12.5mg microzide overnight delivery
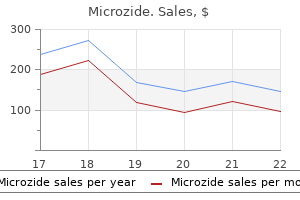
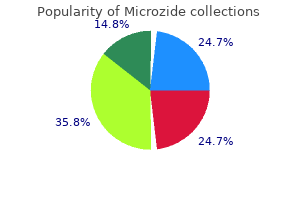
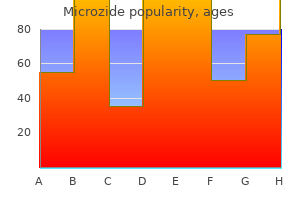
The prevalence of asymptomatic cardiac disease in children with systemic sclerosis is not known (289-294) heart attack 3964 purchase microzide toronto. Unfortunately, there are not many investigative studies in the literature that provide more information on the cardiac risks and risk factor associations in juvenile onset systemic scleroderma. Endomyocardial biopsy is neither a risk-free procedure nor is it used very often in practice. The available information on cardiac involvement mostly comes from autopsy results that only represent the extreme end of the spectrum of the disease. It appears that while the cardiac involvement is not common in juvenile onset scleroderma, its presence suggests a poor prognosis. The prevalence of asymptomatic cardiac involvement in childhood systemic scleroderma is not known. Early and aggressive therapy with immunosuppressant medication, fibrinolytic medication, and supportive therapy may help to prevent cardiac disease and improve the outcome in patients with juvenile onset systemic scleroderma. It is also important to monitor children with local scleroderma for systemic disease. Since then, it is increasingly recognized that the incidence of cardiac sarcoidosis is far more common than previously thought. When it does occur, cardiac involvement in sarcoidosis is still often overlooked due to the lack of awareness of its possibility, its slow subclinical progression, and the absence of any robust and reliable diagnostic tool (297). Cardiac involvement in children and adults appears to be unusual in most areas of the world, but for unexplained reasons it is far higher in Japanese population than the rest of the world, affecting up to 50% to 78% of sarcoidosis patients. In Japanese patients, 85% of deaths with sarcoidosis are due to cardiac involvement (298-300). They reported that clinical features and presentations in their cohort were similar to that of adults but they found cardiac involvement to be more frequent in younger patients and adolescents than in adults (302-306). Several groups report that the significance of cardiac involvement from prognostic point of view is not known (195) while other groups believe it to be potentially fatal and a bad prognostic sign (296,298,307-309). Of the patients who were found to have cardiac involvement, 35% did not have cardiac symptoms while there was a history of heart failure, arrhythmias, and/or conduction defects in 65%. Clinical diagnosis group Ifendomyocardial biopsy specimens do not demonstrate noncaseating epithelioid cell granulomas, extra cardiac sarcoidosis is diagnosed histologically or clinicallyifthe disease satisfies the following conditions and more than one in six basic diagnostic criteria are present. One in four of the major criteria and two or more of the five minor criteria are satisfied. Abnormal echocardiography: regional abnormal wall motion or morphologic abnormality (ventricular aneurysm, wall thickening). Nuclear medicine: perfusion defect detected by 201thallium or 99 m technetium myocardial scintigraphy. Sarcoidosis can affect the pericardium, myocardium, or endocardium with equal frequency (296,313). These autopsy findings support recent clinical findings that the real incidence of clinical cardiac involvement in sarcoidosis may be between 5% and 50% (314). Cardiac disease is not necessarily always secondary to cor pulmonale or lung involvement as previously thought but isolated cardiac involvement can occur at any age and stage of the disease (296,314) in the absence of pulmonary and even any other systemic involvement. Sometimes cardiac involvement only got attention of physicians after the pulmonary disease resolved (315). Occasionally cardiac involvement may be the first presentation of the disease (306). The severity and duration of pulmonary disease cannot predict the presence and extent of cardiac involvement (316). Echocardiography is recommended to diagnose the cardiac involvement in patients with sarcoidosis. Echocardiography may be useful if it demonstrates a classic basal interventricular septal thinning or localized ventricular aneurysmal dilation, usually without coronary artery disease. Less frequently, pericardial effusion, cardiac tamponade, and cardiac failure may be seen (195,317,323). These complications generally occur in patients with widespread myocardial involvement (311,324). Corticosteroids are the mainstay of the treatment for cardiac sarcoidosis but have not shown survival benefit in prospective trials (101,298). Other disease-modifying medications and immunosuppressants such as methotrexate, azathioprine, hydroxychloroq uine, chloroquine, cyclophosphamide, cyclosporine A, thalidomide, pentoxyphylline, and infliximab have been used with varying success (306,308,312,325-327). A combination of steroids and another immunosuppressant may be used to limit steroid side effects. In patients with disseminated myocardial involvement, the use of antiarrhythmic drugs and automated implantable cardiac defibrillator as bridge therapy while waiting for cardiac transplant has been advocated to prevent sudden death (312). Estimates of the prevalence of arthritis and other rheumatic conditions in the United States: Part I. Determination of anti-citrullinated peptide antibodies in the sera of patients with juvenile idiopathic arthritis. Cardiac tamponade in juvenile chronic arthritis: report of two cases and review of publications. Large pericardial effusion requiring pericardiocentesis as cardinal sign of macrophage activation syndrome in systemic onset-juvenile idiopathic arthritis. Prevalence of pericardia I effusion by echocardiography in juvenile rheumatoid arthritis. A patient diagnosed with pauciarticular juvenile rheumatoid arthritis after a mechanical prosthetic valve replacement due to aortic regurgitation. Cardiac operations for North American children with rheumatic diseases: 1985-2005. The incidence of pediatric rheumatic diseases: results from the Canadian Pediatric Rheumatology Association Disease Registry. Description of 37 cases in children and a discussion of endocrine therapy in 32 of the cases. Review for the generalist: the antinuclear antibody test in children-When to use it and what to do with a positive titer. Correlation of Sm antibody titers with disease activity and other laboratory parameters. Juvenile-onset systemic lupus erythematosus: different clinical and serological pattern than adult-onset systemic lupus erythematosus. Heart valve involvement (Libman-Sacks endocarditis) the antiphospholipid syndrome. Immunological and clinical differences between juvenile and adult onset of systemic lupus erythematosus. Cardiac involvement in systemic lupus erythematosus: ana torno-pathological study. Cardiovascular manifestations of systemic lupus erythematosus: current perspective. Cardiac disease in systemic lupus erythematosus: prospective study of 70 patients. Libman-Sacks endocarditis in systemic lupus erythematosus: prevalence, associations, and evolution. Echocardiography and pulmonary function testing in childhood onset systemic lupus erythematosus. Assessment of myocardial perfusion and function in childhood systemic lupus erythematosus. The American College of Rheumatology 1990 criteria for the classification of vasculitis. Takayasu disease masquarading as interruption of the aortic arch in a 2-year-old child. Clinical manifestations of Takayasu arteritis in India and Japan-new classification of angiographic findings. Association of antiphospholipid valvulopathy in systemic lupus erythematosus: a systematic review.
Order generic microzide from india
Transient and isolated peripheral nerve impairment such as facial palsy blood pressure in elderly generic 12.5 mg microzide amex, phrenic nerve paralysis, or sensorineural hearing loss has also been described (59,60). If the patient remains untreated or is treated with aspirin only, the febrile course usually lasts from 1 to 3 weeks. The patient may show transient anemia and leukocytosis with increased numbers of neutrophils and bands. Children who have recurrent disease appear be at increased risk of coronary complications (13). All clinical features are rarely present at the same time, so the diagnosis requires sequential evaluation of the patient with detailed day-by-day history of the present illness. Elevations of liver function tests, including plasma gamrna-glutarnyl transpeptidase, transaminases, and bilirubin, are also common (62,64). Lumbar puncture may show findings compatible with aseptic meningitis, with a predominance of mononuclear cells, but with normal glucose and protein levels (65). Clinical Features: Cardiovascular During the acute phase, patients may manifest signs of myocarditis, such as sinus tachycardia out of proportion to the fever, gallop rhythm, and sometimes muffled heart tones. A pericardial effusion by echocardiography is not uncommon, but the effusions generally measure <1 mm (72); pericardial tamponade is very rare (73). Systolic murmurs are often heard owing to increased cardiac output and anemia, and approximately one-quarter of patients have mitral insufficiency (72). The Japanese National Kawasaki Disease surveillance data estimates the incidence of coronary aneurysms to be between 10. An aneurysm in the distal arterial segment is usually but not always accompanied by an aneurysm in the proximal segment of the same artery. Aneurysms with internal diameters >8 mm or a z-score of ~10 (so-called giant aneurysms) present disproportionately higher risks of myocardial infarction as compared with aneurysms of smaller dimensions (75,76). Several risk scores have been formulated to predict the development of coronary artery aneurysms based on clinical and laboratory data at presentation (77-81). Younger age in particular seems to be an important predictor for worse presentation. For these patients, one should consider alternative diagnoses (see Diagnosis and Differential Diagnosis, Table 59. Rarely, the chest x-ray may show localized pulmonary infiltration or pleural effusion. Patients whose coronary aneurysms persist ~1 year after the onset of the disease may show a thin, eggshell-like calcification outlining the aneurysms. Myocardial dysfunction is associated with a greater risk of coronary artery dilation (72). Echocardiography is usually repeated at 2 and 6 weeks after the onset of illness to see the extent of coronary involvement and to guide therapy. For patients with giant aneurysms, we perform echocardiograms twice weekly early in the illness, then weekly through the first 45 days of illness, monthly until the 3rd month, and then every 3 months for the first year to assess for thrombosis. For long-term cardiac follow-up, echocardiography is useful for evaluating global left ventricular function, regional wall motion characteristics, and competency of mitral and aortic valves. Proximal segments of the right and left coronary arteries may be visualized in nearly all patients. Visualization of distal coronary artery segments may be technically demanding, necessitating patient sedation, use of special views (87), and careful optimization of machine settings. Standards published by the Japan Kawasaki Disease Research Committee use an empiric definition of abnormality (89). By these standards, a coronary artery is classified as abnormal if (a) the internal diameter is >3 mm in children younger than 5 years of age; (b) the internal diameter is >4 mm in children ~5 years of age; (c) if the internal diameter of a segment measures 1. Representative electrocardiogram leads in a 4-month-old girl with Kawasaki disease recorded on illness days 17 and 20. The latter tracings show marked decrease in R-wave voltage (V2-V5), indicative of acute anterior wall infarction, which was proven at autopsy. Chest pain is reported much less frequently in children younger than 4 years of age. Approximately one-third of the patients are asymptomatic at the time of infarction, which often occurs at rest or during sleep, and infrequently during exertion (82). Fatality associated with the first episode of myocardial infarction has been reported to be 22%, with a progressively worsening mortality rates with subsequent attacks. Preexisting obstructions in two or more major coronary arteries or in the left main coronary artery are associated with increased mortality. Published normative coronary artery dimensions by echocardiography encompass such a wide range of values that there is a significant overlap between normal and abnormal arteries (90-92). Therefore, an alternate aneurysm classification schema considers the size of the coronary in relation to the size of the patient (61). When z-scores are used, the following cutpoints have been proposed: a small aneurysm has z-score ~ 2. Virtually all types of stress tests performed in adults with ischemic heart disease have been applied to the pediatric population. These include nuclear perfusion scans with exercise (93,94), exercise echocardiography (94), stress echo cardiography using pharmacologic agents, such as dobutamine (95,96), dipyridamole, or adenosine (97), magnetic resonance stress imaging, with quantification of regional perfusion (98), and stress myocardial contrast echocardiography (99-101). The combination of resting and stress myocardial perfusion imaging using thallium 201 or a technetium-99m-based compound has high sensitivity but moderate to low specificity in detecting coronary artery obstruction (102). Nevertheless, the technique is useful in longitudinal follow-up of patients with known coronary pathology. The predictive value of stress tests for coronary artery disease requiring intervention is a function of the probability of significant disease in the population tested (Bayes theorem). For example, false-positive tests are more likely in patients with a low prior probability of coronary disease. Used appropriately, the results of stress testing may guide the decision to refer a patient for invasive evaluation. In the older child, exercise stress testing best simulates everyday life exposure and should be accompanied by some imaging technique to enhance sensitivity to detect ischemia. Some studies reported abnormalities in noninvasive vascular testing, including brachial artery reactivity testing (112) and pulse wave velocity (113-115), while other studies do not confirm these results (116,117). Patients who have never had coronary abnormalities should be counseled on modifiable risk factors for future atherosclerotic cardiovascular disease. Children who develop small- to medium-sized coronary artery aneurysms also tend to have good prognosis, at least through childhood, because their coronary arteries usually undergo regression to normal lumen diameter. Among coronary arterial segments with aneurysms, approximately half will regress to normal internal lumen diameter within 1 to 2 years (54,55,111). Regression appears to occur by neointimal thickening due to migration, transformation, and proliferation of smooth muscle cells derived from the tunica media (54) and replacement of the inflammation with fibroblasts and extracellular matrix. However, vessels with regressed aneurysms, even with normal appearing lumens, may have an abnormally thick intima-medial layer as seen by coronary intravascular ultrasonography (119), with thicker intima in vessels that had greater initial diameters (120). In addition, these vessels have a reduced capacity for vasodilation when challenged by infusion of nitrates (non-endothelium-dependent vasodilators) and may undergo paradoxical vasoconstriction in response to acetylcholine (an endothelium-dependent vasodilator) (121-123). A postmortem histologic study in children who died years later due to unrelated causes showed extensive intimal thickening in coronary artery segments (53). Large or complex aneurysms are less likely to undergo regression and place patients at risk for ischemic heart disease. Later onset myocardial ischemia or infarction is more likely due to acute thrombosis at the site of progressive coronary artery stenosis due to myointimal proliferation; in severe cases, myocardial infarction or ischemic cardiomyopathy may result. According to a nationwide hospital survey in Japan, 73% of myocardial infarctions occurred during the first year after illness onset invasive testing is required. There is little incremental value in angiography if echocardiography clearly shows a small solitary aneurysm in continuity with normal proximal and distal segments in an asymptomatic patient. Selective coronary arteriography is advantageous over aortic root injection because aneurysms, obstructions, and collateral arteries can be precisely delineated. Our current practice is to perform cardiac catheterization for angiography at 1 year after the onset of illness in patients with complex or large coronary aneurysms who cannot be imaged in other ways, who have symptoms of ischemia, or in whom findings would guide therapeutic decisions. Because peripheral artery aneurysms may occur, particularly in children with giant aneurysms, angiograms of peripheral arteries, including the subclavian arteries, internal mammary arteries, and iliaci femoral vessels should be performed in children undergoing radiographic coronary angiography. Serial right coronary arteriograms in a boy who developed Kawasaki disease at 3 months of age. B: Follow-up study obtained 16 months later shows near-complete regression of the aneurysm. Fortunately, spontaneous myocardial revascularization through formation of collateral arteries and recanalization is common. Serial right coronary angiograms in a girl who developed Kawasaki disease at 2 months of age.
Purchase microzide cheap
A mouse model for mitochondrial myopathy and cardiomyopathy resulting from a deficiency in the heart/muscle isoform of the adenine nucleotide trans locator blood pressure chart in canada 12.5mg microzide free shipping. Novel organ-specific circulating cardiac autoantibodies in dilated cardiomyopathy. Circulating cardiac-specific autoantibodies as markers of autoimmunity in clinical and biopsy-proven myocarditis. Cardiac-specific overexpression of tumor necrosis factoralpha causes lethal myocarditis in transgenic mice. Therapeutic effect of anti-tumor necrosis factor-alpha antibody on the murine model of viral myocarditis induced by encephalomyocarditis virus. Interleukin-2 suppressed myocarditis in the acute stage but enhanced the condition in the subsequent stage. Long-term outcome of fulminant myocarditis as compared with acute (nonfulminant) myocarditis. Adenoviruses and enteroviruses as pathogens in myocarditis and dilated cardiomyopathy. Myocarditis and inflammatory cardiomyopathy: microbiological and molecular biological aspects. Active Coxsackieviral B infection is associated with disruption of dystrophin in endomyocardial tissue of patients who died suddenly of acute myocardial infarction. Immunosuppressive therapy for active lymphocytic myocarditis: virological and immunologic profile of responders versus nonresponders. Therapy with immunoglobulin suppresses myocarditis in a murine coxsackievirus B3 model. Extracorporeal membrane oxygenation for the support of infants, children, and young adults with acute myocarditis: a review of the Extracorporeal Life Support Organizarion registry. Molecular remodelling of dystrophin in patients with endstage cardiomyopathies and reversal in patients on assistance-device ther- 134. Clinical and pathologic findings of myocarditis in two families with dilated cardiomyopathy. Analysis of the coxsackievirus B-adenovirus receptor gene in patients with myocarditis or dilated cardiomyopathy. The coxsackie-adenovirus receptor induces an inflammatory cardiomyopathy independent of viral infection. Adenovirus infection in the lung results in graft failure after lung transplantation. Coxsackievirus B3 myocarditis in C3H1HeJ mice: description of an inbred model and the effect of exercise on virulence. Effect of delayed captopril therapy on left ventricular mass and myonecrosis during acute coxsackievirus murine myocarditis. Guidelines for the diagnosis and treatment of chronic heart failure: executive summary (update 2005): the Task Force for the Diagnosis and Treatment of Chronic Heart Failure of the European Society of Cardiology. Vaccination with coxsackievirus B3 virus-like particles elicits humoral immune response and protects mice against myocarditis. Denfield ardiomyopathies are defined as diseases of the myocardium associated with cardiac dysfunction (1). Whether this apparent difference in usual age of onset is due to case ascertainment or true differences in the disease onset is unknown. Beyond infancy, boys had a higher incidence of cardiomyopathy than girls in the study by Lipshultz et al. Only hypertrophic and unspecified cardiomyopathies occurred with higher frequency in boys in the Nugent et al. Approximately 30% of patients, in whom family history was reported, had a positive family history (3-37). The diversity of the phenotypic expression of troponin mutations in families suggests that additional genetic or environmental factors or both playa role in disease expression. The overlapping genotypic-phenotypic correlations are also evident in a report by Olson et al. The proband was a child with a myosin light-chain mutation resulting in a cardiomyopathy with midcavitary hypertrophy and restrictive physiology that was inherited in an autosomal recessive pattern. Overall, the incidence of cardiomyopathies is higher in children <1 year of age when all types of cardiomyopathy are considered (6,7). Only two of the patients were 19 at the time of diagnosis with the remainder <18 years old. Clinically unaffected family members were either heterozygotes or lacked the mutant allele. Congestive heart failure and pericardial constriction were diagnosed during infancy in 12% and 6% of the patients, respectively, in a report by Karlberg et al. Characteristic craniofacial features included scaphocephaly, facial triangularity, high and broad forehead, and low nasal bridge in more than 90% of the patients. Other findings included a peculiar high-pitched voice (96%), yellowish dots in ocular fundi (79%), cutaneous naevi flammei (65%), hepatomegaly (45%), and fibrous dysplasia of long bones (25%). Desmin is a myofibrillar protein that is the chief intermediate filament of skeletal and cardiac muscle (41). It maintains the structural and functional integrity of the myofibrils and functions as a cytoskeletal protein linking Z bands to the plasma membrane. It is characterized by developmental delays, short stature, facial dysmorphisms, and progressive skeletal deformities. Cardiac anomalies are reported in approximately 14% of affected males with cardiomyopathy being one of the rare but reported cardiac abnormalities, including one patient with a restrictive phenotype (33). Emery-Dreifuss muscular dystrophy was first described as an X-linked disorder caused by mutations in the gene encoding for emerin on chromosome Xq28 (38). It occurs most frequently in tropical and subtropical Africa, particularly Uganda and Nigeria. However, it is also found in tropical and subtropical regions throughout the world. Hypereosinophilia, likely related to parasitic infections, has occurred in some patients. Familial occurrence, and in some countries a high incidence in some ethnic groups, suggests a possible genetic predisposition (57,58). The disease is most commonly biventricular, followed by pure left ventricular involvement approximately 40% of the time and purely right ventricular in 10% (62). The clinical picture may include weight loss, fever, cough, rash, and heart failure. Therapy for the hypereosinophlia may include corticosteroids, hydroxyurea, or vincristine, but this area of therapy is usually not directed by a cardiologist. Surgical approaches have included mitral and/or tricuspid valve repair or replacement and excision of fibrotic endocardium and may be useful for symptom palliation of intractable heart failure. Infiltrative and Storage Diseases complex varies with the site or sites of involvement. Symptoms from pulmonary venous congestion result from left-sided disease, while right-sided disease results in signs and symptoms from systemic venous congestion. Involvement of the mitral or tricuspid valve apparatus can result in significant valvular regurgitation. Histologic changes occur in predominantly three areas: the left ventricular apex, the mitral valve apparatus, and the right ventricular apex that may extend to the supporting structures of the tricuspid valve. Small patches of fibroelastosis may occur in the outflow tracts, but the elastin component is thought to be secondary and not a primary part of the process. Eosinophilia is not typically a prominent feature in contrast to Leffler endocarditis. Nephropathic cystinosis is an autosomal recessive disease that leads to multi organ failure from intracellular accumulation of cystine (67). Dixit and Greifer reported one patient followed from infancy who developed a cardiomyopathy with restrictive features in adulthood and had extremely high cystine levels in the myocardium. Sarcoidosis is a none as eating granulomatous disorder that is more common in adults than in children. Although the family history is positive in only approximately 30% of this population, a genetic basis or predisposition for the development of the disease is likely. Patients who have ascites, hepatomegaly, and edema are frequently referred to a gastroenterologist first.
Generic microzide 25mg with mastercard
Nonmalignant congenital intrapericardial lesions may occur blood pressure charts readings cheap microzide on line, including pericardial cysts, extralobar pulmonary sequestration, cystic lymphangioma, bronchogenic cysts, and pericardial teratomas (66-70). Pericarditis can occur as a complication of certain chemotherapy agents, listed in Table 62. Diagnosis of the cause of a malignant effusion can be made using cytologic analysis and culture of pericardia I fluid (72). Patients who have received mediastinal irradiation are at increased risk of pericardia I involvement after chemotherapy. Up to 5% of patients receiving mediastinal irradiation will develop pericarditis, typically from 2 months to 2 years after treatment (73). The patient may present with only mild symptoms or may progress to fulminant constrictive pericarditis Kawasaki Disease During the acute phase of Kawasaki disease, one-third of patients have a pericardial effusion, which typically resolves within 2 weeks. Effusions related to this inflammatory process do not commonly progress to tamponade, but this has been reported (52,53). Drug-Induced Pericarditis Drug-induced pericarditis may occur in patients treated with the medications listed in Table 62. Patients with hypersensitivity reactions to penicillin and cromolyn sodium in association with pericardial effusion have been reported (55,56). Hypothyroidism the hypothyroid patient with a pericardia I effusion most commonly is asymptomatic. It occurs in up to 80% of patients with myxedema, but is rare in patients with only mild hypothyroidism (57). Cardiac tamponade is exceedingly uncommon due to the slow accumulation of fluid (57). Patients present with paradoxical bradycardia, unlike others with pericardial effusions who usually have tachycardia. Most effusions will resolve gradually after initiation of thyroid hormone replacement therapy. The pericardial fluid obtained is milky-colored, with elevated triglyceride and protein levels. Patients should be given a low-fat or median-chain triglyceride diet, initiated after a period of parenteral nutrition without oral intake to allow resolution of the chylous effusion. Some patients may require palliation with a pericardial window, pericardiectomy, or placement of a pericardioperitoneal or pleuroperitoneal shunt (59,60). Successful use of intravenous octreotide has been reported in some patients with chronic chylous pleural effusions (61). Chest radiograph of an adolescent patient who presented with chest pain after an esophagogastroduodenoscopy procedure. Perforation of the esophagus had occurred, with resultant pneumopericardium evident. Because there is pericardial and pleural inflammation, these patients frequently have pleuritic chest pain. Postpericardiotomy syndrome typically occurs as a single episode, although it can recur weeks to years later. Postpericardiotomy syndrome may produce irritability, malaise, decreased appetite, and arthralgias. While postpericardiotomy syndrome may occur after any cardiac operation, it is most frequent after repair of atrial septal defects, ventricular septal defects, and Tetralogy of Fallot (77). Serum laboratory evaluation may reveal nonspecific inflammatory markers, including elevated erythrocyte sedimentation rate or C-reactive protein, and an elevated white blood cell count. Echocardiography may reveal an effusion, which typically reaches its maximal size by the 10th postoperative day (77). Aspirin is the primary anti-inflammatory medication recommended, in doses as high as 30 to 75 mg/kg/d in four divided doses for 4 to 6 weeks. Patients with recurrent effusions may require pericardiocentesis or pericardiectomy (88,89). Recurrent and Chronic Pericarditis Pericarditis recurs when the underlying disease relapses, or when an effusion reaccumulates after discontinuation of previously effective medical therapy (4,93). Patients have been treated successfully with immune modulators including azathioprine and cyclophosphamide (95). Intravenous immunoglobulin has been reported to be effective in some patients with chronic pericarditis (97). Congenital Abnormalities of the Pericardium Absence of the Pericardium Complete or partial absence of the pericardium is rare. Up to one-third of patients have an associated cardiac defect or pulmonary anomaly, including bicuspid aortic valve, atrial septal defect, patent ductus arteriosus, tetralogy of Fallot, pulmonary sequestration, or bronchogenic cyst (98). Although usually asymptomatic, patients can present with nonspecific symptoms such as dyspnea, light-headedness, and chest pain. Rarely, sudden death occurs due to herniation of the left atrium, left atrial appendage, or right atrium through the defect (99). The diagnosis is not typically made by echocardiography, although unusual scanning windows, cardiac hypermobility, and abnormal ventricular motion may be present (100). This can be performed either by patch closure of the defect, or by enlargement of the defect to prevent incarceration of the herniated tissue. Patients with complete absence of the pericardium usually are asymptomatic and require no treatment (98). Pericardial Cysts Pericardial cysts are congenital anomalies resulting from failure of fetal lacunae to coalesce into the pericardial coelom (101). A cyst can become infected or cause bronchial compression, and the patient may have chest pain, dyspnea, or cough (102,103). Sometimes cysts present as previously unknown masses in the thoracic cavity, and infection or neoplasm must be excluded (104). The superior and inferior vena cavae may be dilated due to elevated ventricular diastolic and central venous pressures. Doppler echocardiography demonstrates marked respiratory variation of both left- and right-sided flows. With inspiration, there is an exaggerated decrease in the mitral inflow velocity (mitral E velocity) and an exaggerated increase in tricuspid inflow velocity (tricuspid E velocity) (109). Conversely, in expiration, there is an exaggerated increase in mitral inflow velocity and an exaggerated decrease in tricuspid inflow velocity. The definitive treatment for constrictive pericarditis is radical pericardiectomy (96,108). Constrictive pericarditis is characterized by a thickened and fibrotic pericardium that restricts ventricular filling. While focal constriction has been reported, the constrictive process usually involves the entire pericardium. Constrictive pericarditis can develop as an idiopathic process, but most commonly represents the end stage of various forms of pericarditis (105,106). With constriction, diastolic expansion of the ventricles is limited causing hemodynamic compromise. Early diastolic filling will be normal, with limited mid and late diastolic filling. Pulmonary wedge and central venous pressures are increased due to elevated ventricular filling pressures (107). Auscultation may reveal a diastolic filling sound corresponding to abrupt cessation of ventricular filling ("precordial knock") (105,108). Chest radiography may be normal or may display pericardial calcification in 25% of patients. Restrictive cardiomyopathy is characterized by markedly abnormal diastolic function with preserved systolic function. The differentiation between constrictive pericarditis and restrictive cardiomyopathy often is difficult (107,112-114). Echocardiographic measurements of diastolic function in children often are confounded by factors including preload, heart rate, age, and body size (115). Differentiating between constriction and restriction is critical, since the definitive treatments for these disorders are markedly disparate (pericardiectomy vs. Cardiac catheterization can be useful in differentiating constriction from restriction. This study only evaluated adult patients and requires validation in a pediatric cohort.
Cheap 12.5mg microzide free shipping
Some studies suggest that in select patients in whom clinical or anatomic concerns are absent by history blood pressure ranges in pregnancy buy generic microzide 25 mg on line, physical exam, and echocardiography, cardiac catheterization may not be necessary prior to stage 2 palliation. Late Fontan Concerns Staged palliation for single-ventricle physiology has undergone a series of surgical revisions that have reduced early postoperative Fontan mortality from 20% to <2% (324,325). Despite the significant morbidities associated with the Fontan operation, overall late mortality (range 4 months to 18 years) continues to decrease from 25% in the early experience to 5% in the recent era (325,326). Over the recent decades, indications for successful Fontan have been modified from the initial "Ten Commandments" described by Choussat and Fontan. From this list, specific physiologic risk factors for a failing Fontan prevail and relate to ventricular performance, atrioventricular and aortic valve function, and pulmonary circulation (328). Ventricular dilation, however, may persist in some patients due to early volume overload, as well the presence of aortopulmonary collaterals that are common in patients with chronic cyanosis. The failing systemic ventricle after staged palliation can be attributed to systolic dysfunction, diastolic dysfunction, or both (329-332). Systolic dysfunction is characterized by reduced contractility and an ejection fraction of <50%. Diastolic dysfunction is more difficult to define, but is evident by increased ventricular end-diastolic pressure and the rate of ventricular relaxation (333,334). As a result, late ventricular dysfunction and subsequent failure of Fontan circulation become clinically evident with symptoms of lower functional class, exercise intolerance, dyspnea, fatigue, and syncope (335, 336). Hypoxemia Slight hypoxemia with Sa0 2 in the low 90s is common after Fontan completion even when residual atrial-level shunts (fenestrations) are absent (321,328). Desaturation also commonly occurs in patients with residual anatomic shunts such as a persistent atrial-level shunt (fenestration) or acquired collateral circulation within the lung. Most collateral vessels originated from the internal mammary arteries and thyrocervical trunk with fewer vessels originating from the brachiocephalic vessels (337). The collateral circulation that forms after Fontan palliation plays no role in gas exchange, produces right-to-left intrapulmonary shunts, and might contribute to progressive ventricular dysfunction as a source of chronic volume overload (338). Hence, the impact of intrapulmonary collateral circulation on oxygen saturation is variable but often most pronounced in the presence of progressive ventricular dysfunction. This elevation in abdominal venous pressures presumably leads to intestinal congestion, lymphatic obstruction, and enteric protein loss (342). Diastolic dysfunction, as mentioned previously, that results in low cardiac output in the face of elevated venous pressures, or even with venous pressures considered normal for Fontan physiology (<15 mm Hg), predisposes the patient to mesenteric ischemia and subsequent intestinal mucosal injury leading to the onset of enteric protein losses (328,342). Thromboembolism Patients with Fontan circulation have a lifelong risk of thromboembolic complications, particularly stroke and pulmonary embolism. In smaller series, the diagnosis of thrombus formation was more common with transesophageal echo with a reported prevalence of 17% to 30% (350). In the past, this sensitization required prospective cross-matching of the donor and recipient in order to find a suitable donor. Currently, the availability and use of the virtual cross-matching technique (373) has eliminated the need for prospective cross-matching. This technique (374) can lead to shorter wait times and better outcomes as a listing strategy for the group of sen~itized patients. In addition, although the sensitized group of patients may have a higher risk of antibody-mediated rejection after transplantation, this also can be monitored carefully post-transplantation by vigilant surveillance for the potential development of donordirected antibodies and by the rapid and early intervention for antibody-mediated rejection if necessary. Several centers have reported their results for heart transplantation in patients with previous Fontan operations. Gamba reviewed results from 1990 to 2002 in 14 patients who underwent heart transplantation after a previous Fontan operation. Michielon evaluated the incremental risk factors for early mortality after heart transplantation. Transition to heart transplantation occurred from a shunt in 10 patients, a bidirectional cavopulmonary anastomosis in nine patients, and after Fontan failure in six patients. Michielon concluded that heart transplantation for patients with single-ventricle physiology is associated with substantial early mortality while the bidirectional cavopulmonary anastomosis provides the best transition to heart transplantation (376). In this study, it should be noted that risk factors for death while waiting for cardiac transplantation included a young age, status 1 listing, shorter interval since the Fontan operation, and the need for mechanical ventilation. Several studies report the presence of arrhythmias at the time of thrombus detection (349-352). Finally, liver dysfunction and coagulation factor deficiency, particularly protein C deficiency, have been identified in patients thought to have good outcomes after the Fontan operation; however, they appear to be time-related phenomena that resolve over time (353,354). The optimal anticoagulation regimen for the patient after the Fontan operation is still unclear and is the subject of current ongoing investigation. Arrhythmias Late atrial arrhythmias have a reported incidence of 10% to 5% in patients with Fontan physiology (326,328,334,335,355). Sinus node dysfunction, the presence of atrial suture lines, and increased atrial pressure have all been implicated in the etiology of late arrhythmias. Several series have reported this outcome with a decreased incidence of atrial tachyarrhythmias or pacemaker insertion for sinus node dysfunction in patients who underwent the extracardiac Fontan when compared to those patients subjected to the lateral tunnel Fontan (312,356,357). Conversely, Cohen reported no early benefit with either approach early after the Fontan operation (314). Actuarial survival of patients who underwent transplant at 1 month, 1, 5, and 7 years was 91 %, 84%, 76%, and 70%, respectively. This actuarial survival did not take into account the group of patients that died prior to an available donor heart. Intermediate-term follow-up of this group of patients has shown good growth and development (360). Evidence of neurodevelopmental delay has been noted in 11 %, with normal psychomotor development in 91 % and a normal developmental index in 96% (360,370). Donor availability continues to be a limiting factor to primary transplantation with the donor shortage resulting in 25% to 30% mortality while on the waiting list. Neurologic outcomes are influenced by patient-related factors as well as preoperative, perioperative, and long-term risk factors. These must be taken into consideration when counseling parents or investigating the causes of an identified delay. Routine developmental screening, beginning at 6 months of age in infants with complex heart disease has been shown to be useful in identifying patients who would benefit from early intervention therapy to reduce delays (402). Eighty-eight percent reported minimal activity limitations and 84% rated school performance as average or above-average. Despite these encouraging parental perceptions, one-third of these children were receiving special education services. Longer waiting time prior to transplantation was found to have a negative effect on later neurocognitive outcomes. Surgical approach, staged palliation versus transplantation, was not associated with any measure of developmental outcome in a group of 47 school-aged children representing four institutions. Wernovsky and Newburger (403) postulated that these similar findings, despite dramatically different treatment strategies, are evidence of the important impact of genetic factors, congenital brain abnormalities and insults incurred during the pre- and perioperative period. In the Pediatric Heart Network cross-sectional study of 537 Fontan survivors at 6 to 18 years of age, parents reported problems with attention in 46%, learning in 43%, development in 24%, and behavior in 23% (398) demonstrating the wide spectrum of neurologic impact of complex heart disease. However, operative factors typically only account for a small portion of the variance in outcomes (241,393,394,404,405). However, the mean scores for each domain were within normal limits for all groups (406). Postoperative Sv02 values <40% were independently associated with poorer developmental outcomes. These studies have evaluated children at multiple different ages and stages of repair. Their findings will serve as a guide for future care and provide important information for counseling children, families, educators, and other health care practitioners. The definition of quality, however, can be provided only by the children and families living the experience. Parents reported that their children had more social problems and decreased activities, and were more withdrawn than healthy children. Teachers also reported children with single-ventricle heart disease to be more withdrawn in the classroom setting.
Order microzide from india
Symptomatic pericarditis with a pericardial effusion occurs usually at times of systemic disease activity with some combination of fever blood pressure chart man generic microzide 25mg free shipping, rash, and arthritis. These children usually develop acute substernal chest pain and difficulty while breathing, especially when lying flat. The children are tachycardic and may have a friction rub at the lower left sternal border on auscultation of the heart, especially if the pericardial effusion is small to moderate in severity. Occasionally there may be minimal associated pericardial fluid, which does not meet echocardiographic criteria for a pathologic effusion. The diagnosis of cardiac tamponade is a clinical diagnosis including elevated neck veins with loss of x and y descents, pulsus paradoxus, tachycardia, and hypotension all of which indicate impaired cardiac output secondary to per~cardial fluid impairing ventricular filling (see Chapter 62, Pericardial Diseases/Effusions). Emergent pericardiocentesis is indicated for cardiac tamponade and can be lifesaving. In 11 of 20 patients with an abnormal echocardiogram, there was no other objective evidence of pericarditis by chest radiograph or electrocardiography. Twenty-one of the sixtyfour (34%) had a pericardial effusion with five having large effusions, eight having moderate effusions, and eight having small effusions. All 13 of the children with large and moderate effusions had symptoms while none of the children with small effusions noted had any symptoms. It may result in heart failure and arrhythmias, which may be a fatal complication. Cardiac manifestations include tachycardia, hypotension, dyspnea secondary to pulmonary edema, abdominal distention secondary to ascites and poor cardiac output, lower extremity edema in older children and teenagers, cool extremities secondary to poor perfusion and low cardiac output, and feeding intolerance in infants. Arrhythmias are rare, but can be life threatening, and may require antiarrhythmic therapy or cardioversion. Rarely, mechanical devices such as intra -aortic balloon pumps or ventricular assist devices may be required to maintain cardiac output until ventricular function improves. The treatment of cardiac tamponade requires an emergency pericardiocentesis to restore adequate cardiac output. If treatment appears prudent, nonsteroidal anti-inflammatory drug therapy such as naproxen (15 mg/kg/day in two doses) or indomethacin (1 to 2 mg/kg/day in two doses) are preferable to corticosteroids. Corticosteroid therapy should start with a 1- to 3-day course of intravenous methylprednisolone at a dose of 15 to 30 mg/kg/dose per day in a single dose. The treatment of myocarditis and endocarditis is similar to the treatment for more severe pericarditis; high-dose corticosteroid treatment with possible remissive therapy. In children with congestive heart failure, angiotensin receptor blockers such as lisinopril are used to improve left ventricular function and reduce ventricular remodeling. It is uncommon in children but with its potential disease severity, must be considered in any child with multisystem disease and no obvious infectious or malignant cause. Patients with lupus comprise only 1% to 5% of the children seen in pediatric rheumatology clinics (21,22). In one study, the onset of lupus in girls under 12 is three times more common than in boys and after 12 years, the girls outnumber the boys by 10:1 (23). For example, it can start with arthritis, rash, serositis including pericarditis, nephritis and/or nephrosis, thrombocytopenia or other cytopenias, vasculitis, central nervous system problems such as seizures and psychosis, and other clinical presentations. Rashes such as the classic malar butterfly rash, a palatal rash or ulcerations, and/or vasculitic lesions on the palms and soles are common. Other typical lupus signs are buccal ulcerations, hair thinning or alopecia, and Raynaud phenomenon. Less common early signs and symptoms might include chest pain due to pericarditis or pleuritis, hypertension, a photosensitive rash, abdominal pain, chorea, or a peripheral neuropathy. Cardiac involvement may not be obvious and the clinician must keep a high level of awareness of potential cardiac complications. Elevated erythrocyte sedimentation rate, polyclonal hypergammaglobulinemia, and elevated (X2-globulins are often seen (35). A urinalysis should be done to check for proteinuria and hematuria, two indicators. It is also prudent to order a chemistry panel of tests to assess liver and renal function. The clinical presentation of pericarditis related to lupus is identical to any other patient presenting with acute pericarditis including substernal chest pain, difficulty lying flat, or pain with inspiration. Nonrheumatic causes are more likely such as viral pericarditis, bacterial and mycobacterial pericarditis, idiopathic pericarditis, and pericarditis associated With tumors. Anterior chest wall pain in children may rrurruc the presentation of pericarditis to some extent. These problems include mild problems such as gastrointestinal reflux, costochondritis, and a pain augmentation syndrome. More senous problems such as pleuritis, pneumonia, pneumonitis, pulmonary embolus, myocardial ischemia or infarction, and pulm<:mary hypertension may present in any lupus patient and mimic symptoms of pericarditis. As ventricular function deteriorates, the patient may develop signs of volume overload such as poor appetite and ability to eat, abdominal distention/ascites, respiratory distress/pulmonary edema or signs of decreased cardiac output such has hypotension, poor perfusion, and narrowed pulse pressure. All layers of the heart may be affected as well as the coronary and pulmonary arteries. When visualized, the lesions are typically tiny irregular vegetations of 2 to 4 mm in diameter that are seen on the valve itself or on the subvalvular apparatus. These patients had no nodules but rather had thickening or stiffness of the aortic or mitral valves that led to regurgitation and rarely, stenosis (51). It is likely that anti phospholipid antibodies have a role in these endocardial lesions resulting in the layering of thrombotic material on the endocardial surface of the heart and valves. Four children had myocardial perfusion scan abnormalities that could be reversed and one child had a fixed myocardial perfusion defect (55). Lipid abnormalities and antiphospholipid antibodies were found in a significant number of the study population. Milder cases may only require the long-term lupus therapy required for other organ systems. Close follow up for cardiac progression, particularly with worsening regurgitation, infective endocarditis, and thromboembolic complications. Valvular disease can also be treated with antiplatelet medication or anticoagulant therapy although there are no large studies looking at antiplatelet therapy versus anticoagulation therapy with warfarin and most data are from small case series or reports (59). Subclinical involvement is common and it is likely that as our tools for detection improve, the degree of pathology found in these patients may increase. It is likely that antiphospholipid antibodies playa role in this pathology as well. There are several contributors to this increased risk including the high rate of dyslipidemia and hypertension as well as decreased flow-mediated dilation (66,67). These heart abnormalities may present simply as dizziness or palpitations but also may lead to sudden death. These children often presented later in the disease course with shortness of breath or overt heart failure. Children with Raynaud phenomenon and anti phospholipid antibodies were more likely to have more severe pulmonary hypertension. Seventy-three of ninety-four cases had the skin rash, which was seen frequently around the eyes, which also involved other areas of skin. Nine cases had structural defects including five with an atrial septal defect, two with ventricular septal defect, and two with enlarged atria. Forty-four of the ninety four patients had hematologic changes including 28 with thrombocytopenia, 11 with leukopenia, and 34 with anemia. Thirty cases had hepatic or splenic issues; 28 with an enlarged liver or spleen, 24 with abnormal liver function tests, 6 with splenomegaly, and 4 with cholestasis. The liver involvement (15% to 25%) may be reflected in elevated liver enzymes and cholestasis. Neurologic abnormalities described include nonspecific white matter changes, calcium deposits in the basal ganglia, hydrocephalus, and blood vessel changes (a vasculopathy). It was difficult to detect the first-degree heart block in these fetuses using echocardiography. Many of the children with complete heart block require pacemakers; however, some patients will resolve their heart block and not require pacemaker placement. The timing of pacemaker placement is critical as transvenous systems cannot be placed until the child is older. In infants requiring pacemaker placement, the procedure is more invasive requiring epicardial placement of the leads with the generator being placed in the abdominal wall.
Purchase 25mg microzide with amex
Specialty-specific Challenges Equipoise and Execution the logistics of designing and executing a clinical trial are often greater than those of performing an observational study blood pressure medication for cats buy microzide 12.5 mg. Equipoise must exist at the beginning and throughout the study period, meaning that the investigators must be convinced that there is insufficient evidence regarding the superiority or equivalency of one intervention over another or standard of care, otherwise it would be unethical to withhold the superior intervention from subjects. There are a number of challenges regarding clinical trials specific to pediatric and congenital cardiology and cardiovascular surgery, as outlined in Table 78. One of the major advances in overcoming some of these obstacles was the funding and formation in 2001 of the Pediatric Heart Network by the U. The Pediatric Heart Network is a consortium of leading North American pediatric cardiology programs, together with a data coordinating center, aimed at performing multi-institutional studies, and has successfully completed some landmark clinical trials(6-9). Errors in the execution can influence the degree to which the findings from Feasibility A major factor that keeps many important clinical trials from being performed is lack of feasibility. The degree to which the actual findings can be inferred to reflect the truth in the designed study reflects internal validity. Errors in the design can influence the degree to which the findings can be inferred to reflect the actual truth or the answer to the research question, which is referred to as external validity. These studies are meant to satisfy regulatory requirements for industry prior to marketing a drug or device, and are used to inform clinical recommendations and evidencebased practice. These trials are powered to detect a clinically meaningful impact on an outcome that is immediately relevant to the patient, such as mortality, symptomatic morbidity, and functional health or quality of life. They are aimed at monitoring the incidence of adverse events, particularly those that are rare, and to determine long-term effectiveness and safety. Questions, Hypotheses, and Aims intervention and determining feasibility, to more definitive determinations of efficacy, effectiveness, and safety. Each phase provides preliminary data and evidence to inform the next phase, creating a body of evidence that will eventually inform recommendations and evidence-based clinical decision making. These phases are particularly applicable to interventions involving investigational new drugs and devices, and proceed in a defined sequence, as noted in Table 78. The aims of each phase are different, and inform the choice of approach and study design. Given that large scale efficacy and effectiveness trials are risky endeavors, these phases help to ensure that sufficient rationale and preliminary data inform their design and execution. Phase I studies are usually the bridge from experiments in animal models to human subjects. Phase I studies are usually not randomized or controlled (no comparison group), are small in scale, and are aimed at determining short-term safety and tolerability, dosing (including the maximally tolerated dose and toxicity) and administration through pharmacodynamic and pharmacokinetic testing, and preliminary results regarding effectiveness. A focused question will define the study population, the intervention and comparison, and the primary outcome for the clinical trial. The process of specification of the question forms the rationale for the clinical trial that is proposed. A wellconceived background to a proposal also represents the starting point for the discussion section of a manuscript once the study results are determined. In outlining these sections, one usually begins by defining the broad topic area, and then honing down to the specific area of controversy or uncertainty. The rationale is provided from both the published literature and preliminary work by the investigators. The rationale should lead directly to a statement of the research question (stated as a question), which leads to a statement of the primary aim of the trial (the question rephrased as an action item). The relevance and significance of the question being pursued is another important aspect of the rationale. There are many dimensions to relevance and significance, which can be qualitatively or quantitatively supported. The answer may provide evidence leading to further lines of inquiry, may impact the care of patients, leading to reductions in disease burden or risk, or improvements in patient level outcomes, or may inform clinical recommendations, guidelines, or health policy. It should ideally be based on knowledge of the published literature and preliminary work and, hence, be an informed guess. The hypothesis should be specified at the same time that one poses the study question, which should be before any data are collected. Study aims represent the main and secondary study questions, but are rephrased as an action item. The primary study aim should include the defining characteristic of the study population, the intervention and comparison being studied, and the primary outcome (the main or most important outcome). Secondary aims are usually structured around subgroup comparisons, other types of outcomes, and mechanistic explorations. Secondary aims and hypotheses should be relevant to the primary aim, but provide a greater degree of breadth and depth to the study, which can increase the relevance and significance of a trial. Primary and secondary outcomes should be clearly specified and justified and relate directly to the study aims and underlying research questions. In the design phase of clinical trial development, much consideration is usually given to choosing the primary outcome. A hypothesis regarding the differential impact of the study interventions on the primary outcome informs the sample size calculations specifying the number of subjects required. Secondary outcomes are outcomes of interest that may be related to the primary outcome, either by association or informing a mechanistic relationship. The most common secondary outcomes are measures of adverse effects or events, pathophysiologic parameters, or health care system factors, such as utilization or costs. All aspects of the intervention and its application (what, how, when, where, who) should be considered and exactly specified in advance. In pediatric trials, particular attention should be given to dosing and formulation, and to monitoring for adverse effects. The specification of the interventions should be such that they can be replicated and applied in further studies, adapted to different populations and scenarios, or implemented in clinical practice. If aspects of the application of the intervention are likely to be influencers of outcomes or to un blind the allocation assignment, then precautions should be taken to have as many aspects as possible replicated identically for the comparison. This may include identical formulation and application of study drug and placebo, or the use of sham procedures. Often, particularly for pediatric patients, the undue burden of taking placebo or undergoing sham procedures cannot be supported due to ethical concerns. Some clinical trials aim to determine if one intervention is better or safer than either usual or standard care, placebo or nonintervention, or an alternative study intervention (superiority trial). These trials are relevant when a new intervention has advantages over an established or alternative intervention (reduced costs, greater availability, improved feasibility, better tolerance, and acceptability) but there is a need to establish that outcomes will be at least equivalent and noninferior. The threshold for defining noninferior depends on the advantages of the new intervention, and there may be a trade-off for accepting some decrease in efficacy. It is characterized by subjects being recruited and randomized concurrently to only one of either an intervention or comparison, and followed concurrently to a specified single study end point. Crossover clinical trials are a variation of the parallel group design whereby subjects are first randomized to either the intervention or comparison for a specified period of time, and then reassigned to the opposite of the initial allocation for a second specified period of time. It allows each subject to receive both intervention and comparison in randomized order. It is often used when the number of study subjects is limited and when the outcomes occur over a relatively short period of time. It allows both within group and between group comparisons, with each subject acting as their own control or comparison, which also helps to minimize bias and allows for paired analyses. Besides increased logistical issues, one of the major limitations of this design is the problem of dropouts, since the subjects are followed longer, have increased exposure to adverse effects, and may not wish to continue with a second period of possible placebo or a less-desirable alternative. Another limitation is the potential for carryover effects, whereby the effects of the initial intervention continue to operate over the second period to influence outcomes. A factorial design allows the study of more than one intervention together (interaction) as well as separately (independent). The least complex factorial design randomizes subjects to one of four groups-neither intervention (comparison), both interventions, and each intervention separately-and is called a 2 x 2 factorial design. These aspects can have important impacts on the validity of the results and their generalizability, and are outlined in Table 78. Definition of the study population begins with examination of the aims and hypotheses of the clinical trial. One wishes to infer that the results of the trial for those subjects studied will be representative of the truth if the trial had been performed in the universe of potential subjects, or the target population. Of the accessible population, some subjects cannot be contacted, will prove not appropriate for study, may decline to participate or may start but not complete their participation, and represent the actual study subjects. The degree to which, at each stage, the subjects are similar to the target population will inform the validity of inferences based on the results from the actual study subjects.