60 caps shallaki visa
Diagnosis is via demonstration of the characteristic cysts in bronchial aspirates muscle relaxant pills over the counter generic shallaki 60 caps with mastercard, bronchial lavage or lung biopsy. Fungi, predominantly candida, are now amongst the most frequently isolated organisms in intensive care units. Patients particularly at risk of frequent fungal infections are neutropenic children and adults. Diagnosis of disseminated fungal infections is difficult but may be diagnosed with certainty if a patient develops endophthalmitis or a positive fungal culture is made from an organ such as the kidney or lung. Empirical treatment should be given to patients with candida in the urine or heavy colonisation at other sites if their clinical condition is deteriorating. Antisepsis is the attempt at the prevention of growth and multiplication of micro-organisms that cause sepsis. Prophylactic antifungal treatment may sometimes be responsible for fungal infections by species other than Candida albicans. The fungi that cause the infections normally live as commensals in the gut lumen and on mucocutaneous surfaces. A susceptible host may be infected either endogenously by organisms from his own gastrointestinal tract or exogenously through hand contact as a result of poor hygiene. Translocation across the gut mucosal barrier may occur but some form of mucosal disruption may also be required. A diagnosis of invasive disease requires the presence of the fungus in normally sterile tissues whilst dissemination is defined as invasion of non-continuous organs secondary to haematogenous spread. Failure to identify and treat those with disseminated fungal infection results in high mortality. If multiple sites are colonised there will be an increased risk of severe infections in patients recovering from abdominal surgery. Present-day pathogens are often resistant to antibiotics, a major problem being methicillin-resistant Staph. Commensal bacteria are potential pathogens, and infection may result if the balance is disturbed by a breach of the body defences or if an organism normally a commensal at one site gains access to another site where it is not a commensal. A detailed knowledge of the normal flora is required to distinguish normal flora in culture from pathogens responsible for infection. Personnel should wear protective theatre clothing, caps to cover the hair, clean theatre underdress, gowns and masks. Chlorhexidine, povidoneiodine or alcoholic chlorhexidine are suitable for hand preparation. Lights above the operating table should be kept dust free to prevent potentially bacteria-laden particles landing in the wound. As far as the patient is concerned, the bed linen and clothes must not be allowed in the theatre area. Any shaving that is carried out should be carried out immediately prior to surgery and not some time before which may allow staphylococci to colonise small lacerations in the skin. Disinfection of the skin at or near the operation site should be carried out and the skin at or near the site of the wound separated from the rest by drapes or occlusive drapes. The incubation period is six weeks to six months and the period of infectivity is from six weeks before onset of the symptoms and possibly indefinitely thereafter. Some epidemic strains are multiresistant, exhibiting resistance to aminoglycosides, macrolides and other antistaphylococcal agents which include the topical agent mupirocin, which has been used to eradicate the organism from carriers. Control depends on a combination of hygiene measures such as isolation of patients with diarrhoea and hand washing (alcohol does not kill spores) between contact with patients and careful use of problem antibiotics such as clindamycin and injectable cephalosporins. Following infection, antibodies are formed against all three of the viral antigens but there are important clinical consequences of their identification. Carriers with a persistence of the e-antigen are much more likely to infect others. It has been shown that surgeons who possess the e-antigen may infect their patients during operative procedures. The severity of the symptoms does not necessarily equate with the extent of the liver disease. Of the remainder 20% will progress to cirrhosis within 20 years and of that 20%, some will progress to liver failure and some will develop hepatocellular carcinoma. Immunological failure results in opportunistic infections and an increased risk of malignancy. Asymptomatic viraemia occurs for up to three months after exposure and patients are infective during this period. Antiviral antibodies are now present in the blood and the patient is infective and this phase may continue for many years. Some patients may develop persistent generalized lymphadenopathy following seroconversion which lasts for up to three months with few or no constitutional symptoms. Appropriate theatre technique should be adopted as follows: - only absolutely necessary personnel should be in theatre. Universal precautions taken include those precautions taken to protect theatre staff from infection with all cases. Any patient considered as a risk should be indicated as belonging to a high-risk category in the operating list; under no circumstances should the disease causing the risk be placed upon the operating list, for reasons of patient confidentiality. The injured person should visit the occupational health department or the nearest emergency department as soon as possible. At the occupational health or emergency department, the following detailed information should be obtained: with deep needle stick injuries who are exposed to large volumes of blood. The drug is highly toxic and should not be used during pregnancy or breast-feeding. Side effects include nausea, malaise, fatigue, headache and bone marrow suppression. Sterilisation by steam under pressure is the most commonly used method in hospitals. Steam condenses on the surface of the instruments in the autoclave, giving up a large amount of latent heat of vaporisation required for its production. Continuous recordings should be made of the temperature in the autoclave, and all sterilisers should have a preset automatic cycle which cannot be interrupted until the cycle is completed. These glass tubes contain fluid which changes from red to green after appropriate exposure. Sterile packs can be identified as appropriately sterilised by changing colour of heat sensitive inks on the pack (Bowie-Dick test). Moist heat is more effective than dry heat because it penetrates materials better and denatures proteins of the cell walls of micro-organisms. If antibody levels are low, a dose of hyperimmune anti-hepatitis B IgG plus one dose of vaccine should be given. Similar procedures should be followed when the source patient cannot be identified or refuses to be tested. The process is not suitable for materials that are denatured or damaged at the required temperature. It may be used for solids, non-aqueous liquids, and to sterilise objects that will stand the heat in enclosed (airtight) containers. All items must be thoroughly cleaned and dried before they are placed in a hot air oven. Formaldehyde Dry saturated steam in combination with formaldehyde kills vegetative bacteria, spores, and most viruses. Adequate prior cleaning of the instruments is required before exposing to formaldehyde. Otherwise, where items are contaminated with body fluids, proteins will be fixed and deposited on the equipment. Disinfection has to be distinguished from cleaning, which is a process which physically removes contamination but does not necessarily inactivate micro-organisms. The efficacy of disinfection depends on several factors: for example, the length of exposure, or the presence of blood, faeces, or other organic matter which may reduce the efficacy of the disinfection process. Some examples of disinfection are given below: Irradiation Sterilisation by ionising radiation is an industrial process and is used commercially for large batches of suitable objects.
Discount shallaki generic
Systemic necrotizing vasculitis is associated with hairy cell leukemia muscle relaxant lactation shallaki 60 caps visa, which is also associated with a high occurrence of polyarteritis nodosa. Sweet syndrome (acute febrile neutrophilic dermatitis) is associated with malignancy in 15% of cases, usually acute leukemia. Fever, leukocytosis, and a characteristic eruption of painful, erythematous papules on the head, neck, and upper extremities compose the syndrome. Erythema nodosum, a variety of panniculitis, is associated with Hodgkin lymphoma and leukemia. Polyarthritis or symptoms that mimic polymyalgia rheumatica, which may be the presenting manifestation of the malignancy. Two-thirds of patients with myeloproliferative disorders have hyperuricemia and hyperuricosuria. The occurrence of acute gouty arthritis in these patients has been markedly reduced with the routine prescription of allopurinol prophylactically. The extremely painful periosteal reaction usually involves the extensor surfaces of the legs and forearms. Clubbing should be self-evident; patients should be questioned about the duration of the abnormality. Joint pain, subcutaneous fat necrosis (panniculitis), and eosinophilia occasionally constitute the presenting features of pancreatic cancer. Myelodysplastic syndromes are associated with a variety of phenomena of suspected autoimmune pathogenesis. No distinguishing features of rheumatic syndromes define the coexistence of cancer. The following syndromes should strongly suggest a thoughtful search for malignancy, particularly if they first occur at 50 years of age. Explosive seronegative polyarthritis presenting with swollen and tender joints, with a predilection for the lower extremities sparing the small joints and wrists, and with mild nonspecific synovitis identified by synovial biopsy 2. Raynaud phenomenon (often with asymmetric involvement of the fingers and progression to necrosis) 6. It is usually symmetric and may resemble rheumatic fever or juvenile rheumatoid arthritis. In 25% of cases, adjacent bone may develop osteolytic lesions, osteoporosis, or osteoblastic changes. Chronic leukemic arthritis is uncommon; it is usually symmetric but is otherwise similar to the acute type both in radiographic patterns and in response to therapy. The problem occurs more often in patients with large tumors, bone invasion, history of large alcohol intake and heavy smoking, poor dentition, poor oral hygiene, and poor nutritional status. The mandible becomes brittle and superinfected, resulting in pain, fractures, and draining fistulas. Mucosal ulceration or necrosis (occasionally, a fistula) with exposure of bone and, occasionally, cutaneous fistulas c. Radiographs showing a osteolytic lesion of the mandible, sometimes with a radiodense sequestrum or involucrum. Manifestations should not be clinically evident for at least 4 months after completion of treatment. Aggressive management (1) Hyperbaric oxygen treatments (2) Surgical resection of the nonviable portion of the mandible (3) A combination of hyperbaric oxygen and surgical resection B. Postirradiation pathologic fractures of the femoral neck may rarely complicate pelvic irradiation. Radiation-induced bone sarcomas have been reported after high-dose irradiation of both benign and malignant lesions. Soft tissue radiation injury depends on dose and those structures which are encompassed by the radiation fields directed to the bony site. Myalgia, stiffness, and elevation of serum creatine kinase following external neck irradiation may be the result of radiation-induced hypothyroidism. Increased pressure in the intramedullary space causes the sudden onset of hip pain. Capsular irritability is demonstrated by flexing the hip and medially rotating the thigh. Removal of bony cores from the necrotic areas predictably, if incompletely, relieves pain and may favorably alter the natural history of osteonecrosis if done before the occurrence of secondary changes, such as collapse of subchondral bone and articular cartilage. Postchemotherapy rheumatism is a syndrome of myalgias and arthralgias that usually develops within 1 to 3 months after completing adjuvant chemotherapy for breast cancer. Extensive workups for breast cancer recurrence or for inflammatory rheumatologic disease are not needed in this setting. Arthralgias associated with taxanes (paclitaxel and docetaxel) usually begin 2 to 3 days after treatment and resolve within 5 days. Arthralgias associated with hormonal therapy occur frequently in patients being treated with aryl aromatase inhibitors (anastrozole, letrozole, exemestane) for breast cancer. Arthralgia and subjective joint stiffness are common complaints, occurring in up to 40% of women who are being treated with one of these agents. The problem often is not solved by changing agents within that class of drugs and may lead to discontinuance of such therapy. Arthralgias have also been reported in patients treated with tamoxifen but to a lesser extent and severity. These occurrences remain significant because long-term treatment is affected by their development. Cases of scleroderma and Raynaud phenomenon have been noted in association with the use of bleomycin. Raynaud phenomenon is a common toxicity of treatment with cisplatin, oxaliplatin, vinblastine, or bleomycin. Many therapeutic regimens in cancer treatment carry the risk of promoting osteoporosis. Therapies involving corticosteroids or causing hypogonadism, including androgen-deprivation therapy and aromatase inhibitors, are the most common causes. Cytotoxic drugs that have been implicated in the development of osteoporosis include methotrexate and ifosfamide. The risk of osteoporosis should be assessed with osteodensitometry when indicated. Treatment with hormone replacement, calcium with vitamin D, bisphosphonates, and/or denosumab can be considered when appropriate. Use of highdose glucocorticoids is also associated with an increased risk of developing osteonecrosis (avascular necrosis of bone). Musculoskeletal pain, occasionally severe, occurs rarely with the use of these agents. Furthermore, "atypical fractures" (transverse femoral fractures and metatarsal stress fractures) have been observed with long-term bisphosphonate use in patients both with and without cancer. Long-term pamidronate treatment of advanced multiple myeloma patients reduces skeletal events. Balloon kyphoplasty versus non-surgical fracture management for treatment of painful vertebral body compression fractures in patients with cancer: a multicenter, randomized controlled trial. Hypertrophic pulmonary osteoarthropathy as a paraneoplastic manifestation of lung cancer. Management of pulmonary cement embolism after percutaneous vertebroplasty and kyphoplasty: a systematic review. Musculoskeletal syndromes associated with malignancy (excluding hypertrophic osteoarthropathy). Methylmethacrylate pulmonary emboli: radiographic and computed tomographic findings. Normal limits in adults are as follows: Hematocrit Red blood cell count Red blood cell mass Men 52% 5.
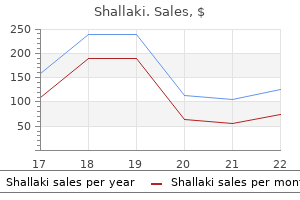
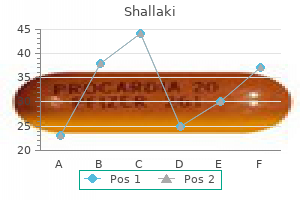
| Comparative prices of Shallaki | ||
| # | Retailer | Average price |
| 1 | Barnes & Noble | 214 |
| 2 | Dell | 444 |
| 3 | Darden Restaurants | 314 |
| 4 | Kroger | 272 |
| 5 | OfficeMax | 750 |
| 6 | AutoZone | 231 |
| 7 | Dollar Tree | 980 |
Order shallaki 60caps amex
Bimanual examination should show a nontender cervix and uterus muscle relaxer 7767 buy shallaki 60 caps, without adnexal tenderness or masses or pain on cervical motion (if present, see Chapter 93). The appearance of the discharge is not pathognomonic and testing needs to confirm any suspicion. Collect urine for possible culture and pregnancy tests that may influence treatment. Swab the cervix or urethra to culture for Neisseria gonorrhoeae and swab the endocervix to test for Chlamydia (see Chapter 83). Touch pH indicator paper (Hydrion pH papers, ColorpHast pH Test Strips) to the vaginal mucus. A more expensive alternative that appears to be more effective and has fewer side effects is tinidazole (Tindamax), also taken as a single 2-g oral dose. The patient must abstain from alcohol for 24 hours postmetronidazole and 3 days after the last dose of tinidazole because of the disulfiram-like activity of these drugs. Advise the patient and her partner to refrain from intercourse or to use a condom until therapy has been completed and patient and partners are asymptomatic, at least 7 days. Follow-up is unnecessary for men and women who become asymptomatic after treatment or who are initially asymptomatic. Pregnant women who are symptomatic with trichomoniasis may be treated with a single 2-g dose of metronidazole, although 500 mg bid for 5 to 7 days is much better tolerated in patients already prone to nausea. Multiple studies and meta-analyses have not demonstrated a consistent association between metronidazole use during pregnancy and teratogenic or mutagenic effects in infants. However, one study did note preterm labor increased when treating with metronidazole orally, thus treatment of asymptomatic pregnant patients can be delayed until after delivery. This will relieve symptoms but is unlikely to eradicate the organisms; thus delayed treatment postdelivery will be needed. It is secreted in vaginal secretions for 72 hours postingestion and is at least as effective as intravaginal treatment. Alternatively, if the oral route is not preferred or medication interaction precludes its use, miconazole (Monistat), 200-mg vaginal suppositories should be recommended. In patients with severe discomfort secondary to vulvitis, low-potency steroid creams used for the first 48 hours, in combination with a topical antifungal cream may be of benefit. Women with medical conditions such as uncontrolled diabetes or those receiving corticosteroid treatment also require more prolonged. During pregnancy, only topical azole therapies, applied for 7 days, are recommended. The patient only needs to return for follow-up visits if her symptoms persist or recur within 2 months of her initial treatment. For recurrent infections, Fluconazole may be repeated and thus taken days 1, 4, and 7. Gastrointestinal side effects are fairly common, and serious side effects can occur. For recurrent Candida, the American Infectious Disease Society recommends 10 to 14 days of a topical or oral azole, such as miconizole or clotrimazole, followed by 6 months of either a clotrimazole 200-mg vaginal suppository twice weekly or weekly doses of oral fluconazole 150 mg. If the diagnosis is bacterial vaginosis, prescribe metronidazole (Flagyl), 500 mg orally bid for 7 days; or tinidazole (Tindamax) can be used orally at 1 g daily for 5 days or 2 g daily for 2 days (taken with food). Alternative therapy includes metronidazole as a single 2-g oral dose (noted to have lower efficacy than the above mentioned regimen); clindamycin, 300 mg orally bid for 7 days; or clindamycin ovules, 100 mg intravaginally qhs for 3 days. A topical single dose bioadhesive form of clindamycin is available (Clindesse); the patient uses one applicator. Clindamycin-resistant organisms can develop in the vaginal mucosa postintravaginal treatment. Intravaginal treatment is more expensive but carries fewer gastrointestinal side effects than the oral form, and some patients prefer using intravaginal products for treating this vaginosis. During pregnancy, prescribe metronidazole, 500 mg orally bid or 250 mg orally tid for 7 days, or clindamycin, 300 mg orally bid for 7 days. Some prefer to use oral rather than topical therapy in pregnancy because it may also treat subclinical coinfections. Vaginal treatment is less preferred in pregnancy because of concerns about possible preterm labor. She should avoid routine douching, perfumed soaps and feminine hygiene sprays, and tight, poorly ventilated clothing. The differential Ninety percent of all cases of vaginitis are caused by bacterial vaginosis, vulvovaginal candidiasis, or trichomonal vaginitis. However, there are noninfectious causes as well- physiologic leukorrhea, a generally nonmalodorous, mucous-like, white or yellowish discharge without other symptoms, is usually estrogen induced. Atrophic vaginitis, caused by estrogen deficiency leads to inflammation of the vagina, and topical estrogen is the treatment of choice. Desquamative inflammatory vaginitis is rare, with signs and symptoms of pain, profuse discharge, and epithelial cell exfoliation. Clindamycin, for its antibacterial as well as its anti-inflammatory effect, works well for these patients. Seminal plasma allergy is in the differential; although rare, it presents with postcoital itching, burning, edema, and erythema and can have systemic symptoms as well. What Not To Do: Do not blindly prescribe creams or other therapies for nonspecific symptoms of vaginitis. Perform the appropriate physical examination and laboratory tests before initiating one of the treatment regimens recommended. Do not miss underlying pelvic inflammatory disease, pregnancy, or diabetes, all of which can potentiate vaginitis. It is unlikely to achieve therapeutic levels in the urethra and perivaginal glands where infection is also located, and is considerably less efficacious than oral preparations. Do not recommend the use of commercially obtainable unstandardized Lactobacillus for treatment of bacterial vaginosis. Recurrence rates are high, and vaginal Lactobacillus replacement remains a clinical research endeavor. Do not miss candidiasis because the vaginal secretions appear essentially normal in consistency, color, volume, and odor. Discussion Trichomoniasis and bacterial vaginosis are often grouped together, despite major differences in etiology, pathophysiology, and transmission implications. The reason that these two entities are frequently considered together is that they present with elevated vaginal pH, major shifts in vaginal flora, and abnormal vaginal discharge that is characteristically malodorous. Trichomonas vaginalis is a parasite that is transmitted primarily through sexual activity. During pregnancy, infection has been associated with delivery of low-birth-weight infants and preterm deliveries. Diagnosis is typically made by identification of motile trichomonads on a saline wet preparation. It is important to note that wet-mount examination can be negative in up to 50% of culture-confirmed cases. However, because studies have demonstrated poor a correlation between vaginal symptoms and the final cause of vaginitis, clinicians should not treat vaginal complaints empirically based on patient history alone. Although this approach to diagnosis is not unreasonable, accuracy can be improved by using complete Amsel criteria. This includes (1) milky homogeneous adherent discharge, (2) vaginal pH greater than 4. Bacterial vaginosis has been so called because of the absence of inflammatory signs traditionally associated with C. Symptoms and signs are extremely nonspecific and can be simulated by a variety of noninfectious causes. Symptoms alone do not allow clinicians to distinguish confidently between the causes of vaginitis. However, if there is no itching, candidiasis is less likely, and lack of perceived odor makes bacterial vaginosis unlikely. Presence of a "high cheese" odor on examination is predictive of bacterial vaginosis, whereas lack of odor is associated with candidiasis.
Cheap shallaki 60 caps online
The development of blast crisis may be accompanied by infection or bleeding due to neutropenia or thrombocytopenia muscle relaxant headache order line shallaki, respectively. The peripheral blood smear in the chronic phase is often described as appearing like a bone marrow aspirate smear due to presence of all stages of myeloid cell maturation. Myeloblasts constitute <15% of the leukocytes in the peripheral blood, and promyelocytes plus blasts combined compose <30% in the chronic phase. Eosinophil and basophil counts are often elevated, but basophils constitute <20% of the peripheral blood leukocytes in the chronic phase. Thrombocytosis is common, and the platelet count may exceed 1,000,000/L at presentation. The hemoglobin level is usually normal, but a mild normocytic, normochromic anemia can be present. Bone marrow aspiration and biopsy should be performed on all patients as part of the diagnostic evaluation. In all cases, the marrow is markedly hypercellular as a result of massive myeloid hyperplasia, resulting in a markedly increased myeloid-to-erythroid ratio. Fibrosis may also be present in variable amounts but is rarely profound in the chronic phase. Cytogenetic analysis should be performed at the time of bone marrow examination on all patients. Cytogenetics are particularly important to determine if additional chromosomal abnormalities associated with advanced disease are present. This Chronic Myelogenous Leukemia 595 assay does not require dividing cells and is more sensitive than cytogenetics at detecting minimal residual disease during therapy. Peripheral blood leukocytosis due to increased numbers of mature and immature neutrophils 2. Bone marrow hypercellular with granulocytic proliferation and often expansion of small megakaryocytes with hypolobated nuclei 7. Platelets 1,000,000/L unresponsive to therapy or 100,000/L unrelated to therapy 4. Cytogenetic evidence of clonal evolution (cytogenetic abnormalities in addition to the Ph1 chromosome) C. There is no myeloid left shift or increased percentage of myeloblasts in the blood or bone marrow. Ongoing assessment of response during therapy has emerged as a much more important predictor of progression-free survival. Advanced-phase disease, especially blast crisis, conveys an adverse prognosis and warrants referral to a tertiary center capable of transplant evaluation. The standard dose of imatinib is 400 mg/d for chronic phase and 600 mg/d for advanced disease. Potential side effects include fluid retention, nausea, diarrhea, muscle cramps, skin rash, fatigue, and myelosuppression. If moderate toxicity warrants dose reduction, re-escalation to a standard dose should be attempted once side effects abate. There is some evidence that second-generation kinase inhibitors, such as dasatinib and nilotinib, may be associated with more rapid achievements of therapeutic milestones. Acquired imatinib resistance is defined as loss of a previous hematologic or cytogenetic response. Clinical case series have suggested that the V299L and F317I mutations confer relative resistance to dasatinib, while the Y253H, E255V/K, and F359V/C mutations are moderately resistant to nilotinib. Patients with the T315I mutation should be referred to a center that is evaluating investigational agents for this mutation. Common side effects include myelosuppression, fluid retention (especially pleural effusion), diarrhea, rash, and bone pain. Dasatinib impairs platelet function and can cause serious gastrointestinal or intracranial bleeding in conjunction with severe thrombocytopenia. Common side effects include myelosuppression, arthralgias and myalgias, rash, and nausea. The same considerations are appropriate for patients who experience treatment failure on imatinib, but dose escalation of imatinib is not likely to provide prolonged benefit. Transplantation is typically reserved for patients who do not have an adequate response to second-line therapy. However, there should be evidence of progressive reduction of disease burden prior to that time point. Failure to achieve this end point by 3 months is considered a primary treatment failure and warrants a change in treatment. Minor cytogenetic response (MiCyR) is the presence of the Ph1 chromosome in 36% to 65% of bone marrow metaphases. Response monitoring should include a bone marrow aspiration and biopsy at baseline and every 3 to 6 months until a complete cytogenetic response is achieved. Therefore, bone marrow cytogenetics remains the gold standard of response assessment. Goals of therapy should be to prevent progression to advanced disease using a dose and schedule of drug with acceptable side effects. Therefore, the goal of therapy should be to suppress the disease to the lowest possible level. This is most important in young patients who would be expected to live with their disease for longer than there is outcome data from clinical Chronic Myelogenous Leukemia 599 trials. For older patients or those with multiple comorbidities, less aggressive cytoreduction may be adequate to prevent disease progression during their lives. Close initial monitoring of potential clinical and laboratory abnormalities is recommended. For patients taking dasatinib, physical examinations should routinely evaluate for development of a pleural effusion. The disadvantage of transplantation is that there is a 15% to 20% risk of mortality at 1 year in young patients, and the risk increases with the age of the patient. The risks and benefits of ongoing medical therapy versus transplantation must be highly individualized and should be discussed in detail with patients as therapy proceeds. Allogeneic transplants using 10/10 matched unrelated donors produce survival results approximately 5% points lower than for patients receiving transplants from matched related donors. Younger patients who are considered good candidates for an allotransplantation should be referred to a transplant center to discuss this option. Should a second chronic or accelerated phase be achieved, allogeneic stem cell transplantation is the only option that confers a chance of long-term survival. Patients who experience severe cytopenias (neutrophils < 500/L or platelets < 20,000/L) on treatment should have a bone marrow biopsy to determine if the low counts are due to the drug or the disease. If the bone marrow is hypocellular without increased blasts, then treatment should be held until the neutrophils are 1,000/L and the platelets are 20,000 to 50,000/L. If increased numbers of blasts persist in the bone marrow, treatment should be continued, and the bone marrow biopsy should be repeated in 2 to 4 weeks if the cytopenias persist. Leukapheresis rapidly decreases the granulocyte count for short periods of time but is time-consuming and expensive. Platelet counts that incorrectly show improvement may be found in patients with marked leukocytosis and advancing disease. The false platelet count happens because the granulocytes become disrupted in the test tube, and automatic platelet counting machines enumerate the larger leukocyte granules as platelets. The paradox is resolved by reviewing the peripheral blood smear and estimating platelet numbers. Fewer than 20% blasts (myeloblasts, monoblasts, and promonocytes) must be present in the bone marrow, and dysplasia must involve one or more myeloid lineages. If dysplasia is not evident, there must be a clonal cytogenetic abnormality, the monocytosis must have been present for at least 3 months, and other potential causes of the monocytosis must have been excluded. Leukocytosis in the range of 11,000 to 50,000/L (because of increased numbers of both granulocytes and monocytes) is present in most patients, but leukopenia occasionally occurs. Granulocytic hyperplasia with increased numbers of promyelocytes and myeloblasts is prominent. The myeloid series in the marrow often has monocytoid features, but pure monocytic hyperplasia is unusual. Cytogenetic abnormalities occur in approximately 20% to 40% of cases, but the Ph1 chromosome is absent. The criteria for determining the appropriateness of this therapy should be extrapolated from the experience with myelodysplastic syndrome.
Safe 60 caps shallaki
An alternative to using nonabsorbable packing is to use absorbable packing material spasms during sleep cheap 60caps shallaki mastercard. The advantages are that there is nothing to remove later, and there is more patient comfort. Choices of absorbable packing material include oxidized cellulose (Surgicel, Johnson & Johnson, New Brunswick, N. The anterior balloon is then inflated with the recommended volume of saline to prevent the posterior balloon from becoming unseated and possibly obstructing the airway. If a commercial posterior balloon device is not available, a 12-Fr Foley catheter may be used. Insert the catheter in to the affected nasal cavity until the balloon is well in to the posterior nasal cavity. Pull the partially inflated balloon anteriorly until it is snug against the posterior turbinates. If there is pain or displacement of the soft palate, remove some of the saline from the balloon. Secure the Foley anteriorly by placing an umbilical clamp over the catheter as it exits the nose. The specialist may use electrocautery, transpalatal injection of vasoconstrictors, endoscopic cautery, surgical ligation, or embolization procedures. If on the other hand, as will most commonly occur, the bleeding has stopped with your interventions, observe the patient for 15 to 30 minutes. If there is no further bleeding from the nares or from the posterior pharynx, the patient may be discharged. If the hemorrhage is suspected to have been large, determine that the patient is not symptomatically orthostatic, and check hemoglobin and hematocrit before discharging. Choices of antibiotics include cephalexin (Keflex), amoxicillin/ clavulanate (Augmentin), clindamycin (Cleocin), and trimethoprim/sulfamethoxazole (Bactrim). Packs for minor bleeds may be removed early; bleeds that are difficult to control or in patients on anticoagulants should be kept in the full 5 days. Warn the patient about not sneezing with his mouth closed, bending over, straining, or picking his nose. Patients with simple nosebleeds can be referred to their primary care doctor for removal of the packing or for a recheck. If pain is a problem, Tylenol should be suggested and aspirin and other nonsteroidals avoided. Prescribe hydrocodone bitartrate/acetaminophen (Vicodin) if you think the pain will not be controlled with Tylenol. If the patient returns with mild oozing of blood from around an anterior pack, you may be able to stop the bleeding without removing the pack. Try injecting a vasoconstrictor directly in to the sponge (not in to the patient), or adding air to a nasal balloon pack. When removing a compressed cellulose sponge pack, soften it with 1 to 2 mL of water or saline and wait 5 minutes, thereby reducing trauma, pain, and the incidence of rebleeding. What Not To Do: Because of the nasopulmonary reflex, arterial oxygen pressure will drop about 15 mm Hg after the nose is packed. With packing in place, these patients are at risk for desaturation and may need admission. Do not waste time trying to locate a bleeding site if brisk bleeding is obscuring your vision in spite of vigorous suctioning. Have the patient blow out any clots and insert the medicated cotton pledgets immediately or go directly to anterior packing. Do not order routine clotting studies unless there is persistent or recurrent bleeding, use of anticoagulants or other evidence of an underlying bleeding disorder. Do not cauterize or place a painful device in the nose before providing adequate topical anesthesia unless rapid hemorrhaging requires it. It will only serve as a plug in the anterior nares rather than as a hemostatic pack. Do not discharge a patient as soon as the bleeding stops, but keep him for 15 to 30 minutes more. Posterior epistaxis typically stops and starts cyclically and may not be recognized until all of the aforementioned treatments have failed. Children tend to bleed secondary to nose picking; adolescents bleed secondary to facial trauma associated with athletic activity or fighting. Epistaxis in the middle-age patient is more often the harbinger of neoplastic disease. Nosebleeds in the elderly are generally the result of underlying vascular fragility in combination with blood-thinning medications. Nosebleeds are more common in winter, no doubt reflecting the low, ambient humidity indoors and outdoors and the increased incidence of upper respiratory tract infections. In contrast, posterior bleeding may be asymptomatic or may present insidiously as nausea, hematemesis, anemia, hemoptysis, or melena. Causes of epistaxis are numerous; dry nasal mucosa, nose picking, and vascular fragility are the most common causes, but others include trauma, foreign bodies, blood dyscrasias, nasal or sinus neoplasm or infection, septal deformity or perforation, atrophic rhinitis, hereditary hemorrhagic telangiectasis, and angiofibroma. Epistaxis that results from minor blunt trauma in healthy individuals rarely requires any intervention and will spontaneously subside with head elevation alone and avoidance of any nasal manipulation. Specific antihypertensive therapy is rarely required and should be avoided in the setting of significant hemorrhage. Hereditary hemorrhagic telangiectasia is the most common systemic disorder of the vascular system that affects the nasal mucosa. Blood dyscrasias can be found in patients with lymphoproliferative disorders, immunodeficiency, systemic disease, or in the alcoholic patient. Thrombocytopenia can lead to spontaneous mucous membrane bleeding, with platelet counts of 10,000/mm3 to 20,000/mm3. One study of chronic nosebleeds in children showed that a third of these patients can be expected to have a coagulation disorder. Because of the nasopulmonary reflex, arterial oxygen pressure will drop about 15 mm Hg after the nose is packed, which can be troublesome in a patient with heart or lung disease and often requires hospitalization and supplemental oxygen. At times, the history is not revealed, and the child simply presents with a purulent discharge, pain, bleeding, or hearing loss. An adult might have a pencil eraser or "Q-tip" come off in the ear canal while trying to remove earwax. Most dramatically, a panic-stricken patient arrives complaining of a "bug crawling around" in his ear. There may be severe pain if the object or insect has scratched or stung the canal or tympanic membrane. What To Do: Use an otoscope to inspect the ear canal while pulling up and back on the pinna to help straighten the ear canal, thereby providing a better view. Mineral oil, 2% lidocaine (Xylocaine), or benzocaine/antipyrine (Auralgan) works well. If a hard or spherical object remains tightly wedged in the canal, attempt to roll the foreign body out by getting behind it with a right-angle nerve hook, ear curette, or wire loop. An alternative removal technique is to take a drop or two of cyanoacrylate (Super Glue, Dermabond), and place it on the end of the wooden shaft of a cotton swab. A small magnet or iron-containing metallic foreign body can be removed by touching a pacemaker magnet to a metal forceps and then, at the same time, touching the forceps to the foreign body, withdrawing all of the magnetized objects together. Alligator forceps are good for grasping soft objects, such as cotton, paper, and certain insects.
Syndromes
- Impotence
- Do light circular massage with your fingertips around your lower belly area.
- Not relieved by bed rest
- If you have diabetes, heart disease, or other medical problems, your surgeon will ask you to see your regular doctor.
- S. pneumoniae
- Prolonged, excessive, and unexplained sweating
- Spinal tap in extremely sick children
- Your child has abscess or growth on their tonsils.
Buy shallaki with amex
This occurrence appears to result largely from aberrant rearrangements of the immunoglobulin genes that normally produce antibodies in the malignant plasma cells spasms side of head purchase shallaki line. Biopsy of a solitary osteolytic lesion, masses, skin nodules, or enlarged lymph nodes may be necessary in selected cases. Because myeloma can be a "patchy disease" in the bone marrow, there is marked heterogeneity in different parts of the bone marrow in terms of the percentage of tumor involvement. This will determine if there is spinal cord involvement and can help to determine the extent of myeloma involvement in the spine. Computed tomography scan (avoiding the use of contrast dyes) for evaluation of suspected extradural extraosseous plasmacytoma d. These assessments may identify patients who could benefit from bisphosphonate therapy. Bone formation and resorption markers may predict risk of skeletal complications but should not be performed routinely. Serum viscosity, cryoglobulins, and rectal biopsy or analysis of joint effusions for amyloid are obtained when indicated. Some serum immunoglobulin properties that have clinical relevance are listed in Table 22. Protein electrophoresis is extremely valuable for recognizing cases of monoclonal gammopathies and for following quantitative changes in spikes. M-proteins appear as tall, narrow, sharply defined peaks (spikes) that reflect their structural homogeneity. IgA spikes are usually broader because the molecule tends to form polymers of different sizes; they are located in the region. IgD spikes usually cause only slight deflections in the pattern because the protein is present in a relatively small concentration. Light chains are not ordinarily found in the serum because light chains are rapidly catabolized by the kidney or excreted in the urine. Light chain spikes may be found in the serum of patients with renal insufficiency or in instances in which polymerization of light chains has occurred. This normal ratio is usually maintained when excretion of light chains is owing to renal disease but is significantly altered when the excretion is caused by malignant gammopathies. Benign immunoglobulin G (IgG) gammopathy: normal levels of albumin and gamma globulins plus a peak in the g region. This assay can be important for following patients who have deteriorating renal function (more accurately than 24-hour urine paraprotein levels, which may be unreliable for patients with kidney dysfunction and oliguria) or who have nonsecretory myeloma (a serum light chain may be detected and followed). The usefulness of this assay in following patients long term has not yet been clearly demonstrated, however. Plasma is not used because elevated levels of fibrinogen can markedly affect the results. To establish the diagnosis, serial evaluations of the patient and M-protein level must be done for several months or years. The most important findings that suggest malignant disease are significant and progressive increases in the serum M-protein or urinary light chain concentration. A very small percentage of patients with myeloma present with an IgM monoclonal gammopathy; these patients have typical features of myeloma with osteolytic bone disease, renal dysfunction, or both. Despite the high correlation of 2m levels with renal function, 2m has emerged as an important independent prognostic factor. Elevated 2m levels are also found in patients with acute or chronic myelocytic leukemia, lymphoproliferative disorders, myeloproliferative disorders, myelodysplastic syndromes, benign or malignant liver diseases, and autoimmune diseases. Median survival has dramatically improved among these patients with most patients now living more than 7 years and many living more than 10 years. The development of complications, such as hyperviscosity, hemorrhage, or infection, contributes to death. Age >60 years, male gender, reduced IgM levels, and hemoglobin <10 g/dL are associated with shortened survival time. Its presence is often associated with other poor prognostic chromosomal abnormalities. Chromosome anomalies previously thought to predict a better outcome, such as those involving chromosome 11, are no longer considered to be predictive of improved survival. Increasing degrees of azotemia were associated with progressively shorter life expectancies. Advances in plasmapheresis, dialysis, and supportive care have diminished this prognostic factor. The outcome for patients whose renal function normalizes with initial therapy is not different from that for patients who present with normal renal function. Whether the depth of response to therapy is related to overall survival is controversial. Only patients who show progressive disease during initial therapy definitely have a worse outcome. In general, the extent of response from initial therapy, as long as the patient does not show disease progression, is not a very good prognostic factor. Paradoxically, patients who respond too rapidly to therapy with melphalan and prednisone (>50% reduction in <3 months) have a poor prognosis. However, complete disappearance of the paraprotein predicts an improved survival in some but not all studies. Certainly, long-term maintenance of a complete disappearance of the M-protein is associated with an improved outcome. Bone marrow infiltration by small lymphocytes, plasmacytoid lymphocytes, and plasma cells in a diffuse, interstitial, or nodular pattern c. Although alkylating agents were considered the initial therapy of choice, this is no longer the case. Current treatment options include rituximab, bortezomib, immunomodulatory agents, and purine analogs. Many patients can be started on rituximab alone, or if more serious disease exists, rituximab may be combined with bortezomib and dexamethasone, or cyclophosphamide and fludarabine, or cladribine. In addition, treatment with rituximab may be associated with an initial rise in IgM, the so-called "flare" response, followed by a drop in serum IgM levels and tumor burden. If progressive disease develops >6 months following treatment, the same therapy can be repeated. If progressive disease develops in <6 months, the alternative class of drugs should be tried. These may include other bortezomib/rituximab combinations including anthracyclines or bendamustine. Immunomodulatory agents, including thalidomide or lenalidomide with steroids, may also be tried. Only patients showing significant rises in M-protein levels should have additional diagnostic studies (bone marrow aspirate and biopsy, skeletal survey). It may be useful to obtain periodic bone density studies on these patients because of their higher risk to develop bone loss and fractures. The disease progresses in most patients, but patients may do well for many months or years before progression occurs. The risk is highest (10% per year) during the first 5 years, 3% per year during the next 5 years, and 1% per year after 10 years of follow-up. Significant risk factors for more rapid progression to symptomatic disease include a level of paraprotein >3 g/dL, the IgA subtype, increased numbers of circulating plasma cells, increased ratio of bone marrow abnormal versus normal plasma cells, and bone marrow showing >10% plasma cells. Patients are observed without treatment until the disease progresses to symptomatic or active disease (anemia, hypercalcemia, renal insufficiency, bone lesions) or associated amyloidosis. Several clinical trials are underway attempting to slow the progression of disease with the use of single-agent thalidomide or lenalidomide. Treatment with monthly intravenous bisphosphonates has been shown to reduce the risk of skeletal complications in these patients, but these drugs have not delayed the time to progressive disease; however, these studies involved a relatively short treatment period (1 year) with bisphosphonates. Among patients with severe bone loss demonstrated on bone densitometry, it is certainly reasonable to consider treatment with these antibone resorptive drugs. Notably, the newer agents show higher response rates when combined with glucocorticoids or cytotoxic agents.
Purchase shallaki from india
There may be "allergic shiners"-infraorbital darkening thought to be caused by chronic venous pooling-or an "allergic salute" in children who rub their noses upward because of nasal discomfort spasms quadriceps purchase shallaki amex, sometimes producing a persistent horizontal crease across the nose. Mild bilateral conjunctivitis with nonpurulent discharge is strongly suggestive of an allergic cause when it is accompanied by pruritus. The patient with a "summer cold" lasting a full month is likely to have allergic rhinitis. Common allergens include airborne dust-mite fecal particles, cockroach residues, animal danders (especially cats and dogs), molds, and pollens (hence the origin of the term hay fever). Vasomotor (idiopathic) rhinitis may occur in response to environmental conditions, such as changes in temperature or relative humidity, odors. Repeated use of intranasal cocaine and methamphetamines may also result in rebound congestion and, on occasion, septal erosion and perforation. In viral rhinitis, patients generally complain of an annoying, persistent mucoid nasal discharge accompanied by nasal and facial congestion, along with a constellation of viral symptoms, including low-grade fever, myalgias, and sore throat. These patients generally seek care, because they feel miserable, cannot sleep, and want relief. On physical examination, there is only nasal mucous membrane congestion, which may appear erythematous, along with cloudy nasal secretions, which may become somewhat yellow and thick after several days. Always keep in mind that young children may place intranasal foreign bodies in their noses. Use a hand-held otoscope or headlamp with nasal speculum to view the anterior nasal airway. In particular, patients who are allergic to house dust mites should use allergen-impermeable encasings on the bed and pillows. For patients with seasonal allergies, pollen exposure can be reduced by having them keep windows closed, using an air conditioner, and limiting the amount of time spent outdoors. Intranasal corticosteroids are the most effective medication class for treatment of allergic rhinitis and should be used as a single first-line agent; although, it should be kept in mind that these are generally expensive items. These preparations are generally not associated with significant systemic side effects in adults. Other options include flunisolide (Nasalide) nasal spray, 2 sprays in each nostril bid (may increase to tid to qid), or, for children 6 to 14 years old, 1 spray in each nostril tid or 2 sprays each nostril bid; mometasone furoate (Nasonex) for adults and children older than 12 years of age, 2 sprays in each nostril qd; and budesonide (Rhinocort Aqua) nasal spray for adults and children older than 6 years of age, 1 spray in each nostril qam. Patients should be instructed to direct sprays away from the nasal septum to avoid irritation and not to tilt the head back when spraying, to avoid having the drug run out of the nasal cavity and in to the throat. Antihistamines are a second-line agent in allergic rhinitis treatment but have less effect on nasal congestion. Prescribe a nonsedating second-generation antihistamine, such as fexofenadine (Allegra), 180 mg qd (for children 6 to 11 years old, 30 mg bid); desloratadine (Clarinex), 5 mg qd; loratadine (Claritin), 10 mg qd, or syrup, 10 mg/10 mL (for children 2 to 5 years old, 5 mg qd; for children 6 to 11 years old, 10 mg qd); cetirizine (Zyrtec), 5 to 10 mg qd, or syrup, 5 mg/5 mL (for children 2 to 5 years old, 1/2 to 1 tsp [2 to 2. An alternative to oral antihistamines is the intranasal antihistamine azelastine (Astelin Nasal Spray) for adults and children older than 12 years of age, 2 sprays per nostril bid. They should be used with caution or not at all in patients with arrhythmias, hypertension, or hyperthyroidism. Prescribe pseudoephedrine (Sudafed), 60 mg q6h; time-released version, 120 mg bid, or syrup, 3 mg/mL (for children 2 to 5 years old, 5 to 30 mg q4-6h; for children 6 to 12 years old, 30 mg q4-6h or 4 mg/kg/day divided q6h [1 mg/kg/dose]). Use must be limited to 3 to 5 days to avoid rebound nasal congestion (rhinitis medicamentosa). The same cautions and contraindications exist for nasal decongestants as for the oral medications. Because of the use of pseudoephedrine in the illegal manufacture of amphetamine drugs, it now must be purchased behind the counter. Other products that have some efficacy in allergic rhinitis are cromolyn sodium, a mast cell stabilizer, and montelukast (Singulair), a leukotriene receptor antagonist, for adults, 10 mg qhs (for children 2 to 5 years old, 4 mg chewable tab qhs; for children 6 to 14 years old, 5 mg chewable tab qhs). Viral Rhinitis Determine which specific symptoms are most bothersome to the patient. Perform a general examination, including a careful nasal examination, to exclude any associated diseases, such as rhinosinusitis, otitis media, bacterial pharyngitis, and asthmatic bronchitis. For nasal congestion, prescribe oral or topical decongestants, as you would for allergic rhinitis (described earlier). Although antihistamines are effective for treatment of rhinitis related to allergy, they are much less effective for rhinitis related to the common cold. Nasal saline irrigation has been shown to have some efficacy in the relief of viral rhinitis. Warm facial compresses, steam inhalation, warm tea, and chicken soup are all comforting, and chicken soup may possibly be therapeutic. Patients with diabetes, immune deficiency, or progressive infection should be placed on a systemic antistaphylococcal antibiotic to avoid potential spread to the cavernous sinus. What Not To Do: Do not prescribe sedating antihistamines for symptoms of hay fever. Do not obtain imaging studies of the sinuses unless the criteria for bacterial rhinosinusitis are met (symptoms lasting more than 7 days and including facial or dental pain or tenderness along with purulent nasal drainage). Antibiotics should only be considered if symptoms persist for more than 7 days and are accompanied by signs of rhinosinusitis (see Chapter 40). Despite numerous randomized trials, the evidence for their effectiveness in reducing the duration of common cold symptoms is still lacking. Within minutes of allergen exposure, immune cells release histamine, proteases, cysteinyl leukotrienes, prostaglandins, and cytokines. Systemic circulation of inflammatory cells permits their infiltration in to other tissues where chemoattractant and adhesion molecules already exist. Consequently, allergic rhinitis is linked to comorbid conditions: asthma, chronic hyperplastic eosinophilic sinusitis, nasal polyposis, and serous otitis media. Effective therapy should ideally be directed at the underlying inflammation and its systemic manifestations. Antihistamines relieve early symptoms, but they do not significantly influence the proinflammatory loop. Oral corticosteroids provide the systemic anti-inflammatory effect needed, but their toxicity precludes extended routine use. Intranasal corticosteroids effectively target the local inflammatory processes of rhinitis, but they only reduce the local inflammatory cells within the nares. Leukotriene modifiers have both systemic anti-inflammatory effects and an acceptable safety profile. Immunotherapy (allergy shots) is the only treatment that produces long-term relief of symptoms. Patients should be considered candidates for these treatments, based on the severity of their symptoms and the failure or unacceptability of the other treatment modalities. Nasal polyps are benign inflammatory growths that arise from the inflamed mucosa lining the paranasal sinuses. Stuffy ears and impaired hearing are common because of associated otitis media with effusion and eustachian tube dysfunction. Fever is present in only half of all patients with acute infection and is usually low grade. A high fever and severe headache usually indicate a serious complication, such as meningitis or another diagnosis altogether. Transillumination of sinuses in the acute care setting is usually unrewarding, but tenderness may be elicited on gentle percussion or firm palpation over the maxillary or frontal sinuses or between the eyes (ethmoid sinuses). Pus may be visible draining below the nasal turbinates (most often in the middle meatus) with a purulent yellow-green or chronic infection, sometimes with a foul-smelling discharge from the nose or running down the posterior pharynx. Shrink swollen nasal mucosa (and thereby provide symptomatic relief of nasal obstruction) with 1% phenylephrine (Neo-Synephrine) or 0. Instill 2 drops in each nostril, allow the patient to lie supine for 2 minutes, and then repeat the process. Examine the nose for purulent drainage before and, when practical, after shrinking the nasal mucosa with a topical vasoconstrictor. Unless contraindicated by age, hypertension, benign prostatic hypertrophy, or underlying cardiac disease, prescribe systemic sympathomimetic decongestants such as pseudoephedrine (Sudafed), 60 mg q6h.
Cheap shallaki online american express
Life-threatening complications include renal failure from precipitation of uric acid or calcium phosphate crystals in the kidney spasms with stretching generic shallaki 60 caps line, seizures from hypocalcemia, and cardiac arrhythmias from hyperkalemia or hypocalcemia. Cardiac arrhythmias or cardiopulmonary arrest develop if the process is not controlled. Patients treated for acute leukemia or Burkitt lymphoma should have measurements of serum levels of potassium, calcium, phosphate, uric acid, and creatinine performed daily for 1 week and every few hours if the syndrome develops. Hemodialysis may be necessary on an emergency basis for patients who do not respond to treatment or who develop renal insufficiency. Tumor lysis syndrome and acute kidney injury: evaluation, prevention and management. Bisphosphonate-related osteonecrosis of the jaw: diagnosis, prevention and management. Emergency management and commonly encountered outpatient scenarios in patients with hyperkalemia. In men, the most common internal malignancies leading to cutaneous metastases are lung cancer (24%), colon cancer (19%), melanoma (13%), squamous cell carcinoma of the oral cavity (12%), and renal cell carcinoma (6%). In women, these are breast cancer (69%), colon cancer (9%), melanoma (5%), lung cancer (4%), and ovarian cancer (4%). Cutaneous involvement by cancer can occur both as a metastatic process and as a direct extension of the tumor to the skin. Metastases to the skin may be delayed 10 to 15 years after the initial surgical treatment of primary melanoma, breast carcinoma, and renal cancer or may be the first indication of an internal malignancy. Inflammatory (erysipelas-resembling erythematous patch or plaque with active border, usually affecting the breast; but other skin sites can also be involved) b. Telangiectatic (papules with violaceous hue caused by accumulation of blood in vascular channels) d. Alopecia neoplastica (painless, well-demarcated, pinkish oval plaques of alopecia caused by hematogenous spread of breast carcinoma), which can occur with other neoplasms as well f. Paget disease (a sharply demarcated, scaling plaque on the nipple or areola representing cutaneous infiltration of cancer) g. Breast carcinoma of the inframammary crease (a cutaneous nodule that may resemble basal cell carcinoma) h. Histiocytoid nodule of the eyelid (presents as a painless eyelid swelling with induration) 2. Cutaneous metastases from lung cancer may appear on any surface, but they are most common on the chest wall and the posterior abdomen; small cell lung cancer metastasizes most frequently to the skin of the back. Lung cancer also has a rare but peculiar tendency to metastasize to the anal area, fingertips, or toes. Skin metastases from colon cancer and rectal cancer usually develop after malignancy has been recognized. They may appear as sessile or pedunculated nodules, vascular nodules, scalp cysts, inflammatory carcinoma, or persistent fistulation after appendectomy. Cutaneous metastasis of gastric cancer is rare, and most cutaneous metastases are typically solitary, nodular, have a firm consistency, and are red or hyperpigmented but 684 I. Anal cancer metastases to skin involve unusual sites, such as the scalp, eyelid, nose, or legs. They usually present as multiple pigmented nodules, but they can also be erythematous or apigmented. Of all urologic malignancies, renal cell carcinoma metastasizes to the skin most frequently, but skin metastases from bladder, prostate, and testicular cancer have also been reported. These metastases are frequently the first sign of renal cell carcinoma, and they can appear very late, up to 10 years after diagnosis. Both clinically and histologically, they may resemble common dermatologic disorders, which lead occasionally to incorrect diagnosis. Malignant lesions in the nail unit can be classified in to three groups: metastatic lesions from a distant primary, cutaneous involvement of a hematopoietic or lymphoproliferative malignancy, and primary cancer at this location. Lung cancer is the most common type of malignancy that can metastasize to the nail bed, followed by genitourinary, breast, head and neck cancers, and sarcomas. Subungual metastases typically present as erythematous enlargement, swelling of the distal digit, or a violaceous nodule. They are frequently painful, but they can also bleed or be hot, pulsatile, and fluctuant. These lesions can be mistaken for infection or trauma; in almost half of affected persons, they are a presenting sign of malignancy. Umbilical metastasis (Sister Mary Joseph nodule) is encountered in 1% to 3% of patients with abdominopelvic malignancy. Survival in these patients, which depends on the type of tumor and treatment modalities, can range from 2 to 18 months. The average survival time from the recognition of skin metastases is 3 months, but it can be years for lymphomas, melanoma, and breast cancer. Diagnosis is based on biopsy results, especially in patients who have not previously been diagnosed with malignancy. Most skin metastases are treated symptomatically, and they tend to regress when the primary tumor responds to systemic therapy. Occasionally, these lesions require treatment with local radiation therapy, surgery, cryotherapy, or photodynamic therapy. Intralesional injections of thiotepa (30 mg), bleomycin, or cisplatin, or electrochemotherapy (in which the effect of intralesional chemotherapy is enhanced by electroporation) have also been utilized. Acanthosis nigricans is characterized by hyperpigmented, velvety plaques on the neck, in the axilla, groin, and antecubital fossa. In most cases, it reflects metabolic disturbances seen in patients with obesity, metabolic syndrome, or diabetes. Inherited abnormality in humans (and Swedish dachshunds) Amyloidosis secondary to nonmalignant disease rarely involves skin. The lesions are primarily in flexural areas, paranasal skin, anogenital regions, the neck, and around the eyes. Bazex syndrome (acrokeratosis paraneoplastica) consists of psoriasiform lesions in the acral areas (ears, nose, nails, hands, feet, elbows, knees). This syndrome is universally associated with malignancy, mainly carcinoma of the upper aerodigestive tract, but also prostate carcinoma, hepatocellular carcinoma, lymphoma, and bladder carcinoma. In nearly two-thirds of cases, cutaneous lesions precede the diagnosis of malignancy. Dermatomyositis and polymyositis belong to a group of idiopathic inflammatory myopathies. Between 15% and 25% of cases of dermatomyositis and about 10% of polymyositis are associated with malignancy. Almost any type of malignancy has been reported in patients with dermatomyositis, but ovarian carcinoma and lung and breast cancer are the most common. Treatment of the malignancy results in symptom improvement, and worsening of symptoms may herald tumor recurrence. These myopathies are typified by proximal muscle weakness with or without tenderness. Flat-topped erythematous papules over the phalangeal joints (Gottron papules) and pinkish-purple discoloration around the eyes (a heliotrope rash) are pathognomic signs of dermatomyositis. Other signs include periungual telangiectasias; patchy discoloration of the skin; red, scaly scalp rash; and photosensitivity. Laboratory work commonly reveals elevated creatinine kinase level, although the cases with normal level of creatinine kinase have been reported, and possibly they are more frequently associated with malignancy. It is almost always a representation of underlying malignancy, and it precedes the detection of malignancy by 1 to 24 months. The treatment consists of surgical removal of the primary tumor, but some improvement can sometimes be observed after therapy with systemic steroids, radiotherapy, and azathioprine. Exfoliative erythroderma syndrome is a generalized erythema of the skin accompanied by a variable degree of scaling. Malignancy accounts for 5% to 12% of cases, and it is most frequently associated with cutaneous T-cell lymphoma, rarely with solid tumors or acute myelogenous leukemia. Hypertrichosis lanuginosa acquisita ("malignant down") refers to the development of fine, unpigmented hair predominantly localized to the head and neck.
Quality 60 caps shallaki
If irradiation above the diaphragm was administered muscle relaxant 503 cheap shallaki 60 caps fast delivery, women should be encouraged to start annual mammograms 5 to 8 years after treatment, or earlier if 40 years of age (whichever comes first). Although alternate combinations may be temporarily useful, long-term disease control is unlikely. The decision depends on the age of the patient, the availability of a donor, bone marrow status, and responsiveness to a salvage chemotherapy regimen. No known available regimen is capable of producing long-term disease-free survival in >10% to 20% of chemotherapy relapsed cases. Singleagent therapy with a nitrosourea, vinca alkaloid, etoposide (possibly the oral form), or combinations of these and other agents may be helpful. Gemcitabine is an active agent, particularly in combination with vinorelbine or platinum. Other second-line and third-line combination chemotherapy regimens are also shown in Appendix D3. Chemotherapy failures with predominantly nodal relapses may benefit from extended-field irradiation, which results in some long-term disease-free survival. Experimental trials would also be appropriate to consider for the treatment of this patient population. High doses of chemotherapy (potentially myeloablative), often combined with total-body irradiation, are administered ("conditioning regimen"), and either autologous bone marrow or peripheral stem cells (mobilized by growth factors) are used to rescue the patient from prolonged myelosuppression. This procedure is performed in most centers with a mortality rate of <5%; the hospital stay averages 3 weeks. About 60% of chemosensitive candidates and 40% of patients failing induction chemotherapy achieve prolonged disease-free survival. Mantle-field irradiation routinely produces a paramediastinal fibrosis that is usually not clinically significant. Therefore, prednisone is avoided after mantle-field irradiation, even if the radiation was administered years earlier. Severe idiopathic pulmonary toxicity is occasionally seen at bleomycin doses of >50 mg, although it usually does not occur until cumulative doses exceed 200 mg/m2. These adverse effects depend partly on the total dose of bleomycin and the radiation field. The risk for radiation pericarditis is relatively small when modern anteroposterior weighted radiation ports are used and when large portions of the heart are not radiated. Radiation pericarditis with or without pericardial effusion or tamponade can develop, however. The incidence of cardiotoxicity is related to the cumulative dose and probably to peak serum levels. Infections associated with depressed cell-mediated immunity and therapy (particularly corticosteroids) include Listeria, Toxoplasma, and Mycobacterium spp. Herpes zoster appears in >25% of patients, particularly in patients with irradiated dermatomes and in those undergoing splenectomy. Generalized cutaneous involvement is not uncommon, but visceral involvement is rare. Splenectomy-related infections involve encapsulated micro-organisms, particularly pneumococci, and less commonly Haemophilus influenzae and Salmonella sp. Vaccination with polyvalent pneumococcal vaccine, haemophilus, and meningococcus is recommended before splenectomy, although its effectiveness in this population is not certain. Early, aggressive treatment with antibiotics of all febrile patients after splenectomy is mandatory. The problem appears to be greatest in patients older than 40 years of age and may be increased in patients undergoing splenectomy. The leukemia generally occurs between 3 and 10 years after treatment, is often associated with total or partial deletion of chromosomes 5 and 7, and has an extremely poor prognosis. Tumors may include breast cancer, sarcoma, melanoma, lung cancer, and other solid tumors. The relative risk for cancer appears to be higher for younger patients and synergistic to other predisposing factors. This significant risk applies to a patient population treated in the 1960s and 1970s; modern strategies limiting radiation exposure may reduce this risk. It consists of shock-like sensations down the back and legs, often precipitated by flexing the neck, and it gradually disappears. Viral etiology and abnormal immune regulation have been implicated in the development of lymphomas. Chronic hepatitis C virus infection has been associated with indolent B-cell lymphoma. Eradication of the infection produces remission in more than two-thirds of patients. Immunodeficiency or immune dysregulation states associated with development of lymphomas include the following: a. Exposure to toxins such as Agent Orange utilized during the Vietnam War is associated with increased lymphoma risk. Approximately 10% of patients with small lymphocytic lymphoma/chronic lymphocytic leukemia will have more than one family member with that or other lymphoproliferative disorders. This scheme was developed in 1982 as the result of a consensus panel made up of distinguished hematopathologists, each previously espousing his or her own classification. However, it does not incorporate accepted information regarding B-cell or T-cell origin of lymphomas and does not recognize a large variety of newly described clinicopathologic entities. It incorporates immunophenotypic characteristics to determine cell lineage and to define subtypes by a more scientific method. Each of the three major prognostic categories (grades) is significantly different from the other (p < 0. National Cancer Institute sponsored study of classifications of non-Hodgkin lymphomas. Cancer 1982;49:2112, with permission) 6 8 10 Intermediate grade (D, E, F, G) High grade (H, I, J) Low grade (A, B, C) be the current classification standard. Leukemias are considered to be an extreme of the spectrum of certain lymphoproliferative disorders. All follicular lymphomas constitute one group with grade designation (grades 1 to 3). Immunoblastic lymphoma is classified as diffuse large cell lymphoma and is no longer recognized as a separate entity. Monoclonal antibodies can identify epitopes on lymphoid cells characteristic of developmental stages of B-cell and T-cell ontogeny. The antibodies are used with flow cytometry in cell suspensions and with indirect immunoperoxidase Non-Hodgkin Lymphoma 531 labeling in frozen sections. Monoclonality of B-cell lymphomas is usually established by showing marked dominance of a single light chain (or) type. Each clone rearranges its genes in a unique way that can be differentiated from the germ line pattern by Southern blot techniques. Identification of gene rearrangements for immunoglobulin and T-cell receptor loci can establish cellular lineage, monoclonality, and sometimes stage of differentiation for lymphoid neoplasms. The application of the polymerase chain reaction method may enable detection of down to one clonal cell in one million using amplification of breakpoint regions by specific primers. The genetic material found at or near the breakpoint of each translocated chromosome is frequently highly informative and provides clues regarding pathogenesis. Such cytogenetic abnormalities can be demonstrated with the use of florescence in situ hybridization techniques to analyze specific genetic abnormalities that a tumor may possess. Production of lymphokines by tumor cells may be related to the symptoms or manifestations of specific lymphomas. The pattern of surface antigens (Appendix C5) found on lymphoma cells when flow cytometry or immunohistochemical staining is used may help identify or corroborate certain lymphoma types.
Generic shallaki 60 caps amex
The main role of bronchoscopy is to exclude infection muscle relaxant 25mg order 60caps shallaki with visa, recurrent malignancy, and diffuse alveolar hemorrhage. Histology reveals diffuse alveolar damage, intra-alveolar mononuclear inflammation, acute and organizing interstitial pneumonia with hyaline membranes, atypical epithelial desquamation, and nodular inflammation or fibrosis. Hypersensitivity reactions demonstrate eosinophilic pneumonitis with focal consolidation. Busulfan lung toxicity may result in atypical, malignant-appearing cells on sputum cytology. Management includes careful patient selection before administering potentially pulmonary toxic drugs or using drugs that potentiate the effect of radiation. Glucocorticoids, such as prednisone, are advocated to minimize lung injury in the symptomatic patient who does not improve with drug withdrawal. Reinitiation of offending drugs is possible and tricky, although this maneuver has been successful at times. The critical need for a specific drug for a specific malignancy weighs heavily in this important decision. However, reinitiation is generally not recommended and is contraindicated in patients with pulmonary fibrosis. Gemcitabine is included in many lung cancer treatment protocols and is a potent radiation sensitizer; when given as concurrent therapy, pulmonary toxicity is prohibitive, even with reduced doses. The frequency of radiation-induced pneumonia appears to be increased by concurrent endocrine therapy for breast cancer. Patients typically develop symptoms such as cough and dyspnea, and also radiographic opacities that usually conform to the prior radiation field. Pneumonitis is proportionately more frequent with increasing radiation doses and portal sizes. The patient usually does not have symptoms, although a dry cough, dyspnea, fever, and leukocytosis may be present. Symptoms caused by subacute radiation pneumonitis usually develop approximately 4 to 12 weeks following irradiation and usually subside within 2 weeks. Pulmonary function testing generally demonstrates a reduction in lung volumes, diffusing capacity, and lung compliance. Glucocorticoids are useful in relief of symptoms of pneumonitis caused by drugs and radiation. The usual dose is at least 60 mg of prednisone per day for 2 to 3 weeks with a slow taper for 3 to 12 weeks. Other Pulmonary Complications 711 Immunosuppressive agents may be considered if glucocorticoids fail. Pentoxifylline, a xanthine derivative that inhibits platelet aggregation, enhances microvascular blood flow, and has immunomodulating and anti-inflammatory properties, may have a role for the treatment of radiation-induced fibrosis in the future. Patients may develop restrictive lung disease, alveolar-capillary block, or cor pulmonale. Corticosteroids have a doubtful role in preventing or treating progression of fibrosis. Pulmonary tumor thrombotic microangiopathy with pulmonary hypertension is characterized by fibrocellular intimal proliferation of small pulmonary arteries and arterioles in patients with metastatic carcinoma, particularly adenocarcinoma. This condition develops when microscopic tumor cell embolism induces both local activation of coagulation and fibrocellular proliferation of intima but does not occlude the affected vessels. This complication should be considered in the differential diagnosis in patients with known carcinoma who develop acute or subacute cor pulmonale. In an autopsy series of nearly 2,000 patients, 8% had metastatic disease involving the heart. Cardiac involvement may arise from hematogenous metastases, direct invasion from the mediastinum, or tumor growth in to the vena cava and extension in to the right atrium. The epicardium is involved in 75% of metastatic lesions, and pericardial effusions are associated with 35% of epicardial metastases. Carcinomas of the lung and breast constitute about 75% of all cases of malignant pericardial effusion. Melanoma, leukemia, lymphoma, soft tissue sarcomas, renal carcinoma, esophageal carcinoma, hepatocellular carcinoma, and thyroid cancer also commonly affect the heart. Pericardial effusion, which is usually insignificant, occurs in 20% of patients with non-Hodgkin lymphoma at the time of presentation. Most myocardial and pericardial metastases are clinically silent; about twothirds are not diagnosed antemortem. Pericardial metastases produce symptoms by causing pericardial effusion with tamponade, constrictive pericarditis, or arrhythmias. Myocardial metastases produce symptoms by causing conduction blocks and arrhythmias. Metastases infrequently cause myocardial rupture, valvular disease, or emboli to other organs. Clinical manifestations arise from decreased cardiac output and venous congestion. Frequently, pericardial tamponade develops slowly, and symptoms resemble those of congestive heart failure. Distant heart sounds with decreased cardiac impulse; possible pericardial friction rub d. Chest radiographs may show enlargement of the cardiac silhouette or a "water bottle" configuration. The findings on echocardiogram of right atrial and ventricular collapse in diastole strongly suggest tamponade. A small catheter should be introduced through the needle in to the pericardial sac and attached to water seal gravity drainage to prevent the recurrence of effusion until the final diagnosis is made. Conservative treatment of malignant pericardial effusion using pericardiocentesis or short-term catheter drainage as needed (with or without instillation of intrapericardial chemotherapeutic drugs) may be effective treatment for some patients. Serious complications of pericardial aspiration through a left parasternal or xiphosternal approach are rare, but they include laceration of the heart or coronary arteries, other vessels, liver, or stomach and (very rarely) a dramatic shock-like reaction. Emergency subxiphoid pericardial decompression under local anesthesia, however, is reported to be associated with no operative mortality. The drainage catheter can be left in place for several days if necessary without increased risk of infection. Overall response rates are reported to be 60% with a dose of 3,500 cGy given over 3 to 4 weeks. Chemotherapeutic drugs or doxycycline may be instilled intrapericardially to induce pericardial sclerosis and obliterate the pericardial space. Pericardial sclerosis results in decreased pericardial fluid reaccumulation in 50% to 75% of patients. The dose and method of administration of intrapericardial drugs are similar to those for malignant pleural effusion (Table 29. Pericardial and Myocardial Metastases 713 and an intravenous line in place in case arrhythmia develops. The development of constrictive pericarditis and refractory heart failure has been reported. There have been no trials comparing pericardial drug instillation to the creation of a pericardial window. The length of hospital stay for any surgical procedure represents a major portion of the life expectancy of these patients. Surgery should be reserved for patients with (1) rapidly accumulating pericardial effusions that cannot be controlled conservatively, (2) radiation-induced constrictive pericarditis, and (3) a life expectancy of 6 months or more. Subtotal pericardiectomy (resection of entire pericardium anterior to the phrenic nerves) is the surgical procedure of choice in patients whose expected survival is reasonably long. Subtotal pericardiectomy is superior to the pericardiopleural window, which may seal off shortly after surgery. Alternative surgical interventions for pericardial tamponade (1) Percutaneous balloon pericardiotomy proved successful in relieving the cardiac tamponade in >90% of cases with few complications. Patients with disseminated malignancy and new, unexplained cardiac arrhythmias that are refractory to treatment should be considered for cardiac irradiation, particularly if there is known mediastinal or pericardial involvement. Nonbacterial thrombotic ("marantic") endocarditis is most common in patients with mucinous adenocarcinoma of the lung, stomach, or ovary, but it can complicate any systemic cancer. Heart murmurs and other stigmata of bacterial endocarditis usually are not present. Endocarditis is manifested by embolic peripheral or cerebral vascular occlusions that may become clinically apparent as acute peripheral arterial insufficiency, progressive encephalopathy, acute focal neurologic defects suggesting a stroke, or acute multifocal neurologic disease.