Buy cheap prednisolone 5 mg
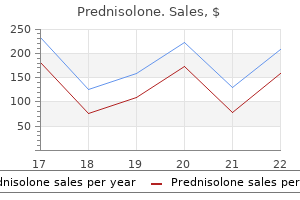
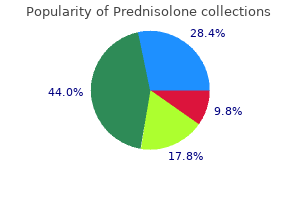
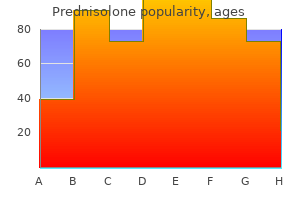
Low Blood Pressure Medications If your blood pressure is too low allergy treatment options mayo clinic purchase prednisolone, your doctor may prescribe medicine to raise it. The medicine most commonly prescribed for low blood pressure is fludrocortisone (Florinef). Notes About Fludrocortisone Fludrocortisone raises blood pressure by helping you to retain salt in your body and to discard potassium in your urine. Possible Side Effects Swelling in the hands or feet, rapid weight gain, water retention, headache. Spironolactone (Aldactone) may have been one of your diuretics before transplantation-this medication should be used very cautiously after transplantation. Notes About Diuretics Take the diuretic early in the day so you will not have to get up several times a night to go to the bathroom. Potassium supplements may be prescribed for a short time to replenish the supply in your blood. Possible Side Effects Low blood pressure, dizziness, lightheadedness, dehydration, more frequent urination, low potassium. Cholesterol-Lowering Medications Lowering your cholesterol may help prevent heart disease. The most commonly used cholesterol-lowering medicines are atorvastatin (Lipitor), simvastatin (Zocor), rosuvastatin (Crestor), pravastatin (Pravachol), and lovastatin (Mevacor). The primary immunosuppressive agents, cyclosporine and sirolimus, are the culprits causing high cholesterol and triglyceride levels in many patients who take them. Notes About Cholesterol-Lowering Medications Cholesterol-lowering medicines usually are taken at night. Possible Side Effects Upset stomach, heartburn, change in the way foods taste, diarrhea, skin rash, headache, constipation, blurred vision, muscle damage. Drug Interactions Some medicines can interfere with the way cyclosporine, sirolimus, and tacrolimus are processed in your body and can lead to very high or very low blood levels of these drugs. Be sure to discuss possible drug interactions with any physician who prescribes a new medicine for you. The antirejection medications that you are taking to prevent and treat rejection tell your immune system to accept your new organ. In doing so, they may also tell your immune system to accept other foreign invaders that it ordinarily would fight. As a consequence, taking antirejection medications can place you at greater risk for developing an infection. The most common infections result from viruses that have been lying dormant in your system or in the donated organ. To prevent infection, you will take antibacterial, antivirus, and antifungal medications for 3 to 6 months after your surgery. If an infection is suspected, your caregivers may take sputum (the substance coughed up from your lungs), blood, and urine samples as well as samples from your catheter, wound, and drain sites. Signs that you may notice include fever, tiredness or fatigue, diarrhea or vomiting, redness or drainage around your incision or tube site, or a cough and sore throat. If an infection develops, it is treated with medication specific for the type of infection. The infectious disease specialist works with the transplant team to manage and treat infections. If an infection develops after you have been discharged from the hospital, it may be treated with antibiotics on an outpatient basis. However, some people need to be readmitted to the hospital for treatment with intravenous medications. The targets of the immune response are different from the targets in acute rejection. This damage occurs very slowly and Chronic rejection Occurs at least 3 months after transplant. Chronic rejection has features on tissue biopsy which are distinct from acute rejection, drug toxicity and other diseases. Thanks to earlier recognition of acute and chronic rejection and the introduction of more powerful immunosuppressive agents (for example, tacrolimus and sirolimus), many of these cases can be successfully reversed. This longer survival comes at a price, however: far more long-term complications than were seen in the past. More attention must therefore be paid to the long-term effects of the immunosuppressive drugs and their cumulative effects. Over the course of many years this combination results in heart attack and stroke. When expected survival after transplantation was short, these long-term issues were of minimal concern. Today, with longer survival being commonplace, heart disease is one of the major causes of death in transplant recipients. The incidence of hypertension is attributed to the primary immunosuppressive agents. Standard antihypertensive medications are effective in treating this complication. Because many patients suffer from malnutrition before transplantation, these individuals are counseled to improve their nutrition afterward to help the healing process. Unfortunately, patients may become accustomed to this increased calorie intake and have a hard time cutting back their food consumption once recovery from surgery has been achieved. The subsequent obesity can decrease mobility and increase the risk of coronary artery disease. Once again, the culprit is often the immunosuppressive agents, particularly tacrolimus and prednisone. The incidence of obesity correlates with diabetes incidence and both are cardiac risk factors. Transplant-associated lymphoma is a feared complication of the immunosuppressive drugs. Chronic renal failure is a recognized complication of all organ transplantation due to the need for immunosuppression. Both tacrolimus and cyclosporine can cause the kidneys to function less than optimally. Additionally, in patients with cirrhosis, heart disease, or renal disease before transplantation, the side effects of diuretic use, hypertension, and diabetes can all contribute to chronic renal failure in recipients of a new organ. Renal failure after the transplantation complicates medical management, leading to increased morbidity and mortality. The incidence of chronic renal disease among recipients of liver transplants is approximately 8% after 1 year, 14% after 3 years, and 18% after 5 years. For patients who have received a heart transplant, the incidence of chronic renal disease is 2% after 1 year, 7% after 3 years, and 11% after 5 years. This does not mean that all these patients need dialysis but rather that their kidneys are not fully functional. Some patients do, indeed, progress to dialysis; kidney transplantation may be indicated in these individuals. A number of factors may predict the risk of developing renal failure, including age (older patients have a higher risk), gender (males have a higher risk than females), pretransplantation kidney function, and presence or absence of pretransplantation hypertension, diabetes, or hepatitis C infection. Overall, non-White, non-African American patients have the lowest risk of chronic renal failure. One technique is to reduce the dose of the primary immunosuppressive agent (that is, tacrolimus or cyclosporine). For those patients with a high risk or history of rejection, mycophenolate (CellCept, Myfortic) can be added to the drug regimen. A recent addition to the immunosuppression armamentarium, sirolimus (Rapamycin, Rapamune), can also reduce the risk. Sirolimus is not toxic to the kidneys and may be used for primary immunosuppression. This drug cannot be used immediately after organ transplantation because it slows wound healing; instead, it is typically prescribed later if concerns about renal dysfunction arise. Numerous resources are available to patients in need of organ transplantation and their families. You can obtain a wealth of information from your primary care physician, specialist, or local transplant center. Here are some tips to help you evaluate a website: Check the "about us" section of the site. Information from drug companies may be reliable, but remember-these companies are in the business of selling products.
Buy prednisolone 40mg with amex
Apixaban is cleared through both the fecal and renal route with the latter accounting for about 25% of drug clearance allergy forecast granbury tx buy prednisolone canada. There was no clinically relevant or statistically significant difference in the frequency of major bleeding in apixaban arms compared with the standard therapy group. Rivaroxaban Rivaroxaban is another highly selective factor Xa inhibitor that has an oral bioavailability of 80% and a half-life of approximately 9 hours. In all three studies, the frequency of the primary efficacy endpoint of deep vein thrombosis as detected on mandatory venography, nonfatal symptomatic venous thromboembolism, and all-cause mortality was less frequent in those treated with rivaroxaban than in those randomized to enoxaparin. There was no significant difference in bleeding complications between the two study drugs. Otamixaban Otamixaban is a noncompetitive inhibitor of factor Xa that is administered intravenously and has a half-life of 2 to 3 hours. Rivaroxaban has also been evaluated for treatment of proximal deep vein thrombosis in two dose-ranging studies. In studies of stroke prevention in patients with atrial fibrillation at high risk of stroke, a rivaroxaban dose of 20 mg once daily is being used. Rivaroxaban has been shown to be effective in the prevention of arterial thrombosis occlusion in the rat carotid artery injury model. Randomization to the three lower doses of the experimental agent was stopped early due to lack of efficacy, while the three higher doses had efficacy similar to that of enoxaparin. Additional studies are needed to determine the efficacy, safety, and optimal dose of this agent. In a dose-escalation study of 174 patients undergoing elective hip arthroplasty, no major bleeds were reported and there was no dose-response trend for clinically relevant nonmajor bleeding. A safety and tolerability study in patients with atrial fibrillation has been completed. Idraparinux 245 A hypermethylated derivative of fondaparinux, idraparinux binds antithrombin with such affinity that its plasma half-life of 80 hours is similar to that of antithrombin. Although the frequency of recurrent venous thromboembolism was similar in the idraparinux and conventionally treated groups in the deep vein thrombosis trial, in the pulmonary embolism patients, idraparinux was less effective than conventional therapy. This difference in efficacy was due to an excess of early fatal and nonfatal recurrences of pulmonary embolism and was associated with an increase in total mortality. In both studies, bleeding rates in the idraparinux-treated patients were similar to or lower than those in the conventional-therapy groups. The efficacy of long-term idraparinux was evaluated in an extension study in which patients who had completed 6 months of initial treatment of deep vein thrombosis or pulmonary embolism with either idraparinux or a vitamin K antagonist were randomized to an additional 6 months of treatment with either once-weekly subcutaneous idraparinux or placebo. Thus, the net clinical benefit of extended treatment with idraparinux appears marginal, at best. After 4576 patients were enrolled, the trial was stopped prematurely because of excess bleeding in those randomized to idraparinux. Elderly patients and those with renal insufficiency appeared to have the highest risk of bleeding with idraparinux suggesting that a reduced dose is needed in such patients. Like idraparinux, idrabiotaparinux is given subcutaneously on a once-weekly basis. The only difference is that the anticoagulant activity of idrabiotaparinux can be rapidly neutralized by intravenous administration of avidin, a large tetrameric protein derived from egg white, that binds to idrabiotaparinux to form a 1: 1 stoichiometric complex that is cleared via the kidneys. Carboxylation of vitamin K-dependent cofactors is catalyzed by a carboxylase that requires the reduced form of vitamin K. During this reaction, reduced vitamin K is oxidized to vitamin K epoxide, which is recycled back to vitamin K by vitamin K epoxide reductase. The vitamin K antagonists inhibit vitamin K epoxide reductase and, to a lesser extent, vitamin K reductase. With depletion of reduced vitamin K, carboxylation of the vitamin K-dependent proteins is inhibited. Indications Although oral anticoagulants have been used in patients with ischemic heart disease for close to half a century, their role in this patient population remains controversial. Both cofactors are inactivated by activated protein C, a naturally occurring anticoagulant that is generated when thrombin binds to thrombomodulin, producing a complex that activates protein C. Strategies aimed at enhancing the protein C anticoagulant pathway include administration of protein C or activated protein C concentrates or soluble thrombomodulin. Drotrecogin Alpha (Activated) Both plasma-derived and recombinant forms of protein C and activated protein C are available. Since approval, two additional clinical trials, one in adults with sepsis and a low risk of death264 and the other in children with sepsis,265 were stopped prematurely due to lack of efficacy and the potential to cause harm because of bleeding. Based on these studies, drotrecogin alpha (activated) appears to have a limited role in patients with sepsis. By blocking vitamin K epoxide reductase, warfarin inhibits the conversion of oxidized vitamin K in to its reduced form. Oral anticoagulation is an alternative for patients at increased risk of thromboembolism. However, the adverse effects associated with warfarin therapy are greater than those of aspirin and monitoring of warfarin treatment is laborious. In individuals who cannot tolerate aspirin, however, warfarin may be a useful alternative, and combination therapy can be considered in patients at high risk for ischemic events. However, life-threatening bleeding was more frequent with combination therapy than with antiplatelet therapy (4. Based on these results, adding warfarin to antiplatelet therapy does not appear to improve efficacy and is associated with an increase in life-threatening bleeding. This inter-individual variation in warfarin dosing may reflect dif- 22 ferences in age, weight, liver function, diet, alcohol intake, concomitant medications, and comorbid illnesses. The decision to use warfarin alone or in combination with aspirin should be based on a careful review of the risks of future vascular and bleeding events, patient compliance with therapy, and the availability of high quality warfarin monitoring. Although aspirin is likely to remain first-line therapy for most patients with coronary artery disease, warfarin therapy may be useful in higher risk patients and those who suffer recurrent events despite aspirin treatment. Anticoagulants Side Effects Bleeding is the most frequent complication of warfarin therapy. The risk of bleeding is influenced by the intensity of anticoagulation; the concomitant use of aspirin, nonsteroidal anti-inflammatory agents, or other drugs that influence hemostasis; a history of bleeding; advanced age; a history of stroke; or the presence of serious comorbid conditions. To circumvent this complication, patients with known protein C or protein S deficiency should be started on maintenance, rather than loading, doses of warfarin after therapeutic doses of heparin have been given. Contraindications and Drug Interactions Patients who have contraindications to anticoagulation therapy should not be given warfarin (see Box 22-1). Because warfarin is teratogenic, its use should be avoided, if possible, in pregnancy. Despite 248 promising data, the role of the other agents in this patient population remains to be clearly delineated. The greatest unmet need in anticoagulation therapy is replacement of warfarin with an orally active agent that can be given in fixed doses without routine coagulation monitoring. Consequently, most of the current attention is focused on new oral anticoagulants. Those in the most advanced stages of development are the oral direct thrombin and factor Xa inhibitors. Dabigatran etexilate and rivaroxaban have been licensed for thromboprophylaxis in patients undergoing hip or knee replacement 22 surgery in Europe and Canada. The challenge for the future will be to determine which of the numerous agents currently under development will provide the greatest efficacy with the greatest degree of safety. Fuster V: Elucidation of the role of plaque instability and rupture in acute coronary events. Yamamo to M, Nakagaki T, Kisiel W: Tissue factor-dependent autoactivation of human blood coagulation factor. Danielsson A, Raub E, Lindahl U, et al: Role of ternary complexes in which heparin binds both antithrombin and proteinase, in the acceleration of the reactions between antithrombin and thrombin or factor Xa. The International Study Group: In-hospital mortality and clinical course of 20,891 patients with suspected acute myocardial infarction randomised between alteplase and streptokinase with or without heparin. Collins R, MacMahon S, Flather M, et al: Clinical effects of anticoagulant therapy in suspected acute myocardial infarction: Systematic overview of randomised trials. Holdright D, Patel D, Cunningham D, et al: Comparison of the effect of heparin and aspirin vs. Theroux P, Waters D, Lam J, et al: Reactivation of unstable angina after the discontinuation of heparin.
Purchase prednisolone uk
H P Postnatal Because of increased risk of postpartum hemorrhage allergy symptoms bags under eyes generic 5 mg prednisolone overnight delivery, ade quate preparations should be made before the delivery. Women who have had placental abruption are more likely to have placental abruption in subsequent pregnan cies (7fold to 17fold risk increase). As previously mentioned, the main role of imaging is exclusion of placenta previa as the cause of vaginal bleeding. Resolution on subsequent examina tions may help to establish the diagnosis of abruption. A more recent attempt to assess the effectiveness and safety of any inter vention after a diagnosis of abruption, based on random ized trials, found no studies that met the inclusion criteria. Mater nal compromise requires stabilization, including volume replacement and blood products as needed, and expedited delivery. In the absence of maternal or fetal compromise, gesta tional age guides the decision. Placental abruption in the United States, 1979 through 2001: temporal trends and potential determi nants. Threatened abortion: a risk factor for poor pregnancy outcome, a population based screening study. Placental abruption and placental hemorrhage: correlation of sonographic findings with fetal outcome. The effect on the likelihood of further pregnancy of placental abruption and the rate of its recurrence. Incidence of placenta accreta has increased dramatically in recent years, in correlation with the increase in the rate of cesarean deliveries. This condition is associated with significant maternal morbidity and is one of the two leading reasons for cesarean hysterectomy. Placenta percreta specifically indicates invasion beyond the uterine serosa, which may involve adjacent organs such as bladder or vessels. One study that retrospectively evaluated first-trimester images of placenta accreta observed that the gestational sacs were located in the lower uterine segment and were abnormally close to the uterine scar. In addition, the study showed thinning of the myometrium in the area of attachment. Although some clinicians use a clinical definition of adherent placenta, the most accurate diagnosis relies on pathologic examination of the placenta. Etiology and Pathophysiology Defects of the decidua basalis are considered the basic predisposing factor that may result in abnormally invasive placenta implantation. This defect is considered to be secondary to failed reconstitution of the endometrium, after repair of a cesarean incision or other uterine surgeries. Histologic confirmation of placenta accreta usually involves demonstration of trophoblasts in direct contact with the myometrium or invading the myometrium. Bladder Placenta Manifestations of Disease Clinical Presentation Placenta accreta may be suspected prenatally in asymptomatic patients with risk factors including history of cesarean delivery and current placenta previa. There have been a few reports of spontaneous uterine rupture and subsequent intraabdominal hemorrhage in the second half of pregnancy9 and cases of placenta accreta manifesting with excessive hemorrhage at the time of dilatation and evacuation in the second trimester10; however, many cases are still not diagnosed until delivery-they are not apparent until difficulties are encountered in separating the placenta in the third stage of labor (which may require manual removal), or heavy bleeding occurs from the implantation site. This elevated rate suggests an abnormal placental-uterine interface, with leakage in to the maternal circulation. However, pregnancies complicated by placenta previa, even with a false-positive diagnosis of accreta, are still at risk for significant postpartum hemorrhage. When accreta is suspected, referral to a high-volume center with experience in cesarean hysterectomy is recommended because studies have shown decreased morbidity at these centers if cesarean hysterectomy is required. Interventional radiology, urology, and vascular surgery specialists may also be required. If accreta is suspected, the surgeon clamps the cord, leaves the placenta in situ, and completes the hysterectomy after closing the uterine incision with a whipstitch. The frequency and complication rates of hysterectomy accompanying cesarean delivery. Risk factors and morbidity in patients with placenta previa accreta compared to placenta previa non accreta. Placenta accreta encountered during dilation and evacuation in the second trimester. Characterization of placenta accreta using transvaginal sonography and color Doppler imaging. Placenta accreta: prospective sonographic diagnosis in patients with placenta previa and prior cesarean section. Usefulness of gray-scale ultrasound and complementary color Doppler ultrasound in the prenatal diagnosis of placenta previa accreta. Use of magnetic resonance imaging and ultrasound in the antenatal diagnosis of placenta accreta. Accuracy of ultrasonography and magnetic resonance imaging in the diagnosis of placenta accreta. Antenatal diagnosis of placenta previa accreta in patients with previous cesarean scar. Regionalization of care for obstetric hemorrhage and its effect on maternal mortality. Postnatal Because placenta accreta may cause massive intrapartum hemorrhage,6 it is one of the leading causes of cesarean hysterectomy. However, hemorrhage, disseminated intravascular coagulation, and infections may complicate this solution. In the absence of conclusive supporting data, such steps to preserve the uterus should be considered only when a patient has a strong desire to preserve fertility. In these cases, both the physician and the patient need to understand the risk of accreta recurring in subsequent pregnancies279 and the potential complications postpartum in the current pregnancy. Neonatal outcome in cases of placenta accreta has been reported to be similar to outcome in cases of previa without accreta. Massive obstetric hemorrhage due to placenta previa/accrete with prior cesarean section. Case-control comparison of cesarean hysterectomy with and without prophylactic placement of intravascular balloon catheters for placenta accreta. Fertility and obstetric outcome after conservative management of placenta accreta. Fetal parts become entangled by amniotic bands, leading to constriction, deformation, and malformation defects. Two major theories have been suggested: the intrinsic theory, proposed by Streeter7 in 1930, and the extrinsic theory, proposed by Torpin8 in 1965. The intrinsic theory argues that disruption during embryogenesis at the time of germ disk and amniotic cavity formation initiates a series of events leading to multiple anomalies. Streeter proposed that amniotic bands are the result, not the cause, of the pathologic process. Various causative factors have been proposed, including teratogens and a vascular insult during early development. Torpin studied the placenta and fetal membranes in affected cases and surmised that primary rupture of the amnion early in gestation2,8 caused the disorder, allowing the fetus to pass from the amniotic cavity to the extraembryonic coelom through the defect. The subsequent contact of the fetus with loose "sticky" mesoderm on the chorionic surface of the amnion would lead to entanglement of fetal parts, causing mechanical disruption, vascular disruption, or both. It has been observed following maternal abdominal trauma; after amniocentesis; and in fetuses with hereditary collagen defects, such as Ehlers-Danlos syndrome and osteogenesis imperfecta. These authors concluded that the malformations observed were caused by three distinct lesions: (1) constrictive tissue bands, (2) amniotic adhesions, and (3) complex anomaly patterns (limbody wall complex). No internal malformations or complex anomalies were noted in this group with constrictive bands. In contrast, cases involving broad amniotic adhesions resulted in more disfiguring malformations. In some instances, the amniotic band may be seen entangling the fetus, restricting movement within the amniotic cavity. Amniotic bands most commonly affect the fetal extremities, with a greater affinity for the distal segments. Defects can range in severity from mild constriction to complete intrauterine limb amputation and fetal demise. For example, oligohydramnios can lead to scoliosis, talipes equinovarus, and joint contractures by limiting fetal movement and exerting direct pressure on developing structures. A,Two-dimensional gray-scale image of the left fetal forearm showing amputation distal to the wrist. Color Doppler interrogation should show blood flow to the region in question if a vascular malformation is present.
Generic prednisolone 5mg on-line
However allergy medicine 035 discount prednisolone online american express, unlike Raman spectroscopy, which uses high-energy laser light in the visible light spectrum, near-infrared diffuse reflectance spectroscopy is the process of understanding how infrared light (750 to 2500 nm) interacts with various molecules. Near-infrared light occurs just beyond the location of red light in the visible spectrum. The amount of light absorbed is proportional to the concentration of that particular molecule, revealing both qualitative and quantitative information about the pathologic process under investigation. Histologic correlation with reflectance patterns of different tissues can potentially detect and distinguish the lipid-rich atheromatous core and become a useful diagnostic tool for the detection of vulnerable plaque. Spectroscopic systems using infrared light have demonstrated the ability to identify cholesterol, high-density lipoprotein, and low-density lipoprotein in arterial wall samples obtained at autopsy. Chemical analyses have shown that correlation of the atheromatous core content using high-pressure liquid chromatography is high. Subsequently, the lipid content of ex vivo specimens of human carotid plaques was successfully measured using near-infrared diffuse reflectance spectroscopy. These same investigators found similar sensitivities and specificities for the identification of lipid-rich plaques in a study of 167 human coronary artery specimens. In a study using this device, large, lipid-rich plaques were identified (sensitivity, 88%; specificity, 79%) through up to 3 mm of blood. Although coronary artery motion may affect the acquisition of data by near-infrared diffuse reflectance spectroscopy, ultrafast systems have been developed that are capable of obtaining spectra data within 6 milliseconds by scanning only a preselected number of wavelengths appropriate for atherosclerotic plaque assessment. Safety was demonstrated, but substantial motion artifacts failed to prove its feasibility. Further technical advancements will address these issues and should improve on the quality of data and image acquisition. Although they share the common goal of identifying the vulnerable plaque, they do so by targeting various components of the atherosclerotic plaque. These imaging modalities should be viewed as complementary; it is likely that a future definition of the vulnerable plaque may be based on a combination of criteria obtained from various imaging modalities. Future identification of a vulnerable plaque may lead to better prognostic evaluations or treatment strategies in patients with coronary artery disease. Yusuf S, Reddy S, Ounpuu S, Anand S: Global burden of cardiovascular diseases: Part I: General considerations, the epidemiologic transition, risk factors, and impact of urbanization. Naghavi M, Libby P, Falk E, et al: From vulnerable plaque to vulnerable patient: Q call for new definitions and risk assessment strategies: Part I. Rioufol G, Finet G, Ginon I, et al: Multiple atherosclerotic plaque rupture in acute coronary syndrome: A three-vessel intravascular ultrasound study. Manfrini O, Mont E, Leone O, et al: Sources of error and interpretation of plaque morphology by optical coherence tomography. Nasu K, Tsuchikane E, Katoh O, et al: Accuracy of in vivo coronary plaque morphology assessment: A validation study of in vivo virtual histology compared with in vitro histopathology. Casscells W, Hathorn B, David M, et al: Thermal detection of cellular infiltrates in living atherosclerotic plaques: Possible implications for plaque rupture and thrombosis. Stefanadis C, Diamantopoulos L, Vlachopoulos C, et al: Thermal heterogeneity within human atherosclerotic coronary arteries detected in vivo: A new method of detection by application of a special thermography catheter. Stefanadis C, Diamantopoulos L, Dernellis J, et al: Heat production of atherosclerotic plaques and inflammation assessed by the acute phase proteins in acute coronary syndromes. Verheye S, Diamantopoulos L, Van Langenhove G, et al: In vivo temperature heterogeneity of atherosclerotic plaques is determined by plaque composition. Stefanadis C, Toutouzas K, Tsiamis E, et al: Thermography of human arterial system by means of new thermography catheters. Larose E, Yeghiazarians Y, Libby P, et al: Characterization of human atherosclerotic plaques by intravascular magnetic resonance imaging. Regar E, Hennen B, Grube E, et al: First-in-man application of a miniaturized selfcontained intracoronary magnetic resonance probe. Komachi Y, Sa to H, Tashiro H: Intravascular Raman spectroscopic catheter for molecular diagnosis of atherosclerotic coronary disease. Jaross W, Neumeister V, Lattke P, Schuh D: Determination of cholesterol in atherosclerotic plaques using near infrared diffuse reflection spectroscopy. Data from observational studies and clinical trials have documented the prognostic usefulness of individual factors for risk stratification. Demographic and historical features, as well as information collected during the initial evaluation, including physical examination findings and electrocardiographic changes, have been used in simple risk stratification schema. Whereas both of these risk scores incorporate features on presentation, dynamic risk stratification may also provide incremental information. An alternative approach has been to treat age as a categorical variable, with the clinician assigning increasing weight for each decade above a certain threshold. For example, half of diabetic patients have concomitant hypertension and one third have concomitant hyperlipidemia. Pathophysiologically, diabetes results in increased oxidative stress36 and the development of advanced glycation end products, which may be proatherogenic. Over the past 2 decades, the worldwide prevalence has increased significantly, with 30 million cases in 1985 and 177 million in 2000; it is estimated that more than 260 million individuals will have diabetes by 2030. Patients with documented biochemical evidence of myocyte necrosis have higher mortality rates than patients without elevations. Consensus panels recommended that a single cut point be adopted based on the 99th percentile in a cohort of healthy individuals and a coefficient of variation less than 10%. Although not specific for myocardial injury, myoglobin is a sensitive marker, especially in the first 4 to 8 hours after the onset of necrosis. The clinical circumstances (A, B, or C) were divided in to secondary angina caused by an extracardiac condition that intensified myocardial ischemia, primary angina presumably caused by plaque rupture, and postinfarction angina. The intensity of medical treatment (denoted with subscripts 1, 2, or 3) ranged from angina occurring in the setting of no treatment, during treatment for chronic angina, and despite maximal anti- 18 ischemic therapy. Prospective validation of the Braunwald classification system confirmed the usefulness of such an approach. Potential predictor variables were selected from baseline characteristics that could be readily identified at presentation and that had previously been reported to be important variables in predicting outcome (Table 18-1). The final model demonstrated excellent calibration of the model predictions to the observed event rates (Hosmer-Lemeshow statistic,87 3. Thus, the risk score is calculated by assigning 1 point for each variable that is present (Table 18-2). Of note, the application of the C-statistic in the setting of prognostication has been debated. However, the C-statistic may not be the ideal parameter to assess models or variables that aim to predict future risk or separate subjects in to distinct risk groups. Thus, it has been suggested that prognostic models should be evaluated based on their calibration and ability to reclassify individuals, in addition to their ability to alter the C-statistic. Second, this pattern was also seen for each individual component of the composite end point (P <. Moreover, such risk scores appear to predict not only which patients will have acute events, but also which patients are at risk for dying or suffering cardiac ischemic events after discharge. The incorporation of these new markers in to existing integrated risk scores may be a useful next step. Nonetheless, the cost and potential complications associated with each of these treatments suggest the need for identifying patients who would derive particular benefit from these therapies. In addition to their powerful prognostic role, troponin levels can also be used to guide therapy. In contrast, among patients with normal troponin levels, there was no demonstrable benefit. Patients with an elevated troponin level had a 39% relative risk reduction in the primary end point with the early invasive strategy versus the conservative strategy. It is pathobiologically plausible that inhibition of platelet aggregation would be particularly important in diabetics. Presentation, diagnosis, treatment, and 28-day case fatality of 3991 events in men and 1551 events in women. Wild S, Roglic G, Green A, et al: Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030.
Diseases
- Infantile dysphagia
- Epidermo Epidermod Epidermoi
- Hypopigmentation oculocerebral syndrome Cross type
- Lindstrom syndrome
- Rokitansky sequence
- Tachycardia
- Say Meyer syndrome
- Jejunal atresia
Purchase prednisolone amex
Fetal kidneys are considered echogenic if the reflectivity of the parenchyma is greater than that of the liver allergy medicine you can take with alcohol buy prednisolone 20mg without a prescription. Polyhydramnios is found in 50% to 60% of cases9,10 likely as a result of impaired fetal swallowing by the enlarged tongue. Macrosomia: Wrong dates; diabetes; and other overgrowth disorders7 such as Simpson-Golabi-Behmel syndrome (X-linked recessive condition), Perlman syndrome (rare autosomal recessive condition), Costello syndrome (unknown etiology, sporadic), and Sotos syndrome (autosomal dominant) need to be considered. Macroglossia21,31: the overall incidence of fetal macroglossia is estimated to be 1: 11,000 to 1: 25,000. Placentomegaly: Placentomegaly is also associated with fetal hydrops, maternal diabetes with fetal macrosomia, triploidy, and molar pregnancy. Omphalocele: Omphalocele is often associated with other anomalies and a 30% incidence of aneuploidy. It is also seen in other syndromes such as pentalogy of Cantrell, cloacal exstrophy, and Meckel-Gruber syndrome. Nephromegaly: Nephromegaly is also seen in polycystic kidneys and Meckel-Gruber syndrome. Echogenic kidneys can be seen with renal dysplasia and cytomegalovirus infection, but in these cases the kidneys are normal in size. Macroglossia may result in airway obstruction at birth, and consultation with a pediatric otolaryngologist is advisable. Delivery should occur in a tertiary center with the neonatal team present and a pediatric otolaryngologist readily available to help manage airway obstruction and intubation difficulties. Extreme cytomegaly of the adrenal fetal cortex, omphalocele, hyperplasia of the kidneys and pancreas, and Leydig cell hyperplasia-another syndrome Presented at the Annual Meeting of Western Society for Pediatric Research, Los Angeles, November 11, 1963. Macroglossia, omphalocele, adrenal cytomegaly, gigantism and hyperplastic visceromegaly. Complexe malformatif familial avec hernie ombilicale et macroglossie-un "syndrome nouveau" Wiedemann-Beckwith syndrome: presentation of clinical and cytogenetic data on 22 new cases and review of the literature. Other possible problems requiring evaluation and treatment include hyperinsulinism and hypoglycemia and other metabolic problems (polycythemia, nephrocalcinosis, hypothyroidism) and feeding difficulties. Surgical repair of omphalocele and imaging of intraabdominal organs to rule out organomegaly, malformations, or tumors may be required. Longterm follow-up requires a multidisciplinary approach including a craniofacial team, endocrinology, orthopedic surgery (if hemihyperplasia and limb asymmetry are present), medical genetics, and urology. Alpha-fetoprotein is measured in the first few years of life to screen for hepatoblastoma. Delivery in a tertiary care center is indicated so that the newborn may receive adequate care to prevent complications from macroglossia and hypoglycemia and undergo surgical repair of omphalocele if present. Beckwith-Wiedemann syndrome: historical, clinicopathological and etiopathogenetic perspectives. Development of the fetal tongue between 14 and 26 weeks of gestation: in utero ultrasonographic measurements. Antenatal manifestation of congenital pancreatoblastoma in a fetus with Beckwith-Wiedemann syndrome. BeckwithWiedemann syndrome presenting with an elevated triple screen in the second trimester of pregnancy. A growthrestricted fetus is at increased risk of perinatal morbidity and mortality, and the risks are carried in to adulthood with an increased risk of cardiovascular disease, hypertension, obesity, diabetes, and osteoporosis, regardless of the gestational age at delivery. There is a direct relationship between fetal growth and adverse outcomes with the greatest risk of perinatal mortality and morbidity at weights below the 3rd percentile. Higher rates are seen in developing countries because of the underlying disease burden and malnutrition. Genetic factors including gender significantly contribute to the variation seen in birth weights. Maternal birth weight and a history of a prior growth-restricted infant or poor pregnancy outcome increase the risk of subsequent pregnancies having growth restriction. Approximately 25% of multiple gestations are growth restricted, with the highest rates seen in monochorionic gestations. Growth restriction is observed in 20% to 25% of fetuses with congenital anomalies. Fetal mortality is increased because of the underlying etiology and associated preterm deliveries. Perinatal mortality rates are four to eight times higher for growthrestricted infants, and morbidity is present in 50% of surviving infants. Any disease that affects the vascular endothelium and the uteroplacental circulation has the potential to affect nutrient delivery. The uterine blood supply derives mainly from the uterine arteries, which give rise to the arcuate arteries that run circumferentially around the uterus. Controversy exists because many fetuses classified as growth restricted are constitutionally small and healthy and are not at risk for adverse outcomes, whereas others who may be above the 10th percentile but are not achieving their growth potential are at higher risk for complications. Physiologic modification of the spiral arteries is necessary to allow the 10-fold increase in uterine circulation necessary for fetal growth. This increase occurs in the second wave of trophoblastic invasion when the spiral arteries are invaded by cytotrophoblastic cells and converted in to uteroplacental arteries. Normal uteroplacental arteries have dilated and tortuous lumina, a noncontinuous endothelial lining, and complete absence of muscular and elastic tissue, which converts the placenta in to a low-resistance organ. Fewer spiral arteries, less branching, and occlusion of the lumina characterize the growth-restricted placenta, with additional wall thickening and fewer gas-exchanging terminal villi, which are poorly branched. The failure of normal development of maternal placental arteries leads to reduced oxygen and nutrient delivery in to the intervillous space, whereas reduction in the number of placental terminal capillaries leads to poor transfer of oxygen and nutrients to the fetus. Normally, abdominal circumference increases in the third trimester because of increasing adiposity and an increase in liver glycogen stores and size. Symmetric growth restriction, which accounts for 20% to 30% of growth-restricted fetuses, refers to a growth pattern in which all fetal organs and growth parameters are decreased proportionally secondary to impairment of early fetal cell growth. Etiologies include genetic or chromosomal causes, early infections, drug or alcohol exposure, and severe early placental insufficiency. Asymmetric growth restriction is characterized by a decrease in abdominal circumference relative to the head circumference. This pattern results from the fetus using nutritional stores in the liver and adapting blood flow to compensate for inadequate placental perfusion. The redistribution of blood flow to more vital organs (brain, heart, and adrenals) at the expense of less vital organs (intestines, muscle, kidneys, lungs) leads to oligohydramnios from decreased renal perfusion and urine output. The decreased tissue perfusion contributes to fetal acidemia and causes direct damage to the deprived tissues. Blood flow alterations as assessed by Doppler velocimetry and the presence of oligohydramnios precede changes in fetal heart rate reactivity and variability. Progressive compensation by the fetus leads to decreased diastolic flow and absent or reversed end-diastolic flow in the umbilical artery. Progressive hypoxemia and acidemia lead to cardiac dysfunction and myocardial ischemia. Tricuspid regurgitation and right-sided heart failure can be detected as venous backflow by sampling the inferior vena cava, ductus venosus, and umbilical vein. Venous Doppler changes occur in more than half of cases before an abnormal biophysical profile or nonstress test. Manifestations of Disease Clinical Presentation the most important tool in the diagnosis of fetal growth restriction is a thorough assessment of underlying risk factors. Uterine and umbilical artery Doppler have not been shown to reduce maternal or perinatal morbidity and mortality in a low-risk population. Genetic counseling and amniocentesis for the diagnosis of aneuploidy or infection can be offered to the patient, especially if there are associated fetal structural abnormalities. Accurate assessment of gestational age is crucial to the diagnosis of growth aberrations. In the second and third trimesters, gestational age estimations range up to 2 weeks and 3 weeks. Over any interval, the abdominal circumference is expected to increase by 1 cm/wk. Serial assessments of growth should be followed using the estimated fetal weight and abdominal circumference measurements, which are the most sensitive in the determination of aberrations. Other growth parameters such as transcerebellar diameter, foot length, and determinations of soft tissue density have been proposed but are not standard in the determination of growth restriction. Doppler Doppler velocimetry is a noninvasive technique frequently used to determine maternal and fetal hemodynamic status. The Doppler effect or Doppler shift occurs because the frequency of reflected energy varies in relation to the velocity of a moving object.
Prednisolone 20mg lowest price
Surprisingly allergy shots reactions swelling buy prednisolone 20mg without a prescription, despite the worldwide use of these agents, pharmacogenomic data are extremely limited. Nevertheless, the significant heritability of many factors implicated in coagulation and fibrinolysis suggests that genetic factors may contribute to the intersubject variability of the pharmacologic effects of fibrinolytics. Additional genetic studies are ongoing to investigate additional genes in the vitamin K cycle to see how they affect warfarin dosing. Furthermore, several warfarin resistance genes and variants have also been identified, but these are rare. With many groups working to develop an effective warfarin dosing algorithm, it is hoped that we may soon have an improved warfarin dosing regimen that reaches a stable maintenance dose of the drug using smaller and fewer dose changes. Inclusion of pharmacogenomic parameters in warfarin dosing also has the potential to reduce hospitalizations by identifying and creating a safer environment for patients at risk of bleeding events. Recent data from a pilot randomized trial support the potential benefits of genotype-based prescribing of warfarin. However, findings from these studies have been variable and some larger cohorts have provided more negative results. Beta Blockers Given the significant heterogeneity of the response to beta blockers, these agents have constituted an important focus of pharmacogenomic research in patients with hypertension and heart failure. Studies in patients with hypertension or heart failure support that this genetic polymorphism is a significant modulator of blood pressure reduction and improvements in left ventricular remodeling produced by beta blockers. Because of the unique sympatholytic effect of bucindolol and the absence of mortality benefit in the main study, these data cannot be extrapolated to other beta blockers. Limited data have suggested that those variations could also influence tolerability to these beta blockers. The lack of consistency between published studies may be attributable to several factors, including insufficient sample sizes. Given the complexity of the pharmacokinetics and pharmacodynamics of beta blockers, as well as the intricacies of the adrenergic system, future trials should adopt a more comprehensive approach that takes all these variables in to consideration. Each of the six currently available statin drugs is regarded as both safe and effective. Several genes have been identified and associated with the pharmacokinetics and efficacy of statins; however, most of the positive associations were described in small studies and failed to be reproduced in larger cohorts. One of the most striking adverse effects of the use of statins is musculoskeletal complaints. This muscle toxicity, commonly manifested clinically as isolated muscle pain, often causes patients to alter their course of therapy. The most extreme manifestation of statin-induced muscle toxicity is rhabdomyolysis. For this reason, membrane transporters have long been hypothesized to contribute to a variety of statin-related clinical outcomes. Moreover, there are currently many international research efforts focused on identifying additional genes that contribute to statin-induced myotoxicity. With all this new information being uncovered about statin 91 pharmacogenomics, it is hoped that in the future patients will benefit from improved screening to achieve better safety and efficacy of lipid-lowering therapy. Nonetheless, in recent years, many have highlighted the inconsistencies in results of genomic and pharmacogenomic studies that may transform the hope of personalized medicine in to an unmet "hype. Third, nongenetic factors such as diet should be assessed and their impact considered. Ultimately, these clinical investigations will be responsible for the fulfillment of the promise of individualized medicine to get the right drug at the right dose to the right patient at the right time. Peetz D, Victor A, Adams P, et al: Genetic and environmental influences on the fibrinolytic system: A twin study. International Human Genome Sequencing Consortium: Finishing the euchromatic sequence of the human genome. Wellcome Trust Case Control Consortium: Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls. Kathiresan S, Melander O, Guiducci C, et al: Six new loci associated with blood lowdensity lipoprotein cholesterol, high-density lipoprotein cholesterol or triglycerides in humans. McPherson R, Pertsemlidis A, Kavaslar N, et al: A common allele on chromosome 9 associated with coronary heart disease. Pare G, Serre D, Brisson D, et al: Genetic analysis of 103 candidate genes for coronary artery disease and associated phenotypes in a founder population reveals a new association between endothelin-1 and high-density lipoprotein cholesterol. Wang H, Yu M, Ochani M, et al: Nicotinic acetylcholine receptor alpha7 subunit is an essential regulator of inflammation. Sibbing D, Stegherr J, Latz W, et al: Cytochrome P450 2C19 loss-of-function polymorphism and stent thrombosis following percutaneous coronary intervention. Schunkert H, Gotz A, Braund P, et al: Repeated replication and a prospective metaanalysis of the association between chromosome 9p21. Wuttke H, Rau T, Heide R, et al: Increased frequency of cytochrome P450 2D6 poor metabolizers among patients with metoprolol-associated adverse effects. Rigat B, Hubert C, Alhenc-Gelas F, et al: An insertion/deletion polymorphism in the angiotensin I-converting enzyme gene accounting for half the variance of serum enzyme levels. Zintzaras E, Raman G, Kitsios G, Lau J: Angiotensin-converting enzyme insertion/ deletion gene polymorphic variant as a marker of coronary artery disease: A metaanalysis. In it, he described the classic symptoms of angina1: this is a disorder of the breast, marked with strong and peculiar symptoms, considerable for the kind of danger belonging to it. The seat of it, and sense of stran gling and anxiety with which it is attended, may make it not improp erly called angina pectoris. When a fit of this sort comes on by walking, its duration is very short, as it goes off almost immediately upon stopping. The clinical syndrome accompanying acute myocardial infarction was described by two Russian physicians, Obrastzov and Strazhesko in 1910,2 and then by William Herrick in 1912. Sampson and Eliaser wrote that "The character of the premonitory attack of pre cordial pain observed in these patients. The effect of nitroglycerin on the premonitory attack was definitely tran sient, with failure of complete relief even on repeated doses. In patients with unstable angina, the attacks, in addition to being more frequent, are also often of longer duration and may occur at rest without an apparent precipitating event. An important distinction was made7 between the fact that subsequent formation of a plateletfibrin thrombus. Coronary vasospasm and vasoconstriction, progression of atherosclero sis, and increased myocardial oxygen demand in the presence of a fixed, limited supply may also play pathogenetic roles. These complicated processes appear to be of para mount importance in the pathogenesis of some of the acute coronary syndromes including unstable angina, myocardial infarction, and sudden coro nary death. This classification has been shown to correlate both with the severity of coronary disease as assessed by arteriography as well as with early mortality (Table 111). From this classification, three principal presen tations of unstable angina are recognized (Table 112). However, women predominate among the rapidly expanding older population with unstable angina. In myocardial infarc tion, this pain characteristically begins abruptly, is steady, and lasts for more than 30 minutes. The discomfort ranges from mild to very severe, depending on patient perception and the mass of myocardium that is ischemic or necrotic. Chest pain that is fleeting, stabbing in nature, positional, pleuritic, reproduced by palpation, or that persists for days is rarely caused by an acute coronary syndrome. The pain in an acute coronary syndrome is most com monly located in the center or left of the chest, with radiation to the left shoulder and arm, neck, and jaw. Rarely, ischemic chest pain may be perceived in the right side of the chest or interscapular region. Severe pain that radiates through the chest in to the back is more suggestive of aortic dissection than acute coronary syndrome. Pain that the patient can localize by pointing with one finger is rarely ischemic in origin; rather, ischemic pain usually occupies a substan tially larger area. Levine), in which a patient places a clenched fist over the chest while describing the pain, is classically seen in acute myocardial infarction. Gastrointestinal symptoms are most commonly seen with ischemia of the inferior rather than the anterior wall. Other symptoms include apprehension or anxiety, syncope, acute heart failure, generalized weakness, and acute mental status changes. When these symptoms, most frequently dyspnea, occur without chest pain they may be referred to as "angina equivalents.
Prednisolone 40mg overnight delivery
Prenatal diagnosis of trisomy 18 provides information for discussions of pregnancy options allergy forecast bastrop tx buy cheap prednisolone line, such as continuation versus termination, surveillance, and mode of delivery. These findings illustrate the importance of completing the anatomic survey as recommended by the American Institute of Ultrasound in Medicine, American Congress of Obstetrics and Gynecology, and International Society of Ultrasound in Obstetrics and Gynecology. Abnormalities can be classified in to major structural anomalies and minor anomalies including soft markers. Different studies report varying incidence of these anomalies in fetuses with trisomy 18. Other heart abnormalities include hypoplastic left heart and coarctation of the aorta. When trisomy 18 is suspected, the hands and feet need to be specifically examined. Genitourinary abnormalities such as pyelectasis; echogenic, absent, or malpositioned kidneys; and hypoplastic genitalia have also been noted. They described a choroid plexus cyst as a large anechoic cyst with a thin remnant of surrounding echogenic choroid, which was noted in 14 of 27 fetuses with trisomy 18. However, if one additional abnormality was found, the maternal ageelated risk increased 20 times, and if two or more abnormalities were found, the risk increased almost 1000 times. Most Common Minor Abnormalities Found in Fetuses with Trisomy 18 Choroidplexuscyst Nuchalfoldthickness>6mm Pyelectasis Echogenicbowel Shortfemurandhumerus(<10thpercentile) Echogenicintracardiacfocus Intrauterinegrowthrestriction Polyhydramnios Singleumbilicalartery 27(38. Trisomies 13 and 18 may share phenotypic features, including ventriculomegaly, enlarged cistern magna, cleft lip/palate, cystic hygroma, and cardiac abnormalities. Various kidney, heart, and limb abnormalities similar to trisomy 18 may be noted with trisomy 13. Features such as holoprosencephaly, polydactyly, and facial clefts are more commonly seen in trisomy 13. The only definitive way to confirm the diagnosis prenatally is chromosome analysis. This confirmation is important because the outcome for trisomy 21 is better, and the prenatal management would be different. Pena-Shokeir I syndrome is an autosomal recessive syndrome, and its features include arthrogryposis, intrauterine growth restriction, low-set malformed ears, small mouth, micrognathia, rocker-bottom feet, pulmonary hypoplasia, and cryptorchidism. Features that distinguish this syndrome from trisomy 18 include scalp edema, lung hypoplasia, and family history. Additional features commonly found in trisomy 18 but not PenaShokeir I are cardiac arrhythmias, omphalocele, and prominent occiput. These investigators suggested this modality to be a powerful adjunct in anatomic evaluation of fetuses with trisomy 18. Also, sonographer experience varies, and image quality may be affected by maternal body habitus and other factors, such as a previous cesarean scar. It also allows earlier termination of pregnancy if desired, which may be associated with less clinical morbidity and emotional difficulty. Postnatal Patients choosing to continue the pregnancy must make decisions regarding delivery and postpartum treatment of the infant. Consultations with neonatal intensive care unit clinicians help with difficult decision making. Closure of ventricular septal defects in patients with trisomy 18 is associated with extended survival. Is second-trimester genetic amniocentesis for trisomy 18 ever indicated in the presence of a normal genetic sonogram Second trimester prenatal ultrasound for the detection of pregnancies at increased risk of trisomy 18 based on serum screening. Role of second trimester sonography in detecting trisomy 18: a review of 70 cases. Three- and 4-dimensional ultrasonography in the prenatal evaluation of fetal anomalies associated with trisomy 18. Fetal nasal bone in screening for trisomies 21, 18 and 13 and Turner syndrome at 11-13 weeks of gestation. Tricuspid regurgitation in screening for trisomies 21, 18 and 13 and Turner syndrome at 11+0 to 13+6 weeks of gestation. Ductus venosus Doppler in screening for trisomies 21, 18 and 13 and Turner syndrome at 11-13 weeks of gestation. First- and second-trimester screening: detection of aneuploidies other than Down syndrome. Maternal serum-integrated screening for trisomy 18 using both first- and second-trimester markers. Prenatal ultrasonographic features of the PenaShokeir I syndrome and the trisomy 18 syndrome. Controversy exists about whether the incidence increases with advancing paternal age. Between 10 weeks and 14 weeks of gestation, risk of trisomy 21 for a 20-yearold woman ranges from 1: 983 to 1: 1140 compared with 1: 229 to 1: 266 for a 35-year-old woman and 1: 15 to 1: 17 for a 45-year-old woman. Individuals with trisomy 21 carry three copies of the entire 21 chromosome or three copies of the critical region of chromosome 21. Etiology and Pathophysiology Most cases of trisomy 21 are due to meiotic nondisjunction (95%), usually in the ovum. Of the remaining 5%, unbalanced translocation accounts for 3% to 4%, and mosaicism accounts for 1%. The additional copy of chromosome 21 presumably causes increased expression of many genes on the chromosome, and the imbalance in expression of trisomy 21 and nonrisomy 21 genes is thought to cause the various phenotypic expressions of the disorder. Definitive diagnosis depends on invasive testing, usually amniocentesis or chorionic villus sampling, although fetal blood sampling has also been used. Using both measurement of nuchal translucency and serum markers in the first trimester was more effective for trisomy 21 screening than using either screening modality alone. Detection was improved, albeit to a lesser degree, after integrated (from 93% to 98%), stepwise (from 97% to 98%), or contingent (from 95% to 97%) screening. Nearly half of fetuses with Down syndrome have heart defects; most common are atrioventricular septal defects (atrioventricular canal), ventricular septal defects, and atrial septal defects. Ultrasound Features of Trisomy 21 Structural Defects Cardiacdefects Ventriculomegaly Duodenalatresia Esophagealatresia/tracheoesophagealfistula Aneuploidy Markers Clinodactyly Absentnasalbone Echogenicintracardiacfocus Echogenicbowel Nuchalfold Pyelectasis Sandalgap Shortlongbones Widenediliacangle Shortearlength syndrome had atrioventricular septal defects, and 35% had ventricular septal defects. Minor markers are seen more commonly than major malformations in an unselected population (Table 160-2). Other statistically significant findings were short femur, short humerus, echogenic intracardiac focus, pyelectasis, echogenic bowel, and ventriculomegaly. Nuchal translucency is the normal subcutaneous fluid-filled space between the back of the fetal neck and the overlying skin. In a large study by the Fetal Medicine Foundation, nuchal translucency had a trisomy 21 detection rate of 77% with a 5% false-positive rate. In these trials, the detection rate of Down syndrome with nuchal translucency measurement alone was 70% with a 5% false-positive rate. There is controversy about whether it is a separate entity or on the severe end of the spectrum of nuchal translucency. Cystic hygroma carries an aneuploidy risk of 50%12 and should raise suspicion of trisomy 21. The soft tissue thickness posterior to the occiput, measured from the outer edge of the bone to the outer edge of the skin, is the nuchal fold. In their study, absent nasal bone was seen in 73% of fetuses with Down syndrome, with a 0. A review of studies evaluating first-trimester nasal bone identification found that this is a sensitive and specific marker in high-risk pregnancies when performed in specialized centers with appropriately trained personnel. With angles less than 45 degrees or more than 135 degrees, the nasal bone may appear artificially absent. In the first trimester, a midsagittal view of the fetal profile should be obtained, with the fetus occupying greater than 50% of the image. The tip of the nose should be seen, and the angle between the transducer and a line passing from the fetal forehead to the chin should be 45 degrees. When the nasal bone is present, three echogenic lines should be visible (tip of nose, skin overlying nasal bone, and nasal bone itself). Many studies have examined the sensitivities of nasal bone measurements for detection of Down syndrome. It may be seen in either ventricle, although it is more common in the left ventricle.
Generic prednisolone 5 mg mastercard
Valved holding chambers (available with masks or mouthpieces) are typically larger allergy testing la crosse wi order 20mg prednisolone visa, which allows the aerosol to expand and remain in the device until inhaled; exhaled air does not return to the chamber. Thus, multiple inhalations can be used to completely empty the aerosol from the chamber. This is particularly important for children with tidal volumes that do not exceed the volume of the holding chamber (Dolovich et al. The advantages of spacer devices and valved holding chambers override the extra cost and bulkiness. Attach a disposable mouthpiece (arrow pointing toward the patient) to the top dial. Then, ask him/her to place his/her lips around the mouthpiece forming a good seal. Compare that inspiratory flow rate with the target flow rate for the selected device (Education/Clinicals, n. Based on how the actual inspiratory flow compares to the target flow rate, coach the child until the proper range is consistently achieved. The reproducibility between measurements seems to be better than is seen with peak flow meters, allowing for more accurate assessments of lung function over time (Tovar & Gums, 2004). Formoterol: Pharmacology, molecular basis of agonism, and mechanism of long duration of a highly potent and selective beta 2-adrenoceptor agonist bronchodilator. Interconversion of leukotrienes catalyzed by purified gamma-glutamyl transpeptidase: Concomitant formation of leukotriene D4 and gamma-glutamyl amino acids. Scientific rationale for inhaled combination therapy with long-acting beta2-agonists and corticosteroids. Cholinergic pathways in the lungs and anticholinergic therapy for chronic obstructive pulmonary disease. Nedocromil Sodium: An updated review of its pharmacological properties and therapeutic efficacy in asthma. Serevent nationwide surveillance study: Comparison of salmeterol with salbutamol in asthmatic patients who require regular bronchodilator treatment. Holding chambers versus nebulisers for beta-agonist treatment of acute asthma (Cochrane Review). Long-acting bronchodilator therapy for the treatment of chronic obstructive pulmonary disease. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Heart, Lung, and Blood Institute. Inhaled medication and inhalation devices for lung disease in patients with cystic fibrosis: A European consensus. Signal transduction and regulation: Are all alpha1-adrenergic receptor subtypes created equal Montelukast and emotional wellbeing as a marker for depression: Results from 3 randomized, doublemasked clinical trials. Anti-immunoglobulin E treatment with omalizumab in allergic diseases: An update on antiinflammatory activity and clinical efficacy. Rise and fall of asthma mortality in England and Wales in relation to use of pressurised aerosols. Use of regularly scheduled albuterol treatment in asthma: Genotype-stratified, randomised, placebocontrolled cross-over trial. A comparative study of the effects of an inhaled corticosteroid, budesonide, and of a 2-agonist, terbutaline, on airway inflammation in newly diagnosed asthma. Conversion of leukotriene D4 to leukotriene E4 by a dipeptidase released from the specific granule of human polymorphonuclear leucocytes. Corticosteroids as inhibitors of cysteinyl leukotriene metabolic and signaling pathways. The Salmeterol Multicenter Asthma Research Trial: A comparison of usual pharmacotherapy for asthma or usual pharmacotherapy plus salmeterol. Mechanisms of betaadrenergic receptor regulation in lungs and its implications for physiological responses. Ipratropium bromide: A review of its pharmacological properties and therapeutic efficacy in asthma and chronic bronchitis. Safety of ingestion of yellow tartrazine by double-blind placebo controlled challenge in 26 atopic adults. Analysis of behaviorrelated adverse experiences in clinical trials of montelukast. The long-acting beta2agonist salmeterol xinafoate: Effects on airway inflammation in asthma. Probing the salmeterol binding site on the beta 2-adrenergic receptor using a novel photoaffinity ligand, [(125)I]iodoazidosalmeterol. The anti-inflammatory effects of leukotriene-modifying drugs and their use in asthma. Central and peripheral mechanisms of narcotic antitussives: Codeine-sensitive and -resistant coughs. Enantiomers of bronchodilating beta2-adrenoceptor agonists: Is there a cause for concern The lungs, respiratory muscles, and nervous control of breathing are less developed in infants than in older children or adults; this predisposes them to respiratory failure. The chest wall of infants is very compliant (less stiff); consequently, they breathe less efficiently than their older counterparts. Their diaphragm is also at a mechanical disadvantage and may be more prone to fatigue. Furthermore, the neurological pathways that control breathing are immature and as a result, infants are more susceptible to apnea, or cessation of breathing. Developmental immaturity is more pronounced in preterm infants, placing them at an even higher risk of respiratory problems. Apnea of prematurity occurs in over 50% of premature infants and in the majority of infants who are less than 1,000 g at birth (Alden et al. It has been associated with sepsis, intracranial hemorrhage, vaccine administration (Klein et al. Additionally, a genetic predisposition is likely as there is a higher incidence of apnea of prematurity in infants born to first-degree consanguineous parents compared with other infants (Tamim, Khogali, Beydoun, Melki, & Yunis, 2003). Premature infants have an imbalance in the neural inputs that stimulate breathing and the inhibitory pathways that depress it. Premature infants have blunted respiratory responses to hypoxia (decreased delivery of oxygen to tissues) and hypercapnia (elevated carbon dioxide levels); they do not appropriately increase their breathing efforts in response to either. The impaired response to carbon dioxide is more pronounced in infants with apnea of prematurity (Gerhardt & Bancalari, 1984). Infants, both term and preterm, develop apnea when their larynx is stimulated, which is known as the laryngeal chemoreflex. Preterm infants have decreased tone in their upper airway, which makes them more susceptible to upper airway obstruction. Sleep mechanisms are immature and they have a decrease in their ability to arouse in response to respiratory problems, particularly in the prone position (Bhat et al. Neonatal lung disease: Apnea of prematurity and bronchopulmonary dysplasia 87 Apnea of prematurity can be central, obstructive, or mixed. Central apnea is the complete cessation of breathing effort; the brain fails to send the appropriate signals to the respiratory muscles to breathe. Hypoxia itself can produce apnea in preterm infants, which may increase the severity and duration of the apneic episode. It may be directly produced by the stimulus that causes the apnea or may be due to enhanced sensitivity to vagal nerve stimulation. However, recent studies do not bear out the association (Di Fiore, Arko, Whitehouse, Kimball, & Martin, 2005). Prone position is associated with an increase in central apneas and a decrease in arousals (Bhat et al. Classically, the infant may turn blue, pale, limp, and mottled and makes little or no respiratory effort. Infants may recover by themselves or may require stimulation in order to terminate the episode.