Safe amoxicillin 1000 mg
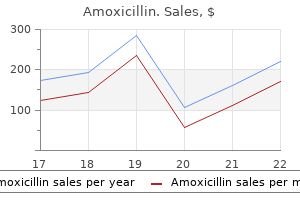
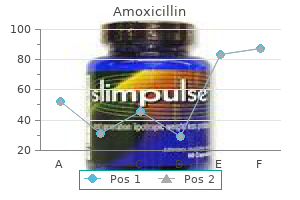
Intraoperatively medicine abbreviations amoxicillin 1000mg amex, a minimally invasive surgical approach is employed whenever possible. Endorgan function is optimized through a goal-directed fluid management strategy involving noninvasive cardiac output monitoring. The mortality rate for radical cystectomy with diversion is approximately 1%, and perioperative complications are common (27. Specific Procedures Partial Cystectomy Nonmalignant indications for partial bladder resection include bladder endometriosis and benign tumors. Whenever partial cystectomy will suffice, the effects of added surgery and poorer quality of life associated with a urinary diversion procedure can be eliminated; hence the current interest in methods to identify bladder cancer patients for whom partial cystectomy with pelvic lymph node dissection may be as good a treatment as radical cystectomy. Selective bladder-sparing protocols that use responsiveness of a tumor to chemotherapy and radiation therapy as a guide to surgical decision making appear to successfully identify about one-third of 3561 the patients whose long-term outcome with partial cystectomy is equivalent to radical cystectomy, without the need for a diversion procedure. Radical cystectomy involves resection of the bladder and related pelvic structures, including pelvic lymphadenectomy of obturator and iliac nodes. In the male, the bladder is removed en bloc with pelvic peritoneum, prostate and seminal vesicles, ureteric remnants, and a small piece of membranous urethra. In the female, the uterus, ovaries, fallopian tubes, vaginal vault, and urethra are removed. Alternate terminology to radical cystectomy for these major procedures include radical cystoprostatectomy in men and radical cystectomy with pelvic exenteration in women. Ileal Conduit and Other Diversion Procedures the concept of ileal conduit surgery is relatively straightforward, involving creation of an ileal pouch that is attached to both ureters and the abdominal wall as a stoma. In contrast, continent diversion procedures are numerous and diverse in their approaches to urine collection and drainage. Continent urinary diversions can be categorized into (1) ureterosigmoidostomy, (2) continent cutaneous diversions, and (3) neobladder diversions to the native urethra. Continent cutaneous reservoirs resemble ileal conduit surgery, but the stomal attachment to the abdominal wall is modified to produce a valve mechanism, with urine drainage achieved by intermittent catheter drainage. Many continent cutaneous variants exist that involve the use of different bowel segments as the source for the reservoir. Finally, continent orthotopic diversions involve neobladder construction from terminal ileum, cecum, or sigmoid colon, which is attached to proximal urethra and its intact rhabdosphincter mechanism. Notably, all urinary diversion procedures involve extensive dissection and are considerably more challenging if the patient has received preoperative radiation therapy. Complications of urinary diversion surgery include bowel obstruction, urinary tract infection, deep venous thrombosis and pulmonary embolism, pneumonia, upper urinary tract damage, and skin breakdown around the stoma. After recovery, patients with urinary diversions are vulnerable to 3562 conditions that require subsequent surgeries; these include problems at the stoma site. Anesthetic considerations for patients who present with existing diversion procedures include metabolic and electrolyte abnormalities such as hyperchloremic metabolic acidosis (common), hypokalemia, hypocalcemia and hypomagnesemia, and high rates of urinary tract infection and pyelonephritis. In addition, these individuals frequently suffer from chronic diarrhea and may have problems related to malabsorption. Although prostate cancer is a disease limited to men, it is the second most common cancer in most countries, with an incidence that increases significantly with age and is approximately 50% more common in AfricanAmerican men than in Caucasian men. A second related concept is also emerging-that prostate cancer may exist in clinically significant (approximately 15%) and insignificant forms. Prostatectomy can be performed using retropubic or perineal approaches and is amenable to endoscopic techniques with or without robotic assistance. The retropubic approach requires the patient to be supine with the bed extended and in Trendelenburg position. This allows access to the prostate gland and related lymph nodes from behind the pubic symphysis (and the best chance of sparing the neurovascular bundle), using either a vertical midline or Pfannenstiel (horizontal low suprapubic) incision. In contrast, the perineal approach requires the patient to be in exaggerated lithotomy and steep Trendelenburg position. Preoperative Considerations Beyond advanced age, relatively few factors predict likelihood of contracting prostate cancer. Family history more than doubles the chances of the disease, while African-American descent increases the risk by approximately 50%. Otherwise, factors such as smoking, obesity, diet, history of vasectomy, prostatitis, or sexually transmitted diseases have little or no effect on prostate cancer risk. Owing to the advanced age of the population presenting for prostatectomy, an emphasis on comorbid disease in preoperative evaluation is particularly relevant. Paraneoplastic syndromes similar to those seen with kidney cancer are occasionally evident in prostate cancer patients. Intraoperative Considerations Anesthetic management for open prostatectomy is similar to that for cystectomy surgery (see earlier), including attentiveness to the potential for major bleeding. Epidural catheter placement is usually in the low thoracic spinal region, guided in part by the chosen option for anesthesia, including spinal/epidural alone, general alone, or combined spinal/epidural and general anesthesia. A surgical block to at least the T10 level is required for procedures 3564 performed using neuraxial block alone. In one study, patients experienced 33% less pain when preemptive epidural dosing occurred prior to incision. Notably, a neuraxial-alone strategy for perineal prostatectomy is likely to be poorly tolerated owing to the uncomfortable exaggerated lithotomy and headdown positioning requirements. Exaggerated lithotomy position for prostatectomy has also been associated in some studies with higher rates of neurologic injury (21% with transient sensory or motor deficit); patients appear to be at greater risk when surgery lasts longer than 180 minutes. As with cystectomy, the approach to intravascular volume assessment during prostatectomy must consider the potential for bleeding and hypovolemia and limited meaningful urine output data; the need for arterial and/or pressure central venous monitoring should be guided by patient comorbidities. Neuraxial anesthesia for prostatectomy has been associated with decreased blood loss in some studies. Nonetheless, most radical prostatectomy patients are not admitted to an intensive care unit. Average blood loss for radical prostatectomy is between 500 and 1500 mL,186 and approximately 10% of patients will require a perioperative blood transfusion. Impaired lymph drainage (lymphocele, leg edema) is associated in some studies with increased rates of postoperative deep venous thrombosis and pulmonary embolism. Currently, retropubic prostatectomy is the most common approach in the United States. Radical Prostatectomy Radical prostatectomy involves removal of the entire prostate gland, seminal vesicles, and generally the surrounding nerves and veins. Preservation of one or both cavernous nerves (part of the neurovascular bundle on each side of the prostate) can improve postsurgery quality of life. Notably, the incidence of positive margins with tumor resection during radical prostatectomy is significant (30%). The value of more aggressive resection with sural nerve grafting to address erectile dysfunction remains unclear. Laparoscopic and Robotic Prostatectomy Minimally invasive laparoscopic and robotic-assisted approaches to prostatectomy are gaining popularity (see Chapter 44). Although these techniques are characterized by less pain, shorter hospital stays, faster recovery, and improved patient satisfaction,192 they also present added challenge for the anesthesiologist, including prolonged procedure duration, the risk of hypothermia, occult blood loss, and the physiologic stresses of pneumoperitoneum and exaggerated Trendelenburg with or without lithotomy positioning. Laparoscopic and robotic prostatectomy procedures require general anesthesia with endotracheal intubation. Standard monitoring and adequate intravenous access must be established prior to patient positioning because 3566 access after positioning is very difficult. Pulse oximeter probe placement should avoid the earlobe to anticipate the potential for inaccurate readings in this location, presumably related to the venous engorgement with head-down positioning and pneumoperitoneum. As with all robotic surgeries, because of the fixed position of the robot arms, movements such as coughing can cause injury internally or at port sites, so care must be taken to maintain adequate depth of anesthesia and neuromuscular blockade. Exaggerated Trendelenburg positioning is required for the procedure, and some practitioners deliberately refrain from dosing epidural catheters to avoid cephalad spread of epidural drugs during the procedure. Steep Trendelenburg positioning (30 to 45 degrees head-down) to facilitate pelvic access during laparoscopic and robotic prostatectomy increases the risk of several important complications. Arms should be placed on angled armboards prior to lowering the end table section during lithotomy positioning to minimize the risk of pinched or crushed fingers. Beyond brachial plexus protection with shoulder padding, attention should be paid to radial (at the humerus), ulnar (at the elbow), and lateral femoral cutaneous (by the lithotomy leg holders) nerves to minimize axonal injuries. Finally, because oral ulceration and even conjunctival burns have been attributed to lithotomy-related reflux of gastric contents, steps such as preoperative antacid therapy, stomach drainage by orogastric tube, and waterproof eye taping should all be considered. Lack of easy access to the patient is a concern during robotic prostatectomy, primarily caused by the sheer size of current robot arms.
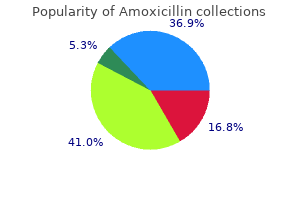
Order amoxicillin master card
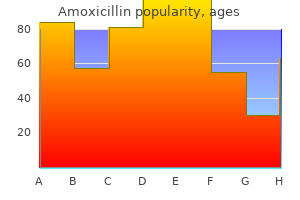
Insulin and dextrose can be repeated two or three times at 30- to 45-minute intervals medications known to cause weight gain order online amoxicillin, if necessary. The differential diagnosis between hypovolemic, diabetic, and alcoholic acidosis, all of which have anion gaps, requires measurement of blood lactate, urinary ketone bodies, and blood sugar and assessment of intravascular volume. Alcoholic ketoacidosis is treated with intravenous dextrose, whereas diabetic ketoacidosis is managed with insulin. No specific treatment except intravenous normal saline exists for alcoholic lactic acidosis. Symptomatic treatment with sodium bicarbonate has serious disadvantages, including leftward shift of the oxyhemoglobin dissociation curve causing decreased O2 unloading, a hyperosmolar state secondary to the excessive sodium load, hypokalemia, further hemodynamic depression, overshoot alkalosis a few hours after giving the drug, and intracellular acidosis if adequate ventilation or pulmonary blood flow cannot be provided. Nevertheless, because of the possibility that severe acidosis can cause dysrhythmias, myocardial depression, hypotension, and resistance to exogenous catecholamines, some clinicians administer bicarbonate to buy time if the pH is below 7. Intraoperative Death Death is a much greater threat during emergency trauma surgery than it is in any other operative procedure. The damage control principle, originally proposed for abdominal trauma, is now applied to injuries at other anatomic sites, including chest, pelvis, extremities, and soft tissues. Postoperative care may involve obtaining a further medical history and description of the mechanism of injury from the patient, if he or she is awake, or from relatives, and performing tertiary survey to identify possible missed injuries. The concerns in the early postoperative period are similar to those of the intraoperative phase. Pain control in this group of patients may have more than a humanitarian purpose; it can improve pulmonary function, ventilation, and oxygenation, especially in patients with chest and abdominal injury. A multidimensional pain control strategy may be used, including various combinations of regional analgesia, if coagulopathy is not a concern; intravenous opioids as patient-controlled analgesia or as bolus doses; nonsteroidal anti-inflammatory agents, if nephrotoxicity, gastric ulceration, or bleeding risks do not exist; acetaminophen; and low-dose (20 to 30 mg/hr) ketamine, particularly in patients with a known history of opioid. For sedation in mechanically ventilated patients, both propofol (25 to 75 g/kg/min) and midazolam (0. Small boluses of midazolam (3 to 5 mg), propofol (50 mg), morphine (2 to 3 mg), or fentanyl (25 to 50 g) may also be given as required. In a study aimed at finding the predictors of acute renal failure, trauma was one of the seven independent predictors of this complication. Decreased urine flow rate alone is not a good predictor, and the blood urea nitrogen does not rise until at least 24 hours after surgery or trauma. They are comparable in their ability to differentiate the type and severity of kidney injury. Serum creatinine kinase levels increase in these patients; levels above 5,000 units/L are associated with renal failure. A clear supernatant suggests myoglobin, whereas a rose color indicates hemoglobin. The traditional prophylaxis for renal failure after rhabdomyolysis includes fluids, mannitol, and bicarbonate. Depending on the severity of kidney injury a nephrology consultation and renal replacement therapy is indicated. Abdominal Compartment Syndrome Abdominal compartment syndrome results from intra-abdominal hypertension with organ dysfunction after major abdominal trauma and surgery (primary syndrome), although other patients may develop the syndrome without surgery, for example, during massive fluid resuscitation following major trauma or burns (secondary syndrome). Values above 20 to 25 mmHg may indicate inadequate organ perfusion and necessitate abdominal decompression, which, if delayed, may result in progression to multiorgan failure and death. Image in the center is a patient whose abdomen was left open but covered with nonadhesive dressing. In other words, unlike in the past, intra-abdominal hypertension is seldom a harbinger of abdominal compartment syndrome or multiorgan failure. It is believed that limiting crystalloid infusion is the most important factor in this salutary evolution. Venous thromboembolism in patients with blunt trauma: are comprehensive guidelines the answer In hemodynamically unstable patients, resuscitation takes precedence over radiologic diagnosis. Management is symptomatic and includes tracheal intubation, positivepressure ventilation with FiO2 of 1. These patients were managed using the clinical management guidelines recommended by the Eastern Association for the Surgery of Trauma. Removable vena cava filters are now available and are likely to be used prophylactically in high-risk patients more often than permanent filters, which are associated with long-term 3833 complications. In patients with severe hemodynamic depression or cardiac arrest unresponsive to resuscitative measures, thrombolytic agents may be considered despite the risk of hemorrhage. Comparison of mannitol and hypertonic saline in the treatment of severe brain injuries. The relationship between mortality and preexisting cardiac disease in 5,971 trauma patients. A,B,C,D, echo: limited transthoracic echocardiogram is a useful tool to guide therapy for hypotension in the trauma bay: A pilot study. Damage control radiology in the severely injured patient: What the anesthetist need to know. Prospective evaluation of early missed injuries and the role of tertiary truama survey. Total intravenous anesthesia including ketamine versus volatile gas anesthesia for combat-related operative traumatic brain injury. Effect of video laryngoscopy on trauma patient survival: A randomized controlled trial. National Emergency X-Radiography Utilization Study criteria is inadequate to rule out fracture after significant blunt trauma compared with computed tomography. Absence of clinical findings reliably excludes unstable cervical spine injuries in children 5 years or younger. Outcomes of pediatric patients with persistent midline cervical spine tenderness and negative imaging result after trauma. Flexion and extension views are not cost-effective in a cervical spine clearance protocol for obtunded trauma patients. Spinal cord injury without radiologic abnormality in children: A systematic review and meta-analysis. Comparative effectiveness of using computed tomography alone to exclude cervical spine injuries in obtunded or intubated patients: Meta-analysis of 14,327 patients with blunt trauma. Cervical spine collar clearance in the obtunded adult blunt trauma patient: A systemic review and practice management guideline from the Eastern Association for the surgery of trauma. Advocating policy with patient safety in the balance: the case of cervical spine clearance. Utility of magnetic resonance imaging in diagnosing cervical spine in children with severe traumatic brain injury. Manual in-line stabilization increases pressures applied by the laryngoscope blade during direct laryngoscopy and orotracheal intubation. Cervical spinal motion during intubation: Efficacy of stabilization maneuvers in the setting of complete segmental instability. Motion of cadaver model of cervical injury during endotracheal intubation with a Bullard laryngoscope or a Macintosh blade with and without in-line stabilization. Management of maxillofacial injuries with severe oronasal hemorrhage: A multicenter perspective. Transcatheter arterial embolization in the treatment of maxillofacial trauma induced life-threatening hemmorrhages. Utilization of tracheostomy in craniomaxillofacial trauma at a level-1 trauma center. Anesthetic management of complete tracheal disruption using percutaneous cardiopulmonary support system. Airway management following repair of cervical tracheal injuries: A retrospective, multicenter study. Acute tracheoesophageal burst injury afteer blunt chest trauma: Case report and review of the literature. Incidence, risk factors, and outcomes for occult pneumpthoraces in victims of major trauma. Pulmonary contusion: An update on recent advances in clinical management World J Surg. Critical evaluation of pulmonary contusion in the early post-traumatic period: Risk of assisted ventilation.
Syndromes
- General paresis
- Have you noticed an increase in anxiety?
- Folicle stimulating hormone (FSH)
- Deep vein thrombosis (blood clots that form when someone is inactive or confined to bed)
- Vaginal dryness
- Inspect all the tissues of your shoulder joint and the area above the joint -- the cartilage, bones, tendons, and ligaments.
- Agitation
Discount generic amoxicillin uk
The timed symptoms bipolar purchase amoxicillin toronto, or programmed intermittent epidural bolus technique is a new method for maintaining epidural analgesia. In this technique, the pump is programmed to deliver a bolus dose at regular intervals. Presumably, the bolus administration of drugs into the epidural space results in better distribution of the drug solution. Before ambulation, women should be observed for 30 minutes after initiation of neuraxial blockade to assess maternal and fetal well-being. During delivery, the sacral dermatomes may be blocked with 10 mL of bupivacaine (0. Many parturients have adequate analgesia for delivery without an additional bolus dose, particularly if epidural analgesia has been maintained for a long interval (hours). However, instrumental vaginal delivery may require a denser block than that obtained with dilute local anesthetic solutions. Spinal analgesia with fentanyl (15 to 25 g) or sufentanil (2 to 5 g) in combination with plain bupivacaine (1. A potential disadvantage of single-shot spinal analgesia is that the duration of labor, even in a rapidly progressing multiparous woman, may be longer than anticipated. Furthermore, if the woman requires an urgent cesarean delivery, a new anesthetic will need to be initiated. However, spinal anesthesia (a "saddle block") is a safe and effective alternative to general anesthesia or pudendal nerve block for instrumental delivery in parturients without pre-existing epidural analgesia. After identification of the epidural space using a conventional (or specialized) epidural needle, a longer (127 mm), pencilpoint spinal needle is advanced into the subarachnoid space through the epidural needle. After intrathecal injection, the spinal needle is removed and an epidural catheter is inserted. Intrathecal injection of fentanyl (10 to 25 g) or sufentanil (2 to 5 g) alone or more commonly in combination with bupivacaine (1. Spinal opioid alone provides complete analgesia for the early latent phase of labor. However, the addition of bupivacaine is necessary for satisfactory analgesia during advanced labor. The most common side effects of intrathecal opioids are pruritus, nausea, vomiting, and urinary retention. The incidence of pruritus is lower if opioid is coadministered with local anesthetic. Presumably, uterine 2859 tachysystole and decreased uteroplacental perfusion occur as a result of rapid decrease in circulating maternal epinephrine levels after initiation of analgesia or as a result of hypotension after sympatholysis. Spinal opioid provides complete analgesia without the need for local anesthetic in early labor, thus avoiding an acute decrease in preload, and almost always allowing motivated women to ambulate because there is no motor block. The onset of sacral analgesia is accomplished significantly faster with much less drug than initiation of lumbar epidural analgesia. Five to ten milliliters of dilute local anesthetic solution is injected submucosally via a needle guide in the vagina into the left and right lateral vaginal fornices. Although paracervical block effectively relieves pain during the first stage of labor, the technique has fallen out of favor during childbirth because it is associated with a high incidence of fetal asphyxia and poor neonatal outcome, particularly with the use of bupivacaine. Performing the block with dilute local anesthetic solutions, allowing 5 to 10 minutes to elapse between injections on the left and right sides, and limiting the block to women with less than 8 cm cervical dilation, may decrease the incidence of complications. Pudendal Nerve Block the pudendal nerves, derived from the sacral nerve roots (S2 to S4), supply the vaginal vault, perineum, rectum, and parts of the bladder. The nerves are easily anesthetized transvaginally where they loop around the ischial spines. Ten milliliters of dilute local anesthetic solution deposited behind each sacrospinous ligament can provide adequate anesthesia for outlet forceps delivery and episiotomy repair. Inhalation Analgesia and General Anesthesia Inhalation labor analgesia is uncommon in the United States, although its use is more common in other parts of the world (see Chapter 18). Nitrous oxide, 50% by volume, is the most commonly used inhalation agent for analgesia during labor. The mother is trained to intermittently self-administer the gas at the onset of a contraction. Studies are conflicting as to whether nitrous oxide provides benefit to the parturient; its safety for the fetus and the neonate has also not been well studied. General anesthesia is rarely used for vaginal delivery, and precautions against gastric aspiration must always be observed (see General Anesthesia in the section Anesthesia for Cesarean Delivery). General anesthesia may be required when time constraints prevent induction of regional anesthesia. However, in current practice, intravenous nitroglycerin (50 to 250 g) has largely replaced the need for general anesthesia for uterine relaxation. Anesthesia for Cesarean Delivery the most common indications for cesarean delivery include arrest of dilation, nonreassuring fetal status, cephalopelvic disproportion, malpresentation, prematurity, prior cesarean delivery, and prior uterine surgery involving the corpus. A 2001 survey of obstetric anesthesia practices in the United States revealed that most patients undergoing cesarean delivery do so under spinal or epidural anesthesia. Neuraxial Anesthesia Blockade to the T4 dermatome is necessary to perform cesarean delivery without maternal discomfort. The most common complication of neuraxial anesthesia is hypotension and the attendant risk of decreased uteroplacental perfusion (see Hypotension in the section on Anesthetic Complications). Measures to decrease the incidence and severity of hypotension include left uterine displacement, intravenous fluid administration, and the liberal use of vasopressors to prevent and treat hypotension. Most anesthesiologists administer a nonparticulate antacid before induction of anesthesia for pulmonary aspiration prophylaxis. Intraoperative monitoring mimics that for all anesthetics, although blood pressure should be measured frequently (every several minutes) for the first 20 minutes after initiation of anesthesia. Although supplemental oxygen is frequently administered, there is no evidence of benefit to the mother, the fetus, or the neonate. Although postcesarean delivery analgesia should take the nursing infant into account, very small amounts of drugs administered to the mother actually cross into breast milk, and even smaller amounts are absorbed from the neonatal gut. Prolonged (12 to 24 hours) postoperative pain relief in the postpartum patient can be provided by intrathecal morphine (100 to 150 g)74 or epidural morphine (3. Delayed respiratory depression is a rare but potentially devastating complication; therefore, patients who receive neuraxial opioids must be monitored carefully in the postoperative period. Spinal Anesthesia Subarachnoid block is probably the most commonly administered neuraxial anesthetic for cesarean delivery because of its simplicity, speed of onset, and reliability. It is an alternative to general anesthesia for almost all but the most emergent of cesarean deliveries. Despite an adequate dermatomal level for surgery, women may experience varying degrees of visceral discomfort and nausea and vomiting, particularly during exteriorization of the uterus and traction on abdominal viscera. Improved perioperative anesthesia and analgesia can be provided with the addition of fentanyl (10 to 20 g), sufentanil (2. Fentanyl has a rapid onset, but is short acting and provides little additional postoperative analgesia. In contrast, morphine has a longer latency than fentanyl, but will also provide anesthesia for 12 to 18 hours after delivery. Lumbar Epidural Anesthesia In contrast to spinal anesthesia, epidural anesthesia is associated with a slower onset of action and a larger drug requirement to establish adequate sensory block. The major advantages of epidural compared with single-shot spinal anesthesia are the ability to titrate the extent and duration of anesthesia. To avoid unintentional intrathecal or intravascular injection, correct placement of the epidural needle and catheter is essential. This is especially true because epidural anesthesia for cesarean delivery necessitates the administration of large doses of local anesthetic. Aspiration of the epidural catheter for blood or cerebrospinal fluid is not reliable for detection of catheter misplacement, particularly with singleorifice catheters. Thus, most anesthesiologists administer a test dose before the initiation of surgical anesthesia. Addition of epinephrine (15 g) with careful hemodynamic monitoring may signal intravascular injection if followed by a transient increase in heart rate and blood pressure. The use of an epinephrine test dose (15 g) in obstetrics is controversial because false positive results do occur (10% increase in heart rate), especially in laboring women. Rapid 2863 injection of 1 mL of air with simultaneous precordial Doppler monitoring appears to be a reliable indicator of intravascular catheter placement. The most commonly used agents for obstetric epidural anesthesia are 2% lidocaine with epinephrine, 5 g/mL (1:200,000) and 3% 2-chloroprocaine. Adequate anesthesia is usually achieved with 15 to 25 mL of local anesthetic solution, administered in divided doses over 5 to 10 minutes.
Purchase amoxicillin 250 mg with amex
Oral Routes Oral routes of medications have been used for decades in neonates and children for managing pain moroccanoil treatment order 650 mg amoxicillin with amex. The commonly used oral analgesics include 2983 nonsteroidal analgesics including acetaminophen (10 to 15 mg/kg) and ibuprofen (5 to 10 mg/kg), and opioids, including hydrocodone (0. There may be some pharmacogenetic changes associated with the use of codeine in infants; thus, it is falling out of favor in use across all ages. A larger dose than is usually given orally is needed in infants to achieve good blood levels, because of unreliable absorption. A dose of 20 to 30 mg/kg of rectal acetaminophen is generally recommended for postoperative pain control. Diclofenac, a commonly available rectal suppository in Europe, is frequently used in infants for postoperative pain control. Intravenous Analgesia Opioids are the mainstay of analgesia in neonates and infants in the postoperative period. Morphine and fentanyl are frequently used in the neonatal intensive care unit for analgesia. However, the potential for opioid tolerance after prolonged infusion of opioids is somewhat common. To decrease the likelihood of opioid tolerance,44 one can rotate opioids or add other medications including continuous intravenous naloxone142 and intravenous methadone. Other intravenous nonsteroidal anti-inflammatory medications and intravenous acetaminophen, have been introduced. Intravenous ketorolac, a nonsteroidal anti-inflammatory drug, has been used successfully 2984 in neonates and infants for pain control at a dose of 0. However, if the surgical procedure is relatively short and by itself does not require postoperative ventilation, the clinician should carefully select drugs, as well as doses of anesthetic drugs and relaxants, that will not necessitate prolonged postoperative ventilation or intubation. Postoperative ventilation places the neonate at added risk because of the problems associated with mechanical ventilation, the trauma to the subglottic area, and the potential development of postoperative subglottic stenosis or edema. Special Considerations Maternal Drug Use during Pregnancy Many drugs taken during pregnancy can affect the fetus and neonate. During pregnancy, maternal drug use of cocaine, marijuana, and others leads to a host of problems for the neonate. Cocaine use, for instance, results in a reduced catecholamine reuptake, which may result in the accumulation of catecholamines. This accumulation has circulatory effects on the uterus, the umbilical blood vessels, and the fetal cardiovascular system. Three major problems affecting the infant are premature birth, intrauterine growth retardation, and cardiovascular abnormalities, including low cardiac output. The clinical implication of this finding is that these neonates may be unstable enough in the first day of life that it may be advantageous to postpone surgery, if possible, until the second or third day of life. There is also an increase in structural cardiovascular malformations and electrocardiographic abnormalities. Temperature Control and Thermogenesis the newborn is at risk for significant metabolic derangements caused by hypothermia. Newborns, and especially preterms, do not have the normal compensatory mechanisms that infants and children have when exposed to a cold environment. The newborn does not shiver, increase activity, or effectively vasoconstrict like older children or adults do in response to cold. In addition, the newborn has a larger body surface area-to-weight ratio that promotes heat loss, as well as low levels of subcutaneous fat for insulation. The primary mechanism the newborn has to respond to heat loss is nonshivering thermogenesis. Norepinephrine stimulates increased metabolism in a specialized tissue, brown fat, which contains a high concentration of mitochondria and has abundant vascular supply. Stimulated lipolysis results in heat production, with side effects of increased oxygen consumption and production of ketone bodies and water. The aerobic activity results in diversion of cardiac output to the deposits of brown fat around the kidneys, under the sternum, and between the scapulae. Because the diuresis, diversion of cardiac output away from the core circulation, and metabolic acidosis are maladaptive, every effort should be made to prevent nonshivering thermogenesis in the newborn. Efforts to minimize nonshivering thermogenesis in the newborn are based on minimizing heat loss, both during transport to and from the neonatal intensive care unit and in the operating room. Transport should be done with the newborn in an incubator or in an open bed with overhead heaters. In the operating room, the room temperature is raised to its maximal level to minimize loss by conduction. Placing the patient on a forced-air warming blanket can reduce conductive heat loss. Using plastic wrap or commercially available covers and hats to minimize heat loss from the head and all other areas not in the surgical field is also beneficial. The goal of all these activities is to maintain a neutral thermal environment, minimizing the stress that hypothermia can induce in the perioperative period. A complicating factor is that anesthetic agents can reduce or eliminate thermogenesis, removing any ability to compensate for cold stress. Characteristics include airway smooth muscle hyperplasia, peribronchiolar fibrosis, enlarged alveoli, and disorganized pulmonary vasculature. Many patients improve as they age, but reactive airways, recurrent pulmonary infections, and a prolonged oxygen requirement are seen in some patients. Anesthetic concerns in these patients include evaluation of baseline oxygenation and potential presence of active bronchoconstriction. These patients often benefit from prophylactic bronchodilator therapy before induction. The baseline measure of oxygenation is important because these patients have less pulmonary oxygen reserve and may desaturate quickly with induction of anesthesia and hypoventilation. Although postanesthetic ventilation is not usually required, a high index of suspicion should be used if there is significant clinical evidence of poor lung function preoperatively. Postoperative Apnea Apnea and bradycardia are well-recognized, major complications during and after surgery in neonates. The infants at highest risk are those born prematurely, those with multiple congenital anomalies, those with a history of apnea and bradycardia, and those with chronic lung disease. Decreased ventilatory control and decreased responsiveness to hypoxia and hypercarbia may be potentiated by anesthetic agents. Respiratory muscle fatigue may also play a role because neonates have a smaller percentage of type I fibers in their diaphragm and intercostal muscles. In addition, hypothermia and anemia also contribute to the development of postoperative apnea. However, some infants require mask ventilation or even prolonged intubation and ventilatory 2987 support. Caffeine and theophylline (metabolized to caffeine) act by increasing central respiratory drive and lowering the threshold of response to hypercarbia, as well as stimulating contractility in the diaphragm. Caffeine is favored because of its wider therapeutic margin and decreased propensity for toxicity. Administering caffeine prophylactically to infants at risk of postoperative apnea to ensure adequate serum levels may prevent the need for prolonged periods of postoperative ventilatory support. The question remains as to which infant should be admitted and monitored after outpatient surgery and for how long. Although the incidence of significant apnea and bradycardia is highest in the first 4 to 6 hours after surgery, it can occur up to 12 hours after surgery. An insightful approach to interpreting the various small studies is to stratify the risk of apnea, as done by Cote et al. Using 95% confidence limits, the authors found that the probability of apnea in nonanemic infants free of recovery room apnea was not less than 5% until postconceptual age was 48 weeks with gestational age of 35 weeks. This risk was not less than 1%, until a postconceptual age of 56 weeks with a gestational age of 32 weeks or a postconceptual age of 54 weeks and gestational age of 35 weeks. This type of analysis allows the clinician to determine which patients should be admitted on not only the criteria of gestational and postconceptual ages but also the amount of risk they are willing to assume. The very preterm infant, especially those under 1,200 g of weight, are at highest risk, with an incidence of significant disease about 2%. Acute retinal changes are seen in about 45% of susceptible preterm neonates, but there is spontaneous regression in most, permitting development of normal vision. In the fetus, developing blood vessels grow gradually 2988 from the macula toward the edges of the developing retina. In full-term newborns, this process is complete at birth or in the first few weeks, but continues for a longer period in the preterm infant.
Order cheap amoxicillin line
If necessary to correct respiratory depression medicine 93 948 generic 1000 mg amoxicillin otc, the drug should be given directly to the newborn intramuscularly (0. Nonetheless, ketamine is a useful adjuvant to inadequate regional analgesia during vaginal delivery or for obstetric manipulations. Constant communication is required with the patient to ensure that she is awake and able to protect her airway. Regional Analgesia Regional techniques provide excellent analgesia with minimal depressant effects on the mother and the fetus. Hypotension resulting from sympathectomy is the most frequent complication of central neuraxial blockade. Therefore, maternal blood pressure should be monitored at regular intervals, typically every 2 to 5 minutes for approximately 15 to 20 minutes after the initiation of the block and at routine intervals thereafter. The use of regional analgesia may be contraindicated in the presence of coagulopathy, acute hypovolemia, or infection at the site of needle insertion. Chorioamnionitis without frank sepsis is not a contraindication to central neuraxial blockade in obstetrics, provided antibiotics have been administered. Because of ethical considerations and methodologic difficulties, it is difficult to design clinical studies to examine the effects of neuraxial analgesia on the progress of labor and mode of delivery. Randomized controlled trials have found no difference in the rate of cesarean delivery in women who received neuraxial compared with systemic opioid labor analgesia. However, large randomized trials and a metaanalysis of these trials found no difference in the rate of cesarean delivery in women randomized to early neuraxial compared with systemic opioid analgesia. Effective analgesia during the first stage of labor may be achieved by blocking the T10 to L1 dermatomes with low concentrations of local anesthetic, usually combined with lipid-soluble opioids. Combining drugs allows the use of lower doses of both drugs, thus minimizing side effects and complications of each. For the second stage of labor and delivery, the nerve block should be extended to include the S2 to S4 segments in order to block pain from vaginal and perineal distension and trauma. Long-acting amides such as bupivacaine or ropivacaine are most frequently used because they produce excellent sensory analgesia while sparing motor function, particularly at low concentrations (<0. Although some studies have found that ropivacaine is associated with less motor blockade than equipotent doses of bupivacaine, there was no difference in the rate of instrumental vaginal delivery among women randomized to receive epidural levobupivacaine, bupivacaine, or ropivacaine for maintenance of labor analgesia. There is controversy regarding the need for an epidural test dose when using dilute solutions of local anesthetic. Because catheter aspiration is not always diagnostic, particularly when using singleorifice epidural catheters, some experts believe that a test dose should be administered to improve detection of an intrathecally or intravascularly placed catheter. Analgesia may be maintained with a continuous infusion (8 to 12 mL/hr) of bupivacaine (0. Data are conflicting as to whether a background infusion improves analgesia; however, a background infusion may be helpful in selected parturients. Thirty percent to 50% of the hourly dose is often administered as a background infusion. However, 2% lidocaine with epinephrine and sodium bicarbonate (1 mEq/10 mL lidocaine) and fentanyl may also be used when the rapid conversion of pre-existing epidural labor analgesia to surgical anesthesia is required for urgent cesarean delivery. Lidocaine should be administered with epinephrine, as lidocaine without epinephrine does not consistently provide satisfactory surgical anesthesia. Unintentional intravascular injection of bupivacaine is associated with a high incidence of maternal mortality. A metaanalysis of studies comparing different anesthetic solutions for extension of labor epidural analgesia for cesarean delivery concluded that ropivacaine provided denser anesthesia compared with bupivacaine or levobupivacaine. The standard technique uses the same spinal dose of local anesthetic as one would use for standard spinal anesthesia. After 15 minutes, if anesthesia is inadequate, the block is extended by injecting supplemental local anesthetic via the epidural catheter. A third technique is also associated with a lower incidence of hypotension without prolonging onset time. A small dose of spinal local anesthetic is followed by the routine injection of additional anesthetic through the epidural catheter approximately 5 minutes after the intrathecal dose. General Anesthesia General anesthesia may be necessary when absolute or relative contraindications exist to neuraxial anesthesia. General anesthesia should be used cautiously in women with asthma, upper respiratory tract infection, obesity, or a history of difficult tracheal intubation. Preoperative airway evaluation is particularly important in pregnant women because the inability to intubate the trachea and provide effective ventilation is the leading cause of maternal death related to anesthesia. Pulmonary aspiration prophylaxis should be administered and the patient should be positioned with left lateral tilt to prevent aortocaval compression. To minimize the risk of hypoxemia during induction, denitrogenation for 3 to 5 minutes with a tight-fitting mask is essential. Although somewhat controversial,87 a rapid-sequence induction is usually performed. A trained assistant applies cricoid pressure until the airway is properly secured with a cuffed endotracheal tube. Once correct placement of the endotracheal tube is confirmed with capnography and auscultation, the obstetrician may proceed with incision. Although some experts advise attempting to maintain cricoid pressure throughout, this practice may actually make visualization of the glottis and mask ventilation more difficult in some patients. However, if the fetus is in extremis, airway management with a mask or supraglottic airway device may be an acceptable alternative. However, the incidence of intraoperative awareness appears to be unacceptably high with this technique. After delivery, the nitrous oxide concentration can be increased and/or an intravenous amnestic. General anesthesia for cesarean delivery is associated with lower neonatal Apgar scores at 1 minute compared with neuraxial anesthesia93; however, the Apgar scores at 5 minutes are comparable. Therefore, an individual trained in neonatal resuscitation should be present at delivery of the infant. After delivery, prophylactic intravenous oxytocin is administered to decrease the risk of uterine atony and anesthesia may be deepened with an opioid and benzodiazepine, as necessary. The usual blood loss during cesarean delivery is 750 to 1,000 mL; transfusion is rarely necessary. During the most recent period, 2867 case-fatality rates from general anesthesia fell, whereas those for neuraxial anesthesia rose. Anesthesia-related mortality was most often associated with cesarean delivery (86%). The leading causes of death were intubation failure or induction problems (23%), respiratory failure (20%), and high spinal or epidural block (16%). Women who have recently eaten, are laboring, received systemic opioids, or have frequent heartburn are of greatest concern. Comprehensive airway evaluation, prophylactic administration of nonparticulate antacids, and use of regional anesthesia decrease the risk of aspiration. General anesthesia may be unavoidable occasionally; therefore, awake intubation may be indicated in women in whom airway difficulties are anticipated. Labor lowers the risk of hypotension in term pregnant women compared with nonlaboring women. Blood pressure should be monitored frequently (every 2 to 3 minutes) after the induction of neuraxial anesthesia. Techniques to reduce the incidence of hypotension during neuraxial anesthesia include left uterine displacement, intravenous fluid, and vasopressor administration. Maintaining the maternal blood pressure close to baseline reduces the incidence of maternal nausea and vomiting and is associated with higher umbilical artery pH values. Phenylephrine is equally efficacious to ephedrine for treating maternal hypotension and results in less fetal acidosis. Phenylephrine may be administered as a bolus dose (100 to 150 g) to treat hypotension99 or as a continuous prophylactic infusion (starting rate, 25 to 50 g/min). Unintentional intrathecal administration of epidural medication as a result of dural puncture or catheter migration may also result in this complication.
Buy cheap amoxicillin 500mg line
An increase in Hct during the first day suggests inadequate fluid resuscitation because hemolysis and sequestration are actually expected to cause a decrease in this parameter medicine to help you sleep purchase generic amoxicillin. Acute anemia, as may occur during excision and grafting of burns, is usually well tolerated. Blood replacement is usually not initiated until the Hct is decreased to 20% to 24% in healthy patients requiring limited operations, to approximately 25% in those who are healthy but need extensive procedures, and to 30% or more when there is a history of pre-existing cardiovascular disease. Dopamine in small doses (5 g/kg/min) and/or -adrenergic agents may improve urine output without further need for fluids. In contrast, aqueous topical agents such as 5% silver nitrate solution may cause hyponatremia and its consequences of cerebral edema and seizure secondary to electrolyte leaching. Central pontine demyelination may occur if the hyponatremia is corrected rapidly with salt solutions. Indeed there is some evidence to suggest that hourly monitoring of urine output as an end point of resuscitation compared to sophisticated hemodynamic monitoring provides similar outcomes in terms of mortality, organ function, length of hospital or intensive care stay, duration of mechanical ventilation, and burn-related complications such as pulmonary edema, compartment syndromes, or infection. They may not be readily available in some burn units, may lack proof of accuracy, and may be invasive, presenting a risk to patients who are already in a critical clinical state. Several measures are suggested to improve the accuracy of computing fluid requirement, such as a nomogram or an electronic calculator. For every 10 kg above 80 kg of body weight, 100 mL/hr is added to the calculated rate. The Rule of Ten appears accurate for patients weighing between 40 and 140 kg, overestimating the rate for patients below 40 kg and underestimating for those above 140 kg of body weight. If actual body weight is used, the calculated fluid need is lower than that determined for normal-weight patients. If ideal body weight is used, which is rare in clinical practice, the patient may receive a higher resuscitation volume. Morbidly obese patients are likely to have higher acidosis, organ dysfunction, and mortality. It has been shown that fluid intake in the second 24 hours correlates with that of the first 24-hour period; the higher the resuscitation volume during the first period, the higher the fluid intake during the second 24 hours. Generally the actual fluid volume administered exceeds the amount calculated by this formula by a factor of 1. An ultrasound-guided technique or a surgical cutdown may be necessary to facilitate access. The radial artery is the vessel of choice in abdominal or chest trauma in which the aorta may be cross-clamped, making a femoral or dorsalis pedis cannula nonfunctional. The right radial artery is preferred in cases of chest trauma in which cross-clamping of the descending aorta might result in occlusion of the left subclavian artery. In mechanically ventilated patients, the magnitude of systolic pressure variation (the difference between the maximum and minimum systolic pressures over the respiratory cycle) and its delta down component (the difference between systolic pressures at end-expiration and the lowest value during the respiratory cycle) can provide reliable information about the intravascular volume status and predict responsiveness to fluid loading. A systolic pressure variation over 5 mmHg and a delta down over 2 mmHg suggest hypovolemia and responsiveness to fluid. Measuring the right ventricular volume alone can provide information about the adequacy of the intravascular volume. This technique also allows visualization of fat and air entry into the right heart, or into the left heart through a patent foramen ovale during internal fixation of lower extremity fractures. Other qualitative findings to be looked for during evaluation of heart function with the parasternal short axis view at the level of the papillary muscles are inward motion of the endocardium, myocardial thickening, longitudinal motion of the mitral annulus, and geometry of the left ventricle. Urine Output Urine output is routinely monitored as an indicator of organ perfusion, hemolysis, skeletal muscle destruction, and urinary tract integrity after trauma. Its reliability in monitoring perfusion is decreased by prolonged shock prior to surgery and osmotic diuresis caused by administration of mannitol or radiopaque dye. Dark, cola-colored urine in the trauma patient suggests either hemoglobinuria resulting from incompatible blood transfusion or myoglobinuria caused by massive skeletal muscle destruction after blunt or electrical trauma. Although the definitive diagnosis is made by serum electrophoresis, rapid differential diagnosis can be made by centrifugation of a blood specimen. Pink-stained serum suggests hemoglobinuria, whereas unstained serum indicates myoglobinuria. Prevention involves inducing diuresis with fluids and mannitol and, in myoglobinuria, although controversial, additional alkalinization of the urine with sodium bicarbonate to pH greater than 5. Red-colored urine usually is caused by hematuria, which, in the traumatized 3802 patient, suggests urinary tract injury. Oxygenation Trauma patients frequently develop hypoxemia (O2 saturation <90%), hypothermia, hypotension, and/or decreased peripheral perfusion. Of the available O2 saturation (SpO2) devices, finger or earlobe pulse oximeters are more affected by decreased perfusion than forehead probes, probably because the latter senses the pulsation of the supraorbital artery, a branch of the carotid artery, which is presumably less affected by shock or hypothermia. However, SpO2 results with the forehead monitor may be affected by venous pulsation, especially in patients receiving positive-pressure ventilation or in any situation that distends the tributaries of the superior vena cava. They can also measure noninvasive continuous hemoglobin concentration with reasonable accuracy. Organ Perfusion and Oxygen Utilization As discussed previously, unrecognized hypoperfusion may lead to splanchnic ischemia with resulting acidosis in the intestinal wall, permitting the passage of luminal microorganisms into the circulation and release of inflammatory mediators, causing sepsis and multiorgan failure. Subsequent organ failure may occur if it decreases below a value of 170 mL/min/m2, indicating a flow-dependent phase of O2 utilization. However, it is possible that dysoxia may be present in an individual organ in the presence of a normal overall O2 extraction ratio. The maximum amplitude is the widest portion of the curve and indicates the absolute strength of the fibrin clot. The -angle is the slope of the external divergence of the tracing from the R-value point, indicating the speed of clot formation and fibrin crosslinking. The value of this parameter is determined by both coagulation factors and platelets. Hypothermia can cause coagulopathy by interfering with both platelets and coagulation factors. Results of coagulation parameters are obtained within 10 to 15 minutes because of activation with specific materials for each of clotting, platelet, and fibrinogen function. The varying contribution of these conditions to the clinical picture of a given patient necessitates priority-oriented planning. If a rapid-sequence induction is contemplated, ketamine and etomidate may confer advantages over propofol. In equipotent doses in normovolemic patients, they produce less cardiovascular depression. Contrary to findings of increased mortality with prolonged etomidate infusion, a single induction dose (0. Its longer duration of action may be disadvantageous and may lead to hypoxia, if both ventilation and intubation prove to be impossible. Under these circumstances, one of the available videolaryngoscopes or other aids can be employed to overcome the problem. Sugammadex can also be utilized to encapsulate rocuronium or vecuronium and recover spontaneous breathing in a reasonably short period. Bradycardia, dysrhythmias, and cardiac arrest may occur after succinylcholine in the presence of hypoxia and hypercarbia. Some of these complications may also follow an apparently uneventful intubation performed without succinylcholine. Hypovolemia In the absence of controlled human studies of anesthetic drug effects in hemorrhage and hemorrhagic shock, our current knowledge in this area is based on the results of experimental work, mostly in swine, and clinical 3807 experience from managing trauma victims. Our planning process for deciding how to use anesthetic agents is further complicated by the damage control resuscitation principle, specifically permissive hypotension. The facts that should drive decision making in this regard are as follows: First, anesthetic agents not only have direct cardiovascular depressant effects but also inhibit compensatory hemodynamic mechanisms such as central catecholamine output and baroreflex (neuroregulatory) mechanisms, which maintain systemic pressure in hypovolemia. Second, hemorrhage and hypovolemia alter the pharmacokinetics and pharmacodynamics of almost all anesthetic agents and often lead to a higher than normal blood concentration of intravenous agents and increased sensitivity of the brain and heart. Preferential distribution of the cardiac output to the brain and the heart, cerebral hypoxia, dilutional hypoproteinemia producing a larger free fraction of intravenous drugs, and acidosis all seem to be responsible for these effects. Third, hemorrhage and hypovolemia have different hemodynamic effects in the absence and presence of trauma. In the presence of trauma pain and a catecholamine surge, maintain blood pressure despite significant intravascular volume depletion and ischemia of vital organs such as the brain and the heart.
Chinarinde (Cinchona). Amoxicillin.
- Are there any interactions with medications?
- Are there safety concerns?
- Hemorrhoids, varicose veins, colds, leg cramps, influenza, malaria, fever, cancer, mouth and throat diseases, enlarged spleen, muscle cramps, loss of appetite, and stomach discomforts such as bloating and fullness.
- How does Cinchona work?
- Dosing considerations for Cinchona.
- What is Cinchona?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96418
Discount amoxicillin 500 mg amex
Laparoscopic radical nephrectomy: the new gold standard surgical treatment for localized renal cell carcinoma medications rights buy amoxicillin in india. Is laparoscopic partial nephrectomy as effective as open partial nephrectomy in patients with renal cell carcinoma Comparison of 1,800 laparoscopic and open partial nephrectomies for single renal tumors. Living kidney donation: A comparison of laparoscopic and conventional open operations. Chronic pain following donor nephrectomy: A study of the incidence, nature and impact of chronic post-nephrectomy pain. Efficacy and safety of continuous local infusion of ropivacaine after retroperitoneoscopic live donor nephrectomy. Continuous infusion of local anesthesia after living donor nephrectomy: A comparative analysis. Left ventricular loading modifications induced by pneumoperitoneum: A time course echocardiographic study. Comparison of three perioperative fluid regimes for laparoscopic donor nephrectomy: A prospective randomized dosefinding study. Changes in lung and chest wall properties with abdominal insufflation of carbon dioxide are immediately reversible. Goal-directed intraoperative fluid administration reduces length of hospital stay after major surgery. Enhanced recovery after surgery protocols for radical cystectomy surgery: Review of current evidence and local protocols. A new concept for early recovery after surgery for patients undergoing radical cystectomy for bladder cancer: Results of a prospective randomized study. Preemptive epidural analgesia and recovery from radical prostatectomy: A randomized controlled trial. Transient lower extremity neurapraxia associated with radical perineal prostatectomy: A complication of the exaggerated lithotomy position. Re: Transient lower extremity neurapraxia associated with radical perineal prostatectomy: A complication of the exaggerated lithotomy position. General versus spinal anesthesia in patients undergoing radical retropubic prostatectomy: Results of a prospective, randomized study. Catastrophic venous air embolus during prostatectomy in the Trendelenburg position. Anesthesia for radical prostatectomy, cystectomy, nephrectomy, pheochromocytoma, and laparoscopic procedures. Intraoperative and early postoperative complications of radical retropubic prostatectomy. Interposition nerve grafting during radical prostatectomy: cumulative review and critical appraisal of literature. Anesthetic technique for radical prostatectomy surgery affects cancer recurrence: A retrospective analysis. Transcranial Doppler monitoring during laparoscopic anterior lumbar interbody fusion. Does anaesthetic technique affect the outcome after transurethral resection of the prostate Anaesthesia for transurethral prostatectomy: A comparison of spinal intradural analgesia with two methods of general anaesthesia. Irrigation fluid absorption during transurethral resection of the prostate: Spinal vs. Body temperature changes during prostatic resection as related to the temperature of the irrigating solution. Surgical and anaesthetic considerations in transurethral resection of the prostate. Transurethral prostatectomy: Immediate and postoperative complications: A cooperative study of 13 participating institutions evaluating 3,885 patients. Morbidity, mortality and early outcome of transurethral resection of the prostate: A prospective multicenter evaluation of 10,654 patients. Meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic enlargement. Tranexamic acid in control of primary hemorrhage during transurethral prostatectomy. Transurethral prostatectomy: a long-term follow-up study of 166 patients over 80 years of age. Evaluation of fluid absorption during holmium laser enucleation of prostate by breath ethanol technique. Transurethral prostatic resection syndrome: A new perspective: Encephalopathy with associated hyperammonemia. Visual disturbances: An unusual symptom of transurethral prostatic resection reaction. Patterns of irrigating fluid absorption during transurethral resection of the prostate as indicated by ethanol. Feasibility of percutaneous nephrolithotomy under assisted local anaesthesia: A prospective study on selected patients with upper urinary tract obstruction. The association between regional anesthesia and acute postoperative urinary retention in women undergoing outpatient midurethral sling procdures. Urological injuries during cesarean section: Intraoperative diagnosis and management. The advancement of pure local anesthesia for penile surgeries: Can an outpatient basis be sustainable A current review of the etiology, diagnosis, and treatment of pediatric pheochromocytoma and paraganglioma. Regional anesthesia can provide physiologic benefits and facilitate recovery compared to general anesthesia. General anesthesia is appropriate for surgeries not amenable to and/or patients with contraindications to regional techniques. Orthopedic surgery patients may have limited mobility and may require special attention to avoid positioning-related injury. Patients presenting for spine surgery should be evaluated carefully for potential airway challenges and/or impaired respiratory function. Major spine surgery frequently involves significant bleeding, and blood conservation techniques should be considered. Intraoperative monitoring of spinal cord function should be used for surgeries where the cord is at risk of injury. Catastrophic venous air embolism during spine surgery may present as unexplained hypotension with high end-tidal nitrogen and low end-tidal carbon dioxide. Nerve injury may result from surgical trauma and/or nerve blockade in the setting of pre-existing neurologic deficits. In the sitting position, for every 20 cm of difference in height of the head from the heart, there is a 15-mmHg difference in mean arterial pressure. Ephedrine, atropine, and glycopyrrolate should be available for management of hypotensive bradycardic events occurring during surgery in the beach chair position. Interscalene blocks cause hemidiaphragmatic paresis and can cause respiratory compromise in patients with reduced pulmonary function. Venous thromboembolism is a common complication of lower extremity orthopedic surgery performed with inadequate thromboprophylaxis. The American Society of Regional Anesthesia has released guidelines for safe use of regional anesthesia in the setting of antithrombotic or thrombolytic therapy. Introduction to Orthopedic Anesthesia Perioperative management of the patient undergoing orthopedic surgery involves knowledge of orthopedic surgical techniques and associated complications, including nerve injury. Expertise in regional anesthetic techniques for both surgical anesthesia and postoperative analgesia is of paramount importance. Appropriate patient positioning produces optimal surgical conditions while avoiding complications related to stretch, pressure, 3610 and hemodynamic changes. Orthopedic procedures can be associated with major blood loss; therefore, one must be familiar with tourniquet use, controlled intraoperative hypotension, blood salvage techniques, use of antifibrinolytics, fluid resuscitation (see Chapter 16), transfusions, and related complications (see Chapter 17). Orthopedic surgical patients benefit greatly from early mobilization and rehabilitation, both of which can be expedited by specific anesthetic techniques and proactive postoperative analgesia. A multimodal approach, often utilizing neuraxial and/or peripheral nerve blocks, can enhance recovery and improve functional outcomes. Patients undergoing major orthopedic surgery are at high risk for venous thromboembolism. Knowledge of current pharmacologic and mechanical methods of thromboprophylaxis is required, and regional techniques must be managed so as to minimize associated bleeding risk. Preoperative Assessment All patients should undergo medical and laboratory testing appropriate to their medical history and planned procedure (see Chapter 23). Preoperative assessment of the orthopedic patient must include special attention to potential airway difficulties, considerations relating to mobility and intraoperative positioning, and medication history related to opioid dependence and anticoagulation status.
Buy amoxicillin once a day
Chronotropic and hemodynamic incompetence in response to various challenges such as sustained handgrip medications similar to vyvanse amoxicillin 500 mg visa, ice water hand submersion, Valsalva maneuver, and tilt table testing has demonstrated autonomic neuropathy in 43% of cirrhotic patients. Risk factors for coronary artery disease in cirrhotic patients are similar to those of other patient populations: hypertension, dyslipidemia, age, gender, and obesity. Because many of these patients cannot exercise, pharmacologic stress testing is most commonly employed. Unfortunately, studies 3263 investigating the predictive value of noninvasive functional testing, particularly dobutamine stress echocardiography, have generally shown poor sensitivity and variable quality of negative predictive value (75% to 89%). Renal Dysfunction the hallmarks of renal dysfunction in cirrhosis are the seemingly inappropriate avid retention of sodium and free water, together with renal hypoperfusion and consequent decreased glomerular filtration. Immune complex nephropathies such as IgA nephropathy and membranous proliferative glomerulonephropathy are associated with chronic hepatitis C infection. These include such diseases as amyloidosis, systemic lupus erythematosus, autoimmune hepatitis, polycystic liver disease, and Alagille syndrome. Thus, cirrhotic patients are very sensitive to the prostaglandin inhibition of nonsteroidal anti3264 inflammatory medications. Aminoglycosides, angiotensin-converting enzyme inhibitors, and angiotensin receptor blockers are other drug groups associated with nephrotoxicity in cirrhotic patients. Despite the expectation that contrast administration would be nephrotoxic, there is no evidence to support that concern. Although they were once considered variants of the same disorder, it has become increasingly clear that they must be treated as two different entities. More effective has been therapy targeting the underlying pathology that leads to the renal vasoconstrictive response, that is, reduction of portal hypertension and/or splanchnic vasodilation. Choices among these therapies are to some extent dictated by drug availability because, for example, terlipressin is not available in the United States. In countries where terlipressin is available, terlipressin plus albumin volume expansion is also an option. In addition, there are two types of vascular abnormalities unique to the setting of portal hypertension, which have significant morbidity and mortality. Their severity may even overshadow the underlying liver disease, so much so that their presence and severity influences candidacy for liver transplantation. Type I lesions are more common and are manifested as precapillary dilations at the alveolar level. This, together with the usually hyperdynamic circulation of the cirrhotic patient, allows insufficient time for oxygen diffusion through the entire stream of capillary blood. This results in a central stream of poorly oxygenated blood that is functionally shunted. This lesion is easily correctable with the administration of oxygen, because increased FiO2 increases oxygen diffusion through the dilated capillary. Suspected contributing factors include nitric oxide, splanchnic endotoxemia, decreased clearance of inflammatory mediators, and 3268 angiogenesis. Post-livertransplantation correction of hypoxemia is almost universal, although it may take up to a year to do so. The specific diagnostic criteria put forth by the European Respiratory Society Task Force on Hepatopulmonary Diseases108 follow: 1. Furthermore, as with other types of pulmonary hypertension, increased levels of endothelin are also thought to play a role. Therapy includes conventional measures such as diuresis, as well as some specific vasodilator therapy. Calcium channel blockers, often used in other patients with pulmonary hypertension, are contraindicated in this population because they promote mesenteric vasodilation and worsen portal hypertension. Other drugs used include prostanoids, phosphodiesterase inhibitors, and endothelin antagonists. Reported success with these modalities is on the basis of case reports or case series, and no one therapy has emerged as definitive. However, it must be administered as a continuous infusion via central access with little tolerance for interruption of the infusion. It has also been associated with splenomegaly and worsening thrombocytopenia, sufficient to limit its use. Although there are concerns for hepatic toxicity, published case reports and case series have not documented significant increases in liver enzymes with its use. Nonetheless, it is an option for a select group of patients whose pulmonary hemodynamics and cardiac function suggest they will tolerate the procedure. Neuropsychologic assessment focuses on level of consciousness, attention and ability to follow commands, and effect. This is most often graded on a 0 to 4 scale using the West Haven criteria (Table 46-9). However, focal neurologic findings should prompt appropriate imaging to rule out structural neurologic lesions, because these patients are at risk for intracranial bleeding and are not 3271 immune to other neurologic pathologies such as ischemic brain disease, abscess, and tumor. Ammonia is a byproduct of nitrogen-containing compounds that is toxic and must be removed from the body. The liver is the primary site of ammonia metabolism and excretion via the urea cycle, but the brain, skeletal muscle, and possibly kidneys contribute as well. Unfortunately, neither the brain nor the skeletal muscle is capable of utilizing the urea cycle and instead use glutamine synthetase to synthesize glutamine from ammonia and glutamate. Because these are the cells capable of metabolizing ammonia, as ammonia levels rise intracellular levels of glutamine rise in concert. There are two consequences to this: (1) Glutamine, which is osmotically active, pulls water intracellularly, causing astrocyte swelling and cerebral edema; and (2) glutamate, which is an important excitatory neurotransmitter, is first released and then consumed in producing glutamine. Experimental in vitro evidence has demonstrated a glutamate release from astrocytes in response to elevated levels of ammonia. The differential diagnosis includes other metabolic encephalopathies such as uremia, sepsis, glucose and electrolyte abnormalities, and endocrinopathies. Because cirrhotic patients are exquisitely sensitive to sedative medications and have impaired hepatic (and often renal) metabolism, careful search for possible drug-related encephalopathy should be undertaken. Once other potential causes have been eliminated, the next step should be a systematic search for an underlying cause or precipitating factor (Table 46-11). Once identified, treatment or elimination should commence as soon as possible and may be sufficient for clinical improvement. If addressing the underlying cause does not produce improvement, the 3273 next step is to employ therapy designed to either reduce the production of or increase the excretion of ammonia. First, anaerobic bacteria in the colon ferment lactulose to produce weak acids and acidify the colon. Secondly, it is proposed that this acid milieu is also cathartic, and that catharsis augments reduced absorption. Table 46-10 Proposed Nomenclature of Hepatic Encephalopathy Although simple reduction in protein intake seems an intuitive solution, in fact protein restriction may be harmful for cirrhotic patients who tend to have little nutritional reserve due to poor intake and who have likely lost nutritional ground with every hospitalization. Nonhepatic causes include malignancy, cardiac failure, renal disease, pancreatitis, and tuberculosis. Perhaps the most expeditious study to define the nature of newonset ascites is a paracentesis. It is calculated as the difference between simultaneously measured serum and ascites albumin levels. Hyponatremia is common among cirrhotic patients with ascites and generally does not warrant fluid restriction unless the serum sodium level is below 120 to 125 mEq/L. Observations in liver transplant recipients suggest limiting correction to 16 mEq/L or less over an 8-day period. Once 3275 patients become refractory to maximum standard medical therapy, the 6month mortality is 21%. Although current practice is to replace albumin when ascitic fluid is drained, this practice is not well supported by randomized prospective trials.
1000mg amoxicillin free shipping
For those patients who are unable to lose weight by more conservative means medicine gabapentin 300mg capsules purchase amoxicillin canada, bariatric surgery has been shown to result in dramatic histologic and chemical improvement, with decreased steatosis/inflammation on biopsy and decreases in serum aminotransferases. Prior episodes of jaundice, particularly in relationship to surgical procedures and anesthesia, should be thoroughly investigated. Alcohol consumption, use of recreational or illicit drugs, medications (including herbal products), presence of tattoos, sexual promiscuity, consumption of raw seafood, and a history of travel to areas in which hepatitis is endemic should be sought. Symptoms of fatigue, anorexia, weight loss, nausea, vomiting, easy bruising, pruritus, dark-colored urine, biliary colic, abdominal distention, and gastrointestinal bleeding warrant further investigation for the presence of liver disease. Physical examination findings suggestive of active liver disease include icterus, palmar erythema, spider angiomas, gynecomastia, 3281 hepatosplenomegaly, ascites, testicular atrophy, petechiae, ecchymoses, and asterixis. In the absence of findings suggestive of liver disease, routine laboratory tests to assess hepatocellular integrity and hepatic synthetic function are not warranted. Routine laboratory testing may yield false-positive results, and true-positive results are infrequent in asymptomatic patients. As a result, minor elevations of liver-enzyme results-those less than twice the normal range-may be of no clinical importance. Nonetheless, in the presence of abnormal results (in an asymptomatic patient) the safest approach is to repeat the results; in the absence of elevations greater than twice the upper limits of normal it is reasonable to proceed with surgery. Medications include selected antibiotics, antiepileptic drugs, lipid-lowering agents, nonsteroidal anti-inflammatory agents, and sulfonylureas. Herbal medications and drugs of abuse are also associated with liver-enzyme abnormalities. Based on retrospective, small case series from the 1960s and 1970s, acute hepatitis confers a prohibitive risk for elective surgery. In a series of 36 patients with undiagnosed hepatitis who underwent laparotomy (for suspected biliary obstruction or hepatic malignancy) nearly one-third died. The majority of patients suffered complications that included bacterial peritonitis, wound dehiscence, and hepatic failure. In the absence of accumulating evidence, consensus opinion is that elective surgery should be postponed in patients with acute hepatitis. A number of studies have investigated the risk of surgery in patients with cirrhosis. They identified five factors-albumin, bilirubin, ascites, encephalopathy, and nutritional status-as important prognostic factors for patients with cirrhosis. Each of the factors was categorized according to three levels of severity and combined to generate a composite score leading to an assignment of one of three classes of severity (class A, B, or C, with C representing the most severe hepatic dysfunction). The score was originally designed for patients undergoing portosystemic shunt procedures, but has subsequently been applied to patients with cirrhosis undergoing other surgeries. In studies conducted over multiple decades, the modified Child score performed similarly in predicting postoperative mortality: 10% in Child A, 17% to 30% in Child B, and 60% to 80% in Child C. In the cohort of patients undergoing abdominal surgery, the c-statistic improved to 0. However, based on the list of complications, the authors recommend that these patients should preferably have surgery at institutions with a liver transplant center. However, there is little evidence to support specific goal-directed targets for preoperative care. The perioperative risk depends more on the operative site and the degree of liver impairment than the anesthetic technique. Upper abdominal surgery (cholecystectomy), when compared to hysterectomy, was associated with liver-enzyme abnormalities, whereas the anesthetic technique (halothane, enflurane, or fentanyl) was not. For instance, 1-year mortality in patients with six risk factors was over 80%; mortality with two risk factors was approximately 30%. In addition to optimizing medical management, efforts should be made to minimize surgical risk through the consideration of less invasive surgery. Gallstones are twice as common in cirrhotic patients as in patients without cirrhosis. In uncontrolled retrospective studies the advantages included low mortality and shorter hospital stay. The decision is based on the presence of preoperative systemic hypotension due to vasodilation, anticipated blood loss, the need for intraoperative laboratory studies, coexisting disease, and age. Pulmonary artery catheterization is used for patients with known or suspected pulmonary artery hypertension and for patients with a low cardiac ejection fraction. Thus, avoidance of high neuraxial block and hypotension seems prudent in patients with advanced liver disease. Many patients with advanced hepatic disease may not warrant consideration for neuraxial techniques due to coagulopathy and/or thrombocytopenia. Nerve blockade may be appropriate even when neuraxial blockade is contraindicated. Volatile Anesthetics Volatile anesthetics decrease hepatic blood flow, albeit to a variable degree. Halothane is more likely than other inhaled anesthetics to cause cardiovascular depression and results in the greatest reduction of hepatic blood flow. Newer volatile agents, including isoflurane and sevoflurane, have less significant effects on hepatic blood flow. This dose-dependent reduction in hepatic blood flow does not occur with sevoflurane. In animal studies both sevoflurane and isoflurane maintain the hepatic arterial buffer response, which increases hepatic arterial blood flow in the presence of reductions of portal blood flow. Halothane hepatitis, described earlier in this chapter, is largely responsible for these concerns. However, there is little evidence to suggest that other volatile anesthetics are responsible for hepatic complications. However, the incidence of liver injury correlates with the extent to which inhaled anesthetics undergo oxidative metabolism. Because there is no pathognomonic liver pathology, the diagnosis is based on the exclusion of other causes and a history of recent exposure. The potential for toxic metabolites seems related to the degree of in vivo biotransformation of the various halogenated anesthetics. This fact led to the suggestion that patients sensitized to other volatile anesthetics could be safely anesthetized with sevoflurane. Nitrous Oxide Nitrous oxide administration has not been shown to cause hepatocellular injury in the absence of hepatic hypoxemia. However, the clinical significance of these effects is unclear, although prolonged or repeated exposure could induce a vitamin B12 deficiency. A rare syndrome of lactic acidosis, lipemia, rhabdomyolysis, hyperkalemia, myocardial failure, and death has been reported after prolonged infusions of propofol. Some authors have suggested that morphine causes spasm in the sphincter of Oddi, but a review failed to show a differential effect, concluding that morphine may be preferred over meperidine for the treatment of patients with acute pancreatitis due to less risk of seizures. Factors that affect hepatic clearance include blood flow to the liver, the fraction of the drug unbound to plasma proteins, and intrinsic clearance. Clearance of drugs in this class is affected by protein binding, the induction or inhibition of hepatic enzymes, age, and hepatic pathology, but clearance is not significantly affected by hepatic blood flow. Regardless of the route of administration, drugs with high extraction ratios are significantly affected by alteration in hepatic blood flow, which can occur with hemodynamic changes or hepatic inflow clamping during liver resection. As is commonly the case for drugs with low extraction ratios, the elimination half-life can be prolonged (diazepam t1/2 = 43 hours). Studies have shown conflicting effects of cirrhosis on the metabolism of midazolam, possibly due to changes in protein binding. Because only the unbound drug is available for metabolism by hepatic enzymes, the elimination may be unaffected despite a reduction in intrinsic hepatic clearance. However, the volume of distribution of thiopental, another drug with a low extraction ratio, is not altered in cirrhotic patients. However, the altered pharmacodynamic effects that occur in patients with encephalopathy frequently lead to an increased sensitivity to sedatives and analgesics. Prolonged elimination is more prominent with morphine and meperidine than the shorter-duration synthetic opioids, although contradictory data exist that suggest pharmacokinetics is not significantly altered by liver disease. The clearance of the meperidine metabolite normeperidine is reduced in liver disease, which can lead to neurotoxicity.
Amoxicillin 500mg mastercard
Blood pressure and heart rate changes during short duration laryngoscopy for tracheal intubation: influences of viscous or intravenous lidocaine symptoms ringworm cheap amoxicillin 250mg with amex. Efficacy of lignocaine in the suppression of the intraocular pressure response to suxamethonium and tracheal intubation. Ventricular fibrillation and tachycardia after intravenous atropine for treatment of bradycardias. Autonomic cardio-respiratory reflex reactions and super selective ophthalmic arterial chemotherapy for retinoblastoma. Autonomic cardio-respiratory reflex reactions and super selective ophthalmic arterial chemotherapy for retinoblastoma (letter). The technique of ophthalmic arterial infusion therapy for patients with intraocular retinoblastoma. Echothiophate iodide therapy in children: effect upon blood cholinesterase levels. Lack of side effects from topically administered 10% phenylephrine eye drops: a controlled study. Prescription of ocular beta-blockers in patients with obstructive pulmonary disease: does a central electronic medical record make a difference Medical consequences of stopping anticoagulants prior to intraocular surgery or intravitreal injections. Safety of continuing warfarin therapy during cataract surgery: a systematic review and meta-analysis. The perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th ed). The use of perioperative antithrombotic agents in posterior segment ocular surgery. Haemorrhage and risk factors associated with retrobulbar/peribulbar block: a prospective study in 1383 patients. Practice alert for the perioperative management of patients with coronary artery stents: a report by the American Society of Anesthesiologists Committee on Standards and Practice Parameters. Risk of major adverse cardiac events following noncardiac surgery in patients with coronary stents. A survey of ophthalmic anesthetists on managing pacemakers and implanted cardiac defibrillators. Sneezing reflex associated with intravenous sedation and periocular anesthetic injection. Universal protocol for preventing wrong site, wrong procedure, wrong person surgery. Positive pressure ventilation and the laryngeal mask airway in ophthalmic anaesthesia. The laryngeal mask airway for intraocular surgery: effects on intraocular pressure and stress responses. The effect of the laryngeal mask airway on coughing after eye surgery under general anesthesia. Comparison of needle path, anesthetic dispersion, and quality of anesthesia in retrobulbar and peribulbar blocks. Retrobulbar anesthesia risk: do sharp needles really perforate the eye more easily than blunt needles Ocular decompression devices: liquid mercury balloon versus the tungsten powder balloon. A comparative rabbit model study of two ultrasound devices evaluating intraorbital thermal and structural changes. Medial canthus single-injection episcleral (sub-Tenon) anesthesia: computed tomography imaging. Lidocaine 2% gel versus lidocaine 4% unpreserved drops for topical anesthesia in cataract surgery: a randomized controlled trial. Association between tamsulosin and serious ophthalmic adverse events in older man following cataract surgery. Ropivacaine-lidocaine versus bupivacainelidocaine for retrobulbar anesthesia in cataract surgery. Color Doppler ultrasound measurements after topical and retrobulbar epinephrine in primate eyes. Second cluster of strabismus cases after periocular anesthesia without hyaluronidase. Role of hyaluronidase in diplopia after peribulbar anesthesia for cataract surgery. Effect of intraocular pressure reducer on ocular and optic nerve blood flow in phakic rabbit eyes. Documenting the subjective patient experience of first versus second cataract surgery. International variation in anesthesia care during cataract surgery: results from the International Cataract Surgery Outcomes Study. Anaesthesia techniques for cataract surgery: a survey of delegates to the Congress of the International Council of Ophthalmology, 2002. What determines patient satisfaction with cataract care under topical local anesthesia and monitored sedation in a community hospital setting Rethinking anesthesia strategies for patients with traumatic eye injuries: alternatives to general anesthesia. Local anesthesia with intravenous sedation for surgical repair of selected open globe injuries. Combined topical anesthesia and sedation for open-globe injuries in selected patients. Cervicofacial subcutaneous emphysema and pneumomediastinum after retinal detachment surgery: just another monitored anesthesia eye case. Permanent postoperative vision loss associated with expansion of intraocular gas in the presence of a nitrous oxide- 3501 137. Delayed intraocular foreign body removal without endophthalmitis during Operations Iraqi Freedom and Enduring Freedom. Excess comorbidities associated with malignant hyperthermia diagnosis in pediatric hospital discharge records. Effect of droperidol pretreatment on postanesthetic vomiting in children undergoing strabismus surgery. Low-dose droperidol versus standarddose droperidol for prevention of postoperative vomiting after pediatric strabismus surgery. Effect of propofol on the incidence of postoperative vomiting after strabismus surgery in pediatric outpatients. Comparison of the analgesic and emetic properties of ketorolac and morphine for paediatric outpatient strabismus surgery. Injuries associated with regional anesthesia in the 1980s and 1990s: a closed claims analysis. The American Society of Anesthesiologists Postoperative Visual Loss Registry: analysis of 93 spine surgery cases with postoperative visual loss. Postcataract ptosis: a randomized, doublemasked comparison of peribulbar and retrobulbar anesthesia. Early exploration of diplopia with magnetic resonance imaging after peribulbar anaesthesia. Autoregulation of urine flow does not occur, but a linear relationship between mean arterial pressure above 50 mmHg and urine output is observed. During periods of reduced renal perfusion, the metabolically active medullary thick ascending limb may be especially vulnerable to ischemic injury. The physiologic response to surgical stress invokes intrinsic mechanisms for sodium and water conservation. Renal cortical vasoconstriction causes a shift in perfusion toward juxtamedullary nephrons, a decrease in glomerular filtration rate, and retention of salt and water result. Likewise, anesthetic agents have not been shown to interfere with the renal response to physiologic stress. The single most reliable predictor of new postoperative need for dialysis is preoperative renal insufficiency.