Buy norpace pills in toronto
These include adult data on decreased bone density as well as pediatric studies showing increased risk for respiratory infections and Clostridium difficile infection medications not to take with blood pressure meds buy 150mg norpace with visa. Children who symptomatically do not respond to acid suppression may require additional evaluation for EoE or gastroparesis, as discussed later in this chapter. Medical therapy to limit the number of reflux episodes, irrespective of acidity, is quite limited. Aspiration of refluxed gastric contents is controlled by fundoplication, but aspiration during swallowing is not affected. Fundoplication is associated with a number of complications, such as gagging/retching, gas bloat, or dumping syndrome, so it should be reserved for those patients who cannot be managed medically. Esophageal peristalsis may be diminished, absent, or even retrograde on manometric testing. Disorders of gastric emptying present with symptoms such as nausea, early satiety, and vomiting, often from meals ingested many hours prior. Treatment for motility disorders of the esophagus is often supportive, as there are no commonly employed medications that improve esophageal peristalsis. Children may need to restrict bolus size and often require a significant proportion of their calories by liquid formulas. Because of the risk of worsening gagging and retching after surgery, we typically do not recommend fundoplication in children with esophageal or gastric dysmotility, though there are few data in the literature. Erythromycin is an antimicrobial with a prokinetic side effect that is employed to improve gastric emptying. Other possible therapies include endoscopic administration of Botox to the pylorus, with or without concomitant pyloric dilatation (for temporary relief) or surgical pyloroplasty (for long-term relief). Tachyphylaxis, or decreased response, is an issue with histamine receptor antagonists such as ranitidine. In adults with true erosive esophagitis, mucosal healing with proton pump inhibitors can take up to 2 months. Important factors in pathogenesis include defects in the barrier function of the epithelium that are promoted by the downregulation of genes encoding the proteins that are involved in maintaining the adhesion between squamous cells. Although tissue eosinophilia is a marker of disease activity, lymphocytes and mast cells also participate in the inflammatory infiltrate. More than 70% of affected individuals are male, and twothirds of patients are otherwise atopic, with asthma, eczema, and/or IgE-mediated food allergy. There is a strong familial predisposition for EoE, as indicated by up to a 64-fold increased relative risk among first-degree relatives. Family and twin studies support a strong genetic link but also indicate that there must be an environmental trigger to initiate the disorder in susceptible individuals. Younger children often present with feeding problems, whereas abdominal pain or vomiting are characteristic features in elementary school-aged children. Nevertheless, because there is sufficient concern that EoE might pose difficulties after airway reconstruction, we manage EoE and confirm histologic recovery from it prior to reconstructive airway surgery. As such, it is essential that biopsies be obtained irrespective of the endoscopic appearance, and that a minimum of five biopsies of the esophagus be taken to minimize the risk of missing the diagnosis by sampling error. Precise identification of the offending antigens is a challenge, as food allergy testing by standard skin prick testing and serum specific IgE levels usually fail because the mechanism of immune response to the antigen in EoE does not primarily involve IgE. They must be maintained indefinitely, as the recurrence rate of the disease is virtually 100% if they are discontinued. Unfortunately, symptom resolution does not imply resolution of the histologic inflammation, so repeat endoscopy is recommended to confirm histologic remission of the disease with any change in therapy or diet, even if symptoms have diminished. The resulting dysphagia can be improved by esophageal dilatation, although diet or medical therapy is preferred to manage the inflammatory process directly. Twenty-four hour ambulatory simultaneous impedance and pH monitoring: a multicenter report of normal values from 60 healthy volunteers. Association between body mass index and gastroesophageal reflux symptoms in both normal weight and overweight women. Patients with gastro-oesophageal reflux disease and cough have impaired laryngopharyngeal mechanosensitivity. The problem of pediatric laryngotracheal stenosis: a clinical and experimental study on the efficacy of autogenous cartilaginous grafts placed between the vertically divided halves of the posterior lamina of the cricoid cartilage. Pharmacokinetics and pharmacodynamics of lansoprazole in children with gastroesophageal reflux disease. Fracture risk and bone mineral density reduction associated with proton pump inhibitors. Proton pump inhibitors as a risk factor for paediatric Clostridium difficile infection. Therapy with gastric acidity inhibitors increases the risk of acute gastroenteritis and community-acquired pneumonia in children. Endoscopic intrapyloric injection of botulinum toxin A in the treatment of children with gastroparesis: a retrospective, open label study. Eosinophilic esophagitis: updated consensus recommendations for children and adults. Severity of esophageal eosinophilia predicts response to conventional gastroesophageal reflux therapy. Genome-wide association analysis of eosinophilic esophagitis provides insight into the tissue specificity of this allergic disease. Twin and family studies reveal strong environmental and weaker genetic cues explaining heritability of eosinophilic esophagitis. Proton pump inhibitor-responsive oesophageal eosinophilia: an entity challenging current diagnostic criteria for eosinophilic oesophagitis. Histopathologic variability and endoscopic correlates in adults with eosinophilic esophagitis. Newly developed and validated eosinophilic esophagitis histology scoring system and evidence that it outperforms peak eosinophil count for disease diagnosis and monitoring. Effect of six-food elimination diet on clinical and histologic outcomes in eosinophilic esophagitis. Elemental diet is an effective treatment for eosinophilic esophagitis in children and adolescents. A randomized, double-blind, placebo-controlled trial of fluticasone propionate for pediatric eosinophilic esophagitis. Oral viscous budesonide: a potential new therapy for eosinophilic esophagitis in children. Analysis of symptoms and endoscopic findings in 117 patients with histological diagnoses of eosinophilic esophagitis. Dissociation between symptoms and histological severity in pediatric eosinophilic esophagitis. Esophageal dilation in eosinophilic esophagitis: effectiveness, safety, and impact on the underlying inflammation. The overall management of these patients often includes surgical airway intervention. We have found that minimizing the risk of operative failure can best be achieved through the collaborative efforts of a well-coordinated interdisciplinary team. Thorough clinical and operative examinations should be performed, with involved health professionals being aware of conditions and risk factors that can significantly impact clinical outcomes. This article presents an overview of the critical aspects of otolaryngologic management of this complex patient population in the context of the collaborative model used at our institutions. We briefly discuss the initial assessment, mitigating factors that can affect airway reconstruction, and perioperative management of specific airway pathology. Microlaryngoscopy and rigid bronchoscopy are performed with the primary goal of identifying anatomic levels of airway obstruction from the larynx to the carina. The supraglottis is evaluated with attention given to the possibility of supraglottic obstruction, such as laryngomalacia and supraglottic stenosis. The vocal fold level is then evaluated for posterior glottic stenosis, anterior glottic web, and laryngeal cleft. It should be noted that the posterior glottis is an area that is suboptimally evaluated by flexible bronchoscopy.
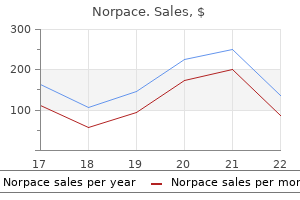
Generic norpace 100 mg on line
Cardiac enzymes are irrelevant in the patient with suspected myocardial contusion treatment without admission is known as purchase 150mg norpace mastercard. Prospective randomized controlled trial of operative rib fixation in traumatic flail chest. Indications, complications, and surgical techniques for pediatric tracheostomies-an update. Establishing a role for intra-pleural fibrinolysis in managing traumatic haemothoraces. Tracheobronchial injury by blunt trauma in children: is emergency tracheobronchoscopy always necessary Conservative and surgical treatment of acute posttraumatic tracheobronchial injuries. Traumatic wet lung; observations on certain physiologic fundamentals of thoracic trauma. A caveat to the performance of pericardial ultrasound in patients with penetrating cardiac wounds. Serum troponin-I as an indicator of clinically significant myocardial injury in paediatric trauma patients. Cardiac and great vessel injuries in children after blunt trauma: an institutional review. Pediatric emergency department thoracotomy: a large case series and systematic review. Evaluation and management of blunt traumatic aortic injury: a practice management guideline from the Eastern Association for the Surgery of Trauma. Progress in the treatment of blunt thoracic aortic injury: 12-year single-institution experience. Evolution in management of adolescent blunt aortic injuries-a single institution 22-y experience. A case report of traumatic aortic rupture in a pediatric patient: a possible role for endovascular management as a bridge to definitive repair. Videothoracoscopic drainage of mediastinal abscess: an alternative to thoracotomy. Penetrating left thoracoabdominal trauma: the incidence and clinical presentation of diaphragm injuries. There have been reports that plasma cell granulomas are usually preceded by respiratory infections. Most of these lesions are slow growing, although in some rare cases they can spread quickly, leading to airway compromise. They can differ in location from the chest wall, to the mediastinum, to the lung itself. A lung mass in the pediatric population is 10 times more likely to be a benign process than a malignant one. The most common location of chest tumors is the mediastinum, and mediastinal masses can be further divided by their location into three compartments: anterior, middle, and posterior mediastinum. Mediastinal masses tend to occur early in the pediatric population, with around 40% of mediastinal masses occurring before the age of 2. The lesions are usually located peripherally in the parenchyma of the lung but have also been noted, rarely, to be located centrally, as well as within the chest wall. Etiology the etiology of tumors of the chest ranges widely, depending on the location of the tumor. In terms of primary pulmonary lesions, tumors can arise from both the tracheobronchial tree and the pulmonary parenchyma itself, and they can accompany a wide variety of subtypes, from benign (inflammatory pseudotumor and hamartomas) to malignant (bronchial adenoma, bronchogenic carcinoma, pleuropulmonary blastoma). While the name adenoma suggests a benign process, bronchial adenomas can become malignant. There are three histologic types of bronchial adenomas: carcinoid, cylindroma, and mucoepidermoid. They are low-grade tumors, which can metastasize, but most are slow-growing tumors that can grow into the bronchial wall. Carcinoid syndrome itself is rare, although it has been reported in the pediatric population. These lesions are typically seen in patients less than 40 years old, with the majority in the pediatric population occurring in the age group between 8 and 12 years old. They are the most common benign lung tumors in the pediatric population, making up more than 50% of benign lesions and 20% of all primary lung lesions. Therefore, depending on the etiology, the incidence and epidemiology differ widely. Despite the wide differential, using a systemized approach can lead to the correct diagnosis and treatments that lead to favorable outcomes for the patient. This article covers the wide range of processes that can lead to solid tumors in the pediatric population in the chest, how to organize them within systems, and their most common manifestations and treatments. Bronchial adenomas usually present with vague pulmonary symptoms such as fever, cough, chest pain, recurrent pneumonitis, and hemoptysis as the tumor slowly grows into the airway and causes incomplete obstruction. The rarity of these disorders commonly causes a delay in diagnosis, often for years. The tumors usually involve the right main bronchus and are 5 times more likely to be seen in boys. Treatment consists primarily of resection of a segment, lobe, or complete lung, according to the degree of involvement, which may be done thoracoscopically or via thoracotomy, depending on the location and extent of the lesion. Luminal excision by bronchoscopy should not be done because it does not permit complete removal of the tumor. Rarely a bronchial adenoma can be removed by bronchial or sleeve resection, followed by airway reconstruction. They are primarily mesenchymal tumors and are divided into benign and malignant disease, with up to 60% being malignant. Chest wall masses often present as seemingly innocuous lumps that are noticed on the chest, which may demonstrate growth. They are typically slow-growing and asymptomatic, but pain can be a presenting symptom that raises the concern for a malignant process. A small percentage of these tumors can have effects on respiratory mechanics, depending on their location and size. Benign tumors of the chest wall are less common than malignant ones and have a wide variety of etiologies. The most common soft tissue benign lesion of the chest wall derives from the myofibroblast,17 including infantile myofibromatosis and desmoid fibromatosis tumor. Infantile myofibromatosis typically presents at birth or early in life and usually undergoes spontaneous regression. In contrast, desmoid fibromatosis can be more challenging to deal with, as they originate as overgrowths of fibrous tissue that can extend through muscle and fascial planes. Full excision can be challenging, and these patients often undergo multiple surgeries. Most pediatric bronchogenic carcinomas are undifferentiated adenocarcinomas, with squamous cell carcinomas being much less common in the pediatric population, in contrast to the adult population. Usually asymptomatic, the majority of cases present late in the course of the disease leading to a poor prognosis; the mortality is more than 90%, with a mean duration of survival of only 7 months. Localized lesions can be resected with postoperative chemotherapy, but this applies to only a small subset of patients. These typically occur in younger children prior to the age of 6 years and can behave aggressively with high rates of metastasis.
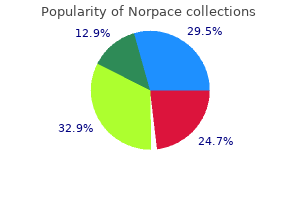
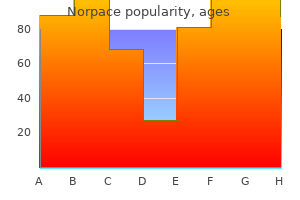
| Comparative prices of Norpace | ||
| # | Retailer | Average price |
| 1 | Dollar Tree | 291 |
| 2 | Gap | 856 |
| 3 | Subway | 358 |
| 4 | DineEquity | 941 |
| 5 | Trader Joe's | 939 |
| 6 | Ross Stores | 397 |
| 7 | Best Buy | 255 |
| 8 | Darden Restaurants | 947 |
| 9 | RadioShack | 631 |
Buy 100 mg norpace visa
Pneumonia due to Rhizopus is usually an insidious segmental pneumonia that is slowly progressive despite antifungal therapy treatment x time interaction purchase norpace master card. Cavitation may occur, and dissemination to brain and other sites occurs because of the propensity of the organism to invade blood vessels. Death may occur suddenly with massive pulmonary hemorrhage, mediastinitis, or airway obstruction. The specific diagnosis usually depends on demonstration of the organism in specimens obtained by open, transbronchial, or needle-aspiration biopsy. As with Aspergillus, treatment with amphotericin B and possibly surgical resection as early as possible is critical to achieving a cure. Posaconazole has good activity against mucormycosis, which can be aggressive and relatively resistant to voriconazole. Candida Species Though important as a cause of fungal sepsis and secondary hematogenous pulmonary involvement, primary Candida pneumonia is unusual. The prominent histologic features of primary Candida pneumonia include bronchopneumonia, intraalveolar exudates, and hemorrhage. Amphotericin B is usually the treatment of choice for invasive Candida infections, along with flucytosine if synergism is desired. The imidazole antifungal agents, including ketoconazole, fluconazole, and itraconazole, have activity against C. Although fluconazole prophylaxis, as well as the use of hematopoietic growth factors, has led to a reduction in the frequency of early Candida infections in patients at risk, many institutions have experienced an increase in azole-resistant nonalbicans Candida infections. Such combination therapies take advantage of different therapeutic targets of the various antifungals, possibly reducing the emergence of resistant organisms. Histoplasmosis is especially associated with exposure to bird or bat fecal material103; as a result, it is a fairly common infection in immunocompetent children and may be asymptomatic or lead to an acute pneumonia with fever, hilar adenopathy, and pulmonary infiltrates. Both can cause chronic granulomatous pulmonary disease and lead to extrapulmonary dissemination. In the immunocompromised patient, particularly pediatric oncology patients, histoplasmosis may present as an acute illness with fever, cough, and diarrhea, or in a disseminated form with additional features of hepatosplenomegaly, fevers, and adenopathy. Blastomycosis is much less common in adult or pediatric oncology patients, and may be associated with dermatologic manifestations such as skin ulcers, in addition to diffuse chronic pulmonary infiltrates. Cryptococcus Neoformans Cryptococcus neoformans is a yeast that causes protean clinical manifestations in immunocompromised patients, often involving the meninges, endocardium, skin, and lymph nodes. The diagnosis of cryptococcosis relies on demonstration of the organism histologically, in biopsy tissue or pleural fluid,108 or by culture methods. These fungi cause skin and soft tissue infections and occasionally invade the lungs and sinuses. For example, Scedosporium apiospermum (formerly Pseudallescheria boydii) causes invasive disease in solid-organ transplant patients, with lung involvement in 50%111; it is difficult to distinguish histologically from Aspergillus. Other rare fungal pathogens seen in immunocompromised patients include filamentous fungi of which there are several species, including Dactylaria gallopava, Cladophialophora bantiana, and Exophiala. Other rare Gram-negative organisms that cause pneumonia in the immunocompromised host include Legionella pneumophila and Capnocytophaga sp. It is important to realize that factors such as geographic location, changes in infection control, prophylactic antimicrobial protocols, and technological advances all have an effect on microbial predominance. Pseudomonas aeruginosa is an additional important cause of pneumonia and sepsis in hospitalized immunocompromised children. Significant risk factors for bacterial infections include neutropenia, the presence of indwelling venous catheters, and perineal skin lesions. More unusual bacterial causes of pneumonia include Listeria monocytogenes, a gram-positive rod that causes primarily septicemia in immunocompromised patients, with subsequent pulmonary involvement. Corynebacteria (commonly called diphtheroids) are gram-positive bacilli or coccobacilli that exist as saprophytes on mucous membranes and skin. Pleural effusions may also occur as a result of increased hydrostatic or decreased oncotic pressure. Lymphatic vessels that drain the lungs can be overwhelmed or disrupted in transplantation. Infection or injury in the thoracic, mediastinal, or abdominal cavity can lead to sympathetic effusions or empyema. Pleural effusions can occur in up to 40% of children who undergo liver transplantation,139 are predominantly rightsided, and are thought to occur as a result of disruption of diaphragmatic lymphatic channels. Between 14% and 25% of pediatric patients require pleural drainage because of significant respiratory compromise. This is primarily caused by sepsis, but in the case of liver and small bowel transplantation, other risk factors should be considered as potential causes. Primary infection later in life usually causes only lymphadenopathy and mild systemic symptoms. Its usual routes of transmission are water- or food-borne, but person-to-person transmission is possible. For example, pulmonary copathogens may be isolated in as many as 53% of patients with parainfluenza pneumonia. Recovery of bacteria from respiratory secretions in this scenario may represent airway colonization rather than invasive parenchymal disease. Poor excursion of the diaphragm can lead to impaired cough and airway clearance, resulting in atelectasis and pneumonia. Diaphragmatic function can be impaired by swelling in the subdiaphragmatic area, as well as phrenic nerve injury when the suprahepatic vena cava is clamped during liver transplantation. This is especially true for patients in whom the abdomen is not completely closed in the immediate postoperative period. In this situation, the important abdominal muscles that are needed for cough are impaired. Airway clearance and the use of a mechanical in-exsufflator (cough assist device) can help clear secretions and prevent atelectasis in the immediate postoperative period. Since physiotherapy to the chest wall may be painful after sternotomy, oscillating positive expiratory pressure devices and incentive spirometry (in patients who can cooperate) and intrapulmonary percussive ventilation (in those that cannot cooperate) can be invaluable in the postoperative period. When diaphragmatic dysfunction or paralysis is present, plication of the diaphragm can be considered (utilized in up to 25% of patients with diaphragm paralysis). Corticosteroid use should be considered and may be effective, although supportive data are limited. This unregulated growth of B cells can range from benign polyclonal B lymphocyte expansion to aggressive immunoblastic B cell lymphomas. Both are potent immunosuppressants that confer less nephrotoxicity than calcineurin inhibitors. They have been increasingly popular because of their overall favorable side-effect profile. However, sirolimus and everolimus cause interstitial pneumonitis at both therapeutic and supratherapeutic drug levels. Metastatic pulmonary calcifications can occur in patients with kidney or hepatic failure, and while usually benign, can lead to restrictive lung disease. Furthermore, their nodular appearance on chest radiographs can mimic nodules from infection or malignancy (see the previous section). These conditions should be considered if unexpected pulmonary complications including prolonged hypoxemia and recurrent atelectasis develop in the posttransplant period. Renal transplant patients may be at higher risk because of manipulation of pelvic veins, although this has mainly been reported in adult patients. Childhood cancers are treated with a combination of surgery (primarily for solid tumors), chemotherapy, and radiotherapy.
Effective 100mg norpace
Although this syndrome can occur without a predisposing cause symptoms ulcer buy 150 mg norpace otc, it is usually associated with depressed cellular immunity caused by malnutrition, hematologic malignancies, or immunosuppressive therapy. Sensitivity increases to nearly 100% if seven consecutive daily stool specimens are examined in an expert laboratory, although this may not always be very practical. The treatment is medical, and the goal is elimination of all the worms; therefore, repeated treatment is sometimes needed. Thiabendazole is only available for veterinary use in the United States; however, it is still used in other countries. Screening strategies should be considered in patients who may be particularly vulnerable to Strongyloides infections. As with any of the other parasitic infections, the best method of prevention includes proper disposal and treatment of sewage material. From the bronchi, the eggs reach the mouth and are either spit out or swallowed and then excreted in stool. The hatched miracidium invades the first intermediate host (one of several families of snails), and after a protracted asexual cycle, they form sporocytes that turn into cercariae. These then enter the second intermediate host (crustaceans); here they encyst and form the infectious metacercariae that reach the definitive mammalian host. Once eaten by the definitive host, the metacercariae encyst in the duodenum, penetrate the intestinal wall to reach the liver, and change into flukes. Human infection occurs by eating crustaceans that contain the parasite metacercariae. As the life cycle of the fluke suggests, it can cause both pulmonary and extrapulmonary disease involving the brain, liver, skin and rarely eyes as well as other parts of the body. The host response also adds to the damage in the lungs when the host immune response takes the form of eosinophilic infiltration and the subsequent development of a cyst of host granulation tissue around the flukes. The release of cyst contents can cause bronchopneumonia, and the cyst wall may fibrose and become calcified. In extrapulmonary infections, the flukes may form cysts, abscesses, or granulomata. Most human disease is caused by Paragonimus westermani and occurs following consumption of raw, undercooked, or alcohol pickled crustaceans (namely shellfish). Occasionally ingestion of raw meat from a mammalian host may also cause the disease. More than 30 species have been reported worldwide with at least 10 that can infect humans. Paragonimiasis is rare in children, because they are less likely to indulge in consumption of exotic food and because this helminth is not transmitted by fecal-oral transmission, by person-to-person contact, or from consumption of infested water. Pulmonary paragonimiasis has acute and chronic stages with different clinical manifestations. The main clinical manifestations of paragonimiasis are respiratory symptoms and eosinophilia. Once the flukes reach the lungs, the patient can have cough, dyspnea, and chest tightness or even pain; systemic symptoms of fever, malaise, and night sweats may also be present. Chills and urticarial rash may occur, leading to the diagnosis of a viral syndrome. The diagnosis of paragonimiasis is frequently not made in the acute stage of the disease. Most patients look well, and the disease may resemble chronic bronchitis or bronchiectasis with a worsening cough that starts out dry and becomes productive and profuse. Other conditions to consider include bronchial asthma, chronic bronchitis, pulmonary neoplasm, and other parasitic infections endemic for the region. Pulmonary paragonimiasis can be complicated by lung abscess, pneumothorax, pleural adhesions, empyema, and interstitial pneumonia. As noted previously, pulmonary disease may be associated with abdominal (hepatic or peritoneal) and cerebral disease. However, in chronic paragonimiasis, chest radiography may show various abnormalities, including patchy nodular or linear infiltration, well-defined homogeneous densities, pleural thickening, effusion, and calcification. A systemic review of the literature on cystic echinococcosis frequency worldwide and its associated clinical manifestations. Eosinophilic pneumonias in children: a review of the epidemiology, diagnosis, and treatment. Human toxocariasis: diagnosis, worldwide seroprevalences and clinical expression of the systemic and ocular forms. In the United States, the most likely patient is a refugee, a recent immigrant, or someone with a recent history of travel. Similar to other protozoal infections, the definitive diagnosis can be made by identifying the characteristic golden brown, ellipsoidal operculated protozoal eggs. The characteristic operculated eggs can be identified in sputum or stool specimens, although the sensitivity of the tests is low. Bronchoalveolar lavage also has been successful in identifying the eggs and making the diagnosis. In complicated pulmonary paragonimiasis, the eggs can be identified in pleural fluid or lung abscess material. The epidemiology and public health importance of toxocariasis: a zoonosis of global importance. Toxocara infection in the United States: the relevance of poverty, geography and demography as risk factors, and implications for estimating county prevalence. A systematic review of toxocariasis: a neglected but high prevalence disease in Brazil. Factors affecting disease manifestation of toxocariasis in humans: genetics and environment. Toxocara seropositivity, atopy and wheezing in children living in poor neighborhoods in urban Latin America. Pulmonary toxocariasis masquerading as metastatic tumor nodules in a child with osteosarcoma. Toxocariasis mimicking liver, lung and spinal cord metastases from retinoblastoma. Toxocara infection and diminished lung function in a nationally representative sample from the United States population. Diagnosis of human toxocariasis by antigen capture enzyme linked immunosorbent assay. Biological, epidemiological and clinical aspects of Echinococcosis, a zoonosis of increasing concern. Cystic echinococcosis in Bulgaria 1996-2013, with emphasis on childhood infections. Echinococcus granulosus sensu lato genotypes infecting humans-review of current knowledge. First report of Echinococcus shiquicus in dogs from eastern Qinghai-Tibet plateau region, China. Hydatid disease involved in the heart, liver, and the kidney that caused sudden death: case report. Justified concern or exaggerated fear: the risk of anaphylaxis in percutaneous treatment of cystic echinococcosis-a systematic literature review. Comparison of the protoscolocidal effectiveness of hypertonic saline, povidone-iodine and albendazole solutions in an experimental lung hydatid cyst model. Appropriate approach to bronchobiliary fistulas: a case series with hydatid disease and algorithm of case-based management. Rare reason for pulmonary embolism: one case of pulmonary hydatid cyst and review of the literature. Hydatid disease of the central nervous system: a review of literature with an emphasis on Latin American countries.
100mg norpace otc
Incidence of pneumonia in mechanically ventilated patients treated with sucralfate or cimetidine as prophylaxis for stress bleeding: bacterial colonization of the stomach symptoms 7dp5dt cheap norpace amex. Gastric colonization and pneumonia in intubated critically ill patients receiving stress ulcer prophylaxis: a randomized, controlled trial. Occurrence of ventilator-associated pneumonia in mechanically ventilated pediatric intensive care patients during stress ulcer prophylaxis with sucralfate, ranitidine, and omeprazole. Characteristics of gastroesophageal reflux and potential risk of gastric content aspiration in children with cystic fibrosis. Lipid-laden macrophages in bronchoalveolar lavage fluid as a marker for pulmonary aspiration. Lipid-laden macrophage index and inflammation in bronchoalveolar lavage fluids in children. Lipid-laden alveolar macrophage and lactose assay as markers of aspiration in neonates with lung disease. Non-acid gastro-oesophageal reflux in children with suspected pulmonary aspiration. Pepsin, a reliable marker of gastric aspiration, is frequently detected in tracheal aspirates from premature ventilated neonates: relationship with feeding and methylxanthine therapy. Pepsin, a marker of gastric contents, is increased in the tracheal aspirates from preterm infants who develop bronchopulmonary dysplasia. Gastric vs small-bowel feeding in critically ill children receiving mechanical ventilation. Assessment of the prevalence of microaspiration by gastric pepsin in the airway of ventilated children. Pepsin like activity in bronchoalveolar lavage fluid is suggestive of gastric aspiration in lung allografts. The presence of pepsin in the lung and its relationship to pathologic gastroesophageal reflux. Therapy with gastric acidity inhibitors increases the risk of acute gastroenteritis and communityacquired pneumonia in children. Surfactant proteins A and D in children with pulmonary disease due to gastroesophageal reflux. Necessity for surgery in children with gastrooesophageal reflux and supraoesophageal symptoms. Laparoscopic antireflux procedures in the management of gastroesophageal reflux following esophageal atresia repair. Can laparoscopic antireflux surgery improve the quality of life in children with neurologic and neuromuscular handicaps Complications of gastroesophageal antireflux surgery in neurologically impaired versus neurologically normal children. Retching and vomiting in neurologically impaired children after fundoplication: predictive preoperative factors. Fundoplication and gastrostomy versus image-guided gastrojejunal tube for enteral feeding in neurologically impaired children with gastroesophageal reflux. Laparoscopic-assisted jejunostomy: an effective procedure for the treatment of neurologically impaired children with feeding problems and gastroesophageal reflux. The management of drooling in children and patients with mental and physical disabilities: a literature review. The radionuclide salivagram in children with pulmonary disease and a high risk of aspiration. Using the radionuclide salivagram to detect pulmonary aspiration and esophageal dysmotility. Agreement of aspiration tests using barium videofluoroscopy, salivagram, and milk scan in children with cerebral palsy. Botulinum toxin A injection of salivary glands in children with drooling and chronic aspiration. Effect of botulinum toxin in the treatment of drooling: a controlled clinical trial. When are bilateral submandibular gland excision and parotid duct ligation indicated Four-duct ligation: a simple and effective treatment for chronic aspiration from sialorrhea. Salivary gland surgery for control of chronic pulmonary aspiration in children with cerebral palsy. The maturation of feeding and swallowing skills evolves in a natural and seemingly effortless progression in typically developing infants and children. Given that the pharynx is a shared pathway for breathing and swallowing, precise coordination of respiration and swallowing ensures maintenance of airway protection during feeding. Intact anatomy and function of the aerodigestive tract and normal development of neural control mechanisms are essential. Feeding and swallowing dysfunction (pediatric dysphagia) occurs in infants and children because of a multitude of factors, including structural anomalies in the aerodigestive tract, static or degenerative neurologic conditions affecting the range and strength of the necessary musculature, and cardiopulmonary conditions that result in respiratory compromise with oral feeding attempts. Etiologies of dysphagia are not mutually exclusive, and often multiple interacting factors are present. The multifactorial nature of feeding and swallowing disorders necessitates the involvement of multiple disciplines in the evaluation and management process. Therefore a team approach is efficacious in the consideration of issues that involve disciplines including, but not limited to , otolaryngology, gastroenterology, pulmonary medicine, radiology, occupational therapy, nutrition therapy, and speech pathology. This article will review the clinical and procedural evaluation and management of infants and children presenting with feeding and swallowing from a multidisciplinary perspective. Anatomy, Physiology, and Development the larynx serves three functions: connection of the upper and lower respiratory airway, closure for protection of the lower airway during swallowing, and generation of sound for voice. Identification of the maturational changes that occur in the anatomy of the aerodigestive tract and in the ontogeny of feeding and swallowing development is fundamental in delineating physiologic abnormalities and in defining the effect of compensatory strategies for improvement of laryngeal function. In terms of anatomy, there are differences in the size and location of the structures associated with the key laryngeal functions in the infant as compared with the child or adult. At birth, the larynx is positioned relatively high in the neck, located adjacent to cervical vertebrae C1 to C3, and later descending to levels C6 to C7. The thyroid cartilage of the pediatric larynx is rounded, the epiglottis may have an omega shape, and the cricoarytenoid joints and vocal processes are proportionately larger than in the adult larynx. As the infant grows, the prominent buccal pads decrease, the oral cavity increases in size, and the relative size of the tongue decreases. More space is available for differentiated tongue movements during both feeding and speaking. Elongation of the pharynx occurs as does the maturational descent of the larynx from C3 to C6 by approximately 3 years of age. As the larynx descends, increased neuromuscular control of the structural Epidemiology There is no universal, standardized clinical assessment instrument available that covers the range of ages and conditions that have accompanying pediatric dysphagia. Therefore standardized data collection and reporting are not possible, and the true epidemiology of pediatric dysphagia is largely unknown in infants and children. Available assessment protocols are targeted toward specific age ranges and condition types, for example, for characterizing preterm infant feeding behaviors, assessing oral motor skill development, and documenting signs and symptoms of dysphagia in specific diagnoses or conditions. It has been widely reported that at least 25% of typically developing children experience some type of feeding difficulty, such as chewing difficulty, choking, or texture refusal. Knowledge of the specific mechanisms of dysphagia associated with congenital and acquired medical conditions is essential. Adverse consequences of dysphagia include inadequate nutritional intake and the aspiration of secretions, food, and liquid leading to potential pulmonary contamination, infection, and morbidity. Clinical pathways for multidisciplinary assessment, medical management, and dysphagia treatment are discussed. Collaboration and communication are essential between services to ensure comprehensive assessment and optimal management. There are further structural and regulatory interrelationships within the brainstem, specifically the medulla. Anatomic changes in oral and pharyngeal structural relationships, as well as maturation of the central nervous system during the first 2 years of life, are reflected in the transition to mature oral motor/feeding and swallowing skills.
Syndromes
- Have you lost any weight recently?
- Endoscopic retrograde cholangiopancreatography (ERCP)
- Tenderness
- Rest completely (other than walking for daily activities) for at least 2 weeks.
- Highlight possible fears, anxieties, or guilt specific to sexual behaviors or performance
- Bone that is sticking through the skin
- Clobetasol propionate
- Infertility and failure to develop normal male genitals
- Loss of muscle function or feeling
- Nasal mucosal biopsy
Purchase 100 mg norpace with visa
Percutaneous thoracic duct embolization as a treatment for intrathoracic chyle leaks in infants treatment 8th feb norpace 150mg without a prescription. Hemothorax as a complication of subclavian vein cannulation with haemodialysis catheter-case report. The absorption of atmospheric air will take place within hours, whereas oxygen is absorbed within minutes. Foreign bodies in the lower respiratory tract may lead to partial or complete occlusion of a bronchus, and complete occlusion will cause atelectasis. With an initial incomplete occlusion, the foreign body may cause inflammation of the mucous membranes, with resulting mucosal swelling and increased respiratory secretions causing complete obstruction of the bronchial lumen and the development of atelectasis. Misplaced endotracheal intubation may cause total collapse of one lung when the distal part of the tracheal tube is located in a main bronchus (most often the right one). Inflammatory processes within the bronchial tree are among the most common causes of obstruction of the bronchial lumen, including bronchial asthma (often eosinophilic inflammation)6 and acute bronchiolitis due to respiratory syncytial virus infections. Destruction of the bronchial epithelium may alter the airway surface liquid, with an effect on surfactant function; it may thus enhance the tendency for bronchial collapse. In both bronchopulmonary dysplasia and respiratory distress syndrome of prematurity, abnormal surfactant function may contribute to the formation and persistence of atelectasis. Many diseases increase the susceptibility of the respiratory tract to infection and lead to the accumulation of mucus, which predisposes to the development of atelectasis. These 1027 the word atelectasis stems from two Greek words: ateles, meaning "imperfect," and ektasiz, meaning "expansion. Congenital atelectasis is usually due to incomplete expansion of the lungs, including primary and secondary congenital atelectasis. The most common cause of atelectasis is loss of air in lung tissue that was previously expanded, thus resulting in the collapse of a lung or lung tissue. Etiology and Pathogenesis Several mechanisms associated with a variety of pulmonary and extrapulmonary diseases may cause atelectasis. Pulmonary causes include obstruction of the bronchial lumen (the most common cause) and increased surface tension of the fluid lining the respiratory tract and alveoli. Extrapulmonary causes include compression of airways and lung tissue from outside the lung and weakness of respiratory muscles in neuromuscular disease. Obstruction of the bronchial lumen by mucus may have several causes, such as airway inflammation and impaired clearance of airway mucus caused by increased mucous viscosity (cystic fibrosis), reduced ciliary function, or a weak cough reflex secondary to neuromuscular disease. Pathogenic Mechanisms Congenital pulmonary airway malformations may prevent the normal aeration of parts of the lungs at birth due to lack of communication of the main bronchial tree with the affected parts of the lungs that have never been inflated, thus causing primary atelectasis. However, a secondary atelectasis may develop shortly after birth if a congenital malformation occludes or narrows the bronchial lumen, thus presenting as a differential diagnosis to primary atelectasis. At more proximal levels no such collateral communications exist, and occlusion of the bronchial lumen initially leads to air trapping in lung tissue peripheral to the occluded bronchus. Congenital atelectasis is due to incomplete expansion of the lungs, including primary and secondary congenital atelectasis, whereas the most common causes of later atelectasis are loss of air in lung tissue previously expanded or collapse of a lung or lung tissue. Occlusion of the bronchial lumen is the most common cause and may be due to airways inflammation and mucous plug, to increased viscosity of the bronchial mucus and to foreign bodies, among other causes. In occlusion of the bronchial lumen, the air of the occluded lung tissue has gradually been absorbed by the perfusing blood. The middle right lobe is often the location of atelectasis caused by pulmonary infections as bronchiolitis or airways inflammation during asthma and is often called middle-lobe syndrome. Atelectasis may occur without clinical signs; plain chest radiography at end-inspiration is important for diagnosis. Multislice computed tomography may point to the diagnosis when plain x-rays do not suffice, and magnetic resonance imaging is well suited for the diagnosis and follow-up of atelectasis. Bronchography combined with diagnostic and therapeutic bronchoscopy may be diagnostic in selected cases. Chest physiotherapy is often the first-line treatment, but its efficacy is not yet proven. Middle-lobe atelectasis has been associated with positive bacterial cultures; in such cases antibiotic treatment may be tried. Bronchoalveolar saline lavage with or without direct instillation of dornase alfa has been tried on rare occasions, and lobectomy has been tried in cases of persistent right-middle-lobe and left-lower-lobe syndrome not responding to intensive medical therapy. Stent placement has been tried in carefully selected patients, with biodegradable stents offering a new alternative. Infants with bronchiolitis who develop lobar atelectasis are more likely to have severe disease and require admission to the intensive care unit,17 while exhaustion and sudden severe deterioration may indicate the development of massive atelectasis affecting a whole lung. Preterm infants with bronchiolitis are at higher risk of developing atelectasis,17 and younger children in general are more at risk of developing atelectasis than older children and adults owing to less well developed collateral ventilation effected by the pores of Kohn and the canals of Lambert. Atelectasis may not cause detectable abnormalities on clinical examination; thus the diagnosis must be made radiologically. There may be impaired oxygen saturation, decreased expansion of the chest on the affected side, dullness to percussion, and diminished or absent breath sounds. If the atelectasis is partial or airway obstruction is not complete, crackles may be heard during inspiration and expiration. In some cases of significant or even whole-lung atelectasis, oxygen saturation may be normal, since alveolar hypoxia can induce reflex vasoconstriction and thus minimize ventilation/ perfusion mismatch. Paradoxically, intubation and mechanical ventilation of such patients with supplemental oxygen may cause a temporary deterioration in oxygen saturation due the abolition of the protective vasoconstrictive reflex, thus inducing intrapulmonary shunting and the perfusion of unventilated, atelectatic lung tissue that does not take part in gas exchange. Bronchiectasis, usually caused by recurrent or long-standing airway inflammation, is often complicated by atelectasis. Rounded atelectasis, seen more often in adults than children, is mostly asymptomatic and associated with chronic pleural disease, lung fibrosis, or pleural effusions. Diagnosis the prompt diagnosis of atelectasis in children is important, since early detection and subsequent treatment may lead to an improved outcome. For example, postoperative atelectasis is not uncommon, particularly in children undergoing cardiac surgery. Flexible bronchoscopy has a role in the diagnosis of atelectasis when there is suspected airway obstruction due to , for example, foreign-body inhalation, mucous plugging, endobronchial tuberculosis, airway malacia, external compression from a vascular ring, enlarged lymph nodes, or an enlarged heart. The most frequently used modality for the diagnosis of atelectasis is chest radiography. Frontal projection is always included, but sometimes lateral views are better suited, as in atelectasis of the right middle lobe and the lower lobes. Sometimes fluoroscopy is also used to delineate difficult locations of increased opacification. Fluoroscopy may also be used to diagnose air trapping and mediastinal shift when a foreign body is suspected. In older children, however, an x-ray at end-inspiration followed by another at end-expiration will suffice. Shift of the mediastinum and tracheal contours toward the affected side is quite common, but these general signs may be absent if emphysema develops in the ipsilateral lung or if the atelectasis occurs together with ipsilateral pleural effusion. A summary of major findings on chest radiography related to extent and location of the atelectasis is presented in Table 70. The use of a controlled ventilation protocol reduces the frequency of atelectasis in these children. Chest radiograph shows atelectasis of the right upper lobe and elevation of the interlobar fissure. Computed tomography after sedation shows extensive dependent atelectases in both lungs (Video 70. Bronchiectasis is most pronounced in the atelectatic left-sided middle lobe (Video 70. Ultrasound shows atelectasis of the left lung (a), which is clearly seen next to pleural effusion (p) (Video 70. Bronchography is rarely used but may be combined with diagnostic and therapeutic bronchoscopy in selected cases to show short segments of localized stenosis or bronchomalacia. Treatment and Management the cause of the atelectasis and the presence of any preexisting condition will determine the type of treatment and the need for future prophylactic measures.
Purchase discount norpace online
Chest tube insertion is indicated for a tension pneumothorax or simple pneumothorax associated with respiratory distress or shock symptoms bone cancer discount 100mg norpace with visa. Prompt relief and pulmonary expansion can be anticipated if the source of the intrapleural air has been controlled. If the pulmonary air leak persists or recurs, the possibility of tension pneumothorax is circumvented by the insertion of one or more intercostal tubes connected to water-seal drainage with low-pressure suction. Most instances of traumatic tension pneumothorax require tube drainage for permanent decompression, although needle aspiration is indispensable for emergency management. Stubborn bronchopleural fistulas that continue to remain widely patent despite adequate intercostal tube drainage may need thoracotomy and repair or resection of the affected lung segment. An open pneumothorax ("sucking" chest wound) in which atmospheric air has direct, unimpeded entrance into and exit from the pleural space is a second, equally urgent, thoracic emergency. Ingress of air during inspiration and egress during expiration produce an extreme degree of paradoxical respiration and mediastinal flutter, which is partially regulated by the size of the chest wall defect in comparison with the circumference of the trachea. If a considerable segment of chest wall is open, more air is exchanged at this site than through the trachea, because the pressures are similar. Inspiration collapses the ipsilateral lung and drives its alveolar air into the opposite side. Obviously, under these circumstances, little effective ventilation is taking place because of the tremendous increase in the pulmonary dead space and the decrease in tidal volumes. The diagnosis is readily made by inspection of the thoracic wound and the peculiar sound of air rushing in and coming out of the wound. This acts as a one-way valve allowing air to escape from the pleural space on expiration but sealing and preventing further air entry on inspiration. Hemothorax Blood in the pleural cavity is perhaps the most common sequel of thoracic trauma, regardless of type. Bleeding sources are abundant, with either systemic (high pressure) or pulmonary (low pressure) sources. Systemic bleeding usually originates in the chest wall from the intercostal vessels. Tracheobronchial Trauma Rupture of the trachea or bronchus in infants and children is usually preceded by a sharp blow to the anterior part of the neck (clothes-line injury), by penetrating injuries, or severe compression injury of the chest against a closed glottis. Discontinuity of a major airway is characterized by intrathoracic tension phenomena. When the leak is massive, unilateral or even bilateral pneumothorax is present compromising not only the respiratory function, but also cardiac venous return. Proximal upper airway lesions often present with pneumomediastinum and subcutaneous emphysema, followed by bilateral pneumothorax. This is due to the intramediastinal location of the trachea, directing any air leak to this space, which is in continuity with the neck compartments. When the distal airway is involved, the air leak opens easily into the pleural space causing tension pneumothorax and a persistent air leak. Conventional chest radiographs may show pneumomediastinum, pneumothorax, and subcutaneous emphysema. Air tracheobronchogram can suggest the diagnosis in the presence of a compatible clinical picture. The initial management of bronchial rupture consists of maintenance of a patent airway and decompression of the pleura and mediastinum by thoracostomy tubes connected to closed drainage with suction. Occasionally, multiple tubes may be necessary for control of the associated air leak. Tracheobronchial transection with massive air leak resulting in the inability to ventilate is the rare indication to clamp a thoracostomy tube. This should be followed by emergent, expeditious transport to the operating room for bronchoscopy and immediate repair of the defect, as this maneuver may result in tension pneumothorax. Operative repair requires thoracotomy, usually primary repair, and reinforcement with a pleural or muscular flap. Small iatrogenic injuries related to placement of an endotracheal tube may heal with conservative management. Additionally, small traumatic injuries confirmed by bronchoscopy without signs of sepsis, evidence of major connection with the mediastinal space, or associated esophageal injuries may be amenable to nonsurgical treatment. Smaller tears may heal spontaneously with tracheostomy alone; others result in stricture and require selective operative repair. Once the period of emergency is over, operative debridement and closure of the chest wound is necessary. Hemorrhage from pulmonary vessels is usually self-limiting unless major tributaries have been transected. It is important to note that a child can accumulate about 40% of his/her blood volume in the chest. The immediate findings are those of blood loss compounded by respiratory distress. The trachea and apical impulse may be dislocated, the percussion note is flat, and the breath sounds are indistinct. The actual diagnosis is confirmed by thoracentesis if time allows after adequate radiographic studies. Management of hemothorax is accomplished by total evacuation of air and blood with a large-bore chest tube. Most often, the evacuation of blood will obliterate the pleural space, and pleural apposition will tamponade parenchymal bleeding. Small-volume hemothorax may be safely observed as long as cardiorespiratory mechanics are not altered. Clotting, loculation, and infection may supervene despite vigorous initial therapy. Publications from the adult literature support early thoracoscopy and drainage of the retained hemothorax in order to avoid late infections. With the development of a fibrothorax, the lung becomes incarcerated and the chest wall is immobilized, chronically altering cardiorespiratory dynamics. These injuries are associated not only with pulmonary, but also with hepatic and cardiac contusions. Distribution of this force to the great veins of the mediastinum and jugular system leads to venous distention. Extravasation of blood, purplish edema of the head, neck, and upper extremities, and possible central nervous system changes due to intracerebral edema and petechial hemorrhages may also occur with traumatic asphyxia. The pulmonary contusion is represented pathologically by edema, hemorrhage, and atelectasis. Clinically, there may be dyspnea, cough, chest pain, hemoptysis, hypoxia, hypercarbia, and mental confusion. The face and the neck can be grotesquely swollen, with crepitus and submucosal/subconjunctival hemorrhage. There is no need for evidence of external trauma or fractured ribs in a child, and accordingly, the indication for chest radiograph is merely the possible history of a blast, acceleration (fall), or deceleration (automobile) injury. Pulmonary contusions, hemothorax, pneumothorax, and pneumomediastinum may all be encountered. With mild injuries, the subcutaneous emphysema and purplish hue gradually and spontaneously disappear over several days. Patients with more serious blast injuries are initially treated for anoxia and hypotension, and attention is then directed to atelectasis, pulmonary edema, and pleural complications. Rapid progression of the mediastinal and subcutaneous emphysema indicates a serious disruption of the trachea, bronchi, or lungs, and may require intercostal tube drainage or even thoracotomy. The possibility of injury to the heart also exists in the presence of blunt trauma to the anterior hemithorax, laceration from fractured sternum or ribs, or severe compression between the sternum and the vertebral column. The most common mechanism is blunt trauma, which is most often sustained by adolescent patients in motor vehicle collisions. The clinical manifestations of a myocardial contusion are arrhythmia, hypotension and, in severe cases, aneurysms from myocardial wall weakness. Blood loss with perforation varies from exsanguination, to cardiac tamponade, to minimal bleeding.

Buy genuine norpace line
Surfactant protein-C promoter variants associated with neonatal respiratory distress syndrome reduce transcription treatment kitty colds order norpace 150mg mastercard. Surfactant protein-B 121ins2 heterozygosity, reduced pulmonary function, and chronic obstructive pulmonary disease in smokers. Two novel mutations in surfactant protein-C, lung function and obstructive lung disease. Pulmonary alveolar proteinosis: a spectrum of cytologic, histochemical, and ultrastructural findings in bronchoalveolar lavage fluid. Diagnosis of pulmonary histiocytosis X by immunodetection of Langerhans cells in bronchoalveolar lavage fluid. Intraoperative chest tube removal following thoracoscopic lung biopsy results in improved outcomes. Bronchoalveolar lavage protein biomarkers in children with surfactant dysfunction mutations; an aptamer proteomics approach. Diagnostic value of transbronchial, thoracoscopic, and open lung biopsy in immunocompetent children with chronic interstitial lung disease. Although some respiratory diseases occur rarely in the pediatric population, knowledge of these disorders is valuable from a number of perspectives. Timely diagnosis and treatment of rare disorders can be made only if the practitioner is familiar with the entity in question. Furthermore, elucidation of the pathophysiology underlying rare disorders can be applied to understanding both normal respiratory physiology and related but more prevalent disorders. This article characterizes both selected disorders with a primary respiratory component and respiratory disease occurring secondary to systemic disorders, with emphasis on interstitial lung disease. Foundations provide invaluable information, support, and advocacy to families and patients affected by rare diseases and also function as important resources for practitioners. These patients may display a less severe pulmonary component and may 817 Respiratory Disorders of the Lymphatic System A number of rare disorders related to dysregulation of lymphatic development occur in pediatric patients from infancy to adolescence. The normal pulmonary lymphatic system is composed of two interconnected pathways: one drains the subpleural space and outer surface of the lung, while the other follows bronchovascular bundles to drain the deeper portions of the lung (see Chapters 6 and 36). In disorders that present outside of the neonatal period, such as lymphangiomatosis, disease is associated with abnormalities of lymphatic growth. Furthermore, a significant number of children with pulmonary lymphatic disorders also manifest lymphatic involvement of other organ systems, congenital cardiac disease, and chromosomal disorders. Respiratory disorders of the lymphatic system may present at any age and include pulmonary lymphangiectasia, lymphangioma, and lymphangiomatosis. Lymphangioleiomyomatosis is a distinct disease that presents with dyspnea, pneumothorax, and pulmonary cysts. Pulmonary alveolar microlithiasis is often asymptomatic in the pediatric population despite impressive radiologic findings with chest imaging. Pulmonary manifestations of ataxia telangiectasia, Gaucher disease, Niemann-Pick disease, and dyskeratosis congenita can lead to severe respiratory disease. Lung disease due to neurofibromatosis or Hermansky-Pudlak syndrome typically occurs in adults but can be severe. Although alpha-1 antitrypsin deficiency rarely, if ever, causes pulmonary disease in pediatric patients, knowledge of the disorder holds value for pediatric respiratory practitioners related to implications for genetic screening and patient/provider education. In later-presenting forms, initial symptoms include chronic tachypnea, recurrent cough, and wheezing. Because lymphangiectasia may be part of a systemic dysplasia, consideration should also be given to careful evaluation for extrapulmonary disease manifestations, such as gastrointestinal involvement, bone disease, or skin lesions from draining lymphatics. Chest radiography often reveals interstitial infiltrates and hyperinflation, with or without pleural effusion. One report suggests improved survival with aggressive interventions and modern neonatal intensive care. Both children presented with nonspecific respiratory symptoms and recurrent pneumonia without identification of pathogens; neither had overt extrapulmonary manifestations of lymphatic dysplasia. Lung biopsy shows septal widening with prominent and muscularized lymphatics (D and E, hematoxylin and eosin), as illustrated by D240 immunostaining highlighting the lymphatic endothelium (F). Lymphangioma, Lymphangiomatosis, and Gorham-Stout Disease Abnormal proliferation of lymphatic vessels distinguishes lymphangioma, lymphangiomatosis, and Gorham-Stout disease from other lymphatic disorders of the lung. Whereas lymphangioma refers to a solitary malformation, lymphangiomatosis refers to the presence of multiple lymphangiomas and is less common than the occurrence of a single lymphangioma. Gorham-Stout disease is a related syndrome characterized by chylothorax and bone cysts, with lymphangioma seen on biopsy. Lymphangiomatosis is a severe disease characterized by the occurrence of numerous lymphangiomas, often affecting multiple organs. Involvement of the liver, soft tissue, spleen, bones, mediastinum, and lungs may occur. Individuals with thoracic involvement may present with cough, chest pain, dyspnea, or wheezing. Medical therapy for lymphangiomatosis using sirolimus or interferon alpha-2b has been reported, with the aim of halting the lymphatic proliferation that is the hallmark of the disease. Phosphate is a waste product of this degradation and will build up in cells unless properly removed. Sarcoidosis, tuberculosis, histoplasmosis, and idiopathic pulmonary hemosiderosis can be considered in the differential diagnosis. This accumulates within macrophages and is identified pathologically as Gaucher or foam cells. In the lung, infiltration of Gaucher cells may occur within alveoli, interstitial spaces, around airways, or within pulmonary vasculature. Respiratory manifestations include recurrent infections related to immunodeficiency, chronic aspiration due to swallowing dysfunction, ineffective airway clearance, and interstitial lung disease. Most patients die young of respiratory causes or malignancies, with a disparately higher mortality rate among African Americans historically. Patients with recurrent respiratory infections and poor vaccine responses are candidates for immunoglobulin replacement therapy. Neuromuscular involvement, discoordinated swallowing, and impaired mucociliary clearance should be evaluated and managed, as for many patients susceptible to these disorders. Lung function measurement can be challenging because of neurologic abnormalities but can be useful to define bronchodilator response and to monitor lung function over time. In the lung, buildup of foam cells containing sphingomyelin occurs within alveoli, alveolar walls, lymphatic spaces, and the pleural space. However, a number of pulmonary complications, including pulmonary fibrosis and hepatopulmonary syndrome, have been described after bone marrow transplantation. Familiarity with the disorder is of value to pediatric pulmonologists since pediatric practitioners are responsible for educating patients and families regarding genetic testing and providing anticipatory guidance for those who carry the diagnosis. Neutrophil elastase degrades elastin and extracellular matrix elements located within the lower respiratory tract that normally function to maintain the structural integrity of the lung. In addition to cigarette smoking, exposure to kerosene heaters, employment in agriculture, and exposure to other pollutants from biomass fuel sources have all been implicated in the development of emphysema. Summary Rare lung disorders influence the care of children with respiratory diseases in a number of fundamental ways. Understanding of normal biologic function is often facilitated via characterization of the disrupted pathways occurring in rare diseases. This knowledge can then be applied to related diseases that occur with higher prevalence. Concerns exist regarding the psychological ramifications of being diagnosed during childhood with a disease that may not manifest for decades, if at all. Clinical improvement of diffuse lymphangiomatosis with pegylated interferon alfa-2b therapy: case report and review of the literature. Multifocal infiltrative lymphangiomatosis in a child and successful treatment with sirolimus. Gorham-Stout syndrome in a male adolescent-case report and review of the literature. Gorham-Stout syndrome with chylothorax: successful remission by interferon alpha-2b. Gorham-Stout Disease successfully treated with sirolimus and zoledronic acid therapy. Marked smooth muscle cell proliferation of the lung in a preadolescent girl with repeated pneumothorax and progressive dyspnea.
Purchase cheap norpace
Although spine fusion was once considered as first-line therapy medicine 2015 buy online norpace, long-term follow-up studies on children fused while growing have demonstrated significant restrictive chest wall disease proportional to the length of spine that was fused and the location of the apex prior to surgery. Recently, a growth-friendly device that can be advanced noninvasively using a magnetically driven mechanism has been approved for clinical use, dramatically reducing the number of operative expansion procedures for each growing child. This device has reduced the cumulative complication rate for repeated surgeries as well. Depending on the duration and amount of growth remaining, each of these devices must be replaced with a larger version after several years. Preliminary results obtained a few years after surgery suggest that this procedure promotes continued spine growth even for abnormal vertebrae, with no increase in curve amplitude. Postoperative studies with serial measurements of vital capacity under anesthesia over 3 years demonstrated an improvement in absolute lung volume but no change or slight loss of lung function expressed as a percentage of predicted norms. Over this longer interval, serial measurements of vital capacity fell by 28% of predicted normal values, suggesting that current surgical treatments do not maintain normal lung growth despite some degree of spine curve correction. There is some suggestion that lung function may be better preserved when children undergo nonfusion surgical correction of the scoliosis when they are less than 6 years of age. However, to reduce surgical complications, several spine centers resort to serial casting in children less than 5 years of age, followed by surgical intervention in those who do not improve. The effect of serial casting on pulmonary function over time has not been reported. The surgical strategy for an individual child is developed on a case-by-case basis, and varies among spine centers according to local experience and expertise. Preoperative halo traction has been used to minimize the severity of the spine curvature prior to surgery, particularly when the spine is flexible. The issues in patients with neuromuscular diseases are more complex (severity of deformity, pelvic obliquity, associated nutritional, neurological, and cardiopulmonary problems). Although surgery provides significant benefit with regard to quality of life, the consequences on long-term pulmonary function depend on the underlying disease and the nature of the spine deformity. New surgical devices are now being proposed to improve the severe lordosis that occurs in children with spina bifida. One device is attached from rib to rib (shorter device on the lateral film) and one is attached from ribs to the spine. Therefore preoperative assessment of pulmonary function, including overnight oximetry and the assessment of hypercapnia, should be performed as a guide to prevent and treat postoperative complications. Children with skeletal dysplasia and those with cervical vertebral involvement often have upper airway obstruction and pose intubation challenges at the time of surgery. The most frequent respiratory problems reported in the immediate postoperative course of surgery for scoliosis include atelectasis, pneumonia, pulmonary edema, pulmonary fat emboli, and respiratory failure. Immediate pulmonary complications result from multiple factors such as the surgical procedure itself, the degree of preoperative pulmonary disability, the intraoperative fluid management, the transient limitation of chest wall expansion as a result of pain, and the effects of anesthetics and analgesics. In neuromuscular diseases, respiratory muscle weakness, cough impairment, and swallowing disorders increase the risk of immediate postoperative pulmonary complications. Children with adolescent idiopathic scoliosis whose vital capacities are less than 40% predicted have a three-fold increase in pulmonary complication rate following spine fusion compared to those with better preoperative lung function. Noninvasive ventilation and mechanical in-exsufflation devices can be of invaluable help in patients with and without neuromuscular weakness in the immediate postoperative period. Spine fusion reduces the spinal curvature, but improvements in lung volume and arterial oxygenation only become apparent late after surgery. The decrease in vital capacity usually lasts for 6 weeks to 3 months after fusion but can persist for up to 1 year. Combined anterior fusion and posterior spine fusion is more likely than posterior fusion alone to impair lung function postoperatively for longer periods; the combined fusion approach also reduces the likelihood of further scoliosis postoperatively. Management of Hypoplastic Thorax Syndromes the recent development of expandable titanium devices has led to novel interventions with short-term respiratory improvements over several years, although the long-term outlook-even with these new surgical interventions- remains unclear. Several surgical procedures have been proposed and used clinically to increase thoracic cage size. These include the interposition of adjacent ribs with titanium connectors to make the existing ribs longer. The latter can then be regularly expanded to increase the thorax as the child grows. Children with Jarcho-Levin syndrome have received growth-friendly spine distraction devices to further increase thoracic height and width, although lung function following surgical interventions has not been reported. Sleep, sleep disordered breathing, and nocturnal hypoventilation in children with neuromuscular diseases. Congenital and childhood myotonic dystrophy: current aspects of disease and future directions. Systematic review of surgical treatment techniques for adult and pediatric patients with pectus excavatum. Extent of spine deformity predicts lung growth and function in rabbit model of early onset scoliosis. The characteristics of thoracic insufficiency syndrome associated with fused ribs and congenital scoliosis. Sleep-disordered breathing in Duchenne muscular dystrophy: an assessment of the literature. Improvement of survival in Duchenne muscular dystrophy: retrospective analysis of 835 patients. Self-reported quality of life and depressive symptoms in children, adolescents, and adults with Duchenne muscular dystrophy: a cross-sectional survey study. Quality of life of adult men with Duchenne muscular dystrophy in the Netherlands: implications for care. Quality of life of patients with Duchenne muscular dystrophy: from adolescence to young men. Neuropsychological and neurobehavioral functioning in Duchenne muscular dystrophy: a review. Relationship between peak cough flow and spirometry in Duchenne muscular dystrophy. Assessment of sleep-related breathing disorders in patients with Duchenne muscular dystrophy. The sleep characteristics in symptomatic patients with Duchenne muscular dystrophy. Increasing severity of pectus excavatum is associated with reduced pulmonary function. Evaluating cardiopulmonary response in pediatric patients with pectus excavatum using the james cycle ergometer protocol. Predictors of change in postoperative pulmonary function in adolescent idiopathic scoliosis: a prospective study of 254 patients. Obstructive lung disease is common in patients with syndromic and congenital scoliosis: a preliminary study. Phenotype characterization and natural history of spondylothoracic dysplasia syndrome: a series of 27 new cases. Prediction of thoracic dimensions and spine length on the basis of individual pelvic dimensions: validation of the use of pelvic inlet width obtained by radiographs compared with computed tomography. Spinal muscular atrophy type I: do the benefits of ventilation compensate for its burdens Spinal muscular atrophy type 1: are proactive respiratory interventions associated with longer survival Palliative care in children with spinal muscular atrophy type I: what do they need Long-term effects of lung volume recruitment on maximal inspiratory capacity and vital capacity in duchenne muscular dystrophy. Twenty-four hour noninvasive ventilation in Duchenne muscular dystrophy: a safe alternative to tracheostomy. Efficacy of mechanical insufflation-exsufflation in extubating unweanable subjects with restrictive pulmonary disorders. Surgical management of severe scoliosis with high-risk pulmonary dysfunction in Duchenne muscular dystrophy. Dysphagia in Duchenne muscular dystrophy: practical recommendations to guide management. Evolving paradigms in clinical pharmacology and therapeutics for the treatment of Duchenne muscular dystrophy. Practice guideline update summary: corticosteroid treatment of Duchenne muscular dystrophy: Report of the Guideline Development Subcommittee of the American Academy of Neurology.
Buy norpace once a day
A multicenter symptoms jet lag discount norpace online amex, prospective, randomized, double-blind, placebo-controlled trial of corticosteroids and intravenous cyclophosphamide followed by oral azathioprine for the treatment of pulmonary fibrosis in scleroderma. Systemic sclerosis and bilateral lung transplantation: a single centre experience. Childhood sarcoidosis in Denmark 1979-1994: incidence, clinical features and laboratory results at presentation in 48 children. Mycobacterial catalase-peroxidase is a tissue antigen and target of the adaptive immune response in systemic sarcoidosis. Development of a sarcoidosis murine lung granuloma model using Mycobacterium superoxide dismutase A peptide. Endobronchial involvement and airway hyperreactivity in patients with sarcoidosis. The value of endoscopic ultrasound after bronchoscopy to diagnose thoracic sarcoidosis. Endobronchial ultrasoundguided transbronchial needle aspiration prevents mediastinoscopies in the diagnosis of isolated mediastinal lymphadenopathy: a prospective trial. Paralysis and a perihilar protuberance: an unusual presentation of sarcoidosis in a child. Methotrexate is steroid sparing in acute sarcoidosis: results of a double blind, randomized trial. Effective reduction in the serum 1,25-dihydroxyvitamin D and calcium concentration in sarcoidosisassociated hypercalcemia with short-course chloroquine therapy. Effectiveness of chloroquine and hydroxychloroquine in treating selected patients with sarcoidosis with neurological involvement. Infliximab therapy in patients with chronic sarcoidosis and pulmonary involvement. The clinical course of sarcoidosis: presentation, diagnosis, and treatment in a large white and black cohort in the United States. Severe pulmonary hypertension in pediatric primary Sjogren syndrome: a case report. The American College of Rheumatology 1990 criteria for the classification of Churg-Strauss syndrome (allergic granulomatosis and angiitis). Clinical and immunological features of drug-induced and infection-induced proteinase 3-antineutrophil cytoplasmic antibodies and myeloperoxidase-antineutrophil cytoplasmic antibodies and vasculitis. Wegener granulomatosis in children and adolescents: clinical presentation and outcome. Wegener granulomatosis in childhood: prolonged survival following cytotoxic therapy. Ulcerative colitis presenting with bronchiolitis obliterans organizing pneumonia in a pediatric patient. Pulmonary artery involvement as first manifestation in three cases of Takayasu arteritis. Henoch-Schonlein purpura and pulmonary hemorrhage: a report and literature review. Alveolar hemorrhage in antibasement membrane antibody disease: a series of 28 cases. The most frequent offenders are chemotherapeutic agents used in the treatment of childhood neoplasms (Table 59. Hypersensitivity lung disease, noncardiogenic pulmonary edema, pleural effusion, bronchiolitis obliterans, and alveolar hemorrhage are also encountered. Although some drug-induced pulmonary damage is reversible, persistent and even fatal dysfunction may occur. Lung reactions occasionally are temporally remote from exposure to chemotherapeutic agents. The mechanism of toxicity is thought to be direct injury to lung cells in most cases, but immunologic and central nervous system-mediated mechanisms seem to play a role in the toxicity of certain agents. Identified risk factors associated with cytotoxic drug therapy vary, but they include cumulative dose, age of patient, prior or concurrent radiation, oxygen therapy, and use of other toxic drugs. When patients are treated with combinations of potentially toxic drugs or with a toxic drug plus irradiation to the chest or high concentrations of oxygen, as is common in the treatment of childhood cancers, specific offenders often cannot be identified. There is little if any evidence that children are more susceptible to drug-related pulmonary injury, and in fact, they may be less susceptible to some agents such as bleomycin. The clinical presentation of drug-induced lung disease often includes fever, malaise, dyspnea, and nonproductive cough. Radiologic studies almost always demonstrate diffuse alveolar and/or interstitial involvement. Segmental or lobar disease, particularly if unilateral, should suggest another diagnosis. Abnormal pulmonary function, indicative of restrictive or obstructive disease, may be found before appearance of roentgenographic lesions. Its major use in children is in the treatment of Hodgkin disease and other lymphomas. Because of the high frequency of pulmonary reactions and the utility of bleomycin for generating animal models of lung fibrosis, this agent has been studied more thoroughly than others. Pulmonary damage develops in two distinct patterns, most commonly progressive fibrosis and uncommonly an acute hypersensitivity reaction. Chemotherapeutic agents are most frequently implicated, although toxic effects of other medications have been recognized. Reactions to chemotherapeutic agents may be doserelated; most reactions to noncytotoxic agents develop idiosyncratically. Clinical/pathologic syndromes described include diffuse interstitial pneumonitis and fibrosis, hypersensitivity pneumonitis, noncardiogenic pulmonary edema, pleural effusion, bronchiolitis obliterans, and alveolar hemorrhage. Presenting symptoms vary but often include fever, cough, and dyspnea, and radiologic studies demonstrate diffuse alveolar and/or interstitial abnormalities. Other disorders, including infection, hemorrhage, lung disease related to underlying disease, and radiation damage, must be considered. Although some drug-induced lung injury is reversible, persistent and even fatal dysfunction may occur. Survivors of childhood cancer require follow-up as lung disease may develop remotely from drug exposure and be progressive. More precise information about risk factors, including genetic predisposition and mechanisms of injury, along with more sensitive diagnostic and monitoring approaches are needed for development of improved therapeutic strategies, including early intervention. Pulmonary disease secondary to bleomycin occurs in as many as 40% of patients receiving the drug,12 and a recent systematic review identified bleomycin exposure (along with alkylating agents) as a significant risk factor for longterm pulmonary toxicity. When more than 283 mg/m2 is administered, 50% of adult patients develop severe pneumonitis. The combination of radiotherapy or high inspired oxygen concentrations and bleomycin produces more lung injury than either alone. Pulmonary toxicity associated with relatively small quantities of bleomycin has been reported during combination drug therapy,18 and pediatric sarcoma or Hodgkin disease patients receiving bleomycin have increased risk for radiation pneumonitis. Direct toxicity may be mediated by oxidant injury, either through the production of reactive oxygen metabolites or through inactivation of antioxidants. Data supporting this mechanism include the findings that pretreatment of rodents with antioxidants, or upregulation of the antioxidant gene transcription factor Nrf2, can reduce subsequent bleomycin-induced pulmonary fibrosis. As the illness progresses, there is a decline in vital capacity and total lung capacity, which is characteristic of restrictive lung disease. In both interstitial pneumonitis and hypersensitivity lung reactions, patients typically present with a dry hacking cough and dyspnea; these signs occur only on exertion in mild cases, but profound respiratory distress accompanies advanced illness. Chest radiographs in symptomatic patients most commonly demonstrate diffuse linear densities. Treatment with bleomycin is a significant predictor of long-term respiratory symptomatology and pulmonary function decrements in survivors of Hodgkin disease. Although pulmonary toxicity is uncommon, it does produce severe and even fatal lung damage. Cyclophosphamide appeared to result in greater pulmonary toxicity than fludarabine in one pediatric series when either agent was combined with busulfan for prehematopoietic cell transplantation conditioning. Cyclophosphamide also may predispose to toxicity when medications such as bleomycin, azathioprine, and carmustine are used subsequently. Little is known regarding the relationship of dose, duration, and frequency of administration to the appearance of parenchymal disease in humans, although cytotoxicity appears to be dose-related in rats.