Cheap 300mg allopurinol free shipping
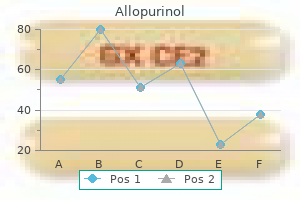
Revision surgery for pseudarthrosis is usually indicated if there are signs of neurologic deficit or if there is deformity and mechanical axial pain felt to be attributable to the nonunion gastritis thin stool allopurinol 300mg with visa. Once a complication has been encountered, rapid diagnosis and treatment are paramount in avoiding worsening neurologic function, increased morbidity, and even death. Pedicle screws can be 4 times stronger than lateral mass screws for insertion in the midcervical spine: a biomechanical study on strength of fixation. Surgical options in the treatment of subaxial cervical fractures: a retrospective cohort study. Subaxial cervical pedicle screw insertion with newly defined entry point and trajectory: accuracy evaluation in cadavers. A five-year report on a survey of the membership of the Cervical Spine Research Society by the Morbidity and Mortality Committee. Technique for drilling instrument monitoring electrical conductivity in pediatric cervical spine screw insertion: a preliminary report. Posterior cervical fixation using a new polyaxial screw and rod system: technique and surgical results. A simple technique of posterior wiring in traumatic instability of the mid to lower cervical spine. Evaluation of anatomic landmarks and safe zones for screw placement in the atlas via the posterior arch. Prior to the development and adoption of laminoplasty, multilevel laminectomy had been used extensively in the management of myelopathy caused by multilevel spondylosis, ossification of the posterior longitudinal ligament, and developmental cervical spinal stenosis. The first unilateral open-door laminoplasties in the 1980s showed the benefits of simultaneous multilevel decompression and preserved posterior musculature to prevent postoperative progression of cervical kyphosis and instability. The anterior approach is more commonly used when three or fewer levels are involved with concurrent loss of cervical lordosis in the absence of dynamic instability. A posterior approach is generally indicated when greater than three levels are involved and cervical lordosis is preserved. Prior to the advent of laminoplasty, the typical posterior management of cervical spondylotic myelopathy included the earlier-mentioned laminectomy with or without fusion. Initially, satisfactory results were found, though in recent years postoperative complications, particularly post-laminectomy cervical kyphosis, have given rise to alternative surgical approaches to posterior cervical decompression. In addition, by preserving the muscular attachments posteriorly for the paraspinal muscles, the posterior tension band is maintained, thus theoretically preventing postoperative cervical kyphosis. The ideal candidate for laminoplasty is a patient with multilevel cervical stenosis causing myelopathy, with a lordotic alignment and only a mild or secondary complaint of axial neck pain. Variations in these techniques differ largely on how the lamina is secured into its new position or how the exposure in made. Initially, the hinges were sutured or tethered with wire to surrounding tissue or propped open with bone or synthetic grafts. Recent innovations have adapted plates and screws to securely fix the lamina in place and are favored among many high-volume laminoplasty surgeons. This increases the spinal canal diameter and the hinged lamina is held open with a cortical bone graft spacer or specific laminoplasty plates. The sagittal spinous process splitting approach involves splitting the spinous processes with a high-speed burr to create two hemilaminas. Furthermore, by avoiding a bicortical trough laminectomy laterally, the risk of injury to the lateral epidural venous elements is significantly reduced. The shoulders are often taped down to allow for lateral fluoroscopic imaging of the lower cervical spine. A reverse Trendelenburg position is used to decrease venous pressure and thus blood loss. Neuromonitoring of somatosensoryevoked potentials is generally recommended and employed for cervical laminoplasty, while the routine use of motor-evoked potentials is less common. Neuromonitoring allows for immediate detection and early intervention in cases of decreased spinal cord perfusion or severe hypotension. For this reason, anesthesia providers typically use an arterial catheter for continuous blood pressure monitoring. Complications of Laminoplasty undergoing cervical spine surgery with somatosensory-evoked potential monitoring and found degradation in evoked potentials in 17 (2. Intraoperative fluoroscopy can be used to localize the landmarks for skin incision and operative dissection and is especially useful in patients whose body habitus makes palpation of physical landmarks more challenging. In both cases, the laminoplasty is opened sequentially at each level with an understanding that adequate opening and subsequent decompression often require multiple levels to be opened. The fascial closure should be watertight and the skin closed meticulously, especially in patients with redundant soft tissue. Postoperative care involves typical wound care and most importantly limited use of brace immobilization. The evidence strongly suggests that postoperative immobilization following laminoplasty increases the risk of lost motion and axial neck pain. In general, neurologic recovery is expected in the majority of patients treated with laminoplasty, with studies suggesting that approximately 80% of patients will experience some type of improvement. A mean recovery rate of 55% with a range of 20 to 80% has been reported based on Japanese Orthopaedic Association Scale used to assess for myelopathy. Yonenobu et al compared laminoplasty with multilevel anterior corpectomy and found the complication rates to be four times higher in the corpectomy group, 29 versus 7%. An extensive systematic review by Yoon et al demonstrated a diverse collection of relatively low-quality outcome data, which demonstrated a similar efficacy of both procedures in the treatment of cervical spondylotic myelopathy. When comparing the incidence of transient nerve root palsy across multiple approaches to the cervical spine, it is apparent that this complication is least likely in cases of laminoplasty. In the largest ever series of multilevel cervical decompressions Nassr et al found that the incidence of C5 motor palsy was highest with laminectomy and fusion (9. There were no residual deficits in the laminoplasty group with the highest rate of residual deficits in the laminectomy and fusion group (~ 27. Despite this atrophy, there was no correlation between the degree of atrophy and cervical curvature; therefore, it is likely that other factors such as facet joint insults are more important than atrophy of cervical musculature in producing cervical kyphosis following posterior decompression. To this end, evidence has emerged to suggest that loss of lordosis and subsequent kyphosis is in part attributable to detachment of the 11. The incidence ranges markedly from 6 to 60% and it is unclear whether this wide range of results is associated with the laminoplasty technique itself, the time at which neck pain is reported relative to surgery, or the assessment of what constitutes significant postoperative neck pain. Mochida et al reported a "spring back" rate of 40% with associated deterioration in clinical examination. Furthermore, laminoplasty plates have been developed and employed to rigidly fix the lamina in their open positions. Kimura et al described a "boomerang" deformity, where the spinal cord is compressed during posterior migration in an inadequately split lamina. The concept of a post-laminectomy membrane formation resulting in compression of neural elements and subsequent recurrence of myelopathic symptoms has been postulated and discussed for some time. Several studies refute this concept and specifically Herkowitz reported that though the post-laminectomy membrane exists in many cases, it did not compress the spinal cord or nerve roots in patients undergoing reoperation following cervical laminectomy. The ideal hinge results in a plastic "greenstick" deformation of the bone as it is opened. If a lamina hinge fracture occurs postoperatively, the failed segment may require surgical decompression depending on the presence of neurologic symptoms clinically. Wound infections following laminoplasty have been reported to be approximately 3 to 4%, which is consistent with other posterior cervical procedures. It is important to achieve a watertight fascial closure to minimize the rate of infection. Surgeons must be aware of the potential complications and management thereof with the laminoplasty procedure. Surgical treatment for ossification of the posterior longitudinal ligament of the cervical spine.
Allopurinol 300mg online
For disease in the sinonasal cavity gastritis diet ������� allopurinol 300mg lowest price, often a preauricular approach is used; this can be extended inferiorly into a cervical incision and superiorly into a hemicoronal incision. The root of the zygoma, the zygomaticofrontal suture, and the zygomaticomaxillary suture are osteotomized and the bone flap is temporarily removed if access to the infratemporal fossa is needed. Dislocation of the mandibular condyle, or occasionally a mandibulotomy, can improve visualization and access. Alternatively, an anterior facial translocation approach may be used to access the infratemporal fossa. In this approach, a Weber-Ferguson incision is extended laterally from the lateral canthus until the preauricular incision is reached. Medial Maxillectomy A medial maxillectomy can be performed either endoscopically or via an open approach for sinonasal tumors that arise from the middle meatus. After the bone has been dissected from the soft tissue, four osteotomies are performed, which are followed by three anterior to posterior osteotomies. The anterior cuts are (1) through the infraorbital rim (with preservation of the infraorbital nerve), (2) through the anterior wall of the maxillary sinus, (3) from the floor of the sinus to the piriform aperture, and (4) through the frontal process of the maxilla. Following this, the anterior to posterior osteotomies are as follows: (1) along the medial orbital floor; (2) along the floor of the lateral nasal wall; and (3) along the superior aspect of the lateral nasal wall. Once these are done, a final fourth posterior osteotomy is performed, freeing the specimen from the pterygoid plates. Infrastructural Maxillectomy When a tumor arises from the hard palate, or from the maxillary sinus, and erodes inferiorly into the oral cavity, an infrastructure maxillectomy can be used to resect the tumor. It can be performed entirely transorally, or through a lateral rhinotomy or midface degloving approach. Total Maxillectomy A total maxillectomy is typically approached through either a lateral rhinotomy or Weber-Ferguson incision. For disease involving the orbit, orbital incisions are required to include orbital exenteration. Resection of the entire orbital floor is required for suprastructural disease, in contrast to the infrastructure maxillectomy. In this procedure, the periorbita is dissected free from the medial orbital wall and the orbital floor. These osteotomies are then extended with anterior to posterior osteotomies through the medial and lateral orbital walls. Next, the floor of the orbit must be released with an osteotomy to release the superior aspect. Inferiorly, a palatal osteotomy and a lateral osteotomy through the zygomaticomaxillary buttress are made. Lastly, the specimen is released with a posterior vertical osteotomy behind the maxillary tuberosity with a curved osteotome. This anatomical region is very vascular containing the pterygoid venous plexus and the internal maxillary artery, and careful hemostasis must be achieved. The open craniofacial resection was described by Smith et al18 and popularized by Ketcham et al19 in the 1960s. A WeberFerguson or later rhinotomy approach is often used for transfacial access and a maxillectomy is performed to free the specimen from below. Alternatively, the inferior aspect can be performed endoscopically ("endoscopic assisted craniofacial resection") or the entire procedure (including superior osteotomies) can be performed endoscopically with no external cuts. Evisceration entails removing the contents of the eye (typically with a curette) and is done for severe endophthalmitis. Enucleation involves removing the globe, but the extraocular muscles and the conjunctiva are preserved. Exenteration is required for extrinsic malignant tumors with invasion of the orbit. Controversy exists as to the extent of orbital invasion requiring exenteration as some argue that invasion of the bony orbit without transgression of the soft tissues does not require an orbital exenteration, since the local control rates remain unchanged whether the eye is removed or not. To do this, a circumferential skin incision is made around the superior and inferior lid lash line. Musculocutaneous flaps are raised superiorly and inferiorly to the orbital rims, and these flaps can be re-approximated after the exenteration. When the lid skin is involved, a circumorbital incision is made around the orbital rim. The periorbita is then dissected off of the bony orbit and the skin is removed en bloc with the orbital contents. If there is concern about posterior extension, frozen section margins may be sent from the nerve at the orbital apex. Hard palate reconstruction can be performed with prosthodontics, or with autologous tissue (often free tissue transfer). Separation of the oral cavity from the nasal cavity is important for everyday functions, such as deglutition and speech. Obtaining appropriate projection of the maxilla is also very important for cosmesis. These grafts can be harvested from septal mucosa, or from the resected middle turbinate. An inlay graft of fascia, or a synthetic dural substitute, can be placed under the graft if the defect is large enough. This flap can be harvested from the sphenoid face up to the nasal sill and the inferior cut can be taken down onto the nasal floor if the defect is expected to be large. The superior cut typically should be approximately 1 cm below the skull base to preserve olfactory function. This flap should not be harvested from the septum if it is involved with disease, limiting its use in cases when the 5. Graphic image showing the various layers used in the reconstruction of an anterior skull base defect. It is often harvested using a bicoronal incision and can be used to achieve separation of the nasal cavity from the intracranial contents. An advantage of this flap includes the fact that it is outside of the treatment field, and therefore if neoadjuvant radiotherapy was used, it should be spared. In addition, because it is extranasal, there is no fear about tumor seeding with it, which can be a concern with intranasal pedicled flaps. The buccinator flap, based off of the facial artery, is another pedicled flap that can be used to close anterior defects if a pedicled flap is desired and the intranasal options are unavailable. Intracranial complications following surgery of the skull base can be devastating. An anatomical and roentgenologic study with reference to transsphenoid hypophysectomy. Outcomes and complications of endoscopic approaches for malignancies of the paranasal sinuses and anterior skull base. Comparison of transnasal endoscopic and open craniofacial resection for malignant tumors of the anterior skull base. Efficacy of transnasal endoscopic resection for malignant anterior skull-base tumors. Endoscopic endonasal management of olfactory neuroblastoma: a retrospective analysis of 10 patients with quality of life measures. Comparison of outcomes for open versus endoscopic approaches for olfactory neuroblastoma: a systematic review and individual participant data meta-analysis. Outcome results of endoscopic vs craniofacial resection of sinonasal malignancies: a systematic review and pooled-data analysis. Preservation of the eye in the treatment of sinonasal malignant neoplasms with orbital involvement. Maxillary reconstruction is complicated and there are many different classification systems and algorithms used to define the various defects. Alternatively, they may be reconstructed with a pedicled or free tissue flap with vascularized osseocutaneous or osseomyogenous flaps (such as a scapula free flap, fibular free flap, or iliac crest free flap) and subsequently be rehabilitated with a denture or implantretained prosthesis. The decision to obturate or reconstruct with a free flap depends on surgeon preference, as well as patient factors. Local complications such as bleeding may occur after maxillary surgery because of the highly vascular pterygoid plexus and due to injury of the sphenopalatine and/or internal maxillary arteries. Postoperative bleeding from maxillectomy cavities may be initially managed with packing or operative ligation of offending vessels.
| Comparative prices of Allopurinol | ||
| # | Retailer | Average price |
| 1 | Advance Auto Parts | 210 |
| 2 | Wendy's / Arby's Restaurants | 578 |
| 3 | Ross Stores | 884 |
| 4 | Tractor Supply Co. | 244 |
| 5 | Foot Locker | 550 |
| 6 | Albertsons | 102 |
Order 300 mg allopurinol overnight delivery
Transgastric or transduodenal endoscopic drainage with placement of conventional stents or lumenapposing stents is often the preferred approach gastritis stomach pain buy allopurinol 300mg otc. Diuretics, serial paracentesis or thoracentesis, and octreotide Chronic Pancreatitis 309 are also used. Many patients benefit from endoscopic placement of a stent across a disrupted pancreatic duct. Obstruction may be caused by a pseudocyst or by fibrosis and inflammation in the pancreatic head. Most patients die from an associated condition, such as complications from continued alcohol use or smoking, or from pancreatic cancer or postoperative complications. Pearls the diagnosis of chronic pancreatitis requires a high index of clinical suspicion in a patient presenting with chronic abdominal pain. Tobacco use and ongoing alcohol use predict a worse prognosis, and patients should be encouraged to stop smoking and alcohol consumption. A 55yearold man with alcoholic chronic pancreatitis presents to the emergency department with hematemesis for the past hour. His blood pressure is 92/63 mmHg, pulse rate 115 per minute, and respiratory rate 18 per minute. A 58yearold woman is referred for evaluation of a recent 30lb weight loss and abnormal liver biochemical test results. She has a known history of chronic pancreatitis related to chronic tobacco use, and she takes pancreatic enzyme replacement for malabsorption and steatorrhea. The bile duct is 7 mm in diameter compared with 5 mm on a previous imaging study 2 years earlier. Abdominal imaging shows pancreatic calcifications and a dilated pancreatic duct consistent with chronic pancreatitis. A 59yearold man with alcoholic chronic pancreatitis presents with a complaint of oily stools seven or eight times per day. B Patients with pseudocysts are at risk for having bleeding from either vessels within the pseudocyst or from pseudoaneurysm formation related to erosion of the pseudocyst into an adjacent vessel. Appropriate treatment would involve embolization of a pseudoaneurysm by interventional radiology. Splenectomy is the treatment of choice for bleeding gastric varices resulting from splenic vein thrombosis. The patient presents with weight loss and increasing dilatation of the bile duct, raising concern for possible malignancy in the head of the pancreas. C the most common form of chronic pancreatitis in southern India and other tropical areas including Africa, southeast Asia and Brazil, is tropical pancreatitis. Hereditary pancreatitis and autoimmune pancreatitis are possible diagnoses in this case, but because the patient is from southern India, tropical pancreatitis is more likely. D Patients with chronic pancreatitis may have exocrine pancreatic insufficiency, leading to malabsorption and steatorrhea. The most appropriate therapy is pancreatic enzyme replacement with coated pancreatic enzymes. He describes his stools as watery and small in volume, but denies blood in the stool. He does not take any prescription or over thecounter medications, and denies recent antibiotic use. Laboratory tests including a complete blood count, comprehensive metabolic panel, stool culture for bacteria, stool examination for ova and parasites, and stool Clostridium difficile toxin assay are negative. A capsule endoscopy shows normal small intestinal mucosa and a normal appearing ileocolonic anastomosis. Bile Bile is an alkaline, lipidrich micellar solution that is isosmotic with plasma and consists of water, electrolytes, and organic solutes such as bile acids, phospholipids. Prior to secretion into the bile canaliculi, primary bile acids are conjugated to glycine or taurine to form bile salts. Conjugation increases water solubility, preventing passive reabsorption from the small intestine. Ursodeoxycholic acid has also been used as an oral therapy to dissolve small to mediumsized cholesterol gallstones. Primary bile acids and salts reach the small intestine, where they are converted by intestinal bacteria to secondary bile acids, deoxycholic acid and lithocholic acid, through dehydroxylation. Factors that increase bile acid synthesis promote mobilization and excretion of cholesterol; factors that decrease bile acid synthesis increase the total body pool of cholesterol; factors that decrease intestinal reabsorption of bile acids increase synthesis of bile acids and therefore excretion of cholesterol. After a meal is ingested, the gallbladder contracts in response to cholecystokinin, and bile is secreted into the cystic duct, which drains into the duodenum via the bile duct. About 600 mg per day of bile acids and bile salts are not absorbed and are excreted in the stool. The majority of the bile acids are taken up by hepatocytes and secreted back into bile canaliculi. The bile acids are actively reabsorbed from the renal tubules, and less than 2% is excreted in urine. Disorders of Bile Acid Metabolism Cholesterol Gallstones (see also Chapter 21) Up to 20% of women and 8% of men over age 40 develop cholesterol gallstones. Bile Acid Metabolism 319 these stones are comprised mostly of cholesterol monohydrate. Bile pigments, proteins, calcium salts, and fatty acids make up the remainder of the stone. Pregnancy predisposes to gallstone formation because of increased cholesterol saturation during the third trimester and sluggish postprandial gallbladder contraction. Women taking oral contraceptive pills have increased hepatic uptake of dietary cholesterol, stimulation of hepatic lipoprotein receptors, and biliary cholesterol secretion, which predispose to gallstone formation. Patients who experience rapid weight loss, as occurs after gastric bypass surgery, often develop cholesterol stones secondary to increased mobilization of tissue cholesterol and increased biliary secretion of cholesterol, as well as decreased enterohepatic circulation of bile acids. Biliary sludge can also lead to gallstone formation and can be seen in conditions that cause gallbladder hypomotility such as prolonged fasting, burns, surgery, pregnancy, total parenteral nutrition, and oral contraceptive use. Pigment Gallstones (see also Chapter 21) Black pigment stones may be seen with hemolytic anemia as in sickle cell anemia, in which elevated levels of bilirubin result from an increased breakdown of red blood cells. Brown pigment stones contain calcium bilirubinate, calcium phosphate, cholesterol, and organic material and may form in the setting of biliary stasis, as occurs with a bile duct stricture. Bile acid excess Bile acid deficiency Length of resection Compensatory hepatic synthesis of bile acid Steatorrhea Response to lowfat diet Response to oral cholestyramine <100 cm Yes No No Yes 100 cm No Yes Yes No Bile Salt Diarrhea Impaired bile acid reabsorption due to surgical resection of the terminal ileum, loss of terminal ileal surface area. The nature of bile salt diarrhea and its management depend on the length of terminal ileum that is compromised (Table 20. Bile acid exposure may also increase colonic mucosal permeability and cause direct mucosal damage. However, patients may experience postcholecystectomy diarrhea if the bile acid pool size exceeds the amount of bile acid absorbed by the ileal transport system. This state is usually only transient, and patients often respond to treatment with an oral bile acid sequestrant such as cholestyramine, colestipol, or colesevelam. Small Intestinal Bacterial Overgrowth Small intestinal bacterial overgrowth can lead to deconjugation of bile acids in the proximal small intestine, thereby reducing intraluminal bile acid distribution, impairing formation of micelles, and in some cases leading to steatorrhea. Bile Acid Metabolism 321 Pearls Bile acids and salts serve as the major excretory pathway for cholesterol.
Purchase allopurinol 300mg mastercard
They are located slightly posterior and on each side of the opening of the vagina gastritis diet zone discount allopurinol 300 mg line. Each opens into the vestibule by a 2 cm duct, situated in the groove between the hymen and the labium minora. The epithelium of the Bartholin duct is cuboidal near the gland, but becomes transitional and finally stratified squamous near the opening of the duct. Perineum Perineum is the diamond-shaped region between the thighs, which corresponds to the outlet of the pelvis and presents It includes perineal pouches (superficial and deep); ischiorectal fossa; pudendal canal and anal canal. Boundaries: Anterior: Pubic symphysis, arch and the arcuate ligament Anterolateral: Ischiopubic rami Lateral: Ischial tuberosities Postero-lateral: Sacrotuberous ligaments Posterior: Tip of the coccyx Floor: Skin and fascia Roof: Pelvic diaphragm and associated fascia It is divided into an anterior urogenital triangle and a posterior anal triangle by a line drawn across the surface connecting the ischial tuberosities. Pelvis Perineal Pouches Urogenital triangle contains the superficial and deep perineal pouches (spaces): Superficial Perineal Pouch It lies between the perineal membrane (inferior fascia of the urogenital diaphragm) and the Colles fascia (membranous layer of superficial perineal fascia). It is an open compartment, due to the fact that anteriorly, the space communicates freely with the potential space lying between the superficial fascia of the anterior abdominal wall and the anterior abdominal muscles. The superficial perineal muscles are removed in the left of the diagram to show crus and bulb of the penis. The superficial perneal muscles have been removed in the left half of the diagram to show bulb of the vestibule and greater vestibular gland. Deep perineal pouch is enclosed in part by the perineum, and located superior to the perineal membrane (inferior fascia It lies between the superior and inferior fasciae of the urogenital diaphragm. Recently the deep pouch is being described as the region between the perineal membrane and pelvic diaphragm. It contains muscles like external urethral sphincter and deep transverse perinei, attaching to the perineal body. The term urogenital diaphragm should not be confused with the pelvic diaphragm (pelvic floor), which is a true diaphragm supporting the pelvic viscera. The ducts pass through the perineal membrane to reach superficial perineal pouch and open into the bulbous portion of the spongy (penile) urethra. Perineal Fascia Perineal fascia has two parts (superficial and deep) and each of these can be subdivided into superficial and deep parts. On either side it is firmly attached to the margins of the rami of the pubis and ischium, lateral to the crus penis and as far back as the tuberosity of the ischium. Posteriorly, it curves around the superficial transverse perineal muscle to join the lower margin of the perineal membrane. It emerges from the inferior side of the perineal membrane and continues along the ventral (inferior) penis without covering the scrotum. It separates the skin and subcutaneous fat from the superficial perineal pouch and covers the muscles in the pouch. It becomes continuous with the dartos tunic of the scrotum, with the superficial fascia of the penis, and with the Scarpa fascia of the anterior abdominal wall. Straddle injuries may rupture of the bulbous spongy urethra below the perineal membrane, leading to extravasation of urine into the superficial perineal pouch, which may spread inferiorly into the scrotum, anteriorly around the penis, and superiorly into the lower part of the abdominal wall. Location: It is the roof (superior boundary) of the superficial perineal pouch, and the floor (inferior boundary) of the deep perineal pouch. It is thickened anteriorly to form the transverse ligament of the perineum, which spans the subpubic angle just behind the deep dorsal vein of the penis (or clitoris). Apex is directed forward, and is separated from the arcuate pubic ligament by an oval opening for the transmission of the deep dorsal vein of the penis (or clitoris). Lateral margins are attached on either side to the inferior rami of the pubis and ischium, above the crus penis. Base is directed toward the rectum, and connected to the perineal body, posteriorly. Relations: It is continuous with the deep layer of the superficial fascia behind the superficial transverse perineal muscle, and with the inferior layer of the diaphragmatic part of the pelvic fascia. Perforations: It lies between the urogenital diaphragm and the external genitalia and is perforated by the urethra (and vagina). Arteries to the bulb, and the ducts of the bulbourethral glands pierce pass through it. It is also pierced by the deep arteries of the penis (or clitoris), one on either side close to the pubic arch and by the dorsal arteries and nerves of the penis (or clitoris) near the apex of the fascia. Its base is perforated by the perineal vessels and nerves, while between its apex and the arcuate pubic ligament the deep dorsal vein of the penis (or clitoris) passes upward into the pelvis. It is contributed by mainly two muscles: sphincter urethrae and deep transverse perinei. Perineal body is a fibromuscular body attached at the posterior border of perineal membrane in the midline. Other contents are: Crura of penis (males) / Crura of clitoris (females), bulb of penis (males) / Vestibular bulbs (females), Greater vestibular glands (female). It is a mixed (sensory and motor) nerve to supply skin and skeletal muscles of perineum. Anal Triangle and Ischiorectal Fossa Anal Triangle has two components: Muscles and Ischiorectal fossa Muscles of the Anal Triangle: External anal sphincter, Obturator internus, levator ani and coccygeus muscles. Boundaries: Anterior: Urogenital diaphragm (with perineal membrane) Posterior: Gluteus maximus (and sacrotuberous ligament) Superomedial: Sphincter ani externus and levator ani Lateral: Obturator internus muscle (with obturator fascia) on ischial tuberosity Floor: Skin Roof: Meeting point of obturator fascia (covering obturator internus) and inferior fascia of the pelvic diaphragm (covering levator ani muscle). Contents: Inferior rectal neurovascular bundle (nerve, artery and vein); fat; perineal branches of the posterior femoral cutaneous nerve, and the pudendal canal (with pudendal nerve, internal pudendal artery and vein). Note: Pudendal canal is formed either by the splitting of the obturator fascia (or by separation between the fascia lunata and the obturator fascia). Urinary Bladder and Urethra Urinary Bladder Urinary Bladder is the hollow viscus with prominent smooth muscle (detrusor) walls which is a temporary reservoir for It is situated below the peritoneum and extends upward above the pelvic brim as it fills; may reach as high as the umbilicus the empty bladder is tetrahedral-shaped and consists of a posterior surface, anterior surface, superior surface, apex, and neck. Relations: Posterior surface (Fundus or Base) Upper part is separated from rectum by the rectovesical pouch containing coils of the small intestine. Lower part is separated from rectum by the terminal parts of vas deferens and seminal vesicles. In females the base of bladder is separated from the cervix of uterus and by the vesicouterine pouch. Anterior surface is related to the pubic symphysis and retropubic space of Retzius. Superior surface is related to the peritoneal cavity (covered by peritoneum), sigmoid colon, and terminal coils of the ileum. In the female, the peritoneum is reflected posteriorly to the uterus forming the vesicouterine pouch. Apex is located posterior to the upper part of the pubic symphysis and is related to the one median umbilical ligament or urachus (a remnant of the allantois in the fetus).
Purchase allopurinol 300 mg with visa
Acalculous cholecystitis typically occurs in critically ill patients in the setting of major surgery gastritis diet green tea purchase 300 mg allopurinol, prolonged total parenteral nutrition, or extensive trauma. Clinical Features Typical symptoms include a prolonged (>3 hours) episode of biliary pain that may be associated with nausea, vomiting, and fever. Diagnosis Treatment Patients suspected of having acute cholecystitis should be admitted to the hospital, and intravascular volume and electrolytes should be repleted. A cephalosporin such as cefuroxime or ceftriaxone is effective in mild acute cholecystitis. In severely ill patients, piperacillintazobactam, a carbapenem, or a thirdgeneration cephalosporin, each in combination with metronidazole, is recommended. A prolonged (>3 hours) episode of biliary pain associated with nausea, vomiting, and fever should raise suspicion for acute cholecystitis. Diagnosis Gallstones and Complications 331 Treatment Treatment of asymptomatic choledocholithiasis is recommended due to the risk of lifethreatening complications, including acute pancreatitis and cholangitis. Laboratory tests: leukocytosis with a left shift, hyperbilirubinemia, and elevated serum alkaline phosphatase and aminotransferase levels are the typical laboratory findings. A single intravenous broadspectrum antibiotic, such as cefoxitin, is sufficient in mild cases. In severely ill patients, broadspectrum antibiotics similar to those used in acute cholecystitis are indicated. The antibiotic regimen should be adjusted if blood cultures grow the offending organism. Acute cholangitis is a lifethreatening complication of gallstones that should be identified early and treated promptly. Uncommon Gallstone Complications Gallstone Ileus Gallstone ileus is defined as smallbowel obstruction caused by a gallstone. The gallstone passes into the intestine through a cholecystoenteric fistula that forms after an episode of cholecystitis. The most common site of gallstone impaction is the terminal ileum or ileocecal valve. Many patients with gallstone ileus may have serious concomitant medical illnesses such as coronary artery disease, diabetes mellitus, or pulmonary disease. Delayed diagnosis due to the intermittency of symptoms is not uncommon and leads to a high mortality rate (50%). Gallstone ileus is diagnosed with a plain film of the abdomen: radiographic findings include pneumobilia (air in the biliary tract), dilated smallbowel loops suggestive of partial or complete smallbowel obstruction, and a stone impacted in the bowel (see Chapter 27). Diagnosis Mirizzi Syndrome Mirizzi syndrome is a rare complication of prolonged cholelithiasis. It is defined as jaundice caused by obstruction of the extrahepatic duct secondary to a gallstone impacted in the cystic duct. Porcelain Gallbladder Porcelain gallbladder is defined as intramural calcification of the gallbladder wall, and is associated with gallstones in more than 95% of cases. It is also associated with an increased risk of gallbladder carcinoma, which can occur in up to 5% of individuals. The incidence of gallbladder cancer depends on the pattern of gallbladder wall calcification, with selective mucosal calcification causing a significant cancer risk compared with diffuse intramural calcification, which does not seem to increase the risk of gallbladder cancer. Emphysematous Cholecystitis Persons with emphysematous cholecystitis have a clinical presentation similar to those with acute cholecystitis. The etiology of emphysematous cholecystitis is related to cystic duct ischemia secondary to atherosclerosis. Therefore, elderly persons (without gallstones) and persons with diabetes mellitus are at increased risk of developing emphysematous cholecystitis. Gasforming organisms infect the gallbladder wall and lead to gas pockets that are evident on abdominal imaging. Therefore, emergent treatment with broadspectrum antibiotics that include anaerobic coverage and early cholecystectomy is recommended. Gangrenous Cholecystitis Gangrenous cholecystitis is a severe form of acute cholecystitis that results in gallbladder wall necrosis and perforation. The clinical presentation is similar to that of acute nongangrenous cholecystitis; gangrene is often not suspected preoperatively. Treatment is with broadspectrum antibiotic coverage and emergent, usually open, cholecystectomy. Pearls the most common type of gallstones are cholesterol stones; women are affected much more commonly than men. Asymptomatic gallstones generally do not require treatment except in persons at high risk of gallbladder cancer. Acute cholangitis requires immediate antibiotic therapy and urgent bile duct decompression. A 92yearold woman with a history of dementia, coronary artery disease, critical aortic stenosis, and atrial fibrillation presents to the office for evaluation of a 6month history of occasional right upper quadrant pain. The pain is infrequent (every few months) and is often precipitated by a fatty meal. Laboratory tests, including a complete blood count and comprehensive metabolic panel, are normal except for a mildly elevated serum alkaline phosphatase level. Right upper quadrant ultrasonography shows cholelithiasis, with no evidence of cholecystitis, and a dilated bile duct with intraductal stones. He continues to be febrile despite treatment with broadspectrum antibiotics for 24 hours. Ultrasonography shows gallbladder wall thickening, and air in the 336 Pancreas and Biliary System gallbladder wall. Ultrasonography shows evidence of gallstones but no other abnormality; the liver size is normal. Laboratory tests including serum aminotransferase, alkaline phosphatase, and bilirubin levels are normal. Answers 1 A the patient describes symptoms consistent with biliary pain, likely from cholelithiasis. The differential diagnosis includes choledocholithiasis, cholecystitis, pancreatitis, gastroesophageal reflux disease, and peptic ulcer disease. In patients who are not surgical candidates, oral ursodeoxycholic acid can be considered for the treatment of symptomatic gallstones. Acute cholangitis is caused by a stone impacted in the bile duct, with secondary bacterial proliferation. It is likely that this patient has black pigment stones, given his history of sickle cell disease. Irrespective of the type of gallstone, the treatment of choice for acute cholangitis is broadspectrum antibiotics followed by biliary decompression. A cholecystectomy is not required urgently but should be considered once the acute cholangitis resolves. B the patient has acute cholangitis as evidenced by fever, abdominal pain, jaundice, and altered mental status. Cholangitis is a lifethreatening condition and requires urgent biliary decompression. If the patient is hemodynamically unstable, percutaneous cholecystostomy should be performed. Ultrasonography that is negative for gallstones does not alter the management of cholangitis. Antibiotic coverage should be initiated and followed immediately by a cholecystectomy. Stones in the bile duct, even if asymptomatic, should be removed because of an increased risk of complications.
Syndromes
- Excessive bleeding
- Do you usually have regular periods?
- Loss of urine without meaning to urinate
- Bluish skin color
- Imipramine, a tricyclic antidepressant, works much like the alpha-adrenergic and anticholinergic drugs
- Can dress self, only requiring assistance with laces, buttons, and other fasteners in awkward places
Cheapest allopurinol
Although erosive esophagitis is a possibility gastritis diet ���� buy generic allopurinol on-line, this patient has infrequent reflux symptoms, and erosive esophagitis is a less likely cause than pillinduced esophagitis. She describes the discomfort as a constant dull ache that usually occurs postprandially and is associated with nausea, but not vomiting. At age 40, she had a colonoscopy for rectal bleeding, which was unremarkable except for hemorrhoids. Her past medical and surgical history is unremarkable except for seasonal allergies. Physical examination reveals a blood pressure of 114/80 mmHg, pulse rate 67 per minute, and body mass index 22. The remainder of the examination, including an abdominal examination, is unremarkable. The bacterium produces urease, which breaks down urea to ammonia and carbon dioxide and is required for the survival of H. Clinical Features Typical symptoms: these occur in <20% of patients and include dyspepsia (epigastric pain, fullness, or bloating, often with nausea and eructation). When present, findings include epigastric tenderness and occult blood in the stool, or melena (black or maroon stools resulting from gastrointestinal bleeding). Peritoneal signs (rebound abdominal tenderness, guarding, and rigidity) signify a perforated ulcer, and a succussion splash is seen with partial or complete gastric outlet obstruction. The advantages and disadvantages of each test must also be taken into consideration (Table 3. Rapid urease test* Excellent sensitivity and specificity Expensive and requires infrastructure and trained personnel Inexpensive and provides rapid Sensitivity significantly reduced in the posttreatment setting results. Excellent specificity and very good sensitivity in properly selected patients Excellent specificity. Allows determination of antibiotic sensitivities Excellent sensitivity and specificity. Allows determination of antibiotic sensitivities Expensive, difficult to perform, and not widely available. Only marginal sensitivity Methodology not standardized across laboratories and not widely available 3. Unpleasantness associated with collecting stool * the sensitivity of all invasive and noninvasive tests that identify active H. The absence of chronic gastritis (inflammation) on histologic examination of a gastric mucosal biopsy specimen is good evidence of the absence of H. Either triple therapy, a fourdrug concomitant quadruple therapy, or a bismuth quadruple therapy regimen is recommended. Gastroesophageal reflux disease may increase in frequency or severity after the eradication of H. Pearls Because a small percentage of gastric ulcers are actually ulcerated gastric carcinomas, all gastric ulcers must be assessed carefully to distinguish a benign from a malignant ulcer. An upper endoscopy reveals a duodenal ulcer with active bleeding that is treated endoscopically. A 30yearold man presents to the emergency department with the sudden onset of severe abdominal pain. He states that he has been training for a marathon and has been taking ibuprofen for myalgias. Although a repeat upper endoscopy should be considered to confirm healing of a gastric ulcer and *exclude gastric cancer, it is not necessary for a duodenal ulcer. D Any of the tests listed can detect signs of a perforated ulcer (free air in the abdomen). Lopez and Edward Lin Clinical Vignette A 64yearold man with a 40 packyear smoking history presents with a complaint of severe dysphagia for solids and worsening dysphagia for liquids. If the stomach cannot serve as a conduit, a more complex colonic or jejunal interposition may be performed instead. The transhiatal approach involves an upper midline incision to create a gastric conduit and a left transverse supraclavicular or left neck incision parallel to the sternocleidomastoid to access and dissect the cervical esophagus. The gastric conduit is then delivered into the posterior mediastinum to create the esophagogastric anastomosis in the cervical region. The Ivor Lewis approach involves an upper midline incision to create a gastric conduit in a manner similar to that for the transhiatal approach, followed by a right thoracotomy to mobilize the intrathoracic esophagus for an intrathoracic anastomosis. The threehole, or McKeown, approach is carried out through separate upper midline, thoracic, and cervical incisions. This approach is thought to provide a better exposure to the surrounding structures and to decrease the risk of idiopathic injury; it also allows an extensive lymphadenectomy to be performed. Laparoscopic, thoracoscopic, and robotassisted approaches have also been employed in the hope of decreasing the morbidity of multiple incisions while replicating the results of the open approaches. A feeding jejunostomy may also be placed for adequate nutritional support during recovery. Indications Malignant neoplasms of the esophagus, including squamous cell carcinoma, adenocarcinoma, small cell carcinoma, leiomyosarcoma, rhabdomyosarcoma, fibrosarcoma, liposarcoma, lymphomas, and metastatic lesions. Rarely, neuromotor dysfunction of the esophagus such as achalasia, distal esophageal spasm, or scleroderma. Complications Early postoperative complications of an esophagectomy can involve bleeding due to inadequate hemostasis during the operation, arrhythmias, and respiratory complications such as atelectasis and pneumonia. Endoscopic examination revealing gross ischemia of the conduit requires immediate takedown of the conduit and wide drainage, with plans for a staged reconstruction. Rarely, if only a small portion of the stomach is ischemic, the ischemic portion can be resected with immediate reconstruction. A water soluble contrast study can help to identify the location and magnitude of the leak. Opening of the neck wound and daily dressing changes are usually sufficient management for leaks confined to the neck. For a leak arising from the mediastinum, exploration and drainage are often required. Common Upper Gastrointestinal Surgeries 53 Complete or Partial Fundoplication Clinical Vignette A 42yearold man complains of a persistent burning sensation in the epigastrium, acid taste in his mouth, and intermittent regurgitation. Despite a maximum dose of antisecretory medication, upper endoscopy shows Los Angeles Class B esophagitis and a small hiatal hernia (see Chapter 1). A 24hour ambulatory esophageal pH study correlates the symptoms with reflux episodes. Indications Persistent gastroesophageal reflux despite maximal medical therapy to suppress gastric acid secretion is the most common indication for a fundoplication. Large hiatal or paraesophageal hernias often require surgery to reposition the stomach back within the abdominal cavity. To prevent future herniation of the stomach into the thoracic cavity, some surgeons believe that a Common Upper Gastrointestinal Surgeries 55 fundoplication that serves as a buttress should be performed after repair of the diaphragmatic crura; however, postsurgical dysphagia may occur following a fundoplication.
300 mg allopurinol with amex
Pulmonary vasodilatation causes intrapulmonary shunting gastritis diet xyngular discount allopurinol 300mg fast delivery, leading to hyperperfusion of the lungs and reduced oxygenation of venous blood transported via the pulmonary arteries and returned to the heart. Consequently, there is rapid blood flow through the dilated pulmonary circulation that leads to inadequate oxygenation of erythrocytes and clinical hypoxia. Clinical Features Platypnea is defined as dyspnea that worsens when the patient sits upright but improves when the patient is lying down. Platypnea occurs because of orthodeoxia, or a decrease in arterial oxygen tension >4 mmHg when the patient moves from the supine to upright position because increased blood circulating at the lung bases is shunted away from alveoli. Other symptoms and signs include shortness of breath, cyanosis, digital clubbing, and hypoxia. Multiple spider telangiectasias on the face and chest may be markers of intrapulmonary vascular dilatations. Portopulmonary Hypertension Definition Pulmonary arterial hypertension in the setting of portal hypertension with elevated pulmonary resistance and a normal pulmonary artery wedge pressure. Portopulmonary hypertension is a rare but serious complication of portal hypertension that, if untreated, can result in rightsided heart failure and death. Theories include increased vascular flow causing shear stress that may trigger remodeling of the vascu lar endothelium and portosystemic shunting. A decrease in the phagocytic capacity of the cirrhotic liver may allow circulating bacteria and toxins to enter the pulmonary circulation, thereby causing cytokine release, which triggers vascular inflammatory changes. Clinical Features Dyspnea on exertion (the most common presenting symptom), orthopnea, and signs of volume overload are typical. Physical examination may reveal a loud second pulmonary valve heart sound, murmurs of tricuspid and pulmonary regurgitation, and a right ventricular heave. Diagnosis Screening with echocardiography may reveal an elevated right ventricular pressure systolic pressure or rightsided heart failure. Rightsided heart catheterization is necessary to confirm the diagnosis and determine the severity. Histopathology of the lung may show intimal fibrosis, smooth muscle hyper trophy, and characteristic plexiform lesions in small arteries and arterioles. Patients with moderate or severe portopulmonary hypertension are often placed on pharmacologic pulmonary vasodilator therapy with the primary goals of reducing the mean pulmonary artery pressure to <35 mmHg and then considering liver transplantation. Cirrhotic Cardiomyopathy Definition As cirrhosis progresses, the loss of a hyperdynamic circulation and decreased cardiac output occurs in parallel with diastolic dysfunction. Clinical Features Patients are usually asymptomatic or have mild shortness of breath or chest pain. Prognostic Scoring Systems for Cirrhosis Once complications of cirrhosis develop, mortality rates are high. Various scoring systems have been developed to determine the prognosis and the need for transplantation. Major limitations of this scoring system include the subjective evaluation of the degree of ascites and encephalopathy and the classification into just three classes. It has been modi fied by the United Network for Organ Sharing to facilitate objective alloca tion of donor organs for patients in need of liver transplantation, with the severity of liver disease guiding prioritization. Outcomes: the 5year survival rate in adults posttransplantation is approx imately 70% in the United States. All hospitalized patients with cirrhosis and ascites should undergo a diagnostic paracentesis. The patient is admitted to the hospital, and a diagnostic paracentesis is performed. B It results from increased intrahepatic resistance and an increase in portal blood flow. C It is measured by calculating the difference between the central venous pressure and the portal vein pressure. A large volume paracentesis is not necessary and can precipitate circulatory dysfunction. D Newly diagnosed ascites requires a paracentesis with ascitic fluid analysis to determine the etiology of the ascites and rule out infection. Causes of prehepatic portal hypertension, such as portal vein thrombosis, may indicate a normal sinusoidal gradient, as in this case. B Portal hypertension results from intrahepatic resistance to blood flow and increased portal venous blood inflow. Increased portal venous blood flow is caused by decreased release of nitric oxide in the intrahepatic sinusoids coupled with increased release of nitric oxide and vasodilatation in both the splanchnic and systemic circulation. Willingham Clinical Vignette A 36yearold woman presents to the emergency department with a oneday history of epigastric pain radiating to the back. Physical examination reveals a blood pressure of 144/85 mmHg, pulse rate 89 per minute, and temperature 100. Abdominal ultrasonography reveals a normal gallbladder with no wall thickening, pericholecystic fluid, or gallstones. Anatomy the pancreas is a retroperitoneal organ that lies posterior to the stomach. Tumors in the head of the pancreas may cause compression of the duodenum leading to gastric outlet obstruction. The body of the pancreas lies between the portal confluence and the abdominal aorta. Due to its proximity to the local vasculature, pancreatic adenocarcinoma frequently invades the portal vein, celiac axis, and/or superior mesenteric artery early in the course. Therefore, pancreatic cancer is often advanced and unresectable at the time of presentation. Splenic vein thrombosis can occur in patients with pancreatitis and pancreatic tumors. The uncinate process of the pancreas is tucked in posteriorly behind the superior mesenteric artery and vein. The distal portion of the bile duct runs through the pancreatic parenchyma in the head and joins with the pancreatic duct. Mass lesions in the head of the pancreas may present with painless jaundice resulting from extrinsic compression of the distal bile duct. The common channel formed by the union of the bile duct and pancreatic duct terminates at and drains through the major papilla. Gallstones that pass from the gallbladder may obstruct biliary and pancreatic outflow, resulting in elevated liver biochemical test levels and/or gallstone pancreatitis. The accessory pancreatic duct, called the duct of Santorini, drains through the minor papilla and usually communicates with the main pancreatic duct, the duct of Wirsung. The pancreatic duct is typically greatest in diameter in the head of the pancreas. The ductules drain into larger interlobular ducts, which drain into the main pancreatic duct. Enzymatic secretion is stimulated by small peptides, fat, and carbohydrate in the duodenum and is upregulated by cholecystokinin and acetylcholine. The dorsal bud grows more rapidly than the ventral bud, and forms the majority of the pancreas (the superior portion of the head, the body, and the tail). The ventral pancreas initially arises in the duodenum on the opposite side from the dorsal bud. The ventral bud rotates and fuses with the dorsal bud to become the inferior portion of the head and the uncinate process. The proximal portion of the dorsal duct becomes the duct of Santorini in most adults. The main dorsal pancreatic duct drains through the minor papilla, and the ventral duct drains separately through the major papilla. This is thought to be due to reduced outflow of pancreatic secretions through a diminutive or stenotic minor papilla.
Order allopurinol us
Injury to a dominant sigmoid sinus/jugular bulb during surgery might result in thrombosis and cerebral venous hypertension gastritis diet �� discount allopurinol online mastercard. The patient has to be well informed about the potential complications of the surgery which could be worse than nonresection. Other treatment options include radiation or surgical debulking with a planned subtotal tumor removal for any compressive symptoms. This jugular fossa meningioma mass extends inferiorly along the post-styloid parapharyngeal space and protrudes intracranially into the posterior fossa causing mass effect on the cerebellum. This can reflect a combination of reactive hyperostosis and/or tumor infiltration. The sagittal image shows the tumor tracking along the dura in the posterior fossa. Radiation is associated with long-term local tumor control without the associated morbidities of surgery. In those presenting in the subacute stage of denervation, the presence of tongue fasciculation may be a dominant symptom. There is an expansile remodeling of the right lateral clivus and the adjacent occipital bone. Axial (d), coronal (e), and sagittal (f) enhanced T1-weighted images show a heterogeneously enhancing mass. The large extracranial component extends down the right poststyloid parapharyngeal space with displacement of the internal carotid artery anteriorly. Large hypoglossal schwannomas can have sizable intracranial and extracranial components. Care should be taken when assessing for putative hypoglossal schwannoma, as asymmetric enhancement in the hypoglossal canal can be seen due to the presence of normal robust venous drainage or rarely a persistent hypoglossal artery. The rate of growth on serial scans is also important to note in those patients who are being followed up without intervention. Gradient-weighted or susceptibility-weighted imaging will show areas of internal low signal corresponding to the presence of residual bone fragments and or blood products. One should also assess for the presence of other lesions involved in the context of von HippelLindau syndrome (such as cerebellar, spinal, or retinal hemangioblastomas and choroid plexus papillomas). Intratumoral calcific spicules and posterior rim calcification are reported to be present in 100% of the cases. Foci of high signal Prognosis and Treatment If the tumor is slow growing, then watchful waiting can be adopted. If the tumor is rapidly growing, then intervention should be considered to prevent further hearing loss. Axial T1- (b), T2- (c), and postcontrast T1-weighted (d) images show a corresponding enhancing lesion causing mass effect on the adjacent cerebellum and also extending into the vicinity of the left dural sigmoid sinus. Imaging Imaging of metastatic disease can be quite variable resulting in solitary, multifocal, or diffuse disease. If the metastasis gives rise to a sclerotic bony reaction, the lesions will show very low T1 and T2 signal. Fat-saturated contrast-enhanced T1-weighted images will show an enhancing bone marrow mass with or without extraosseous soft tissue component. The location of the metastatic disease can be bony, dural based, leptomeningeal, or a combination of any of these locations. Skull base bony metastases from extracranial primaries occur in 4% of cancer patients. In children and young adults, histiocytosis and embryonal rhabdomyosarcoma also need to be considered. Of note, malignant otitis externa and primary skull base osteomyelitis can have an aggressive appearance and mimic a malignancy. Leptomeningeal carcinomatosis is the malignant infiltration of the pia, arachnoid, or both. The leptomeninges (arachnoid) extend along the cisternal and canalicular segments of the facial and vestibulocochlear nerves and metastases can seed into these locations. Intracranial metastases are becoming increasingly common as the survival rate of cancer patients is improving. There are metastatic lesions situated in the left jugular fossa and laterally in the left petrous bone (long arrow; a). There are extensive permeative erosive changes in the left petroclival junction with erosion of the left jugular tubercle and extension into the left hypoglossal canal (short arrow; b). Multilevel sclerotic metastases to the cervical and upper thoracic vertebral bodies are also present (red arrows; c). This patient initially presented with a left vocal cord paralysis of unknown cause. There is abnormal enhancement within the interhemispheric fissure (arrow; b) and circumferentially along the midbrain and basal cisterns. Pathologically, cholesterol granulomas are pseudocysts containing cholesterol crystals, inflammatory cells including macrophages, and multinucleated giant cells encased by a fibrous capsule. Cholesterol granulomas of the petrous apex are relatively aggressive lesions and are the most common primary lesion of the petrous apex accounting for approximately 60% of lesions in this location. Cholesterol granulomas occur most commonly in young to middle-aged adults without apparent sexual predilection. Two hypotheses have been put forward regarding the pathophysiology of cholesterol granulomas. The classical obstruction-vacuum Prognosis and Treatment Skull base, dural, or leptomeningeal metastases are often late events in the disease course and indicate a poor prognosis. Instead, therapy is aimed at preserving neurological function and improving or maintaining quality of life. Surgery is rarely considered only for either excisional biopsy or decompression of a tumor mass effect. In the brain, typical treatment consists of whole brain radiation, while in the spine, regions demonstrating gross disease are radiated as there is morbidity associated with bone marrow function that could preclude patients from systemic therapy. Typical doses range from 20 Gy in 5 fractions to 30 Gy in 10 fractions as a short course palliative approach. The arrow shows leptomeningeal cancer seeding into the right internal auditory canal. The hemorrhage occludes outflow resulting in trapped blood products, anaerobic metabolism into cholesterol and granulomatous reaction. As the pseudocyst expands, bone erosion continues leading to new hemorrhage and continuation of the cycle. The clinical presentation of cholesterol granulomas is variable depending on the size and local extent of the lesion. In one cohort of 90 patients with petrous apex cholesterol granulomas, the most common symptom was headache (56. Fat suppression allows distinction of the intrinsic T1 hyperintense fatty marrow within the petrous apex, from the T1 hyperintense blood degradation products of the cholesterol granuloma. There may be minimal enhancement of the fibrous capsule, but there should not be any significant internal enhancement. There are several lesions of the petrous apex that should be included in the differential diagnosis and can be distinguished from cholesterol granulomas based on imaging features (Table 3. Prognosis and Treatment Historically, asymptomatic patients were managed with primary observation and symptomatic patients were treated surgically. Given the indolent nature of many cholesterol granulomas, there is now growing support for observation in many cases, Table 3.
Generic allopurinol 300 mg visa
Patient satisfaction scores and radiographic preservation of adjacent level biomechanics were both found to be statistically superior to fusion diet gastritis erosif purchase generic allopurinol on-line. Taken together, these studies suggest that the Coflex device has similar outcomes to traditional surgical decompression with some measurable benefits over instrumented fusion for patients with stenosis also requiring surgery, at least at short-term follow-up. Similarly, a prospective study of 36 patients compared patients with lumbar stenosis treated with the Aperius device to those treated with a traditional decompression. A recent review of approximately 100,000 Medicare patients treated surgically for lumbar spinal stenosis revealed that despite being used in an older population, spacers result in less medical complications than laminectomy or fusion (1. Although some studies have suggested complication rates up to 20% with interspinous spacer insertion, in the largest randomized controlled trials the complication rates have been found to be similar to traditional surgical techniques with total complication rates at 2 years of approximately 8 to 10%. Studies have found that only approximately 17% of patients with neurogenic claudication meet these strict inclusion criteria and would be appropriate for interspinous spacer insertion. Implantation of the X-Stop device requires 11 to 150 N of force and the spinous process fractures with between 95 and 786 N of force depending on bone mineral density. Because of this potential complication, most patients undergoing interspinous spacer placement have postoperative restrictions placed on their extension range of motion. When device dislocation does occur, surgical treatment commonly includes removal of the interspinous device with revision decompression and instrumented fusion of the involved spinal segments. The repetitive compression loading of the spinous processes and preserved rotational and lateral bending motion can lead to bone erosion or heterotopic ossification. Bone erosion of the spinous processes has been reported in several patients leading to recurrent symptoms necessitating implant removal and decompressive procedures. Interspinous Spacer Complications interventions in a well-selected patient population. Spacer insertion may lead to decreased medical complications in the perioperative period, although some studies suggest increased revision rates at 2-year follow-up. Beyond the risks associated with all posterior lumbar spinal operations, interspinous spacers carry the additional risks of spinous process fracture and device displacement. Until then, they remain a viable option in treatment of lumbar spinal stenosis with similar expected outcomes to traditional surgical interventions. Interspinous spacers compared with decompression or fusion for lumbar stenosis: complications and repeat operations in the Medicare population. Analysis of complications in patients treated with the X-Stop Interspinous Process Decompression System: proposal for a novel anatomic scoring system for patient selection and review of the literature. Dynamic interspinous process stabilization: review of complications associated with the X-Stop device. Erosion of the spinous process: a potential cause of interspinous process spacer failure. Heterotopic ossification in vertebral interlaminar/interspinous instrumentation: report of a case. Longer term follow-up will reveal any effect on adjacent level disease formation and the survivorship of the implants themselves. The mechanism of decompression of these devices vary, with some allowing for direct decompression, and providing some degree of interlaminar stabilization. Although interspinous spacers minimize traditional surgical risks through less invasive and shorter surgeries, they carry unique risks including spinous process fracture and implant migration. Lumbar interspinous spacers: a systematic review of clinical and biomechanical evidence. The effects of an interspinous implant on the kinematics of the instrumented and adjacent levels in the lumbar spine. This approach utilizes the collection of loose connective tissue anterior to the sacrum. This space has been referred to as the retrorectal space, but in recent years it is more commonly termed the presacral space. When combined with a posterior stabilization procedure (which can be performed percutaneously), advocates of this approach have suggested that the initial stability achieved surpasses the traditional constructs because the surrounding stabilizing structures of the motion segment are left undisturbed. The sacrum and rectum are separated by the mesorectum, a layer of adipose tissue containing blood vessels, lymphatics, and rectal lymph nodes. The smaller width in females was suggested to be because of the volume occupied by the uterus. Dixon reported that men have more fat within the abdominal cavity, possibly accounting for the larger width of the presacral space. Parke, upon anatomic study, found the middle sacral artery to be only a minor contributor to significant segmental arteries, through bilateral segmental branches. At the lumbosacral junction, the total distance between the left common iliac vein and the right common iliac artery measured an average of 33. This was treated by an emergent diverting ileostomy and 6 weeks of intravenous antibiotics, followed by later reversal. The rectal injury was detected intraoperatively and a general surgeon was consulted who identified two rectal perforations by intraoperative colonoscopy. Whereas no residual of the rectal injury occurred, the patient ultimately went on to develop a painful pseudoarthrosis and underwent a subsequent posterior fusion with iliac fixation. Gram-negative, in addition to standard gram-positive coverage, should also be considered for prophylactic antibiotics. A small skin incision (2 cm) is made just lateral to the sacrococcygeal junction below the paracoccygeal notch. After division of the subcutaneous tissues, the presacral space is accessed in a retroperitoneal manner by puncturing the anorectal fascia/ligament. Finger dissection in the presacral space anterior to the coccyx and lower sacrum mobilizes the retroperitoneal fat anteriorly. A blunt introducer assembly is then slowly advanced along the anterior midline of the sacrum under frequent biplanar fluoroscopic control. The threaded dowel (TranS1 screw) is then inserted axially across the disc space to provide anterior column support and maintain or restore disc height. Implants with differential thread counts on each end can be used to distract the disc space using a reverse Herbert screw effect. Pelvic Hematoma Given the anatomic considerations described above, significant blood loss is not typically associated with the presacral approach. They felt that bleeding observed during their presacral procedure was typically bony bleeding from the intraosseous tunnel drilled. Such an injury is more likely to occur if the presacral space is inadequately developed. In one case, the patient became tachycardic postoperatively, and required transfusion of packed red blood cells totaling 5 units given over the first four postoperative days. These authors speculated that the hematomas were a result of injury to presacral or middle sacral vasculature, although the precise etiologies were never determined. They offered that those patients might have benefitted from the application of hemostatic agents in the presacral space and at the opening of the intraosseous tunnel through the sacrum. It is important to entertain these possibilities, however, if such a procedure is being considered for an outpatient or surgery center setting. Careful attention to preoperative preparation with isolation of the anus out of the prepared field, along with a meticulous closure, seems paramount to minimize the frequency of such events. Lindley reported two cases of sacral fracture in their series of 68 cases for a rate of approximately 3%. The other patient was treated with long iliac bolts that stabilized the sacral fracture and led to resolution of associated L5 nerve root pain. The authors observed that some patients have quite large ventral S1 foramina; therefore, great effort should be taken to obtain a starting point as close to the midline as possible. Moreover, the disc heights at 24 months were noted diminished compared to the Wound Infection the close proximity of the skin incision to the anus might suggest that the presacral technique might have a high rate of postoperative contamination and subsequent wound infection. Two of the relatively large series, however, did not report any wound infections in their experiences involving 26 and 27 patients, respectively. Two of the four cases were successfully treated with empiric antibiotics (ertapenem or moxifloxacin). All of the cases in this series responded well to treatment with no infectious sequelae.
Allopurinol 300mg generic
The body has a groove on its posterior surface for the flexor hallucis longus tendon gastritis diet 3 day buy allopurinol 300mg free shipping. Talar neck fracture causes avascular necrosis of the body of the talus, because most of the blood supply to the talus passes through the talar neck. It forms the heel of the foot, articulates with the talus superiorly and the cuboid anteriorly, and provides an attachment It shows a shelf like medial projection called the sustentaculum tali, which supports the head of the talus (with the spring ligament). Sustentaculum Tali the upper surface of this process assists in the formation of talocalcaneonavicular joint. The groove on the lower surface is occupied by the tendon of flexor hallucis longus and the margins of groove give the medial margin provides attachment to Spring ligament anteriorly. Flexor digitorum accessorius (Medial head) is attached distal to the groove for flexor hallucis longus. Navicular is a boat-shaped tarsal bone lying between the head of the talus and the three cuneiform bones. Cuboid is the most laterally placed tarsal bone and has a groove for the peroneus longus muscle tendon. Cuneiform bones are three wedge-shaped bones that form a part of the medial longitudinal and proximal transverse arches. They articulate with the navicular bone posteriorly and with three metatarsals anteriorly. Metatarsus consists of five metatarsals and has prominent medial and lateral sesamoid bones on the first metatarsal. Phalanges consists of 14 bones (two in the first digit and three in each of the others). This tendon also passes deep to the flexor retinaculum along with the other long muscles of the posterior leg - Tibialis posterior and Flexor digitorum longus, which insert into the sole bones. Joints Functionally, there are three compound joints in the foot: Clinical subtalar joint between the talus and the calcaneus, where inversion and eversion occur about an oblique axis. Transverse tarsal joint, where the midfoot and forefoot rotate as a unit on the hindfoot around a longitudinal axis, augmenting inversion and eversion Remaining joints of the foot, which allow the pedal platform (foot) to form dynamic longitudinal and transverse arches. Table 27: Joints of foot Joint Subtalar (talocalcaneal, anatomical subtalar joint) Type Articulating Surfaces Joint capsule Fibrous layer of joint capsule is attached to margins of articular surfaces Ligaments Medial, lateral, and posterior talocalcaneal ligaments support capsule; interosseous talocalcaneal ligament binds bones together Plantar calcaneonavicular (spring) ligament supports head of talus Movements Blood supply Nerve supply Talocalcaneonavicular Plane Inferior surface synovial joint of body of talus (posterior calcaneal articular facet) articulates with superior surface (posterior talar articular surface) of calcaneus Synovial joint Heads of talus Talonavicular articulates with calcaneus and part is ball and socket navicular bones type Inversion and Posterior eversion of foot tibial and fibular anteries Joint capsule incompletely encloses joint Gliding and rotatory movements possible Anterior tibial artery via lateral trasal artery, a branch of dorsalis pedis artery (dorsal artery of foot) Plantar aspect: medial or lateral plantar nerve 977 Self Assessment and Review of Anatomy Articulating Surfaces Blood supply Nerve supply Dorsal aspect: deep fibular nerve Joint Calcaneocuboid Type Joint capsule Ligaments Dorsal calcaneocuboid ligament, plantar calcaneocuboid, and long plantar ligaments support joint capsule Dorsal and plantar cuneonavicular ligaments Dorsal, plantar, and interosseous tarsometatarsal ligaments bind bones together Dorsal, plantar, and interosseous intermetatarsal ligaments bind lateral four metatarsal bones together Collateral ligaments support capsule on each side; plantar ligament supports plantar part of capsule Collateral and plantar ligaments support joints Movements Inversion and eversion of foot; circumduction Plane Anterior end Fibrous capsule synovial joint of calcaneus encloses joint articulates with posterior surface of cuboid Cuneonavicular joint Tarsometatarsal Anterior navicular articulates with posterior surfaces of cuneiforms Anterior tarsal bones articulate with bases of meatatarsal bones Common capsule encloses joints Separate joint capsules enclose each joint Little movement occurs Gliding or sliding Deep fibular: medial and lateral plantar nerves: sural nerve Intermetatarsal Plane Bases of metatarsal Separate synovial joint bones articulate joint capsules with each other enclose each joint Little individual Lateral movement metatarsal occurs artery (a branch of dorsalis pedis artery) Flexion, extension, and some abduction, adduction, and circumduction Digital Flexion and branches of extension plantar arch Digital nerves Metatarsophalangeal Condyloid Heads of synovial joint metatarsal bones articulate with bases of proximal phalanges Hinge Head of one synovial joint phalanx articulates with base of one distal to it Interphalangeal Subtalar (Talocalcaneal) Joints There are two joints between the talus and calcaneum: Posterior talocalcaneal joint and anterior talocalcaneonavicular joint. It is formed between the concave facet on the inferior surface of the body of talus and convex facet on the middle one-third of the superior surface of the calcaneum. Ligaments Lateral & medial talocalcaneal ligaments, interosseous talocalcaneal ligament, cervical ligament. Interosseous talocalcaneal ligament is the chief bond of union between the talus and calcaneum, occupies sinus tarsi and separates the talocalcaneal joint from the talocalcaneonavicular joint. It extends upward from upper surface of the calcaneum to the tubercle on the inferolateral aspect of the neck of talus. The round head of the talus fits into the socket formed by the calcaneum, navicular, and spring ligament. It is a compound articulation consisting of anterior talocalcaneal and talonavicular joints. Lower Limb Ligaments: Spring ligament, Medial limb (calcaneonavicular part) of bifurcate ligament. Spring ligament (plantar calcaneonavicular ligament) extends from the anterior margin of the sustentaculum tali to the plantar surface of navicular bone between its tuberosity and articular margin. Spring ligament is made up of two distinct structures: the superomedial calcaneonavicular portion and the inferolateral calcaneonavicular portion. The dorsal surface of the superomedial calcaneonavicular portion has a triangular fibrocartilaginous facet on which part of the talar headrests. Its plantar surface is supported medially by the tendon of tibialis posterior and laterally by the tendons of flexors hallucis longus and digitorum longus; its medial border is blended with the anterior superficial fibres of the medial (deltoid) ligament. Transection of the spring ligament leads to instability of the hindfoot, including talar head plantar flexion and adduction, consistent with pes planovalgus (adult acquired flatfoot) deformity. Ligaments: Lateral limb (calcaneocuboid part) of bifurcate ligament, Long plantar ligament, Short plantar ligament. Its medial limb (calcaneonavicular part) is attached to the dorsolateral surface of the navicular bone and its lateral limb (calcaneocuboid part) to the dorsomedial surface of the cuboid bone. Long planar ligament extends from triangular plantar surface of the calcaneum to the lips of the groove on cuboid and beyond it to the bases of the middle three metatarsals (second to fourth). It converts the groove on the plantar surface of cuboid into a tunnel for the passage of tendon of peroneus longus. Eversion: Lateral border of the foot is raised so that the sole faces outside (laterally). Other involved joints are transverse tarsal/midtarsal joints (calcaneocuboid & talonavicular). Axis of Movements the movements of inversion and eversion take place around an oblique axis which runs forward, upward, and medially passing from the back of calcaneum through the sinus tarsi to emerge at the superomedial aspect of the neck of talus. Tarsometatarsal Joint (Lisfranc Joint) is the articulation of the tarsal bones with the metatarsals. Arterial Supply Dorsalis pedis artery lies between the extensor hallucis longus and extensor digitorum longus tendons midway between the medial and lateral malleolus, where the dorsal pedal pulse can be palpated. Arcuate artery runs laterally across the bases of the lateral four metatarsals and gives rise to the second, third, and fourth dorsal metatarsal arteries. First dorsal metatarsal artery Deep plantar artery enters the sole of the foot and joins the lateral plantar artery to form the plantar arch. The sole of the foot receives blood from the medial and lateral plantar arteries derived from the posterior tibial artery. Nerves Table 28: Nerves of foot Nervea Saphenous Origin Femoral nerve Course Arises in femoral triangle and descends through thigh and leg: accompanies great saphenous vein anterior to medial malleolus: ends on medial side of foot Pierces deep fascia in distal third of leg to become cutaneous; then sends branches to foot and digits Passes deep to extensor retinaculum to enter dorsum of foot Larger terminal branch of tibial nerve Passes distally in foot between abductor hallucis and flexor digitorum brevis; divides into muscular and cutaneous branches Passes laterally in foot between quadratus plantae and flexor digitorum brevis muscles; divides into superficial and deep branches Distribution in Foot Supplies skin on medial side or foot as far anteriorly as head of 1st metatarsal Superficial fibular Common fibular nerve Deep fibular Medial plantar Supplies skin on dorsum of foot and all digits, except lateral side of 5th and adjoining sides of the 1st and 2nd digits Supplies extensor digitorum brevis and skin on contiguous sides of 1st and 2nd digits Supplies skin of medial side of sole of foot and sides of first three digits; also supplies abductor hallucis, flexor digitorum brevis, flexor hallucis brevis, and first lumbrical Supplies quadratus plantae, abductor digiti minimi, digital minim brevis; deep branch supplies plantar and dorsal interossei, lateral three lumbricals, and adductor hallucis; supplies skin on sole lateral to a line splitting 4th digit Lateral aspect of hindfoot and midfoot Lateral plantar Smaller terminal branch of tibial nerve Sural Usually arises from branches of both tibial and common fibular nerves Tibial and sural nerves Passes inferior to the lateral malleolus to lateral side of foot Pass from distal part of the posterior aspect of leg to skin on heel Calcaneal branches Skin of heel Cutaneous Innervation of Foot Peroneal nerve has 2 branches: superficial and deep. The area over the great saphenous vein is supplied by the branches of femoral nerve, mainly the medial cutaneous branch of thigh and the saphenous nerve in the leg. Altered sensation over the area of great saphenous vein in leg may occur secondary to damaged saphenous nerve, as Tibial nerve supplies the sensations over the back of the leg and the sole of the foot. Sural nerve is a branch of tibial nerve and runs along the short saphenous vein and supplies the dorsum of foot along its lateral border (including the little toe). Lateral longitudinal arch is contributed by the calcaneus, the cuboid bone, and the lateral two metatarsal bones. It is supported by the peroneus longus tendon and the long and short plantar ligaments. Medial longitudinal arch is contributed and maintained by the of the talus, calcaneus, navicular, cuneiform, and three medial metatarsal bones. The keystone is the head of the talus, which is located at the summit between the sustentaculum tali and the navicular bone. It is supported by the spring ligament and the tendon of the flexor hallucis longus. Flat foot (pes planus or talipes planus) is a condition of disappearance or collapse of the medial longitudinal arch with eversion and abduction of the forefoot and leads to pain as a result of stretching of the plantar muscles and straining of the spring ligament and the long and short plantar ligaments. Transverse arches: Proximal (metatarsal) arch is formed by the navicular bone, the three cuneiform bones, the cuboid bone, and the bases of the five metatarsal bones of the foot.