Cheap purim amex
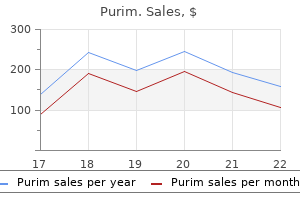
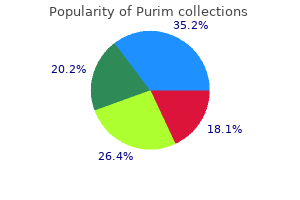
The tympanometer measures the flow of sound energy into the middle ear under conditions of changing air pressure chapter 9 medications that affect coagulation purchase purim 60 caps online. When the air pressure is equal on both sides of an intact eardrum, with the drum in neutral position, the transmission of sound energy through the tympanic membrane is at its maximum. The peak on the tympanogram represents the pressure at which the flow of sound energy is maximal. For example, in a normal air-filled middle ear cavity, the peak occurs at ambient atmospheric pressure. With eustachian tube dysfunction (a retracted eardrum but no middle ear effusion), the peak occurs in the negative pressure range on the recording. With middle ear effusion, the sound energy flow into the middle ear is reduced, which produces a flat tympanogram. A flat tympanogram may also result from cerumen, foreign body, or from occlusion of the opening of the probe by the wall of the external auditory canal. In a perforated eardrum, the sound energy is readily transmitted through the hole in the drum throughout the entire pressure range, resulting in a flat tympanogram. When performed by experts, tympanometry and pneumatic otoscopy have equivalent sensitivity (approximately 90%) and specificity (70%-80%). Tympanometry is neither more accurate nor more convenient than is properly performed pneumatic otoscopy. Tympanometry is advantageous if the clinician is unsure of the otoscopic findings. Acoustic Reflectometry Acoustic reflectometers are used to detect middle ear effusion. The device directs sonar-like sound waves of varying frequency toward the tympanic membrane and measures the intensity of reflected sound. The frequency of maximal reflected sound depends on the distance of the probe from the eardrum. Middle ear effusion is detected not by the frequency but by the magnitude of maximal reflected sound. When middle ear effusion is present, reflectance is increased in comparison with that in the airfilled middle ear. Improvements in technology have been made such that reflectometry includes spectral gradient analysis. It has a lower sensitivity and specificity than properly performed pneumatic otoscopy in detecting middle ear effusion. Because the accuracy of current models decreases in infants younger than 1 year, this technique should not be used in infants younger than 6 months of age. In contrast, in acute mastoid osteitis, also called acute coalescent mastoiditis, there is destruction of bone trabeculations in the mastoid air cells. Magnetic resonance imaging should be used for diagnosing intracranial mass lesions (brain abscess) and soft tissue sequela of infection, while magnetic resonance venography would identify dural sinus thrombosis. C 400 100 0 200 Differential Diagnosis Most disorders of the external and middle ear are readily apparent after the examination of the ear (see Tables 4. If examination findings are unremarkable, the clinician should consider referred pain (see Table 4. C, A tympanogram with a negative peak pressure, indicating eustachian tube obstruction. The external canal can become vulnerable to infection from excessive moisture from warm humid weather, moisture in the canal, or swimming. The moisture may cause small abrasions in the protective lipid layer of skin in the ear canal. Dryness or presence of underlying skin conditions (such as eczema) and trauma (including cotton ear swabs) can also predispose the external canal to infection. Less commonly, otorrhea draining from a perforated tympanic membrane secondary to otitis media may cause otitis externa. The presenting symptoms are often intense pain (especially with manipulation of the pinna, pressure on the tragus, or jaw movement), erythema, and otorrhea. While otitis externa can occur at all ages, occurrence peaks between 7 and 12 years of age, with 10% of people having an episode in their lifetime. Pseudomonas aeruginosa is the predominant organism causing otitis externa, but staphylococcal species (Staphylococcus aureus and coagulase-negative staphylococci) and streptococci have been isolated. Gram-negative organisms, such as Enterobacter, Proteus, and Klebsiella species, and fungal organisms, such as Candida and Aspergillus species, have also been isolated. Treatment consists of a topical suspension, commonly ofloxacin or ciprofloxacin combined with hydrocortisone or dexamethasone. If there is marked edema of the canal, antibacterials may not reach the site of infection. In this case, the canal should be cleaned with gentle suction, and a cotton wick should be inserted into the auditory canal. Antibacterial suspension is then dripped into the wick, which allows the medication to diffuse further into the ear canal. If the infection progresses, the patient may need parenteral antibacterials and consultation with an otolaryngologist. It occurs when the infection progresses into the cartilaginous structures of the ear canal. Treatment requires systemic antibacterials and can require surgical debridement of tissue. The illness may result in chondritis and osteitis of both the middle and inner ears. It is not clear whether the virus alone or a combination of virus and bacteria are involved in the pathogenesis. Several studies have documented the presence of viruses (10%-44% with or without bacteria) in the middle ear fluid of children with otitis media. Viruses enhance bacterial adherence and colonization in the nasopharynx, impair local host immune defenses, and cause eustachian tube dysfunction. In addition, because resistance genes are frequently linked, organisms with resistance to -lactam drugs are more likely to be resistant to sulfa antibacterials and to the macrolide class. Nonetheless, high-dose amoxicillin remains the best oral antibiotic available for drug-resistant S. In adults, diabetes mellitus is a common predisposing condition, though it is not a common comorbidity in children. Presenting symptoms include a markedly swollen and laterally displaced pinna associated with fever, malaise, and persistent, deep-seated otalgia out of proportion to findings on examination. Pseudomonas aeruginosa is the most commonly isolated pathogen, and coverage should include antibacterials directed against it. Surgical intervention may be necessary to obtain cultures for therapy guidance and provide local tissue debridement. The viral infection enables pathogenic bacteria in the nasopharynx to ascend through the eustachian tube into the middle ear either by impairing local host defenses or by eustachian tube dysfunction. Evaluating the treatment of otitis media is complicated by the high rate of spontaneous resolution of the infection. Some authorities suggest withholding antibacterials in children with low risk for complications. In the Netherlands, antibacterial therapy is commonly delayed until 48-72 hours after the diagnosis, to determine whether there is spontaneous resolution of the infection. Criteria for antibacterial treatment or observation in children with nonsevere illness:* 1) 6 mo: antibacterial treatment No 9 Does the child have fever 39 C and/or moderate or severe otalgia No 10 Amoxicillin at a dose of 80-90 mg/kg/day is the initial antibacterial of choice for most children. Systems are in place for ready communication with the clinician, reevaluation, and obtaining medication if necessary. Clinician should initiate antibacterial treatment for children initially managed with observation or change antibacterial treatment for patients initially managed with antibacterial therapy. Antibacterial choice should be based on the likely pathogen(s) present and on clinical experience. High-dose amoxicillin (80-90 mg/kg/day given in two divided doses) is the appropriate initial therapy for most cases (Table 4. Because otitis media is usually a self-limited illness, the use of broad-spectrum antibacterials for the initial treatment should be discouraged because standard, such as the Netherlands and Denmark, rates of acute mastoiditis are slightly higher (1-2 episodes per 100,000 person-years) than in countries with higher rates of antibacterial use.
Generic purim 60 caps free shipping
The disease is particularly severe in very young children shakira medicine order purim cheap, often because of a delay in diagnosis with subsequent perforation. The thinness of the appendix and the paucity of the omentum in younger children may result in rapid, unimpeded spread of intraabdominal infection after rupture. Diagnosis An accurate and early diagnosis is critical for avoiding perforation and peritonitis and for excluding other causes of abdominal pain. Appendicitis usually manifests initially with a gradual onset of periumbilical (occasionally epigastric) pain, which may begin as a dull ache but becomes constant (or, less often, colicky) and of mild to moderate intensity. Furthermore, the appendix may irritate the bladder, causing urinary frequency and dysuria. Pain may transiently stop, but as local peritonitis develops, the pain will continue but shift to the right lower quadrant. The shifting of pain from the periumbilical area to the right lower quadrant area may take 12-36 hours but usually occurs in 2-8 hours and may not yet be evident in an acute onset of less than 4-6 hours. McBurney point corresponds to the location of the base of the appendix and is found by placing the little finger of one hand in the umbilicus and the thumb on the anterior superior ileal spine. The index finger, if extended perpendicularly to the abdominal wall, identifies McBurney point. Unfortunately, the appendix is not always in its classic position; thus, appendicitis may produce pain in the pelvis, in the retrocecal area (back or flank pain, psoas muscle spasm with limp), or elsewhere. They can be anxious while watching where examiners place his/her hands, be motionless, walk slowly, get on the examining table with difficulty, or exhibit a nondistended but tender abdomen with voluntary guarding, reduced bowel sounds, and point tenderness in any area overlying the appendix. Perforation or extensive gangrene should be suspected in the presence of progression for more than 36-48 hours; high fever; diffuse abdominal pain and tenderness; a rigid, board-like abdomen; leukocytosis; a right lower quadrant mass; and other signs of generalized peritonitis (see Table 10. Laboratory and Radiographic Testing Ultrasonography has been of benefit in the diagnosis of appendicitis and in excluding other important disease processes (Table 10. A, the appendix may be located anteriorly, medially, or retrocecally or in the pelvis. Because the bowel may be quite mobile in some patients, the appendix may be located in many different sites in the abdomen. There is subsequent risk for intestinal obstruction and tubal infertility in females. Pancreatitis Pancreatitis is an acute inflammatory condition of the pancreas and is often a result of obstruction of the pancreatic duct. Release and activation of pancreatic digestive enzymes subsequently result in extensive destruction (autodigestion) and necrosis of pancreatic and, if severe, adjacent tissue. Proteolysis, fat necrosis, and hemorrhage are noted in severe or fatal cases of pancreatitis, which is often complicated by multiorgan dysfunction syndrome. Pancreatitis is less common in children than in adults, in whom the cause is often alcohol ingestion or gallstones. The etiologic factors in childhood encompass a broad differential diagnosis and often include passage of biliary stones, drugs (valproate), multisystem diseases (hemolytic uremic syndrome, cystic fibrosis), trauma (including child abuse), biliary or pancreatic anatomic anomalies, infections, and metabolic conditions (hypercalcemia, hypertriglyceridemia) (Table 10. Ultrasonography helps define other disease processes, such as mesenteric adenitis. Gastroenteritis is one of the more common conditions to be considered in the differential diagnosis (Table 10. Treatment Appendicitis is treated by surgical appendectomy and ligation of the stump by open or laparoscopic methods. If an abscess is present in the right lower quadrant and the patient demonstrates few signs of toxicity, elective nonurgent appendectomy may be delayed to permit preoperative rehydration and broad-spectrum antibiotic therapy. If the appendix is not perforated, some centers treat with only broadspectrum antibiotics. In operative appendicitis, parenteral antibiotics are given before surgery and are continued postoperatively only in the presence of frank contamination, such as gangrenous or perforated appendicitis. The duration of antibiotic therapy is determined by the presence of infectious complications. If the appendix appears normal, other intraabdominal sources of pain should be sought during the surgery. Manifestations Manifestations of acute pancreatitis include intense epigastric abdominal pain that may be described as steady, boring, constant, achelike, knifelike, and exacerbated by recumbency, that radiates to the back, upper abdominal quadrants, or the scapula. The patient often assumes a hunched-over or knee-chest lateral fetal posture and may manifest epigastric tenderness; bowel sounds may be reduced or absent. Signs of peritonitis suggest more extensive necrosis, as do signs of spreading hemorrhage, such as blue-green discoloration of the flanks (Grey Turner sign) or of the periumbilical region (Cullen sign). The diagnosis is confirmed by an elevated serum amylase and/or lipase level (lipase levels may be elevated initially with normal amylase values). Adverse prognostic factors in severe acute pancreatitis include the presence of leukocytosis (white blood count >16,000/mm3), hyperglycemia (glucose level >200 mg/dL), a high lactic dehydrogenase level (>350 U/L), and a high aspartate aminotransferase level (>250 U/L) on admission and a decrease in hematocrit value (>10%), an increase in blood urea nitrogen level (>5 mg/dL), a low calcium level (<8 mg/ dL), hypoxia (PaO2 <60 mm Hg), acidosis (base deficit >4 mmol/L), or severe dehydration by 48 hours of hospitalization. Complications Complications of pancreatitis include local tissue necrosis with or without superinfection (pancreatic abscess), fistulization (to colon), left-sided pleural effusion, gastrointestinal hemorrhage (ulceration, vascular rupture, splenic rupture), shock, coagulopathy, acute kidney injury, myocardial depression, acute respiratory distress syndrome, hyperglycemia, hypocalcemia, subcutaneous nodules (fat necrosis), hypoalbuminemia, mental changes, and retinopathy. During surgery, the patient was found to have a perforated appendix and early periappendiceal abscess. Ten days before admission to the hospital, she was seen by a physician because of abdominal pain. She had been partially treated with antibiotics for a presumed "strep throat" in the interim. When she presented to the hospital, she again had pain in the right lower quadrant, especially when the ultrasound transducer was pressed over the area. Enteral alimentation should be initiated as soon as possible, even with a partial ileus, as early feeds are not associated with increased pain, 175 longer hospital course, or elevation in serum lipase. Additional therapies include prophylactic antibiotics in acute necrotizing pancreatitis. Cholelithiasis Gallstones are uncommon in children, but they complicate chronic diseases, such as hemolytic anemia (sickle cell anemia, spherocytosis), cholestatic jaundice in which total parenteral nutrition is given, and other cholestatic diseases. Gallstones may result from prematurity or drug intake (furosemide, ceftriaxone), or they may be idiopathic. Biliary obstruction (stone in cystic or common bile duct) often results in jaundice; sudden onset of severe, sharp right upper quadrant pain; localized deep tenderness in the right upper quadrant (superficial tenderness suggests an associated cholecystitis); and emesis. The pain is episodic and colicky, but often constant, superimposed with waves of more intense pain, and may radiate to the angle of the ipsilateral scapula, back, or other areas of the abdomen or chest. There may be associated diaphoresis, pallor, tachycardia, weakness, nausea, and lightheadedness. A round or pear-shaped, tender mass may be palpated in the right upper quadrant of the abdomen if the gallbladder is distended. Many patients with single or multiple gallstones without obstruction are asymptomatic. Acute cholecystitis is caused by inflammation of the gallbladder wall as a result of duct obstruction. B, Duration of abdominal pain before the diagnosis of ectopic pregnancy was confirmed among 654 patients. The Murphy sign is demonstrated by palpating an acutely inflamed gallbladder, which causes the patient to halt respiration and feel the pain. Acute perforation is uncommon in children but is characterized by sudden worsening of pain or a new abrupt onset of excruciating epigastric pain. There is associated pallor, faintness, weakness, syncope, diaphoresis, and a rigid abdomen. Intermittent severe, episodic pain can be frightening to both families and care providers because it may be an indication of serious disease. It has been reported to occur in 10-15% of children between the ages of 4 and 16 years. Pain pathways can initially be influenced by the presence of pathology such as inflammation or tissue damage that often persists despite the absence of identifiable pathology. The term functional abdominal pain refers to pain that has no anatomic, histologic, or "organic" etiology. A common feature among patients with functional gastrointestinal disorders is the heightened sensitivity to experimental pain, also known as visceral hyperalgesia. A unifying theory of all functional gastrointestinal disorders is the alteration of the brain-gut axis that can present with clusters of symptoms related to abnormal signals arising from the gastrointestinal tract or abnormal processing of signals in the central nervous Diagnosis the diagnosis is confirmed by ultrasonography that demonstrates acalculous or calculus-induced cholecystitis or acute duct obstruction by a stone. Treatment Some treatment of obstructing stones may include endoscopic, open, or laparoscopic cholecystectomy.
Diseases
- Common variable immunodeficiency
- Mental retardation short stature Bombay phenotype
- Chromosome 6, partial trisomy 6q
- X chromosome, duplication Xq13 1 q21 1
- Acute monocytic leukemia
- Chromosome 13 ring
- Microphtalmos bilateral colobomatous orbital cyst
- Opthalmoplegia progressive external scoliosis
Generic 60 caps purim with mastercard
It is imperative that patients identified by the screening program receive a rapid treatment dynamics buy purim visa, accurate, and definitive diagnosis because the clinical implications and therapies for the various forms of hyperphenylalaninemia are different. All genetic forms of hyperphenylalaninemia are caused by defects that directly or indirectly affect the activity of the enzyme phenylalanine hydroxylase. Treatment should start within the first month of life to avoid irreversible neurologic damage. When started early, treatment is generally effective in preventing the long-term neurologic sequelae of this disease. However, standard treatment appears unable to prevent more subtle intellectual and behavioral disabilities. They appear to tolerate a higher dietary protein intake while maintaining acceptable serum phenylalanine concentrations. Standard dietary management corrects the hyperphenylalaninemia that these patients have, but does not improve the neurologic problems related to their neurotransmitter deficiencies. Many newborn infants now go home from the hospital before 24 hours of age, thereby creating problems for screening programs. Screening before 24 hours increases the risk of a false-negative result, whereas delaying screening until after discharge increases the risk of poor compliance. Those who have a positive screening result require prompt attention, including plasma amino acid analysis. If the plasma phenylalanine concentration and the plasma phenylalanineto-tyrosine ratio are increased, the patient should be placed on a low-phenylalanine diet. The most common clinical presentations are listed in Table 99-3, along with a differential diagnosis of the categories of metabolic disorders that may be associated with each presentation. Similarly, most maternal illnesses, including inborn errors, do not affect the developing fetus. She also has an increased risk of having a child with major birth anomalies, including intrauterine growth restriction, microcephaly, mental retardation, and a congenital heart defect, as well as a broad range of minor anomalies. Gastrointestinal abnormalities Hairorskinabnormalities Hematologicabnormalities Hepaticdysfunction(see Table99-5) Fetal Diseases Affecting the Mother As a rule, inborn errors of metabolism of the fetus do not affect the pregnant mother. It often produces a severe coagulopathy, hypoglycemia, and fulminant hepatic failure. Women with either of these disorders improve remarkably after delivery, suggesting that the fetus is causing a toxic effect on the mother that resembles that seen in patients with inborn errors of fatty acid oxidation. Long-chain 3-hydroxyacylCoA dehydrogenase deficiency can be seen as an isolated deficiency or as part of trifunctional protein deficiency that affects all three enzyme activities. The fetus, in turn, is at risk for significant postnatal problems associated with its enzyme deficiency. There are, however, several groups of disorders that include significant exceptions: congenital disorders of glycosylation, fatty acid -oxidation disorders, respiratory chain disorders, neurotransmitter disorders, and peroxisomal disorders (see Dysmorphic Syndromes). Although most of the clinical disorders that affect the developing fetus are discussed later, the disorders that can lead to congenital ascites or hydrops fetalis are discussed here. The neurologic difficulties, such as altered consciousness (encephalopathy), altered tone, or seizures, are discussed elsewhere in this book (see Chapters 59 and 62). As noted in these chapters, these neurologic difficulties are most commonly caused by infection, brain malformations, or hypoxemicischemic encephalopathy, and less commonly by inborn errors of metabolism. Although it is important to evaluate a patient for these common problems, it is also important to remember that inborn errors of metabolism can also produce brain malformations and can mimic the clinical picture of hypoxic-ischemic encephalopathy. The distinction between these two groups is somewhat arbitrary because patients with a disorder that produces metabolic encephalopathy often have seizures, and conversely, patients with a disorder that produces metabolic seizures often have encephalopathy. Nevertheless, the distinction is useful because patients generally fall more easily into one group than the other. A number of specific metabolites are overproduced as a result of a particular enzyme deficiency. In excess, these metabolites serve as endogenous toxins that impair other metabolic or physiologic processes. Disruption of these processes leads, in turn, to production of additional metabolites, which further impair cellular processes. Early interruption of the cascade through such relatively simple measures as fluid and caloric support might abort episodes of metabolic decompensation. Physicians who care for children who present with a metabolic disorder in late infancy, childhood, or even adulthood often receive a retrospective history of "sepsis" in the neonatal period that was never confirmed by culture and that resolved spontaneously; these episodes might have represented an interrupted metabolic intoxication syndrome. Early nonspecific supportive treatment can abort the pathologic cascade or delay the onset of a more fulminant course until a provisional metabolic diagnosis and specific treatment become available. The symptoms and signs of neonates who develop metabolic encephalopathy generally do not appear on the first day of life but usually begin later in the first week. The initial symptoms are often poor feeding associated with a poor suck and irritability. Muscle tone is decreased, sometimes marked by a fluctuating pattern of decreased and increased tone. In the case of urea cycle defects, hyperammonemia increases the respiratory drive, leading to hyperpnea. These symptoms often progress rapidly, sometimes within a matter of hours, but more often during the course of a few days. It is important to suspect a metabolic disorder as early as possible in its course to interrupt the progression of symptoms because many of these disorders are life threatening. The diagnostic evaluation of a newborn suspected of having a metabolic encephalopathy should include testing for disorders of amino acid metabolism, organic acid metabolism, the mitochondrial respiratory chain, and the urea cycle (see Table 99-3). The differential diagnosis for these patients can often be narrowed by the presence of other clinical or routine laboratory findings, such as acidosis, hyperammonemia, hypoglycemia, ketosis, or lactic acidemia. The diagnosis will be narrowed further by performing more specialized laboratory testing, including plasma amino acid analysis, urine organic analysis, plasma carnitine analysis with acylcarnitine profile, and urine carnitine analysis with acylcarnitine profile. Effort should be made to perform a prompt and vigorous laboratory evaluation of the patient suspected of having a metabolic encephalopathy because many of them are potentially treatable. The disorders that produce metabolic encephalopathy are discussed later in this chapter. Metabolic Seizures There are an ever-growing number of inborn errors of metabolism that have been recognized as a cause of seizures in the neonatal period or early infancy. As in the case of patients who present with a metabolic encephalopathy, many of the disorders that produce neonatal seizures are potentially treatable. The approach to laboratory testing of these patients should include the same laboratory testing noted in the preceding for the evaluation of patients with suspected metabolic encephalopathy. In addition, the patient with a suspected metabolic seizure disorder should undergo additional, specialized testing for both potentially treatable and untreatable disorders, with emphasis directed toward identification of potentially treatable disorders. The clinical features, biochemical basis, diagnostic testing, treatment, and prognosis for several of the disorders that produce metabolic seizures are provided in the following. The disorders are presented in three groups: treatable disorders, potentially treatable disorders, and untreatable disorders, to allow the attending physician to prioritize his or her diagnostic evaluation. Treatable Disorders the treatable disorders include folinic acid-responsive seizures, glucose transporter type I deficiency, pyridoxinedependent epilepsy, and pyridoxal 5-phosphatedependent epilepsy. More specifically, patients with both disorders share the same biochemical abnormalities. Patients who are identified as having folinic acidesponsive seizures based on clinical responsiveness to folinic acid and then shown to have the biochemical and genetic evidence of pyridoxine-dependent epilepsy should be treated with a combination of folinic acid (3-5 mg/kg per day) and pyridoxine (15-30 mg/kg per day). The biochemical hallmark of these seizure disorders is cerebral folate deficiency. Neither disorder has been reported to produce seizures during the neonatal period. Glucose transporter type 1 deficiency is (in almost all cases) an autosomal dominant disorder that reduces glucose transport by approximately 50%, leading to impaired energy production by the brain and a range of neurologic abnormalities. They can have a variety of seizure types, including partial, generalized, or myoclonic seizures. Many affected infants also develop episodic eye movements, ataxia, oculomotor apraxia, developmental delay, microcephaly, and "stroke like events with reversible hemiplegia" as they get older. Glucose transporter type 1 deficiency can be treated successfully with a low-carbohydrate, high-fat diet (ketogenic diet), which provides ketones as an alternative fuel source for the brain.
Order purim cheap
Microphthalmia (small eye) is a common congenital defect that can be mildly expressed z pak medications discount purim express. A unilateral large globe caused by monocular myopia can produce a relative ptosis in the contralateral normal eye. It may be associated with other eye abnormalities or syndromes such as Duane syndrome. Often associated with other lid or ocular abnormalities, congenital entropion is an in-turning of the lid margin, most often of the lower lid. If the lashes on the lid margin rub the cornea and cause corneal abrasions, surgery is necessary. Epiblepharon is an extra fold of skin along the lower lid that can cause lashes to turn inward. This condition usually requires no treatment and is most often seen in infants of Asian ancestry. This condition usually improves spontaneously during the first 2 years of life, but if it persists, consideration should be given to surgical correction. Because the lashes are soft when the child is younger, lashes rubbing against the cornea tend not to produce symptoms. But beyond age 1, as the lashes get thicker and harder, corneal irritation leading to abrasion and even ulceration not controlled with simple lubrication with ointments warrants earlier surgical intervention. The condition could be idiopathic or inherited, unilateral or bilateral, congenital or acquired. When looking straight ahead, the normal lid should elevate to a point at least midway between the pupil and the upper margin of the cornea. The term ankyloblepharon is used to designate this condition, which may be dominantly inherited. Simple excision of the bridging tissues between the eyelids is all that is required to separate the lids. Often a congenital nevus will not be noticed until puberty, when pigment begins to accumulate and the lesion is thought to be growing. Occasionally they appear to be free in the orbit or lid without demonstrable direct connection to a suture line. They are benign choristomata that grow slowly but will thin out the adjacent bone. If a dermoid cyst is ruptured by accidental trauma or surgery, severe local inflammation can result if the extruded contents are not irrigated from the wound. They may virtually occur in any body location, including the upper or lower lids and orbit. In infants, the hemangioma usually is not well encapsulated, and frequently periorbital and orbital lesions will occur in association with similar lesions elsewhere on the body. Although observation of lid involvement assists in making the diagnosis, a biopsy might be required to exclude other orbital tumors if the hemangioma lacks a superficial component. Crying or straining by the infant often causes the mass to increase in size and assume a bluish coloration. Digital pressure on the superficial portion of the tumor is rapidly reversed, demonstrating the high flow of capillary hemangioma. Congenital capillary hemangiomata are inconsequential at birth but grow rapidly during the first 6 months of life. Until recently, treatment was oral use or intralesional injections of steroids, subcutaneous interferon, or excision of the lesion. Central artery occlusion is a rare but well-described complication of steroid injection with permanent vision loss. However, its use, although relatively uncommon, necessitates that side effects such as hypotension and hypoglycemia be monitored closely. Other eyelid lesions include, but are not limited to , plexiform neuromas secondary to neurofibromatosis type-1, amyloid depositions, and juvenile xanthogranuloma. Eyelash Abnormalities Lashes may be redundant, absent, misdirected, or discolored. The condition may be inherited or acquired through mucous membrane diseases of the conjunctival sacs, infectious process, or trauma. Trichiasis is a lash that grows from a normal location but is misdirected toward the ocular surface. Congenital trichiasis patients should be examined for Down syndrome or signs of ectodermal dysplasia. If a second row of lashes is present in the area of the meibomian glands (metaplasia), the condition is referred as distichiasis. This condition usually results in contact of the lashes with the cornea, producing corneal irritation and abrasions. Excessive eyelash growth can result as a side effect from multiple medications, including topical prostaglandin analogues and epidermal growth factor receptor inhibitors. Hypertrichosis involving the eyebrows, forehead, and upper lid appears in the Cornelia de Lange syndrome, a pathologic dwarfism associated with multiple congenital anomalies. The fetal lanugo persists into adult life, creating an abundant covering of hair on the eyebrows, forehead, eyelids, and other areas of the body. Although the usual cause of epiphora is a blockage of the nasolacrimal ducts (dacryostenosis), the possibility of congenital glaucoma is the most important consideration in the differential diagnosis. Less commonly, tearing can result from an obstruction of the common canaliculus, congenital absence of the lid puncta, or dacryocystitis. Epiphora can occur as the result of corneal abrasion, corneal foreign body, or nasal and facial lesions that irritate the fifth cranial nerve. Chronic nasal congestion also may produce epiphora by mechanically blocking the nasolacrimal duct. Dacryostenosis may be present in up to 7% of neonates and creates a stagnant pooling of tears in the lacrimal sac that contributes to chronic or recurrent dacryocystitis. The inflammation is marked by a purulent exudate in the medial canthal area of the conjunctiva. Severe dacryocystitis can produce swelling and induration of the lacrimal sac medial and inferior to the medial canthus. Treatment of mild nasolacrimal infection consists of topical antibiotic drops or ointment. If surrounding cellulitis is suspected, systemic administration of medication and locally applied heat may be required. Repeated massage of the lacrimal sac at the medial canthal area serves to flush out the stagnant tears, decrease the risk for infection, and "pop" open the nasolacrimal obstruction. If the epiphora continues, a lacrimal probe passed through the nasolacrimal duct to the nose usually creates an adequate opening. Probing between 6 and 12 months of age is sometimes performed in an office setting under topical anesthesia with the baby swaddled in a sheet. In more than 90% of children with congenital dacryostenosis, the obstructions spontaneously correct during the first year of life. If persistent, treatment is then offered, but requires general anesthesia because these children are too large to swaddle for an office probing. Surgical options include simple probing, silicone tube intubation, or balloon dilation of the lacrimal system. Similar lesions found higher than the medial canthus should be suspected to be encephalocele. The distended lacrimal sac is filled with clear fluid, feels firm or fluctuant to palpation, and does not pulsate like a frontal encephalocele. If the patient presents with signs of a dacryocystocele infection, admission to a pediatric intensive care unit for intravenous antibiotics is required. Reflex tearing from ocular irritation or psychogenic (emotional) tearing may not develop for weeks to months after birth. Infants do not usually have symptoms from dry eyes unless in rare conditions such as alacrima from a congenital lack of tear glands or RileyDay syndrome. During the first month of life, an infant with alacrima from any cause might not appear different from the normal infant because tear production is minimal during this period. The usual time of discovery is at 6 to 12 months of age after the lack of tears has produced changes such as scarring or ulceration of the cornea. At 1 to 2 months of age, early symptoms of dry eye are conjunctival hyperemia and photophobia.
Discount purim online amex
American Academy of Pediatrics symptoms 7 dpo bfp purim 60 caps on line, Section on Ophthalmology; American Association for Pediatric Ophthalmology and Strabismus; American Academy of Ophthalmology; American Association of Certified Orthoptists. Hormonal, metabolic, and neuroradiologic abnormalities associated with septooptic dysplasia. Clinical and molecular evaluation of probands and family members with familial exudative vitreoretinopathy. Neonatal facial movements in the first minutes of life-eye opening and tongue thrust: an observational study. Incidence, distribution, and duration of birthrelated retinal hemorrhages: a prospective study. Balloon catheter dilation for treatment of older children with nasolacrimal duct obstruction. Normal values and standard deviations for pupil diameter and interpupillary distance in subjects aged 1 month to 19 years. Contralateral occipital depression related to obstetric forceps injury to the eye. Eye manifestations of intrauterine infections and their impact on childhood blindness. Second nonocular tumors in survivors of heritable retinoblastoma and prior radiation therapy. Incidence, ocular findings, and systemic associations of ocular coloboma: a populationbased study. Ophthalmologic findings in Cornelia de Lange syndrome: a genotype-phenotype correlation study. Prevalence of retinal hemorrhages in pediatric patients after in-hospital cardiopulmonary resuscitation: a prospective study. Cycloplegic and mydriatic agents for routine ophthalmologic examination: a survey of pediatric ophthalmologists. The morning glory disc anomaly: contractile movement, classification, and embryogenesis. The syndrome of frontonasal dysplasia, callosal agenesis, basal encephalocele, and eye anomalies-phenotypic and aetiological considerations. Superselective catheterization of the ophthalmic artery for intraarterial chemotherapy for retinoblastoma. Surgical technique, visual outcome, and complications of pediatric intraocular lens implantation. The Alaska Haemophilus influenzae type b experience: lessons in controlling a vaccine-preventable disease. Molecular study of 33 families with Fraser syndrome: new data and mutation review. Retinal phenotype-genotype correlation of pediatric patients expressing mutations in the Norrie disease gene. Arteriovenous aneurysm of the midbrain and retina, facial nevi and mental changes. The introduction of closed incubators with the use of high levels of supplemental oxygen caused inhibition of the growth of retinal vessels in premature infants, eventually resulting in a complete retinal detachment behind the lens. Pathogenesis Retinopathy of prematurity is initiated as an arrest of normal retinal neuronal and vascular development in the preterm infant. Vascular growth may resume normally, but when it does not, there can be a pathological aberrant vascularization of the retina. As the intrauterine environment has a mean partial pressure of oxygen (pO2) below 50 mm Hg, unregulated supplemental oxygen given to premature infants with respiratory distress can drive oxygen saturations to abnormally high levels. The neovessels (induced by growth factor overshoot) poorly perfuse the retina and are leaky, leading to fibrous scar formation and retinal detachment. Multicenter trial of cryotherapy for retinopathy of prematurity: 32-year outcome-structure and function. However, increased target oxygen was associated with more pulmonary complications. Additional attention must also be paid to nutritional components such as adequate protein and appropriate fats, as well as appropriate use of glucose and other carbohydrates. In particular, it has been shown in animal studies that lack of omega 3 polyunsaturated fatty acids increases susceptibility for retinopathy. Loss of growth factors normally found in utero is also a major risk factor for the disease. The lower the gestational age and birth weight, the more profound is the loss of factors provided by the intrauterine environment. It was published in two parts throughout the world46,47 and was revisited in 2005. Second, the extent of the disease is described by the number of clock hours involved within the zone. Therefore, one can describe how many clock hours of retina is affected by which severity in detail by using this description method. Rates of progression are variable, and the worst prognosis is associated with onset of severe disease in zone I (most immature) that can rapidly progress to type 1 disease with high risk of retinal detachment. Onset in zone 2, or a slower evolution of the disorder, leads more often to complete resolution. Ablative treatment of nonvascularized retina helps to prevent blindness, but does not address the underlying cause of retinopathy of prematurity or other co-morbidities, which is the failure of normal neural and not meet criteria for plus disease). As in previous classifications, the degree of vasculopathy at the vascularavascular transition is divided into stages 1 through 5. Stages 1 through 3 are increasing degrees of abnormal blood vessel growth (neovascularization) with vessels growing into the vitreous in stage 3. Stage 4 is partial retinal detachment, and stage 5 is complete retinal detachment, both of which carry a poor prognosis for normal vision. In stage 3, extraretinal neovascularization may become severe enough to cause total retinal detachment (stage 5), which most often leads to blindness. Itisstillsomewhatdifficultto see the detail because of the underlying pinkish hue that masks the contrast. B, Fluorescein angiography documents retinal vascular anatomy in much better detail, as the fluorescein dye lights up only the retinal vasculature and every other structure is dark. Revised indications for the treatment of retinopathy of prematurity: results of the Early Treatment for Retinopathy of Prematurity Randomized Trial. A significant treatment effect with bevacizumab was seen for retinopathy of prematurity in zone 1, but not zone 2. The blocker propranolol has been proposed as a potential treatment to reduce retinal neovascularization,69 and clinical studies are underway in Israel and Italy. However, investigators of a 2012 study70 report that propranolol does not reduce retinopathy in a mouse model of retinopathy of prematurity. Results of a metaanalysis suggest that the carbohydrate inositol can reduce the number of infants with stage 3 or higher cases of retinopathy of prematurity. Adapted from American Academy of Pediatrics, American Association for Pediatric Ophthalmology and Strabismus, and American Academy of Ophthalmology. The algorithm must be used in conjunction with regular screening, but in Sweden it has reduced the number of eye examinations by up to 35%. Neonatologists and ophthalmologists must work closely together to ensure an efficient tracking system for timely examination of these infants and to be certain that follow-up examinations occur at the best times both in the hospital and after discharge or transfer. The goal is to ensure that infants who reach criteria for retinal ablation are treated to minimize vision loss. Trends in outcomes for very preterm infants in the southern region of Sweden over a 10-year period. Trends in the incidence of retinopathy of prematurity in Lothian, south-east Scotland, from 1990 to 2009. Incidence of retinopathy of prematurity in extremely premature infants over an 18-year period. Quantification of oxygen-induced retinopathy in the mouse: a model of vessel loss, vessel regrowth and pathological angiogenesis. Studies on the effect of high oxygen administration in retrolental fibroplasia, I: nursery observations. Vascular endothelial growth factor/vascular permeability factor expression in a mouse model of retinal neovascularization. Postnatal serum insulin-like growth factor I deficiency is associated with retinopathy of prematurity and other complications of premature birth.
Syndromes
- Debris trapped under the nail
- Are both eyes bulging?
- Hoarseness or changing voice
- Irritation and itching of the genital area
- Brain abscesses may lead to loss of neurological function.
- Acute pulmonary histoplasmosis
- Tube through the mouth into the stomach to empty the stomach (gastric lavage)
Buy cheap purim 60 caps line
This testing is often not needed if the clinical findings are consistent with bronchiolitis medicine you can take while pregnant generic purim 60 caps with amex. Suctioning and supplemental oxygen remain the cornerstone of treatment for bronchiolitis. Unlike asthma, the wheezing accompanying bronchiolitis is often less responsive to bronchodilators. Nonetheless, patients with significant hypoxia and hypercapnia may receive a trial treatment with aerosol bronchodilators to determine if this may improve symptoms, which may be continued if infants do show improvement. Infants with bronchiolitis do not respond to treatment with antiinflammatory agents, such as corticosteroids, so these are not recommended. Severely ill patients may require mechanical ventilation; heated, humidified, high-flow nasal cannula oxygen has been shown to decrease intubation rates and can be used in children with severe respiratory distress. Treatment with exogenous surfactant or helium-oxygen mixtures for severely ill infants requiring intubation and mechanical ventilation has yielded mixed results and remains experimental. For treatment purposes, patients who had 2 exacerbations requiring oral systemic corticosteroids in the past 6 months, or 4 wheezing episodes in the past year, and who have risk factors for persistent asthma may be considered the same as patients who have persistent asthma, even in the absence of impairment levels consistent with persistent asthma. Mycoplasma pneumoniae Infections One of the basic tenets regarding respiratory infections in children is that "bacteria do not make you wheeze. Atypical pneumonia (diffuse infiltrates with nonlobar pattern; fever, malaise, myalgias) is often caused by M. Vocal Cord Dysfunction A functional disorder that mimics asthma, vocal cord dysfunction is typically manifested as wheezing, dyspnea, and shortness of breath refractory to treatment with inhaled bronchodilators. Vocal cord dysfunction should be considered in patients with wheezing who present with atypical findings or those who are difficult to treat. The wheezing is produced by adduction of the vocal cords during inspiration and expiration. The resultant high-pitched inspiratory and expiratory noises are transmitted to the chest, although the sounds are best appreciated over the larynx. The diagnosis is established by direct laryngoscopy, which demonstrates paradoxical motion of the vocal cords. If both main stem bronchi or the trachea are obstructed (typically by larger foreign bodies), the patient may have asphyxia and sudden death; aspiration of foreign bodies in the distal airways often takes a more indolent course. Aspiration of foreign bodies is most common in children between 1 and 4 years of age, particularly in boys or in children with neurologic disorders or delayed development. The most common objects aspirated by children are small toy parts, coins, marbles, balloons, and food products. Endobronchial aspiration of peanuts, raisins, popcorn kernels, or seeds tends to produce more difficulties than other kinds of foreign bodies (metallic or plastic objects) because, in addition to causing physical obstruction of the airway, vegetable matter produces an intense, local inflammatory response secondary to chemical and allergic bronchitis. Esophageal foreign bodies can produce significant respiratory symptoms as a result of extrinsic compression of the posterior trachea. This compression can produce respiratory distress, stridor, and wheezing, especially in infants and young children. Dysphagia and vomiting can be late symptoms associated with an esophageal foreign body. The typical clinical manifestation after the acute event is abrupt respiratory distress, characterized by choking, gagging, cyanosis, and a harsh, paroxysmal cough (see Chapter 2). However, because many aspiration events occur while children are unsupervised, the history of foreign body ingestion or aspiration is frequently not elicited. Because the object is most frequently aspirated into the main stem or segmental bronchi (distal airway), the wheezing is typically unilateral. Physical examination may also reveal a decrease in breath sounds on the obstructed side, prolongation of the expiratory phase, and a tracheal shift. In some instances, retained foreign bodies in the airways can produce a persistent pneumonitis, and the chronic inflammatory response can result in bronchiectasis or lung abscess. Retained foreign body should be considered in a child with presumed asthma or pneumonia who is not improving with appropriate treatment. For treatment purposes, patients who had 2 exacerbations requiring oral systemic corticosteroids in the past year may be considered the same as patients who have persistent asthma, even in the absence of impairment levels consistent with persistent asthma. Radiopaque foreign bodies are generally easily visualized by radiographic studies. Radiolucent foreign bodies may become apparent on inspiratory or expiratory chest radiographs, lateral decubitus films, fluoroscopy, or barium swallow studies when an esophageal foreign body could be compressing the posterior tracheal wall. Because an occasional foreign body may not lodge in a bronchus, typical radiologic findings may not be seen. If a foreign body is likely to be present, rigid bronchoscopy for examination of the lower airway and foreign body removal is indicated. Flexible bronchoscopy provides an excellent visualization of the airway and should be reserved for when other diagnoses appear to be much more likely. Epiglottitis is the most serious life-threatening infection in this area and must be identified quickly. A history of prior intubation in a patient with stridor and respiratory distress should raise concern for vocal cord paralysis or subglottic stenosis. Croup Laryngotracheal bronchitis (croup) is generally a slowly progressive, mild, self-limited viral inflammation of the subglottic larynx occurring in infants and young children. The most common causes are parainfluenza virus types 1 and 3, influenza A, respiratory syncytial virus, and adenovirus. The circumferential cricoid cartilage, which comprises the subglottic airway just below the vocal cords, is the narrowest part of the upper airway in a child. The inflammation associated with a viral infection in this location causes airway obstruction as edema develops within the confines of the cricoid cartilage. Most patients will develop mild rhinorrhea, cough, and low-grade fever prior to characteristic barky cough and inspiratory stridor (see Chapter 2). Stridor typically worsens when the patient is upset or active, and improves with warm humidified air. Unless the airway obstruction is severe, the child generally has Stridor Stridor, a harsh medium-pitched sound typically heard on inspiration, is caused by turbulent airflow in the upper airway. The phase of respiration in which stridor occurs is helpful in identifying the site of the airway obstruction. The relative anatomy of the upper airway in an adult versus in an infant is shown in. The most common cause of stridor of infants and young children is laryngomalacia, Congenital anomalies should be suspected in children with recurrent or persistent stridor. If a patient develops drooling or rapid progression of respiratory distress, epiglottitis or bacterial tracheitis should be considered. If the diagnosis is not clear, obtaining a lateral neck radiograph is indicated and will show the classic "steeple" sign. Management varies from outpatient observation with parent education to endotracheal intubation. For mild cases, the patient must be well hydrated; the use of extra humidity is soothing to the airways and helps to keep secretions from being tenacious, so that they are less likely to become obstructive. In more severe cases (stridor at rest, retractions), nebulized epinephrine used as a mucosal vasoconstrictor may provide relief. Usually, patients being treated in this manner are observed in the hospital for a possible "rebound" effect that may occur 2-6 hours after treatment. Parenteral or oral dexamethasone is a safe and effective additional therapy for moderate to severe croup; steroid use has decreased the requirement for endotracheal intubation. If intubation is needed, an endotracheal tube one-half to one size smaller than that used for a child with a normal airway of the same age and size is chosen. In atypical cases of recurrent croup or in patients in whom extubation is difficult, an endoscopic evaluation of the airway with laryngoscopy and bronchoscopy is necessary to exclude an underlying anatomic abnormality. Bacterial Tracheitis Bacterial tracheitis is a bacterial superinfection of a previous tracheal (croup, influenza virus) viral process and is usually caused by Staphylococcus aureus. Relative comparative anatomy of the larynx in an infant (left) and an adult (right).
Order purim visa
Deprivation amblyopia is caused by opacities in the visual axes such as cataracts or corneal scars or macular and optic nerve conditions medicine 3604 pill discount purim 60caps overnight delivery. If the visual obstruction is not cleared by 3 or 4 months of age, amblyopia becomes very dense and unresponsive to treatment; hence, there is urgency to identify and treat congenital cataracts. Treatment of underlying causes of amblyopia is important for the success of therapy. Nystagmus can be unilateral or bilateral; it can be horizontal, vertical, torsional, or a combination of the above. Jerk nystagmus has one direction faster; pendular nystagmus has both directions of equal speed. Although these classifications are useful for documentation and monitoring, they have limited value in treatment approach. Dividing nystagmus based on etiology has more value for managing this type of abnormal eye movement. In infancy, nystagmus can be divided in to nystagmus secondary to poor vision, nystagmus associated with neurologic anomalies, and various types of congenital/infantile nystagmus. Optic nerve atrophy, hypoplasia, or severe optic nerve anomalies along with early-onset retinal dystrophies or macular scars are the main causes for nystagmus associated with poor vision in infancy. Patching is the oldest and most often used method in all forms of monocular amblyopia. Atropine daily can be used as first-line therapy in monocular moderate amblyopia or as a second line in patch failure. If bilateral amblyopia is present because of high refractive error, glasses are prescribed. On the other hand, genes that control the development and function of the eye are spread on multiple chromosomes. Therefore, it is not surprising that the majority of chromosomal anomalies involve the eye in some form. Following is a selection of eye features that are important given their frequency or severity. Because of this, children with Down syndrome should be examined by an ophthalmologist during infancy and periodically after that. From front to back, the eye findings are as follows: significant refractive errors, amblyopia, nystagmus, strabismus, nasolacrimal duct obstruction, epicanthus, telecanthus, upward slant of palpebral fissures, blepharitis, keratoconus, glaucoma, iris nodules (Brushfield spots), cataract, and optic nerve swelling. Caution should be exercised when using dilating drops in these children because they can have an exaggerated systemic reaction to atropine. The Blind Infant the definitions of blindness that are used in literate children (legal blindness Snellen visual acuity less than 20/200 or visual field less than 20 degrees) are not applicable to infants. The majority of tests used to estimate vision in infants give at most 20/400 vision at birth and vision less than 20/40 by 1 year of age. This is suggested by history and examination clues: absence of any light reaction including no pupillary reaction, absent eye movements, nystagmus early in life, searching eye movements, oculodigital sign, paradoxic pupillary reaction (dilation with light), staring at bright lights, and waving of hands between the eyes and a light source. Important medical history details include history of prematurity, perinatal hypoxia, and family history of blindness at a young age. Three major causes for blindness at this young age are: obvious eye malformations; anterior visual pathways disease (retina, optic nerve, chiasm), which can be subtle; and cerebral visual impairment. For more subtle cases of anterior visual pathway disease versus cerebral visual impairment, nystagmus can be the distinguishing factor, as it is normally present in the former and absent in the latter. The possibility of cerebral visual impairment, suggested by normal structure of the eye and no nystagmus, can be confirmed with normal vestibulo-ocular response with prolonged "after" nystagmus. Absence of vestibulo-ocular reflex and nystagmus suggests the presence of congenital motor apraxia, bilateral Duane syndrome, or Ms syndrome, when the baby cannot move the eye but vision may still be good. Likewise, after a generalized seizure, the movements of the eye or reaction to visual stimuli can be suppressed and simulate blindness, with recovery after the postictal period. Other eye features in this syndrome are microphthalmia, cyclopia, short/slanted palpebral fissures, ptosis, hypertelorism, corneal opacities, luxation of the lens, coloboma of the lens, persistent tunica vasculosa lentis, persistent fetal vasculature formerly known as persistent hyperplastic primary vitreous, typical coloboma of the choroid, and retinal dysplasia. Ankyloblepharon filiforme adnatum (strands joining the upper and lower lids together) is very suggestive of trisomy 18. Less frequently, strabismus, cyclopia, colobomatous microphthalmia, microcornea, corneal opacities, congenital glaucoma, posterior subcapsular cataract, and retinal depigmentation are present in this syndrome. This creates a situation in which cells throughout the body have only one copy of the tumor suppressor gene and are vulnerable to lose that copy and start developing tumors, among them retinoblastoma, which tends to be bilateral and start at a young age. Other ocular abnormalities are almost always present and severe, including microphthalmia, iris and choroidal colobomas, ptosis, cataracts, down-slanting palpebral apertures, and epicanthus. Goldenhar syndrome is probably a variant of this group, with characteristic limbal dermoids and orbital lipodermoids. Limbal dermoids are reported more frequently than lipodermoids and are occasionally bilateral. Another common finding is an upper eyelid coloboma almost always on the more affected side. Eye Findings in Craniofacial Syndromes Eye abnormalities can be associated with congenital anomalies of the face, skull, or head in both craniosynostotic and nonsynostotic forms. About 10% of patients with Pierre Robin sequence have Stickler syndrome as well, with the additional features of high myopia, propensity for retinal detachment, cataracts, deafness, and arthritis. Proptosis is secondary to maldeveloped, small orbits and can further be complicated by lagophthalmos, exposure keratopathy, or globe subluxation. Globe subluxation, when the globe protrudes anteriorly to the eyelids, is an ocular emergency that needs to be treated by the caregiver or medical personnel immediately to avoid optic nerve ischemic damage with permanent vision loss. One approach for globe subluxation is to place a finger on the visible conjunctiva in the interpalpebral area and apply firm pressure until the globe is behind the eyelids. Lagophthalmos, leading to exposure keratopathy, can result in significant corneal dryness, severe infection, corneal scar, and even corneal melt that can cause globe perforation. For this reason, lagophthalmos requires aggressive treatment to prevent dry eyes, using methods such as frequent lubrication with eye drops, gels, or ointment; moisture chamber; taping of the eyelids closed at night; and/or tarsorrhaphy. Edema is secondary to increased intracranial pressure because of the limited expansion of the cranium and less often because of a mass effect caused by compressive optic neuropathy resulting from a tight optic canal. Optic atrophy and related vision and visual field loss is the end result of long-standing optic nerve edema. Strabismus is a common occurrence in craniosynostosis with V pattern exotropia and inferior oblique overaction seen as characteristic types. Because of comparable cranial and orbital anomalies, eye findings can be similar in the other craniosynostosis syndromes such as Crouzon syndrome, Apert syndrome,58 Saethre-Chotzen syndrome, and Pfeiffer syndrome. Eye disorders, which are less frequently encountered, include hypertelorism and downslanting palpebral fissures, dacryostenosis, strabismus, nystagmus, ptosis, severe myopia, and pupillary abnormalities. Other eye involvement has been described: microphthalmia, refractive errors, and vertical strabismus. Congenital torticollis is one of the deformation syndromes that can have ophthalmic implications, as it may be confused with superior oblique palsy with compensatory head posture. Eye Findings in Neurocutaneous Disorders (Phakomatosis) Eye findings are important manifestations in phakomatoses, a group of disorders featuring discrete hamartomas in multiple organ systems, including the skin and the brain. Four disorders have been designated as classic phakomatoses, with other conditions sometimes included as well. From the four classic phakomatoses-neurofibromatosis, tuberous sclerosis, encephalotrigeminal angiomatosis, and retinal angiomatosis-only the first three are active in infancy or early childhood. Retinal lesions, called astrocytic hamartomas (or "phakomas") have one of two distinct appearances. Phakoma type 1 is seen at a very young age and has the appearance of gray-white nodules with a smooth, flat surface and indistinct borders. Consequently, these lesions are difficult to visualize, and special techniques are employed on indirect ophthalmoscopy to avoid missing the early lesions. Neurofibromatosis 1 (von Recklinghausen disease) is characterized by melanocytic and glial cell lesions distributed in the brain, skin, and eye. The occurrence of these lesions is highly age dependent, with some features present early in life with stabilization or regression, whereas other features start late with subsequent progression throughout life. Neuroimaging should be obtained in patients with ocular pulsations, neurofibromas of the eyelid, afferent pupillary defect, or optic nerve swelling. Progressive enlargement of the globe or buphthalmos is seen if glaucoma with high intraocular pressure is present before 2 years of life. Iris Lisch nodules that are often sought to help in early diagnosis are rarely seen in infants and in only 25% by 2 years, with 90% presence by puberty. Ocular Trauma Two types of eye trauma are seen only in infants: birth trauma and shaken baby syndrome.
Buy cheap purim 60caps line
The average age of presentation in bilateral cases is about 10 months symptoms 6 year molars buy purim canada, and 21 months in unilateral cases. Magnetic resonance imaging of the brain may detect a pinealoblastoma46 (trilateral disease). Leukocoria is detected more often by a parent or family member (80%) than a medical professional, despite routine screening with red reflex. Screening the red reflex after dilation might be a way to detect retinoblastoma in its early stage, with improved visual prognosis and ocular survival. Mutation or inactivation of both alleles in a vulnerable retina cell results in transformation of the cell into retinoblastoma. Hence, all infants with strabismus require a fundus examination with dilated pupils to exclude retinoblastoma. With further enlargement, the tumor produces secondary glaucoma, which may be associated with pain and photophobia or symptoms identical to those of congenital glaucoma. With extension into the anterior chamber, an opaque layer of leukocytes (pseudohypopyon) or spontaneous bleeding (hyphema) can occur. Massive necrosis of the tumor can cause a presentation mistaken for orbital cellulitis. The diagnosis of retinoblastoma is made noninvasively by examination under anesthesia with ophthalmoscopy, orbital ultrasound, and fluorescein angiography. The treatment of retinoblastoma involves a team approach among pediatric oncologists, radiologists, and ophthalmologists. The most significant factor in the prognosis is the stage of disease when treatment is instituted. When retinoblastoma is limited to the eye, 98% of patients can expect 5-year disease-free survival. Hematogenous spread to the bone and liver,80 along with direct spread to the brain, indicates a very poor prognosis. Local treatment modalities for early, small tumors include photocoagulation, plaque radiotherapy, transpupillary thermotherapy, and cryotherapy. Enucleation continues to be a treatment modality that is often used in unilateral advanced retinoblastoma to avoid chemotherapy. Selective intra-arterial chemotherapy is also being investigated as an enucleation-sparing procedure. Patients with the familial form of retinoblastoma also are at risk for developing secondary malignancies. It is semitransparent and located in the superficial posterior pole of the retina. The diagnosis of tuberous sclerosis is based on clinical criteria and can be confirmed with molecular gene testing for chromosome 9q34 and chromosome 16p13. They are thought to be congenital abnormalities, but remodeling may occur over the years. Growth into the orbit can cause diplopia, proptosis that is usually nonpulsatile, orbital bruit, and conjunctival vascular dilatation. Congenital/ infantile esotropia, early accommodative esotropia, esotropia associated with neurologic conditions or prematurity, and sensory esotropia are frequent forms of comitant esodeviation in infancy. Some of the more common strabismus seen in childhood is infantile strabismus, accommodative esotropia, and sensory strabismus. That is when the eyes are converged in order for both eyes to be able to look at the same target (the eyes turn toward each other compared with a resting parallel state). The oculomotor system receives information from each eye and superimposes the images. This mechanism of superimposing is also used by the brain to ensure the eyes are aligned at all times, by providing a check and balance between the two images acquired from each eye. The oculomotor system requires a certain level of vision in both eyes to maintain ocular alignment. If vision is lost in one or both eyes, the brain does not have the full ability to maintain alignment, and an ocular misalignment may follow. Unilateral vision loss results more often in esodeviation, unlike older ages when it results more in exodeviation. It is paramount therefore to visualize macula in evaluation of esotropia in infants. Incomitant deviations are variable on various gaze positions and result from impairment of the globe movements secondary to muscular restrictions or muscular weaknesses. Fractures with entrapment of muscles or orbital tumors can cause restrictive strabismus. Cranial nerve palsies and congenital myasthenia gravis are main causes for nonrestrictive incomitant strabismus in infants. In cranial fourth nerve palsy, compensatory head position to the opposite side along with incomitant vertical strabismus can be noticed as early as a few months of life. Other forms of incomitant strabismus-alphabet patterns, Duane syndrome, or Brown syndrome-are likely present at this age group, but hard to diagnose given the low degree of cooperation. To further complicate the evaluation of strabismus in infancy, two conditions can be confused with true strabismus. Early in infancy, there could be small angle misalignments of variable magnitude before the establishment of firm foveal fixation. This condition resolves with development of foveal fixation and binocularity and establishment of firm control of eye movements; this type of misalignment leaves no long-term consequences. Another condition is pseudostrabismus, which can present as pseudoesotropia or pseudoexotropia. In pseudoesotropia, the large nasal bridge, prominent epicanthal folds, or other configurations of the face in the infant can create an appearance of inward deviation of one or both eyes. Symmetric red reflexes and corneal light reflexes with no eye shift at cover-uncover test, differentiate pseudoesotropia from true esotropia. It is important to remember that epicanthal folds may exist with true esotropia, and if there is an intermittent esotropia, the eye may be straight on one examination. Treatment of strabismus is done by a pediatric ophthalmologist after a complete eye examination, including careful cycloplegic refraction and dilated fundus examination. Surgery is the main treatment in infantile esotropia and is performed after correction of significant refractive errors and treatment of associated amblyopia. Surgery should be undertaken early to increase chance of binocular cooperation (4-6 months in healthy infants). Infantile nystagmus syndrome is diagnosed based on clinical characteristics, seemingly unaffected vision, and absence of other neurologic signs. On the other hand, in spasmus nutans (triad of nystagmus, head nodding, and torticollis) brain imaging is mandatory. Fine and rapid, asymmetric nystagmus seen in spasmus nutans can resemble nystagmus seen in chiasmal glioma. Hence the benign nature of spasmus nutans can be demonstrated only retrospectively after disappearance (usually within 2 years). Hoyt and co-workers have reported that opsoclonus may occur as a transient phenomenon in healthy neonates. The major diagnostic consideration for opsoclonus in the first several years of life is a neural crest tumor such as neuroblastoma. Neuroblastoma is found in approximately half of cases with opsoclonus in this age range. It is a consequence of various organic processes that interfere with development of vision during a critical young age. Amblyopia can develop at any time during the "sensitive period" of visual development, usually during the first 7 years in humans, and can be treated if discovered within this same time frame of plasticity. Even if the organic causes are present, the amblyopia might still be partially responsive for the decreased vision and important to treat in a timely manner for a better success rate. Strabismic amblyopia occurs in children who first develop strabismus and then favor one eye. The constantly deviated eye will then develop amblyopia; hence, strabismic amblyopia is always unilateral. Refractive amblyopia results from large refractive errors that create significant blurry vision. Regular contusions and lacerations happen at this age also but with decreased frequency compared with late ages, owing to decreased mobility in infants. Such findings, however, should increase the suspicion of associated intraocular injuries. Retinal hemorrhages are common after delivery, occurring in 78% of newborns after vacuum delivery, 30% after normal vaginal delivery or with forceps assists, and only 8% after cesarean delivery.

Purim 60 caps without a prescription
The physical examination reveals tachycardia and decreased heart sounds symptoms 5 weeks pregnant purim 60 caps fast delivery, and chest radiography shows a massively enlarged heart. Cardiomyopathy may be congenital, may have a metabolic or toxic cause, may be familial, or may be idiopathic. Other causes of cardiac failure, such as severe hypertension, renal failure, and severe anemia, should also be sought. Systemic ventricular failure caused by obstructing lesions, such as aortic stenosis, coarctation of the aorta, or mitral stenosis, also causes increased pulmonary vascular engorgement and edema, which results in the same symptoms as those for a large left-to-right shunt. Depending on the severity of the left ventricular outflow obstruction, systemic blood flow may be decreased, resulting in poor perfusion and metabolic acidosis. If blood flow into the systemic ventricle from the Cystic Fibrosis Cystic fibrosis is a multisystem disorder that involves the eccrine and mucous secretory glands. Inherited as an autosomal recessive trait, cystic fibrosis is the most common life-shortening genetic disease in white children and is an important cause of chronic suppurative lung disease (see Chapter 2). Chronic infection and inflammation lead to the weakening and destruction of the airway wall, which results in bronchiectasis, the abnormal dilatation of the subsegmental airways, and in pulmonary abscesses. The pulmonary deterioration characteristic of cystic fibrosis is rather insidious and is characterized by increasing airway obstruction over a period of years. However, some infants and children with cystic fibrosis can present in acute respiratory distress because of pneumonia, empyema, or pneumothorax. Tachypnea, wheezing, cyanosis, and metabolic acidosis are typical presenting signs. Accurate diagnosis depends on echocardiography; cardiac catheterization may be needed in complex cases. Other Metabolic derangement that results in acidosis can produce tachypnea and possible dyspnea. Common causes of acidosis include diabetic ketoacidosis, sepsis, and ingestions (such as aspirin). The presence of multisystem involvement in addition to respiratory distress should lead to arterial blood gas determination, urinalysis, and possibly a toxicology screen. Neurologic Children with certain primary neurologic disorders, such as increased intracranial pressure or neuromyopathic weakness, may present in respiratory distress. Common symptoms include irregular respirations, hypoventilation, or hyperventilation. The distress may be secondary to respiratory, cardiovascular, hematologic, or central nervous system diseases. Once the cause is identified, treatment should be started quickly to avoid progression to respiratory failure. It is imperative to identify the symptoms of impending respiratory failure and not delay treatment with unnecessary clinical or radiologic studies. It is also important not to miss a foreign body, which with time may produce chronic respiratory disease that is often confused with pneumonia or asthma. Signs of a more chronic process include lack of resolution with normal therapy, chronicity of symptoms, positive family history, digital clubbing, weight loss, and/or failure to thrive. These signs should prompt further work-up and consultation with a pulmonary specialist as needed. Asthma will rarely cause digital clubbing, so its presence should raise concern for another primary lung disease process. Importance of acute Mycoplasma pneumoniae and Chlamydia pneumoniae infections in children with wheezing. Antibiotics for community-acquired lower respiratory tract infections secondary to Mycoplasma pneumoniae in children. Acute Inflammatory Upper Airway obstruction (Croup, Epiglottitis, Laryngitis, and Bacterial Tracheitis). Allergic bronchopulmonary aspergillosis: review of literature and proposal of new diagnostic and classification criteria. Executive summary: the management of community acquired pneumonia in infants and children older than 3 months: Clinical practice guidelines by the Pediatric Infectious Disease Society and the Infectious Diseases Society of America. An official American Thoracic Society clinical practice guidelines: Classification, evaluation, and management of childhood interstitial lung disease in infancy. Allergic bronchopulmonary aspergillosis: New concepts of pathogenesis and treatment. The second most common cause of ear pain is otitis externa, followed by dermatitis and infections of the pinna (see Table 4. A careful examination of the pinna, external auditory canal, and tympanic membrane can help the clinician identify most causes of ear pain. When the findings are normal, the clinician should consider referred pain (Table 4. On otoscopic exam, the external canal is erythematous and there is typically drainage. Relapsing polychondritis also involves swelling and redness of the pinna; this condition is usually bilateral and recurrent, and other cartilaginous structures are affected. With referred ear pain, such as from tooth decay or teething, there are often additional symptoms associated with the respective head and neck structures (see Table 4. Patients with ear pain secondary to maxillary sinusitis may also complain of headaches and purulent rhinorrhea. Physical Examination In a child presenting with a chief complaint of ear pain, the general examination includes the temperature, the respiratory rate, and a determination of whether the infant or child has a toxic appearance. Then the clinician proceeds with the complete head, eyes, ears, nose, oral cavity, and throat examination and with an appropriately focused physical examination of other pertinent systems. The clinician should inspect the pinna and adjacent tissues for dermatitis, redness, and edema. The pinna, including the cartilaginous portions, and the mastoid process are palpated for any tenderness. Erythema, swelling, and tenderness over the mastoid process suggest mastoiditis; whereas localization of these findings to the external auditory canal and the pinna suggests otitis externa. In both conditions, the swelling may be so severe that the pinna is laterally displaced. The opening of the external ear canal is also examined for the presence of discharge or exudate. Most disorders of the external ear can be detected through this examination (see Tables 4. Otoscopy provides an opportunity to indirectly view the middle ear through the tympanic membrane. The middle ear is normally an airfilled cavity that transmits sound from the eardrum to the ossicle and then into the internal ear. Otoscopy begins by properly positioning and, if necessary, restraining the patient. Both shoulders and hips need to be stabilized so that the patient cannot roll during the examination. Cerumen (ear wax) is a waxy substance consisting of glandular discharge from cells in the outer external canal mixing with exfoliated epithelial cells. Cerumen can both obscure visualization of the eardrum leading to diagnostic errors and be a cause of otalgia if History Older, verbal children with ear pain are often able to localize and accurately describe their symptoms. Even though ear pulling is associated with ear pain, it is neither specific nor sensitive in the diagnosis of ear disease. In taking a history from a child who presents with ear pain, the clinician must distinguish between true ear pain and the sensation of fullness and discomfort that children experience when they have an effusion or retracted tympanic membrane secondary to a dysfunctional eustachian tube. A careful review of systems should elicit associated fevers, sore throat, reflux symptoms, otorrhea, neurologic symptoms, and symptoms of sinusitis. Acute otitis media presents with abrupt onset of otalgia associated with middle ear fluid, signs and symptoms of inflammation, and local or systemic infection. To view the eardrum properly, the examiner should remove the wax by irrigating the ear canal gently with lukewarm water, lift the wax out with a blunt curette, or dissolve the wax by placing 1-2 drops of docusate sodium liquid in the canal for 10-15 minutes. Contraindications for irrigation or use of a cerumenolytic solution are the presence of a tympanostomy tube, a perforated tympanic membrane, or an organic foreign body. During the insertion of the speculum, the clinician should note any redness, edema, tenderness, exudate, furuncles, or vesicles that may be present in the external auditory canal. In some illnesses (otitis externa), the ear canal may be so edematous that the speculum cannot be inserted and the eardrum cannot be seen. In addition, in neonates and in some children with craniofacial anomalies such as trisomy 21, the external canal may be so small that it precludes an accurate assessment of the tympanic membrane.
Order purim amex
Because the conjunctival sac is absent or small treatment 12mm kidney stone purim 60caps cheap, attempts to separate the lids from the ocular structures are usually unsuccessful, and surgical correction is not advisable in most circumstances. Causes include familial, syndromic, and chromosomal abnormalities and environmental influences during gestation. Simple microphthalmia is a condition in which there is an abnormally small eye but with intact internal organization. It may be associated with other ocular features of importance: a high degree of hypermetropia, retinal folds, a tendency for choroidal effusions, and the late occurrence of glaucoma. Typically this form is associated with other ocular anomalies such as colobomas of the iris, ciliary body, fundus, or optic nerve, or colobomatous orbital cysts. It is often accompanied by other congenital anomalies, such as central nervous system defects and mental retardation, and has been observed in isolation, in genetic defects. However, the lids remain closed and can be partially fused, and they are smaller and sunken without the support of the eye. Treatment involves reconstruction of the orbit to improve the appearance of the face. Because of the heterogenicity of associated findings, infants with microphthalmia should be evaluated by both an ophthalmologist and a geneticist. An apparently enlarged eye may be caused by colobomatous microphthalmia with an associated large cyst, congenital megalocornea, or congenital glaucoma (see p. Colobomatous microphthalmia results when the embryonic optic vesicle fails to close. Tissue that originally should have become intraocular is encased in a cystic structure outside the eye in the orbit. If the cyst becomes sufficiently large that proptosis occurs, the microphthalmic eye simulates an enlarged eye. The overlying conjunctiva and the conjunctival vessels superimpose a filmy, vascular pattern. A generalized bluish discoloration of the underdeveloped sclera is normal in premature infants. Rarely, a congenital weakness in a small area of the sclera produces a bluish bulge called a staphyloma. The lightblue color is caused by thinness of the sclera that transmits the darker color of the underlying uveal tissue. Osteogenesis imperfecta may be associated with a similar bluish discoloration of the sclera in the term neonate because of inadequately developed scleral collagen. Blue sclera may also be seen in other systemic diseases such as Marfan syndrome, EhlersDanlos syndrome, and Crouzon syndrome. Intrascleral nerve loops appear as darkly pigmented dots about 3 to 4 mm from the limbus. Congenital ocular melanosis and oculodermal melanosis (nevus of Ota) occur as a unilateral slateblue pigmentation in infancy. There are no other features of congenital glaucoma, such as elevated intraocular pressure, tearing, photophobia, or conjunctival injection. Megalocornea as an isolated finding is usually inherited in an autosomal dominant manner. Megalophthalmia, which is commonly inherited as an X-linked recessive trait, is characterized by deep anterior chambers, subluxation of the lens, hypoplastic iris, and cataract formation in early adult life. A corneal diameter of less than 10 mm may be an isolated finding or may be associated with other ocular anomalies. Cases of autosomal dominant and recessive inheritance of microcornea have been described. In the normal term infant, a similar appearance may be seen for the first 48 hours after delivery. A persistently hazy or cloudy cornea suggests congenital glaucoma or birth injury. This condition is characterized by bilateral cloudy corneas, normal corneal diameter, and normal intraocular pressure. If this measurement exceeds 12 mm, congenital glaucoma must be considered, especially if corneal haze, tearing, and photophobia are present. Associated ocular findings include glaucoma, corneal pannus, cataract, abnormal optic discs, and foveal hypoplasia. Because the fovea subserves our best vision, its maldevelopment causes the nystagmus and poor visual acuity. The classic symptoms of congenital glaucoma include tearing, light sensitivity, and blepharospasm. Congenital glaucoma can occur as a primary disease or secondary to numerous other ocular conditions or systemic syndromes. In addition to visual impairment from glaucomatous damage, amblyopia from visual deprivation or anisometropia can prevent a successful visual outcome. The prognosis depends on the age of onset, time to diagnosis, and associated ocular and systemic conditions. Unlike glaucoma in adults, the treatment is surgical in the vast majority of cases, and medical management is used only for temporizing the condition or better visualization for various surgical procedures. It can occur as a single ocular finding, have a Mendelian mode of inheritance, be associated with a chromosomal abnormality, or be associated with other malformation syndromes (Box 103-4). Aganglionic megacolon (Hirschsprung disease) can also be associated with iris heterochromia. Abnormal Red Reflex this is one of the most important abnormalities that requires immediate evaluation. The term leukocoria is used to describe a white pupil seen by the naked eye or during the red reflex test. Because the infant sleeps much of the time and the pupils are small, a white pupil often is not noticed until the infant becomes more alert and active. False-positive red reflex test results are commonly caused by small pupils, shifting gaze, limited patient cooperation, poor illumination from the ophthalmoscope, and examiner inexperience. Regardless, these patients should be over-referred to the ophthalmologist to ascertain the true-positive results. Abnormal red reflexes can also result from misaligned eye or high or asymmetric refractive errors. Because typical iris colobomas result from an abnormal closure of the embryonic fissure, they also may be associated with a coloboma of the ciliary body, fundus, or optic nerve. When the optic nerve or macula is involved in the coloboma, visual difficulty occurs. It is always wise to evaluate the fundus for a pathologic condition when an iris coloboma is detected. Atypical colobomas, which vary from a small notch in the pupil to the absence of an entire segment of the iris, are not usually associated with visual difficulties. The lens grows continuously during life, laying down new lens fibers on its external surface much as an onion does. The lens is preserved in capsules (anterior and posterior), and has a nuclear core and surrounding cortical portion. Childhood cataracts can be classified as congenital, infantile, or juvenile, depending on the age of onset. Congenital and infantile cataracts are responsible for about 10% of all blindness worldwide. The etiology of pediatric cataracts can be broadly classified and summarized as hereditary, metabolic. Furthermore, cataracts can be classified according to their morphology as diffuse/total, anterior polar, lamellar, nuclear, posterior polar, posterior lentiglobus, posterior (and anterior) subcapsular, persistent hyperplastic primary vitreous, and traumatic. The size and shape of a cataract depends on the area of the lens that is being formed at the time the damage or developmental defects occur. Damage that occurs in the early embryonic period produces opacifications in the center of the lens. The membranes are remnants of the anterior fetal vascular supply of the lens that failed to atrophy in the seventh month of gestation.