Stendra 200mg for sale
The plaintiff must prove causation by showing of a reasonably close causal connection between the alleged negligent act (or omission) and the resulting injury symptoms shingles purchase 200mg stendra mastercard. However, in addition, the alleged act of malpractice must be shown to also be the proximate cause. The concept of legal causation can be difficult for physicians to comprehend because it does not refer to a strict scientific causation. Causation in fact is defined using the "but for" test, which requires a showing that "but for" the act or failure to act, the complication or injury would not have occurred. Did You Know In medical malpractice cases, physicians are generally not liable for negligence for errors in judgment, but can be liable for care that falls outside recognized standards of good medical practice, defined as care that a reasonably competent and skilled health care professional, with similar training, would provide under similar circumstances. The term damages attempts to quantify the actual ascertainable injuries suffered by the plaintiff. The term damages is broad and encompasses a range of financial, physical, and emotional injuries. The intent of awarding compensatory damages in a tort action is to "make the plaintiff whole again," which, in most medically related injuries, is an obvious legal fiction but nonetheless the best attempt at compensation. Special damages include economic injuries such as subsequent hospitalization or rehabilitation costs, costs of assistance or custodial care, lost wages, or lost earning capacity. General or noneconomic damages address emotional injuries such as loss of companionship (consortium), mental anguish, grief and pain, and suffering. Punitive, or exemplary damages, may also be sought if the alleged conduct can be shown to be wanton and willful, reckless, fraudulent, intentional, grossly negligent, or malicious. In the event that the elements of medical negligence cannot be proven or the case is relatively straightforward, a theory of medical liability can also be premised in the doctrine of res ipsa loquitur, which literally translates as "the facts speak for themselves. However, in general, a case can be submitted to the jury on the theory of res ipsa loquitur only when the plaintiff can establish that (a) the event is one that ordinarily does not occur in the absence of negligence; (b) the event was caused by an agency or instrumentality within the exclusive control of the defendant; and (c) the event cannot have been due to any voluntary action or contribution on the part of the plaintiff. Examples of res ipsa loquitur claims include retained instruments, positioning injuries, and intraoperative burns and do not usually require expert testimony. Medical malpractice insurance indemnity policies provide insurance coverage for claims arising from alleged malpractice. The malpractice carrier has two principal obligations to the insured: the duty to defend and the duty to indemnify. In order to provide a legal defense, an insurance carrier will typically retain knowledgeable and experienced defense counsel and pay the legal fees on behalf of the defendant physician. The duty to indemnify requires the carrier to pay the amount of a settlement or judgment on a covered claim within the set policy limits. Occurrence policies cover incidents that occur during the policy period, even if it is reported in the future following expiration or discontinuance of that policy. Claims-made policies will only cover occurrences where both the event and the claim occur during the life of the policy. Because the average malpractice claim is made 1 to 2 years following an incident, claims-made policies usually require that the physician purchase either "nose" or "tail" coverage in order to maintain coverage during job or insurer-to-insurer transitions. European Federation of Internal Medicine Medical professionalism in the new millennium: A physician charter. An anesthesiologist working in a mass casualty incident triages patients to settings of emergent care, delayed care, or expectant care. An anesthesiologist provides the highest level of care, without regard to personal gain or societal interests. A healthy 2-month-old, former preterm boy is undergoing an elective inguinal hernia repair under general anesthesia. A preoperative "timeout" takes place for all members of the team to review the surgical safety checklist. Prior to administering a local anesthetic field block, the surgeon, nursing staff, and anesthesiologist review and agree on the correct drug and dose for the child. When the surgeon and anesthesiologist disagree on the maximum local anesthetic dose for the child, the procedure is briefly halted to consult with the hospital pharmacy. On her first day in her anesthesiology clerkship, the medical student assisting the anesthesiologist notices a large volume of air in the intravenous tubing, but refrains from telling the anesthesiologist due to her insecurity. A healthy, mentally competent, 55-yearold married father of three teenage children is about to undergo an elective open repair of an iliac artery pseudoaneurysm. Contact hospital risk management to obtain a court order to transfuse blood products, should unexpected life-threatening bleeding occur intraoperatively. Discuss the issue with the patient to confirm his wishes (even if doing so might put his life in danger) and to discuss potential alternative treatments. The National Practitioner Data Bank collects and releases information related to the professional conduct and competence of physicians and other health care providers, including which of the following Medical malpractice is a type of negligence that is argued in civil court, as opposed to criminal court. Civil malpractice disputes are generally filed in state trial courts and final judicial authority generally rests in the state court of appeals. Civil malpractice disputes can be filed in federal courts only in specific instances where federal issues are involved. Once a defendant physician receives a proper summons, the defendant has only a limited time to respond to the complaint. Occurrence policies only cover occurrences where both the event and the claim occur during the life of the policy. Claims-made policies usually require the physician to purchase a "tail" policy to maintain malpractice coverage for incidents that occurred during the life of the policy but the malpractice claim was filed after the policy ended. Insurance carriers are not required to pay the amount of a settlement or judgment, even if the amount is within set policy limits. A 75-year-old mentally competent woman with no living relatives is scheduled to undergo hip replacement surgery and has granted legal and documented "simple power of attorney" to her otherwise unrelated and mentally competent housemate. Advances in surgical interventions along with increased incidences of respiratory failure due to polio epidemics led to an increased demand for physicians specializing in the care of critically ill patients, especially patients with respiratory failure. However, <10% of practicing intensivists are anesthesiologists, and the majority of intensivists in the United States continue to be pulmonary physicians. Fortunately for those interested in this specialty, the future need for intensivists is expected to be much greater than the supply. New technologies, equipment, and medications along with increased understanding of diseases and pathophysiology allow for the treatment of increasingly ill patients. More recently, as the economics of health care delivery have received increased attention, the focus on delivering evidence-based, cost-effective care has also increased. Although the entire spectrum of critical care is beyond the scope of this chapter, widely applicable aspects of contemporary critical care are reviewed here. The second part of the chapter provides an overview of the management for some commonly encountered diagnoses. The entire chapter focuses on evidencebased practices that may improve both patient outcomes and health care system performance in the perioperative setting. Staffing Advances in medical and surgical therapeutics have increased the complexity of care for an aging and increasingly ill population. It has become clear that providing the best care for such a population requires a knowledge base and skill set that are highly specialized and that involving intensivists in the care of critically ill patients is desirable. Patient outcomes appear to be further improved by the addition of multidisciplinary providers to intensivist led teams. These practices significantly reduce costs and medication-related adverse events and are also associated with decreased patient mortality (2). Considering the potential benefits and the minimal economic investment required for checklist implementation, their use is strongly recommended. In fact, many of the care processes discussed in this chapter commonly appear on checklists and should be considered for every patient, every day. Resource Management In 2014, the Critical Care Societies Collaborative released a list of "Five Things Physicians and Patients Should Question" in critical care as part of the Choosing Wisely campaign. The campaign is designed to reduce unnecessary interventions that lack cost-effectiveness and has been supported by many medical specialties. At the top of the list is a recommendation to not order diagnostic studies (chest x-rays, blood gases, blood chemistries and counts, and electrocardiograms) at regular intervals. Compared with the practice of ordering tests only to answer clinical questions or when doing so will directly affect management, the routine ordering of tests increases costs, does not benefit patients, and may in fact harm them. Opioids are the primary modality of treating moderate to severe pain in critically ill adults. However, they have undesirable side effects including nausea, constipation, respiratory depression, and alteration of mental status. When titrated to similar endpoints, there is not one opioid medication that has been shown to be superior to others. In order to reduce opioid-related side effects, nonopioid analgesics such as acetaminophen, nonsteroidal anti-inflammatory drugs, local anesthetics, ketamine, and -aminobutyric acid analogues may be used in conjunction with opioids.
Buy stendra 100mg without a prescription
Some of the preganglionic bers in the prevertebral plexus do not synapse in the sympathetic ganglia of the plexus treatment 2 degree burns purchase on line stendra, but pass through the system to the adrenal gland where they synapse directly with cells of the adrenal medulla. These cells are homologues of sympathetic postganglionic neurons and secrete adrenaline and noradrenaline into the vascular system. Preganglionic sympathetic bers may synapse with postganglionic motor neurons in ganglia and then leave the ganglia medially to innervate thoracic or cervical viscera. They may ascend in the trunk before synapsing; after synapsing, the postganglionic bers may combine with those from other levels to form named visceral nerves, such as cardiac nerves. Often, these nerves join branches from the parasympathetic system to form plexuses on or near the surface of the target organ; for example, the cardiac and pulmonary plexuses. Spinal cord levels T1 to T5 mainly innervate cranial, cervical, and thoracic viscera. The preganglionic bers in these nerves are derived from spinal cord levels T5 to L2. Ce rvic al Sympathetic cardiac nerves Sympathetic trunk Gray ramus communicans T1 to T4 Cardiac plexus Sympathetic cardiac nerves White ramus communicans 26. Like the visceral motor nerves of the sympathetic part, the visceral motor nerves of the parasympathetic part generally have two neurons in the pathway. Cranial nerve preganglionic parasympathetic bers Sacral preganglionic parasympathetic bers In the sacral region, the preganglionic parasympathetic bers form special visceral nerves (the pelvic splanchnic nerves), which originate from the anterior rami of S2 to S4 and enter pelvic extensions of the large prevertebral plexus formed around the abdominal aorta. These bers are distributed to pelvic and abdominal viscera mainly along blood vessels. Postganglionic bers leave the ganglia, join the branches of the trigeminal nerve [V], and are carried to target tissues (salivary, mucous, and lacrimal glands; constrictor muscle of the pupil; and ciliary muscle in the eye) with these branches. These branches contribute to plexuses associated with thoracic viscera or to the large prevertebral plexus in the abdomen and pelvis. When present, postganglionic parasympathetic neurons are in the walls of the target viscera. Visceral sensory bers that accompany sympathetic bers are mainly concerned with detecting pain. Visceral sensory bers accompanying sympathetic bers Visceral sensory bers accompanying parasympathetic bers Visceral sensory bers follow the course of sympathetic bers entering the spinal cord at similar spinal cord levels. However, visceral sensory bers may also enter the spinal cord at levels other than those associated with motor output. Visceral sensory bers in the vagus nerve [X] include those from cervical viscera, and major vessels and viscera in the thorax and abdomen. Visceral sensory bers from pelvic viscera and the distal parts of the colon are carried in S2 to S4. Usually, this happens when the pain information comes from a region, such as the gut, which has a low amount of sensory output. These afferents converge on neurons at the same spinal cord level that receive information from the skin, which is an area with a high amount of sensory output. As a result, pain from the normally low output region is interpreted as coming from the normally high output region. Pain is most often referred from a region innervated by the visceral part of the nervous system to a region innervated, at the same spinal cord level, by the somatic side of the nervous system. For example, irritation of the peritoneum on the inferior surface of the diaphragm, which is innervated by the phrenic nerve, can be referred to the skin on the top of the shoulder, which is innervated by other somatic nerves arising at the same spinal cord level. The enteric system the enteric nervous system consists of motor and sensory neurons and their support cells, which form two interconnected plexuses, the myenteric and submucous nerve plexuses, within the walls of the gastrointestinal tract. Each of these plexuses is formed by: ganglia, which house the nerve cell bodies and associated cells; and bundles of nerve bers, which pass between ganglia and from the ganglia into surrounding tissues. Neurons in the enteric system are derived from neural crest cells originally associated with occipitocervical and sacral regions. Interestingly, more neurons are reported to be in the enteric system than in the spinal cord itself. Sensory and motor neurons within the enteric system control re ex activity within and between parts of the gastrointestinal system. These activities can occur independently of the brain and spinal cord, but can also be modi ed by input from preganglionic parasympathetic and postganglionic sympathetic bers. Preganglionic s ympathetic Pos tganglionic s ympathetic Preganglionic paras ympathetic Vis ceral afferent Vagal afferent Prevertebral s ympathetic ganglion Blood ves s el Mes entery Longitudinal mus cle layer Circular mus cle layer. Peritoneum Myenteric plexus Submucos a mus cle Submucous plexus Submucos a Ente ric ne rvo us s ys the m 29 the Body Nerve plexuses Nerve plexuses are either somatic or visceral and combine bers from different sources or levels to form new nerves with speci c targets or destinations. These plexuses include cardiac and pulmonary plexuses in the thorax, and a large prevertebral plexus in the abdomen anterior to the aorta, which extends inferiorly onto the lateral walls of the pelvis. The massive prevertebral plexus supplies input to and receives output from all abdominal and pelvic viscera. Somatic plexuses Major somatic plexuses formed from the anterior rami of spinal nerves are the cervical (C1 to C4), brachial (C5 to T1), lumbar (L1 to L4), sacral (L4 to S4), and coccygeal (S5 to Co) plexuses. Except for spinal nerve T1, the anterior rami of thoracic spinal nerves remain independent and do not participate in plexuses. The back also contains the spinal cord and proximal parts of the spinal nerves, which send and receive information to and from most of the body. The skull, scapulae, pelvic bones (ileum, ischium, pubis), and ribs also contribute to the bony framework of the back and provide sites for muscle attachment. Next are ve sacral vertebrae fused into one single bone called the sacrum, which articulates on each side with a pelvic bone and is a component of the pelvic wall. Fus ed cos tal element Foramen trans vers arium 7 Cervical vertebrae Rib 12 Thoracic vertebrae. Inferior to the sacrum is a variable number, usually four, of coccygeal vertebrae, which fuse into a single small triangular bone called the coccyx. Typical vertebra A typical vertebra consists of a vertebral body and a posterior vertebral arch. Extending from the vertebral arch are a number of processes for muscle attachment and articulation with adjacent bone. The vertebral body is the weightbearing part of the vertebra and is linked to adjacent vertebral bodies by intervertebral discs and ligaments. The size of vertebral bodies increases inferiorly as the amount of weight supported increases. The vertebral arch forms the lateral and posterior parts of the vertebral foramen. The vertebral foramina of all the vertebrae together form the vertebral canal, which contains and protects the spinal cord. Superiorly, the vertebral canal is continuous, through the foramen magnum of the skull, with the cranial cavity of the head. Superior ve rte bral notch Vertebral body Pedicle Superior articular proces s Trans ve rs e proce s s (fus ed rib ele ment) Lamina Ve rtebral a rch Inferior vertebral Infe rior notch articular proces s Spinous proces s. The two laminae are at sheets of bone that extend from each pedicle to meet in the midline and form the roof of the vertebral arch. A spinous process projects posteriorly and inferiorly from the junction of the two laminae and is a site for muscle and ligament attachment. A transverse process extends posterolaterally from the junction of the pedicle and lamina on each side and is a site for muscle and ligament attachment and articulation with ribs in the thoracic region. Also projecting from the region where the pedicles join the laminae are superior and inferior articular processes. Between the vertebral body and the origin of the articular processes, each pedicle is notched on its superior and inferior surfaces. These superior and inferior vertebral notches participate in forming intervertebral foramina. When viewed from above, the atlas is ring shaped and composed of two lateral masses interconnected by an anterior arch and a posterior arch. The superior articular facets are bean shaped and concave, whereas the inferior articular facets are almost circular and at. The atlanto-occipital joint allows the head to nod up and down on the vertebral column. The posterior surface of the anterior arch has an articular facet for the dens, which projects superiorly from the vertebral body of the axis. The dens is held in position by a strong transverse ligament of atlas posterior to it and spanning the distance between the oval attachment facets on the medial surfaces of the lateral masses of the atlas.
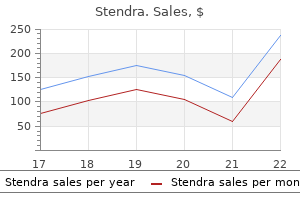
Buy cheap stendra 200 mg
The likelihood of subsequent development of invasive mole or choriocarcinoma is much lower for a partial mole than for a complete mole medications for bipolar buy cheap stendra. A characteristic fetal anomaly with triploidy is 3-4 syndactyly of the digits of the hands. The patient may not have much uterine enlargement, and vaginal bleeding may be the first clue to its presence. Metastases are common, particularly to the lungs distantly and vagina locally, and chemotherapy results in a near-100% cure rate. Such a condition is usually of no major consequence in utero, but it could lead to a greater chance for cord trauma with tearing of one of the vessels and bleeding during the delivery process. By itself, the lack of one umbilical artery, which may occur from agenesis or atrophy, has minimal impact on the developing fetus. Less than 1% of singleton and about 5% of twin live births are accompanied by a two-vessel cord. The significance of this umbilical cord anomaly is its association with other fetal anomalies. Observation of a two-vessel cord on inspection of the placenta at the time of delivery should prompt one to look carefully for additional anomalies in a newborn. A true knot is uncommon but could potentially constrict the blood vessels and lead to fetal demise. The consistency of the cord is like a rubber band, difficult to completely tighten. An umbilical cord pseudoknot (lower panel) is quite common and is an incidental finding. It is an exaggerated loop of one umbilical artery, because it is longer than the vein. The abnormal vessel shown here has the shape of a clothoid loop, which should be recognizable to aficionados of roller coaster rides, because this loop maintains lower, constant gravitational force in transit around the loop. This is usually an incidental finding, but a nuchal cord could interfere with descent through the birth canal during delivery and increases the risk for umbilical cord trauma or constriction of the blood flowing through the cord. The cause of the demise in this case is the marked twisting, or torsion, of the umbilical cord. Torsion may result from increased fetal movement, which abnormally lengthens the cord, allowing the fetus to rotate more freely. This represents the consequence of extensive, diffuse fibrin deposition, associated with a condition known as maternal floor infarction, and sometimes called a "gitterinfarkt. The amount of fibrin in this condition is far greater than the scattered, small deposits of intervillous fibrin regularly observed within a term placenta. This condition is uncommon, but it has a tendency to recur in subsequent pregnancies. Some cases may be associated with maternal coagulopathies, such as antiphospholipid syndrome. Syncytial knots may increase in number in the placenta during the first week after demise. Meconium spillage is a complication occurring at or near term, typically when there is fetal distress with loss of anal sphincter tone and passage of meconium into amniotic fluid. A clue to this occurrence is greenish staining of fetal skin or fetal surface of the placenta as shown here. Evidence of fetal distress, followed by observation of greenish staining to the fetal or placental surfaces, should raise suspicion for meconium spillage. Orange-brown balls of meconium (shaped like a rugby ball) and numerous flattened squames or desquamated fetal skin cells that are found in the amnionic fluid are shown here within alveoli. Meconium is an irritant that leads to respiratory distress and chemical pneumonitis. At birth, tracheal suction and lung lavage may be useful to help remove the meconium. In most cases of vulvar disease, the Paget cells are not associated with an underlying malignancy. It is difficult to determine how far these cells extend in the skin, so recurrences are common after wide excision. At the right the epithelium is convoluted and the cells are shorter, crowded, and with nuclei showing hyperchromatism. Cervical adenocarcinomas are less common than squamous carcinomas, accounting for 15% of cervical malignancies. Called sarcoma botryoides, this is a rare form of embryonal rhabdomyosarcoma, found most often in infant girls and girls younger than age 5. They arise from preexisting leiomyomata and have a similar microscopic appearance, with low mitotic count. Note the two pale granulomas here, including a large Langhans giant cell at the upper right. Disseminated Mycobacterium tuberculosis infections may involve the female genital tract, including the fallopian tube. The large epithelial cells have abundant clear cytoplasm that resembles hypersecretory gestational endometrium. They may occur in association with ovarian endometriosis or endometrioid carcinoma, so that they are likely variants of endometrioid adenocarcinoma. Note the abundant fibrous stroma between the smaller cystic areas lined by various epithelia, including serous, mucinous, and transitional (Brenner). Shown here is a pure hilus cell tumor resembling the male Leydig cell tumor, derived from clusters of polygonal cells arranged around hilar vessels. Note the large lipid-laden Leydig cells with distinct borders, and corpus albicans at the left. Patients have masculinization with hirsutism, voice changes, and clitoral enlargement. These tumors are usually grossly solid, without the prominent skin and hair of a mature teratoma. Lower genital tract, brain, lung, liver, kidney, and gastrointestinal tract are the most common sites for metastases, and this defines a higher stage. Even metastases can respond to chemotherapy, and the cure rate can still approach 75%. Despite the invasion, most of these lesions are self-limited and can be removed by curettage after pregnancy. There is continuing thrombosis and fibrosis with shrinkage of vessels, along with hyalinization of the decidual plate, which is eventually shed as the endometrium regenerates. The placenta separates during delivery above the decidua basalis and below the Nitabuch fibrin membrane. A lesion smaller than 5 cm in a third-trimester placenta might not significantly compromise placental function, because of the large reserve capacity for fetal vascular exchange. If the mass is not large or not central in location, it may be incidental, because the placenta has significant reserve capacity. The vessels vary in size, are lined by benign endothelial cells, but are not large. This vascular hyperplasia in the terminal chorionic villi is likely caused by prolonged low-grade hypoxia with uteroplacental abnormalities. These vessels are not bathed by maternal blood, so there is no effective exchange of gas or nutrients, and so a region of chorangiosis is nonfunctional. This incidental finding has no clinical significance and must be distinguished from amnion nodosum. These nodules represent foci of precipitated fetal cells and vernix caseosa along with overgrowth of the amniotic epithelium and embedded desquamated fetal skin cells to produce the small nodules. Amnion nodosum is more likely to occur when there is oligohydramnios (too little amnionic fluid). There is an increased incidence of premature delivery, oligohydramnios, abruptio placentae, and intrauterine fetal demise associated with this condition. Macromastia may occur unilaterally or bilaterally with increased sensitivity to hormonal stimulation and may be called juvenile hypertrophy when it occurs at the time of puberty. Rarely, a supernumerary breast may produce a subcutaneous mass anywhere from the axilla to the perineum.
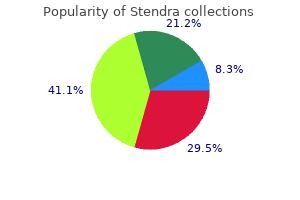
Purchase stendra 200 mg visa
These lesions are symmetrically distributed treatment xanthelasma eyelid purchase stendra, most often at the elbows and wrists, or the glans penis in men. The linear arrangement of the lichenoid lesion at the left is an example of the Koebner phenomenon (also occurring with psoriasis), in which lesions appear on the skin at the sites of trauma. White dots or lines known as Wickham striae appear at the right in papular lesions. Skin lesions typically spontaneously resolve in 1 to 2 years, leaving hyperpigmented areas where the lesions were present. Nail findings (left panel) occurring in 10% of patients include longitudinal grooving and ridging, onycholysis (shown), and subungual hyperkeratosis. This bandlike lymphocytic infiltrate involves the dermalepidermal junction (interface), and the basal layer of keratinocytes may undergo degeneration and necrosis, whereas the stratum granulosum often increases in thickness. The localization at the dermal-epidermal junction is typical of immune complex deposition. Oral mucosal ulcerative lesions may be present for months before the onset of skin involvement. Areas affected include the scalp, face, axilla, groin, trunk, and points of pressure. The vesicles and bullae rupture easily, leaving shallow erosions covered with dried serum and crust. These lesions can become progressively larger, and more lesions can appear, leaving considerable skin surface denuded after rupture. Corticosteroid therapy halts progression of the disease, and immunosuppressive therapy may be required for maintenance therapy. Some cases of pemphigus represent a paraneoplastic syndrome, most often with a non-Hodgkin lymphoma. With immunofluorescence using antibodies directed against IgG, an intercellular staining pattern is observed here, producing a netlike pattern. The lesions shown here developed with bullous pemphigoid, which typically affects older individuals and involves cutaneous and mucosal surfaces. These lesions filled with clear fluid may reach several centimeters in size, but they do not rupture as easily as the lesions of pemphigus. Flexural regions of the axillae, groin, forearms, abdomen, and inner thighs are most often involved. The inflammatory infiltrate can include fibrin along with lymphocytes, eosinophils, and neutrophils. Oral lesions may occur in 10% to 15% of cases, and they follow the appearance of skin lesions. An association with intestinal celiac disease is shown with IgA and IgG antibodies formed against ingested gliadin protein found in gluten of grains such as wheat, barley, and rye, and also directed against reticulin with marked bright green immunofluorescence (right panel). The reticulin is part of anchoring fibrils that connect epidermal basement membrane to the dermis. The characteristic microscopic finding shown here is collections of neutrophils within the dermal papillae, forming papillary microabscesses. Over time, these areas can coalesce, with subepidermal blister formation (left panel). Acne occurs in nearly all teenagers and young adults after puberty to some degree. It results from increased sebaceous gland sebum production with an increase in androgenous steroid hormone production. Sebum and keratinaceous debris block hair follicles, leading to comedone formation. Bacteria such as Propionibacterium acnes in the comedones cause inflammation and enlargement, forming a pustule or nodule. Acne is most often self-limited and generally abates in young adulthood, but about 10% to 20% of adults may continue to manifest acne. Boys are affected more than girls, although acne may persist longer in young women. Treatment with a synthetic vitamin A derivative (isotretinoin) is often successful. Such lesions may reach several centimeters in size over weeks to months and then fade. In some cases an underlying systemic inflammatory condition, such as a granulomatous disease. Note the extensive inflammation of subcutaneous adipose tissue with infiltration by lymphocytes, histiocytes, multinucleated giant cells, and septal fibrosis (left panel). If part of a spectrum of persistent erythema and telangiectasia known as rosacea, telangiectasia progresses to pustules and papules, and finally rhinophyma with permanent thickening of the nasal skin. Rosacea occurs most often in adult women, mediated by abnormally high levels of cathelicidin contributing to cutaneous innate immunity. The rare autosomal dominant Osler-Weber-Rendu syndrome (hereditary hemorrhagic telangiectasia) affects blood vessels throughout the body and results in a bleeding tendency. The rubbing of skin surfaces in the fold makes them more prone to chafing of the epidermis, and the warm, moist environment encourages fungal and bacterial growth. These striae can arise on the abdomen, breasts, buttocks, and thighs in association with weakening of the dermal elastic tissue. These lesions tend to grow slowly over several years before they begin to regress over 6 months to 2 years. These lesions are usually a few millimeters to 1 cm in size and are most often located on the dorsa of the hands. Lesions can also appear on the face (verruca plana), on the soles of the feet (verruca plantaris), or on the palms of the hands (verruca palmaris). They are most often found on the skin of the trunk and anogenital region but may appear elsewhere, as here on the face. This is a self-limited disease and the lesions usually resolve within 18 months in immunocompetent persons. These molluscum bodies may be identified with Giemsa staining of the cheesy material expressed from the center of a lesion. Various dermatophytes can produce irregular areas of eczema or irregular pigmentation, crusting, or scaling. Viewing the areas with fluorescent light (Wood lamp) may reveal the autofluorescence of these fungi. The more elongated body louse (or head louse, which is similar) is shown in the left panel. These wingless insects (note the six legs) live by biting and sucking on the blood of the human host. The focal irritation they cause can lead to scratching and excoriation that may become secondarily infected. The body louse (Pediculus humanus corporis) is also the vector for Rickettsia prowazekii (epidemic typhus), Borrelia recurrentis (relapsing fever), and Bartonella quintana (trench fever, bacillary angiomatosis, endocarditis, lymphadenopathy). The female mite burrows under the stratum corneum, typically on the hands, but also in the genital region of males and periareolar region of females. The mode of transmission is direct human skin-to-skin contact, but these organisms can survive on clothing for 2 to 3 days. A variant called crusted scabies and resembling psoriasis occurs with numerous mites over extensive areas of skin; persons with immune compromise or poor health are at risk. The lesions are caused by accidental percutaneous penetration and subsequent migration of larvae of various nematode parasites found in soils, such as Ancylostoma, Necator, and Strongyloides. Either body region may be infected, however, by either subtype to produce clinically and histologically indistinguishable disease. Diagnosis can be aided by cytologic smears of lesions, by serologic titers, and by viral culture. In the right panel, keratinocyte intranuclear inclusions are highlighted in dark brown with immunohistochemical staining. Viral replication begins within epithelium and underlying dermis or submucosa and spreads to nerve endings, where it is transported intra-axonally to neurons in ganglia. Antiviral agents, such as acyclovir and valacyclovir, help to suppress viral replication but cannot eliminate latent virus. Grossly, red-to-blue papules may increase to protruding or subcutaneous nodules, with some resemblance to Kaposi sarcoma.
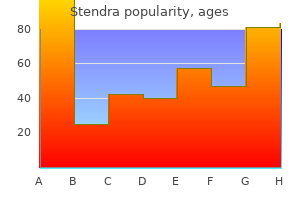
Order stendra 200mg overnight delivery
Intramuscular Induction Occasionally a patient may not be able to cooperate with any element of preoperative preparation medications via g-tube cheap stendra 100 mg mastercard. Intramuscular injection of ketamine (3 to 5 mg/kg) may be the best option in these circumstances, but this requires a careful team approach and family preparation to be safe and successful. Pediatric Airway Management Understanding the anatomical and physiologic differences between adults, infants, and children is necessary to provide safe and successful airway management tailored to the infant or child. In general, these differences and their impact on airway management are greatest in the neonatal and infant period. Anatomically, an infant has a larger occiput, a larger tongue size relative to the size of the oropharynx, and a more cephalad larynx (Table 33-5). The larger occiput may promote airway obstruction and interfere with laryngoscopy when a head pillow is used to achieve the classic sniffing position. Instead, a shoulder roll is often more useful both for promoting a patent airway and for facilitating direct laryngoscopy. Furthermore, the shape of the larynx is cylindrical, as in the adult, so it is important to remember clinically because the endotracheal tube fit (resistance to endotracheal tube passage) must be assessed after it has passed through the vocal cords. A leak pressure of less than 20 to 25 cm H2O should be targeted to minimize this risk. Normal healthy infants have overlap with tidal breathing and closing volumes, and their oxygen consumption rates are nearly three times that of an adult, so under anesthetized conditions, their functional residual capacity is reduced (Table 33-2). The clinical impact of this is rapid oxyhemoglobin desaturation following brief periods of apnea, resulting in shorter times to perform apneic intubation techniques. Did You Know Infants and young children have a relatively large tongue and a more cephalad larynx effectively shortening the distance in which the oral, pharyngeal, and tracheal axes must be aligned to achieve laryngeal exposure during direct laryngoscopy. Difficult airway management in pediatric patients often requires deep sedation or general anesthesia. Anesthetic Conditions for Laryngoscopy and Endotracheal Intubation Traditionally, intubation of the trachea in children is performed following induction of anesthesia and administration of a nondepolarizing neuromuscular blocker. It has become common practice to perform laryngoscopy and endotracheal intubation under deep anesthesia without neuromuscular blockade. This can be done with deep sevoflurane anesthesia alone, but it is also often performed with a propofol bolus. Insufficient depth of anesthesia without neuromuscular blockade may result in coughing, laryngospasm, oxyhemoglobin desaturation, and regurgitation. Food and Drug Administration applied a black box warning for succinylcholine contraindicating its use for routine airway management. However, in the absence of absolute contraindications to succinylcholine (malignant hyperthermia susceptibility, history of burns, etc. Direct Laryngoscopy Traditionally the straight blade (Miller) has been used in children, although there is little or no comparative evidence to show that this blade performs better than 33 Neonatal and Pediatric Anesthesia 639 the curved blade (Macintosh) (see Chapter 20. After sweeping the tongue, the blade tip is advanced beyond the vallecula and the epiglottis is directly lifted. Alternatively, the straight blade can be used in the manner of the Macintosh and the epiglottis lifted indirectly with the blade tip in the vallecula. Laryngeal Masks and Supraglottic Airways Laryngeal mask airways are frequently used in pediatric anesthesia. Laryngeal masks with gastric drain channels as well as laryngeal masks designed to facilitate intubation are available in pediatric sizes. Endotracheal Tube Selection Historically, uncuffed endotracheal tubes were recommended in children; however, in the current era, cuffed tubes are in most circumstances superior. The incidence of postintubation stridor is less when properly sized cuffed tubes are used, possibly from the decreased need or frequency of repeated laryngoscopy for tube change when too small a tube is placed initially. Cuffed endotracheal tubes also offer advantages of improved sealing of the trachea, which decreases operating room pollution, allows for lower fresh gas flows, improves ventilator performance, and may offer greater protection from macroaspiration. When tracheal intubation is performed, the correct tracheal tube size must be chosen. In infants and smaller children, a half-size smaller should be selected when a cuffed tube is used. Tracheal Intubation and Positioning of the Endotracheal Tube Indications for tracheal intubation in children are largely similar to those for adults. In addition, many anesthesiologists intubate the trachea and control ventilation in neonates and preterm infants in the absence of other traditional indications. Careful attention must be paid to positioning the tracheal tube tip in the midtrachea. Small tube movements may result in endobronchial intubation or inadvertent extubation in infants. Assessing the adequate depth of the endotracheal tube can be performed by deliberately advancing the endotracheal tube into the main-stem bronchus while simultaneously auscultating and providing breaths with hand-bag ventilation. When the endotracheal tube enters the right or left mainstem bronchus, breath sounds will be absent in the opposite side respectively. The tube is then withdrawn by 1 cm in infants and 2 cm above the carina and breath sounds should be used to confirm both lungs are being ventilated. When a cuffed tube is used, it may be easier and more reliable to position the tube so that the cuff can be palpated by ballottement in the suprasternal notch. This translates to the tip of the tube being in an intrathoracic and midtracheal location. If a "traditional" rapid sequence induction is performed, nearly all infants will have an oxyhemoglobin saturation 640 Clinical Anesthesia Fundamentals below 90% after 1 minute of apnea. Temperature Management Children are at increased risk of hypothermia under anesthesia; infants and in particular premature infants and neonates are at greatest risk. Radiation Evaporation Convection Conduction Neonates under anesthesia behave as poikilotherms; their temperature approaches that of their surroundings. Hypothermia can be prevented and normothermia maintained using a combination of strategies tailored to the individual patient. Warming the operating room prior to arrival (convection or radiation), forced air warming (convection), use of a circulating warm water mattress (conduction), heated humidified gases or humidified moisture exchanger (evaporation), and overhead infrared warming lights (radiation) are among the available methods. Intravenous Fluid Requirements Intravenous fluid requirements in fasting children are usually determined using the 4-2-1 rule. The hourly infusion rate is calculated as 4 mL/kg for the first 10 kg, plus 2 mL/kg for the second 10 kg, and 1 mL/kg for each additional kilogram. Fasting fluid deficits are calculated based on this formula and the duration the child has been non per os. The generally accepted guideline is 50% of the deficit replaced in the first hour, followed by 25% of the deficit replaced in hour 2, and hour 3 to complete the entire deficit. Infants under 6 months of age, and neonates in particular, are at increased risk of hypoglycemia with fasting durations commonly seen in anesthetic practice. Did You Know Hypovolemia associated with hemorrhage is the most common cardiovascular cause of perioperative cardiac arrest in children. Although transfusion thresholds are ultimately tailored to the individual patient and clinical scenario, in most scenarios red blood cell transfusion is indicated when the hemoglobin is below 7 g/dL (13,14) and is often indicated sooner depending on the age of the patient and clinical scenario (10,11). Packed red blood cells (5 mL/kg) can be expected to raise the hemoglobin approximately 1 g/dL. Indications for hemostatic blood component therapy are similar to those for adults. Usually indicated for platelet counts <50,000/L; higher thresholds may be used for certain procedures. Myelomeningocele Spina bifida refers to a range of congenital anomalies of the central nervous system. The most common is a myelomeningocele, which involves bulging of the spinal cord into a sac filled with cerebrospinal fluid.
Jarilla (Chaparral). Stendra.
- Are there any interactions with medications?
- Dosing considerations for Chaparral.
- What is Chaparral?
- Are there safety concerns?
- Arthritis, cancer, sexually transmitted diseases, tuberculosis, colds, skin conditions, stomach ailments (cramps, gas), weight loss, urinary and respiratory infections, and chicken pox.
- How does Chaparral work?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96770
Order 200mg stendra fast delivery
Vascular endothelial cells may present antigens to blood T cells that adhere to vessel walls chi infra treatment generic stendra 50 mg amex, and this process may contribute to the recruitment and activation of effector T cells in cell-mediated immune reactions. Endothelial cells in grafts also are targets of T cells reacting against graft antigens (see Chapter 17). The physiologic significance of antigen presentation by these cell populations is unclear. In the 1940s, to analyze the genetic basis of graft rejection, investigators produced inbred mouse strains by repetitive mating of siblings. Different strains may express different alleles and are said to be allogeneic to one another. By breeding congenic strains of mice that rejected grafts from other strains but were identical for all other genes, these investigators showed that a single genetic region on chromosome 17 is primarily responsible for rapid rejection of tissue grafts, and this region was called the major histocompatibility locus (histo, tissue). Initially, this locus was thought to contain a single gene that controlled tissue compatibility. However, occasional recombination events occurred within the H-2 locus during interbreeding of different strains, indicating that it actually contained several different but closely linked genes, many of which were involved in graft rejection. The genetic region that controlled graft rejection and contained several linked genes was named the major histocompatibility complex. This task became feasible when it was discovered that individuals who had received multiple blood transfusions and patients who had received kidney transplants had antibodies that recognized cells from the blood or kidney donors, and that multiparous women had circulating antibodies that recognized paternal cells. Other polymorphic genes that contribute to graft rejection to a lesser degree are called minor histocompatibility genes; we will return to these in Chapter 17, when we discuss transplantation immunology. This was a puzzle to immunologists because transplantation is not a natural phenomenon, and there was no reason that a set of genes should be preserved through evolution if the only function of the genes was to control the rejection of foreign tissue grafts. Immunologists found that inbred strains of a single species (guinea pigs or mice) differed in their ability to make antibodies against some simple synthetic polypeptides, and responsiveness was inherited as a dominant Mendelian trait. Polymorphism refers to variations in a gene among individuals in an outbred population. But the selective pressures that have preserved such a vast number of alleles in the population are not understood. The I-A allele found in the inbred mouse strain with the Kk and Dk alleles is called I-Ak (pronounced I-A of k). This is one of the mechanisms by which innate immunity stimulates adaptive immune responses. The expression of many of the proteins involved in antigen processing and presentation is coordinately regulated. About three quarters of the chain polypeptide is extracellular; a short hydrophobic segment spans the plasma membrane, and the carboxy-terminal residues are located in the cytoplasm. The amino-terminal 1 and 2 segments of the chain, each approximately 90 residues long, interact to form a platform of an eight-stranded, antiparallel -pleated sheet supporting two parallel strands of helix. The ends of the class I peptidebinding cleft are closed so that larger peptides cannot be accommodated. Class I molecules are composed of a polymorphic chain noncovalently attached to the nonpolymorphic 2-microglobulin (2m). Like the 3 segment, 2microglobulin is structurally homologous to an Ig domain and is invariant among all class I molecules. The fully assembled class I molecule is a trimeric complex consisting of an chain, 2-microglobulin, and a bound peptide, and stable expression of class I molecules on cell surfaces requires the presence of all three components of the complex. The reason for this is that the interaction of the chain with 2-microglobulin is stabilized by binding of peptide antigens to the cleft formed by the 1 and 2 segments, and conversely, the binding of peptide is strengthened by the interaction of 2-microglobulin with the chain. Four strands of the floor of the cleft and one of the -helical walls are formed by the 1 segment, and the other four strands of the floor and the second wall are formed by the 1 segment. The carboxyterminal ends of the 2 and 2 segments continue into short connecting regions followed by approximately 25-amino acid stretches of hydrophobic transmembrane residues. In both chains, the transmembrane regions end with clusters of basic amino acid residues, followed by short hydrophilic cytoplasmic tails. The mechanisms and significance of these processes are discussed later in this chapter. These processes ensure that T cells are normally tolerant to self antigens (see Chapter 15). Once bound, the peptides and their associated water molecules fill the clefts, making extensive contacts with the amino acid residues that form the strands of the floor and the helices of the walls of the cleft. Many class I molecules have a hydrophobic pocket that recognizes one of the following hydrophobic amino acids-valine, isoleucine, leucine, or methionine-at the C-terminal end of the peptide. Some class I molecules have a predilection for peptides with a basic residue (lysine or arginine) at the C terminus. The mechanism is called antigen processing and is the focus of the remainder of the chapter. The pathways of antigen processing play a key role in determining the types of microbes and protein antigens that these classes of T cells recognize and respond to . We first describe these two pathways of antigen processing and then their functional significance. Sources of Protein Antigens Degraded in Proteasomes Microbial proteins present in the cytosol that undergo proteasomal degradation are derived from microbes (typically viruses) that replicate and survive in the cytosol of cells, extracellular bacteria that inject proteins into the cytosol, and various extracellular organisms that are phagocytosed and their proteins are transported from vesicles into the cytosol. Peptides that are presented in association with class I molecules may also be derived from microbes and other particulate antigens that are internalized into phagosomes but escape into the cytosol. Some microbes are able to damage phagosome membranes and create pores through which the microbes and their antigens enter the cytosol. For instance, pathogenic strains of Listeria monocytogenes produce a protein called listeriolysin that enables bacteria to escape from vesicles into the cytosol. This figure depicts proteasomal proteolysis of a protein synthesized within the cell or that is ingested into a phagosome and then transported into the cytosol. Proteins produced in the endoplasmic reticulum that either do not fold properly or fail to assemble correctly in this compartment are translocated out of the endoplasmic reticulum and are degraded in proteasomes. These types of proteins are often found in damaged cells and tumors and are involved in T cell responses against antigens from these cells. Proteasomes are large multiprotein enzyme complexes with a broad range of proteolytic activity that are found in the cytoplasm and nuclei of most cells. A proteasome appears as a cylinder composed of a stacked array of two inner rings and two outer rings, each ring being composed of seven subunits, with a cap-like structure at either end of the cylinder. The proteins in the outer rings are structural and lack proteolytic activity; in the inner rings, three of the seven subunits (1, 2, and 5) are the catalytic sites for proteolysis. The proteasome performs a basic housekeeping function in cells by degrading many damaged or improperly folded proteins. Protein synthesis normally occurs at a rapid rate, about six to eight amino acid residues being incorporated into elongating polypeptide chains every second. This process is error prone, and it is estimated that approximately 20% of newly synthesized proteins are misfolded. These newly translated but defective polypeptides, as well as proteins that are damaged by cellular stresses, are targeted for proteasomal degradation by covalent linkage of several copies of a small polypeptide called ubiquitin. Proteins with chains of four or more ubiquitins are recognized by the proteasomal cap and then are unfolded, the ubiquitin is removed, and the proteins are threaded through proteasomes, where they are degraded into peptides. The proteasome has broad substrate specificity and can generate a wide variety of peptides from cytosolic proteins (but usually does not degrade them completely into single amino acids). Thus, proteasomes are organelles whose basic cellular function has been adapted for a specialized role in antigen presentation. The synthesis and assembly of class I molecules involve a multistep process in which peptide binding plays a key role. Appropriate folding of the nascent chains is assisted by chaperone proteins, such as the membrane chaperone calnexin and the luminal chaperone calreticulin. Several viruses have evolved mechanisms that interfere with class I assembly and peptide loading, emphasizing the importance of this pathway for antiviral immunity (see Chapter 16). Proteins that are targeted to lysosomes include extracellular proteins captured by endocytosis, pinocytosis, or phagocytosis; cell surface proteins that are being endocytosed and degraded; and intracellular proteins that may be membrane-bound, vesicular, or cytosolic that are routinely included in autophagosomes during the process of autophagy. Macrophages also express receptors for the Fc portions of antibodies and receptors for the complement protein C3b, which bind antigens with attached antibodies or complement proteins and enhance their internalization. After their internalization, protein antigens become localized in intracellular membrane-bound vesicles called endosomes. The endosomal pathway of intracellular protein traffic communicates with lysosomes, which are denser membrane-bound enzyme-containing vesicles. Particulate microbes are internalized into vesicles called phagosomes, which may fuse with lysosomes, producing vesicles called phagolysosomes or secondary lysosomes.
Buy stendra 100mg online
Overlying epithelial cell (podocyte) foot processes are effaced (giving the appearance of fusion) and run together symptoms vertigo buy stendra overnight delivery, which leads to loss of the normal anionic charge barrier such that albumin selectively leaks out, and proteinuria ensues, often with nephrotic syndrome. Only 3 of 10 glomeruli in the entire biopsy specimen were involved, a focal process. This disease is focal, involving some glomeruli, and segmental, involving part of the glomerulus. Both proteins are components of the slit diaphragm between podocyte foot processes. On light microscopy there is mesangial proliferation, increased mesangial matrix, mesangial immune complex deposition, accentuation of the lobular architecture, and increased leukocytes. Most cases occur in adolescents and young adults, with both nephrotic and nephritic features. The dense deposits within the basement membrane often coalesce to form a ribbonlike mass of deposits. The deposits result from activation of the alternative complement pathway, evidenced by a reduced serum C3 with normal C1 and C4. Patients with dense deposit disease often have circulating C3 nephritogenic factor (C3NeF). The rare condition, called partial lipodystrophy with C3NeF activity, may be accompanied by dense deposit disease. Antiglycan antibodies form and lead to immune complexes deposited within the mesangium of the glomeruli. Some viruses and bacteria express N-acetylgalactosamine on their cell surfaces so that infection may promote antiglycan antibody formation; IgA nephropathy may initially appear in association with an upper respiratory or gastrointestinal infection. This disease most often tends to be mild, but recurrent, and continues with normal renal function for years. Some cases are associated with celiac disease and some with chronic liver disease from decreased IgA clearance. In general, greater immune complex deposition and more cellular proliferation suggest a worse prognosis. In this case there is extensive immune complex deposition in the thickened glomerular capillary loops, giving a wire-loop appearance. Although onset of microscopic hematuria or proteinuria occurs in childhood, renal failure is more likely to occur in adults. The renal tubular cells appear foamy because of the accumulation of neutral fats and mucopolysaccharides, seen here imparting a pale red appearance with a fat stain. In contrast, renal diseases that are "nephrotic" are characterized by the presence of protein spilled into the urine. Steadily increasing serum creatinine and urea nitrogen are clues to this progression. The cortex is fibrotic, the glomeruli are sclerotic from hyaline obliteration, there are scattered interstitial chronic inflammatory cell infiltrates, and the arteries are thickened. Tubules are often dilated and filled with pink casts and give an appearance of "thyroidization. Diminished renal clearance of phosphate predisposes to secondary hyperparathyroidism. This glomerulosclerosis is caused by metabolic alterations with hyperglycemia, with a marked increase in mesangial matrix from cellular damage secondary to nonenzymatic glycosylation of proteins. Also note the markedly thickened arteriole at the lower right, which is typical of hyaline arteriolosclerosis seen in diabetic kidneys. In early stages of this disease, microalbuminuria is present, but it progresses to overt proteinuria that presages renal failure. Diffuse glomerulosclerosis is associated with long-standing type 1 or 2 diabetes mellitus. Changes of glomerulosclerosis with diabetes mellitus take a decade or longer to develop and gradually worsen. Patients with diabetes mellitus, whether type 1 or 2, are at risk for many renal diseases, including nephrosclerosis, pyelonephritis, and papillary necrosis, in addition to glomerulosclerosis. The end-stage renal disease seen here with small native kidneys and granular surfaces was treated in the left panel with renal transplantation. The transplant kidney is placed in the pelvis because this is technically easier, and there is usually no point in trying to remove the native kidneys, which may still produce erythropoietin. In this case the patient developed chronic rejection, which is why the transplant kidney is slightly swollen with focal hemorrhages. In the right panel the smaller reddish kidney has undergone infarction from renal arterial thrombosis. The distribution of necrosis and apoptosis is more segmental with ischemic injuries, as shown here, with some tubules still having intact epithelium, whereas others show considerable damage. Lesser degrees of injury with loss of the brush border and cell swelling are common. The patient can be maintained on dialysis until the recovery phase occurs with polyuria. Incompetence of the vesicoureteral valve can predispose to reflux with retrograde flow of urine. In children this is most often caused by congenital shortening of the intravesical portion of the ureter. Decreased bladder contraction from autonomic neuropathy or spinal cord injury can lead to reflux in adults. In either case, there is an increased risk for urinary tract infection, and the inflammation from infection further exacerbates the reflux. Shown here are numerous inflammatory cells, mainly neutrophils, filling renal tubules and extending into the interstitium. This case of acute pyelonephritis resulted from an ascending urinary tract infection that started in the bladder. Nearly all such cases are caused by bacterial organisms, including Enterobacteriaceae (Escherichia, Klebsiella, Proteus, Providencia, Edwardsiella, Enterobacter) and streptococci and staphylococci. Urinary stasis from congenital anomalies, obstructive uropathy, or decreased bladder emptying may predispose to ascending urinary tract infection. This pattern of acute pyelonephritis is most typical of hematogenous dissemination of infection to the kidney in patients with septicemia. Ascending urinary tract infection leading to acute pyelonephritis is more common than the hematogenous route. A rare complication not seen here is papillary necrosis, which is more likely to occur in patients with diabetes mellitus or urinary tract obstruction. This is an uncommon but severe complication of acute pyelonephritis, particularly in patients with diabetes mellitus or urinary tract obstruction. Papillary necrosis may also occur with analgesic nephropathy or sickle cell disease. An extensive acute pyelonephritis complicated this process, and the infection became complicated by a perinephric abscess that extended to the right flank region, seen here as irregular areas of decreased attenuation within the skeletal muscle of the posterior flank and back on the right. Appearing here is a hornlike stone extending into a dilated calyx, with nearly unrecognizable pale yellow to tan overlying thinned residual cortex and medulla. This has followed severe inflammation and atrophy from hydronephrosis and pyelonephritis. Nearly complete or total obstruction with extensive inflammation destroys renal parenchyma. Nephrectomy may be done in cases of pyonephrosis because the kidney becomes nonfunctional and serves only as a source of continuing infection. If this process is unilateral, the problem originates from a disease involving a location from the ureteral orifice up to the renal pelvis. In this case, an obstructing urinary tract calculus had been present for many years. Vesicoureteral reflux, most often manifesting in childhood, could produce a similar finding. If the obstructive process were bilateral, the underlying disease would originate in the bladder trigone or urethra (or the prostate around the urethra of males) or some process. There are coarse, discrete, corticomedullary scars that overlie dilated, blunted, or deformed calyces. If severe there is loss of concentrating ability with polyuria and urine specific gravity of 1. Lymphocytes and plasma cells characteristic of chronic pyelonephritis are seen at high magnification (right panel).
200 mg stendra amex
It is a major surgical procedure and is associated with high morbidity and mortality rates (10% to 15%) symptoms 4 dpo bfp order stendra amex. There are multiple surgical procedures for esophagectomy that combine three fundamental approaches: transthoracic approach, transhiatal approach, and minimally invasive surgery. Outcomes are improved with early extubation, thoracic epidural analgesia, and vasopressor or inotrope infusions to support blood pressure (1,3,7). Tracheal Resection Tracheal resection is indicated in patients who have a tracheal obstruction as a result of a tracheal tumor, trauma (most commonly due to postintubation stenosis), congenital anomalies, vascular lesions, or tracheomalacia. However, intratracheal masses may lead to airway obstruction with induction of anesthesia and should be managed similarly to anterior mediastinal masses (see below). Did You Know Suction applied to a chest tube placed after pneumonectomy can cause mediastinal shift, resulting in hemodynamic collapse. Did You Know Restrictive fluid strategy for patients under going pulmonary and esophageal surgery has become controversial because of a concern about its potential to induce acute kidney injury. After the tracheal resection is completed, most patients are kept in a position of neck flexion to reduce tension on the suture line. Bronchopleural Fistula A bronchopleural fistula may be caused by rupture of a lung abscess, bronchus, bulla, cyst, or parenchymal tissue into the pleural space; erosion of a bronchus by carcinoma or chronic inflammatory disease; or stump dehiscence of a bronchial suture line after pulmonary resection. The complications of bulla rupture can be lifethreatening due to hemodynamic collapse from tension pneumothorax or inadequate ventilation due to a resultant bronchopleural fistula. If bronchial disruption occurs early in postresection patients, it can also be life-threatening. Late or chronic postresection disruption is managed with chest tube drainage or with the Clagett procedure, which includes open pleural drainage and the use of a muscle flap to reinforce the bronchial stump. However, depending on the context, awake intubation maintenance of spontaneous ventilation may be used (1,3). Bronchiectasis, Lung Abscess, and Empyema Infectious conditions, including bronchiectasis, lung abscess, and empyema, are indications for thoracic surgery, such as decortication. Anesthetic considerations for these conditions include the need for lung isolation to protect uninvolved lung regions from soiling by pus. Due to the inflammation, surgery is technically more difficult, and there is a greater risk of massive hemorrhage, particularly during decortication. If the lung has been chronically collapsed, expansion should be done gradually to avoid the development of pulmonary edema upon re-expansion (1). Mediastinal Masses Tumors of the anterior mediastinum include thymoma, teratoma, lymphoma, cystic hygroma, bronchogenic cyst, and thyroid tumors. Did You Know In a patient with an anterior mediastinal mass, a history of supine dyspnea or cough may be predictive of airway collapse following induction of general anesthesia. During induction of general anesthesia, airway obstruction is the most common and feared complication. A history of supine dyspnea or cough should alert the anesthesiologist to the possibility of airway obstruction upon induction. General anesthesia and muscle relaxants will exacerbate extrinsic intrathoracic airway compression due to reduced lung volume and tracheobronchial diameters, bronchial smooth muscle relaxation, and loss of the normal transpleural pressure gradient that dilates the airways during spontaneous inspiration and minimizes the effects of extrinsic intrathoracic airway compression. The other major complication is cardiovascular collapse secondary to compression of the heart or major vessels. Patients who are symptomatic or have evidence of airway or cardiovascular involvement on imaging should have diagnostic procedures performed under local or regional anesthesia whenever possible. Alternatively, spontaneous ventilation should be maintained with either an inhalation induction or titration of an agent such as ketamine. Intraoperative life-threatening airway compression may respond to repositioning of the patient (it must be determined before induction if there is a position that causes less symptoms) or rigid bronchoscopy and ventilation distal to the obstruction (this means that an experienced bronchoscopist and equipment must always be immediately available in the operating room for these cases). Myasthenia Gravis Myasthenia gravis is an autoimmune disease of the neuromuscular junction, in which affected patients have weakness due to a decreased number of acetylcholine receptors at the motor endplate. Medical treatments for myasthenia gravis include anticholinesterases, such as pyridostigmine, immunosuppressive drugs, such as steroids, and plasmapheresis. On the day of surgery, patients should continue their usual pyridostigmine dosing. Myasthenic patients are unpredictably resistant to succinylcholine and extremely sensitive to nondepolarizing blockers. Alternatively, 34 Anesthesia for Thoracic Surgery 665 inhalational induction with a volatile agent may be performed. Referral for surgery early in the course of the disease, preoperative medical stabilization, and minimally invasive surgical approaches have made the need for postoperative ventilation infrequent (1,3,10). When thoracotomy pain is controlled, the risk of pulmonary complications is decreased. In patients with coronary artery disease, thoracic epidural local anesthetics also seem to reduce myocardial oxygen demand. When there is a relative or absolute contraindication to placement of a thoracic epidural, another excellent choice for analgesia is a paravertebral infusion of local anesthetic via a catheter. This may be placed by the anesthesiologist using a landmark or ultrasound-guided technique or directly by the surgeon during an open thoracotomy. Other options for analgesia include intercostal blocks and the use of patient-controlled opioid analgesia with multimodal analgesia, such as the use of acetaminophen, gabapentin, and nonsteroidal anti-inflammatories. Institutions differ in their practices regarding the use of catheter techniques versus intravenous patient-controlled analgesia for minimally invasive thoracic surgeries (1,3). Complications As mentioned previously, respiratory and cardiac complications account for the majority of morbidity and mortality following thoracic surgery. There are multiple potential complications that can occur in the immediate postoperative period, such as torsion of a remaining lobe after lobectomy, dehiscence of a bronchial stump, hemorrhage from a major vessel, or cardiac ischemia or arrhythmias. Among these possible complications, two will be discussed in more detail: respiratory failure and cardiac herniation. Respiratory Failure Patients with decreased respiratory function preoperatively are at increased risk of postoperative respiratory complications. In addition, age, the presence of coronary artery disease, and the extent of lung resection play major roles in predicting postoperative respiratory failure. Chest physiotherapy, incentive spirometry, and early ambulation are also crucial in order to minimize pulmonary complications after lung resection. For an uncomplicated lung resection, early extubation is desirable to avoid potential complications that can arise due to prolonged intubation and mechanical ventilation. Current therapy to treat acute respiratory failure is aimed at supportive measures that provide better oxygenation, treat infection, and provide vital organ support without further damaging the lungs (1). Cardiac Herniation Acute cardiac herniation is an infrequent complication of pneumonectomy when the pericardium is incompletely closed or the closure breaks down. It usually occurs immediately or within 24 hours after chest surgery and is 666 Clinical Anesthesia Fundamentals Did You Know One of the catastrophic complication of pneu monectomy is cardiac herniation, and it requires immediate surgical treatment to ensure survival. In contrast, when the cardiac herniation occurs after a left-sided pneumonectomy, there is less cardiac rotation, but the edge of the pericardium compresses the myocardium. This may lead to myocardial ischemia, the development of arrhythmias, and ventricular outflow tract obstruction. The differential diagnosis of hemodynamic instability after thoracic surgery should include massive intrathoracic hemorrhage, pulmonary embolism, or mediastinal shift from improper chest drain management. Immediate diagnosis and surgical treatment of cardiac herniation by relocation of the heart to its anatomic position is key to patient survival. Maneuvers to minimize the cardiovascular effects include positioning the patient in the full lateral position with the operated side up. Vasopressors or inotropes are required to support the circulation while exploration takes place (1). Pulmonary morbidity following esophagectomy is decreased after introduction of a multimodal anesthetic regimen. A systematic review of randomized trials evaluating regional techniques for postthoracotomy analgesia. What is the most common concurrent illness identified preoperatively in thoracic surgical patients Initiation of one-lung ventilation to the dependent lung in a patient in the lateral position decreases ventilation perfusion mismatching because: A. If hypoxia occurs during one-lung ventilation, the first step in treatment after confirming administration of 100% oxygen is: A. In a patient requiring lung resection for treatment of right-sided bronchiectasis, the optimal management of the airway would include: A. Montzingo Sasha Shillcutt Patients with heart disease present unique challenges for the anesthesiologist.