Buy topiramate online
The role of the liver in intestinal transplant was first suggested by a group at the University of Pittsburgh who reported that patients receiving liverinclusive intestinal transplants had a lower risk for graft loss from rejection symptoms emphysema purchase topiramate canada. However, when antibodies are reduced following either treatment, kidney transplants may be performed across a positive crossmatch without hyperacute rejection. More recently, bortezomib, a 26S proteasome inhibitor that has proapoptotic effects on plasma cells has been shown to decrease antibody production in sensitized patients. With supporting data, logistic considerations would have limited interest in sharing livers for more histocompatible recipients. At that time the low tolerance for prolonged ischemia was considered a major barrier to sharing livers over a wide geographical area. Most cases have been confirmed by demonstrating a high proportion of donor lymphocytes in the circulation. Engraftment tests using short tandem repeats when donor material is available can distinguish and quantify donor cells in the recipient circulation. Such clear cases are extremely rare when a genetically unrelated individual is the donor. This complexity may be related to the older senescent recipient immune system being more easily suppressed than the younger, more vigorous immune system of the donor. A recent study111 of 321 living donor transplants showed the failure rate was significantly lower (3. The differences were not apparent among recipients with other diseases or recipients of deceased donor grafts. Whether this interpretation is correct remains to be demonstrated, but the observation is interesting and may be a consideration in donor selection. This is a complex area, and the levels of involvement are not yet well understood. The authors suggest that group 2 homozygous allografts may be better allocated to high-risk recipients. There are indications that with smaller-size grafts from splitting or from living donors, the actions of antibodies may play an even larger role in the outcome. The risks are higher when the donor is much younger than the recipient and when the donor is a first-degree relative. Although the symptoms often mimic drug reactions or viral infection, early skin or bowel disturbances, especially with good liver function, should prompt investigation of lesions and tests for high levels of donor cells in the circulation. Study on transplantation immunity after total body irradiation: clinical and experimental investigation. Renal homografts in patients with major donor-recipient blood group incompatibilities. Hyperacute rejection of kidney allografts, associated with pre-existing humoral antibodies against donor cells. Impact of preservation-induced liver injury on the risk of rejection of rat and human liver grafts. Older donor livers show early severe histological activity, fibrosis, and graft failure after liver transplantation for hepatitis C. Anti-A of donor lymphocyte origin in three recipients of organs from the same donor. Lymphocytotoxic antibody responses to transfusions in potential kidney transplant recipients. High one-month liver graft failure rates in flow cytometry crossmatch-positive recipients. Increased bile duct complications and/or chronic rejection in crossmatch positive human liver allografts. Susceptibility of liver allografts to high or low concentrations of preformed antibodies as measured by flow cytometry. Preformed antibodies detected by cytotoxic assay or multibead array decrease liver allograft survival: role of human leukocyte antigen compatibility. Does a positive lymphocyte cross-match contraindicate living-donor liver transplantation? Serum haemolytic classical and alternative pathways of complement in infancy: agerelated changes. Positive pretransplant crossmatches predict early graft loss in liver allograft recipients. Apheresis therapy for livingdonor liver transplantation: experience for apheresis use for living-donor liver transplantation at Kyoto University. Graft versus host disease after liver transplantation - a single center experience and review of literature. Protective effect of highmobility group box 1 blockade on acute liver failure in rats. The benefits of interferon treatment in patients without sustained viral response after living donor liver transplantation for hepatitis C. Transplant accommodation in highly sensitized patients: a potential role for Bcl-xL and alloantibody. C4d in acute rejection after liver transplantationa valuable tool in differential diagnosis to hepatitis C recurrence. Clinical implications of flow cytometry crossmatch with T or B cells in living donor liver transplantation. Liver recipients harbouring anti-donor preformed lymphocytotoxic antibodies exhibit a poor allograft survival at the first year after transplantation: experience of one centre. Pretransplant predictors of survival after intestinal transplantation: analysis of a singlecenter experience of more than 100 transplants. Plasmapheresis and intravenous immune globulin provides effective rescue therapy for refractory humoral rejection and allows kidneys to be successfully transplanted into cross-match-positive recipients. The use of antibody to complement protein C5 for salvage treatment of severe antibodymediated rejection. Terminal complement inhibition decreases antibody-mediated rejection in sensitized renal transplant recipients. The use of a reversible proteasome inhibitor in a model of Reduced-Size Orthotopic Liver transplantation in rats. Proteasome inhibition with bortezomib: an effective therapy for severe antibody mediated rejection after renal transplantation. Long-term outcome of human leukocyte antigen mismatching in liver transplantation: results of the National Institute of Diabetes and Digestive and Kidney Diseases Liver Transplantation Database. A large, single center investigation of the immunogenetic factors affecting liver transplantation. Human leukocyte antigen and adult living-donor liver transplantation outcomes: an analysis of the organ procurement and transplantation network database. Graft-versus-host disease after liver transplantation: documentation by fluorescent in situ hybridisation and human leucocyte antigen typing. Acute graft-versus-host disease after living donor liver transplantation with donor-dominant one-way human leukocyte antigen matching at two Loci. Recipients who receive a human leukocyte antigen-B compatible cadaveric liver allograft are at high risk of developing acute graft-versus-host disease. Unsuccessful treatment of four patients with acute graft-vs-host disease after liver transplantation. Acute graftversus-host disease after liver transplantation: role of withdrawal of immunosuppression in therapeutic management. Infliximab treatment for steroid-refractory acute graft-versus-host disease after orthotopic liver transplantation: a case report. Acute graft-versus-host disease after liver transplant: novel use of etanercept and the role of tumor necrosis factor alpha inhibitors. Decreased risk of graft failure with maternal liver transplantation in patients with biliary atresia. Antibody-mediated rejection of renal allograft in combined liver-kidney transplant. Rapid method for the analysis of peripheral chimerism in suspected graft-versus-host disease after liver transplantation. Impact of family history of diabetes on beta-cell function and insulin resistance among Chinese with normal glucose tolerance. An essential role for natural killer cells in augmentation of allograft survival mediated by donor spleen cells.
Generic topiramate 100mg line
Though Lyme disease cases have been reported in nearly every state, cases are reported based on the county of residence, not necessarily the county of infection new medicine effective topiramate 200mg. Although pets may represent a spirochete reservoir, it is unlikely that humans can be infected directly by them. Lyme borreliosis is a multisystem illness that primarily involves the skin, nervous system, heart, and joints (Table 19-2). Arthritis in patients with chronic Lyme disease may be associated with a long-standing infiltration of the joints by B. It may not be triggered simply by the presence of circulatingimmunoglobulinG(IgG)antibodiesagainstouter surfaceproteins. Arareearly manifestation of Lyme disease is Borrelia lymphocytoma, a violaceous, tumor-like swelling or nodule at the base of the earlobe or nipple caused by a dense lymphocytic infiltrate of thedermis. The carditis usually follows a self- limitedandmildcourse,buttemporarypacingmaybeneeded inasmallpercentageofpatients. NeurologicManifestations Neurologic abnormalities occur in approximately 15% of untreated patients. Mononuclearcell,antigenspecific responses develop during spirochetal dissemination andhumoral(antibody)immuneresponsessoonfollow. IntheUnitedStates,approximately20%to 30% of Lyme patients have positive responses, usually of the IgM isotype, during this period, but by convalescence 2 to 4 weeks later, about 70% to 80% have seroreactivity even after antibiotictreatment. Themostseriousdisadvantages of current techniques are low sensitivity and lengthy processingtime. Inaddition,false-positivereactionscanresult from cross-reactivity in tests for Lyme disease. For example, tick-borne relapsing fever spirochetes, Borrelia hermsii, are closely related to B. Common antigens are shared among the Borrelia organisms and even with the treponemes. The18-,23- to25-(OspC),31-(OspA),34-(OspB),37-,39-,83-,and 93-kDa bands are the most specific, but may appear later or notappearatall. Lane 2,Humanserum(IgG)reactive with the 10 antigens scored in recommended criteria for blot scoring; lines indicate other calibrating antibodies. Becauseofitsshorthalf-lifeandneedforhighlevels, amoxicillin is usually administered along with probenecid. Ehrlichia chaffeensis,theetiologic agent of human monocytic ehrlichiosis in the United States, was demonstrated to cause disease in a patient from Arkansaswithtickbitesin1987. Epidemiology Although the prevalence rates are low, human ehrlichiosis is endemic in the United States. DiagnosticEvaluation Laboratory studies have indicated that the hematologic, hepatic, and central nervous systems are usually involved in humanehrlichiosis. IntheUnitedStates,theseinclude theAmericandogtick(Dermacentor variabilis),RockyMountain wood tick (Dermacentor andersoni), and brown dog tick (Rhipicephalus sanguineus). Symptomscanincludefever,rash(occurs2to5daysafter fever; may be absent in some cases), headache, nausea, and vomiting. Also, IgM antibodies are less specific than IgG antibodies and more likelytoyieldafalse-positiveresult. Forthesereasons,physicians requesting IgM serologic titers should also request a concurrentIgGtiter. Becoming nationally notifiable is an important step toward monitoringdiseaseoccurrence. Babesiosis is seen most frequently in older individuals, splenectomizedpatients,orimmunocompromisedpatients. The gold standard for their identification is the visualization of the intraerythrocytic organisms in thick or thinbloodfilms. TreatmentandPrevention Standardized treatments for babesiosis have not been developed. Antimicrobial therapy is recommended for splenectomized or immunodeficient patients, older patients, and patientswithsevereinfections. Exchange transfusion has been effective for patients with a high level of parasites (>10%), severe disease, or massive hemolysis. Fecal contamination of food or water, soiled hands, inadequately cooked or infected meat, and raw milk can be major sources of human infection. The risk for infection is higher in many developing and tropical countries, especially whenpeopleeatundercookedmeat,drinkuntreatedwater,or areextensivelyexposedtosoil. Evidence has shown that the number of infants born in the United States each year with congenital T. Itisestimatedthat6of1000pregnantwomeninthe United States will acquire primary infection with Toxoplasma during a 9-month gestation. Prevention of infection in pregnant women should be practiced to avertcongenitaltoxoplasmosis(Box20-1). Although spontaneous recovery follows acute febrile disease, the organism can localize and multiply in any organ of the bodyorthecirculatorysystem. Box 20-1 Methods for Prevention of Congenital Toxoplasmosis Avoid touching mucous membranes of the mouth and eye while handling raw meat. Avoid contact with or wear gloves when handling materials that are potentially contaminated with cat feces. IgMantibodies tend to appear earlier and decline more rapidly than IgG antibodies. IgMantibodieshave been reported to persist as long as 12 years after the acute infection. IgG antibodies usually appear within 1 to 2 weeks of the infection,peakwithin1to2months,fallatvariablerates,and usually persist for life. The avidity result is determined using the ratios of antibody titrationcurvesofurea-treatedanduntreatedserum. Histologic Diagnosis Demonstration of tachyzoites in tissue sections or smears of body fluid. In cases of current Toxoplasmosis infection, the earliest that Toxoplasma antibodies can be detected is after infection. This test is a qualitative screening procedure and cannot be used to detect increases in antibody titer or to diagnose active infection. The virus has been isolated in urine, saliva, feces, breast milk, blood, cervical secretions, virus-infected grafts fromadonor,semen,vaginalfluid,andrespiratorydroplets. Anoperational definition of latency can include the conditions of a dynamic relationship between the virus and host, along with evidence of latency and reactivation of a latent infection. Infection interferes with immune responsiveness in normal and immunocompromised individuals. Although nasopharyngeal carcinoma is rare in North American and European whites, it is one of the most common cancers in southern China and parts of Southeast Asia. Blood transfusion from an immune donor to a nonimmune recipient may produce a primary infection in the recipient known as infectious mononucleosis postperfusion syndrome. Clinically apparent infectious mononucleosis has an estimatedfrequencyof45/100,000inadolescents. Inchildren younger than 5 years, infection is asymptomatic or frequently characterized by mild, poorly defined signs and symptoms. Asmallerpercentage of patients develop hepatomegaly or splenomegaly and hepatomegaly. Thepediatricpopulation is of particular concern because more than 50% of children younger than 4 years with infectious mononucleosis are heterophilenegative. Paul-Bunnell Screening Test Principle the classic Paul-Bunnell test is a hemagglutination test designed to detect heterophile antibodies in patient serum when mixed with antigen-bearing sheep erythrocytes. Exposure of patient serum to guinea pig cells, which are rich in Forssmanantigen,andtobeeferythrocytes,whicharepoorin Forssman antigen, produces differential absorption. Reporting Results: Qualitative Method Positive A positive infectious mononucleosis reaction will have dark clumpsagainstablue-greenbackground,distributeduniformly throughoutthetestcircle. Negative A negative reaction will have no agglutination but may have fine granularity against a brown-tan background. Reporting Results If the pattern of reactivity demonstrates reduced titers with either beef or guinea pig cells, the antibody source can be attributed to one of the heterophile antibody types. Detectable levels of heterophile antibody may persist formonthsand,morerarely,foryears,insomeindividuals. Safe and effective vaccines have been available for hepatitis B since 1981 and for hepatitisAsince1995.
Buy 200mg topiramate with visa
Approximately 100 distinct substances have been identified as being secretedbymonocytes-macrophages medicine quinidine buy topiramate 100mg visa. This triggers the activation of integrins, which leads to firm leukocyte arrest on the endothelium. These interactions occur through cell surface receptors that mediatecell-cellbinding,oradhesion,ofleukocytes. Neutrophil tether to and roll on P- and E-selectin expressed on activated endothelial cells. Sepsis begins when the innate immune system responds aggressively to the presence of bacteria. In addition to the involvement of these receptors in a varietyofimmunefunctions,integrinmoleculesplayarole inthespreadofmalignantcells. Themajorcauseofdeathin malignant disease is not the primary tumor but rather the metastasis of tumor cells to distant sites within the body. This process occurs when phagocytes attempt to engulf particles that are too large. Individualswithamarked decreaseofneutrophils(neutropenia)orseveredefectsinneutrophil function frequently have recurrent systemic bacterial infections. As a result, patients have life-threatening infections and granulomatous complications. Other signs and symptoms include early onsetofbacterialinfections,includingskininfections,mucositis,otitis,gingivitis,andperiodontitis. In this disorder,azurophilicgranulesarepresent,butmyeloperoxidase is decreased or absent. Specific Granule Deficiency Specific granule deficiency is believed to be an autosomal recessivedisease. As a result of this enzyme deficiency, cerebroside accumulates in histiocytes (macrophages). Niemann-Pickdisease affects infants and children, with an average life expectancyof5years. Qualitative disorders of monocytes-macrophages manifest as lipid storage diseases, including a number of rare autosomal recessive disorders. Resistance to infection can be impaired,atleastpartially,becauseofadefectinmacrophage function. Theprognosisvaries;withmilddisease,thepatientmay live a relatively normal life, whereas with severe disease the patientmaydieprematurely. Affectedindividualsdonot have increased susceptibility to viral infections or malignant neoplasms. Inaddition,thebacteriamustbe intracellular and not extracellular for the test result to be positive. Choosefromthefollowinganswers: E ngulfment C hemotaxis P hagosomeformation A dherence Bacterium Segmented neutrophil 37. Peakman M, Vergani D: Basic and clinical immunology, ed 2, Edinburgh, 2009,ChurchillLivingstone. The immunologically specific cellular component of the immune system is organized around two classesofspecializedcells,TlymphocytesandBlymphocytes. Theseepidermal cells then interact with lymphocytes in the skin and in draininglymphnodes. Circulating blood has enough mature T cells to produce a graft-versus-host reaction. These cells are responsible for cellular immune responses and are involved in the regulation of antibody reactions in conjunction with Blymphocytes. Thymocytes that express gamma and delta chains follow a different developmental pathway. An adaptive immune response consistsofdistinctphases;thefirstthreeare therecognitionofantigen,activationoflymphocytes,andeliminationofantigen(effector phase). The response declines as antigenstimulated lymphocytes die by apoptosis, restoringhomeostasis,andtheantigen-specific cells that survive are responsible for memory. Theseprinciples apply to humoral immunity (measured by B lymphocytes) and cell-mediated immunity (mediatedbyTlymphocytes). This increases the probability that an individual lymphocyte will encounter an antigenthatbindstoitsreceptor,therebytriggeringactivation and proliferation of the cell. This process, clonal selection, accounts for most of the basic properties of the adaptive immunesystem. Thesedivisionsarenotabsolute,withconsiderableoverlap or redundancy in function among the different subsets. Note that many cells have detached from the surface, some cells are swollen, and a few cells exhibit the morphology of normal cells. SuppressorT lymphocytes, orT suppressor (Ts) cells, are functionally definedT cells that downregulate the actions of otherTandBcells. Inthispathway, proteins in the cytoplasm are cleaved into peptide fragments about 20 amino acids in length. Theantigensarethenprocessed in a series of intracellular acidic vesicles called endosomes. The difference in structure of the distal regions of the alpha and beta chains allows the development of different clones ofT cells. These events stimulate the activation of at least three intracellular signaling cascades. T cell activation is a complex reaction involving transmembrane signaling and intracellular enzymeactivationsteps. Moredifferentiated(butstillimmature) B cells have intact cytoplasmic IgM and surface IgM. After binding and cooperative interaction withT cells, B cells undergo transformation into plasma cells. As the responseproceeds,otherisotypes(IgG,IgA,andIgE)emerge from Ig class switching. Theproliferative response of T lymphocytes to mitogens or antigens such as Mycobacterium tuberculosis or varicella-zoster virus is impaired. Althoughthetotalnumber of B cells and total Ig concentration remain unchanged, the serum concentration of IgM is decreased and IgA and IgG concentrationsareincreased. Ifabnormal results are subsequently found, the diagnosis is an innate immunedeficiency. ThenumberofTlymphocytes,theprimaryeffectorcellsin cell-mediated reactions, can be determined by several techniques. Research-Based Tests Variousproceduresareresearch-based,includingalymphocyte antigen and mitogen proliferation panel. Table4-5 Next Steps in Evaluation of Suspected Immunodeficiency Based on Physical Findings Physical Manifestations Recurrentsevereviralor fungalinfections. Inthecirculatingblood,lymphopeniaisgenerallypresent, although in some cases the concentration of lymphocytes is normal. Infants have failure to thrive, recurrent or chronic pulmonary infections,oralorcutaneouscandidiasis,chronicdiarrhea,recurrent skininfections,gram-negativesepsis,urinarytractinfections, andseverevaricella. Inaddition, diminished lymphoid tissue and abnormal thymus architecture are observed. Peripheral lymphoid tissues are hypoplastic and demonstrate paracortical lymphocyte depletion.
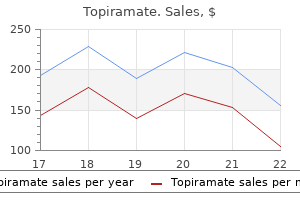
| Comparative prices of Topiramate | ||
| # | Retailer | Average price |
| 1 | Gap | 152 |
| 2 | Starbucks | 491 |
| 3 | A&P | 362 |
| 4 | Amazon.com | 985 |
| 5 | HSN | 853 |
| 6 | Publix | 171 |
| 7 | Brinker International | 198 |
| 8 | McDonald's | 155 |
| 9 | Best Buy | 565 |
Order generic topiramate online
This biopsy specimen also showed severe bile duct damage of the interlobular bile ducts symptoms of kidney stones cheap 100 mg topiramate amex, which is characterized by eosinophilic transformation and uneven nuclear spacing (arrows). This biopsy shows almost complete bile duct loss, which is demonstrated by an immunohistochemical stain for cytokeratin 7 (bottom). Only two small interlobular bile ducts are observed in one portal tract (arrowheads). Severe or very late stage chronic rejection can also result in loss of the small hepatic artery branches. Top left inset shows the lack of bile ducts and lack of hepatic artery branches in this portal tract. Included are plasma cellrich infiltrates and interface and perivenular necroinflammatory activity. It is inappropriate to provide a "rejection grade" when the diagnosis of rejection is uncertain. From Banff schema for grading liver allograft rejection: an international consensus document. Bile duct inflammation damage 1 2 Chronic Rejection General Considerations Chronic rejection is defined as immunological injury that usually evolves from severe or persistent acute rejection and results in potentially irreversible damage to bile ducts, arteries, and veins. Whether chronic rejection increases with time after transplantation, as in other organs, depends on how it is defined. If one includes idiopathic posttransplant hepatitis and newly described perivenular and subsinusoidal fibrosis in this category, the incidence is higher than the 5% figure quoted earlier. Defined in this way, chronic rejection might also increase with time, especially in suboptimally immunosuppressed recipients, regardless of how it is defined. Several studies, however, have shown that the early phase of chronic rejection is potentially reversible,110,206,210,211 which in turn depends on preservation of ductules and surrounding microvasculature. Compared to acute rejection, chronic rejection is usually associated with less severe inflammation, overall, eosinophils are less common, and the inflammatory infiltrate is composed primarily of lymphocytes, plasma cells, and mast cells. The nuclear changes are combined with eosinophilic transformation of the cytoplasm and bile ducts only partially lined by biliary epithelial cells. Latestage chronic rejection is characterized by bile duct loss involving more than 50% of portal tracts; arteriolar loss can also be seen. Arterial loss is considered present when less than 77 % of the portal tracts contain hepatic artery branches. Bile ductartery parallelism can also be used to define ductopenia as at least one unpaired artery in more than 10% of all portal tracts or two unpaired arteries in different portal tracts. Late chronic rejection (currently rare) can present with both bile duct and arterial loss,208,209 which makes it difficult to apply these algorithms. Portal tract recognition should be based primarily on the location of the putative structurecholestasis in chronic rejection is centrilobular. A ductular reaction at the interface zone is unusual in chronic rejection, unless the liver is recovering from chronic rejection206,210,211 or coexistent biliary tract strictures are present. Cytokeratin 7 can also be used to detect ductular metaplasia of periportal hepatocytes. The latter can be substantiated by periportal hepatocyte copper deposits, which are not seen in chronic rejection. The terminal hepatic venules and surrounding perivenular parenchyma in early chronic rejection show subendothelial and/or perivenular mononuclear inflammation, consisting of lymphocytes, pigment-laden macrophages, and plasma cells,197,207 which are accompanied by perivenular hepatocyte dropout and mild perivenular fibrosis. Perhaps the combination of venopathy and obliterative arteriopathy blunts any regenerative response. This system semiquantitatively grades the severity of fibrosis in three separate compartments: portal/ periportal, subsinusoidal, and perivenular, on a scale of 0 to 3. A final diagnosis of classic chronic rejection should be based on a combination of the clinical, radiological, laboratory, and histopathological findings. In a biopsy specimen, minimal diagnostic criteria for chronic rejection are: (1) senescent changes, affecting a majority of the bile ducts, with or without bile duct loss; or (2) convincing foam cell obliterative arteriopathy; or (3) bile duct loss affecting greater than 50% of the portal tracts. This is because obliterative and foam cell arteriopathy can be directly observed in the first-, second-, and third-order branches of the hepatic arterial tree in and around the liver hilum. Accumulation of the foamy macrophages usually first occurs in the intima, which triggers proliferation of intimal, and migration of medial, donor-derived myofibroblasts. Eventually the marked intimal thickening/luminal narrowing causes medial thinning as arteries attempt to dilate and compensate for reduced arterial flow. Compensatory mechanisms eventually fail, and the entire wall can be completely replaced by foam cells, or the artery undergoes thrombosis, causing necrosis of large bile ducts and ischemic cholangiopathy. Foamy macrophages can also be seen around bile ducts and veins in the connective tissue. Large perihilar bile ducts can also show focal sloughing of the epithelium, papillary hyperplasia, mural fibrosis, and acute and chronic inflammation. Staging of chronic rejection assumes that the diagnosis has already been correctly established and implies information about the potential for recovery. Late chronic rejection suggests that limited potential for recovery and retransplantation should be considered, if otherwise clinically indicated. Some patients appear to persist in the acute/early stage for months or years, whereas others rapidly develop severe fibrosis and late changes within the first year after transplantation or within weeks or months after the first onset. It is not well established therefore that all patients proceed 84 HistopatHology of liver transplantation 1139 sequentially in an orderly fashion from the early to late chronic rejection. Some cases show predominantly or exclusively either bile duct loss or arteriopathy alone, but usually both features occur together. Instead staging provides information about the likelihood of reversal, which should be correlated with other clinical and laboratory parameters. Differential Diagnosis A chronic rejection diagnosis is primarily based on damage and loss of small bile ducts and perivenular fibrosis in needle biopsy specimens because arteries with pathognomonic changes are rarely sampled. Therefore a diagnosis of chronic rejection based on biliary epithelial cell senescence or loss or perivenular fibrosis alone should first exclude other nonrejection-related causes of ductal injury and loss or perivenular fibrosis. Features that favor biliary strictures/obstructive cholangiopathy include112 (1) bile duct loss in some portal tracts accompanied by a ductular reaction in others, (2) neutrophil clusters within the lobules, (3) bile infarcts, (4) deposition of copper/copper-associated protein in periportal hepatocytes, and (5) hepatocanalicular cholestasis out of proportion to the prevalence of ductopenia (<50%). Cholangiography and/or angiography may be required in some cases to distinguish between chronic rejection and biliary stricturing/obstruction. Such studies usually show "pruning" and poor peripheral filling in chronic rejection. Isolated ductopenia involving less than 50% of portal tracts can be seen without significant elevations of liver injury test results. Whether these uncommon cases are an early phase of chronic rejection is uncertain. The most reliable algorithm to establish a chronic rejection diagnosis is to review prior biopsy findings and closely correlate the histopathological findings with the clinical course. However, a high index of suspicion for bacterial, fungal, and viral infections should always be maintained. Bacterial and fungal infections often arise in nonviable tissue; therefore most necrotic tissue should be routinely subjected to special stains for bacteria and fungi. Histopathological manifestations of deep fungal and bacterial infections are familiar to most pathologists and beyond the intended scope of this chapter. These viruses do not usually cause clinically significant acute hepatitis in immunocompetent individuals; they can, however, cause acute hepatitis in immunologically naive and immunodeficient individuals. The vast majority of adults in the general population have been infected with these viruses and harbor "latent" infections kept in check by humoral and cellular immunity. In contrast, depending on age, most children have not yet been infected and are susceptible to primary infection and acute hepatitis with these viruses. However, most adult recipients carry latent infections and develop "reactivation" infection/ disease. In contrast, most pediatric recipients are immunologically naive and develop primary infections/disease. In general, primary infections produce more severe disease than reactivation infections. All types of infections result in periodic viral nucleic acid or protein shedding into the peripheral circulation, where it can be monitored. An emerging challenge is compartmentalized disease, detectable in tissue biopsy specimens, but not in various serological assays. Under current management schemes, infected hepatocytes rarely contain diagnostic nuclear and/or cytoplasmic inclusions; instead, inclusions are now limited to patients who are overimmunosuppressed and not adequately monitored or treated. Diagnostic features include large eosinophilic intranuclear inclusions surrounded by a clear halo accompanied by small basophilic or amphophilic cytoplasmic inclusions that can be seen in any cell type.
Generic topiramate 200mg with visa
Two types exist, type 1 (low antigen level and low functional protein) and type 2 (normal antigen level with low function) medications for rheumatoid arthritis buy genuine topiramate line. Familial Mediterranean Fever this defect in protease in peritoneal and synovial fluid is transmitted as an autosomal recessive trait on chromosome 16. Patients with this defect experience recurrent episodes of fever and inflammation in the joints and pleural and peritoneal fluids. Cytokines are synthesized and secreted by the cells associated with innate and adaptive immunity in response to microbial and other antigen exposures (Tables 5-6 and 5-7). The generic term cytokines has become the preferred name for this class of mediators. Lymphokines is another term used to describe cytokines produced by activated lymphocytes. As cytokines are discovered and characterized, they are assigned a number using a standard nomenclature. Cytokines are polypeptide products of activated cells that control a variety of cellular responses and thereby regulate the immune response. Many cytokines are released in response to specific antigens; however, cytokines are nonspecific in that their chemical structure is not determined by the stimulating antigen. Hematopoietic and lymphoid cell compartments are regulated by a complex network of interacting cytokines. Their action is usually limited to affecting cells in the local area of their production, but they can also have systemic effects. Cytokines act on other cells by bonding to cytokine receptors on the surface of cells. Individual cytokines have characteristic functions and differ in how they transduce signals as a result of binding. All cytokine receptors consist of one or more transmembrane proteins whose extracellular portions are responsible for cytokine binding and whose cytoplasmic portions are responsible for initiating the intracellular signaling pathways. These molecules modulate inflammation and immunity by regulating growth, mobility, and differentiation of lymphoid cells. Interferons the interferons are a group of cytokines discovered in virally infected cultured cells. This interference with viral replication in the cells by another virus led to the term interferon. Its ability to augment the activity of many cytokines has resulted in clinical trials in a number of different diseases. Tumor Necrosis Factor Tumor necrosis factor is the principal mediator of the acute inflammatory response to gram-negative bacteria and other infectious microbes. The syndrome known as septic shock is a complication of severe gram-negative bacterial sepsis. The cytokine that interacts with this receptor is called c-kit ligand, or stem cell factor, because it acts on immature stem cells. Stem cell factor may also play a role in sustaining the viability and proliferative capacity of immature T cells in the thymus and mast cells in mucosal tissues. These proteins are necessary for the survival, proliferation, and differentiation of precursor cells of the immune system. These factors were found to induce phenotypic transformation in nonneoplastic cells and subsequently were termed transforming growth factors. It inhibits the proliferation and differentiation of T cells and the activation of macrophages. Overview A group of glycoproteins associated with the acute-phase response are collectively called acute-phase proteins or acute-phase reactants. The various acute-phase proteins rise at different rates and in varying levels in response to tissue injury. The increased synthesis of these proteins takes place shortly after a trauma and is initiated and sustained by proinflammatory cytokines. Synthesis and Catabolism All the acute-phase proteins are synthesized rapidly in response to tissue injury. In addition, strenuous exercise triggers an inflammatory response similar to that in sepsis. Indices of the inflammatory response, especially to exercise, include leukocytosis, release of inflammatory mediators and acute-phase reactants, tissue damage, priming of various white blood cell lines, production of free radicals, activation of complement, coagulation, and fibrinolytic cascades. Some, the negative acute-phase proteins, actually decrease, possibly resulting from a loss of protein from the vascular space. In addition, acute-phase proteins can be modified by causes other than inflammation. In addition, liver insufficiency or leakage through the kidney or gut lesions can lower these reactants. The rate of change and peak concentration of separate acute-phase reactants vary with the component and the clinical situation. The levels of complement components, C3 and C4, and ceruloplasmin do not rise for several days. This mismatch in acute-phase protein levels is most often the result of increased catabolism and elimination from the circulation of certain proteins. More than 20 acute-phase proteins have a definable role in inflammation (Box 5-2). Profiles of inflammatory changes yield detailed information but rarely provide major evidence for diagnosis or treatment. Aspirin-like drugs do not suppress acute-phase proteins in inflammation, allowing optimal therapy in the shortest time and minimizing ongoing inflammation and joint damage. Other Acute-Phase Reactants 1-Antitrypsin is an acute-phase protein that increases in acute inflammatory reactions. Generalized vasculitis, such as in immune complex disease, may result in inappropriately low levels of 1-antitrypsin, probably resulting from increased elimination of complexes with leukocyte lysosomal enzymes. Defects in the complement components C3a and C5a and the opsonin C3b result in serious infections. In addition, immune complex disease and gram-negative bacteremia result in low levels of complement components, particularly C3 and C4, because the components are consumed during complement activation. If both disorders are present, complement consumption may be masked, making it deceptive to use complement measurement as the only index of immune complex deposition in disease. The detection of complement breakdown products is more useful than the measurement of total complement component concentrations. It is more desirable to measure C3 breakdown products than total C3 in conditions such as peritonitis or pancreatitis. Lymphomas may result in a marked increase in C1 esterase inhibitor, with little other change. Diagnostic categories of acute inflammation can include bacterial causes and nonbacterial causes such as trauma, chronic inflammation, and viral disease. In addition to these hematologic tests, several tests are of direct value in immunologic testing. She had a history of chronic cholecystitis; recent x-ray studies revealed stones in the gallbladder and a large stone in the biliary duct. During surgery, a large stone was removed from the duct, and a cholangiogram showed no further obstructions of the hepatic or common bile ducts. Immediately after drawing the blood work, the patient was started on a broad-spectrum antibiotic and discharged on hospital day 15. A positive reaction is reported when the undiluted specimen or the 1:5 diluted specimen demonstrates agglutination, or when both exhibit agglutination. Negative Reaction the absence of visible agglutination and the presence of opaque fluid constitute a negative reaction. A negative reaction is reported only when both the undiluted specimen and the 1:5 diluted specimen exhibit no visible agglutination.
Generic topiramate 100 mg without prescription
Histopathological analysis remains the gold standard of diagnosis; it provides valuable information regarding prognosis and allows a tailored approach to therapy symptoms vaginal yeast infection discount topiramate. Copyright 2013 the American Society of Transplantation and the American Society of Transplant Surgeons. Epstein-Barr virus and posttransplant lymphoproliferative disorder in solid organ transplantation. There are no well-established published data to date to support the widespread use of these strategies in the clinical arena. Appropriate therapy of this condition requires a multidisciplinary approach involving transplant physicians and surgeons, infectious disease specialists, and both medical and radiation oncologists. Under most circumstances the first step of treatment is reduction of immunosuppression to the lowest tolerated dose to avoid graft rejection. The main predictors of poor response were bulky disease, advanced clinical stage, and older age at diagnosis. Unfortunately, these strategies have not been associated with significant clinical improvement or are still under active research. These efforts ultimately resulted in the development of the so-called Milan criteria by Mazzaferro et al in 1996. All patients received adjuvant chemotherapy with doxorubicin for the first 20 postoperative weeks. They found a significant improvement in 5-year survival among 109 recipients on sirolimus (83%) compared with 2382 on other immunosuppressant drugs (69%). However, true recurrent disease tends to occur within the first 2 years after transplant and can present in one or more sites simultaneously. The most commonly affected locations include the lung (50%), liver (49%), and bone (26%). Treatment of these lesions is palliative; good symptomatic control can be obtained with external beam radiation therapy and occasionally with zoledronic acid (intravenous bisphosphonate). Recurrence was confined to the liver in 5 patients (16%), was extrahepatic in 20 patients (65%), and was both extrahepatic and intrahepatic in 6 patients (19%). The median overall survival after starting sorafenib was 19 months, the median time to disease progression was 6. Other adverse events included dyslipidemia in a third of the patients, hand-foot syndrome in 55% (mostly mild to moderate), and diarrhea in 77%. Notably, sorafenib had to be discontinued in 3 patients due to severe hepatotoxicity. Recurrence probability Cholangiocarcinoma Cholangiocarcinoma represents the second most common primary liver malignancy, with an incidence of 1. On occasion, a lifesaving transplant may be acceptable in circumstances where recipient expected survival without transplantation is short. Copyright 2011 the Authors, copyright 2011 the American Society of Transplantation and the American Society of Transplant Surgeons. Initially successful single-center experiences have led other transplant centers to adopt this treatment strategy, with over 20 centers (including our own institution) in the United States offering this modality in selected patients with perihilar cholangiocarcinoma. In a recent study from the United States, 287 patients with perihilar cholangiocarcinoma from 12 transplant centers underwent neoadjuvant radiation and chemotherapy followed in most cases by liver transplant. Of the 214 patients who did undergo liver transplantation, the overall cancer-free survival at 2, 5, and 10 years was 78%, 65%, and 59%, respectively. These survival rates are similar to what has been described in the liver transplant literature in other patient populations. Noticeably, the posttransplant recurrence of cholangiocarcinoma in this select group of patients was 20%, and the vast majority of these patients succumbed to the disease. The most important prognostic factor was tumor size greater than 3 cm, because the 5-year recurrence-free survival rate was only 32% compared with 69% in those with tumors less than 3 cm. A total of 26 patients (19%) developed cancer recurrence at a median of 23 months (range 1 to 128) after transplantation. Nonetheless, recurrence of cholangiocarcinoma is seen in 19% of recipients and is associated with a very high mortality rate. As new therapies to treat cholangiocarcinoma become available, they could be offered to patients identified at higher risk for disease progression before transplantation or in whom posttransplant recurrence is diagnosed. Extrahepatic Malignancies Data available from the kidney transplant literature demonstrate a low recurrence rate of pretransplant malignancies in this population. For example, in a large registry of kidney transplant recipients from Australia and New Zealand, 210 of 11,894 had a history of malignancy (1. In a large single-center study from Germany, 37 of 606 transplant recipients (6%) had a history of malignancy before transplantation. The neoplasms consisted of 11 hematological malignancies, 22 solid malignant tumors, and 4 premalignant conditions. The median interval between diagnosis of the malignancy and liver transplant was 43 months (with a wide range of <1 to 321 months). Seven patients were transplanted at the time of presentation with acute Budd-Chiari syndrome secondary to myeloproliferative disorder and were hence diagnosed with the malignancy shortly before transplant. In contrast, of the remaining 30 patients, 8 (27%) were diagnosed or treated for their malignancy within 2 years of transplant, 8 (27%) were diagnosed or treated 2 to 5 years before transplant, and 14 (46%) had been treated for cancer more than 5 years before transplant. None of the 11 recipients with a history of hematological malignancy experienced recurrence or transformation of disease during a follow-up of up to 131 months. Of the recipients with a history of solid organ cancer, only 1 had recurrent disease. Three weeks later, he underwent colectomy and nodal resection but unfortunately died 6 months after liver transplant with generalized metastatic disease. None of these patients had metastatic disease, and all remained tumor-free after liver transplant. The 5- and 10-year probability of recurrence in this group of patients was 3%, compared with 7% and 15% for de novo malignancy at 5 and 10 years posttransplant from the same transplant center. Borrowing from the kidney transplant literature, and based on the presumed risk for recurrence, pretransplant malignancies can be loosely categorized as low, intermediate, or high risk for recurrence. Accordingly, recommended waiting times after cancer remission before listing for transplant have been published. Although these guidelines are useful, it is up to each transplant center to have its own criteria for listing patients with prior malignancies. When confronted with uncommon malignancies, an individualized approach with input from oncologists is warranted. In an effort to assess the impact of pretransplant malignancy on mortality in transplant recipients, Swedish investigators identified a population-based cohort of solid organ transplant recipients transplanted between 1970 and 2008. Out of close to 10,500 eligible recipients, 416 (4%) had a history of malignancy unrelated to the indication for transplantation. Three quarters were kidney transplant recipients, but liver transplant recipients constituted 11% of the cohort. Twenty percent of the patients received transplants less than 2 years from cancer diagnosis; 50%, 2 to 10 years after cancer diagnosis; and 30%, more than 10 years after cancer diagnosis. Among nonkidney transplants, longer waiting times from cancer diagnosis to transplantation were not associated with improved mortality, suggesting that the specific type of malignancy has a greater impact on cancer recurrence and mortality than the waiting time. This fact is especially relevant when trying to expand the donor pool, and hence organs from donors with a history of or with certain types of active malignancies will need to be evaluated for suitability for transplantation. They created six risk categories and suggested risk categorizations for specific tumor types based on our current understanding of the biological characteristics of these neoplasms. In this large cohort, only 1 donor with glioblastoma multiforme was found to transmit the disease to 3 recipients, all of whom succumbed to the disease. The only other case of donor-derived malignancy was that of a donor with a remote history of melanoma (32 years before donation) who transmitted the disease to a single recipient. Although donor-derived malignancy is rare, the morbidity and mortality of recipients with this diagnosis is very high. The aim of cancer screening programs is to detect cancer at an early stage, allowing potentially curative treatment to be provided and to improve patient survival. Because liver transplant recipients are at increased risk for cancer, it seems justified to follow cancer-screening strategies Table 86-6). Most transplant centers have their own posttransplant screening protocols, and there is scant evidence supporting any particular screening protocol. After introduction of an intensified screening program, detection of de novo cancer increased from 5% to 13% and more de novo malignancies were diagnosed at an earlier stage.
Discount topiramate 200 mg without prescription
The arterial revascularization is achieved either by anastomosis to the recipient left hepatic artery stump or to a donor iliac artery conduit from the suprarenal or infrarenal aorta medications similar buspar order discount topiramate line. The portal vein to the native liver is narrowed in these cases to avoid graft atrophy due to insufficient venous flow. A nonabsorbable tie is placed around the native right portal vein to narrow it down by about 70% until the portal pressure is slightly lower than that measured in the left portal vein (about 1 to 2 mm Hg lower). In cases of metabolic diseases the portal vein to the native liver is narrowed to ensure the graft receives sufficient inflow to avoid atrophy. A nonabsorbable tie is placed surrounding the native right portal vein (above) until portal pressure is slightly lower than left portal vein pressure (about 1 to 2 mm Hg lower). We perform common and left portal vein pressure measurements before and after narrowing (below). Right Auxiliary Partial Orthotopic Liver Transplantation Recipient extended right hepatectomy is performed; the hilar dissection is confined to the right side, with minimal dissection of the bile duct. The right hepatic artery is ligated to the right of the common bile duct, and the right branch of the portal vein is exposed. The right side of the liver needs to be mobilized from the inferior vena cava sufficiently to expose the right hepatic vein and a satisfactory cuff of cava for subsequent anastomosis. The suprahepatic vena cava of the right lobe is implanted using a piggyback technique to an extended right hepatic vein orifice opened inferiorly for a wide cavocavostomy. The donor portal vein is anastomosed end-to-end to the right portal or end-to-side to the main trunk. Arterial revascularization is achieved using either the recipient right hepatic artery or a donor iliac artery conduit from the suprarenal or infrarenal aorta. When performing right auxiliary liver transplantation for acute liver failure, a temporary partial portocaval shunt (below) may help hemodynamic stability and reduce blood during partial hepatectomy of the native liver. The incidence of relaparotomy is higher for drainage of intra-abdominal collection or for bleeding. Secondary hemorrhage occurs more commonly because of the associated renal failure and the continuing postoperative need for renal replacement therapy in many of these patients. The use of heparin and other anticoagulants should be considered carefully in light of this risk. These patients have been managed with a combination of lamivudine and hepatitis B immune globulin for a period of up to 1 year after transplant. These measures have been taken to reduce the likelihood of disease recurrence, even though one patient who received no prophylaxis remained free of virus. Follow-up and Immunosuppression the postoperative recovery of liver function may differ from that observed after whole-liver transplantation. The coagulopathy may correct more slowly, particularly if the graft volume is small. The serum transaminase levels may not fall in the normal trajectory because of a contribution from the injured native liver. The diagnosis of acute rejection may be challenging, because less marked elevation of the serum transaminase levels is seen compared with whole-liver replacement (depending on the relative graft size). Diagnosis of rejection was delayed in our first patient because no abnormality of liver function was noted other than a modest elevation of serum bilirubin level, which was thought to be due solely to poor portal venous inflow. Our experience has shown that mild cases of unconjugated hyperbilirubinemia should be investigated with graft biopsy to exclude rejection. However, we believe that many of the previously observed poorly functioning grafts have been the result of low-grade venous outflow complications that evolve into small-forsize syndrome. A small number of patients have persistent cholestasis and residual portal hypertension as a result. Currently we perform these investigations at 3, 6, and 12 months after transplantation, and the decision to reduce immunosuppression is usually made at 6 months or when signs of healthy regeneration are seen on biopsy. Gradual weaning may be required to initiate low-grade graft rejection and to stimulate regrowth of the native liver. The majority of patients who survive long term can be withdrawn from their immunosuppressive therapy. However, this must be performed gradually; otherwise an episode of severe acute rejection may be precipitated and lead to graft thrombosis and loss before sufficient regeneration has occurred. The timing of immunosuppression reduction will depend on the rapidity of liver regeneration, which in turn is dependent on the cause of liver failure and the volume and function of the graft. However, the larger volume of graft transplanted in this group (right lobe) will tend to inhibit native liver regeneration. In the subacute group the regeneration is less rapid, as observed by sequential imaging. As a consequence, reduction and withdrawal of immunosuppression tends to be later. Abrupt immunosuppression withdrawal is associated with hepatic artery thrombosis, particularly in large grafts. Graft atrophy occurs with controlled immunosuppression withdrawal, and there is seldom a need to excise these grafts ("vanishing graft syndrome"). The majority of patients are young and at greatest risk for the complications of prolonged exposure to immunosuppression. This should be considered as the best option for appropriate patients with suitable grafts. Emergency subtotal hepatectomy: a new concept for acetaminophen-induced acute liver failure: temporary hepatic support by auxiliary orthotopic liver transplantation enables long-term success. Routine use of auxiliary partial orthotopic liver transplantation for children with fulminant hepatic failure: Preliminary report. Auxiliary liver transplantation for fulminant hepatitis B: results from a series of six patients with special emphasis on regeneration and recurrence of hepatitis B. How can we share the portal blood inflow in auxiliary partial heterotopic liver transplantation without portal hypertension? Functional portal flow competition after auxiliary partial orthotopic living donor liver transplantation in noncirrhotic metabolic liver disease. How does auxiliary liver transplantation regulate alloreactivity in sensitized kidney transplant patients? Auxiliary liver and combined kidney transplantation prevents hyperacute kidney rejection in highly sensitized patients. Successful combined partial auxiliary liver and kidney transplantation in highly sensitized cross-match positive recipients. Postischemic inflammatory response in an auxiliary liver graft predicts renal graft outcome in sensitized patients. Is indoleamine 2,3-dioxygenase important for graft acceptance in highly sensitized patients after combined auxiliary liver-kidney transplantation? Immunological advantage on small bowel graft induced by simultaneously transplanted liver in porcine auxiliary liver/small bowel transplantation. Preclinical experiment of auxiliary partial orthotopic liver transplantation as a curative treatment for hemophilia. Auxiliary partial orthotopic living donor liver transplantation for a child with congenital absence of the portal vein. Resolution of hepatopulmonary syndrome after auxiliary partial orthotopic liver transplantation in Abernethy malformation. Auxiliary partial orthotopic living donor liver transplantation with a small-for-size graft for congenital absence of the portal vein. Auxiliary partial orthotopic living donor liver transplantation as an aid for small-for-size grafts in larger recipients. Auxiliary liver transplantation with arterialization of the portal vein for acute hepatic failure. Long-term follow-up of auxiliary orthotopic liver transplantation for the treatment of fulminant hepatic failure. Auxiliary liver transplantation: regeneration of the native liver and outcome in 30 patients with fulminant hepatic failurea multicenter European study. Auxiliary partial orthotopic liver transplantation for acute liver failure: the Hannover experience.
Order topiramate 200 mg with visa
Lastly symptoms gout cheap 100mg topiramate mastercard, developments in the field of tissue engineering are still at an early stage. The physiologic response of the small bowel of the dogs to ischemia including prolonged in vitro preservation of the bowel with successful replacement and survival. Intestinal transplantation at the University of Nebraska Medical Center: 1990-2001. Indications for pediatric intestinal transplantation: a position paper of the American Society of Transplantation. Lessons learned in pediatric small bowel and liver transplantation from living related donors. Simultaneous or sequential combined living donor-intestine transplantation in children. Living-related intestinal transplantation: first report of a standardized surgical technique. Evolution of the immunosuppressive strategies for the intestinal and multivisceral recipients with special reference to allograft immunity and achievement of partial tolerance. Pearls and Pitfalls · Early and timely referral to an intestinal rehabilitation center for evaluation is key for successful outcome and improved long-term survival. Long-term outcome, growth and digestive function in children 2 to 18 years after intestinal transplantation. Quality of life after pediatric intestinal transplantation: the perception of pediatric recipients and their parents. Longterm survival, nutritional autonomy, and quality of life after intestinal and multivisceral transplantation. Initial experience using rapamycin immunosuppression in pediatric intestinal transplant patients. Preliminary experience with Campath 1H (C1H) in intestinal and liver transplantation. Intestinal transplantation in children: a summary of clinical outcomes and prognostic factors in 108 patients from a single center. Management of Epstein-Barr virus-induced posttransplant lymphoproliferative disease in recipients of solid organ transplantation. Chemotherapy for posttransplant lymphoproliferative disorder: the Israel Penn International Transplant Tumor Registry experience. An acquired cause resulting from an in utero insult that interrupts the normal process of differentiation and orientation has been postulated in view of the frequent association between abnormal situs and other rare congenital defects. Theoretically any disturbance in the programmed sequence of rotation and organogenesis during this period may result in vascular and visceral anomalies. Regardless, the constellation of defects associated with abnormal situs renders surgical intervention technically challenging. Significant technical problems were encountered, and no patient survived more than 11 days. Since our last review, there have now been 90 transplants performed worldwide for these conditions. The most common technical complications reported were primary nonfunction (6%), hepatic artery thrombosis (10%), portal vein thrombosis (3%), and biliary leaks/strictures (10%). Development of the portal vein occurs during the fifth to seventh embryonic weeks. At this stage the duodenum is intimately associated with the right, left, and communicating branches of the vitelline veins. A, Normal (retroduodenal) development of the duodenum relative to the right (Rt), left (L), and communicating branches of the vitelline vein. B, Differential atrophy of the communicating branches of the vitelline vein produces preduodenal positioning. In this section a review with recommendations for preoperative assessment, intraoperative conduct, and postoperative management is undertaken. Evaluation of patients with abnormal situs should not differ radically from that of other patients. Standard radiographic assessment at evaluation for transplantation includes a posteroanterior and lateral chest x-ray examination as well as a duplex ultrasound examination of the liver. However, if the hepatic vascular anatomy is not clear, then contrast-enhanced cross-sectional imaging in the form of computed tomography angiography or magnetic resonance angiography should be undertaken. In general the use of a smaller donor allows maximum flexibility when whole organs are transplanted. A donor-to-recipient weight ratio less than 1 is optimal and recommended for whole-organ donors. Standard donor liver procurement techniques are suitable, and vascular conduits must be available for use. Because there is no right lobe, the size considerations noted earlier do not apply. The regions include Europe, North America (N America), South America (S America), Asia, and Australia. Depicted are (1) multiple spleens, (2) a right-sided stomach with malrotation of the intestine, (3) arterial inflow off the superior mesenteric artery, (4) venous inflow off the preduodenal portal vein, (5) venous outflow via a cloaca of hepatic veins with the right hepatic vein oversewn in this diagram, and (6) Roux-en-Y choledochojejunostomy. This is obviously dependent on the location of the right atrium, thus emphasizing the importance of levocardia or dextrocardia. Several groups have successfully used a reduced-size graft consisting of the *References 22, 23, 33, 35, 45, 48. In this case the larger anatomical right lobe fits into the left upper quadrant that lacks a spleen. Although these options have been technically successful in a limited number of patients and offer an alternative for graft placement, the vast majority of recipients with abnormal situs have been well served by either a whole-organ or segmental donor allograft. Anastomosis directly to the right atrium, although not reported in any of the abnormal situs patients, is possible. Orthotopic liver transplantation in patients with biliary atresia and situs inversus. The suprahepatic vena cava outflow is oversewn, and the infrahepatic vena cava now becomes the outflow for the graft and is sutured to the recipient left-sided vena cava. Portal venous inflow is from the recipient mesenteric circulation, and hepatic arterial inflow is established from the aorta. In this case auxiliary positioning was chosen because of the presence of portal vein (pv) thrombosis, as well as the other associated vascular anomalies associated with situs inversus. The cirrhotic liver is left in position, and decompression of the mesenteric circulation is achieved through a venous conduit from the superior mesenteric vein (Sup mesenteric v). In this instance the liver is flipped 180 degrees on itself so that the caudate lobe and inferior vena cava are most anterior. The key principle for hypoplastic portal veins, either preduodenal or retroduodenal, is to dissect the vein more proximally until a vein with adequate diameter is obtained. Should this maneuver not prove adequate, the use of jump grafts directly off the splenic or mesenteric veins is another option. It is essential to obtain adequate inflow from an artery of suitable caliber and flow. In cases in which aberrant arterial anatomy is associated with poor inflow, the use of direct anastomoses to the aorta or aortic conduits is strongly recommended because of the excellent results reported. As a consequence, choledochocholedochostomy is rarely used to achieve biliary continuity in these patients. This is particularly important for postoperative radiographic studies and invasive studies such as liver biopsy. The results from published series indicate that the technical challenges presented by patients with abnormal situs are significant but that successful engraftment is possible if the following principles are used: 1. Standard preoperative evaluation of patients with abnormal situs is essential for operative planning, as well as for identification of associated conditions. Donor selection should attempt to procure a smaller graft to allow maximum flexibility during placement. The use of segmental grafts should be considered in cases in which a smaller donor is not available. Awareness of associated arterial and portal venous anomalies is crucial for successful grafting. Pearls and Pitfalls · Situs inversus and situs ambiguus are infrequent congenital malformations of unknown cause that can commonly be associated with biliary atresia.