Cheap viagra plus 400 mg free shipping
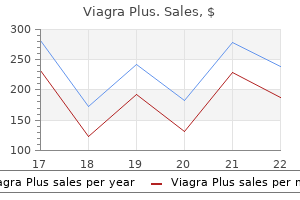
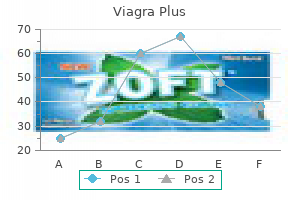
Treatment algorithms may have some usefulness erectile dysfunction related to prostate purchase viagra plus cheap, but it is prudent to systematically evaluate each case and formulate a unique treatment plan. Neurological symptoms caused by vascular steal, venous hypertension, or seizure may improve after targeted embolization, providing some benefit during the latency period after radiosurgery. Frequently cited features include nidus characteristics (diffuse versus compact), details of the arterial supply (number, location, size), presence of deep perforator supply, details of the draining veins (number, size), flow rate (high versus low), perinidal angiogenesis, and the specific pattern of arterial shunting. It may be mixed with varying amounts of ethiodized oil or glacial acetic acid to control the rate of solidification. Tantalum or tungsten powder may also be added to the mixture to increase its radiopacity. Intraoperative pictures show the blue microcatheter within a cortical artery that appears to have active blood flow (B). The catheter lumen can be seen after cauterization and transection of the partially embolized arterial feeder (C). With respect to the last point, differing philosophies exist, and it is unclear which approach is best. Some practitioners take an aggressive approach, attempting to embolize all accessible feeding pedicles or to directly occlude nidal compartments, whereas other practitioners are more conservative. Selective catheterization of a prominent deep lateral lenticulostriate feeder was subsequently performed (D). Glue cast, both intranidal and along the lenticulostriate feeder, can be seen on anteroposterior skull fluoroscopy (E). Repeat arteriography showed no further filling from the embolized deep lenticulostriate feeder, greatly facilitating subsequent surgical resection (F). The n-butyl cyanoacrylate glue cast at the end of the third embolization session can be seen on skull fluoroscopy (D). Good results have been reported in retrospective series by groups using each strategy. An aggressive posture toward preoperative embolization probably makes surgery easier and possibly even makes it safer. In general, pre-radiosurgical embolization may be performed with the objectives of volume reduction, latency period risk reduction, and/or the elimination radioresistant features. These limitations have prompted consideration for post-radiosurgery embolization as an alternative. Adjuvant embolization may address features such as associated aneurysms or arterial pedicles thought to result in symptomology resulting from steal. Similarly, angioarchitectural features that confer radioresistance such as high-flow fistulas may be targeted for occlusion in conjunction with radiosurgery. Complications, most of which do not result in permanent neurological injury, are reported in 5% to 15% of cases. In many cases, a relatively high upfront risk is acceptable if the subsequent surgical risks are reduced and long-term cure is possible. Rapid advancement in endovascular technology has enabled interventionalists to specifically target unique angioarchitectural features that pose the greatest threat during either surgery or the radiosurgery latency period. A population-based study of brain arteriovenous malformation: long-term treatment outcomes. The effect of embolization with n-butyl cyanoacrylate prior to surgical resection of cerebral arteriovenous malformations. A prospective, multicenter, randomized trial of the Onyx liquid embolic system and n-butyl cyanoacrylate embolization of cerebral arteriovenous malformations. The natural history of symptomatic arteriovenous malformations of the brain: a 24-year follow-up assessment. Concurrent arterial aneurysms in brain arteriovenous malformations with haemorrhagic presentation. Comparison of n-butyl cyanoacrylate and Onyx for the embolization of intracranial arteriovenous malformations: analysis of fluoroscopy and procedure times. Incidence and prevalence of intracranial vascular malformations in Olmsted County, Minnesota, 1965 to 1992. A systematic review of the frequency and prognosis of arteriovenous malformations of the brain in adults. Morbidity of intracranial hemorrhage in patients with cerebral arteriovenous malformation. Tumors Arising from the Blood-Vessels of the Brain; Angiomatous Malformations and Hemangioblastomas. The myth of the Brooks method of embolization: a brief history of the endovascular treatment of carotidcavernous sinus fistula. Calibrated leak balloon microcatheter: a device for arterial exploration and occlusive therapy. Surgery for unruptured arteriovenous malformations of the brain is better than conservative management for selected cases: a prospective cohort study. The failure of preoperative ethylene-vinyl alcohol copolymer embolization to improve outcomes in arteriovenous malformation management: case series. Complications of modern diagnostic cerebral angiography in an academic medical center. The relationship of coexisting extranidal aneurysms to intracranial hemorrhage in patients harboring brain arteriovenous malformations. Characteristics of arteriovenous malformations associated with cerebral aneurysms. The natural history and predictive features of hemorrhage from brain arteriovenous malformations. Cerebral arteriovenous malformations and associated aneurysms: analysis of 305 cases from a series of 662 patients. The influence of hemodynamic and anatomic factors on hemorrhage from cerebral arteriovenous malformations. Factors associated with intracranial hemorrhage in cases of cerebral arteriovenous malformation. Large and deep brain arteriovenous malformations are associated with risk of future hemorrhage. Features predictive of brain arteriovenous malformation hemorrhage: extrapolation to a physiologic model. Angioarchitectural characteristics of brain arteriovenous malformations with and without hemorrhage. A supplementary grading scale for selecting patients with brain arteriovenous malformations for surgery. Angioarchitecture determines obliteration rate after radiosurgery in brain arteriovenous malformations. Angiographic features help predict outcome after stereotactic radiosurgery for the treatment of pediatric arteriovenous malformations. Endovascular treatment of intracranial arteriovenous malformations with Onyx: technical aspects. Comparison of nbutyl cyanoacrylate and Onyx for the embolization of intracranial arteriovenous malformations: analysis of fluoroscopy and procedure times. Embolization of cerebral arteriovenous malformations achieved with polyvinyl alcohol particles: angiographic reappearance and complications. Surgical embolization of cerebral arteriovenous malformations through internal carotid and vertebral arteries. Catheter embolization of intracranial arteriovenous malformations as an aid to surgical excision. Adjuvant embolization with n-butyl cyanoacrylate in the treatment of cerebral arteriovenous malformations: outcomes, complications, and predictors of neurologic deficits. Stereotactic radiosurgery for arteriovenous malformations after embolization: a casecontrol study. Long-term results of gamma knife surgery for partially embolized arteriovenous malformations. Hemorrhagic complications after endovascular treatment of cerebral arteriovenous malformations. The most common manifestation in patients with this lesion is hemorrhage, followed by seizures and, less often, focal neurological deficits. The consequence of a hemorrhage is significant: death in 6% to 29% of cases and permanent morbidity in 16% to 35%.
Order genuine viagra plus on-line
If present erectile dysfunction treatment nyc discount 400mg viagra plus amex, the second anterior choroidal artery should also be preserved, and with a large superiorly projecting aneurysm, the recurrent artery of Heubner may be on the medial aspect of the aneurysm and must be preserved. After the two sides of the neck of the aneurysm are defined, a clip of appropriate length, usually straight, is slowly applied with the lower blade above the anterior choroidal artery and the upper blade against the superior aspect of the neck of the aneurysm (Video 385-1). After securing the aneurysm, the surgeon must check to ensure the patency of the anterior choroidal artery and the absence of perforating vessels between the blades of the clip. According to a new classification system, the cisternal segment of the aneurysm is divided into preoptic and postoptic parts. At the preoptic part, perforating vessels arise from the superolateral area and pass laterally. Unfortunately, there is no reliable technique for confirming the patency of the anterior choroidal artery except for direct visualization and inspection of flow inside the artery. An intraoperative angiogram could be used as a confirmatory test as long as the anterior choroidal artery is visible on the angiogram. Videoangiography with indocyanine green is another potentially useful adjunct in improving the safety of this procedure, as is neurophysiologic monitoring with the use of motor evoked potentials. Although flow may be apparent in the vessel, some patients still have postoperative deficits. The number of times a temporary clip is applied appears to be associated with ischemic events. Excessive temporal lobe retraction is avoided because it may rip the dome of the aneurysm, which frequently adheres to the mesial temporal lobe. In 70% of the cases, the anterior choroidal artery arises as a single trunk from the inferior aspect of the neck of the aneurysm. It runs in a lateral course, which makes it readily visible from the lateral side, and it can be duplicate or, in rare cases, triplicate. When more than one artery is involved, the aneurysm generally arises in relation to the largest branch. The key to the success of this operation is to preserve the anterior choroidal artery because occlusion of this artery may lead to contralateral hemiparesis, hemianopia, and hemisensory deficit. The surgeon then dissects the lateral aspect of the carotid artery, moving toward the proximal aspect of the neck of the aneurysm. It is usually easier to start the dissection on the inferior aspect of the neck to define the anterior choroidal artery and the plane between it and the aneurysm and to have proximal control. Retraction of the medial carotid artery should be avoided to prevent tearing of the aneurysm. After defining the lower border of the aneurysm neck, the surgeon moves to the superior aspect. Sometimes surgeons resect a small piece of the medial aspect of Aneurysms of the Internal Carotid Artery BifurcationAneurysms Anatomy. It sends perforating branches to the basal forebrain and gives rise to the recurrent artery of Heubner, which passes medial to the carotid bifurcation and its lenticulostriate perforating vessels. These perforating vessels usually supply the basal ganglia but may also supply the optic apparatus, hypothalamus, and mesial temporal lobe. The positioning and standard pterional craniotomy are done in the same manner described for aneurysms of the posterior communicating artery. With the aid of the microscope, the surgeon should split the sylvian fissure widely. Only then can the arachnoid membrane around the bifurcation be rolled up to expose the neck of the aneurysm and the perforating vessels. The dome of the aneurysm, which is usually buried into the substance of the basal forebrain, should not be disturbed. A small frontal corticotomy may be performed to facilitate visualization of the lenticulostriate and the recurrent artery of Heubner. With posteriorly pointing aneurysms, it is harder to dissect the recurrent artery of Huebner. Elective temporary clipping may be employed to allow full dissection and visualization of the perforating vessels before clipping. The clip should not exceed the size of the aneurysm, in order to avoid clipping the lenticulostriate perforating vessels, the recurrent artery of Heubner, the basal vein (vein of Rosenthal), or the deep sylvian vein. After clip placement, the vessels are inspected and checked with Doppler imaging, and the aneurysm is punctured with a 25-gauge needle to ensure obliteration. Meticulous hemostasis is secured, followed by dural closure and then closure of the craniotomy and the soft tissues. In addition, the dome may project anteromedially, displacing the anterior perforating vessels or the pituitary stalk, or both, in the medial direction. These aneurysms should be clipped carefully after the positioning and the approach are tailored to each case individually on the basis of the angiographic features. Proximal control remains the key issue in preventing intraoperative disasters, and proper visualization of medial structures is vital. Sometimes, and depending on the exact location of the proximal part of the neck of the aneurysm, drilling of the anterior clinoid process should be performed as described earlier. B, Exploration after pterional craniotomy; the left carotid bifurcation, the middle cerebral artery, and the left anterior cerebral artery are visible. C, Partial trapping of the aneurysm by temporary clipping of the internal carotid artery and the left anterior cerebral artery before dissection of the neck. They are fragile and can rupture during microsurgery, causing postoperative rebleeding more frequently than do saccular aneurysms. The diagnosis of these rare aneurysms is crucial before surgery because the strategy for clipping or other treatment is different than that for saccular aneurysms. Magnetic resonance studies of the aneurysm wall may also help determine the presence of a dissection process because the true physiopathologic process of these rare aneurysms is not clearly known. Endovascular embolization is not generally recommended for this kind of aneurysm because of the large base and the very loose fibrinous tissue of the dome. New endovascular options such as flow diverters have has shown reasonable results in few patients, but their efficacy has not been validated in larger series. Testing the competency of collateral flow should be part of the preoperative planning and decision making. Application of an encircling clip is another method that has limits because of the possibility that the perforating vessel may have to be sacrificed. Up to 28% of patients require a second therapeutic intervention to secure the aneurysm. Wrapping the aneurysm is another alternative; however, because of the fragility and likelihood of further aneurysm growth, the success rate after wrapping alone is low. The most important point in the management of these aneurysms is thorough preoperative diagnosis and planning for every possible scenario in order to avoid hemorrhagic and ischemic complications. Axel Perneczky advocated the keyhole approach in the 1980s, the aim being to make the minimal craniotomy needed to access deep-seated lesions. The supraorbital/keyhole craniotomy has been widely studied in cadaveric series and case series reports have shown its advantages and disadvantages, especially in comparison with open procedures. This technique allows for a wider operative field at depth at the cost of a smaller working angle; this is key for patient selection for this operation. With less dissection of the temporalis muscle, a smaller opening in the bone, and minimal brain manipulation, it makes for a faster, less painful recovery. This technique is also useful for treating a wide range of tumors in the anterior skull base; the optic, suprasellar, and parasellar regions; and the temporal and frontal lobes. In addition, in this era of endovascular treatment of the majority of aneurysms, those encountered by the neurosurgeon are of the complex varieties: multilobulated aneurysm, giant aneurysm, fusiform aneurysm with poor dome-to-neck ratio, or aneurysm in arterial branches originating from the neck or body. The choice of craniotomy should be based on the experience of the surgical team and the familiarity with a given approach. With good patient selection, the rates of morbidity and mortality of this approach are approximately the same as those for more open techniques. The combined rate of morbidity and mortality associated with intraoperative rupture is as high as 30% to 35%. The type of reaction to the intraoperative rupture is determined by when it happens. Proximal control is crucial, and the surgeon must be able to apply a temporary clip on the parent vessel before dealing with the aneurysm. If the rupture occurs before exposure of the aneurysm, two large-bore suctions should be in the wound immediately: one on the hole of the aneurysm (with the aid of cotton patties if the surgeon prefers) to help visualize the proximal vessel, which is then temporary clipped, and another temporary clip may be applied to the distal vessel. The dissection is then done with the patient in a condition of high blood pressure to reduce the ischemic insult.
Diseases
- Wiedemann Grosse Dibbern syndrome
- Astasia-abasia
- Sensorineural hearing loss
- Willebrand disease
- Batten Turner muscular dystrophy
- Anterior horn disease
Order viagra plus with american express
Intraoperative Doppler should be employed before and after clipping to establish baselines and to immediately detect any sonographic changes erectile dysfunction definition discount viagra plus 400mg otc. Cerebrovascular applications reported have included elective and ruptured intracranial aneurysms (Videos 388-1 and 388-2), intracranialextracranial revascularization, cerebral arteriovenous malformations, and dural arteriovenous fistulas. In our center, these techniques are used in a complementary fashion and on occasion are also complemented by intraoperative Doppler ultrasound. Moderate intracranial atherosclerosis in a 68-year-old patient with an incidental middle cerebral artery aneurysm. Clip application can be challenging because atherosclerosis can prevent complete closure of aneurysm clips or cause slippage with occlusion of adjacent vessels. Clips with higher closing strength, multiple clips, or unique application strategies may be necessary to safely ligate such lesions. The first reported use of adenosine in intracranial aneurysm surgery was described by Sollevi and colleagues. The single case of intraoperative cardiac arrest requiring chest compressions reported in the literature occurred in a patient in whom redosing of adenosine was done before full recovery of cardiac function from the preceding dose. Visualization of distal branches and small lenticulostriate arteries is often limited; the aneurysmal wall frequently incorporates the parent vessel or its branching arteries; and calcification, atheroma, or intraluminal thrombus at different stages is present. Aneurysmal sac thrombectomy and endarterectomy are often required for adequate reconstruction, which requires temporary trapping. Reductions of metabolic oxygen consumption with propofol or barbiturates, preoxygenation, modest hypothermia, induced hypertension, and temporary circulatory arrest have all been used in giant aneurysm surgery with variable rates of success. An ultrasonic aspirator is often used to evacuate the intraluminal thrombus more rapidly to reduce temporary occlusion time. Aneurysmorrhaphy must be carefully performed to avoid intimal injuries on the parent vessel, which can result in dissection and occlusion. Thrombotic aneurysms often develop thick necks that may require higher closing pressure clips or tandem clip configurations with fenestrated clips to achieve full aneurysmal obliteration. Incidental severe intracranial atherosclerosis and moderate-sized (8-mm) middle cerebral artery aneurysm in a 73-year-old patient. No therapy (endovascular or surgical) was recommended because of the high morbidity associated with either intervention. Distal subtraction angiography (A) and computed tomography (B) demonstrate evidence of severe atherosclerosis; note the narrowing of the distal M1 segment. If a low-flow bypass is anticipated preoperatively, the vessel pedicle is dissected out with the opening. High-flow extracranial-intracranial bypasses using saphenous vein or radial artery grafts may need to be considered for fusiform aneurysms involving more than one branch. Although the detailed technical nuances are beyond the scope of this chapter, several points deserve mentioning. If a bypass is considered likely, preoperative planning for graft harvesting is necessary to select the proper vessel without endangering the donor site. We occasionally perform a preemptive bypass in anticipation of the need for flow augmentation, whether or not it is ultimately needed. In salvage situations, the anterior temporal artery may be dissected and used as donor if an extracranial graft is not available. Analysis of 561 patients with 690 middle cerebral artery aneurysms: anatomic and clinical features as correlated to management outcome. Risk of rebleeding after treatment of acute hydrocephalus in patients with aneurysmal subarachnoid hemorrhage. Traumatic middle cerebral artery aneurysm: case report and review of the literature. Unruptured intracranial aneurysms-risk of rupture and risks of surgical intervention: International Study of Unruptured Intracranial Aneurysms Investigators. A clinical study of the relationship of timing to outcome of surgery for ruptured cerebral aneurysms. Peripheral large or giant fusiform middle cerebral artery aneurysms: report of our experience and review of literature. Multiple intracranial aneurysms followed left atrial myxoma: case report and literature review. Shared associations of nonatherosclerotic, large-vessel, cerebrovascular arteriopathies: considering intracranial aneurysms, cervical artery dissection, moyamoya disease and fibromuscular dysplasia. Aneurysmal rupture without subarachnoid hemorrhage: case series and literature review. The risk of rebleeding after external lumbar drainage in patients with untreated ruptured cerebral aneurysms. The pterional and suprabrow approaches for aneurysm surgery: a systematic review of intraoperative rupture rates in 9488 aneurysms. Retrograde dissection of the temporalis muscle preventing muscle atrophy for pterional craniotomy. The utility and limitations of intraoperative near-infrared indocyanine green videoangiography in aneurysm surgery. Indocyanine-green videoangiogram to assess collateral circulation before arterial sacrifice for management of complex vascular and neoplastic lesions: technical note. Safety, efficacy, and cost of intraoperative indocyanine green angiography compared to intraoperative catheter angiography in cerebral aneurysm surgery. Near-infrared indocyanine green video angiography: a new method for intraoperative assessment of vascular flow. Evaluation of surgical microscopeintegrated intraoperative near-infrared indocyanine green videoangiography during aneurysm surgery. Comparing indocyanine green videoangiography to the gold standard of intraoperative digital subtraction angiography used in aneurysm surgery. Adenosine-induced flow arrest to facilitate intracranial aneurysm clip ligation: dose-response data and safety profile. Adenosine for temporary flow arrest during intracranial aneurysm surgery: a single-center retrospective review. Adenosine-induced transient asystole for intracranial aneurysm surgery: a retrospective review. Ogilvy Microsurgical treatment of intracranial aneurysms represents a significant technical challenge for any neurosurgeon. Mastery of the surgical techniques required to treat aneurysms in these locations remains critical to the ability to offer a complete array of treatment methods. Further description of the suboccipital approach to treat posterior circulation aneurysms by Schwartz2 in 1948 added to the growing field. The surgical treatment of posterior circulation aneurysms, like much of neurosurgery at this time, was limited by poor surgical lighting and instruments. Further advancements in skull-based techniques, equipment, and neuroanesthesia led to an improved ability to provide treatment for these lesions. As endovascular methods for the treatment of aneurysms have improved, the utilization of coiling, stenting, or flow diversion techniques have in many centers become the firstline treatment of posterior circulation aneurysms owing to the less invasive nature and the lower associated risk of cranial nerve deficits. This paradigm shift occurred after the introduction of the Guglielmi detachable coil in 19915 and was further strengthened by the results of the International Subarachnoid Aneurysm Trial in 2002, which demonstrated lower rates of poor outcomes at 1 year with coiling rather than clipping of ruptured aneurysms. The telovelo-tonsillar segment begins at the tonsillar midpoint, continues superiorly to the roof of the fourth ventricle, at which point it loops again to descend inferiorly and posteriorly to the tonsillobiventral fissure. The cortical segment gives off a medial trunk to supply the vermian surface and a lateral trunk to supply the tonsillar and hemispheric surface. This important vessel then descends on the ventral surface of the medulla and spinal cord at the anterior median fissure, supplying the pyramids, the medial lemniscus, and the hypoglossal nuclei and nerves. An artistic demonstration of the five segments of the posterior inferior cerebellar artery. The first two segments have an intimate relationship with the brainstem and associated cranial nerves and are best approached through a standard far lateral suboccipital craniotomy. The third, tonsillomedullary segment is generally approached through an extended far lateral suboccipital craniotomy. Fusiform aneurysms that involve the entire circumferential arterial segment are less common. Alternative strategies to traditional microsurgical clipping often involve direct vessel sacrifice or a combination of trapping and bypass. The reported 5-year cumulative rupture rates for aneurysms of the vertebrobasilar system as well as the posterior communicating artery measuring less than 7 mm, 7 to 12 mm, 13 to 24 mm, and 25 mm or greater were 2. The highest rates of rupture were found at the anterior communicating artery, the posterior communicating artery, and the basilar tip. Interestingly, the vertebral artery and posterior inferior cerebellar artery did not demonstrate the same significantly high rupture rates as in the International Study of Unruptured Intracranial Aneurysms.
Buy viagra plus 400mg low cost
A diagnosis may be suggested by multisystem clinical involvement and laboratory features (Box 16 erectile dysfunction doctors san antonio purchase viagra plus on line. There is often a broad range of severity among patients with the same genetic disorder, making diagnosis on clinical grounds often challenging. New treatment options have become available for some patients with periodic fever syndromes, and patients require specialist supervision. Children or adolescents present with bone pain, sometimes accompanied by swelling; the most common affected areas are long bones (tibia), but ribs, clavicle, vertebrae or mandible can be involved. Radiographs show osteolytic changes similar to osteomyelitis, and a bone scan may show lesions that are asymptomatic. Many children with rheumatic diseases have continuing disease activity or relapses in adulthood, or sequelae from previous disease activity, which require ongoing medical treatment. Musculoskeletal Disorders in Children and Adolescents 111 Healthcare transition for youths with childhoodonset rheumatic diseases describes the movement of patients from child and familycentred paediatric care to adultoriented healthcare systems. Education and support are paramount, particularly with complex treatment regimes and the impact on adolescent behaviours, such as avoidance of pregnancy and excess alcohol in those taking methotrexate. Both conditions are rare below the age of 50 and peak in patients aged over 70 years. Women are affected three times more frequently than men, and whilst it can affect any ethnic group, it is more common in northern Europeans. This highly disabling condition is the most common inflammatory rheumatological disorder of older people. Whilst it may affect any large or medium sized artery, it has a propensity to affect the branches of the external carotid artery, particularly the posterior ciliary arteries that supply the optic nerve and the superficial temporal artery (hence the use of the alternative name temporal arteritis). Prompt recognition and early treatment are essential to prevent longterm complications, including permanent loss of vision. There are clinical and pathogenetic links between temporal arteritis, giant cell arteritis and polymyalgia rheumatica, which has led to the concept that they are manifestations of a disease spectrum that affects the same disease population. The two entities may occur in the same patient simultaneously, at different time points or independently. Symptom onset is often rapid and dramatic, with bilateral pain and stiffness in the shoulders and hips causing marked functional impairment. Patients often report problems lifting heavy objects, getting off the toilet or rolling over in bed. Atypical presentation may lead to diagnostic difficulty, and as such early referral for specialist assessment can be helpful in nonclassic cases. The publication of provisional classification criteria, whilst not intended for diagnostic use (Table 17. Later, fibrosis and repair may predominate, the artery may have a nodular indurated feel to it and the pulse is almost absent. It is important to consider atypical presentations as only half of patients report a temporal headache and 24% have no headache symptom at all. Systemic features, including polymyalgia symptoms, weight loss, fatigue and fever, may dominate, making diagnosis challenging. Late complications of large vessel involvement including aortic aneurysm and stenosis may complicate the disease course. The arteries are visibly thickened and inflamed; palpation of the vessel is painful. Here, the sixth nerve is clearly involved aorta by clinical and imaging assessment, as aneurysmal rupture is a cause of premature mortality in these patients. In a specialist setting, vascular assessment with ultrasound, computed tomography/magnetic resonance imaging or conventional angiography may be required to assess the activity and extent of vascular involvement. Multinucleated giant cells and macrophages are attacking the elastic tissue and ingesting it. Anterior transverse ultrasound image of the right shoulder with maximum internal rotation of the arm. There is limited trial evidence to support clinicians in reducing the dose of oral glucocorticoid and patients need to be counselled that treatment may last 2 years or more, and that they might experience a spike in symptoms as the glucocorticoid dose is reduced. Patients with an incomplete response to glucocorticoids should be referred for specialist assessment. There is a lack of trial evidence supporting the use of other drugs (such as leflunomide and tocilizumab) although they may be used by specialists under careful supervision for some patients not responding to usual treatment. Patients should be fully informed about potential side effects and provided with a steroid information card. Gastroprotection with a proton pump inhibitor should be considered, especially in older patients. Blood pressure and serum glucose should be monitored, especially in patients with preexisting hypertension and diabetes. The lifetime risk of adult onset rheumatoid arthritis and other inflammatory autoimmune rheumatic diseases. It is possible to achieve good disease control but life long followup is needed to prevent and treat flares, to limit the complications due to damage and reduce the risk of premature death. Thus, it is important that the primary care physician, patient and hospital specialists are involved closely in the management of these diseases. Lcanavanine in alfalfa (but still debatable) Causes Systemic lupus erythematosus is a multifactorial disease due to a complex interplay of genetic and environmental factors that vary between individuals (Boxes 18. Defective clearance of apoptotic cells and immune complexes contributes to pathogenesis, with the activation of complement playing a major role in tissue damage. Antiphospholipid antibodies are a specific family of autoantibodies directed against anionic phospholipids located in cell membranes. The pathogenic mechanisms in antiphospholipid syndrome relate to the prothrombotic effects of these antibodies in vivo. Nevertheless, the consistent trend reflects that the burden of disease is highest in women and higher among nonwhite ethnic groups (Table 18. These criteria were designed not for diagnosis but for classifying patients into studies and clinical trials. For example, a 25yearold woman with malar rash, positive antinuclear antibody and histologically proven glomerulonephritis obviously has systemic lupus erythematosus, despite fulfilling only three criteria (Table 18. This variability may be due to true population differences or to dissimilar methods of case ascertainment. Other constitutional symptoms of active disease include fever, malaise, anorexia, lymphadenopathy and weight loss. The most common form of anaemia is a normochromic normocytic anaemia of chronic disease. Some patients develop an antibodymediated haemolytic anaemia and others an iron deficiency anaemia secondary to peptic ulceration or gastritis (usually due to nonsteroidal antiinflammatory drugs. Subacute cutaneous lupus erythematosus is a nonscarring rash found in areas of the body exposed to the sun. Discoid lesions are chronic scarring lesions that heal with hypo or hyperpigmentation. Musculoskeletal manifestations Generalized arthralgia with early morning stiffness and no swelling is very common. Indeed, secondary causes of myopathy are more common and can be caused by corticosteroids, antimalarials and lipidlowering agents. Avascular necrosis and infection should be suspected if the patient complains of sudden onset, severe pain in only one joint. Renal biopsy is helpful for assessing the severity, nature, extent and reversibility of the involvement and is an important guide to treatment and prognosis. For example, those with mesangial nephritis (class I) rarely progress to renal failure.
Purchase viagra plus with visa
Diverse effects of fibronectin and laminin on phenotypic properties of cultured arterial smooth muscle cells erectile dysfunction 17 generic 400 mg viagra plus free shipping. Developmental regulation of the laminin 5 chain suggests a role in epithelial and endothelial cell maturation. Microscopic examinations of experimental aneurysms at the fenestration of the anterior cerebral artery in rats. Matrix metalloproteinases 2 and 9 in human atherosclerotic and non-atherosclerotic cerebral aneurysms. Immunocytochemical studies of atherosclerotic lesions of cerebral berry aneurysms. Expression of structural proteins and angiogenic factors in normal arterial and unruptured and ruptured aneurysm walls. Complement activation associates with saccular cerebral artery aneurysm wall degeneration and rupture. A comparative study of patients without vascular diseases and those with ruptured berry aneurysms. Morphometric analysis of reticular and elastin fibers in the cerebral arteries of patients with intracranial aneurysms. Histological and morphometric observations on the reticular fibers in the arterial beds of patients with ruptured intracranial saccular aneurysms. Smooth muscle cells and the formation, degeneration, and rupture of saccular intracranial aneurysm wall-a review of current pathophysiological knowledge. Physical factors in the initiation, growth, and rupture of human intracranial saccular aneurysms. Elastin degradation in the superficial temporal arteries of patients with intracranial aneurysms reflects changes in plasma elastase. Serum elastase and alpha1-antitrypsin levels in patients with ruptured and unruptured cerebral aneurysms. Apoptosis of medial smooth muscle cells in the development of saccular cerebral aneurysms in rats. Increased expression of phosphorylated c-Jun amino-terminal kinase and phosphorylated c-Jun in human cerebral aneurysms: role of the c-Jun aminoterminal kinase/c-Jun pathway in apoptosis of vascular walls. Involvement of mitogen-activated protein kinase signaling in growth and rupture of human intracranial aneurysms. Cathepsin B, K, and S are expressed in cerebral aneurysms and promote the progression of cerebral aneurysms. Simvastatin suppresses the progression of experimentally induced cerebral aneurysms in rats. Macrophage-derived matrix metalloproteinase-2 and -9 promote the progression of cerebral aneurysms in rats. Prevention of rat cerebral aneurysm formation by inhibition of nitric oxide synthase. Mouse model of cerebral aneurysm: experimental induction by renal hypertension and local hemodynamic changes. Disruption of gene for inducible nitric oxide synthase reduces progression of cerebral aneurysms. Gene expression during the development of experimentally induced cerebral aneurysms. Association between semicarbazide-sensitive amine oxidase, a regulator of the glucose transporter, and elastic lamellae thinning during experimental cerebral aneurysm development: laboratory investigation. Velocity profile and wall shear stress of saccular aneurysms at the anterior communicating artery. Wall shear stress on ruptured and unruptured intracranial aneurysms at the internal carotid artery. Regional accumulations of T cells, macrophages, and smooth muscle cells in the human atherosclerotic plaque. T lymphocytes from human atherosclerotic plaques recognize oxidized low density lipoprotein. Adventitial infiltrates associated with advanced atherosclerotic plaques: structural organization suggests generation of local humoral immune responses. Accumulation of activated mast cells in the shoulder region of human coronary atheroma, the predilection site of atheromatous rupture. Mast cells in neovascularized human coronary plaques store and secrete basic fibroblast growth factor, a potent angiogenic mediator. Co-accumulation of dendritic cells and natural killer T cells within rupture-prone regions in human atherosclerotic plaques. Colocalisation of intraplaque C reactive protein, complement, oxidised low density lipoprotein, and macrophages in stable and unstable angina and acute myocardial infarction. Association between complement factor H and proteoglycans in early human coronary atherosclerotic lesions: implications for local regulation of complement activation. Elevated levels of lipoprotein (a) in association with cerebrovascular saccular aneurysmal disease. Intra-aneurysmal hemodynamics in a large middle cerebral artery aneurysm with wall atherosclerosis. Genomewide linkage in a large Caucasian family maps a new locus for intracranial aneurysms to chromosome 13q. A balanced translocation truncates neurotrimin in a family with intracranial and thoracic aortic aneurysm. There are two important goals in the treatment of patients with intracranial aneurysms. In addition, the safety and efficacy of the treatment options and skill and experience of the practitioners need to be considered. The present chapter reviews the factors involved in decision making in the management of patients with cerebral aneurysms. Many patient-related factors will determine outcome irrespective of how the aneurysm is treated. Choosing the treatment modality that is safest and most efficient for each individual patient is an important therapeutic decision. This progress is reflected in the decreasing case fatality rate over recent years. By contrast, three quarters of the patients without postoperative neurological deterioration at 24 hours had a good outcome. This includes (1) patient age and comorbid conditions; (2) aneurysm morphology, lesion size, and attendant risk; (3) endovascular versus microsurgical accessibility/suitability, and long-term angiographic outcome; and (4) expected recovery duration and required longterm follow-up. Taken together, the natural history of the patient and the natural history of the particular aneurysm must be considered to determine the optimal approach to treatment. For example, the treatment of a small basilar bifurcation aneurysm in a 40-year-old will differ from that in an 80-year-old despite the similarity in the lesion. Thus exclusive focus on either the patient or the aneurysm is not an optimal management strategy. Patient considerations and the natural history of cerebral aneurysms are reviewed in Chapters 370 and 377. Furthermore, aneurysms that rupture may not be the same as the ones found incidentally. The reader is referred to Chapter 377 for a more detailed review, but a brief understanding of natural history is central to treatment decision making. Several risk factors are associated with development of intracranial aneurysms, including advanced age; hypertension; cigarette smoking; thoracic aortic aneurysms, especially descending ones; and hereditary deficiencies such as polycystic kidney disease, Ehlers-Danlos syndrome, Marfan syndrome, fibromuscular dysplasia, or a family history of aneurysm disease. To date, there have been no population-based clinical studies to examine the cost effectiveness of screening for intracranial aneurysms. Posterior aneurysm locations include the posterior circulation and posterior communicating artery. In carefully selected patients, flowdiverting stents may be used for complex aneurysms that recur after surgery. Raaymakers and coworkers47 also performed a meta-analysis from a Medline search between 1966 and 1996 and identified 61 studies involving 2460 patients. Morbidity rates were greater for large or posterior circulation aneurysms but also were greater in higher quality studies. Similar findings were reported from a Japanese natural history study that included 6697 aneurysms in 5720 patients.
Syndromes
- Difficulty walking
- Visit your eye doctor at least once a year, or more often if you have signs of diabetic eye disease.
- Drainage of blood from the brain area (cerebral ventricular drainage)
- Yellow skin
- Heart rate may be over 100 (normal is 60 to 100 beats per minute)
- Rash
- Bluish-colored lips and fingers
- · Charge a high fee
- Loss of menstrual period
- Your head will suddenly fall forward, your jaw will become slack, and your knees will buckle.
Cost of viagra plus
If spasm around the wire tip occurs erectile dysfunction drugs and infertility generic viagra plus 400 mg with amex, the wire should be retracted until its tip bounces freely with arterial pulsations, as seen fluoroscopically; in addition, control angiography should demonstrate satisfactory flow in the instrumented vessel. The probability of vessel wall failure as a result of critical wall tension is proportional to the product of the balloon inflation diameter and inflation pressure, divided by vessel wall thickness. Consequently, the dilating force applied to the vessel wall, the diameter of the balloon in relation to the diameter of the unstretched cerebral artery, and the maximum distention of the cerebral artery determine the probability of vessel wall rupture. Mechanical testing of unfixed human cerebral arteries harvested within 12 hours of death shows irreversible plastic deformation with inflation pressures in the range of 0. However, when balloons are constrained by constricted arteries, the inflation pressure can rise dramatically with each additional increment of inflation volume. Therefore, it is safest to keep the diameter of the inflated balloon below the basal diameter of the treated arterial segment. As with all types of hemorrhagic complications, anticoagulation should be reversed as rapidly as possible with protamine. Intracranial hypertension should be controlled medically and with ventricular drainage as necessary. Control angiography should be performed through the guide catheter to assess hemostasis while the balloon is inflated. If bleeding persists around the balloon, the surgeon should consider repositioning the balloon or placing a second balloon. Depending on the affected vessel, sacrifice by coil embolization may be necessary but may be incompatible with an acceptable outcome. If necessary, a second embolization-capable microcatheter should be used while the balloon remains in place. In some cases, sustained balloon occlusion for 30 to 60 minutes produces durable hemostasis that continues after the balloon is deflated. In other cases, the rupture is converted to a pseudoaneurysm, which may be amenable to coil embolization with or without a stent for vessel reconstruction. In our experience, such pseudoaneurysms are difficult to control by coil embolization alone. Embolization with a combination of coils and a liquid embolic agent, performed in a balloon remodeling technique, is more likely to be successful. Longer balloon lengths that extend across the entire treatment segment are advantageous in that they limit the number of inflations necessary to complete treatment. This avoids repetitive injury to transition segments bridging sequentially dilated segments and prevents loss of balloon radiopacity (visbility) when single-lumen balloon catheters are used. When successive dilations are performed, they should be done in the distal-to-proximal direction, which avoids instrumentation of freshly dilated segments. Treatment paradigms will continue to evolve as new medications become available, diagnostic modalities are discovered, and the pathophysiologic characteristics of vasospasm are better understood. Because of these promising future developments, vascular neurosurgeons and interventionalists should remain attuned to such changes and tailor treatment regimens accordingly. American Heart Association Stroke Council; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; Council on Cardiovascular Surgery and Anesthesia; Council on Clinical Cardiology. Comparison of balloon angioplasty and papaverine infusion for the treatment of vasospasm following aneurysmal subarachnoid hemorrhage. Intracranial pressure changes induced during papaverine infusion for treatment of vasospasm. Intracranial pressure monitoring during intraarterial papaverine infusion for cerebral vasospasm. The efficacy and safety of angioplasty for cerebral vasospasm after subarachnoid hemorrhage. Effect of intraarterial verapamil on the diameter of vasospastic intracranial arteries in patients with cerebral vasospasm. High-dose intraarterial verapamil in the treatment of cerebral vasospasm after aneurysmal subarachnoid hemorrhage. Intraarterially administered verapamil as adjunct therapy for cerebral vasospasm: safety and 2-year experience. The prophylactic use of transluminal balloon angioplasty in patients with Fisher grade 3 subarachnoid hemorrhage: a pilot study. Both treatment modalities are viable options, and as each patient is different, so is each aneurysm. The decision to treat and which method of treatment to use is complex and involves consideration of the natural history of cerebral aneurysms (see Chapter 377), characteristics of the patient and the aneurysm, and the risks involved in any treatment (see also Chapter 379). Understanding the risks entails familiarity with the status of current techniques of treatment. As already noted, many of these considerations are extensively reviewed in other chapters (see Chapters 379 and 384-398). Another important factor in the success of treatment is a skull base approach to the aneurysm, which, by removal of enough bone, makes less retraction necessary. Proximal and Distal Control Securing control of blood flow both proximal and distal to the aneurysm being treated serves to prevent devastating hemorrhage in the event of intraoperative rupture and also softens the aneurysm, thereby aiding in perianeurysmal dissection and eventual clip placement. In many aneurysms of the anterior circulation, proximal and distal control may be accomplished with relative simplicity by dissection of the parent artery proximal and distal to the aneurysm in question and placement of a temporary clip at both locations. Temporary clips have a less aggressive closing force than do permanent clips, which prevents damage to or dissection of the artery being clipped. In some cases, however, proximal control of the parent vessel may be impractical because bone or other anatomy obscures the proximal portion of the parent vessel. In these cases, alternative techniques are often employed to decrease blood flow to the aneurysm. If proximal control cannot be secured intracranially or extracranially (as may be the case with some aneurysms of the proximal basilar artery, for example), adenosine-induced bradycardia and hypotension may prevent catastrophic hemorrhage and provide enough proximal control to allow for effective dissection and clipping. Thus dissection of, and maneuverability within, the subarachnoid space are fundamental in cerebrovascular surgery. Particularly in the setting of subarachnoid hemorrhage, this dissection can be made difficult by the presence of hemorrhagic byproducts, inflammatory reactions, fibrinous adhesions, and, occasionally, edema that renders the brain resistant to manipulation. Therefore, although the dissection can be difficult, it is vital to optimize the conditions to make it as easy and safe as possible. First, it is important to treat hydrocephalus before the craniotomy because it is the easiest way to treat one of the causes of brain swelling. Hydrocephalus is often associated with a subarachnoid hemorrhage, and a ventriculostomy on the opposite side of the craniotomy will effectively treat this association. In other cases, as in the interhemispheric approach to aneurysms of the pericallosal artery (to be described), gravity may assist with brain mobilization, in such a way that additional mechanical retraction is often not required. The surgeon may also effectively reduce brain swelling by administering intravenous hypertonic solutions or pharmacologic metabolic suppressive agents. The majority of intracranial aneurysms, however, may be approached and treated with the use of a minimal number of cranial approaches, each of which can be modified in a variety of ways to suit the particular structure of the aneurysm being treated. A, Pterional craniotomy for approach to aneurysms of the middle cerebral artery; skin incision is represented by dashed red line, bur holes by yellow circles, and the craniotomy by blue dashed line. B, Pterional craniotomy depicting intracranial view of an aneurysm in the middle cerebral artery after craniotomy. Positioning the patient is placed supine with a shoulder roll under the ipsilateral shoulder. The head is placed in three-point pin fixation, rotated 10 to 45 degrees to the contralateral side, and translated anteriorly. The vertex is then rotated 10 to 20 degrees toward the floor, which places the malar eminence at the highest point of the operative field and allows gravity to pull the frontal and temporal lobes away from the sylvian fissure, so that less frontal and temporal lobe retraction is necessary. During scalp dissection, it is preferable to avoid injury to the superficial temporal artery or violation of the temporalis fascia. Some surgeons prefer to bluntly dissect the plane between the galea and temporalis fascia/pericranium before incising the galea in this area, in efforts to prevent inadvertent entry into the temporalis muscle, which could make reapproximating the muscle slightly more difficult during closure. In the majority of cases, the frontal sinus is not entered during the pterional craniotomy, but if the patient has a large frontal sinus, it may be prudent to prepare a vascularized pericranial graft at this time for repair of any frontal sinus violations during the procedure. The techniques by which the temporalis muscle may be incised, mobilized, and retracted are numerous; each has its own virtues and limitations. The temporalis fascia may be incised inferior to the superior temporal line and at the posterior aspect of the skin incision (leaving a cuff of muscle fascia in both locations to assist with muscle fascia reapproximation during closure), and both scalp and temporalis muscle may be elevated as one unit, both being reflected anteriorly.
Effective 400mg viagra plus
Of the surgical patients erectile dysfunction and alcohol generic viagra plus 400 mg free shipping, 12 improved postoperatively, 2 remained stable, and 3 deteriorated. Importantly, the 3 patients managed conservatively demonstrated a stable neurological examination over a follow-up of 3 to 9 years. Bian and coworkers reported postoperative improvement of symptoms in 16 patients with symptomatic spinal cord cavernous angiomas. Patients presenting with rapid deterioration from Foix-Alajouanine syndrome are at risk for permanent disabling neurological injury from venous hypertension and venous thrombosis. Transarterial embolization allows for a rapid occlusion of the feeding pedicle and immediate reduction of venous hypertension until definitive microsurgical intervention can be performed, if necessary. SurgicalTechnique Most cavernous angiomas are amenable to resection by the posterior approach. Lateral and anterolaterally placed lesions can be accessed with costotransversectomy, sectioning of the dentate ligaments, and mildly rolling the cord to the contralateral side. Cavernous angiomas of the posterior half of the cord are associated with a lower incidence of iatrogenic injury during surgery and a better clinical prognosis than ventrally located lesions. Following dural opening, cavernous angiomas that extend to the cord surface are identified by hemosiderin staining and blue discoloration of the pia. The pia is opened, ideally where the mass presents to the surface, and dissection proceeds in the gliotic plane. The bipolar forceps are used to coagulate the surface of the lesion and collapse it inward. At the margins, the cavernous angioma may be adherent to the surrounding tissue, and the lesion may have to be removed in multiple pieces. Complete resection is necessary because residual pieces of cavernous angioma often result in symptomatic rehemorrhage. A third administration was given to evaluate for residual shunting within the resection bed. Outcomes Postsurgical outcomes are largely dependent on preoperative neurological function (Table 414-6). Additional data suggest that patients with a prolonged history (>3 years) of symptoms before resection fare worse than patients with a shorter duration of symptoms126; 15% to 25% of surgical patients experience a worsening neurological deficit immediately following surgery. However, in most cases, the postoperative deficits resolve and patients exhibit improvement or stabilization. Maslehaty and colleagues retrospectively reviewed 14 patients with symptomatic spinal cavernous angiomas treated with microsurgical resection125; 7 patients demonstrated rapid improvement postoperatively, whereas the remaining 7 patients slowly improved and reported a favorable outcome. Steiger and associates reported 20 clinically symptomatic patients treated with either conservative management (3 patients) or microsurgical resection (17 patients). Intraoperative Arteriography Intraoperative arteriography provides evaluation of blood flow, highlights relationships between feeding arteries and draining veins, and defines the complex angioarchitecture of spinal vascular malformations. Disadvantages include that it can be time-consuming and technically difficult with patients in the prone position. However, long metal sheaths that can be exposed alongside the buttocks improve the ease with which the procedure can be performed. She had an abrupt onset of severe headache, stiff neck, and weakness and numbness of the left upper and lower extremities 11 days before admission. Note that in D the coiled, dilated arterialized veins conceal the site of the fistula and obscure visualization of the aneurysm. To reduce blood flow through the fistula, a coil was positioned in the distal portion of the principal feeding artery, a posterior spinal artery, just proximal to the small aneurysm (G, arrow) the day before the fistula was interrupted surgically and the large varix was excised. At surgery, opening of the dura and arachnoid (J) exposed the extramedullary varix (white arrow), the blue-gray color of an intramedullary varix just beneath the pia (black arrow), and the tortuous arterialized veins overlying the spinal cord superiorly. The tortuous arterialized veins covering the extramedullary portion of the patent part of the aneurysm (J, white arrow) have been dissected free and displaced superiorly. Exposure of the anterolateral margin of the spinal cord on the left side revealed the major feeding vessel and the small aneurysm that arose from it (K). A vertical pial incision was made over the site of the pial discoloration (J, black arrow) covering the most superficial extension of the intramedullary component of the patent aneurysm, just medial to the posterior nerve root entry zone. The soft, gliotic tissue at the interface between the spinal cord and the aneurysm was used to dissect the aneurysm from the spinal cord and fully expose the darkly colored patent (M, white arrows) and the gray-white thrombosed (M, black arrow) intramedullary portions of the aneurysm, and the fistula was interrupted and the aneurysm excised (N). Dissection required rotation of the aneurysm such that in M, the extramedullary component of it (J, white arrow) is ventral and cannot be seen. The large arrows in P and Q indicate the coil, and the intermediate-sized arrows show the ventral medullary arteries supplying the anterior spinal artery. Intraoperative neurophysiologic monitoring is standard practice at many centers in the surgical management of myelopathy due to degenerative disease and spinal tumors. Significant variability in the normal vasculature of the spinal cord can result in complex patterns that are difficult to interpret. Intraoperatively, temporary occlusion of feeding arteries before permanent sacrifice allows monitoring to reflect ischemic changes in function of the spinal cord. En passage vessels may be identified with this technique, allowing for distinction between branches purely feeding the nidus and those supplying the spinal cord. Neurophysiologic monitoring can also be useful during the dissection of the nidus within the gliotic plane. Diminished signals alert the surgeon to excess manipulation and allow countermeasures to be performed, such as temporarily halting retraction or resection, elevating the blood pressure, and irrigating the spinal cord. A major limitation of these tests is spread of the agent to vascular territories outside of the injected vessel, leading to false-positive results. Provocative testing can be a useful surgical adjunct but should be in combination with the detailed knowledge of vascular anatomy that can only be obtained from arteriography. Conservative management has no role in the treatment of these lesions because persistent venous hypertension within the coronal venous plexus leads to venous congestion of the cord, potential venous thrombosis, and irreversible cord injury. Embolization, which can be performed rapidly, is a useful adjunct in patients presenting with acute and rapid neurological deterioration from malignant venous hypertension (Foix-Alajouanine syndrome). Venous congestion, cord compression, and hemorrhage, individually or combined, can produce neurological deficits of varying severity. Management of these lesions can be through embolization, microsurgical resection, or a combination of both. Depending on fistula type, embolization, microsurgical obliteration, and embolization combined with surgery represent treatment options. Asymptomatic and minimally symptomatic spinal cavernomas can be managed conservatively. Prompt diagnosis and intervention greatly improve the likelihood of an optimal clinical outcome for all types of spinal vascular malformations. Application of it over time permitted distinctions between the various types of vascular abnormalities and the development of logical classification schemes. Successful management depends on the avoidance of iatrogenic neurological impairment. Outcomes are related to lesion type and early diagnosis and intervention, when the neurological impairment is limited. Evaluation of angiographically occult spinal dural arteriovenous fistulae with surgical microscopeintegrated intraoperative near-infrared indocyanine green angiography: report of 3 cases. Microvascular anatomy of dural arteriovenous abnormalities of the spine: a microangiographic study. Outcome after the treatment of spinal dural arteriovenous fistulae: a contemporary singleinstitution series and meta-analysis. Cerebral cavernous hemangiomas or cavernomas: incidence, pathology, localization, diagnosis, clinical features and treatment. Intradural extramedullary spinal arterio-venous malformations fed by the anterior spinal artery. Successful treatment of a group of spinal cord arteriovenous malformations by interruption of dural fistula. Intraspinal extramedullary arteriovenous fistulae draining into the medullary veins. Vascular malformations of the spinal cord: intrathecal perimedullary arteriovenous fistulas fed by medullary arteries. Neurological Surgery: A Comprehensive Reference Guide to the Diagnosis and Management of Neurosurgical Problems. Spinal epidural vascular malformation presenting in association with a spontaneously resolved acute epidural hematoma. Paraplegia due to posttraumatic pelvic arteriovenous fistula treated by surgery and embolization.
Generic 400 mg viagra plus fast delivery
Although radiation changes in large arteries look very similar to the atherosclerotic changes seen in the carotid bulb in atherosclerotic vaso-occlusive disease erectile dysfunction specialist doctor purchase viagra plus canada, the spectrum of radiation stenosis is more varied. Cervical and cerebral angiography remains the "gold standard" for evaluating potential radiation stenosis. A patch graft arterial repair was necessary in 79% of the surgically treated patients. This is primarily because of concerns associated with soft tissue fibrosis, operating through an area of a previous myocutaneous flap, and more proximal arterial involvement. The long-term efficacy of stenting in this setting has yet to be analyzed, but the short-term results are promising. The 30-day postprocedure complication rate was 0 of 23 (0%), and no new neurological symptoms were reported. With a mean follow-up time of 28 months (range, 5 to 78 months), 15 of the 19 vessels (79%) developed no new stenosis, 2 of 19 (11%) had repeat angioplasty and stent placement, and 1 of 19 (5%) had a repeat angioplasty. In 2010, Dorresteijn and colleagues99 reported their outcomes of carotid artery stenting for radiation-induced stenosis. The restenosis rates were 17%, 33%, and 42% at 3, 12, and 24 months, respectively, but none of these patients developed symptoms. From the registry of the first 2001 patients, the investigators reported that patients with anatomic risk had a significantly lower rate of 30-day major adverse events than patients with physiologic risks (2. Anatomic dissection revealed that the structure was contained in a dense meshwork at the base of the carotid bifurcation. Believing that the structure was nerve tissue, he called it the "intercarotid ganglion. Years later, Kohn defined the carotid body as chromaffin cells embedded in the sympathetic nerve fibers around the carotid artery and coined the term paraganglion. The report detailed an aggressive tumor resection with division of the carotid artery; jugular vein; and vagus, hypoglossal, and sympathetic nerves. Treatment Some authors have reported that it is more difficult to dissect plaques caused by radiation stenosis than to dissect atherosclerotic plaques because the former are more adherent to the intima. Two thirds of the patients had severe scarring or fibrosis of the skin of the neck, and 4 patients had permanent tracheostomies. Complications were limited to two restenoses, two wound infections, and four cranial nerve palsies. These early attempts included ligation and resection of the carotid artery bifurcation, but no attempts at reconstruction. The tumor recurred at its original site within a year and required reexcision, as reported by Keen and Funke105 and Paltauf. By the 1960s and 1970s, several hundred cases of carotid body tumors had been reported, but the complication rates associated with surgical treatment were still high. The larger series reported mortality rates of 5% to 15% with surgical excision, cerebrovascular complications in 8% to 20% of patients, and postoperative cranial nerve injuries in 32% to 44% of patients. Photomicrograph of carotid body tumor showing the characteristic histologic clusters of cells known as Zellballen, composed of octahedral cells in a glomerulus-like shape. The vascular supply is from the carotid bifurcation, and the primary innervation is the carotid sensory branch of the glossopharyngeal nerve. Embryologically, the carotid body may have constituents of both the third branchial arch mesoderm and neural elements of the neural crest ectoderm. Tumors of these cells have also been known as paragangliomas, glomus tumors, and chemodectomas. Tumors of similar histology arise in several locations, including the ciliary body of the orbit, aortic-pulmonary paraganglia, carotid body (glomus caroticum), middle ear (glomus tympanicum), ganglion nodosum of the vagus nerve (glomus vagale), jugular body (glomus jugulare), and adrenal medulla (pheochromocytoma). Although most glomus tumors appear to be composed of nonchromaffin cells that are physiologically silent, some contain secretory granules that may secrete catecholamines similar to pheochromocytomas. In high-altitude populations, carotid body tumors show a marked female preponderance, as high as 12: 1,117 and even at sea level, the predominance of carotid body tumors in women is still apparent, at a ratio of 2: 1. An autosomal dominant expression of bilateral tumors, however, occurs in 32% of patients with a familial occurrence. Gardner and coworkers125 reviewed 11 patients with carotid body tumors, 3 of whom had other head and neck paragangliomas. Seminal genetic studies have indicated an increased expression of the oncogenes c-myc, bcl-2, and c-jun in most carotid body tumor specimens studied. Histology Carotid body tumors consist of epithelioid cells grouped into cords or clusters, also known as Zellballen. Several reports have detailed the chromaffin-positive nature of the secretory granules, indicating that the carotid body and tumors of it may be capable of secreting catecholamines such as norepinephrine and dopamine. Clinical Presentation Paragangliomas are slow-growing, benign tumors arising from chemoreceptors located in blood vessel walls. The most common location is at the carotid body, and the most common manifestation is a palpable neck mass in the high cervical region. Less common initial presentations include cranial nerve deficits such as laryngeal dysfunction (hoarseness), difficulty swallowing, and unilateral tongue atrophy or weakness. Typically, diagnosis is between 30 and 60 years of age, and the youngest reported patient was 7 years old. A, Coronal magnetic resonance imaging with gadolinium enhancement of carotid body tumors can help surgical planning by demonstrating the cervical level of the carotid bifurcation as well as the superior and inferior extent of the tumor. B, Preoperative magnetic resonance angiogram of the cervical vessels showing characteristic splaying of the external and internal carotid arteries near the carotid bifurcation in larger tumors. The ascending pharyngeal artery often provides most of the vascular supply, and the superior thyroid artery almost always provides a minority contribution. If angiography is planned, a concomitant session to embolize the tumor can be coordinated. Studies have shown that preoperative embolization significantly reduces blood loss during resection of a carotid body tumor. Clinicians must be aware of the potential comorbidity of a pheochromocytoma and that some carotid body tumors secrete catecholamines. In such patients, -adrenergic blockade must be induced pharmacologically 2 weeks before surgery. After this blockade is established, -adrenergic blockade is recommended to control heart rate and cardiac arrhythmias. Characteristics of Tumor Growth In an effort to assess the preoperative risks of tumor resection, Shamblin and associates136 revised a classification scheme for carotid body tumors. Digital subtraction angiography demonstrates a characteristic tumor blush at the carotid bifurcation. The carotid body tumor is typically fed by the ascending pharyngeal artery, with a smaller contribution from the superior thyroid artery. In this challenging group, the superior laryngeal and hypoglossal nerves may traverse the tumor. They are problematic only in their local invasion of vascular and nervous structures and, occasionally, the oropharynx. Distant metastases have been reported in lymph nodes, bone, lung, liver, pancreas, thyroid, kidney, brain, and breast. As mentioned, a thorough medical evaluation is necessary, particularly to rule out endocrine abnormalities. Tumor size is crucial to determine whether preoperative embolization is necessary. In general, small tumors (<2-3 cm) are good surgical candidates, and no preoperative embolization is needed. Superselective catheterization is usually needed when embolizing these lesions so as to selectively occlude abnormal vascular feeders while preserving normal blood flow through the carotid artery. In general, surgery should be done within 48 hours of the embolization procedure to avoid local soft tissue inflammatory response. Diagnostic cerebral angiography is also equally important for assessing collateral blood flow. In such cases, surgeons may anticipate intraoperative shunting to maintain adequate cerebral blood flow. For example, a small group I tumor may be accessed through a transverse incision along a cervical skin crease, giving the best cosmetic result. Here, an oblique incision along the medial border of the sternocleidomastoid muscle is indicated.
Cheap viagra plus 400 mg on line
The arteriovenous shunting vessels result in recruitment of arterial feeding vessels (sump effect) with secondary venous hypertension impotence juicing order viagra plus 400mg with amex. The estimated age- and sex-adjusted incidence from a population-based study was 0. The anterior fossa, tentorial incisura, sylvian and middle fossa, and sagittal sinus are less common locations. Thus, a six-vessel conventional arteriogram including external carotid injections remains the "gold standard. These fistulas are generally small or located near the occiput and are not associated with cortical venous drainage. The clinical behavior, including the initial findings, natural history, and prognosis, is a complex function of multiple factors, such as location, mode of venous drainage, and magnitude of flow. External carotid artery injection demonstrates early filling of the transverse-sigmoid dural sinus consistent with a dural arteriovenous fistula. For example, in a large meta-analysis, the annual hemorrhage rate in those without cortical venous drainage was 0%. Fistula multiplicity may also increase the risk for hemorrhage as the initial symptom, and hemorrhage was 3 times more likely in those with multiple fistulas in one study. These symptoms are often the result of increased dural venous drainage or venous hypertension. Presence of cortical venous drainage increases the risk for venous hypertension and potential for nonhemorrhagic neurological deficits that may be either focal (seizure, focal deficits) or diffuse (dementia, parkinsonism). PulsatileTinnitus Pulsatile tinnitus is the most common initial symptom and is frequently associated with high-flow fistulas in the transversesigmoid sinus location. Compression of the carotid artery and jugular vein or occipital artery may result in a reduction in bruit intensity and provide a clue to the diagnosis. Other mechanisms include brain edema secondary to venous hypertension, compression of the trigeminal nerve, and inflammation as a result of venous thrombosis. More worrisome causes of headaches include associated hemorrhage, hydrocephalus, or pseudotumor secondary to generalized venous hypertension. Hemorrhage Intraparenchymal hemorrhage, subarachnoid hemorrhage, and subdural hemorrhage may occur. Patients with retrograde cortical venous drainage have a higher likelihood of initially presenting with hemorrhage. Acute or gradual progression from one grade to the next has been documented, usually heralded by new neurological symptoms. Outcome Patients with cortical venous drainage are at higher risk for significant morbidity, whereas those without cortical venous drainage have a more benign course. In addition, proptosis or extraocular eye muscle enlargement may be visible on the image. Definitive diagnosis and characterization of the fistula (direct versus indirect; origin of feeders; evidence of cortical venous drainiage) is made by conventional arteriography, which should include injections250 of bilateral common, internal, and external carotid arteries. Patients with cortical venous drainage, visual loss, neurological symptoms, and significant pain often undergo treatment, and thus few natural history series exist. Because these lesions are congenital anomalies, the term developmental venous anomaly is preferred over venous angioma because the latter implies proliferation of abnormal vasculature. A variety of classifications can be used (hemodynamic flow, etiologic, or anatomic). Direct fistulas (Barrow type A) are those in which there is a rupture or tear in the carotid-cavernous segment leading to a direct connection between the internal carotid artery and the cavernous sinus. Symptoms of either type may include pulsatile tinnitus, proptosis, conjunctival vein arterialization, chemosis, retro-orbital pain, and ophthalmoplegia. These symptoms are related to venous hypertension and reduced venous drainage from the orbits. Over time, this can result in choroid and retinal detachment, central retinal venous thrombosis, and reduction in visual acuity. Jung and colleagues studied this finding using diffusion-weighted and perfusionweighted imaging and demonstrated it may represent vasogenic edema with congestion and delayed perfusion. During the venous phase, however, arcades of veins or caput medusae are visualized converging into a large venous channel. They are typically located at the junction of the superficial and deep venous systems. Previous studies have also shown an increased risk for hemorrhage with posterior fossa lesions294-297 and in association with pregnancy. These cases were also reported before 1985, and other pathology may not have been found because of the poorer resolution of imaging at that time. In another series, just 4 of 30 patients had persistent symptoms (2 with seizure, 1 with ataxia, and 1 with headache). No new hemorrhage or focal deficits developed in the 45-month follow-up in these patients. It is not clear whether a subset may exist that will require more aggressive treatment. FocalNeurologicalDeficits Rarely, venous anomalies may thrombose and result in infarction. No pathologic evidence of ischemic changes or microhemorrhages has been demonstrated. Definition Capillary telangiectases are vascular malformations composed of dilated capillaries with normal intervening neural tissue. Microscopically, they consist of ectatic individual vessels with thin capillary walls that course among normal architectural elements without adjacent gliosis or hemosiderin deposition. In addition, the authors believe this to be a high estimate of risk because of the nature of tertiary care referrals. A review of 27 cases from the literature revealed that 5 Etiology and Pathogenesis Controversy exists regarding the pathogenesis of capillary telangiectasia. It often appears as a brush-like area of enhancement, most commonly located in the pons. The "dot" is a more hyperintense area within the "spot" of the capillary telangiectasia that is likely the draining vein. Vague, nonspecific neurological symptoms often lead to the incidental discovery of capillary telangiectasia. In the largest single-center clinical series, Sayama and colleagues report on 105 definite capillary telangiectasia cases diagnosed radiologically. Of these, only two were symptomatic (both with seizures), and both had large (>1 cm) capillary telangiectases. Case reports of all types of neurological symptoms, including hemorrhage, seizures, cranial nerve palsies, extrapyramidal disorders, and focal hemispheric syndromes, have been described. A T1-weighted contrast magnetic resonance image demonstrates a faint blush in the pons consistent with a small capillary telangiectasia. The differential diagnosis of an enhancing lesion includes capillary telangiectasis, neoplasm, subacute infarction, and demyelinating or inflammatory disease. In addition, capillary telangiectasia is the only one in this group of pathologies that is composed of sacs of stagnant blood with deoxyhemoglobin and therefore exhibits susceptibility dephasing, which is evident only on gradient echo or susceptibility weighted images. Intracranially, they are most often solitary; however, multiple lesions have been described. They have been described in association with all types Natural History the risk for hemorrhage is assumed to be low; however, there are no large case series with extensive follow-up. In a study by Lee and colleagues, 18 patients were monitored over a mean of 23 months, with no reported bleeding or neurological deficits. Cerebral hemorrhage, cranial neuropathies, and increased intracranial pressure have all been described. Thus, presentation with myelopathy is common when the cutaneous lesion is on the body. Ipsilateral to the vascular malformation, the patient often demonstrates a port-wine stain (facial capillary malformation). The condition is progressive and also associated with immune deficiency and carries a risk for neoplasia. Typically, the diagnosis is made by clinical features, an elevated -fetoprotein level, low serum immunoglobulin levels, and genetic testing. Patients have capillary malformations on the surface of the skin of the face, arms, and legs that appear small, round, and often red. Outcome after spontaneous and arteriovenous malformation-related intracerebral haemorrhage: population-based studies.
Purchase viagra plus with amex
Surgical treatment of 127 anterior choroidal artery aneurysms: a cohort study of resultant ischemic complications erectile dysfunction vitamin buy viagra plus 400 mg fast delivery. The keyhole concept in aneurysm surgery-a comparative study: keyhole versus standard craniotomy. The A4 and A5 segments run over the body of the corpus callosum, with the transition between the two segments delineated arbitrarily at the level of the coronal suture. Duplication of the A1 segment, another rare but surgically important anatomic variant occurred in 2% of cases, and is unilateral. Unlike the A1 perforators, the majority (51%) terminate in the suprachiasmatic region, with only 15% reaching the anterior perforated substance. We have previously reviewed the anatomy and history of this artery, which was described by Johann Otto Leonhardt Heubner (1843-1926), a German pediatrician, in 1872. The artery of Heubner supplies the anterior striatum (caudate nucleus and putamen), a portion of the outer segment of the globus pallidus, and the anterior limb of the internal capsule. Injury also causes dysfunction of the tongue and palate, which can be documented only during a careful swallowing evaluation. In most patients, these deficits tend to resolve completely in a matter of months. Anatomy of the anterior circulation with the major branches and perforators of the internal carotid artery, of the M1 segment of the middle cerebral artery, of the A1 and A2 segments of the anterior cerebral artery, and of the anterior communicating artery. Most consider it the pericallosal artery, with the callosomarginal as a branch of the pericallosal, whereas others use the term to define one of the two branches at the bifurcation of the distal A1 segment, the other branch being the callosomarginal artery. The second definition leads to confusion when the callosomarginal artery is absent, as is the case 18% of the time, thus creating ambiguity as to where the pericallosal artery begins. It originates from the A2 segment in only 10% of cases and from the A4 segment in 12% of cases. These important branches supply the optic chiasm, anterior hypothalamus, medial portion of the anterior commissure, pillars of the fornix, and anterior-inferior portion of the striatum (caudate nucleus and putamen). Perlmutter and Rhoton5 reported a range of zero to four perforators in their study of 50 brains. Anatomy of the subfrontal gyri and sulci in relation to the course of the olfactory nerve. Superiorly, it reaches into the interhemispheric fissure, where it is bounded by the rostrum of the corpus callosum. Yaargil notes that the lateral boundary of the lamina terminalis cistern is a thickened band of arachnoid fibers that stretch between the area immediately medial to the olfactory nerve and the optic nerve. Importantly, the artery of Heubner and the orbitofrontal artery originate within the lamina terminalis cistern. When performing the arachnoid dissection, it is important to remember that the optic nerves and optic chiasm are not found in the lamina terminalis cistern, but in the chiasmatic cistern. Anterior communicating artery aneurysms originate within the lamina terminalis cistern. The A1 segment originates within the carotid cistern before coursing within the lamina terminalis cistern over either the optic chiasm (70% of the time) or the optic nerve (30% of the time). Therefore, a clear understanding of the anatomic boundaries of this cistern is important. This is probably so because the higher hydrodynamic pressures generated by the dominant A1 segment drive the growth of the aneurysm. By contrast, inferior-pointing aneurysms are the worst in this respect because elevation of the frontal lobes can avulse the dome from the optic chiasm, optic nerves, or the dura of the interoptic space early in the subarachnoid dissection. Anterior-pointing aneurysms have the most favorable orientation in relation to the hypothalamic and infundibular perforators, and posterior-pointing aneurysms have the worst orientation in this respect. For this reason, anterior-pointing aneurysms are usually easier to clip, and posteriorpointing ones are usually the most difficult. Brain relaxation is obtained with a Mannitol infusion, mild hyperventilation, drainage of the arachnoid cisterns, and fenestration of the lamina terminalis. Choice of the Side of the Craniotomy We approach the aneurysm from the side of the dominant A1 segment. Approaching the aneurysm from the side of the dominant A1 segment might not confer a significant advantage in terms of proximal control; however, it does offer the advantage of exposing the neck of the aneurysm before the dome. When the A1 segments are of equal diameter, we advocate a right (nondominant) craniotomy. This head position allows the frontal lobes to fall away from the skull base and facilitates the microsurgical exposure. However, this approach has the disadvantage of requiring early retraction of the ipsilateral frontal lobe, which can decompress the aneurysm dome before identification of the paired A2 segments. This incision is more aesthetic than one placed anteriorly along the edge of the hairline. Dissection of the Temporalis Muscle A subfascial dissection can be used as described by Yaargil and colleagues. This technique protects the frontal branch of the facial nerve, which runs along the surface of this superficial temporalis fascia. The incision is started a few millimeters anterior to the tragus at the upper border of the root of the zygoma and extended superiorly to the linea temporalis. At the linea temporalis, it is curved anteriorly to the midline, ending at the edge of the hairline. The anterior frontal bur hole should be approximately 2 cm off the midline in the midpupillary line and as low on the forehead as the skin flap allows. The keyhole bur hole should be positioned inferior to the linea temporalis and posterior to the frontozygomatic process to preserve the aesthetically important contours of these prominences. This stretch crosses the frontosphenoidal and the temporosphenoidal sutures and encompasses the lateral aspect of the greater wing of the sphenoid bone and the anterior-inferior portion of the squamous portion of the temporal bone, just superior to the root of the zygoma. The fourth bur hole is made below the linea temporalis slightly on the coronal plane of the temporal bur hole. The fifth posterior frontotemporal hole is placed equidistant from the two adjacent bur holes. After the bone flap is removed, the edge of the remaining temporosquamosal bone is removed with a Leksell rongeur starting above the root of the zygoma and proceeding anteriorly until the greater wing of the sphenoid is encountered. This bulky, pyramidal structure gradually leads to a more slender structure, which is the lesser wing of the sphenoid. This is drilled until the dural sleeve of the superior orbital fissure is reached. Removal of these bony structures allows for a tangential approach to the circle of Willis along the posterior curve of the lesser wing of the sphenoid. The orbital roof and inner table of the frontal bone are also drilled at this stage. It is important not to drill through the orbital roof into the periorbita because this technical error invariably results in a swollen, ecchymotic eye. If the frontal sinus is entered, it should be exenterated, packed with muscle, and sealed with fibrin glue. Before replacing the bone flap toward the end of the procedure, a pedicled galeal graft is reflected over the opening into the sinus, sutured to the dura, and pinched in place between the edges of the bone flap and frontal ledge. The dura is opened in a curvilinear fashion from the medial edge of the craniotomy in the frontal region to the lateral edge of the craniotomy in the temporal region and reflected anteriorly. Three sutures are then placed over the region of the sphenoid wing, the anterior fossa ledge, and the middle fossa ledge to retract the base of the dural flap, which otherwise may obstruct the view along the skull base. Sutures are placed over the region of the sphenoid wing, the anterior fossa ledge and the middle fossa ledge to retract the base of the dural flap, which would otherwise obstruct the view along the skull base. Freeing the anterior frontal lobe from the burden of the temporal lobe allows for easier retraction of the frontal lobe. The sylvian fissure is on average 6 cm long and can be divided into three 2-cm portions. Following opening of the fissure in its middle third for approximately 5 mm, the tip of a microirrigation device can be inserted into this opening to allow for insufflation of the cistern. The sylvian cistern consists of both a shallow superficial component and a more capacious deep component.