Discount 2.5 mg indapamide visa
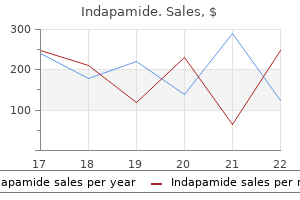
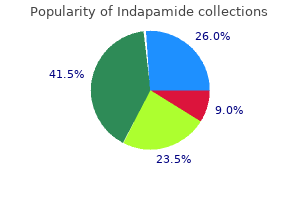
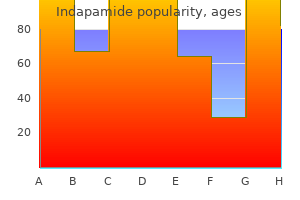
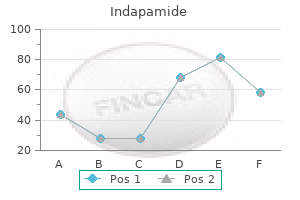
Explain to the patient that although he or she feels recovered blood pressure jokes purchase indapamide now, this is not the case. The feeling is similar to that which occurs when one has had some alcohol and feels normal but is unable to function at normal capacity. Alternative escorts that may occur to the patient or the dentist include taking a taxicab, car service. The only person who should be permitted to escort the patient home is a relative or close friend of the patient, a person who can remain with the patient until he or she has recovered. I have come to describe the acceptable escort as "a responsible adult, a person who has a vested interest in the health and safety of the patient. Without the suggested training or experience, I do not believe that this combination of techniques should be used. Oral drugs should not be used for deep sedation because of the lack of titratability of this route of drug administration. Fixed drug combinations are frequently mentioned in legal depositions where morbidity or mortality has occurred. An oft-heard statement is, "But I gave this same dose of drugs to 10,000 other patients without ever having a problem. If we were to solely consider the newspaper account, we would have to say that intravenously administered drugs are dangerous. The degree of control maintained by the administrator over intravenously administered drugs is second only to that available with inhalation sedation. If the techniques described in this book are followed and the dentist does not experiment with increased dosages or transportation in which the escort is a stranger to the patient. Very often, remarks made in a lecture are misconstrued, and an important concept may be improperly understood. Having several office personnel attending the course will minimize the chance of this occurring. It is a new technique and must be used many times in that environment before it becomes integrated into the practice routine. One must anticipate that extra time may be required during the first 50 or so cases. Administering drugs intravenously is easy and safe (if basic rules are followed regarding titration). Unfortunately, most dentists do not wish to "practice" venipuncture on their patients. There are several possible places where one might improve his or her technique of venipuncture. Inadequate monitoring during the procedure Though that paper was published in 1983, sadly, these same three factors are still implicated as causations in many recent dental office morbidities and mortalities. Although not scientifically valid, these numbers do illustrate the safety of the basic techniques discussed in this section. In a 1981 survey of 188 dentists who completed this course, it was found that they had completed more than 53,664 cases in private practice without any serious complications. Rodgers states that during this period, a number of previously undiagnosed medical problems were discovered. Oregon Academy of General Dentistry, Oregon Health Sciences University School of Dentistry. New drugs, equipment, and monitoring devices become available almost every year, and it is only through continuing education that it is possible for the dentist to evaluate these items properly, some of which are initially touted by their developers as panaceas. These guidelines present a basic overview of the requirements for a competency course in moderate sedation. These include courses in enteral moderate sedation and parenteral moderate sedation. The teaching guidelines contained in this section on moderate sedation differ slightly from documents in medicine to reflect the differences in delivery methodologies and the practice environment in dentistry. For this reason, separate teaching guidelines have been developed for moderate enteral and moderate parenteral sedation. Moderate sedation: a drug-induced depression of consciousness during which patients respond purposefully to verbal commands, either alone or accompanied by light tactile stimulation. No interventions are required to maintain a patent airway, and spontaneous ventilation is adequate. Repeated dosing of an agent before the effects of previous dosing can be fully appreciated may result in a greater alteration of the state of consciousness than is the intent of the dentist. E Further, a patient whose only response is reflex withdrawal from a painful stimulus is not considered to be in a state of moderate sedation. The following definition applies to administration of moderate and deeper levels of sedation: Titration: administration of incremental doses of an intravenous or inhalation drug until a desired effect is reached. Although the concept of titration of a drug to effect is critical for patient safety, when the intent is moderate sedation, one must know whether the previous dose has taken full effect before administering an additional drug increment. Teaching Administration of Moderate Sedation these guidelines present a basic overview of the requirements for a competency course in moderate sedation. The teaching guidelines on moderate sedation contained in this section differ slightly from documents in medicine to reflect the differences in delivery methodologies and practice environment in dentistry. Completion of a prerequisite nitrous oxide-oxygen competency course is required for participants combining moderate sedation with nitrous oxide-oxygen. Course Objectives: Upon completion of a course in moderate sedation, the dentist must be able to: 1. Discuss the prevention, recognition, and management of complications associated with moderate sedation. Administer moderate sedation to patients in a clinical setting in a safe and effective manner. Discuss the abuse potential, occupational hazards, and other untoward effects of the agents utilized to achieve moderate sedation. Describe and demonstrate the technique of intravenous access, intramuscular injection, and other parenteral techniques. Discuss the precautions, indications, contraindications, and adverse reactions associated with the drug(s) selected. Administer the selected drug(s) to dental patients in a clinical setting in a safe and effective manner. Describe a protocol for management of emergencies in the dental office and list and discuss the emergency drugs and equipment required for the prevention and management of emergency situations. Discuss principles of advanced cardiac life support or an appropriate dental sedation/anesthesia emergency course equivalent. Demonstrate the ability to diagnose and treat emergencies related to the next deeper level of anesthesia than intended. Patient evaluation and selection through review of medical history taking, physical diagnosis, and psychological considerations. Definitions and descriptions of physiological and psychological aspects of anxiety and pain. Description of the sedation anesthesia continuum, with special emphasis on the distinction between the conscious and the unconscious state. Pharmacology of local anesthetics and agents used in moderate sedation, including drug interactions and contraindications. Patient monitoring using observation and monitoring equipment, with particular attention to vital signs, ventilation/breathing, and reflexes related to consciousness. Maintaining proper records with accurate chart entries recording medical history, physical examination, informed consent, time-oriented anesthesia record, including the names of all drugs administered including local anesthetics, doses, and monitored physiological parameters. Prevention, recognition, and management of complications of venipuncture and other parenteral techniques. Prevention, recognition, and management of systemic complications of moderate sedation, with particular attention to airway maintenance and support of the respiratory and cardiovascular systems. Documentation of Instruction: the course director must certify the competency of participants upon satisfactory completion of training in each moderate sedation technique, including instruction, clinical experience, managing the airway, intravascular/intraosseous access, and reversal medications. Faculty: the course should be directed by a dentist or physician qualified by experience and training. This individual should possess a current permit or license to administer moderate or deep sedation and general anesthesia in at least one state, have had at least 3 years of experience, including formal postdoctoral training in anxiety and pain control. Dental faculty with broad clinical experience in the particular aspect of the subject under consideration should participate. In addition, the participation of highly qualified individuals in related fields, such as anesthesiologists, pharmacologists, internists, cardiologists, and psychologists, should be encouraged. A participant-faculty ratio of not more than four-to-one when moderate sedation is being taught allows for adequate supervision during the clinical phase of instruction.
Discount indapamide 1.5mg online
Remifentanil differs from other -receptor agonists in that it is metabolized by esterases located in the systemic circulation; other agents are hepatically metabolized blood pressure chart dr oz discount indapamide express. Ultiva (Bioniche Pharma): (remifentanil) 1-mg/3-mL vial, 2-mg/5-mL vial, and 5-mg/10-mL vial. The use of alfentanil and sufentanil in general anesthesia has been evaluated in depth121,122; they are quite well accepted, especially for short surgical procedures. Alfentanil has received considerable attention in dentistry and other outpatient surgical procedures. Remifentanil is an opioid agonist for use during general anesthesia and monitored anesthesia care. New steady-state concentrations occur within 5 to 10 minutes after changes in infusion rates. Remifentanil is useful in attenuating the hemodynamic response to intubation and helps maintain cardiovascular stability during anesthesia. Remifentanil alone does not provide reliable amnestic effects or adequate anesthetic depth for general surgery; the concurrent use of inhaled anesthetics and/or hypnotics is required. The respiratory-depressant effects of remifentanil must be taken into consideration when given to critically ill patients. Remifentanil has analgesic effects and may be used in pain management of intensive care and postoperative patients; however, the injection is rarely given for extended periods. In the 1960s success was attained with the introduction of pentazocine, the first drug with both opioid agonist and opioid antagonist properties to be marketed (1967). Pentazocine the chemical formula for pentazocine is 1,2,3,4,5,6-hexahydro6,11-dimethyl-3-(3-methyl-2-butenyl)2,6-methano-3-benzazocin-8-ol lactate. Pentazocine was introduced in 1967 as a nonnarcotic opioid in both oral and parenteral formulations. Pentazocine initially gained some popularity within dentistry as an alternative to the opioid agonists. It is therefore usually administered after the patient has received one or more drugs. When titrated slowly, the usual dose required (in combination with other drugs) for sedation is approximately 20 mg. Warnings Despite early claims to the contrary, experience with pentazocine has demonstrated that both psychological and physical dependence can develop. For routine outpatient sedation in the dental setting, there is rarely an indication for pentazocine administration in pregnant patients. Another significant untoward effect of pentazocine is the occurrence of acute neuropsychiatric manifestations, such as visual hallucinations, disorientation, confusion, mental depression, disturbing dreams, and dysphoria. Management of reactions that do occur is symptomatic, with vital signs monitored and recorded regularly during the reaction, although stimulation of the receptor will produce these same responses. Readministration of pentazocine to this same patient at future dates should be avoided, if possible, to minimize the possibility of recurrence. The administration of pentazocine to patients younger than 12 years is not recommended because of a lack of clinical data. The drug package insert for pentazocine recommends that ambulatory patients receiving parenteral pentazocine be cautioned not to operate machinery, drive cars, or unnecessarily expose themselves to hazards. Each mL contains pentazocine lactate equivalent to 30 mg base and 2 mg acetone sodium bisulfite, 1. The chemical incorporates the molecular features of the opioid agonist oxymorphone hydrochloride (Numorphan) with that of the opioid antagonist naloxone hydrochloride (Narcan). In clinical practice, nalbuphine is considered equianalgesic to morphine when administered in equal doses. Its duration of action is slightly longer than that of morphine (approximately 3 to 6 hours). A 10-mg dose of nalbuphine is equivalent to approximately 50 to 75 mg of meperidine. Patients with extensive liver disease appear to exhibit a greater number of adverse side effects from the usual clinical dose, a response indicating a decreased rate of metabolism of the drug by the liver. Pentazocine should be administered with caution to patients with seizure disorders. Nalbuphine possesses ceiling effects for respiratory depression, whereas its analgesic effects may become more pronounced with increasing doses. Gal et al demonstrated a plateau effect for both respiratory depression and analgesia for nalbuphine in doses up to 0. Nalbuphine therefore possesses a ceiling effect on both the degree and the duration of respiratory depression. This is in contrast to butorphanol, which has a ceiling effect only on the degree of respiratory depression, not its duration. Romagnoli and Keats considered nalbuphine an ideal drug for patients with heart disease because it was devoid of hemodynamic effects except those associated with the relief of pain and anxiety. One of the potential benefits of the opioid agonist-antagonist analgesics is a limited or absent drug dependence and abuse liability. They noted a dramatic reversal of respiratory depression and a restoration of normal ventilation within 5 minutes. Of greater importance is that nalbuphine provided substantial analgesia after reversal of the opioid-induced respiratory depression, which extended well into the postoperative period. The drug undergoes metabolism in the liver; oral doses of nalbuphine undergo a significant hepatic first-pass effect, and only 20% of an orally administered dose is biologically available. Nalbuphine cannot, however, be combined with diazepam because a milky white precipitate forms. Adverse Effects When nalbuphine is used solely as an analgesic, the most frequently noted adverse effect is sedation, which is reported in 36% of patients. Other common adverse responses (occurring in more than 3% of patients) include the following: Sweaty, clammy feeling Nausea and vomiting Dizziness, vertigo Dry mouth Headache 9% 6% 5% 4% 3% Overdose Overdose of nalbuphine is exceptionally rare but possible. Contraindications In the dental outpatient environment nalbuphine is contraindicated for use in patients who are allergic or hypersensitive to it. When the pure opioid agonists (morphine, meperidine, and fentanyl) are administered, both the rate and depth of respiration are depressed in a dose-related manner until apnea occurs. Pregnant patients should not receive nalbuphine unless the advantages of its administration clearly outweigh its potential disadvantages. Because nalbuphine is metabolized in the liver and excreted through the kidneys, it is possible that patients with impaired hepatic or renal function may overrespond to usual dosages. Dosage When administered intravenously, nalbuphine should be titrated to clinical effect. When nalbuphine is administered after diazepam or midazolam, the depth of sedation is rarely increased. However, recovery from sedation is somewhat less complete than that observed when diazepam or midazolam is administered alone. It is only at dosages considerably greater than these that the ceiling effect on respiratory depression is noted. In doses up to 10 mg of nalbuphine, the degree of respiratory depression should not be profound, but will be equivalent to that induced by 10 mg of morphine or 50 to 75 mg of meperidine. The chemical formula of butorphanol is levo-N-cyclobutylmethyl-6,10, -dihydroxy-1,2,3,9,10,10-hexahydro-(4H)-10,4iminoethanophenanthrene tartrate. Maximum blood levels occur in 5 minutes and thereafter decline in a biphasic manner. The major route of elimination of butorphanol and its metabolites is through the kidney (75%), with biliary excretion accounting for 15% of the dose. Butorphanol is highly lipid soluble and concentrates in adipose tissue and excretory organs. Other common side effects were as follows166,173: Floating, pleasant feelings Nausea Clamminess, sweating Headache Vertigo Dizziness Lethargy 7% 7% 5% 2% 2% 2% 2% Effect on Respiration Butorphanol has properties similar to those of pentazocine and nalbuphine with respect to respiratory depression and opioid antagonist properties. This and other studies have demonstrated that butorphanol does not produce a dose-related effect on respiration in contrast to that observed with opioid agonists, such as morphine and meperidine. Increasing doses of butorphanol did, however, produce a longer duration of respiratory depression, although the degree of depression did not increase.
Generic indapamide 2.5 mg online
A patient with histrionic personality disorder saw a robed figure at the foot of her bed lifting his index finger to his mouth to caution her to silence arrhythmia unspecified icd 9 code cheap indapamide 2.5mg mastercard. The image was sharp and vivid but was recognized as being seen with the inner eye. The patient knew that the figure was not at the foot of the bed and that other people in the room could not see him. When she tried to relate the figure in space to the background of her field of vision, in this case the walls and curtains of the room, she realized that she could not do so; it had no definite location in external space, that is, outside herself. To summarize, the significance of hallucination is that it almost always denotes a morbid mental state. The significance of pseudohallucination is in its differential diagnosis from hallucination, as pseudohallucination is not necessarily psychopathologic. The experience concerns how the individual regards the boundaries of self and is discussed further with other disorders of self-image. Dening and Berrios have reviewed 56 cases, 53 from the literature and three of their own. Males predominated, with a ratio of two to one, and the mean age of subjects was 40 years. Both neurologic and psychiatric disorder occurred in about 60% of cases (different subjects), with epilepsy in approximately one-third. Decreased consciousness occurred in 45%, delirium in 18% and 9% of subjects were dead within 1 year. Visual imagery or narcissism was present in one-third of subjects, and depersonalization in 18%. Almost always, the subject saw his own face; quite often, he was lying in bed at the time. This subjective experience was complex, with different components and causes rather than unitary. Negative autoscopy has also been described, in which, for instance, the patient looks in the mirror and sees no image at all. They are not of diagnostic importance, as they occur in schizophrenia, epilepsy and other organic states and also as hypnagogic hallucinations in healthy people. The phenomenon is quite definitely experienced as a perception by the patient and not just as a belief or an idea. According to Zilboorg and Henry (1941), hypnagogic hallucinations were first mentioned by Aristotle. It is known that the consciousness level fluctuates considerably in different stages of sleep, and both types of abnormal perception probably occur in a phase of increasing drowsiness: the structure of thought, feelings, perceptions, fantasies and, ultimately, self-awareness becomes blurred and merges into oblivion. They are also described with narcolepsy, cataplexy and sleep paralysis to form a characteristic tetrad of symptoms (see Narcolepsy for descriptions). Toxic states such as glue sniffing, acute fevers (especially in children), postinfective depressive states and phobic anxiety neuroses are other conditions that may be associated with these perceptions. The importance of these phenomena in psychopathology is to recognize their nature and realize that they are not necessarily abnormal, even though they may be truly hallucinatory. A schizophrenic patient heard hallucinatory voices only when water was running through the pipes of his ward. He heard no phonemes for most of the time, but when he heard water rushing through the pipes along the wall, he became very distressed by voices that told him to damage himself. He was terrified of the content of these voices because he was afraid he might act on them. He could readily separate the noise of water from the voices, and the latter never occurred apart from the former, but both perceptions were recognized as distinct and real. Another patient heard voices when the radio or television was switched on, alongside the broadcast voices; he had persecutory delusions that these activities were carried out deliberately to upset him and he became very distressed, and at times violent, as a result. The patient saw and heard the 7 Pathology of Perception 101 act of writing and was quite sure that it accounted for the tactile sensation in her abdomen. A stimulus in one sensory modality producing a hallucination in another is called a reflex hallucination. This is, in fact, a hallucinatory form of synaesthesia, mentioned earlier as the experience of a stimulus image in one sense modality simultaneously producing an image in another, for example, the feeling of discomfort caused by seeing and hearing somebody scratch a blackboard with their fingernails. Another reflex hallucination occurred in a woman who experienced pain whenever certain words were mentioned. Functional and reflex hallucinations are not themselves of diagnostic or theoretical significance, but they require mentioning for completeness and recognition to identify other more important symptoms with confidence. In cases of hemineglect, there has been interest in whether the observed deficits in imagery are due to inattention or to impairment of mental imagery. Bisiach and Luzzatti (1978) described abnormalities in individuals with hemineglect. Their patients were asked to describe the Piazza del Duomo in Milan from two standpoints: facing the cathedral and with their backs to the cathedral. From both standpoints, the subjects were unable to describe the right side of the scene despite having correctly described it from the previous standpoint. In other words, even in imagination the mental representation of the piazza was unilaterally deficient for the right side. For the first time, this showed that without hemineglect, that is, visual inattention for space, failure of imagery was still possible. The field of sensation varies all the time as individual sensations in different modalities from the outside world and from inside oneself compete for attention. The essential nature of sensation has been explored by studying its absence, as revealed by research on the effects of sensory deprivation (Zubek, 1969). This topic is only given brief mention, as it is somewhat peripheral to psychiatry. Sensory deprivation was studied using Canadian college students as volunteers (Bexton et al. The subjects, wearing translucent goggles and gloves with cardboard cuffs, lay on a bed in a light but partially soundproof room; there was a continual background noise. This experience was found to be extremely unpleasant and, despite being paid, subjects were not prepared to remain in this state for more than 3 days. This technique has been refined subsequently to blot out external sensations more completely. Depending on the completeness of deprivation of other sensations, abnormal perception occurs in modalities other than vision. Subjects show an altered affective state: they become panicky, restless, irritable or, alternatively, bored and apathetic. Despite considerable neuropsychological research with valuable findings for investigating the sensory environment in growth and development, developing brain interconnections, neurochemistry and neurophysiology, the study of sensory deprivation has not so far made as big an impact on descriptive psychopathology as was initially expected. What part of the effects of deprivation is due to failure of development and what to loss of behaviours already established How can one extrapolate from the experience of normal individuals in a highly abnormal environment to those who are psychiatrically ill Many studies in sensory deprivation are described by Riesen (1975), who links the experimental data to neurologic function and development. The distinction has been made between sensory deprivation and perceptual deprivation. Persistent auditory hallucinations: coping mechanisms and implications for management. Alloaesthesia without impairment of consciousness after right putaminal small haemorrhage. Reinforcement of vocal correlates of auditory hallucinations by auditory feedback: a case study. Cognitive vulnerability to auditory hallucinations: impaired perception of memory. Fantasy is often used as a means of reducing the unpleasant affective component of sensory deprivation. The subject may become disoriented and show increasing difficulty with problem solving and concentration.
Discount indapamide uk
It is understandable that surgeons would decry the use of anesthesia blood pressure ranges for athletes buy indapamide online, particularly when it was not readily available to all surgeons, some of whom witnessed their patients gravitating to competitors who could offer the administration of anesthesia. In 1859 a physician at a public meeting opined that "[p]ain is the wise provision of nature, and patients ought to suffer pain while their surgeon is operating; they are all the better for it, and recover better. Haggard opined that "the very suffering which a woman undergoes in labor is one of the strongest elements in the love she bears for her offspring! Organized dentistry was not shy about speaking to , for instance, both sides of the debates about darwinian theories of the origin of species. Reminiscent of the medical science fiction in television and motion picture versions of Star Trek, the Dr. Anesthesiology was a regularly discussed, if not debated, topic in the Dental Cosmos. Dentist Charles Teter argued for the preeminence of nitrous oxid [sic] as the agent of choice for dental procedures, stating: "I am sure that in the judgment of the thoughtful, experienced man there can be no favorable comparison" (with nitrous oxide with any other agent). Of course, techniques of nitrous oxide administration differed somewhat from those recommended today. Teter advised that "this gas must be given at least 80 per cent pure" (oxygen could be added for longer cases). Teter also supplemented his nitrous oxide with the "intelligent use of preanesthesia narcotics, such as morphin [sic], atropin [sic], and scopolamin [sic]. If the dentist is not capable of anesthetizing his patient and keeping him anesthetized to the completion of this work, he should send his patients to one more competent. Teter admonished that "[t]here is an increasing demand for general anesthetics in dental surgery" and "[t]he time is soon coming in this country when there will be laws passed to restrict the administration of anesthetics, and it behooves the dental profession to see that the subject is given a prominent place in the curriculum of our colleges. Unless this is done, the dental profession will be greatly humiliated by having the right to administer anesthetics annulled. Guido Fischer of the University of Greifswald, Germany, who argued for the use of local anesthesia in dentistry. Fischer proposed: "The efforts of modern medicine are more and more concentrated upon an endeavor to limit general anesthetics as much as possible, and to have local anesthetics take their place, by the endeavor to develop these to the highest perfection. Local anesthesia is also commonly used by specialists, and most surgical procedures can be performed with local anesthesia only. In the early twentieth century, dental anesthesia services continued to be provided by a cadre of dentists, but the profession as a whole began to gravitate to the administration of local anesthesia for almost all dental procedures. Fisher opined: "In dentistry local anesthetics should be the only kind used, and one should resort to general anesthetics only in exceptional cases. Fischer never defines "exceptional," he does admit that "obstinate or timid" patients may need to be narcotized with ether or ethyl bromid [sic]. Also: "There is one inconvenience which still attaches to cocain, viz, its often very toxic influence on the living tissues. Patients did so despite the condemnation of anesthesia by professional society spokespersons after controversial dental entrepreneurs, such as Gardner Q. Parker believed that patients avoided dentistry because of pain, ignorance, procrastination, and lack of money, and of these, fear was the strongest deterrent. He aggressively advertised his services, reportedly removed 357 teeth in 1 day on a vaudeville stage, and coincidentally developed 30 West Coast dental offices that grossed more than $3 million annually in the early twentieth century. Not surprisingly the profession gradually began to embrace anesthesia not only as a morally acceptable form of therapy but also one that would attract patients. It can be argued that what set the exodontists apart from other generalists who also removed teeth was the provision of pain control modalities, other than local anesthesia, administered as single-operator anesthetists. Many members of the American Society of Exodontists became very proficient at removing a great number of teeth in the time it took a patient administered 100% nitrous oxide to regain normal skin color after intentionally induced cyanosis. A case can be made that the provision of general anesthesia by the exodontists is what directly led to the development of the specialty of oral and maxillofacial surgery. Hubbell started a postdoctoral course of training that would include 2 years of surgery and an additional year of general anesthesia. Hubbell experimented with sodium thiopental and found it to be a wonderfully appropriate drug for oral surgery that had advantages over techniques such as 100% nitrous oxide. In addition, at times dentists found that they were unable to gain staff privileges at hospitals because of a prejudicial requirement for medical school training. Many oral surgeons predictably began providing the anesthesia needed and demanded by their patients in their own offices. Beginning in the 1930s, oral surgeons developed not only the first outpatient surgical centers (a concept not embraced by medicine until the 1970s), but also became the experts at single-operator anesthetist procedures, a technique that is a recognized standard of care today. Participating in a more limited fashion in these residency programs were hospital-based oral surgery residents who spent at least 3 months of their residencies training with anesthesia residents. This group would be composed of dentists who had 2 or more years of full-time training in anesthesiology. Their purpose in part was to establish advanced programs for continuing education in pain and anxiety control for dentistry and pursue the development of a specialty in anesthesiology in dentistry. In 1952 as the medical specialty in anesthesiology grew, dentistry began to believe that the role of anesthesiology in dentistry might be threatened. Kinney suggested the development of a society for those interested in all forms of pain control for dental patients. According to the paper, office-based oral surgery anesthesia had one death per 432,000 anesthetics. Dentist graduates of these programs were trained equivalently to their physician colleagues and provided anesthesiology services for the full scope of surgical procedures. There is no question that an alleged advantage medical anesthesiologists will trumpet is the additional safety available from a dedicated anesthesia provider rather than a single-operator anesthetist who provides both anesthesia and surgical services. This is despite the fact that no studies have ever shown such to be true and have shown that single-operator anesthetist office-based oral and maxillofacial procedures are historically safer than comparable hospital-based procedures. Although the surgical duration of these anesthetics was often very brief, the sheer average number of cases provided by individual oral surgeons was significantly more than the vast majority of any other type of anesthesia provider. The purpose of the study was to combat those who were perceived as planning to take away traditional oral and maxillofacial surgery office anesthesia. Similarly, state dental boards now also require the successful completion of an in-office examination before issuing a permit to dentists desiring to administer sedation or general anesthesia to their patients. However, without a specialty in anesthesiology in dentistry in Great Britain, there were no advanced training opportunities for dentists. As a result of the Poswillo report, dentists in Great Britain now have lost the ability to administer general anesthesia. Whereas the Poswillo report and its adverse sequelae were frightening revelations to dental anesthesia providers in most of the United States, the information was all old news to dentists in Alaska, who had lost their privilege as single-operator anesthetists in the 1970s. Courts routinely found that anesthesia care is the practice of medicine, but is also the practice of dentistry, nursing, and even veterinary medicine. Single-digit losses in the house prevented dentistry from having a specialty in anesthesiology. In 1999 five of the six mandatory requirements for specialty recognition were met, but, interestingly, the house did not believe that there was a sufficient "need or demand" for recognized anesthesiology-mediated advanced pain control services in dentistry. First, the profession also subsequently successfully opposed an effort to amend the Oregon constitution to allow any person to advertise, providing the advertisement was true. For instance, dentists have had to fight many battles within state legislatures to provide anesthesia and other services,91 which they are trained to do. Dentist anesthesiologist Gaither Everett was forced to litigate and appeal his right to practice as a dentist anesthesiologist in the state of Washington to the Washington Supreme Court. Finally, in 2013 the federal government issued a singular dentist anesthesiologist taxonomy number (1223D0004X). Similar to controversies regarding dental amalgam, which would likely never be accepted with the techniques and materials that are available in the twenty-first century, the historical oral and maxillofacial model of anesthesia delivery remains unsurpassed as far as cost effectiveness and relative safety for patients who undergo similar procedures within the hospital environment. There also exists a group of dentists who provide intravenous sedation during which the practitioners assiduously avoid doses of drugs that would render patients not only unconscious or apneic, but simply nonresponsive to verbal communication or without adequate spontaneous ventilation. Dentists who provide intravenous sedation are the least controversial of the factions with an interest in advanced pain control in dentistry. Three or 4 months of incidental anesthesia training within a surgical specialty does not equate with 2 or more years of a dedicated residency in anesthesiology.
Diseases
- Epidermolysa bullosa simplex and limb girdle muscular dystrophy
- Juvenile myoclonic epilepsy
- Hereditary type 2 neuropathy
- Oncocytoma
- Prolymphocytic leukemia
- Vitamin E familial isolated, deficiency of
- Foreign accent syndrome
- Weaver-like syndrome
- Pseudohermaphroditism
- Croup
Discount 2.5 mg indapamide with visa
Monitoring devices are applied blood pressure joint pain buy 1.5 mg indapamide fast delivery, supplemental O2 and local anesthetic are administered, and the procedure is started. Extrapyramidal reactions, especially tardive dyskinesia, are not uncommon side effects of the phenothiazines (promethazine and chlorpromazine). Should these develop, management requires the administration of diphenhydramine (see Chapter 7). Maximum effects are seen in 20 to 60 minutes, with a recovery time of 2 to 6 hours. As with all parenteral sedation techniques, monitoring is essential to patient safety. Inhalation Sedation Inhalation sedation with N 2O-O2 remains the most used technique of sedation, as well as the most nearly ideal sedation technique for pediatric dentistry. In a survey of pediatric dental residents and pediatric dentists in the United Kingdom, Woolley et al found that inhalation sedation was the preferred technique of 98% of practicing pediatric dentists and 97% of pediatric dental residents. The major difficulties encountered with this technique in children are twofold: first, the lack of potency of N2O-O2 may render the technique ineffective in the management of the more apprehensive patient; and second, some children will object to the placement of the nasal hood. The patient may be attempting to move his or her face away from the nasal hood and be crying or screaming; however, the patient will be receiving a high concentration of N2O (not 70% because of significant air dilution) at this time. The nasal hood should be maintained close to , but not on, the face for a few moments until the child quiets. At this time, the percentage of N2O must be lowered to approximately 25% to 30% and then titrated to an appropriate level for the patient. One of the more unpleasant problems when N2O-O2 is used in pediatric patients is vomiting. Though uncommon, the incidence of vomiting in pediatric patients is significantly greater than that seen in adults. Mouth breathing decreases the volume of N2O being inhaled and lessens the level of sedation. I highly recommend its application whenever inhalation sedation (or for that matter any sedative technique) is used. Another method, used in the absence of a rubber dam, is to tell the mouth-breathing patient that some "special water" is being placed into their mouth and that he or she cannot swallow it. To keep the water in the mouth, the patient will have to raise his or her tongue to the roof of the mouth, thereby eliminating mouth breathing. The first may be used with a patient who is somewhat cooperative and is able and willing to communicate with the dentist. The younger child may be unable to understand the terms usually used to describe the sensations associated with N2O for the adult patient. Playing a game with the child is an effective means of determining the level of sedation. As the child inhales through this space mask, the "astronaut" will begin to float in space. Questioning the child about his or her feelings can help determine the level of sedation. The second technique is used in situations in which the apprehensive child is less communicative. The eyelids of the patient begin to close, and the patient may yawn administration of N2O-O2 (see Chapter 15) to meet more realistically the requirements of the pediatric patient. Inhalation sedation was, by a significant margin, the most recommended technique of sedation for pediatric patients when administered by general dentists and pediatric specialists, in a survey of dentist anesthesiologists. Concentrations of N2O required to provide clinically adequate sedation in the child who readily accepts the nasal hood are virtually identical to those seen in adults. The overwhelming majority of children receiving N2O-O2 are adequately sedated at concentrations between 30% and 45% N2O. Screaming and crying patients will breathe through their mouths to a much greater degree than is usual and therefore do not receive as great a volume of N2O being delivered through the nasal hood. As illustrated in the figure, the patient is rather young and has been placed in a physical restraint. This process may need to be repeated throughout the dental treatment in some patients. The patient who does not permit the nasal hood to be placed on the nose poses a greater challenge. The following technique will, however, provide the dentist with an increased chance of success. When the dentist believes that the patient is adequately sedated, treatment is attempted. As discussed in Chapter 28, I believe that there is potential risk involved in this procedure if used by the inexperienced dentist who is not trained in recognizing unconsciousness and in airway management. When adequate operating room and outpatient moderate and deep sedation experience and training have been received. Adequate monitoring of the patient, especially of the respiratory system, is essential. N2O-O2 must always be titrated; fixed concentrations should never be administered to all patients because not all patients react in the same manner. Both the amount and type of food ingested must be considered when determining an appropriate fasting period. Although this technique of drug administration is the most reliable and, when used as described, very safe, its use is seldom taught in pediatric dentistry residency programs. Other techniques such as inhalation or oral sedation, either alone or in combination, will likely provide a successful outcome. When administered via these routes, the benzodiazepines have a fixed, somewhat short duration of clinical action (<1 hour). Following a pretreatment visit at which the patient is thoroughly evaluated (medically, dentally, and psychologically) for suitability for sedation and after presedation instructions are given to the parent or guardian, the patient returns to the dental office for treatment. The patient is monitored continuously (via pulse oximetry) during this induction period. At 10 or 15 minutes the patient is placed into the dental chair, enveloped in a physical restraint, and inhalation sedation added (30% to 50% N2O). The patient is usually somewhat cooperative but perhaps not relaxed enough to permit the dental treatment to commence. However, in many situations the patient is not yet cooperative as the stimulation of treatment starts. Cardiovascular function and airway patency (blood pressure, heart rate and rhythm, respiratory rate, and O2 saturation) are satisfactory and stable. For a very young or handicapped child incapable of the usually expected responses, the presedation level of responsiveness or a level as close as possible to the normal level for that child should be achieved. The pediatric patient shall be accompanied to and from the treatment facility by a parent, legal guardian, or other responsible person. It is preferable to have two adults accompany children who are still in car safety seats if transportation to and from a treatment facility is provided by one of the adults. Fentanyl is occasionally administered to aid in sedation and when a degree of analgesia is desirable at the conclusion of the dental procedure. Immediately (20 to 30 seconds) before the administration of a palatal local anesthetic, a dose of 5 to 10 mg of propofol is injected as a bolus. Increments of 10 mg of propofol enable the procedure to be completed successfully without prolonging the recovery period to any significant degree. At the completion of treatment, the patient receives 100% O2, the room lights are turned on (to stimulate the patient), and the dental chair is positioned to make the patient somewhat uncomfortable. The goal at this time is to stimulate the patient to hasten their recovery and discharge. When recovery is deemed adequate (see following discussion), the patient is dismissed in the custody of a parent or guardian. This technique should be used only by persons well trained in deep sedation, general anesthesia, and airway management. The patient postsedation score must be approximately equal to the baseline (presedation) score.
Buy indapamide cheap
Religious delusions may be grandiose in nature blood pressure 60 0 discount indapamide master card, for example, a patient in the United Kingdom who believed that she was an emissary of God to the Birmingham Housing Department. So religious delusions are not caused by excessive religious belief or by the wrongdoing that the patient attributes as cause, but they simply accentuate that when a person becomes mentally ill his delusions reflect, in their content, his predominant interests and concerns. Sometimes, it can be difficult to make the distinction between religious delusion and the experience of an unusual religious belief or practice. Affective illness may be followed by the killing of children by depressed mothers or the killing of their wife or sometimes also children by husbands; suicide may follow immediately or later (Higgins, 1990). An elderly woman spent the day rushing round the house wringing her hands and telling her worried family that she was wretched, worthless and only deserved to die. When it was suggested to her that she come into hospital, she assumed that she would be killed on arrival, and she asked whether this could take place there and then so that she could receive her just desserts. Nihilistic delusions are the reverse of grandiose delusions, in which oneself, objects or situations are expansive and enriched; there is also a perverse grandiosity about the nihilistic delusions themselves. Feelings of guilt and hypochondriacal ideas are developed to their most extreme, depressive form in nihilistic delusions. Hypochondriacal delusions may also occur in schizophrenia and have the characteristics of other schizophrenic ideas. Thus a patient believed that his bodily functions were being interfered with by rays emitted from a planet and that this was part of a plot to control his thoughts and behaviour. Hypochondriacal delusions are discussed further in association with hypochondriasis in Chapter 14; however, other features of hypochondriasis, such as bodily preoccupation, disease phobia and conviction of the presence of disease with nonresponse to reassurance, are in fact more common than delusion (Pilowsky, 1967). Facial pain is described in Chapter 15 and other delusion-like ideas and overvalued ideas of the body in Chapter 14. Hypochondriacal delusions are commonly associated with delusional disorder in the International Classification of Diseases, 10th revision (previously known as paranoia; World Health Organization, 1992). Munro (1988) has described delusional disorder as an encapsulated monodelusional disorder with several subtypes, such as erotomanic, grandiose, jealous, persecutory, somatic and unspecified; the concept has developed from the older term paranoia (Munro, 1997). He has described the somatic type as monosymptomatic hypochondriacal psychosis and, of 50 cases, the three main groups were: 1. In a factor analysis of the features of delusional disorder, four independent factors were identified, suggesting considerable heterogeneity of the condition (Serretti et al. The first factor incorporated core depressive symptoms, which may be either a depressive syndrome reactive to stresses deriving from delusional 8 Delusions and Other Erroneous Ideas 121 ideation or a comorbid mood disorder, or both. The complaint was always presented with great intensity, and patients were utterly convinced of the physical nature of the disorder. Hypochondriacal delusions may also occur with administration of drugs, both prescribed and those of abuse. Koro (Lapierre, 1972) is an unusual condition that has been described as an example of hypochondriacal delusion. Yap (1965) describes this as a culture-bound depersonalization syndrome and considers it to be a manifestation of acute anxiety associated with folk beliefs concerning sexual exhaustion. It has occurred in epidemic proportions among Malays in Singapore (Gwee, 1963) but has also been described in individual cases in a French Canadian (Lapierre, 1972), in a West Indian, a Greek Cypriot (Ang and Weller, 1984) and in an Englishman (Berrios and Morley, 1984). This suggests that the belief is based on physiologic changes that are likely to be due to anxiety. In essence, the penile change is similar to tachycardia, hyperhidrosis or other features of sympathetic arousal associated with anxiety. A group of patients who in some respects are intermediate between those suffering from somatic delusions and delusions of infestation are those who were described by Videbech (1966) as suffering from chronic olfactory paranoid syndromes; these have also been referred to as having olfactory reference syndrome (Pryse-Phillips, 1971). Characteristically, these patients have a fixed and unalterable belief that they smell but do not have hallucinations or other olfactory experience. There is a severe phobic reaction, with the behaviour of other people interpreted as finding their smell offensive and aversive. Delusions of Infestation Delusions of infestation have been described by Hopkinson (1970) and by Reilly (1988). It is probably most common as a symptom of circumscribed hypochondriasis in affective psychosis, along with other depressive symptoms, but it also occurs in paranoid schizophrenia, in monosymptomatic hypochondriacal psychosis (delusional disorder), in organic brain syndromes or with neurotically determined conditions. Patients have believed that they had a spider in their hair, worms and lice beneath the skin or infestation with various insects. The delusion may be accompanied by other depressive delusions or overvalued ideas of being dirty, guilty, unworthy or ill. These delusions may also occur in schizophrenia, in which condition they characteristically take on a bizarre character and are accompanied by other schizophrenic symptoms. A 49-year-old mother of four children, one of whose sons had developed a schizophrenic illness, complained of recurrent pain in her vagina that she explained as being caused by a parasite that had migrated from her stomach, where it had been responsible for epigastric pain diagnosed earlier as hiatus hernia (McLaughlin and Sims, 1984). She described the parasite as wandering through her bloodstream and as having been responsible for various aches and pains she had experienced in the past. She related having passed multiple small red worms and worm casts in her faeces and, on one occasion, a two-inch green frog. Delusions of infestation may occur in organic states with tactile hallucinations, in delirium tremens during alcohol withdrawal and in cocaine addiction. They may be described in cerebrovascular disease, in senile dementia and in other brain disease, and they have been ascribed to disorder of the thalamus. Overvalued ideas and delusion-like ideas of infestation sometimes occur in people with personality disorder of anankastic or paranoid type with no psychotic illness. Sometimes, the condition is precipitated by a skin disease and becomes a delusional elaboration of existing tactile symptoms. It has been suggested that the symptom develops in stages: first, abnormal cutaneous sensation; then an illusion develops; and finally, the fully formed delusion of infestation occurs. As mentioned earlier, delusional infestation is now viewed as one form of delusional disorder, in particular being a subtype of monosymptomatic hypochondriacal psychosis. Occasionally, a delusion (delusional intuition) is transferred from a psychotic person to one or more others with whom they have been in close association, so that the recipient shares the false belief: the principal acquires the delusion first and is dominant, the associate becomes deluded through association with the principal. The associate is usually socially deprived or disadvantaged, mentally or physically. Separation of the pair is often followed by remission of symptoms in the associate. In folie induite, a person who is already psychotic adds the delusions of a closely associated person to his own. It has been considered that the principal is always psychotic (Soni and Rockley, 1974), but the associate may or may not be psychotic. It is also not of any particular clinical value, and the psychopathologic differences are questionable (Hughes and Sims, 1997). He claimed that employees of the firm had been following him everywhere and interfering with his own house. His wife believed this story initially and produced supposedly corroborative evidence. A year later, following his inpatient treatment, she no longer accepted the plot and she believed her husband to be mentally ill.
Cheap indapamide 2.5mg with mastercard
An example of this relationship would be when one is called to an emergency room to treat a trauma victim blood pressure chart while exercising order indapamide 2.5 mg. Dentists are allowed relatively wide latitude in what is reasonable therapeutic intervention in these scenarios. This latitude may even be legislated at times, for instance, by granting dentists in these situations sovereign immunity, or the same protection the king (state or federal government) enjoys from prosecution in the promulgation of duties. Specifically, one needs to consider emergencies that occur during elective procedures for known patients in the private dental office. However, when the circumstances include an emergency, the guidelines present are less defined because of the unexpected presentation of the problems that need to be immediately addressed. Examples abound wherein reasonable standard-of-care decisions were made throughout a case in which a bad result occurred. Additionally, patients generally are resilient, and poor clinical decisions do not always lead to adverse outcomes. However, it has been proposed that three basic types of errors can lead to the development of critical situations that otherwise could be prevented. But emergencies may occur secondary to dentists who have extended themselves beyond their routine experiences in medical or surgical therapy. It is never optimal to routinely perform surgical or therapeutic procedures one is not thoroughly familiar with. One legitimate circumstance for such an extension would be when dealing with an emergency. Even if one desires to simply maintain status quo licensure, continuing education is usually mandated by most state professional boards. The lesson to be learned is if one is not experienced in providing a certain elective treatment, perhaps that treatment should be deferred. The second commonly found error is a lack of information for the situation at hand. The third source of poor decisions is due to a lack of aggressiveness when something amiss is noted. As an example, at what blood pressure does one become concerned enough to alter routine treatment protocol An example of the third type of poor decision might be demonstrated by alleged conduct reported in March 2008 that led to the closing of multiple southern Nevada endoscopy centers, loss of physician and nursing professional licenses, development of individual and class action civil lawsuits involving more than 40,000 patients, and criminal investigation of those health professionals involved in the situation. According to a Clark County Health District press release, the centers were initially closed because of unsafe injection practices (using the same syringe on multiple patients). A foreseeable result or consequence is one that the reasonable man would expect might occur. Contrarily an unforeseeable result is one that a reasonable man would not expect to occur. For instance, one might reasonably expect inflammation after a surgical procedure, such as the intraoral administration of local anesthetic. However, one would generally not foresee that a patient would typically lose vision after local anesthetic administration for dentistry, although the phenomenon has been reported. This statement is obviously true, but the mere foreseeability of a single life-threatening event sometime during decades of practice does not make that event, when and if it ultimately occurs, expected. Certainly, if dentists routinely expected to be faced with life-threatening events in their offices, the entire nature of the profession would have to change. However, even the most careful practitioner through no fault of his or her own will, given a long enough career, experience emergency situations. So many factors play a part in the judicious practice that it would be impossible to discuss them in a single text, let alone a chapter. Prevention and Preparation Carefully review the prevention and preparation recommendations elsewhere in this text. Following the admonitions therein Respondeat Superior Respondeat superior (let the superior reply) is the legal doctrine that assigns liability for employee conduct to the employer. Even if the dentist is well trained in dealing with various emergencies, if his staff is not trained for their concomitant duties, optimal emergency treatment will be compromised. Perceived or real emergencies may arise after normal office hours, and one must make reasonable arrangements to properly deal with such situations. Not surprisingly, in the wake of the developing investigation about unsafe injection practices in southern Nevada in March 2008 (see "Poor Decisions" previously), local area hospitals began to distribute guidelines for safe needle and syringe use. Just as it seems health professionals must constantly be reminded about basic concepts, such as hand washing, those using instruments necessary for intravenous sedation or any other treatment must use those instruments in a safe fashion. Malamed, occasionally asks a series of relevant questions: Is a dentist absolutely required to manage a potentially life-threatening emergency One can easily find eloquent arguments both for and against the societal duty to rescue. Distilling the question to its elemental issue, does society want to legally mandate rescues, or does society want to preserve individual freedom to accept or reject rescue responsibility and potential liability In 1964 a resident of New York City screamed for help from the street outside her apartment when attacked by a knife-wielding criminal. It is well documented that many neighbors witnessed the attack and the wounded woman helpless on the sidewalk. Patrons watched a rape attack for more than an hour without intervention or a call for help. College student Jeremy Strohmeyer was convicted of the sexual assault and murder of 7-year-old Sherrice Iverson. Regularly, such cases in which a life could have likely been saved by minimal intervention come into the legal system. Almost uniformly, courts decline to impose any liability on individuals who decline the responsibility and potential liability involved in a rescue. However, persons with special relationships to the victim may be required to attempt to effect a rescue. Some such persons considered to have special relationships include family Professional Relationships It would seem judicious to develop relationships with colleagues, including specialist dentists and physicians, for times when consultation would be helpful. Patients reasonably expect to have access to their dentist as necessary for perceived or real emergencies. If the primary caregiver is not going to be available, arrangements with another dentist to take calls for the practice are strongly recommended. Collegiality Occasionally, patients choose to or are not able to follow up with their original dentist or those designated for follow-up as necessary. A common denominator seen in almost all malpractice litigation is criticism, warranted or not, to the patient from a health care professional seen secondarily about the original treatment. This criticism is usually proffered without consultation with the original dentist. Currently, only Minnesota and Vermont have statutes requiring rescue under certain circumstances. However, Good Samaritan statutes are found uniformly in state law because legislatures want to encourage rescues by removing potential liability, although some liability may always attach. Good Samaritan statutes are aptly named and intended by states to promote moral behavior. Religious and philosophic leaders throughout history have championed selfless service to others. The lesson offered is that if the Samaritan can rescue his enemy, we are thus admonished to also serve our neighbor and fellow man. Dentists shall be obliged when consulted in an emergency by patients not of record to make reasonable arrangements for emergency care. Calling 911 is likely the minimal effort that would be required to fulfill rescue obligations in the dental office and requires no professional expertise whatsoever. For instance, a known epileptic in the waiting room who has a seizure would likely be evaluated differently than a child who seizes secondary to an absolute or relative local anesthetic overdose. The dentist who calls 911 and goes to lunch is in a different position than one who is actively helping treat the emergency by, for instance, maintaining an airway. The dentist who is deciding whether or not to relinquish the emergency care of his patient to another must reasonably weigh the risk and benefit of such conduct. Some physicians, such as radiologists, pathologists, or psychiatrists, may have minimal airway training.
Cheap indapamide 2.5 mg visa
A cutting instrument and pain in operative medicine are two ideas which never present themselves separately to the mind of the patient heart attack 30 year old female buy indapamide now, and it is necessary for us surgeons to admit their association. The trend emphasizing the pain of dentistry is continued in the popular culture today, for instance, in movies such as Little Shop of Horrors, Marathon Man, and the Dentist. These two injections have evolved to more than 300 million dental local anesthesia administrations performed annually in the United States. Local anesthesia was indeed preceded by the development of sedation and general anesthesia by dentists. That notices were published in Rochester, New York,11 and St Louis, Missouri,12 warning the populace to "look out for" and "beware" of the "villain" Morton is not surprising. Morton sued the infirmary for infringing on his patent for the use of ether for surgical procedures. The issue of whom the honor of the initial development of anesthesia belonged grew to involve even the U. Once anesthesia was quickly adopted by medicine, it was denounced not only by some surgeons but even from the pulpit. Within a few short years of its organization, more dentists have been trained annually in oral sedation protocols than graduate in all dental anesthesiology, oral and maxillofacial surgery, and intravenous sedation training programs combined. Further, it takes time to develop into efficient dental professionals after graduation. However, despite their student and/or recent graduate status, even such individuals readily recognize that their education is sadly lacking in pain control modalities needed and demanded by their future patients. This is evidenced by the fact that those contemporary recent graduates surveyed would support an increase in tuition and fees to gain more, or even any, advanced pain control knowledge while in school. All the current dental models of anesthesia delivery mentioned earlier have been shown to be safe and effective. Mutual respect and collegial cooperation between dental groups, currently struggling against economically competing dental colleagues to maintain their anesthesia status quo from perceived threats within the profession, would lead to synergistic and exponential growth of anesthesiology in dentistry. A specialty would also be the most effective buffer against compromising attacks from nondental anesthesia providers. Compromise will likely occur from timely opportunistic pressure exerted by significantly more numerous anesthesia provider groups outside of dentistry (Table 41. Of course, legal colleagues will be more than willing to continue to adjudicate the controversies. Dentists administer more local anesthetics and general anesthetics per trained provider than any other health profession. Dentists perfected outpatient general anesthesia techniques decades before their medical colleagues even considered outpatient general anesthesia a reasonable option. Dentist anesthesia providers have at least equivalent, if not better, morbidity and mortality statistics compared with other professions providing anesthesia services. Throughout the United States, state dental boards have fully implemented statutes designed to ensure the qualified provision of dental anesthesia, whereas such statutes are currently in place in only a few states for medicine. Yet when one looks at the relatively minimal patient-perceived presence of dentistry in the anesthesia world, it is apparent that dentistry has not handled its gift of pain control to the world with the fiduciary care anesthesiology should have been afforded. Before this publication, no such accreditation was possible for the many decades that dentists were trained in general anesthesia. For instance, each resident must do a minimum of 500 deep sedations or general anesthetics, 200 of which must be intubated general anesthetics, and at least 50 must be nasotracheal intubations, and 20 cases must incorporate advanced airway techniques, such as fiber-optic intubation, laryngeal mask airway, etc. A minimum of 100 cases must be for children 6 years old or younger, and 50 cases must be for special-needs patients. There are three major benefits to the profession that will be derived from the accreditation of dentist anesthesiologist residency programs97: 1. Because there is a huge increased need and demand for dentists to provide advanced sedation and anesthesia services for other dentists, accreditation should provide increased funding opportunities to support more residents and residency programs to meet that need and demand. Accreditation by dentistry helps cement anesthesia at its highest level as within the scope of dental education and within the scope of the clinical practice of dentists. To describe, delineate and differentiate these conditions, the morbid psychological phenomena that constitute the subjective experience of patients need to be carefully assessed, elicited and recorded. In other words, descriptive psychopathology is concerned with the selection, delimitation, differentiation and description of particular phenomena of experience, which through the use of accepted terminology become both defined and capable of repeated identification. It can be said that descriptive psychopathology is the fundamental professional skill of the psychiatrist; it is, possibly, the only diagnostic skill unique to the psychiatrist. It is considerably more than just carrying out a clinical interview of a patient or even listening to the patient, although it necessarily involves both of these. Its accurate application involves the deployment of empathy and understanding (we shall return to these later). Of course, for the rational practice of psychiatry there is a need for knowledge of the basic neurosciences; appropriate factual knowledge of psychology, sociology and social anthropology is also required. With these, there is a need for a comprehensive working knowledge of general medicine, especially neurology and endocrinology. This could be considered to be the minimum knowledge base that is essential for practising psychiatry. However, it is descriptive psychopathology that provides the foundation of clinical psychiatric practice. The subjective phenomena that are revealed during the clinical assessment, coupled with observable behaviours, ultimately determine the clinical judgements that influence treatment and management decisions. It relies on the method of phenomenology by focusing on experienced phenomena to establish their universal character. How the mind should be conceived for the purposes of psychopathology, what its faculties, functions or elements are (if there are any), how these can be distinguished, and how mental disorders can be comprehended by an application of these concepts are philosophic questions. Manfred Spitzer (1990) Psychiatry is that branch of medicine that deals with morbid psychological experiences. By definition, in the medical conditions that are central to psychiatric practice, psychological phenomena are important as causes, symptoms and observable clinical signs and also as therapeutic agents. Descriptive psychopathology as distinct from other forms of psychopathology eschews explanation of the phenomena that it describes. Hence, descriptive psychopathology guards against and avoids theory, presupposition or prejudice. This constraint of descriptive psychopathology acts to secure the conceptual framework of phenomenology, restricting it to the actual experience of the patient. It is important to distinguish psychopathology from nosography, which is the description of single illnesses with provisional and characteristic features that lay the foundation for diagnosis (Stanghellini and Fuchs, 2013). Neither is it merely symptomatology nor pathology of the psyche (Stanghellini and Aragona, 2016; Stanghellini and Fuchs, 2013). It is, as elaborated later, a highly formalized and methodical system designed to inquire into and describe abnormal mental phenomena. Explanatory psychopathologies, in contrast, often assume that mental phenomena are meaningful. In psychoanalysis, for example, at least one of several basic mechanisms are assumed to be taking place, and the mental state becomes understandable within this framework. Explanations of what occurs in thought or behaviour are based on these underlying theoretical processes, such as transference or ego defence mechanisms. For example, with a delusion descriptive psychopathology tries to describe what it is that the person believes, how he describes his experience of believing, what evidence he gives for its veracity and what is the significance of this belief or notion to his life situation. An attempt is made to assess whether this belief has the exact characteristics of a delusion and, if so, of what type of delusion. Having made this phenomenological evaluation, the information gained can be used diagnostically, prognostically and hence therapeutically. Some of the contrasts between descriptive and psychoanalytic psychopathology are summarized in Table 1. Analytical or dynamic psychopathology, however, would be more likely to attempt to explain the delusion in terms of early conflicts repressed into the unconscious and now able to gain expression only in psychotic form, perhaps on a basis of projection. The content of the delusion would be considered an important key to the nature of the underlying conflict, which has its roots in early development. Descriptive psychopathology makes no attempt to say why a delusion is present; it solely observes, describes and classifies. There are other radically different models of psychology that regard mental experience, including thoughts, Psychodynamic Explanatory Behavioural etc.