Claritin 10 mg with mastercard
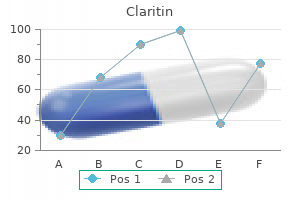
The extent of the reflection and length of vertical releasing incisions should be noted allergy forecast huntington wv generic claritin 10 mg overnight delivery. The alveolar mucosa is not incised, and great care must be taken to avoid cutting or perforating the entire mucoperiosteal flap. Once the periosteum is cut, the flap can be extended enough to cover the membrane and graft. This is a technically difficult procedure, but it is one that should be mastered to avoid exposing the membrane. It is generally reserved for teeth where surgical access would be difficult, non-healing lesions, or patient limitations that prevent conventional root-end surgery. Access to the apices of this tooth is extremely challenging because locating and instrumenting through a deep tunnel in bone is very demanding. Anatomic limitations include a mandibular premolar that is in very close proximity to the mental foramen and mandibular molars that are in very close proximity to the inferior alveolar canal [146]. Perforations in areas not accessible surgically include the proximal surface of tooth in the interdental area or in a furcation [146]. Patient management and limitations can prevent disabled patients from being able to undergo endodontic microsurgical procedures or to maintain the position required for the surgeon to use the microscope. It is important to explain the procedure to the patient and to present the risks and benefits of the procedure. The risk of fracture and resorption should be explained, as well as the understanding that if the procedure is not performed the tooth would probably have to be extracted. Teeth with fused roots are generally good candidates, unless they have interseptal bone. Teeth with straight roots and a furcation where bone is present are good candidates. The occlusal surface of the tooth should be relieved, so the tooth has little or no occlusal contact. A sterilized rubber band is placed over the handle of the extraction forceps, ensuring the forceps beaks will stay closed once the tooth is extracted. This allows the tooth to be held in the forceps for the entire procedure while the tooth is out of the mouth [146]. Elevators and periotomes should not be used to elevate against the root of the tooth. Likewise, the beaks of the forceps should be kept off of the cementum on the root above the cementoenamel junction. This increases the chance of fracture of the crown during extraction, but it decreases the chance of resorption developing later. It is important to be patient during the extraction, because expanding the cortical plates of bone is a slow and deliberate process. If there is a cyst or granuloma attached to the root and it comes out with the tooth, the socket does not need to be curetted. Even if granulation tissue remains in the socket, nothing should be curetted from the socket. Due to the root-end resection and the expansion of the cortical plates of bone, it is generally easy to replant the tooth. Once the tooth is back in the socket, the facial and lingual (or palatal) cortical plates of bone are compressed and the patient is asked to bite on a cotton roll or a wooden stick to insure the tooth is seated properly and stabilized [146]. The tooth should be in minimal or no occlusion; however, slight occlusal function will speed healing. If splinting is required, it should be minimal, such as sutures crossed over the occlusal surface, or a periodontal pack [146]. Borrowing from the dental traumatology literature, a flexible splint produces the best outcome [149]. To be consistent with dental traumatology guidelines [149], tetracycline, penicillin, or amoxicillin for one week should be prescribed to help prevent inflammatory resorption, although definitive human studies are lacking on their benefit. The patient should follow a soft dental diet for one to two weeks and should be instructed in home oral hygiene care to keep the area clean. Other negative outcomes include periapical rarefaction due to periapical inflammation, chronic pain, or fracture of the crown or root [146]. Fortunately, there is a favorable outcome in most studies, although the success rates and techniques are varied. Root amputations and hemisection techniques in endodontics Although the topic for root amputations and hemisections of molars are now less common due to the success of osteointegrated implants, there are still cases when these techniques are the best option for a patient. The defective or periodontally involved root and that part of the crown are then removed. Bicuspidization is the surgical division of a mandibular molar (as in a hemisection), but the crown and root of both halves of the tooth are retained. Teeth requiring root resections, should have adequate endodontic treatment before the root resection. The root canal in the root to be resected should be filled with either amalgam or a composite resin to the level where the resection will be made. Gutta-percha does not provide an adequate seal in the resected root because it will be exposed to oral fluids. It is essential that there is a restorative plan for the proper coronal restoration of teeth undergoing respective procedures. Mandibular molars that require resective treatment should almost always only be treated by hemisection or bicuspidization, because a root amputation leaves an unfavorable leverage situation on the remaining root and will lead to fracture of the tooth [156]. The adjacent teeth mesial and distal to the affected tooth have large restorations that might warrant a three-unit fixed bridge. There are patient risk factors such as poor plaque control, or the patient is a smoker.
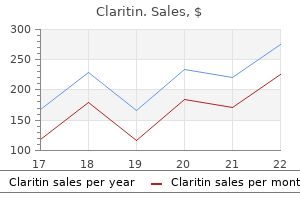
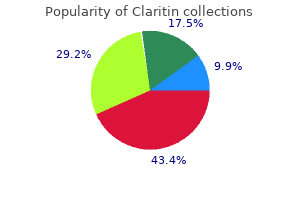
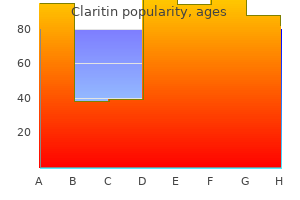
Cost of claritin
It remains to be established whether viral infections (herpes zoster and other viruses) can initiate endodontic pathosis in the absence of bacterial infection allergy forecast wilmington nc purchase claritin pills in toronto. As noted in Chapter 8, the exact nature of viral involvement in pathogenesis of periapical lesion development is also poorly understood and data on the association of viral infections with pathogenesis of endodontic pathosis are equivocal at this time (Jakovljevic and Andric 2014; Jakovljevic et al. Carrier or heterozygous state is expressed as sickle cell trait and is much milder in its clinical presentation. Sickle cell anemia is characterized by sickle shape of the red cells due to substitution of a single amino acid-valine for glutamic acid-at the sixth residue of the chain of hemoglobin (Little et al. Interestingly, sickle cell anemia tends to be prevalent in communities and countries where malaria (which results from infection by the parasite Plasmodium falciparum) is endemic, such as central African countries. It has been shown that this type of anemia confers protection against malaria by reducing adhesion of parasite-infected erythrocytes to endothelial cells of the microvasculature of the brain and other organs, which causes the life-threatening complications of malaria (Cholera et al. Two case series have been reported in which sickle cell anemia seemed to be involved in the pathogenesis of pulpal and periapical disease. One study showed that patients with systemic allergies were more likely to have endodontic flareups than patients without allergies (Torabinejad et al. In another study, patients undergoing bone marrow transplantation and who had asymptomatic periapical lesions in relation to endodontically treated teeth were divided into two groups. In one group, retreatment, root-end resection, or extraction was performed while the control group had no treatment carried out before the bone marrow transplant. The dependent variables were number of days in the hospital with neutropenia (<500/mL) or elevated temperature (>100 F). The results showed no significant differences between the two groups (Peters et al. With respect to long-term outcomes, in one study 66 patients, who had normal or immunocompromised medical status, were followed for a minimum of 30 months (Marending et al. The study showed that endodontic treatment outcome was significantly dependent on whether they were in the normal or immunocompromised group. Conversely, another study examined the effects of osteoradionecrosis on endodontic treatment outcomes (Lilly et al. In this study, endodontic treatment of 22 patients was performed on teeth in the area of irradiation with a mean of 5000 cGy within the previous 6 months. The study showed a success rate of 91%, which was consistent with that of other endodontic outcome studies of noncompromised patients. Locally invasive neoplasms such as ameloblastoma, which arises from odontogenic tissues, like other jawbone radiolucencies, may present in close proximity to teeth, thus mimicking the presentation of endodontic infections. In this context, it is of interest that primary neoplasms have rarely if ever been reported in the dental pulp. Reports have been published of metastatic neoplasms in the maxilla or mandible, causing radiolucent lesions, occasionally with invasive resorption of the root, pain, parasthesia, including numbness. While the tooth root and pulp may be affected in these situations, clearly, proper diagnosis and appropriate corrective therapy, which may include endodontic therapy, must be performed in consultation with the treating physician or surgeon. Examples of these neoplasms include those that arise in the lung, prostate, breast, pancreas, or colon. More recently, it was shown that inoculating the pulp space of mice with Porphyromonas gingivalis, isolated from a patient with 396 Endodontic Microbiology persistent endodontic infection, caused translocation of the organism to the placenta, systemic inflammation, and premature birth (Ao et al. Another group showed that pregnant rats developed not only systemic inflammation, but also insulin resistance when periapical lesions were induced (Bain et al. Finally, selective serotonin reuptake inhibitors, commonly used for the treatment of depression and anxiety, have been shown to mediate bone resorption, and were recently shown to interfere with the healing of implants (Wu et al. Another category of patients at risk of osteonecrosis, particularly following surgical procedures, are patients on intravenous bisphosphonates. Bisphosphonates interfere with osteoclast action, thereby reducing bone resorption. Animal studies have shown that bisphosphonates reduce periapical lesion size (Xiong et al. The risk of osteonecrosis with oral bisphosphonates is significantly reduced, compared to intravenous drugs. One study showed no effects of oral bisphosphonates on the outcome of nonsurgical endodontic treatment (Hsiao et al. In one review it was shown that they cause osteonecrosis following implant placement in about 2% of cases (Boquete-Castro et al. In a rodent model, these drugs were shown to cause osteonecrosis during the pathogenesis of periapical lesions (Aghaloo et al. In addition to their cholesterol-lowering properties, statins have been known for a long time to have osteoconductive properties. A recent animal study showed that simvastatin reduced the size of induced periapical lesions in a rodent model (Lin et al. In patients, statins have been linked to pulp canal calcifications, thereby fostering their association with mineralization of hard tissues (Pettiette et al. Likewise, metformin (a hypoglycemic agent commonly used for the treatment of type 2 diabetes) reduced periapical lesion size in animal models (Liu et al. Genetic variations generally refer to differences in the phenotype of the host that are related to their gene expression and follow the Mendelian pattern of inheritance. These variations may allow an inflammatory mediator, a growth factor, or a receptor to be over- or underexpressed, thus leading to a variation in the pathogenesis of disease or the rate of healing. Several other gene polymorphisms have been studied, and showed less prominent or no associations with postoperative responses to endodontic treatment (Aminoshariae and Kulild 2015). In this study, periapical granulomas and cysts had significantly higher methylation of this gene than gingival controls, indicating that Endodontic Infections and Systemic Disease 397 methylation has an important role in the suppressive activity involved in chronic periapical lesions. In developing countries, and regions in industrialized countries where there is limited access to dental care, these types of infection are seen with some prevalence and contribute to numerous hospital emergency room visits. The literature contains several reports of spreading endodontic infections to cause mediastinitis (Garatea-Crelgo and Gay-Escoda 1991; Bonapart et al. He then developed a brain abscess and was treated for 6 weeks in a hospital emergency room, but eventually died as a result of complications of this condition. Therefore, it is clear that endodontic infections can result in spreading, life-threatening, infections. Routine acute endodontic infections, which are seen frequently in dental and endodontic practices, may result in a number of signs and symptoms of systemic inflammation, albeit with less morbidity. These include fever, malaise, regional lymphadenopathy, anorexia, somnolence, accelerated degradation of skeletal muscle proteins, hypotension, and hepatic synthesis of a number of proteins such as complement and coagulation proteins (Kumar et al. Like other types of acute infections, these infections may also result in leukocytosis and increased erythrocyte sedimentation rate. All investigated acute phase proteins decreased significantly 3 months after treatment (Marton et al. There 398 Endodontic Microbiology are several other markers of systemic inflammation such as proinflammatory cytokines. Elevated systemic antibodies (immunoglobulins) indicated exposure to bacteria (oral and otherwise). A recent systematic review and meta-analysis examined the association of 31 systemic molecular markers with apical disease (Gomes et al. Meta-analysis showed that serum levels of IgA, IgG, and IgM were significantly increased in humans with apical periodontitis compared to healthy controls. More recently, it was shown that men and women with periapical lesions may have different expressions of markers of cardiovascular disease (Cotti et al. It appears that extrusion of bacteria occurs whether or not the instruments in the necrotic pulp cases are maintained within the canal or extend past the working length (Debelian et al. A study showed that the instrumentation itself appears to be causative of an increase in the incidence of bacteremia perioperatively, compared to preoperatively (Savarrio et al. It is of interest in this study that instrumentation of cases with vital pulp resulted in no bacteremia, and that the incidence of bacteremia was not different in patients with primary or persistent endodontic infections. Preoperative bacteremia in patients with chronic infections was found in only 7% of all cases (Savarrio et al.
Claritin 10mg
Although this view is particularly valuable in assessing for pericardial effusion allergy vaccine order 10mg claritin free shipping, it has limited utility in estimating ejection fraction. Subxiphoid View of the Heart 702 Although the apical view yields a rather complete and anatomically familiar representation of the heart, it can be the most difficult of the three primary windows to obtain consistently. Direct the indicator toward the bed, rotating toward the left axilla to sharpen the image. Apical View of the Heart 704 Pericardial Effusion the detection of a hemodynamically significant pericardial effusion may be the most important and timely diagnostic appraisal to be made in a critically ill patient. The signs and symptoms of pericardial effusion (and even tamponade) may be clinically occult. The incidence of the abnormality in patients presenting with dyspnea can be as high as 14%; roughly 4% of emergency department patients with dyspnea have symptomatic effusions. The physician can synthesize the clinical picture with echocardiographic findings to determine the significance of this abnormality. Such a dark fluid collection posterior (far field) to the pericardial stripe indicates a pleural effusion, a "masquerader" of pericardial effusion. In the subxiphoid view, an effusion often appears as an anechoic stripe anterior (near field) between the liver and the right ventricle and is surrounded by the bright white of the pericardium. Note that fluid collects posteriorly in the dependent area, the most common site for effusions in this window. The effusion appears anterior to the unlabeled dark circle (the descending thoracic aorta), a clue that this is a pericardial (rather than pleural) effusion. Generally, an effusion is dark (if it is fresh blood) or has a mixed density (if it contains clotted blood). Ejection Fraction Left ventricular function should be assessed in critically ill patients because it can reveal the cause of the illness and provide prognostic information to guide fluid therapy. During sepsis, cardiac dysfunction can develop in those who had normal cardiac function at baseline. Fluid resuscitation guided by echocardiographic findings is endorsed in the Surviving Sepsis Campaign protocol. Most clinicians prefer to estimate ejection fraction by visually assessing the left ventricle, as opposed to eliciting a more timeconsuming series of measurements from static images or "cine" extrapolations. The left ventricle is described as hyperdynamic when its walls appear to nearly touch in systole and are relatively small compared with the chamber itself (indicating poor ventricular filling). An anterior mitral valve leaflet that "slaps" up against the septum usually indicates normal left ventricular function. An anterior mitral valve leaflet that does not come closer than 7 mm to the ventricular septum represents significant depression. This measurement can be easily obtained by less-experienced sonographers and correlates well with visual estimates of left ventricular ejection fraction made by those well versed in echocardiography. For a significantly depressed ejection fraction, especially when pulmonary edema is evident, aggressive fluid resuscitation should be limited and applied with close observation. Consider vasopressor therapy and the early addition of inotropic agents to support cardiac and pulmonary function. The finding of a hyperdynamic heart is particularly valuable, as it suggests that the patient might benefit from volume resuscitation. Dynamic measurements of ventricular ejection fraction and cardiac output generally are beyond the limited echocardiographic studies performed in the acute setting; however, they are described in this chapter to provide a complete scope of practice. Right Ventricular Strain 710 Echocardiography is not a substitute for lung imaging in the diagnosis of pulmonary embolism because no sonographic finding is sufficiently specific for the disorder. After excluding tamponade and more readily assessed causes of circulatory compromise such as tension pneumothorax, a bedside echocardiogram can provide evidence to suggest a hemodynamically compromising pulmonary embolism. Data suggest that the imaging modality can accurately assess right ventricular strain in the acute setting. This manifests in several ways, including increased right ventricular size and wall-motion changes. In cases of of acute right ventricular strain, the right chamber enlarges and may equal or exceed the size of the left ventricle. The echocardiographic windows most valuable for this comparison are the apical, subxiphoid, and parasternal views. Excessive right ventricular strain causes dilation and hypokinesis of the right ventricle. In the setting of pulmonary embolism, the classic finding of hypokinesis of the right ventricular freewall with sparing of the right ventricle apex (McConnell sign) may be more suggestive of acute pulmonary embolism as distinct from other causes of chronic right ventricular strain. The left ventricle (arrow) has bowed in response to the pressure differential between the right and left ventricles, the so-called "D sign. Even normotensive patients with these findings have a significantly higher risk of inpatient mortality and shock related to the embolism. An ischemic myocardium can have a variety of appearances, described as hypokinetic (decreased systolic thickening), akinetic (no systolic thickening), or dyskinetic (outward bowing of the wall in systole). These findings can occur globally, as in diffuse cardiomyopathy, or segmentally, as in a singularly compromised vascular territory. Sonographers can get their 713 bearings by first locating the interventricular septum, using this landmark to identify other areas of the myocardium. From the septum, the transducer can be scanned toward the right shoulder and then toward the left hip, panning through the entire left ventricle. Thoracic Aorta Examination A thoracic aortic dissection can be identified rapidly with close inspection of the descending artery. Critical bedside diagnoses have been described in an increasing number of case reports. The addition of color flow enables the study of blood flow relative to the dissection flap. Features suggestive of aortic dissection include an intimal flap or dilated aortic root (>3. Descending thoracic aorta; circled hypoechoic area with hyperechoic, mobile, linear dissection flap (arrow). The boxed area includes the aortic outflow tract and somewhat dilated aortic root. Recent debate, especially in the sepsis literature, has elaborated on the concept of fluid responsiveness - defined as the likelihood that cardiac output (and therefore perfusion) will increase in response to volume infusion. The differential diagnosis includes massive pulmonary embolus, tamponade, significant pulmonary hypertension, volume overload with cardiac dysfunction, restrictive heart disease, intrinsic positive end-expiratory pressure, tension pneumothorax, and any cause of elevated intrathoracic pressure. Lung Examination Emergency and critical care physicians increasingly are using ultrasonography to evaluate lung pathologies. The most established applications include detecting the presence of lung sliding, excluding pneumothorax or an unventilated lung (as with mainstem intubation), and imaging the costophrenic angles to reveal pleural effusion. Parenchymal lung processes such as pulmonary edema (and other causes of interstitial fluid, including pulmonary contusion and acute lung injury) and pneumonia can be readily identified by bedside ultrasound. Pneumothorax is routinely diagnosed via chest radiograph; however, this approach can be time-consuming and insensitive. Although x-ray remains the best means for confirming pneumothorax size, ultrasonography also can make such predictions when the lung point can be seen. These lower-frequency tools allow deeper penetration and imaging of lung parenchyma at the expense of detail. A linear transducer may be preferable when performing a focused examination for pneumothorax. Beginning at the second or third intercostal space, visualize the bright, hyperechoic pleura between the ribs (the ribs appear as bright, semicircular surfaces with shadowing distally). Image the lung in at least three interspaces, bilaterally, while focusing on the location in which a pneumothorax might be expected (ie, the highest-altitude area of the chest, where air would collect), and where the pain is most concentrated. Depending on the clinical situation, this examination also may be performed as part of a more comprehensive lung protocol, employing curvilinear or phased-array transducers. A normal lung rapidly dissipates echoes and therefore does not provide an image that can be clearly resolved by ultrasound. Side-to-side movement of the bright pleural interface or lung artifacts, as in B-lines (arrows); rib shadow (R). Additionally, horizontal, hyperechoic lines that arise at regular intervals from the pleural line are called A-lines. A progressive disappearance of A-lines occurs with increasing lung density, as may be the case with various types of lung pathologies.
Generic claritin 10 mg visa
The introduction of a premixed sealer eliminates the potential for heterogeneous consistency during mixing allergy forecast iowa city discount claritin 10 mg without a prescription. When the sealer is placed in the root canal, the material absorbs water from the dentin tubules, causing a hydration reaction of the dicalcium silicate and tricalcium silicate. Calcium phosphate reacts with calcium hydroxide at the same time to precipitate hydroxyapatite and water. This water continues to be used for the hydration of the calcium silicates and leads to the formation of a composite network of gel-like calcium silicate hydrate, which mixes with the hydroxyapatite bioceramics and forms a hermetic seal inside the root canal. A study on bioceramic sealer showed that even if the sealer extrudes out of the canal, the patient might not experience any pain as compared to other conventional sealers, because the sealer hardens to form hydroxyapatite, which is osseoconductive [23]. This hydroxyapatite has the ability to expand and harden inside the canal, which helps to create a perfect seal with the walls. Conventional retreatment techniques can be used to remove this sealer when it is used in combination with gutta-percha, but Hess and colleagues [24] observed in retreatment cases that removal of bioceramic sealer using solvent and a rotary instrument and reaching the correct working length was not easy, and patency was gained in only 20% of their experimental samples. It produces calcium hydroxide, which is released in solution and produces an interstitial layer that resembles hydroxyapatite structures in simulated body fluids. Being an entirely inorganic material, Portland cement undergoes chemical shrinkage following hydration. Its role as a sealer where it adheres well to dentin and obturating material, its cohesive strength, wetting properties, low viscosity, cytotoxicity, and biocompatibility were later compared to other sealers. Most experiments are laboratory based or in animal models, which may differ from a clinical scenario. The major components are tricalcium silicate and dicalcium silicate, with inclusion of calcium sulfate as setting retardant, bismuth oxide as a radiopacifier, and a small amount of tricalcium aluminate. Tricalcium aluminate is necessary for the initial hydration reaction of the cement. The liquid part consists of viscous aqueous solution of a water-soluble polymer to improve the workability and flow. The powder consists of fine hydrophilic particles that form a gel in the presence of moisture. The main constituents are tricalcium silicate, tricalcium oxide, and tricalcium aluminate. The most significant difference is the presence of large amounts of calcium carbonate, which is intended to increase the release of the calcium ions and improve the adhesion to the dentinal walls with adequate flow and biocompatibility. But Fillapex (Angelus Odonto) Fillapex is a recent introduction; it is made of two pastes. It delivers easily and exhibits excellent handling characteristics and an improved setting time. Salicylate resin is tissue friendly and therefore a better choice over epoxy-based resins. The two pastes combine in a homogeneous mix to form a rigid but semipermeable structure. It exhibits an alkaline pH, has a good flow rate, has an ideal working time of 35 minutes, is antimicrobial, and has a low film thickness to easily penetrate into the accessory canals. This sealer demonstrated stable leakage values at 15 and 30 days and good sealing ability. However, at 60 days, the material exhibited a considerable increase in leakage and low flow rate. This helped in increasing the sealing ability of the sealer due to greater expansion achieved. Fluoride ions can penetrate into the dentin and enhance the mineralization of the dentin. The setting reaction involves the continuous formation of hydration products that contribute in reducing the microchannels in the sealer. The pH is increased up to 12 and may play a protective role in preventing bacterial recontamination of a filled root canal. There are two prerequisites for the monoblock to function as a mechanically homogeneous unit. First, the materials that constitute the monoblock should have the ability to bond strongly and mutually to each other, as well as to the substrate that the monoblock is intended to reinforce. Second, these materials should have a modulus of elasticity that is similar to that of the substrate. Monoblocks in the root canal spaces may be classified as primary, secondary, or tertiary depending on the number of interfaces present between the bonding substrate and the bulk material core. A classic example of primary monoblock would be obturating the root canals with gutta-percha without using the sealer. The lack of sufficient strength and stiffness is the major drawback, and this led to the development of secondary monoblocks. Secondary monoblock Conventional sealers do not bond strongly to dentin and gutta-percha; therefore, gutta-percha does not form a monoblock, even with the use of a resin-based sealer. Although glass ionomer cements and resin-modified glass ionomer cements bond to root dentin and have been marketed as root canal sealers, they do not bond to gutta-percha [35, 36]. The combined use of a sealer and a core material introduces additional interfaces into a monoblock during obturations. Secondary monoblocks have two circumferential interfaces, one between the cement and dentin and another between cement and the core material. A classic example is the use of sealer for obturation, wherein one interface is between the gutta-percha point and sealer and the second one is between the sealer and the root canal wall. Their bondability to the radicular dentin and root canal materials is also superior compared to other cements. However, the monoblock concept is explained first for better understanding of their setting reaction. Monoblock concept the term monoblock, meaning a single unit, has been employed in dentistry since the turn of the century. Tertiary monoblock A third circumferential interface is introduced between the bonding substrate and the abutment material by coating the nonbondable gutta-percha with materials that make them bondable to the sealers, thus creating tertiary monoblocks. Because the tertiary interface exists as an external coating on the surface of the gutta-percha, such systems are designed to be used with either a single-cone technique or placement of accessory cones without lateral compaction, to avoid disrupting the external coatings. Fiber posts that contain an external silicate coating or nonpolymerized resin composite for lining root canals that are oval or not perfectly round or wide so that the fiber post can be fitted properly are considered a tertiary monoblock. Challenges with monoblocks Although the idea of creating a mechanically homogeneous unit with root dentin is excellent in theory, accomplishing these ideal monoblocks in the root canal space is challenging, because bonding to dentin is compromised by volumetric changes that occur in resin-based materials during polymerization. There appears to be no adhesive root canal material that can perfectly obturate the canal space with a tight seal that consists of different interfaces, simultaneously improving the fracture resistance of the tooth. Even when the effect of dentin permeability in endodontically treated teeth is minimal, entrapment of residual moisture within the root canal can result in the permeation of this unbound water through hydrophilic adhesive layers [37, 38]. This can work as stress raisers and promote crack growth and propagation during loading along the interface. The highly unfavorable and complex geometry of the substrate, namely root canal space, also proves to be detrimental to the polymerization of the resin cements or sealers. However, continued research and development is carried out and is likely to result in improvements. However, all the root canal filling materials available today have a modulus of elasticity that is far less as compared to dentin. Though it demonstrated ease of application, antibacterial properties, and adaptability to the canal wall, adverse inflammatory reactions and leakage issues were also observed [39, 40]. The generation of an endodontic seal is dependent on the penetration of the hydrophilic sealer into the dentinal tubules and lateral canals following removal of the smear layer. Although both the tensile bond strength and apical seal to intraradicular dentin may be improved using a dual-cured self-etching primer/adhesive, there is still a potential problem of rapid polymerization of the adhesive in an environment with reduced oxygen concentration [44, 45].
Discount claritin online amex
Adverse effects include nausea allergy treatment products purchase claritin without prescription, emesis, hypokalemia, and inconsequential hyperglycemia. The use of adrenergic agents such as dopamine, epinephrine, and isoproterenol also has been explored in the pharmacologic management of unstable bradyarrhythmias. As a result, they should be used only temporarily to provide a bridge to more definitive management with transcutaneous or transvenous cardiac pacing. Transcutaneous pacing is markedly easier to perform and frequently effective, but it is quite uncomfortable for the patient unless ample pain medication or continuous sedation is administered. Because sedative-hypnotic agents might worsen perfusion in the already unstable patient, this technique typically is reserved as a temporizing measure in emergent situations. Transcutaneous pacemakers generally have two connections to the patient: a set of pads for delivering the pacing current and leads for monitoring. If feasible, the pads should be placed in an anteroposterior position, with the anterior pad as close as possible to the point of maximum cardiac impulse, and the posterior pad directly opposite the anterior in the left perithoracic region. Two variables require adjustment: the energy output required to pace the patient and the rate at which pacing occurs. Complications include pain, local tissue injury, and failure to detect underlying ventricular arrhythmias. Central venous access is required and best established via the right internal jugular or left subclavian vein. The pacing electrode is then advanced through the vein under electrocardiographic guidance. The balloon-tipped catheter is inserted into the central line and advanced approximately 10 cm. At this point, the pulse generator is activated in the "sense" mode, and the pacing wire is further advanced into the ventricle until cardiac electrical activity is detected. At this time, the balloon is deflated, the generator is switched to the "pace" mode, and the current is increased from the minimal setting used during the first phase (eg, <0. This electrical capture should be apparent on the rhythm monitor as the wire is advanced up to 10 cm and placement in the right ventricle can be confirmed by recognition of a left-bundle branch block pattern. If capture does not 252 occur, the wire should be withdrawn back to the initial 10-cm mark and the process should be repeated. For instance, highly trained endurance athletes can have a resting heart rate in the range of 40 to 50 beats/min. In addition, adverse medication effects can trigger sinus bradycardia, either through unintentional exposure or purposeful ingestion. These situations require immediate diagnosis and emergent intervention to prevent cardiovascular collapse. Sinus bradycardia is defined as the presence of sinus rhythm with a rate slower than 60 beats/min. Idioventricular Rhythm (Bradycardia) An idioventricular rhythm results from a pacemaker site located in the distal intraventricular conduction system or within the ventricular myocardium. With rates of less than 40 beats/min, the idioventricular 257 rhythm will support marginal perfusion at best. This rhythm is most common in cardiac arrest patients who demonstrate electrical activity on the cardiac monitor yet have no palpable pulse. However, if the pacemaker site is in the ventricular septum, the complexes may be only minimally widened. Preexisting intraventricular conduction delay (ie, bundle-branch block) accompanied by a junctional escape rhythm is indistinguishable from a faster idioventricular rhythm. Atropine and other medications are unlikely to restore appropriate perfusion in patients with compromising idioventricular rhythms; cardiac pacing likely will become necessary in these presentations. Specific therapies (eg, attention to hyperkalemia or cardioactive medication poisonings) also should be considered. These abnormalities are most common in acutely ill patients with significant hemodynamic compromise. While minimal variability can be seen because of changes in heart rate and autonomic tone, this prolongation typically is fixed and unchanging. In addition, the rhythm is regular with uniform, consistent P-P and R-R intervals. If the conduction ratio is other than 2:1, the rhythm can appear irregular with grouping of conducted beats separated by the nonconducted beat. The descriptor "highgrade" is applied when more than one P wave in a row is nonconducted. In this case, the atria and ventricles are working independently without any electrical communication. In complete heart block, the atrial pacemaker is faster than the escape pacemaker, which can be either junctional or ventricular; therefore, the atrial rate is faster than the ventricular rate. The escape rhythm most often occurs in a regular manner as well, again with constant and unchanging R-R intervals. There is a complete lack of electrical communication between the atria and the ventricles. Even in these cases, the block is not of concern in and of itself; rather, its presence can be predictive of a more significant conduction abnormality. In this situation, the clinician should consider increasing the level of patient surveillance and prepare for more aggressive resuscitative therapy. Transcutaneous pacing pads should be applied even on asymptomatic patients out of concern for deterioration while other causes of the abnormality (eg, hyperkalemia) are explored. Specific Management Considerations Certain tachyarrhythmias require urgent rhythm-specific therapy, whereas others need treatment aimed at correction of the underlying cause of the dysrhythmia. Determination of patient stability, or lack thereof, will guide early management decisions. In some cases, the first appropriate treatment is the vagal maneuver, including carotid massage or initiation of the diving reflex. It generally is a safe choice with an excellent record of successful arrhythmia termination in this setting. In each of these presentations, prolonged pauses or short periods of asystole have been observed. In other clinical situations, the effects of adenosine are antagonized by methylxanthines such as caffeine and theophylline. It is important to correctly define a "failure" in the administration of adenosine. In such situations, repeat dosing at the same level is unlikely to succeed; a higher dose should be given if possible. It is given intravenously at a dose of 5 mg, and can be repeated two additional times at appropriate intervals if the desired effect is not observed. Esmolol, a parenteral beta-blocker with a relatively short duration of effect, also can be used in place of the longer-duration agents if hypotension is a concern. If the desired clinical response does not occur, it can be repeated at a dose of 0. Caution must be exercised regarding hemodynamic stability; not all patients who present with one of these arrhythmias require electrical cardioversion. This abnormality should be considered a "reactive rhythm," and treatment should be focused on the cause(s), including hypovolemia, hypoxia, fever, medication/toxin effect, and pain/ anxiety (a diagnosis of exclusion). It is the uncommon patient who requires a beta-blocker or calcium channel blocker. The use of an agent with a longer serum half-life can assist in the conversion to sinus rhythm; this therapy can be used in full or partial dose, combined with repeat adenosine administration. The baseline can be isoelectric or exhibit fibrillatory waves of varying morphologies at a rate of 400 to 700 beats/min. The amplitude of the fibrillatory waves is suggestive of the underlying pathology. The rate varies, but a ventricular response of approximately 170 beats/min is common, representing the "natural" rate of atrial fibrillation (ie, not altered by another disease state or medications). Typically, the P waves appear as downward deflections called flutter waves, which are marked by a characteristic "sawtooth" appearance. Most commonly, the atrial rate is regular, usually 300 beats/min, with a range from 250 to 350 beats/min.
Purchase claritin 10 mg on line
Treatment objectives are to optimize healing of the periodontal ligament and maintain pulp vitality allergy usa foundation claritin 10mg low price. This is accomplished by relieving the tooth from occlusion and having the patient avoid using the concussed teeth for a week to reduce any pressure, which in turn reduces the stress on the periodontium. Vitality should be tested as well at recall visits because there is a risk of pulp necrosis mainly with mature teeth [17]. In immature teeth, due to continuous root development, the risk of pulpal necrosis is much less. Subluxation Subluxation is defined as a modest injury to the teeth that affects the supporting structure of the affected tooth with abnormal loosening but without tooth displacement. Diagnostic signs and treatment are similar to those for concussion injury except for managing the mobility of the traumatized tooth. Sensibility testing at the time of the trauma is negative, indicating a transient pulpal damage that is usually reversible. The prognosis is usually favorable, and the affected tooth returns to its normal condition within two weeks. Mobile permanent teeth may need to be stabilized and occlusal interferences relieved. A flexible splint may be placed for two weeks if the patient feels pain and discomfort. Mature permanent teeth with closed apices may undergo pulpal necrosis due to associated injuries to the blood vessels at the apex. Therefore, until a definitive pulpal diagnosis is reached, monitoring and testing the affected teeth is important at one week, six to eight weeks, and one year. The tooth is not mobile and is locked into the new position, giving a metallic sound, resembling an ankylosed tooth, during percussion. The tooth usually is not tender to touch, and pulp sensibility testing yields negative results. Radiographic findings show an increase in the periodontal ligament space, rupture of the periodontal ligament, and displacement of the apex toward or through the labial bone plate. Treatment in mature teeth consists of repositioning the tooth using firm and gentle digital pressure. Forceps may be used to disengage the tooth from its bony locked position and then repositioned. The alveolar bone is also repositioned into its correct position to maintain alveolar integrity. If pulpal necrosis is anticipated or if the tooth is displaced more than 5 mm, pulp should be extirpated within 48 hours to prevent root resorption. Follow-up is every two weeks while the splint is in place and then six to eight weeks, six months, and annually up to five years. In primary immature teeth, continuous development of the root can be confirmed by radiographs indicating revascularization. The teeth may be allowed to passively reposition if this does not interfere with occlusion. If interferences are present, the tooth should be repositioned and splinted to the adjacent teeth for one to two weeks to allow healing. Such teeth have an increased risk of developing pulp necrosis compared to teeth that are left to spontaneously reposition. Follow-up is at two to three weeks and clinical observation and radiographs at six to eight weeks and one year. The tooth is tender to touch and percussion, with little or no response to a sensibility test. This is dependent on the degree of displacement of the tooth and its stage of development. In primary immature teeth, treatment depends on the degree of displacement, occlusal interference, and time to exfoliation. If the injury is not severe (less than 3 mm of extrusion) the tooth may be repositioned or allowed to spontaneously align. But when the injury is severe or the tooth is nearing exfoliation or the patient is uncooperative, extraction should be considered as the treatment of choice. In a permanent mature tooth with a closed root apex, there is increased risk of pulpal necrosis and periapical rarefaction. Active repositioning of the tooth with digital pressure into its anatomically correct position should be initiated as soon as possible. Steady and firm finger pressure should be applied in an apical direction to displace the clot formed between the floor of the socket and the tooth apex. B, A radiograph showing an open apex and chipped crown of upper right central tooth. In severe injuries, the tooth becomes intruded and locked in the alveolar bone, causing compression of the periodontal ligament and fracture of the alveolar socket. The tooth apex is usually displaced labially toward or through the labial bone plate when the affected tooth is of a primary dentition. The position of the primary tooth in relationship to the developing permanent may be determined by a lateral radiograph. Radiographic findings reveal that the tooth is displaced apically and the periodontal ligament space is not continuous or may be absent from all of the root. The cementoenamel junction is also located more apically in the intruded tooth in comparison to its adjacent tooth. There are three treatment modalities recommended to reposition the intruded tooth. If the intrusion is less than 3 mm, allow for spontaneous eruption in case of immature teeth with incomplete root formation, and monitor the self-eruption over 6 weeks. If there is no movement within a few weeks, initiate an orthodontic repositioning procedure. In either event, initiate orthodontic forced eruption or surgical repositioning if the tooth does not erupt spontaneously. If the intrusion is between 3 and 7 mm, orthodontic repositioning should be performed over a few weeks to allow the periapical tissues to heal. The pulling force should be very minimal to help healing of the periodontal ligament and alveolar bone over time. Teeth should be splinted with a soft splint to allow physiologic tooth movement up to 4 weeks. Root canal therapy should be initiated with calcium hydroxide 2 to 3 weeks after surgery. Management of injuries to the hard dental tissues and pulp Avulsion Avulsion is defined as the complete displacement of a tooth out of its socket. Exfoliated, avulsed, or knocked-out teeth are synonyms for the most serious and critical situation that can happen to adolescents. In young people, most avulsions occur during contact sports like football, basketball, handball, rugby, and boxing. Slipping in bathrooms or other wet floors, car accidents, and bicycling are contributing factors and are common among elderly persons and adolescents. Chapter 7: Dental traumatic injuries 161 the most important element for the treating dentist in dealing with traumatic injuries is the awareness of different modalities of treatment for both immature and mature teeth. Radiographs are necessary to rule out intrusion if the avulsed tooth is not found. The viability of the periodontal cells depends on the length of time the tooth was out of the mouth, the storage medium used before reaching the dentist, and the stage of development of the tooth. Long-term prognosis also depends on the viable cells of the periodontal ligaments and the extent of damage to the cementum and pulpal tissues. Inflammatory resorption, replacement resorption, and ankylosis are the most significant and common complications after replantation of the avulsed teeth. The best first aid is to wash the tooth under running cold water for a few seconds, if possible, and immediately replant the tooth in its socket at the site of the accident by holding the tooth by its crown part and let the patient bite on a piece of gauze.
Discount claritin uk
In vitro comparison of intact endodontically treated teeth with and without endo-post reinforcement allergy testing joondalup buy genuine claritin. The prosthodontic management of endodontically treated teeth: a literature review. Resistance to root fracture of dowel channels with various thicknesses of buccal dentin walls. Questions 1 For post and core fabrication in multirooted teeth A It is essential to make posts for each canal. A Zinc oxide eugenol B Zinc phosphate C Resin modified glass ionomer D Resin cements 3 Ferrule effect means A Tooth preparation must extend 2 mm beyond the cervical margin of the tooth. A To resist crown rotation B To resist post rotation C To provide a ferrule effect D All of the above 8 the cast post should be sandblasted by the lab before it is returned for fitting. A True B False 10 When cementing a post A Cement should be placed on the post only. Dentoalveolar traumatic injury is one of the most commonly encountered dental emergencies; it occurs quite often in preschool- and school-age children and in young adults. Dental trauma can result in fractured, displaced, or lost teeth, which can have functional or esthetic effects on the individual. It can affect or involve the dental pulp (directly or indirectly), and it can cause extensive damage to the surrounding tissues. This chapter talks about various traumatic dental injuries and their current protocols of management. It is imperative to rule out any neurological involvement or any other systemic injuries. Object speed, size, and shape also plays a role in how much damage occurs to the teeth and surrounding supporting structure. A sharp object can cause more soft tissue damage than a larger blunt object such as football or fist punch during a fight or an elbow hit during basketball game. Children with an overjet exceeding 4 mm and with incompetent lips and a mouth-breathing habit are more prone to such injuries. Preventive measures are essential during sports activities such as mouth guards, helmets. The best measure for preventing dental and oral injuries is education on both how to avoid them and what to do if an injury occurs, which should include students, teachers, and parents. General considerations When faced with a traumatic injury, the biggest challenge for the clinician is to calm the patient and the parents in their panic and confused state. The dental practitioner should be able to reassure them and guide them on what to do if they call the dental office over the phone. It is critical to obtain standardized data from the patient or accompanying person [5]. Check for any previous dental injury, and obtain a medical history for allergies or any serious illness. This will have an impact on the outcome and prognosis of the treatment and even on the treatment plan. The type of occlusion and any disturbances in the bite should be determined at this stage. A proper diagnosis, treatment planning, and followup are critical to ensure a favorable outcome. The primary goal is to delineate an approach for the immediate and urgent care of traumatic dental injuries. Trauma cases need long-term follow-up and evaluation at intervals for at least five years. Clinical examination Check for any fractures of the bone or the dentoalveolar complex, any abnormal tooth mobility or tooth displacement, and any tenderness to touch and/or percussion. A pulp sensibility test, usually at the time of trauma, will give negative results. Radiographic examination Radiographs are essential for detecting root fractures, intrusions, extent of root development, periapical damage, degree of tooth displacement, position of unerupted teeth, fractures of the mandible or maxilla, the presence of tooth fragments, and foreign bodies in soft tissue. Although some radiographs show negative findings at the initial appointment, they are important as baseline comparisons with subsequent radiographs. Several projections and angulations are routinely recommended, but the clinician should decide which radiographs are required for the patient. Recommended views are periapical view with 90-degree horizontal angle with central beam through the tooth in question, occlusal view, periapical view with lateral angulations from mesial or distal aspects, and soft tissue radiographs in case of soft tissue lacerations. Additional information, including if the patient vomited or lost conscious, had bleeding from the nose or ears after the injury, was in a state of confusion, or had blurred vision can help the treating dentist in deciding whether or not to pursue medical consultation [6]. Instructions to the patient or guardian calling from the site of the injury should include specific information relating to the type of injury. If the tooth has displaced (moved from original position in the socket) but is still in the socket, the patient should rush to the dentist. If the tooth crown is fractured, the patient should find the fractured piece and bring it along. The patient should hold the tooth from its crown and Chapter 7: Dental traumatic injuries 155 information about the traumatized teeth [7, 8]. They provide enhanced visualization, particularly in cases of root fractures and lateral luxation. There is a growing concern amongst healthcare professionals regarding tooth discoloration with tetracycline, especially in children whose teeth are not completely developed or erupted. Initial treatment Once the diagnosis is established and the local anesthetic is given, the tooth should be examined. If any contamination is visible, the tooth surface should be cleaned with saline and chlorhexidine 0. In cases of displacement or root or bone fracture, use digital pressure to replace the tooth in its normal position before splinting. A short-term, flexible, nonrigid splint is recommended for tooth and bone fractures and for luxated or avulsed teeth. In cases of root fractures in the middle and cervical third of the tooth and alveolar fractures, rigid splinting is recommended. Splinting maintains the repositioned tooth in its correct position and provides patient comfort and improved function. A flexible splint for 2 weeks is generally used for subluxation and extrusive luxation. Lateral luxation (flexible splint), root fractures (rigid), and alveolar fractures (rigid), usually require 4 weeks of splinting [9]. In avulsion cases, where the teeth are not present, fixation is obtained by using firm pressure to realign the bone fragments and stabilize the area by suturing the gingival tissues. Every effort should be made to preserve the pulp vitality in cases of immature permanent teeth to ensure continuous root development. Vitality tests (hot, cold, and electric) may be performed to determine the status of the pulp. At the time of injury, these are not very reliable diagnostic tools because they can give a false positive response or no response. Emerging therapies have been under research and have demonstrated the ability to regenerate vital pulp tissue. In immature teeth, it is best not to initiate a root canal unless there are signs of necrotic pulp or radiographic changes. Root canal treatment can be initiated 7 to 10 days after trauma just before removing the splint. Patient instructions and follow-up Both patient and parents should be advised and given instructions regarding the care of injured teeth for optimal healing and prevention of any further injury. Instructions should include consumption of soft diet for one week, avoidance of participation in contact sports, maintenance of good oral hygiene by using a soft tooth brush and rinsing with an antibacterial like chlorhexidine 0. The patient should be recalled for follow-up after 2 weeks, 6 to 8 weeks, 6 months, 1 year, and yearly for 5 years. The classification has been modified and updated by Andreasen and colleagues [12]. The management of these injuries is categorized individually for explanatory purposes. Management of injuries to the periodontal tissues Concussion Concussion is defined as an injury to the tooth supporting structures without abnormal loosening or displacement of the tooth. There may be bleeding around the gingiva as a result of injury to the tooth supporting structures.
Trusted 10mg claritin
However allergy symptoms jaw pain cheap claritin 10mg fast delivery, odontoblasts do not share direct cellular communication with neurons and a synaptic communication between these two cell types has never been demonstrated. Therefore, despite increased gained knowledge in odontoblast physiology, their direct role in nociception remains elusive. Several members of this ionotropic family have been directly implicated in nociception when expressed in sensory neurons (Julius 2013). This thermosensitive channel is activated by noxious heat (temperature >43 C) through the recently discovered release of endogenous oxidized metabolites of linoleic acid. These inflammatory mediators are usually released in a cascade that comprises an "inflammatory soup"(Julius and Basbaum 2001; Cunha et al. Whenever the concentration of any given mediator is sufficient to bind and activate its receptors in the nociceptors, intracellular signaling pathways are triggered. Many intracellular signaling pathways are known to sensitize or activate nociceptors. For example, local elevation of prostaglandin E2 activates protein kinase A leading to nociceptor sensitization, while increased tissue amounts of bradykinin activates phospholipase C and protein kinase C, leading to nociceptor activation. Thus, allodynia can be produced by inflammatory mediators that sensitize nociceptors. Interestingly, the dull, throbbing pain sensation typically associated with activation of C nociceptors is often reported by patients with irreversible pulpitis. The process known as central sensitization occurs when the primary afferent signal is amplified at this central terminal. Central sensitization represents a major component in inflammatory hyperalgesia and allodynia (Woolf 1996). Interventions at this receptor in the central terminals induce either reduction or enhancement of central sensitization generated by repeated C-fiber discharge. Clinically, central sensitization can be observed in patients complaining of persistent pain even after the removal of inflamed peripheral tissue with endodontic and restorative procedures or in allodynia felt in teeth and tissue surrounding an offending tooth. Studies have shown that the presence of preoperative pain increases the risk of postoperative pain (Torabinejad et al. Furthermore, preemptive analgesia during surgical procedures is associated with reduced postoperative pain in many situations (Woolf and Chong 1993; Reuben 2007). This suggests that patients who seek endodontic assistance at the first sign of symptoms, and who receive treatment under adequate profound anesthesia, have better postoperative prognosis because of the decreased likelihood of developing central sensitization. Despite these significant technical advances, pain may persist following adequate therapy, with a reported frequency of 5. Although an endodontic treatment may be deemed adequate when evaluating periapical radiographs, pain may persist for longer than 6 months. The evaluation of periapical radiographs has been traditionally used as an outcome measure of endodontic success. Therefore, persistent postendodontic pain of odontogenic origin may be associated with symptomatic apical periodontitis not detected with conventional radiographic imaging methods. From this perspective, persistent pain may result from the failure to completely eliminate the original etiologic factors. While nonodontogenic pain conditions must be considered in the differential diagnosis of persistent postendodontic pain, these findings indicate that certain cases of posttreatment pain may result from persistent symptomatic apical periodontitis. There are many factors that predispose patients to persistent post-treatment apical periodontitis. These include host factors such as systemic diseases that modulate the immune system. In addition, both cytokines are also known to sensitize nociceptors, being important players in inflammatory thermal hyperalgesia and mechanical allodynia (Ferreira et al. The frequency of nonodontogenic pain lasting longer than 6 months following root canal therapy has been found to be about 3% of cases (Nixdorf et al. This suggests that, at least in part, some teeth may have been misdiagnosed as being the source of the pain and have been erroneously endodontically treated. Another study found that approximately half of the cases with diagnosis of nonodontogenic pain following root canal therapy were related to referred pain from temporomandibular disorders (Nixdorf et al. Importantly, the majority (63%) of the patients reporting persistent pain following root canal therapy also reported a history of chronic pain elsewhere in the body. This is an important observation because there is growing recognition that patients with a history of chronic pain such as temporomandibular disorders have higher levels of psychosocial symptoms, affective distress, somatic awareness, and pain catastrophizing (Fillingim et al. Indeed, new research suggests that many chronic pain disorders reflect a centralized pain state that amplifies pain perception far beyond levels perceived by patients without chronic pain disorders (Tracey et al. Simply put, patients with a history of chronic pain are predisposed to persistent pain following root canal therapy. These findings are in agreement with the finding that moderate to severe preoperative pain and presence of chronic pain are predictors of postoperative pain (Polycarpou et al. It is noteworthy that nonodontogenic pain following root canal therapy is a relatively rare occurrence in patients with nonchronic pain. When bacteria gain access to the pulp, a significant inflammatory response is initiated. Bacteria can induce tissue injury and inflammation through three general pathways. First, bacteria can release tissue modifying agents such as enzymes capable of degrading host tissue elements. Third, chronic bacterial infections can lead to activation of specific or adaptive immune response (Baumgartner and Falkler 1991). First, it is known that endodontic infections are polymicrobial with a predominance of strict anaerobic and facultative aerobic bacteria (Fabricius et al. These receptors recognize specific and highly conserved nonself molecular microbial signatures. Thus, these specialized receptors represent the gateway of the innate immune response against invading microorganisms. Thus, nociceptors in the dental pulp are particularly equipped to directly sense bacteria (Wadachi and Hargreaves 2006). Upon the release of these cytokines, the inflammatory reaction amplifies rapidly as infiltrating immune cells start releasing more inflammatory mediators which act in concert to promote the cardinal signs of inflammation: edema and pain. Nociceptors express the receptors for numerous inflammatory mediators and activation of these receptors leads to the sensitization of these pain-sensing fibers (Byers et al. Some of these mediators such as bradykinin and prostaglandins evoke an acute sensitization of nociceptors by triggering local intracellular events. The activation of a peptidergic subset of nociceptors is often accompanied by a vasodilation reaction (Simone et al. Certainly, the enhanced activation of these nociceptors in inflammatory conditions leads to neuropeptide release. For example, elevated levels of substance P have been found in the pulp of patients with irreversible pulpitis (Bowles et al. The mechanism for neuronal-generated inflammation is called neurogenic inflammation and is often intertwined with classic inflammatory processes due to a positive feedback loop. It has been suggested that odontoblasts have a monitoring and functional role in pulpal inflammation because they represent the first biologic barrier, between mineralized tissues and the dental pulp, encountered by pathogens. Odontoblasts are highly specialized cells that express a "molecular repertoire" far greater than that needed for simple dentin production and deposition. Together, these cells then release inflammatory mediators leading to the indirect sensitization of nociceptors by bacteria. The sensitization of nociceptors in infections is classically believed to be caused by the release of inflammatory mediators from bacteria-activated immune cells. This novel finding raises the possibility that sensory neurons are able to "sense" the presence of Gram-negative bacteria. These data have exciting clinical significance, because deeper carious lesions and primary periapical lesions are predominantly associated with Gram-negative bacteria. In these patients, there are decreased levels of inflammatory mediators, which normally would result in attenuated inflammatory pain. This high penetration and dentin affinity may explain the persistence of this highly immunogenic molecule following chemomechanical preparation (Martinho and Gomes 2008).