Purchase online tegretol
The leading mechanisms of injuries are fall muscle relaxant during pregnancy buy cheap tegretol 100mg, lacerations, and piercing injuries, with cleanup being the primary activity at the time of injury. Together, they are the most common types of disasters and account for at least half of all disaster-related deaths. Lava flows tend not to result in high casualties, because they are easily avoidable. The "composite" type of volcano is associated with a more violent eruption from within the chimney. These eruptions are associated with air shock waves, rock projectiles (some with high thermal energy), release of noxious gases, pyroclastic flows, and mud flows (lahars). Pyroclastic flows and lahars are often fast moving and are the main cause of damage and deaths from volcanoes, as evidenced by the small eruption of the Nevado del Ruiz in Colombia that killed more than 23,000 people. Ash is also responsible for the clogging of filters and machinery, causing electrical storms and fires, and interfering with Landslides Landslides are more widespread than any other geologic event. They are defined as downslope transport of soil and rock resulting from natural phenomena or man-made actions. Landslides can also occur secondary to heavy storms, volcanic eruptions, and earthquakes. Pending an assessment, needs can be anticipated, such as search and rescue, mass-casualty management, and emergency shelter for the homeless. It originated from the quadruple reassortment swine influenza (H1N1) virus closely related to the North American and Eurasian swine lineage. However, this new virus circulated only in humans, with no evidence of transmission between humans and animals. Within weeks, the virus quickly spread worldwide through humanto-human transmission. By June 19, 2009, all 50 states in the United States, the District of Columbia, Puerto Rico, and the U. The virus was most likely to strike children, young adults, and those with underlying pulmonary and cardiac disease. A national influenza vaccination campaign was launched in the United States in October 2009, and the first H1N1 vaccine was made available at that time. Despite the rapid response of the authorities, developing countries in the Southern Hemisphere experienced delays and shortages of the vaccines. Thus, research and developmental work have been encouraging for developing a "universal" influenza vaccine that could provide efficacious cross-reactive immunity and induce broad protection against different variants and subtypes of the influenza virus. Elective procedures should be minimized when resources are limited, and critical care capacity should be augmented. Safe practices and safe respiratory equipment are needed to minimize aerosol generation when caring for patients with influenza. Triage criteria should be objective, transparent, and ethical and applied justifiably and publicly disclosed. The H1N1 virus is expected to take on the behavior of a seasonal influenza virus and to circulate for some years. Although the mortality of confirmed cases has been documented to be as high as 68% in the affected nations of West Africa, if patients are quickly recognized and given appropriate aggressive supportive care, the case fatality ratio drops dramatically. From a mass-casualty perspective, it rapidly became clear that the aforementioned nations of West Africa did not have adequate governmental infrastructure to create Ebola treatment units nor were they able to strictly implement the necessary public health infrastructure of hygiene and isolation. This left hospital officials confused about the best manner in which to protect their employees. Second, the standard existing paradigm of local and state health agencies providing adequate resources, information, and guidance to health facilities may not be adequate; a rapid top-down federalized approach may be required. Clearly, more resources must be allocated to our federal health agencies to prepare for such possible events in the future. Because most attacks occur without warning, the local healthcare system will be the first and most critical interface for detection, notification, rapid diagnosis, and treatment. The best defense in reducing casualties will therefore rest on the ability of medical and public health personnel to recognize symptoms and provide rapid clinical and epidemiologic diagnosis of an event. This requires that healthcare providers be well informed of potential biological, chemical, and nuclear agents. Biological Weapons Biological weapons can be either pathogens (disease-causing organisms such as viruses or bacteria) or toxins (poisons of biological origin). They can be spread through various means, including aerial bombs, aerosol sprays, explosives, and food or water contamination. Multiple factors including particle size of the agent, stability of the agent, wind speed, wind direction, and atmospheric conditions can alter the effectiveness of a delivery system. Over 4115 deaths and 70,000 injuries have been ascribed to them during the years 1950 to 1994. Injuries most commonly seen are complex contaminated soft-tissue injury (50%), fractures (30%), head injury (10%), and blunt trauma to the chest and abdomen (10%). Some of the largest civilian disasters in North America have been related to the transportation of HazMat. The hazard risk to a healthcare facility increases with its proximity to a chemical plant or highway, and such factors should be considered in the emergency preparedness plan of a hospital. Since the terrorist attacks in September 2001 and intentional *Simple: care that does not require unusual equipment or excessive use of time or personnel. General features that should alert healthcare providers to the possibility of a bioterrorism-related outbreak include82 the following: 1. An unusual increase in the number of people seeking care, especially with fever or respiratory and gastrointestinal complaints 4. An endemic disease rapidly emerging at an uncharacteristic time or in an unusual pattern 5. Lower attack rates among people who had been indoors, especially in areas with filtered air or closed ventilation systems, versus people who had been outdoors 6. Clusters of patients arriving from a single locale and large numbers of rapidly fatal cases 7. Any patient presenting with a disease that is relatively uncommon and has bioterrorism potential. This tool guides infection-control professionals and healthcare epidemiologists in the development of practical and realistic response plans for their institutions in the event of a bioterrorism attack. Chemical Weapons Chemical incidents are accidental or intentional events that threaten or do expose responders and members of the public to a chemical hazard. Agents that have been commonly used as chemical weapons are also used in industrial processes. Most industrial incidents occur at an interface between transport, storage, processing, use, or disposal of hazardous chemicals, where these systems are more vulnerable to failure, error, or manipulation. The catastrophic effect of these agents has been utilized several times in the past for military purposes, and with the proliferation of these weapons, civilian populations are now faced with a significant threat. Muscarinic symptoms include lacrimation, bronchorrhea, bronchospasm, miosis, salivation, rhinorrhea, vomiting, and diarrhea. Nicotinic receptor stimulation produces muscle fasciculations, flaccid paralysis, tachycardia, and hypertension. Sarin presents as a vapor threat, and the onset of symptoms is within seconds, with a peak effect in 5 minutes. Exposed victims who are asymptomatic after 1 hour are unlikely to be contaminated. The cardinal rule in decontaminating patients is to remove and dispose of all articles of clothing. Most of the care is supportive and includes mechanical ventilation for respiratory failure and treatment of arrhythmias. In smaller doses they cause tachypnea, headache, dizziness, anxiety, and vomiting. They are highly toxic, and sufficient levels can cause death within 5 minutes of inhalation.
Buy 400 mg tegretol mastercard
Canadian Association of Radiologists: consensus guidelines for the prevention of contrast-induced nephropathy spasms meaning in urdu tegretol 400mg without a prescription. Review of radiation risks from computed tomography: essentials for the pediatric surgeon. Practice management guidelines for identification of cervical spine injuries following trauma: update from the eastern association for the surgery of trauma practice management guidelines committee. Clinical clearance of the cervical spine in blunt trauma patients younger than 3 years: a multi-center study of the American Association for the Surgery of Trauma. Low plasma D-dimer concentration predicts the absence of traumatic brain injury in children. Costs of childhood physical abuse: comparing inflicted and unintentional traumatic brain injuries. The eye in child abuse: key points on retinal hemorrhages and abusive head trauma. Emotional considerations and attending involvement ameliorates organ donation in brain dead pediatric trauma victims. In 2014, 27,737 organs were transplanted in the United States, with over 122,000 patients on the waiting list. Increasing the rate of donor registry participation and consent has the greatest impact on the number of available organs. However, approximately 20% to 30% organs are lost before procurement despite aggressive medical management after intent for donation has been made. Often, potential donors are excluded by caregivers based on notions of donor criteria or ethical concerns regarding the conflict of care. With the permission of the family, blood may be sampled to determine the suitability of a donor before brain death. If devastating, unsurvivable head injury is recognized in a potential donor, basic resuscitation may begin before the declaration of brain death. Events leading to brain death include hypertension with bradycardia (Cushing response) as the pons becomes ischemic. Further involvement of the medulla creates unopposed sympathetic stimuli that trigger a catecholamine "storm. Spinal cord ischemia and loss of sympathetic denervation result in severe hypotension. This is exacerbated by simultaneous ischemia of the pituitary and hypothalamus and the loss of homeostatic control. These events occur in varying magnitude or velocity, thus making management even more difficult. Moreover, treatment strategies administered before brain death are often directed toward maintaining cerebral perfusion, often to the detriment of other organs. Post-declaration management focuses on reversing this state and preventing further organ damage. These algorithms focus on ongoing resuscitation and provide evidence-based therapy, as well as a platform for future research in the field, both nationally and within regional donor networks. Immediate goals include establishing baseline organ function and stabilizing organ physiology. If not already in place, a central venous catheter and arterial catheter are inserted. Blood, urine, and bronchial cultures are obtained, and baseline biochemical values and infectious titers are determined. Lungs and heart are evaluated by performing basic chest radiography, echocardiography, and bronchoscopy. These are used to maximize the number of organs that can be transplanted per donor. These physiologic goals are specific but are also fairly broad and similar to basic resuscitation. This illustrates the importance of goaldirected care and timeliness of its implementation. Standard insulin protocols should also be continued because donors can be profoundly hyperglycemic. After adequate volume loading, vasopressors are often required to maintain perfusion pressure. End organ perfusion should be monitored by measuring oxygen delivery or central venous oxygen saturation. Low-dose supplementation increases the rate of high-yield procurement (>4 organs per donor) and should be used as a part of donor resuscitation. Strategies for preventing renal injury include avoidance of nephrotoxic agents and maintenance of hydration. Large volume administration improves kidney and liver graft function by correcting hypernatremia. Some societies advocate the use of colloids such as albumin to prevent water accumulation in the lungs. However, sodium levels should be monitored closely because this can worsen graft function. Dysfunction of the anterior pituitary gland is less consistent, with the variable effects of hormones given to counteract the loss of corticotropin and thyroid-stimulating hormone. Pulmonary edema after brain death results from elevated afterload due to catecholamine surge combined with increased venous return and decreased left ventricular function. Using this protocol, Critical Pathway for the Organ Donor Collaborative Practice the following professionals may be involved to enhance the donation process. Department of Health and Human Services, Health Resources and Services Administration, Division of Transplantation. Physiologicchangesduring brain stem death-lessons for management of the organ donor. Page 2 of 2 Proprietary and confidential information Do not reproduce or make available to third parties without prior written consent from Donor Alliance, Inc. More importantly, thyroid hormone administration did not exert detrimental effects on graft survival. The ischemic brain increases the levels of core inflammatory mediators that then cross the blood-brain barrier. Few studies have evaluated steroid use in isolation from other hormonal therapies. Most randomized trials on steroid administra- tion have yielded neutral results, whereas observational studies have generally demonstrated improved hemodynamics and oxygenation status, increased organ yield, and improved graft function. Despite these mixed results, steroids are a widely utilized tool for organ donor resuscitation. Limited supply of cadaveric donor organs requires attentive pretransplant management to increase their availability and function. Maintenance of organs after brain death is extremely difficult because of hypothermia, acidosis, hypovolemia, pulmonary edema, cardiac arrhythmias, and profound hypotension. Important aspects of management include identification of potential donors, early hemodynamic stabilization with volume and vasopressor resuscitation, frequent reassessment of organ function and resuscitation endpoints, and provision of hormone replacement when indicated. Designated protocols can help focus on resuscitation and ensure the development of evidence-based guidelines. Although newer therapeutic modalities are promising, they require further research. Brain death imparts profound changes to physiology including hemodynamic instability and loss of homeostatic control due to hypothalamic and pituitary ischemia. Up to 30% of transplantable organs are lost during the management of the brain-dead donor. Goal-directed care of the donor after declaration of brain death can increase organ yield. The cornerstones of donor management include intravascular resuscitation, vasopressor administration, and hormone replacement therapy. Although controversial due to cohort size and retrospective nature of the study, this is a widely cited paper for proponents of hormone resuscitation. This review provides a thorough yet concise overview of the physiologic changes that occur during brain death. Physiologic changes during brain stem death-lessons for management of the organ donor. Intensivist-led management of brain-dead donors is associated with an increase in organ recovery for transplantation. Organ donor management in Canada: recommendations of the forum on medical management to optimize donor organ potential.
Purchase tegretol with paypal
Multiple surgeries were performed under local peripheral nerve blocks spasms just below sternum purchase genuine tegretol line, with guillotine amputations being frequent. The command center eventually provided psychiatrists to manage the posttraumatic stress syndrome and a buddy system for the follow-up support. Although many small teams and a large volume of supplies were dispatched, an organized response was delivered under the leadership of Dr. Benjamin arrived in Port-au-Prince 3 days after the initial event, and after rapid assessment of needs and resources, organized the deployment of the 27-member critical care team to his home country, which arrived on January 20. The team remained on-site for 2 weeks and was responsible for postanesthesia and postoperative care delivery, with Dr. Benjamin being deputized as the director of critical care and recovery at the national hospital. The home institution effectively secured anonymous donations of private jets able to transport the team personnel and some 3000 pounds of medical supplies per flight. The team delivered intensive care with minimal technology but with kindness and dignity toward the suffering population. This was a truly integrated response with both language and cultural sensitivities and capabilities, which are very important in catastrophic situations that will take decades for the local population to recover from. The preceding discussion suggests that combinations of dialysis, orthopedic surgery, pediatric trauma, security, transportation, posttraumatic stress treatment, and cultural and language sensitivities are crucial in earthquakes. One of the most experienced managers and thought leaders in disaster management, Dr. Eric Noji, enumerated the most important factors in public health after disasters: environmental health, epidemic management, immunization, controlling the spread of human immunodeficiency virus/acquired immunodeficiency syndrome, management of dead bodies, nutrition, maternal and child health, medical services, and thorough public health surveillance. It is a common error to deliver a few weeks of heroic quality care and then abandon the population to the ravages of destroyed infrastructure, including public health organization. Ash is a main cause for respiratory-related syndromes and conjunctival and corneal injury. Problems related to communication (ashes cause serious interference) and transportation (poor visibility and slippery roads) are likely. Reducing the risk for vulnerable groups of being exposed to ash, raising awareness of the risk associated with ash (health and mechanical risk), and maintaining food security conditions over the long term (lava, ash, and acid rain cause damage to crops and livestock) can help limit suffering. On the basis of central pressure, wind speed, storm surge, and potential destruction, their severity is graded on a scale of 1 to 5 (Saffir Simpson scale). Cyclones during 1970 and 1991 in Bangladesh claimed 300,000 and 100,000 lives, respectively, because of flooding. Unlike biological weapons, disease secondary to release of chemical agents is likely to be more obvious, rapid in onset, and homogeneous. However, they pose serious problems for emergency care providers because of their potential to cause a large number of casualties rapidly and their potential for secondary contamination. Any emergency medical or public health response to a major incident involving a chemical warfare agent will require coordination among local, state, and federal organizations. Improvised nuclear devices are made of uranium or plutonium constructed by a nongovernmental source and limited by the critical mass of nuclear material. They yield less destructive power than a conventional nuclear warhead but are still capable of contamination effects. Their destructive capacities are enormous, and they contaminate a vast perimeter of space depending on the yield. Approximately 50% of the energy released from a nuclear bomb is due to the blast and shock waves, giving a majority of the survivors blast-related injuries and creating extensive infrastructure damage. About 35% of the energy released is thermal radiation (in orders of tens of millions of degrees), giving rise to high-degree skin burns. Depending on the size of the device and the altitude of detonation, an electromagnetic pulse is generated with the explosion. This is capable of disrupting all electrical equipment within 20 km to several hundreds of kilometers. Immediate ionizing radiation consists of gamma, beta, neutron, and a small amount of alpha radiation. Induced radiation occurs because of neutron-induced gamma activity of the immediate soil, silicon, manganese, aluminum, zinc, copper, and sodium. Fallout is the fusion of various radionuclides generated in the fission reaction with condensation, producing a snowflake-like debris that falls to earth. Fallout is a potential form of delayed radiation exposure and can cause internal contamination. Large-scale decontamination should be managed outside the hospital area as far as is possible, but plans for indoor decontamination should also be in place. A radiation emergency area (both in and out of the hospital) should be designated, with checkpoints nearing the cold zone. Management plans for the safe disposal of human waste and bodies should be in place so as not to increase the exposure risk. Triage of patients should be done on the basis of doing the greatest good for the greatest number. On the basis of predictive models, isolated irradiation, burns, and blast-related injuries would constitute 40% of injuries. Attending to trauma victims should take precedence over all other medical issues, because a given patient is not likely to succumb immediately from radiation injury. In determining patient viability, three parameters are of the most use: time of onset of vomiting, decrease in the absolute lymphocyte count over a 24-hour period, and presence of conventional trauma burns. Armed Conflict Armed conflict continues to be the most preventable and most destructive of man-made disasters in terms of human physical and emotional suffering, economic loss, and environmental destruction. Specific healthcare issues during these conflicts that are relevant to the intensivist include trauma from blast injuries, projectiles, and crush-related injuries; communicable diseases due to the breakdown of public infrastructure and mass displacement of populations; and burns and radiation-related injury. Treatment of these entities is often difficult because of a large volume of patients, lack of qualified medical personnel on-site, and inadequate supplies and equipment. It is important to emphasize that initial recognition of the medical syndromes and appropriate intervention are critical to minimizing morbidity and mortality. Appropriate triage, knowledge of field management of each syndrome, flexibility to adapt to each situation, ability to ignore natural differences among different specialties, and recognition of limits of medical care that can be provided in overwhelming situations are key to a good disaster medical response. In the following paragraphs, we discuss commonly encountered medical syndromes in a disaster situation. Blast Injuries Bombs contain an array of compounds such as nitroglycerin, trinitrotoluene, and others that are encased in a metal or plastic case. Decomposition of the solid or liquid compound into gas leads to massive dissipation of energy and pressure that creates a blast wave (shock wave). This destructive effect can be increased by the presence of nuts, nails, and bolts in the casing. Water transmits blast waves more efficiently than air, with the greatest impact being on structures that are the deepest. Primary blast injury is caused solely by the blast wave and almost always affects air-filled structures such as the lung, ear, and gastrointestinal tract. The presence of tympanic membrane rupture may indicate exposure to a high-pressure wave and is thought to correlate with more severe organ injury. Secondary blast injury is caused by the rapid acceleration of small fragments caused by the blast injury. Miscellaneous blast-related injuries encompass all other injuries caused by explosions. The most common injuries associated with fatality in blast incidents include subarachnoid hemorrhage (66%), fracture of the skull (51%), lung contusion (47%), tympanic membrane rupture (45%), and liver laceration (34%). Unfortunately, the extent of the blast injury cannot be assessed during the course of rapid triage examinations. In the absence of overt trauma, a focused physical examination should include examination for ruptured tympanic membrane, hypopharyngeal contusions, hemoptysis, and auscultation for wheezing. The presence of a ruptured tympanic membrane is almost always an indicator that the patient has been exposed to a blast wave powerful enough to cause serious damage. The thorax is frequently involved in a blast injury, manifesting with wheezing, hemoptysis, pneumothorax, hemothorax, and air embolism.
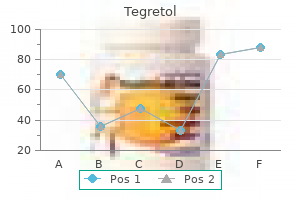
| Comparative prices of Tegretol | ||
| # | Retailer | Average price |
| 1 | Publix | 479 |
| 2 | Ross Stores | 364 |
| 3 | RadioShack | 350 |
| 4 | Meijer | 717 |
| 5 | Bed Bath & Beyond | 154 |
| 6 | IKEA North America | 485 |
| 7 | The Home Depot | 906 |
Order tegretol with visa
As with costosternal joint pain muscle relaxant natural order online tegretol, and rib fractures, a significant number of patients who suffer from intercostal neuralgia first seek medical attention because they believe they are suffering a heart attack. If the subcostal nerve is involved, patients may believe they are suffering from gallbladder disease. The pain of intercostal neuralgia is due to damage or inflammation of the intercostal nerves. The pain is constant and burning in nature and may involve any of the intercostal nerves as well as the subcostal nerve of the twelfth rib. Testing Plain radiographs are indicated in all patients who present with pain thought to be emanating from the intercostal nerve to rule out occult bony pathology, including tumor. If trauma is present, radionuclide bone scanning may be useful to rule out occult fractures of the ribs and/or sternum. Computed tomographic scanning of the thoracic contents is indicated if occult mass is suspected. Differential Diagnosis As mentioned, the pain of intercostal neuralgia is often mistaken for pain of cardiac or gallbladder origin and can lead to visits to the emergency department and unnecessary cardiac and gastrointestinal workups. If trauma has occurred, intercostal neuralgia may coexist with fractured ribs or fractures of the sternum itself, which can be missed on plain radiographs and may require radionuclide bone scanning for proper identification. Signs and Symptoms Physical examination of the patient suffering from intercostal neuralgia will generally reveal minimal physical findings unless there was a history of previous thoracic or subcostal surgery or cutaneous findings of herpes zoster involving the thoracic dermatomes. In contradistinction to the above-mentioned musculoskeletal causes of chest wall and subcostal pain, the patient suffering from intercostal neuralgia does not attempt to splint or protect the affected area. Careful sensory examination of the affected dermatomes may reveal decreased sensation or allodynia. With significant motor involvement of the subcostal nerve, the patient may complain that his or her abdomen bulges out. Pathologic processes such as pulmonary embolism, infection, and Bornholm disease can be responsible for the inflammation of the pleura. Treatment Initial treatment of intercostal neuralgia should include a combination of simple analgesics and the nonsteroidal anti-inflammatory agents or the cyclooxygenase-2 inhibitors. Traditionally, the tricyclic antidepressants have been a mainstay in the palliation of pain secondary to intercostal neuralgia. The selective serotonin reuptake inhibitors such as fluoxetine have also been used to treat the pain of intercostal neuralgia and, although better tolerated than the tricyclic antidepressants, they appear to be less efficacious. Gabapentin should be started with a 300-mg dose redundant at bedtime for 2 nights. The drug is then increased in 300-mg increments, given in equally divided doses over 2 days as side effects allow, until pain relief is obtained or a total dose of 2400 mg daily is reached. At this point, if the patient has experienced partial relief of pain, blood values are measured and the drug is carefully titrated upward using 100-mg tablets. The local application of heat and cold may also be beneficial to provide symptomatic relief of the pain of intercostal neuralgia. For patients who do not respond to these treatment modalities, intercostal nerve block using local anesthetic and steroid may be a reasonable next step. In addition to the dorsal spine pain, which radiates in a thoracic dermatomal distribution, the patient with thoracic radiculopathy may experience associated paresthesias, numbness, weakness, and, rarely, loss of superficial abdominal reflexes. The causes of thoracic radiculopathy include herniated disk, foraminal stenosis, tumor, osteophyte formation, vertebral compression fractures, and, rarely, infection. Signs and Symptoms the patient suffering from thoracic radiculopathy will complain of pain, numbness, tingling, and paresthesias in the distribution of the affected nerve root or roots. Decreased sensation, weakness, and, rarely, superficial abdominal reflex changes are demonstrated on physical examination. Occasionally, a patient suffering from thoracic radiculopathy will also experience compression of the thoracic spinal nerve roots resulting in myelopathy. Thoracic myelopathy is most commonly due to midline herniated thoracic disk, spinal stenosis, demyelinating disease, tumor, or, rarely, infection. Patients suffering from thoracic myelopathy will experience varying degrees of neurologic disturbance based on the level and extent of cord compression. Thoracic myelopathy represents a neurosurgical emergency and should be treated as such. Pain syndromes that may mimic thoracic radiculopathy include dorsal spine strain, thoracic bursitis, thoracic fibromyositis, inflammatory arthritis, mononeuritis multiplex, infectious lesions such as epidural abscess, and disorders of the thoracic spinal cord, roots, plexus, and nerves. Although this testing provides the clinician with useful neuroanatomic information, electromyography and nerve conduction velocity testing will provide the clinician with neurophysiologic information that can delineate the actual status of each individual nerve root and the thoracic plexus. Screening laboratory testing consisting of complete blood count, erythrocyte sedimentation rate, and automated blood chemistry testing should be performed if the diagnosis of thoracic radiculopathy is in question. Thoracic epidural blocks with local anesthetic and steroid have been shown to be extremely effective in the treatment of thoracic radiculopathy. In addition, the joints are subject to invasion by tumor either from primary malignancies, including thymoma, or from metastatic disease. Coughing may be difficult, and this may lead to inadequate pulmonary toilet in patients who have sustained trauma to the anterior chest wall. The costosternal joints and adjacent intercostal muscles may also be tender to palpation. Magnetic resonance imaging of the joints is indicated if joint instability or occult mass is suspected. Signs and Symptoms Physical examination of the patient suffering from costosternal syndrome will reveal that the patient will vigorously attempt to splint the joints by keeping the shoulders stiffly in neutral position. Pain is reproduced with active protraction or retraction of the shoulder, deep inspiration, and full elevation of the arm. Shrugging of the shoulder may also reproduce the Differential Diagnosis As mentioned, the pain of costosternal syndrome is often mistaken for pain of cardiac origin and can lead to visits to the emergency department and unnecessary cardiac workups. Neuropathic pain involving the chest wall may also be confused or coexist with costosternal syndrome. Pathologic processes such as pulmonary embolus, infection, and Bornholm disease can inflame the pleura. Treatment Initial treatment of the pain and functional disability associated with costosternal syndrome should include a combination of the nonsteroidal anti-inflammatory agents or the cyclooxygenase-2 inhibitors. The use of an elastic rib belt may also help provide symptomatic relief and help protect the costosternal joints from additional trauma. For patients who do not respond to these treatment modalities, injection of the costosternal joints may be a reasonable next step. The manubrium articulates with the body of the sternum via the manubriosternal joint. The joint articulates at an angle called the angle of Louis, which allows for easy identification. The joint is a fibrocartilaginous joint, or synchondrosis, that lacks a true joint cavity. Above, the manubrium articulates with the sternal end of the clavicle and the cartilage of the first rib. The joint is often traumatized during acceleration/deceleration injuries and blunt trauma to the chest. The joint is also subject to invasion by tumor from primary malignancies, including thymoma, or metastatic disease. Magnetic resonance imaging of the joint is indicated if joint instability is suspected. Injection of the manubriosternal joint with local anesthetic will serve as both a diagnostic and therapeutic maneuver. Differential Diagnosis As mentioned, the pain of manubriosternal joint syndrome is often mistaken for pain of cardiac origin and can lead to visits to the emergency department and unnecessary cardiac workups. If trauma has occurred, costosternal syndrome may coexist with fractured ribs or fractures of the sternum itself, which can be missed on plain radiographs and may require radionuclide bone scanning for proper identification. Neuropathic pain involving the chest wall may also be confused or coexist with manubriosternal joint syndrome. Examples of such neuropathic pain include diabetic polyneuropathies and acute herpes zoster involving the thoracic nerves.
Tegretol 200 mg sale
Evidence must be used to discuss the mistakes muscle relaxants yahoo answers cheap generic tegretol canada, and performance management strategies put in place to ensure that the mistakes are acknowledged and learnt from. Whenever possible, it is best to speak directly to the member of staff who has made the mistake, informing them of the outcome and any action you have taken. If necessary, involve another senior member of staff or your manager in the discussion. Ensure that you are aware of local policies and proce dures to minimize the risk of mistakes occurring. This can range from a patient becoming verbally abusive because of a long wait for medicines to be dispensed to an armed robbery of a community pharmacy. The emotional distress can be i in a healthcare setting because staff might feel unprepared for this type of behaviour from a patient or customer they are trying to help. If healthcare teams have strategies to review and discuss inci dents of threatening behaviour, staff find this useful for coping and learning. Being pre pared for this type of incident, and knowing strategies to deal with or defuse such a situation, is of great value. Hand over any money or goods demanded, because insurance cover can replace loss but not lives. If you have to go into a room alone with them, leave the door open and make sure a colleague is close by to give you backup if necessary. Explain to the patient how to make a written complaint if they wish (frequently the patient will back down at this point). In an extreme situation, it may be necessary to enlist the help of security staff or even call the police. Limit setting In some situations, it might not be possible to avoid continued contact with a patient who has been aggressive or violent towards staff. This might be an inpatient who needs further medical care or someone attending for further outpatient appointments or repeat prescriptions. In these cases, it might be possible to avoid further threatening incidents by setting limits. An effective system is to draw up a contract detailing what is expected of the patient and what behaviour is considered unacceptable, and, in return, what the patient can expect from the healthcare team. The contract should state what will happen if the patient breaks the limits-usually a single warn ing, followed by withdrawal of services if the limits are broken again. These contracts can be very helpful in controlling patient behaviour, but it must be a twoway process-healthcare staff must also stick to their side of the contract both in terms of providing care and being prepared to carry out the threat of withdrawing care if the limits are broken. If faced with this situation, even the busiest pharmacist should try to spend some time comforting or supporting the patient as best they can. Even if you have had to deal with the same situation yourself, it is presumptuous to state that you know how another person feels. As appropriate, suggest that they might like to speak to a senior member of staff-e. Just sitting with a patient for a few minutes while they get their emotions under control can be very helpful. Although in general, patients spend most of their final year of life at home, 90% of patients spend some time in hospital and 55% die there. As a pharmacist, you might not be as closely involved in the care of a dying patient as the nursing or medical staff, but it is still a situation that affects most pharmacists at some stage. Some pharmacists, such as those working in palliative care, oncology, or intensive care units, may be quite involved in the care of both the dying patient and their family. It is important to let these processes happen, while supporting the patient and family sensitively. Providing information about the illness enables the patient and family to make informed decisions about medical care and personal and social issues, and this is where you can help. Patients and relatives may perceive doctors as being too busy to answer their questions or be embarrassed to ask. A pharmacist might be perceived as having more medical knowledge (and being less busy! If the patient asks you directly whether they are dying, it is probably not appropriate for a pharmacist to confirm this. An appropriate response might be to ask why they are asking you this or to enquire what they have been already told and then formulate an appropriate response. Answer these questions as fully as you can, without overloading the patient with information. Be practical with your information and remember that some cautions become irrelevant at this stage-e. However, you could help the patient to formulate the question so that they feel better able to ask the doctors. The information you provide will depend on the situation and your level of expertise. The patient or the circumstances of their illness/death might remind you of the death of a close relative or friend. Talking to a colleague, hospital chaplain, or close friend might help, but bear in mind that you must maintain confidentiality. Attending the funeral can benefit healthcare workers, in addition to giving the family support. Avoid wearing a uniform, remove identification badges and bleeps, and consider whether wearing a symbol, such as a red or pink ribbon, would be inappropriate. If you are unsure whether it would be appropriate to attend, discuss it with a senior member of staff-e. However, you might be aware that a patient has expressed this desire to other staff. Whatever your personal view on the morality of euthanasia, you should treat the patient the same as any other. However, it is generally considered acceptable to give treatment that is adequate to control symptoms, even if this could shorten the duration of life, provided that the primary intent is symptom control. If you have any concerns about the appropriateness of therapy/doses in this situation, you should discuss this with the prescriber and/or a senior colleague. Although not a common occurrence, clinical pharmacists can be the first to realize that a patient has died, often quietly in their bed or a chair. Find a nurse or a member of the medical team immediately to deal with the patient, as appropriate. It might be useful, as part of the pharmacist induction, to visit the mortuary, because dealing with death requires professional support. This might be because of a lack of scientific evidence, but it is more fre quently where moral, religious, or other values have a significant influence on decisionmaking. Thus, medical ethics differs from research ethics; the latter is concerned with evaluating whether clinical trials are appropriate, safe, and in the best interests of the participants and/or the wider pop ulation. Many hospitals have a medical ethics committee in addition to a research ethics committee. They might produce guidelines to cover certain issues, but frequently a committee does not give a definite answer and simply provides a forum for debate. However, there are occasions where pharmacists are faced with dilemmas for which there is no clear course of action. In many instances, there is not a right or wrong answer and different people might make different-but equally justifiable-decisions based on the same set of circumstances.
Purchase tegretol 200mg with amex
Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine and American Society for Parenteral and Enteral Nutrition: executive summary spasms under right rib cage order 400mg tegretol fast delivery. Bleck cervical approach can be performed by a physician trained in this technique. Freshfrozenplasma and platelets should be infused to correct hematologic abnormalities before the procedure. This is usually the most rostral space employed because the adult spinal cord ends at L2. Walk the fingers down the spinous processes to identifytheL4-5andL5-S1interspaces,andmarkthemontheskin. Ponce Mejia, Jovany Cruz Navarro, Santhosh Sadasivan, Shankar Gopinath, Bartley Mitchell, and Claudia S. Immediatelydistal to the jugular foramen, the vein dilates, forming the jugular venous bulb. Catheterplacementiseasier,andcontinuousoxygensaturation measurements will usually be better on the side with the greatestbloodflow. As you advance the needle, maintain negative pressure in the syringe until the vein is punctured. Careshouldbetakeninremoving the catheter, as the fiberoptics may be damaged if the catheter is withdrawnimproperly. Theguide wire can be visualized in both cross-sectional and longitudinal views within the lumen of the internal jugular vein in the ultrasoundscreen. Blood and debris may be removed from the cables with a towel and aqueous soap solution that also may contain formaldehyde. Diagnosis of traumatic carotid-cavernous sinus fistula by monitoring venous oxygen saturation in the jugular bulb: report of two cases. The physiology behind direct brain oxygen monitors and practical aspectsoftheiruse. Monitoringcerebraloxygenation:experimental studies and preliminary clinical results of continuous monitoring of cerebrospinal fluid and brain tissueoxygentension. Close the incision wound with sutures, and secure the catheter to the scalp with nylon suture. Using an external flexible catheter inserted into the lateral cerebral ventricles. Fiberoptic monitors are zeroed before insertion and are not affected by the patient position or bed height. The rate of catheter-related infection is lower with intraparenchymal than intraventricularcatheters. Neurologic outcome of posttraumatic refractory intracranial hypertension treated with external lumbar drainage. Theright neck and the appropriate groin region are prepared and draped in a sterile fashion, and anesthesia is achieved with a local anesthetic. The wire is then replaced, and, using it as a guide, sequentially larger dilators are passed. Itisveryimportanttoensure that the wire moves freely during dilatation as well as cannula insertion. Kinking can be prevented by gentle traction on the wire applied by an assistant as the dilator or cannula is passed. The preferred drainage site is the femoral vein, and the cannula is advanced to just below the caval-atrial junction. Ifdecreased heparinization and low flow in this system are concerns, heparin of 0. The median sternotomy is the least favored as this site is associated with more bleeding complications. The cannulae may be tunneled inferior to the sternum and the chest then closed for hemostasis. Bass L aparoscopy has proven itself an accurate diagnostic tool in a wide spectrum of clinical scenarios. Etiologies include acalculous cholecystitis, intestinal ischemia, intestinal perforation, peptic ulcer disease complications, pseudomembranous colitis, diverticulitis, and pancreatitis, to name a few. While those above occur relatively infrequently, associated morbidity and mortality are significant. The reported mortality rates specific to acalculous cholecystitis and mesenteric ischemia range from 50% to 100%. A significant contributor to the high morbidity and mortality rates is a delay in diagnosis. Such delays are multifactorial and include failure to consider the diagnosis, difficulty in obtaining the diagnosis secondary to patient safety issues, and the lack of accuracy of the diagnostic modalities. Critically ill patients also have numerous other potential sources of sepsis, further complicating the picture. As such, surgical consultations are often sought in these patients; indications include abdominal pain, abdominal distention, a fever of unknown etiology, sepsis of unknown etiology, inexplicable acidosis, enteral intolerance, and others. Patients with portal hypertension are at an increased risk of bleeding due to the inadvertent injury of dilated venous collaterals that are not normally present within the abdominal wall. Finally, the inferior epigastric artery is at risk for injury during trocar placement, and careful attention should be paid to avoid its consistent location within the rectus sheath. Blind techniques can be used if deemed safe and can minimize the incision necessary for peritoneal access. If the procedure is performed for a trauma patient, inspection of the diaphragm should be the first step (to reduce risk of tension pneumothorax if diaphragm injury). A quick inspection around the abdominal cavity for any obvious signs of peritonitis. If found, terminate the procedure and prepare for the formal therapeutic operation. Complete the inspection as you would with formal exploration, in an organized fashion, including all abdominal and pelvic viscera in addition to peritoneal surfaces. Use of bedside laparoscopy to identify intestinal ischemia in postoperative cases of aortic reconstruction. Postoperative abdominal complications in cardiopulmonary bypass patients: a case controlled study. The acute surgical abdomen after cardiac surgery involving extracorporeal circulation. Acute illnesses necessitating urgent abdominal surgery in neutropenic cancer patients: description of 14 cases and review of the literature. Diagnostic laparoscopy in the intensive care patient: avoiding the nontherapeutic laparotomy. Hemodynamic effects of the laparoscopic pneumoperitoneum during sepsis in a porcine endotoxic shock model. Experimental animal models demonstrate hemodynamic compromise in septic animals undergoing laparoscopy, usually secondary to the associated hypercarbia and acidosis. In 6 of the 11 patients studied, the use of bedside laparoscopy avoided nontherapeutic open laparotomy. Haemodynamic changes during laparoscopic cholecystectomy in the high risk patient. The role of peritoneoscopy (laparoscopy) in the evaluation of the acute abdomen in critically ill patients. Morphine-augmented hepatobiliary scintigraphy in the severely ill: caution is in order. Accuracy of diagnostic laparoscopy for early diagnosis of abdominal complications after cardiac surgery. Bedside diagnostic laparoscopy to diagnose intraabdominal pathology in the intensive care unit.
Order tegretol with amex
Private patients usually have private health insurance quetiapine muscle relaxer cheap tegretol 200 mg with visa, which covers some, or all, of the costs of private treatment. Hospitals should have specific policies in place for patients requesting additional private care in accordance with this guidance. Furthermore, sales of pharmacy and prescription-only medicines had to be under the supervision of a pharmacist. It was recognized that, to improve the range of services available in pharmacies, pharmacists must be able to work more flexibly and be allowed to undertake their role out of the pharmacy for a limited period to make better use of their clinical training and the skills of pharmacy staff, and hence the concept of the responsible pharmacist was developed. Responsible pharmacists-hospital pharmacists the responsible pharmacist changes to the Medicines act only affect those hospitals that have registered all or part of their pharmacy premises with the General Pharmaceutical Council. If you have a registered pharmacy within the hospital, the law and standards for responsible pharmacists will apply. This means that the registered pharmacy is required to have a responsible pharmacist when it is operating as a pharmacy business. The responsible pharmacist is the pharmacist appointed by the employer, who is responsible for securing the safe and effective running of the pharmacy at that time. The responsible pharmacist continues to be responsible for securing the safe and effective running of the pharmacy during any periods of absence. If there is more than one pharmacist working in the pharmacy at any one time, only one can be the responsible pharmacist. Pharmacy record this is an important legal document, it should show who the responsible pharmacist is on any particular given day and time. The record must be kept for at least 5yrs and must be available at the premises for inspection. Notice display the notice is important to ensure that the public can identify the pharmacist who is responsible for the safe and effective running of the registered pharmacy. Absence of the responsible pharmacist a responsible pharmacist can be absent from the pharmacy for a maximum of 2h during the business hours of the pharmacy when the pharmacy is operational. The responsible pharmacist continues to be responsible for the safe and effective running of the pharmacy throughout this absence. Gene therapy can be divided into two main categories: gene replacement and gene addition. For gene therapy to be successful, a therapeutic gene must be delivered to the nucleus of a target cell, where it can be expressed as a therapeutic protein. The greatest challenge to gene therapy is finding a vector that can transfer therapeutic genes to target cells specifically and efficiently. They have a unique ability to enter (infect) a cell, delivering viral genes to the nucleus using the host cell machinery to express those viral genes. Replication-deficient viruses have had the viral genes required for replication and the pathogenic host response removed. This prevents the virus replicating and the potential for the therapeutic virus to reverse back to a pathogenic virus. The deleted genes are replaced by a therapeutic gene, thus allowing the delivery and expression of the therapeutic gene without subsequent spread of the virus to surrounding cells. Some gene therapy vectors are able to replicate under genetically specified conditions. There is the potential for infectious hazards with gene therapy, including possible transmission of the vector to hospital personnel. Therefore, consideration has to be given to protecting both the environment and the staff handling these agents, because of the uncertain effects of specific genes on normal human cells, potential for operator sensitization on repeated exposure, and the potentially infective nature of some products. Some gene therapy agents might require handling in negative-pressure isolators in separate specific aseptic facilities. Trusts undertaking clinical trials with gene therapy products should have a local Genetic Modification Safety Committee, a Trust biological safety officer, and local biological safety officers for the units handling these trials. Genetically modified organisms are classified as one of four classes (1, 2, 3, and 4) and their classification determines the level of containment required to control the risk. Class 1 activities are unlikely to result in harm to humans or the environment and require containment level 1. Development of procedures to address health and safety considerations for the administration of gene therapy within the clinical setting. For example, genetic make-up may determine variations in liver enzymes that are produced, which in turn affect drug metabolism. This has enabled drug development to be much more targeted, so that only patients with specific characteristics receive the appropriate drugs. There will be issues regarding the quality of the tests, their initiation, communication to the patient, and the implication of the test to treatment. The general public would need to be more widely educated about pharmacogenetics and its implications. Currently there are some home test kits available, but the sale of these is not regulated. This means that some of the test kits available have no guarantee of being validated or of producing accurate results. For example, there is concern that some individuals may not be able to obtain insurance policies if their genetic test results are considered negatively. There is also concern about the privacy and confidentiality of genetic information, where it should be stored, and who would have access to it. Drug companies may only research drugs for diseases that are straightforward to treat, rather than those that could be used for rarer diseases. In addition, pharmacogenetic testing may predict for future risks of disease or raise implications for other family members, which adds to the ethical issues of informing patients and their families. This means that in the future, patients will be prescribed drugs specific to their conditions, taking into account genetic factors when deciding on dosage regimens. In addition, there may be a loss of any benefit of, for example, racemic mixtures. The current regulations are detailed in the Hazardous Waste Regulations 2009, and further guidance specifically for community pharmacies are detailed in the Department of Health document Health Technical Memorandum 07-01: Environment and Sustainability-Safe management of healthcare waste. The storage, carriage, processing, and supply of waste are all subject to stringent controls designed to minimize the negative effects of waste on the environment. The Environment agency or the relevant local authority is the enforcement authority for the legislation. Depending on the circumstances, and in cases of doubt, either can be contacted for advice. Policies Hospital or community pharmacies must have a waste management policy that details general themes, including dealing with pharmaceutical waste such as cytotoxics. The guidance also details the types of containers that need to be used for segregation and transportation of the different types of waste. Medicines brought into hospital by patients Medicines brought into hospital by the patient are the property of the patient and should only be sent to pharmacy for destruction with the prior agreement from the patient or their agent. Handling waste within the pharmacy the Hazardous Waste Regulations 2005 introduced significant changes for pharmacies. They required pharmacies to separate hazardous waste medicines from non-hazardous waste. Hazardous waste medicines and non-hazardous waste medicines must be separated before they are sent to a suitably authorized waste contractor for incineration. Whenever waste that may contain some hazardous waste medicine is sent for incineration, it is required to be consigned as though it were hazardous and needs to be accompanied by a hazardous waste consignment note.
Purchase tegretol visa
Universal changes in biomarkers of coagulation and inflammation occur in patients with severe sepsis muscle relaxant erowid order tegretol on line amex, regardless of causative micro-organism. Early activation of coagulation and fibrinolysis in traumatic brain injury and spontaneous intracerebral hemorrhage: a comparative study. The current status of thromboprophylaxis after trauma: a story of confusion and uncertainty. It is defined as a sudden transfer of energy (thermal, electrical, mechanical, chemical, or radiation) that is physiologically intolerable or as damage that results in psychologic harm, deprivation, or maldevelopment. In the United States, injury remains the leading cause of mortality in children and remains a significant health burden. This chapter provides an overview of caring for critically injured pediatric patients. Additionally, policies and protocols that are understood and adhered to by all team members should be in place. The initial resuscitation team is usually led by a surgeon and performs best when led by an attending trauma surgeon. The prepared trauma team improves performance in resuscitation as well as outcome of the patient. The pediatric critical care physician has expertise in life-support therapies including mechanical ventilation, renal replacement therapies, and treatments to prevent secondary brain injury. Such teams should include all necessary trauma team members and work to develop treatment algorithms and protocols. There is mounting evidence that this approach leads to improved outcomes in pediatric trauma and is soon becoming the standard of care. This concept advocated that the trauma system be broadened to include all phases of injury and also include a multidisciplinary approach for the treatment of trauma. Trauma systems have now matured to include a network of verified trauma centers within most states and regions. In most states, trauma centers meeting stated criteria become "verified" to deliver a specified level of care based on available resources. Level 1 trauma centers are considered the highest verification level and provide comprehensive, multidisciplinary care to injured patients. Verified trauma centers also participate in regional, state, and national quality improvement initiatives by reporting their data. Trauma centers also frequently participate in research to advance the care of injured patients. It is well recognized that trauma systems and dedicated trauma centers improve outcomes and reduce mortality secondary to injury. Trauma centers with specialized expertise in pediatric trauma continue to show advantages for injured children when compared to other centers without such expertise. Pediatric injury requires dedicated expertise, and children have improved outcomes with reduced mortality when admitted directly from the injury scene compared to those admitted by hospital-tohospital transfer. The trauma team refers to all who care for the trauma patient, from the initial resuscitation to hospital discharge. Other healthcare personnel may also be included in the trauma team, such as clergy, mental health specialists, and rehabilitation physicians. While special consideration is given to anatomic and physiologic differences of children, the priorities of resuscitation remain the same as those in adults. A primary survey is conducted to rapidly assess the patient and identify all potential life-threatening injuries. The first priority remains assessment of the airway for patency and maintainability and cervical spine stabilization. Adequate airway control must be obtained while maintaining cervical spine immobilization. When intubation is required, most trauma patients should be orally intubated with direct cricoid pressure, and the most experienced clinician should perform intubation. Doses are adjusted for patient weight, and guidelines are available on the Broselow tape. The reason for intubation as well as the types of injuries present dictate the medications used. Tracheal tube placement should be confirmed by end-tidal carbon dioxide monitoring, by auscultation of the abdomen and both sides of the chest, and by a chest radiograph. Evaluation of unequal breath sounds with a correctly positioned endotracheal tube should raise concern for a hemothorax or pneumothorax. Tracheal deviation, though rare, may help with the diagnosis of tension pneumo- or hemothorax. Breath sounds are transmitted easily in children, and a simple pneumothorax is often not apparent until a chest radiograph is obtained. After successful airway establishment and ventilation, the circulation must be assessed. Pulses, perfusion, capillary refill, heart rate and rhythm, and blood pressure should be evaluated. Intraosseous access or venous cut-down should be considered if peripheral access is difficult to obtain. Young children have vigorous compensatory mechanisms and will preserve blood pressure despite losing more than 25% of their circulating blood volume. The heart rate is the most sensitive indicator of hypovolemia in pediatric trauma patients. Thready pulses and altered mental status are evident with a loss of 30% to 45% of blood volume and represent a dangerous scenario as cardiovascular collapse will be imminent. Resuscitation with red blood cells, plasma, and platelets in a ratio of 1: 1: 1 along with appropriate use of coagulation factors such as cryoprecipitate, as well as rapid surgical control, may be necessary for ongoing hemorrhage. The attending pediatric surgeon should direct the resuscitation of a pediatric patient with active hemorrhage. All infused fluids and blood products should be warmed as pediatric patients are at high risk of hypothermia. Hypotension contributes to secondary injury to the brain and other vital organs and must be treated aggressively. Trauma victims who are pulseless at the scene have an almost uniformly fatal outcome. Most cardiac arrests associated with blunt trauma are a result of multisystem injuries, including severe brain injury. The patient should be log rolled to inspect the spine and back and complete the assessment of obvious injuries. A rectal examination should only be performed one time when clinically appropriate as determined by the attending pediatric surgeon. Children lose heat due to their increased body surface area to volume ratio and should be warmed with lights and blankets. Following the primary survey and stabilization, necessary laboratory studies are performed, and radiology studies including a chest x-ray and pelvic x-ray should be obtained. Injuries are documented, necessary consultations are placed, and the team decides on the disposition of the patient. Secondary injury refers to the injury that occurs after impact and is considered both preventable and potentially reversible. Pathologic alterations in respiratory, hemodynamic, and cellular function occur, which may lead to secondary injury and cell death. The pathways to neuron death include inadequate oxygen and nutrient supply secondary to hypoxia and decreased cerebral blood flow. Other neuronal injuries occur secondary to inflammation, oxidative stress, and apoptosis. There is little evidence to support the routine use of corticosteroids or the prophylactic use of antiseizure medication. The underlying goal is airway protection and respiratory support to prevent hypoxemia and hypercarbia. Hyperoxia and brief, aggressive hyperventilation is indicated only if the clinical examination reveals signs of acute cerebral herniation. These maneuvers should be directed by neurosurgery and are usually initiated immediately before operative intervention. Normotension or mild hypertension and mild hypervolemia are indicated to support cardiac output and cerebral blood flow. Sedation can be accomplished with low-dose fentanyl, dexmedetomidine, and intermittent doses of benzodiazepines or barbiturates. Small airway diameter combined with penetrating or blunt injury to the neck can produce rapid airway obstruction.