Buy generic benadryl on-line
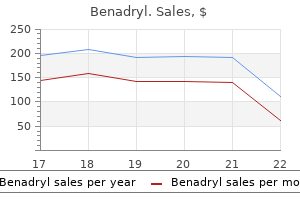
Additionally allergy medicine makes you drowsy order benadryl 25 mg mastercard, propofol is used more commonly given its pharmacokinetics are not altered in liver failure. Efficacy of L-ornithine L-aspartate in acute liver failure: a double-blind, randomized, placebo controlled study. Arterial ammonia and clinical risk factors for encephalopathy and intracranial hypertension in acute liver failure. Brain edema and intracranial hypertension in fulminant hepatic failure: pathophysiology and management. Intracranial hypertension in acute liver failure: pathophysiological basis of rational management. Moderate hypothermia prevents cerebral hyperemia and increase in intracranial pressure in patients undergoing liver transplantation for acute liver failure. Moderate hypothermia in patients with acute liver failure and uncontrolled intracranial hypertension. Assessment and management of cerebral edema and intracranial hypertension in acute liver failure. The effect of hypertonic sodium chloride on intracranial pressure in patients with acute liver failure. Intravascular volume depletion may also be present due to poor oral intake from altered mental status. Norepinephrine may be the optimal vasopressor to augment organ perfusion and preserve hepatic blood flow. Mechanical ventilation may be required but positive end-expiratory pressure can worsen cerebral edema and decrease hepatic blood flow. Replacement therapy is recommended only in the setting of hemorrhage or prior to invasive procedure. Plasma glucose concentration should be monitored and hypoglycemia managed with continuous glucose infusions. Likewise platelet transfusion is not recommended without spontaneous bleeding or prior to invasive procedures. The use of gastrointestinal hemorrhage prophylaxis with a proton pump inhibitor is recommended. The coagulopathy of acute liver failure and implications for intracranial pressure monitoring. Prevention of renal failure by ensuring adequate systemic blood pressure, treating infections, and avoiding nephrotoxic agents is important. Intravascular volume deficits are often present on admission and volume replacement is required. Acute renal failure may occur due to dehydration, hemodynamic changes similar to hepatorenal syndrome, or acute tubular necrosis. Renal failure may be even more common with acetaminophen overdose or other toxic ingestions due to direct nephrotoxicity causing acid-base disturbances and lactic acidosis. Prompt fluid resuscitation with crystalloids for low arterial pressure, or colloids in pre-hepatorenal syndrome along with midodrine and octreotide, have been suggested. If renal dysfunction, fluid balance, and metabolic derangements necessitate renal replacement, continuous renal replacement therapy should be used for hemodynamic and metabolic stability. Risk factors and outcomes of acute kidney injury in patients with acute liver failure. Defective cellular and humoral immunity as well as presence of indwelling catheters, coma, broad-spectrum antibiotics, and medications that suppress immunity all predispose to infection. Localizing symptoms of infection such as fever and sputum production are frequently absent, and the only clues to an underlying infectious process may be worsening of encephalopathy or renal function. There must be a low threshold for obtaining frequent cultures (blood, urine, and sputum), chest radiographs, and paracentesis. Bacteria that enter through the skin, such as streptococci and staphylococci, tend to predominate and therefore broad-spectrum antibiotics (quinolones or third-generation cephalosporin) are generally used. Fungal infections, particularly in the setting of broad-spectrum antibiotics, are also common and disseminated fungemia is a poor prognostic sign. Aggressive surveillance is essential, as prophylactic antibiotics have shown little benefit, though empiric antibiotic administration can be considered where infection or the likelihood of sepsis is high. Liver Transplantation Liver transplantation has changed survival from as low as 15% in the pretransplant era to over 60%. A recent large prospective study evaluating the 2-year outcomes of initial survivors (alive after 3 weeks from initial enrollment) demonstrated a high survival rate of over 75%, but patients that received liver transplants had a significantly higher 2-year survival of over 90% compared to those that had spontaneous survival. The age of recipient, severity of pretransplant illness, and nature of graft used all contribute to outcome in emergent liver transplant. Parenteral nutrition should be used only if enteral feeding is contraindicated as it increases the risk of infection. Severe restriction of protein is not beneficial; 60 g/day of protein is generally reasonable. Correction of hypokalemia is essential as hypokalemia increases renal ammonia production, potentially exacerbating encephalopathy. Timely availability of an allograft is one of the major factors determining transplant outcomes. Ten percent of the overall group (one-fourth of patients listed for transplantation) died on the waiting list. Other studies have reported death rates of those listed for transplant as high as 40%. Liver transplantation for fulminant hepatic failure: experience with more than 200 patients over a 17-year period. Two-year outcomes in initial survivors with acute liver failure: results from a prospective, multicentre study. Patients with other etiologies had a survival rate of less than 25% without transplantation. With the potential option of liver transplantation, survival has dramatically increased. In addition, better critical care management and the trend toward more benign causes also contribute to improved survival rates, with spontaneous survival around 50%. Potentially helpful indicatorsa of poor (transplant-free) prognosis in patients with acute liver failure. Liver Support Systems Liver support systems attempt to support the patient until recovery or serve as a bridge to transplant. Artificial support systems provide detoxification, while bioartificial support systems also provide synthetic function by using cellular material. Clinical experience with bioartificial systems is mostly confined to small numbers of patients in uncontrolled trials. One systematic review of 12 randomized trials (with a total 483 patients) assessing artificial and bioartificial support systems for acute or acute-on-chronic liver failure as a "bridge" to transplantation showed no significant effect on mortality compared with standard medical therapy. Acetaminophen levels should be drawn on initial evaluation, yet depending on the timing of ingestion, acetaminophen levels may not be elevated even in overdose. Several studies evaluating these criteria have shown positive predictive values ranging from 70% to nearly 100% and negative predictive values from 25% to 94%. Fulfillment of these criteria suggests that without transplantation, the patient has a very high mortality risk. Intravenous administration is given as 150 mg/kg loading dose over 15 minutes, followed by maintenance at 50 mg/kg for over 4 hours and then 100 mg/kg over 16 hours. No studies have shown any difference between oral and intravenous routes of administration. Additionally, alcohol use, starvation, and acute illness may deplete glutathione, predisposing to liver injury from acetaminophen. Suicidal intent, a history of previous suicide attempts, or evidence of substance abuse may preclude transplant consideration. Phase 1 (first 24 hours) symptoms include anorexia, nausea/vomiting, lethargy, and diaphoresis.
Buy benadryl with american express
The most significant differences between gastric dysplasia/adenoma and the intestinal type of adenocarcinoma relate to cellularity and dyshesion allergy forecast galveston order discount benadryl line. A sample from an adenocarcinoma is usually highly cellular, with many isolated cells, as well as tight and loose clusters of cells. Goblet cells of intestinal metaplasia are rarely isolated cells, except in liquid-based preparations, and they lack nuclear atypia (angulation and hyperchromasia). Their incidence appears to have increased in the last five decades, and this increase is most prominent in the stomach and rectum. The monomorphic cells have a moderate amountofcytoplasmandasalt-and-pepperchromatinpattern. One way to avoid this pitfall is to identify intact cells and base a diagnosis on these cells only. The final subtyping often depends on subsequent histologic sampling with immunophenotyping, molecular studies, or both. Because the tumor cells are predominantly in the lamina propria, cellularity is high only when ulceration exposes them to the brush. Otherwise, if the mucosa is intact, diagnostic cells may be sparse or absent altogether. As a result, only two-thirds or fewer of biopsy-proven gastric lymphomas are detected by cytologic sampling. Although a poorly differentiated carcinoma sometimes presents a pattern of isolated cells or bare nuclei, a careful search usually uncovers small groups or fragments of malignant cells that are recognizably epithelial. Mutations make c-kit function independently of stem cell factor, leading to increased cell division. All are considered potentially malignant; the risk of progression depends in part on the location of the tumor, its size, and its mitotic rate. Patients who develop resistance to imatinib are treated with other tyrosine kinase inhibitors like sunitinib. Duodenum Infections Brush cytology of the duodenum is useful to detect Giardia lamblia, an intestinal parasite that causes diarrhea and is usually acquired from contaminated drinking water. Small round basophilic bodies dot the surface of glandular epithelial cells (smear, Papanicolaoustain). This possibility should be kept in mind when examining a specimen from an immunocompromised patient. They are seen only when the plane of focus is shifted to the surface of the cells where the organisms reside. When in doubt, a confirmatory Grocott methenamine silver stain can be used to highlight them. Other common lesions of the duodenum, including epithelial repair, adenocarcinoma, neuroendocrine tumors, and infections, resemble their counterparts in the stomach. Adenoma and Adenocarcinoma Premalignant lesions, including adenomas, are more common in the colon than in the stomach or small bowel. Even when only a low-grade premalignant lesion is present on the cytologic specimen, an unsampled coexisting carcinoma elsewhere in the lesion cannot be excluded. Therefore surgical resection of the entire lesion is indicated when a diagnosis of a premalignant lesion of the small bowel is suspected or rendered on cytology. When the lesion is diffuse or ill defined, multiple biopsy specimens should be taken. The cytologic findings in ulcerative colitis have been described, but it is not customary to obtain cytologic specimens in this setting. Colonoscopy with biopsy is widely performed to screen for colonic neoplasia and colitis, particularly inflammatory bowel disease, and cytologic examination is not definitive in establishing the diagnosis of adenoma/dysplasia and active or chronic colitis. It is easier to distinguish a low-grade premalignant lesion from a carcinoma; a high-grade premalignant lesion is quite difficult to distinguish from an invasive malignancy. The degree of cellularity, dyshesion, and nuclear atypia helps to distinguish a high-grade premalignant lesion from a frankly malignant one, but the difference is quantitative, not qualitative. Anal cytology specimens should sample the entire anal canal, including keratinized and nonkeratinized squamous epithelium and the anorectal transformation zone. A Dacron swab moistened with tap water is inserted blindly 5 to 6 cm into the anal canal past the anal verge and into the rectal vault. For this reason, the terminology of the Bethesda System for Reporting Cervical Cytology. Value of cytology in detecting intestinal metaplasia and associated dysplasia at the gastroesophageal junction. Esophageal cytology in the follow-up of patients with treated upper aerodigestive tract malignancies. Cytologic detection of esophageal squamous cell carcinoma and its precursor lesions using balloon samplers and liquid-based cytology in asymptomatic adults in Llinxian, China. Pilot study of cytological testing for oesophageal squamous cell dysplasia in a high-risk area in Northern Iran. Wide-area transepithelial sampling with 3-dimensional cytology: does it detect more dysplasia or yield more hype Endoscopic ultrasound-guided fine needle aspiration biopsy for diagnosis of lymphoproliferative disorders: feasibility of immunohistological, flow cytometric, and cytogenetic assessments. Evaluation of fineneedle aspiration biopsy under direct vision gastrofiberscopy in diagnosis of diffusely infiltrative carcinoma of the stomach. Endoscopic needle aspiration cytology: a new method for the diagnosis of upper gastrointestinal cancer. Endoscopically directed fine needle aspiration biopsy of gastric and esophageal lesions. Endoscopic ultrasonography as an adjunct to fine needle aspiration cytology of the upper and lower gastrointestinal tract. Combined endosonography and fine-needle aspiration cytology in the evaluation of gastrointestinal lesions. Cytologic screening for esophageal cancer in a high-risk population in Anyang County, China. Comparison of ThinPrep preparations to other preparation types in gastrointestinal cytology: observations from the College of American Pathologists Interlaboratory Comparison Program in Nongynecologic Cytology. Comparison of ThinPrep UroCyte and cytospin slide preparations for gastrointestinal specimens: evaluation and retrospective performance review. Endoscopic biopsies and cytologic brushings of the esophagus are diagnostically complementary. Adjunctive endoscopic brush cytology in the detection of upper gastrointestinal malignancy. Correlation of endoscopic brush cytology with biopsy in diagnosis of upper gastrointestinal neoplasms. Comparison of brush cytology before or after biopsy for diagnosis of gastric carcinoma. Prospective comparison of the value of brushings before and after biopsy in the endoscopic diagnosis of gastroesophageal malignancy. Utility of liquid-based cytologic examination of distal esophageal brushings in the management of Barrett esophagus: a prospective study of 45 cases. Esophageal balloon cytology and subsequent risk of esophageal and gastric-cardia cancer in a high-risk Chinese population. Endoscopic brush cytology and biopsy in the diagnosis of cancer of the upper gastrointestinal tract. Opportunistic disorders of the gastrointestinal tract in the age of highly active antiretroviral therapy. Intestinal metaplasia is the probable common precursor of adenocarcinoma in Barrett esophagus and adenocarcinoma of the gastric cardia. Reproducibility of the diagnosis of dysplasia in Barrett esophagus: a reaffirmation. Cytologic features of premalignant glandular lesions in the upper gastrointestinal tract.
Cheap benadryl 25 mg online
They look benign on sonographic and laparoscopic examination: they are unilocular allergy vacuum buy benadryl with a mastercard, smooth-surfaced, translucent, and thin-walled. Multiple follicle cysts are common in juvenile hypothyroidism, ovarian hyperstimulation syndrome, and polycystic ovary disease. Accuracy the reported sensitivity for a diagnosis of malignancy ranges widely from 25% to 93%,14,18,23,24,26-31 although some of the higher estimates are likely inflated because borderline tumors were excluded from analysis. It may be sparsely cellular, containing only histiocytes and blood, or markedly cellular (sometimes alarmingly so), with numerous granulosa cells that are isolated and in large clusters. Because follicle cysts appear benign sonographically and laparoscopically, they are managed conservatively to preserve the ovary. Theca interna cells have an eccentrically placed ovoid nucleus and a moderate amount of cytoplasm. Theca externa cells are indistinguishable from spindle-shaped ovarian stromal cells. The highly cellular cases are termed cellular follicle cysts and account for between 23% and 76% of all follicle cysts. They have a round nucleus with coarsely granular chromatin and one or two small nucleoli. When ciliated or mucinous epithelium is identified, the cyst is of surface epithelial origin and not a follicle cyst. Cellular follicle cysts are a potential pitfall: because of their cellularity and conspicuous mitotic activity, they may raise the possibility of a granulosa cell tumor or carcinoma. The fluid may be hemorrhagic and composed of numerous, predominantly isolated luteinized granulosa cells with round or pyknotic nuclei. Macrophages with hemosiderin or the yellow hematoidin pigment and smaller luteinized theca interna cells are also seen. Endometriotic Cyst Endometriosis affects women of reproductive age and is often associated with infertility. It can result in a cystic tumor-like mass of the ovary, known as an endometriotic cyst or endometrioma. For an unequivocal diagnosis, identification of two of the following features is required: endometrial glands, endometrial stroma, and hemosiderin. The cells are small and have indistinct borders; nuclei are round or oval; nucleoli are inconspicuous; and cytoplasm is scant and sometimes vacuolated. The diagnosis of endometriosis is easily made when both cytologically benign epithelial and stromal cells are present. It is impossible to distinguish an endometriotic cyst from a hemorrhagic corpus luteum when epithelial cells are absent because luteinized granulosa and theca cells resemble histiocytes. Simple Ovarian, Paraovarian, and Paratubal Cysts Simple cysts of the ovary or fallopian tube are most common in postmenopausal women and result from an invagination of mesothelium or the surface epithelium. They are usually small and multiple and lined by a single layer of benign columnar, cuboidal, or flattened epithelium. The cytologic features of simple ovarian, parovarian, and paratubal cysts are identical. When small cuboidal epithelial cells are seen (rarely), they are usually arranged in tight clusters or sheets. If ciliated cells are present, however, the lesion is either a serous cyst or a hydrosalpinx. They are seen in serous cysts, cystic teratomas, and hydrosalpinx (Papanicolaoustain). Hydrosalpinx Hydrosalpinx, a complication of salpingitis, presents as a large cystic adnexal mass. The distended fallopian tube is filled with clear fluid and is lined by ciliated epithelium. These findings are identical to those seen with serous ovarian and paraovarian cysts. It presents as a palpable adnexal mass that can be visualized by ultrasonography or computed tomography. Most cases result from an ascending infection of the lower genital tract by sexually transmitted pathogens like Neisseria gonorrhoeae, Chlamydia trachomatis, and Mycoplasma genitalium. Aspirated material is thick and yellow and composed of numerous polymorphonuclear leukocytes and abundant necrotic debris. When these elements are seen during a rapid interpretation of the aspirated material, additional passes should be performed to obtain samples for microbiologic study to identify the causative organism. Surgery is considered for those patients who do not respond to antibiotic therapy. If the cyst fluid does not contain ciliated cells or detached ciliary tufts, the findings are nonspecific. They are divided histologically into serous (the most common), mucinous, endometrioid, clear cell, Brenner, seromucinous, and undifferentiated types. The lining cells are isolated, often retaining their columnar shape, or arranged in clusters and honeycomb-like sheets with sharply defined cell membranes. Diagnosing a mucinous cystadenoma is straightforward when mucinous epithelium is identified. If nuclear atypia is present, a borderline tumor or carcinoma should be suspected. The cuboidal cyst lining cells, if present, have a uniformly round or oval nucleus and are arranged in crowded clusters. The cyst is lined by benign ciliated cells that have a basally placed nucleus, terminal bar, and cilia (Papanicolaoustain). Most are solid, but some contain small or large cystic areas that may show mucinous differentiation. Benign Brenner tumors are composed of nests of transitionaltype epithelium (resembling urothelial cells) embedded in a dense fibrous stroma. Aspirates show sheets of transitional-type cells, the nuclei of which resemble coffee beans because they are oval and have a prominent longitudinal groove. Globular hyaline structures that stain bright orange with the Papanicolaou stain are seen48; their composition and significance are not known. The differential diagnosis includes a granulosa cell tumor, the cells of which also have longitudinal grooves. Ovarian tumors, however, sometimes present as pelvic masses so large that they significantly alter pelvic anatomy. The high-grade serous carcinoma is by far more common, composed of large pleomorphic cells lining the cystic areas, forming papillary projections, and invading the stroma. Low-grade serous carcinomas account for only 5% of all serous carcinomas and are composed of a more uniform population of cells with minimal pleomorphism. As with serous carcinoma, the serous borderline tumor can be both solid and cystic. The degree of nuclear atypia resembles that of a low-grade serous carcinoma, and therefore it is not possible to distinguish between the two cytologically29,36; the diagnosis of carcinoma is based on identifying stromal invasion. Nevertheless, borderline tumors are generally of lower grade than high-grade serous carcinomas, and therefore some generalizations are possible. Psammoma bodies accompanied by a rim of malignant cells are seen in some but not all cases. Although aspirates of cellular follicle cysts, like those of a serous carcinoma, can be highly cellular and show mitotic activity, follicle cysts have uniform nuclei and negative sonographic or laparoscopic findings. As mentioned above, the distinction between a borderline tumor and a serous carcinoma is possible only on the surgically excised specimen. The distinction between serous carcinoma and other epithelial malignancies such as mucinous carcinoma and clear cell carcinoma, especially with poorly differentiated tumors, is sometimes difficult. Mucinous Borderline Tumor and Mucinous Carcinoma Mucinous carcinomas are less common than serous carcinomas, accounting for only 3% to 4% of all primary ovarian carcinomas. Aspirates from mucinous carcinomas are cellular, composed of isolated cells and cells in sheets or grouped in irregular clusters. Cells from well-differentiated tumors are columnar, contain mucin, and have mild nuclear atypia. Aspirates from mucinous borderline tumors are a common cause of false-negative results.
Discount 25mg benadryl amex
However allergy shampoo for dogs 25 mg benadryl overnight delivery, such treatment has not resulted in survival benefit or delay in the need for liver transplantation. In patients with a dominant stricture, management with endoscopic dilatation with or without stenting is usually recommended. The percutaneous approach is reserved for patients with a proximal dominant stricture in whom an endoscopic approach failed. Importantly, brush cytology and/or endoscopic biopsy should be performed to exclude a superimposed malignancy prior to endoscopic therapy for a dominant stricture. Immunoglobulin G4-associated cholangitis: clinical profile and response to therapy. High-dose ursodeoxycholic acid for the treatment of primary sclerosing cholangitis. This score is valuable in assessing prognosis and determining the timing for liver transplantation. The risk is increased after endoscopic manipulation of the extrahepatic biliary tree. However, cholangitis can also develop spontaneously with high-grade obstructing strictures. Patients with coexisting inflammatory bowel disease and cirrhosis are at the highest risk. On imaging studies, it is often difficult to distinguish a dominant stricture from a cholangiocarcinoma. In particular, persistent serum bilirubin elevations lasting longer than 3 months identified a novel risk factor correlating with a poor outcome. Natural history and prognostic factors in 305 patients with primary sclerosing cholangitis. Inflammatory bowel disease is associated with poor outcomes of patients with primary sclerosing cholangitis. Characterization, outcome and prognosis in 273 patients with primary sclerosing cholangitis. Low risk of hepatocellular carcinoma in patients with primary sclerosing cholangitis with cirrhosis. One hundred thirty-four (44%) of the patients were asymptomatic at the time of diagnosis and 22 of the 134 (22%) became symptomatic during the median follow-up period of 63 months. The median survival rate from the time of diagnosis to death or liver transplantation was 12 years. The independent predictors influencing prognosis were age, serum bilirubin concentration, and liver histologic changes. Median survival from the time of diagnosis to death or liver transplantation was 9. Gallstones are often found incidentally during abdominal ultrasonography, which has >95% sensitivity for cholesterol stones 1. In ~80% of cases gallstones remain asymptomatic; in symptomatic patients, biliary colic is almost always present, often radiating to the right scapula or shoulder. Laparoscopic cholecystectomy is indicated in patients with symptomatic gallstones. Major complications of gallstone disease requiring treatment are acute cholecystitis, choledocholithiasis, obstructive jaundice, cholangitis, and pancreatitis. Acute cholangitis caused by an obstructing gallstone should be treated by endoscopic removal of the stone under antibiotic coverage as soon as possible. A complex solubilizing system in bile is required to keep cholesterol in solution. If this system fails, or if its capacity is exceeded by hypersecretion of cholesterol into bile, cholesterol precipitates and gallstones may develop. The prevalence of gallstone disease is lower in Asians (ranging from 3% to 15%) and very low (<5%) in Africans. Certain ethnic groups are particularly susceptible; among Native Americans in the western United States, the prevalence of gallstones is over 75%. Epidemiologic surveys and family clustering point to the critical role of genetics in determining susceptibility to gallstones. The genetic component in the pathogenesis of symptomatic gallstone disease in the Swedish population has been estimated to be about 25%. In the United States, it is the gastrointestinal disorder that, after gastroesophageal reflux disease, accounts for the second-highest costs. The clinical manifestations of gallstones include episodic abdominal pain, acute cholecystitis, obstructive jaundice, cholangitis, and pancreatitis. In Western industrialized countries, >90% of gallstones consist mainly of cholesterol. This gene defect is associated with extremely low phosphatidylcholine levels in bilecausing cholesterol precipitation. The gender difference at least partly results from endogenous estrogens, which increase biliary cholesterol secretion and cholesterol saturation of bile. Pregnancy increases the risk of gallstones because impaired gallbladder emptying, caused by progesterone, combines with the influence of estrogen, which increases cholesterol hypersecretion. In obese persons an overproduction of cholesterol causes cholesterol hypersecretion into bile and thus predisposes to gallstone formation. Loci from a genome-wide analysis of bilirubin levels are associated with gallstone risk and composition. Genetic and environmental influences on symptomatic gallstone disease: a Swedish study of 43,141 twin pairs. Genotype-phenotype relationships in the low-phospholipid-associated cholelithiasis syndrome: a study of 156 consecutive patients. Predictors of gallstone composition in 1025 symptomatic gallstones from Northern Germany. Sterol transporter adenosine triphosphate-binding cassette transporter G8, gallstones, and biliary cancer in 62,000 individuals from the general population. Cholesterol stones account for more than 90% of all gallstones in Western industrialized countries. Pigment stones are composed primarily of calcium bilirubinate; they contain less than 20% cholesterol. General Increasing age Female gender Ethnicity Family history Diet Overnutrition High calorie Low fiber High refined carbohydrates Lifestyle Low-grade physical activity Prolonged fasting Rapid weight loss Weight cycling Pregnancy and parity Oral contraceptives Associated conditions Obesity Metabolic syndrome Estrogen replacement therapy A. Cholesterol Stones Because cholesterol is practically insoluble in water, solubilizing lipids (bile acids and phospholipids) are required for its incorporation into bile. Supersaturation of bile with cholesterol is the thermodynamic requirement for the formation of cholesterol gallstones. Cholesterol crystals Cholesterol stone Biliary secretion and solubilization of cholesterol. Cholesterol and phosphatidylcholine reach the bile as metastable unilamellar vesicles, which are converted into water-soluble stable mixed micelles by the bile acids. If the secretion of cholesterol into bile exceeds the solubilizing capacity of bile acids and phospholipids, cholesterol-rich vesicles remain, which aggregate into large unstable multilamellar vesicles from which cholesterol crystals precipitate. If all cholesterol phosphatidyl vesicles cannot be converted into water-soluble mixed micelles, unstable cholesterol-rich vesicles remain. The unstable vesicles aggregate into large multilamellar vesicles from which cholesterol crystals precipitate. These crystals-if not expelled from the gallbladder-become entrapped in gallbladder mucin gel, where they grow and agglomerate to form stones. The pathogenesis of cholesterol hypersecretion is multifactorial, with genetic and environmental components. Cholesterol supersaturation of bile-An excess of biliary cholesterol in relation to its carriers (phospholipids and bile acids) is a sine qua non condition for the formation of cholesterol gallstones. It may result from hypersecretion of cholesterol, hyposecretion of bile acids or phospholipids, or a combination of the two. Relative cholesterol hypersecretion is by far the most common cause of supersaturation of bile.
Purchase genuine benadryl on-line
Water-soluble gel lubricant allergy medicine and caffeine cheap benadryl online, if used, should be applied sparingly to the posterior blade of the speculum, avoiding the tip: excessive lubricant can result in an unsatisfactory specimen. ThinPrep Pap Test the practitioner obtains the ThinPrep Pap sample with either a broom-type device or a plastic spatula/endocervical brush combination. The sampling device is swirled/rinsed in a methanol-based preservative solution (PreservCyt) for transport to the cytology laboratory and then discarded. This results in a thin deposit of cells in a circle 20 mm in diameter (contrast 1. Thesamplevialsitsona stage, and a hollow plastic cylinder with a 20 mm diameter polycarbonate filter bonded to its lower surface is inserted into the vial. In most cases, only a fraction of the sample is used to prepare the slide used for diagnosis. If needed, the residual sample is available for additional ThinPrep slide preparation, cell block preparation, or molecular diagnostic testing. Unlike the ThinPrep method, the practitioner snips off the tip of the collection device and includes it in the sample vial. In addition to preparing an evenly distributed deposit of cells in a circle 13 mm in diameter, the method incorporates a final staining step that discretely stains each individual slide. In the 1990s, researchers in the United States and Canada established private enterprises supported by venture capital to develop a commercial automated screening instrument. Foremost in the field were AutoCyte (formerly Roche Image Analysis Systems), Cytyc, Neopath, and Neuromedical Systems. A three-way merger took place in 1999, when AutoCyte, after purchasing the intellectual property of Neuromedical Systems, merged with Neopath to form a new company called TriPath Imaging, acquired in 2006 by Becton Dickinson. Neither is approved in the United States for automated screening of nongynecologic cytology specimens. Stained and coverslipped ThinPrep slides are placed in a cartridge (each cartridge holding 25 slides), and up to 10 cartridges are loaded onto the bench-top imager. The server is electronically linked to one or more Review Scopes in the laboratory. A Review Scope resembles a standard microscope but is augmented with an automated stage, a pod that controls the stage and objectives, and a keypad. The scope also has a camera that reads the slide identifier when the slide is loaded onto the stage. If no abnormal cells are found Automated Screening Historical Overview Automated cytology screening devices have been under development since the 1950s. The first computerized screening system was developed in the United States by Airborne Instruments Inc. The difficulty of the task was soon appreciated, especially the inherent problems with analyzing smears prepared in the conventional manner. AftertheThinPrepslideshave been imaged on the Imager, they are brought to the microscope for location-guided review. This can be done using the "Autoscan" function on the Review Scope, with preset, customized user screening preferences. Truth adjudication was performed by expert review of all abnormal cases and a proportion of negative slides. In this mode, the device is used in the initial screening of smears: it identifies up to 25% of slides as requiring "no further review" based on a low slide score. Slides below a cutoff are considered "no further review," and those above the cutoff are triaged for full manual review. Any slide deemed unsuitable for analysis because of preparation or coverslipping problems requires manual review. It is up to the laboratory to define what constitutes a Pap test result from a high-risk patient. In this method, a low-scoring "no further review" population of slides is archived without further manual screening, whereas the higher scoring "review" population of slides undergoes guided screening as described above. Accuracy and Reproducibility the sensitivity of cytology for detecting preinvasive squamous and glandular lesions is difficult to establish, but it is clearly far from perfect. The few relatively unbiased studies show that the mean sensitivity of the Pap test is 47% (range 30% to 80%), and the mean specificity is 95% (range 86% to 100%). The interobserver reproducibility of cytologic interpretations is also less than perfect. In other laboratories it was replaced (or supplemented) by descriptive terms borrowed from histologic classifications of squamous lesions. Squamous cancer precursors were originally divided into carcinoma in situ, a high-risk lesion of immature, undifferentiated atypical cells, and dysplasia (subdivided into mild, moderate, and severe), the latter a lower-risk lesion of more mature squamous cells. The 2014 Bethesda System, like its predecessors, recommends a specific format for the cytology report, including an explicit statement on the adequacy of the specimen, a general categorization, and an interpretation/result. In 1988, the Bethesda System proposed three categories for specimen adequacy: "satisfactory," "less than optimal" (renamed "satisfactory but limited by. Nevertheless, the 2014 Bethesda System advocates mentioning the presence or absence of a transformation zone component and permits comments on obscuring elements. It is easy to determine whether a specimen is adequate or unsatisfactory in most cases. Slides received without patient identification or broken beyond repair should be rejected as unsatisfactory. An appropriately labeled smear with an adequate complement of well-preserved squamous and endocervical cells is clearly satisfactory. The cellularity of the squamous cell component is estimated; laboratories are not expected to count individual cells. In borderline cases, techniques are available for estimating adequacy: reference images for smears and a spot-counting procedure for liquidbased preparations. The average number of squamous cells is then compared against tables that take into account the objective, the eyepiece field number, and the diameter of the circle that contains cellular material. An additional slide can be prepared when the initial slide has insufficient cellularity, in the hopes that the new slide will be more cellular. In certain clinical settings, particularly in women with atrophy and after radiation therapy to the pelvis, a lower number may be adequate. In these situations, cytologists are expected to use their judgment when evaluating adequacy rather than rigidly applying the numerical criteria. An endocervical component is considered present if 10 or more endocervical or squamous metaplastic cells, either isolated or in groups, are present. The data on the endocervical component as a measure of sample adequacy are contradictory. Currently, a smear without endocervical cells is not considered unsatisfactory, although the absence of an endocervical/transformation zone component is mentioned as a "quality indicator. Specimens are categorized according to the most significant abnormality identified. Method for Estimating the Adequacy of the Squamous Component of Liquid-Based Preparations. Interpretation and Results Recommended terminology for reporting findings is listed in Table 1. Mentioning nonneoplastic findings, other than organisms, is optional, given that many clinicians desire the Pap test report to be as concise as possible. Nevertheless, many cytologists believe it is important to document that certain findings were interpreted as benign, particularly those that can mimic a neoplasm. In Squamous Cells the ectocervix is lined by a stratified squamous epithelium that matures under the influence of estrogen. Intermediate cells have a larger nucleus measuring 8 m in diameter, which is not pyknotic but instead has a finely granular texture. Superficial and intermediate cells are the predominant cells in cytologic samples from women of reproductive age. Because a Pap test does not usually scrape off the entire thickness of the epithelium but only the upper few layers, immature cells near the base of a mature epithelium are not usually sampled.
Acer nikoense (Nikko Maple). Benadryl.
- How does Nikko Maple work?
- Are there safety concerns?
- Eye conditions and liver disorders.
- What is Nikko Maple?
- Dosing considerations for Nikko Maple.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=97091
Purchase benadryl 25 mg mastercard
These complications reinforce the need to evaluate patients carefully for swallowing disorders prior to performing a capsule endoscopy study allergy testing questionnaire discount benadryl online master card. The risk of retention of the capsule endoscope in patients with known or suspected Crohn disease. Colon Capsule Endoscopy Colonic capsule endoscopy has been introduced as an alternative method for performing screening colonoscopy. However, studies looking at the ability of colon capsule endoscopy to detect polyps have had variable results. In a meta-analysis that included 626 patients, the colon capsule had a sensitivity of 73% and a specificity of 89% for detecting polyps. In a subsequent study with 545 patients, the sensitivity of capsule endoscopy for polyps 6 mm or larger was 39% and the specificity was 88%. A metaanalysis evaluating the accuracy of colon capsule endoscopy in detecting polyps. Accuracy of capsule colonoscopy and computed tomographic colonography in individuals with positive results from the fecal occult blood test. However, in many instances there is poor visualization of areas of mucosa due to quick passage, inability to insufflate, tangential views, and debris. Additionally, in approximately 15% of cases, the capsule does not reach the colon prior to the battery running out (currently about 8 hours). Complications, limitations, and failures of capsule endoscopy: a review of 733 cases. Push enteroscopy with an overtube, however, can at most be advanced to 160 cm beyond the ligament of Treitz. With the advent of wireless capsule endoscopy, it is now possible to visualize the entire length of the small bowel, but capsule endoscopy lacks biopsy and therapeutic capability. Lesions detected by capsule endoscopy that are beyond the reach of a push enteroscope can now be evaluated using deep small bowel enteroscopy. Total enteroscopy is possible in some cases with balloon- or spiral-assisted enteroscopy and has the advantage of allowing for biopsies and for therapeutic interventions. For a retrograde (per anus) study, a standard colonoscopy preparation is employed. It has also been used to biopsy and dilate small bowel strictures, to screen for disease recurrence in patients with a history of small bowel malignancies, to evaluate patients with refractory celiac disease, and to retrieve foreign bodies (eg, video capsules). In patients who have undergone Roux-en-Y gastric bypass, it can visualize the defunctionalized stomach and gain access to the bile and pancreatic ducts. The European experience with double balloon enteroscopy: indications, methodology, safety and clinical impact. Double balloon enteroscopy-The double balloon enteroscopy system is composed of an enteroscope, an overtube, and a balloon pump controller. The examination can be carried out using conscious sedation or propofol, although some centers prefer general anesthesia due to the length of the study and the potential for patient discomfort. During an antegrade study, the scope and overtube are advanced until both are within the duodenum. The balloon on the end of the overtube is then inflated to anchor the small bowel. When the scope can no longer be advanced, the balloon at the tip of the scope is inflated, again anchoring Wireless Capsule endosCopy & deep small BoWel enterosCopy 425 3. Spiral enteroscopy-Spiral enteroscopy uses an enteroscope designed for double or single balloon enteroscopy and an over-tube with a soft, raised helical spiral. The system was developed as an alternative to balloon-assisted enteroscopy in the hope that it would be a simpler and faster method. Reported insertion depths are similar to those seen with antegrade studies performed using balloon-assisted enteroscopy. The balloon on the overtube is then deflated and the overtube is advanced until it reaches the end of the scope. With both balloons inflated, the scope and the overtube are gently withdrawn until resistance is met. This sequence is repeated until the lesion of interest is reached or until the scope can no longer be advanced. When a retrograde approach is employed, the scope and overtube are advanced until they are both within the terminal ileum, and the same sequence is then carried out. The double balloon enteroscope has a forceps channel that will accommodate biopsy forceps, argon plasma coagulation probes, bipolar hemostasis probes, cytology brushes, Roth nets, snares, and injection needles. Single balloon enteroscopy-The single balloon enteroscopy system is similar to the double balloon system except that instead of employing a balloon on the end of the enteroscope, the tip of the enteroscope is angulated sharply to anchor the scope. The data available on outcomes come primarily from research on double balloon enteroscopy, although results reported for single balloon and spiral enteroscopy are similar. In a study of 1765 patients undergoing double balloon enteroscopy, the diagnostic yield overall was 48%. The yield was highest for patients with an indication of Peutz-Jeghers syndrome (82%), followed by mid-gastrointestinal bleeding (53%), and Crohn disease (47%). It was lowest for patients with an indication of abdominal pain (19%) or diarrhea (16%). A therapeutic procedure was carried out during double balloon enteroscopy in 529 patients (30%). Other interventions included polypectomy (4%), dilation of small bowel stenoses (2%), and injection therapy at bleeding sites (2%). A second study of 353 patients found a similar diagnostic yield of 75% for small bowel lesions. Sixty percent of the patients were being evaluated for suspected small bowel bleeding, 10% had chronic abdominal pain, 9% had a polyposis syndrome, 8% had Crohn disease, and 13% underwent the study for other indications, including foreign body extraction. Endoscopic therapy was performed in 59%, and medical therapy was initiated or changed in 19%. Not surprisingly, the majority of patients who received endoscopic therapy suffered from small bowel bleeding (74%). A comparative evaluation of single balloon enteroscopy and spiral enteroscopy for patients with mid-gut disorders. Perforations have been reported, including multiple perforations following chemotherapy for lymphoma and following small bowel polypectomy. Perforation is also associated with surgically altered gastrointestinal tract anatomy (eg, ileoanal anastomosis or an ileostomy), with a perforation rate in one study of 3% in this setting. The overall major complication rate in the study discussed above of 1765 patients undergoing double balloon enteroscopy was 1. All of the complications in patients undergoing polypectomy occurred after the removal of polyps that were larger than 3 cm. Thus, while the overall rate of complications is low, patients undergoing polypectomy should be advised that there is a significant complication rate associated with the removal of large polyps, as are often seen in Peutz-Jeghers syndrome. However, given that the alternative in these patients is intraoperative enteroscopy, which has a morbidity rate up to 30% and a mortality rate of 2%, deep small bowel enteroscopy is still an attractive option.
Syndromes
- Women may do a monthly breast self-exam.
- Nephrolithiasis (kidney stones)
- Death
- Diabetes
- Adults: not measured
- Women age 19 year and older: 75 mg/day
Discount benadryl 25mg overnight delivery
Ancillary studies to assess for clonality (flow cytometry allergy medicine 11 month old 25 mg benadryl visa, immunocytochemistry) can be invaluable in such circumstances. Squamous-Lined Cysts Squamous-lined cysts include congenital cysts, encompassing dermoid and branchial cleft cysts. Also in this category are the sporadic simple lymphoepithelial cysts, usually found within the parotid glands of middle-aged men. Typically unilateral and solitary, they probably arise from either entrapped salivary duct tissue within intraparotid lymph nodes or from branchial cleft remnants. Lymphoid elements do not help in the distinction from a cystic salivary gland neoplasm, because some neoplasms have a prominent lymphoid infiltrate. Lymphoma can be excluded using flow cytometry, which demonstrates a polyclonal population of lymphoid cells in these benign cystic lesions. Identification of a salivary gland neoplasm rests on the recognition of the characteristic cell type(s) associated with that tumor. Most importantly, a cystic metastatic squamous cell carcinoma must also be considered. Nevertheless, a cystic well-differentiated squamous cell carcinoma is occasionally difficult to distinguish from a benign squamous-lined cyst. Even in the absence of definitive evidence of malignancy, it is prudent to report benign-appearing squamous-lined cysts descriptively and include the differential diagnosis of a developmental and lymphoepithelial cyst. An accompanying explanatory note can emphasize the need for clinical correlation to exclude a more significant lesion and a recommendation that any persistent mass be excised to exclude malignancy. Occasional metaplastic epithelial cells and normal salivary gland cells are also seen. The nonspecific constellation of findings described herein is also seen in some low-grade mucoepidermoid carcinomas, which, like mucoceles and retention cysts, contain muciphages. The following features, typical of a low-grade mucoepidermoid carcinoma, can help distinguish it from one of its benign mimics: a residual mass after aspiration; greater cellularity; more severe cytologic atypia; and at least an occasional cluster of intermediate and epidermoid cells. Mucoepidermoid carcinoma can be mentioned in the differential diagnosis, with an educational note. This approach helps avoid a false-negative interpretation in the case of a low-grade mucoepidermoid carcinoma. Mucin-Containing Cysts the umbrella term mucin-containing cysts refers to a heterogeneous group of lesions that include a malignant neoplasm (mucoepidermoid carcinoma), inflammatory conditions (chronic sialadenitis with mucinous metaplasia), and acquired cysts. Acquired cysts, comprising the mucocele and retention cyst, occur more commonly in the submandibular and sublingual glands than the parotid. Mucoceles are pseudocysts because they lack an epithelial lining, whereas retention cysts are lined by squamous, columnar, or oncocytic epithelium. The remainder of the smear is often hypocellular, with scant or absent acinar cells and scattered groups of ductal cells as are seen in chronic sialadenitis. In the salivary gland, amyloid is also encountered in association with an extramedullary plasmacytoma. This example proved to be a mucocele, but identical findings can be seen in a low-grade mucoepidermoidcarcinoma(Romanowskystain). The most commonly encountered site is the superficial parotid, often the tail of the gland at the angle of the jaw. On physical examination, the nodule is firm, reflecting the abundance of chondromyxoid matrix. When present as individual cells, epithelial cells are indistinguishable from myoepithelial cells. The myoepithelial cells have a variety of appearances: spindle-shaped (the most common), epithelioid, clear-cell, and plasmacytoid. Unlike epithelial cells, myoepithelial cells are commonly found individually, within matrix material, in loose clusters, or in larger, haphazardly arranged clusters. Although the matrix of adenoid cystic carcinoma stains with a similar intensity, the features are otherwise distinctive. In at least two-thirds of cases, the typical constituents are readily appreciated, without unusual features, and the diagnosis is straightforward. A metastasizing mixed tumor is a cytologically benign pleomorphic adenoma in a distant site. Isolated plump spindle-shaped and plasmacytoid myoepithelial cells are scattered about (Romanowskystain). The differential diagnosis in such cases includes basal cell adenoma and adenocarcinoma (in the case of an epithelial-rich lesion) and myoepithelioma (in the case of a myoepithelial-rich lesion). Severe atypia, however, particularly if accompanied by necrosis or mitoses, raises the possibility of carcinoma ex pleomorphic adenoma. The combination of mucinous and squamous metaplasia is especially challenging because it raises the specter of mucoepidermoid carcinoma. The myoepithelial cells of a myoepithelioma are identical to those of a pleomorphic adenoma. Although this error has no clinical consequence, a generic interpretation of a benign "myoepithelial cell-rich neoplasm," under a Neoplasm: Benign heading, accompanied by a differential diagnosis, is prudent in such circumstances. Immunohistochemistry is helpful; although S-100 is diffusely positive in schwannoma and often positive in myoepithelial cells, myoepithelial cells also stain for one or more of the following: p40, p63, keratins, smooth muscle actin, glial fibrillary acidic protein, and calponin. Of these, p40 and p63 have the greatest value among the current immunohistochemical markers of myoepithelial differentiation. An important caveat: p40 and p63 also stain cells showing squamous differentiation. Clear cell myoepithelioma resembles other neoplasms with clear-cell differentiation, like epithelial-myoepithelial carcinoma, acinic cell carcinoma, mucoepidermoid carcinoma, and metastatic renal cell carcinoma. Necrosis, pleomorphism, mitotic activity, coarse chromatin, and prominent nucleoli are distinguishing features. It can exhibit a variety of histologic patterns: solid, tubular, trabecular, membranous, and mixed patterns. More extensive atypia, as in these cases, merits the interpretation "pleomorphic adenoma with atypia. The matrix of a basal cell adenoma stains brightly cyanophilic or eosinophilic with the Papanicolaou stain and basophilic to metachromatic with Romanowskytype stains. The neoplastic cells, of epithelial and myoepithelial derivation, have a "basaloid" appearance. A more specific interpretation than basaloid neoplasm is not possible (Romanowsky stain). This pattern is nonspecific and seen in a variety of matrix-containing basaloid neoplasms (Romanowskystain). A subset of this basal cell adenoma subtype is associated with the autosomal dominant Brooke-Spiegler syndrome. In most instances, however, a basaloid squamous cell carcinoma exhibits overt cytologic features of malignancy, including necrosis, marked atypia, and mitotic activity. The differential diagnosis includes chronic sialadenitis, benign tumors, low-grade malignancies, and high-grade malignancies. The solid variant of adenoid cystic carcinoma, basal cell carcinoma of the skin,125 metastatic and primary small cell carcinomas, polymorphous adenocarcinoma, and other rare malignant basaloid tumors-basaloid squamous cell carcinoma,126-128 and basal cell adenocarcinoma116,129-132-are all in the differential diagnosis. Unlike the other conditions on this list, chronic sialadenitis is typically sparsely cellular and has a background of chronic inflammation. Although cytologic atypia, necrosis, and significant mitotic activity exclude basal cell adenoma, the absence of these malignant features does not exclude a malignancy like adenoid cystic carcinoma119,120 and basal cell adenocarcinoma. Basal cell adenoma, polymorphous adenocarcinoma, epithelialmyoepithelial carcinoma and the solid variant of adenoid cystic carcinoma can contain occasional stromal cylinders like those of the usual type of adenoid cystic carcinoma. Stromal material in basal cell adenomas often surrounds the neoplastic cells, in contrast to adenoid cystic carcinoma, in which the neoplastic cells almost always surround stroma. The matrix of basal cell adenoma can be hyalinized and show dense staining characteristics with the Papanicolaou stain, whereas in adenoid cystic carcinoma the matrix is more typically transparent. Basal cell adenoma/adenocarcinoma occur most commonly in the parotid, whereas polymorphous adenocarcinoma arises almost exclusively in the minor salivary glands. Clinical evidence of malignancy can be helpful in distinguishing among these entities. Pilomatricoma is a skin adnexal tumor that frequently occurs in the head and neck region.
Benadryl 25mg
The spread of blood is limited to one side of the brain due to dural reflections such as the tentorium cerebelli and falx cerebri allergy symptoms yeast order genuine benadryl. Contrast the spread of subdural hematomas to that of epidural hematomas that are limited in their spread due to the sutures. Defined as bleeding into the subarachnoid space usually due to a ruptured cerebral V Subdural hematoma. However, trauma to the head may stretch and rupture a bridging (cerebral) vein, resulting in bleeding into the subdural space (subdural hematoma). Because the damaged vessel is a vein, the increase in intracranial pressure and the effect of compressing the brain is much slower when compared to an epidural hematoma, which is caused by tearing of an artery. As a result, a subdural hematoma may develop over a period of days or even a week. Enlarging the subdural space is one factor that increases the risk ofa subdural hematoma. Forms a sheath around blood vessels as they course into the fissures and sulci and penetrate the brain. Through that circuitry the brain directs movement, processes sensory input, and processes language and communication, learning, and memory. Located in the middle cranial fossa below the lateral sulcus; functions include auditory processing, language recognition, interpretation of visual stimuli, and the formation of new and long-term memories. Suspended from the hypothalamus by the infundibulum and housed in the sella turcica (a depression in the sphenoid bone). The cerebral hemispheres consist of elevations (gyri) and valleys (sulci), with a longitudinal cerebral fissure separating the two cerebral hemispheres. Each cerebral hemisphere is divided into lobes, which correspond roughly to the overlying bones of the skull Frontal lobe. Located in the anterior cranial fossa; contains the primary motor cortex, which regulates motor output (voluntary movement). Additional functions include hypothesizing future consequences from current actions, conscience, short-term memory, planning, and motivation. Positioned between the frontal and occipital lobes above the lateral sulcus; contains the primary sensory cortex, which directs the integrating of sensory input. Located in the posterior cranial fossa above the tentorium cerebelli; contains the primary visual cortex, which is the visual processing center of the brain. The cerebral aqueduct is a portion of the ventricular system and courses through the center of the midbrain to connect the third and fourth ventricles. Located at the level of the foramen magnum; serves as a major autonomic reflex center that relays visceral motor control to the heart, blood vessels, swallowing, respiratory system, and gastrointestinal tract. Arachnoid granulations are projections of the arachnoid mater along the superior sagittal sinus. Each lateral ventricle communicates via the interventricular foramen (of Monro) with the third ventricle. Despite all of these protections, trauma to the brain and spinal cord can still occur and can result in devastating injuries and deficits. In children, this results in hydrocephalus, a condition in which the head enlarges because the skull bones have not yet fused. In adults, however, hydrocephalus is a different challenge because the skull is rigid. A midline narrow space located between the left and right diencephalon below the lateral ventricles. The third ventricle communicates with the fourth ventricle via the cerebral aqueduct (of Sylvius). The internal carotid artery traverses the carotid canal within the petrous part of the temporal bone. The terminal branches of the basilar artery provide vascular supply to the part of the brain base that is superior to the tentorium cerebelli. Courses through the optic canal to supply the retina, orbit, and part of the scalp. Courses superior to the optic chiasma into the longitudinal cerebral fissures and courses along the corpus callosum, providing blood supply to the medial sides of both cerebral hemispheres. The middle cerebral artery sends many branches to the lateral sides of the cerebral hemispheres and central branches into the brain. This configuration of arteries in the circle of Willis provides redundancy for collateral circulation. In other words, if one of the arteries supplying the circle or a section of the circle becomes narrowed or blocked, blood flow from collateral vessels can often preserve blood supply to the brain well enough to avoid the symptoms of ischemia. Therefore, if an end artery becomes narrowed or blocked, ischemia may occur in the region of the brain that is uniquely supplied by that end artery. A balloon-like outpouching of a cerebral arterial wall that is berry shaped (hence, the name). This outpouching most often reflects a gradual weakening ofthe arterial wall as a result of chronic hypertension or arteriosclerosis and places the artery at risk to rupture, causing a stroke. Some cerebral vessels are inherently weak and susceptible to berry aneurysms, such as the arteries associated with the circle of Willis, where small communicating arteries connect larger cerebral arteries (internal carotid, vertebral, and basilar arteries). After penetrating the dura mater, the vertebral arteries then course along the inferior aspect of the medulla oblongata before converging into the basilar artery on the pons. The two vertebral arteries and the basilar artery are often referred to as the "vertebrobasilar system of arteries. Arises from the vertebral arteries, courses along, and supplies the anterior region of the spinal cord. An abnormal collection of blood vessels where a direct connection exists between a supplying artery and a draining vein. Vascular malformation allows high-pressure arterial blood to enter the lower pressure venous structures, causing both structures to dilate. These anomalous connections cause blood to bypass the normal capillary bed (shunting). Bleeding may occur because the thin-walled veins rupture due to the elevated pressures. J B ~White dashed line outlining the cerebral arterial circle (of Willis) Anterior inferior. Like spinal nerves, cranial nerves are bundles of sensory and motor neurons that conduct impulses from sensory receptors and innervate muscles or glands. Innervate skeletal muscles derived from somites, including the extraocular and tongue muscles. Innervate skeletal muscles derived from the branchial arches, including the muscles of mastication and facial expression, and the palatal, pharyngeal, laryngeal, trapezius, and sternocleidomastoid muscles. Innervate involuntary (smooth) muscles or glands, including visceral motor neurons that constitute the cranial outflow of the parasympathetic division of the autonomic nervous system. The preganglionic neurons originate in the brainstem and synapse outside the brain in parasympathetic ganglia. A neuron is a single sensory or motor nerve cell, whereas a nerve is a bundle of neuronal fibers (axons). Cranial nerves have three types of sensory and three types of motor neurons, known as modalities. Therefore, a nerve may be composed of a combination of sensory or motor neurons. Innervate almost all of the structures of the head and neck, such as the skin, mucous membranes, muscle, and glands derived from the pharyngeal arches. However, after coursing through their respective optic canals, the right and left optic nerves engage in a redistribution of axons at the optic chiasma, located just anterior to the pituitary stalk. The optic chiasma is created by neurons from the nasal half of each retina crossing over to the opposite side. The nerves ascend through the cribrifonn foramina of the ethmoid bone to reach the olfactory bulbs. The olfactory neurons synapse with neurons in the bulbs, which course to the primary and association areas of the cerebral cortex.
Discount 25mg benadryl with visa
The splanchnic vasodilation causes increased capillary pressure and permeability that contribute to ascites allergy shots dust mites cheap benadryl 25mg on line. Splanchnic arterial vasodilation also results in increased venous return and increased cardiac output as it acts as an arteriovenous fistula. This, in turn, can result in pulmonary vasodilation and infrequently results in the hepatopulmonary syndrome. A large volume of blood enters and leaves the portal venous system rapidly due to decreased splanchnic resistance. The hyperdynamic circulation leads to vasodilation of the pulmonary circulation to allow increased venous return. Initially, plasma volume, cardiac output, and heart rate increase because the splanchnic circulation behaves functionally as a large arteriovenous fistula. With progression of liver disease, portal pressure increases further, as does splanchnic vasodilation. The renin-angiotensin-aldosterone system and sympathetic nervous system become activated in parallel with intense reduction in urinary sodium excretion to values of less than 10 mEq/24 h. Symptoms and Signs Patients with decompensated cirrhosis and ascites often exhibit peripheral stigmata of chronic parenchymal liver disease. The triad of findings of hepatomegaly, ascites, and increased venous collateral of the anterior abdominal walls always indicates the presence of portal hypertension. A diagnosis of cirrhosis can be made on the basis of two physical findings and two laboratory findings. The two physical findings are asterixis and ascites; the two laboratory findings are hypoalbuminemia (serum albumin levels <2. Imaging Studies In patients with ascites it is important to obtain an ultrasound examination not only to confirm the diagnosis of ascites, but also to assess the patency of the portal and hepatic veins. This is because portal or hepatic vein thrombosis can occur in the setting of cirrhosis of the liver. Ultrasonography can detect as little as 100 mL of fluid in the peritoneal cavity whereas on physical examination ascitic fluid volume usually needs to exceed 2 L to be evident. Patients with cirrhosis can develop umbilical hernias when long-standing ascites is present. Laboratory Findings Patients with ascites should always be evaluated with diagnostic paracentesis to determine the cause. In patients with cirrhotogenic ascites, measurement of urine electrolytes is important. If ascites is due to cirrhosis, urine sodium excretion will be low (eg, frequently <10 mEq/24 h) and potassium excretion increased to a value of greater than 30 mEq/24 h. This can also be used as a baseline measurement to determine the effectiveness of diuretic therapy as distal-acting agents such as spironolactone frequently cause a reversal of the abnormal sodium-potassium ratio. Management of Sodium Balance Because sodium retention is a major factor in the development of ascites, a key goal of therapy is the attainment of a negative sodium balance. Accordingly, appropriate sodium restriction is very important in the treatment of ascites and in maintenance of cirrhotic patients who are ascites free. In older studies severe salt restriction (22 mmol/24 h) was associated with a shorter time for resolution of ascites. Patients need detailed dietary instructions as to hidden sources of sodium in their diet. Bed rest often facilitates diuresis because upright posture activates sodium-retaining systems and impairs renal profusion and sodium excretion. It is usually not necessary to restrict water intake unless the serum sodium is less than 125 mEq/dL. Water restriction should not be prescribed if fever, sepsis, bleeding, or azotemia are present. It is reasonable to expect patients with cirrhosis and ascites who have been placed on a diuretic regimen and sodium restriction to lose between 0. Losses greater than this can occur, especially with brisk diuresis, and may precipitate an episode of oliguric hepatic failure. Diuretics are usually required in patients with ascites, especially those with moderate to severe ascites who retain sodium avidly and for whom sodium restriction will not be sufficient to retain negative sodium balance. This can be increased cautiously to 400 mg/day, but one needs to watch for hyperkalemia and metabolic acidosis. An effect of spironolactone can be noted as early as 3 days after initiation of treatment. Effective therapy with spironolactone usually results in a reversal of the potassiumsodium abnormalities in the urine, with an increase of sodium excretion to greater than 10 mEq/day and a decrease in potassium secretion. This would suggest that the patient is obtaining salt-laden foods in the hospital or surreptitiously ingesting large amounts of fluid (eg, >2500 mL/24 h). In this regard, patients may also be ingesting large amounts of ice, as one pint of ice intake yields over 800 mL of fluid. American Association for the Study of Liver Diseases Postgraduate Course Syllabus. Definition and management of refractory ascites- Five percent of cirrhotic patients with ascites develop refractory ascites. The following criteria are usually employed to establish diagnosis of refractory ascites. Furosemide given intravenously as a bolus results in higher initial concentrations of the drug being delivered to the renal tubule, but this may not be sustained. Accordingly, a furosemide drip infusing 20 mg/h can be effective in restoring diuretic responsiveness by achieving sustained elevated furosemide levels in the renal medulla. In this setting, it is reasonable to consider adding either metolazone or hydrochlorothiazide, which acts on the ascending limb, in addition to administering furosemide at 20 mg/h intravenously. The rationale for including albumin is that studies have indicated that side effects occurred in 30% of patients undergoing large-volume paracentesis alone compared with 16% in patients who had paracentesis plus albumin replacement. Large-volume paracentesis is more effective than diuretics in eliminating ascites and shortening the duration of hospitalization. However, it should be emphasized that this procedure does not eliminate the need for continued diuretic therapy. Cumulative probabilities of transplantfree survival and of hepatic encephalopathy were estimated using Kaplan-Meyer methodology. In two earlier multicenter, randomized trials, the efficacy of tolvaptan was evaluated in patients with chronic euvolemic or hypervolemic hyponatremia. In two earlier multicenter, randomized, double-blind, placebo-controlled trials, oral tolvaptan did effect an increase in serum sodium from baseline to day 4. However, in a recent, large randomized controlled trial which was specific for cirrhotics, 1200 patients with uncomplicated ascites were evaluated. It was concluded that satavaptan is not clinically beneficial in the long-term management of ascites in patients with cirrhosis. Because of the risk of side effects it has been recommended that the use of tolvaptan be limited to the inpatient setting to correct severe hyponatremia (Na+ <125 mEq/L). Transjugular intrahepatic portosystemic shunt for refractory ascites: a meta-analysis of individual patient data. Complications of Diuretic Therapy Significant complications can result from inappropriate use of diuretic therapy. One should be very careful about administering diuretics to cirrhotic patients hospitalized with marked wasting, cachexia, and tense ascites, as oliguric hepatic failure can be triggered in these fragile patients.