Generic levitra professional 20 mg with visa
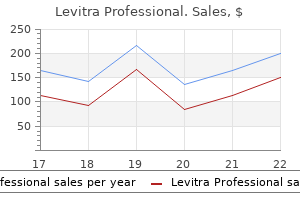
Heterozygotes have not been known to develop clinical disease or require treatment erectile dysfunction incidence age levitra professional 20 mg. Efforts to identify clear patterns of correlation between genotype and phenotype have been largely disappointing in Wilson disease. With the opportunity of confirming a diagnosis of Wilson disease by direct identification of mutations, the spectrum of manifestations of Wilson disease has been found to be even wider than previously recognized. Mutation analysis should also be carried out to distinguish asymptomatic patients from heterozygotes. Three markers are usually adequate for an unambiguous result: D13S314, D13S301, and D13S316. The proband (arrow) and asymptomatic sibling confirmed as affected are shown as filled circles. Diagnosis of First-Degree Relatives If mutations have been identified in a patient, mutational analysis is easily carried out in first-degree relatives (siblings, parents, and offspring) by direct testing for the mutations found in the patient. If mutations have not been identified, accurate diagnosis can be achieved using markers flanking the gene. The most useful genetic markers are stretches of dinucleotides or trinucleotides that show extensive variability in the normal population, so that parents within any one family will carry different alleles of these markers. It is important that informative markers flank the gene, because an erroneous diagnosis could result if markers on only one side of the gene are informative and a recombinant event has occurred close to the gene. The combination of markers, or haplotype, reliably indicates the genetic status within the family. According to marker studies or genetic diagnosis, an occasional person considered as a result of biochemical testing to have a high probability of being an asymptomatic patient has been shown to be a heterozygote. Therefore, confirmation of the genotype is highly recommended before treatment is initiated. Conversely, if the clinical diagnosis of a heterozygote is uncertain, genetic diagnosis can be highly informative. In the absence of genetic analysis, screening should include physical examination, liver biochemical tests, serum copper and ceruloplasmin measurements, a basal 24-hour urinary copper determination, and a careful slit-lamp examination. Children 6 years of age or younger who appear to be unaffected should be rechecked at yearly intervals over the next 5 to 10 years. Accumulating data indicate that the incidence of Wilson disease in children of patients with Wilson disease is higher than predicted. Therefore, screening of all first-degree relatives, not just siblings, is mandatory. With effective lifelong chelation treatment, most patients live normal, healthy lives. Starting treatment early is critical, and the outcome is best for patients in whom the disease is diagnosed and treatment begun when the patient is asymptomatic. Whether routine institution of chelation or zinc therapy in infancy (<2 years of age) is advantageous or deleterious remains unknown. The dose of trientine in children is not established (approximately 20 mg/kg/day in divided doses). Typical dosing is 25 mg of elemental zinc 3 times daily until adult stature (50 kg body weight) is achieved, when the adult dose of 50 mg of elemental zinc 3 times daily is used. The dose in children can also be titrated to achieve optimal 24-hr urinary copper excretion. Penicillamine, which is the sulfhydryl-containing amino acid cysteine substituted with 2 methyl groups, greatly increases urinary excretion of copper; only the d-penicillamine form is used clinically. The neurologic status of patients with mainly neurologic symptoms may worsen initially after treatment with d-penicillamine is started80; most, but not all, recover with cautious continued use of d-penicillamine. Substituting trientine or zinc reduces this risk of a poor outcome, but all these drugs entail some possibility of neurologic deterioration. Starting with a low dose of d-penicillamine and increasing the dose slowly over 2 to 4 weeks may help avoid this adverse effect. A febrile reaction with rash and proteinuria develops in some patients within 7 to 10 days of beginning treatment. Although d-penicillamine can be restarted slowly along with glucocorticoids, changing to an alternative chelator is preferred. Adverse reactions involving the skin include various types of rashes, pemphigus, and elastosis perforans serpiginosa. Aplastic anemia occurs rarely and does not always reverse when d-penicillamine is stopped. These severe side effects require immediate discontinuation of d-penicillamine and use of a different chelator. Whether lifelong treatment with d-penicillamine is free of adverse consequences is not entirely clear. Patients who have taken d-penicillamine for 30 to 40 years may have chronic skin changes with loss of elastic tissue. In view of these side effects, maintenance therapy with d-penicillamine should be at the lowest effective dose. Trientine, or triethylenetetramine dihydrochloride, is the usual second-line treatment for patients who are intolerant of d-penicillamine. Copper is chelated by forming a stable complex with the 4 constituent nitrogens in a planar ring. Trientine increases urinary copper excretion and may interfere with intestinal absorption of copper. Trientine is a less potent chelator than d-penicillamine, but the difference is not clinically important. Trientine produces little significant toxicity in patients with Wilson disease-apart from causing occasional gastritis and inducing iron deficiency, apparently by chelating dietary iron. Adverse effects of d-penicillamine resolve and do not recur during treatment with trientine. Trientine is highly effective, even in patients with advanced liver fibrosis or as initial treatment in children. The postulated mechanism of action is through the induction of metallothionein in enterocytes. The metallothionein has a greater affinity for copper than for zinc and preferentially binds copper from the intestinal contents. Once bound, the copper is not absorbed but is lost in the feces as enterocytes are shed during normal turnover. Zinc may interfere with lipid peroxidation and enhance the availability of glutathione. Problems with zinc therapy include gastritis, which is a common side effect, and uncertainty about dosing. Using a zinc salt other than zinc sulfate may minimize gastritis; most zinc salts are equally acceptable for the treatment of Wilson disease. Food interferes with the effectiveness of zinc, and some investigators recommend that no food be eaten for 1 hour before or after a dose of zinc is taken. An alternative approach is to be less rigorous about avoiding zinc at mealtimes and to titrate the dose according to the urinary copper excretion. Long-term studies suggest that zinc is more effective in neurologic Wilson disease than in hepatic Wilson disease. The adequacy of treatment is assessed by measurement of basal 24-hour urinary copper excretion, which should be high with either oral chelator (200 to 500 g/day or 3 to 8 mol/day) and low with zinc (30 to 75 g/day or 0. The patient must be asked specifically about general well-being and adherence to the drug regimen. With zinc treatment, adherence can be checked by measurement of 24-hour urinary zinc excretion (>2 mg/day) or serum zinc (>12. Elevated serum aminotransferase levels that were previously normal may signal nonadherence and evidence of ongoing hepatic damage. Patients diagnosed while still asymptomatic may be at greater than average risk for lapsing into nonadherence. For patients who present with decompensated chronic liver disease, combining zinc with a conventional chelator (preferably trientine) has become a popular treatment strategy even in the absence of extensive validation. This intensive short-term induction regimen is best suited to patients with severe hepatic or neurologic disease85 and remains semi-investigational. Ammonium tetrathiomolybdate was investigated as treatment of severe neurologic Wilson disease because, unlike d-penicillamine, it is not associated with early neurologic deterioration. A new formulation, bis-choline tetrathiomolybdate, has excellent stability and is pharmacologically equivalent to ammonium tetrathiomolybdate. More detailed information about the total-body disposition of copper and molybdate is needed.
Buy levitra professional line
A review of pathophysiology and management of fetuses and neonates with meconium ileus for the pediatric surgeon erectile dysfunction statistics nih purchase levitra professional 20 mg otc. Abdominal symptoms in cystic fibrosis and their relation to genotype, history, clinical and laboratory findings. Guidelines for the diagnosis and management of distal intestinal obstruction syndrome in cystic fibrosis patients. Intestinal obstruction syndromes in cystic fibrosis: meconium ileus, distal intestinal obstruction syndrome, and constipation. Ivacaftor-treated patients with cystic fibrosis derive long-term benefit despite no short-term clinical improvement. Effects of lumacaftor-ivacaftor therapy on cystic fibrosis transmembrane conductance regulator function in phe508del homozygous patients with cystic fibrosis. Suramin increases cartilage proteoglycan accumulation in vitro and protects against joint damage triggered by papain injection in mouse knees in vivo. A guide to interpreting estimated median age of survival in cystic fibrosis patient registry reports. Hereditary pancreatitis in North America: the Pittsburgh-Midwest Multi-Center Pancreatic Study Group Study. Clinical characteristics of hereditary pancreatitis in a large family, based on high-risk haplotype. Expression and penetrance of the hereditary pancreatitis phenotype in monozygotic twins. Cystic fibrosis liver disease: outcomes and risk factors in a large cohort of french patients. Risk factors for hepatic steatosis in adults with cystic fibrosis: similarities to nonalcoholic fatty liver disease. A single centre experience of liver disease in adults with cystic fibrosis 1995-2006. Bile salt kinetics in cystic fibrosis: influence of pancreatic enzyme replacement. Risk of gastrointestinal cancers in patients with cystic fibrosis: a systematic review and meta-analysis. Cancer risk in nontransplanted and transplanted cystic fibrosis patients: a 10-year study. Acute pancreatitis and pancreatic cancer risk: a nationwide matchedcohort study in denmark. Evidence-based practice recommendations for nutrition-related management of children and adults with cystic fibrosis and pancreatic insufficiency: results of a systematic review. Options for addressing exocrine pancreatic insufficiency in patients receiving enteral nutrition supplementation. Increased fat absorption from enteral formula through an in-line digestive cartridge in patients with cystic fibrosis. Hereditary pancreatitis amlodipine trial: a pilot study of a calcium-channel blocker in hereditary pancreatitis. Type of pain, pain-associated complications, quality of life, disability and resource utilisation in chronic pancreatitis: a prospective cohort study. Quality of life in chronic pancreatitis is determined by constant pain, disability/unemployment, current smoking, and associated co-morbidities. Pain in chronic pancreatitis: the role of reorganization in the central nervous system. Evidence of pancreatic neuropathy and neuropathic pain in hereditary chronic pancreatitis. Pancreatic neuropathy results in "neural remodeling" and altered pancreatic innervation in chronic pancreatitis and pancreatic cancer. Total pancreatectomy and islet autotransplantation in chronic pancreatitis: recommendations from PancreasFest. Risk of pancreatic adenocarcinoma in patients with hereditary pancreatitis: a national exhaustive series. Cigarette smoking as a risk factor for pancreatic cancer in patients with hereditary pancreatitis 2001. Germline variants and risk for pancreatic cancer: a systematic review and emerging concepts. Clinical characterization of patients with hereditary pancreatitis and mutations in the cationic trypsinogen gene. Mutation analysis of the cationic trypsinogen gene in patients with pancreatic cancer 2000. Pathology analysis reveals that dysplastic pancreatic ductal lesions are frequent in patients with hereditary pancreatitis. Motivations and concerns of patients with access to genetic testing for hereditary pancreatitis. Shwachman syndrome: exocrine pancreatic dysfunction and variable phenotypic expression. Segregation analysis in Shwachman-Diamond syndrome: evidence for recessive inheritance. Draft consensus guidelines for diagnosis and treatment of Shwachman-Diamond syndrome. Variable clinical presentation of Shwachman-Diamond syndrome: update from the North American Shwachman-Diamond Syndrome Registry. Shwachman syndrome: phenotypic manifestations of sibling sets and isolated cases in a large patient cohort are similar. Shwachman-Bodian Diamond syndrome is a multi-functional protein implicated in cellular stress responses. Deficiency of Sbds in the mouse pancreas leads to features of Shwachman-Diamond syndrome, with loss of zymogen granules. Pluripotent stem cell models of shwachman-diamond syndrome reveal a common mechanism for pancreatic and hematopoietic dysfunction. Ataluren-driven restoration of Shwachman-Bodian-Diamond syndrome protein function in Shwachman-Diamond syndrome bone marrow cells. Proceedings: studies on the mechanism of fat absorption in congenital isolated lipase deficiency Gut 1975;16:838. Enterokinase and trypsin activities in pancreatic insufficiency and diseases of the small intestine. Mutations in the proenteropeptidase gene are the molecular cause of congenital enteropeptidase deficiency. The interrelationship of enterokinase and trypsin activities in intractable diarrhea of infancy, celiac disease, and intravenous alimentation. Acute pancreatitis as an initial manifestation of parathyroid carcinoma: A case report and literature review. Primary hyperparathyroidism with pancreatitis: experience of management in 5 patients with review of literature. Computed tomography and ultrasonography findings for an adult with Shwachman syndrome and pancreatic lipomatosis. Shwachman-Diamond syndrome: early bone marrow transplantation in a high risk patient and new clues to pathogenesis. Pathophysiology of the pancreatic defect in Johanson-Blizzard syndrome: a disorder of acinar development. Pearson Syndrome: a retrospective cohort study from the Marrow Failure Study Group of A. Pearson syndrome: unique endocrine manifestations including neonatal diabetes and adrenal insufficiency. Site-specific deletions of the mitochondrial genome in the Pearson marrow-pancreas syndrome. Agenesis of the dorsal pancreas: a rare cause of insulin-dependent diabetes without abdominal pain: Case report. For example, gallstones are the dominant etiology in Southern Europe and alcohol in Eastern Europe, with intermediate gallstone-to-alcohol ratios in Northern and Western Europe. However, estimates of incidence are inaccurate because the diagnosis of mild disease may be missed and death may occur before diagnosis in 10% of patients with severe disease.
Generic 20 mg levitra professional visa
Risk factors associated with Helicobacter pylori infection among children in a defined geographic area erectile dysfunction pump on nhs levitra professional 20mg with visa. Acute gastritis with hypochlorhydria: report of 35 cases with long-term follow up. Adaptive Helicobacter genomic changes that accompanied a host jump from early humans to large felines. Tyrosine phosphorylation of the Helicobacter pylori CagA antigen after cag-driven host cell translocation. Biological activity of the Helicobacter pylori virulence factor CagA is determined by variation in the tyrosine phosphorylation sites. Helicobacter pylori CagA protein activates serum response element-driven transcription independently of tyrosine phosphorylation. Phosphorylation-independent effects of CagA during interaction between Helicobacter pylori and T84 polarized monolayers. Altered states: involvement of phosphorylated CagA in the induction of host cellular growth changes by Helicobacter pylori. Disruption of the epithelial apical-junctional complex by Helicobacter pylori CagA. Interleukin 8 (-251T>A) polymorphism in children and teenagers with Helicobacter pylori infection. Activation of activator protein 1 and stress response kinases in epithelial cells colonized by Helicobacter pylori encoding the cag pathogenicity island. Interleukin-8 induction by Helicobacter pylori in human gastric epithelial cells is dependent on apurinic/apyrimidinic endonuclease-2/redox factor-1. Sulforaphane inhibits extracellular, intracellular, and antibiotic-resistant strains of Helicobacter pylori and prevents benzo[a]pyrene-induced stomach tumors. N-acetylcysteine prevents the development of gastritis induced by Helicobacter pylori. A M(r) 34,000 proinflammatory outer membrane protein (oipA) of Helicobacter pylori. Natural antibiotic function of a human gastric mucin against Helicobacter pylori infection. Attachment of Helicobacter pylori to human gastric epithelium mediated by blood group antigens. Helicobacter pylori adhesin binding fucosylated histo-blood group antigens revealed by retagging. Helicobacter pylori activates Tolllike receptor 4 expression in gastrointestinal epithelial cells. Intact gram-negative Helicobacter pylori, Helicobacter felis, and Helicobacter hepaticus bacteria activate innate immunity via Toll-like receptor 2 but not Toll-like receptor 4. Helicobacter pylori strainspecific differences in genetic content, identified by microarray, influence host inflammatory responses. Mice deficient in protein tyrosine phosphatase receptor type Z are resistant to gastric ulcer induction by VacA of Helicobacter pylori. Association of specific vacA types with cytotoxin production and peptic ulceration. Induction of gastric epithelial cell apoptosis by Helicobacter pylori vacuolating cytotoxin. Importance of Helicobacter pylori oipA in clinical presentation, gastric inflammation, and mucosal interleukin 8 production. Nod1 responds to peptidoglycan delivered by the Helicobacter pylori cag pathogenicity island. Helicobacter pylori urease is a potent stimulus of mononuclear phagocyte activation and inflammatory cytokine production. Expression of interleukin-18, a Th1 cytokine, in human gastric mucosa is increased in Helicobacter pylori infection. Helicobacter pylori modulates lymphoepithelial cell interactions leading to epithelial cell damage through Fas/Fas Ligand interactions. H(+),K(+)-atpase (proton pump) is the target autoantigen of Th1-type cytotoxic T cells in autoimmune gastritis. Helicobacter pylori infection induces antibodies cross-reacting with human gastric mucosa. Potential role of molecular mimicry between Helicobacter pylori lipopolysaccharide and host Lewis blood group antigens in autoimmunity. Helicobacter pylori arginase inhibits nitric oxide production by eukaryotic cells: a strategy for bacterial survival. Virulent strains of Helicobacter pylori demonstrate delayed phagocytosis and stimulate homotypic phagosome fusion in macrophages. Selective inhibition of Ii-dependent antigen presentation by Helicobacter pylori toxin VacA. Role of chronic inflammation and cytokine gene polymorphisms in the pathogenesis of gastrointestinal malignancy. Increased risk of noncardia gastric cancer associated with proinflammatory cytokine gene polymorphisms. A proinflammatory genetic profile increases the risk for chronic atrophic gastritis and gastric carcinoma. American College of Gastroenterology guideline on the management of Helicobacter pylori infection. Accuracy of Helicobacter pylori diagnostic tests in patients with bleeding peptic ulcer: a systematic review and meta-analysis. Effect of proton pump inhibitors and antacid therapy on 13C urea breath tests and stool test for Helicobacter pylori infection. Helicobacter pylori and antimicrobial resistance: molecular mechanisms and clinical implications. The most important diagnostic modalities for Helicobacter pylori, now and in the future. Evaluation of four different fecal tests for determination of cure after Helicobacter pylori treatment. Application of polymerase chain reaction-based assays for rapid identification and antibiotic resistance screening of Helicobacter pylori in gastric biopsies. The Toronto consensus for the treatment of Helicobacter pylori infection in adults. Gastric intestinal metaplasia and early gastric cancer in the west: a changing paradigm. The severity of endoscopic gastric atrophy could help to predict Operative Link on Gastritis Assessment gastritis stage. Operative link for gastritis assessment gastritis staging incorporates intestinal metaplasia subtyping. Efficacy of Kyoto classification of gastritis in identifying patients at high risk for gastric cancer. Utilizing of a subtyping of intestinal metaplasia as marker of gastric cancer risk. Helicobacter pylori infection and chronic atrophic gastritis: associations according to severity of disease. Gastric intestinal metaplasia is associated with gastric dysplasia but is inversely correlated with esophageal dysplasia. Pepsinogens to distinguish patients with gastric intestinal metaplasia and Helicobacter pylori infection among populations at risk for gastric cancer. Detection of gastric atrophy by circulating pepsinogens: a comparison of three assays. Lewis antigen expression and other pathogenic factors in the presence of atrophic chronic gastritis in a European population. Endoscopic diagnosis of cytomegalovirus gastritis after allogeneic hematopoietic stem cell transplantation. A novel model might predict the risk of chronic atrophic gastritis: a multicenter prospective study in China. Should increased levels of urinary 8-hydroxydeoxyguanosine in chronic gastritis imply intestinal metaplasia or gastric atrophy
Levitra professional 20mg with mastercard
But in patients undergoing extensive resection of the antrum and corpus erectile dysfunction related to prostate cheap levitra professional 20 mg otc, prolonged symptoms and chronic gastric neuromuscular dysfunction are likely. Lower esophageal resection for esophageal cancer includes resection of the fundus. Pyloroplasty is performed to facilitate gastric emptying, but the loss of the fundus and variable amounts of the corpus (that may encompass the pacemaker region) often leads to chronic nausea, gastric dysrhythmias, and gastroparesis. Ingested food is retained in the remnant fundus and fails to empty into the corpus203; the corpus fails to mix and empty gastric contents even though the anastomosis is widely patent. The Roux-en-Y gastroenterostomy operation may result in the Roux syndrome in which postprandial pain, bloating, and nausea develop. Delayed gastric emptying is due to "functional obstruction" by the Roux limb as the neuromuscular dyssynchrony within the Roux limb prevents emptying of the stomach. In the gastric "sleeve" resection for obesity, two thirds of the stomach is removed including portions of the fundus, corpus, and antrum. After the sleeve resection, gastric emptying of liquid and solid test meals is accelerated, but there are few studies available for review. Postfundoplication gastroparesis and early satiety, bloating, prolonged fullness, and nausea may occur. These patients have altered fundic relaxation, delayed gastric emptying, and gastric dysrhythmias, possibly on the basis of vagal nerve injury during or after the fundoplication procedure. Gastric smooth muscle dysfunction is another mechanism of delayed gastric emptying in some patients with diabetes. Gastric smooth muscle contractility in diabetic rats is reduced in response to electrical stimulation. Type 2 diabetes mellitus patients with gastroparesis are older, have milder delays in gastric emptying, and more severe early satiety. This patient had electrical and contractile abnormalities of the stomach as documented by the tachygastria and gastroparesis. Ischemic gastroparesis is distinct from acute mesenteric ischemia, which presents as an abdominal catastrophe with an acute abdomen and gangrenous small intestine (see Chapter 118). Chronic mesenteric ischemia is usually due to progressive atherosclerosis or hyperplasia of the intima of the arteries of the celiac, superior mesenteric, or inferior mesenteric artery. Collaterals of these obstructed arteries form over time so that neuromuscular function of the stomach is preserved, at least for some time. Bypass graft surgery or dilatation of the stenotic arteries results in resolution of symptoms, eradication of gastric dysrhythmias, and reversal of gastroparesis. On the other hand, superior mesenteric artery syndrome is not accepted as a cause of mechanical obstruction that leads to gastroparesis, nausea, and vomiting. Patients with idiopathic (discussed below), diabetic, or postsurgical gastroparesis may have a subtype of gastroparesis-obstructive gastroparesis due to pyloric dysfunction. This subtype is important because endoscopic and surgical treatments are directed towards the pylorus. Fixed Pyloric Obstruction Fixed obstructive gastroparesis refers to delayed emptying due to mechanical obstruction at the pylorus or duodenal bulbar or postbulbar area by tumor, chronic peptic ulcer or inflammation, rings, or webs. Gastroparesis may actually be obstructive gastroparesis due to pyloric stenosis or postduodenal bulb cancer. Functional Pyloric Obstruction A more subtle type of gastric outlet obstruction occurs in pylorospasm. The "spasm" of the pylorus may cause postprandial right upper quadrant abdominal pain in the setting of gastroparesislike symptoms. Pylorospasm of the pylorus prevents normal gastric peristaltic waves from empting chyme into the duodenum. In these patients dilatation of the pylorus with a 20-mm balloon for 2 minutes or botulinum toxin A injections into the pylorus decreased postprandial symptoms. If these disorders are identified, then the gastroparesis may be secondary to these specific diseases. Importantly, postprandial distress symptoms are also similar to symptoms associated with gastroparesis. These neurologic disorders include Ehlers-Danlos syndrome,239 postural orthostatic tachycardia syndrome,240 spinal cord and head injuries, amyotrophic lateral sclerosis, myasthenia gravis, a variety of muscular dystrophies, and Parkinson disease (see Chapter 37). This mismatch of plasma glucose and insulin can result in symptomatic hypoglycemia. The rapid small bowel transit and poor absorption of the ingested nutrients lead to an osmotic form of diarrhea. Idiopathic rapid emptying is diagnosed in patients with no history of gastric operations or other causes. However, the ingestion of meals stimulates the disordered gastric neuromuscular apparatus, and early satiety, prolonged epigastric fullness, epigastric discomfort or pain, mild to severe nausea, and vomiting are then experienced. Vomitus that contains undigested, chewed food is strong evidence for gastroparesis. Prolonged postprandial fullness, weight loss, and female gender are predictive factors for gastroparesis. In addition, the foods are not normally triturated by peristaltic waves if the pylorus has been incised. Thus, liquid and solid nutrients are rapidly emptied or "dumped" into the duodenum or jejunum. The dumping syndrome symptoms include nonspecific abdominal discomfort, bloating, and nausea and vomiting. These symptoms are usually experienced in the first hour after ingestion of foods. Sweating and lightheadedness, however, may occur and be followed by abdominal cramps and diarrhea that occur 2 to 4 hours after the meal and are additional clues to the dumping syndrome. A thorough review of the causes of nausea and vomiting is required (see Chapter 15), and an appropriate differential diagnosis should be considered (see Box 50. Rumination refers to the effortless return of ingested liquids and solid foods into the mouth without burning, bitter taste, or nausea. Patients with rumination have impaired gastric accommodation and a more sensitive relaxation of the lower esophageal sphincter pressure in response to gastric distention. Abdominal pain, in contrast to the abdominal discomfort of bloating and nausea, occurs in approximately 20% of patients with gastroparesis. On the other hand, the epigastric discomfort or pain in some gastroparesis patients may originate from the stomach: excessive muscle tone of the fundus, high-amplitude antral contractions, pylorospasm, or hypersensitivity of the stomach are potential causes of pain. The categories are (1) gastroparesis with gastric dysrhythmia, (2) gastroparesis with normal gastric electrical rhythm, (3) normal gastric emptying with gastric dysrhythmia, and (4) normal gastric emptying with normal gastric electrical rhythm. The 4 categories provide a conceptual framework for understanding the spectrum of gastric neuromuscular disorders and providing an approach to therapy (see Table 50. These patients may have fixed mechanical obstructions of the pylorus and duodenum that are reversible with operation. The gastroparesis-like symptoms may be due to poor gastric relaxation or gastric visceral hypersensitivity in response to distension with the water load or caloric satiety tests. Diagnoses of nongastric disorders should also be considered in this patient group. Auscultation over the epigastrium may detect bruits that indicate stenoses of the celiac or superior mesenteric arteries. Pain and tenderness that are precisely localized to healed abdominal incisions and increase when the head is flexed and anterior abdominal muscles are contracted (positive Carnett sign) suggest the pain is from an abdominal wall syndrome and not the stomach. The reversible obstructive causes of gastroparesis due to fixed pyloric stenosis or functional pylorospasm and ischemic gastroparesis due to chronic mesenteric ischemia must be excluded because these entities are reversible. If gastric emptying is normal, then gastric dysrhythmia and gastric accommodation disorders may be the neuromuscular disorders that are relevant to the symptoms. Electrical Therapy Acustimulation Acustimulation (mild electrical stimulation of acupuncture points) reduces nausea of pregnancy, nausea due to chemotherapy agents, postoperative nausea, and the nausea of motion sickness285,286 and symptoms related to gastroparesis. Patients who have gastroparesis and tachygastria have severe electrical and contractile abnormalities of the stomach. The treatment includes prokinetics, antinauseant therapies, and dietary counseling. Metoclopramide, a substituted benzamide related to procainamide, is a useful prokinetic antiemetic but has a "black box" warning. Cisapride was not approved for gastric emptying disorders but increased gastric emptying rates and decreased dyspepsia symptoms in some patients.
Diseases
- Retinohepatoendocrinologic syndrome
- Nevus sebaceus of Jadassohn
- Retinoblastoma
- Pulmonary atresia with ventricular septal defect
- Miosis, congenital
- Gaucher-like disease
Buy levitra professional with a visa
Treatment outcomes associated with surgery for gallbladder cancer: a 20-year experience erectile dysfunction at 25 order line levitra professional. Fourteen year surgical experience of gallbladder cancer: validity of curative resection affecting survival. A 21-year analysis of stage I gallbladder carcinoma: is cholecystectomy alone adequate Surgical treatment of patients with T2 gallbladder carcinoma invading the subserosal layer. A curative resection improves the postoperative survival rate even in patients with advanced gallbladder carcinoma. Gallbladder cancer: defining the indications for primary radical resection and radical re-resection. Tumor location is a strong predictor of tumor progression and survival in T2 gallbladder cancer: an international multicenter study. Biliary tract cancer treatment: 5,584 results from the biliary tract cancer statistics registry from 1998 to 2004 in Japan. Survival after resection of ampullary carcinoma: a national population-based study. Controlled 15-year trial on screening for colorectal cancer in families with hereditary nonpolyposis colorectal cancer. Incidence, sites of origin, and immunohistochemical and histochemical characteristics of atypical epithelium and minute carcinoma of the papilla of Vater. Tumors of the ampulla of Vater: histopathologic classification and predictors of survival. Survival benefit of adjuvant chemoradiotherapy in patients with ampulla of vater cancer: a systematic review and meta-analysis. Meta-analysis of adjuvant therapy following curative surgery for periampullary adenocarcinoma. Malignant carcinoid tumor of the gallbladder: a case report and review of literature. Primary carcinoid tumor of the gallbladder: resection of a case metastasizing to the liver and analysis of outcomes. Extrahepatic bile duct carcinoid tumors: malignant biliary obstruction with a good prognosis. Carcinoid of the extra-hepatic bile duct: a case report with long-term follow-up and review of literature. Granular cell tumor as an unusual cause of obstruction at the hepatic hilum: report of a case. Granular cell tumor of the biliary system: a report of 2 cases with cytologic diagnosis on endoscopic brushing. Lymphangioma of the major duodenal papilla presenting as acute pancreatitis: treatment by endoscopic snare papillectomy. Multiple primary liver lipomas in a patient with chronic hepatitis B: a case report. Different clinicopathologic findings in two histologic types of carcinoma of papilla of Vater. Carcinoma of the ampulla of Vater: comparative histologic/immunohistochemical classification and follow-up. Treatment utilization and surgical outcome of ampullary and duodenal adenocarcinoma. Clinical significance of pathologic subtype in curatively resected ampulla of Vater cancer. Recurrence and prognostic factors of ampullary carcinoma after radical resection: comparison with distal extrahepatic cholangiocarcinoma. Staging of ampullary and pancreatic carcinoma: comparison between endosonography and surgery. A single-institution review of 157 patients presenting with benign and malignant tumors of the ampulla of Vater: management and outcomes. Clinicopathologic analysis of ampullary neoplasms in 450 patients: implications for surgical strategy and long-term prognosis. Prognostic significance of extracapsular lymph node involvement in patients with adenocarcinoma of the ampulla of Vater. Predictors of long-term survival following resection for ampullary carcinoma: a large retrospective French multicentric study. Pancreaticoduodenectomy is curative in the majority of patients with node-negative ampullary cancer. Nodal microinvolvement in patients with carcinoma of the papilla of Vater receiving no adjuvant chemotherapy. Influence of preoperative therapy on short- and long-term outcomes of patients with adenocarcinoma of the ampulla of Vater. Primary malignant melanoma of the common bile duct: a case report and literature review. Primary biliary malignant lymphoma clinically mimicking cholangiocarcinoma: a case report and review of the literature. Diagnostic benefit of biliary brush cytology in cholangiocarcinoma in primary sclerosing cholangitis. Biliary dysplasia in primary sclerosing cholangitis harbors cytogenetic abnormalities similar to cholangiocarcinoma. Precancerous bile duct pathology in end-stage primary sclerosing cholangitis, with and without cholangiocarcinoma. Primary sclerosing cholangitis as a premalignant biliary tract disease: surveillance and management. Intrahepatic ductal dilatation can be visualized easily, and the size of the bile duct can be documented. These limitations may be pronounced in obese patients due to the increased distance the ultrasound wave must travel, thereby reducing the resolution and depth of the image. Radiologic therapy of the biliary tract is performed via a percutaneous approach by interventional radiologists. The decision to proceed with an endoscopic or radiologic approach is often based on local expertise; other considerations include physician referral patterns, the location of a lesion within the biliary tract, failure of one method, and altered anatomy as a result of prior surgery. Solid material such as choledocholithiasis will appear as well-defined, dark filling defects within the bile duct. The cause remains unclear, but reports suggest that patients with preexisting kidney disease (renal failure) are at greatest risk. Images acquired in the axial plane can be reconstructed sagittally or coronally and reformatted 3 dimensionally. Bile ducts thus appear as low-attenuation structures that are best visualized if dilated. Aside from extrapancreaticobiliary structures, the transgastric approach provides images of the pancreatic neck, body, and tail, as well as the gallbladder and left intrahepatic ducts, whereas the transduodenal approach allows imaging of the pancreatic head, gallbladder, ampulla, and bile duct. A, Radiographic image showing contrast material injection into the biliary tract through a 19-gauge needle. A variety of catheters, guidewires, and stents are available to allow therapeutic interventions to be performed. A plastic pig tail stent is often placed within the metal stent to prevent stent occlusion. A, Radiographic image showing injection of contrast material into the biliary tract through a 19-gauge needle. Following fluoroscopic confirmation of guidewire placement, the echoendoscope and needle are removed, while the guidewire position is maintained. In the first, a duodenoscope is inserted alongside the guidewire and advanced to the ampulla, where the guidewire is found and used to assist in cannulation. Alternatively, the distal end of the guidewire can be grasped using a forceps or snare and withdrawn through the mouth, either through the accessory channel or along with the endoscope; a duodenoscope can then be back-loaded over the guidewire and advanced to the ampulla. By either method, the ultimate aim is to endoscopically provide relief of obstruction. Two meta-analyses of randomized trials of balloon sphincteroplasty versus sphincterotomy have shown that the rates of pancreatitis and need for mechanical lithotripsy are significantly higher, but the risk of bleeding is significantly lower, with balloon sphincteroplasty than with sphincterotomy.
Buy levitra professional with visa
Factors that influence fragmentation include the size erectile dysfunction myths and facts discount levitra professional 20mg on line, microcrystalline structure, and architecture of the stone. Although the composition of the stone does not influence successful lithotripsy, only cholesterol stone fragments are dissolved effectively by bile acid therapy, which can be used in combination with lithotripsy. Efficacy the percentages of patients who are free of stones after 6 and 12 months is 47% to 77% and 68% to 84%, respectively. Multiple small stone fragments seen 1 day after lithotripsy (B) have disappeared 6 weeks after lithotripsy (C). Side effects of lithotripsy include petechiae of the skin at the site of shock-wave delivery (8%), hematuria (4%), and liver hematomas (<1%). Biliary pain develops in approximately one third of patients; cystic duct obstruction develops in 5%; and complications of stone passage, such as biliary pancreatitis, develop in less than 2%. Open Cholecystectomy Karl Langenbuch, a surgeon in Berlin, is credited with performing the first cholecystectomy in 1882. Since then, cholecystectomy has remained the main therapeutic option for the management of patients with gallstones, largely because of its remarkable success in relieving symptoms and its low morbidity. In prospective studies, 90% to 95% of patients who undergo cholecystectomy experience substantial or complete relief of their symptoms. Bile Duct Stones Extracorporeal shock-wave lithotripsy has also been used in the management of choledocholithiasis. Intracorporeal electrohydraulic lithotripsy has been shown to be effective in this setting as well. These treatment options are reserved for patients who fail conventional endoscopic measures (see Chapter 70), mechanical lithotripsy, or surgical treatment of choledocholithiasis (see later). Appropriate indications for shock-wave lithotripsy are large stones impacted in the bile duct that are not amenable to endoscopic extraction, intrahepatic stones, stones above a biliary stricture, cystic duct remnant stones, and bile duct stones associated with Mirizzi syndrome (compression of the common hepatic duct) (see Chapter 65). Selection of patients for shock-wave treatment of bile duct stones is similar to that for treatment of uncomplicated gallbladder gallstones. Mild, transient hemobilia occurs in 10% of patients, and biliary sepsis develops in 4% following the procedure. Other complications are similar to those seen after lithotripsy for gallbladder stones. Because of the potential for septic complications, preprocedure endoscopic, nasobiliary, or percutaneous biliary drainage is performed. Technique the technique of open cholecystectomy has not changed substantially since its first description. After exploring the abdomen and taking down any adhesions to the gallbladder, the gallbladder is dissected from the gallbladder fossa in a retrograde fashion, from the fundus down to the infundibulum. When the gallbladder has been mobilized, the cystic artery and duct are readily identified. A cholangiogram may be performed to look for bile duct stones or to confirm the anatomy. An alternative approach is to perform a dissection of the triangle of Calot structures, as is done during laparoscopic cholecystectomy (see later), prior to removing the gallbladder from the liver. The triangle of Calot is the space bordered by the cystic duct, cystic artery, and inferior edge of the gallbladder. Dissection and identification of these structures permits safe division of the cystic duct and minimizes the chance of bile duct injury. For example, 7888 cholecystectomies were performed in Utah in 2005; 96% of these operations were laparoscopic cholecystectomies, and 4% were open procedures. A review of the National Hospital Discharge Database from 1997 to 2006 showed that 12% of Results the risk of open cholecystectomy has declined over the years. The mortality rate is considerably lower in patients operated on electively for biliary pain, with an average of less than 0. In a report of the entire Danish experience with cholecystectomy from 1977 to 1981, patients under 50 years of age had a risk of death of 0. Of 11,808 patients who underwent cholecystectomy at the New York Hospital-Cornell Medical Center between 1932 and 1978, the risk of death from elective cholecystectomy for chronic cholecystitis was 0. Likewise, the morbidity rate, mean length of hospital stay, and average hospital charges were significantly higher in the older patients than in the younger group. Most mortality following cholecystectomy is related to cardiac disease, particularly myocardial infarction. In a large survey of 28,621 patients who underwent cholecystectomy in the 1960s, complications occurred in 4. Complications related specifically to cholecystectomy include bile leaks, bile duct injury, and acute pancreatitis. Of these complications, bile duct injury is the most serious and often requires endoscopic therapy and, in some cases, complicated and technically difficult surgical repair. Alternatively, bile duct injury can lead to benign biliary stricture formation and bile duct obstruction with secondary biliary cirrhosis and liver failure. The rate of bile duct injury during open cholecystectomy is not known precisely but has been estimated to be 1 in 200 to 600 cases. Unusual amounts of bleeding, severe inflammation, and emergency operations do not play as great a role in these injuries as might be supposed. Early postoperative mortality following cholecystectomy in the entire female population of Denmark, 1977-1981. Historically, laparoscopic cholecystectomy was an outgrowth of diagnostic laparoscopy and the early efforts of gynecologists at operative laparoscopy. The development of laparoscopic cholecystectomy was predicated on technical advances in miniaturized video cameras and other specialized equipment. Prophylactic antibiotics are not administered routinely to patients with uncomplicated gallstone disease, including biliary pain. Sequential compression stockings are used to reduce the risk of lower extremity thromboembolism. To view the abdominal contents and provide room for instruments, a space is developed by inducing a pneumoperitoneum Laparoscopic Cholecystectomy After the first reports in the late 1980s, laparoscopic cholecystectomy rapidly gained acceptance as the technique of choice for the management of the patient with biliary pain and complications of gallstones. Pneumoperitoneum is achieved by either a closed technique in which a Veress needle is inserted into the peritoneum through a small incision, followed by placement of an operating trocar, or by a direct, open technique in which the operating trocar is placed directly into the abdomen under direct visualization through a small incision. After the pneumoperitoneum has been established, a trocar is placed at the umbilicus and a laparoscope is introduced. Three additional trocars are placed in the upper abdomen under direct vision for inserting operating instruments and retractors. In this approach, the entire hepatocystic triangle is dissected, exposing the cystic duct and artery, infundibulum of the gallbladder, and junction of the gallbladder and cystic duct, before a cholangiogram is performed or the cystic duct and artery are divided. The assistant retracts the gallbladder fundus cephalad, anterior to the liver, and the infundibulum laterally. The surgeon, operating through the epigastric port, identifies and dissects the cystic duct and artery circumferentially. Special care must be taken to identify the junction of the cystic duct and gallbladder, to ensure that the bile duct has not been isolated inadvertently. If the cholangiogram shows normal anatomy and no evidence of choledocholithiasis, the cholangiocatheter is removed and the cystic duct and artery are divided between small metal clips. The gallbladder is then dissected out of the liver bed and delivered through the umbilical incision, usually with a specimen retrieval bag. Care is taken to avoid perforation of the gallbladder during its dissection from the liver because the spillage of gallstones and bile has been shown to increase the risk of postoperative fever and intra-abdominal abscess formation. In the 2010s, laparoscopic cholecystectomy has been performed by some surgeons using a single-incision laparoscopic surgery approach in which the operating surgeon introduces the laparoscope and surgical instruments into the abdomen via a single operating port placed at the umbilicus. This technique has the advantage of improved cosmetics over the traditional 4-port laparoscopic approach. The single-incision laparoscopic surgery procedure has not gained wide acceptance because of longer operating times, higher cost, a higher rate of wound complications and hernias, and, possibly, a higher rate of bile duct injury. Large population studies from Australia and Sweden have demonstrated the importance of routine intraoperative cholangiography in decreasing the frequency of major bile duct injuries. Despite these observations in favor of routine cholangiography, the low frequency of unsuspected bile duct stones and low rate of bile duct injury serve as the basis for most surgeons adopting a selective approach to using cholangiography. Cholangiography is done when the history is suggestive of possible bile duct stones.
Generic levitra professional 20mg free shipping
The added diagnostic value of post reflux swallow induced peristaltic wave index and nocturnal baseline impedance in refractory 1reflux disease studied with on therapy impedance monitoring erectile dysfunction what is it order 20mg levitra professional overnight delivery. Association of esophagitis and esophageal strictures with diseases treated with non-steroidal anti-inflammatory drugs. The role of diet and lifestyle measures in the pathogenesis and treatment of gastroesophageal reflux disease. Relationship between the acidity and osmolality of popular beverages and reported postprandial heartburn. Medical and surgical management of reflux esophagitis: a 38-month report on a prospective clinical trial. Self-selection and use patterns of over-the-counter omeprazole for frequent heartburn. Review article: promotility drugs in the treatment of gastro-oesophageal reflux disease. Effect of azithromycin on acid reflux, hiatus hernia and proximal acid pocket in postprandial period. Ranitidine controls nocturnal gastric acid breakthrough on omeprazole: a controlled study in normal subjects. Gastric acid control with esomeprazole, lansoprazole, omeprazole, pantoprazole and rabeprazole: a five-way crossover study. Efficacy and safety of lansoprazole in the treatment of erosive reflux esophagitis. Oral pantoprazole for erosive esophagitis: a placebo-controlled, randomized clinical trial. Short-term management of refractory reflux esophagitis with different doses of omeprazole or ranitidine. Esomeprazole (40 mg) compared with lansoprazole (30 mg) in the treatment of erosive esophagitis. Outcomes of atypical symptoms attributed to gastroesophageal reflux treated by laparoscopic fundoplication. Traditional reflux parameters and not impedance monitoring predict outcome after antireflux surgery in extraesophageal reflux. Value of preoperative esophageal function studies before laparoscopic antireflux surgery. Continued (5-year) follow-up of a randomized clinical study comparing antireflux surgery and omeprazole in gastroesophageal reflux disease. Aspiration between laparoscopic anti-reflux surgery and recurrence of gastroesophageal reflux. Long-term outcome of medical and surgical therapies for gastroesophageal reflux disease: follow-up of a randomized controlled trial. No evidence for efficacy of radiofrequency ablation for treatment of gastroesophageal reflux disease: a systematic review and meta-analysis. Oesophagitis is as important as oesophageal stricture diameter in determining dysphagia. Long-term omeprazole treatment in resistant gastroesophageal reflux disease: efficacy, safety, and influence on gastric mucosa. Systematic review of the risk of enteric infections in patients taking acid suppression. A prospective, randomized, double-blind, placebo-controlled trial of endoscopic steroid injection from recalcitrant esophageal peptic strictures. Systematic review: the role of self-expanding plastic stents for benign esophageal strictures. Outcome of oesphageal selfdilation for patients with refractory benign oesophageal strictures. However, some authorities argue that cardiac-type mucosa, which is composed almost exclusively of mucus-secreting cells, also is metaplastic,4 has malignant predisposition, and can be considered diagnostic of Barrett esophagus. Barrett esophagus is the condition in which an abnormal columnar epithelium that has both gastric and intestinal features and that is predisposed to malignancy replaces the stratified squamous epithelium that normally lines the distal esophagus. The columnar-lined esophagus causes no symptoms, and the condition has clinical importance only because it is a risk factor for esophageal adenocarcinoma, a tumor whose frequency has increased more than 7-fold over the past several decades. The condition is rare in children younger than age 10 and virtually nonexistent in children younger than age 5. In the general adult population of Western countries, the prevalence of Barrett esophagus (predominantly short segment) is between 1. However, more recent studies suggested that the cancer risk for such patients is even lower, in the range of only 0. First, the endoscopist must ascertain that columnar epithelium lines 1 cm or greater of the distal esophagus. Second, biopsy specimens of that columnar epithelium must show evidence of metaplasia, which is a change from one adult tissue type to another. Endoscopically, columnar epithelium has a reddish color and velvet-like texture that can be distinguished readily from normal esophageal squamous epithelium, which is pale and glossy. There is disagreement among experts regarding the histologic type of epithelium required to confirm that there is metaplasia in the esophagus. The reddish color and velvet-like texture of the Barrett epithelium contrast sharply with the pale and glossy appearance of the esophageal squamous epithelium. Obesity also is associated with elevated serum levels of proproliferative hormones such as insulin-like growth factor I and leptin, and with decreased levels of the antiproliferative hormone adiponectin, factors that may contribute to carcinogenesis in Barrett esophagus. It has been proposed that the declining frequency of infection with Hp in Western populations also may be contributing to the rising frequency of esophageal adenocarcinoma (see Chapter 48). Individual patients may exhibit any, all, or none of those abnormalities, and their prevalence in Barrett esophagus is disputed. For example, some investigators have described normal gastric acid secretion in patients with longsegment Barrett esophagus. Unlike squamous cells, for example, Barrett cells secrete mucins and express the tight-junction protein claudin 18, features that render the epithelium more resistant to acidpeptic attack. The boxes in orange are the facilitating features such as genomic instability and a tumor-promoting microenvironment that may allow Barrett cells to quickly acquire the physiologic attributes of cancer cells. More recently, Hanahan and Weinberg added 2 additional physiologic hallmarks of malignancy: the ability to reprogram energy metabolism to support continuous proliferation, and the ability to evade destruction by immune cells (T and B lymphocytes, macrophages, and natural killer cells). Although a single such alteration may have multiple disparate effects, conceptually it can be useful to classify the alteration according to the major physiologic cancer attributes that it endows. Insensitivity to antigrowth signals occurs primarily through the inactivation of tumor suppressor genes. Reactivation of the enzyme telomerase, which enables the cells to replace telomeres needed for cell division, can endow the cells with limitless replicative potential. Neoplasms can increase their vascular supply by secreting angiogenic factors such as vascular endothelial growth factor. Finally, for neoplastic cells to invade and metastasize, they must dissociate themselves from surrounding cells by disrupting cell adhesion proteins such as the cadherins and catenins, and by degrading the extracellular matrix through the secretion of enzymes such as matrix metalloproteases. In Barrett esophagus, the acquisition of these core physiologic attributes of malignancy is facilitated by genomic instability and a tumor-promoting microenvironment. Although there have been some promising studies, especially those using panels of biomarkers,49 gastroenterology societies presently do not endorse the routine clinical use of biomarkers for clinical management of patients with Barrett esophagus. Recent advances in genomic techniques such as whole-genome sequencing and whole-exome sequencing (which is limited to gene coding regions) have contributed greatly to knowledge of how Barrett cells become tumor cells. Oncogene activations appear to occur later, because they are found only in dysplastic and cancerous tissues. The identification of novel gene-environment interactions by these new "omics" approaches may well revolutionize our understanding of how Barrett esophagus develops and progresses to esophageal adenocarcinoma. Dysplasia (also called intraepithelial neoplasia) can be viewed as the histologic expression of genetic and epigenetic alterations that favor unregulated cell growth. Dysplasia is categorized as low grade or high grade depending on the degree of histologic abnormalities, with more pronounced abnormalities assumed to reflect more severe genetic damage and greater potential for carcinogenesis. Pathologists have difficulty distinguishing low-grade dysplasia in Barrett esophagus from reactive changes caused by reflux esophagitis, and interobserver agreement for the diagnosis of low-grade dysplasia may be less than 50%. Interobserver agreement is better (approximately 85%) for high-grade dysplasia, but there is substantial disagreement among pathologists in distinguishing high-grade dysplasia from intramucosal carcinoma (see Chapter 48). In the traditional pathway, step-wise accumulation of alterations in the tumor suppressor gene p16, followed by oncogene activation, and genomic instability eventually lead to cancer formation.
Buy levitra professional 20 mg fast delivery
This approach erectile dysfunction drugs cialis cheap levitra professional 20 mg online, combined with restriction of alcohol, tobacco, and estrogen, has been shown to produce remission. Based on the observation that skin-related symptoms are inversely related to skin pigmentation, agents such as oral -carotene have been suggested to improve sunlight intolerance; however, systemic reviews have found insufficient evidence to confirm efficacy. The incidence is higher in northern Europe (1 per 8000) and in the SaguenayLac-St. Jean region of Quebec, Canada (1 per 1846), where a founder effect has been documented. In a multicenter study, van Spronsen and associates showed that 77% of patients with tyrosinemia presented before the age of 6 months. The 1- and 2-year survival rates were 38% and 29%, respectively, if patients presented between birth and 2 months of age, and 74% and 74%, respectively, if they presented between 2 and 6 months. Survival for both time intervals rose to 96% if the first symptoms appeared after age 6 months. These patients usually present after one year of age with hepatomegaly, rickets, nephromegaly, hypertension, and growth retardation. The pathologic changes in the liver differ between the acute and chronic forms of the disease. In the acute form, the liver may appear enlarged with a pale nodular pattern or may be shrunken, firm, and brown. Micronodular cirrhosis, fibrotic septa, bile duct proliferation and plugging, steatosis, pseudoacinar and nodular formations, and giant cell transformation may be found on histologic examination. Patients with the chronic form of the disease have a higher level of reversion and a lower frequency of liver dysplasia. In histologic specimens, micronodular and macronodular cirrhosis may be present, as may steatosis, fibrotic septa, and a mild lymphoplasmacytic infiltrate. If the specific gene mutation in a family is known, early genetic diagnosis can be made from chorionic villus biopsy specimens as well. Treated patients exhibited improved liver synthetic function, as reflected by a shortening of the prothrombin time, as well as decreased serum aminotransferase levels and a reduction in liver parenchymal heterogeneity and nodules on imaging. This step requires the cofactor N-acetyl glutamate, which is synthesized from N-acetyl CoA and glutamic acid by N-acetyl glutamate synthetase. Arginase then catalyzes the breakdown of arginine to urea and ornithine in the final step of the pathway. Several amino acid transporters, such as citrin, an aspartate/glutamate carrier protein that supplies aspartate to the urea cycle, are involved in shuttling metabolites into the urea cycle. Excess nitrogen in the form of amino acids can be shunted to alternative pathways of waste-nitrogen excretion by the medicinal use of sodium benzoate and sodium phenylacetate, leading to the generation of hippurate and phenylacetylglutamine, respectively. Later presentations (>30 days) have been reported in up to two thirds of patients,169,170 and late-onset adult presentations have been reported in cases associated with an illness or dietary change171,172 or with psychiatric symptoms, which may be the initial presenting feature. Symptoms include irritability, poor feeding, vomiting, lethargy, hypotonia, seizures, coma, and hyperventilation, all secondary to hyperammonemia. Genetic defects in each of these enzymes have been reported, and their overall incidence has been estimated to be 1 in 35,000 births, although partial defects may make the number much higher. Alternative pathways that are used therapeutically for waste nitrogen disposal are also illustrated (dotted lines). Urine Argininosuccinase Fumarate levels of less than 200 mol/L and greater than 1000 mol/L, respectively. Blood gas analysis shows respiratory alkalosis secondary to the hyperventilation caused by the effects of ammonia on the central nervous system. Blood urea nitrogen levels are typically low but can be elevated during times of dehydration or hypoperfusion. Neurologic symptoms, which can also be episodic, include ataxia, developmental delays, behavioral abnormalities, combativeness, biting, confusion, hallucinations, headaches, dizziness, visual impairment, diplopia, anorexia, and seizures. Such episodes can be precipitated by high-protein meals, viral or bacterial infections, medications, trauma, or surgery. Infants may present after being weaned from breast milk to infant formulas, which have a higher protein content. Symptoms can mimic those of other acute neonatal problems, such as infections, seizures, and pulmonary or cardiac disease. Later presentations can mimic other behavioral, psychiatric, or developmental disorders. The first clue may be an elevated serum ammonia level with near normal serum aminotransferase levels and without metabolic acidosis. Direct enzyme analysis can be performed and can be useful in patients who have a partial deficiency or who present in adulthood. Early neonatal diagnosis leads to improved survival, so prenatal enzyme and genetic linkage analysis can be carried out in family members of known carriers to aid in early diagnosis. The use of oral lactulose to lower the nitrogen load has not been studied in this patient population. Given the extremely high ammonia levels often encountered, continuous arteriovenous hemodialysis or hemofiltration is frequently required. Arginine, carnitine, and long-chain fatty acids are usually present in low levels in these patients and should be supplemented. Further therapy and protein restriction are then tailored to the patient; those with a severe disorder may need essential amino acids to supplement their protein intake. Further studies examining the outcome of treatment compared with the type of dietary therapy and nutritional support received are needed. A possible exception to this is in patients transplanted before the age of one year, in whom developmental, and possible neurocognitive, outcomes may improve. Hyperammonemia is unusual in affected persons, but hyperammonemic coma and death have been reported. The disease is characterized by indolent deterioration of the cerebral cortex and pyramidal tracts, leading to progressive dementia and psychomotor retardation, spastic diplegia progressing to quadriplegia, seizures, and growth failure. Many guanidine compounds may accumulate in the blood and cerebrospinal fluid of these patients, which could play an important pathophysiologic role, and guanidinoacetate, a well-known potent epileptogenic compound, has demonstrated usefulness as a target for the therapeutic monitoring of patients with arginase deficiency. The diagnosis is confirmed by enzymatic analysis, which can be performed prenatally on cord blood samples. Treatment consists of protein restriction and, when needed, sodium phenylbutyrate. With advances in molecular biology, genetics, and mass spectrometry, several different inborn errors in bile acid synthesis and transport have been identified as causes of clinical disease. For some of the disorders, this progress has led to improved diagnosis and life-saving therapy. These complementary tests allow rapid, sensitive, and cost-effective bile acid profiling and mutation screening to aid clinical diagnosis in patients with intrahepatic cholestasis. Secondary metabolic defects that impact primary bile acid synthesis include peroxisomal disorders, such as cerebrohepatorenal syndrome of Zellweger and related disorders, and Smith-Lemli-Opitz syndrome. The former bypasses the enzymatic block and provides negative feedback to earlier steps in the synthetic pathways, whereas the latter displaces toxic bile acid metabolites and serves as a hepatobiliary cytoprotectant. Deficiency of 4-3-oxosteroid 5-reductase usually leads to neonatal cholestasis, which rapidly progresses to synthetic dysfunction and liver failure. Clinical symptoms and signs include adult-onset progressive neurologic dysfunction. After significant neurologic pathology is established, the effect of treatment is limited and deterioration may continue. In some patients, liver disease with features of a cholangiopathy has been present. Oral glycocholic acid therapy has been shown to be safe and effective in improving growth and fat-soluble vitamin absorption in children and adolescents with these disorders. Therefore, determining whether these changes are primary or secondary to the liver dysfunction may be difficult, and a detailed biochemical evaluation is necessary. Initially, defects in bile acid synthesis were discovered with the use of liquid secondary ionization mass spectrometry; specifically, fast atom bombardment ionization mass spectrometry allowed direct analysis of bile acids from a drop of urine. More advanced mass spectrometry approaches, including electrospray ionization tandem mass spectrometry, as well as gene sequencing techniques, have subsequently been applied. The mass spectra generated permit accurate identification of the absence of primary bile acids and presence of atypical bile acids specific to each primary defect. This disorder is caused by deficient activity of the second step in the bile acid synthetic pathway, the conversion of 7-hydroxycholesterol into 7-hydroxy-4-cholesten-3-one. This reaction is catalyzed by a microsomal 3-hydroxy-5-C27steroid oxidoreductase; deficiency of this enzyme results in the accumulation of 7-hydroxycholesterol within the hepatocyte.