Generic 100mg danazol amex
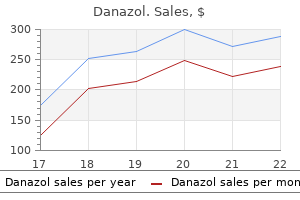
Patients undergoing radioactive treatment showed a significant longer progression-free survival pregnancy urinary tract infection cheap danazol 50mg with amex. Prognosis Clinically, the carcinoid syndrome is generally a manifestation of advanced disease. Carcinoids from various sites differ not only in the percentage developing the carcinoid syndrome but also in their aggressiveness. Survival rates for patients with various carcinoids depend on the site, the extent of the tumor, and tumor biology. In patients with only localized disease, the 5-year survival rate for midgut carcinoids is about 65%, not essentially higher than that for patients with regional metastases. Atypical lung carcinoids have significantly shorter survival, only 50% 5-year survival rate. Other factors that correlate with lower survival rates are high CgA level at diagnosis and high proliferation index (Ki67). In an earlier study performed by our group, 30% of the patients died of carcinoid heart complications. The mechanism behind the flushing and diarrhea is unknown, but it has been postulated to be mediated through prostaglandins stimulated by calcitonin. Therapy with tyrosine kinase inhibitor vandetanib can reduce these symptoms and present an antitumor effect. Most patients with mastocytosis have an indolent course, but some forms of mastocytosis are aggressive. Hepatomegaly and splenomegaly can be due to infiltration of mast cells, and hepatic fibrosis is also common. Other mediators of the syndrome are the release of prostaglandin D2, tryptase, and heparin. The diagnosis is made by measurement of histamine and histamine metabolites in the urine. As in the treatment of allergic anaphylaxis, epinephrine is effective in reversing the hypotension associated with mast cell mediator release275; thus these patients should have constant access to epinephrine in the form of subcutaneous injection or inhalation. Chronic therapy to prevent acute attacks includes antihistamine therapy combined with inhibition of prostaglandin biosynthesis. Blockade of both histamine H1 and H2 receptors is required to prevent the vasodilator effect of histamine. Aspirin has been used, but some patients cannot tolerate it because of side effects in the gut and allergic reactions. Malignant carcinoid of the small intestine with metastases to the liver, valvular disease of the right side of the heart (pulmonary stenosis and tricuspid regurgitation without septal defects), peripheral vasomotor symptoms, bronchoconstriction, and an unusual type of cyanosis; a clinical and pathologic syndrome. Carcinoids (argentaffin-cell tumors) and nerve hyperplasia of the appendicular mucosa. Histogenetic, histochemical, immunohistochemical, clinical and therapeutic aspects. Genomic alterations in well-differentiated gastrointestinal and bronchial neuroendocrine tumors (carcinoids): marked differences indicating diversity in molecular pathogenesis. Regulation of neuroendocrine differentiation in gastrointestinal carcinoid tumor cells by notch signaling. Prognostic impact of novel molecular subtypes of small intestinal neuroendocrine tumor. Survival analysis of 200 pulmonary neuroendocrine tumors with clarification of criteria for atypical carcinoid and its separation from typical carcinoid. One hundred years after "carcinoid"; epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. Carcinoid tumors: analysis of prognostic factors and survival in 301 patients from a referral center. A unique syndrome associated with secretion of 5-hydroxytryptophan by metastatic gastric carcinoids. Histamine release from a gastric carcinoid: provocation by pentagastrin and inhibition by somatostatin. Gastric carcinoid tumors: the biology and therapy of an enigmatic and controversial lesion. Serotonin, catecholamines, histamine, and their metabolites in urine, platelets, and tumor tissue of patients with carcinoid tumors. Tachykinins in carcinoid tumors: their use as a tumor marker and possible role in the carcinoid flush. Neuropeptide K: a major tachykinin in plasma and tumor tissues from carcinoid patients. Measurement and partial characterization of the multiple forms of neurokinin A-like immunoreactivity in carcinoid tumours. Chromogranin A: current status as a precursor for bioactive peptides and a granulogenic/sorting factor in the regulated secretory pathway. Determination of residues in chromogranin A-(16-40) required for inhibition of parathyroid hormone secretion. Vasostatins, comprising the N-terminal domain of chromogranin A, suppress tension in isolated human blood vessel segments. The syndrome of carcinoid and acquired valve lesions of the right side of the heart. Serotonin, catecholamines, and spontaneous midgut carcinoid flush: plasma studies from flushing and nonflushing sites. Increased intestinal non-substance P tachykinin concentrations in malignant midgut carcinoid disease. Flushing and plasma substance P concentration during infusion of synthetic substance P in normal man. Substance K: a novel mammalian tachykinin that differs from substance P in its pharmacological profile. A review of its pharmacology and preliminary clinical findings in novel applications. Telotristat ethyl, a tryptophan hydroxylase inhibitor for the treatment of carcinoid syndrome. Carcinoid heart disease: relationship of circulating vasoactive substances to ultrasounddetectable cardiac abnormalities. The cardiac disease associated with the carcinoid syndrome (carcinoid heart disease). Transoesophageal echocardiography improves the diagnostic value of cardiac ultrasound in patients with carcinoid heart disease. Involvement of transforming growth factor-beta in the formation of fibrotic lesions in carcinoid heart disease. Correlation of high serotonin levels with valvular abnormalities detected by cardiac catheterization and echocardiography. Serotonin mechanisms in heart valve disease I: serotonin-induced up-regulation of transforming growth factor-beta1 via G-protein signal transduction in aortic valve interstitial cells. Comparison of cardiovascular and bronchoconstrictor effects of substance P, substance K and other tachykinins. Studies of the carcinoid syndrome: its relationship to serotonin, bradykinin, and histamine. Clinical features, diagnosis, and localization of carcinoid tumors and their management. Review of the anaesthetic management of 21 patients undergoing laparotomy for carcinoid syndrome. Octreotide treatment of carcinoid syndrome: analysis of published dose-titration data. Resolution of acromegaly after removal of a bronchial carcinoid shown to secrete growth hormone releasing factor. Gastric carcinoids and neuroendocrine carcinomas: pathogenesis, pathology, and behavior. Mucosal argyrophil endocrine cells in pernicious anaemia and upper gastrointestinal carcinoid tumours.
Purchase line danazol
Menopausal hot flushes usually involve the whole body and are accompanied by intense sweating women's health center jackson ms 200 mg danazol. Postmenopausal women in whom a true carcinoid syndrome is developing can differentiate between the two types of flushes. The diarrhea is often accompanied by abdominal cramping, and endocrine, paracrine, and mechanical factors contribute to this condition. A variety of tumor products, including serotonin, tachykinins, histamines, kallikrein, and prostaglandins, can stimulate peristalsis, electromechanical activity, and tone in the intestine. Malabsorption can result from intestinal resections, from lymphangiectasia, secondary to mesenteric fibrosis, from bacterial overgrowth, and secondary to a tumor partially obstructing the small bowel or rapid intestinal transit. Increased secretion by the small bowel, malabsorption, or accelerated transit can overwhelm the normal storage and absorptive capacity of proximal colon and result in diarrhea, which may be aggravated if the reabsorptive function of the colon is impaired. In a study of patients with elevated serotonin levels and the carcinoid syndrome, transit time in the small bowel and colon was significantly decreased in comparison with that of normal subjects. This indicates that in patients in whom the carcinoid syndrome is associated with diarrhea, major alterations in gut motor function occur that affect both the small intestine and the colon. Many patients with carcinoid tumors have undergone wide resection of the small intestine, and they may be affected by the symptoms of short-bowel syndrome. Serotonin is believed to be responsible for the diarrhea in the carcinoid syndrome by its effects on gut motility and intestinal electrolyte and fluid secretion. Findings of new collagen beneath the endothelium of the endocardium is almost pathognomonic for carcinoid heart disease. Echocardiography can demonstrate early lesions in about 70% of patients with the carcinoid syndrome, whereas routine clinical examinations detect them in only 30% to 40%. Both of these agents control the hormonal release and excess that are thought to be involved in the fibrotic process. In a study performed in 1987,26 40% of patients with carcinoid tumors died of cardiac complications related to the carcinoid disease. Data from 2008 reveal that this complication is a rare event and that patients usually die of the effects of a progressive tumor. The facial flushing associated with carcinoid tumors should be distinguished from idiopathic flushing and menopausal hot flushes. Histologically, the plaque-like thickenings in the endocardium consist of myofibroblasts and fibroblasts embedded in a stroma that is rich in mucopolysaccharides and collagen. The weight-reducing drugs fenfluramine and dexfenfluramine appear to interfere with normal serotonin metabolism and have been associated with valvular lesions identical to those seen in carcinoid heart disease. Carcinoid crisis is a clinical condition characterized by severe flushing, diarrhea, hypotension, hyperthermia, and tachycardia. Type 3 represents sporadic gastric carcinoids occurring without hypergastrinemia and pursue a more malignant course, with 50% to 60% developing metastases. These tumors are more common in women than in men and are usually identified endoscopically during diagnostic evaluation for anemia or abdominal pain. Other Manifestations of the Carcinoid Syndrome Fibrotic complications other than heart lesions may be found in patients with carcinoid tumors. They include intra-abdominal and retroperitoneal fibroses, occlusion of the mesenteric arteries and veins, Peyronie disease, and carcinoid arthropathy. Narrowing and occlusion of arteries and veins by fibrosis are potentially life threatening. Ischemic loops of the bowel might have to be removed, and this procedure ultimately causes shortbowel syndrome. The diagnosis of a carcinoid tumor may be suspected from clinical symptoms suggesting the carcinoid syndrome or from the presence of other clinical symptoms, or it can be made in relatively asymptomatic patients from the histopathologic findings at surgery or after liver biopsy for unknown hepatic lesions. These immunohistochemical stains have replaced the old silver stains, the argyrophil stains by Grimelius and Sevier-Munger. The argentaffin stain by Masson to demonstrate content of serotonin has also been replaced by immunocytochemistry with serotonin antibodies. However, urinary and platelet measurements of serotonin itself can give additional information. For midgut carcinoids, the sensitivities were 100%, 92%, and 82%, respectively, and for hindgut carcinoids they were 20%, 0%, and 60%, respectively. Attempts have been made to identify more specific and sensitive serum markers for carcinoid tumors that might allow earlier diagnosis. It has been shown that CgA and CgB are more abundant than CgC in human neuroendocrine tissues. Furthermore, a correlation between levels of plasma chromogranin and extent of disease was found (p < 0. Importantly, plasma CgA might be elevated in other conditions such as chronic atrophic gastritis, treatment with proton-pump inhibitors, or impaired kidney function. Plasma neuropeptide K levels have been reported to be elevated in 46% of patients with midgut carcinoids, whereas only 9% of patients with foregut carcinoids displayed elevated levels. Telotristat ethyl, an inhibitor of the enzyme tryptophan hydroxylase, reduces the serotonin levels. Prednisolone in doses of 15 to 30 mg/day gives occasional relief in some cases with severe flushing and diarrhea. During the past 30 years, synthetic somatostatin analogues (octapeptides) have been developed for clinical use. Octreotide is the most commonly available drug; other analogues are lanreotide and vapreotide. This cross-talk modulates the intracellular signal and gives a fine tuning of the mediated effects. The therapeutic goals are to ameliorate and improve clinical symptoms, abrogate the tumor growth, improve quality of life, and (if possible) prolong overall survival. Symptomatic control of the carcinoid syndrome includes lifestyle changes, diet supplementation, and specific medical treatment that reduces the clinical symptoms related to the different components of the carcinoid syndrome. Avoiding stress, both psychologic and physical, as well as substances such as alcohol, spicy foods, and medications that precipitate a flushing reaction might be sufficient in early cases. Normally, about 1% of body tryptophan is used for production of serotonin; in carcinoid tumors, however, as much as 60% of the available tryptophan may be consumed for the synthesis of serotonin, and this can result in tryptophan and niacin deficiencies. Therefore supplemental niacin to prevent the development of pellagra has been recommended over the years. Many patients have undergone resection of the terminal ileum, which can result in vitamin B12 and folic acid deficiencies. A few patients need bronchodilators such as salbutamol, which interacts with -adrenergic receptors and does not induce flushing. The diarrhea seen in the carcinoid syndrome might be controlled by loperamide or diphenoxylate. The recommended dose for octreotide is 100 to 150 g two or three times a day, a standard treatment for controlling clinical symptoms. Ultrahigh-dose octreotide has generated significant antitumor responses in patients resistant to standard dose therapy. All types of carcinoid tumors, irrespective of functionality, can now be treated with octreotide. Carcinoid crisis is a life-threatening complication of the carcinoid syndrome and can occur spontaneously or may be associated with stress and anesthesia, chemotherapy, and infections (see earlier discussion). Patients usually experience severe flushing, diarrhea, abdominal pain, and hypotension. Continuous infusion with somatostatin analogues, 50 to 100 g/hour, is recommended and usually alters the lifethreatening condition. It is also recommended that patients be given subcutaneous somatostatin analogues before surgery or other stressful situations. Side effects of somatostatin analogue therapy have generally not been serious and occur in 20% to 40% of patients. They include pain at the injection site, gas formation, diarrhea, and abdominal cramping. Significant long-term side effects include gallstone formation, sludge in the gallbladder, steatorrhea, deterioration of glucose tolerance, and hypocalcemia. Symptomatic and biochemical control may be obtained in 40% to 50% of patients with the recommended doses of 3 to 5 million units of recombinant interferon alfa-2a or interferon alfa-2b three to five times per week subcutaneously.
Order 100mg danazol overnight delivery
However pregnancy kicks danazol 100 mg low cost, even when efficacious, for most subjects, the beneficial effect was not durable. Concerns related to the activation of Epstein-Barr virus infection, the duration of C-peptide preservation, and the protocol by which the drugs are administered have further limited their development. Indeed, although somewhat dated, a widely recognized effort notes more than 200 such means. Excitement is derived from the specificity and the relatively low risk of these therapies compared with immunosuppression. The basic concept behind immunologic vaccination is the induction of regulatory T lymphocytes that target a given beta-cell antigen and, on encountering the target antigen. Examples of combinations with respect to immune intervention would include an induction component using drugs targeting inflammation and T-/B-cell memory and a maintenance component that could involve antigens to induce tolerance to beta cells. Patients with a kidney transplant receive immunosuppressive drugs that, given the nature of clinical monitoring for renal transplant rejection. Several studies suggest that improved results for pancreatic transplantation occur in the setting of simultaneous pancreas and kidney transplantation versus transplantation of pancreas alone. With a successful pancreas transplant, hyperglycemia is immediately reversed for most, and there is growing evidence of improved long-term outcomes. Nevertheless, the surgery is extensive, and there are many potential complications associated with the transplant. Perhaps for these reasons, along with improvements in diabetes management (and thus reducing long-term complications, including kidney failure), it appears that the procedure peaked in the mid- to late 2000s, with declines in the number of procedures performed in the United States thereafter. Indeed, with islet autotransplantation in patients with pancreatitis, most patients become insulin independent and remain so. This so-called Edmonton protocol has subsequently been tested in a series of specialized centers throughout North America and Europe. It is clear that in many centers, albeit with varying degrees of success, islet cell transplant can prove effective. For most of the patients who achieve insulin independence, resumption of use of low doses of insulin is necessary within 2 years, and by 5 years the benefits of the form of therapy wane. Further research to achieve tolerance without long-term immunosuppression is essential, as is continued development of systems allowing for xenogeneic transplantation. Of immense promise for the future are therapies involving the use of surrogate beta-like cells. Disorders Associated With Immunity to Insulin/Insulin Receptor Insulin Autoimmune Syndrome the insulin autoimmune syndrome, also termed Hirata syndrome, is rare and is typically associated with hypoglycemia. Interestingly, and for reasons unknown, the disease occurs most commonly in persons of Asian descent. Therefore, although whole-pancreas and islet cell transplantation have both become highly operationalized and often effective procedures, the quantitative paucity of suitable organ donor tissues, taken together with complications associated with immune suppression, have severely limited their widespread therapeutic application. First, beta cells, the primary cell sought for stem cell development, in their natural setting do not exist in isolation. Hence, the notion of generating a cell therapy in the absence of a full complement of islet cells. In addition strong consideration must continue to be given toward averting what likely would be an assault on the target tissue-both autoimmune and alloimmune, depending on the setting. To this end, effort for any so-called protective devices should encompass a need to (1) provide biocompatibility; (2) see ample blood supply to sustain cellular survival and functional beta-cell mass capable of imparting normoglycemia; (3) prevent sensitization and be immune protective; (4) trap potentially oncogenic cells; and (5) allow for rapid response of insulin, in terms of both activating and suppressing insulin secretion, to changing glucose concentrations. Indeed, essentially all patients treated with recombinant human insulin produce anti-insulin antibodies. Allergic reactions can occur with insulin analogues, modifications of recombinant human insulin, although this is uncommon. More common features include allergies to affiliated lubricants; preservatives; and plastics in bottles, stoppers, syringes, and needles. It appears that antiinsulin receptor autoantibodies can act as either antagonists or agonists for this disease. The symptoms and signs are related to the presence of hyperglycemia and the resulting effects on fluid and electrolyte balance, which include polyuria, polydipsia, polyphagia, weight loss, and blurred vision. Particularly in children, the onset of symptoms can occur over a brief period, and families may be able to date the onset with considerable accuracy. Variable effects on mental status may be seen, ranging from slight drowsiness to profound lethargy and even coma if the condition has been untreated for a significant period. If the presentation is uncomplicated, the remainder of the fluid and electrolyte measurements may be completely normal. At presentation, the C-peptide level (a surrogate marker for insulin secretion) is generally in the low-normal range and declines over time. However, residual C-peptide may be detected throughout the natural history of diabetes. In reference laboratories, pancreatic autoantibodies are present in approximately 98% of individuals at diagnosis, but most commercial laboratories do not provide either the full spectrum of assays or equivalently sensitive or specific assays, resulting in both false-negative and -positive assays (discussed previously). Furthermore, antibody titers diminish over time and may be less prevalent in certain ethnicities. Management requires orchestrated efforts on the part of the person with diabetes, family members, and the multidisciplinary health care team. Important stakeholders may vary, depending on the age of onset of the disease, comorbid conditions, stages of transition throughout the life span, from early childhood through adolescence and young adulthood to adulthood and the middleage years, then finally culminating in the advancing years of the geriatric population. These management activities require constant vigilance, with attention to treatment needs 24 hours per day, 7 days a week, every year. Such a rigorous management program requires input of a multidisciplinary treatment team, composed of an endocrinologist or physician with specific training and interest in diabetes, a certified diabetes educator, a dietician, and a mental health professional (either a social worker or psychologist) with diabetes behavioral health expertise. Other team members can include an exercise physiologist, an ophthalmologist or optometrist with diabetes expertise, a podiatrist, a nephrologist, and other specialists as indicated. Visit frequency for diabetes care depends on the age at diagnosis, duration of disease, and presence of comorbidities. Initial visits usually entail 2 to 3 sequential days of multidisciplinary visits, followed by visits in 2 to 3 weeks, then 1 to 2 months later. Thereafter, diabetes follow-up care generally occurs quarterly, especially in childhood when there is need to monitor growth and development. Both weight and height, along with vital signs, should be obtained at every quarterly visit, and Tanner staging should be performed at least annually for pediatric patients. Similarly, weights and vital signs should be obtained at each visit along with timely screening for complications and cardiovascular risk factors. In childhood, initial management education is directed to the parents/guardians, whereas a family-based approach to care continues throughout adolescence. Diabetes management is also tailored to the needs and desires of the person with diabetes, creating an individualized care approach. It remains important to reassess management approaches during the various developmental stages, especially during puberty, when physiologic insulin resistance coupled with psychosocial turmoil can lead to increased insulin needs and deteriorating glycemic control. Chapter 36 Type 1 Diabetes Mellitus 1425 Glycemic Targets the fundamental approach of individualized care is based on the treatment goal of achieving glycemic targets. Notably, at the time of that clinical trial, there were no rapid-acting or long-acting insulin analogues; only short- and intermediate-acting insulin preparations were available (see insulin regimens in the following). Intensive insulin therapy yielded superior glycemic control to conventional insulin therapy, with HbA1c levels that were approximately 2% lower in the intensively treated group than in the conventionally treated group, medians of 7% and 9%, respectively. The target HbA1c goal for any single person with diabetes needs to reflect his or her risk of severe hypoglycemia, as well as hyperglycemia, considering the presence of comorbidities that may interfere with survival. Attention to both nutrition and exercise is fundamental in glycemic management, as well for overall health and cardiovascular disease prevention. There is need to provide education on these lifestyle issues to the persons with diabetes and to the family members of young children and adolescents with diabetes, especially given the global epidemic of childhood and adult overweight/obesity. These knowledge areas are addressed in diabetes self-management education and support and should begin at diagnosis and progress as disease duration increases and the needs of the person with diabetes change. Nutrition Therapy Medical nutrition therapy addresses diabetes-specific issues, such as those related to the carbohydrate content of foods, to limit postprandial glycemic excursions, as well as ways to maintain normal growth in the pediatric population and to avoid excessive weight gain across the life span.
Buy danazol 200 mg on-line
In diabetic macular disease menstruation yahoo danazol 200 mg low price, macular edema involving the fovea or nonperfusion of the capillaries in the central macula is responsible for the loss of vision. Abnormal thickening of the central retina (usually 1 mm in diameter central retinal subfield) due to increased vascular permeability. Because central involvement is more likely to cause visual impairment, it is commonly used as a threshold for treatment. Thickening of the retina in the macular region of sufficient extent and location to threaten central visual function. A gray or white area lesion in the nerve fiber layer of the retina resulting from stasis of axoplasmic flow caused by microinfarcts of the retinal nerve fiber layer. A multicenter, randomized clinical trial designed to address whether intensive insulin therapy could prevent or slow the progression of systemic complications of diabetes mellitus. The first multicenter, randomized clinical trial to demonstrate the value of scatter (panretinal) photocoagulation in reducing the risk of vision loss among patients with all levels of diabetic retinopathy. A multicenter clinical trial evaluating early vitrectomy for patients with very advanced diabetic retinopathy or nonresolving vitreous hemorrhage. A multicenter, randomized clinical trial that addressed at what stage of retinopathy scatter (panretinal) photocoagulation was indicated, whether focal photocoagulation was effective for preventing moderate vision loss due to clinically significant macular edema, and whether aspirin therapy altered the progression of diabetic retinopathy. A type of laser treatment whose main goal is to reduce vascular leakage, either by focal treatment of leaking retinal microaneurysms or by application of therapy in a gridlike pattern for patients with clinically significant macular edema. Proliferative diabetic retinopathy of defined extent, location, or clinical findings that is particularly associated with severe vision loss. An early vascular abnormality consisting of an outpouching of the retinal microvasculature. Elevation of intraocular pressure caused by the development of neovascularization in the anterior segment of the eye. Retinal neovascularization that is located more than 1500 m away from the optic disc. Neovascularization occurring on the iris (rubeosis iridis), usually as a result of extensive retinal ischemia. An advanced level of diabetic retinopathy in which proliferation of new vessels or fibrous tissue occurs on or within the retina. Larger areas of these complications as well as new vessels that are near the optic disc are associated with greater risks of vision loss. Thus if the center of the macula is not involved there is often not a compelling reason to treat. International Classification of Diabetic Retinopathy and Diabetic Macular Edema vitreous hemorrhage, or preretinal hemorrhage). Macular edema is subclassified as mild (some retinal thickening or hard exudates in the posterior pole but distant from the center of the macula), moderate (retinal thickening or hard exudates approaching the center of the macula but not involving the center), or severe (retinal thickening or hard exudates involving the center of the macula). From Grading diabetic retinopathy from stereoscopic color fundus photographs-an extension of the modified Airlie House classification. Chapter 37 Complications of Diabetes Mellitus 1469 without relying on reference to the standard photographs of the Airlie House Classification of diabetic retinopathy. Other Ocular Manifestations of Diabetes All structures of the eye are susceptible to complications of diabetes. The consequence of these changes can range from being unnoticed by both patient and physician, to symptomatic but not sight threatening, to requiring evaluation to rule out potentially life-threatening underlying causes other than diabetes. Mononeuropathies of the third, fourth, or sixth cranial nerves can arise in association with diabetes; mononeuropathy of the fourth cranial nerve is least likely associated with diabetes and warrants workup for other causes. In one review of cranial nerve palsies treated in a diabetic patient population in 1967, 42% of mononeuropathies were not diabetic in origin. The percentage of all extraocular muscle palsies attributable to diabetes mellitus is estimated at 4. Diabetes-induced third-nerve, fourth-nerve, and sixthnerve palsies are usually self-limited and should resolve spontaneously in 2 to 6 months. The optic disc can be affected by diabetes in a variety of ways other than vasoproliferation. Diabetic papillopathy is a diagnosis of exclusion and must be distinguished from other causes of disc swelling such as true papilledema from increased intracranial pressure, pseudopapilledema such as optic nerve head drusen, toxic optic neuropathies, neoplasms of the optic nerve, and hypertension. Because diabetes poses an increased risk for developing open-angle glaucoma, the disc pallor following remission of retinopathy or laser photocoagulation must be considered when evaluating the optic nerve head for glaucoma. A diabetic ocular complication with potentially serious consequences is neovascularization of the iris. Neovascularization of the iris occurs in 4% to 7% of diabetic eyes and may be present in 40% to 60% of eyes with proliferative retinopathy. Usually new iris vessels are first observed at the pupillary border, followed by a fine network of vessels over the iris tissue progressing into the filtration angle of the eye. Closure of the angle by the fibrovascular network results in neovascular glaucoma, which can lead to irreversible optic nerve damage and vision loss due to the rise in intraocular pressure. Diabetes is the second leading cause of neovascular glaucoma, accounting for 32% of cases. Other approaches such as goniophotocoagulation, topical or systemic antiglaucoma medications, and antiglaucomatous filtration surgery are available when needed. Thus a more durable therapy such as scatter laser photocoagulation is often performed. The cornea of the diabetic person is more susceptible to injury and slower to heal after injury than is the nondiabetic cornea. Consequently, diabetic patients using contact lenses should exercise caution to avoid contact lens overwear and to maintain careful monitoring. Refractive change can be significant and is related to fluctuation of blood glucose levels with osmotic lens swelling. Ocular symptoms, complaints, or other associated medical issues can necessitate earlier evaluation. They have also established recommendations for vitrectomy surgery for diabetic eye complications. Comprehensive Eye Examination An accurate ocular examination detailing the extent and location of retinopathy-associated findings is critical for determining monitoring and treatment decisions in patients with diabetic retinopathy. As detailed later, most of the blindness associated with advanced stages of retinopathy can be averted with appropriate and timely diagnosis and therapy. Unfortunately, many diabetic patients do not receive adequate eye care at an appropriate stage of their disease. The fundamentals of a comprehensive eye examination for the nondiabetic patient have been detailed by the American Academy of Ophthalmology382 and the American Optometric Association. The schematic flow chart presents major principles involved in determining routine ophthalmic follow-up and indications for treatment in nonpregnant patients with diabetes. The examination of the patient with diabetes should be similar, with additional emphasis on portions of the examination that relate to problems particularly relevant to diabetes. Dilated ophthalmic examination is superior to undilated evaluation because only 50% of eyes are correctly classified as to presence and severity of retinopathy through undilated pupils. The schematic flow chart shows major principles involved in determining routine ophthalmic follow-up and indications for treatment in pregnant patients with diabetes. Ocular symptoms, complaints, or other associated ophthalmic or medical issues can necessitate earlier evaluation or an altered approach. Because retinopathy can progress rapidly in pregnant patients with diabetes, careful and more frequent evaluation is often indicated. The onset of vision-threatening retinopathy is rare in children prior to puberty, regardless of the duration of diabetes391,392; however, significant retinopathy can arise within 6 years of disease if diabetes is diagnosed between the ages of 10 and 30 years. Treatment may be indicated prior to conception for patients who are at risk for vision loss if their diabetic retinopathy were to worsen during pregnancy. Patients who become pregnant should have a comprehensive eye examination in the first trimester of pregnancy. Close follow-up throughout pregnancy is indicated, with subsequent examinations determined by the findings present at the first-trimester examination. Because significant sight-threatening retinopathy can initially occur with no or minimal visual symptoms, patients with no clinically evident diabetic retinopathy and no known ocular problems still require annual comprehensive ophthalmic examinations even if they are totally asymptomatic. Fluorescein angiography and optical coherence tomography angiography can also Chapter 37 Complications of Diabetes Mellitus 1473 Follow-up dependent on ocular status Is treatment for diabetic retinopathy or macular edema indicated This schematic flow chart details general photocoagulation treatment approaches in patients with diabetic retinopathy or diabetic macular edema. These are only general guidelines, and actual treatment choices can be affected by numerous other factors, including findings in the same eye or in the contralateral eye and systemic issues.
Order danazol 50 mg online
Used individually menstrual questions answered buy danazol 50mg low cost, appropriate long-term oral antibiotics with antiinflammatory effects include: tetracycline, 500 mg twice daily; erythromycin, 500 mg twice daily; doxycycline, 100 mg twice daily; or minocycline, 100 mg twice daily. A 10-week course of clindamycin, 300 mg twice daily, plus rifampicin, 600 mg twice daily, also has shown efficacy (Gener, 2009). These include systemic cyproterone acetate (an antiandrogen available in Europe), corticosteroids, isotretinoin, cyclosporine, and inflixirnab. Hu and Haefner (2018) have published their successful treatment of severe disease after vulvectomy with skin grafting and vacuumassisted closure. No cure is available, yet treatment goals include basic vulvae skin hygiene and pain management with topical analgesics such as 5-percent lidocaine ointment. In cases resistant to topical corticosteroids, oral corticosteroids can help decrease inflammation. Examples include systemic lupus erythematosus, human immunodeficiency virus infection, erythema multiforme, Stevens- ohnson syndrome, pemphigus, pemphigoid, sarcoidosis, and syphilis. A thorough history and physical examination usually suffice to link genital lesions with preexisting conditions. However, biopsy of vulvovaginal lesions may provide a new and unexpected diagnosis if the disorder has not yet manifest elsewhere. Acanthosis nigricans is commonly associated with obesity, diabetes mellitus, and polycystic ovarian syndrome. Thus, if signs or symptoms of these are present, appropriate evaluation is indicated. Common to these conditions, insulin resistance with compensatory hyperinsulinemia is thought to promote the skin thickening of acanthosis nigricans. Rarely, acanthosis nigricans is caused by other insulin-resistance or fibroblast growth-factor disorders (Saraiya, 2013). Last, topical vitamin D analogs such as calcipotriene can promote plaque improvement (Bohm, 1998). Aphthous Ulcers Nearly 25 percent of women in the second and third decade of life will experience these self-limited mucosa! The ulcers are normally self-limited, but persistent lesions can lead to painful scarring (Rogers, 2003). Diffuse areas of increased pigmentation arc usually encountered on the labia minora and fourchette. However, this may also he seen with pigment variation of chronic inflammatory dermatoscs. Focal dyspigmentation raises concern for premalignant or malignant conditions, and prompt biopsy avoids diagnostic delay. Knife-cut ulcers In the lablocrural folds and perineum are commonly seen with vulvar Crohn disease. Swgery often can be avoided or delayed with appropriate vulvar care, nutrition, and close collaboration with a gastroenterologist. Common nevi arc classified into three groups: junctional, compound, and dermal, depending on whether the mclanotic nc:vus cells are located at the cpidermis-dermis junction, c:x:tcnd into the dermis, or evolve over time to reside entirely with. Dermal nevi may appear bluish or have normal skin coloration depending on the depth of the ncvus c:clls and may be raised, papillary, or pedunculatcd. The American College ofObstetricians and Gynecologists (2016a) recommends biopsy of all such lesions. Namely, asymmetry, uneven pigmentation, irregular border, diameter >5 mm, or erosion or fissuring merits biopsy Edwards, 2010). Atypia or anatomically challenging biopsies, such as those near the clitoris, may prompt referral to clinicians with spccialU. Beh~et disease is characterized by mucocutaneoug le&ions (ocular, oral, and genital) and associated symmic vasculitis. Oral and genital ulcers appear similar to aphthous ulcers and generally heal with. The exact etiology of B~et disease remains unknown, although genetic and autoimmune etiologics are suspected. Accordingly, for those suspected of Beh~et disease, referral to a rheumatologist for additional terting and treatment is recommended. The larger wlvar acrochordon shown here was excised due to mechanical symptoms fi"om Its size. Autoimmune diseases such as Hashimoto thyroiditis, Graves disease, diabetes mellitw, rheumatoid arthritis, psoriasis, and vulvar lichen sderosus are associated with vitiligo Boissy, 1997; Vrijman, 2012). Most commonly, depigmenw:ion is symmetric and generalized, although dimibution may be acral limbs, can) and localized. Sometimes confused with the epithelial changes seen with lichen sclerosus, vitiligo preserves normal skin texture and contour and is otherwise asymptomatic. No cure is presently available fur vitiligo, and spontaneous rcpigmentation is rare. Less commonly, malignant lesions arise on the vulva and are typically of squamous cell epithelial origin. Most often seen on the neck, axilla, or groin, these skin-colored polypoid masses are usually devoid of hair and generally measure 1 to 6 mm in diameter but can grow 1arge. Surgical removal i& likewise recommended fur chronic irritation or cosmetic concerns. Auoehordons have been linked to diabetes mellitus, and insulin-mediated fibrobla&t proliferation may explain this relationship (Demit, 2002). Seborrheic ltmztosis may be observed in women with concurrent lesions on the neck, face, or trunk. These lesions typically appear sharply circumscribed, slightly raised, and waxy or scaly. The malignant potential of these slow-growing lesions is minimal, therefore excision is offered only in eases of discomfort or dis6gurement. Knatoacanthoma is a rapidly growing keratinocyte proliferation originating in a pilosebaceous gland. Untreated, the le&ion usually spontaneously regresses within 4 to 6 month& and leaves only a slightly depressed scar. Some consider keratoacanthoma benign, whereas others classify it as a well-differentiated squamous cell carcinoma. Nevertheless, its bistologic resemblance to this cancer merits surgical excision in most cases with a 4- to 5-mm margin. Syringoma is a benign ecctine (sweat gland) tumor fuund most frequently on the lower eyelid, ncdt, and fa. Rarely, the vulva may be involved bilaterally with multiple 1- to 4-mm 6nn papules. Surgical excision to exclude leiomyosarcoma is sound, and recurrence has been reported (Niel&en, 1996). FihWlmlt is a benign tumor rarely wing from deep vulvar connective tissue by:6broblast proliferation. Larger lesions often become peduneulated with a long stalk and may cause pain or dyspareunia. Surgical excision is indicated fur symptomatic lesions or if the diagnosis is unclear. Similar to fibromas, observation is reasonable in the absence of patient complaints, although symptoms may prompt surgical excision. Ed/Jpic bm#t tisS11e may dcvclop along the theoretical milk lines, which extend bilaterally from the axilla through the breast to the mons pubis. Importantly, these typically soft masses may also dcvdop breast pathologies including fibroadcnoma, phyllodes tumor, Paget disease, and invasive adcnocarcinoma. Whereas most cysts and abscesses lead to labial asymmetry, smaller cysts may be detected only by palpation.
Buy danazol on line
Although the presence of a large amount of blood in the preretinal space or vitreous cavity is not damaging to the retina menopause quality of life scale generic danazol 200mg otc, these intraocular hemorrhages often cause vision loss by blocking the visual axis. Vitreous hemorrhage can also decrease the ability to visualize the retina and thereby limit the ability to adequately diagnose and treat other retinal disease. Membranes on the retinal surface can be induced by blood and result in wrinkling and traction on the retina. Although all retinal neovascularization, given sufficient time, eventually becomes quiescent, as with most scarring processes there is progressive fibrosis of the new vessel complexes that is associated with contraction. In short, causes of vision loss from complications of diabetes mellitus include retinal ischemia involving the fovea, macular edema at or near the fovea, preretinal or vitreous hemorrhage, retinal detachment, and neovascular glaucoma. Vision loss can also result from more indirect effects of vasculopathy in diabetic patients, such as retinal vessel occlusion, accelerated atherosclerotic disease, and embolic phenomena. In the younger-onset group, 86% of blindness was attributable to diabetic retinopathy. In the older-onset group, in which other eye diseases were also common, 33% of the cases of legal blindness were due to diabetic retinopathy. Additionally, intensive insulin therapy reduced the progression of diabetic retinopathy by 34%, to 76%, and had a substantial beneficial effect over the entire range of retinopathy severity. These results underscore the fact that although intensive therapy might not prevent retinopathy completely, it reduces the risk of retinopathy onset and progression. Microaneurysms are outpouchings of the capillary walls that can leak fluid and result in intraretinal edema and hemorrhages. Flame-shaped hemorrhages occur in inner retina closer to the vitreous, and dot-blot hemorrhages occur deeper in the retina. Intraretinal microvascular abnormalities are either new vessel growth within the retinal tissue itself or shunt vessels through areas of poor vascular perfusion. It is common for intraretinal microvascular abnormalities to be located adjacent to cotton-wool spots. Cotton-wool spots are caused by microinfarcts in the nerve fiber layer of the retina. Venous caliber abnormalities, also known as venous beading, are generally a sign of severe retinal hypoxia. In some cases of extensive vascular loss, however, the retina may actually appear free of nonproliferative lesions on clinical examination. Such areas are termed featureless retina and are a sign of severe retinal hypoxia. Neovascularization with fibrous tissue contraction can distort the retina and lead to traction retinal detachment. The most common cause of vision loss from diabetes, however, is macular disease and macular edema. Severe visual loss is defined as best corrected acuity of 5/200 or worse on two consecutive visits 4 months apart. This represents vision loss substantially worse than the 20/200 or worse limit defined as legal blindness. Chapter 37 Complications of Diabetes Mellitus 1475 Diabetes Assessment 1 Month After Initial Injections(s) No Does patient have macular edema Yes No Injection and Return in 1 Month No Fluorescein angiogram usually not indicated Yes Is patient pregnant or allergic to fluorescein dye The schematic flow chart details a general algorithm for appropriate use of fluorescein angiography in the ocular evaluation of patients with diabetes mellitus. Rationale and application of the protocol S anti-vascular endothelial growth factor algorithm for proliferative diabetic retinopathy. The total treatment is usually applied over one to three sessions, spaced 1 to 2 weeks apart. The most desirable effect is to see a regression of the new vessels, although stabilization of the neovascularization with no further growth can result. In Protocol S, 38% of the eyes treated with ranibizumab were eligible to defer monthly injections due to sustained stability of neovascularization at least once over the first 2 years of follow-up, and retinal neovascularization was completely resolved at 44% of visits through 2 years. The actual outcome data from this study is not entirely applicable today due to dramatic advances in surgical techniques and the advent of laser endophotocoagulation that have occurred in the intervening years. Over 2 years, intravitreal steroid administration resulted in a 32% relative risk reduction for retinopathy progression as compared to sham treatment. Typically, injections are performed monthly with a loading dose of at least four to six injections. On average, eight to nine injections are performed in the first year of treatment. The average number of injections required to maintain the beneficial visual acuity gains declines substantially to three or four in the second year, one or two in the third year, and zero to one in years 4 and 5. After 1 year, ranibizumab as applied in the trial resulted in a nine-letter mean gain (p < 0. However, in eyes with baseline vision of 20/50 or worse, aflibercept provided visual gains superior to those achieved with bevacizumab at 1 and 2 years, and vision outcomes were superior to ranibizumab at 1 but not 2 years. These lesions are identified clinically or by fluorescein angiography and consist primarily of leaking microaneurysms. When leakage is diffuse or microaneurysms are extensive, photocoagulation may be applied to the macula in a grid configuration, avoiding the fovea region. Two multicenter randomized prospective clinical trials were undertaken to address both the effectiveness and safety of both routes of steroid administration. The development of cataract was likely a large contributor to declining visual acuity in the steroid-treated group after the first 6 months. Investigations of varying drug dosages to identify the optimal treatment concentration and development of sustained drug delivery devices to limit risks, costs, and inconvenience associated with repeated intraocular injections are underway. Control of Systemic Disorders and Effect of Systemic Medications In addition to the importance of intensive glycemic control in reducing the onset and progression of diabetic retinopathy as discussed earlier, it is critical for the optimal ocular health of diabetic patients that several other systemic considerations be optimized. Elevated blood pressure exacerbates the development and progression of diabetic retinopathy. Overall, hypertension appears to be a significant risk factor in the development and progression of diabetic retinopathy and should be rigorously controlled. Until the results of specific trials investigating the blood pressure levels required to minimize end-organ damage in patients with diabetes are known,431 target blood pressure should most likely be maintained as low as safely possible. The frequent coexistence of retinal and renal microangiopathies with factors that affect both complications, such as associated hypertension and disease duration, make it difficult to establish. In addition, rapidly progressive retinopathy, especially in a patient with a long history of diabetes where retinopathy previously has been stable, should suggest the need for renal evaluation. There have been limited reports of resolution of macular edema and hard exudate with improvement or stabilization of visual acuity in erythropoietin-treated patients after an increase in mean hematocrit. In summary, diabetes is clearly a multisystem disease requiring a comprehensive medical team approach. Even with regard to ocular health, this necessitates the involvement of multiple health care specialists for optimal patient care. Natural History of Nephropathy in Type 1 Diabetes Nephropathy and specifically proteinuria in the setting of diabetes have been known for more than 100 years, and the classic structural features of glomerulosclerosis were described more than 70 years ago. This is partly because significantly more patients are surviving to see the full presentation of this condition. Consequently, few patients were able to survive the course of their renal disease. By comparison, in 1996, the median survival in an equivalent population was more than 17 years. Diabetic nephropathy is characterized clinically as a triad of hypertension, proteinuria, and ultimately renal impairment. In Western countries, diabetes is the leading single cause of end-stage renal disease. Furthermore, the presence and severity of diabetic renal disease significantly contributes to the risk of these conditions.
Diseases
- Pfeiffer Mayer syndrome
- Mild cognitive impairment
- Miosis, congenital
- Emery Nelson syndrome
- Adrenal hyperplasia, congenital
- Aganglionosis, total intestinal
- Wallis Zieff Goldblatt syndrome
- Mental retardation multiple nevi
Order danazol us
When do you offer patients re-resection and what is the evidence for this practice Re-resection therefore improves staging accuracy elderly women's health issues generic 200 mg danazol with visa, which is critical as the treatment of T1 disease differs significantly from T2 disease. For G3pT1 disease, 30% of patients will never have a recurrence, 30% will undergo deferred cystectomy and 30% will die of metastatic disease. Radiotherapy has shown no increase in progression-free interval, progression-free survival or overall survival. Patient and disease factors should be taken into account when deciding on treatment with intravesical immunotherapy or primary radical cystectomy. Fluorescence cystoscopy has been used to detect carcinoma in situ but does have a 35% false-positive rate on biopsy. It is often associated with long-term inflammation and irritation of the bladder from catheterisation, stone disease or schistosomiasis (in sub-Saharan Africa). It generally presents with haematuria in advanced stages and carries a poor prognosis. Cystoscopy reveals an invasive ulcerative lesion often on the trigone or lateral walls of the bladder. Adenocarcinoma of the bladder is rare and accounts for less than 1% of all bladder tumours. It is either primary (de novo carcinoma often on the trigone or posterior wall of the bladder) or secondary (metastatic or associated with an urachal remnant). In urachal adenocarcinoma, the urachal remnant is patent in one-third of patients. Histology shows mucous-secreting cells in a glandular, colloid or signet ring pattern. Clinically an important consideration is to identify a colonic tumour extending into the bladder. The treatment is with radical cystectomy with excision of the urachus and umbilicus but with aggressive management the 5-year survival rate is only 40%. There is no proven role for chemotherapy in this rare tumour, which often presents with muscle-invasive disease at diagnosis. Flexible cystoscopy shows a large invasive looking bladder tumour on the posterior wall of the bladder. Staging of bladder cancer is done through a combination of clinical, histological and radiological means. Radiologically, the bladder is staged locally and also for evidence of loco-regional lymph nodes and metastatic disease. Following detailed visual inspection of the whole urethra and bladder, I would resect the tumour separately in parts including the exophytic portion and edges of resection, and send it as the superficial specimen. I would then resect the underlying muscle to assess muscle invasion and send this separately. Some authorities advocate prostatic biopsies if radical treatment and orthotopic neobladder construction are considered. N1 disease is metastasis in a single lymph node within the true pelvis (hypogastric, obturator, external iliac or presacral), N2 disease is a metastasis in multiple lymph nodes in the true pelvis, and N3 disease is metastasis in one or more common iliac lymph nodes. Pelvic nodes >8 mm and abdominal node >10 mm in the short axis are taken as significant. A bone scan to look for distant metastatic disease can be considered but is not routinely required unless there are specific symptoms or signs. Is this man suitable for radical treatment and how would you decide between radical treatment options The patient should be seen along with a specialist nurse and preferably a family member. His treatment options are radical cystectomy (with ileal conduit or neobladder formation) or radical radiotherapy. A Cochrane review demonstrated a better overall survival benefit with surgery in comparison to radical radiotherapy at 5 years (36% versus 20%) [28]. Although the 5-year survival rates appear better with radical cystectomy, this may be because radical radiotherapy is likely to be given to patients with significant comorbidity. More importantly, no direct randomised comparisons are available between these two treatment options and therefore the patient should have the opportunity to discuss each treatment option in detail including the risk profile of each procedure. Manual dexterity is essential if a neobladder is being considered in order to be able to perform intermittent self-catheterisation. In which situations is radical cystectomy the treatment of choice as compared to radical radiotherapy Complications, such as ileo-ileal anastomotic leak, ureteroileal anastomotic leak, deep vein thrombosis, pulmonary embolus, stroke, myocardial infarction and death, must be discussed with the patient as well as disease recurrence. Patients requiring an ileal conduit need to be aware of the late complications, including risks of stomal stenosis, anastomotic stricture, herniation and metabolic sequelae, such as a hyperchloraemic metabolic acidosis. For a patient receiving an ileal neobladder the operation carries risks of impotence, incontinence or retention. Female surgical candidates should be aware of the risk of shortening and narrowing of the vagina. Is there any advantage to lymphadenectomy and to what extent should it be carried out Lymphadenectomy is an important step in radical cystectomy, providing accurate staging and therapeutic effect. Is there any advantage to laparoscopic or robotic-assisted laparoscopic radical cystectomy It has been noted that the critical factor for outcome is not the technique but rather the surgeon experience and institutional volume. What proportion of men will have prostate cancer detected in a cystoprostatectomy sample Is there any evidence for the use of adjuvant or neoadjuvant chemotherapy in muscleinvasive (non-metastatic) bladder cancer The evidence for adjuvant chemotherapy in muscle-invasive (non-metastatic) bladder cancer is limited and is not advocated for routine use. However, adjuvant chemotherapy is recommended to patients with muscle-invasive disease and/or lymph node positive disease. This is a modest increase in survival, and the numbers are relatively small in the relevant trials. Therapeutic benefit has only been observed with cisplatin-based combination chemotherapy. The disadvantages of neoadjuvant chemotherapy are the associated morbidity and the potential delay in cystectomy in chemotherapy non-responders, which may affect outcome. Do you know of any trials relating to the treatment of muscle-invasive bladder cancer If there has been a good response to chemotherapy in the radiotherapy arm, they will have radiotherapy, and if not, they will have cystectomy. This trial should hopefully help to answer several questions about the relative efficacy of radiotherapy and cystectomy as well as the benefits of neoadjuvant chemotherapy. The secondary outcomes include comparing the safety, efficacy and outcomes of the different techniques. Tell me what options are available for urinary diversion following radical cystectomy The most commonly used method of diversion in the United Kingdom is the ileal conduit.
Generic 200 mg danazol with mastercard
Higher mortality rates are found in diabetics women's health physical therapy buy 100mg danazol free shipping, alcoholics and those with colorectal sources of infection who often have a less typical presentation, greater delay in diagnosis, and more widespread extension. Are there any scoring systems which can predict mortality and outcome in these patients Hyperbaric oxygen therapy has shown some promise in shortening hospital stays, increasing wound healing, and decreasing the gangrenous spread when used in conjunction with debridement and antimicrobials. It is often iatrogenic and frequently occurs after a well-meaning healthcare professional has examined the penis or inserted a urethral catheter and forgotten to replace the foreskin in its natural position. It develops when the tip of the foreskin retracts proximal to the coronal sulcus and becomes fixed in position and develops a constriction ring. Severe oedema of the foreskin occurs within several hours, depending on the tightness of the ring of the foreskin. In most cases, manual compression of the glans with placement of distal traction on the oedematous foreskin allows reduction of the paraphimotic ring. What is different about the dorsal band traction technique and how is it performed Most methods of reduction of paraphimosis focus on decreasing the oedema before reduction. This technique uses the basic surgical principles of traction and countertraction by applying a pair of Adson forceps directly to the band formed by the retracted preputial opening. This is a technique in which the oedematous prepuce is first cleaned with an antiseptic cream and then a 26-gauge needle (outer diameter 0. Using gentle but firm pressure, the oedema fluid is then expressed from the foreskin until it had been completely decompressed, allowing easy reduction of the prepuce. However as the tissue planes can be difficult it is advisable to wait until the oedema has settled completely. If all procedures fail it is possible to perform a dorsal slit under a local anaesthetic. Laboratory guidelines for postvasectomy semen analysis: Association of Biomedical Andrologists, the British Andrology Society and the British Association of Urological Surgeons. Results of 1,469 microsurgical vasectomy reversals by the Vasovasostomy Study Group. Elective indications include protection of anastomosis (pyeloplasty, ureteric reimplantation), to overcome extrinsic ureteric compression, prior to chemotherapy to optimise renal function in obstructive uropathy and pre-operatively (gynaecological or colorectal surgery) to aid identification of 341 the ureter. Emergency indications include relief of ureteric obstruction and management of ureteric trauma. As well as those of actual insertion, complications can be divided into common and rare, as described in Table 14. Ureteric stents are manufactured from a variety of polymers, such as polyurethane and styrene-ethylene-butylene (C-flex). The radio-opacity of stents is increased by coating them in metals such as bismuth and barium. Metallic ureteric stents are variably used for benign or malignant ureteric strictures, Variations include hydrophilic wires (such as the Terumo wire), guidewires with a hydrophilic tip. The tipless variety may allow easier access using the flexible scope, and avoid trauma to the collecting system (easily inserted into renal calyx if necessary). Baskets are commonly made of nickel-titanium memory-shape alloy (Nitinol), and range in size, from about 2 to 3. Harold Hopkins, telescopes consisted of fine lenses cemented into long metal cylinders separated by long airspaces. Optic fibres are flexible glass (or plastic) fibres that allow light to pass through them via a process termed total internal reflection. Optic fibres are grouped together in a parallel fashion and protected by external plastic sleeves. These leads consist of non-coherent fibres, and are relatively inexpensive to produce. In this case, the orientation of the fibres at the proximal end must be the same as the orientation at the distal end to prevent image distortion. Flexible cystoscopes and both semi-rigid and flexible ureterorenoscopes have traditionally used a fibre-optic system, although some newer scopes utilise a digital system. As well as a non-coherent bundle of fibres to transmit light from the external light source, a fibre-optic endoscope utilises a coherent glass fibre bundle, which transmits light back to the eye-piece of the scope in an ordered fashion. Light is transmitted via a process known as total internal reflection through many thousands of fibres and the resultant image can be visualised directly or via a camera-stack system. In common with rigid scopes, a working channel allows the passage of irrigation and instruments into the patient, although this channel is often of a smaller calibre. A flexible endoscope has a deflecting tip, which moves in response to the deflecting lever controlled by the surgeon. As many of the elements of the flexible scope are not heat resistant these scopes cannot be sterilised but rather decontaminated only. Semi-rigid ureteroscopes utilise fibre-optics encased in a metal sheath, and not a rodlens system. This provides the surgeon with a rigid instrument while permitting certain flexibility and is ideal for operating in the ureter. Digital endoscope systems utilise a chip at the distal end of the scope which captures and transmits a digital image. The image tends to be of a much higher quality and the light cable and camera are integrated within the system, removing the need for extra cables and a heavy camera-piece to be attached to the hand-piece of the scope. These instruments are more expensive and at the present time tend to be slightly larger diameter than fibreoptic devices but will no doubt play an important role in the future of endo-urology. The development of disposable flexible ureterorenoscopes is currently being evaluated. What are the approximate lengths, diameters and working channel configurations of the major endo-urological instruments Semi-rigid ureteroscopes vary in size dependent on manufacturer and working channel configuration. It should be remembered that they use fibre-optics for image transmission rather than the rod-lens system of traditional rigid instruments, and hence have a relatively small diameter that usually obviates the need for formal ureteric dilatation. Flexible ureteroscopes (ureterorenoscopes) configurations vary dependent on age and model. The distal end of the instrument is less than 9 Fr, and modern instruments may be even smaller (5. The endoscope may be inserted by means of a hydrophilic access sheath, placed over a guidewire. Adult cystoscope sheaths are generally between 17 and 25 Fr, and approximately 30 cm long. The components of the cystoscope are the telescope (rod-lens), bridge, obturator and sheath. Sterilisation is defined as the complete destruction of living organisms (including spores and viruses). This differs from disinfection, which is a process used to remove most viable organisms, but one which does not necessarily inactivate some viruses and bacterial spores. Cleaning is a process which physically removes contamination but does not necessarily destroy micro-organisms. Autoclaving is a process that combines heat and pressure to sterilise instruments. By combining pressure with heat the temperatures of liquids such as water may be raised above their usual boiling points to facilitate the process. The three variables used in autoclaving are therefore pressure, temperature and time. The actual timing of the whole process is longer than these figures of course, as the machines need to safely heat up and down.
Purchase danazol online now
In fact breast cancer walks 2014 cheap 200 mg danazol amex, it appears that the more attention that is given to the blood glucose results at a visit, the more frequent the monitoring by the patient and the lower the HbA1c. Providing adequate financial support for such services may be challenging for health systems, but this is necessary to limit the burden placed upon providers. Similarly, it may also be challenging for patients and providers to keep current on the array of available equipment and supplies for glucose testing and handling of the resulting data. A useful resource in this regard is the annual Consumer Guide, which is published as the January issue of Diabetes Forecast, a magazine for laypeople with diabetes and their families. These devices sample subcutaneous interstitial fluids at frequent intervals and can report the results either in real time or upon demand. Curves/plots represent glucose frequency distributions by time regardless of date. A smartphone may serve as the receiver, and appropriate apps will give real-time glucose information, updating every 5 minutes. Trend arrows are shown, and information can be shared with providers as well as family members or other supporting individuals. However, once scanned, the reader will display the present glucose value as well as a rate of change arrow and a recording of the glucose trend over the last 8 hours. If the sensor is scanned every 8 hours, a continuous chart of the glucose trends can be viewed. A strong rationale for this decision is that protection against hypoglycemia is of heightened importance in older patients. Under normal circumstances a decline of glucose concentrations below 70 mg/ dL (<3. Symptoms of hypoglycemia may or may not result from these responses, but declines below this threshold, termed level 1 hypoglycemia, are considered important as alerts to allow protection against more worrisome declines of glucose. Level 2 hypoglycemia is defined as glucose documented at or lower than 54 mg/dL (3 mmol/L). Repeated declines to this range are considered clinically significant because they can cause blunting of compensatory hormone responses and loss of warning symptoms ("hypoglycemia unawareness"), and thereby increase the risk of more dangerous lows. Level 3 is considered severe hypoglycemia, defined as requiring assistance by another person, whether a friend or family member or a medical provider. Although hypoglycemia can directly cause such events through falls and cardiac arrhythmias, this relationship with serious medical outcomes is thought to be partly related to an association of hypoglycemia with other causes of risk, including concurrent illness, inconsistent eating patterns, malnutrition and weight loss, physical frailty, and cognitive impairment. Nonetheless, level 3 severe events are markers of risk and call for both conservative glycemic management and renewed attention to other aspects of care. They are most effective when presented as parts of a comprehensive plan of self-management with the goal of moving the focus of care from the provider to the individual with diabetes. The provider has little connection with day-to-day care, thus the patient needs the tools, confidence, and a plan for self-management. These include the time of diagnosis, annual reassessments, when complicating factors arise, and the time of critical transitions in medical care or life circumstances. The need for a team approach has long been recognized in diabetes care and remains a critical ingredient for success. The providers (physicians and advanced practice providers) enrich their care with the help of nurses, dietitians, exercise specialists, behavioral specialists, pharmacists, podiatrists, and other medical and surgical specialists. Beyond these traditional pillars of lifestyle management there is growing attention to psychosocial concerns as well as interest in various forms of stress reduction, relaxation, and sleep management. Group sessions provide added support as do programs that involve peer groups and health coaches without a traditional medical professional directly involved. A summary of general nutritional principles for people with diabetes is shown in Table 35. It is very helpful to know how many meals the patient eats in a day, and at what times. Therefore carbohydrate sources high in protein should be avoided when trying to treat or prevent hypoglycemia. Education and awareness regarding the recognition and management of delayed hypoglycemia are warranted. Nonnutritive sweeteners are generally safe to use within the defined acceptable daily intake levels. This information should be reassessed periodically, with specific suggestions for changes that are achievable. A pattern of snacking from dinner until bedtime or consistently overeating on weekends can create difficulties. Achieving a 5% weight loss more consistently yields significant metabolic benefits than lower levels of weight loss. Patients who lost less than 5% of body weight had insignificant HbA1c reductions, similar to that in the control group. Of those in the intervention group who lost 5% to 10 % of body weight, 34% ended with HbA1c below 6. The reduction of HbA1c was often accompanied by less use of pharmacologic agents as well. Glucose levels after meals are strongly influenced by the carbohydrate content of the diet. These include the "plate method," carbohydrate exchange lists, and even simple portion control tactics. Therefore including some protein and fat in each meal and snack is useful, and these macronutrient groups along with fiber content can attenuate the effect of carbohydrate on postprandial elevations. Low carbohydrate diets, including ketogenic diets, have grown in popularity and are associated with decreased postprandial glucose and a reduction in HbA1c. In many cases the postprandial glucose decreases with lower carbohydrate intake, but fasting glucose may be higher. The glycemic index refers to the glucose response to equal amounts of carbohydrates in various foods. This index has proven somewhat difficult to use for meal planning, and studies evaluating the benefit of lowering glycemic index have yielded mixed results. Although dietary fats clearly have an impact on total caloric intake (related to their caloric density) and on circulating lipids, they have little effect on glycemia. Fat intake is a contributor to obesity and is the critical nutrient for cardiovascular risk management. It is recommended that people with diabetes (and everyone in general) consume a diet that is modestly restricted in calories (if overweight) and contains less than 10% of total calories as saturated fat and less than 10% as polyunsaturated fat. Higher carbohydrate diets can raise postprandial glucose and triglycerides but are much less calorically dense than higher fat diets and have a higher thermic effect, both of which tend to promote weight loss. Dietary protein similarly has little impact on glucose levels, although amino acids do promote insulin secretion. Metabolism of protein results in the formation of acids and nitrogenous waste, which can lead to bone demineralization and glomerular hyperfiltration. Restriction of protein intake to 10% to 20% of total calories minimizes potential adverse long-term effects of high protein intake. However, recent guidelines do not support the notion that dietary protein need be reduced in those with chronic kidney disease. Still, there may be some benefit on HbA1c and lipid profiles for those ingesting at least 15 g of fiber per 1000 kcal compared to lower fiber diets. Alcohol in moderation (up to one drink per day for adult women or two drinks per day in adult men) is not specifically recommended but is considered acceptable. Moderate red wine intake may result in mild improvement in some lipid parameters but seems to have little effect on glucose control. Nonnutritive sweeteners such as aspartame, aceK, saccharin, stevia, or sucralose do not appear to impact lipid parameters, insulin secretion, or blood pressure independent of weight loss. Sodium restriction to less than 2300 mg per day is recommended, and lower sodium diets may have additional benefit in some individuals with hypertension. Some clinicians are convinced of the utility of magnesium, chromium, zinc, folic acid, pyridoxine, cyanocobalamin, vitamin A, vitamin C, vitamin E, vanadium, selenium, garlic, and other micronutrients. Many patients are convinced that nutritional supplementation is healthful, and it is often counterproductive to engage in scholarly discussion of the nature of the evidence base for their decision. At a minimum, discussion should include the documented efficacy of more classic lifestyle and pharmacologic interventions and the idea that these efforts should not be ignored. For example, ketogenic diets or low carbohydrate diets have limited long-term evidence of benefit or risk at the present time. However, if a patient or practitioner wants to use a lower carbohydrate higher protein/fat reduced calorie diet, that choice may be associated with short-term improvements in glycemia, cardiovascular risk markers, and weight. Exercise is associated with improved glycemic control, insulin sensitivity, cardiovascular fitness, and quality of life.
Purchase line danazol
Frequency and predictors of hypoglycaemia in type 1 and insulin-treated type 2 diabetes: a population-based study women's health clinic philadelphia buy cheapest danazol and danazol. Risk of hypoglycaemia in types 1 and 2 diabetes: effects of treatment modalities and their duration. United Kingdom Prospective Diabetes Study 24: a 6-year, randomized, controlled trial comparing sulfonylurea, insulin, and metformin therapy in patients with newly diagnosed type 2 diabetes that could not be controlled with diet therapy. Frequency and symptoms of hypoglycaemia experienced by patients with type 2 diabetes treated with insulin. Clinical characterisation of severe hypoglycaemia-a prospective population-based study. Frequency of severe hypoglycemia requiring emergency treatment in type 1 and type 2 diabetes: a population-based study of health service resource use. Recall of severe hypoglycaemia and self-estimated state of awareness in type 1 diabetes. Neuropsychological profiles of young people with type 1 diabetes 12 yr after disease onset. Association between hypoglycemia and dementia in a biracial cohort of older adults with diabetes mellitus. The British Diabetic Association Cohort Study, I: all-cause mortality in patients with insulintreated diabetes mellitus. Acute complications and drug misuse are important causes of death for children and young adults with type 1 diabetes: results from the Yorkshire Register of diabetes in children and young adults. Long-term mortality in a nationwide cohort of childhood-onset type 1 diabetic patients in Norway. Confirmation of hypoglycemia in the "dead-in-bed" syndrome, as captured by a retrospective continuous glucose monitoring system. Risk of hypoglycaemia with oral antidiabetic agents in patients with type 2 diabetes. Impact of differing glucose-lowering regimens on the pattern of association between glucose control and survival. Risk of cardiac arrhythmias during hypoglycemia in patients with type 2 diabetes and cardiovascular risk. Severe hypoglycemiainduced lethal cardiac arrhythmias are mediated by sympathoadrenal activation. Prolonged cardiac repolarisation during spontaneous nocturnal hypoglycaemia in children and adolescents with type 1 diabetes. Antecedent hypoglycemia impairs autonomic cardiovascular function: implications for rigorous glycemic control. Hypoglycemia and diabetes: a report of a workgroup of the American diabetes association and the endocrine Society. Individualized glycemic goals and an expanded classification of severe hypoglycemia in diabetes. Identification of type I diabetic patients at increased risk for hypoglycemia during intensive therapy. A reliable and reproducible test for adequate glucose counterregulation in type I diabetes mellitus. Evidence for a vicious cycle of exercise and hypoglycemia in type 1 diabetes mellitus. Sleep-related hypoglycemia-associated autonomic failure in type 1 diabetes: reduced awakening from sleep during hypoglycemia. Hypoglycemic symptoms and decreased beta-adrenergic sensitivity in insulin-dependent diabetic patients. Avoidance of hypoglycemia restores hypoglycemia awareness by increasing beta-adrenergic sensitivity in type 1 diabetes. Preserved sensitivity to beta2-adrenergic receptor agonists in patients with type 1 diabetes mellitus and hypoglycemia unawareness. Recent antecedent hypoglycemia reduces autonomic responses to , symptoms of, and defense against subsequent hypoglycemia. Hypoglycemia-associated autonomic failure in diabetes: maladaptive, adaptive, or both Unawareness of hypoglycaemia and inadequate hypoglycaemic counterregulation: no causal relation with diabetic autonomic neuropathy. Impact of nocturnal hypoglycemia on hypoglycemic cognitive dysfunction in type 1 diabetes. Brief twice-weekly episodes of hypoglycemia reduce detection of clinical hypoglycemia in type 1 diabetes mellitus. Restoration of hypoglycaemia awareness in patients with long-duration insulin-dependent diabetes. Glucagon, catecholamine and pancreatic polypeptide secretion in type I diabetic recipients of pancreas allografts. Pancreatic response to mild non-insulin-induced hypoglycemia does not involve extrinsic neural input. The physiology and pathophysiology of the neural control of the counterregulatory response. Activation of human medial prefrontal cortex during autonomic responses to hypoglycemia. Attenuation of counterregulatory responses to recurrent hypoglycemia by active thalamic inhibition: a mechanism for hypoglycemia-associated autonomic failure. Increased brain lactate concentrations without increased lactate oxidation during hypoglycemia in type 1 diabetic individuals. Lactate preserves neuronal metabolism and function following antecedent recurrent hypoglycemia. Impaired glutamatergic neurotransmission in the ventromedial hypothalamus may contribute to defective counterregulation in recurrently hypoglycemic rats. Epidemiology of severe hypoglycemia in the diabetes control and complications trial. Correlation between minimal secretory capacity of pancreatic beta-cells and stability of diabetic control. Determinants of severe hypoglycemia complicating type 2 diabetes: the Fremantle diabetes study. Risk factors of severe hypoglycaemia in adult patients with type I diabetes-a prospective population based study. Beta-cell function and the development of diabetes-related complications in the diabetes control and complications trial. Impact of C-peptide preservation on metabolic and clinical outcomes in the diabetes control and complications trial. Prevention of hypoglycemia while achieving good glycemic control in type 1 diabetes: the role of insulin analogs. Predictors of fear of hypoglycemia in adolescents with type 1 diabetes and their parents. Fear and other disturbances of severe hypoglycaemia in children and adolescents with type 1 diabetes mellitus. Improved biomedical and psychological outcomes 1 year after structured education in flexible insulin therapy for people with type 1 diabetes: the U. Continuous glucose monitoring for hypoglycemia avoidance and glucose counterregulation in long-standing type 1 diabetes. Continuous glucose monitoring, future products, and update on worldwide artificial pancreas projects. Diabetes technologycontinuous subcutaneous insulin infusion therapy and continuous glucose monitoring in adults: an Endocrine Society clinical practice guideline. Continuous subcutaneous insulin infusion versus multiple daily injections in individuals with type 1 diabetes: a systematic review and meta-analysis. Effect of insulin analogues on frequency of non-severe hypoglycaemia in patients with type 1 diabetes prone to severe hypoglycaemia: the HypoAna trial. Comparison of insulin glargine 300 units/mL and 100 units/mL in adults with type 1 diabetes: continuous glucose monitoring profiles and variability using morning or evening injections.