Cheap minocycline 50mg line
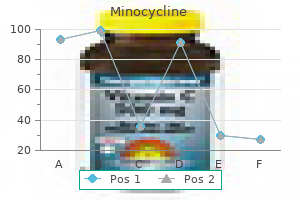
Large multilamellar droplets are emulsified further by bile salts to the mixed micelle antibiotics for uti uk purchase minocycline online from canada. Mixed micelles and unilamellar vesicles can be absorbed from the intestinal lumen. Bile salts are reabsorbed in the terminal ileum and undergo enterohepatic circulation. The prevertebral sympathetic ganglia integrate the peripheral reflex pathways and preganglionic sympathetic fibers from the spinal cord. Brain centers supply sympathetic and parasympathetic outflow to the gut via the autonomic nervous system, and the gut sends sympathetic and parasympathetic outflow to the central nervous system. Neural control of the stomach involves vagal reflexes responsible for passive relaxation (allows food bolus to enter) and regulation of lower esophageal sphincter tone (prevents reflux). In the stomach and small and large intestine, pacemaker activity within the muscle layers controls rhythmic, phasic contractions. Retropulsion is the expulsion of noxious substances from the small intestine back into the stomach followed by vomiting. Nerve fibers from sympathetic nervous system innervate gut lymphoid tissue and control inflammatory and anti-inflammatory functions. Inflammatory signals stimulate vagal afferents, which feed into brain nuclei and return efferent signals back to the gut via the vagus, releasing acetylcholine, which inhibits macrophage activity and cytokine release. These mechanisms maintain the beneficial interaction between normal bacterial flora, the gut epithelium, and its immune function. Oxygen diffusion is flow rated, and as flow increases, more oxygen is delivered to the distal villi. Prostaglandins are locally produced and vasodilate during low-flow states and after mucosal injury. The degree of hyperemia varies with nutritional content, and fat induces the highest blood flow. During circulatory shock, splanchnic vasoconstriction preserves cardiac output and gut epithelium can become hypoxic. Restoration of blood flow generates oxygen radicals and intestinal reperfusion injury. Tachyphylaxis occurs in 60% of patients after 7 days, due to downregulation of motilin receptors. Nutrition provided to the gut protects the mucosal barrier and delivers nutrients critical for immune function. Protein calorie malnutrition is associated with leukotriene reduction and impaired microbial ingestion and killing. Targets for specific nutritional manipulation include the mucosal barrier, cellular immunity, and the inflammatory response. The mucous coat acts as a filter, allows small nutrients to pass, and blocks large molecules (antigens, pathogens). The cell surface is a barrier; microvilli density, rhythmic movement, and negative charge repel macromolecules, antigens, and microorganisms. Disease processes that result in altered charge, decreased microvilli number, or microvilli atrophy increase susceptibility to disease and infiltration by antigens and microorganisms. Antigens pass into the enterocyte and are either taken up via endocytosis and degraded by lysosomes (major pathway), or pass through the cell untouched into the systemic circulation (minor pathway). During infection and inflammation, costimulatory cytokine production in conjunction with antigen presentation by the enterocyte on its cell surface generates a significant immune response. Neither conclusive benefit nor adverse outcome of glutamine supplementation during critical illness has been shown. Arginine, a precursor for multiple proteins and signaling molecules, can enter the body as arginine or as citrulline. Clinical trials studying oral citrulline in children who underwent cardiopulmonary bypass and were at risk to develop pulmonary hypertension showed promising results. Nucleotide biosynthesis is severely impaired during catabolic stress or protein malnutrition. Rapidly dividing cells are the most sensitive to this loss, and immune cells are exceptionally susceptible. Leucine promotes protein synthesis and inhibits protein degradation via a leucinespecific signaling of the mechanistic target for rapamycin. A clear position on the effectiveness and safety of immuno-enhanced diets for both children and adults has yet to be determined. Probiotics are live microorganisms that confer a health benefit by maintaining or repopulating a damaged microbiome. Theories for this conferred cytoprotection include enhanced intestinal barrier function, improved mucus production, and upregulation of protective cytokines and innate and cellular immune responses. Large-scale, well-designed trials are needed to determine the future of probiotic use in critically ill individuals. The basal metabolic rate is the energy expended at rest in a neutral temperature under fasting conditions (12-hour fast). For any of the calculations, a large variation between individuals should be considered when their measured energy expenditure is compared to the calculated amount. Large variations in critically ill children lead to inaccurate predictions using these equations. To improve accuracy, infused feeds should be constant for 12 hours and intermittent feeds held for 4 hours, ventilator settings must remain constant for 6 hours, and no procedures (including dialysis) performed for 2 hours before testing. Recommendations for protein and energy requirements in healthy individuals are (requirements in critically ill children are varied): Infants 2. It is imperative to provide adequate carbohydrate calories to minimize autocatabolism. Glucose is the preferred energy substrate for the brain, red blood cells, and renal medulla. Without 738 adequate carbohydrate replacement, catabolism of the diaphragm and intercostal muscles additionally compromises respiratory function in an already ill child. The glycerol released is converted to pyruvate and shuttled into glucose metabolism as a gluconeogenic precursor. Unlike fat, the body has no storage depots of protein; 98% of the amino acids are incorporated in proteins. Protein recycling represents the major pathway for amino acid/protein utilization. Children should receive a maximum of 30% of total calories from fat and no more than 10% of calories from saturated or unsaturated fats. Micronutrients Micronutrients are classified as vitamins (A [retinol], B1 [thiamin], B2 [riboflavin], B3 [niacin], B5 [pantothenic acid], B6 [pyridoxine], B7 [biotin], B9 [folate], B12 [cobalamin or cyanocobalamin], C, D, E [tocopherol], and K), trace elements/minerals (zinc, iron, copper, selenium, fluoride, iodine, chromium, molybdenum, cobalt, and manganese), and amino acids (glutamine, arginine, homocysteine). Vitamin A deficiency leads to decreased retinal function and is the leading cause of blindness in developing nations. A deficiency of B1 results in dry beriberi (characterized by peripheral neuropathy), wet beriberi (characterized by neurologic and cardiovascular abnormalities-congestive heart failure), and cerebral beriberi (Wernicke 739 disease). Thiamine disease is associated with inadequate intake (malnutrition) and alcoholism or loss (hemodialysis). The cardiac disease is somewhat reversible, while the neurologic injury remains fixed.
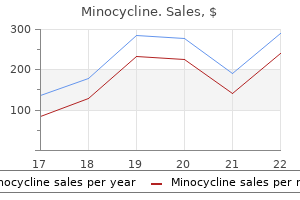
Minocycline 50 mg visa
In children <9 years antimicrobial medication generic minocycline 50mg line, spinal injuries are more frequent in the atlas, axis, and upper cervical vertebrae. Spinal Cord Injury without Radiographic Abnormality the anatomic characteristics of the young child. The clinical features range from tingling dysesthesias or numbness to frank weakness or paralysis. The preferred application of painful stimuli is the medial side of the arms or legs; this will help to differentiate a localization of pain response from abnormal flexor or extensor posturing. Phase 1: Prehospital Care Basic life support involves a rapid primary survey to identify and quickly treat lifethreatening injuries. The protection of the cervical spine, correction of airway obstruction, and general cardiopulmonary resuscitation take precedence. Intracranial hypertension with impending herniation is inferred from the presence of dilated, unresponsive pupils or a triad of systemic hypertension, bradycardia, and an abnormal breathing pattern. Lidocaine pretreatment can attenuate the laryngeal reflex and sympathetic response. Intubation should be accompanied by in-line stabilization of the neck by an assistant or use of a cervical collar. Trauma patients may have delayed gastric emptying, and large-bore suction devices should be available. Injury above the upper thoracic spine levels may lead to loss of sympathetic tone and hypotension without a compensatory increase in heart rate. Abnormal carotid neck pulses, bruits, and Horner syndrome indicate traumatic carotid dissection. The neck should be immobilized in an appropriate-size collar, and manipulation should be kept to a minimum. Lower cervical injury may spare the diaphragm but abolishes accessory muscle strength, decreases vital capacity, and causes retention of secretions. With injuries at T11, respiratory function, vital capacity, and cough can be normal. Unilateral or bilateral dilation that is unresponsive is an indication for emergent hyperventilation, brain imaging, and potential surgical intervention. Unilateral pupil dilation unreactive to direct stimulation but consensually reactive is caused by absent light perception in that eye or a deafferentated pupil. Injury to the midbrain tectum may result in pupils that are at midposition and fixed to light but retain hippus, the ciliospinal reflex, and response to accommodation. Injury to different portions of the brain leads to distinctive abnormal breathing patterns 393 that may help localize the area of injury. B: Hyperventilation, or tachypnea, indicates damage in the rostral brainstem or tegmentum. C: Apneustic breathing or prolonged sustained end-inspiratory pauses indicate damage at the midpontine or caudal pontine level. D: Cluster breathing (periodic respirations that are irregular in amplitude) indicates lower pontine or high medullary injury. E: Ataxic respiration (completely random and irregular breathing) indicates medullary damage. Patterns must be assessed as unilateral, bilateral, spontaneous, or occurring only after stimulation. Appropriate localizing and flexor responses in a comatose patient imply that sensory pathways are functioning and that the pyramidal tract from the cerebral cortex to effector is functioning, at least partially. Unilateral absence of responses is consistent with an interruption of the corticospinal tract. Decorticate rigidity is flexion of the arms, wrist, and fingers, with adduction in the upper extremity and extension, internal rotation, and plantar flexion in the lower extremity. This motor pattern occurs if the impairment of brainstem activity is located above the level of the red nucleus, as seen with lesions involving the corticospinal pathways at the internal capsule, cerebral hemisphere, or rostral cerebral peduncle. Decerebrate rigidity consists of opisthotonus with the teeth clenched, the arms extended, adducted and hyperpronated, and the legs extended with the feet plantar flexed. Functional Integrity of the Spine and Spinal Cord the patient should be log-rolled (with the head kept in-line) to examine the entire spine. The functional integrity of the spinal cord is evaluated by a thorough motor and sensory examination. Complete injury is signified by loss of motor function, segmental reflexes, and sensation below a given level. The zone of partial preservation is an area adjacent to the neurologic level in which abnormal sensory and motor findings are noted. An area of abnormal findings that is not contiguous with the postulated level qualifies as incomplete injury. Flaccid areflexic paralysis and anesthesia to all modalities characterize spinal shock. Imaging of the spine should be obtained in all patients with pain or tenderness of the neck or back, sensory or motor deficits, an impaired level of consciousness, or with painful, distracting injuries outside of the spinal region. The standard practice for cervical radiographs includes anteroposterior, lateral, and odontoid views. Lateral views should be screened for changes in vertebral alignment, bony structure, intervertebral space, and soft tissue. In the conscious child, immobilization can be discontinued when the pain has resolved and flexion and extension radiographs reveal no apparent injury. In adult patients, 60 mm Hg is often targeted but goals may be individualized based on cerebral oxygenation and autoregulation. Other "first-tier" therapies include elevation of the head 30 degrees and keeping the head midline (reducing obstruction to cerebral venous return). Hypertonic saline (typically 3%) may be better tolerated than mannitol can precipitate renal failure. Mannitol causes an immediate viscosity-reduction or pressure-mediated reflex vasoconstriction and a late osmotic effect to shift water out of brain tissue, but osmotic diuresis can lead to hypotension and hyponatremia. About 3% hypertonic saline may be better tolerated than mannitol, since sodium loading increases intravascular volume as opposed to diuresis and dehydration. Starting treatment with 3% hypertonic saline to gain acute control may avoid hypoperfusion when volume status is low. Phase 5: Therapies for Refractory Intracranial Hypertension Second Tier: Surgical Options Surgical therapy may be required acutely to evacuate a mass lesion or as treatment for intracranial hypertension refractory to medical therapy. Third Tier: Other Medical Therapies Third-tier medical measures include the use of barbiturate-induced coma, hypothermia, and hyperventilation. The most common complication of barbiturate treatment is hemodynamic compromise and hypotension. Recent analysis raises concern for increased mortality with hypothermia but still suggested that hyperthermia be avoided. Generally, earlier in the course of therapy, such management is avoided unless there is a temporizing treatment before emergency surgery. Early seizures occur within 7 days and late seizures occur after 7 days following injury. The significance of subclinical seizures and the importance of early treatment are not understood. Irrespective of cause, hyperthermia must be controlled, as it may worsen neurologic outcome. Growth-hormone, gonadal, and thyroid assessment is not necessary in the acute phase. Since 1998, concerns have been raised about the studies supporting steroid use and the increased incidence of infection and avascular necrosis with steroid treatment. Prior terms used to describe the constellation of abusive injuries include "shaken baby syndrome," "inflicted traumatic brain injury," "inflicted childhood neurotrauma," "nonaccidental traumatic brain injury," and "intentional traumatic brain injury.
Diseases
- Waardenburg syndrome type 2
- Pontoneocerebellar Hypoplasia
- Booth Haworth Dilling syndrome
- Radius absent anogenital anomalies
- Hypotelorism cleft palate hypospadias
- Kearns Sayre syndrome
- Post-partum depression
- Proliferating trichilemmal cyst
Purchase minocycline no prescription
If abnormal antibiotics for acne how long to take cheap 50 mg minocycline overnight delivery, and motor neuropathy is suspected, the tongue should be sampled next by the submental route. Abnormal results will indicate that the motor neuronopathy is generalized rather than due to segmental spinal cord involvement. M-wave: Excitement is conducted along motor neuron from stimulus to recording at muscle fiber (orthodromic); M-wave increases as stimulus increases. F-wave: Excitement is conducted along motor neuron from stimulus to nerve body (antidromic) before returning along the motor neuron to the muscle fiber (orthodromic); F-wave increases slightly as stimulus increases. H-wave: Excitement 300 is conducted along the sensory neuron to the motor neuron (antidromic), and then travels down motor neuron to muscle (orthodromic); H-wave decreases as stimulus increases. It is common for sensory nerve fibers to be affected due to associated dorsal root ganglionopathy, which makes distinction from early neuropathy difficult. Reinnervated motor units (an expected feature of anterior horn cell disease) may not have developed. Fibrillation potentials are regarded as an important sign, but can be seen in other conditions. Affected babies usually have intrauterine growth retardation and present at 3 months of age with respiratory compromise. Investigation shows an abnormality of the diaphragm, often unilateral and suggestive of a diaphragmatic eventration. It is not unusual for the infant to have surgery that reveals a very thin diaphragm and then be unable to wean from the ventilator. Widespread denervation in the diaphragm, often with no abnormality in the intercostal muscles (found during passage through the chest wall), is pathognomonic. Response may be missed because the recording is not long enough to allow the long distal motor latency to be captured. Because affected patients continue to produce the fetal form of the acetylcholine receptor (containing a gamma subunit), the weakness is less profound. Rapsyn (receptor-associated proteins of the synapse) mutations may also be associated with apnea. Nemaline rod myopathy and minitubular (centronuclear) myopathy are among the few myopathies that are sufficiently devastating to require ventilatory support from birth. Historically, poliovirus was the most common infection causing anterior horn cell disease. These children present with gastrointestinal or respiratory illness preceding an ascending weakness and neuropathic pain. Infantile botulism is due to colonization of the intestine and production of toxin by Clostridium botulinum. Infantile botulism is most common in specific regions possibly related to climatic environments that support spore development or construction work causing spores to be airborne. These children may also be born with arthrogryposis, and the mother will have had a succession of miscarriages. The diagnosis is often delayed; this is a rare disorder and testing for acetylcholine receptor antibodies looks for those against the adult, not the fetal, form. The neuropathy is usually an axonal neuropathy, with the motor nerve affected more than the sensory. Studies of the nerves notice the differences in the evoked responses from the muscle according to whether you stimulate the nerve or the muscle itself. Other studies include those looking at muscle fiber conduction velocity or at muscle fiber excitability. Compound muscle action potentials from the tibialis anterior muscle of a patient with critical illness neuropathy (left) and critical illness myopathy (right). Note the higher amplitude with direct muscle stimulation compared with nerve stimulation in the patient with critical illness neuropathy, whereas there is little difference in amplitude between direct muscle and nerve stimulation in the patient with critical illness myopathy. The lower limb nerves seem more susceptible to injury, and in particular the sciatic nerve. The neurophysiologic findings of sciatic nerve palsy require the demonstration of abnormalities in the peroneal and the tibial elements of the nerve. Recovery 304 from sciatic nerve palsies can be poor because of the long distance for the nerve to regrow. Neuromuscular weakness manifests as rapid shallow breathing from decreased tidal volume and minute ventilation. An ineffective cough results in retention and aspiration of secretions and microatelectasis. Lack 306 of muscle tone also results in unopposed recoil pressure of the lung that results in decreased functional residual capacity and impaired gas exchange. Weakness of oropharyngeal muscles causes choking, slurred speech, dysphonia, difficulty clearing secretions, or aspiration. Patients may have shortness of breath at rest or on exertion, or nonspecific symptoms such as restlessness, difficulty sleeping, or fatigue. Early morning headache, daytime somnolence, and poor school performance suggest nocturnal hypoventilation. Patients with an intact diaphragm but weak intercostal and abdominal muscles may develop respiratory distress while upright. Paradoxical breathing occurs when, during inspiration, the chest wall is pulled inward due to weak intercostal muscles while the abdomen expands outward as the diaphragm contracts downward (a rocking motion of chest and abdomen). Spirometry A single-breath counting test may be used to follow progression of weakness. In children older than 5 years, spirometry is used to monitor progression of weakness. Maximum inspiratory pressure is measured at residual volume, and maximum expiratory pressure is measured at total lung capacity. Life-threatening respiratory failure occurs when vital capacity drops below 20 mL/kg or 30% of predicted values. Tracheostomy Advantages of early tracheostomy include increased comfort, airway safety, and easier weaning from ventilation. Some disease-specific data suggest that children are less likely to require tracheostomy than are adults. General Supportive Care General care should prevent complications from immobilization and includes physiotherapy, splints to prevent contractures, prevention of deep vein thrombosis, and careful positioning and repositioning. In patients with facial nerve palsy, eye care prevents desiccation and corneal injury. It can occur at any age (incidence increases with age), in any race, and in all climates. An infectious illness in the month preceding the onset of neurologic symptoms is present in 70% of cases. The Miller Fisher variant is characterized by a triad of ophthalmoplegia, ataxia, and areflexia. Molecular similarity of myelin and ganglioside antigens to constituents of the infecting organism results in a hyperimmune response. Demyelinating lesions occur along the entire peripheral nerve including the nerve roots. Dysautonomia, including dizziness, hypertension, excessive sweating, and tachycardia, can occur. The symptoms progress for a median of 7 days and plateau for a variable period and then improvement begins. The signs of autonomic dysfunction are sinus tachycardia, bradycardia, or hypertension. Severely affected patients have arrhythmias and changes in vasomotor tone that manifest as hypotension and blood pressure lability. Loss of vasoregulation is associated with exaggerated hemodynamic responses to drugs and anesthetics. Hyponatremia and excess antidiuretic hormone may be caused by hypovolemia, hypotension, or positivepressure ventilation.
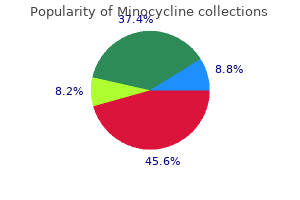
Cheap 50mg minocycline visa
Many patients make a full clinical and radiologic recovery after conservative measures virus 24 purchase 50 mg minocycline amex, including slow reduction of blood pressure and maintenance of normal oxygenation. Diabetes and inborn errors of metabolism can cause acute focal neurologic symptoms and signs (metabolic stroke) due to either vascular injury or direct tissue injury, which may be permanent or transitory. Metabolic diseases associated with stroke include homocystinuria, Fabry disease, Menkes disease, organic acidemias, and urea cycle disorders. The concepts of "brain attack" and the management of acute stroke in stroke centers have received widespread publicity. In contrast, in many children, the correct diagnosis is not made for days or weeks. Children may present with status epilepticus resistant to first-line therapy, with a reduced level of consciousness, with signs of intracranial hypertension or imminent central or uncal herniation. The head of the bed should be flat; this maneuver optimizes perfusion to the brain but risks aspiration in those with nausea and vomiting and compromised airway protection. Additional tests include an electrocardiogram, arterial blood gas, serum electrolytes, renal function tests, liver function tests, a complete blood count including platelets, toxicology studies, and clotting studies (prothrombin time, international normalized ratio, and activated partial thromboplastin time). The Four Targets of Early "Ischemic Stroke" Care the four targets for ischemic stroke care include acute therapy to optimize neurologic status, etiologic workup for secondary prevention, prevention of neurologic deterioration or medical complications, and recovery and rehabilitation. Optimizing the Neurologic Status In instances where there is no hemorrhage, emergency therapy focuses on reestablishing blood flow. A hypertensive patient may be "autoregulating" at a new set-point for blood pressure and regional cerebral blood flow. However, emergency control of hypertension is required when there is evidence of hypertensive end-organ damage. Anticoagulation is required for cardiac embolic disease, documented large artery occlusive clot. The major concern and risk is hemorrhagic transformation in the evolution of a large infarct. The use of anticoagulation in patients with cardiac disease is more controversial and influenced by the cardiac pathology and by neurologic and imaging findings. It is important that the vascular pathology is defined so that conditions requiring urgent management. Conventional angiography is required to diagnose small-vessel vasculitis, cortical venous thrombosis, and, sometimes, dissection, particularly in the posterior circulation. Clinical trials of decompressive craniectomy for adults with malignant ischemic stroke have shown increased survival and improved functional outcome when surgery is performed within 48 hours of stroke onset. Reports in children suggest that good outcome is possible even in the presence of signs of herniation. The main priorities are to prevent cerebral herniation if the blood collection is space-occupying, reverse coagulopathy, exclude sinovenous thrombosis, and to treat vasospasm with volume expansion. Although less common, aneurysms are associated with a significant rebleeding risk, particularly soon after presentation. A vascular team should evaluate these children so that an individualized management strategy, targeted at preventing recurrence, can be implemented. Additional risks include hydrocephalus (with resultant impaired cerebral perfusion) and hematoma enlargement with deterioration or herniation. Consideration should be given to the effects of bed position on hemodynamics, oxygenation, and neurologic status. If neurologic findings worsen with elevation of the head, the patient should remain flat. In cases of cerebellar or posterior fossa hemorrhage, the indications for surgery include a displaced fourth ventricle, early obstructive hydrocephalus, compression of the brain stem, and decreased level of consciousness. In cases of supratentorial hemorrhage, the indications for surgery include location close to the brain surface, hematoma volume >20 mL, and decreased level of consciousness. Primary prevention of stroke is possible if these children are screened appropriately and transfused indefinitely. If available, exchange transfusion (using a manual regime or erythrocytapheresis) is recommended over simple transfusion. Parenchymal cells (neurons, astrocytes, oligodendrocytes, or microglia) do not tolerate prolonged durations of ischemia. Neuronal and glial cell death can result from necrotic, apoptotic, and autophagic pathways. Necrosis is characterized by mitochondrial energy failure leading to cellular swelling, loss of membrane integrity, and an inflammatory response in surrounding tissues. Autophagy is an adaptive response to starvation, and results in autodigestion of cellular proteins and organelles to feed the cell. The degree of brain injury and outcome correlate with the duration of the no-flow state. Cardiac Arrest Mortality after cardiac arrest is very high, and despite the plasticity of the developing brain, neurologic outcomes can be dismal. Poor outcomes may be related to the hypoxemia and hypoperfusion prior to no-flow ischemia seen during asphyxial cardiac arrest. The need for three or more doses of epinephrine or >30 minutes of resuscitation is associated with poor neurologic outcome. Patients with witnessed cardiac arrest have better outcomes than those with unwitnessed cardiac arrest. Survival rate to hospital discharge is higher for in-hospital versus out-of-hospital cardiac arrest patients, with 65% of survivors having good neurologic outcome. At a microscopic level, there are areas of "no-reflow" interspersed with areas of restored blood flow and microinfarcts. Brain regions that are selectively vulnerable include the thalamus, amygdala, hippocampus, and striatum. It is hypothesized that vasospasm, perivascular edema, and increased blood viscosity play a role in the development of this "no-reflow" phenomenon. This hyperemic phase may be essential for neuronal functional recovery, and postarrest hypotension worsens neurologic outcome. The duration and degree of delayed hypoperfusion is associated with impairment of functional recovery, especially if not matched by a lower metabolic rate. Nonoxidative or anaerobic cerebral metabolism adds an additional level of complexity. Extreme hyperventilation and hypocarbia could exacerbate hypoperfusion, and should be avoided in the early postresuscitation period. Controversy surrounds the target PaO2 during resuscitation and the postresuscitation period; supplementary oxygen may increase oxidative stress on reperfusion. It is logical to target normocarbia and normoxia in patients during and after cardiac arrest. The relationship between pressure autoregulation and outcome is not clear in infants and children. Oxygen stores are depleted ~20 seconds after cardiac arrest, and there is loss of consciousness. This is a period when the brain is at risk of secondary injury, and may represent a therapeutic target. Pathobiology after Reperfusion Reperfusion and restoration of oxygen delivery to injured brain leads to increases in free radicals, and initiation of redox-sensitive cell-signaling pathways. Unique aspects in cellular energy metabolism and connectivity play a role in this susceptibility, since these regions do not have especially vulnerable microcirculatory patterns. Time to initiation of resuscitative efforts can strongly impact survival and neurologic outcome. Establishment of an airway for ventilation and oxygenation is imperative to the pediatric population, since most pediatric arrests have an asphyxial etiology.
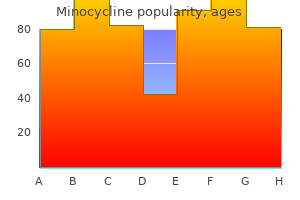
Discount 50 mg minocycline otc
Superior Constrictor the muscle fibers originate from four sites: (1) the ptery goid hamulus recommended antibiotics for sinus infection cheap minocycline 50 mg with amex, (2) the pterygomandibular raphe (from Table 2. Site Base of skull and superior constrictor muscle of the pharynx Structures traversing the space Auditory tube Levator veli palatini muscle (soft palate muscle) Ascending pharyngeal artery (branch off the external carotid artery) Ascending palatine artery Tonsillar artery (off the ascending palatine artery, off the external carotid artery) Stylohyoid ligament (from styloid process to hyoid bone) Stylopharyngeus muscle inserting into thyroid lamina Glossopharyngeal nerve along the posterior part of the pharyngeal wall Superior laryngeal artery (off the superior thyroid artery, off the external carotid artery) and vein Internal laryngeal artery (off the superior laryngeal nerve, off the vagus nerve) Inferior laryngeal artery (off the thyrocervical truck, off the subclavian artery) and vein Recurrent laryngeal nerve (off the vagus nerve) Superior and middle constrictor muscles Middle and inferior constrictor muscles Below the inferior constrictor muscle of the stylopharyngeus muscle to go downward to its attachment on the pharynx as well as the styloglossus muscle and the lingual and glosspharyngeal nerves to go forward toward their destinations on the tongue. The Longitudinal Muscles There are three longitudinal muscles that enable dilata tion and elevation of the pharynx. Palatopharyngeus: Palatopharyngeus has two heads-the anterior and posterior heads-and thus two origins from the back of the hard palate and the palatine aponeuro sis. An arch is formed by the downward angulation of the two heads and they fuse and form the palatophayngeus muscle that, covered by mucosa, travels behind the pala tine tonsil. This muscle not only raises the palatopharyn geal fold that forms the posterior arch of the fauces, but it also inserts into the back part of the thyroid lamina, blending together at this point with stylopharyngeus and salpingopharyngeus. Palatopharyngeus has a twofold action: it elevates the larynx and the pharynx and makes the oral surface of the palate more concave with its arch. Salpingopharyngeus: this narrow trumpetshaped muscle arises at the inferior cartilaginous margin of the phar yngotympanic/auditory tube and blends inferiorly with the palatopharyngeus muscle to insert into the posterior border of the thyroid lamina. It raises the larynx and the pharynx during swallowing and draws up the pharyngeal walls. In addition, during swallowing, it opens the orifice to the pharyngotympanic tube and thus allows for pres sure equalization in the middle ear. Stylopharyngeus: As its name implies, this muscle takes its origin from the styloid process on the skull base and passes obliquely across the superior constrictor and into the middle constrictor to its final destination on the thyroid lamina. Inferior Constrictor the inferior constrictor fibers originate from two main sites: (1) the oblique line of the thyroid lamina and (2) the lateral aspect of the cricoid cartilage and, in essence, is a fusion of two muscles, thyropharyngeus and cricopharyn geus. These parts are named based on their origins of the thyroid and cricoid cartilages. In a similar fashion to the fibers of the superior and middle constrictor, the fibers of thyropharyngeus muscle angle medially and backward and fuse at the pharyngeal raphe on the posterior aspect of the pharynx. Its upper fibers overlap with the middle constrictor muscle as they ascend upward. However, the cricopharyngeus muscle forms a continuous band from one side of the cricoid round to the other side, enclosing the pharynx. This lowest part of the pharynx thus has no midline raphe, is continuous with the muscle fibers of the esophagus, and, instead, has a sphincteric function at this part of the pharynx. There is an important difference with the upper eso phageal sphincter, in that its upper border lies inside the inferior border of the inferior constrictor, unlike the infe rior constrictor that overlaps the middle constrictor, and the middle constrictor in turn overlapping the superior constrictor. Chapter 2: Clinical Anatomy of the Pharynx and Esophagus Stylopharyngeus raises the larynx and pharynx and dilates the pharynx during swallowing. The main blood supply is from the ascending pharyngeal and palatine arteries, the tonsil lar artery (a branch off the facial artery), the lingual artery, two branches of the maxillary artery (greater palatine and pharyngeal arteries), as well as the supe rior laryngeal artery and the inferior laryngeal artery, which is a branch of the thyrocervical trunk in the root of the neck. Venous Drainage the venous drainage of the phaynx is predominantly via the pharyngeal venous plexus situated on the posterior aspect of the pharynx and from there into the internal jugular vein. However, it also has connections to the pterygoid venous plexus located on the pteryoid muscles in the infratemporal fossa of the face. Sensation to the orophar ynx is predominantly off the glossopharyngeal nerve, although the valleculae are supplied by the internal laryn geal nerve (a branch off the superior laryngeal nerve, which is off the vagus). The tonsils are supplied by the glossopharyngeal nerve as well as by a branch off the maxillary division of the trigeminal nerve, the lesser pala tine nerve. Nerves Virtually all of the motor supply to the pharynx is via the pharyngeal plexus, a network of nerves from the vagus nerve and the cranial part of accessory nerve and the glossopharyngeal nerve overlying the middle constric tor on the posterolateral pharyngeal wall. However, the recurrent laryngeal nerve and the external laryngeal nerve (a branch off the superior laryngeal nerve), both of which are branches of the vagus nerve, supply the lowest part of the pharynx, the cri copharyngeus muscle. Like the rest of the alimentary tract, the esophagus consists of two spirally arranged layers of mus cle, a longitudinal outer layer and a circular inner layer, both of which facilitate peristalsis. Where Nasopharynx Auditory tube What Spread of infection Blocked ears Why Connection between the nasopharynx and middle ear. This connection is the reason why an ear infection commonly complicates a throat infection. When inflamed, predominantly in children, adenoids can lead to snoring and sleep apnea, as they can almost completely fill the nasopharynx. Can cause mouth-breathing, blockage of the auditory tube, deafness, and middle ear infection. Although the tonsil has a plexiform venous drainage system around the tonsillar hemicapsule, the main culprit in a posttonsillectomy bleed is generally the paratonsillar vein (or external palatine vein) within the capsule. The glossopharyngeal nerve also supplies the middle ear (the tympanic branch) and thus pain can be referred to the ear during an episode of tonsillitis. Drainage is via an incision in the softest region or the prominent part of the abscess. Small foreign bodies can lodge here in the vallecula, typically breadcrumbs or fish bones, and cause a bout of coughing. It is also a site where malignancies may grow to a substantial size asymptomatically, at which point they present with metastatic cervical lymphadenopathy. As the lower part of the pharynx is circular and sphincteric, it remains closed most of the time. To overcome this, it helps to get the patient to swallow to allow relaxation of the sphincter momentarily. Behind the cricoid cartilage, the inferiormost pharyngeal sphincter muscle-cricopharyngeus-is pre dominantly closed, briefly opening only on swallowing or to allow vomitus to be expelled. This is the site of the first of three anatomical constrictions within the esophagus. The mediastinal or thoracic part of the esophagus (from suprasternal notch to diaphragm) passes through the posterior mediastinum, behind the pericardial sac, to reach the diaphragm, and enters the abdominal cavity through the diaphragmatic hiatus at the level of the tenth thoracic vertebra, the site of the third anatomical constriction. Anterior to the esophagus in this region are the trachea and the left main bronchus and posterior to it are the descending aorta (close to the diaphragm only), the thoracic duct, and the azygos vein. Divisions For descriptive purposes, the esophagus is divided into three parts: (1) cervical, (2) mediastinal/thoracic, and (3) abdominal (or the upper, middle, and lower parts)-the upper two of which are striated muscle and the lower is smooth muscle. The overlying mucous membrane also has three components: epithelium, lamina propria (a con nective tissue layer), and muscularis mucosae (smooth muscle), which is at its thickest in the esophagus despite being present throughout the alimentary tract. Cervical Esophagus In the cervical region (from cricopharyngeus to supra sternal notch), the esophagus travels posterior to the trachea and thyroid gland and anterior to the verte bral column surrounded by prevertebral fascia. In this region, at the esophageal inlet, it is continuous with the laryngopharynx. In close proximity, on either side, are the abdominal esophagus (diaphragm to the cardiac por tion of the stomach) is relatively short, between 1 and 2cm long, and lies below the diaphragm between the third anatomical constriction and the gastroesophageal junction (or cardiac orifice), the site at which the esopha gus meets the stomach. Below the esophageal hiatus, the abdominal esophagus runs forward and to the left, leav ing a groove on the left liver lobe as it travels forward. This same peritoneum, on the right side, forms the highest part of the lesser omentum and, on the left side, forms the highest part of the greater omentum. Several factors prevent reflux of gastric contents from the stomach back into the esophagus. For instance, the lower 3 cm of the esophagus is a highpressure zone and contents are prevented from going backward due to this. Positive intraabdominal pressure on this part of the esophagus has a similar effect. Additionally, the slinglike fibers from the right diaphragmatic crus contract to pre vent reflux, and the acute angle at which the esophagus meets the stomach physically impedes reflux of gastric contents. Sympathetic innervation is from the greater and lesser splanchnic nerves, which travel lateral to the esophagus plastered against the posterior thoracic wall. The cervical portion is supplied by the inferior thyroid artery, the thoracic portion by branches off the thoracic aorta (bronchial and esophageal branches), and the abdominal portion by the inferior phrenic artery and the left gastric artery. The venous drainage of the esophagus has signifi cant clinical relevance as it forms one of the few portal systemic anastomoses within the body, more commonly encountered in the diseased state. Where Cervical (upper) esophagus "from cricopharyngeus to suprasternal notch" Outside lumen of esophagus What is to a submucosal plexus from where the blood drains to a periesophageal plexus. The segmental drainage from esophageal veins arising from this plexus mimics the arte rial supply. The thoracic esophagus, at its distal parts, drains into the azygos venous system (azygos, hemiazy gos, intercostal, and bronchial veins), while the abdomi nal esophagus drains into the hepatic portal venous system, via the left gastric vein. Lymphatics Lymph drainage from the esophagus is extensive and predominantly via the left gastric and celiac nodes. Why the close proximity of the recurrent laryngeal nerve to this part of the esophagus means that malignancies here can impinge on the nerve causing symptoms in the larynx and present with dysphagia and hoarse voice.
Syndromes
- Severe change in pH (too much or too little acid in the blood, which leads to damage in all of the body organs)
- Birth control pills
- Never try to clean the ear by putting any object, such as a Q-tip, into the ear canal.
- If the bleeding is severe, get medical help and take steps to prevent shock. Keep the injured body part completely still. Lay the person flat, raise the feet about 12 inches, and cover the person with a coat or blanket. DO NOT move the person if there has been a head, neck, back, or leg injury, as doing so may make the injury worse. Get medical help as soon as possible.
- Grunting and snorting
- Shortness of breath
Order minocycline 50mg amex
In the past antibiotics making me tired buy minocycline 50 mg with visa, all patients were treated at least initially by a conservation approach (medially-nonsurgical) with sialagogues, massage, heat, fluids, and antibiotics. If a stone can be identified by palpation in the floor of mouth, a transoral slitting of the submandibular duct over the calculus with submandibular gland excision can be an alternative. Performing such intraoral surgery is difficult, and failure to extract the stone is the main problem. If no computed tomography scan is done, then possible second or multiple stones may be missed. Duct stenosis from scarring, with obstruction and recurrence of symptoms, is a risk. Pediatric: Pediatric sialolithiasis is said to represent only 3% of all sialolithiasis (Patel and Karlis, 2009). The duration of symptoms is much shorter than in adults, with diagnosis and treatment being made within 1 year of the onset of obstructive symptoms. In a review of 29 pediatric patients (aged <18 years) over a 10-year period with sialolithiasis from South Korea (Chung, et al. In the adult group, the calculi were in the distal duct and in the proximal duct in 44. The postoperative complications, one developed a ranula formation, and others had a transient lingual dysesthesia, temporary mandibular branch of the facial nerve weakness. They report that <120 pediatric sialolithiasis cases have been reported (Chung, et al. Because of the location of the stones in the pediatric patients, the associated risks of recurrence, and complications associated with open surgery, the role of sialoendoscopy has been reported in a small number of cases. The authors conclude that interventional sialoendoscopy allows early treatment of pediatric sialolithiasis and stenosis in most cases, and can avoid classical open surgery (Faute, et al. In the past, it was considered to be associated with dehydration in early postoperative elderly patients. Eighty per cent (80%) of submandibular stones are radiopaque, suggesting that after performing an occlusal X-ray of the floor of mouth to confirm a likely obstructing ductal stone. The treatment of each case will commence with rehydration, with adequate analgesia and empiric oral or intravenous antibiotics. In the absence of confirmation of stone obstruction etiology, a conservative approach should be followed, and only if there develops an abscess should incision and drainage be performed (Patel and Karlis, 2009). The use of sialography may demonstrate evidence of terminal ductal sialectasis or ductal stenosis, with decreased gland emptying rates suggestive of poor gland function. Ultimately if after several episodes the gland will remain swollen, occasionally painful and the patient may request local excision (Carlson, 2009). A) the importance of a computed tomography scan in detecting a smaller, secondary stone. Mycobacteria infection either typical or atypical forms specifically affecting the submandibular triangle are exceedingly rare, and even if they do, they infect the surrounding lymph nodes rather than the salivary tissue itself. Radioiodineinduced obstructive sialadenitis: Recently it has been recognized that sialadenitis can present in a group of patients who have been treated with radioactive iodine for well differentiated thyroid cancer (Dingle, et al. The typical sialoendoscopic findings reported included pale ductal mucosa, thick mucus plugs, ductal debris, and duct stenosis. Complete 174 Section 1: Head and Neck resolution of symptoms can be achieved in >50% of patients by repeated sialendoscopy with duct irrigation, an improvement reported in an additional 35% of patients and in a few other patients after failed symptom improvement after repeated sialoendoscopic procedures, volunteered for a parotidectomy (Prendes, Orloff and Eisele, 2012). Significance of unilateral submandibular gland excision on salivary flow in non-cancer patients. Salivary morbidity and quality of life following radioactive iodine for well-differentiated thyroid cancer. Impact of submandibular gland excision on salivary gland function in head and neck cancer patients. The changes in submandibular gland size and function following chorda tympani section. Over the past 20 years, the introduction of new diagnostic tools and imaging techniques has substantially improved diagnosis, with the incidence of idiopathic salivary gland obstruction reduced to <5% of cases (Witt, et al. Ultrasonography is considered a valuable diagnostic technique, especially in the case of stones, but it has the limitation of being operator-dependent procedure. Sialoendoscopy has more recently partially filled a diagnostic gap because it allows direct visualization. Salivary duct dilatation for duct stenosis, under sialoendoscopic control, is very useful but not universally available. The role of adenectomy for salivary gland obstructions in the era of sialendoscopy and lithotripsy. Persistent/Progressive Submandibular Mass Patrick J Bradley 16 Chapter Overview 16. An unusual cause for a submandibular swelling is a prolapsed sublingual gland that prolapses through a dehiscence in the mylohyoid muscle. Other contents of the triangle include lymph nodes that lie outside the fascia and number between 6 and 10 normally, fatty tissue, nerves, arteries, and veins. These other structures within the triangle may present as a painless mass or lump, and occasionally neighboring condition or diseases from the mouth or neck may initially present as a submandibular swelling but their likely origin should be investigated and examined for, prior to proceeding to any surgery. Diseases within the submandibular triangle in children that require surgery are uncommon (Hockstein, et al. Most pediatric submandibular triangle lesions are inflammatory and resolve 176 Section 1: Head and Neck Flowchart 16. Infrequently, the lesions persist and surgical excision is performed, either for treatment or for diagnostic purposes. In contrast, the older adult is more likely to have a neoplastic lesion lymphoma, squamous cell carcinoma, or a salivary neoplasm-benign or malignant (Munir and Bradley, 2008). The inflammatory processes of the submandibular salivary gland are more common in the teenager and young adult. Management in Children Submandibular triangle tumors that affect children are rare in the pediatric population and the tumors are often slow growing; little is lost by starting treatment with antibiotic therapy (Hockstein, et al. Amoxicillin with clavulanic should be commenced, and lesions that do not initially respond to antibiotic therapy may be treated with an extended course or with a different agent (vancomycin or a macrolite). For lesions that persist despite a 2-week course, imaging studies should be performed. Solid lesions should be excised employing oncologic principles (Patel and Karlis, 2009). A past history of systemic disease, malignancy or local dental caries, or treatments may give a clue as to which direction further enquiries will follow. Some lesions may arise in the superficial tissues and may be easily diagnosed on physical examination. Most common cystic lesions include plunging ranulas, dermoid and epidermoid cysts, Chapter 16: Persistent/Progressive Submandibular Mass Table 16. Pediatric Incidence Salivary tumors+ Benign Malignant Parotid+ Benign Malignant Submandibular+ Benign Malignant Sublingual+ Benign Malignant Minor salivary glands+ Benign Malignant + Percentage of all. Diagnostic difficulties may be encountered when the diagnosis of ranula has been misdiagnosed, resulting in the recurrence of symptoms and inappropriate management, with associated risks, complications, and frustrations of surgery (Jain, Morton and Ahmad, 2012). The purpose is to ascertain the presence of a radioopaque calculus and to exclude an underlying dental abscess. Since the introduction of sialoendoscopy, it is more readily a separate salivary ductal disease from parenchymal disease. The major causes of salivary ductal disease, as currently classified, are lithiasis, stenosis, and dilatation. The current goal of management of sialadenitis and sialolithiasis is to preserve the gland, with removing the gland as a final effort in eliminating salivary gland infection (Rahmati, Gillespie and Eisele, 2013). The Plunging Ranula the plunging ranula, also known as diving or cervical ranula, is a pseudocyst formed by extravasation of mucous from the sublingual gland into the submandibular space. Most plunging ranulas appear in the second or third decade of life, but there have been reports of presentation in infancy that, along with, marked preponderance of ranula in people of Asian origin, and anatomical anomalies in the mylohyoid muscle, point toward a congenital etiology (Morton, Ahmad, and Jain, 2010; Harrison, 2010). Treatment is surgery, in the form of transoral excision of the sublingual gland and evacuation of the cystic contents as sole treatment for plunging ranula, has resulted 16. The abundance of IgG4-positive plasmacytes in the affected salivary glands might be related to the pathogenesis of these diseases.
Generic minocycline 50mg on line
Unilateral loss of function may be related to trauma in the neck common antibiotics used for sinus infection discount minocycline online mastercard, which may be surgical in origin after. Twitching or fasciculation may be seen in irritative and compressive lesions of the nerve trunk near its origin, and may be seen rarely after radiation therapy. The nerve is easily damaged in this area as it is superficial, and can be cut in the first incision. It will cause wasting and fasciculation of the ipsilateral side, and deviation of the tongue to that side. This syndrome occurs when the sympathetic supply of the neck is disturbed, and can occur postoperatively, where the sympathetic trunk has been damaged, as in the case of removal of a schwannoma or other tumor. Trismus (Difficulty in Opening Mouth) Zahoor Ahmad, Randall P Morton 23 Chapter Overview 23. A limitation in the ability to open the mouth can have serious health implications, including reduced nutrition due to impaired mastication, difficulty in speaking, and compromised oral hygiene. If any of these muscles are damaged, individually or in a group, they can cause limitations in the opening of the mouth. If all three fingers fit between the central incisors, mouth opening is considered functional and normal. Limitations caused by factors external to the joint include neoplasms, acute infection, myositis, systemic diseases (lupus, scleroderma, etc. Late effects of intermaxillary fixation after mandibular fracture or other traumas may result in trismus. Trismus has a negative impact on quality of life in this population (Louise, et al. It may make physical re-examination difficult if limited mouth opening precludes adequate visualization of the site. Trismus can be seen as an extrapyramidal side effect of metoclopramide, phenothiazines, and other medications. Experience suggests that the combination of surgery and radiation to treat cancers of the head and neck patients pose an increased risk to develop trismus. Trismus will decrease the resonating space in the oral cavity and, thereby, diminish the quality of the voice. In cancer patients who have received radiation to the mandible, oral hygiene is of particular importance. Infection of the mandible can cause further complications, including osteoradionecrosis. These are serious quality-of-life issues that require significant attention, and overlooking them can lead to malnutrition, dehydration, social disorders and muscle/joint degeneration. Severe trismus makes it difficult or impossible to insert dentures; oral hygiene is compromised and there is an increased risk of aspiration. These changes mimic arthritic changes, and may be accompanied by inflammation and pain. Left untreated, degenerative processes may continue, ultimately becoming permanent. Disuse atrophy, seen by reduction in muscle as well as shortening of muscle fibers, is observed within days of immobilization. Patients with this condition may experience significant weight loss, and may have significant nutritional deficits. This is of particular importance at a time when the patient is attempting to recover from surgery, chemotherapy, or radiation treatment. It is generally accepted that weight loss of >10% of initial body weight is considered significant; it indicates inadequate nutritional intake and is very frequently seen in patients with trismus. Rapid motion may create the reflex that causes muscles to contract, thereby making stretching of connective tissue difficult or even impossible. A normal swallow requires an individual to manipulate the food into a cohesive bolus prior to propulsion. If the tongue cannot move properly due to limited mouth opening, the bolus may not be formed properly, leading to post-swallow excess residue. The combination of compromised mastication, poor bolus organization and increased residue has the potential to lead to aspiration of part or all of the bolus. Chapter 23: Trismus (Difficulty in Opening Mouth) Over the years, there have been wide arrays of apparatus that have attempted to treat trismus. Devices range from a variety of cages that fit over the head, to heavy springs that fit between the teeth. In some places, screws are placed between the central incisors and hydraulic bulbs placed between the teeth; however, the most commonly used treatment appears to be tongue depressors, and they seem to work well. These are stacked, forced and held between the teeth in an attempt to push the mouth open over time. A number of studies have demonstrated the efficacy of one particular product: the Therabite Jaw Motion Rehabilitation System. Hold the open position to the maximum opening that can be sustained without pain for 7 seconds. Expected Results of Therabite: A typical patient will gain between 1 and 4 mm of opening in the first session (in ~1 minute). Only by continuing to stretch and mobilize for many sessions per day will any lasting benefit be achieved. The patient places one end of the spatulas in the mouth, then presses the other end, which acts as a lever and helps to open the mouth. Regular use of this device can help to achieve maximal mouth opening (Mehana, 2010). Trismus related to head and neck cancer is difficult to treat with exercise therapy (Dijkstra, et al. Botulinum A Toxin the toxin does not improve trismus, but significantly improves pain scores and masticator spasms (oromandibular dystonia) (Hartl, et al. Many patients presenting with "sinus headache" fulfill the diagnostic criteria for either migraine or tension headache (Cady and Schreiber, 2002; Silberstein, 2004; Jones, 2009; Ravindran and Baraniuk, 2010; Cashman and Smyth, 2012). Comorbidities such as anxiety, depression, fibromyalgia, chronic fatigue, irritable bowel, and low back pain are also frequently present in these patients (Naranch, et al. Furthermore, considering the nose and sinuses as potential causes of headache/facial pain, neurological, dental, rheumatologic, and musculoskeletal conditions may need inclusion in a differential diagnosis. An oto laryngologist, who wishes to accurately diagnose and usefully treat patients presenting with "sinus headache," has to move away from a simplistic "cause and effect" 248 Section 1: Head and Neck pain model to a central sensitization pain model. A "whole person" multidisci plinary approach involving diet, sleep, exercise, stress reduction, nutritional supplements, and medication may be required in the management of more complex facial pain patients (Bartley, 2007). Management Depending on the clinical diagnosis, a wide range of treatment options is available. Many of these interventions are outside the conventional knowledge base of many otolaryngologists, but some knowledge is useful if an otolaryngologist wishes to provide comprehensive diagnosis and care. The following approach is recommended: Exclusion and/or treatment of any obvious or clinically important pathology such as sinus and dental infection as well as temporal arteritis in an older age group. Although there are frequently patient concerns, neoplasia in the absence of other clinical signs rarely presents as a pain syndrome per se. Patients with a neck injury or significant neck pain in the absence of any sensory or motor disturbances may need specialist musculoskeletal referral and treatment.
Order minocycline overnight
Vitamin K also may be administered although this will make re-coumadinization more difficult infection x ray discount minocycline online mastercard. The management of bleeding due to thrombolytic therapy includes cessation of all anticoagulant therapy, application of pressure to the bleeding site, and correction of hemostatic defects. Aminocaproic acid (Amicar) or tranexamic acid (Lysteda; Cyklokapron) may be used in significant hemorrhage following thrombolytic therapy. Platelet Disorders Platelets are critical for "primary hemostasis" (interaction of platelets with the endothelium). Quantitative Platelet Disorders A decreased number of circulating platelets reflects increased peripheral destruction or sequestration, decreased marrow production, or a combination. Splenectomy may be required in patients with serious bleeding who do not respond to medical management, and this approach is chosen less often in children than in adults. Drug-induced, immune-mediated platelet destruction is usually reversible, and withdrawal of the offending drug prevents further platelet destruction. Drug-induced, nonimmune thrombocytopenia occurs with most cancer chemotherapeutic agents that produce marrow suppression. The thiazide diuretics, cimetidine, ethanol, and several cephalosporin and penicillin antibiotics may suppress platelet production. Generalized infection and many viral illnesses cause bone marrow suppression or immune platelet destruction. Gaucher disease causes thrombocytopenia by replacing marrow with nonhematopoietic cells. Platelets may also be destroyed by high body temperatures seen in severe hyperthermic syndromes. The more specific heparin-induced platelet injury assay (serotonin release assay) is recommended for confirmation. Anticoagulation with an alternate agent must be initiated because delayed thrombosis can occur up to 30 days after removal of heparin exposure. The direct thrombin inhibitors are preferred, as they carry no risk of crossreacting with the heparin-dependent antibodies. Qualitative Platelet Disorders In most cases, discontinuing offending drugs restores platelet function. New drugs that target the adenosine diphosphate P2Y12 receptor on the surface of platelets. Because many of the adverse drug-related platelet effects are reversible, medications should be discontinued promptly (if not essential for treatment) or substituted for drugs not associated with platelet dysfunction. Current practice sets the threshold for routine prophylactic platelet transfusions at <10,000/L. Autoimmune disorders associated with increased peripheral platelet destruction, disorders of splenic sequestration, and drug-related thrombocytopenia are unlikely to benefit from platelet transfusion as transfused platelets may be rapidly removed from circulation or exhibit impaired function upon exposure to drugs in circulation. An exception is that children who are to have invasive procedures may benefit from platelet transfusion immediately before the procedure. Both inherited and acquired risk factors have been identified in children who subsequently develop thromboembolic phenomena (Table 95. Thromboprophylaxis There is no consensus for thromboprophylaxis in children and actual practice varies greatly. Congenital heart disease patients who have undergone the Fontan operation are sensitive to warfarin and lower doses should be used. Thrombolytic therapy is not recommended as firstline therapy for thrombosis in newborn infants because of the high risk of hemorrhage. Data for children are lacking, and so adult dosing guidelines are generally followed. Consultation with the pediatric hematologist is recommended before initiating thrombolytic therapy. The heme groups are identical, but the amino acid sequences of the globin chains differ imparting unique functional characteristics (including oxygen affinity). The persistence of HbF offers a protective effect in patients with certain hemoglobinopathies. Erythrocytes and Hemoglobin: the substitution of valine for glutamine in the -globin chain destabilizes oxygenated hemoglobin (accelerated denaturation), and reduces the solubility of deoxygenated hemoglobin. These changes damage the erythrocyte cell membrane, reduce membrane flexibility and the ability to traverse capillary beds, and result in ischemic injury. The destruction of globin chains results in oxidation of iron to the ferric state and increased generation of superoxide, hydrogen peroxide, and hydroxyl radicals. These potent oxidants combined with liberated iron, denature erythrocyte surface proteins, alter cation permeability, and disrupt phospholipid membrane structure. Disruption of ion transport mechanisms results in erythrocyte dehydration, increased corpuscular hemoglobin concentration, accelerated hemoglobin polymerization, and intracellular oxidant injury. A vicious cycle is initiated within the erythrocyte that disturbs flow characteristics and results in stagnant microvascular 969 blood flow, blood vessel obstruction, and distal tissue ischemia. These adhesion molecules and activated endothelial cells potentiate vascular inflammation. Activated endothelial cells promote thrombosis and vasculopathy through increased interactions with abnormal erythrocytes, activated leukocytes, the hemostatic pathway, and activated platelets. The degree of affinity between erythrocytes and endothelium correlates with clinical severity. Circulating platelet-derived factors such as thrombospondin facilitate erythrocyte adherence to endothelial cells. Autopsy studies demonstrate diffuse arteriolar thrombosis and interstitial fibrotic lesions unrelated to large-vessel thrombotic or embolic disease. Depletion of glutathione, the major antioxidant of the erythrocyte, is linked to hemolytic rate and the development of pulmonary hypertension. Close monitoring and maintenance of oxygenation by administration of supplemental oxygen are recommended. Transit time through the circulation is affected by dehydration, systemic hypotension, tourniquet use, and vasoconstriction. Fluid management should provide generous intravascular hydration to preserve euvolemia. The administration of sodium bicarbonate does not prevent perioperative pain crises. The white blood cell count and differential do not help distinguish between infection and infarction. If osteomyelitis is suspected, antimicrobials effective against Staphylococcus aureus and Salmonella species should be started while awaiting bone biopsy. Successful pain management modalities include acetaminophen, nonsteroidal anti-inflammatory medications, opioids (intermittent or patientcontrolled administration), and regional anesthesia (epidural analgesia or nerve blocks). Ketorolac may be useful but is contraindicated if hemorrhagic stroke is suspected. Expert titration of opioid therapy is essential to achieve pain relief, allow deep breathing exercises, promote ambulation, minimize splinting and avoid respiratory depression. Psychology and 971 psychiatry services should assist with identification and treatment of depression and paincoping strategies. The type of transfusion is based on the desired effect(s) and desired speed of improvement of hemoglobin concentration and hemoglobin S fraction. Exchange transfusion therapy can be accomplished in infants using an arterial catheter for blood withdrawal and venous access for infusion of blood.
Cheap minocycline 50mg without a prescription
Patients with vagal nerve stimulators and patients with transplanted organs have disruptions in their cholinergic anti-inflammatory pathways virus like ebola generic minocycline 50 mg mastercard. Assessment and Treatment of Immune Suppression due to Critical Illness Withdrawal of Unnecessary Immune Suppressants Drugs that mimic the acute stress response, such as catecholamines and steroids, should be tapered as soon as hemodynamics and underlying conditions allow. Opioids specific for the - or receptors may induce less immune suppression; therefore, methadone and fentanyl may be slightly less immunosuppressive than morphine. Receptor affinity predicts that buprenorphine, hydromorphone, oxycodone, oxymorphone, and tramadol are the least immunosuppressive. They mobilize to sites of infection or injury and release cytotoxic molecules to eliminate microbes. Deficits in phagocyte function or number cause impaired wound healing and recurring infections. As cells differentiate from hematopoietic stem cells, they undergo five divisions and mature in the storage pool for ~5 days. The nucleus contracts from the ovoid shape of the promyelocyte to the "band," and finally the mature neutrophil with a three- to five-lobed nucleus. The elimination of foreign microorganisms through phagocytosis, generation of reactive oxygen metabolites, and release of microbicidal substances depend on the mobilization of neutrophilic granules and secretory vesicles. The primary (azurophil) granule forms early (myeloblast) and contains myeloperoxidase and neutrophil elastase. Exocytosis of granules occurs in reverse order, with secretory granules being the easiest to mobilize and the primary granule the least easy, requiring strong phagocytic stimuli. The -defensins have microbicidal activity against fungi, bacteria, enveloped viruses, and protozoa. They are important as a reservoir of matrix-degrading enzymes and membrane receptors required during neutrophil extravasation. Neutrophils contain three metalloproteinases that degrade major structural components of the extracellular matrix and are important for the extravasation of neutrophils. The secretory vesicles are endocytic and constitute a reservoir of membrane-associated receptors required at the earliest phases of neutrophil localization. Maturation of the neutrophil and granule protein synthesis are achieved by transcription 598 factors. Within the circulation, half of the neutrophils are in the flowing stream, and the other half are inaccessible to phlebotomy (the marginating pool). Neutrophilia occurs after the administration of glucocorticoids, with 60% of the response due to mobilization from the marginated pool, 10% due to increased bone marrow release, and 30% due to lengthened half-life in circulation. In response to inflammatory stimuli or infection, neutrophil production and release significantly increase. Neutrophil Localization in Infection the first defense against microbes is local immunity. The epithelial surface functions as a physical barrier and releases antimicrobial peptides. If the microbial burden exceeds these processes, then neutrophil recruitment is required to control the infection. The cytokines activate macrophages that reside in the submucosa, which amplifies the proinflammatory signal with additional release of proinflammatory chemokines and cytokines. The endothelium of the nearby postcapillary venule, under the immunologic pressure of proinflammatory cytokines, transforms from a nonadhesive surface to a proadhesive surface through the expression of specific ligands on the endothelial surface. Selectins are responsible for the initial capture of the neutrophil from the free-flowing stream and their rolling on the endothelial surface. The neutrophil must breach the venular wall, including the pericyte sheath and the venular basement membrane. Perivascular mast cells and macrophages are also rich sources of neutrophil and monocyte chemoattractants. The egress across the venular wall is significantly slower than across the endothelium itself. Locomotion through the subendothelial matrix requires additional integrins, which recognize matrix proteins, including fibronectin, 599 collagen, vitronectin, and vimentin. Locomotion results in the release of both gelatinase granule and secretory vesicle contents. In many situations, neutrophil recruitment does not occur in the sequence just described. Neutrophils or platelets already recruited to an inflammatory focus can recruit other neutrophils. In vascular beds (such as the liver, kidney, and lung), geometric constraints affect neutrophil localization. As neutrophils are exposed to inflammatory mediators, as occurs in sepsis, they become more rigid. The physical trapping of an activated neutrophil alone may be sufficient to result in injury, as described in following sections. Opsonophagocytosis and Microbial Killing the ingestion and disposal of microbes is a major aspect of neutrophil function. To facilitate recognition of microbes by neutrophils, these targets are "decorated" with serum opsonins. Opsonins include proteolytic fragments derived from the complement cascade and specific immunoglobulins. Receptors that recognize opsonized bacteria are present on the neutrophil surface. As neutrophil receptors are activated, the plasma membrane "ruffles" and assumes a bipolar configuration, with the formation of a "head" (or pseudopod) and "tail" (or uropod). The pseudopod surrounds the microbe and fuses at the distal end to form a phagolysosome. The particle is internalized and generally completely surrounded by plasma membrane. Release of myeloperoxidase from the primary granule is important for oxygen-dependent killing. The respiratory burst refers to the coordinated consumption of oxygen and production of metabolites when neutrophils are confronted with appropriate stimuli, actions that are the basis of all oxygen-dependent killing by neutrophils and other phagocytes. Neutrophils are tethered from the free-flowing stream and roll on the endothelial lining of the blood vessel, an interaction mediated by all three members of the selectin family. Integrins and their ligands, the immunoglobulin gene superfamily, mediate the transition from rolling to arrest. The neutrophils then crawl over the surface of the endothelium until they migrate through the endothelial monolayer. Neutrophils emigrate out of the blood vessel across the endothelial cell lining and crawl through the basement membrane and along the connective tissue. These integrins interact with their specific epitopes in the basement membrane structural proteins. Upon encountering bacteria, neutrophils surround them with plasma membrane, forming a phagolysosome. In the phagolysosome, both oxygen-dependent and oxygen-independent mechanisms are operative, resulting in bacterial killing. A central feature of the inflammatory pathology of acute sepsis is accumulation of activated neutrophils within the microcirculation of highly vascular organs such as the liver, leading to immune-mediated tissue damage and organ dysfunction. However, accumulation of neutrophils in the liver enhances clearance of pathogens from the circulation (both viruses and bacteria). Modulation of the Immune Response the neutrophil has key roles, in both the innate and acquired immune systems, beyond bacterial clearance. Haptoglobin, an acute-phase protein, is present in the specific granules of neutrophils. In addition to being antimicrobial, defensins (from the primary granule) are chemotactic for lymphocytes and monocytes and contribute to the secondary wave of leukocytes required for resolution of infection. Neutrophils enter lymphoid organs and can modulate the adaptive immune response by inhibiting rather than augmenting the response of T and B cells to immunization.
Order generic minocycline
Hyperphosphatemia is managed with oral phosphate binders virus ti 2 order minocycline 50mg with amex, such as sevelamer hydrochloride, or aluminum hydroxide. The epidural space is the most common area for spinal cord metastasis with the thoracic spine being the most common site. Craniospinal T1- and T2-weighted magnetic resonance imaging is the study of choice to demonstrate epidural involvement, intraparenchymal spread, or compression of nerve roots. Therapy (usually corticosteroids) should be initiated as soon as the diagnosis is considered. Later therapy may include radiation if the tumor is radiosensitive, surgery if there is severe spinal instability, rapidly progressive symptoms, or progressive symptoms in spite of radiation, and chemotherapy if the diagnosis is leukemia/lymphoma or neuroblastoma. Patients with posterior mediastinal masses are 923 at risk for spinal cord compression. Lesions affecting the tracheobronchial tree may cause dyspnea, orthopnea, stridor, cough, and respiratory distress. Tumor masses compressing the great vessels may cause head and neck edema with or without neurological deficit. Supine position or sedation may worsen symptoms or lead to cardiopulmonary arrest, so careful planning of evaluation and management is necessary. Airway instrumentation should be performed in a controlled environment by experienced anesthesiologists with surgical and cardiopulmonary support available when possible. In most situations, endotracheal intubation takes place in conscious and spontaneously breathing patients employing topical anesthetic techniques with light sedation and avoiding neuromuscular blocking agents. Reinforced endotracheal tubes of decreased diameter but sufficient length to extend beyond the compression may be necessary. Extracorporeal membrane oxygenation or cardiopulmonary bypass back-up should be considered. Prebiopsy cytoreductive therapy using corticosteroids or radiation may be required in patients presenting with severe airway compromise (may reduce the ability to make a definitive diagnosis). Progressive venous congestion and airway compression usually cause facial engorgement, headache, plethora, cyanotic facies, cough, dyspnea, orthopnea, hoarseness, stridor, and dysphasia with or without pleural and/or pericardial effusions. Once the definitive diagnosis is reached, the appropriate chemotherapeutic plan will reduce tumor load rapidly with improvement of symptoms. Thrombolytic therapy should be considered in patients with extensive thromboembolism if no contraindications. Other infections to be considered include invasive fungi (mucormycosis), bacterial necrotizing pneumonias due to Staphylococcus aureus, Pseudomonas aeruginosa, Klebsiella, and tuberculosis. Noninfectious etiologies include primary endobronchial tumors, diffuse alveolar hemorrhage, bronchiectasis, and foreign bodies. Aggressive treatment of associated coagulopathy, thrombocytopenia, and anemia and appropriate antibiotics or antifungals are warranted. Bronchoscopy should be considered if endoluminal control of the bleeding is feasible. Other options include bronchial arteriography with transcatheter embolization in nonsurgical candidates, wedge resection of the affected lung segment, or lobectomy. Conditions that increase the risk of bowel obstruction include surgery, radiation therapy, opioid use, prolonged bed rest, malnutrition, and electrolyte abnormalities. Dexamethasone and octreotide are effective in relieving symptoms in most patients with malignant bowel obstruction. Surgery is indicated for patients with complete mechanical obstruction, partial mechanical obstruction not responding to medical treatment, peritonitis, and frank perforation. The "classic triad" of intussusception includes colicky pain, abdominal mass, and bloody stools. Ultrasonography is more accurate than abdominal radiographs and can detect the lead point and other intra-abdominal pathology. The treatment of choice is surgical reduction of the intussusception and resection of the inciting pathology rather than radiologic reduction using contrast enema. The most common etiologies that require emergent evaluation include hemorrhage, hemolysis, and splenic sequestration. Anemia, regardless of etiology, results in a decreased O2-carrying capacity and, when severe, decreased O2 delivery. Ferritin and serum iron are low, and total iron-binding capacity and transferrin are increased. Iron deficiency is most common in children <3 years and results from inadequate iron intake during a period of rapid growth. In older children and adults with iron deficiency, occult blood loss should be suspected and should prompt a gastrointestinal evaluation. Enteral ferrous sulfate is preferred; parenteral administration (with iron dextran) is an option if compliance or tolerance is an issue. Transfusion is usually recommended for children with or without cardiorespiratory symptoms when Hb is 4 g/dL. In children who have Hb values between 4 and 6 g/dL, treatment practices vary and the decision to transfuse can be based on symptoms, available resources, comorbid conditions (malaria, fever), and end-organ manifestations. Hemolytic anemia and autoimmune hemolytic anemia can be caused by either intracellular or extracellular disorders. Extracorpuscular disorders include immunemediated destruction, mechanical fragmentation, infections, drugs, chemicals, and venoms. Lack of this enzyme allows rapid depletion of antioxidants and subsequent denaturation of the Hb unit. Evaluation reveals a rapidly falling Hb, low haptoglobin, increased bilirubin metabolites in the urine, positive Coombs tests, and abundant spherocytes on smear. Clinically significant hemolysis can occur with either IgG or IgM antibodies, but usually with IgG. It usually occurs in children 6 months to 3 years and is commonly preceded by a viral illness. Bone marrow infiltration can result from malignant cells, inherited metabolic disorders, or infections (fungus, tuberculosis). Regardless of the process, the result is a normocytic anemia with a low reticulocyte count. These patients can have lymphadenopathy, hepatomegaly, splenomegaly, reticulocytopenia, neutropenia, thrombocytopenia, and circulating immature cells. Bone marrow examination is essential in this setting to establish the correct diagnosis. Acquired aplastic anemia is defined as peripheral blood pancytopenia with bone marrow hypocellularity in the absence of underlying malignant or myeloproliferative disease. The principal pathophysiologic mechanism is thought to be immune-mediated destruction of 927 hematopoietic stem cells by cytotoxic T lymphocytes. Drug-induced causes account for 50% of all cases and result from either toxic effects or immune-mediated phenomena. Common toxic agents include ionizing radiation, chemotherapeutic drugs, antibiotics (chloramphenicol), hydrocarbons (benzene), antiinflammatory medications (phenylbutazone, indomethacin), and metals (gold). Other drugs with a risk for aplastic anemia are anticonvulsants (fosphenytoin, phenytoin, carbamazepine) and quinacrine. Megaloblastic anemia may be caused by decreased vitamin absorption or impaired metabolism. Decreased vitamin B12 absorption in children results from limited nutritional intake or intestinal malabsorption. Agents that impair B12 absorption include metformin, colchicine, neomycin, para-aminosalicylic acid, and slow-release potassium chloride. Causes of folate deficiency include sepsis, pregnancy, malignancy, chronic hemodialysis, and medications. Approximately 50% of patients on long-term phenytoin have low folate levels, and 30% have red-cell macrocytosis, and megaloblastic changes in the bone marrow. Methotrexate, trimethoprim, triamterene, and pyrimethamine inhibit dihydrofolate reductase and cause megaloblastic anemia that is not folate responsive during long-term and high-dose therapy. Acute megaloblastic anemia may also be caused by prolonged or repeated nitrous oxide anesthesia. Hemoglobinopathies Primary hemoglobinopathy describes structural abnormalities of Hb that are often inherited. In normal human maturation, HbA (22) becomes the dominant form, taking over from the HbF (22) during the first year of life.