Buy cefuroxime 500 mg free shipping
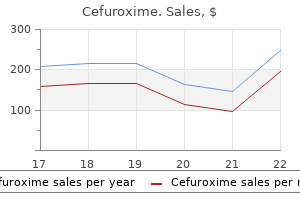
The umbilical cord begins to dry soon after birth symptoms 3 days past ovulation order 500mg cefuroxime with mastercard, becomes loose from the skin by 4 to 5 days, and falls off by 7 to 10 days. R edness/ umbilical erythema, foul odor, or wetness/ oozing of the cord may indicate omphalitis. Subconjunctival or scleral hemorrhages are a common result of the pressures of labor and birth. A lateral upward slope of the eyes with an epicanthal fold may indicate syndromes of mental, physical, or chromosomal aberrations. The absence o red ref ex may indicate tumors or congenital cataracts accompanying rubella, galactosemia, or disorders of calcium metabolism. Chorioretinitis is often found in congenital viral diseases such as cytomegalovirus and toxoplasmosis. Scleral blueness is associated with osteogenesis imper ecta and scleral yellowness with jaundice. Brain injury may be indicated by a constricted pupil, unilaterally dilated fixed pupil, nystagmus, or strabismus. Hydrocephalus is a condition in which an increase in cerebrospinal fluid creates an abnormally large and growing head. The researchers concluded that a difference of 20 mm Hg is more likely due to random variability than to coarctation and recommended that if weak/ absent pulses are present and coarctation is suspected, an echocardiogram is necessary. Vernix, a white, cheeselike material that contains quantities of -tocopherol and surfactant proteins that provide significant protection from infection, normally covers the body of the fetus and decreases with increased gestational age. Discoloration of the vernix occurs with intrauterine distress, postmaturity, hemolytic disease, and breech presentations. Mongolian spots caused by the presence of pigmented cells may cover the sacral-gluteal areas of infants of color. The degree of generalized pigmentation varies and is less intense in the newborn period than later in life. Note the size, shape, color, and degree o ecchymosis, erythema, petechiae, or hemangiomas. Meconium staining, which occurs in 10% to 20% o newborns, is indicative o prior etal distress. Milia caused by retained sebum are pinpoint white spots on the cheeks, chin, and bridge of the nose. L ortic inear regression (broken lines) and 95%con dence lim (solid lines) o systolic and diits astolic blood pressures on birth w in healthy new inants. L regression (broken lines) and 95%con dence lim (solid lines) inear its on birth w in healthy new in ants. Tissue turgor is the sensation of fullness derived from the presence of hydrated subcutaneous tissue and intrauterine nutrition. Test the elasticity of the skin by grasping a fold of skin between the thumb and forefinger. A loss o normal skin turgor resulting in peaking o the skin is a late sign o dehydration. A generalized hardness of the skin is a sign of sclerema that occurs in debilitated, stressed infants. If the angle of placement is greater than 10 degrees from vertical, it is abnormal. The level of placement is determined by drawing an imaginary line from the outer canthus of the eye to the occiput. Slapping hands or other sharp noises will normally elicit a twitching in the eyelid or a complete Moro reflex. Mal ormed or malpositioned (low-set or rotated) ears are often associated with renal and chromosomal abnormalities and other congenital anomalies. Abnormalities such as skin tags or sinuses may be associated with renal tract abnormalities or hearing loss. Check the patency o the alae nasi by (1) obstructing one nostril, closing the mouth, and observing breathing rom the open nostril; (2) placing a stethoscope under the nostrils that will " og" the diaphragm and auscultate breathing; or (3) passing a so t catheter (i necessary). Obstructions can be caused by drugs, infections, tumors, nasal discharge, nasal cysts, and mucus. Choanal atresia, a membranous or bony obstruction in the nasal passage, may be unilateral or bilateral. Choanal atresia is characterized by the noisy breathing, cyanosis, and apnea o the quiet in ant (mouth closed) as opposed to the pink color o the same crying in ant (mouth open). The mouth may be examined here or at the end of the examination when the infant is crying loudly with a wide-open mouth. A large tongue (macroglossia), cle t lip or palate (including submucous cle t), or high-arched palate may be associated with abnormal acies or be an isolated nding. I copious secretions or distress in eeding is present, it is o ten the result o esophageal atresia or tracheoesophageal stula. Con ormation o the newborn chest is cylindric with an anteroposterior ratio o 1:1. Asymmetry of the chest may be caused by diaphragmatic hernia, paralysis of the diaphragm, pneumothorax, emphysema, pulmonary agenesis, or pneumonia. Fullness o the thorax caused by increased anteroposterior diameter occurs with an overexpansion of the lung. R etractions, an inward pull o the so t parts o the chest while inhaling, indicate air-entry interference or pulmonary disease. Enlargement of breasts because of maternal hormones occurs in either sex on the second or third day. A racture o the clavicle is evidenced by a palpable mass, crepitation, tenderness at the racture site, and limited arm movements on the a ected side. Ambiguous genitalia result from incomplete or altered differentiation and require urology consultation. Hypospadias exists if the urethral opening is on the ventral surface of the penis. Inguinal or scrotal swelling, discoloration, palpable masses, and pain/ tenderness with palpation may be an inguinal hernia, testicular torsion, trauma, tumor, or hydrocele-a collection of fluid in the scrotal sac. Visualize and check the patency o the anal opening by waiting or meconium passage (it is optional to check patency by gently inserting a so t rubber catheter; do not use rigid objects such as glass rectal thermometers). Deviations rom normal include curvature o the vertebral column, pilonidal dimple, pilonidal sinus, spina bi da, or myelomeningocele. A study of spinal congenital dermal sinuses found an increased incidence (greater than 50%) of neurologic deficit, intradural tumors, or tethered cords; recommendations included a prompt radiologic evaluation and neurosurgical consultation so that timely intervention could preserve or improve neurologic function. The infant is capable of adduction, flexion, internal rotation, extension, and symmetry of movement. Simian creases may indicate chromosomal abnormalities that are frequent causes of deformity. Palsies caused by fractures, dislocations, or injury to the brachial plexus are recognized by limited movement of the extremity. Fractures may also be present with edema, palpable crepitus, or the "palpable spongy mass sign" over the clavicle. Note the normal position of flexion (develops according to gestational age) and abduction. A full range of motion is possible, including the "frog position"-a rotation of the thighs with the knees flexed. Osteogenesis imperfecta, a rare genetic defect of collagen production that results in brittle bones, manifests as multiple fractures and deformities. Paralysis of both legs is caused by severe trauma or congenital anomaly of the spinal cord. Fractures may be present and are characterized by limited movement and edematous, crepitant areas. R ecoil appears systematically as flexion first develops in the lower extremities and then in the upper extremities. Both legs should return promptly to the flexed position in accordance with the gestational age of the infant. The evaluation and documentation o the development o the nervous system in the normal newborn should be o paramount interest to all the health care clinicians caring or the newborn. Fortunately, or the most part, some portions o the neurologic examination are carried out as a component o the general physical examination o the newborn (activity, resting posture, symmetry, head size and morphology, rooting reflex, muscle tone, primitive reflexes, tremors and twitching, cry, recoil). Performing a complete and thorough physical examination of the newly born is paramount. First, because a newborn is recovering from the stress of birth, the neurologic examination is not reliable until after the infant has successfully completed the transition to extrauterine life.
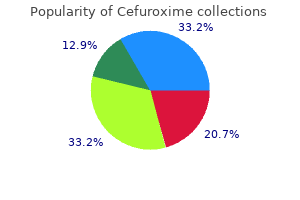
Discount 250 mg cefuroxime free shipping
Very long-chain fatty acids (>20 carbons) enter peroxisomes via an unknown mechanism for oxidation symptoms xanax overdose buy cheap cefuroxime 500mg line. Fatty acyl- CoA synthetase, on the outer mitochondrial membrane, activates the fatty acids by attaching CoA. The fatty acyl portion is then transferred onto carnitine by carnitine acyltransferase-1 for transport into the mitochondria. Carnitine acyltransferase-1 transfers the fatty acyl group to carnitine (outer mitochondrial membrane). Carnitine acyltransferase-2 transfers the fatty acyl group back to a CoA (mitochondrial matrix). Carnitine acyltransferase-1 is inhibited by malonyl-CoA from fatty acid synthesis and thereby prevents newly synthesized fatty acids from entering the mitochondria. Insulin indirectly inhibits -oxidation by activating acetyl-CoA carboxylase (fatty acid synthesis) and increasing the malonyl-CoA concentration in the cytoplasm. The carnitine transport system is most important for allowing longchain fatty acids to enter into the mitochondria. In a fasting state, the liver produces more acetyl-CoA from -oxidation than is used in the citric acid cycle. Much of the acetyl-CoA is used to synthesize ketone bodies (essentially two acetyl- CoA groups linked together) that are released into the blood for other tissues. Non-ketotic hypo- glycemia should be strongly associated with a block in hepatic -oxidation. Decreased acetyl-CoA lowers pyruvate carboxylase activity and also limits ketogenesis. Clinical Correlate Ackee, a fruit that grows on the ackee tree found in Jamaica and West Africa, contains hypoglycin, a toxin that acts as an inhibitor of fatty acyl-CoA dehydrogenase. After a period of prostration that may last as long as 18 hours, more vomiting may occur, followed by convulsions, coma, and death. The presence of severe hypoglycemia and absence of ketosis (hypoketosis) is strongly suggestive of a block in -oxidation. The episode in this case was precipitated by the 3-day gastroenteritis (vomiting/fasting). Hallmarks of this disease include: Muscle aches; mild to severe weakness Rhabdomyolysis, myoglobinuria, "red urine" Episode provoked by prolonged exercise especially after fasting, cold, or associated stress Symptoms may be exacerbated by high-fat, low-carbohydrate diet Muscle biopsy shows elevated muscle triglyceride detected as lipid droplets in cytoplasm Primary treatment: cease muscle activity and give glucose A somewhat similar syndrome can be produced by muscle carnitine deficiency secondary to a defect in the transport system for carnitine in muscle. Propionic Acid Pathway Fatty acids with an odd number of carbon atoms are oxidized by -oxidation identically to even-carbon fatty acids. The difference results only from the final cycle, in which even-carbon fatty acids yield two acetyl-CoA (from the 4-carbon fragment remaining) but odd-carbon fatty acids yield one acetyl-CoA and one propionyl-CoA (from the 5-carbon fragment remaining). Propionyl-CoA is converted to succinyl-CoA, a citric acid cycle intermediate, in the two-step propionic acid pathway. Because this extra succinyl-CoA can form malate and enter the cytoplasm and gluconeogenesis, odd-carbon fatty acids represent an exception to the rule that fatty acids cannot be converted to glucose in humans. In a patient with megaloblastic anemia, it is important to determine the underlying cause because B12 deficiency, if not corrected, produces a peripheral neuropathy owing to aberrant fatty acid incorporation into the myelin sheets associated with inadequate methylmalonylCoA mutase activity. Excretion of methylmalonic acid indicates a vitamin B12 deficiency rather than folate. Cardiac and skeletal muscles and renal cortex metabolize acetoacetate and 3-hydroxybutyrate to acetyl-CoA. Normally during a fast, muscle metabolizes ketones as rapidly as the liver releases them, preventing their accumulation in blood. After a week of fasting, ketones reach a concentration in blood high enough for the brain to begin metabolizing them. Ketogenesis (Liver) and Ketogenolysis (Extrahepatic) Clinical Correlate In untreated type 1 diabetes mellitus, there is no insulin. Ketogenesis Ketogenesis occurs in mitochondria of hepatocytes when excess acetyl-CoA accumulates in the fasting state. Acetone is a minor side product formed nonenzymatically but is not used as a fuel in tissues. It does, however, impart a strong odor (sweet or fruity) to the breath, which is almost diagnostic for ketoacidosis. Note the important times at which the brain switches from: Glucose derived from liver glycogenolysis to glucose derived from gluconeogenesis (~12 hours) Glucose derived from gluconeogenesis to ketones derived from fatty acids (~1 week) In the brain, when ketones are metabolized to acetyl-CoA, pyruvate dehydrogenase is inhibited. This important switch spares body protein (which otherwise would be catabolized to form glucose by gluconeogenesis in the liver) by allowing the brain to indirectly metabolize fatty acids as ketone bodies. Fuel Use in the Brain During Fasting and Starvation 247 Section I Molecular Biology and Biochemistry Ketoacidosis In patients with type 1 insulin-dependent diabetes mellitus not adequately treated with insulin, fatty acid release from adipose tissue and ketone synthesis in the liver exceed the ability of other tissues to metabolize them, and a profound, life-threatening ketoacidosis may occur. The basis for this observation is not completely understood, although type 2 disease has a much slower, insidious onset, and insulin resistance in the periphery is usually not complete. Once insulin is administered, however, blood potassium levels need to be monitored. Chronic hypoglycemia, which is often present in chronic alcoholism, favors fat release from adipose. Ketone production increases in the liver, but utilization in muscle may be slower than normal because alcohol is converted to acetate in the liver, diffuses into the blood, and oxidized by muscle as an alternative source of acetyl-CoA. In pathologic conditions, such as diabetes and alcoholism, ketoacidosis may develop with life-threatening consequences. In diabetic and alcoholic ketoacidosis, the ratio between acetoacetate and -hydroxybutyrate shifts and -hydroxybutyrate predominates. The urinary nitroprusside test detects only acetoacetate and can dramatically underestimate the extent of ketoacidosis and its resolution during treatment. Home monitors of both blood glucose and -hydroxybutyrate are available for diabetic patients. Lysosomes contain many enzymes, each of which removes specific groups from individual sphingolipids. Genetic deficiencies of many of these enzymes are known, and the diseases share some of the characteristics of I-cell disease discussed in Chapter 4. The attending physician noted massive hepatomegaly and splenomegaly, marked pallor, and hematologic complications. White cells were taken to assay for glucocerebrosidase, and the activity of the enzyme was found to be markedly below normal. Outside the brain, glucocerebroside arises mainly from the breakdown of old red and white blood cells. In the brain, glucocerebroside arises from the turnover of gangliosides during brain development and formation of the myelin sheath. Without the proper degradation of glucocerebroside due to a lack of glucocerebrosidase, it accumulates in cells and tissues responsible for its turnover. The easy bruising is due to a low blood platelet count, and the lethargy is due to the anemia. Enzyme replacement therapy results in the reduction of hepatosplenomegaly, skeletal abnormalities, and other Gaucher-associated problems. The major drawback of therapy using intravenously administered recombinant glucocerebrosidase is its prohibitive cost (several hundred thousand dollars per year). Fabry Disease In contrast to the other sphingolipidoses (Tay-Sachs, Gaucher, Niemann-Pick) which are all autosomal recessive, Fabry disease is the only one that is X-linked recessive. Fabry is caused by a mutation in the gene that encodes the lysosomal enzyme alpha-galactosidase. Fabry disease presents during childhood or adolescence: Burning sensations in the hands which gets worse with exercise and hot weather Small, raised reddish-purple blemishes on the skin (angiokeratomas) Eye manifestations, especially cloudiness of the cornea Impaired arterial circulation and increased risk of heart attack or stroke Enlargement of the heart and kidneys Often there is survival into adulthood but with increased risk of cardiovascular disease, stroke. Enzyme replacement therapy is available and, although expensive, slows the progression of the disease. As part of a study to quantify contributors of stress to hyperglycemia and ketosis in diabetes, normal hepatocytes and adipocytes in tissue culture were treated with cortisol and analyzed by Northern blotting using a genespecific probe. Which of the following signs or symptoms would most likely occur upon fasting in this child Hypolacticacidemia Ketoacidosis Hyperglycemia Dicarboxylic acidosis Hyperchylomicronemia 3.
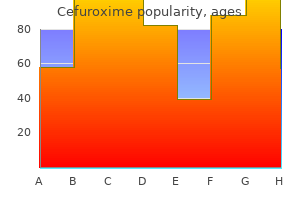
Buy cefuroxime in united states online
Further reading 337 the most common neck mass seen in clinical practice is an enlarged lymph node symptoms when quitting smoking order generic cefuroxime pills. Neck lumps in people over 35 years should be considered malignant unless proven otherwise. Treatment planning for malignant diseases of the neck must be undertaken in a multidisciplinary setting where appropriate expertise is available. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Dysphagia is thought to influence up to 20 per cent of people older than 50, greater numbers of patients admitted to hospitals and even greater numbers admitted to nursing homes. Impairment of swallowing decreases quality of life and can cause significant morbidity and mortality. Dysphagia may arise from the oral cavity, oropharynx, hypopharynx or along the length of the oesophagus. Dysphonia is a disorder of voice, dysarthria a disorder of speech and dysphasia one of language. It is important to understand these definitions to tease out a collection of frequently overlapping presenting symptoms, of which dysphagia is commonly the most important to the patient. Beyond that it becomes the oropharynx containing the posterior third of the tongue, the tonsils and the soft palate. The hypopharynx is directly below the oropharynx and is the widened start of the upper cervical oesophagus that is just posterior to the larynx. Food has to pass through all of these areas; therefore, pathology in any area or combination of areas can result in dysphagia. The epithelium is of the stratified squamous type and houses a rich supply of minor salivary glands. The sensory innervation of the oral cavity is from the mandibular and maxillary branches of the trigeminal nerve, with special sense (taste) to the tongue via contributions of the chorda tympani to the lingual nerve. The motor supply to the muscles of the tongue is via the hypoglossal nerve, and the muscles of mastication are supplied via the mandibular branch of the trigeminal. The oropharynx and hypopharynx are a fibromuscular tube in continuity with the nasopharynx where the tube attaches to the skull base. The tube is formed from three overlapping constrictor muscles with contributions from the stylopharyngeus and palatopharyngeus. The nerve supply to the musculature of the pharynx is via the pharyngeal plexus with fibres from the vagus and glossopharyngeal nerves and a small contribution from sympathetics. The sensory innervation is via the glossopharyngeal nerve to the pharyngeal mucosa and posterior third of the tongue, with some contribution from the internal branch of the superior laryngeal nerves inferiorly. The oesophagus is variable in length and, starting from the lower border of the cricoid cartilage, is approximately 25 cm long, passing through the diaphragm to join the stomach. Along its journey through the mediastinum, it is crossed by the great vessels and left main bronchus, with an upper cricopharyngeal sphincter and a lower sphincter at the gastro-oesophageal junction. The blood supply to the oesophagus is segmental, superiorly supplied by the inferior thyroid arteries, below that by the aorta and bronchial arteries and inferiorly by the left gastric artery. Inferiorly, the innervation is via two plexuses contributed to by the greater splanchnic nerves, sympathetic fibres and the parasympathetic vagus nerves: the submucosal plexus of Meissener and the myenteric plexus of Auerbach, found between the two muscular layers. The mucosa is non-keratinizing stratified squamous epithelium which becomes columnar at the gastro-oesophagal junction. Deep to the mucosa is the submucosa and a muscular tube composed of two layers; a circular and an outer longitudinal muscular layer wraps the mucosa and submucosa. Swallowing can be divided into three phases: oral, pharyngeal and oesophageal, each with its distinct neuromuscular mechanism. The tongue elevates, pressing the bolus against the soft palate and propelling it backwards until it passes through the palatoglossal arch, initiating the involuntary pharyngeal phase of swallowing. The first action in this second phase of swallowing is raising and tensing of the soft palate to close off the nasopharynx and prevent nasal regurgitation. The base of the tongue pushes onto a raised pharyngeal muscular tube as the larynx and hyoid bone rise and closure of the laryngeal inlet occurs. The reflex closure of the larynx is stimulated by the superior laryngeal nerve and is airway protective with rapid adduction of the vocal folds, false cords and arytenoids. The pharyngeal constrictors direct the bolus to the piriform sinuses and posterior pharyngeal wall, and the cricopharyngeus opens to allow passage of the bolus into the upper oesophagus. The third or oesophageal stage of swallowing is involuntary and slower, with the peristaltic wave pushing the bolus to the stomach. Aetiology 341 Investigations for pharyngeal disease are covered in Chapter 18, but the core investigations comprise a contrast swallow, functional endoscopic evaluation of swallow, videofluoroscopy, manometry and cross-sectional imaging. Eating and drinking is of critical importance for patients, as demonstrated by significant psychosocial outcomes and a large reduction in quality of life scores in dysphagic patients. Frequently, dysphagia is complicated by aspiration of food contents requiring cessation of oral feeding; shortterm alternatives of nasogastric feeding tubes or long-term feeding options such as gastrostomy tubes are not popular with patients. This allows early identification of at-risk patients, reduces the risks associated with dysphagia, aspiration and refeeding, and keeps patients swallowing longer with physical therapies and rehabilitation. Congenital, infectious and neoplastic causes of dysphagia are covered in greater detail elsewhere, so they will not be discussed further here. Any history of head or cervical spine trauma, unexplained oropharyngeal bleeding, dysphonia and neck swelling should be included. Examination should include visualization of the upper aerodigestive tract and systematic testing of cranial nerves. Ingestion of caustic substances requires identification of the substance to allow appropriate systemic management in addition to managing the local oral, pharyngeal and oesophageal injury. Careful examination for entry and exit wounds, surgical emphysema and blood-stained secretions should be undertaken, and may suggest a penetrated viscus. Steroids and anti-inflammatory preparations should be enquired about as they may exacerbate symptoms. Examination can be normal, but there may be signs of oedema and erythema, particularly in the posterior larynx. Investigations In addition to a trauma series, tailored cross-sectional imaging of the head, skull base, neck and chest with oral contrast may reveal a mucosal breach or cause for a cranial nerve injury. Should the severity of injury not allow this, a separate contrast swallow at a later date will be helpful. Management Failure of symptomatic improvement despite empirical treatment requires further investigation with an oesophago-gastroscopy to visualize the lower thoracic oesophagus and to exclude hiatus herniation. For cases refractory to these measures, surgery may be appropriate, including fundoplication of the stomach. Management Primary resuscitation of the patient is of paramount importance; thereafter, exclusion of a head or cervical spine injury is mandatory. Synchronous assessment of the airway should be considered, as disruption of swallowing may be an early sign of impending airway compromise. If a perforated viscus is suspected without a vascular injury, then cessation of oral intake, rigid endoscopy when practicable and insertion of a nasogastric tube will inform management. Isolated penetrating injury to the pharyngeal or oesophageal mucosa will heal quickly but should be covered with antibiotics. Caustic injuries frequently affect the distal oesophagus, and after healing, any stricture formation is treated with dilatation. An intermittent history of dysphagia to solids with some aspiration may be found, typically in middle-aged females, although the incidence is declining. Signs and symptoms of iron deficiency anaemia may also be present, including lethargy, glossitis, angular chelitis, koilonychia and pallor. Signs of heart failure and chronic renal impairment may be present in addition to musculoskeletal involvement. Direct or flexible oesophagoscopy may be performed and will aid in excluding the rarely associated post-cricoid carcinoma but may not demonstrate an abnormality. Management Correction of iron deficiency anaemia may resolve any symptoms and the web; for those in whom it does not, then oesophagoscopy and dilatation may be successful.
Quality cefuroxime 250 mg
A 9-week-old boy 9 medications that can cause heartburn purchase cefuroxime line, healthy at birth, begins to develop symptoms of ketoacidosis, vomiting, lethargy, seizures and hypertonia. A child with white-blond hair, blue eyes, and pale complexion is on a special diet in which one of the essential amino acids is severely restricted. A chronically ill patient on long-term (home) parenteral nutrition develops metabolic acidosis, a grayish pallor, scaly dermatitis, and alopecia (hair loss). These symptoms subside upon addition of the B vitamin biotin to the alimentation fluid. Items 10 and 11 A 64-year-old woman is seen by a hematologist for evaluation of a macrocytic anemia. Both homocysteine and methylmalonate were elevated in her blood and urine, and the transketolase level in her erythrocytes was below normal. What is the best evidence cited that the anemia is due to a primary deficiency of cyanocobalamin (B12) Macrocytic anemia Elevated methylmalonate Low transketolase activity Elevated homocysteine Severe malnutrition 11. In response to a B12 deficiency, which of the additional conditions may develop in this patient if she is not treated Substrate and energy source for synthesis of -aminolevulinate in the heme pathway. Converted to glutamate in a reaction requiring the coenzyme form of pyridoxine (B6) 16. A 62-year-old man being treated for tuberculosis develops a microcytic, hypochromic anemia. A decrease in which of the following enzyme activities is most directly responsible for the anemia in this man Cytochrome oxidase Cytochrome P450 oxidase Pyruvate kinase -Aminolevulinate synthase Lysyl oxidase 17. Following a 3-week hospitalization, acute intermittent porphyria was initially diagnosed based on a high level of urinary -aminolevulinic acid. Decreased blood pH and uric acid crystals in urine Decreased blood pH and increased lactic acid in blood Increased blood glutamine and increased orotic acid in urine Increased blood ammonia and increased urea in urine Megaloblastic anemia and increased methylmalonic acid in blood 19. A 69-year-old male presents to his family physician with a complaint of recent onset difficulty in performing activities of daily living. Amino acid degradation Catecholamine synthesis Ganglioside degradation Prostaglandin synthesis Sphingolipid degradation 283 Section I Molecular Biology and Biochemistry Answers 1. Given these symptoms, the defect is in the urea cycle and the elevated orotate suggests deficiency of ornithine transcarbamoylase. Homocysteine, the substrate for the enzyme, accumulates increasing the risk of deep vein thrombosis and disrupting the normal crosslinking of fibrillin. Deficiency of homocysteine methyltransferase would cause homocystinuria, but would also predispose to megaloblastic anemia. Adults with alcaptonuria show a high prevalence of ochronotic arthritis due to deficiency of homogentisate oxidase. Maple syrup urine disease; substrates are branched chain -ketoacids derived from the branched chain amino acids. These children may be blond, blue-eyed, and pale complected because of deficient melanin production from tyrosine. Pregnant woman with megaloblastic anemia and elevated serum homocysteine strongly suggests folate deficiency. Iron deficiency presents as microcytic, hypochromic anemia and would not elevate homocysteine. Macrocytic anemia, elevated homocysteine, and macrocytic anemia can be caused by either B12 or folate deficiency. A distractor may be D, but this would be the cause of a B12 deficiency, not a result of it. Sideroblastic anemia in a person being treated for tuberculosis (with isoniazid) is most likely due to vitamin B6 deficiency. This leads to dopamine deficiency in the brain and results in resting tremors, bradykinesia, cog-wheeling of the hand joints, and rigidity of musculature. The diseases involving amino acid degradation (choice A), ganglioside degradation (choice C), and sphingolipid degradation (choice E) do not match the presentation seen in the case. In the salvage pathways, preformed purine and pyrimidine bases can be converted into nucleotides by salvage enzymes distinct from those of de novo synthesis. These patients also all have hyperuricemia because purines cannot be salvaged, causing gout. Synthesis involves a cytoplasmic carbamoyl phosphate synthetase that differs from the mitochondrial enzyme with the same name used in the urea cycle. The pediatrician started the newborn on a bottle-fed regimen containing folate, vitamin B12, vitamin B6, and iron. This enzyme contains two activities, orotate phosphoribosyltransferase and orotidine decarboxylase. The lack of pyrimidines impairs nucleic acid synthesis needed for hematopoiesis, explaining the megaloblastic anemia in this infant. Orotic acid accumulates and spills into the urine, resulting in orotic acid crystals and orotic acid urinary obstruction. Uridine administration relieves the symptoms by bypassing the defect in the pyrimidine pathway. All three enzymes are targets of antineoplastic drugs and are summarized in Table I-18-1. Also note that: the amino acids glycine, aspartate, and glutamine are used in purine synthesis. However, they have elaborate salvage mechanisms for acquiring purines from the host to synthesize their own nucleic acids to grow. The concentration of free Pi decreases as it may in galactosemia, hereditary fructose intolerance, and glucose-6-phosphatase deficiency. Salvage enzymes recycle normally about 90% of these purines, and 10% are converted to uric acid and excreted in urine. When purine catabolism is increased significantly, a person is at risk for developing hyperuricemia and potentially gout. Lacking both B-cell and T-cell function, children are multiply infected with many organisms (Pneumocystis carinii, Candida) and do not survive without treatment. Experimental gene therapy trials have not yet yielded completely successful cures. Bridge to Pharmacology Thiazide diuretics (hydrochlorothiazide and chlorthalidone) may cause hyperuricemia. Bridge to Pathology Treatment of large tumors with chemotherapeutic regimens or radiation may cause "turnor lysis syndrome" and excessive excretion of uric acid, resulting in gout. Hyperuricemia and Gout Hyperuricemia may be produced by overproduction of uric acid or underexcretion of uric acid by the kidneys. Hyperuricemia may progress to acute and chronic gouty arthritis if uric acid (monosodium urate) is deposited in joints and surrounding soft tissue, where it causes inflammation. Both sources of uric acid are transported in the blood to the kidneys for excretion in urine. Hyperuricemia and gout often accompany the following conditions: Clinical Correlate Gout Acute gouty arthritis, seen most commonly in males, results from precipitation of monosodium urate crystals in joints. The crystals, identified as negatively birefringent and needle-shaped, initiate neutrophilmediated and acute inflammation, often first affecting the big toe. Chronic gout may manifest over time as tophi (deposits of monosodium urate) develop in soft tissue around joints, leading to chronic inflammation involving granulomas. Acute attacks of gout are treated with colchicine or indomethacin to reduce the inflammation. Chronic hyperuricemia, because of underexcretion, is treated with a uricosuric drug (probenecid). These mutations include complete deletions of the gene, point mutations that result in an increased Km for hypoxanthine and guanine for the enzyme, and mutations that cause the encoded enzyme to have a short half-life.
Purchase cefuroxime mastercard
Lack of these intermittent fetal heart rate accelerations usually indicates a fetal sleep cycle medicine 512 cheap 250mg cefuroxime with mastercard. However, many other intrinsic and extrinsic factors, including fetal acidosis, may lead to an absence of these intermittent accelerations in heart rate. Examples include but are not limited to medication exposure, maternal smoking, uteroplacental insufficiency, and fetal structural or chromosomal anomaly. One advantage to evaluation of several different fetal biophysical variables is enhanced specificity of testing with a diminished incidence of delivery for false-positive results. However, the absence of a given marker may be difficult to interpret, because it may simply reflect normal periodicity. The biophysical activities that mature first in fetal development disappear last as acidosis worsens. Given that the first marker to appear in development is the last to disappear with worsening fetal acidosis, the absence of fetal tone has been found to be associated with high perinatal morbidity and mortality rates. Chronic sustained fetal hypoxia or acidosis may produce a protective redistribution of cardiac output away from less vital fetal organs. R edistribution of fetal blood flow may be so profound that renal perfusion decreases to the point that oligohydramnios is established. When the largest vertical amniotic fluid pocket within the uterus is less than 1 cm, the perinatal mortality rate is as high as 110 per 1000. The role o Doppler flow assessment o the etal arterial and venous systems in the prediction o in utero well-being is also accepted. Measurement of umbilical artery velocity is used as a method of fetal surveillance for growth-restricted fetuses. Specifically, decreased or absent end-diastolic flow may appear days before conventional antenatal tests become abnormal. In this procedure, real-time ultrasonography is used to guide the insertion of a needle into the umbilical vein or artery. Samples of fetal blood can be obtained, or, as in the case of red cell isoimmunization, transfusions can be carried out. American College of O bstetricians and Gynecologists: Committee O pinion Number 279: Prevention of early-onset group B streptococcal disease in newborns, Obstet Gynecol 100:1405, 2002. American College of O bstetricians and Gynecologists: Practice Bulletin: Antepartum fetal surveillance. Clinical management guidelines for obstetrician-gynecologists, Int J Gynaecol Obstet 68:175, 2000. American College of Obstetricians and Gynecologists: Practice Bulletin: Clinical management guidelines for obstetriciangynecologists, Number 43, May 2003: Management of preterm labor, Obstet Gynecol 101(5 pt 1):1039, 2003. American Academy of Pediatrics: American Congress of O bstetricians and Gynecologists, and March of Dimes Birth Defects Foundation: Guidelines for perinatal care, ed 7, Elk GroveVillage, Ill, 2012. Bell J, Harvey-Dodds L: Pregnancy and injecting drug use, Br Med J 336:1303, 2008. Burd L, R oberts D, Olson M, Odendaal H: Ethanol and the placenta: a review, J Matern Fetal N eonatal Med 20:361, 2007. The relationship of marginal and decreased amniotic fluid volumes to perinatal outcome, Am J Obstet Gynecol 150:250, 1984. Doria A,Tincani A, Lockshin M: Challenges of lupus pregnancies, Rheumatology 47:iii9, 2008. Ferrero S, Pretta S, Nicolette A, et al: Myasthenia gravis: management issues during pregnancy, Eur J Obstet Gynecol Reprod Biol 121:128, 2005. Clinical management guidelines for obstetrician-gynecologists: obstetric analgesia and anesthesia, Obstet Gynecol 100:177, 2002. Hashimoto K, Kasdaglis T, Jain S, et al: Isolated low-normal amniotic fluid volume in the early third trimester: association with adverse perinatal outcomes, J Perinat Med 41:349, 2013. Soto E, Bahado-Singh R: Fetal abnormal growth associated with substance abuse, Clin Obstet Gynecol 56:142, 2013. Surbek D, Drack G, Irion O, et al: Antenatal corticosteroids for fetal lung maturation in threatened preterm delivery: indications and administration, Arch Gynecol Obstet 286:277, 2012. Tekin A, O zkan S, Caliskan E, et al: Fetal pulse oximetry: correlation with intrapartum fetal heart rate patterns and neonatal outcome, J Obstet Gynaecol Res 34:824, 2008. Tincani A, Bazzani C, Zingarelli S, et al: Lupus and the antiphospholipid syndrome in pregnancy and obstetrics: clinical characteristics, diagnosis, pathogenesis, and treatment, Semin Thromb Hemost 34:267, 2008. Tomson T, Perucca E, Battino D: Navigating toward fetal and maternal health: the challenge of treating epilepsy in pregnancy, Epilepsia 45:1171, 2004. Jimenez-Muro A, Nerin I, Samper P, et al: A proactive smoking cessation intervention in postpartum women, Midwifery 29:240, 2013. Kalidindi M, Ganpot S, Tahmesebi T, et al: Myasthenia gravis and pregnancy, J Obstet Gynecol 27:30, 2007. Kirby R: Maternal phenylketonuria: a new cause for concern, J Obstet Gynecol Neonatal Nurs 28:227, 1999. Maillot F, Lilburn M, Baudin J, et al: Factors influencing outcomes in the offspring of mothers with phenylketonuria during pregnancy: the importance of variation in maternal blood phenylalanine, Am J Clin N utr 88:700, 2008. Motta M, Tincani A, Meroni P, et al: Follow-up of children exposed antenatally to immunosuppressive drugs, Rheumatology 47:iii32, 2008. Odent M: Primal health: understanding the critical period between conception and the first birthday, ed 2, East Sussex, 2002, Clairview. Wong S, Ordean A, Kahan M: Substance use in pregnancy, J Obstet Gynaecol Can 33:367, 2011. If transfer of the mother is not possible because of risk outweighing potential benefit, the objective then shifts to optimizing delivery and birth of the high-risk infant. In the latter situation, it is necessary to have adequately trained professionals to resuscitate and stabilize the infant before his or her transfer to a medical center that has the appropriate expertise and resources. For perinatal transport to effectively support highrisk mothers and their fetuses, as well as sick newborn infants, each country, state, or region must identify its perinatal resources with respect to physical and human capabilities. This review should include classification of levels of care and expertise, as well as mapping of resources as they exist within specific geographic areas. Classification of perinatal resources according to the different levels of care as recommended by the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists in their Guidelines for Perinatal Care5 will direct organization, identification of resources, and roles of patient referral and retrieval centers, as well as reveal the natural elevation of care within the geographic area of question (Table 3-1). Historically, regionalization has been recommended as the most effective and cost-efficient use of perinatal resources. In countries in which universal health care is the norm, regionalization is more easily implemented, whereas in market-driven health care systems in which deregionalization is predominant, these provisions for care become more challenging. Women who are at risk for complications and pose significant risk for adverse outcomes or whose neonates are likely to require intensive care support should be considered candidates for referral during the antepartum period. Once resources are identified and classified, a model for integration of perinatal services may be constructed. Strategic planning at this level will direct the design of the organizational structure of the perinatal transport system, including identification of leadership functions, the different member nurseries/ units and their roles, and the definition and process for perinatal elevation of care. This integration will then allow for the creation of a system for continuous data collection and analysis, facilitating a systems approach to problem solving and the implementation of quality improvement strategies within the system. In G uidelines for perinatal care, ed 7, E G lk rove V illage, Ill, 2012, T A he cadem y. Leadership One proposed model is the implementation of a leadership team that comprises a medical director, administrative director, and quality director. This team approach enables collaborative and timely oversight of the transport system with potential for growth and quality improvement. Me dic al Dire c to r Clinica l Ove rs ight S ta nda rdiza tion of Tre a tme nt Clinica l Ente rpris e Tra ns port Me dica l Control Guide line s for Tra ns port P ra ctice Imple me nta tion of Ne w the ra pie s for Tra ns port in continuous quality improvement, process analysis, and management. In association with the medical director and administrator, the quality director is responsible for the development and maintenance of a transport database for operational management, quality assurance, and analysis. Integral to the regional transport system is the creation of a centralized communication center with a perinatal regional hotline. R oles within this center include referring physician, dispatcher, bed locator, and transport medical control officer (obstetrician and neonatologist). The inclusion of specialized personnel in the initial communication process may support rendering institutions appropriate treatment strategies while decreasing diagnostic discordance. This access should be staffed 24 hours per day, 7 days per week and should be unencumbered. The ability to support communication among the referring physician, the dispatcher, and the medical control officer simultaneously can speed up decision making and the initiation of transport.
Richleaf (Stone Root). Cefuroxime.
- Are there safety concerns?
- Bladder inflammation, edema, headaches, indigestion, kidney stones, stomach problems, some urinary problems, and water retention.
- How does Stone Root work?
- Are there any interactions with medications?
- What is Stone Root?
- Dosing considerations for Stone Root.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96133
Cheap 250 mg cefuroxime with mastercard
Children with significant sleep apnoea will develop poor growth with failure to gain weight treatment viral conjunctivitis discount cefuroxime online american express. This is partly due to difficulty eating a normal diet owing to the obstruction caused by the tonsils and adenoid during swallowing; gagging and choking is a common feature. These children also breathe against an obstruction all night and are effectively exercising to breathe, burning many calories. It is important to explain to parents or patients that tonsillectomy is ineffective in managing recurrent viral sore throats, coughs and colds or ear infections. In older children and young adults without a history of frequent tonsillitis, glandular fever sometimes leads to frequent and recurrent infections in History and examination 535 interferes with the normal release of endocrine growth factors. Where unusual adenoidal enlargement with no infection is present, or where there is smooth asymmetrical enlargement of one tonsil, consider lymphoma. Following imaging, send biopsy material as a fresh specimen to allow full immunohistochemistry. In the United Kingdom, post-streptoccal nephritis is uncommon, but occasionally children are referred by renal physicians for tonsillectomy for this condition. In the United Kingdom, consideration of tonsillectomy would follow two or more admissions to hospital with severe tonsillitis and/or peritonsillar abscess (quinsy). Deep crypts on the surface of the tonsils can lead to trapping of fetid mucosal debris with severe and unpleasant halitosis. Other than gargling to clear the crypts of debris, the only effective remedy is tonsillectomy. Specific attention to nasal obstruction, possible atopy and rhinitis, sleep disturbance and eating are important. Difficulties with speech, articulation and eating may be due to a large adenoid and large, obstructing tonsils. Parents will sometimes bring a video clip of their child sleeping, and this is very helpful supporting information. Enquire about infective episodes of tonsillitis, including the frequency, severity, time off school or nursery and need for medication, both analgesics and antibiotics. A full history of medication, prescribed, over the counter and alternative or complementary is important. If this is suspected, refer to a haematologist for full coagulation and clotting assessment. Examine the external nose, looking for a skin crease in the supra-tip region that may indicate frequent nose rubbing due to irritation secondary to rhinitis, causing nasal obstruction. In children, anterior rhinoscopy is easier using a halogen light auriscope with a large ear speculum. Older children may tolerate nasendoscopy with topical intranasal local anaesthetic spray, such as co-phenylcaine, to assess adenoidal size. It is, however, generally possible to assess the form and size of the tonsils with a bright light and no depressor. Management of type 2 diabetes mellitus should follow local paediatric guidelines for diabetic children undergoing elective surgery. While the image gives only a two-dimensional view of the nasopharynx, reduction of the postnasal airway in the context of the history supports the diagnosis of adenoidal hyperplasia. Safe day case surgery for this group relies on appropriate surgical and anaesthetic skills and techniques, pre-emptive fluid replacement, anti-emetics and analgesia, avoiding narcotic analgesia and emetic anaesthetic. Assessment of the adenoid is made digitally prior to curetting the adenoid from the nasopharynx, and haemostasis achieved with gauze swab tamponade. Techniques employing direct vision have the advantage of reduced blood loss (<4 mL vs. While the microdebrider is faster than curettage, the suction coagulator is significantly cheaper. The Coblator is also suitable for adenoidectomy, but the cost of the device precludes its use unless tonsillectomy is carried out at the same time. Where a bifid uvula is noted or a submucous cleft identified, a partial adenoidectomy, sparing the tissue at the lower part of the nasopharynx, reduces the risk of velopharyngeal insufficiency. Where the tonsils are enormous, it can be helpful to remove these prior to adenoidectomy. If using diathermy or Coblation, care must be taken to avoid burns around the mouth and face. Paraffin or petroleum jelly should never be used as a lubricant for the lips prior to surgery. Both are inflammable, and are a hazard when using diathermy; using these to lubricate the lips may also cause slippage of the mouth gag and risk damage to the teeth. Tonsillectomy may be carried out using cold steel dissection, hot bipolar diathermy, a combination of these or radiofrequency Coblation dissection. Diathermy should never be combined with Coblation because of the higher risk of severe secondary haemorrhage. Diathermy dissection causes less blood loss but is more painful with a slightly higher secondary haemorrhage rate. Coblation tonsillectomy in children is generally a near bloodless procedure, with less post-operative pain, but with the reputation for a higher secondary haemorrhage rate. Some combined Coblation and diathermy in the same patient, resulting in a very high secondary haemorrhage rate. If severe enough to require a return to theatre, diathermy or postnasal packing to the adenoid bed may be required. Secondary haemorrhage should raise the possibility of a clotting or coagulation defect. Following tonsillectomy, the secondary bleed rate is typically between 1 per cent and 4 per cent. While the bleeding may stop spontaneously, return to theatres to arrest the haemorrhage should not be delayed, particularly in a child, where the blood volume (approximately 80 mL/kg body weight) and reserve are correspondingly smaller. Where ties, diathermy or Coblation do not achieve haemostasis, oversewing the faucal pillars may be necessary. Transfusion is uncommonly required, but always establish intravenous access, administer fluids (avoiding dextrose-saline) and send blood for a full blood count and crossmatch at the time of presentation. In older children, particular care is needed, particularly if the secondary incisors have erupted. These incisors are large but the mandible immature, and it is safer to Complications / Adverse drug effects 539 use an adult gag, which will rest lateral to the incisors. When taking consent for surgery, it is mandatory to include a warning about possible damage to teeth. Where there are loose deciduous teeth, take consent preoperatively to remove these under anaesthetic, avoiding the possibility of inhalation during the operation or during recovery from anaesthesia. Routine plain imaging of the cervical spine prior to surgery is not considered necessary in uncomplicated cases. A swab hidden from view may be retained in the nasopharynx, tonsillar fossa or laryngo-pharynx. The nasopharynx should be gently suctioned to clear any clot before removing the gag. It is better to use an angled rose-tipped sucker in the mouth and through the nostrils to clear the nasopharynx. Failure to do so may lead to the clot falling onto the larynx during recovery and causing potentially fatal acute airway obstruction. It may lead to significant problems with hypernasal speech and swallowing, severe enough to cause nasal regurgitation of fluids. It is mandatory to assess the palate and uvula for submucous cleft of the palate prior to surgery, as surgery often unmasks pre-existing palatal dysfunction in a child with a bifid uvula with or without a submucous cleft about to undergo adenoidectomy. Using a direct-vision technique, it is possible to perform a partial adenoidectomy, clearing the choanal airway but leaving the adenoid intact at the velopharyngeal junction. This is more common following suction diathermy adenoidectomy, and many surgeons prescribe a short course of antibiotics, which abolishes this fetor. Rarely, retropharyngeal and mediastinal abscesses may occur as a result of trauma and secondary infection of the adenoid bed.
Syndromes
- Do not smoke. Smoking increases your risk of developing more severe dysplasia and cancer.
- Obesity
- Stomach pain that does not go away after a bowel movement
- Myxedema
- You touch, kiss, or shake hands with someone who is infected by the virus
- How to care for the skin around the tube
Cefuroxime 250 mg sale
The gastrocThere are four principal surgical approaches to nemius is elevated posteriorly to expose the the tibial plateau; the choice of approach is posterolateral corner of the tibia and the dictated by the type of fracture treatment quotes generic cefuroxime 250 mg with amex. The posteromedial incision is made as above, and extended transversely across the popliteal fossa. The medial head of gastrocnemius is retracted or, if necessary, released to allow an extensive submuscular plane to be developed. Direct posterior approach this approach is used occasionally for avulsion fractures at the posterior cruciate ligament insertion or for access to the popliteal vessels, but is not commonly chosen for tibial plateau fractures. Ligation of the medial geniculate branches allows the neurovascular bundle to be retracted laterally. This exposes the posterior joint capsule, which is then divided to expose the knee joint. The fracture and joint surface are exposed, cleared of clot and bone fragments, reduced, and then provisionally fixed and compressed with k-wires and bone clamps. Three or four lag screws with washers, or a contoured, low-profile buttress plate, are then applied to provide compression. The patient can be placed prone, lateral, or supine with the knees flexed over the table edge. Percutaneous screws Simple split (type I) fractures can often be reduced closed by ligamentotaxis. A medial approach is then made and the fracture is reduced and compressed with a buttress plate. Entirely undisplaced medial condyle fragments can be fixed from the lateral side using intraoperative clamp compression and then fixation with a locked plate but, more commonly, double plating through two incisions is required. A separate anterolateral exposure is then performed, and the rest of the plateau is reduced on to this keystone. Frame treatment is principally indicated for management of complications, including infection, malunion and non-union. This allows percutaneous reduction of the fracture under arthroscopic view prior to percutaneous fixation (Table20. External fixation Fine wire frames can be used for complex fractures with severe soft tissue damage. Small arthrotomy incisions are used to reduce the fracture and allow interfragmentary compression screw placement. Complex intra-articular fractures of the lower limb may require 12 weeks of non-weight-bearing. This period is reduced where the fracture is simple, bone quality good and fixation secure, and the patient is a reliable non-smoker. Key point Bicondylar plating through a single midline anterior incision, with the elevation of both medial and lateral flaps, requires significant stripping and may compromise the blood supply to the wound edges and the fracture fragments. It can also be affected by stress fractures in military recruits, runners and dancers. Fractures of the proximal and distal thirds have a different mechanical behaviour from mid-shaft fractures and caution is required when fixing these. The vulnerability of the soft tissue envelope, particularly anteromedially, and the threat of compartment syndrome both require careful consideration. Palpate the dorsalis pedis and posterior tibial pulsations, and mark their locations with ink to allow later reassessment. Consideration should be given to fixing these fractures, even if they are initially undisplaced. The anterior compartment is most commonly affected, so passive plantar flexion of the ankle and toes is unexpectedly painful. Paraesthesia and hypoaesthesia in the distribution of the nerves travelling through the affected compartment. Check the distributions of the superficial peroneal, deep peroneal and tibial nerves. There is most commonly weakness of foot and hallux dorsiflexion (anterior compartment) and foot eversion (lateral compartment). The fracture is normally easy to There may be clear deformity, which should identify but careful attention should be be reduced on recognition. Carefully assess given to the possibility of an intra-articular the integrity of the skin, looking for laceraextension. An anatomical Tibial shaft fractures reduction is not required, but the tibia should be out to length and straight, in neutral rotation, and with no areas of bony prominence under the skin. The thumbs are then used to palpate the subcutaneous tibial crest at the level of the fracture to assess adequacy of the reduction, and to correct any residual translation. Note that a belowknee backslab is insufficient, as it will not control rotation at the fracture (see p. Careful clinical and radiographic monitoring is required to ensure that the fracture does not displace during this period. For example, where there is apex-medial angulation only (normal lateral film), the plaster should remain intact medially. Where there is lateral angulation along with posterior angulation, the apex will be posterolateral, and this is where the plaster should remain intact. Spring the cast open on this hinge by 2 cm, wedging it open with a small piece of cork. A, A mid-diaphyseal fracture in a child, treated in a long-leg cast, has displaced into varus. Open fractures are managed as an emergency or urgently, depending on the degree and nature of contamination present. However, the ankle joint is usually stable and fibula plating increases the stiffness of the construct and the chance of a non-union of the tibia. Surgicaltechniques Most tibial fractures are managed by intramedullary nailing, although plates and external fixators are also used. Concurrent fibular fractures should generally be ignored; they heal well once the tibia has been stabilized. Tibial shaft fractures surgery, without exposure or stripping of the fracture or the periosteum, with a construct that is biomechanically intrinsically very stable (p. Reaming is almost always employed, as it allows the implantation of larger, stronger nails with stronger screws, and is associated with greater union rates than unreamed nails (p. Primary nailing of open fractures after adequate assessment and debridement is usually appropriate. The injured limb rests over a bolster placed behind the distal femur so as not to compress the popliteal fossa. Alternatively, a Denholm pin or wire can be placed through the calcaneus to control the foot. The injured leg rests over a radiolucent triangle, with the foot secured and controlled by an assistant. Reduction It is essential to achieve an accurate reduction during reaming and nailing. If reaming is performed in a malreduced tibia, the nail will follow the same path and leave the tibia malaligned. The application of traction, then rotational correction, is often sufficient to reduce the fracture. It is essential for any technique, even simple external pressure with a mallet, to be maintained until the nail is fully inserted. Continued 462 Chapter20:Tibia Proximal tibial fractures behave differently and the incision may be made over the lateral aspect of the patellar tendon (see below). If the guide-wire position is changed to improve its position on one fluoroscopic view, the orthogonal view must also be checked before proceeding. Threaded guide-wire insertion: After the starting point is checked fluoroscopically, a threaded guide wire is passed into the proximal tibia.
Discount generic cefuroxime canada
Following this back is a way of finding the geniculate ganglion and facial nerve from the middle fossa medications zolpidem order cefuroxime on line amex. External ear 363 the great vessels, especially the carotid in front and internal jugular vein behind, passing from the posterior cranial fossa into the neck. If the physician looks closely, he or she can see a canal within a canal; the tendon for the tensor tympani passes this way also, all worryingly close to the carotid canal. This is composed of skin-covered yellow elastic cartilage but for the lobule, which is purely fatty areolar tissue. The relative safety of piercing the lobe, avoiding cartilage, is obvious to clinicians. The tragus is anterior to the external meatus, a source of cartilage or perichondrium in tympanoplasty. The antihelix is, of course, the fold that can be lacking and augmented in pinnaplasty correction of bat ears. With the oblique lie of the tympanic membrane, the anterior canal is longer, passing into the acute tympanomeatal sulcus. The outer one-third of the canal is cartilage and the medial two-thirds bony, but the two do meet at an angle; hence the need for traction on the pinna to straighten the canal at otoscopy. Only the outer third has wax glands and hair follicles, but defects in the floor, the fissures of Santorini, are notorious routes of infection from necrotizing otitis externa spreading to the parotid and skull base. Deeper in the bony canal are two longitudinal sutures, a challenge to any surgeon in raising an intact tympanomeatal flap. The tympanomastoid and, especially, a well-developed petrotympanic suture line can only be exposed by sharp dissection, if flaps are not to tear. The innervation of the pinna and the external ear canal has some clinical relevance. Hence the vesicles seen in Ramsay Hunt syndrome, the cough on stimulating the ear, the earache of tonsil cancer and the occasional numb pinna after parotidectomy. Its relevance is the proximity of the trigeminal and abducens nerve roots and the rare Gradenigo syndrome. In those with highly pneumatized temporal bones, mastoid sepsis can extend to the petrous apex causing retro-orbital pain and diplopia (due to a lateral rectus palsy) with a discharging ear. This is an anteroposterior dent in the undersurface of the mastoid giving attachment to the posterior belly of the digastric. Follow it forward to the stylomastoid foramen, where the facial nerve exits the skull base. In mastoid drilling, its reversed inner surface, now the digastric ridge (not groove), is a similarly useful landmark for the exit point of the descending facial nerve. The blood supply comes from the superficial temporal and post-auricular arteries, whilst the deep meatus is supplied by a deep auricular branch of the maxillary artery. Its diameter is approximately 1 cm and its area 85 mm2, of which only 55 mm2 is physiologically effective. The pearly grey membrane of the pars tensa will show a light reflex unless inflamed but is generally too opaque to allow clear view of the ossicles, other than the handle of the malleus. A few blood vessels will pass vertically, parallel to and immediately posterior to the handle in health. The joint between the incus and the stapes lies deep to the posterosuperior segment but is rarely evident unless the drum is thinned or retracted onto it. If it is visible, confirming its integrity is fundamental to evaluation of conductive losses. In the same quadrant, the chorda tympani nerve passes from posteriorly, lateral to the long process of the incus and medial to the neck of the malleus. It is at risk of trauma in elevating the membrane for any middle ear exploration, and taste disturbance in the ipsilateral tongue may result. The membrane itself is said to show the elasticity of rubber and is made up of three layers. Superficially is keratinizing squamous epithelium, a curious finding in an area not expected to experience wear and tear. A failure of migration of this keratin is the basis of diseases such as keratosis obturans or cholesteatoma. Atrophic loss of this layer weakens the drumhead and allows retraction pockets and adhesions. Conversely, hyaline degeneration and calcification produce the characteristic white plaques of tympanosclerosis. The tympanic fibrocartilaginous annulus encircles the membrane edge and sits in the corresponding bony sulcus. Superiorly, the middle layer is deficient (but not absent), forming the pars flaccida, easily overlooked by the novice otoscopist but the origin of many a cholesteatoma. Above the level of its superior bony margin, but deeply in the attic, lies the bulk of the ossicular chain, the heads of the malleus and the incus. Unless there is significant bony marginal erosion of the outer attic wall or scutum, these are invisible to the examiner. Indeed, air cells can extend well beyond the mastoid to the petrous apex or into the root of the zygoma, with obvious implications in disease. The cavity is lined with a modified respiratory mucosa that undergoes a transition passing posteriorly. In health, only the most anterior and inferior portions show typical mucociliary epithelium with goblet cells. The dura frequently dips even lower laterally, over the external canal, tending to drive the unguarded surgeon progressively lower in drilling and towards the descending facial nerve. Inferiorly, equally thin bone, which can indeed be dehiscent, protects the bulb of the internal jugular vein from the myringotome, passing deep to the vestibular system. The anterior wall is pierced by the eustachian tube and the canal for the tensor tympani, and laterally lies the tympanic membrane and outer attic wall. The aditus leads into the antrum, but most importantly guides one to that essential surgical landmark, the prominence of the lateral semicircular canal, immediately medial to the short process of the incus. The pyramidal eminence lies on the posterior wall below the aditus and is there to allow the stapedius tendon to insert into the stapes neck. It is, however, also a landmark dividing two vertical grooves, fundamental to the evolution of mastoid surgery. The stapedius muscle is innervated by the facial nerve, and so the trunk, in its descending portion just deep to the pyramid, forms a vertical ridge. The medial wall is what the exploring surgeon encounters and what separates the middle from the inner ear. The first accommodates the stapes footplate, the latter, below it, is less obvious. The true round window membrane lies oblique to the view at tympanotomy, within a deep round window niche. Mucosal folds within this cavity are easily mistaken for the membrane itself, especially by the credulous, when seeking a perilymph fistula. Anterior to both windows is a distinct convex bulge, created by the basal turn of the cochlea, the promontory. A consistent landmark for the geniculate ganglion is the processus cochlearformis, especially as it is relatively resistant to erosion. All books agree on its value in finding the entry point of the facial nerve; few accurately describe how the two relate. Lying in a bony tunnel, it must be slightly more medial than the processus cochlearformis. The facial nerve then passes in the horizontal or fallopian canal, which rarely lacks some dehiscence, especially above the oval window. Passing posteriorly and slightly downwards, it courses superior to the stapes footplate, hopefully not so dehiscent as to challenge footplate surgery. It will now pass inferior to the lateral semicircular canal, towards its second turn or genu. Erosion of the lateral canal by disease is commonly associated with facial nerve exposure (and resulting paralysis) at just this point. Just as the lateral semicircular canal is curving back into the labyrinth, at its posterior end, the facial nerve takes that right angle turn into its descending portion.
Cefuroxime 500 mg sale
Blunt injury: for example treatment 1st degree av block order 250 mg cefuroxime visa, road traffic accident, blow to the neck (contact sports) or strangulation. It is important to appreciate that even in the absence of any external signs, internal laryngeal injury may still have occurred. These chemicals cause burns to the upper airway, producing oedema, mucosal haemorrhage and ultimately tissue loss. This chapter will focus on external trauma, but the principles of management of the airway remain the same for inhalation injuries to the larynx. Initially, the larynx is compressed against the vertebral column and is fractured along the prominence. This will lead to further swelling, bleeding and possible tissue fragments emerging into the laryngeal lumen. A simple way to understand blunt airway emergencies is to consider the larynx as a box. Trauma causes swelling, which will occur inside the box, thus reducing the airway. In such cases the vocal cords roll back on themselves and the epiglottis may fall back into the airway. It is imperative to note that with trauma to the larynx and trachea, other structures may be injured. This is an important issue as laryngo-tracheal injuries may be underdiagnosed in the presence of multiple traumas where other presenting injuries may overshadow that of the upper airway, which can lead to serious consequences for the patient. The force and mechanism of trauma will dictate the injuries; this may be purely oedema, which typically reaches its maximal peak around 12 hours after the injury. These patients may have mild dysphonia and possibly neck pain (secondary to the trauma) as their only presenting symptoms. Coughing can also occur owing to damage to the internal larynx and secretions such as blood. Pain in the region should also alert the clinician to a possible laryngeal fracture. Signs of upper airway trauma are bruising, tenderness, surgical emphysema, deformed contour of the laryngeal framework and granulations over injured cartilage. Bleeding into the laryngeal lumen may occur, along with fragments (such as cartilage) protruding into the lumen, and oedema. Oedema develops over time (minutes to hours), so symptoms on first presentation may not indicate how perilous the airway may become. If it is deemed safe (see later discussion), then the airway should be inspected using flexible transnasal laryngoscopy, which should be done by an experienced otolaryngologist. As these patients often have multiple injuries, it is essential to include examination of other viscera in the neck. It can be appreciated that any blood, cartilage, oedema or disruption such as arytenoid dislocation will narrow this lumen, producing symptoms such as stridor, dyspnea and altered voice. In cases with minimal oedema on laryngeal examination, a course of intravenous steroids with observation on a high-dependency ward is a reasonable course of management. Use of cricoid pressure to help view at intubation is contraindicated to an already disrupted larynx. First, patients who are conscious will try to maintain their own airway, but if given sedative medication they may not, which then poses a risk of losing the airway in cases of failed attempts to intubate. Surgical emphysema is a cardinal sign of airway breach and must be investigated carefully. In these cases intubation may worsen the anatomical injuries along with worsening the situation if it fails. As a general principle patients with mild to moderate injuries should be transferred to the operating theatre where an experienced anaesthetist should try to intubate the patient in the presence of an otolaryngologist prepared to perform an emergency tracheostomy should intubation fail. In the case of a high-velocity injury (severe trauma) where the larynx has been split or shattered, there is a definite argument for tracheostomy under local anaesthetic being the first line management of the airway. In patients where there is any doubt to the state of the airway and symptoms are increasing in severity, a secure airway via intubation is a priority with a low threshold for tracheostomy. Once the airway has been secured and any scans have been undertaken, the patient can and should then undergo suspension micro-laryngoscopy and rigid pharyngo-oesophagoscopy to assess the extent of injuries. Hence patients with these injuries are more readily intubated and taken to theatre where exploration and direct closure of tracheal and laryngeal injuries are performed. These patients usually have exquisite pain on swallowing, and an internal inspection of the larynx should be performed to delineate other injuries. This will cause malunion and may need excision, although this would be at a later stage as an elective procedure. This should be treated by open reduction and fixation with (mini) plates or wire if needed. Any associated soft tissue injuries to the larynx should be repaired if possible (including mucosal tears), and, if necessary, vocal cords that have lost attachment anteriorly to the thyroid cartilage should be re-suspended. It is important to cover exposed cartilage with mucosa or perichondrium to minimize granulation tissue formation and long-term scarring. Any degree of displacement should be reduced and fixed; otherwise, impaired function will ensue. In cases where webbing is likely, adhesions forming between two areas on either side of the laryngeal lumen, a stent can be sutured into position with a covering tracheostomy. The stent should be removed in theatre typically after 10 to 14, days and the patient can often be decannulated (tracheostomy removed) at the same time. These injuries need to be corrected as soon as possible (ideally within 48 hours); otherwise, longterm sequalae are more likely. However, such injuries need to be treated with great respect and experienced airway practitioners sought as soon as feasibly possible. These patients may have little to no airway signs at the site of trauma, and other coexisting injuries, such as overt bleeding from a chest injury, may occupy the minds of the treating team. It may not be apparent an upper airway injury has occurred until symptoms from laryngeal oedema develop some hours later or the patient fails extubation after successful surgery on another anatomical site. In contrast, other patients may have marked symptoms, such as stridor at the trauma scene, and will require swift, decisive and often courageous attempts by non-airway specialists to secure the airway as a matter of urgency. Once the airway is secured and anatomical injury has been assessed and dealt with, these patients can still have lifelong morbidity in a personal, social and employment setting from necessitating long-term tracheostomy or voice disorders. The acute dangers and potential great morbidity from such injuries necessitate a team approach by experienced practitioners with a good understanding of the diagnosis and treatment of laryngotracheal injury. Early treatment comprises securing the airway and giving consideration to the voice. Early appropriate intervention is generally recommended to minimize long-term adverse sequelae including laryngeal scarring and subglottic stenosis. Patients with laryngeal trauma can have long-term problems with phonation and breathing, ultimately needing tracheostomy. Inability to protect the airway (aspiration) may also mean long-term tracheostomy. These patients may have a narrower airway, either owing to structural damage or vocal cord palsy as a result of trauma to the recurrent laryngeal nerve. Management of subglottic stenosis is challenging and should be done in specialized centres. A tracheostomy implies that this opening has a connection to an opening in the skin, i. The early operations were associated with a very high mortality and became an established technique only in the nineteenth century when a large number were performed on patients suffering from diphtheria. The overall literature on the procedure is extensive, and a significant percentage deal either with a paediatric population or with percutaneous procedures. This chapter will discuss tracheostomies that can be temporary and reversed/closed if required and will deal with the technique as it applies to an adult population. The chapter will not discuss the permanent, non-reversible tracheostomy that is performed as part of a laryngectomy. This chapter should be read in conjunction with Chapter 59 on paediatric tracheostomy. These include the lamina of the thyroid cartilage, usually easily identified in the central compartment of the neck by an obvious notch on its superior border. Inferior to the thyroid lamina is the crico-thyroid membrane and, in turn, the cricoid cartilage. The trachea is attached to its inferior border and is a cartilaginous/membranous tube extending into the mediastinum and bifurcating at the carina.