Buy aurogra 100mg overnight delivery
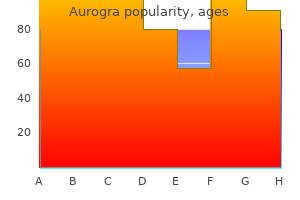
These groups of bers constitute the descending m otor pathways from the prim ary m otor cortex erectile dysfunction drug companies cheap 100mg aurogra with visa. The corticospinal bers pass to the m otor neurons in the anterior horn of the spinal cord, while the corticonuclear bers pass to the m otor nuclei of cranial nerves. Corticospinal bers: Only a sm all percentage of the axons of the corticospinal bers originate from the large pyram idal neurons in lam ina V of the precentral gyrus (the lam inar structure of the m otor cortex is shown in D). Eight y percent of the bers cross the midline at the level of the m edulla oblongata (decussation of the pyram ids) and descend in the spinal cord as the lateral corticospinal (pyramidal) tract. The uncrossed bers descend in the cord as the anterior corticospinal (pyramidal) tract and cross later at the segm ental level. Most of the axons term inate on intercalated cells whose synapses end on m otor neurons. Note: the basic pat tern of som atotopic organization described earlier at the spinal cord level is found at all levels of the pyram idal tract. Corticonuclear bers: the m otor nuclei and m otor segm ent s of the cranial nerves receive their axons from pyram idal cells in the facial region of the prem otor cortex. Besides this contralateral supply, axons also pass to several cranial nerve nuclei on the sam e (ipsilateral) side, resulting in a bilateral innervation pat tern (not shown here). This dual supply is clinically important in lesions of the facial nerve, for exam ple (upper versus lower face) (see D, p. Notes on the "pyram idal tract": Som e authors interpret this term as applying strictly to the portion of the tract below the decussation of the pyram ids, while other authors apply the term to the entire tract. Most publications, including this atlas, use "pyram idal tract" as a collective term for all of the ber tract s described here. Som e authors derive the term not from the decussation of the pyram ids but from the giant pyram idal cells (Bet z cells) in the cerebral cortex (see C and p. Functiona l Systems Anterior corticospinal tract Corticonuclear fibers B Somatotopic representation of the skeletal muscle in the precentral g yrus (motor homunculus) Anterior view. As a result, they require a larger representation area in the cortex than regions supplied by fewer neurons. This cortical representation is analogous to that in sensory innervation, where areas of varying size are also represented in the cortex (postcentral gyrus; compare with the sensory hom unculus in C, p. The axons for the head area are the corticonuclear bers, and the axons for the trunk and lim bs are the corticospinal bers. The lat ter bers split into t wo groups below the telencephalon, form ing the lateral and anterior corticospinal tract s. Besides the corticospinal and corticonuclear bers described above, a variet y of axons descends from the cortex to various sub cortical regions and into the spinal cord. The following subcortical regions also receive cortical e erent bers: the corpus striatum, thalam us, red nucleus, pontine nuclei, reticular form ation, inferior olive, dorsal colum n nuclei (these nuclear regions are described on p. The supraspinal e erent bers listed above consist partially of axon collaterals from pyram idal tract neurons and partially of separate axons. D Laminar structure of the motor cortex (= area 4 in the precentral g yrus) the axons from giant pyram idal cells (Bet z cells) in lam ina V account for only a sm all percentage (< 4%) of the axons that m ake up the corticospinal tract. In all, however, only about 40% of the axons of the pyram idal tract originate in area 4. The rem aining 60% com e from neurons in the supplem entary m otor elds and other cortical areas (see p. The basal nuclei (ganglia) are subcortical nuclei of the telen-cephalon that have a role in the planning and execution of m ovem ent s. They are the central relay station of the extrapyram idal m otor system and m ake up alm ost all the central gray m at ter of the cerebrum. The only other central gray-m at ter structure is the thalam us, which is prim arily sensory ("gateway to consciousness") and is involved only secondarily, through feedback m echanism s, in m otor sequences. In addition to these three nuclei, there are other nuclei that are considered functional component s of the m otor system (also shown here). In a strictly anatom ical sense, only the telencephalic structures listed above are constituent s of the basal nuclei (ganglia). Som e textbooks m istakenly include the subthalamic nucleus of the diencephalon (see p. Functional disturbances of the basal nuclei are characterized by m ovem ent disorders. Functiona l Systems Supplem entary m otor cortex Prim ary m otor cortex Som atosensory cortex Prem otor cortex Parietal lobe Cortical efferent fibers to brainstem and spinal cord Thalamus Centrom edian nucleus Ventral lateral nucleus Subthalam ic nucleus Putam en Globus pallidus, lateral segm ent Globus pallidus, m edial segm ent Compact part Reticular part Substantia nigra B Flow of information betw een motor cortical areas and basal gang lia: motor loop the basal ganglia are concerned with the controlled, purposeful execution of ne voluntary movements. They integrate information from the cortex and subcortical regions, which they process in parallel and then return to motor cortical areas via the thalam us (feedback). Neurons from the premotor, prim ary m otor, supplementary motor, and somatosensory cortex and from the parietal lobe send their axons to the putamen (see p. Initially, there is a direct (yellow) and indirect (green) pathway for relaying the inform ation out of the putamen. In the direct pathway (yellow), the neurons of the putamen project to the medial globus pallidus and to the reticular part of the substantia nigra. Both nuclei then return feedback signals to the motor thalamus, which projects back to motor areas of the cortex. The indirect pathway (green) leads from the putamen through the lateral globus pallidus and subthalamic nucleus to the medial globus pallidus, which then projects to the thalam us. An alternate indirect route leads from the subthalamic nucleus to the reticular part of the substantia nigra, which in turn projects to the thalamus. When inhibitory dopaminergic neurons in the compact part of the substantia nigra cease to function, the indirect pathway is suppressed and the direct pathway is no longer facilitated. Both e ects lead to the increased inhibition of thalamocortical neurons, resulting in decreased movements (hypokinetic disorder. Conversely, reduced activation of the internal part of the globus pallidus and the reticular part of the substantia nigra leads to increased activation of the thalamocortical neurons, resulting in abnorm al spontaneous movements (hyperkinetic disorder. Besides these long descending m otor tract s, the m otor neurons additionally receive sensory input (blue). All impulses in these pathways are integrated by the alpha m otor neuron and m odulate it s activit y, thereby a ecting m uscular contractions. The functional integrit y of the alpha m otor neuron is tested clinically by re ex testing. Because the face and hand are represented by particularly large areas in the m otor cortex (see B, p. The paralysis invariably a ect s the side opposite the lesion (due to decussation of the pyram ids) and is accid and partial (paresis) rather than com plete because the extrapyram idal bers are not dam aged. If the extrapyram idal bers were also dam aged, the result would be contralateral complete spastic paralysis (see below). Lesion at the level of the internal capsule (2): this leads to chronic, contralateral, spastic hem iplegia (com plete paralysis) because the lesion a ect s both the pyram idal tract and the extrapyram idal m otor pathways,* which m ix with pyram idal tract bers in front of the internal capsule. Lesion at the level of the cerebral peduncle (crus cerebri) (3): con-tralateral spastic hem iparesis. Lesion at the level of the pons (4): contralateral hem iparesis or bilateral paresis, depending on the size of the lesion. Because the bers of the pyram idal tract occupy a larger cross-sectional area in the pons than in the internal capsule, not all of the bers are dam aged in m any cases. For example, the bers for the facial nerve and hypoglossal nerve are usually una ected because of their dorsal location. Dam age to the ab - ducens nucleus m ay cause ipsilateral dam age to the trigem inal nucleus (not shown). Lesion at the level of the pyramid (5): Flaccid contralateral paresis occurs because the bers of the extrapyram idal m otor pathways. Lesion at the level of the spinal cord (6, 7): A lesion at the level of the cervical cord (6) leads to ipsilateral spastic hem iplegia because the bers of the pyram idal and extrapyram idal system are closely interwo ven at this level and have already crossed to the opposite side. A lesion at the level of the thoracic cord (7) leads to spastic paralysis of the ipsilateral leg. Lesion at the level of the peripheral nerve (8): this lesion dam ages the axon of the alpha m otor neuron, resulting in accid paralysis. This fact was unknown when pyramidal tract lesions were rst described, however, and it was assumed that a pyramidal tract lesion led to spastic paralysis. Because this fact has few practical implications, spasticit y is still described in some textbooks as the classic sign of a pyramidal tract lesion. In most cases it would be bet ter simply to regard spastic paralysis as a form of central paralysis.
Syndromes
- Hepatitis D
- Avocados
- Do not allow anyone to take a blood pressure reading on the same arm with the access.
- Sputum cultures and analysis
- Troponin T : 0–0.1 µg/L
- Complete blood count (CBC) to check for anemia
- Infection (a slight risk any time the skin is broken)
- High-risk pregnancy care (maternal-fetal medicine)
- Rash

Cheap aurogra 100mg
The virus was originally named Four Corners virus erectile dysfunction 60784 generic aurogra 100 mg with mastercard, referring to the region in the United States where it was found, where the states of Utah, Colorado, New Mexico, and Arizona are joined, but locals objected to the name, and it was renamed Sin nombre, Spanish for "no name. Sin nombre virus is really a virus of the deer mouse; it does not get transmitted from human to human. The virus is found in deer mice from many parts of North America, and sporadic cases of Hantavirus pulmonary syndrome occur throughout the range of the disease. It was first discovered in a hepatitis patient in Japan, in 1997, but there has never been any link to disease. The same virus or a closely related virus is found in primates and many other animals. In pigs it is transmitted from mother to offspring, and this is suspected but not proven in humans. Several surveys for Torque teno virus have been done in various human populations. However, there is a correlation between the amount of virus in an individual and the level of suppression of the immune system, with immunosuppressed people having higher virus loads. This may be useful as a marker of immunosuppression; for example, the immune system must be artificially suppressed by drugs in order for people to receive a donated organ, and Torque teno virus levels can be measured to monitor the effectiveness of the drugs. However, recently a number of viruses have been found that are beneficial to their hosts, and interest in looking at nonpathogenic viruses is beginning to increase. It is possible that in the future we may recognize the importance of the human virome (the collection of viruses in the body), just as we now recognize the importance of the microbiome, which usually refers to bacteria. There are a wide variety of animal viruses from each of the major classification groups (see Introduction). Some pet owners will be familiar with viruses such as Canine parvovirus, Feline leukemia virus, or Rabies virus, because their cats and dogs are vaccinated against these serious diseases. Some of the viruses in this section may be familiar to owners of exotic pets, such as snakes, and some will be known to anglers. Also included here are the viruses that affect livestock, such as Rinderpest virus, which devastated the cattle industry for centuries. In general these are not very well studied unless they cause diseases in animals that are considered important to humans, or they can spill over into domestic animals. This is partly because it is quite difficult to do these studies, but new technologies in determining the genetic code, or sequences of viruses and other entities, are changing our understanding. Recently bats have been studied from this perspective, and found to have an amazing array of viruses. Many viruses that are pathogenic in humans and other animals are found in bats without any apparent disease, although Rabies virus, perhaps the most famous bat virus, causes disease in bats as well as in everything else it is known to infect. In general many viruses in animals do not cause any known diseases, but become problems when they jump into novel species where the virus and the host are not adapted to each other. It became a problem when pigs were imported to Kenya after Rinderpest virus killed many cattle. In Kenya it is found in wild relatives of pigs, including warthogs and bushpigs, and bringing domestic pigs to Africa set up the opportunity for the virus to jump into a new species. It is often lethal in domestic pigs, with symptoms beginning with a fever and malaise, followed by loss of appetite, progressing to a hemorrhagic fever. The symptoms are the same as those seen with "classical swine fever," but this is caused by a different, unrelated virus. This is probably because these animals are the natural host of the virus, and the virus is well adapted to them. Unfortunately there is no treatment for the virus, and attempts to make a vaccine have not been successful. Although many different strains of the virus have been found, it is the only known virus in the genus and family. The particles are in various planes of cross-section with details of membrane and inner proteins clearly visible. Bluetongue is a serious disease of sheep, causing a variety of symptoms, but most notably a swollen, blue tongue. The virus can have a high rate of fatality in lambs, and some strains have a high mortality rate in adult sheep too. Climate change may be increasing spread Bluetongue was not found outside of Africa for many decades. This was followed by recognition of the disease in the United States in 1948, and in Spain and Portugal in the 1950s. Currently it is found in Australia, North and South America, southern Europe, Israel, and Southeast Asia. Comparing the virus genome sequence from different places shows that the isolates from one part of the world are all alike, but different from isolates from other parts of the world. This implies that the virus has been in these places for a long time, but was detected only recently. Bluetongue virus is limited by the range of the biting midges that transmit it, and this range may be expanding to higher latitudes with changes in climate. The disease caused neurological changes and anorexia, and most snakes died from secondary infections. Very specific changes, called inclusion bodies, were seen in cells of infected snakes, so the virus was named Boid inclusion body disease virus. The disease was clearly contagious, because entire colonies could be wiped out, but it was not clear that it was transmitted directly. A virus was suspected as the causative agent, and several viruses were isolated from affected snakes, but only recently has there been good evidence that a specific virus was really the cause of the disease. Boid inclusion body disease virus was isolated from cell cultures derived from affected snakes, and introduced to healthy snakes that developed disease, but it was not re-isolated in the snakes, although the entire process was completed in cell cultures. This is a rigorous standard, and one that is not always adhered to in modern microbiology. This image was made by a technique known as cryo-electron microscopy, where the virus is frozen in water. Although the viral nature of the disease was determined in about 1900, and the disease was studied throughout the nineteenth and twentieth centuries, the details of the virus were not known until the late twentieth century. The reason for variation of the incidence of this disease is not known, but it is likely that shrews are a wild reservoir of the virus, and changes in their populations, or in the exposure of domestic animals to shrews, may account for these fluctuations. Experimental infections in rats showed that the virus makes rodents more aggressive; they display biting behavior, which enhances the spread of the virus. An interesting feature of this virus infection is that disease does not occur in immune-compromised animals. There have been suggestions that the virus could be involved in some human neurological diseases but this is not proven, and recent evidence has largely debunked this idea. The first human genome sequence was completed in 2003 and many additional genomes have been completed since then. But sequences of Bornadisease virus are found in the human genome, and in the genomes of other primates, and of bats, elephants, fish, lemurs, and rodents. The disease can take very different forms depending on the strain of the virus and the age and route of infection, and serious disease is generally seen in young animals less than two years old. Mother to calf transmission keeps the virus in herds When cows are infected at certain stages of gestation the fetus may be aborted, but if it escapes abortion the calf will be infected without any symptoms at birth. The calf will go through its life shedding virus (that is, producing virus and releasing it) to infect other members of the herd, but will be somewhat tolerant of the virus. Infected calves generally have reduced growth, and are more susceptible to other diseases. Sometimes the calf develops the mucosal form of the disease, which is very severe and usually fatal, and includes severe diarrhea and ulcers and lesions on mucosal tissues. It is not clear how this happens, but there are mutations that occur in the virus that could make it more pathogenic, or it is possible that the calf becomes infected with a second, closely related form of the virus. The virus particles are the small red spherical features inside a cell structure known as the endoplasmic reticulum (shown in blue and red). There is a successful vaccine available, but it cannot be administered while the puppies are still nursing or for several weeks after weaning, because maternal antibodies will inactivate the vaccine. This means that there is a window of time when puppies are highly susceptible to getting the disease. Once a dog is infected the virus shedding begins before symptoms appear, and continues for a few days after recovery. Testing is important, and dog breeders must take great care to prevent Canine parvovirus in their facilities, and to use strict isolation procedures should they have a virus-positive dog. A virus from cats Canine parvovirus is almost identical to a cat virus, Feline panleukopenia virus, that has been known since the 1920s.
Purchase aurogra visa
If transfer was going to be delayed impotence antonym generic 100mg aurogra mastercard, or should I be so instructed, then I would proceed with an open reduction through a posterior approach. These images should then be discussed with a specialist in acetabular reconstruction. The fracture could then be exposed, reduced, and secured with lag screws and a posterior plate. If the wall fracture extends superiorly, then it is possible to increase the surgical exposure using a trochanteric osteotomy. What other surgical approaches for the treatment of acetabular fractures are you aware of Access to the anterior aspect can be gained through either an ilioinguinal approach or a Stoppa approach. The former utilizes an incision in the line of the inguinal ligament and provides three windows of access to the anterior column of the acetabulum. The Stoppa approach can be performed through a vertical midline or Pfannensteil incision and also provides access to the anterior column, although a fracture extending higher into the iliac wing may also require use of the outer window of the ilioinguinal approach. There are a number of other extensile approaches, such as the extended iliofemoral approach which allow simultaneous access to anterior and posterior elements. In situations where access to both anterior and posterior elements is required, it may be more appropriate to perform two separate approaches, either in one go or as a staged procedure. Fractures of the acetabulum: classification and surgical approaches for open reduction. These radiographs show an anteroposterior view of the hips and a lateral view of the left hip. The anteroposterior film shows a displaced intrascapsular fracture of the left neck of femur, this is supported by the appearance on the lateral view confirming the presence of a fracture with displacement and some posterior angulation of the femoral head. I would take a history and examine him, ensuring that the possibility of any other injuries had been ruled out. I would want to know his age and activity level, any comorbidities, and the mechanism of injury. The patient is a 45-year-old solicitor who sustained this injury whilst mountain biking. The majority of femoral neck fractures occur in the older population and are the result of lowenergy injuries. This is not the case in younger patients who are active and have fewer medical problems and better bone quality than their older counterparts. The goals of treatment are to preserve the femoral head and avoid arthroplasty if at all possible. I would therefore treat this patient with closed reduction, with the caveat that only an anatomical reduction is acceptable. The femoral head blood supply comes from three main sources: the medial femoral circumflex artery, the lateral femoral circumflex artery, and the obturator artery, although in adults the latter may have little to contribute. The lateral femoral circumflex artery gives off an ascending branch, the inferior metaphyseal artery, and supplies most of the inferoanterior aspect of the femoral head. The largest contributor to the blood supply is the lateral epiphyseal artery, which originates from the medial femoral circumflex artery and courses along the posterosuperior aspect of the femoral neck before supplying the femoral head. When consenting this patient for surgery what particular risks would you warn him about Can you quote the incidence of these complications and any literature to back this up A second prospective study performed by Loizou and Parker in 2009 looked at 1023 patients who had sustained an intracapsular fracture with subsequent internal fixation. The post-operative films show a fracture of the femoral neck not supported by the interlocking antegrade nail. As an isolated injury, the overlying soft tissue envelope and distal neurovascular status should be examined. A complete set of radiographs to include the ipsilateral hip and knee should be obtained, and the remainder of the limb examined for more distal injuries. Then traction should be applied to give temporary stability to the fracture and reduce blood loss and provide analgesia. Definitive treatment should occur promptly, and I would choose to stabilize this fracture with an antegrade reamed intramedullary nail. Assuming the patient is adequately resuscitated and prepared for theatre, I would set the patient up on a traction table, with the affected leg raised and the left leg scissored down to allow access by the image intensifier to both the hip and knee. Looking at the initial radiographs, my first operative concern would be reduction of the fracture, as the injury has led to wide displacement and there is the risk of soft tissue interposition. A Schanz pin could also be used to manipulate either fragment and could safely be inserted from the lateral side. If these techniques do not aid fracture reduction, I would open the fracture site and remove any interposed tissues. In certain situations, largely related to polytrauma, it might be wise to consider a damage control approach involving temporary stabilization of the bone with an external fixator, with a plan to convert this to definitive fixation at a later date. This decision depends on both the physiological status of the patient and the presence of concomitant injuries. In such cases the more prolonged surgery and physiological effects associated with instrumentation of the femoral canal for reamed nailing might prove an unwanted extra physiological hit to the patient and worsen their condition. I would consider alternatives to definitive reamed nailing in instances such as multiple long bone fractures, significant chest injury, and significant closed head injuries. Physiological parameters that might give an indication of the potential need for damage control surgery include serum lactate, which can be easily measured from venous samples on blood gas machines. In polytrauma patients with multiple injuries, I would consider a Damage Control Approach also. This could have been a missed injury from the initial presentation or it may have been a complication of the nailing procedure. The use of one or two implants to treat both fractures is controversial, but I would have chosen a two-implant approach. However, it is easier to apply traction to the femoral neck fracture and achieve a satisfactory reduction if the femoral shaft is one unit. Accuracy of reduction of ipsilateral femoral neck and shaft fractures-an analysis of various internal fixation strategies. Reamed versus nonreamed intramedullary nailing of lower extremity long bone fractures: a systematic overview and meta-analysis. Ipsilateral femoral shaft and neck fractures: are cephalomedullary nails appropriate The early management of patients with multiple injuries: an evidence-based, practical guide for the orthopaedic surgeon. Conversion of external fixation to intramedullary nailing for fractures of the shaft of the femur in multiply injured patients. Techniques of obtaining and maintaining reduction during nailing of femur fractures. How would your surgical technique change if you were treating this fracture in a 30-year-old motorcyclist These are anteroposterior and lateral views of a left knee showing a supracondylar fracture of the distal femur. In addition there is significant degenerative disease in the knee, and notable calcification in the popliteal vessels. Non-operative treatment would require prolonged immobilization of what is likely an already stiff joint, and in addition to the potential for medical complications there is also a risk that the fracture will continue to displace and potentially threaten the overlying soft tissue envelope. It would also be difficult to control the fracture because the arthrosis in the knee will make the joint stiff and there would be a tendency for any movement to preferentially occur at the fracture site, increasing the risk of both further fracture displacement and non-union. Broadly speaking, the surgical options here are internal fixation or primary replacement. If this knee had been relatively symptom free prior to the accident I would elect for fixation through a lateral approach with relative stability, using a periarticular locking plate in bridging mode in order to achieve union. However, if the knee had been symptomatic, it may be more appropriate to perform primary arthroplasty. Because of the position of the fracture, this would be likely to involve a distal femoral replacement with a constrained articulation such as a rotating hinge. Thus, this decision should involve a surgeon with the necessary expertise as well as an analysis of the physiological capacity of the patient to withstand this procedure.

Purchase aurogra 100 mg with amex
In general erectile dysfunction treatment by ayurveda purchase generic aurogra pills, the posterior interval slide is performed as an initial release, and improved excursion of 3 to 4 cm may be obtained. The traction stitches are retrieved through the anterior and posterior portals, respectively. An accessory lateral portal is established in line with the direction of the posterior interval. Tension is applied to the traction stitches, which will help direct the rotator cuff and separate the tendons as the release is performed. Arthroscopic view of a left shoulder through an accessory lateral portal, demonstrating the spine of the scapula, which is used as a landmark to direct the orientation of the posterior interval slide. Care is taken to lift the tips of the scissors away from the bony glenoid to protect the suprascapular nerve. If not previously performed, the capsule in now released under the supraspinatus and infraspinatus tendons, connecting the intra-articular release to the posterior interval slide. Excursion of the supraspinatus tendon and the infraspinatus tendons is then evaluated. If sufficient mobility is obtained to allow tendon repair to bone, then definitive fixation may proceed with standard suture anchor repair to bone. If there is still insufficient excursion, then further mobility may be obtained with an anterior interval slide. Step 5: the Anterior Interval Slide the anterior interval slide involves the release of the leading edge of the supraspinatus tendon from the rotator interval, coracohumeral ligament, and coracoid and subscapularis. Arthroscopic view of a left shoulder through the lateral portal, demonstrating the orientation of the anterior interval slide. The anterior slide is performed toward the base of the coracoid, which can be palpated anterior and medial to the root of the biceps tendon. To perform this release, the rotator cuff is viewed from a lateral or accessory lateral subacromial portal. A traction stitch is placed in the supraspinatus tendon and retrieved through the posterior or posterolateral portal. The base of the coracoid may be palpated as a bony prominence anterior and medial to the base of biceps root. An accessory lateral portal is established in line with the anterior interval toward the base of the coracoid. An arthroscopic scissor is introduced through the accessory lateral portal and the release is performed in line and toward the base of the coracoid. Tension on the traction stitch again will facilitate release and enhance visualization. The anterior release is complete when the bony prominence of the base of the coracoid is encountered. The intra-articular release may then be completed to connect with the anterior interval release. With the anterior interval release, increased excursion of 1 to 2 cm of the supraspinatus is anticipated. Postoperative Protocol the postoperative protocol following rotator cuff repair is individualized and based on the size of the tear and the security of the repair. A more conservative rehabilitation approach is used in massive tears, which require extensive mobilization and releases. Alternatively, a more aggressive rehabilitation program may be utilized in smaller tears treated in the presence of adhesive capsulitis, where the risk of postoperative stiffness is significant. Passive external rotation with the arm at the side is permitted immediately postoperatively and as tolerated. Forward elevation is initiated approximately 6 weeks postoperatively, progressing from passive to active assisted to active forward elevation. Strengthening begins 12 to 14 weeks postoperatively, progressing to functional activities and sport-specific activities 6 to 8 months postoperatively. Potential Complications Complications related to releases are essentially similar to complications related to arthroscopic rotator cuff repair. However, specifically related to mobilization techniques, the suprascapular nerve is at risk, particularly when performing intra-articular releases or interval slides (ie, posterior interval slide). Therefore, extreme care is taken to ensure that the instruments do not penetrate beyond 1. Arthroscopic Rotator Cuff Mobilization Techniques 69 Top Technical Pearls for the Procedure 1. This will improve your orientation in the subacromial space and serve as a landmark for the interval between supraspinatus and infraspinatus tendons. After delineating the tear margins, take time to assess the natural mobility of the rotator cuff tendon to determine whether a tension-free repair may be obtained to bone. Traction stitches will improve the ease of performing the release, improve visualization, and help orient the direction of the release. The posterior interval slide provides the most mobility of all of the individual releases and improves mobility of both the supraspinatus and infraspinatus tendons. The suprascapular nerve may be at risk when performing the posterior interval slide or intra-articular release. Care is taken when performing these slides to ensure instruments are kept as lateral and superior as possible to the bony glenoid. Releases are immediately stopped when the fibrofatty tissue (in the case of the posterior interval slide) or the muscle belly (in the case of the intra-articular release) is identified. Arthroscopic repair of massive, contracted, immobile rotator cuff tears using single and double interval slides: technique and preliminary results. Identification of essential anatomic landmarks in performing arthroscopic single- and double-interval slides. The shoulder-specifically the acromion-strikes the ground first and is driven inferiorly, separating the distal clavicle from its scapular connections. The clinical manifestation of the acute injury is pain, limited shoulder function, and a prominence over the lateral shoulder representing the superiorly displace distal clavicle. Most of the procedures entail transfixing the distal clavicle to either the acromion or the coracoid. Plates, screws, wires, sutures, and tape have all been proposed to stabilize this injury. Standard shoulder arthroscopic equipment is utilized in conjunction with commercially available fixation buttons that allows for fixation of the displaced clavicle to the coracoid. The acute operative stabilization defined for this technique is within 2 weeks from injury. Conditions that may preclude any surgery (ie, bleeding disorders, irreversible blood thinning agents such as Plavix [clopidogrel], and any systemic condition precluding any operation) Arthroscopic Acromioclavicular Joint Repair for Acute Injury 73 Patients not able to tolerate general anesthesia as it is typically utilized for this operation. Although this procedure can be performed under a regional interscalene block alone, the superior shoulder and clavicle are poorly covered with a regional block and would have to be supplemented with local anesthesia. Delayed presentation: It is paramount that this procedure be performed acutely and as soon after the injury as is feasible. The classic presentation is severe pain localized to the top of the shoulder following a fall or athletic injury. Skin integrity is important to first ascertain whether the injury is open, and second to assess for abrasions, which are common given the mechanism of injury. Abrasions and lacerations over the area of expected skin incisions may necessitate a delay in operative treatment. Tenting of the skin may indicate disruption of the trapezial fascia and further support the diagnosis of a type V injury. Traction or direct injury may manifest as neurological deficit in the ipsilateral upper extremity. Alternatively, a type V injury has also been defined as greater than 2 cm of absolute superior displacement of the clavicle. The surgeon should be familiar with routine shoulder arthroscopy, instrumentation, and labral repair. Standard arthroscopy is first performed, but both the posterior entry portal and the anterior portals should be made slightly more lateral than usual to visualize and to allow easier access to the base of the coracoid. The shoulder joint should first be examined arthroscopically for concomitant pathology. Step-by-Step Description of the Procedure the patient is positioned in either a beach chair or lateral decubitus position. The authors prefer a commercially available beach chair positioner that allows easy access to the posterior shoulder for arthroscopy.
Aurogra 100mg sale
The toxin is a serious problem for humans impotence heart disease buy aurogra 100 mg cheap, but it is an advantage to the bacteria, because it allows it to invade the human gut, and provides a means of passing the bacteria on to water supplies in huge numbers through diarrhea, where it can infect further hosts. Thus the virus is really a beneficial virus for its bacterial host, although it makes a deadly contribution to the spread of cholera. W, Phage and the Origins of Molecular Biology, Centennial edition (Cold Spring Harbor Laboratory Press, 2007) C,C H. Moe, Hiro Morimoto, Peter Nagy, Glen Nemerow, Don Nuss, Hiroaki Okamoto, Toshihiro Omura, Ann Palmenberg, Maria-Louise Penrith, Julie Pfeiffer, Welkin Pope, David Prangishvili, Eugene V. Ikbal Agah Ince, Acibadem University, School of Medicine, Dept of Medical Microbiology, Istanbul, Turkey: 194. Harold Fisher/Visuals Unlimited, Inc: 228; Steve Gschmeissner: 18R; Kwangshin Kim: 66; Mehau Kulyk: 216; London School of Hygiene & Tropical Medicine: 54; Moredun Animal Health Ltd: 109; Dr. Every effort has been made to trace copyright holders and obtain their permission for use of copyright material. The publisher apologizes for any errors or omissions in the list above and will gratefully incorporate any corrections in future reprints if notified. Picture credits the publisher would like to thank the following for permission to reproduce copyright material: Courtesy Dwight Anderson. From Structure of Bacillus subtilis Bacteriophage phi29 and the Length of phi29 Deoxyribonucleic Acid. Surgeons must understand basic knot-tying principles in order to create the strongest possible arthroscopic repair. The overall strength of a surgical repair construct, either arthroscopic or open, is defined by the "weakest link" in the chain. In many cases, the biomechanical weak link is the suture knot, as opposed to the suture material, suture anchor, or biological tissue being repaired. Although "super sutures" decrease the risk of intraoperative suture breakage, high tensile load to failure does not guarantee a secure surgical knot. Surgeons must be diligent and use meticulous operative technique in order to maximize the quality and consistency of arthroscopic knots. Bench-top practice and objective performance feedback can enhance overall proficiency, even for the most experienced surgeon. Indications Most arthroscopic shoulder repair procedures utilize knot-tying skills. It is useful to first consider the primary objective, which is secure apposition that holds tissues in proper position until biologic healing can be achieved. In the absence of healing, all suture constructs will eventually fail under the influence of cyclic load. Foremost, how much "gap" can be tolerated during the healing process since sutures loosen under the influence of postoperative cyclic loads For example, after an arthroscopic rotator cuff repair, can the local tissues tolerate a small gap between tendon and bone and still achieve successful healing of the cuff Is the critical gap affected by patient age, systemic disease, or local degeneration (eg, tendinosis) Should the same threshold apply to suture loops that are tied for tissue-to-tissue repair such as capsular plication to treat multidirectional shoulder instability or side-to-side repair of large rotator cuff ruptures At this time, there are no definitive scientific answers to some of these basic questions. However, consider the critical threshold to be less than 3 mm of gap formation to facilitate optimal tissue healing, at least for rotator cuff repair. A 3-mm threshold is a reasonable standard as surgeons practice and test knots in vitro, even though it is an oversimplification to apply the same threshold for all repair conditions. Tendon-to-bone healing and soft tissue-to-soft tissue healing usually take somewhere between 6 and 12 weeks to achieve a decent modicum of strength at the repair site (under normal physiologic conditions). With a modest estimate of hundreds of loading cycles per day, repair constructs are expected to be subjected to thousands of loading cycles during the healing process. Postoperative gap formation can interfere with healing at the tissue-bone interface. The next logical question pertains to the in vivo loads experienced by arthroscopic repair constructs after surgery. This is a very difficult question to answer since there are little to no biomechanical data from direct postoperative measurement. Loads at the tendon-bone interface after rotator cuff repair are greater with muscle activation compared to passive motion. Local tissue loads would be extremely high during a sudden accidental event, such as a fall, which can cause catastrophic failure of the repair construct. Based on biomechanical modeling,1 it is estimated that the force applied via the suture to cuff might be as high as 60 N per suture for an idealized 4-cm long rotator cuff tear (assuming a maximal supraspinatus muscle force of about 300 N and a 3-anchor/3-suture repair). Additional sutures should decrease the load per suture assuming uniform load sharing for all sutures. However, this condition is probably not met in vivo, where it is extremely difficult to achieve a perfectly balanced repair. It seems logical that the "tightest" suture loop would see the greatest initial load, with load transferred to the next tightest loop upon loosening or failure of the first loop. Peak suture-tissue forces are decreased by use of multiple sutures that distribute load evenly to multiple points of tissue fixation. In addition to requiring increased surgical time, those may include local tissue devascularization (which could interfere with healing), excessive bulk (ie, within the joint or in the subacromial space), and tangling of sutures to be tied in relatively tight spaces. Loads in the neighborhood of 300 N would be unusual under most postoperative conditions. However, failure of an arthroscopic knot (defined as greater than or equal to 3 mm of loop expansion) can occur at much lower loads, under the influence of repetitive cyclic loads. In some cases, the tissue itself is the "weakest link" of the repair construct, but tissue quality is a variable that the surgeon cannot control before or during surgery. Some surgeons prefer a larger distal hole in the pusher, which allows for deliberate passage over the knot. Double-holed knot pushers and self-tensioning suture devices are also available, but these have largely fallen out of favor. Some knot pushers are open-sided, which allows for engagement of the suture limbs within the joint or within the cannula. These knot pushers tend to disengage from the suture limb (which can be a nuisance), and they can occasionally score or fret the suture (which weakens it). Some surgeons prefer to use a "sixth-finger" design, which allows for persistent tension on the knot while half-hitches are delivered, using one instrument to accomplish both tasks. As with everything, there is a learning curve for this device, and practice is required to master the skill. Controversy remains about whether it is essential to switch the knot pusher from one limb to the other during delivery of reversed hitches on alternating posts. Some surgeons are comfortable flipping posts on sequential throws without changing the knot pusher, simply by preferential pull on one suture strand or the other. Some surgeons prefer to physically swap the knot pusher from one limb to the other, which adds a bit of time to the procedure. This approach facilitates selection of the best technique by each individual surgeon. In general, arthroscopic knots should always be delivered down an arthroscopic cannula. Violation of this principle can result in substantial frustration and sometimes technical failure because sutures can encircle nontarget tissues during knot delivery. It is a very good idea to remove all sutures, other than the 2 strands that are being tied, which usually requires use of a loop grasper or crochet hook to deliver sutures out another portal or cannula. It is easy for sutures to become tangled with one another within the cannula during knot tying and, once they become entangled, it can be extremely difficult to correct.
SPV 30 (Boxwood). Aurogra.
- How does Boxwood work?
- What is Boxwood?
- Are there safety concerns?
- Treating HIV/AIDS, stimulating the immune system, arthritis, detoxifying the blood, and other uses.
- Dosing considerations for Boxwood.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96339

Discount 100mg aurogra otc
Step-by-Step Description of the Procedure A small stab incision is made approximately 3 cm medial to the inferomedial angle and a 30-degree arthroscope is inserted erectile dysfunction therapy treatment aurogra 100mg visa, taking care to remain as parallel to the chest wall as possible. Care should be taken to maintain a fluid pump pressure of less than 50 mm Hg throughout the procedure to avoid excessive fluid extravasation into surrounding tissues. A spinal needle is inserted approximately 3 cm medial to the medial scapular border at a point just inferior to the level of the scapular spine, marking the location of the medial working portal. Once this portal is established, diagnostic arthroscopy is performed using both the 30- and 70-degree arthroscopes to accurately localize the superomedial scapular angle. Using the previously placed spinal needle for orientation, debridement is continued until the superomedial scapular angle is completely exposed. When necessary, access to the supraserratus bursa can be achieved by bluntly penetrating the laterally positioned serratus anterior muscle. If mechanical crepitus is still present and skeletal impingement is still visible following complete bursectomy, superomedial angle resection is then performed. Note that a triangular section of the superomedial scapular angle has previously been resected (arrow). Although a triangular section of bone is typically removed approximately 2 cm superoinferiorly and 3 cm mediolaterally, it is important to mark the extent of the planned resection in every case using several spinal needles, depending on the degree and location of scapulothoracic impingement. This method facilitates complete, accurate bony resection of the superomedial angle without increasing the risk to nearby vascular structures. The operative extremity is again placed through a range of motion while directly visualizing the scapulothoracic space through both portals to confirm both adequate resection and the presence of a smooth articulating surface. The portal sites are closed using a standard technique, a simple sling is applied, and the patient is transferred to the post-anesthesia care unit. Because the scapulothoracic articulation is not surrounded by a joint capsule, some patients may experience significant swelling that can extend down the arm or around the torso within the immediate postoperative period; however, this side effect typically resolves over a period of days. Arthroscopic Bursectomy and Superomedial Angle Resection 283 Postoperative Protocol Active and passive range of motion exercises, such as scapular protraction, retraction, and rotation, are begun immediately postoperatively with a progression toward glenohumeral strengthening at approximately 4 weeks followed by periscapular strengthening at approximately 8 weeks. Most patients return to sports after 3 months of structured and supervised rehabilitation. In all cases, physical therapy protocols should be individualized according to patient tolerance and progress. Potential Complications Although uncommon, there are several important surgical complications unique to this procedure that can be prevented by using appropriate arthroscopic techniques. Injury to the dorsal scapular artery and/or nerve can occur when arthroscopic portals are placed < 3 cm medial to the medial scapular border. The spinal accessory nerve is also in danger when an arthroscopic portal is placed superior to the level of the scapular spine. Puncture of pleural tissue can be avoided by maintaining the arthroscopic instruments at an angle that is approximately parallel with the thoracic cage. Placing the operative limb in the "chicken wing" position increases the potential space between the scapula and the posterior chest wall, which improves arthroscopic visualization. Always establish arthroscopic portals at least 3 cm medial to the medial scapular border and inferior to the level of the scapular spine to prevent injury to important neurovascular structures, such as the dorsal scapular nerve and artery and the spinal accessory nerve. Always use spinal needles to facilitate arthroscopic orientation to avoid excessive bony resection and to prevent neurovascular injuries as a result of excessive superior or lateral dissection. To avoid becoming "lost" in the subscapularis and serratus anterior muscle bellies, it is important to ensure that the arthroscope is advanced down to the posterior thorax. Avoid resection of red muscle fibers, such as those of the subscapularis, as this may produce increased postoperative pain and lengthen rehabilitation. Variable osseous anatomy of costal surface of scapula and its implications in relation to snapping scapula syndrome. The operative treatment of scapulothoracic bursitis in professional baseball pitchers. Scapulothoracic bursitis and snapping scapula syndrome: a critical review of current evidence. Technique and outcomes of arthroscopic scapulothoracic bursectomy and partial scapulectomy. Functional outcomes after arthroscopic scapulothoracic bursectomy and partial superomedial angle scapulectomy. Arthroscopic partial resection of the scapula for snapping scapula: a new technique. Safe zone for arthroscopic resection of the superomedial scapular border in the treatment of snapping scapular syndrome. The senior author described that successful treatment combined anterior and superior labral lesions in 1994. Ricchetti et al reported similar findings in 44 patients who had undergone a panlabral repair. The authors highlight the surgical indications, physical findings, pertinent preoperative imaging, technique, postoperative protocol, and common complications. An excellent surgical result can be achieved if the principles outlined in this chapter are followed. This is especially true when patient guarding is present, which is common in acute, traumatic injuries. Most patients present after several unidirectional dislocations, have positive provocative instability tests in all directions, and have significantly more pain for longer periods of time than patients with focal labral tears. Anterior instability: the anterior apprehension and relocation tests are accurate methods to assess anterior labral pathology. These are often performed best with the patient supine and the scapula stabilized. Patients are often more tolerant of posterior instability testing than anterior instability testing. Most shoulders have a moderate amount of physiologic laxity, so it is useful to examine the contralateral shoulder in order to delineate discrepancies between sides in regard to pain and laxity with posterior instability testing. Ligamentous laxity should be assessed and compared with the contralateral shoulder to delineate benign laxity from instability. Range of motion and rotator cuff strength must be assessed to rule out concomitant pathology. Patients with scapular dyskinesia and winging commonly present with complaints of an unstable shoulder,15 and it is essential to confirm that the periscapular muscles are functioning appropriately. Pertinent Imaging Grashey anteroposterior, scapular Y, and axillary lateral radiographic views are utilized in the initial assessment of most patients with shoulder pain. A Hill-Sachs lesion can often be accentuated on an internal rotation Grashey anteroposterior, and an osseous Bankart lesion or anterior glenoid erosion can be visualized on an axillary lateral in patients with a history of traumatic anterior instability. Alternatively, in patients with a history of anterior glenohumeral instability, a Stryker notch view can be utilized to screen for a Hill-Sachs lesion, and a West Point view can be utilized to screen for an osseous Bankart lesion or glenoid deficiency. A standard 30-degree arthroscope is all that is required if the trans-cuff portal is utilized, which provides excellent visualization of all aspects of the labrum. Seventy-degree cameras are useful when performing labral repairs without the use of this portal. A variety of commercially available tissue elevators are available to free the labrum and prepare the glenoid surface. The authors utilized a radiofrequency blade device (CoVator [Arthrocare]) in order to thoroughly free the labrum and capsule to perform an anatomic repair. Many glenoid-specific suture anchors can be utilized to perform a panlabral repair that usually range from 2. The authors use an average of 5 double-loaded anchors for panlabral repairs (2 posterior, 2 anterior, and 1 superior). Patient anatomy and portal location dictates the optimal device geometry in order to pass the suture, so select the device that allows the optimal angle of attach. This is often a curved device between 45 and 90 degrees for anterior repairs and a straight device for posterior repairs. Positioning and Portals A panlabral repair can be performed in both the beach chair and lateral decubitus position. It is paramount to identify and pad all bony prominences and areas of potential nerve compression during the procedure. Specifically, the brachial plexus and the common peroneal nerve are at risk of compression during procedures performed in the lateral decubitus position.
100 mg aurogra with mastercard
The surface of hem ispheres and verm is shows furrow-like depressions erectile dysfunction causes pdf aurogra 100mg fast delivery, the ssures, which separate the very thin folia from one another. Fissures and folia of the cerebellum correspond to the sulci and gyri of the telencephalon. The occulonodular lobe (b) one of the m ain subdivisions of the cerebellum, is located inferiorly and consists of the paired occuli, their peduncles, and the nodule of the vermis. All tract s to and from the cerebellum pass through the three paired cerebellar peduncles. Mesencephalon Metencephalon Brainstem Pons Cerebellum Medulla oblongata Rhom bencephalon F Cerebellum and brainstem: Terminolog ical peculiarities Topographically, the cerebellum is not part of the brainstem, yet phylogenetically is derived from it. The com bination of pons, cerebellum and m edulla oblongata, the structures which surround the diam ondshaped fourth ventricle, is called the hindbrain or rhom bencephalon. The three-dim ensional representation (b) shows that the term "horn" is used to describe the threedim ensional nature of the anterior, posterior, and lateral colum ns of gray m at ter. At the central core of gray m at ter lies part of the ventricular system, the central canal of the spinal cord. Occasionally, anterior and lateral funiculi are collectively called the anterolateral funiculus. The spinal cord lies within the vertebral canal, which is form ed by the vertebral foram en of all the vertebrae stacked on top of one another and the ligam ents of the vertebral colum n traversing the vertebrae. From there, only certain parts of the spinal cord, the root s, extend further caudally. The spinal nerve prim arily divides into a posterior ram us (B) and an anterior ram us (D). From this motor neuron originates the motor root of a nerve, which extends to the skeletal muscle; b displays a sensory pathway, which runs within the anterolateral system of the spinal cord. It com es from the skin and extends to the (som atosensory) cerebral cortex passing through interm ediate regions (m ainly the thalam us in the diencephalon). The rst neuron of this tract lies in the spinal ganglion and is therefore a neuron of the peripheral nervous system. For this purpose, the spinal cord contains intersegm ental bers (lateral proper fasciculi, not shown here) located in the white m at ter, which are responsible for relaying inform ation within the spinal cord without exiting it. These are intersegm ental bers which arise from cells in the gray m at ter, and, after a longer or shorter course, reenter the gray m at ter and ram ify in it. In term s of their function, the tract s running through the spinal cord are called extrinsic apparatus and the intersegm ental bers intrinsic apparatus. Knowledge of location, course and function of tract s of the spinal cord is essential for understanding clinical symptom s in case of injuries to , or diseases of, the spinal cord. The necessary blood supply is ensured by t wo paired arteries (a): the larger internal carotid a. At the base of the brain- within the subarachnoid space- the branches of these four arteries m erge to form a vascular ring, the arterial circle (of Willis) (b): the arterial circle gives o branches that supply the brain. Note that the arterial circle is essentially fed by 3 m ain vessels- lt/rt internal carothe tid aa. The blood supply from these three sources is connected by posterior and anterior com m unicating aa. In case of im paired circulation, the m erging of these arteries in a vascular ring, to a certain extent allows for compensation of decreased blood ow in one vessel with increased blood ow through another vessel. B Arterial supply to the spinal cord a schem atic representation of blood supply to the spinal cord; b cross section of spinal cord, left lateral and superior view. The great length of the spinal cord, which lies within the narrow vertebral canal, poses signi cant logistical problem s with regard to blood supply. From cranial to caudal direction (due to the decreasing lling pressure in this direction by the vertebral a. These dural venous sinuses are form ed by separation of the t wo layers of dura generally unseparable except in these regions. Unlike true veins, there is no m uscle tissue found in the walls of these venous sinuses, the dura is lined internally by only a layer of endothelium. Deep cerebral veins (not visible here) collect the blood from deeper brain regions and take it to the dural venous sinus system. The dural venous sinus system delivers the collected blood m ainly to the internal jugular v. In a sim ilar fashion to the the true veins of the head, the dural sinuses do not have valves. Blood can ow in either direction exclusively controlled by the existing pressure gradient. Note: Dural venous sinuses are found only in the brain and not in the spinal cord, even though dura also exists in the spinal cord. The connection bet ween the dural venous sinus system and true veins out side the skull allow bacteria to enter the skull from outside even without injury to the bone or the m eninges (see p. D Venous drainage of the spinal cord a cross section of the spinal cord, left, anterior and superior view; b anterior view of the vertebral canal which has been opened and the spinal cord. The venous blood of the spinal cord is collected by the anterior and posterior spinal vv. Unlike the brain in the skull, there is no dural venous sinus system surrounding the spinal cord within the vertebral canal. Note: the complex venous system of the vertebral venous plexus contains m any m ore veins than what would be required for routine blood drainage supporting spinal cord m etabolism. This plexus system serves an additional function acting as a pressure equalizer in the vertebral canal. By m oving large am ounts of blood bet ween internal and external vertebral venous plexuses (both of which have no valves), uctuations in blood pressure in the vertebral canal can be accom m odated (see B and C, p. The com m on visceral sensation- the processing of stim uli from viscera inside the body (interoception)- explained on p. This distinction is important because the location and t ype determ ines the pathway via which the som atic signals are transm it ted. Although proprioception is a form of m echanoreception, it is not further di erentiated. Both exteroception and proprioception is conveyed via spinal nerves (inform ation from torso, neck, lim bs) or in the case of the head, the trigem inal n. Perception through the sensory organs is ultim ately a form of exteroception (red) and therefore a form of som atic sensation. However, for phylogenic reasons, not all sensory organs and their perception is referred to as som atic sensation. Regarding the sensory organs, chem ical stim uli (taste, sm ell) and electrom agnetic waves (optics) in addition to m echanic stim uli (acoustics) play a role. For a is sensory stim ulus to reach consciousness (conscious sensation), it has to reach the sensory cortex of the telencephalon. In addition to location and t ype of stim ulus, the nal destination of the signal transm ission can be distinguished in sensory stim uli. Analogous to som atom otor function, speci c term s for speci c sensory perceptions are used to describe som atic sensation. For signals that are relayed to the cerebellum, by only three neurons, the third neuron lies in the cerebellar cortex. Pain, temperature, and crude m echanoreception (pressure) of the skin and m ucosae are transm it ted in the spinal cord via the sensory spinothalam ic tract. Subtle m echanoreception (vibration, light touch) is transm it ted in the spinal cord via the dorsal colum n (fasciculus gracilis and cuneatus). Thus, a stim ulus in the left arm will pass through the thalam us and be relayed to , and received by, the right cerebral cortex. First and second neurons lie in the spinal ganglion or in the spinal cord; the axon of the second neuron reaches a third neuron in the cerebellar cortex. Note: To a lesser extent, proprioceptive impulses can also be relayed to the cerebral cortex to perceive positional sense via the dorsal colum n: Epicrisis (as part of exteroception) and proprioception run parallel in the sam e tract, but term inate at di erent nuclei. A cranial or spinal nerve transm its the signal from the respective sensory receptor.
Buy generic aurogra 100mg on-line
The arrangem ent of the bers shows that the speci c thalam ic nuclei have connections with all areas of the cortex erectile dysfunction drugs generic order 100mg aurogra with amex. The anterior thalam ic radiation projects to the frontal lobe, the central thalam ic radiation to the parietal lobe, the posterior thalam ic radiation to the occipital lobe, and the inferior thalam ic radiation to the temporal lobe. It contains sensory bers for position sense, vibration, pressure, discrim ination, and touch that are relayed from the nucleus gracilis and nucleus cuneatus. The anterior nucleus establishes both a erent and e erent connections with the cingulate gyrus of the telencephalon. The largest nonspeci c thalam ic nucleus is the centrom edian nucleus, which is one of the intralam inar nuclei. It receives a erent f bers from the cerebellum, reticular form ation, and m edial pallidus. Head of caudate nucleus Globus pallidus, m edial segm ent Globus pallidus, lateral segm ent Putam en Centrom edian nucleus Em boliform nucleus of cerebellum Mam m illary body Reticular form ation of brainstem Mam m illothalam ic fasciculus 336 Neuroanatomy 14. Diencepha lon Ventral lateral nucleus Lateral posterior nucleus Globus pallidus, m edial segm ent Globus pallidus, lateral segm ent Lateral dorsal nucleus Dorsal m edial nucleus Putam en Medial geniculate body Hypothalam us (afferent) Lateral geniculate body C Medial, posterior, and lateral thalamic nuclei: a erent and e erent connections the medial thalamic nuclei receive their a erent input from ventral and intralam inar thalam ic nuclei (not shown), the hypothalam us, the m esencephalon, and the globus/pallidus. Their e erent bers project to the frontal lobe and prem otor cortex, and a erent bers from these regions return to the nuclei. The destruction of these tract s leads to frontal lobe syndrome, which is characterized by a loss of self-control (episodes of childish jocularit y alternating with suspicion and petulance). The posterior nuclei are form ed by the pulvinar, which is the largest nuclear complex of the thalam us. The pulvinar receives a erent bers from other thalam ic nuclei, particularly the intralam inar nuclei (not shown). Its e erent bers term inate in the association areas of the parietal and occipital lobes, which have reciprocal connections with the pulvinar. The lateral geniculate body (part of the visual pathway) project s to the visual cortex, while the m edial geniculate body (part of the auditory pathway) project s to the auditory cortex. The lateral nuclei consist of the lateral dorsal nucleus and lateral posterior nucleus. They represent the dorsal portion of the ventrolateral group and receive their input from other thalam ic nuclei (hence the term "integration nuclei," see p. D Synopsis of some clinically important connections of the speci c thalamic nuclei the speci c thalam ic nuclei project to the cerebral cortex. The table below lists the origins of the tracts that term inate in the nuclei, the nuclei them selves, and the sites to which their a erent bers project. The hypothalam us is the lowest level of the diencephalon, situated below the thalam us. The hypothalam us is a sm all nuclear complex located ventral to the thalam us and separated from it by the hypothalam ic sulcus. Despite its sm all size, the hypothalam us is the com m and center for all autonom ic functions in the body. The Term inologia Anatom ica lists over 30 hypothalam ic nuclei located in the lateral wall and oor of the third ventricle. Only a few of the larger, m ore clinically important nuclei are m entioned in this unit. The coronal section (c) shows the further subdivision of the hypothalam us by the fornix into lateral and m edial zones. The three nuclear groups described above are part of the medial zone, whereas the nuclei in the lateral zone are not subdivided into speci c groups. Bilateral lesions of the m am m illary bodies and their nuclei are m anifested by the K orsako syndrome, which is frequently associated with alcoholism (cause: vitam in B1 [thiam ine] de ciency). A m ajor neuropathological nding is the presence of hem orrhages in the m am m illary bodies, which are sectioned at autopsy to con rm the diagnosis. Diencepha lon Stria term inalis Fornix To reticular form ation Mam m illothalam ic fasciculus Stria m edullaris thalam i Posterior nucleus Medial forebrain bundle Preoptic nucleus Supraoptic nucleus Amygdala Paraventricular nucleus Supraoptic nucleus Tuberohypophyseal tract Hypothalam ichypophyseal tract Posterior lobe of pituitary gland a Hippocam pus Mam m illary body Peduncle of mam m illary body b Retroflex tract Mam m illotegm ental tract Dorsal longitudinal fasciculus C Important a erent and e erent connections of the hypothalamus Midsaggital section of the right hem isphere viewed from the m edial side. Because the hypothalam us coordinates all the autonom ic functions in the body, it establishes a erent (blue) and e erent (red) connections with m any brain regions. The bers of this tract m ediate the exchange of autonom ic inform ation bet ween the hypothalam us, cranial nerve nuclei, and spinal cord. D Functions of the hypothalamus the hypothalam us is the coordinating center of the autonom ic nervous system. Certain functions can be assigned to speci c regions or nuclei in the hypothalam us, and these relationships are outlined in the table. Region or nucleus Function Anterior preoptic region Maintains constant body temperature; Lesion: central hypothermia Responds to temperature changes. While the posterior pituitary lobe is an extension of the diencephalon, the anterior pituitary lobe is derived from the epithelium of the roof of the pharynx. The pituitary stalk (infundibulum) at taches both lobes of the gland to the hypothalam us. Pituitary horm ones are not synthesized in the posterior pituitary lobe (neurohypophysis) but in neurons located in the paraventricular nucleus and supraoptic nucleus of the hypothalam us. They are then transported by axons of the hypothalam ic-hypophyseal tract to the neurohypophysis, where they are released as needed. The peptide horm ones are stored in vesicles (aggregated into large "Herring bodies") in the cell bodies of the neurosecretory neurons and are carried to the posterior lobe by anterograde axoplasm ic transport. Diencepha lon Dorsom edial nucleus C Hypophyseal portal circulation and connections of the hypothalamic nuclei to the anterior pituitary lobe the superior hypophyseal arteries from each side of the body form a vascular plexus around the infundibulum (pituitary stalk). The axons from neurons of the hypothalam ic nuclei (dark red and dark blue arrows) term inate at this plexus and secrete horm ones that have been produced in sm aller (parvocellular) neurons of the hypothalam us. Ventrom edial nucleus Superior hypophyseal artery Tuberoinfundibular tract Inferior hypophyseal artery Capillary Chrom ophobic cells Basophilic cells Acidophilic cells D Histology of the anterior pituitary gland Three t ypes of cells can be distinguished in the anterior pituitary gland using classic histologic m ethods: acidophilic cells, basophilic cells, and chrom ophobic cells. The lat ter have already released their horm ones, and are therefore negative in im m unohistochem ical tests that speci cally detect peptide horm ones; they are not listed in E. The acidophilic (a) cells secrete horm ones that act directly on target cells (non-glandotropic horm ones) while the basophilic (b) cells stim ulate subordinate endocrine cells (glandotropic horm ones). The appropriateness of the term "epithalam us" can be appreciated in this plane of section, which shows the epithalam us riding upon the thalam us (epi = "upon"). The subthalam us contains nuclei of the m edial m otor system (m otor zones of the diencephalon), and has connections with the m otor nuclei of the tegm entum. In fact, the subthalam us can be considered the cranial extension of the tegm entum. It is connected to the diencephalon by the habenula, which contains both a erent and e erent tract s. Its topographical relationship to the third ventricle is seen particularly well in m idsagit tal section (pineal recess). In reptiles, the calvaria over the pineal gland is thinned so that it is receptive to light stim uli. This is not the case in hum ans, although retinal afferent s still com m unicate with the pineal through relay stations in the hypothalam us and the superior cervical (sym pathetic) ganglion, helping to regulate circadian rhythm s. Calci cations (corpora arenacea, "brain sand") are frequently present and m ay be visible on radiographs; they have no pathological signi cance. The pinealocytes produce melatonin, which plays a role in the regulation of circadian rhythm s; it m ay be taken prophylactically, for example, to m oderate the e ects of jet lag. If the pineal ceases to function during childhood, the individual m ay undergo precocious pubert y given that the pineal has signi cant, m ostly inhibitory, e ects on various endocrine system s. Diencepha lon Fornix Habenulointerpeduncular tract Septal nucleus Preoptic region Anterior perforated substance (olfactory area) Interpeduncular nucleus Amygdala Stria term inalis Stria m edullaris of thalam us Habenula Pineal gland Habenulotectal tract Quadrigem inal plate Habenulotegm ental tract Dorsal tegm ental nucleus D Habenular nuclei and their ber connections Midsagit tal section of the right hem isphere viewed from the m edial side.

Buy aurogra no prescription
Because the buccal pad is com posed of fat erectile dysfunction protocol real reviews purchase 100mg aurogra with amex, it is at tenuated in wasting diseases; this is why the cheeks are sunken in patients with end-stage cancer. This coronal section is slightly angled, producing an apparent discontinuit y in the m andibular ram us on the left side of the gure (compare with the continuous ram us on the right side). Above the roof of the sphenoid sinuses is the hypophysis (pituitary), which lies in the hypophyseal fossa. In the cranial cavit y, the plane of section passes through the m iddle cranial fossa. Cranial nerves can be seen passing through the cavernous sinus on their way from the m iddle cranial fossa to the orbit. The superior sagit tal sinus appears in cross-section at the at tachm ent of the falx cerebri. At the level of the cerebrum, the plane of section passes through the parietal and temporal lobes. Intracerebral structures appearing in this section include the caudate nucleus, the putam en, the internal capsule, and the anterior horn of each lateral ventricle. The highest section in this series displays the m uscles in the upper level of the orbit (the orbital levels are described on p. The section cut s the bony crista galli in the anterior cranial fossa, anked on each side by cells of the ethm oid sinus. The sections of the optic chiasm and adjacent optic tract are part s of the diencephalon, which surrounds the third ventricle at the center of the section. The section passes through the posterior (occipital) horns of the lateral ventricles and barely cuts the verm is of the cerebellum in the m idline. The optic nerve is seen just before it s entry into the optic canal, indicating that the plane of section passes through the m iddle level of the orbit. Because the nerve com pletely lls the canal, growth disturbances of the bone at this level m ay cause pressure injury to the nerve. The internal carotid artery can be identi ed in the m iddle cranial fossa, em bedded in the cavernous sinus. The section cuts the oculom otor nerve on either side, which courses in the lateral wall of the cavernous sinus. The falx cerebri and tentorium cerebelli appear as thin lines that com e together at the straight sinus. This section cuts the infratemporal fossa on the lateral aspect of the skull and the temporalis m uscle that lies within it. The plane passes through the lower level of the orbit, and a sm all portion of the eyeball is visible on the left side. This section displays the anterior extension of the t wo greater wings of the sphenoid bone and the posterior extension of the t wo "petrous bones" (petrous part s of the tem poral bones), which m ark the boundary bet ween the m iddle and posterior cranial fossae (see p. The clivus is part of the posterior cranial fossa and lies in contact with the basilar artery. The pontine origin of the trigem inal nerve and it s intracranial course are clearly dem onstrated. This section below the orbit passes through the infraorbital nerve in the accordingly nam ed canal. The zygom atic arch is visible in its entiret y, and portions of the m uscles of m astication m edial to the zygom atic arch (m asseter, temporalis, and lateral pterygoid) can be seen. It is evident that the body of the sphenoid bone form s the bony center of the base of the skull. The space around the anterior part of the cerebellum, the pontocerebellar cistern, is lled with cerebrospinal uid in the living individual. This section passes through the external nose and portions of the cartilaginous nasal skeleton. Cartilaginous portions of the pharyngot ympanic tube project into the nasopharynx. The arterial blood vessels that supply the brain can also be seen: the internal carotid artery and vertebral artery. Note the internal jugular vein and vagus nerve, which pass through the carotid sheath in company with the internal carotid artery. A num ber of cranial nerves that em erge from the skull base are displayed in cross-section, such as the facial nerve coursing in the facial canal. The section at this level passes through the connectivetissue sheet that stretches over the bone of the hard palate. The dens of the axis articulates in the m edian atlantoaxial joint with the facet for the dens on the posterior surface of the anterior arch of the atlas. The transverse ligam ent of the atlas that helps to stabilize this joint can also be identi ed. The vertebral artery and it s accompanying veins are displayed in cross-section, as is the spinal cord. In the occipital region, the section passes through the upper portion of the posterior neck m uscles. The elongated spinous process of the C7 vertebra (vertebra prom inens) is also visible at this level owing to the lordotic curvature of the neck. The triangular shape of the arytenoid cartilage is clearly dem onstrated in the laryngeal cross-section. This view also shows the accessory nerve m edial to the sternocleidom astoid m uscle. The piriform recess can be identi ed at this level, and the vertebral artery is visible in it s course along the vertebral body. The vagus nerve lies in a posterior angle bet ween the com m on carotid artery and internal jugular vein. This view shows the pro le of the phrenic nerve on the scalenus anterior m uscle on the left side. Note the neurovascular structures in the carotid sheath (com m on carotid artery, internal jugular vein, vagus nerve). Due to the curvature of the neck in this specim en, the section also cut s the intervertebral disk bet ween T1 and T2. The illustrations that follow are transverse cross-sections through the neck at progressively higher (m ore cranial) levels (Tiedem ann series). The proxim it y of the pulm onary apex to the brachial plexus shows why the growth of an apical lung tum or m ay dam age the brachial plexus root s. Note also the thyroid gland and its proxim it y to the trachea and neurovascular bundle in the carotid sheath (a thin brous sheet which is not clearly discernible in these views). Sectiona l Ana tomy Arytenoid cartilage Superior thyroid vein Hypopharynx Com m on carotid artery Internal jugular vein Longus colli Thyroid cartilage Sternohyoid Thyrohyoid Om ohyoid Thyroid gland Sternocleidom astoid Scalenus anterior C4 spinal nerve C5 spinal nerve Vertebral vein Scalenus m edius C6 spinal nerve Vertebral artery C6 vertebra Scalenus posterior C7 spinal nerve C7 vertebra Levator scapulae Trapezius Vertebral arch of T1 C Transverse cross-section at the level of the arytenoid cartilage (level of the C6 vertebral body) Caudal view. This cross-section passes through the base of the arytenoid cartilage in the larynx. Sem ispinalis cervicis Splenius cervicis Thyroid cartilage Rim a glot tidis Lam ina of cricoid cartilage Hypopharynx Com m on carotid artery Internal jugular vein C6 vertebra Vertebral artery Vertebral vein Scalenus m edius Scalenus posterior Levator scapulae C8 spinal nerve Trapezius Vertebral arch of T1 Sternohyoid Thyrohyoid Superior thyroid artery Sternocleidom astoid Thyroid gland External jugular vein C5 spinal nerve C6 spinal nerve C7 spinal nerve C7 vertebra D Transverse cross-section at the level of the vocalis muscle in the larynx (junction of the C6/C7 vertebral bodies) Caudal view. The thyroid gland appears considerably sm aller at this level than in views A and B. The m idline structures are particularly well displayed in this plane of section, and the anatom ical structures at this level can be roughly assigned to the facial skeleton or neurocranium (cranial vault). The lowest level of the facial skeleton is form ed by the oral oor m uscles bet ween the hyoid bone and m andible and the overlying skin. This section also passes through the epiglot this and the larynx below it, which are considered part of the cervical viscera. The hard and soft palate with the uvula de ne the boundary bet ween the oral and nasal cavities. The section includes the nasal sep- tum, which divides the nasal cavit y into t wo cavities (sectioned above and in front of the septum) that com m unicate with the nasopharynx through the choanae. Posterior to the frontal sinus is the anterior cranial fossa, which is part of the neurocranium. This section passes through the m edial surface of the brain (the falx cerebri has been rem oved). The cut edge of the corpus callosum, the olfactory bulb, and the pituitary are also shown. This section passes through the inferior and m iddle nasal conchae within the nasal cavit y.

Discount aurogra online master card
Although a di use kind of sensory perception m ay take place at the thalam ic level (especially pain perception) erectile dysfunction low testosterone treatment discount aurogra 100 mg mastercard, cortical processing (by the telencephalon) is necessary in order to transform unconscious perception into conscious perception. The olfactory system is an exception to this rule, although it s olfactory bulb is still an extension of the telencephalon. Note: Major descending m otor tract s from the cerebral cortex generally bypass the thalam us. B Spatial arrangement of the thalamic nuclear groups Left thalam us viewed from the lateral and occipital aspect, slightly rotated relative to the views on p. The thalam us is a collection of approxim ately 120 nuclei that process sensory inform ation. Located beneath the pulvinar, these t wo nuclear bodies contain the nuclei of the medial and lateral geniculate bodies, and are collectively called the metathalamus. The only nonspeci c nuclei shown in this diagram (orange, see F for further details) are the centrom edian nucleus and the intralam inar nuclei. C Nomenclature of the thalamic nuclei Name Alternative name Properties Speci c thalam ic nuclei (cortically dependent) Nonspeci c thalam ic nuclei (cortically independent) Integration nuclei Intralaminar nuclei Palliothalam us Truncothalamus Project to the cerebral cortex (pallium) Project to the brainstem, diencephalon, and corpus striatum Project to other nuclei within the thalam us (classi ed as nonspeci c thalamic nuclei) Nuclei in the white mat ter of the internal medullary lamina (classi ed as nonspeci c thalamic nuclei) 334 Neuroanatomy 14. Diencepha lon Ventrolateral thalam ic nuclei Medial thalam ic nuclei Anterior thalam ic nuclei (1) Ventral anterior nucleus (2) Ventral lateral nucleus (5) Ventral posterom edial nucleus Internal capsule (3) Ventral interm ediate nucleus (4) Ventral posterolateral nucleus Reticular nucleus of thalam us External m edullary lam ina Internal m edullary lam ina Mam m illary body D Division of the thalamic nuclei by the medullary laminae Coronal section at the level of the m am m illary bodies. Several groups of thalam ic nuclei are grossly separated into larger nuclear complexes by brous sheet s called m edullary lam inae. Intralam inar nuclei Midline nuclei E Somatotopic organization of the speci c thalamic nuclei Transverse section. The speci c thalamic nuclei (de ned in B, C) are topographically arranged according to their functional relation to specic regions of the body. A erent bers from the spinal cord, brainstem, and cerebellum are localized to speci c areas of the thalamus, where the corresponding thalam ic nuclei are clustered. This pat tern of somatotopic arrangem ent, a recurring theme in neural organization, is here illustrated for the ventrolateral thalamic nuclei (green in B, D, E). Axons from the crossed superior cerebellar peduncle terminate in the ventral lateral nucleus of the thalamus (2); inform ation on body position, coordination and muscle tone travels by this pathway to the motor cortex, which also shows a pat tern of somatotopic organization (see B, p. The lateral part of the ventral lateral nucleus relays impulses from the trunk and limbs, while the medial part relays impulses from the head. The ventral intermediate nucleus (3) receives a erent input from the vestibular nuclei concerning the coordination of gaze toward the ipsilateral side. The large sensory pathways of the spinal cord (the tracts of the dorsal column) are relayed to the nuclei cuneatus and gracilus, which send their axons through the medial lemniscus to terminate in the ventral posterolateral nucleus (4), while the trigeminal sensory pathways from the head terminate in the ventral posterom edial nucleus (5, trigem inal lemniscus, see p. Topographical localization according to function is a basic principle of neural organization. Anterior thalam ic radiation Central thalam ic radiation Posterior thalam ic radiation Intralam inar nuclei Specific thalam ic nuclei Centrom edian nucleus Reticular nucleus F Nonspeci c thalamic nuclei Coronal sections presented in an oral-to-caudal series. The nonspecic thalam ic nuclei project to the brainstem, to other nuclei in the diencephalon (including other thalam ic nuclei), and to the corpus striatum. They have no direct connections with the cerebral cortex, acting only indirectly on the cortex. The lateral specif c thalam ic nucleus shown in the diagram is the reticular nucleus of the thalam us, which is situated lateral to the other speci c thalam ic nuclei. Inferior thalam ic radiation G Thalamic radiations Lateral ventricle of the left hem isphere. The axons of the speci c thalam ic nuclei (so called because their bers project to speci c cortical areas) are collected into tract s that form the thalam ic radiations. The habenula ("reins") and their nuclei function as a relay station for a erent olfactory impulses. After their relay in the habenular nuclei, their e erent bers are distributed to the salivatory and m otor nuclei (m astication) in the brainstem. A erent connections (blue): A erent im pulses from the anterior perforated substance (olfactory area), septal nuclei, and preoptic region are transm it ted by the stria m edullaris to the habenular nuclei. Certain sm all nuclei are exempt from this m igration and rem ain near the m idline: these are the zona incerta and subthalamic nucleus. The subthalam ic nucleus, substantia nigra, and putam en send a erent bers to the globus pallidus. The globus pallidus in turn distributes e erent bers to these regions and also to the thalam us through a tract called the lenticular fasciculus. Compared to the telencephalon, the brainstem is so sm all that it s part s becom e visible only in m idsagit tal section (b). The purely topographical dem arkation of zones in the brainstem from cranial to caudal is based on its external, m acroscopic structure. The mesencephalon begins im m ediately at the diencephalon and extends to the cranial transverse gyrus of the pons which at its caudal end is separated from the m edulla oblongata by the bulbopontine sulcus. The brainstem extends to the point of exit of the rst spinal nerve after which the spinal cord begins. Also purely topographical criteria are used to subdivide each brainstem section into four parts (see B). All com m unication bet ween the spinal cord and the m ore rostral regions of the brain diencephalon passes though these tract s within the brainstem. Depending on the ow of inform ation, a distinction is drawn bet ween ascending (a erent, to the telencephalon) and descending (e erent, away from the telencephalon) tract s. Note: Since so m any nuclei and tracts lie so closely together in the brainstem, even sm all lesions, for example, in case of bleeding brainstem stroke can cause severe dam age. Cranial to the pons lie the crus cerebri, which contain descending m otor pathways. A part of these bers extend to the pyram ids of the the m edulla oblongata and m ost of them cross over in the pyram idal decussation. The olive, located lateral to the pyram id, contains a large m otor nuclear group, the olivary nuclei. What is striking is the view of the diam ond-shaped fourth ventricle, the oor of which is outlined by several cranial nerve nuclei. The superior colliculi are integrative centers related to visual inform ation and the inferior colliculi are relay stations of the auditory pathway. The brachium ("arm ") of the superior colliculus and the brachium of the inferior colliculus connect these colliculi with their corresponding thalam ic nuclei. Lateral to the fourth ventricle, as a topographic connection between cerebellum and brainstem, are three paired cerebellar peduncles: the superior, m iddle, and inferior cerebellar peduncles. Very clearly displayed in this view is the fact that the ventral curvature of the pons extends into the m iddle cerebellar peduncle, which connects the pons with the cerebellum. The diagram s show the nuclei them selves and the course of the nerves (to save space, the vestibular and cochlear nuclei are not shown). The arrangem ent of the cranial nerve nuclei is easier to understand when we divide them into functional nuclear colum ns. The arrangem ent of these nuclei can be derived from the arrangem ent of the nuclei in the spinal cord (see p. The function and connections of som e of these cranial nerves can be clinically evaluated by testing the brainstem re exes (whose relay centers are located in the brainstem).