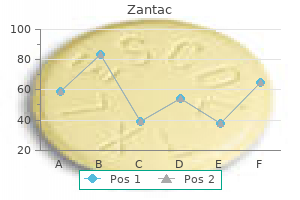
Purchase zantac 150 mg free shipping
Advances in our understanding using this technique have led to the realization that in ow occlusion of the hepatic blood supply can be performed safely for carefully controlled periods even in patients with cirrhotic livers gastritis zyrtec discount zantac 150 mg without a prescription. Furthermore, intermittent occlusion followed by brief periods of reperfusion of the liver will increase the total time of in ow occlusion that can be achieved while still successfully limiting blood loss and reducing the risk for ischemic liver injury. If anything, treatment of pyogenic liver abscess with antibiotic therapy is more di cult and has been complicated by the indiscriminate use of antibiotics over the past several decades. Iatrogenic etiologies of liver abscess may have also been increased by the more invasive and aggressive approaches to benign and malignant pancreatic and biliary tract diseases. Endoscopic retrograde cholangiopancreatography, placement of internal stents, or percutaneous placement of external stents in patients with biliary obstruction can increase the likelihood of the development of a pyogenic liver abscess. Furthermore, immunocompromised patients, such as those receiving cytotoxic chemotherapy for malignant disease, are at increased risk to develop hepatic abscess. However, there is still an occasional role for surgical drainage of a complex or multiloculated abscess. It should not be forgotten in patients treated in the United States because of the number of people who travel to high-risk areas or who have immigrated to the United States from endemic regions. Treatment is generally medical therapy with occasional need for aspiration or percutaneous drainage. An echinococcal or hydatid cyst of the liver is an extremely common cause of cystic liver disease worldwide. It is critical to consider this in the di erential diagnosis of a patient with a liver cyst because aspiration and spillage of the cyst contents can produce an anaphylactic reaction and spread of the scoleces throughout the peritoneal cavity. However, this is rarely successful alone, and treatment of larger lesions may also require very careful percutaneous aspiration of all cyst contents followed by installation of the cyst cavity with protoscolecidal agents. Surgical treatment still has a primary role in management of hydatid cysts of the liver and may include resection of the area of the liver bearing the cyst or complete drainage of the cyst while preventing spillage of cyst contents. Simple liver cysts are diagnosed frequently in patients who are undergoing upper abdominal ultrasound or axial body imaging for some other diagnostic purpose. It is particularly common in patients with malignant disease during staging to be referred to a hepatobiliary surgeon with a nding of cystic lesions in the liver. Asymptomatic simple cysts essentially are a radiographic nding and do not require any therapeutic intervention. In the unusual case of giant cysts that are causing pain or compression on adjacent structures, either an open or laparoscopic unroo ng of the cyst can be performed as long as there is no connection to the biliary tract. A laparoscopic approach is my preferred treatment for patients with symptomatic simple cysts of the liver as the recovery time is rapid and the symptom relief rate without recurrence of symptoms exceeds 95%. If a biliary tract connection is recognized, concern must be raised for a possible biliary cystadenoma or cystadenocarcinoma. Most of the cystic neoplasms are benign, but complete resection of both benign and malignant neoplastic cysts of the liver is mandatory to prevent a local recurrence of disease. Cystadenoma or cystadenocarcinoma should be suggested if aspiration of a cyst reveals either bile-stained or mucinous uid. Similar to asymptomatic simple cysts of the liver, patients with solid benign tumors of the liver are often referred to hepatobiliary surgeons after either a transcutaneous ultrasound or an axial body imaging technique reveals a single or multiple solid lesions. Cavernous hemangiomas, hepatocellular adenomas, and focal nodular hyperplasia may be found in almost one in ve patients undergoing a liver imaging technique. It is not uncommon for an individual patient to have more than one type of benign hepatic tumor. Like asymptomatic simple cysts, hemangiomas and focal nodular hyperplasia of the liver are usually only radiographic ndings and not associated with symptoms. In those unusual situations where these lesions are large or symptomatic, surgical resection with either an open or laparoscopic approach is indicated. Parenthetically, a signi cant proportion of early laparoscopic resections were performed for benign solid tumors of the liver that may have not required any type of resection. A benign solid or cystic neoplasm of the liver in an area that is technically feasible to resect with a laparoscopic approach is not an indication for a resection if the lesion is asymptomatic. In orthotopic liver transplant series that accrued patients after proper patient selection criteria were established the 5-year survival rates vary from 45 to 75%. It is not clear if such screening programs would be cost e ective but this will become an issue due to the increased incidence of this disease in both modern and less developed regions of the world. Hepatitis B vaccinations have made an impact on the incidence of this cancer in portions of the world where chronic hepatitis B infection is hyperendemic. Education and prevention are important factors, but clearly better treatments are also needed for this lethal disease. However, use of sorafenib enhances survival by an average of less than 3 months, so more e ective therapeutic agents for patients with advanced disease must be sought and developed. Cholangiocarcinomas may arise from the extrahepatic bile ducts, the intrahepatic bile ducts, or the gallbladder. For extrahepatic bile duct cancer and gallbladder cancer, identifying the association of tumors in the bile ducts with key vascular, lymphatic, and hepatic structures is critical to optimize the resection. An excellent example is the importance of caudate resection in patients with hilar cholangiocarcinoma as direct extension of these cancers along small bile ducts directly into the caudate is a common site of failure in patients undergoing a resection that does not include the caudate. Resection of regional lymph nodes is recommended in patients with gallbladder cancer and cholangiocarcinoma and is important for staging. It is not clear that adjuvant therapy signi cantly improves the long-term outcome of patients but some small studies of systemic chemotherapy or chemoradiation therapy have suggested improved local disease control and possibly an improved median disease-free survival time. Cholangiocarcinomas generally arise in patients with no evidence of cirrhosis or concomitant risk factors for the development of chronic liver injury so major liver resection can be performed more frequently in this patient population. Discussion in the surgical literature has ranged widely regarding the volume of liver that must be resected as part of an operation for cholangiocarcinoma, particularly for gallbladder cancer or hilar cholangiocarcinoma. My general philosophy and data from our experience indicates that major extended hepatectomy should only be performed if this is the procedure that is required to permit complete resection of the tumor with negative resection margins. As previously noted, resection of the caudate is important as a component of the resection of patients with hilar cholangiocarcinoma, but the volume of other liver that must be resected should be based on leaving as much normal, non-malignant liver as possible after the resection. In most western countries, surgical resection of colorectal cancer liver metastases is a primary focus of many hepatobiliary surgeons. Following the report in the late 1980s of a retrospective analysis of tumor registry data, it was recognized that patients undergoing hepatic resection of colorectal metastases can achieve long-term disease-free and overall survival. While there has not been, and likely never will be a randomized prospective controlled clinical trial comparing resection of colorectal cancer liver metastases with nonsurgical treatment, it is accepted by both the surgical and medical oncology communities that properly selected patients should be considered for surgical treatment of their colorectal cancer liver metastases. Like cholangiocarcinoma, most patients with colorectal cancer liver metastases have relatively normal liver function. Many hepatobiliary surgeons prefer to proceed directly with resection of colorectal cancer liver metastases if the patient has technically resectable disease and an adequate functional hepatic volume remaining after the operation. Others advocate for the use of short courses of neoadjuvant therapy to assess the biological response in the tumors to potentially e ective systemic agents. Ultimately, hepatobiliary surgeons will operate on some colorectal cancer patients who have received extensive systemic therapy. It has now been recognized that patients who initially present with clearly unresectable disease but who have a dramatic response to systemic therapy may be considered candidates for resection and can achieve 5-year survival rates in excess of 35% following operation. Ongoing clinical trials internationally will be important to understand the role of neoadjuvant and adjuvant therapy after surgical resection of colorectal cancer liver metastases. Additionally, we now know that even a small tumor-free resection margin can be associated with improved patient outcomes, so aggressive surgical approaches should be considered even in tumor that is near major central portal or hepatic venous structures. We, and other surgical groups, have also been aggressive about applying staged hepatic resections in properly selected patients. It is important to recognize that discussing such an aggressive surgical approach is considered reasonable and rational because the 5-year survival rate in patients with unresectable colorectal cancer liver metastases treated with active chemotherapeutic drugs continues to be 5% or less. As noted previously, intraoperative ultrasonography is critical for the hepatobiliary surgery performing resection for colorectal cancer, or for other solid tumor liver metastases. Despite improvements in axial body imaging, I still nd additional small tumors not seen on preoperative imaging studies in up to 10% of patients undergoing resection. I routinely map the location of major intrahepatic portal and hepatic venous structures. I also use ultrasonic dissection devices combined with saline-enhanced cautery devices to perform a safe and relatively bloodless liver transection. In ow occlusion can be applied judiciously, but many patients require no in ow occlusion when using vascular stapling and other liver transection techniques. I am not an advocate for any speci c technique as being superior, I am a rm believer that all surgeons should be well versed in use of equipment available for safe hepatic transection and should use techniques with which they are comfortable and con dent in their results.
Buy genuine zantac online
Prior to commencing treatment with azathioprine gastritis diet 3 day buy zantac 150mg online, thiopurine methyltransferase levels should be checked, with monthly monitoring of the full blood count, renal and liver function thereafter. Development of leukopenia, thrombocytopenia, pancreatitis, or a gross derangement in transaminase levels are indications for the termination of treatment. In recent years, in iximab has been used increasingly as a therapeutic alternative to azathioprine. It is generally safe and well tolerated, although screening for tuberculosis is warranted prior to commencing therapy. Massive hemorrhage and perforation are also indications for emergency surgery, but these complications are usually seen in association with acute colitis. Other indications include stricture, dysplasia or cancer, and systemic complications. When toxic acute severe colitis is successfully treated nonoperatively, approximately 50% of patients will require surgery within 1 year. On the other hand, acute colitis or toxic megacolon is still a life-threatening illness especially if a perforation occurs or the patient develops other septic complications. However, patients with acute colitis, without toxic megacolon, can be equally ill, and the risk of perforation is not closely correlated with the amount of colonic dilation. It is recommended that failure after a 24-hour trial of intensive medical therapy is an indication for urgent colectomy in patients with toxic megacolon. Joint involvement of gastroenterologists and surgeons at an early stage and frequent reassessment of patients is critical in making decisions about treatment as well as the timing of various interventions. It may also help Acute perforation is an infrequent occurrence, with the risk directly related to both the extent of bowel disease and the severity of the acute attack of colitis. Although the overall risk of perforation during an attack is less than 4%, the risk may rise to about 10% if the attack is severe. Perforations occur more frequently in the presence of toxic megacolon, but it is important to remember that megacolon is not a prerequisite for the development of perforation. In the presence of a colonic perforation, subtotal colectomy with ileostomy is the procedure of choice. More often, there is di use bleeding from the severely in amed mucosal surface of the bowel. Instead, a subtotal colectomy is usually the preferred option, because these patients tend to be very ill and a lesser operation that does not expose the patient to a potentially hazardous pelvic dissection is better tolerated. Also, preservation of the rectum allows the patient to have a reconstructive procedure in the future. With this approach, some patients may have continued bleeding from the retained rectal segment, but rarely will urgent proctectomy have to be performed. Again, it is important to emphasize that timely surgical intervention in patients with severe acute colitis should be considered because it may obviate this life-threatening complication. Furthermore, the opinion of the gastroenterologist is equally important because he or she has usually followed the patient for a long time and has knowledge of the chronicity and severity of the symptoms as well as the response to medical therapy, whereas the surgeon is disadvantaged because he or she is seeing the patient only at one point in time. Corticosteroids are still the mainstay of medical management of ulcerative colitis, and patients who are steroid-dependent or have quick are-ups of the disease when the steroids are tapered should be advised to have surgery. As stated previously, this is the most subjective indication for surgery and patients will vary in their preferences, and therefore it is important that they be fully informed about the risks and the outcomes that can be expected following surgery. However, there are a few situations where colectomy may be performed where cancer or dysplasia is not con rmed. Also, pseudopolyps, while benign and with no malignant potential, have been identi ed as a predictor of malignancy. Second, individuals who have a stricture generally should be advised to have surgery because it may be impossible to keep the rest of the colon under surveillance. Recent studies have shown that raised lesions that have the endoscopic appearance of sporadic adenomas can be treated safely by polypectomy as long as there are no other areas of dysplasia. It is important to remember that the objective of screening is to identify and treat individuals before they develop cancer, not detect early cancer. Because dysplasia is usually multifocal in ulcerative colitis, the entire colon and rectum should be removed. However, more commonly if patients are su ering from severe extraintestinal manifestations, the intestinal disease is also active. Growth failure is de ned as a cessation of linear growth over a 6-month period or a decrease exceeding one or more standard deviations. However, even with emergency surgery, there are certain measures, such as correction of uid and electrolyte abnormalities, administration of antibiotic and thromboembolic prophylaxis, and stoma marking that should be done. A recent meta-analysis of almost 5000 patients showed that the anastomotic leak rate and surgical site infection rate were the same in patients in whom the mechanical bowel preparation was omitted compared to those who did receive a mechanical bowel preparation. Brown and Buie reviewed the literature and concluded that there is no evidence that supraphysiologic doses of corticosteroids are necessary to prevent hemodynamic instability or adrenal insu ciency in patients who have been on steroids ey recommended that patients should preoperatively. Postoperatively steroids should be weaned slowly to avoid adrenal insu ciency, especially in individuals who have been on steroids for a prolonged period. Alternatively, if enteral feeds are tolerated, surgery may be delayed while the nutritional status of the severely malnourished patient is improved. An ileostomy is frequently required in patients having surgery for ulcerative colitis. When a stoma is sited, it should be placed away from scars and creases and in a location where the patient can visualize it adequately when sitting or lying. Both stoma placement and siting of incisions are extremely important in patients with ulcerative colitis. Serious cardiac and respiratory complications are unusual because most patients having surgery for ulcerative colitis are young. It was not until the 1940s when it became clear that the only de nitively curative treatment of chronic ulcerative colitis is total proctocolectomy or, as a compromise, subtotal abdominal colectomy with ileostomy. However, the ileostomy was fraught with technical problems from the outset, including the optimal location of the ostomy site, surgical construction and attachment techniques, and leak proof collection pouches and skin barriers. It was not until the early 1950s when Brooke in the United Kingdom and Crile and Turnbull in the United States proposed that the ileal stoma could be immediately matured into the skin with primary mucocutaneous suturing. It was his reasoning that a high-volume, low-pressure reservoir could be constructed and attached to the abdominal wall, which could be emptied using a catheter but otherwise would be continent. However, continence was not maintained, and subsequently a valve made out of an intussuscepted segment of small bowel was interposed between the reservoir and the outlet. Patients searching for an alternative to a Brooke ileostomy enthusiastically received the Kock pouch. Unfortunately, the procedure is technically di cult and despite multiple technical revisions to the procedure, there is a high complication rate and need for reoperation. In addition, the patient still has a stoma, leading surgeons to seek other alternatives. Continence and stool frequency was acceptable, and the patients could evacuate via the normal route. In addition, following multiple technical changes, the procedure could be performed with relatively low morbidity, good functional results, improved quality of life, and patient satisfaction. Currently, there are several options for patients requiring surgery for ulcerative colitis. Subtotal colectomy and ileostomy is often performed in patients requiring surgery urgently or emergently. All have advantages and disadvantages, and the patient must be fully informed about the procedures, including the risks and functional results so that he or she may partake in the decision making. However, irrespective of the procedure, most patients following surgery have an improved quality of life. Even in patients with severe colitis, including those with severe bleeding, colectomy alone usually results in a dramatic clinical improvement without the morbidity associated with a potentially hazardous pelvic dissection. Proctocolectomy is only rarely indicated if there is profound hemorrhage from rectal ulceration. A second indication is in individuals with chronic disease who are malnourished and are on high doses of corticosteroids (the equivalent of 30 mg or more of prednisone/ day). While subtotal colectomy is an excellent operation in these situations, it is not a de nitive procedure, and unless there is a contraindication, proctectomy should be performed in the future as there is an ongoing risk of malignancy. A midline incision provides wide access to the abdomen and does not compromise placement of a stoma on either side of the abdomen. Great care should be taken in the handling of the tissues as they may be extremely friable in severe disease or in cases of prolonged steroid use.
Buy zantac 300 mg online
Most lesions are now treated via endoscopic therapy (injection of epinephrine or other sclerosants gastritis symptoms images discount generic zantac canada, electrocoagulation, hemoclipping, rubber band ligation, and photocoagulation) or via angiographic embolization. Surgery is sometimes necessary, at which time the lesion may be oversewn or resected. Typically, the stomach twists along its long axis (organoaxial volvulus), and the greater curvature ips up. It is usually a chronic condition that can be surprisingly asymptomatic and expectant nonoperative management is usually advised, especially in the elderly. Surgery is recommended for symptomatic patients, especially if these are severe and/or progressive. Dyspnea, palpitations, and dysphagia may be seen due to compressive e ects of the distended stomach on the surrounding organs. Symptoms are often relieved with vomiting or, if possible, passage of a nasogastric tube. Elective operation may often be done laparoscopically and usually involves reduction of the stomach and repair of hiatal hernia, with or without gastropexy. Congenital diverticula are rare, true diverticula that typically occur near the gastroesophageal junction and are found on the lesser curve or in the posterior area. Symptoms are due to in ammation and may produce pain or bleeding but perforation is rare. Gastric retention of more than 10% of the standard low-fat meal at 4 hours is indicative of delayed emptying. Severe gastroparesis might result in recurrent hospitalizations, malnutrition, and signi cant mortality. Patients failing medical therapy are often considered for a variety of surgical interventions, the e cacy of which is not well studied. Completion gastrectomy seems to provide symptom relief in postsurgical gastroparesis. Aspiration of the foreign body during removal may occur, as well as potential rupture of drug-containing bags in "body packers. In body packers as well as in patients with large jagged objects, surgical removal is recommended. Endoscopy con rms the diagnosis and may be useful in controlling the bleeding, but 90% of patients stop bleeding spontaneously. In patients who continue to bleed, balloon tamponade; angiographic embolization; or selective infusion of vasopressin, systemic vasopressin, and surgery are other treatment options. Most of the procedures described in this chapter can be performed with minimally invasive techniques. Role of Helicobacter pylori infection and non-steroidal anti-in ammatory drugs in peptic-ulcer disease: a meta-analysis. Relationship between Helicobacter pylori eradication and reduced duodenal and gastric ulcer recurrence: a review. Proximal gastric vagotomy: does it have a place in the future management of peptic ulcer A systematic review of Helicobacter pylori eradication therapy-the impact of antimicrobial resistance on eradication rates. Mechanical endoscopic methods of haemostasis for bleeding peptic ulcers: a review. Endoscopy for acute nonvariceal upper gastrointestinal tract hemorrhage: is sooner better Helicobacter pylori eradication is superior to ulcer healing with or without maintenance therapy to prevent further ulcer haemorrhage. Helicobacter pylori infection after partial gastrectomy for peptic ulcer and its role in relapsing disease. A randomized study comparing laparoscopic versus open repair of perforated peptic ulcer using suture or sutureless technique. Gastric outlet obstruction resulting from peptic ulcer disease requiring surgical intervention is infrequently associated with Helicobacter pylori infection. Preliminary experience with hydrostatic balloon dilation of gastric outlet obstruction. Octreotide, a long-acting somatostatin analog, in the management of postoperative dumping syndrome. Some (eg, partial or total gastric resection) are technically di cult or are of debatable merit (eg, laparoscopic resection for cancer). Laparoscopic wedge resection, combined with either intra-operative endoscopic or radiologic localization, often is possible for most localized, benign lesions such as lipomas, or gastric diverticula, although the incision required to retrieve the specimen may be larger than the initial port incisions. Unidenti ed curved bacilli in the stomach of patients with gastritis and peptic ulceration. Co-adaptation of Helicobacter pylori and humans: ancient history, modern implications. Helicobacter are indigenous to the human stomach: duodenal ulceration is due to changes in gastric microecology in the modern era. Helicobacter pylori test-and-eradicate versus prompt endoscopy for management of dyspeptic patients: a randomized trial. Clinically signi cant gastrointestinal bleeding in critically ill patients in an era of prophylaxis. Increased risk of fundic gland polyps during long-term proton-pump inhibitor therapy. Gastric bezoar complicating laparoscopic adjustable gastric banding and review of literature. American Gastroenterological Association Technical Review on the Diagnosis and Treatment of Gastroparesis. Laparoscopic ultrasound guidance for laparoscopic resection of benign gastric tumors. Gastric adenocarcinoma accounts for over 90% of all cases of gastric cancers globally. Gastric cancer remains the second leading cause of cancer-related deaths worldwide. In fact, death rates attributed to gastric cancer in the Unites States fell by over 40% for males and 32% for females between the years 1990 and 2005. Patients diagnosed with earlier stages of gastric cancer have a distinct advantage in 5-year survival compared to those with more advanced-stage disease. Although the 5-year survival rate for all cases of gastric cancer in the United States between the years 1996 and 2004 was 25%, it was as little as 3% for patients with distant disease and as high as 61% for those who had only localized disease at time of diagnosis. In addition to environmental factors, a clear impact of genetic susceptibility on the risk of developing gastric cancer has been identi ed. Chapter 22 Gastric Adenocarcinoma and Other Gastric Neoplasms (Except Gastrointestinal Stromal Tumors) 465 the development of gastric cancer. Hereditary Forms of Gastric Cancer One of the rst documented cases of hereditary gastric cancer dates back to the 17th century and was described for the family of the French emperor Napoleon Bonaparte. Although evidence from several retrospective studies support an association between a high dietary intake of fruits and vegetables and a decreased gastric cancer risk, this association proved not to be statistically signi cant in prospective trial analyses. Other, more concerning symptoms that are often referred to as alarm symptoms, include weight loss, dysphagia, persistent vomiting, gastrointestinal bleeding, anemia, and a palpable abdominal mass. Another study analyzing patients who underwent urgent endoscopy for the presence of alarm symptoms or dyspepsia unresponsive to empiric therapy found that 3. Although the presence of alarm symptoms is poorly predictive for the presence of cancer, when they are present in gastric cancer patients, the presence and number of alarm symptoms has been shown to correlate with an advanced stage of disease. Here, patients were followed from their initial diagnosis of gastric cancer to their date of death. In patients with advanced disease, a palpable supraclavicular mass, generally on the left side, can be a sign of distant nodal metastasis (the Virchow node). A bulky antral tumor or extensive nodal metastases will occasionally lead to jaundice from bile duct obstruction in the hepatoduodenal ligament. A palpable abdominal mass may be found, sometimes from a bulky primary tumor, but more commonly from omental caking with metastases.
| Comparative prices of Zantac | ||
| # | Retailer | Average price |
| 1 | Menard | 911 |
| 2 | H-E-B | 499 |
| 3 | Delhaize America | 232 |
| 4 | A&P | 704 |
| 5 | J.C. Penney | 153 |
| 6 | Safeway | 574 |
Discount 300 mg zantac visa
Intervention in necrotizing pancreatitis: an evidence-based review of surgical and percutaneous alternatives nervous gastritis diet 150 mg zantac for sale. Percutaneous catheterdirected debridement of infected pancreatic necrosis: results in 20 patients. Long-term follow-up of patients with necrotizing pancreatitis treated by percutaneous necrosectomy. Outcome di erences after endoscopic drainage of pancreatic necrosis, acute pancreatic pseudocysts, and chronic pancreatic pseudocysts. Retroperitoneal approach and endoscopic management of peripancreatic necrosis collections. Surgical results for severe acute pancreatitis-comparison of the di erent surgical procedures. Necrosectomy and laparostomy-a combined therapeutic concept in acute necrotising pancreatitis. Pancreatic abscess: results of prolonged irrigation of the pancreatic bed after surgery. Debridement and closed cavity irrigation for the treatment of pancreatic necrosis. Retroperitoneal and peritoneal drainage and lavage in the treatment of severe necrotizing pancreatitis. Retroperitoneal drainage in the management of the septic phase of severe acute pancreatitis. Most regional and systemic complications occur in association with severe acute pancreatitis. In addition to this variation in content (solid to uid) local complications can also be sterile or infected, with the latter having signi cant prognostic signi cance. A pancreatic pseudocyst is the term that has traditionally been applied to this lesion, but it is now appreciated that the contents may be anywhere on a continuum from entirely solid to entirely uid. While they may be associated with parenchymal necrosis, their presence does not necessarily indicate necrosis or signi cant duct disruption. Chronic pleural e usions as a result of an internal pancreatic stula often are treated with a chest tube, nasojejunal tube feeding, and somatostatin. Persistence or recurrence will require identi cation of a pancreatic leak and either drainage into a Roux-en-Y limb of jejunum or distal resection of the pancreas. Classi cation of the severity of acute pancreatitis: how many categories make sense If spherical or ovoid with sharp margins, suggesting that under some pressure from ongoing leakage, they are more likely to persist. Massive collections of uid around or within the pancreas are more likely to be due to disruption of the main pancreatic duct and are more likely to persist for a number of weeks or continue to increase in size. Intervention, by surgical or radiological drainage, risks introducing infection into a usually sterile collection. An asymptomatic uid collection is managed by observation alone, and only in the presence of infection drainage is usually necessary. Continuous peritoneal lavage does not alter the course of the disease and should not be a routine practice. Endoscopic treatment uses a trans-sphincteric pancreatic duct stent, which can be placed across the sphincter of Oddi (to decrease ductal pressure and facilitate drainage), into the uid collection through the disrupted duct (to drain the collection directly) or across the damaged duct (to redirect drainage from the collection to the duodenum and to stent the duct to reduce the risk of stricture formation). Postnecrotic collections contain both solid and uid components, and are not surrounded by a brous capsule during the rst few weeks. Over time necrotic tissue undergoes liquefaction and forms part of this uid collection. Pseudocyst A pseudocyst is a well-circumscribed uid collection with no associated tissue necrosis that is present for 4 or more weeks after disease onset. However, this is not an absolute distinction as there may be discontinuous epithelium within cystic neoplasms (probably due to pressure atrophy) and partial epithelialization within chronic pseudocysts (facilitated by communication with the main pancreatic duct). As a result, the uid is contained by a developing layer of granulation tissue and brosis that matures over time. Pseudocysts secondary to blunt trauma tend to develop anterior to the neck and body of the gland because the duct is injured where it crosses the vertebral column. In chronic pancreatitis, pseudocysts are thought to develop secondary to obstuction of the pancreatic duct. As a result the risk of pseudocyst complications is probably less than previously considered when pseudocysts were diagnosed on the basis of symptoms. Complications occur in about 10% of cases and the four main complications of pseudocysts are infection, rupture or internal stulation, bleeding, and mass e ect. Rupture into the gastrointestinal tract may be associated with signi cant haemorrhage, that is a sentinel bleed. Rupture into the peritoneum leads to pancreatic ascites and can be a dramatic presentation with acute abdominal pain and rigidity from chemical peritonitis. Bleeding associated with a pancreatic pseudocyst can be a life-threatening complication. Bleeding may occur secondary to erosion of the gut mucosa with the impending development of a cystoenteric stula. More ominous is the direct erosion of a signi cant visceral vessel, including the splenic, gastroduodenal, and middle colic vessels. If time and patient stability permit, emergency selective splanchnic angiography is performed to delineate the site of bleeding, and embolization is attempted. Otherwise, emergency surgery is required, consisting of oversewing of the bleeding vessels and internal or external drainage of the pseudocyst. Occasionally it is possible to resect the pseudocyst, which is e ective in preventing recurrent hemorrhage. A large pseudocyst may exert a mass e ect, and thereby produce early satiety (stomach), partial or complete intestinal obstruction (duodenum, gastric outlet, esophagogastric junction, and rarely small or large bowel), cholestasis (bile duct), and venous thrombosis (portal, superior mesenteric, and splenic veins) leading to portal or segmental hypertension and varices. However, often the early stages of pseudocyst formation are observed radiologically before symptoms develop, and this provides some forewarning. It will demonstrate the key features of a pseudocyst (ie, size, shape, wall thickness, and contents), the nature of the pancreas (ie, presence and extent of necrosis, diameter of pancreatic duct, and features of chronic pancreatitis, including atrophy and calci cation), and the relationship of these to the surrounding organs. In symptomatic cases where treatment is likely, it may be useful to plan further management. Because of the risks of exacerbating pancreatitis, perforation, bleeding, and introducing infection, it is preferably done within 48 hours of any planned drainage procedure. Over 90% of patients with a pseudocyst have some abnormality of the pancreatic duct. A communication of this type is a relative contraindication to external drainage of a pseudocyst. Bleeding usually results in an increase in abdominal pain and possible syncope, tachycardia, and hypotension. Pseudocysts usually contain uid with elevated amylase (>5000 U/mL) and an absence of tumor markers, but this should not be relied on for a de nitive diagnosis. Although not directly correlated, a large pseudocyst is more likely to cause discomfort and pain. In the absence of symptoms or evidence of enlargement, conservative management is usually reasonable. In many centers it has become less common to treat a pseudocyst solely on the grounds of a failure to resolve. An enlarging asymptomatic pseudocyst that has been present for 6 weeks is usually treated. A natural-history study from India indicates that asymptomatic pseudocysts less than 7. Also important is the level of available expertise and experience with the various treatment modalities. If adherent to the stomach or duodenum, the options are di erent than if the pseudocyst is deep within the retroperitoneum and covered by bowel loops. When larger than 6 cm in diameter, and when it continues to enlarge during the rst month, a pseudocyst is more likely to persist and develop complications. Size alone is a poor predictor because resolution can occur even with very large pseudocysts. If multiple pseudocysts are present, then minimally invasive approaches may not be feasible.
Buy zantac 150 mg low price
In contrast gastritis diet jump buy zantac paypal, this particular serotype is rarely found in clinical isolates from Western countries. If the abscess ruptures, peritonitis and sepsis may be presenting features 7,8,11 (Table 43-4). Findings may include an elevated right hemidiaphragm, a right pleural e usion, and/or right lower lobe atelectasis. Abdominal lms may show hepatomegaly, air- uid levels in the presence of gas-forming organisms, or portal venous gas if pylephlebitis is the source. On the other hand, cholangiography, usually through an indwelling biliary stent, may visualize the abscess. Duplex ultrasound of pyogenic liver abscess with intervening portal vessels blocking safe access to percutaneous drainage. Treatment e appropriate treatment for pyogenic liver abscesses requires treatment of the abscess itself and concomitant treatment of the source. Although antibiotics alone may be curative, patients sustain higher risk of failure and complications such as abscess rupture. Percutaneous transhepatic drainage is relatively low-risk and successful treatment method for both polymicrobial liver abscesses and K. Exceptions to this strategy include multiple small abscesses and miliary fungal abscesses. Fluoroquinolones can replace aminoglycosides, and metronidazole can be used instead of clindamycin, especially if an amebic source is suspected. Single-agent therapy with ticarcillin-clavulanate, imipenem-cilastatin, or piperacillin-tazobactam is also acceptable. Metronidazole is ine ective against aerobic organisms, and regimens containing rst-generation cephalosporins have been shown to be inferior in treatment of K. A combination of an aminoglycoside and either an extended spectrum -lactam, such as piperacillin, or second- or third-generation cephalosporin is preferred for patients with K. However, multiple small abscesses frequently imply biliary tract disease and may require biliary drainage for source control. Similarly, fungal abscesses are miliary in nature and not amenable to percutaneous or surgical drainage. Needle aspiration and percutaneous catheter drainage of liver abscesses have similar mortality rates; however, recurrence rates and the requirement for surgical intervention may be greater in those who undergo aspiration alone. A randomized controlled trial by Rajak et al22 in 1998 compared percutaneous needle aspiration to catheter drainage and also found no major complications and no deaths. Most of the candidal liver abscesses in patients with hematologic malignancies are a manifestation of disseminated candidiasis and have high mortality rates. In patients with hematologic malignancies, the yield of positive culture is often less than 50% with the diagnosis usually based on microscopic examination or histopathology from deep tissues. On the basis of pharmacokinetics predictions, uconazole (12 mg/kg/d; 800 mg/d for the 70-kg patient) may be a suitable alternative, particularly in less critically ill patients. With the advent of systemic antibiotics, transperitoneal surgical exploration also was considered a safe surgical approach. Since the 1980s, treatment has shifted to a less invasive approach using percutaneous needle aspiration or catheter drainage to treat pyogenic abscesses. Surgical drainage is currently reserved for patients who have failed nonoperative therapy, those who need surgical treatment of the underlying source, those with multiple macroscopic abscesses, those on steroids, or those with concomitant ascites. Contrast injected into the abscess cavity through a percutaneously placed drainage catheter. Sinogram performed 2 weeks later revealing a decrease in the size of the abscess cavity. Shackl- Chapter 43 Hepatic Abscess and Cystic Disease of the Liver 909 empyema, and pneumonia. Usually, however, the abscess does not rupture but develops a controlled leak, resulting in a perihepatic abscess. Councilman and LaFleur of Johns Hopkins Hospital went on to detail the pathogenic role of amebae and coined the terms "amebic dysentery" and "amebic liver abscess" in 1891. No general consensus has been reached regarding risk factors due to the variability of the patient population being studied (Table 43-5). Entamoeba dispar is associated with an asymptomatic carrier state and not with disease. Normally, no invasion occurs, and the patient develops amebic dysentery or becomes an asymptomatic carrier. In a small number of cases, the trophozoite invades through the intestinal mucosa, travels through the mesenteric lymphatics and veins, and begins to accumulate in the hepatic parenchyma, forming an abscess cavity. Lique ed hepatic parenchyma with blood and debris gives a characteristic "anchovy paste" appearance to the abscess. Low socioeconomic status and unsanitary conditions are signi cant independent risk factors for infection. Humans become reservoirs, and transmission occurs by ingesting food and water contaminated with amebic cysts, or occasionally through person-to-person contact. Invasive amebiasis can include anything from amebic dysentery to metastatic abscesses. Trophozoites invade and induce apoptosis in colonic mucosa, resulting in "buttonhole" ulcers with undermined edges. Diaphragmatic involvement causes right-sided pleural pain or pain referred to the shoulder. Hepatomegaly with point tenderness over the liver or subcostal region is common26 (Table 43-6). In contrast to pyogenic liver abscesses, amebic liver abscesses are more likely to occur in males younger than 50 years who have immigrated or traveled to a country where the disease is endemic. Because amebic abscesses involve destruction of liver parenchyma and are often larger than pyogenic liver abscesses, patients may have an elevated prothrombin time. Diagnostic aspirations are usually done when amebic serologies are negative and a pyogenic cause needs to be ruled out. Numerous studies have demonstrated the inadequacies of microscopic examination for E. Drainage procedures, regardless of the approach, are reserved for those cases in which the diagnosis is questionable or when complications occur. Only 40% have typical sonographic features of amebic liver abscess, and serial scanning shows no change in the ultrasound features despite adequate treatment. Eventually, resolution may be complete or result in a small residual cystic cavity that resembles a simple cyst of the liver. Biopsies of the edge of an ulcer or the wall of an abscess reveal trophozoites with periodic acid-Schi stain. Nitroimidazoles, especially metronidazole, are the mainstays of treatment for invasive amebiasis. Nitroimidazoles with longer half-lives (secnidazole, tinidazole, and ornidazole) are better tolerated and can be given for shorter periods, but these are not available in the United States. At 5 days, an 85% cure rate is achieved, and this response may be increased to 95% by 10 days. Abscess aspiration resulted in improved liver tenderness within the rst 3 days, but no other di erence was demonstrable between the two groups. Bene ts were observed in resolution time of pain and tenderness, but no additional bene t was found with percutaneous needle aspiration plus metronidazole versus metronidazole alone for uncomplicated amebic liver abscesses in hastening clinical and radiologic resolution. Laparotomy is indicated for life-threatening hemorrhage that may or may not be related to abscess rupture, or when the amebic abscess erodes into a neighboring viscus and control of the involved viscus is necessary.
Order zantac in india
Others have used percutaneous intracorporeal electrohydrolic lithotripsy for hepatolithiasis gastritis and back pain buy zantac 300 mg overnight delivery. Using this technique, in a series of 53 patients, complete clearance of stones was achieved in 92%, and during a mean follow-up of 5 years, 9% had recurrent symptoms of biliary obstruction. Remnant stones were found in only one patient and removed by percutaneous choledochoscopy performed through the T-tube site. Patients who underwent an operation were found to have less need for reintervention. Although the evolution of this disease is unclear, it will likely continue to challenge us. With lessons learned from more common biliary pathologies and the application of novel technologies, we would anticipate better outcomes for our future patients. Epidemiology and natural history of common bile duct stones and prediction of disease. Bile infection documented as initial event in the pathogenesis of brown pigment biliary stones. Evaluation of probability of bile duct stone presence by using of non-invasive procedures. Ultrasonic evaluation of common bile duct stones: prospective comparison with endoscopic retrograde cholangiopancreatography. Preoperative ultrasonographic assessment of the number and size of gallbladder stones: is it a useful predictor of asymptomatic choledochal lithiasis Diagnosis of common bile duct stones by intravenous cholangiography: prediction by ultrasound and liver function tests compared with endoscopic retrograde cholangiography. Abnormal common bile duct sonography: the best predictor of choledocholithiasis before laparoscopic cholecystectomy. Scoring system to predict asymptomatic choledocholithiasis before laparoscopic cholecystectomy: a matched case-control study. Predictive factors for synchronous common bile duct stones in patients with cholelithiasis. Role of endoscopic retrograde cholangiopancreatography for suspected choledocholithiasis in patients undergoing laparoscopic cholecystectomy. Noncontrast helical computed tomography versus endoscopic ultrasound for suspected choledocholithiasis and common bile duct dilation: a prospective blind comparison. Prospective evaluation of magnetic resonance cholangiography in patients with suspected common bile duct stones before laparoscopic cholecystectomy. Magnetic resonance imaging of the common bile duct to exclude choledocholithiasis. Evaluation of magnetic resonance cholangiography in the management of bile duct stones. Treatment of bile duct stones: value of laser lithotripsy delivered via percutaneous endoscopy. Percutaneous transhepatic papillary balloon dilatation as a therapeutic option for choledocholithiasis. Methods, indications, and results of percutaneous choledochoscopy: a series of 161 procedures. Gallbladder motility and lithogenicity of bile in patients with choledocholithiasis after endoscopic sphincterotomy. Duodenoscopic sphincterotomy for common bile duct stones in patients with gallbladder in situ. Fate of the gallbladder with cholelithiasis after endoscopic sphincterotomy for choledocholithiasis. Risks of leaving the gallbladder in situ after endoscopic sphincterotomy for bile duct stones. Impact of gallbladder status on the outcome in patients with retained bile duct stones treated with extracorporeal shockwave lithotripsy. Clinical application of a new mechanical lithotripter for smashing common bile duct stones. Outcome of mechanical lithotripsy of bile duct stones in an unselected series of 704 patients. Electrohydraulic lithotripsy in 111 patients: a safe and e ective therapy for di cult bile duct stones. Extracorporeal shock wave lithotripsy for clearance of bile duct stones resistant to endoscopic extraction. Randomized study of intracorporeal laser lithotripsy versus extracorporeal shock-wave lithotripsy for di cult bile duct stones. Long-term follow-up after treatment of common bile duct stones by extracorporeal shock-wave lithotripsy. Fluoroscopically guided laser lithotripsy versus extracorporeal shock wave lithotripsy for retained bile duct stones: a prospective, randomised study. Extracorporeal shock wave lithotripsy for di cult common bile duct stones: initial New Zealand experience. Endoscopic treatment combined with extracorporeal shock wave lithotripsy of di cult bile duct stones. Extracorporeal shockwave lithotripsy of common bile duct stones without preliminary endoscopic sphincterotomy. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are di cult to extract. Treatment of non-extractable common bile duct stones with combination of ursodeoxycholic acid plus endoprostheses. Biliary endoprostheses in elderly patients with endoscopically irretrievable common bile duct stones: report on 117 patients. Retained common bile duct stones: a comparison between biliary stenting and complete clearance of stones by electrohydraulic lithotripsy. Long-term follow-up of patients with gallbladder in situ after endoscopic sphincterotomy for choledocholithiasis. Choledocholithiasis in non-cholecystectomized patients: Endoscopic sphincterotomy and afterwards. Late biliary complications after endoscopic sphincterotomy for common bile duct stones in patients older than 65 years of age with gallbladder in situ. Endoscopic management of common bile duct stones leaving the gallbladder in situ: a cohort study with longterm follow-up. Evaluation of the biliary tree during laparoscopic cholecystectomy: laparoscopic ultrasound versus intraoperative cholangiography: a prospective study of 150 cases. A prospective comparison of laparoscopic ultrasound vs intraoperative cholangiogram during laparoscopic cholecystectomy. Primary closure versus Ttube drainage after laparoscopic choledochotomy for common bile duct stones. Laparoscopic transcystic bile duct stenting in the management of common bile duct stones. Management of common bile duct stones in a single operation combining laparoscopic cholecystectomy and peroperative endoscopic sphincterotomy. Choledochoduodenostomy, transduodenal sphincteroplasty and sphincterotomy for calculi of the common bile duct. Choledochoduodenostomy an important surgical tool in the management of common bile duct stones: a review of 126 cases. Choledochoduodenostomy and sphincterotomy in the treatment of choledocholithiasis. Long-term results of choledochoduodenostomy in the treatment of choledocholithiasis: assessment of 225 cases. Long-term follow-up of patients with side-to-side choledochoduodenostomy and transduodenal sphincterosplasty. Long-term follow-up after choledochojejunostomy for bile duct stones with complex clearance of the bile duct. A technique of biliary tract reconstruction with complete follow-up in 44 consecutive cases. Recurrent biliary stricture: patterns of recurrence and outcome of surgical therapy.
Buy 300 mg zantac with mastercard
Other cancer types include squamous cell carcinoma symptoms of gastritis in babies 300mg zantac with visa, small cell carcinoma, and sarcomas. Adenocarcinomas of the bile duct are classi ed as sclerosing, nodular, or papillary (analogous to the classi cation scheme for gallbladder adenocarcinomas). Metastasis to celiac and/or periaortic and caval lymph nodes are considered distant metastasis; M0, no distant metastasis; M1, distant metastasis present. In patients with intrahepatic cholangiocarcinoma, laboratory studies usually reveal an increased alkaline phosphatase level in the setting of normal bilirubin levels. In patients with extrahepatic cholangiocarcinoma, laboratory tests are usually consistent with the presence of obstructive jaundice. Findings of distal cholangiocarcionomas include dilation of intra- and extrahepatic bile ducts and the gallbladder, with or without a mass in the head of the pancreas. Unilobar bile duct obstruction typically results in atrophy of the a ected liver lobe together with hypertrophy of the una ected lobe (atrophy-hypertrophy complex). Absence of the atrophy-hypertrophy complex can suggest vascular encasement by tumor. For patients who are surgical candidates, an important goal of the preoperative evaluation is determining the proximal and distal tumor extent. It also allows for visualization of the bile ducts both proximal and distal to a stricture. If surgery is not planned, tissue diagnosis can be obtained through endoscopic or percutaneous biopsy. Surgical Therapy As is the case for gallbladder cancer, complete surgical resection is the only potentially curative therapy for patients with cholangiocarcinoma. Available retrospective data and one recently reported multicenter randomized controlled trial22 suggest that among patients undergoing pancreaticoduodenectomy for periampullary cancers, routine preoperative biliary stenting is associated with increased perioperative morbidity rates, especially with respect to infectious complications. However, this experience should not be extrapolated to patients with perihilar cholangiocarcinomas, for whom the relationship between preoperative stenting and operative outcomes is less clear. Some authors believe stents placed preoperatively make intraoperative assessment of tumor extent more difcult. In our experience, bilateral Ring catheters, placed percutaneously into the left and right biliary systems shortly before the time of surgery, greatly facilitates the resection of perihilar cholangiocarcinomas. Surgical Technique Resectable intrahepatic cholangiocarcinomas are treated using standard liver resections, and distal cholangiocarcinomas are treated by pancreaticoduodenectomy. We begin with exploratory laparoscopy to rule out the presence of disseminated disease that may have escaped detection on preoperative imaging. Next, we lower the hilar plate by incising the liver capsule at the base of the quadrate lobe (segment 4) between the gallbladder fossa and the umbilical ssure. At this point we palpate the tumor in an attempt to assess its proximal and distal extent. We then begin mobilization of the extrahepatic biliary tree from its surrounding structures. We then dissect the extrahepatic biliary tree o of the underlying vascular structures, starting distally and working proximally. Chapter 51 Cancer of the Gallbladder and Bile Ducts 1071 Proximal common duct Ring catheters Mobilized gallbladder Portal v. Only after this step is accomplished the possibility of tumor vascular invasion is de nitely eliminated. Dissection here is facilitated by placing vessel loops around the left and right hepatic ducts and placing them on traction as necessary. Because the left duct typically runs along the undersurface of the liver (segment 4) for a longer distance than the right duct, it is usually easier to dissect the left duct rst and encircle it with a vessel loop prior to dissecting the right duct. We nd that the Ring catheters are particularly helpful in the identi cation of the right and left hepatic ducts during this stage of the procedure. Frozen sections of the proximal and distal margins should be checked intraoperatively, with the goal of achieving negative microscopic margins (R0 resection). Reconstruction following resection of Klatskin tumors consists of bilateral hepaticojejunostomies to a 60-cm retrocolic Roux-en-Y limb of jejunum. Small secondary or tertiary biliary branches should be incorporated into the anastomoses or ligated. If Ring catheters have not been placed preoperatively, the Silastic catheters can be placed as follows: Randall stone forceps are inserted into the intrahepatic biliary tree through the transected bile ducts and out the liver surface. Following completion of resection, the Ring catheters are exchanged for Silastic catheters, as described in the text. Using cautery, two small openings in the distal portion of the Roux limb are made, through which the distal ends of the Silastic catheters are placed. We then suture the Roux limb to the undersurface of the liver and to the mesocolon. We suture two large radiopaque clips to the surface of the liver at the sites where each of the Silastic tubes exit. Recently, more aggressive approaches that include the routine application of liver resection, and portal vein resection in select cases, are being reported with increasing frequency. Although the highest 5-year postoperative survival rates have been reported from centers using such aggressive surgical approaches, these extended procedures should be done only if they can be performed with low perioperative morbidity and mortality rates. In addition, some centers have reported the application of preoperative portal vein embolization, to induce lobar hypertrophy and thereby extend the limits of liver resection in patients at risk of developing hepatic insufciency postoperatively. Chapter 51 Cancer of the Gallbladder and Bile Ducts 1073 Finally, orthotopic liver transplantation has been applied to patients with intrahepatic and perihilar cholangiocarcinomas. However, cancer recurrence occurs in over 50% of cases, and 5-year survival rates average only 22%. Long-term survivors have been reported; most of these patients had small, peripheral cholangiocarcinomas discovered incidentally. For patients with known cholangiocarcinoma, liver transplantation following neoadjuvant therapy in carefully selected and staged patients is being studied, with some promising initial results. Adjuvant Therapies Adjuvant chemotherapy, radiotherapy, or chemoradiotherapy is commonly o ered, based on results of retrospective series. However, clear e cacy data derived from prospective randomized clinical trials are lacking. Similarly, neoadjuvant therapy, associated with anecdotal reports of tumor response su cient to permit margin-negative resection in patients with advanced cholangiocarcinoma, needs to be studied further. Palliation e major goal of palliation is relief of symptoms of biliary obstruction. Endoscopic or percutaneous biliary stenting is associated with less morbidity than surgical biliary bypass and is therefore recommended except in patients who are found to have unresectable disease at the time of surgical Specimen L. Endoscopic stenting is the preferred approach for distal bile duct cancers; proximal cancers are more di cult to stent endoscopically and usually require a percutaneous approach. Patients with a Bismuth type I hilar cholangiocarcinoma are usually palliated e ectively with a single biliary stent. However, in a prospective, randomized controlled trial of patients with hilar cholangiocarcinoma, unilateral biliary drainage was found to provide adequate palliation of obstructive jaundice; patients randomized to receive bilateral biliary stents had higher complication rates (cholangitis) but no detectable bene ts. Stenting should be performed using percutaneous or endoscopic techniques postoperatively. For patients who are found to have unresectable disease at the time of open exploration, available retrospective evidence suggests that surgical biliary bypass o ers more durable palliation than percutaneous or endoscopic stenting. Patients with unresectable distal cholangiocarcinoma should undergo choledocho- or hepaticojejunostomy. Segment 3 or 5 bypass is used in patients with advanced perihilar cholangiocarcinoma with predominantly right- or left-sided disease, respectively. Localization of the segment 5 duct is di cult, as no external anatomic landmarks exist and considerable parenchymal dissection if often necessary. External beam radiation and transcatheter brachytherapy may contribute to pain relief and biliary decompression; however the data on the e ects of radiation on survival duration are con icting.
Purchase zantac 300mg visa
Minimal-access approaches to complications of acute pancreatitis and benign neoplasms of the pancreas gastritis relieved by eating purchase zantac 300 mg otc. Minimally invasive approaches to the management of pancreatic pseudocysts: review of the literature. Minimally invasive management of pancreatic abscess, pseudocyst, and necrosis: a systematic review of current guidelines. A comprehensive classi cation of invasive procedures for treating the local complications of acute pancreatitis based on visualization, route, and purpose. Acute necrotizing pancreatitis: intra-abdominal vacuum sealing after necrosectomy. Surgery in the treatment of acute pancreatitis-minimal access pancreatic necrosectomy. Laparoscopic transgastric pancreatic necrosectomy for infected pancreatic necrosis. Laparoscopic-assisted pancreatic necrosectomy: a new surgical option for treatment of severe necrotizing pancreatitis. A technique for laparoscopic-assisted percutaneous drainage of infected pancreatic necrosis and pancreatic abscess. Endoscopic necrosectomy as primary therapy in the management of infected pancreatic necrosis. Perfusion computerized tomography can predict pancreatic necrosis in early stages of severe acute pancreatitis. Echo enhanced ultrasound: a new valid initial imaging approach for severe acute pancreatitis. Usefulness of technetium99m hexamethylpropylene amine oxime-labeled leukocyte scintigraphy to detect pancreatic necrosis in patients with acute pancreatitis. C-reactive protein, antiproteases and complement factors as objective markers of severity in acute pancreatitis. Prophylactic antibiotic treatment in acute necrotizing pancreatitis: Results from a meta-analysis. Meta-analyses on the prophylactic use of antibiotics in acute pancreatitis: many are called but few are chosen. Characteristics of infection with Candida species in patients with necrotizing pancreatitis. Fungal infection but not type of bacterial infection is associated with a high mortality in primary and secondary infected pancreatic necrosis. Clostridium perfringens infection of pancreatic necrosis: absolute indication for early surgical intervention. Con: computerized tomographic aspiration of infected pancreatic necrosis: the opinion against its routine use. Neutrophil metabolic activity but not neutrophil sequestration re ects the development of pancreatitis-associated lung injury. French Consensus Conference on Acute Pancreatitis: Conclusions and Recommendations. Pancreatic Disease Group, Chinese Society of Gastroenterology, Chinese Medical Association. Aggressive endoscopic therapy for pancreatic necrosis and pancreatic abscess: a new safe and e ective treatment algorithm (videos). Infected pancreatic necrosis: translumbar approach and management with retroperitoneoscopy. Trends in minimally invasive intervention for necrotizing pancreatitis: a survey of Australian and New Zealand surgeons. Infected necrosis in severe pancreatitis-combined nonsurgical multi-drainage with directed transabdominal high-volume lavage in critically ill patients. Systematic review of percutaneous catheter drainage as primary treatment for necrotizing pancreatitis. De nitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Early physiological response to intensive care as a clinically relevant approach to predicting the outcome in severe acute pancreatitis. Early prediction of organ failure by combined markers in patients with acute pancreatitis. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. Bene ts and risks of tight glucose control in critically ill adults: a meta-analysis. A ected individuals typically su er a pattern of persistent or recurrent attacks of pain along with progressive pancreatic exocrine insu ciency. Symptoms may also result from extension of the disease process to adjacent organs and vascular structures. Decision making in the management of chronic pancreatitis must be individualized to the speci c anatomic and pathological circumstances, taking into account the extent of local expertise in various diagnostic and therapeutic modalities as well as the fact that there is a relative paucity of high-quality data on the clinical e ectiveness of surgical and medical interventions. Optimal management is facilitated by a multidisciplinary approach that includes surgical, endoscopic, and radiological expertise in addition to nutrition, endocrinology, pain management, and psychosocial support. In fact, pancreatitis represents a far more heterogeneous clinical entity than can be captured by these two simple descriptors. A number of international conferences have been held in order to develop uniform terminology to characterize the spectrum of morphology seen in acute and chronic pancreatitis. According to the Marseille-Rome classi cation of 1988, the term acute pancreatitis is used to refer to single or repeated episodes of abdominal pain associated with a range of potentially reversible pancreatic lesions including pancreatic edema, necrosis, and hemorrhage, as well as peripancreatic uid collections, necrosis, and pseudocysts. Chronic pancreatitis is used to refer to recurrent or persistent abdominal pain that is associated with irreversible and ongoing in ammatory destruction of exocrine parenchyma and, eventually, islets. In practice, however, the distinction between acute and chronic pancreatitis is rarely made based on tissue sampling, and there is no consensus on the de nition of irreversible morphological change. Chronic obstructive pancreatitis is characterized by exocrine atrophy and is associated with duct stenosis caused by tumors, pseudocyst, or scarring from prior acute pancreatitis. Chronic calcifying pancreatitis is characterized by intraductal calci cations and protein plugs, and is often associated with atrophy, stenotic ducts, and areas of acute in ammation or pseudocyst. Chronic in ammatory pancreatitis consists of dense in ltration of mononuclear in ammatory cells. Retention cysts and pseudocysts, seen in both calcifying and obstructive forms, may also become infected. Excessive alcohol ingestion has been associated with chronic pancreatitis ever since the term was introduced by Comfort in 1946. Alcohol ingestion in and of itself does not lead to pancreatitis in experimental animals. Chronic pancreatitis in humans occurs in the absence of signi cant alcohol usage, and, in fact, it is only a small percentage (fewer than 5%) of alcoholics that develop pancreatic disease. However, repeated episodes of acute pancreatitis do not invariably lead to chronic pancreatitis, and chronic pancreatitis may present without prior acute attacks. As with alcohol, most individuals exposed to the other toxic substances associated with pancreatitis do not develop the chronic form of the disease. For these reasons, the concept of identifying risk modi ers rather than etiologies or causes of chronic pancreatitis may be more appropriate in classifying the disease particularly when making decisions regarding patient management. Instead, there is a diversity of etiologic risk factors that contributes to a spectrum of pathological and functional derangements, clinical features, and natural history. A relationship between dose and duration of alcohol use has been repeatedly documented, and there appears to be a threshold level for the risk of pancreatitis at approximately 50 gm (four drinks) per day. Chronic pancreatitis in the setting of alcohol use is associated with pancreatic calci cation and ductal stone formation, but none of the proposed mechanisms is convincingly supported experimentally, and the hypotheses are not mutually exclusive. Included among these is tobacco, which has been shown to confer increased risk of chronic pancreatitis independent of alcohol use.