Order 4 mg decadron with mastercard
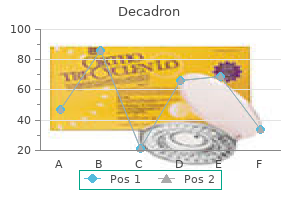
The diffuse form exten- Soft Tissue Tumors Soft tissue tumors are mesenchymal neoplasms that may arise anywhere in the body but are most commonly found within skeletal muscle acne 1cd-9 purchase cheap decadron on line, fat, fibrous tissue or blood vessels. Tumors of peripheral nerves (see Chapter 32) and other tumors of neuroectodermal differentiation may be included in the category of soft tissue tumors. Radiograph of the knee demonstrates confluent erosions of the distal femur and proximal tibia and a soft tissue mass within the joint. At higher power, the cellular infiltrate mainly consists of mononuclear histiocytic synoviocytes, many of which contain brown hemosiderin pigment, and multinucleated giant cells. Although soft tissue tumors may show evidence of differentiation toward a particular cell type (fibroblastic, adipocytic, vascular, myoid, etc. Not all soft tissue tumors can be readily classified by their line of differentiation. However, many do have characteristic and unique genomic abnormalities that are diagnostically useful (Table 30-2). Malignant soft tissue tumors (sarcomas) can metastasize via the bloodstream, usually to the lungs or bone. Patients generally die of metastatic disease rather than local invasion at the primary tumor site. The ability to distinguish sarcoma from benign mimics is key to prognostication; outcome is predicated upon both tumor grade and stage. These criteria are combined with grade and metastatic status for overall staging and risk prediction. A group of genetic disorders associated with soft tissue tumors includes neurofibromatosis type 1, tuberous sclerosis, Osler-Weber-Rendu disease, Li-Fraumeni syndrome and Gardner syndrome. Burns in childhood produce scars, which in rare instances lead to soft tissue fibroblastic tumors many years later. Radiation injury can also contribute to the development of sarcomas, in particular angiosarcoma, osteosarcoma or undifferentiated sarcoma, years after exposure. There is no evidence to support the association of trauma with the development of soft tissue tumors, and injury merely draws attention to a preexisting tumor. Rapidly growing tumors are more likely to be malignant than tumors that develop slowly. Benign tumors are relatively avascular, while most malignant ones are hypervascular. Some soft tissue tumors are classified on the basis of genetic or molecular findings. Most cases occur in young adults who present to medical attention following the rapid growth of the lesion. While nodular fasciitis was long thought to be a posttraumatic reactive condition, the discovery of a recurrent translocation and associated chimeric fusion gene has resulted in a reclassification of this tumor as a form of neoplasia. In addition, cytogenetic abnormalities involving chromosome 15 have been reported in some cases. The affected region on chromosome 15 codes for several proteins involved in tissue repair. Despite these underlying genetic alterations, nodular fasciitis is self-limited and is cured by surgical excision. Fibromatosis Is a Locally Aggressive Proliferation of Fibroblasts Fibromatosis is a locally invasive, slowly growing mass that may occur virtually anywhere in the body. Although histologically similar, there are genetic distinctions between superficial and deep "aggressive" variants of fibromatosis. Fibromatosis does not metastasize, but surgical resection of deep tumors is often followed by local recurrence. Diabetics, alcoholics and epileptics have an increased incidence of fibromatosis, as do patients with familial adenomatous polyposis. Microscopically, the lesion is composed of fascicles of bland spindle cells arrayed in long sweeping fascicles in a collagenous stroma. A photomicrograph demonstrates irregularly arranged malignant fibroblasts characterized by dark, irregular and elongated nuclei of varying sizes. Deep aggressive fibromatosis (desmoid tumor) frequently involves fascia and muscular aponeuroses of the extremities or abdominal wall musculature. Lesions are highly infiltrative and difficult to resect completely, accounting for the high recurrence rates. Fibrosarcoma Is a Malignant Tumor of Fibroblasts Many subtypes of sarcoma show evidence of fibroblastic differentiation. Pure adult fibrosarcoma is a diagnosis of exclusion, which shows no characteristic cytogenetic abnormality and accounts for less than 3% of adult sarcomas. Fibrosarcomas arise from deep connective tissue, such as fascia, scar tissue, periosteum and tendons. Macroscopically, the tumors are sharply demarcated and frequently exhibit necrosis and hemorrhage. The prognosis for high-grade adult fibrosarcoma is guarded; the survival at 5 years is only 40% and at 10 years is 30%. Other variants of fibroblastic sarcomas exist, including low-grade fibromyxoid sarcoma, myofibroblastic sarcoma and myxofibrosarcoma, among others, each with its own distinct pathologic features and clinical course. Because microscopic tongues of tumor extend between preexisting structures, surgical "shelling out" of the lesion is followed by recurrences in half of cases. Specific forms of fibromatosis are identified by their characteristic locations: Palmar fibromatosis (Dupuytren contracture) is the most common form of fibromatosis. In half of cases, the lesion is bilateral, and in 10% of cases, it is associated with fibromatosis in other locations. Fibrous nodules and cord-like bands in the palmar fascia eventually lead to flexion contractures of the fingers, particularly the fourth and fifth digits. Plantar fibromatosis is similar to palmar fibromatosis, except that it is less frequent and involves the plantar aponeurosis. Penile fibromatosis (Peyronie disease) is the least common of the localized fibromatoses. A small proportion of cases remain unclassifiable and may truly represent the most primitive undifferentiated form of sarcoma. Efforts to classify such tumors are important, as pleomorphic rhabdomyosarcoma or leiomyosarcoma may have a slightly worse prognosis. In half of the cases, tumors arise in the deep fascia or within skeletal muscle of the lower limbs. At the molecular level, it shows highly complex chromosomal rearrangements, a phenotype associated with genomic instability. The spindle cells tend to be better differentiated and often show focal fibroblastic features. Often a nonneoplastic population of tumor-infiltrating inflammatory cells is seen, including xanthomatous cells, dendritic or histiocytic cells and a moderate chronic inflammatory reaction. Some tumors contain numerous tumor giant cells, which exhibit intense cytoplasmic eosinophilia. The extent of collagen deposition varies and sometimes dominates the microscopic pattern. Immunohistochemical and ultrastructural studies are generally performed to establish a specific line of differentiation (smooth muscle, skeletal muscle, adipose tissue, etc. If no such differentiation can be demonstrated, then the tumor can be considered to be an undifferentiated pleomorphic sarcoma. The prognosis of adult undifferentiated pleomorphic sarcomas depends on the degree of cytologic atypia, the extent of mitotic activity and the degree of necrosis. Almost half of the patients develop a local recurrence after surgery, and a comparable proportion later manifest metastatic disease, particularly in the lungs. Most occur in the subcutaneous tissues of the upper half of the body, especially the trunk and neck. Lipomas are seen mainly in adults, and patients with multiple tumors often have relatives with a similar history. An angiolipoma is a small, well-circumscribed, subcutaneous lipoma with extensive vascular proliferation that usually occurs in the upper extremities and trunk of young adults. An anaplastic tumor exhibits spindle cells, plump polygonal cells, bizarre tumor giant cells and scattered chronic inflammatory cells.
Plant Protease Concentrate (Papain). Decadron.
- Herpes zoster (shingles).
- What is Papain?
- Digestion problems, diarrhea, hayfever, runny nose, psoriasis, cancer, treating infected wounds, sores, ulcers, intestinal worms, and other conditions.
- How does Papain work?
- Dosing considerations for Papain.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96115
4 mg decadron for sale
When ventricular distension is sufficiently advanced skin care products for rosacea safe decadron 8 mg, fluid will leak trans-ependymally into the white matter, causing interstitial edema. If the blockage occurs within the ventricular system itself, ventricles proximal to the block dilate, while those situated downstream from the block are spared. This is communicating hydrocephalus, meaning that ventricles are unobstructed in fluid flow. Communicating hydrocephalus may complicate subarachnoid hemorrhage or inflammation, resulting in arachnoid scarring, or may result from thrombosis of the dural venous sinuses themselves. Cerebral Edema May Occur Whenever Intracranial Pressure Increases Cerebral edema can set up a self-perpetuating cycle in which increasing edema begets increasing pressure, which in turn begets more edema. In either case, water is driven down its concentration gradient into cerebral tissues until osmotic equilibrium is reestablished. Vasogenic edema: the blood-brain barrier loosens, permitting uncontrolled entry of water into the tissues. Horizontal section of the brain from a patient who died of a brain tumor that obstructed the aqueduct of Sylvius shows marked dilation of the lateral ventricles. Water can enter the brain uncontrollably if the barrier is disrupted or if osmotic forces across it are sufficient to drive water into cerebral tissues. In infants and children, before cranial sutures have fused, the head enlarges sometimes to grotesque proportions as the ventricles dilate. As hydrocephalus is common in infants and treatable by shunting, measurement of the head circumference is a fundamental part of the pediatric physical examination. After sutures fuse, hydrocephalus cannot enlarge the head, but rather increases intracranial pressure. Remarkably, such individuals may retain substantial cognitive abilities, although spasticity may cloak the expression of this intelligence. Slow ventricular enlargement may appear clinically as progressive dementia, gait impairment and urinary incontinence as the long white matter fibers connecting portions of cortex to one another and lower motility centers are stretched apart by relentless expansion of the ventricles. This condition is usually accompanied by normal baseline intracranial pressure and so is called normal-pressure hydrocephalus, which may respond to shunting. This occurs most often in diffuse cortical atrophy, but focal destruction such as occurs at the site of an old infarct may lead to focal compensatory ventricular enlargement. However, evolutionary selection has not yet adequately responded to the need to survive motor vehicle crashes, personal assaults or dives into shallow pools. Injury to the nervous system results from the transfer of kinetic energy to the neural tissues-the degree of injury correlates with the quantity of energy delivered and the time over which it was delivered. This energy transfer may directly disrupt tissues in penetrating injuries, or the energy may be translated into movement and compression of neural structures within the skull or spinal canal in a closed injury. Extreme injury of the brain and cord is possible with minimal disruption of overlying tissues. Conversely, superficial tissues can sustain dramatic injury while the nervous system underneath remains unaltered. Epidural Hematomas Are Often Fatal Epidural hematomas usually result from blows to the head with skull fracture. The intracranial dura is securely bound to the inner aspect of the calvaria and so is analogous to the intracranial periosteum. The temporal bone, being one of the thinnest bones of the skull, is particularly vulnerable to fracture. Populations at highest risk for such injuries include children, men in late adolescence and early adulthood and the elderly. Laceration of a branch of the middle meningeal artery by the sharp bony edges of a skull fracture initiates bleeding under arterial pressure that dissects the dura from the calvaria and produces an expanding hematoma. After an asymptomatic interval of several hours, subfalcine and transtentorial herniation occur, and if the hematoma is not evacuated, lethal Duret hemorrhages will occur. The blood and granulation tissue are surrounded by a sheet of fibrous connective tissue-the "membranes" of a chronic subdural hematoma. Fibroblasts first create a membrane on the calvarial side of the hematoma, the outer membrane. Then they invade the subjacent hematoma to form a fibrous membrane subjacent to the blood clot. It may (1) be reabsorbed and leave only a small amount of telltale hemosiderin; (2) remain static, and perhaps calcify; or (3) enlarge as a result of recurrent microhemorrhages in the granulation tissue. Expansion of the hematoma, and onset of symptoms, commonly results from rebleeding, usually within 6 months. Granulation tissue is fragile and so vulnerable to minor trauma, even that caused by shaking the head. Thus, subdural hematomas can rebleed and create a new hematoma subjacent to the outer membrane. Episodes of sporadic rebleeding expand these lesions periodically and at unpredictable intervals. In addition to granulation tissue and blood, other cellular constituents include plasma cells, lymphocytes and extramedullary hematopoiesis. These may contribute to the cellular dynamics of the subdural hematoma by releasing cytokines and causing cerebral edema in the underlying brain. Stretching of meninges leads to headaches; pressure on the motor cortex produces contralateral weakness; and focal cortical irritation can initiate seizures. Subdural Hematomas Develop More Slowly Than Epidural Hematomas Subdural hematomas are a significant cause of death after head injuries from falls, assaults, vehicular accidents and sporting accidents. The hematomas expand more slowly than epidural hematomas, so their clinical tempo is slower, but once critical increased intracranial pressure is attained, clinical deterioration and death can occur with horrific rapidity. Parenchymal Injuries Produce Variable Symptomatology Traumatic brain and spinal cord injuries range in severity from temporary loss of function with little or no discernible structural damage in concussion, to intermediate damage with hemorrhage and necrosis of the tissue in contusions, to profound disruption of structure and function in lacerations. Blood drains from cerebral hemispheres through veins that cross the subarachnoid space and arachnoid to breach the dura and enter the dural sinus. There is no true subdural space per se, but the inner layer of meningothelial cells of the dura has fewer tight junctions than those in the outer layers of the dura. Since bleeding in this situation is under low venous pressure, it is slow and may stop spontaneously from a local tamponade effect. Granulation tissue forms in reaction to the blood, and the delicate capillaries of this tissue may themselves leak. This leads to gradual accumulation of an ever enlarging subacute, and ultimately chronic, subdural hematoma. A blow that causes an epidural hematoma does not necessarily produce a concussion. Consciousness depends on a functional brainstem reticular formation interacting with the cerebral hemispheres and is lost if either the reticular formation or both hemispheres are damaged. A classic example of concussion occurs in boxing, from a blow that deflects the head upward and posteriorly, often with a rotatory component. These motions impart quick rotational acceleration to the brainstem and cause dysfunction of reticular formation neurons. With head trauma, the dura moves with the skull, and the arachnoid moves with the cerebrum. As a result, the bridging veins are sheared as they cross between the dura and the arachnoid. The right hemisphere exhibits a large collection of blood in the "subdural space," owing to rupture of the bridging veins. Classically, concussion is not associated with gross neuropathology, and since the condition is not lethal, microscopic examination is not possible. Recent advances in diffusion tensor imaging suggest that axonal injury functionally disconnects the reticular activating system from the cerebral hemispheres. Axonal injury and disconnection may also account for cognitive and memory difficulties, vertigo and the feelings that "things are just not quite right" that bedevil people who have sustained "mild" traumatic brain injury. The thicker membrane (arrow) is the exterior membrane and the thinner membrane is adjacent to the brain.
Cheap decadron 0.5 mg otc
Application of the stockholm hierarchy to defining the quality of reference intervals and clinical decision limits acne upper lip decadron 8mg without prescription. Determination of reference limits: statistical concepts and tools for sample size calculation. Confidence intervals around Bayes Cost in multi-state diagnostic settings to estimate optimal performance. Optimal linear combinations of multiple diagnostic biomarkers based on Youden index. Exploring medical diagnostic performance using interactive, multi-parameter sourced receiver operating characteristic scatter plots. Hormone measures in finger-prick blood spot samples: new field methods for reproductive endocrinology. Recent advances in miniaturization-the role of microchip electrophoresis in clinical analysis. A clinically useful method for detecting gonadotropins in children: assessment of luteinizing hormone and follicle-stimulating hormone from urine as an alternative to serum by ultrasensitive time-resolved immunofluorometric assays. Diagnosis of endocrine disease: biochemical diagnosis of phaeochromocytoma and paraganglioma. Saliva as a tool for monitoring steroid, peptide and immune markers in sport and exercise science. Development and validation of a monoclonal antibody enzyme immunoassay for measuring progesterone in saliva. Assessing dehydroepiandrosterone in saliva: a simple radioimmunoassay for use in studies of children, adolescents and adults. Paired-box gene 2 is down-regulated in endometriosis and correlates with low epidermal growth factor receptor expression. Ki-ras mutations and the carcinoembryonic antigen level in fine needle aspirates of the pancreas. Serous cystadenoma of the pancreas: limitations and pitfalls of endoscopic ultrasoundguided fine-needle aspiration biopsy. Perspectives on quality control, risk management, and analytical quality management. Medical devices; pediatric uses of devices; requirement for submission of information on pediatric subpopulations that suffer from a disease or condition that a device is intended to treat, diagnose, or cure; direct final rule. With the inexorable rise in the prevalence of excess weight, this burden is growing in all regions of the world. Diabetes incidence, prevalence, and burden have all increased in recent decades, with the aging of the population being a main driver of these trends. The scenario for burden, while stabilizing in countries with the highest degree of development, is most worrisome for those in the midrange of development. Given this scenario, diabetes, when joined with states of intermediate hyperglycemia, is now also one of the top five risk factors in the world. Iodine deficiency is a highly prevalent public health problem in several countries. Incidence of thyroid cancer has increased globally over the last three decades, although a recent decline has been noted in countries with the highest level of development. The burden of thyroid cancer is higher in low-income and lowmiddle-income countries. The 21st century is now faced with new and complex demands for action at both the population and clinical levels. Of major concern, progress in alleviating disease burden has not resolved longstanding inequities, leaving the less developed countries often with a double load of disease burden, the unresolved old ones and the new ones, thus posing difficult challenges to policymakers and to global health. We will address in this chapter the burden of endocrine diseases, namely obesity and excess weight, diabetes, iodine deficiency/ thyroid goiter, and thyroid cancer, selected on the basis of their importance and the availability of reliable data. The difference in trends between (A) and (B) is caused by population growth, and the difference between (B) and (C) is caused by changes in the age distribution of the population. The total number of cases of a given disease in a specified population at a designated time. It is calculated by multiplying the prevalence of the condition causing health loss. Over the lifespan, rates of obesity decrease slightly from age 2 to the beginning of adolescence, then increase steadily from age 15 and peak between the fourth and seventh decades. This peak comes earlier and at a lower level in men than in women and in countries of lesser versus greater sociodemographic development. At the end of life, prevalence declines,4 in large part due to greater premature mortality among the obese. Although obesity rates are increasing in all geographic regions, both baseline values and rates of increase vary tremendously. In 2016, Pacific Islanders, followed by nations of the Middle East and then several higher income countries of Anglo-Saxon origin, had the greatest frequency of obesity. Examples of extreme country differences in obesity rates for women are seen comparing American Samoa (65. The fraction due to disability has risen from 22% to 28% over recent decades and is anticipated to continue to rise in importance. Like its prevalence, the burden of excess weight, though rising in all regions, is not evenly distributed among nations. The few countries shown in blue had a decrease in burden over this period and the small fraction of countries in yellow, a stable one. For those in tan, brown, light chocolate brown, and dark brown, burden has increased at annual rates of approximately 1%, 3%, 4% and 6%, respectively. The greatest increases are seen across the southern countries of Asia and much of Africa, both above and below the Sahara. Most of the Americas and much of Africa have experienced annual increases ranging from 1. Given their large population size, China, India, the United States, Brazil, and Indonesia accounted for half of all adults with diabetes in 2014. An issue that has generated great concern in recent years is the rising prevalence/incidence of diabetes among the young populations. While incidence of type 1 diabetes has risen worldwide, the increase also results from the rising incidence of type 2 diabetes in the young. Iodine deficiency produces several consequences in humans, collectively called iodine deficiency disorders. Although the number of countries in which iodine intake is adequate has increased in recent decades, many nations still have a clinically relevant prevalence of deficiency. Most of them are low-income and middle-income countries, such as Angola, Burkina Faso, Burundi, Haiti, Mozambique, Sudan, and South Sudan. However, even countries in transition, such as Russia and the Ukraine, and some high-income countries (Finland, Israel, and Italy), present problematic levels. It does not include estimates of subclinical iodine deficiency or nonvisible goiter (grade 1) induced by iodine deficiency. In fact, incidence rates are more than twofold higher in high-income countries compared with low-middle-income countries. This socioeconomic discrepancy is probably due to differences in access to diagnosis, which is more available in high-income countries. This socioeconomic discrepancy is reflecting differences in access to diagnosis and adequate treatment. These data highlight the necessity to improve iodination programs and access to care for patients with thyroid diseases through the development of infrastructure and appropriate patient management in the developing world. These actions could save costs, improve quality of life, and produce a healthier workforce. On the other hand, extension of policies involving iodine supplementation will likely continue to decrease the burden of iodine-related thyroid disease and complications. Access to early diagnosis and treatment of thyroid cancer, especially in countries at low and middle levels of development, will hopefully lead to a continuing decrease in disease burden. Association of type 1 diabetes vs type 2 diabetes diagnosed during childhood and adolescence with complications during teenage years and young adulthood. In fact, the National Guideline Clearinghouse website had 1500 available guidelines with more than 100 guidelines related to endocrine diseases. Moreover, patient panels formulate similar recommendations when compared to physician panels when presented with evidence warranting moderate to high confidence.
Order decadron on line
Transcriptional regulation of growth hormone gene expression by growth hormonereleasing factor acne questionnaire buy cheap decadron 8mg online. Interrelationship between the novel peptide ghrelin and somatostatin/growth hormone-releasing hormone in regulation of pulsatile growth hormone secretion. Novel and conventional receptors for ghrelin, desacyl-ghrelin, and pharmacologically related compounds. Autocrine/paracrine roles of extrapituitary growth hormone and prolactin in health and disease: an overview. Nuclear targeting of the growth hormone receptor results in dysregulation of cell proliferation and tumorigenesis. Fasting enhances growth hormone secretion and amplifies the complex rhythms of growth hormone secretion in man. Leptin regulates growth hormone-releasing factor, somatostatin, and alpha-melanocyte-stimulating hormone but not neuropeptide Y release in rat hypothalamus in vivo: relation with growth hormone secretion. Acute administration of corticoids: a new and peculiar stimulus of growth hormone secretion in man. Activation of the somatotropic axis by testosterone in adult males: evidence for the role of aromatization. Insulin and insulinlike growth factor-I acutely inhibit surface translocation of growth hormone receptors in osteoblasts: a novel mechanism of growth hormone receptor regulation. Distribution and abundance of messenger ribonucleic acid for growth hormone receptor isoforms in human tissues. A common polymorphism of the growth hormone receptor is associated with increased responsiveness to growth hormone. Mechanisms in endocrinology: clinical and pharmacogenetic aspects of the growth hormone receptor polymorphism. Differential kinetics of hormone desensitization and growth hormone stimulation of both tyrosine phosphorylation and serine/threonine phosphorylation. Stat5a and Stat5b proteins have essential and nonessential, or redundant, roles in cytokine responses. The pattern of growth hormone delivery to peripheral tissues determines insulin-like growth factor-1 and lipolytic responses in obese subjects. Identification and characterization of specific binding proteins for growth hormone in normal human sera. Growth hormone receptor and serum binding protein: purification, cloning and expression. Regulation of growth hormone binding protein in man: comparison of gel chromatography and immunoprecipitation methods. Absence of serum growth hormone binding protein in patients with growth hormone receptor deficiency (Laron dwarfism). Importance of growth hormone for the induction of hepatic low density lipoprotein receptors. In vivo stimulation by growth hormone is not mediated by insulin-like growth factor I. The acute effects of growth hormone on amino acid transport and protein synthesis are due to its insulin-like action. Growth hormone acutely stimulates skeletal muscle but not whole-body protein synthesis in humans. Assay-dependent results of immunoassayable spontaneous 24-hour growth hormone secretion in short children. Consensus statement on the standardization and evaluation of growth hormone and insulin-like growth factor assays. Excess mortality associated with hypopituitarism in adults: a meta-analysis of observational studies. Hypopituitary females have a high incidence of cardiovascular morbidity and an increased prevalence of cardiovascular risk factors. Mutations in the growth hormone releasing hormone receptor: a new form of dwarfism in humans. Growth hormone deficiency in adulthood and the effects of growth hormone replacement: a review. Effects of growth hormone administration on inflammatory and other cardiovascular risk markers in men with growth hormone deficiency. Cardiac structural and functional abnormalities in adult patients with growth hormone deficiency. Growth hormone receptor deficiency is associated with a major reduction in pro-aging signaling, cancer, and diabetes in humans. The assessment of growth hormone status in normal young adult males using a variety of provocative agents. Consensus guidelines for the diagnosis and treatment of adults with growth hormone deficiency: summary statement of the Growth Hormone Research Society Workshop on Adult Growth Hormone Deficiency. Growth hormone release after glucagon as a reliable test of growth hormone assessment in adults. The severity of growth hormone deficiency in adults with pituitary disease is related to the degree of hypopituitarism. Transcriptomics and machine learning predict diagnosis and severity of growth hormone deficiency. Detection of growth hormone doping by gene expression profiling of peripheral blood. A 10-year, prospective study of the metabolic effects of growth hormone replacement in adults. Effects of physiologic growth hormone therapy on bone density and body composition in patients with adult-onset growth hormone deficiency. Effects of recombinant human growth hormone therapy on bone mineral density in adults with growth hormone deficiency: a meta-analysis. Effect of long-term growth-hormone substitution therapy on bone mineral density and parameters of bone metabolism in adult patients with growth hormone deficiency. Fracture risk in adult patients treated with growth hormone replacement therapy for growth hormone deficiency: a prospective observational cohort study. Nitric oxide may mediate the hemodynamic effects of recombinant growth hormone in patients with acquired growth hormone deficiency. Monitoring of growth hormone replacement therapy in adults, based on measurement of serum markers. Oral estrogen antagonizes the metabolic actions of growth hormone in growth hormone-deficient women. Prevalence and incidence of diabetes mellitus in adult patients on growth hormone replacement for growth hormone deficiency: a surveillance database analysis. Role of the insulin-like growth factor family in cancer development and progression. National Cooperative Growth Study safety symposium: safety of human growth hormone therapy. Growth hormone treatment of children with brain tumors and risk of tumor recurrence. Growth hormone treatment and risk of second neoplasms in the childhood cancer survivor. Malignant disease and cardiovascular morbidity in hypopituitary adults with or without growth hormone replacement therapy. Life expectancy in patients with pituitary adenoma receiving growth hormone replacement. A randomized controlled trial of low-dose recombinant human growth hormone in the treatment of malnourished elderly medical patients. Skeletal effects of cyclic recombinant human growth hormone and salmon calcitonin in osteopenic postmenopausal women. Growth hormone increases bone mineral content in postmenopausal osteoporosis: a randomized placebo-controlled trial. Disease mongering of age-associated declines in testosterone and growth hormone levels.
Purchase decadron 0.5mg line
These polyps are lined by respiratory epithelium and have mucous glands within a loose mucoid stroma skin care solutions order generic decadron from india, containing plasma cells, lymphocytes and eosinophils. Infection followed chronic obstruction of the orifice caused by adenocarcinoma of the nasal mucosa. Sinusitis Is Inflammation of the Mucous Membranes It usually reflects bacterial infections of the paranasal sinuses. If a sinus ostium is blocked, secretions or exudate accumulate behind the obstruction. Maxillary sinusitis may also be caused by odontogenic infections: bacteria from the roots of the first and second molars penetrate the thin bony plate that separates them from the floor of the maxillary sinus. Incomplete resolution of infection or recurrent acute sinusitis may lead to chronic sinusitis, in which the purulent exudate almost always includes anaerobic bacteria. Overlying skin is often markedly edematous, and subcutaneous cellulitis or a subcutaneous abscess also may develop. Osteomyelitis also may spread rapidly between the outer and inner tables of the skull. Septic thrombophlebitis: Sinus infections that penetrate the bone may spread to frontal and diploe venous systems. Resulting septic thrombophlebitis may involve the cavernous venous sinus through the superior ophthalmic veins and is a potentially life-threatening condition. Intracranial infections: Sinusitis may also spread infection to the cranial cavity. Lesions include epidural, subdural and cerebral abscesses and purulent leptomeningitis. Spread may be via lymphatics and veins and need not involve extensive destruction of bone. Syphilis May Destroy the Nasal Bridge Primary chancres in the nose are rare, but mucosal lesions of secondary syphilis are common in the nose and nasopharynx. In tertiary syphilis, inflammation may involve large portions of the nasal mucosa, underlying cartilage and bone. Perichondrial or periosteal gummas may destroy nasal cartilage and bone, causing the nasal bridge to collapse and producing "saddle nose. If infected, a mucocele may cause a sinus to fill with mucopurulent exudate, called a pyocele. Mucoceles occur most often in the anterior compartments ("cells") of frontal and ethmoid sinuses. Mucoceles of anterior ethmoid or frontal sinuses may be large enough to displace the contents of the orbit and occasionally, erode into the central nervous system. Osteomyelitis: Suppurative infection of nasal sinus walls may spread through Volkmann canals to the periosteum, producing periostitis and subperiosteal abscess. If these Leprosy Is Spread through Nasal Secretions Mycobacterium leprae multiplies best at lower temperatures and so prefers cooler body sites, like the nares and anterior nasal mucosa. Tuberculoid and intermediate forms of leprosy account for most cases (see Chapter 9). The skin around the nares and anterior nasal mucosa shows nodules, ulceration or perforations. Nasal involvement is important as leprosy is spread via nasal secretions teeming with bacilli. Fungus balls, or aspergillomas, occur in immunologically normal patients, usually with chronic sinusitis and poor drainage. In this setting, fungi proliferate to form a dense mass of hyphae that causes nasal obstruction. In the rare rhinocerebral aspergillosis, the organisms penetrate venous sinuses and spread to the meninges and brain. Mucormycosis is a potentially life-threatening infection, particularly in diabetic and immunosuppressed patients. It typically involves the nasopharynx but can invade the skin, bone, orbit and brain. The disease is endemic in Sri Lanka and parts of India, and Central and South America. Rhinoscleroma (Scleroma) Is a Chronic Bacterial Infection Rhinoscleroma is a chronic inflammatory process caused by a gram-negative diplobacillus, Klebsiella rhinoscleromatis. It begins in the nose and usually remains localized there but may extend slowly into the nasopharynx, larynx and trachea. It rarely involves other sites, such as the paranasal sinuses, orbital tissues, skin, lips, oral mucosa, cervical lymph nodes and gastrointestinal tract. Scleroma is endemic in parts of the Mediterranean basin, Asia, Africa and Latin America. Leishmaniasis (Also Known as Kala-Azar) Mucocutaneous leishmaniasis, due to Leishmania braziliensis, commonly affects the nose (see Chapter 9). Initial skin sores heal within a few months, to be followed in some patients by mucocutaneous lesions of the nose or upper lip months or years later. Characteristic large macrophages or Mikulicz cells, contain masses of phagocytosed bacilli. Most Fungal Infections of the Nose and Sinuses Are Opportunistic Pathogenic fungi may involve the nose and paranasal sinuses as part of cutaneous or mucocutaneous infection, particularly in a setting of immunodeficiency (see Chapter 9). Aspergillosis is uncommon, and when it occurs it generally involves a paranasal sinus. Aspergillosis of the sinonasal tract may be noninvasive or invasive, including angioinvasive. A green, nasal mass in a patient with lymphoma demonstrated abundant fruiting bodies. They are composed of a uniform cellular proliferation, which displays an inflammatory cell infiltrate and scattered microcysts. Later, tuberculoid granulomatous responses develop, with few recognizable parasites. Bacterial infection may supervene and lead to soft tissue destruction and collapse of the anterior cartilaginous nasal septum. The sinonasal tract may be the only involved site, or it may be part of systemic disease. Septal perforation and mucosal ulceration may be followed by slowly progressive destruction of the nose and paranasal sinuses, leading to a saddle nose deformity. Constitutional symptoms, such as fever, malaise and weight loss, may accompany resulting "runny nose," sinusitis and nosebleeds. Nasal lesions show ischemic-type necrosis, vasculitis, mixed chronic inflammation, scattered multinucleated giant cells and microabscesses. Surgical resection must extend beyond the boundaries of grossly visible lesions, or they may recur. It resembles a wart (verruca vulgaris) and almost always occurs in the nasal vestibule. There are three morphologically distinct lesions collectively called Schneiderian papillomas: inverted, oncocytic (cylindrical or columnar cell) and fungiform (exophytic, septal) papillomas. Squamous cell carcinoma of the maxillary sinus caused an obvious facial deformity, owing to invasion outside the confines of the sinus. The latter is defined by drooping of the mouth to the side of the facial nerve paralysis. Occupational settings reportedly with increased risk for cancer of the nose and sinuses (but for which a specific chemical agent is not identified) are woodworking in the furniture industry, use of cutting oils and leather textile industries. Most other occupational exposures mainly lead to adenocarcinomas and occur mostly in the maxillary and ethmoid sinuses. Because of these occupational risk factors, cancers of the nose and sinuses occur far more often in men and after age 50. These tumors grow relentlessly and invade adjacent structures but typically do not metastasize.
Purchase decadron pills in toronto
In addition acne underwear buy decadron on line amex, systematic reviews help generate a best estimate of the effect of the clinical intervention based on the body of evidence (and not on a single study) and allow the comparison of this estimate across different studies, which together often encompass a broad range of populations and settings. Moreover, having a summary of the body of evidence allows assessment for the possibility of publication bias. The quality of the evidence reflects the extent of our confidence that the estimates of an effect are adequate to support a recommendation. When high-quality clinical evidence is available across outcomes of most importance, there is good certainty of the potential effects of an intervention, allowing panelists and clinicians to feel confident in the expected outcomes of recommendations. When the quality of evidence is poor, panelists have less confidence in effect estimates and expected outcomes of recommendations. On the other hand, observational studies are considered to provide low-quality evidence because the groups are not balanced in terms of known and unknown prognostic factors at the start of the study. In such cases, the quality of the evidence associated with the most important outcome should guide the quality of the evidence for a particular recommendation. When the gradient between desirable and undesirable effects is narrow, panels are more likely to make a weak recommendation. When high-quality evidence for patient-important outcomes is available, panels are more likely to make a strong recommendation. When only very-low-quality evidence for surrogate markers or less important outcomes is available, panels are more likely to make a weak recommendation. Values and preferences refer to the processes that patients use when considering between alternative treatment options (benefits, harms, cost, and impact on daily life). It can be argued that there is always a degree of uncertainty in terms of the values and preferences of each individual patient. Reliable evidence regarding resource use should be identified and important differences in resource use between alternative management strategies should be considered when grading recommendations. Panelists should consider if the proposed recommendations will be accepted and implemented in clinical practice. For example, they might consider the burden of treatment of a particular treatment agent compared to the alternative. Panelists should consider the impact of recommendations on health inequity and groups that are considered disadvantaged. Clinical Practice Guidelines Recommendations Recommendations have a direction (in favor of or against an intervention), a strength (strong or weak), and a judgment of the quality of the evidence supporting the recommendation (very low, low, moderate, high)12,13,21 (see case study later in the chapter). Strong recommendations assume that most patients faced with this health care decision will choose the proposed intervention given the certainty of potential benefits in important outcomes. In some circumstances, strong recommendation can be based on low-quality evidence. Weak recommendations are usually based on low-quality or very-low-quality evidence. In addition, in cases when the systematic evaluation of the evidence provides high-quality evidence that the benefits and risks of Strong Recommendations Strong recommendations are those in which the panel is confident that the desirable effects of following a recommendation clearly outweigh the undesirable effects. In general, these recommendations are based on high-quality or moderate-quality evidence. Clinicians are encouraged to explore these values and preferences by engaging in shared decision making to reach the optimal medical decision based on the best available evidence and the values of patients. In this case, it would be unreasonable to conduct a trial in which the endocrine team, the primary care provider, and the surgeon would not collaborate to achieve adequate surgical outcomes; in addition, there is indirect evidence that clinical collaboration is beneficial for patient care. Clinical Practice Guidelines in Endocrinology An analysis of the Endocrine Society clinical practice guidelines from 2008 to 2014, including 25 guidelines, found that up to 20% of the recommendations were based on very-low-quality evidence. In fact, an assessment of current clinical trials in endocrinology found that only one in five recommendations that are based on Good Practice Statements this is a special category of clinical practice statements in which a formal evaluation of the literature is not necessary, as there is a large body of indirect evidence to support the benefit of the recommendation and where the evaluation of alternatives in clinical trials would be unproductive and unnecessary. In addition, guideline panelists should seldom use this type of recommendation, as there is the risk of using it to support strong recommendations in the absence of clinical evidence. Using Clinical Practice Guidelines in Patient Care In clinical practice, guidelines can help physicians provide care that is based on the best available evidence and ideally supports patient-centered care. Clinical Question 1: What should we do to improve pregnancy and offspring outcomes in this pregnant woman with gestational diabetes Answer: As per the Endocrine Society guidelines, "Diabetes and Pregnancy,"39 using blood glucose-lowering pharmacologic therapy is recommended if lifestyle therapy is insufficient to maintain normoglycemia in women with gestational diabetes. Clinical Question 2: Of the available treatment options, which glucose-lowering medication would you recommend Answer: Providing evidence-based care for patients with gestational diabetes remains challenging because of the lack of wellconducted clinical trials in this population. Even among the major medical professional societies, including the Endocrine Shortcomings of Clinical Practice Guidelines Although clinical practice guidelines aim to help patients and clinicians collaborate in making better health decisions, there are still limitations in the development and implementation of clinical guidelines to improve care. Jones, a 54-yearold white man with a history of type 2 diabetes, obesity, controlled hypertension, depression, low back pain, sleep apnea, and newonset dyslipidemia. This event would happen despite taking the statin every day for 10 straight years, with the risk of harm. He has a high burden of illness (comorbidities), he takes more than 15 medications with many potential side effects, he has social and financial difficulties, and for Mr. Jones a 10-year risk of 10% versus 6% is simply not enough to start taking statins. This limitation might be secondary to clinical evidence obtained from studies excluding patients with comorbidities. Guideline panelists should therefore be aware of this limitation and favor creating weak or conditional recommendations that promote a patient-centered approach such as shared decision making. While there is no data on guidelines, in 200 diabetes trials in high-impact journals only 1 of 5 trials was focused on a patient-important outcome as the primary objective. Quality and Trustworthiness of Clinical Practice Guidelines Ideally, clinical practice guidelines offer clinicians an easy and accessible way to be up to date with the best available evidence regarding a particular disease. However, it is important to acknowledge that delivering care drawn from "the best available evidence" is not an easy and straightforward task, as to do so means every recommendation should be linked to the best available evidence, preferably based on a systematic review. In addition, as mentioned in the previous discussion about how clinical guidelines are developed, there are strict steps that should be followed and guidelines should be systematically developed by authors with no conflicts of interest for them to be trustworthy. Scope and purpose of the guideline: in which it is important to evaluate if the overall objectives, the clinical questions, and the patients to whom the guideline will apply are specifically described. Stakeholder involvement: assess if the guideline development group or task force includes individuals from all pertinent 4. Rigor in development: observe if systematic methods were used to search for the evidence, if methods for formulating recommendations are valid and adequately described, if there is an explicit link between recommendations and supporting evidence, and if a clear procedure for guideline updates has been provided. Clarity of presentation: assess if the recommendations are specific or unambiguous, that when applicable, different options for management of the condition are clearly presented and that key recommendations are easily identifiable. Applicability: assess if the guideline provides advice or tools that facilitate the clinical practice of the recommendation and the potential barriers and costs in applying the recommendations. Editorial independence: it is critical to recognize the funding source and conflicts of interest of the guideline developers. Conclusions Clinical practice guidelines that are developed following rigorous and systematic methods by a multidisciplinary panel can provide recommendations that can support patient-centered care. In addition to being able to assess the trustworthiness of clinical practice guidelines, clinicians should understand how these recommendations can support care and collaborate with their patients to overcome their limitations. Patient centred diagnosis: sharing diagnostic decisions with patients in clinical practice. The optimal practice of evidence-based medicine: incorporating patient preferences in practice guidelines. The increasing number of clinical items addressed during the time of adult primary care visits. Multimorbidity patterns in the United States: implications for research and clinical practice. Department of Health and Human Services, Agency for Healthcare Research and Quality. Going from evidence to recommendations: the significance and presentation of recommendations. When patients write the guidelines: patient panel recommendations for the treatment of rheumatoid arthritis. Making an overall rating of confidence in effect estimates for a single outcome and for all outcomes. A case for clarity, consistency, and helpfulness: state-of-the-art clinical practice guidelines in endocrinology using the grading of recommendations, assessment, development, and evaluation system.
Syndromes
- Confusion
- Do you have trouble starting the flow of urine?
- Phenothiazines
- EKG (electrocardiogram, or heart tracing)
- Delay or lack of spoken language
- Eat a healthy diet. Soft bland (non-spicy) foods may reduce discomfort during eating.
- Heroin: 1 to 2 days
Buy decadron now
Toxoplasma gondii bradyzoites (arrow) are present in a necrotic inflammatory background acne mechanica discount decadron 4 mg with amex. Entamoeba histolytica leads to amebic brain abscess by spread from a gastrointestinal or hepatic locus. Infarcts and microhemorrhages may both arise from obstruction of blood flow in small vessels by parasitemia. Severity of cerebral malaria also reflects tumor necrosis factor- release by host cells. Cysticercosis caused by infection by Taenia solium, the pig tapeworm, may lead to multiple parasitic cysts up to 1 cm in the parenchyma, intraventricularly or in the basal cisterns. A peculiar form of this infection is racemose neurocysticercosis, in which grape-like clusters and sheets of worm tissues are made, without a fully formed worm. Treatment of neurocysticercosis may lead to massive cerebral edema caused by massive host immune responses to the suddenly necrotic metazoan tissue. From a global health perspective, neurocysticercosis is one of the most common causes of epilepsy and intracranial mass lesions. Echinococcosis results from Taenia echinococcus or Echinococcus granulosus, the dog tapeworm, and produces cerebral cysts that are usually solitary and may be huge, in contrast to the smaller multiple cysts of cysticercosis. Trichinosis is caused by Trichinella spiralis infection of skeletal and cardiac muscle, producing an acute eosinophilic myositis during the invasive phase. The spongiform encephalopathies are biologically remarkable because the causative infectious agents, called prions (proteinaceous infectious particles), lack nucleic acids. Amebic organisms (arrows) resemble macrophages but have much more prominent nucleoli. Brain involvement by Taenia solium may result in solitary or multiple contrast-enhancing masses with surrounding edema. As the parasite begins to die and is detected by the host immune response, the lesions may become symptomatic. The corrugated cuticular surface forms an eosinophilic interface with inflamed adjacent brain. At low magnification, the worm scolex and gastrointestinal tract can sometimes be seen. C more easily transmitted and does not show the species selectivity of other prions. It decimated the cattle industry in the United Kingdom and spread to other regions of the world and to other species including zoo animals, pets and humans. Uniquely, conversion of the native protein to the pathogenic form is autocatalyzed by the pathogenic form itself. The pathogenic protein begets more pathogenic protein from the limitless supply of native protein! The normal prion gene product, prion protein (PrP), is a constitutively expressed cell surface glycoprotein that binds neuronal plasmalemma via a glycolipid anchor. Spongiform degeneration of the gray matter is characterized by individual and clustered vacuoles, with no evidence of inflammation. Medical devices: depth electrodes, surgical instruments (none definitely proven) 4. Captive exotic ungulate spongiform encephalopathy (nyala, gemsbok, eland, Arabian oryx, greater kudu) F. Lesions occur mostly in cortical gray matter but also involve deeper nuclei of the basal ganglia, thalamus, hypothalamus and cerebellum. Transmission of kuru was linked to ritualistic funereal cannibalism in which women and children ate brains of deceased relatives. It attained epidemic proportions in the Fore people but was eliminated when cannibalism ceased. The initial and most prominent clinical feature of kuru is ataxia of the limbs and trunk, due to severe cerebellar involvement. In 70% of cases, insoluble, fibrillar prion proteins accumulate extracellularly in plaques. Symptoms begin insidiously, but usually within 6 months to 3 years, patients exhibit severe dementia leading to death. Thus, recombinant human growth hormone has replaced human pituitaryderived preparations for therapy. When brain biopsies or autopsies are done in prion disease cases, special protocols are used to limit exposure of staff and patients to prions. Conventional autoclaving and most standard disinfectants do not eradicate this hardy infectious agent. With globalization and diversification of economies, cultures and populations, a global perspective is essential in considering infectious diseases. Ease of movement leads to infections previously thought of as exotic or tropic occurring unexpectedly in industrialized countries. Finally, there is the ever present danger of manmade biological agents being deployed. People who emigrate before age 15 from areas with a low prevalence to more temperate endemic areas assume the increased risk associated with their destinations, suggesting that environmental factors are important. They are discrete, with smoothly rounded contours, and are usually in white matter, although they may breach the gray matter. Central myelin is made by oligodendrocytes, while peripheral myelin is made by Schwann cells (see Chapter 31). It becomes symptomatic at a mean age of 30, and women are afflicted almost twice as often as men. This myelin-stained coronal whole brain section of the brain of a patient with long-standing multiple sclerosis shows many areas of myelin loss-plaques (arrows)-with characteristic periventricular demyelination especially prominent at the superior angles of the lateral ventricles. New plaques emerge and regress, only occasionally causing clinical manifestations. Blurred vision or loss of vision in one eye as a result of optic neuritis is often the presenting complaint. In particular, internuclear ophthalmoplegia, caused by disruption of the medial longitudinal fasciculus, strongly suggests demyelinating disease when it occurs in a young person. Acute demyelination within the spinal cord is called transverse myelitis and produces weakness of one or both legs and sensory symptoms in the form of numbness in the lower extremities. Despite the fact that most patients have a chronic relapsing and remitting course, neurologic deficits accumulate gradually and relentlessly. Even in relatively quiescent plaques, there may be axonal attrition leading to irreversible lesions. In established cases, the degree of functional impairment is highly variable, ranging from minor disability to severe incapacity, with widespread paralysis, dysarthria, ataxia, severe visual defects, incontinence and dementia. Patients with severe disability usually die of respiratory paralysis or urinary tract infections. This fresh coronal section shows darker hues of the somewhat irregular periventricular plaques (arrows) reflecting the loss of myelin, which imparts the normal glistening white appearance of white matter. Evolving plaques are marked by selective loss of myelin in regions of relative axonal preservation, lymphocytes clustering about small veins and arteries, influx of macrophages and considerable edema. This sequence emphasizes the focal nature of the injury and its selectivity and severity, as demyelination is total within a plaque. Postinfectious and Postvaccinal Encephalomyelitis Are Immune Responses to Viral Antigens Some viral infections. The disease entails focal perivascular demyelination and conspicuous mononuclear cell infiltrates around small to medium-sized venules in brain and spinal cord white matter. It is suspected to be immune mediated, but its precise pathogenesis remains unclear. Onset of postinfectious encephalomyelitis is heralded by headache, vomiting, fever and meningismus that may be followed by paraplegia, incontinence and stupor. The subcortical white matter of a patient with multiple sclerosis showing multiple small irregular, partially confluent areas of demyelination (arrows).
Cheap decadron master card
Today acne jensen order 4 mg decadron otc, the most common form of neuropathic joint disease is destruction of foot joints in people with diabetic peripheral neuropathy. Destruction of shoulder or other upper extremity joints can occur in patients with syringomyelia, an abnormality affecting the cervical spinal cord. Microscopically, there is marked destruction of articular cartilage and subchondral bone, inciting subchondral sclerosis, cyst formation and large amounts of cartilage and bone detritus within hyperplastic synovium. Although the pathogenesis remains uncertain, it is most likely that loss of innervation to the joint structures brings on a lack of proprioception and pain, abnormal joint mechanics and ultimately joint destruction. The death of chondrocytes leads to a crack in the articular cartilage that is followed by an influx of synovial fluid and further loss and degeneration of cartilage. Below the tidemark, new vessels grow in from the epiphysis, and fibrocartilage (D) is deposited. The fibrocartilage plug is not mechanically sufficient and may be worn away, thus exposing the subchondral bone plate, which becomes thickened and eburnated. If there is a crack in this region, synovial fluid leaks into the marrow space and produces a subchondral bone cyst. A femoral head with osteoarthritis shows a fibrocartilaginous plug (far right) extending from the marrow onto the joint surface. A section through the articular surface of an osteoarthritic joint demonstrates focal absence of the articular cartilage, thickening of subchondral bone (left) and a subchondral bone cyst. The proximal interphalangeal and metacarpophalangeal joints, elbows, knees, ankles and spine are most commonly affected. Commonly, joints of the extremities are simultaneously affected, often in a symmetric fashion. The course of the disease varies and is often punctuated by remissions and exacerbations. The broad spectrum of clinical manifestations ranges from barely discernible to severe, destructive, mutilating disease. Patients who are persistently seronegative for rheumatoid factor probably have disease of a different etiology than those who are seropositive. There are also rheumatoid-like diseases associated with underlying conditions, such as inflammatory bowel disease and cirrhosis. Vascularity increases, with exudation of fibrin into the joint space, which may result in small fibrin nodules that float in the joint (rice bodies). This inflammatory synovium, which now contains mast cells, creeps over the surface of the articular cartilage and adjacent structures and is a pannus (cloak). The pannus erodes the articular cartilage and adjacent bone, probably through the action of collagenase produced by the pannus. The pannus penetrates the subchondral bone; it may involve tendons and ligaments, leading to deformities and instabilities. The pannus may destroy cartilage by depriving it of nourishment; alternately, it may stimulate T lymphocytes to secrete a factor that causes release of lysosomal enzymes. Changes in synovial fluid include a massive increase in volume, increased turbidity and decreased viscosity. The protein content and the number of inflammatory cells in the fluid increase, correlating with the activity of the rheumatoid process. In some cases, the leukocyte count exceeds 50,000/L, with 95% polymorphonuclear leukocytes. A characteristic lesion, the "rheumatoid nodule," is found in extraarticular locations. Beyond the macrophages is a circle of lymphocytes, plasma cells and other mononuclear cells. The overall appearance resembles a peculiar granuloma surrounding a core of fibrinoid necrosis. They are sometimes found in visceral organs, such as the heart, lungs, intestinal tract and even the dura. Nodules in the bundle of His may cause cardiac arrhythmias; in the lungs, they produce fibrosis and even respiratory failure (see Chapter 18). The influx of lymphocytes, plasma cells and mast cells, together with neovascularization and edema, leads to hypertrophy and hyperplasia of the synovium. Proliferating synovium extends into the joint space, burrows into the bone beneath the articular cartilage and covers the cartilage as a pannus. The articular cartilage is eventually destroyed by direct resorption or deprivation of its nutrient synovial fluid. The synovial tissue continues to proliferate in the subchondral region, as well as in the joint. Eventually, the joint is destroyed and becomes fused, a condition termed ankylosis. Hyperplastic synovium from a patient with rheumatoid arthritis shows numerous finger-like projections, with focal pale areas of fibrin deposition. The brownish color of the synovium reflects hemosiderin accumulation derived from old hemorrhage. A microscopic view reveals prominent lymphoid follicles (Allison-Ghormley bodies; arrows), synovial hyperplasia and hypertrophy, villous folds and thickening of the synovial membrane by fibrosis and inflammation. A higher-power view of the inflamed synovium demonstrates hyperplasia and hypertrophy of the lining cells. Unabated disease causes progressive destruction of the joint surfaces and periarticular structures. Eventually, patients manifest severe flexion and extension deformities, associated with joint subluxation, which may terminate in joint ankylosis. There is increased mortality from infection, gastrointestinal hemorrhage and perforation, vasculitis, heart and lung involvement, amyloidosis and subluxation of the cervical spine. The hands of a patient with advanced arthritis show swelling of the metacarpophalangeal joints and the classic ulnar deviation of the fingers. Microscopic view of a rheumatoid nodule shows a central area of necrosis surrounded by palisaded macrophages and a chronic inflammatory infiltrate. They are now recommended early in the course of the disease to prevent progression, induce remission and prevent joint deformities and functional disabilities. These forms of arthritis are now known as spondyloarthropathies and include ankylosing spondylitis, Reiter syndrome, psoriatic arthritis and arthritis associated with inflammatory bowel disease. Although a few patients with ankylosing spondylitis rapidly develop crippling spinal disease, most are able to maintain their employment and live a normal life span. The result is destruction of these joints, after which the spine becomes fused posteriorly. The vertebral bodies are square and have lost most of their trabecular bone, owing to osteoporosis from disuse. It may be accompanied by asymmetric, peripheral arthritis (30% of patients) and systemic manifestations. Pauciarticular arthritis: Children with involvement of only a few large joints, such as the knee, ankle, elbow or hip girdle, account for half of all cases of juvenile arthritis and fall into two general groups. Of these patients, one third have ocular disease, characterized by chronic iridocyclitis (inflammation of the iris and ciliary body). Only a small minority of these children have residual polyarthritis or ocular damage. It occurs almost exclusively in men and usually follows venereal exposure or an episode of bacillary dysentery. More than half of patients develop mucocutaneous lesions similar to those of pustular psoriasis (keratoderma blennorrhagica) over the palms, soles and trunk. In most patients, the disease remits within a year, but in 20%, progressive arthritis develops, including ankylosing spondylitis. Psoriatic Arthritis Of all patients with psoriasis, particularly in those with severe disease, 7% develop an inflammatory seronegative arthritis. Joint disease is usually mild and slowly progressive, although a mutilating form is occasionally encountered. Patients generally present with joint effusion and other manifestations of Lyme disease. Although there may be a transient arthritis with acute infection, some patients can develop chronic Lyme arthritis, which is microscopically identical to rheumatoid arthritis. Enteropathic Arthritis Ulcerative colitis and Crohn disease are accompanied by seronegative peripheral arthritis in 20% of cases and spondylitis in 10%. This form of arthritis also is seen in patients with Whipple disease and after certain bacterial infections of the gut.
Decadron 4mg without a prescription
Others acne 6 months postpartum 8 mg decadron, such as those containing iron, cause retinal degeneration and even discoloration of ocular tissues (siderosis bulbi), effects that may not be evident for several years. Other complications of ocular injuries include cataracts, retinal detachment and glaucoma. Acute inflammation involving the meibomian glands is termed an internal hordeolum, whereas acute folliculitis of the glands of Zeis is an external hordeolum. Chalazion is a granulomatous inflammation centered around the meibomian glands or the glands of Zeis. It is thought to represent a reaction to extruded lipid secretions and usually produces a painless swelling in the eyelid. It is often seen in older persons and patients with disorders of lipid metabolism. The most common cause is thyroid disease, followed by orbital dermoid cysts and hemangiomas. Other orbital conditions can cause proptosis: various inflammatory lesions, lymphomas, developmental anomalies, vascular problems and neoplasms. Proptosis also results from lesions of the paranasal sinuses and intracranial cavity. Conjunctivitis May Be Infectious or Allergic Microorganisms lodging on the surface of the eye frequently cause conjunctivitis, keratitis (corneal inflammation) or a corneal ulcer. The conjunctiva, as well as other parts of the eye, may also become infected by hematogenous spread from a focus of infection elsewhere. This extremely common eye disease is characterized by hyperemic conjunctival blood vessels (pink eye). The inflammatory exudate that accumulates in the conjunctival sac commonly crusts, causing the eyelids to stick together in the morning. As many allergens are seasonal, the allergic conjunctivitis they elicit tends to occur only at particular times of the year. Exophthalmos of Hyperthyroidism Continues Despite Treatment Exophthalmos caused by Graves disease may precede or follow other manifestations of thyroid dysfunction. Exophthalmos resulting from thyroid disease usually occurs in early adult life, especially in women (female-to-male ratio, 4:1). It may be severe and progressive, particularly in middle life, when exophthalmos no longer correlates well with the state of thyroid function. Dysthyroid exophthalmos may be associated with edema of the eyelids, chemosis (conjunctival edema) and limitation of ocular motion. Theories of the pathogenesis of hyperthyroidism-related exophthalmos are discussed in Chapter 27. Trachoma Trachoma is a chronic, contagious conjunctivitis caused by Chlamydia trachomatis. Other ocular manifestations of hyperthyroidism include upper eyelid retraction (due to increased sympathetic tone) and a characteristic stare or apparent proptosis resulting from exposure of the conjunctiva above the corneoscleral limbus. Complications of severe exophthalmos include several potentially blinding complications: corneal exposure with subsequent ulceration, and optic nerve compression. Paradoxically, thyroidectomy may increase the incidence and severity of exophthalmos associated with hyperthyroidism. This infection is the most common cause of blindness in the world and is especially prevalent in Asia, the Middle East and parts of Africa. The disease has been eradicated in the United States and other developed countries. Trachoma is not very contagious, but overcrowding and poor hygienic conditions favor its transmission by fingers, fomites and flies. Spontaneous healing is common in children, but in adults, the disease progresses more rapidly and rarely heals without treatment. Serial persistent or repetitive inflammatory reactions to different strains of the pathogen are believed to cause the serious cicatricial complications. The cellular infiltrate is predominantly lymphocytic, and conjunctival lymph follicles with necrotic germinal centers are characteristic. Eventually lymphocytes and blood vessels invade the superior portion of the cornea between the epithelium and Bowman zone (trachomatous pannus). On microscopic examination, the desquamated conjunctival epithelium Inflammatory Pseudotumor Is a Chronic Idiopathic Inflammatory Condition Inflammatory pseudotumor is associated with a variable degree of fibrosis. These infections are accompanied by regional lymphadenopathy, systemic infection and fever. These usually heal without ulceration, but an acute unilateral follicular conjunctivitis may occur. The cornea of a patient with severe trachoma shows extensive fibrovascular opacity (pannus) in the superior cornea. Other Chlamydial Infections Chlamydia is responsible for a purulent conjunctivitis (inclusion blennorrhea) that develops in newborns, who become infected during passage through the birth canal. The infection is also acquired by swimming in nonchlorinated pools (swimming pool conjunctivitis) or from contact with discharges of infected urethra or cervix. In adults and older children, Chlamydia causes a chronic follicular conjunctivitis with focal lymphoid hyperplasia (inclusion conjunctivitis). Although some of these lesions heal, others enlarge and eventually coalesce to form linear or branching fissures (dendritic ulcers, from the Greek dendron, "tree"). The epithelium between the fissures desquamates, leading to sharply demarcated, irregular geographical ulcers. The corneal ulcers are readily visualized after the cornea is stained with fluorescein. Typically, a central disc-shaped corneal opacity develops beneath the epithelium, owing to edema and minimal inflammation (disciform keratitis). The corneal stroma may become markedly thinned, and the Descemet membrane may bulge into it (descemetocele). Ophthalmia Neonatorum Ophthalmia neonatorum is a severe, acute conjunctivitis with a copious purulent discharge, especially in the newborn, caused by Neisseria gonorrhoeae. The infection, which is a common cause of blindness in some parts of the world, is complicated by corneal ulceration, perforation, scarring and panophthalmitis. Infants usually become infected while passing through the birth canal of an infected mother. Other causative organisms for ophthalmia neonatorum include other pyogenic bacteria and C. Onchocerciasis Leads to Blindness in Tropical Regions the nematode Onchocerca volvulus, which is transmitted by bites of infected blackflies, is by far the most important helminthic infection of the eye (see Chapter 9). This parasite accounts for blindness in at least half a million people in regions of Africa and Latin America in which it is endemic. Microfilariae released from fertilized adult female worms migrate into the superficial cornea, bulbar conjunctiva, aqueous humor and other ocular tissues. The intracorneal microfilariae die and elicit an inflammatory response that leads to corneal opacification and visual impairment (river blindness). Pinguecula and Pterygium Pinguecula is a yellowish conjunctival lump usually located nasal to the corneoscleral limbus. It consists of sun-damaged connective tissue identical to that in similarly injured skin (actinic elastosis; see Chapter 28). Pterygium is a fold of vascularized conjunctiva that grows horizontally onto the cornea in the shape of an insect wing (hence the name). Although clinical manifestations may be limited to the cornea, other tissues are involved in some of these disorders. Arcus Lipoides Is a White Arc Due to Lipid Deposition in the Peripheral Cornea Formerly called arcus senilis because of its frequency in the elderly, arcus lipoides may also form an entire ring, in which case the term annulus lipoides is more appropriate. Although not necessarily associated with increased serum lipid levels, arcus lipoides accompanies certain disorders of lipid metabolism, and its presence alerts the perceptive clinician to the systemic disorder. Band Keratopathy Is an Opaque Horizontal Band across the Cornea the opacification in band keratopathy may contain calcium phosphate (calcific band keratopathy) or noncalcified protein (chronic actinic keratopathy). In calcific band keratopathy, calcium phosphate deposits in a horizontal band across the superficial central cornea in conditions associated with hypercalcemia. However, the disorder most often occurs in the absence of hypercalcemia, as in chronic uveitis.
Purchase decadron with a mastercard
Glucocorticoid receptor function in hepatocytes is essential to promote postnatal body growth acne treatment order decadron line. Diabetes mellitus: its differentiation into insulinsensitive and insulin-insensitive types. Postreceptor insulin resistance contributes to human dyslipidemia and hepatic steatosis. Activation of a member of the steroid hormone receptor superfamily by peroxisome proliferators. Nuclear receptors in disease: thyroid receptor beta, peroxisome-proliferator-activated receptor gamma and orphan receptors. Vitamin D receptor mutations in patients with hereditary 1,25-dihydroxyvitamin D-resistant rickets. Structural overview of the nuclear receptor superfamily: insights into physiology and therapeutics. Structural analysis of nuclear receptors: from isolated domains to integral proteins. Direct repeats as selective response elements for the thyroid hormone, retinoic acid, and vitamin D3 receptors. Cell- and gene-specific regulation of primary target genes by the androgen receptor. A hierarchical network of transcription factors governs androgen receptor-dependent prostate cancer growth. Hormone-dependent coactivator binding to a hydrophobic cleft on nuclear receptors. Ligand binding and co-activator assembly of the peroxisome proliferator-activated receptorgamma. The structural basis of estrogen receptor/coactivator recognition and the antagonism of this interaction by tamoxifen. A signature motif in transcriptional co-activators mediates binding to nuclear receptors. Dynamic regulation of transcriptional states by chromatin and transcription factors. Mice devoid of all known thyroid hormone receptors are viable but exhibit disorders of the pituitary-thyroid axis, growth, and bone maturation. The role of corepressors in transcriptional regulation by nuclear hormone receptors. Activators of peroxisome proliferator-activated receptor gamma have depot-specific effects on human preadipocyte differentiation. Nuclear receptor corepressor and histone deacetylase 3 govern circadian metabolic physiology. Histone deacetylase 3 prepares brown adipose tissue for acute thermogenic challenge. Thyroid hormone signaling in vivo requires a balance between coactivators and corepressors. Hormone-responsive enhancer-activity maps reveal predictive motifs, indirect repression, and targeting of closed chromatin. Transactivation functions of the N-terminal domains of nuclear hormone receptors: protein folding and coactivator interactions. Multi-modulation of nuclear receptor coactivators through posttranslational modifications. Anatomical profiling of nuclear receptor expression reveals a hierarchical transcriptional network. FoxA1 translates epigenetic signatures into enhancer-driven lineage-specific transcription. Nongenomic thyroid hormone signaling occurs through a plasma membranelocalized receptor. Mendelian endocrine disorders are caused by variants found rarely in the population, usually from a relatively small number of genes, and each variant has a large individual effect on disease risk so that in any one individual, most of the disease risk is explained by variants in a single gene. Genetic information is most likely to be of direct clinical use in patients with suspected mendelian syndromes. The Role of Genetics in Endocri ology the sequencing of the human genome has~ hered in an era of genomic medicine. The catalog of protein-coding genes in humans is essentially complete, and the number of associations between genes and specific diseases is growing rapidly. The ability to interpret this variation is less advanced but is improving, as databases of variants and their clinical associations increase in both size and accuracy. Available sequencing data are growing exponentially, and the volume of information places increasing the demand for methods to distinguish pathologic variants from benign ones. Perhaps even more important, it is critical that clinicians understand the limits of such information. We then focus on endocrine disorders, providing an overview of the genetics of endocrine diseases, with illustrative examples from both mendelian disorders (caused by mutations in single genes) and polygenie disorders (in which variation in many genes influences disease risk). Finally, we examine scenarios for clinical uses of genetic information in endocrinology and provide recommendations. Chapter 3 Genetics of Endocrinology 43 Most diseases, including endocrine disorders, are heritable, meaning that genetic variation contributes to disease risk in a population. The detailed discussions of the genetics of these and other disorders can be found throughout this textbook; this chapter provides illustrative examples that illuminate key concepts and refers the reader to the appropriate chapters for additional detail. Heritability: An Estimate of the Importance of Genetic Factors to Disease Causation Relatives resemble each other in many ways. Heritability quantifies, as a proportion, how much of this familial resemblance is due to genetic factors. A trait that has no genetic influence would have a heritability of 0%; a trait that is completely determined by inherited factors would have a heritability of 100%. Most clinically important traits have heritabilities ranging from 20% to 80% (Table 3. Appreciating the heritability of a trait is important when interpreting the contribution of genetic risk factors in disease: genetic factors are less influential for traits with low heritability and are likely to have more predictive or explanatory power for traits with high heritability. In the past, the gold standard for heritability estimation was the comparison of monozygotic and dizygotic twin concordance rates for diseases/traits. Such studies relied on the rationale that an excess of disease correlation between genetically identical individuals (monozygotic twin pairs) compared with those who share only 50% of their genes (dizygotic twin pairs) pointed to the role of genetic factors. However, the validity of comparing twin concordance rates across different families relied on the assumption that the effect of environment was the same for the twin pairs, regardless of whether they were monozygotic or dizygotic twins. More recent methods for heritability estimation can overcome some of these limitations by leveraging subtle fluctuations in genetic similarities between sibling pairs. The heritability estimate from any study must be interpreted in the context of the population in which it is being measured, including the historical period, and variability in environmental factors such as socioeconomic status and nutrition. These factors likely explain the wide range of heritability estimates for type 2 diabetes, ranging from 40% in Finland7 to 80% in Japan. In 1940, this region was divided between Finland and the former Soviet Union with little contact between the two sections over the next 60 years. Finnish Karelians have a sixfold increased rate of type 1 diabetes compared with Russian Karelians. The difference in diabetes rate is likely due to environmental factors, because both Karelian populations recently originated from a common ancestry and therefore likely have similar genetic risk factors for type 1 diabetes. But it was not until 1865 that the Austrian abbot Gregor Mendel, after decades of careful experimentation in pea plants, posited and provided evidence for the modern genetic concept of genes (as coined by the botanist Wilhelm Johannsen in 1909). It was recognized in the early 20th century that certain human phenotypes, including diseases, were inherited according to the same rules that Mendel had described; these diseases are called mendelian. The first description of the molecular basis of a mendelian disease was made for sickle cell anemia, which involved a mutation in a single gene. By tracing the transmission of these polymorphisms in families, it became possible to identify genes causing mendelian human disorders (those caused by altered function in a single gene and that consequently show distinctive patterns of inheritance in families). Biometricians had appreciated in the early 1900s that most continuous and commonly varying traits. Fisher4 provided a general framework explaining continually varying traits as the consequence of polygenic inheritance-that is, polygenic phenotypes are a result of combined, small, and additive effects of variation in many genes simultaneously. Despite this recognition, only a few genetic variants were convincingly connected with polygenic diseases/traits over the next 80 years. When comparing two versions of a human genome, either within the same person or between two different people, about 1/1000 of these bases vary.