epigastric and external pudendal arteries, and branches of the saphenous vein may be encountered in variable positions and number and may be ligated. The fascia lata is opened, and the sartorius muscle is retracted laterally to expose the femoral sheath containing the common femoral artery and vein. Cephalad exposure can be obtained by retracting the inguinal ligament or dividing it for 1 to 2cm. The deep circumflex iliac vein, which often crosses the external iliac artery just above the inguinal ligament, should be carefully identified and ligated if necessary the ligament should be reconstructed if divided. Exposure of Deep Femoral Artery the deep profunda artery dives deeper into the thigh between the pectineus and adductor longus and brevis muscles approximately 3 to 8cm from the inguinal ligament and runs closely along the medial femur. The artery arises from the common femoral artery posterolaterally As it descends along the femur, it gives off a first major branch. The sartorius, muscle acts as an important landmark to identify the zone of the deep femoral artery, similar to that of the pectoralis muscle to the axillary artery the deep femoral artery is. The deep femoral artery can be used as an outflow site in cases where the common femoral artery cannot be used due to scarring or infection in the groin. The first portion of the artery is exposed through the same incision and with a similar dissection as that described for the common femoral artery 43. Once through the fascia lata, the sartorius muscle is retracted medially and the rectus femoris is identified. The more distal deep femoral artery exposure can shorten the distance between inflow and outflow vessels, which reduces the length of conduit required. An alternative posteromedial approach has been developed to access the deep femoral artery through a more medially placed incision. Dissection is performed between the adductor longus muscle anteriorly and the adductor brevis, adductor magnus, and gracilis muscles posteriorly Once these muscles are retracted, the deep femoral artery and accompanying. As the artery passes medially with the rest of the neurovascular bundle, it becomes the popliteal artery Exposure of the. Similar to the exposure of the common femoral artery the fascia lata is incised proximally and the, sartorius muscle is retracted laterally in the proximal thigh or medially in the distal thigh. The superficial femoral vein twists around the artery and receives multiple branches as it ascends to its confluence in the groin. The saphenous nerve must be protected during dissection as it also passes through Hunter canal. Multiple branches are given off in the proximal and middle popliteal artery that supplies the surrounding muscles and knee joint. Three of these important collateral vessels, the superior, middle, and inferior genicular arteries, divide the popliteal artery into three segments to aid in choosing the optimal exposure. To isolate the proximal popliteal artery medially an incision is made along the anterior, border of the sartorius muscle. The sartorius muscle is retracted posterior and the vastus medialis muscle is the retracted anteriorly to expose a fascia to connect the adductor magnus and semimembranosus muscles together. Care must be taken to avoid injury to the saphenous vein during the skin incision and the saphenous nerve that overlies the deep fascia. The fascia is incised and the gastrocnemius muscle is retracted posteriorly and the semitendinosus, gracilis muscles, in the proximal part of the exposure, and sartorius muscle in the distal part can be retracted anteriorly If additional or wider exposure is required, the tendons of these. Within the popliteal neurovascular sheath, the vein is usually medial and encountered first. The fascia lata is incised, and the biceps femoris muscle is retracted posteriorly whereas the, vastus muscle contained by the lateral intermuscular septum is retracted anteriorly A. Of note, the tibial and peroneal nerves are avoided because they are retracted posteriorly between the biceps femoral heads. To expose the below-knee segment, an incision is made over the fibular head and the biceps femoris muscle insertion is identified. The upper third of the fibula is cleared with periosteal elevators, and the bone shaft is resected. Note the transected tendon of the biceps muscle and the intact common peroneal nerve. This approach is particularly useful in entrapment syndromes, aneurysms, reoperations, or other focal pathology 47 Patients are placed in the prone. Once the deep fascia is entered, the sural nerve is retracted laterally the tibial nerve is. The peroneal nerve can be found superiorly within the field but runs laterally along the biceps femoris insertion. Exposure is performed by making a longitudinal incision in the anterolateral aspect of the proximal leg, approximately 2cm lateral to the tibia. The muscles encountered are the anterior tibial muscle anteriorly and the extensor, hallicus longus and extensor digitorum longus muscles laterally As the plane between. In Richardson D, Polk H, Flint M, editors: Trauma: clinical care and pathophysiology, Chicago, 1987, Year Book Medical, p 544. At the ankle the artery and nerve pass medially to laterally deep to the extensor hallucis tendon and emerge between the extensor digitorum and hallicus tendons. The superior extensor retinaculum can be divided to provide additional mobility of the tendons. As the artery passes beneath the inferior extensor retinaculum, it becomes the dorsalis pedis artery. Exposure of the Posterior Tibial Artery the posterior tibial artery comes off of the tibioperoneal trunk approximately 2cm distal to the takeoff of the anterior tibial artery from the popliteal artery 48 the posterior tibial. The same incision for exposure of the distal popliteal artery can be used to expose the tibioperoneal trunk and the proximal posterior tibial artery Once the deep fascia has been incised, the gastrocnemius muscle is retracted. The artery will run between the posterior tibial and flexor digitorum longus muscles, with the tibial nerve deep to the artery. Exposure of more distal posterior tibial artery is similar with the soleus muscle released and retracted and the artery against the flexor digitorum longus muscle. In the distal third of the leg, an incision medial to the calcaneal tendon exposes the posterior tibial neurovascular bundle with the posterior tibial artery and tibial nerve between the flexor digitorum longus and flexor hallicus longus muscles. Using the same exposure for the posterior tibial artery the peroneal artery, is situated deeper along the intermuscular septum. The soleus is taken down and retracted posteriorly along with the posterior tibial neurovascular bundle. The plane of dissection is carried deeper with the peroneal artery running on the anterior surface of the flexor hallicus longus muscle, posterior to the septum.
Purchase 45 mg actos amex
The dissecting hematoma most commonly propagates distally (anterograde) diabetes diet questions and answers order actos online from canada, although proximal (retrograde) or bidirectional migration is also observed. The entry tear is most frequently located a few centimeters above the level of the aortic valve along the greater curvature of the aorta in cases of type A dissection and accounts for nearly 60% of all cases. Compared with other locations in the ascending aorta, the proximal few centimeters of the greater curvature are exposed to relatively greater hemodynamic, shear, and torsional forces. A pivot region located in the descending thoracic aorta just beyond the insertion of the ligamentum arteriosum, where the relatively mobile arch meets the fixed descending thoracic aorta, is the second most common entry site for intimal tears, which will then propagate as a type B dissection (30% of cases). The abdominal aorta is the least common site for entry (3% of cases) despite the high prevalence of intimal-medial ulcers in patients with atherosclerotic disease in this segment. By this mechanism, as many as 20% of dissections that originate in the distal arch or descending thoracic aorta may involve the ascending aorta through retrograde extension. Reentry may be protective because of spontaneous decompression of the false lumen, which, in turn, may reduce the risks of rupture and/or the development of malperfusion syndromes. Aortic Rupture and End-Organ Malperfusion Aortic rupture, defined as a tearing in the vessel wall that results in extravascular hemorrhage, most commonly occurs with trauma and aortic transection but may occur secondary to dissection. Dissection-mediated endorgan ischemia or infarction occurs from (i) mechanical compression of aortic branch vessels by false lumen hematoma, (ii) extension of the dissection plane across the ostium of the branch vessel, or (iii) dynamic vessel inlet obstruction caused by an oscillating intimal flap. Compromise of the coronary, brachiocephalic, mesenteric, renal, spinal, and iliac circulations can occur and result in a myriad of clinical presentations. False Lumen Thrombosis Thrombosis of blood within the false lumen may seal the entry tear, thus eliminating communication with the true lumen and preventing false lumen expansion. However, partial thrombosis of the false lumen has been identified as a risk factor for long-term death in patients with type B dissection. Alternatively, it has been proposed that partial thrombosis of the false lumen is associated with worse clinical outcomes via the promotion of vascular inflammation, tissue hypoxia, and/or neovascularization with weakening of adjacent vascular structures and an increased risk for aortic rupture. The term "dissecting aneurysm" is an inaccurate anachronism because these diseases are not synonymous, a distinction that is particularly important when considering their natural histories and treatments. Predisposing Genetic Factors As is true for aneurysms, any process that leads to the destruction or degeneration of the major supporting elements of the aortic media (elastin, collagen, smooth muscle cells) can predispose to the development of dissection. Although such changes predispose to aneurysm development, dissection may occur prior to significant aneurysm enlargement. In the GenTac registry of patients with a genetically associated thoracic aortic aneurysm, only 4 of the 31 patients (13%) with acute aortic dissection met criteria for intervention on predissection imaging. In (A), hematoxylin and eosin microscopic section of an aorta reveals fragmentation and loss of elastin fibers with cyst-like structures present within the media. Additional investigations have demonstrated that abnormal cell-signaling plays an important role. Notably, more than 70% of patients in both groups were also using -adrenergic receptor antagonist therapy, raising the possibility that these two complimentary therapies may be synergistically effective. Contrary to expectations, neither the 3-year primary end points (rate of change in aortic root z scores) nor secondary end points of the trial differed between treatment groups. Both strategies resulted in a decrease in the rate of aortic root growth over time. Median survival is 48 years, and the most common cause of death is arterial dissection or rupture. This phenotype is believed to be associated with weakening of the aortic wall and increased predisposition to dissection. It appears to be inherited in an autosomal dominant pattern with incomplete penetrance. Acquired Disorders There are numerous acquired disorders that contribute to aortic dissection. The incidence of aortic dissection increases with age (27 per 100,000 for 65 to 75 years old and 35 per 100,000 for 75 years old). Decreased aortic compliance and vulnerability to pulsatile forces predispose to injury and create a substrate for dissection. In one report, ambulatory blood pressure was higher in those who did not survive to hospital admission with aortic dissection. Short- and long-term outcomes following iatrogenic dissection were good, with stent implantation when a coronary artery was involved and conservative therapy in the majority of the remainder. Need for cardiac surgery was rare, with an overall low mortality and long-term complication rate. Aortic atherosclerotic plaques may prevent the longitudinal propagation of a dissection. Dissections arising from sites where the aorta has been incised or cross-clamped may occur intraoperatively or at any time following surgery. Deceleration injury from high-speed accidents results in aortic transection with false aneurysm formation and rupture, most commonly in the region of the aortic isthmus just beyond the origin of the left subclavian artery. Transection results in a transmural tear that is different both pathologically and etiologically from aortic dissection. Dissection in Pregnancy Risk of aortic dissection is fourfold higher during pregnancy but is a rare complication with an estimated incidence of 5. In many cases, pregnancy "unmasks" primary conditions that predispose to aortic dissection. Chronic amphetamine use and/or dependence appears to increase the probability of developing a thoracoabdominal aortic dissection in those aged 18 to 49 years. Current or past use of fluoroquinolones has also been associated with increased risk of aortic aneurysm or dissection. Pheochromocytoma and weight lifting (believed due to intense or repetitious Valsalva maneuvers) also predispose to aortic dissection. Clinical Presentation the most important element of any diagnostic algorithm for a suspected acute aortic syndrome is a high clinical index of suspicion, based foremost on the presenting history and physical examination (Box 32. Absent an appreciation of the cardinal features of dissection, the diagnosis can be missed in a substantial number of patients. Simple clinical prediction rules have been developed to estimate the probability of acute aortic dissection. Utilization of the risk score in two clinical centers found a sensitivity and specificity of 91% and 40%, respectively, when any one risk marker was present. History the diagnosis of aortic dissection may be missed on initial clinical evaluation in approximately one-third of cases, and an equal number are detected only at autopsy. Back pain is more common in type B dissection (occurring in 70%), although not infrequent in type A dissections (occurring in 43%). Syncope is a particularly ominous presenting symptom and may reflect cardiac tamponade from intrapericardial aortic rupture, cerebral malperfusion, and/or neurally mediated hypotension in response to the intense pain of the dissection and occurs in almost 20% of those with a type A dissection. For example, paraplegia may develop when critical impairment of flow to the anterior spinal artery, thoracic intercostals, or the artery of Adamkiewicz occurs. Abdominal pain is an underrecognized symptom of acute aortic dissection; when present, it is associated with elevated in-hospital mortality and increased frequency of malperfusion syndromes. Physical Examination Patients with acute aortic dissection appear ill, uncomfortable, and apprehensive. Hypertension is present in more than two-thirds of type B dissection patients and in approximately one-third of type A patients. Additional auscultatory findings include a soft first heart sound and a grade 1 or 2 midsystolic murmur at the base or along the left sternal border. Pulse deficits occur in 31% of patients with a type A and 19% with a type B dissection. Thus invasive intraarterial monitoring may be necessary in some aortic dissection patients. Elevation of the jugular venous pressure, especially with pulsus paradoxus, may indicate pericardial involvement with tamponade. Superior vena cava syndrome can rarely occur with compression by an expanding false aneurysm along the greater curvature of the ascending aorta. Thoracic dullness to percussion with decreased breath sounds suggests pleural effusion, which is more common in the left chest and is not necessarily indicative of rupture. In fact, pleural effusions are quite frequent with both type A and B dissections and are usually sympathetic in nature, reflective of the intense inflammation associated with the acute tear. In one study of 95 patients with acute aortic dissection, elevated levels of circulating smooth muscle myosin heavy chain protein (> 2. A recent large meta-analysis of 1557 patients found a sensitivity of 98% and negative likelihood ratio of 0. A negative D dimer used in a low-risk population had a posttest probability of acute aortic dissection of 0.
Order discount actos online
The vasculitis of systemic lupus erythematosus is believed to be due to deposition of immune complexes blood glucose vs csf glucose buy actos 15mg otc. Other vasculitic manifestations include palpable purpura and mononeuritis multiplex. Thrombotic disorders of the arterial and venous system occur in patients with lupus and appear to be related to the lupus anticoagulant, not vasculitis. Immunosuppressive therapy with cyclophosphamide has also been shown to have modest benefit in selected patients. Vasculitis Associated With Malignancy Vasculitis associated with malignancy is infrequent. More frequently vasculitides involving small vessels have been described in association, with lymphoproliferative disorders. These have primarily cutaneous manifestations and minimal visceral involvement and are often referred to as paraneoplastic vasculitides. These cases were characterized by cold-induced ischemia, which frequently led to digital artery occlusion and ischemic ulcerations. The symptoms of finger ischemia preceded the diagnosis of malignancy and several of these, patients experienced marked improvement of their hand lesions after removal of the tumor. Buerger Disease Buerger disease, also known as thromboangiitis obliterans, is a clinical syndrome characterized by the occurrence of segmental thrombotic occlusions of small- and medium-sized arteries in the lower and frequently the upper extremities, accompanied by a prominent arterial wall inflammatory cell infiltration. Affected patients are predominantly young male smokers (mean age, 34 years); they usually exhibit distal limb ischemia, frequently accompanied by localized digital gangrene. Buerger disease appears to be on the decline in North America, although there has been an increase in the incidence in women. In patients with peripheral vascular disease, the reported incidence of Buerger disease is 0. Although there have been rare, well-documented reports, both arteriographically and pathologically of iliac177, 178 and visceral artery involvement, in the overwhelming majority of patients with thromboangiitis obliterans, disease is limited to the arteries distal to the elbow and knee. In North America, approximately 50% of patients with Buerger disease have isolated lower extremity involvement, 30% to 40% have upper and lower extremity involvement, and approximately 10% have isolated upper extremity involvement. Although a strong association with tobacco use has been recognized clinically a causal relationship has not been, 175 conclusively demonstrated. Most patients are heavy cigarette smokers, although cases of Buerger disease in users of smokeless tobacco179 and cannabis180 have also been reported. An increased cellular response to tobacco antigen has been noted in patients with Buerger disease, as well as in healthy smokers compared with nonsmokers. Tobacco is currently considered at least a permissive factor and likely a causative factor. Several independent investigators have identified elevated levels of anticollagen antibodies182 and antiendothelial antibodies183 in patients with Buerger disease. Immunohistochemical analysis of the arterial wall of patients with Buerger disease demonstrates accumulation of immunoglobulins and complement in the intimal layer, with sparing of the medial and adventitial layers. In contrast to both atherosclerosis and immune arteritis, the internal elastic lamina remains intact in Buerger disease; therefore, Buerger disease is not a true vasculitis because it lacks vascular wall necrosis. Adjacent veins and nerves are frequently involved in the perivascular inflammatory process. Currently well-established diagnostic criteria exist to make the diagnosis of Buerger, disease (Box 8. Central to the diagnosis is the onset of symptoms before the age of 45 years, a uniform exposure to tobacco, and absence of arterial lesions proximal to the knee or elbow. It is essential to exclude other frequent causes of limb ischemia in young adults. In North America, atherosclerosis is much more prevalent than Buerger disease, and major atherosclerotic risk factors such as hyperlipidemia, diabetes, and hypertension must be absent. Proximal sources of emboli (cardiac, proximal arterial occlusive, or aneurysmal disease), underlying autoimmune disease, hypercoagulable states, trauma, and local lesions (popliteal entrapment, adventitial cystic disease) must also be excluded. Serologic tests for autoimmune disease and hypercoagulable states are typically negative. Similar clinical diagnostic criteria were reported by Shionoya from Japan: (1) smoking history (2) onset before the age of 50 years, (3) infrapopliteal arterial occlusion, (4) either, upper limb involvement or phlebitis migrans, and (5) absence of other atherosclerotic risk factors. After the clinical criteria have been met, objective confirmation of distal occlusive disease limited to small- and medium-sized vessels is required. This confirmation can be done with four-limb digital plethysmography distinct histopathologic findings when, available, or arteriography the arteriographic findings reveal that the extremity arteries. In the upper extremity the ulnar or, radial artery is frequently occluded, and extensive digital and palmar arterial occlusion is uniformly present. In the lower extremity the infrageniculate vessels are extensively, diseased, with diffuse plantar arterial occlusion. Digital plethysmography frequently provides especially important diagnostic information. In the typical patient with Buerger disease, obstructive arterial waveforms are present in all digits, providing objective evidence of widespread digital arterial occlusion or stenosis. Patients with unilateral digital plethysmographic abnormalities should undergo arteriography to rule out a proximal, potentially correctable arterial lesion causing the digital ischemia. In addition, patients with symptoms and objective findings localizing their disease to the distal feet and toes and who have normal hand and finger plethysmography should undergo arteriography to rule out a proximal embolic source for the ischemia. The disease typically undergoes remissions and relapses that correlate closely with the cessation and resumption of cigarette smoking with patients sustaining no further tissue loss following cessation of smoking. Proximal finger amputations are rarely required, and wrist or forearm amputations are rare. We have found thoracic sympathectomy ineffective, and we find no convincing evidence that this procedure is of any significant benefit in these patients. The course of lower extremity Buerger disease stands in marked contrast to that observed with upper extremity involvement. Ischemic rest pain can be severe, and narcotic analgesics are frequently required. Several large series reported a 12% to 31% incidence of major leg amputation over a 5- to 10-year period. If arteriography reveals a patent distal vessel and if autogenous vein is available, a distal arterial bypass may be considered. In our experience and that of others, the long-term results of reconstruction are mediocre. However, published data suggest that acceptable primary (30% to 49%) and secondary (47% to 63%) 5-year patency rates can be achieved in lower extremity bypasses, including inframalleolar bypasses, in patients with Buerger disease. A randomized European trial comparing the oral prostacyclin analog iloprost with placebo demonstrated improved pain control with iloprost, but no improvement in wound healing. This is likely due to a lack of coronary artery involvement in the disease process. These patients may possess characteristic phenotypic features, but they are often not recognized until the patient exhibits a catastrophic vascular complication. The heritable arteriopathies discussed in this chapter include Marfan syndrome, Ehlers-Danlos syndrome, Loeys-Dietz syndrome, cystic medial necrosis, and pseudoxanthoma elasticum. Arteriomegaly is also included in this section, although it is not strictly a heritable disease and there are no distinguishing phenotypic features. Marfan Syndrome Marfan syndrome is an inherited disorder of connective tissue characterized by abnormalities of the skeletal, ocular, and cardiovascular systems, with variable phenotypic expression. Classic Marfan syndrome is caused by mutations in the fibrillin gene on chromosome 15. Both a reduction in fibrillin formation and abnormalities in the fibrillin molecule have been identified. In its classic form, the syndrome is easily recognizable and consists of abnormalities of the eye (subluxation of the lens), skeleton (arachnodactyly extreme limb length, pectus, excavatum or carinatum, and joint laxity), and cardiovascular system (aortic dilation and aortic valvular incompetence). The diagnosis is established on the basis of clinical manifestations in most cases.
Discount actos 45mg on-line
Cold diabetes symptoms at night safe actos 45mg, numbness, or paresthesias of the digits often accompany the phases of pallor and cyanosis. With rewarming, digital vasospasm resolves, and blood flow dramatically increases into the dilated arterioles and capillaries. In addition to rubor and warmth, patients often experience a throbbing sensation during the hyperemic phase. Although the triphasic color response is typical of Raynaud phenomenon, some patients may develop only pallor and cyanosis. Secondary causes of Raynaud phenomenon include collagen vascular diseases, arterial occlusive disease, thoracic outlet syndrome, several neurological disorders, blood dyscrasias, trauma, and several drugs or toxins. Primary Raynaud phenomenon is common and may affect up to 8% of the general population in the United States;5 women are significantly more affected than men. Onset usually occurs before the fourth decade of life, with higher prevalence in cooler climates. Raynaud phenomenon is also known to occur in children, more often in girls than boys, and prevalence increases in age. Later, color changes may develop in additional fingers, and symptoms occur bilaterally. In about 40% of patients, Raynaud phenomenon involves the toes as well as the fingers. Episodes of Raynaud phenomenon are usually precipitated by exposure to a cool environment or by direct exposure of the extremities to low temperatures. Some patients may experience Raynaud phenomenon during either cold exposure or emotional stress; infrequently, emotional stress may be the only precipitating factor. Duration, frequency, and severity of Raynaud phenomenon increase during cold months. Multiple studies have correlated Raynaud phenomenon with vasospastic disorders, including migraine headaches,9 variant angina,10,11 and vasospasm in the kidney,12 retina,13 and pulmonary vessels. For example, metoprolol and propranolol have been successfully used to prevent migraines headaches,15 but are not beneficial in variant angina and may precipitate Raynaud phenomenon. The pulse examination is normal; radial, ulnar, and pedal pulses should be easily palpable. Trophic changes such as sclerodactyly (thickening and tightening of the digital subcutaneous tissue) occur in less than 10% of patients. The physical examination is most important to exclude secondary causes of Raynaud phenomenon. Of all the forms of Raynaud phenomenon, primary Raynaud phenomenon has the most benign prognosis. In a historical group of patients identified by Gifford and Hines20 followed for a period of 1 to 32 years (average 12 years), 16% reported worsening of their symptoms, and 38%, 36%, and 10%, respectively, reported no change, improvement, or disappearance of symptoms. Sclerodactyly or trophic changes of the digits occurred in approximately 3% of patients during follow-up, and less than 1% of patients lost part of a digit. Scleroderma pattern on nailfold capillaroscopy was the most sensitive marker of scleroderma development, while absence of anti-topoisomerase I antibodies was the most specific. It is quite likely that a variety of physiological and pathological conditions may contribute to or cause digital vasospasm (Box 46. Digital vasospasm may be due to vasoconstrictive stimuli, decreased intravascular pressure, or both. Mechanisms that contribute to exercise vasoconstriction include local vascular hypersensitivity to vasoactive stimuli. Low blood pressure, even in a healthy young person, may predispose to Raynaud phenomenon when the person encounters vasoconstrictive stimuli. Pathological conditions that may decrease intravascular pressure include arterial occlusion in proximal arteries. Normally, regulation of peripheral blood flow depends on several factors that include intrinsic vascular tone, sympathetic nervous system activity, hemorrheological properties such as blood viscosity, and various circulating hormonal substances. In contrast to other regional circulations that are supplied by both vasoconstrictor and vasodilator sympathetic fibers, the cutaneous vessels of the hands and feet are innervated only by sympathetic adrenergic vasoconstrictor fibers. In these vascular beds, neurogenic vasodilation occurs by withdrawal of a sympathetic stimulus. Cooling evokes reflex sympathetic-mediated vasoconstriction in the hands and feet via neurons originating in cutaneous receptors. Environmental cooling or cooling of specific body parts, such as the head, neck, or trunk, also causes a reduction in digital blood flow. Local digital cooling also induces vasoconstriction, independent of increased sympathetic tone. Raynaud phenomenon is not a normal physiological response but rather an episode of digital artery vasospasm causing decrease of blood flow to the digits. Vasoconstriction may be defined as the expected reduction in vessel lumen size as a result of endogenous neural, hormonal, or metabolic factors that cause smooth muscle contraction. Vasospasm implies an excessive vasoconstrictor response to stimuli that would normally cause modest smooth muscle contraction, but that instead has resulted in obliteration of the vascular lumen. Patency of the digital artery depends on a favorable balance between the contractile forces of the muscular wall of the digital artery and its intraluminal pressure. Thus, a situation in which there is excessive vasoconstrictive force or decreased intravascular pressure upsets this balance and results in vasospasm. It is with these rather simple concepts that several theories have been proposed to explain the episodic digital vasospasm that defines Raynaud phenomenon. Increased Vasoconstrictive Stimuli Several theories implicate excessive vasoconstrictive stimuli as a cause of Raynaud phenomenon. Postulated causes include local vascular hyperreactivity, increased sympathetic nervous system activity, elevated levels of vasoconstrictor hormones. Local Vascular Hyperreactivity the observation that episodic digital vasospasm occurs during cold exposure has led several investigators to consider the possibility that Raynaud phenomenon occurs as a result of a local vascular hyperreactivity. In 1929, Sir Thomas Lewis observed that following exposure of the finger to cold, vasospasm could be produced even after nerve blockade or sympathectomy. This response led these investigators to hypothesize that digital adrenoceptors were sensitized by cold exposure. Coffman and Cohen reported that systemic cooling also causes an exaggerated reduction in digital blood flow in individuals with Raynaud phenomenon compared to those without. Vasoconstriction, in response to exogenous norepinephrine, also is increased by cooling. Augmentation of adrenergic-mediated vasoconstriction by cooling occurs despite generalized depression of contractile machinery and diminished release of norepinephrine from sympathetic nerve endings in the vessel wall. The most likely hypothesis is that cold causes changes at the level of the adrenoceptor, such as an increase in the affinity for norepinephrine or greater efficacy of the agonist/receptor complex. Whereas cooling slightly depresses 1 adrenergic-mediated vasoconstriction, it markedly augments 2 adrenergic-mediated responses. Conversely, warming augments 1-adrenergic vasoconstriction and depresses 2-adrenergic vasoconstriction. It is therefore an intriguing observation by Keenan and Porter that the density of 2 adrenoreceptors is increased in platelets from patients with Raynaud disease. Whereas prazosin caused no significant change in finger blood flow or finger vascular resistance, yohimbine significantly increased finger blood flow and decreased finger vascular resistance. This study confirmed that postjunctional 2 adrenoceptors are present in human digits and play a more important role than 1-adrenoceptors in sympathetic digital vasoconstriction. Thereafter, Coffman and Cohen demonstrated that compared to normal subjects, patients with Raynaud phenomenon were hypersensitive to the vasoconstrictor effects of clonidine, an 2- adrenoceptor agonist, but not to phenylephrine, an 1adrenoceptor agonist,35 a finding confirmed by several other studies. Overall, these studies suggest that episodic digital vasospasm may be secondary to a predominance of postjunctional 2 adrenoceptors in digits of patients with either primary or secondary Raynaud phenomenon. Increased concentrations of epinephrine and norepinephrine in peripheral venous blood at the wrist were found to be higher in patients with primary Raynaud phenomenon than in normal subjects by one investigator,41 but others found normal local levels of norepinephrine in brachial arterial and venous blood samples. Central thermoregulatory control of skin temperature has also been reported to be comparable in normal individuals and patients with primary Raynaud phenomenon. Cohen and Coffman46 examined the effect of isoproterenol and propranolol on fingertip blood flow after vasoconstriction had been induced by a brachial artery infusion of norepinephrine or angiotensin, or reflexively by environmental cooling. Intraarterial isoproterenol administration increased fingertip blood flow during infusions of norepinephrine and angiotensin, but not during reflex sympathetic vasoconstriction.
Discount actos 45 mg free shipping
Endothelin receptor antagonists for pulmonary hypertension in adult patients with sickle cell disease diabetes mellitus foot care generic actos 45mg overnight delivery. Pulmonary vein stenosis complicating ablation for atrial fibrillation: clinical spectrum and interventional considerations. Rockson Abstract Diseases of the lymphatic circulation reflect either intrinsic (primary) defects or the aftermath of an acquired (secondary) disruption of lymphatic structure or function. Primary lymphatic disorders are thought to arise from faulty development of the lymphatic vasculature or from intrinsic functional derangements. Secondary lymphatic dysfunction most often occurs following disruption of lymphatic channels, typically in the setting of trauma, infection, neoplasia, or surgical interventions. Visceral lymphatic dysfunction reflects the broad constellation of developmental circulatory anomalies of the circulation that concurrently distort lymphatic anatomy, function, or both. Among these, both proliferative lymphatic vascular pathologies and lymphangiectasia figure prominently. Functional consequences include protein-losing enteropathy and chylous serous effusions in the thorax and abdomen. Keywords lymphedema; lymphangiectasia; protein-losing enteropathy; chylothorax; chylous ascites; lymphoscintigraphy; lymphangiography Diseases of the lymphatic circulation reflect either intrinsic, presumptively heritable (primary) defects or the aftermath of an acquired (secondary) disruption of lymphatic structure or function. Without regard to the mechanism, each of these disorders results in a disturbance in lymph transit. In all forms of lymphatic vascular insufficiency, interstitial fluid accumulates and regional swelling ensues when regional lymphatic flow is insufficient to maintain tissue homeostasis. When lymph stasis is chronic, there is accompanying derangement of the soft tissue histological architecture that is nearly always characterized by adipose hypertrophy within the subcutis. The presence of hydrostatic edema and tissue hypertrophy is the defining characteristic of lymphedema, the end-organ failure state of the lymphatic vasculature. Because proliferative pathology of the lymphatic vessels often produces a functionally incompetent vasculature, these conditions are also often typified by the presence of a lymphedema component. When present in the viscera, lymphatic insufficiency can also lead to profound metabolic disturbances. In addition to its role in the preservation of tissue fluid homeostasis, the lymphatic circulation is responsible for immune traffic from the peripheral tissues to the lymphoid organs. Thus, in addition to the presence of edema, lymphatic vascular dysfunction is accompanied by functional compromise of regional and systemic immune responses. Historically, the rather limited therapeutic options for lymphatic disease have reflected an incomplete understanding of the pathophysiology of lymphedema; nevertheless, recent advances in imaging and therapeutics, as well as insights gained from vascular biology, hold promise for the elaboration of more definitive therapies. Anatomy of the lymphatic circulation It was in the 17th century that Gasparo Aselli recognized the lymphatic vasculature as a distinct anatomic entity. While I was attempting this, and for that purpose had opened the abdomen and was pulling down with my hand the intestines and stomach. I suddenly beheld a great number of cords, as it were, exceedingly thin and beautifully white, scattered over the whole of the mesentery and the intestine, and starting from almost innumerable beginnings. I noticed that the nerves belonging to the intestine were distinct from these cords, and wholly unlike them, and besides, were distributed quite separately from them. When I gathered my wits together for the sake of the experiment, having laid hold of a very sharp scalpel, I pricked one of these cords and indeed one of the largest of them. I had hardly touched it, when I saw a white liquid like milk or cream forthwith gush out. Even greater resolution of the anatomy was provided by von Recklinghausen in 1862, with his discovery that the lymphatic endothelium stained darkly with silver nitrate. Using that technique, von Recklinghausen was able to differentiate lymphatic capillaries from the capillaries of the blood vascular system. Most recently, substantial advances in the techniques of immunohistochemistry and transmission electron microscopy have enabled the certain identification of the lymphatic microcirculation and its discrimination from the blood vasculature. These endothelial cells closely resemble those of blood vessels and have a common embryonic origin. They elaborate many identical histologic markers (von Willebrand factor, F-actin, fibronectin, and Weibel-Palade bodies). Unlike systemic capillaries, the basement membrane of lymphatic capillaries is absent or widely fenestrated, allowing greater entry of interstitial proteins and particles. The capillaries join to form larger vessels (100 to 200 m) that are invested with smooth muscle and are capable of intrinsic vasomotion. These vessels, in turn, merge to form larger collecting conduits composed of three distinct layers: intima, media, and adventitia. The collectors possess intraluminal valves: these, separated by millimeters to centimeters, ensure that lymph flow will be directed centrally. The medial channel originates on the dorsum of the foot and runs along the course of the saphenous vein. The lateral channel begins on the lateral aspect of the foot and ascends to the midleg, where the tributaries cross anteriorly to the medial side to follow the course of the medial lymphatics up to the inguinal nodes. Deep lymphatics do not usually communicate with the superficial system except through the popliteal and inguinal lymph nodes. The latter originate in the subcutaneous compartment, follow the course of the deep blood vessels, and eventually pass through the inguinal nodes. Small- and medium-sized lymphatic vessels empty into main channels, of which the thoracic duct is the largest. The duct, approximately 2 mm wide and 45 cm long, ascends from the abdomen through the lower chest just to the right of the vertebral column and anterior to it. At approximately the level of the fifth thoracic vertebra, it crosses to the left of the spine, where it continues to ascend through the superior mediastinum to the base of the neck and eventually empties into the left brachiocephalic vein. Other large right- and left-sided lymphatic ducts may exist, although their arrangement, size, and course are highly variable. Those vessels join with the main thoracic duct or empty directly into great veins; they provide important collateral conduits if the thoracic duct becomes obstructed. Physiology of the lymphatic circulation In 1786 William Hunter and two of his pupils, William Cruikshank and William Hewson, published the results of their work, laying the foundation for the physiology of the lymphatic system. A century later, their theories received experimental support from the physiologic studies of Karl Ludwig and Ernest Starling. Ludwig cannulated lymph vessels, collected and analyzed the lymph, and proposed that it was a filtrate of plasma. Starling elucidated the forces governing fluid transfer from the blood capillaries to the interstitial space and offered evidence that the same forces apply to the lymphatic capillaries. He proposed that an imbalance in those forces could give rise to edema formation: In health, therefore, the two processes, lymph production and absorption, are exactly proportional. Dropsy depends on a loss of balance between these two processes-on an excess of lymph-production over lymphabsorption. A scientific investigation of the causation of dropsy will therefore involve, in the first place, an examination of the factors which determine the extent of these two processes and, so far as is possible, the manner in which these processes are carried out. As first enunciated by Starling, interstitial fluid is largely an ultrafiltrate of blood. Its rate of production reflects the balance between factors that favor filtration out of capillaries (capillary hydrostatic pressure and tissue oncotic pressure) and those that favor reabsorption (interstitial hydrostatic pressure and capillary oncotic pressure). Under normal conditions, filtration exceeds reabsorption at a rate sufficient to create 2 to 4 L of interstitial fluid per day. There is a net filtration of protein (primarily albumin) from the vasculature into the interstitium; approximately 100 g of circulating protein may escape into the interstitial space daily. The interstitial fluid also receives the waste products of cellular metabolism as well as foreign matter or microbes that enter through breaks in the skin or by hematogenous routes. A more recent revisiting of the Starling relationship suggests that the accumulation of capillary filtrate in the tissue spaces is avoided mainly through lymph drainage and not, as was previously thought, through reabsorption. Entry of interstitial fluid into the lymphatic capillary is primarily governed by the prevailing interstitial fluid pressure; under steady-state conditions, this is typically subatmospheric. However, any physical force that increases interstitial fluid pressure will increase lymph flow. According to the Starling equation, increased capillary hydrostatic pressure, decreased plasma oncotic pressure, increased interstitial oncotic pressure, or increased capillary permeability can each result in an increase in tissue lymph production. Lymph flow becomes maximal when interstitial pressure is slightly higher than the atmospheric pressure. Paradoxically, the average prevailing pressure gradients do not seem to favor fluid entry into the terminal lymphatics,10 but it has been proposed that cyclical changes in the existing pressure gradients provide the dynamic force that favors fluid entry.
Buy actos cheap
Effect of beta-blockade on mortality among high-risk and low-risk patients after myocardial infarction diabetes x impotencia discount actos online visa. Comparison of transperitoneal and retroperitoneal approaches for infrarenal aortic surgery: early and late results. Transperitoneal versus retroperitoneal approach for open abdominal aortic aneurysm repair in the targeted vascular National Surgical Quality Improvement Program. Long-term safety of left renal vein division and ligation to expedite complex abdominal aortic surgery. Is it safe to ligate the left renal vein during open abdominal aortic aneurysm repair. Results of supraceliac aortic clamping in the difficult elective resection of infrarenal abdominal aortic aneurysm. Is tube repair of aortic aneurysm followed by aneurysmal change in the common iliac arteries. Dacron versus polytetrafluoroethylene for Y-aortic bifurcation grafts: a six-year prospective, randomized trial. Natural history of atherosclerotic renal artery stenosis associated with aortic disease. Simultaneous aortic and renal artery reconstruction: evolution of an eighteenyear experience. Prophylactic repair of renal artery stenosis is not justified in patients who require infrarenal aortic reconstruction. A perioperative strategy for abdominal aortic aneurysm in patients with chronic renal insufficiency. Mesenteric infarction after aortoiliac surgery on the basis of 1752 operations from the National Vascular Registry. Ischaemic disease of the colon and rectum after surgery for abdominal aortic aneurysm: a prospective study of the incidence and risk factors. Quality of life, impotence, and activity level in a randomized trial of immediate repair versus surveillance of small abdominal aortic aneurysm. Elimination of iatrogenic impotence and improvement of sexual function after aortoiliac revascularization. Prospective follow-up of sexual function after elective repair of abdominal aortic aneurysms using open and endovascular techniques. The incidence of deep venous thrombosis in patients undergoing abdominal aortic aneurysm resection. Infrarenal abdominal aortic aneurysm: factors influencing survival after operation performed over a 25-year period. Long-term survival after elective repair of infrarenal abdominal aortic aneurysm: results of a prospective multicentric study. Abdominal aortic aneurysms: survival analysis of four hundred thirty-four patients. Long term relative survival after surgery for abdominal aortic aneurysm in western Australia: population based study. Comparison of long-term survival after successful repair of ruptured and non-ruptured abdominal aortic aneurysm. Aneurysm rupture is independently associated with increased late mortality in those surviving abdominal aortic aneurysm repair. Long-term survival and late complications after repair of ruptured abdominal aortic aneurysms. Late survival in abdominal aortic aneurysm patients: the role of selective myocardial revascularization on the basis of clinical symptoms. Preoperative imaging is essential prior to any planned endovascular intervention in order to evaluate aortic anatomy, particularly aortic neck diameter and length, as well as the iliofemoral arterial system. Endografts have different features, such as profile, deliverability, and flexibility, which render them more appropriate for certain anatomies. They are generally placed via arteriotomy in the common femoral artery, although percutaneous access is growing in popularity. Some of the initial approaches involved techniques similar, in some fashion, to modern endovascular techniques. Early techniques ranged from simple aortic ligation to aortic wrapping with cellophane. In 1951, the first replacement of an aortic aneurysm with an aortic homograft was described by Dubost. Although excellent results have been obtained with conventional aneurysm repair, it remains a complex, challenging operation that initiates great physiologic stress for patients. This approach allowed for the intraluminal exclusion of an aneurysm with the placement, through the femoral arteries, of an endograft. The hope was that this would decrease the morbidity and mortality of aneurysm repair and allow repairs to be performed in patients with significant comorbidities. The original endograft was constructed of a Dacron tube sutured to a Palmaz stent. Several generations of endografts have since been developed, tested, and put into general clinical use. Our understanding of the complexities of this mode of treatment is only just being realized and examined. The classic teaching is that rupture rates for aneurysms depend on the size of the aneurysm. Rupture rates of 5% to 7% per year are estimated for aneurysms between 5 and 7 cm in diameter, and a greater than 20% rupture rate per year is estimated for larger aneurysms. It at most requires small femoral incisions instead of a large abdominal incision, which may decrease the incidence of postoperative pulmonary complications. The avoidance of extensive retroperitoneal dissection decreases the risk for perioperative bleeding. The period of aortic occlusion is minimal and accounts for the lower incidence of intraoperative hemodynamic and metabolic stress compared with patients undergoing open surgery. There are key aspects of each device and aortic anatomy to be aware of when assessing a patient as a potential candidate for endograft repair. Preprocedural imaging is paramount to properly assess the proximal and distal sites of fixation, as well as to assess the path the endograft will traverse before taking its postdeployment position. Imaging Successful endograft placement is completely dependent on adequate and accurate preoperative planning. Preprocedural imaging allows the surgeon to determine whether a patient is an acceptable candidate for endovascular aortic grafting and which device is best suited for a particular patient; this ultimately allows for determining the proper size of the endograft. Preoperative angiography is now rarely employed and reserved for cases where an adjunctive therapeutic intervention. This technique uses the spin rate of the C-arm around the gantry to acquire images. This technology appears valuable in complicated aortic cases, such as fenestrated branched endovascular aneurysm repair, due to its ability to image graft to graft and graft to aorta apposition without the use of contrast. The axial images may "cut" vessels at an angle, particularly iliac arteries that have some degree of tortuosity-thus creating an ellipse as opposed to visualization of the true lumen diameter. Due to this problem, some physicians recommend three-dimensional (3-D) image processing as a better method to evaluate aortoiliac anatomy for endograft therapy. Its usefulness, however, is often limited by availability and physician expertise. Unless the catheter remains centerline within the aorta, the images produced will be elliptical, which may also provide shorter than required length measurements. Its primary use is at the time of stent graft placement to assess graft position relative to the renal artery ostia; this can help to diminish the amount of contrast agent required. First, it is the site of proximal fixation that will prevent the device from migrating distally. Second, a circumferential seal must be obtained between the graft and the aorta in this area in order to prevent leakage of blood into the aneurysm sac. The exact length of aortic neck required is somewhat device dependent, but most commercially available devices require a 10- to 15-mm length of aortic neck below the level of the most caudal renal artery. D1 represents the diameter at the proximal aspect of the aortic neck, and D2 represents the diameter at the distal aspect of the aortic neck. The distance between D1 and D2, in general, must be 10 to 15 mm in order to adequately place an endograft. In addition, the difference between the diameter at D1 and D2 should not exceed 10%. D4 and D5 represent the diameter within the common iliac artery where the distal fixation point of the aortic endograft occurs.