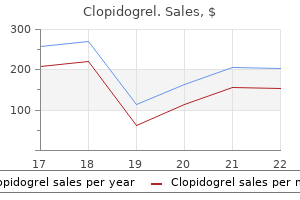
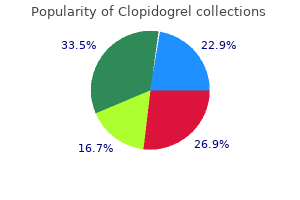
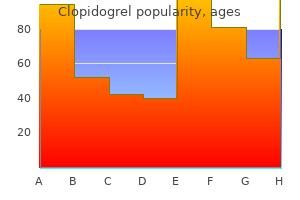
Order clopidogrel 75mg free shipping
It is frequently diseased medications side effects buy generic clopidogrel 75mg online, as the embedded organ has difficulty in contracting and so becomes infected, with subsequent gallstone formation. Developmentally, these peritoneal sheets are due to an extension of the anterior mesentery, which forms the lesser omentum. The sheet may run from the common bile duct laterally over the gallbladder down to the duodenum, to the hepatic flexure of the colon, and even to the right lobe of the liver, perhaps closing the foramen of Winslow. Surgically, their presence should be remembered, so that they are not mistaken for inflammatory adhesions. The peritoneal coat surrounding the gallbladder continues as two approximated leaves to form a fold or mesentery to support the gallbladder from under the surface of the liver. With ageing, omental fat lessens and there is a great caudal displacement of abdominal viscera due to loss of tone in the abdominal and pelvic muscles. Torsion is followed by sudden, severe, constant epigastric and right costal margin pain radiating to the back with vomiting and collapse. Characteristically, a palpable tumour appears, having the features of an enlarged gallbladder. Anomalies of the cystic duct and cystic artery In 20% of people, the cystic duct does not join the common hepatic duct directly but first runs parallel to it, lying in the same sheath of connective tissue. Unless the cystic duct is carefully dissected and its union with the common hepatic duct identified, the common hepatic duct may be ligated, with serious consequences. The cystic artery can arise not, as normally, from the right hepatic artery but from the left hepatic artery or even from the gastroduodenal artery. New advances in evaluation and management of patients with polycystic liver disease. Hepatobiliary fibropolycystic disease: a clinical and histological review of 51 patients. Mechanisms of disease: autosomal dominant and recessive polycystic kidney disease. Mammalian target of rapamycin regulates vascular endothelial growth factordependent liver cyst growth in polycystin2 defective mice. Postmenopausal oestrogen therapy selectively stimulates hepatic enlargement in women with autosomal dominant polycystic kidney disease. Intracranial aneurisms in patients with autosomal dominant polycystic kidney disease: prevalence, risk of rupture and management. Evaluation of ultrasonographic diagnostic criteria for autosomal dominant polycystic kidney disease 1. Effects of angiogenic factor overexpression by human and rodent cholangiocytes in polycystic liver diseases. Octreotide inhibits hepatic cystogenesis in vitro and in vivo: a new therapeutic approach for treatment of polycystic liver diseases. Randomized clinical trial of longacting somatostatin for autosomal dominant polycystic kidney and liver disease. Lanreotide reduces the volume of polycystic liver: a 29 30 31 32 33 34 35 36 37 38 39 40 41 42 randomized, doubleblind, placebocontrolled trial. Embryology of the liver and intrahepatic biliary tract, and an overview of the malformations of the bile ducts. Refining the map and defining flanking markers of the gene for autosomal recessive polycystic kidney disease on chromosome 6p21. The gene mutated in autosomal recessive polycystic kidney disease encodes a large, receptorlike protein. Congenital 44 45 46 47 48 49 50 51 52 53 54 55 56 57 hepatic fibrosis and polycystic kidney disease; role of porta caval shunting and transplantation in three cases. Phenotypic variation and long term outcome in children with congenital hepatic fibrosis. Characteristics of congenital hepatic fibrosis in a large cohort of patients with autosomal recessive polycystic kidney disese. Pulmonary arteriovenous fistulas: an unusual complication of congenital hepatic fibrosis. Congenital hepatic fibrosis (asymptomatic and latent forms) and multiple gastric ulcers. Intrahepatic cholangiocarcinoma arising in congenital hepatic fibrosis: report of an autopsy case. Adenomatous hyperplasia of the liver in a patient with congenital hepatic fibrosis. Carbohydrate deficient glycoprotein syndrome type 1b: phosphomannose isomerase deficiency and mannose therapy. Autosomal recessive polycystic kidney disease: a hepatorenal fibrocystic disorder with pleiotropic effects. Choledochal cyst: anomalous arrangement of the pancreaticobiliary ductal system and biliary malignancy. Expressions of p53 and inducible nitric oxide synthase in congenital choledochal cysts. Role of pressure and pancreatic reflux in the aetiology of choledochal malformation. Solitary cystic dilation of the intrahepatic bile duct: morphology of two autopsy cases and a review of the literature. Carcinoma related 83 84 85 86 87 88 to choledochal cysts with internal drainage operations. Longterm outcomes after hepaticojejunostomy for choledochal cyst: a 10 to 27year followup. A case of primary squamous cell carcinoma of the liver arising in a solitary cyst. Agenesis of the gallbladder in symptomatic adults: a case and review of the literature. Pruritus and fatigue are important symptoms with a significant impact on quality of life. There are three typical presentations: Screening: this is the commonest route of presentation in the modern era. Patients present after identification of characteristic serum biochemistry and/or autoantibodies during a routine health check or monitoring for other health conditions. Advanced disease: Although less frequently seen as a presenting complex than was the case previously, a number of patients still present with the clinical features of advanced liver disease, most typically jaundice and variceal bleeding [6]. The advent of better and more widely available diagnostic tests means that disease is now usually identified in the early stages when cirrhosis is not present and, to reflect this change, the name was changed in 2015 to primary biliary cholangitis [3]. The serum albumin level is usually normal at presentation and the serum IgM is usually raised. This is not reliable for diagnosis, although an increase may add some diagnostic weight. Use of the second method can be useful on those occasions where atypical patterns are encountered. It is important to take the route of presentation into consideration when approaching the newly diagnosed patient. Symptom impact also varies and it is important when approaching patients that as much importance is placed on addressing the often significant symptoms of the condition as on managing advanced disease risk. A definite diagnosis requires the presence of all three criteria and a probable diagnosis requires two. Although this definition was introduced for use in epidemiological studies, it has now entered routine practice. A cellular reaction, including lymphocytes, plasma cells, eosinophils, and histiocytes, surrounds the damaged ducts. Their sites are marked by aggregates of lymphoid cells, and bile ductules begin to proliferate.
Purchase discount clopidogrel online
Hepatocanalicular bile salt export pump deficiency in patients with progressive familial intrahepatic cholestasis symptoms for pneumonia order clopidogrel us. Nasobiliary drainage induces longlasting remission in benign recurrent intrahepatic cholestasis. Defect of multidrugresistance 3 gene expression in a subtype of progressive familial intrahepatic cholestasis. Atp8b1 deficiency in mice reduces resistance of the canalicular membrane to hydrophobic bile salts and impairs bile salt transport. Molecular cloning, chromosomal localization, and functional characterization of a human liver Na+/bile acid cotransporter. Exploring possible mechanisms for primary bile acid malabsorption: evidence for different regulation of ileal bile acid transporter transcripts in chronic diarrhoea. Analysis of ileal sodium/bile acid cotransporter and related nuclear receptor genes in a family with multiple cases of idiopathic bile acid malabsorption. Familial idiopathic adulthood ductopenia: a report of five cases in three generations. Nonsyndromic paucity of intrahepatic bile ducts in infancy and idiopathic ductopenia in adulthood: the same syndrome Antibioticassociated acute vanishing bile duct syndrome: a pattern associated with severe, prolonged, intrahepatic cholestasis. Association of spinocerebellar disorders with cystic fibrosis or chronic childhood cholestasis and very low serum vitamin E. Partial external diversion of bile for the treatment of intractable pruritus associated with intrahepatic cholestasis. The pruritus of cholestasis: 88 89 90 91 92 93 94 95 96 97 98 99 100 evolving pathogenic concepts suggest new therapeutic options. The potent bile acid sequestrant colesevelam is not effective in cholestatic pruritus: results of a double blind, randomized, placebocontrolled trial. Hepatitis and liver dysfunction with rifampicin therapy for pruritus in primary biliary cirrhosis. Bezafibrate normalizes alkaline phosphatase in primary biliary cirrhosis patients with incomplete response to ursodeoxycholic acid. Oral naltrexone treatment for cholestatic pruritus: a doubleblind, placebocontrolled study. Longterm efficacy of sertraline as a treatment for cholestatic pruritus in patients with primary biliary cirrhosis. Treatment of pruritus in chronic liver disease with the 5 hydroxytryptamine receptor type 3 antagonist ondansetron: a randomized, placebocontrolled, doubleblind crossover trial. Analysis of surgical 102 103 104 105 106 107 108 109 interruption of the enterohepatic circulation as a treatment for pediatric cholestasis. Plasmapheresis exerts a longlasting antipruritic effect in severe cholestatic itch. Ursodeoxycholic acid therapy in intrahepatic cholestasis of pregnancy: results in realworld conditions and factors predictive of response to treatment. Low body mass index and use of corticosteroids, but not cholestasis, are risk factors for osteoporosis in patients with chronic liver disease. Bone disease in patients with primary sclerosing cholangitis: prevalence, severity and prediction of progression. Primary biliary cirrhosis is not an additional risk factor for bone loss in women receiving regular calcium and vitamin D supplementation: a controlled longitudinal study. Vitamin Dreceptor genotypes as independent genetic 110 111 112 113 114 115 116 117 118 119 120 predictors of decreased bone mineral density in primary biliary cirrhosis. Prospective study of periostitis and finger clubbing in primary biliary cirrhosis and other forms of chronic liver disease. The pathology of jaundice related renal insufficiency: cholemic nephrosis revisited. Primary biliary cirrhosis, hyperlipidemia, and atherosclerotic risk: a systematic review. Laparoscopic cholecystectomy is the main treatment option for symptomatic gallbladder stones. Chronic biliary tract diseases are rare, complex, and require multidisciplinary management. Introduction Gallstones and benign biliary strictures are the two most common biliary tract disorders that require multidiscipli nary management involving surgeons, endoscopists, and interventional radiologists. Symptoms and laboratory tests may suggest a biliary tract pathology but a thorough history and clinical examination are essential. Gallbladder disease is a common cause of right upper quadrant pain, but there are many other causes, emphasiz ing the need for a careful clinical and radiological evalua tion. Cholestatic liver function tests with or without jaundice, itching, pain, or fever suggest bile duct disease, but these features are not specific. Clinical examination may be useful in showing characteristic tenderness in the right upper quadrant with acute cholecystitis. Splenomegaly raises the question of chronic liver disease, although haematological and other causes need to be remembered. Liver tests (bilirubin, transaminases, alkaline phosphatase, glutamyl transpeptidase) will generally be normal in gallbladder dis ease, although there may be mild abnormalities with acute cholecystitis. Characteristically, serum alkaline phosphatase and glutamyl transpeptidase, with or without bilirubin, are high when bile drainage is impaired. However, a sudden rise (and usually fall) of transaminases may be seen when acute bile duct obstruction occurs due to a gallstone, lead ing to an initial search for a cause of hepatitis. Cases are often straightforward, but a multidisciplinary approach is optimal to avoid inappropriate diagnostic and therapeutic approaches. Note the thick wall of the gallbladder (between black and white arrows) with some pericholecystic fluid (single arrow). Gallbladder has not filled by 60 min, indicating cystic duct obstruction compatible with acute cholecystitis. Sphincterotomy, stone removal, stent insertion, cyto logical sampling, and balloon dilation are the most common interventions. Isotope tracks laterally from gallbladder bed (short arrow) and Ttube track (long arrow). In cases with a high risk of pancreatitis, placement of a pancreatic stent should be considered [7,8]. Gallstones Introduction Gallstones are crystalline deposits in the gallbladder [12]. The prevalence varies between 5 and 25% of the population, with a higher prevalence in Western coun tries, women, and the elderly [13]. Gallstones are broadly of three types: cholesterol, mixed (cholesterol and biliru bin pigment), and pure pigment stones (bilirubin) [14] 260 Chapter 14 Cholesterol stones are formed because of an imbalance between pronucleating factors and their inhibitors in the bile. Factors that lead to cholesterol gallstone formation include excessive biliary cholesterol, low bile salt levels, decreased gallbladder motility, and the phosphatidylcho line level, which normally prevents the crystallization of cholesterol [16]. Haemolysis and chronic bacterial or parasitic infections are considered the main risk factors for pigment stones. There is currently no evidence that lifestyle modifi cations can reduce the incidence of gallstones. In sickle cell disease, haemolysis can be prevented by early diag nosis, prevention of sickling crises, and using prophylac tic antibiotics in those who have undergone splenectomy or had splenic infarction. There is currently no evidence to suggest that prophylactic cholecystectomy is indicated in any patient group without gallstones [17] or that any preventive measures are effective. Cholesterolrich stones predominate (up to 86%); mixed stones comprise around 4%; dominant bilirubin stones are rare [15] (Table 14. Solubilization of cholesterol in bile depends upon whether there is sufficient bile salt and phospholipid (predominantly phosphatidylcholine [lecithin]) to house the cholesterol in mixed micelles. The fragment above shows the concentric structure formed as layer upon layer of cholesterol crystals aggregate. Biliary cholesterol concentration is not related to serum cho lesterol level and depends only to a limited extent on the bile acid pool size and bile acid secretory rate. Changes in bile acid type also reduce the capacity for cholesterol solubilization. A higher proportion of deoxycholate (a secondary bile acid produced in the intestine and absorbed) is found in gallstone patients. This is a more hydrophobic bile salt and, when secreted into bile, extracts more cholesterol from the canalicular membrane, increasing cholesterol saturation.
Buy clopidogrel 75 mg mastercard
The patient may also be screened for elevated levels of IgM in the blood and spinal fluid or specific trypanosomal antibodies by a variety of techniques medications hyponatremia buy clopidogrel canada. Unfortunately, the most effective agent of this type is a highly toxic arsenical, melarsoprol (Mel B). Unfortunately, it is very expensive and is only variably effective in T brucei rhodesiense infections. The tsetse fly is larviparous and carries a larva within its body until mature and ready to pupate. Similarly, eradication of disease reservoirs by the early detection and treatment of human cases and the destruction of wild game has had limited success. Attempts to develop effective vaccines are currently underway but are complicated by the antigenic variability of the trypanosomes. A degree of personal protection can be achieved with insect repellents and protective clothing. Although prophylactic use of pentamidine was once advocated, enthusiasm for this treatment has waned. American trypanosomiasis is a disease produced by T cruzi and transmitted by true bugs of the family Reduviidae, also known as kissing bugs. About 7 to 10 million people, predominantly in Central and South America are infected. Clinically, the infection may present as an acute phase with febrile illness such as seen in children, an indeterminant phase in which symptoms may largely be absent, and a chronic phase in which heart or gastrointestinal maladies are manifest, largely in adults. The circulating trypomastigotes must invade tissue cells, lose their flagella, and assume the amastigote form before binary fission can occur. Continued multiplication as amastigotes and epimastigotes in intracellular nests leads to distention and eventual rupture of the tissue cell. This new generation of trypomastigotes may invade other host cells, thus continuing the mammalian cycle. Alternatively, they may be ingested by a feeding reduviid and develop into epimastigotes within its midgut. Infection in the new host is initiated when the trypomastigotes contaminate either the feeding site or the mucous membranes. Trypanosoma cruzi comprises several strains, each with its own distinct geographic distribution, tissue preference, and virulence. In blood specimens, the trypomastigotes can be distinguished from those of T brucei by their characteristic C or U shape, narrow undulating membrane, and large posterior kinetoplast. Within these areas, it is the leading cause of chronic heart disease, accounting for 25% of all deaths in the 25- to 44-year age group. Transmission occurs primarily in rural settings, where the reduviid can find harborage in animal burrows and in the cracked walls and thatch of poorly constructed buildings. This large (3 cm) insect leaves its hiding place at night to feed on its sleeping hosts. Its predilection to bite near the eyes or lips has earned this pest the nicknames of "kissing bug" and "assassin bug. Infections can also be acquired transplacentally and through blood transfusions or organ transplantations. As many as 300 000 individuals who have immigrated from Central and South America to the United States are infected with T cruzi and likely do not know it! In addition to humans, several wild and domestic animals, including rats, cats, dogs, opossums, racoons, and armadillos, serve as reservoirs for Chagas disease. The close association of many of these hosts with human dwellings tends to amplify the incidence of disease in humans and the difficulty involved in its control. Organ transplantation and transfusion-related infections are rapidly increasing problems in urban settings within endemic areas. More effective blood bank screening provides hope that transmission of this disease will be substantially curtailed in the near future. In order for this to occur, the parasite must survive in the feces of its natural vector on foods that are consumed. In total, more than 1000 cases of infection with T cruzi has been linked with oral infection in different regions of Brazil, Columbia, Bolivia, Guyana Francesa, Argentina, and Ecuador. An estimated 300 000 infected Latin American immigrants are currently living in the United States. Because T cruzi has been found in both vertebrate and invertebrate hosts in the southern United States, there is a possibility of sustained transmission of this organism within this country. Although serologic evidence suggests that the acquisition of human infection in this area is not uncommon, clinically apparent autochthonous cases have been rare. The subsequent dissemination of the organism with invasion of tissue cells produces a febrile illness that may persist for 1 to 3 months and result in widespread organ damage. Any nucleated host cell may be involved, but those of mesenchymal origin, especially the heart, skeletal muscle, smooth muscle, and ganglion neural cells, are particularly susceptible. Cell entry is facilitated by binding to host cell fibronectin; a 60-kDa T cruzi surface protein (penetrin) appears to promote adhesion. With the rupture of the pseudocyst, many of the released parasites disintegrate, eliciting an intense inflammatory reaction with destruction of surrounding tissue. The development of an antibody-dependent, cell-mediated immune response leads to the eventual destruction of the T cruzi parasites and the termination of the acute phase of illness. It has been suggested by some that this results in the production of antibodies that cross-react with host tissue, initiating a sustained autoimmune inflammatory reaction in the absence of systemic manifestation of illness. In the heart, this reaction leads to changes in coronary microvasculature, loss of muscle tissue, interstitial fibrosis, degenerative changes in the myocardial conduction system, and loss of intracardiac ganglia. In the digestive tract, loss of both ganglionic nerve cells and smooth muscle results in dilatation and loss of peristaltic movement, particularly of the esophagus and colon. They begin with the appearance of the nodular, erythematous chagoma 1 to 3 weeks after the bite of the reduviid. The onset of parasitemia is signaled by the development of a sustained fever; enlargement of the liver, spleen, and lymph nodes; signs of meningeal irritation; and the appearance of peripheral edema or a transient skin rash. In a small percentage of symptomatic patients, heart involvement results in tachycardia, electrocardiographic changes, and occasionally arrhythmia, enlargement, and congestive heart failure. In 5% to 10% of untreated patients, severe myocardial involvement or meningoencephalitis leads to death. Chronic disease, the result of end-stage organ damage, is usually seen only in adulthood. Ironically, most patients with late manifestations have no history of acute illness. This may present as arrhythmia, thromboembolic events, heart block, enlargement with congestive heart failure, and cardiac arrest. In some areas of rural Latin America, up to 10% of the adult population may show cardiac manifestations. In the United States, chagasic heart disease in immigrants is usually initially misdiagnosed as coronary artery disease or idiopathic dilated cardiomyopathy. Megaesophagus and megacolon, which are less devastating than the heart disease, are typically seen in more southern latitudes. This geographic variation in clinical manifestations is thought to be attributable to a difference in tissue tropism between individual strains of T cruzi. Megaesophagus leads to difficulty in swallowing and regurgitation, particularly at night. Megacolon produces severe constipation with irregular passage of voluminous stools. If the results are negative, a laboratory-raised reduviid can be fed on the patient, then dissected and examined for the presence of parasites, a procedure known as xenodiagnosis. Alternatively, the blood may be cultured in a variety of artificial media or experimental animals. In the diagnosis of chronic disease, recovery of the organisms is the exception rather than the rule, and diagnosis depends on the clinical, epidemiologic, and immunodiagnostic findings.
Purchase generic clopidogrel line
If the fatty liver is sufficiently severe to merit admission to hospital symptoms stomach cancer purchase generic clopidogrel pills, the patient has usually been drinking heavily for some time and may be anorexic. Symptoms may include nausea and vomiting with periumbilical, epigastric, or right upper quadrant pain. Clinically, it can be difficult to separate the fatty liver patient from one with mild alcoholic hepatitis or even wellcompensated cirrhosis. Such cases may be asymptomatic with only a history of alcohol misuse and abnormal serum enzyme tests and/or macrocytosis. The clinical syndrome of acute alcoholic hepatitis is much more florid in presentation. Severe hepatic decompensation may be precipitated by vomiting, diarrhoea, an intercurrent infection, or prolonged anorexia. In this situation, transaminase levels are very high and distinct from alcoholic hepatitis alone [4]. The patient may experience pain over an enlarged, tender liver and an arterial hepatic bruit may be heard. Vascular spiders are usual and there may be signs of associated liver failure such as ascites, encephalopathy, and a bleeding diathesis. When present, gastrointestinal haemorrhage is frequently from a local gastric or duodenal lesion, rather than necessarily related to portal hypertension. Cirrhosis Established cirrhosis can present without acute alcohol related hepatitis and the picture can resemble any end stage liver disease. Points suggesting alcohol as an aetiological agent include the history of alcohol abuse (which may be denied), the hepatomegaly, and the extrahepatic features of hazardous drinking. Extrahepatic features Bilaterally enlarged parotids are common and are analogous to those seen with other types of malnutrition. There may be muscle wasting and falls may be complicated by fractures due to alcoholinduced osteoporosis. Dupuytren contracture of the palmar fascia is related to alcohol and not to the cirrhosis [41]. Hepatorenal syndrome seems particularly common in advanced liver disease caused by alcohol. Arrhythmias, hypertension, cardiomyopathy, and coronary artery disease are all associated with alcohol consumption. Cancer of the oropharynx, oesophagus, colon, and breast are more common in hazardous drinkers. Zone 3 fibrosis, perivenular sclerosis, and alcoholrelated hepatitis are all unfavourable histological features as they indicate a risk of progressing to cirrhosis [42]. Histological cholestasis is a bad prognostic indicator in alcohol related hepatitis. A mixed pattern of steatosis, giant mitochondria, and continued hazardous drinking predicted these serious developments [43]. While giant mitochondria appear to confer increased risk in the long term with regard to fibrosis development, they also associate with a better shortterm prognosis in the acute alcoholic hepatitis setting (see Table 25. Clinical and laboratory features with an independently poor prognostic significance are encephalopathy, low serum albumin, increased prothrombin time, low haemoglobin level, and large oesophageal varices [44]. Patients with encephalopathy, persistent jaundice, and azotaemia are very liable to develop the hepatorenal syndrome. Those with a markedly prolonged prothrombin time unresponsive to vitamin K and with a high serum bilirubin have a particularly bad outlook [45]. This score can then be used to inform treatment decisions and has been used to identify patients for clinical trials [46,47]. In recent years, however, the general management of patients with alcoholic hepatitis has improved, with an associated improved survival. The outlook in alcoholrelated cirrhosis is much better than that due to other causes. It depends on the ability of the patient to abstain, which in turn is related to family support, financial resources, and socioeconomic state. Some patients may benefit from pharmacological therapy to help achieve abstinence and prevent relapse. Disulfiram, acamprosate, and naltrexone are effective but either contraindicated or uninvestigated in severe liver disease [54]. Conflicting results came from initial studies that included patients with disease of all severities. A failure of the bilirubin level to drop after 7 days of corticosteroid treatment identifies steroid nonresponders. Management of alcohol withdrawal can be challenging in patients with advanced alcoholrelated liver disease. Symptomtriggered treatment with shorteracting benzodiazepines such as lorazepam are recommended in this setting. Patients with severe physical problems are more likely to abstain than those who present with psychological issues. In a longterm followup of men attending a liver clinic, severe medical illness was strongly associated with the decision to stop drinking [52]. Some psychological and pharmacological treatments are available to help abstinence and prevent relapse Alcohol and the Liver 507 Infection developing after corticosteroid treatment is more frequently seen in patients who are nonresponders to corticosteroid therapy than in responders [59]. Active sepsis and bleeding are contraindications, but steroids may be considered after these complications have been controlled if the clinical picture that remains is consistent with alcoholic hepatitis. At present, the evidence suggests that corticosteroids reduce shortterm mortality, with those showing evidence of improvement in serum bilirubin after 1 week (as quantified by the Lille score) being likely to have a longerterm benefit from continued treatment. Pentoxifylline was shown to improve survival in severe disease by 40% in one study [60]. This is in keeping with other recent studies, which showed no effect of pentoxifylline either alone, or in combination with prednisolone, in comparison with prednisolone alone [61,62], or as salvage treatment for patients not showing improvement with corticosteroids [63]. Hence there is little evidence for the continued use of pentoxifylline in the management of alcoholic hepatitis even in situations where corticosteroids are thought to be contraindicated. One study found a reduction in infections and a reduction in onemonth mortality in comparison with corticosteroids alone. Trials of combination antioxidants (including Nacetylcysteine) have been disappointing, with no evidence of survival benefit either combined with, or compared with, corticosteroids [65,66]. Nutritional supplementation may have a role in improving medium to longterm survival in patients with severe alcoholrelated hepatitis. However, implementation of an intensive programme of enteral nutritional support is difficult because of poor tolerance of nasogastric feeding. It may be that the ability to take an adequate nutritional intake is a marker of better outcome relative to those who are severely anorexic and/ or intolerant of nasogastric feeding, rather than being due to the therapeutic nature of the nutrition itself [67]. Cirrhosis While there may be some collagen remodelling with time when liver injury has ceased, cirrhosis is essentially irreversible and therapy is then directed at the complications. Drug metabolism is impaired and particular care must be taken, especially with sedatives. In spite of initial concerns about comorbidities, graft and patient survival is similar to that for other transplant indications. The 5year survival is improved with transplantation and the greatest benefit is seen in those with the most severe disease [69]. Patients should be monitored closely to detect relapse early and to treat those who return to hazardous drinking. In some cases, the period of abstinence required may be reduced to 3 months if survival is unlikely beyond this. One of the main reasons for the period of abstinence is that many patients will recover during this time and then not need transplantation. Liver transplantation for corticosteroidunresponsive alcoholic hepatitis has been advocated.
Cheapest generic clopidogrel uk
Intranuclear viral inclusions are seen in biliary epithe lium and rarely in hepatocytes symptoms 7 days before period 75mg clopidogrel with amex. Herpes simplex Liver involvement may occur with fulminating viraemia, contracted at birth from maternal genital herpes. Congenital rubella syndrome Neonatal hepatitis this may be due to: (1) intrauterine infections, (2) endo crine causes such as hypothyroidism, or (3) inherited diseases including chromosomal abnormalities. Intrauterine infection Immunity is reduced in the neonate, and virus infections are frequent and very liable to persist. Similarly, older children with immunodeficiency such as agammaglobulinemia or who are receiving immunosuppressive therapy are at risk. Jaundice develops within the first 2 days with hepatos plenomegaly, cholestasis, and slightly elevated serum transaminase levels. Hepatic histology shows giant cell hepatitis, bile in swollen Kupffer cells and ductules, focal hepatocellular necrosis, and portal fibrosis. Intrauterine parvovirus B19 can cause severe neonatal giant cell hepatitis, fulminant liver failure, or aplastic anaemia [19]. Cytomegalovirus Congenital toxoplasmosis is rare and results from mater nal infection in the third trimester. Neonatal hepatitis is associated with neurological involvement with chorioret initis, cerebral calcifications, hydrocephaly, or micro cephaly. The liver shows periportal mononuclear cell infiltration, extramedullary haemopoiesis with increased stainable iron, and histiocytes containing Toxoplasma. It is diagnosed by finding Toxoplasma IgM antibodies and treated with pyrimethamine and sulfadiazine. It is usually acquired via the placenta or breast milk from an asymptomatic mother, or from blood products. The disease may be fulminant with intense jaundice, purpura, hepatosplenomegaly, chorioretinitis, cataracts, and pulmonary defects. Survivors may run a long course Congenital syphilis is increasing again in frequency [20]. Varicella Varicella may occur in newborn infants if maternal infec tion occurs within 14 days of delivery. It is characterized by jaundice, extensive skin and multisystem involvement, especially pneumonia. In severe or fatal cases hepatic parenchymal involvement can be demonstrated [21]. There may also be midline facial abnormalities, nystagmus and microgenitalia in boys. The diagnosis is made by identifying a low thyroid stimulating hormone and free thyroxine level, with low earlymorning cortisol. Older children have a similar picture to adults with the same spectrum of infections, primary lymphoma, and Kaposi sarcoma. Hepatic histology shows more giant cell transformation and fewer granulo mas [23]. Diffuse, lymphoplasmocytic infiltration is associated with lymphoid interstitial pneumonia. Hepatitis A, B, and C Trisomy 18 is associated with growth retardation, skele tal abnormalities, and complex congenital heart disease. Trisomy 21 the association between trisomy 21 and neonatal chol estasis or extrahepatic biliary atresia is reported. The number of cases have diminished with developments in molecular and genetic technology. Neonatal hepatitis in preterm infants Neonatal hepatitis is an increasingly common referral due to improved survival of premature infants. Most are associated with risk factors for cholestasis including parenteral nutrition and sepsis. It is important to differ entiate this from other causes of cholestasis including biliary atresia, which may have an atypical presentation in this age group. Examination of stool colour and fasting ultrasound examination for gallbladder size are useful investigations to exclude biliary atresia. Liver biopsy is only indicated if there is persistent conjugated hyperbili rubinemia and/or abnormal liver biochemistry. Prolonged parenteral nutrition the aetiology of parenteral nutritionrelated liver disease is complex and is associated with prematurity, low birth weight, and recurrent sepsis [27]. It is related to difficulties in enteral feeding, impaired enterohepatic circulation of bile acids and consequently reduced bile formation, bil iary stasis, and sludging. Liver biopsy shows nonspecific changes with features of extrahepatic biliary Infections with these viruses in the neonate do not cause jaundice or neonatal hepatitis unless there is acute liver failure or severe hepatitis (see later). Bacterial infection outside the liver In the neonate, an immature reticuloendothelial system with decreased complement and opsonins impair the ability of leucocytes to phagocytose bacteria. Conjugated hyperbilirubinaemia may occur with sepsis or localized extrahepatic infection, such as urinary infection [24]. Serum aminotransferases may be slightly elevated, but hepatosplenomegaly is uncommon. Jaundice may also occur with streptococcal, staphylococcal, and Gram negative bacterial septicaemia. Endocrine disorders Hypothyroidism Hypothyroidism is usually associated with an unconju gated hyperbilirubinaemia or the neonatal hepatitis syn drome and should be excluded in every patient. The diagnosis is con firmed by finding low serum thyroxine and triiodothyronine levels with high thyroidstimulating hormone, and by observing the effects of therapy. However, infants with intestinal failure may require combined liver and bowel transplantation [27]. Insertion of reactive loop into parent A-sheet Interaction with reactive enzymes Reactive loop Normal Inherited disease in the neonate 1Antitrypsin deficiency 1Antitrypsin is synthesized in the rough endoplasmic reticulum of the liver. Deficiency results in the unopposed action of these enzymes, particularly neutrophil elastase, which leads to pulmonary alveolar damage and emphysema [28]. Z and S are the most frequent abnormal alleles, which put an individual at risk of disease. The combination results in normal, intermediate, low, or zero serum 1antitrypsin levels. Liver disease, however, only occurs with mutations where 1anti trypsin accumulates in hepatocytes. Normally, the reactive loop swings in between the helices of the socalled Asheet of the protein, where it interacts with elastase and other enzymes. This is not due to deficient circulating 1antitrypsin levels, since other phenotypes with low circulating levels do not develop hepatic damage. However, mutation of the 1antitrypsin pro tein is not the only reason for its retention. Cells from individuals with 1antitrypsin liver disease also have a reduction in the autophagy and endoplasmic reticulum associated degradatory pathways [30]. These modifiers may pro vide targets for therapeutic intervention, for example autophagy enhancers demonstrated efficacy against liver disease in animal models and are currently undergoing clinical trial [28]. Clinical picture 1Antitrypsin deficiency is the commonest inborn error of metabolism to present with persistent neonatal jaundice. Infants may present with intrauterine growth retarda tion, cholestasis, failure to thrive, hepatomegaly, or the Liver in the Neonate, in Infancy, and Childhood 597 vitamin Kresponsive coagulopathy. The latter is more likely in breastfed infants or those not given prophylac tic vitamin K at birth. A contracted gallbladder on a fasting ultrasound and delayed or absent radioisotope excretion on hepatobil iary scanning may indicate severe intrahepatic cholestasis. Management the clinical presentation is with jaundice, hepatomegaly, failure to thrive, and meconium ileus. Extrahepatic biliary obstruction may be due to inspissated bile plugging the common bile duct [35], which can be removed by choledochotomy. Occurrence of neonatal hepatitis in cystic fibrosis does not predict early development of cirrhosis. Alagille syndrome (arteriohepatic dysplasia) [36] this is an autosomal dominant condition with an inci dence of 1: 100 000 live births worldwide. This multisys tem disorder is associated with cardiac, facial, renal, ocular, and skeletal abnormalities.
Purchase cheap clopidogrel line
These abnormalities do not necessarily correlate with one another or with the degree of impairment observed clinically medications to treat bipolar order 75 mg clopidogrel free shipping, although, in general, their severity increases as the clinical condition worsens. It is also apparent that many patients with cirrhosis who appear neuropsychiatrically unimpaired may exhibit disturbances of neurophysiological function and impairment of psychometric performance. These individuals may subsequently develop clinical features of hepatic encephalopathy attesting to the spectral nature of the syndrome. Hepatic Encephalopathy in Patients with Cirrhosis 153 Classification [2,4] the classification of hepatic encephalopathy, in patients with cirrhosis, has been the subject of considerable and ongoing debate. There is general agreement that patients with overt hepatic encephalopathy should be classified in relation to the severity of their clinical symptoms; the West Haven criteria, first formulated in 1977, are still considered adequate for this purpose [5] (Table 10. There is also agreement that overt hepatic encephalopathy should be classified in relation to the time course of the clinical syndrome; the terms employed are episodic, recurrent, and persistent. Episodic/recurrent hepatic encephalopathy Episodic hepatic encephalopathy develops over a period of hours or days in patients who have previously been clinically stable. In a high proportion of these individuals an obvious precipitating factor(s) can be identified [7] (Table 10. These produce their effect by: (1) further depressing hepatic or cerebral function; (2) increasing the nitrogenous load; or (3) stimulating an inflammatory response. Patients may return to normal following an episode of overt hepatic encephalopathy; the improvement in their clinical status is usually apparent before improvements Table 10. Patients are classified as having recurrent hepatic encephalopathy if they experience two or more episodes of overt hepatic encephalopathy within a time frame of 6 months or less [4]. Persistent hepatic encephalopathy A small number of patients show persistent but stable evidence of hepatic encephalopathy. Parkinsonian features may be prominent with a fine tremor unaffected by intention, pronounced rigidity, staccato speech, and a shuffling gait. Cerebellar features are often encountered manifesting as gait disturbance, truncal ataxia, an intention tremor, and dysarthria. Some fluctuation in the clinical picture may be observed in relation to various precipitants and usually manifests as a worsening of the predominant clinical features rather than by a change in conscious level. It presents as a progressive spastic paraparesis without sensory impairment or sphincter dysfunction [9,10]; the clinical syndrome is accompanied by degenerative change in the spinal cord. Clinical and biochemical evidence of liver disease may be equivocal or absent, and the neuropsychiatric disorder may dominate the picture. Minimal hepatic encephalopathy Patients with cirrhosis who have no clinical features of hepatic encephalopathy but evident impairment of cerebral functioning on testing are classified as having minimal hepatic encephalopathy. Use of the term minimal emphasizes the fact that hepatic encephalopathy exists as a spectrum of change with quantitatively distinct features relating to severity but it does not adequately convey the fact that this condition can have a detrimental effect on outcome. Dissatisfaction with the term minimal has resulted in the introduction of the term covert hepatic encephalopathy. While this approach may be pragmatic it is not clear how informative or valuable it is in clinical and particularly research settings. Indeed it has already been shown that patients classified as having covert hepatic encephalopathy behave, when tested, as two relatively independent groups [11,12]. Thus, the term minimal hepatic encephalopathy, as currently defined, will be retained in the remaining text. In people with cirrhosis who have no evidence of neuropsychiatric impairment the risk of developing an episode of overt hepatic encephalopathy, within 5 years of presentation, varies from 5% to 25% depending on the presence or absence of other risk factors [4]. In people with cirrhosis who have had an episode of overt hepatic encephalopathy the cumulative risk of developing a further episode is 40% at 1 year [15]. The presence of minimal hepatic encephalopathy significantly increases the risk of developing overt hepatic encephalopathy [23]. Diagnosis [30] the first step in the diagnosis of hepatic encephalopathy is to determine whether or not the patient has evidence of neuropsychiatric dysfunction. This should then be followed by confirmation that the features displayed are characteristic of hepatic encephalopathy and careful exclusion of a range of other conditions which may present with similar features. In the absence of clinical features a similar approach to the identification of relevant abnormalities will be required to establish the diagnosis of minimal hepatic encephalopathy. Rather, there are a number of individual Prevalence and consequences Overt hepatic encephalopathy is one of the complications of cirrhosis which, together with ascites and variceal haemorrhage, defines hepatic decompensation. The prevalence of minimal hepatic encephalopathy varies from 20% to 80% depending Hepatic Encephalopathy in Patients with Cirrhosis 155 techniques accessing different aspects of cerebral function that can be used singly, or in combination, to provide diagnostic information. In practice, any measure with a proven relationship with the behavioural, prognostic and, possibly, pathophysiological features of this syndrome can be used as a surrogate marker. Neurological examination including mental state assessment [31] this should include: 1) A careful and detailed neuropsychiatric history and examination, paying particular attention to changes in memory, concentration, cognition, and consciousness; to changes in energy and activity levels; and to overall healthrelated quality of life; 2) Use of twograding systems to assess mental status: the West Haven criteria [5] (Table 10. Additional instruments such as the Mini Mental Score Test [33], which have been widely applied in this patient population, can also be used; 3) A comprehensive neurological examination looking particularly for evidence of subtle motor abnormalities, including: hypomimia, dysarthria, increased tone, reduced speed or difficulty executing rapid, alternating movements, ataxia, increased deep tendon reflexes, impaired postural reflexes, and abnormal movements such as tremors, particularly asterixis. The presence of sensory change and/or focal features would suggest an alternative or additional diagnosis; 4) the exclusion of other potential causes of neuropsychiatric abnormalities, including: concomitant neurological disorders such as subdural haematoma and Wernicke encephalopathy; other metabolic abnormalities, such as those associated with diabetes and renal failure; and, intoxication with alcohol or drugs. Corroborative reports from relatives or friends, particularly in relation to observed rather than subjective changes in behaviour and mental state, should be obtained. Psychometric performance [30,34] Patients with minimal hepatic encephalopathy generally show deficits in attention, visuospatial abilities, fine motor skills, and working memory while other cognitive abilities are relatively preserved. Patients with overt hepatic encephalopathy show additional disturbances in psychomotor speed, executive function, and concentration. A large number of psychometric tests have been evaluated in this patient population but none is specific for the diagnosis of this condition. For this reason test batteries are generally more reliable than single tests, and tend to be more strongly correlated with functional status. It has a reported sensitivity of 96% and specificity of 100% for the diagnosis of Grade I hepatic encephalopathy [36]. Test scores have to be normalized for a number of confounding variables; normative data are now available in several countries. Computerbased psychometric tests may allow a more precise quantification of reaction times and more refined testing [30]. Number connection tests A and B: the time taken to join the numbers, or numbers and letters, in sequence, is recorded. Digit symbol test: the number of correct symbols inserted into the blank squares below the numbers in 90 seconds is recorded. Serial dotting: the time taken to place a dot in the centre of each circle on the page is recorded. Line tracing: the time taken to trace a line between the two guidelines, without moving the paper, and the number of errors made are recorded. Triphasic waves or arrhythmic delta activity occur with more severe grades of encephalopathy; coma is characterized by slow, lowvoltage delta activity with sequences of electric silence. These features are not specific as they can also be observed in other metabolic and druginduced encephalopathies [38]; however, these conditions are usually easily distinguished on clinical grounds. The advent of lowcost, wireless headsets might encourage more widespread use of this technique [41]. It discriminates patients with minimal hepatic encephalopathy with a sensitivity of 61% and a specificity of 79% [42]. There are some differential effects in relation to age and the aetiology of the underlying liver disease [45]. Testing requires intact binocular vision and, for some commercial equipment, normal colour vision. Patients are shown a series of random letters and are asked to respond to predefined sequences designated as targets or lures.
Diseases
- Chromosome 10 Chromosome 12
- Neonatal ovarian cyst
- Howard Young syndrome
- MPO deficiency
- Tick paralysis
- Caroli disease
- Cone-rod dystrophy
- Twin-to-twin transfusion syndrome
Purchase 75 mg clopidogrel amex
This is a horizontal fibrotic furrow or pedicle on the anterior surface of one or both lobes of the liver just below the costal margin [13] symptoms 0f brain tumor buy clopidogrel once a day. The mechanism is unknown, but it affects elderly women who have worn corsets for many years. It presents as an abdominal mass in front of and below the liver and is isodense with the liver. Interference with the portal supply or biliary drainage of a lobe may cause atrophy. Left lobe atrophy found at postmortem or during scanning is not uncommon and is probably related to reduced blood supply via the left branch of the portal vein. The lobe is decreased in size with thickening of the capsule, fibrosis, and prominent biliary and vascular markings. Loss of left lobe parenchyma in this instance develops by the process of ischaemic extinction due to impaired flow from the affected large portal vein branch. This large vessel extinction process should be distinguished from cirrhosis in which the entire liver is affected by numerous intrahepatic and discrete extinction lesions, which affect small hepatic veins and portal vein branches during the course of inflammation and fibrosis. Hence, in cirrhosis the entire liver surface is diffusely converted to regenerative parenchymal nodules surrounded by fibrosis. Obstruction to the right or left hepatic bile duct by benign stricture or cholangiocarcinoma is now the most common cause of lobar atrophy [14]. This rare lesion may be an incidental finding associated, probably coincidentally, with biliary tract disease and also with other congenital abnormalities. It must be distinguished from lobar atrophy due to cirrhosis or hilar cholangiocarcinoma. Hepatic surgery (partial hepatectomy, liver transplantation) is feasible, but complex. Other conditions associated with displacement of the liver from its location in the right upper quadrant include congenital diaphragmatic hernias, diaphragmatic eventration, and omphalocoele. Anatomical abnormalities of the gallbladder and biliary tract are discussed in Chapter 14. This is soon joined by the cystic duct from the gallbladder to form the common bile duct. The common bile duct runs between the layers of the lesser omentum, lying anterior to the portal vein and to the right of the hepatic artery. Passing behind the first part of the duodenum in a groove on the back of the head of the pancreas, it enters the second part of the duodenum. The duct runs obliquely through the posteromedial wall, usually joining the main pancreatic duct to form the ampulla of Vater (c. Using endoscopic cholangiography, the duct diameter is usually less than 11 mm, although after cholecystectomy it may be more in the absence of obstruction. The duodenal portion of the common bile duct is surrounded by a thickening of both longitudinal and circular muscle fibres derived from the intestine. It always lies above the transverse colon, and is usually next to the duodenal cap overlying, but well anterior to , the right renal shadow. The fundus is the wider end and is directed anteriorly; this is the part palpated when the abdomen is examined. The valves of Heister are spiral folds of mucous membrane in the wall of the cystic duct and neck of the gallbladder. The mucosa is in delicate, closely woven folds; instead of glands there are indentations of mucosa which usually lie superficial to the muscle layer. The gallbladder wall consists of a loose connective tissue lamina propria and muscular layer containing circular, longitudinal, and oblique muscle bundles without definite layers, the muscle being particularly well developed in the neck and fundus. The distensible normal gallbladder fills with bile and bile acids secreted by the liver, concentrates the bile through absorption of water and electrolytes and with meals contracts under the influence of cholecystokinin (acting through preganglionic cholinergic nerves) to empty bile into the duodenum. This branch of the hepatic artery is large, tortuous, and variable in its anatomical relationships. The venous drainage is into the cystic vein and thence into the portal venous system. The arterial blood supply to the supraduodenal bile duct is generally by two main (axial) vessels which run beside the bile duct. These are supplied predominantly by the retroduodenal artery from below, and the right hepatic artery from above, although many other vessels contribute. This pattern of arterial supply would explain why vascular damage results in bile duct stricturing [16]. These drain through the cystic gland at the neck of the gallbladder to glands along the common bile duct, where they anastomose with lymphatics from the head of the pancreas. The gallbladder and bile ducts are liberally supplied with nerves, from both the parasympathetic and the sympathetic system. The upper border of the right lobe is on a level with the 5th rib at a point 2 cm medial to the right midclavicular line (1 cm below the right nipple). The upper border 6 Chapter 1 of the left lobe corresponds to the upper border of the 6th rib at a point in the left midclavicular line (2 cm below the left nipple). The lower border passes obliquely upwards from the 9th right to the 8th left costal cartilage. In the right nipple line it lies between a point just under to 2 cm below the costal margin. It crosses the midline about midway between the base of the xiphoid and the umbilicus and the left lobe extends only 5 cm to the left of the sternum. A line is drawn from the left anterior superior iliac spine through the umbilicus; its intersection with the right costal margin indicates the position of the gallbladder. The lower edge should be determined by palpation just lateral to the right rectus muscle. This avoids mistaking the upper intersection of the rectus sheath for the liver edge. The lower edge may be displaced downwards by a low diaphragm, for instance in emphysema. Common causes of a liver palpable below the umbilicus are malignant deposits, polycystic or Hodgkin disease, amyloidosis, congestive cardiac failure, and gross fatty change. Rapid change in liver size may occur when congestive cardiac failure is corrected, cholestatic jaundice relieved, or when severe diabetes is controlled. The surface can be palpated in the epigastrium and any irregularity or tenderness noted. Pulsation of the liver, usually associated with tricuspid valvular incompetence, is felt by manual palpation with one hand behind the right lower ribs posteriorly and the other anteriorly on the abdominal wall. The upper edge is determined by fairly heavy percussion passing downwards from the nipple line. The lower edge is recognized by very light percussion passing upwards from the umbilicus towards the costal margin. Method I: the gallbladder is found where the outer border of the right rectus abdominis muscle intersects the 9th costal cartilage. The anterior liver span is obtained by measuring the vertical distance between the uppermost and lowermost points of hepatic dullness by percussion in the right midclavicular line. Friction may be palpable and audible, usually due to recent biopsy, tumour, or perihepatitis. The venous hum of portal hypertension is audible between the umbilicus and the xiphisternum.
75 mg clopidogrel with mastercard
Viral serologies may identify potential aetiologies; the appropriate IgM antibodies are useful in identifying hep atitis A and B treatment knee pain buy 75 mg clopidogrel with mastercard. Liver biopsy, if performed, will show specific viral inclusions, but the presence of skin lesions merit initiation of acyclovir therapy. However, paracetamol levels are often unde tectable in the setting of unintentional cases if symptoms have already developed. Paracetamol protein adducts correlate with hepatotoxicity and remain detect able for up to 12 days after ingestion. The detection of adducts, currently a researchonly assay, may provide an important clinical tool when it becomes more widely available [32]. Antinuclear antibodies, smooth muscle antibodies, antibodies to liver/kidney microsomes type 1, and immunoglobulin levels should be checked for possible autoimmune hepatitis; liver biopsy may help to establish the diagnosis and is encouraged in indeterminate case settings [26]. Serum ceruloplasmin is unhelpful in fulminant Wilson disease since levels are low in nearly 50% of all forms of acute liver failure [25]. Determination that the ratio of alkaline phosphatase to bilirubin of less than 4 and aspar tate aminotransferase to alanine aminotransferase is greater than 2. Use of a checklist may be helpful to be certain that all diagnostic possibilities are entertained and treatment options considered [33]. Abdominal imaging and liver biopsy Abdominal ultrasound is used to assess for vasculature patency and mass lesions. Hepatic nodularity may be observed on imaging, reflecting regenerative nodules and confluent necrosis rather than cirrhosis [34]. Liver histology can show considerable variability of necrosis that may be prognostically misleading though necrosis >75% of hepatocytes has been shown to have worse outcomes without liver transplant [36]. Transjugular liver biopsy should be performed if there is any suspicion of malignancy or autoimmune hepatitis, since each of these diagnoses would suggest a different therapeutic approach. Complications and management of acute liver failure Acute liver failure represents a syndrome precipitated by various causes rather than a single disease. Treatment has focused on the management of complications except for a few aetiologyspecific thera pies (Table 5. The pathogenesis of hepatic encephalopathy is multi factorial (Chapter 8) and centres on failure of the liver to remove toxic, mainly gutderived, substances including ammonia from the circulation. The onset of encephalopathy is often sudden, may pre cede jaundice, and, unlike chronic liver disease, may be associated with agitation, changes in personality, delu sions, and restlessness. Management of the portosystemic encephalopathy of cirrhosis has centred on lactulose and nonabsorbable antibiotics. However, lactulose has shown no benefit in acute liver failure and may increase aspiration risk and bowel distension, which complicates transplantation. There is not enough evidence to recommend non absorbable antibiotics in acute liver failure. The prognosis for patients with stage 1 or 2 encepha lopathy (confused or drowsy) is relatively good. Progression of encephalopathy may be trig gered by infection; however, the use of prophylactic antibiotics remains controversial, with no firm evidence of benefit [44]. The cause is not fully understood and is probably multi factorial, influenced by altered brain osmolality, cellular metabolism, and cerebral blood flow. The net blood sup ply to the brain depends on the balance between carotid arterial pressure and intracerebral pressure (cerebral perfusion pressure = mean arterial pressure - intracra nial pressure). Cerebral blood flow autoregulation (main tained blood flow despite falling or rising blood pressure) is lost in patients with fulminant hepatic failure [46]. This can lead to relative intracranial hypertension due to increasing cerebral blood flow and interstitial water, as well as cerebral hypoperfusion and hypoxia due to sys temic hypotension. Clinically, raised intracerebral pressure is suggested by systolic hypertension (sustained or intermittent), increased muscle tone and myoclonus, which progress to extension and hyperpronation of the arms and extension of the legs (decerebrate posturing). If not controlled by treatment, this clinical picture progresses to loss of pupillary reflexes and respiratory arrest from brainstem herniation. Haematoxylin and eosin slide demonstrates centrilobular necrosis with surviving periportal hepatocytes. Trichrome stain shows cirrhosis with bands of fibrosis surrounding regenerative nodules. Haematoxylin and eosin slide (right) shows severe hepatocyte injury with ballooning degeneration, microsteatosis, and cholestasis. Victoria blue stain highlights copper pigment within the hepatocytes (H) and Kupffer cells (K). Cerebral oedema may be decreasing in prevalence, per haps due to earlier referral to tertiary centres and emer gent transplantation [48]. General management of cerebral oedema includes limiting stimulation, elevating the head to at least 30 degrees, and correction of acidosis and electrolytes. Additional therapies focus on decreas ing cerebral oedema by increasing intravascular osmotic gradient (hypertonic saline, mannitol) [49]. Use of hyper ventilation, barbiturates, indomethacin have fallen out of favour and no survival benefit has been shown with hypo thermia [50,51]. Trials are needed to test further its efficacy in established intracranial hypertension. Volume overload can develop and ultra filtration may be necessary in the setting of renal impairment. Nearly 60% of intracranial hypertension cases respond and mannitol has been shown to improve survival [49]. Coagulopathy the liver synthesizes nearly all the coagulation factors, inhibitors of coagulation and proteins involved in the fibrinolytic system (Chapter 4). The coagulopathy of fulminant hepatic failure is thus complex and due not only to factor deficiency, but also to enhanced fibrinolytic activity and decreased platelet number and function. Overall, there appears to be less clinically significant bleeding in acute liver failure than might have been assumed from the obvious derangements in prothrombin time and platelet levels. Thromboelastography may be of value in determining need for specific therapy to improve coagula tion abnormalities. Despite prolonged prothrombin time, most patients with acute liver failure have been found to have normal haemostasis as measured by thromboelas tography [53]. Coagulopathy is managed by routine intra venous or subcutaneous vitamin K initially, and rarely requires additional measures. A recent analysis of changes over the past 16 years in management of acute liver failure, suggested that severity of illness had not changed but that outcomes had improved. Fewer transplants and more patients survived without transplant between 2007 and 2013 than in the previous 8 years, despite a diminished use of plasma and red blood cell replacement therapy. Indeed, less may be more, since there should be fewer instances of transfusionassociated lung injury if use of fresh frozen plasma is kept to a minimum [54]. Platelet transfusions have specifically been linked to acute lung injury and should also be minimized [55]. Metabolic derangements Hypoglycaemia is found in up to 40% of patients with acute liver failure. Plasma insulin levels are high due to reduced hepatic uptake; gluconeogenesis is reduced in the failing liver. Blood glucose levels less than 60 mg/dL should be treated with a continuous infusion of 10% dex trose. Hypokalaemia is common and due in part to urinary losses with inadequate replacement, and administration of glucose. Other electrolyte changes include hypophos phataemia, hypocalcaemia, and hypomagnesaemia. Respiratory alka losis results from central hyperventilation, due to direct stimulation of the respiratory centre by unknown toxic substances.
Discount clopidogrel 75mg
A minority present with symptoms and signs of cirrhosis and portal hypertension with ascites and variceal haemorrhage medicine x 2016 clopidogrel 75 mg sale. Chronic cholestasis leads to fat malabsorption and steatorrhoea, deficiency of fatsoluble vitamins, and osteopenic bone disease. The serum bilirubin concentration is normal at diagnosis in more than half of the patients; serum immunoglobulin G (IgG) and IgM levels may be raised in around 50%. Elevated serum IgG4 levels have been reported in approximately 10% of patients [28]. The most prominent features are seen in the portal tracts, with inflammation, periductal fibrosis, bile duct proliferation, and, in later stages, bile duct loss. Elevated IgG4 IgG4associated cholangitis is a secondary form of sclerosing cholangitis (see separate section later). Because it is corticosteroid responsive, this condition is an important diagnosis to make or exclude. These patients often have a more aggressive disease course [34], but as yet the most appropriate management has not been defined for this group. However, it is important that patients understand the wide variability in disease severity, and also that a certain proportion of patients (possibly up to 40%) may never need a liver transplant. A number of prognostic models have been proposed, typically using biochemical results. The revised natural history model published by the Mayo Clinic (including age, bilirubin, aspartate aminotransferase, albumin, and variceal bleeding) is commonly used [36]. The degree of cholangiographic abnormality has been reported to correlate with outcome [38,39]. Elastography by ultrasound or magnetic resonance techniques may also provide prognostic information [40,41], but the result may be less accurate because of the presence of cholestasis [42]. However, a number of treatment options should still be considered, including those for symptoms and complications. It is important to be aware of the risk of sideeffects (osteopenia in particular) and to monitor the treatment response closely. Patients with cholestatic liver disease are particularly prone to deficiency of fatsoluble vitamins. Bone density should also be monitored and appropriate treatment for osteopenia instituted as early as possible. Medical treatment of cholestatic pruritus is difficult (see Chapter 13) and only sporadically very effective. Cholestyramine is the first choice, followed by rifampicin, naltrexone, and sertraline as secondline options [50]. All these options have issues related to tolerance of the medication and the sideeffects. Endoscopic therapy should be considered when there are clinically relevant or worsening symptoms. As discussed in the next section, endoscopy plays an important role in surveillance for, and diagnosis of, malignancy. Immunecentred trials mainly focus on the potential aberrant homing of lymphocytes from the gut to the liver. Finally, several approaches are being explored that are directed at altering the gut microbiota. There needs to be an increased awareness of the possibility of an associated biliary malignancy in this period, particularly in patients who present with progressive jaundice, abdominal pain, and weight loss [62]. The growth pattern is typically diffusely infiltrating; a definite tumour mass is often not found in early stage disease. In appropriately trained hands, when there is quiescent disease and adequate bowel preparation, nontargeted fourquadrant biopsies are therefore not needed, yet are still commonly used [71]. Impaired quality of life, mainly due to refractory pruritus or recurrent bacterial cholangitis, may be an indication for transplantation in selected patients [74]. Cholangiocarcinoma is generally considered a contraindication to liver transplantation. In a few centres, patients with early stage hilar cholangiocarcinoma are considered for liver transplantation, following an extensive preoperative protocol to reduce the tumour burden [68]. To remove as much of the involved extrahepatic bile duct as possible, a hepaticojejunostomy has previously been the preferred surgical procedure. The standard ducttoduct biliary anastomosis is also sometimes performed if feasible. Posttransplant causes of secondary sclerosing cholangitis need to have been excluded (Table 18. Surgical resection or liver transplantation is a treatment option but only in highly selected patients [68]. Palliative biliary stenting can relieve symptoms of cholestasis, and chemotherapy can be used following general guidelines for cholangiocarcinoma. Hepatocellular carcinoma surveillance should be performed according to standard guidelines as in patients with cirrhosis. As in all areas of medicine, there should be a high index of suspicion for unusual explanations for common clinical syndromes, such as cholestasis. Ischaemia and traumaassociated sclerosing cholangitis Unlike the hepatic parenchyma, which depends on dual blood flow from the portal vein and hepatic artery, the bile ducts rely on arterial blood flow to maintain their integrity. In many cases of traumaassociated sclerosing cholangitis (violent or iatrogenic), the mechanism is also likely ischaemia rather than direct duct injury. Ischaemic biliary lesions are a common complication (up to 10%) of liver transplantation. Infectious cholangitis Choledocholithiasis and associated severe cholangitis can lead to sclerosing cholangitislike changes in any individual. Cholangiocarcinoma development is also seen in chronic helminthic infections (Clonorchis sinensis and Opisthorchis viverrini in particular). Opportunistic infections Chronic opportunistic infections may occur in immunodeficiency syndromes. The clinical implications of the latter observations are not clear, and colectomy prior to liver transplantation should not be performed unless otherwise indicated. Sclerosing cholangitis has been reported to be the most common hepatobiliary disease in children with primary immunodeficiencies. Drugrelated sclerosing cholangitis Direct toxicity due to hepatic artery drug injections is a very rare cause of sclerosing cholangitis [83]. Chronicity and cholangiographic abnormalities have also been reported in patients with cholestatic druginduced liver injury [86]. IgG4associated cholangitis is considered in patients with two or more of the main manifestations. There is a risk of relapse after stopping treatment, and many patients require longterm immunosuppression [88]. Biopsies of the duodenal papilla are easily taken [89], yet have only moderate diagnostic sensitivity. Care must be taken to avoid injury to the papilla, which carries an increased risk of postprocedural pancreatitis. In the future, diagnosis of IgG4associated sclerosing cholangitis may become easier with the implementation of new diagnostic algorithms and techniques [90,91]. Sclerosing cholangitis in systemic inflammatory diseases Bile duct disease, which may mimic sclerosing cholangitis on cholangiography, occurs in the context of a variety of inflammatory and noninflammatory systemic conditions. The burden of large and small duct primary sclerosing cholangitis in adults and children: a populationbased analysis. Populationbased epidemiology, malignancy risk, and outcome of primary sclerosing cholangitis. Increased frequency of autoimmune diseases in patients with primary sclerosing cholangitis.
Buy line clopidogrel
Typically medicine xalatan discount 75mg clopidogrel with amex, leukocytosis, marked peripheral eosinophilia, and elevated levels of IgM, IgG, and IgE immunoglobulins are present. It is more common and severe in visitors to endemic areas, in whom it may persist for 3 months or more. Retained eggs induce inflammation and scarring, initiating the final and most morbid phase of schistosomiasis. Early in the infection, the inflammatory response is vigorous, producing lesions more than 100-fold larger than the inciting egg itself. Fibroblasts stimulated by factors released by both retained eggs and the granulomas lay down scar tissue, rendering the earlier, granulomainduced vascular obstruction permanent. As would be expected, the severity of tissue damage is directly related to the total number of eggs retained. In S haematobium infection, the bladder mucosa becomes thickened, papillated, and ulcerated. In severe infections, the muscular layers of the bladder are involved, with loss of bladder capacity and contractibility. Calcification of the bladder wall is occasionally seen, and approximately 10% of patients harbor urinary tract calculi. Chronic Salmonella bacteriuria with recurrent bouts of bacteremia has been reported in Egypt, where squamous cell bladder carcinoma is frequently seen as a late complication of disease. Other urogenital organs may also be involved, including the spermatic cord, testes, fallopian tubes, ovaries, and vagina. In S mansoni and S japonicum infections, the bowel mucosa is congested, thickened, and ulcerated. Eggs deposited in the larger intestinal veins may be carried by the portal blood flow back to the liver, where they lodge in the presinusoidal capillaries. The resulting inflammatory reaction leads to the development of periportal fibrosis and hepatic enlargement. In contrast to cirrhosis, in most cases of schistosomiasis liver function is well preserved. Infected persons who subsequently acquire hepatitis B or C viruses develop chronic active hepatitis more frequently than those without schistosomiasis. Presinusoidal obstruction of blood flow can result in portal hypertension and serious manifestations of portal obstruction. Eggs that are carried around the liver in the portosystemic collateral vessels may lodge in the small pulmonary arterioles, where they produce interstitial scarring, pulmonary hypertension, and right ventricular failure. Immune complexes shunted to the systemic circulation may induce glomerulonephritis. Occasionally, eggs may be deposited in the central nervous system, where they may cause epilepsy or paraplegia. Some differences between the clinical presentation of schistosomiasis mansoni and that of schistosomiasis japonicum have been noted. Manifestations of the latter disease typically occur earlier in the course of the infection and tend to be more severe. When involvement of the central nervous system develops, it is more likely to occur in the brain than in the spinal cord. On the other hand, immune complex nephropathy and recurrent Salmonella bacteremia are more commonly seen in hepatosplenic S mansoni infections. The latter phenomenon is apparently related to the ability of Salmonella to parasitize the gut and integument of the adult fluke, providing a persistent bacterial focus within the portal system of the infected patient. In S haematobium infections, eggs are most numerous in urine samples obtained at midday, especially the last drops voided. When examination of the sediment yields negative results, eggs may sometimes be recovered by filtering the urine through a fine membrane. Cystoscopy with biopsy of the bladder mucosa may be required for the diagnosis of mild infection. Results of rectal biopsy may be positive when those of repeated stool examinations are negative. Because dead eggs may persist in tissue for a long time after the death of the adult worms, active infection is confirmed only when the eggs are shown to be viable. This may be performed by observing the eggs microscopically for movement of flame cell cilia or by hatching them in water and watching for motile miracidia to emerge. Quantitation of egg output may be useful in estimating the severity of infection and in following response to treatment. Conventional serologic tests detect circulating antibodies with sensitivities exceeding 90%, but cannot distinguish active from prior infection. They are particularly helpful in the diagnosis of Katayama syndrome in those returning from endemic areas. Moreover, because antigen levels drop rapidly after successful therapy, these tests may prove helpful in distinguishing active from inactive disease. This cancer is caused by a prolonged cycle of injury, at locations where eggs lodge in the bladder wall, or where they exit into the urine, triggering inflammation, repair, and scar. Over time, the squamous cells involved may become dysplastic or malignant; in effect, this is a cancer triggered by inflammation. Antihistamines and corticosteroids may be helpful in ameliorating their more severe manifestations. The maturing organisms seem resistant to antiparasitic medications, thus no immediate postexposure prophylaxis after water exposure is possible. In the late stage of schistosomiasis, therapy is directed at interrupting egg deposition by killing or sterilizing the adult worms. Praziquantel, which is active against all three species of schistosomes, is the agent of choice. Unfortunately, reports suggest decreased efficacy of this single-dose oral agent in areas where it has been used in mass therapy programs; in this setting, repeat dosing is an option, although S mansoni infections acquired in such areas may be treated with oxamniquine (not available in the United States). Artemisinin derivatives have worked well in experimental settings, and may be useful in select cases; fostering Plasmodium resistance in patients coinfected with malaria is a real concern. Programs aimed at interrupting transmission by the provision of pure water supplies and the sanitary disposal of human feces are often beyond the economic reach of nations most seriously affected. Chemical molluscicides have been effective in limited trials, but less successful when used over large areas for prolonged periods. Mass therapy of the infected human population has until recently been severely limited by the toxicity of older agents, or by unanticipated consequences, such as the unsanitary injection of tartrate emetic in Egypt, an antiparasitic drug that provided little benefit in terms of schistosomiasis but perversely transmitted Hepatitis C to thousands of patients. Praziquantel has proved to be more suitable for this purpose, albeit at the risk of selecting drug resistance. Furthermore, without other control measures, discontinuation of mass therapy can result in a rapid rebound of active disease. In 2009, a report of an extensive controlled study in an area of Southeastern China that was hyperendemic for S japonicum yielded remarkable results that are most instructive. These included removal of cattle from snail-infested grasslands, providing mechanized equipment to farmers, improving sanitation of drinking water, building lavatories and latrines, providing boats with fecal matter containers, and implementing intensive health education programs. The infection rates fell dramatically in the intervention villages as compared to nonintervention areas. Thus, a multipronged approach such as this offers the best hope for lasting control. Currently, there is intense interest in developing a vaccine suitable for human use. A vaccine made from irradiated S bovis cercariae, which was developed for cattle, appears to confer a significant degree of protection against infection. Although a similar live vaccine would not be practical for human populations, the success of the animal vaccine has provided clues to potential immunoprotective mechanisms in human schistosomiasis. Monoclonal antibodies have been used to identify a number of schistosomula and adult antigens thought to be capable of inducing protective immunity; more than a dozen antigens are now in various stages of investigation as vaccine candidates. One month after his return to the United States, he developed fever and chills, accompanied by cough, urticaria, arthralgia, abdominal pain, and diarrhea. Laboratory studies demonstrated leukocytosis and marked eosinophilia, with elevated immunoglobulin levels.