20 gm eurax free shipping
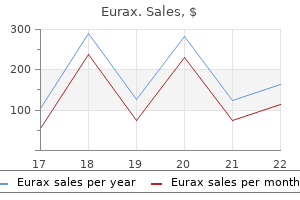
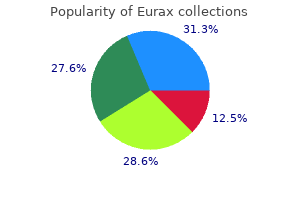
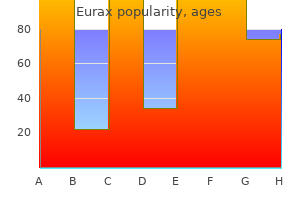
They typically occur when there is any sort of obstruction of milk flow in the lactating breast skin care 5-8 years generic eurax 20 gm without prescription. In the physical examination, maneuvers to accentuate the skin changes such as "hands on hips" or "arms raised over the head" assist in evaluating for these findings. Most clinicians excise any dominant 3D mass occurring in a woman older than 35 years or in those with an increased likelihood of mammary cancer (family history). H istologic analysis from the excisional biopsy will most likely confirm the diagnosis of cancer. In females in the adolescent years or in their twenties, the most common cause of a dominant breast mass is a fibroadenoma. The best way to image the breast of a woman less than age 30 is usually ultrasound due to the dense fibrocystic changes that interfere with mammographic interpretation. Ultrasound can differentiate a solid versus a cystic mass, and sometimes can suggest a fibroadenoma; nevertheless, tissue should be obtained to confirm the diagnosis. In a woman who has a "red tender indurated breast" who is nonlactating, inflammatory breast cancer must be ruled out. Inflammatory breast cancer is aggressive in nature, and the skin changes occur due to the cancer cells within the subdermal lymph channels. Immediate diagnosis and therapy are crucial, whereas delay with various antibiotics would be detrimental. Interestingly, inflammatory breast cancer occurs more in younger patients, although women of any age can be affected. Although the biggest risk factor for breast cancer in general is age, breast malignancy does occur in younger patients. A red inflamed breast in a nonlactating woman should be evaluated for possible inflammatory breast cancer. She had used the contraceptive diaphragm or birth control until she went into menopause 1 year ago. Her surgical history includes a myomectomy or symptomatic uterine ibroids 10 years ago. Understand that the age of the patient is usually the biggest risk factor for breast cancer. Understand that normal imaging of a palpable breast mass does not rule out cancer. The physical examination is aimed at screening for common and/ or serious conditions, such as hypertension, thyroid disease, cervical cancer (Pap smear), colon cancer (stool for occult blood), and breast cancer. Despite the normal imaging, there is a possibility that the breast mass is malignant. Fine-needle aspiration is an acceptable diagnostic modality, but would not be able to discern ductal carcinoma in situ versus invasion. Needle biopsy is usually preferred rather than excision to better plan future surgeries. The combination of the clinical examination, the imaging, and the needle biopsy is called the triple test. When all three tests agree (benign or malignant), this concordant result is > 99% accurate. If any one parameter suggests cancer, even in the face of the other two being negative, most experts will recommend excision of the mass to assess for malignancy. These are tumor suppressor genes, such that a mutation in the gene confers a markedly increased risk of breast cancer and ovarian cancer. It is the second leading cause of female cancer deaths in the United States, exceeded only by lung cancer. It is also the most frequently diagnosed cause of death from cancer in women worldwide. Established risk factors for breast cancer include age, personal or family history of breast cancer or precancerous lesions, reproductive factors (early menarche and late menopause), hormonal treatment, postmenopausal obesity, alcohol consumption, exposure to ionizing radiation, and genetic predisposition. The prevalence of breast cancer is age specific, and age is the most important risk factor. One in 2500 women will develop breast cancer at the age of 20 years; whereas 1 in 30 women will develop breast cancer at the age of 60 years, giving an overall lifetime risk of 1 in 8. One common way breast cancer is first discovered is a mass palpated by the patient. Clinical breast examination every 3 years should be performed for women from ages 20 to 39 years. Routine self-breast examination is no longer recommended due to false positive rates; however, breast self awareness still has utility. In other words, the patient may be aware of the texture and consistency of her breasts and should report changes. In general, age is the most significant risk factor for breast cancer, but other parameters are important to consider. Thus, any palpable dominant mass, regardless of mammographic findings, requires histologic diagnosis. Those technologies are not alternatives to mammography for women with average risk of breast cancer. Ultrasonography is an established adjunct to mammography, useful in evaluating young patients and other women with dense breast tissue and in differentiating a cyst from a solid mass. For nonpalpable lesions, the biopsy requires ultrasound-guided core needle biopsy or stereotactic core needle biopsy. N early 30% of breast cancers have some familial component, but < 10% are caused by inherited mutations in major breast cancer susceptibility genes. When the fluid obtained from a breast cyst is straw-colored and the mass disappears, then the fluid can be discarded and no further therapy is needed. H owever, when the fluid is a different color such as bloody, then the fluid should be sent for cytology. Lumpectomy and lymph node sentinel node biopsy is performed for proven breast cancer for staging. Tamoxifen therapy may be used for postmenopausal women with estrogen receptor positive breast cancer after surgery. H ormone receptor status does play some role but not as s significantly as the lymph node condition. Infiltrating intraductal carcinoma is the most common histological subtype of breast cancer. This patient very well could have inflammatory breast cancer since she has redness and warmth of the breast and is not lactating. Women at the age o 35 years or greater with a amily history o breast cancer should have annual mammography. The most common cause o unilateral serosanguineous nipple discharge rom a single duct is intraductal papilloma. In iltrating ductal carcinoma is the most common histological type o breast cancer. A breast cyst in which the luid is straw-colored or clear and the breast mass upon aspiration disappears may be observed. Her past medical history is remarkable for mild hypertension controlled with an oral thiazide diuretic agent. On examination, her blood pressure is 140/84 mm Hg, heart rate is 70 beats per minute, and she is afebrile. Considerations this 59-year-old woman is going to her doctor for routine health maintenance. The mammogram reveals a small cluster of calcifications around a small mass, which is one of the classic findings of breast cancer. With this mammographic finding, it is of paramount importance to obtain tissue for histologic diagnosis. Because of the high risk of malignancy, a stereotactic-directed core biopsy is indicated. Current radiation levels from mammography have been shown to be safe and cause no increased risk in developing breast cancer. The radiation exposure is < 10 rad per lifetime if annual mammograms begin at age 40 years and continue up to age 90.
Discount eurax 20 gm overnight delivery
Cai Y et al: Altered trafficking and stability of polycystins underlie polycystic kidney disease acne glycolic acid purchase 20 gm eurax. Due to the marked enlargement, only half of the kidney is framed within this image. The normal architecture is severely distorted by numerous cysts distributed throughout the renal parenchyma. Cysts Hemorrhagic and Proteinaceous Cysts (Left) these cysts demonstrate the spectrum of findings that may be present within cyst contents. The other 2 adjacent cysts contain proteinaceous material that show varying degrees of eosinophilia. Cysts affect all levels of the nephron, from the glomerulus to the collecting ducts. Columnar Epithelial-Lined Cyst Glomerular Cyst (Left) Some cysts are lined by epithelia with columnar morphology. This is distinct from the enlarged, hyperplastic hobnailed cells seen in acquired cystic disease. Tumors can usually be detected on gross examination after breadloafing at 1 cm, and appear as solid yellow or white nodules. Since most renal pyramids angle toward the collecting system from an anterior or posterior direction, rounded medullary cysts are often seen. The newborn had the Potter sequence with Potter facies, which is characterized by low posteriorly rotated ears, recessed chin, broad nose and epicanthic folds, all present in this case. The neonate presented with respiratory failure and massive abdominal enlargement due to bilateral cystic kidneys. Notice the numerous small round cysts that represent cross-sectional profiles of cortical collecting ducts. The collecting system includes the renal pelvis and ureters, and the bladder is normally formed. The cysts impart a sponge-like quality to the kidneys, not to be confused with medullary sponge kidney. This creates the sponge-like quality in gross appearance and sponge-like texture of the kidney when handled. The cysts are predominately located within the renal medulla, and are caused by disruption of the collecting ducts. Although the cortex appears well preserved, notice that it is very thin with few nephron generations and there is ectasia of proximal tubules. However, there is marked dilation of deep cortical and medullary collecting ducts. It has a much firmer texture than normal liver, reflecting the presence of periportal fibrosis. The ductules have complex irregular shapes and typically are arrayed at the periphery of the portal triad. Rather than the round bile ductules of a normal triad, this duct is markedly irregular with a complex branching conformation. The kidney appears edematous and slightly enlarged with prominent corticomedullary cysts. Hypertrophied Proximal Tubules Joubert Syndrome (Left) Patient with Joubert syndrome has tubular basement membrane duplication highlighted with Jones silver stain. While this is not a specific finding, it is characteristic of this group of diseases. Hepatic Fibrosis Hepatic Fibrosis (Left) the liver is diffusely nodular, diagnostic of cirrhosis. If a solid nest of clear cells was present then this would be classified as a clear cell renal cell carcinoma. Such cysts have often been referred to as atypical cysts and are believed to be a precursor lesion for clear cell renal cell carcinoma. One is multicystic with thin, translucent cyst septa indicative of a benign lesion. The larger cyst contains blood but also has yellow nodules representing a clear cell renal cell carcinoma. Multiple Renal Cell Carcinomas Clear Cell-Lined Cyst (Left) this is a small 1 mm benign cyst. In contrast to simple cortical cysts common in adult kidneys, this cyst is lined by cells with complete cytoplasmic clearing and low-grade nuclear features. The cyst is lined by a single layer of clear cells and has a thin fibrous pseudocapsule. Because of the stratified layer of clear cells it is classified as an atypical cyst, possibly destined to become a cystic clear cell renal cell carcinoma. It consists of several small, confluent acinar structures with centrally located red blood cells. The other lesion is associated with prominent sclerosis and contains a central cyst. The sclerotic areas harbored nests of clear cells, indicating the presence of renal cell carcinoma. The sclerosis is a regressive feature and correlates with a low volume of tumor cells. Multiple small nodules of clear cell renal cell carcinoma are visible within this hemorrhagic tumor. The tumor cells are arranged in nests and acini and have Fuhrman grade 1 and 2 nuclei. There is hemorrhage in the acini centers, a common finding in these vascular neoplasms. The cells lining the cystic spaces and the cells within the septa appear identical. The cytoplasmic clearing results from extraction of abundant lipid and glycogen, characteristic of clear cell carcinomas. In this section, distant from the main tumor, there is a clear cell-lined cyst and 2 small solid nests of clear cell carcinoma. There are also several smaller cysts, more difficult to appreciate in this photograph. It shows numerous variably sized cysts and extensive areas of sclerosis; however, no neoplasms were present. However, severe nuclear atypia does not indicate malignancy, which is based upon tumor size, presence of necrosis, and invasive behavior. Angiomyolipomas can range from large grossly visible tumors to microscopic tumors. Angiomyolipoma Angiomyolipomatous Change (Left) Angiomyolipomatous change, or more simply angiomyolipomatosis, refers to the infiltration of individual to small collections of myoid or lipid-rich cells (seen here), or both, throughout the renal parenchyma. The lining cells are plump with abundant eosinophilic cytoplasm and occasionally appear stratified. Tuberous Sclerosis Complex Cystic Diseases Kidney With Multiple Cysts Multiple Cysts and Angiomyolipoma (Left) External surface of a kidney from a patient with tuberous sclerosis shows multiple cysts of various sizes. Multiple Angiomyolipomas Microscopic Angiomyolipomas (Left) Multiple fleshy to fattyappearing tumors are grossly apparent in this cross section of a kidney from a patient with tuberous sclerosis. The patient presented with flank pain and had retroperitoneal hemorrhage; note the adherent blood surrounding the kidney. Myoid Cell-Rich Angiomyolipoma Angiomyolipoma With Epithelial-Lined Cyst (Left) Angiomyolipomas can show variable amounts of myoid cells and lipid-rich cells. In this micrograph, the abnormal tissue consisting of fat, smooth muscle, and small blood vessels percolates through the renal cortex. Subtle Angiomyolipomatous Lesions Focal Cysts and Ectatic Tubules (Left) this is an example of a relatively intact portion of renal parenchyma. The cells comprising the cystic epithelium have plump eosinophilic cytoplasm with a hobnail pattern and are much larger than cells in noncystic tubules. Cyst With Plump Epithelial Lining Microcyst With Hobnailed Patten (Left) the small cyst here is lined by cells with abundant cytoplasm. The individual cells are much larger than the surrounding proximal and distal tubule cells. In contrast, some patients with cystic disease show marked destruction of the renal parenchyma between and around cysts.
Diseases
- Phenylalanine hydroxylase deficiency
- Pachydermoperiostosis
- Atypical lipodystrophy
- Blethen Wenick Hawkins syndrome
- Sucrose intolerance
- Warburton Anyane Yeboa syndrome
- Gastro-enteropancreatic neuroendocrine tumor
- Nakajo syndrome
- Human ewingii ehrlichiosis
- Leber optic atrophy
Buy eurax 20gm overnight delivery
Note the less prominent staining of the tumor cells as compared to the smooth muscle cells of the muscularis propria skin care 777 discount eurax 20 gm. The tumor primarily involves the submucosa and muscularis propria; however, mucosal involvement is noted in some cases. Wang J et al: Clear Cell Sarcoma-like Tumor of the Gastrointestinal Tract: An Evolving Entity. Metastatic clear cell sarcoma and melanoma may feature these giant cells as well, however, and therefore must always be considered and excluded. Although not shown here, microcystic foci and rosette-like structures have also been reported in this tumor. A patchy lymphoplasmacytic infiltrate is often present, and a peripheral multinucleated foreign body giant cell reaction may also be seen. Amyloid Congo Red Stain (Left) A Congo red stain highlights amyloid deposits with a prominent red-orange coloration. Care must be taken, however, as Congo red can also stain collagen, albeit somewhat less intensely. Pasternak S et al: Soft tissue amyloidoma of the extremities: report of a case and review of the literature. The adjacent connective tissue contains bland fibroblasts and generally appears histologically innocuous. Nonepithelial Lining Reactive Changes (Left) the connective tissue between the cysts often shows a variable degree of reactive change, and foci of subtle myxoid change, resembling myxoma, are common. In some cases it can also spill into the surrounding connective tissue (shown), occasionally inciting a reactive myofibroblastic or vascular proliferation. Superimposed basophilic calcification often varies from cyst to cyst and ranges from heavy involvement to absent. Calcification Multinucleated Giant Cells (Left) Histiocytes and multinucleated giant cells are commonly identified in association with calcium apatite crystals in active tumoral calcinosis. Occasionally, the calcium deposits are rounded and lamellated (shown), resembling psammoma bodies or possibly even parasitic ova. Both are characterized by fibrosclerosis of region adipose and connective tissue with a variable prominent chronic inflammatory infiltrate. Chronic Inflammatory Infiltrate Fat Necrosis (Left) Fat necrosis is a common finding in sclerosing mesenteritis, but may be seen in other disorders. It is identified by eosinophilic to clear/foamy histiocytes associated with adipocytes. Am J Surg Pathol 33: 1330-1340, 2009 Zen Y et al: Retroperitoneal fibrosis: a clinicopathologic study with respect to immunoglobulin G4. The presence of this feature is often readily noticed during gross sectioning of the specimen. IgG4-Related Sclerosing Disease IgG4-Related Sclerosing Disease (Left) Fibrosis with a storiform or loose-swirling pattern is characteristic of IgG4-related sclerosing disease. Phlebitis IgG4(+) Plasma Cells (Left) this image shows inflammation and destruction of a vein (lymphocytic or obliterative phlebitis) within the setting of IgG4-related sclerosing disease. Cardiac muscle is usually identified in histologic sections near the base of the myxoma. Myxoid Stroma Myxoma Cells (Left) the constituent cells of cardiac myxoma generally show small hyperchromatic nuclei, which may number from 1 to several. Corded Growth Hemorrhage and Hemosiderin (Left) Hemorrhage is common in cardiac myxoma and is hardly surprising given the vascularity of this tumor. Hemosiderin deposition is also easily identified in most cases, even away from areas of hemorrhage. Thrombus Formation Thick-Walled Vessels (Left) In some cases of cardiac myxoma, a collection of thickwalled and often tortuous blood vessels can be identified, particularly near the base/pedicle of the tumor. Neutrophils may also be identified and in some cases might possibly represent an overlying, coexisting infection. Inflammatory Infiltrate 784 Cardiac Myxoma Other Entities Calcification Smooth Luminal Contour (Left) Stromal calcification may be seen in some cases of cardiac myxoma, particularly tumors localized to the right atrium. Foci of calcification superimposed upon elastic fibers have been referred to as Gamna-Gandy bodies. This surface is often lined by tumor cells, which may show focal increases in cellularity, reminiscent of synovial lining. Papillary/Villous Configuration Exaggerated Papillary/Villous Configuration (Left) Less commonly, a cardiac myxoma may show a irregular papillary or villous luminal configuration, which can also be appreciated grossly. This variant has a higher risk of shedding tumor emboli due to its relative friability. Histologically, it is characterized by loose fascicles of fibroblastic spindled cells. Infiltrative Border Bland Cytology (Left) the cytologic features of cardiac fibroma are uniformly bland, and there is often a conspicuous component of stromal collagen and small, irregular elastic fibers. These lesions are well circumscribed and commonly show thinning of the overlying squamous epithelium. Stromal vessels are prominent, and a chronic inflammatory infiltrate may be seen. Nuclei are often slightly irregular in contour, with vesicular to stippled chromatin and small nucleoli. Large tumors may be confused clinically with a nonovarian pelvic mesenchymal tumor. Stromal Collagen Cellular Fibroma (Left) Some ovarian fibromas are highly cellular and appear to contain comparatively little stromal collagen. Thick collagen bands are common in this tumor and may be seen in both the cellular and hypocellular zones. Paraganglioma arising in the adrenal gland is usually referred to as a pheochromocytoma. This growth pattern is not well developed in all tumors, however, and may be absent. Intranuclear pseudoinclusions are common, as are scattered nuclei with enlargement and pleomorphism. The vessels are often compressed and sinusoidal but larger ectatic or "staghorn" vessels can also be seen, as depicted in this image. Amato B et al: Surgical resection of carotid body paragangliomas: 10 years of experience. These are associated with the sympathetic chain and arterial plexuses and include the adrenal medulla and organ of Zuckerkandl. Carotid Body Carotid Body (Left) this low-power image shows a normal carotid body in connective tissue at the bifurcation of the carotid artery in the neck. This structure represents an aggregate of chemoreceptor tissue that is not encapsulated. Note the larger and less rounded nests in the lower right of the image as compared to the smaller, rounder nests in the upper left. In the setting of extensive intratumoral hemorrhage, a vascular neoplasm may even be considered. In some cases, they can be numerous and prominent in areas, closely resembling solitary fibrous tumor at low power, as depicted. Note the characteristic thin delicate cytoplasmic processes and nuclei of these cells. It is a highly vascularized neoplasm and features vessels ranging from interconnecting thinwalled capillary channels to larger, ectatic vessels. A prominent blood-filled capillary vascular network is often easily appreciated, as depicted. The classic case shows irregular nests, cords, and alveolar spaces within a prominent fibrocollagenous stroma. Biphasic Morphology Melanin Pigment (Left) the larger eosinophilic cells characteristically contain melanin pigment, which may be abundant.
Purchase eurax with a visa
Small strips of schwannian stroma separate the neuroblasts and neuropil acne under beard best eurax 20gm, imparting a nested or multinodular appearance. The neuropil is composed of a dense tangle of fibrillary, eosinophilic cytoplasmic processes. The Schwann cell component can be demonstrated by immunohistochemistry for S100 protein. Subtle Schwannian Stroma Hemorrhage and Necrosis (Left) Neuroblastomas are commonly hemorrhagic with areas of necrosis. Differentiating Neuroblastoma Differentiating Neuroblasts (Left) Differentiating neuroblasts are characterized by an increased amount of eosinophilic cytoplasm, an eccentrically placed nucleus, and vesicular chromatin. An estimated result is usually considered acceptable, as counting 5,000 cells can be tedious. The marrow has been extensively replaced by sheets of metastatic small round cell tumor and shows no areas with normal trilineage hematopoiesis. This finding predicts poor prognosis, although the amount of amplification does not relate to outcome. The Schwann cells lack nuclear atypia and demonstrate nuclear immunoreactivity for S100 protein. The ganglion cells are present in clusters in this tumor, differing from the pattern in maturing ganglioneuroma in which they are present as single cells. Adequate sampling, generally 1 section per centimeter of tumor, is required to make an accurate diagnosis. This case gave rise to a lung metastasis that had a strikingly similar architecture. Cords Within Myxoid Matrix Physaliferous Cells (Left) Tumor cells with bubbly vacuolated cytoplasm ("physaliferous cells") are a characteristic finding in chordoma; however, they are not always present and are not required for the diagnosis. Fluorescence in situ hybridization is a useful ancillary diagnostic tool for extraskeletal myxoid chondrosarcoma. Most cases show a prominent myxoid stroma, and cellularity varies from low and dispersed to highly compact. Ismail H et al: Treatment of undifferentiated embryonal sarcoma of the liver in children-single center experience. It is almost always associated with a bronchus and often forms an endobronchial mass. Architectural Features Reticulated Pattern (Left) this medium-power micrograph highlights the reticulated pattern composed of cords and clusters of epithelioid cells with abundant eosinophilic cytoplasm within a myxoid stroma. The neoplastic cells have round to ovoid nuclei and eosinophilic cytoplasm and are arranged in cords, clusters, and single cells. In this example, a neoplastic area is surrounded by a peripheral rind of dense collagen, which is surrounded by a band of chronic inflammatory cells. This high-power micrograph depicts clusters of epithelioid cells with round, vesicular nuclei and abundant eosinophilic cytoplasm. In this case, the cells are large epithelioid cells with abundant cytoplasm and vesicular round nuclei. They are infiltrative and poorly circumscribed spindle cell neoplasms, and often contain invaginations of benign surface respiratory epithelium (not shown). Recondo G Jr et al: Spindle epithelial tumor with thymus-like differentiation: A case report and comprehensive review of the literature and treatment options. Note the numerous curvilinear arterioles that are spread evenly throughout the tumor. Generally, only the anterior/inferior edge of the liver is palpable on a physical exam. The liver is covered with peritoneum, except for the gallbladder bed, porta hepatis, and the bare area. Peritoneal reflections form various ligaments that connect the liver to the diaphragm and abdominal wall, including the falciform ligament, the inferior edge that contains the ligamentum teres, and the obliterated remnant of the umbilical vein. The structures in the porta hepatis include the portal vein (blue), hepatic artery (red), and the bile ducts (green). While these may help to fix the liver in position, abdominal pressure alone is sufficient, as evidenced by orthotopic liver transplantation, after which the ligamentous attachments are lost without the liver shifting position. The diaphragmatic peritoneal reflection is the coronary ligament whose lateral extensions are the right and left triangular ligaments. The falciform ligament separates the medial and lateral segments of the left lobe. Conversely, hepatic venous branches lie between hepatic segments and interdigitate with the portal triads, but never run parallel to them. Segments are numbered in a clockwise direction, starting with the caudate lobe (segment 1), which cannot be seen on this frontal view. The falciform ligament divides the lateral (segments 2 and 3) from the medial (segments 4A and 4B) left lobe. The horizontal planes separating the superior from the inferior segments follow the course of the right and left portal veins. Flow in the left portal vein is directed towards the transducer, indicating that the flow is hepatopetal and therefore normal. When measuring velocity, proper angle correction is the key to obtaining accurate velocities. This is the typical anatomy in this location, although anatomic variants of the right hepatic artery may occur in which the hepatic artery may be located anterior to the common bile duct. Notice that the normal hepatic parenchyma is slightly hyperechoic compared to the normal kidney. Note the hepatic veins have no discernible wall, whereas the portal veins have slightly echogenic walls. Normal gallbladder wall thickness should be measured at the interface with the liver and should be less than 3 mm in thickness. The extrahepatic bile duct, hepatic artery, and portal vein run in the lesser omentum. The fundus of the gallbladder extends beyond the anterior-inferior edge of the liver and can be in contact with the hepatic flexure of the colon. The duct lumen is irregular due to redundant folds of mucosa, called the spiral folds of Heister, that are believed to regulate the rate of filling and emptying of the gallbladder. The cystic duct joins the hepatic duct to form the common bile duct, which passes behind the duodenum and through the pancreas to enter the duodenum. Most accessory ducts are on the right side and usually enter the common hepatic duct, but they may enter the cystic or common bile duct. While referred to as "accessory," these ducts are the sole drainage of bile from at least 1 hepatic segment. Ligation or laceration can lead to significant hepatic injury or bile peritonitis. Ideally, a patient must fast for at least 4 hours to allow for adequate gallbladder distension. The intrahepatic bile ducts are localized within the portal triads, which are visible by the prominent echogenic walls of the portal veins in these triads.
Proven eurax 20gm
Skin examination revealed numerous eczematous plaques with open acne 2009 dress best 20gm eurax, crusted lesions as well as papillomatous warts. A complete blood count showed an elevated white blood cell count of 14,000 cells l-1 with a marked eosinophilia of 5000 cells l-1, hemoglobin of 13 g dl-1, and elevated platelet count of 700,000 cells l-1. Immunoglobulin levels revealed normal IgG, low IgM, and a significantly high IgE of 15,000 mg dl-1. Despite having received vaccinations, Mariam had poor vaccine titers to tetanus and pneumococcus. Abdominal imaging showed prominent dilatation of the intrahepatic and extrahepatic biliary system, caused by chronic inflammation that had led to scarring and stricture formation. She underwent an endoscopic retrograde cholangiopancreatography and a biliary sphincterotomy to release the obstruction of her biliary tree. Once her infection was cleared, she was placed on an aggressive regimen of topical steroids and emollients to treat her severe eczema. Although her total IgG level was elevated, because of the poor function of her antibodies she was placed on intravenous immunoglobulin replacement every 3 weeks. Mariam underwent fully matched hematopoietic stem cell transplantation from her donor sister and is currently doing well with resolution of her eczema, recurrent infections, and food allergy, as well as normalization of her IgE, eosinophil count, and lymphocyte profile. Infections of the hepatobiliary tree by viruses or parasites, namely Cryptosporidium, often result in chronic inflammation, scarring, and destruction of the biliary tree, referred to as sclerosing cholangitis. Central nervous system infections have also been seen, particularly with Epstein-Barr virus, with the potential for devastating consequences. These include squamous cell carcinomas related to chronic cutaneous viral infections, as well as lymphomas and smooth muscle tumors caused by Epstein-Barr virus. Autoimmune phenomena include destruction of red blood cells (hemolytic anemia), hypothyroidism, and blood vessel inflammation (vasculitis). Abnormal skewing of the immune system results in marked elevations in eosinophil and IgE levels. Defective integrin-mediated signaling negatively affects T cell survival, with a resulting peripheral T cell lymphopenia commonly seen. Impaired actin accumulation at the cytotoxic synapse of natural killer cells is another factor likely responsible for impaired viral immunity. Early treatment is recommended, as patients who have already acquired chronic infections are at risk for a complicated transplantation course, owing to the chance of viral reactivation during myeloablative therapy and graft-versus-host disease. In those who have not undergone stem cell transplantation, supportive care is critical, including intravenous immunoglobulin as well as antibiotic and antiviral prophylaxis. An effective immune response requires that leukocytes be able to move rapidly from a quiescent state to an activated one upon stimulation. To function efficiently, leukocytes have to modulate their energy production and biosynthetic processes in concert with the needs of the cell throughout their lifespan. This requires that cellular metabolism be carefully regulated and tightly linked to the state of the immune cell. Through a combination of external stimuli, intracellular signaling cascades, and transcriptional events, metabolism is regulated tightly to match the demands of a given cellular state. This important link between metabolism and immunity is best illustrated in T lymphocytes. Stimulation of effector T cells through their T cell receptors and costimulatory molecules induces a switch in their metabolic program from -oxidation to aerobic glycolysis. This enables the T cells to keep up with the demand for rapid growth and proliferation. Lipid oxidation is replaced by lipid biosynthesis along with the generation of other macromolecules that are needed for cell proliferation and differentiation during an immune response. The transition of effector T cells to memory T cells is marked by a reversal of the metabolic program. These changes match the lower energy requirement of memory T cells that is needed for immune surveillance. This pathway promotes aerobic glycolysis and supports the generation of effector T cells. James was born without complications but had multiple episodes of acute otitis media and respiratory infections requiring antibiotic treatment during his childhood. When he was 7 years of age, he was admitted to the hospital for persistent fever, productive cough, and increased work of breathing. A chest X-ray showed opacity of the right lower lobe consistent with pneumonia and his respiratory culture grew Hemophilus influenzae. Two years later, he was admitted again with mild respiratory distress due to pneumonia in the left lower lobe. His respiratory virus panel was negative, and sputum culture grew Streptococcus pneumoniae. In both instances, he improved shortly after initiation of intravenous antibiotics. His lymphadenopathy and splenomegaly did not improve after two weeks of antibiotic treatment. Additional laboratory tests were performed after his visit to the Immunology Clinic. He follows up regularly in the Immunology Clinic and has had no significant infections since the initiation of treatment. In the steady-state setting, each catalytic subunit is normally associated with an inhibitory subunit and the heterodimer dissociates upon activation by specific stimuli. Based on your knowledge of different metabolic programs in T lymphocytes, what is likely the primary substrate utilized by regulatory T cells for energy production The genes encoding the p110and p85 subunits are found on chromosomes 1 and 5, respectively. Why are heterozygous mutations in either of these genes sufficient to cause disease Fungal infections range from mucocutaneous candidiasis and deep dermatophytosis to invasive candidiasis, invasive aspergillosis, and pneumocystosis. Multiple primary immunodeficiencies may underlie fungal infections in children and young adults. In this case, we focus on immune disorders that increase susceptibility to mucocutaneous candidiasis. Candida species are commonly part of normal mucocutaneous flora, but can also cause superficial or invasive candidiasis. Superficial infections can affect the mouth, esophagus, digestive and genital mucosa, nails, and skin. By contrast, invasive Candida disease affects viscera or other sterile sites, like blood and cerebrospinal fluid. Although the mucocutaneous epithelium is the obligate port of entry to deeper infections, mucocutaneous disease and invasive disease are almost always mutually exclusive, which suggests that they have distinct immunopathogenic pathways. Candidiasis is mostly caused by Candida albicans, a polyphenic yeast that changes its morphology based on environmental cues, primarily switching between a single-celled and a hyphal form. Each form expresses unique surface antigens that are recognized by only a subset of host cell receptors. The morphological and antigenic variation of Candida is necessary to produce human disease and different forms are detected in histopathological examination of mucocutaneous disease versus cultures from patients with invasive candidiasis. Therefore, morphological identification of different Candida forms corresponds to distinct immunopathogenic defects in patients. Marylin Cassedy is a 10-year-old female with a history of recurrent oral thrush and perineal candidiasis since age 2 and recurrent pneumonias and chronic diarrhea since age 4. Nonetheless, she received intravenous pulse steroids along with red blood cell and platelet transfusions. She remains stable on anakinra, cyclosporine, and prednisone to prevent further activation of her immune system. These patients have a high fungal burden on their skin and mucosal surfaces, but their risk of developing disseminated candidiasis is low. Ultimately, this results in production of defensins and other molecules with antifungal activity.
Syndromes
- Pneumonia - cytomegalovirus
- High blood pressure
- Coma
- X-rays
- Medications (muscle relaxers, anti-spasticity medications) can reduce the muscle overactivity.
- The task may have already been learned
- Neurosyphilis
- Nausea and vomiting
Generic 20 gm eurax
After an evaluation for the recurrent abortions including karyotype of the parents acne under arms purchase eurax amex, hysterosalpingogram, vaginal sonogram, and testing for antiphospholipid syndrome, the obstetrician concludes the uterine fibroids are the etiology. Which of the following types of uterine fibroids would most likely lead to recurrent abortion She is currently asymptomatic and expressed surprise that she had "growths" of the uterus. If she were to develop symptoms, which of the following would be the most common manifestation W hile pushing during the second stage of labor, she is noted to have fetal bradycardia associated with some vaginal bleeding. Submucosal myomata Umbilical cord prolapse Uterine rupture Placental abruption Fetal congenital heart block 41. The patient has finished her childbearing, but adamantly refuses surgical management for her fibroids. A 45-year-old G2P2 woman has significant heavy menstrual bleeding due to uterine fibroids. The pelvic ultrasound shows two large uterine fibroids- one in the anterior corpus and one in the uterine fundal region. Which of the following is the best way to ensure that the uterine fibroids are not leiomyosarcoma Submucousal fibroids are the fibroids most likely to be associated with recurrent abortion because of their effect on the uterine cavity. The contours of the endometrium are altered and therefore, less favorable for implantation. There may be insufficient vasculature to provide adequate blood supply to the growing embryo if it were to implant along the side of the endometrium containing a submucosal fibroid. In the second trimester of pregnancy, the other answer choices are not associated with an increased risk of recurrent abortion because they do not alter the integrity of the endometrium. Menorrhagia is the most common symptom of uterine fibroids, and severe menorrhagia often leads to anemia. Infertility and recurrent abortion may occur with submucosal fibroids due to the effects on the uterine cavity, whereas impingement on the ureters is most likely to occur with subserosal fibroids, but these are much less common than menorrhagia. Pelvic pain is not very common, and many uterine fibroids are asymptomatic and only require monitoring. If the uterine leiomyomata are large enough, patients may complain of pressure to the pelvis, bladder, or rectum. Though rare, a uterine fibroid on a pedicle may twist, leading to necrosis and severe pain. Extensive myomectomies sometimes necessitate cesarean delivery because of the risk of uterine rupture. Most practitioners use the rule of thumb that if the endometrial cavity is entered during myomectomy, a cesarean delivery should be performed with pregnancy. As with uterine rupture, fetal bradycardia may also occur if the umbilical cord becomes prolapsed, but cord prolapse is not a risk factor from having a myomectomy. A submucosalmyomata is related to problems with fertility and implantation of the embryo, not problems during labor such as uterine rupture. Placental abruption is not associated with fetal bradycardia or as a risk after myomectomy. Myomectomies do not cause congenital anomalies or disease processes to occur in a developing fetus. The rapid growth of the uterus suggests leiomyosarcoma; the diagnosis and treatment are surgical, especially in a woman of nonchildbearing age. Also, substantial growth of uterine fibroids in postmenopausal women is unusual due to the lower estrogen levels. Once a fibroid degenerates into cancer, progestin therapy and gonadotropin-releasing hormone agonists have no more effect on the tumor and are no longer treatment options for shrinking the mass. For a relatively large uterus due to fibroids, uterine artery embolization is the best alternative therapy to surgery. Although rare, leiomyosarcoma does occur and can be very difficult if not impossible to distinguish from a uterine fibroid. Thus, percutaneous biopsy or even better surgical resection and pathological examination are the best ways to assess for leiomyosarcoma. Endometrial biopsy and uterine D&C are usually not helpful to evaluate for leiomyosarcoma. The most common symptom of uterine fibroids is menorrhagia, heavy bleeding during menses. The physical examination consistent with uterine leiomyomata is an irregular pelvic mass that is mobile, midline, and moves contiguously with the cervix. Leiomyosarcoma rarely arises from leiomyoma; rapid growth or a history of prior pelvic irradiation should raise the index of suspicion. Significant growth in suspected uterine fibroids in a postmenopausal woman is unusual and generally requires surgical evaluation. Asymptomatic uterine fibroids require surgical intervention in the presence of unexplained rapid growth, ureteral obstruction, or the inability to differentiate the fibroid from other types of pelvic masses. Robotic-assisted, laparoscopic, and abdominal myomectomy: a comparison of surgical outcomes. On pelvic examination, the uterus is 4-week size and nontender, and there are no adnexal masses. She states that the pain was intense last night, and that something that looked like liver passed per vagina. Know that a normal ultrasound examination does not rule out the presence of an ectopic pregnancy. Understand the clinical presentations of and the treatments for the different types of abortions. Considerations In scenario 1, this 18-year-old patient complains of lower abdominal pain and vaginal spotting. Although there are numerous possible causes, the priority should be to assess for possible pregnancy and especially possible ectopic pregnancy. She does not have a history of sexually transmitted diseases, which if present would be a risk factor for an ectopic pregnancy. The physical examination is unremarkable and ultrasound does not show any adnexal masses. She noted intense cramping pain the night before and passed something that looked like liver to her. This may be tissue, although the gross appearance of presumed tissue can be misleading. The clinical picture of passage of tissue, resolution of cramping and bleeding, and a closed cervical os are consistent with a completed abortion. N otably, this patient is of advanced maternal age, and spontaneous abortions are more common in older patients. The most common cause identified with spontaneous abortion is a chromosomal abnormality of the embryo. The cervix remains open due to the continued uterine contractions; the uterus continues to contract in an effort to expel the retained tissue. Because all the tissue has passed, the uterus no longer contracts, and the cervix closes. The more difficult assessment is in the first 6 to 7 weeks of gestation when the status of the pregnancy and location of the pregnancy are uncertain. It is of paramount importance to determine if the woman is hypotensive, volume depleted, or has severe abdominal or adnexal pain. These patients will most likely need laparoscopy or laparotomy since ectopic pregnancy is probable. For asymptomatic women, the quantitative human chorionic gonadotropin level is useful. Another option would be a single progesterone level: levels > 25 ng/ mL almost always indicate a normal intrauterine gestation, whereas values < 5 ng/ mL usually correlate with a nonviable gestation.
Buy eurax pills in toronto
These deposits fail to stain with methenamine silver in contrast to the glomerular basement membrane skin care unlimited purchase eurax 20gm mastercard. The glomerular capillary lumina are obliterated, and an occasional foam cell is seen. Mise et al: Renal prognosis a long time after renal biopsy on patients with diabetic nephropathy. An Y et al: Renal histologic changes and the outcome in patients with diabetic nephropathy. Diabetic Nephropathy Glomerular Diseases Mesangial Hypercellularity Mesangial Sclerosis (Left) the glomerulus is enlarged with diffuse mesangial sclerosis and moderate proliferation. The glomerular basement membranes are mildly thickened, although this is best seen by electron microscopy. Acute Interstitial Nephritis Armanni-Ebstein Lesion (Left) Biopsies from patients with diabetic nephropathy often have substantial interstitial inflammation with eosinophils. Systematic studies have not found correlations with drug therapy, only with interstitial fibrosis and tubular atrophy. The proximal tubules have basal vacuoles shown to contain lipid in this autopsy case. Arteriolar hyalinosis is seen at the vascular pole, and synechia at the tubular pole probably results in an atubular glomerulus. Mesangiolysis Microaneurysm (Left) Capillaries form a microaneurysm capping one of the mesangial nodules. It is possible that thrombosis and organization of the microaneurysm are responsible for the nodule. Vague laminations are evident in the nodules, suggesting recurrent episodes of injury and organization. Matrix in Mesangium Arteriolar Hyalinosis (Left) Within the mesangium, sometimes accentuated mesangial matrix fibers can be seen (termed diabetic fibrillosis). These fibers measure approximately 10 nm in diameter and are not composed of immunoglobulin or amyloid. Glomerular basement membranes are possibly only segmentally thickened with no appreciable duplication. Philadelphia: Lippincott, Williams & Wilkins, 2007 Kuppachi S et al: Idiopathic nodular glomerulosclerosis in a non-diabetic hypertensive smoker-case report and review of literature. Mesangial expansion is also present, compatible with early glomerular nodule formation, and well-formed nodules were present in other glomeruli. Leishmania donovani Entamoeba histolytica Filaria Candida albicans Histoplasma capsulatum Coccidioides immitis Viruses, Fungi, Parasites Dengue virus Varicella zoster Hantavirus Influenza virus Human immunodeficiency vIrus Coxsackie virus (A-4, B-5) Parvovirus B19 Infectious Causes of Thrombotic Microangiopathy Enteric Pathogens E. Capillaries are congested, with erythrocytolysis, and there are neutrophils and karyorrhexis. All glomeruli are typically involved (diffuse), and entire glomerular tufts are affected (global). Prasto J et al: Streptococcal infection as possible trigger for dense deposit disease (C3 glomerulopathy). Neutrophils, as well as occasional eosinophils, can be seen in glomerular capillaries. The glomerulus is also hypercellular with neutrophils and eosinophils in glomerular capillary loops. About 30% of biopsied cases have > 50% crescents, a poor prognostic finding in adults but probably not in children. Capillary loops are characteristically not patent due to endocapillary hypercellularity and endothelial swelling. These can be distinguished from artifactual bleeding from the biopsy procedure by their compaction & mixing with proteinaceous material. This biopsy is from 3-year-old girl with hypertension, "Coca-Cola" urine, 3+ protein & blood on urinalysis, Cr 2. Nodules are evident, but the neutrophils in capillaries indicate an additional process. This child died after a streptococcal infection & was reported as a clinicopathologic case in 1929 by Cabot and Mallory. Stratta P et al: New trends of an old disease: the acute post infectious glomerulonephritis at the beginning of the new millenium. Kanjanabuch T et al: An update on acute postinfectious glomerulonephritis worldwide. Haas M et al: IgA-dominant postinfectious glomerulonephritis: a report of 13 cases with common ultrastructural features. Haas M: Incidental healed postinfectious glomerulonephritis: a study of 1012 renal biopsy specimens examined by electron microscopy. The interstitium contains an inflammatory infiltrate, including scattered eosinophils. Overlying podocytes that are effaced and reactive contain increased numbers of cytoplasmic organelles. This glomerulus has endocapillary hypercellularity with loss of patency of capillary loops. IgA Deposition Mesangial Deposits (Left) the amorphous, electron-dense deposits are primarily in the mesangium in S. A mild interstitial nephritis is also evident with occasional neutrophils and eosinophils. Mesangial Hypercellularity and Mild Interstitial Nephritis Endocapillary Hypercellularity (Left) Mesangial and endocapillary hypercellularity are evident with loss of patent capillaries in this diabetic patient who had S. Mesangial IgA Mesangial IgG (Left) IgG with a predominately mesangial pattern commonly accompanies IgA in S. Prominent C3 is present primarily in the mesangium and was accompanied by IgA and IgG. C3 is usually more intense than IgA in this condition, in contrast to IgA nephropathy. Subepithelial Deposit Subepithelial Deposit With Cupping (Left) Subepithelial deposits are found in S. Cellular Crescent Granular Deposits of C3 (Left) Immunofluorescence of C3 shows granular positivity in a 68-year-old man with staphylococcal endocarditis. Endocarditis Glomerular Diseases "Flea Bitten" Kidney Hypercellular Glomerulus (Left) the surface of the kidney has innumerable red spots resembling flea bites in a patient with endocarditis due to nongroupable, nonhemolytic streptococcal infection of a calcified aortic valve. Hypercellular Glomeruli and Tubular Injury in Endocarditis Segmental Glomerular Hypercellularity (Left) In glomerulonephritis associated with endocarditis, hypercellular glomeruli and tubular debris can be seen. Fibrinoid Necrosis Glomerular Capillary Thrombus (Left) Segmental fibrinoid necrosis in a glomerulus due to endocarditis (bacteroides) is shown. This feature led to the view that glomerular lesions of endocarditis were "embolic," however, the glomerulonephritis is now known to be largely mediated by immune complexes. The pattern of deposits is atypical for both membranous and postinfectious glomerulonephritis. Rolla D et al: Post-infectious glomerulonephritis presenting as acute renal failure in a patient with Lyme disease. Extensive effacement of the podocyte foot processes correlates with the presence of nephroticrange proteinuria. Protein reabsorption droplets are noted in an adjacent podocyte with extensive foot process effacement. Correlation with clinical and laboratory data is necessary to confirm the association with hepatitis C infection. Focusing up and down on the microscope reveals a characteristic refractile appearance due to the staining quality of the prominent accumulation of immune complexes. A rare intact glomerulus shows very mild mesangial hypercellularity and mesangial matrix expansion. This finding alone should prompt careful searching for focal segmental glomerulosclerosis and additional level sections should be ordered if needed. Ki-67 Proliferative Glomerular Epithelial Cells Segmental IgM (Left) Proliferation of visceral & parietal epithelial cells as well as tubular epithelium is characteristic of collapsing glomerulopathy regardless of cause & persists even at the end stage, as shown in this Ki-67 stain.
20gm eurax amex
Active antibody-mediated rejection acne x tretorn buy eurax 20 gm free shipping, chronic, membranoproliferative glomerulonephritis with immune complexes vs. Acute tubulointerstitial (type I) rejection, polyomavirus nephritis, 806 Acyclovir. Antibody-mediated allograft rejection, 938 Antibody-mediated rejection - C4d immunohistochemistry/immunofluorescence, 1074 - chronic, hereditary endotheliopathy, retinopathy, nephropathy, and stroke vs. Anti-glomerular basement antibody disease (Goodpasture), microscopic polyangiitis vs. Antiphospholipid antibody syndrome, mimicking of vasculitis by, 457, 458 Antitubular basement membrane antibody nephritis, druginduced acute tubulointerstitial nephritis vs. Antiviral tubular toxicity, in renal allograft disease, 939 Aortic dissection, renal artery stenosis vs. Autosomal recessive renal tubular dysgenesis, renin mutation with tubulointerstitial nephritis vs. Complement deficiencies, membranoproliferative glomerulonephritis with immune complexes vs. Cryocrystalglobulinemia, 259 Cryoglobulinemia, 259 - mixed, membranoproliferative glomerulonephritis with immune complexes vs. Drug-induced granulomatous interstitial nephritis and vasculitis, granulomatosis with polyangiitis (Wegener) vs. Infectious diseases, membranoproliferative glomerulonephritis with immune complexes vs. Pauci-immune necrotizing and crescentic glomerulonephritis, IgG4-related disease vs. Retrograde cortical venous invasion, examination, 1047 Rhabdomyolysis - acute tubular injury vs. Smith-Lemli-Opitz syndrome, associated with congenital anomalies, 829 Smoking-associated nodular glomerulosclerosis. Systemic or renal parasitic infection, eosinophilic granulomatosis with polyangiitis vs.
Order 20gm eurax overnight delivery
On day 7 in the hospital acne face mask purchase 20 gm eurax free shipping, she is diagnosed with severe features of preeclampsia and the decision is made to administer magnesium sulfate and deliver the baby. W hich of the following findings is most likely present in this patient to necessitate delivery You explain that it is to prevent the seizures that may complicate preeclampsia and may even cause death. Pedal edema is not pathologic; nondependent edema, such as of the face and hands, may be consistent with preeclampsia but does not indicate severity of disease. Uric acid levels are known to be elevated with preeclampsia; however, it is not a criterion for severe preeclampsia. In general, the criteria for severe preeclampsia indicate end-organ threat, and generally require delivery for gestational age at or > 34 weeks, and depending on the nature of the threat and the stability of the patient, perhaps delivery at an earlier gestational age. Although the pregnancy is only 28 weeks, in light of the severe feature of preeclampsia with marked thrombocytopenia, the best treatment is magnesium sulfate and delivery. When preeclampsia with severe features is diagnosed, delivery depends on the nature of the threat, the stability of the patient/ fetus, and the gestational age. If the platelet count was higher (90 000), expectant management may be entertained at a tertiary center. Oral antihypertensive therapy, such as labetalol, may be given to the patient to control blood pressure; however, it should not be used as the "treatment" for severe preeclampsia. The most common cause of maternal death due to eclampsia is intracerebral hemorrhage. Patients with gestational hypertension or preeclampsia without severe features do not necessarily require magnesium sulfate for seizure prophylaxis. Magnesium sulfate has been proven to be superior to other anticonvulsants such as valium, Dilantin, or phenobarbital. In the preterm patient with mild preeclampsia, expectant management is generally employed until severe features are noted or the pregnancy reaches 37 weeks. In other words, the risks of prematurity usually outweigh the risks of the preeclampsia until end-organ threat is manifest. H ad this patient been at term, the best step in management would be to induce labor; this is because at term, the risks of prematurity are minimal. Severe, but not mild hypertension associated with preeclampsia, should be controlled with hypertensive medication. For the patient in this scenario, neither induction nor cesarean section is indicated since she is not yet at term. Proteinuria of 5 g over 24 hours is no longer criteria of a severe feature of preeclampsia and does not correspond to maternal or fetal outcome. Mild thrombocytopenia (80 000-100 000) that is stable may be judiciously observed in this patient (in a tertiary care center). Corticosteroid therapy is the single most important intervention to impact on the neonatal outcome in a pregnancy < 34 weeks when delivery is expected imminently (within 7 days). Magnesium sulfate is often given during this time of carefully monitoring the platelet count and liver function tests, but not necessarily delivery. Magnesium sulfate and delivery is an option, but more information such as assessment of fetal status would give a more complete picture. The management of preeclampsia without severe features in a preterm pregnancy is observation until severe features are noted, or term gestation is reached. Severe features complicating preeclampsia or superimposed preeclampsia at a gestational age of 34 weeks or higher should be given magnesium sulfate and delivered. Gestational hypertension is when a pregnant woman has hypertension after 20 weeks of gestation without proteinuria or other evidence of preeclampsia. Acute onset severe hypertension (160 systolic or 110 diastolic) persisting > 15 minutes is considered a hypertensive emergency. The fetal heart rate tracing reveals a baseline heart rate of 120 bpm and a reactive pattern. What test of the vaginal fluid prior to digital examination may indicate risk for preterm delivery What medication can be given to decrease the risk of neurological impairment in the baby The fetal heart rate tracing reveals a baseline heart rate of 120 bpm and is reactive. Medication for neuroprotection: Magnesium sulfate may be given for pregnancies of < 32 weeks when there is imminent delivery. Understand that the basic approach to preterm labor is tocolysis, identification of an etiology, steroids, and magnesium sulfate (if appropriate). The monitor indicates uterine contractions every 3 to 5 minutes, and her cervix is dilated at 3 cm and effaced at 90%. Because of the significant prematurity, many practitioners may elect to treat for preterm labor. A single examination revealing 2-cm dilation and 80% effacement in a nulliparous woman would be sufficient to diagnose preterm labor. Another objective test for preterm delivery risk is transvaginal cervical length ultrasound measurements. A shortened cervix, especially with lower uterine segment changes (funneling or beaking of the amniotic cavity into the cervix), is worrisome. Tocolysis should be initiated, unless there is a contraindication (such as intra-amniotic infection or severe preeclampsia). A careful search should also be undertaken to identify an underlying cause of preterm labor, such as urinary tract infection, cervical infection, bacterial vaginosis, generalized infection, trauma or abruption, hydramnios, or multiple gestations. Last, recent studies have shown that if the pregnancy is < 31 6/ 7 weeks, starting magnesium could help the neurodevelopment of the preterm baby, reducing cases of cerebral palsy in preterm infants. In a nulliparous woman, uterine contractions and a single cervical examination revealing 2-cm dilation and 80% effacement or greater are sufficient to make the diagnosis. The most commonly used agents are indomethacin, nifedipine, terbutaline, and ritodrine. Its best utility is a negative result, which is associated with a 99% chance of not delivering within 1 week. Also an impinging of the amniotic cavity into the cervix, so-called funneling, increases the risk of preterm delivery. H owever, a short cervix or a positive fetal fibronectin alone should not be used exclusively to diagnose preterm labor in an acute situation, as the positive predictive value is poor. This is the subset of preterm births that are most rapidly increasing and comprises most preterm deliveries. The incidence in the United States is approximately 11% of pregnancies, and it is the cause of significant perinatal morbidity and mortality. The main symptoms of preterm labor are uterine contractions and abdominal tightening. The diagnosis is established by confirming cervical change over time by the same examiner, if possible, or finding the cervix to be 2-cm dilated and 80% effaced in a nulliparous woman. Tocolysis is considered if the gestational age is less than 34 to 35 weeks, and steroids are administered if the gestational age is < 34 weeks. Recent randomized controlled trials have suggested that magnesium sulfate is not effective as a tocolytic agent but may be useful for fetal neuroprotection. N ifedipine reduces intracellular calcium by inhibiting voltage-activated calcium channels. Side effects include pulmonary edema, respiratory depression, neonatal depression, and, if given for a long term, osteoporosis. Pulmonary edema is often the most serious side effect, and is seen more often with the -agonist agents.
Buy eurax 20 gm otc
Chancroid is a rare cause of infectious vulvar ulcers in the United States acne essential oil recipe purchase eurax 20 gm line, although worldwide it is quite common; thus, cases occurring in the United States are related to ports of entry. Genital herpes can cause recurrent painful genital sores, and herpes infection can become severe in people who are immunosuppressed. Syphilis typically presents during the first stage of the disease as a small, round, and painless chancre in the area of the body exposed to the spirochete. The Bartholin glands, responsible for vaginal secretions, are located at the entrance of the vagina; they may enlarge into painless abscesses when they become clogged and infected. Vulvar carcinoma typically is nontender, ulcerative, and is more common in postmenopausal women. Herpes simplex virus is the most common cause of infectious vulvar ulcers in the United States. The cervix, vagina, and vulva must be inspected carefully for lesions in a patient in labor with a history of herpes simplex virus. Acyclovir and analogous agents given in pregnancy during primary episodes can decrease the duration of viral shedding and duration of lesions. The patient states that 4 weeks previously, after she had engaged in sexual intercourse, she experienced some vaginal spotting. Long-term management: Expectant management as long as the bleeding is not excessive. Understand that the ultrasound examination is a good method for assessing placental location. Because of the painless nature of the bleeding and lack of risk factors for placental abruption, this case is more likely to be placenta previa, defined as the placenta overlying the internal os of the cervix. Placental abruption (premature separation of the placenta) usually is associated with painful uterine contractions or excess uterine tone. The history of postcoital spotting earlier during the pregnancy is consistent with previa because vaginal intercourse may induce bleeding. The ultrasound examination is performed before a vaginal examination because vaginal manipulation (even a speculum examination) may induce bleeding. Complete placenta previa (A), marginal placenta previa (B), and low-lying placentation (C) are depicted. When the patient complains of antepartum hemorrhage, the physician should first rule out placenta previa by ultrasound even before a speculum or digital examination, since these maneuvers may induce bleeding. At times, transabdominal sonography may not be able to visualize the placenta, and transvaginal ultrasound is necessary and is more reliable for visualizing the internal cervical os. The natural history of placenta previa is such that the first episode of bleeding does not usually cause sufficient concern as to necessitate delivery. H ence, a woman with a preterm gestation and placenta previa is usually observed on bed rest and complete pelvic rest in an effort to prolong gestation and avoid morbidity of fetal prematurity. The bleeding from previa rarely leads to coagulopathy, as opposed to that of placental abruption. Because the lower uterine segment is poorly contractile, postpartum bleeding may ensue. Several risk factors have been cited including parity, increased maternal age, smoking, multiple gestations, prior curettage, and prior cesarean delivery. Of note, placenta accreta (invasion of the placenta into the uterus) is more common with placenta previa, particularly in the presence of a uterine scar such as after a cesarean delivery. Timing of delivery depends on clinical circumstances for placenta previa and placenta accreta. The N ational Institutes of H ealth concluded that elective delivery is ideal at 36-37 completed weeks for these patients, but practices still vary. There is no demonstrated benefit to performing amniocentesis for fetal lung maturity prior to delivery at any gestational age. An ultrasound is performed revealing that the placenta is covering the internal os of the cervix. Schedule an amniocentesis at 34 weeks and deliver by cesarean if the fetal lungs are mature C. Multiple gestation, with the increased surface area of placentation, is a risk factor for placenta previa. H ypertension is not a risk factor for placenta previa; however, it is one of the main risk factors for placental abruption. Polyhydramnios, due to the excess amount of amniotic fluid in the amniotic sac, is also a risk factor for placenta abruption. Salpingitis involves inflammation and infection of the fallopian tubes and over time may lead to permanent scarring of the tubes. Since this particular process is limited to the tubes, there is not an increased risk of placenta previa; rather there is an increased risk of ectopic pregnancy. Unlike placenta abruption, placenta previa is not commonly associated with coagulopathy, painful bleeding, or having a profuse first episode of bleeding. The main distinguishing factor between a previa and abruption is the presence or absence of pain. With abruption, painful uterine contractions are typically the chief complaint, whereas previa is painless. A patient with previa should not deliver vaginally since the lower uterine segment is poorly contractile, and postpartum bleeding may ensue. Ultrasound should be performed first to rule out previa, speculum examination second to assess the cervix and look for lacerations, and finally digital examination. Performing either a speculum examination or digital examination before evaluating the patient with ultrasound puts the patient at risk for hemorrhage. In the setting of a previa, the lower uterine segment and cervix are highly vascularized, and varices of the cervix may be visualized on speculum examination in some situations; however, the speculum itself may cause trauma to these varices and induce bleeding. A blind digital examination may result in further separation of the placenta from the uterus, which could also cause significant bleeding. Very often, a marginal or low-lying placenta previa at the early second trimester will resolve by transmigration of the placenta. It is too early to discuss scheduling a cesarean delivery since the placenta previa may resolve and allow for vaginal delivery. An ultrasound should be repeated in the third trimester to see whether or not the placenta has migrated. If there is suspicion that a percreta exists, a previa has most likely already been diagnosed in the late second trimester or third trimester, so a scheduled cesarean delivery would most likely already be in the plan. During the cesarean, the physician will be able to assess the extent of the placental implantation and base management on how far the placenta has penetrated through the uterine wall. Placenta percreta and increta are usually diagnosed during a cesarean delivery and not radiographically. Amniocentesis for fetal lung maturity is not necessary in the setting of placenta previa at any gestational age. Even if the patient has a placenta previa at the time of delivery, both the mother and baby have an excellent prognosis if a cesarean delivery is performed. Ultrasound is the diagnostic test of choice in assessing placenta previa and should be performed before digital or speculum examination. Placenta previa, in the face of prior cesarean deliveries, increases the risk of placenta accreta. When placenta previa is diagnosed at an early gestation, such as second trimester, repeat sonography is warranted since many times the placenta will move away from the cervix (transmigration). A late-preterm, early-term stratified analysis of neonatal outcomes by gestational age in placenta previa: defining the optimal timing for delivery. Magnetic resonance imaging of clinically stable late pregnancy bleeding: beyond ultrasound. Effectiveness of timing strategies for delivery of individuals with placenta previa and accreta.