Cheap orlistat 120 mg amex
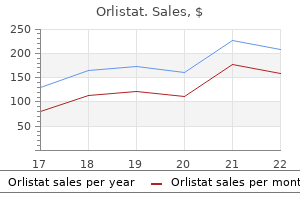
She has no symptoms to suggest a rare cause of secondary hypertension weight loss in a month discount orlistat master card, pheochromocytoma (0. She attributes her weight gain to being somewhat less active due to symptomatic knee osteoarthritis. Leading Hypothesis: Atherosclerotic Renal Artery Stenosis Textbook Presentation Patients generally have either very abrupt hypertension, hypertension that worsens over 6 months, or hypertension refractory to treatment with 3 drugs. The classic patient with atherosclerotic renal artery stenosis has other vascular disease (cerebrovascular disease, coronary artery disease, peripheral arterial disease) or risk factors such as smoking or diabetes. Does not necessarily cause hypertension and can exist in patients with essential hypertension. Renovascular hypertension means hypertension caused by renal hypoperfusion as a result of renal artery stenosis. Some patients with bilateral renal artery stenosis present with episodic, unexplained pulmonary edema ("flash pulmonary edema"); echocardiograms in such patients show normal systolic function. One study reported that, in a population of high-risk patients, a 20% increase in creatinine had 100% sensitivity and 70% specificity for the diagnosis of renal artery stenosis (defined as > 50% bilateral stenosis). Sudden, unexplained pulmonary edema; unexplained heart failure; refractory angina 6. Should listen over all 4 abdominal quadrants and also spine and flanks between T12 and L2 2. Must differentiate between systolic bruits and continuous (systolic and diastolic) bruits a. Hypokalemia is often seen as a result of stimulation of aldosterone release; metabolic alkalosis is also often seen. Can also be therapeutic through performance of angioplasty or placement of stent in the rare cases this is indicated b. Complications include bleeding, dissection, embolization, and contrast nephropathy. Duplex ultrasonography (2-dimensional ultrasound imaging combined with Doppler flow measurements) a. Results can vary depending on the level of experience of the technician and the body habitus of the patient. Randomized, controlled trials have not shown that stenting is better than medical therapy with regard to preventing progression of renal disease or cardiovascular events. Have you crossed a diagnostic threshold for the leading hypothesis, renovascular hypertension Primary aldosteronism needs to be considered in patients with resistant hypertension, especially those with hypokalemia. Alternative Diagnosis: Primary Hyperaldosteronism Textbook Presentation Primary hyperaldosteronism is usually diagnosed when a patient with hypertension has unexplained hypokalemia or when a patient has resistant hypertension. Rarer causes include microadenomas, unilateral adrenal hyperplasia, and adrenal carcinoma. Prevalence uncertain in patients with hypertension and unprovoked hypokalemia; 1 study reported a prevalence of 50% C. Because aldosterone is being produced autonomously, it is not suppressed by volume expansion, as it is normally. Most patients have a normal potassium level; 48% of those with aldosterone-producing adenomas and 17% of those with bilateral adrenal hyperplasia are hypokalemic. There are 3 steps in the diagnosis of primary hyperaldosteronism: screening, confirmatory testing, and determining the subtype. Ideally, prior to measurement, the patient should have a normal potassium level and liberal sodium intake. Laparoscopic adrenalectomy should be considered when lateralized aldosterone excess is demonstrated by adrenal vein sampling. You stop the hydrochlorothiazide, substituting chlorthalidone, a longer acting diuretic. He ran out of his medications 6 months ago and was unable to obtain refills because of financial problems. J falls into the "hypertensive urgency" rather than the "hypertensive emergency" category. Nevertheless, hypertensive emergency is always the "must not miss" diagnosis in such patients (Table 23-10). On further history, he has no shortness of breath, chest pain, edema, abdominal pain, feelings of confusion, vomiting, or focal weakness or numbness. Lungs are clear, jugular venous pressure is not elevated, there is an S4 and a 2/6 systolic ejection murmur without an S3, abdomen is nontender, there is no peripheral edema, and neurologic exam is normal. Hypertensive urgency or emergency occurs in about 1% of adults with hypertension; with urgency occurring in three-quarters of these patients. The most common presenting symptoms are headache (22%), epistaxis (17%), faintness (10%), psychomotor agitation (10%), chest pain (9%), and dyspnea (9%). There are several ways to approach treatment, depending on the overall condition of the patient, whether the patient has been treated previously, and the ability of the patient to return for follow-up. In patients who have stopped their medications, it is usually sufficient just to restart them. Beginning treatment with more rapid-acting agents, such as oral labetalol or clonidine, and then transitioning to longer acting agents; patients can be observed for several hours to assess their response to the short-acting agents. J wants to know if he can have a couple of acetaminophen tablets for his headache, get his prescriptions, and leave; he has to pick up his son at school. Have you crossed a diagnostic threshold for the leading hypothesis, hypertensive urgency Alternative Diagnosis: Hypertensive Emergencies Patients with hypertensive emergencies frequently present with chest pain (27%), dyspnea (22%), and neurologic deficits (21%). Cerebral infarction is found in about 24% of patients, with about 22% having pulmonary edema, 16% hypertensive encephalopathy, and 12% heart failure. Acute coronary syndromes, aortic dissection, subarachnoid hemorrhage, and pulmonary edema are discussed in other chapters. Textbook Presentation Patients present with the acute or subacute development of lethargy, confusion, headache, and visual disturbances, sometimes followed by seizures (focal or generalized) and coma. Failure of autoregulation leads to cerebral vasodilation, endothelial dysfunction, and cerebral edema. Generally in the posterior regions of the brain due to relatively sparse sympathetic innervation of the vertebrobasilar territory leading to more disruption of autoregulatory mechanisms, increased perfusion, and edema 3. There is little evidence to guide the choice of agents; commonly used medications include labetalol, esmolol, fenoldopam, clevidipine, nitroprusside, and nicardipine. J has no signs or symptoms of stroke, intracranial hemorrhage, pulmonary edema, myocardial ischemia, or aortic dissection. He has a headache, but he does not have other symptoms, such as lethargy or confusion, to suggest hypertensive encephalopathy. You instruct him to fill his prescriptions after he picks up his son at school, to take the amlodipine tonight, and then to take all 3 medications in the morning. Table 23-11 lists symptoms, taken from a series of patients with pheochromocytoma, about half of whom presented with paroxysmal hypertension and about half of whom had persistent hypertension. Pretest probability of 4% in patients with incidentally discovered adrenal masses C. Plasma free metanephrine is the single best test to rule out pheochromocytoma (Table 23-12). Patients should fast overnight and be supine for 20 minutes prior to the blood draw. Because caffeine and acetaminophen interfere with the assay, patients should avoid caffeine for 12 hours and acetaminophen for 5 days prior to testing. The overall (sporadic and hereditary cases) sensitivity at this cut off is 99% with a specificity of 89%. A plasma metanephrine > 236 ng/L is 100% specific for the diagnosis of pheochromocytoma.
Orlistat 120mg low cost
The A-V valves exhibit no specific lesions weight loss pills johannesburg generic orlistat 60 mg with amex, and the semilunar valves are entirely unaffected. On the right side, the ventricular configuration results in filling and obliterating the ventricular cavity with a mass of thrombus and organizing fibrous tissue. Although it may detach and produce a massive embolus in rare cases, the thrombus is usually firmly attached and does not loosen, so infarctions are uncommon. Beneath the thickened endocardium, there are small blood lagoons-dilated thebesian veins-and from these and the endocardial scar tissue, tongues of fibrous tissue extend into the inner third or half of the myocardium, but never involve its full thickness. The major coronary vessels are normal; no changes are seen in the minor vessels except for an occasional small focus of inflammatory cells and, in late stages when fibrosis is severe, an obliterative arteritis. Severe calcification may develop in the valve or mural endocardium, which is important radiologically, indicating that the constriction is endocardial, not pericardial, although a large pericardial effusion may be present. The heart weight may be increased but is often reduced, and despite the voluminous atria, the ventricles often are small and shrunken. The disease may be biventricular, and the clinical manifestations may change depending on which ventricle is most diseased. Patients have high Characteristic recession of right apex, forming bizarre notch: enlargement of right atrium Dense collagen layer lining left ventricle, involving posterior papillary muscle and chordae tendineae, demarcated by a ridge, sparing outflow tract; posterior mitral cusp adherent to wall; mural thrombi central venous pressure and may show exophthalmos. The posterior A-V valve cusp is severely damaged regardless of the ventricle affected, with resulting mitral and tricuspid incompetence and usually stenosis. Whatever the cause, the pathogenesis is destruction of the endocardium and underlying myocardium of the ventricular-inflow areas, with the formation of scar tissue. Elastic tissue in the affected areas is almost entirely lost, and elastosis is infrequently seen, except at the edges of the scar. At autopsy the changes of congestive heart failure are seen, usually with considerable effusion into the serous cavities. However, electron microscopy shows swelling and necrosis of the endothelial cells, an eosinophilic infiltration of both the endocardium and the thebesian veins, focal necrosis of myocardial fibers with an eosinophilic infiltration, and an eosinophilic arteritis of the small coronary arteries with an occasional focus of fibrinoid necrosis. Scar tissue may cover the papillary muscle and shorten and thicken the chordae tendineae, thus distorting the A-V valve, which itself usually exhibits valvulitis with vegetations. The myocardium has areas of necrosis, sometimes with frank hemorrhage, organization, and scarring; the lesions often involve the full thickness of the ventricular myocardium. Between the myocardium and the thickened endocardium, small blood lagoons may be detected in dilated thebesian veins. A great eosinophilic infiltration usually is present in the necrotic and fibrosing areas of the myocardium. The original endocardium is largely destroyed, replaced by scar tissue with some elastosis. In more chronic cases, tissue eosinophilia may diminish or disappear, the arteries show only an obliterative arteritis, and severe endomyocardial scarring is found, usually maximal at the apex and spreading to involve the endocardial inflow and outflow tracts. The basic arteritis may result in cerebral, abdominal, or renal manifestations initially, or arthralgias, muscle pains, and in some cases polyneuritis. High blood eosinophil count is most important in diagnosis, with levels as high as 130,000 cells/mm3 reported. It appears to be a specific type of heart disease, the basic lesion a form of verrucous angiitis that especially affects the subendocardial blood vessels. At any stage that death occurs, severe lesions of congestive heart failure with large effusions in the serous cavities are found, as well as multiple infarctions in the lungs and often in the brain, spleen, kidneys, and other organs as well. Mural thrombi are present in the ventricles and may be small or may cover two thirds of the mural endocardium, interfering mechanically with A-V valve function. The heart valves show no specific lesions, and the main coronary arteries are normal. In acute cases the endocardium not covered by thrombus is neither thickened nor opaque, although a fine surface deposition of fibrin may be seen. Small, dark spots may be visible, representing hemorrhagic polyps on the endocardial surface. In more chronic cases, irregular plaques of fibroelastotic endocardial thickening are found, scattered irregularly over the inflow and outflow tracts, but most evident at the apex. The focal fibrin deposits may form polyps, and hemorrhaging polyps may produce the black spots. In the acute stages the myofibers show little change, and the loss of striation, nuclear hyperchromatism, and fragmentation appear to be anoxic. The episodes may be repeated over many months, with the intervals of improvement progressively shorter and periods of congestive failure progressively protracted. It has a seasonal incidence, as does adult cardiovascular beriberi, in regions where the disease is caused by a diet deficient in a simple staple such as husked rice. Beriberi is sometimes seen as an acute disease in alcoholic patients with a restricted diet. The crucial feature of all these types is that they respond to adequate thiamine quickly, except in the most severe terminal cases. The heart must increase its workload to meet the demand of this hyperkinetic circulation, and the rapid return of blood to the heart leads to disproportionate right-sided dilatation and hypertrophy. The basic change apparently is in the peripheral circulation, with a great opening of arteriovenous anastomoses, especially in striated muscles. When terminal, death results from the sudden failure of the heart to meet the sustained call for high output. It has been impossible thus far to define specific changes caused by thiamine deficiency in human hearts with cardiovascular beriberi. The hearts invariably exhibit a degree of right-sided dilatation and hypertrophy, but the microscopic findings may show only myofiber hypertrophy, with enlargement and hyperchromatism of the nuclei, which are cigar shaped or blunt ended. Watery vacuolation of the myofibers and interstitial edema have often been recorded, along with fatty infiltration and varying degrees of myocardial fibrosis. The lesions seen in animals are similar to those induced by extreme potassium deficiency, but a combination of thiamine and potassium deficiency does not produce the lesions. Thiamine deficiency may occur in otherwise wellnourished individuals; most patients have diets typically low in protein and fat but high in carbohydrates, thus developing multiple deficiencies. In the light of current views on the metabolic derangements in thiamine deficiency, it seems unlikely that a state of chronic beriberi heart disease could exist. The cause of the cardiomegaly is still obscure in some patients, including women later in pregnancy or in the postpartum state, called peripartum cardiomyopathy. In many cases, alcohol is the most important factor, although similar conditions also affect those who do not drink alcohol. Radiologic and ultrasonic examination is usually unhelpful other than in demonstrating a grossly enlarged heart, which typically continues to increase in size. Unfortunately, if the cause was not found in life, it cannot be satisfactorily established at autopsy. Evidence of congestive heart failure is found with an enlarged heart, compounded by varying degrees of hypertrophy and dilatation. The endocardium may be normal or covered in part by mural thrombi, or may be patchily thickened and opaque. Cellular infiltration of variable intensity is seen; the cell types vary but typically include Greatly enlarged heart Greatly dilated and moderately hypertrophied heart. Little or no fibrosis of endocardium; mural thrombi in left ventricle and left auricle Thrombus Diffuse foci or irregular fibrosis, replacing cardiac muscle fibers Infiltation of cardiac muscle with lymphocytes and monocytes; edema and occasional giant cell Vacuolation of myocardial fibers and interstitial edema similar to that seen in beriberi an infiltrate of lymphocytes and monocytes and occasionally a giant cell. The most common findings are four-chamber enlargement, left ventricular hypokinesis, and decreased fractional shortening. However, in the presence of highly active antiretroviral therapy, these manifestations are relatively rare. Pulmonary hypertension, which is more commonly seen in the younger population, is usually caused by left ventricular dysfunction. Any use of injected drugs can transmit bacteria (most often Staphylococcus aureus) from the skin into the bloodstream. This can result in septic emboli to the lung, pneumonia, and infective endocarditis of any valve, especially tricuspid and pulmonary. Tobacco smoking increases sympathetic activity and catecholamines, constricts blood vessels, and increases blood pressure. Although there is some evidence that light intake of alcohol is beneficial, it is not recommended that a person who does not drink alcohol should start, since even low levels of alcohol may increase blood pressure.
Cheap orlistat 60 mg mastercard
Some become large enough that they cause lung hypoplasia and can also impede caval blood return weight loss pills that really work by dr oz orlistat 120mg visa, thus causing polyhydramnios and hydrops fetalis. In patients who are in no distress after birth, resection is usually delayed until the child is between six and 18 months of age. The risks of infection and cancer remain the major indications for elective resection. Bronchoalveolar carcinoma, pleuropulmonary blastoma, and rhabdomyosarcoma have been reported to arise in these lesions, but the incidence is considered very low. The most common procedure is a lobectomy, although segmentectomy has been reported as well. They may also occur in the abdomen, usually in the vicinity of the left adrenal gland. Most intralobar sequestrations are found in the lower lobes, with only 15 percent in the upper lobes. It is important to remember that there may be a communication of the sequestration with the foregut (esophagus or stomach). Most patients should have a minimum baseline measurement of hemoglobin, and a type and screen with blood readily available in complex resections (see Chapter 12, Bronchoscopy, for additional discussion). Principles of pulmonary resection access to the lung anesthesIa consIderatIons Many lung operations in children can be successfully performed using a standard endotracheal tube without single lung ventilation. If required, single lung ventilation can be accomplished in infants and young children by either selective main stem intubation or the use of bronchial blockers, which make the main stem intubation usually technically easier and more reliable. However, for lobectomies, it is preferable to have the ipsilateral lung decompressed. Postoperative pain relief after a thoracotomy is another important consideration, and the use of thoracic epidurals should be liberally considered. Epidurals Operations on the lung can be performed in two ways, via thoracotomy or thoracoscopy. The second is a posterolateral thoracotomy, which is the most common method used for open lung resections. A third approach through a prone position is employed to reduce spillover of infected secretions into the contralateral lung. However, with modern anesthesia techniques allowing single lung ventilation, as well as more effective antimicrobial therapy, this approach is less common. A median sternotomy is used by some surgeons when bilateral wedge resections are required, such as in osteosarcoma metastases. The incision is performed below the level of the nipple in the fourth, fifth, or sixth interspace, taking care not to injure the breast bud in a prepubertal female. The ribs are approximated loosely with an absorbable pericostal stitch (polygalactin). The muscle fascia is approximated with a running absorbable suture, followed by subcutaneous closure with either a running or interrupted suture and subcuticular closure of the skin (both with absorbable suture). The upper arm is allowed to lie on the same side with support to prevent excessive stretching of the arm as well as the brachial plexus. A wide preparation is done from the vertebral column posteriorly to the sternum anteriorly. The nipple and areola are marked, as is the tip of the scapula, to help guide the incision. These muscles may be partially or completely divided as needed to gain wider access during the operation. Care is taken not to divide the paraspinal muscles, but to free them up longitudinally. After the resection is performed, a chest tube may be placed a couple of interspaces below the incision. Lung biopsies, wedge resections, and lobectomies can be performed using this approach. The clear benefits in cosmesis, decreased pain and length of stay, and potentially less scoliosis have been the driving forces, but have yet to be proven. For thoracoscopic resections of any kind, the patient is placed in a decubitus position, as described previously. It is important to extensively use gravity as a retractor and the surgeon should vary the position accordingly. A Veress needle is placed into the chest carefully just above a rib to avoid the neurovascular bundle. These positions are variable and can move one or two interspaces up or down as needed, and for lobectomy are typically located in the anterior axillary line. Upon completion of the procedure, a chest tube may be placed through one of the dependent port sites and secured. Indications for biopsy include infectious processes, diffuse parenchymal diseases, and presence of lung nodules where a diagnosis of an inflammatory or malignant process is being considered. Thoracoscopic procedures allow visualization of the entire lung making a small wedge resection easy to perform with a stapling device. An open operation with a small anterolateral thoracotomy is also a reasonable technique for a wedge biopsy with a stapling device. The apex is visualized and wedges of parenchyma with blebs are removed using an endoscopic stapling device. Again, if there is an air leak from the staple line, a further firing of the device after removing the blade or using a stapler that has been reinforced with bovine pericardium may be helpful. Fibrin glue can be applied over the staple line as an adjuvant to help control air leaks. The most important considerations are adequate visualization and exposure of the hilar structures, namely, the blood vessels and bronchus. In most instances, it is better to dissect out and control the pulmonary arterial branches first, venous drainage second, and the bronchus last. Occasionally, as in the case of a severe, purulent infectious process, it is better to divide the bronchus first. The anatomic considerations involved in the removal of different lobes will now be discussed in detail. The surgeon must have a complete understanding not only of the normal anatomy but also of the variations in anatomy that are frequently encountered during lung resections. It should be noted that considerable variation in vascular anatomy occurs, but the usual pattern is shown in the illustration. The first vessel to be encountered will be the superior pulmonary vein which will have the upper and middle lobar branches. The main pulmonary artery is identified behind the superior pulmonary vein, and dissection is carried out peripherally to expose the superior and inferior pulmonary arterial trunks. The superior pulmonary arterial trunk, with its branches to the anterior, posterior, and apical segments, is exposed and then branches individually ligated. The superior lobe vein is identified and dissected laterally, usually exposing three segmental pulmonary veins. It is often easier and safer to ligate the individual venous branches peripherally and in the lung parenchyma. The oblique fissure is then opened and completed between the upper and lower lobes. This permits the dissection of the posterior ascending segmental pulmonary arterial branch, which ordinarily comes off the pulmonary artery after the middle lobe branches. All the vessels are best managed by ligation with non-absorbable suture, as well as suture ligation proximally. Right mainstem bronchus Right pulmonary artery Superior pulmonary vein 6a Upper Middle Lower 6b After division of the arterial and venous branches of the right upper lobe, adventitial tissue surrounding the bronchus is cleared away. Teasing the lung off the vessels is a good technique to use in these cases to gain length and ensure no compromise to the main vessel. This maneuver also allows for thermoligation of smaller vessels which may be somewhat safer. Thoracoscopically, the same choices exist for handling the bronchus, with most surgeons preferring interrupted sutures, especially in small children. Torsion of the right middle lobe has occurred after an upper lobectomy, and the right middle lobe should be sutured to the right lower lobe if the major fissure is complete after a right upper lobectomy is performed.
Cheap 60mg orlistat otc
There were multiple left-sided diverticuli and a right-sided diverticulum with a nonbleeding visible vessel weight loss quit drinking orlistat 60mg with mastercard. He remained in the hospital for about 48 hours during which there was no recurrent bleeding and his Hgb remained stable. M is a 39-year-old man who arrives at the emergency department after vomiting blood. After about an hour he vomited "a gallon of blood" with no other stomach contents. Almost immediately afterward, he had a second episode of hematemesis and called 911. The hematemesis is a pivotal point in this case and localizes the source of the bleeding to above the ligament of Treitz. Although not always present, preceding symptoms of abdominal distress are common with peptic ulcer disease and gastritis. A MalloryWeiss tear is also possible, but the patient would report vomiting before the onset of bleeding. He drinks at least a fifth of hard liquor and a 6-pack of beer daily for the last 20 years. There is no ascites but the spleen is palpable about 2 cm below the costal margin. Given the alcohol history, scleral icterus, and splenomegaly, a hemorrhage from esophageal varices needs to move above peptic ulcer disease on the differential diagnosis. There are stigmata of chronic liver disease and frequently a history of previous hemorrhages. Esophageal varices are portosystemic collaterals that dilate when portal pressures exceed 12 mm Hg. The Child-Turcotte-Pugh system classifies patients based on the severity of their cirrhosis. The system takes into account the presence of encephalopathy, ascites, hyperbilirubinemia, hypoalbuminemia, and clotting deficiencies (Table 19-5). Because variceal bleeding carries such a high mortality, the goal is to detect varices before they bleed so that prophylactic treatment can be initiated. Patients with cirrhosis but without splenomegaly or thrombocytopenia are at the lowest risk for having varices (4%). One study has the sensitivity and specificity of physicians predicting variceal hemorrhage at 82% and 96%, respectively. Beta-blockers (usually propranolol or nadolol) effectively decrease portal pressures. Patients at higher risk for bleeding should also undergo band ligation of the varices. Portosystemic shunt procedures, either surgical or transjugular, should be considered. Patients with variceal bleeding are at high risk for bacterial infections, especially spontaneous bacterial peritonitis. Administration of antibiotics (ceftriaxone or norfloxacin), given prior to endoscopy, have been shown to decrease both the rate of bacterial infections and mortality. Given the prevalence of liver disease in these patients there is often coagulopathy related to factor deficiency or thrombocytopenia. Somatostatin or octreotide should be given as soon as variceal hemorrhage is suspected. Balloon tamponade may be used as a temporizing measure prior to endoscopic therapy. Have you crossed a diagnostic threshold for the leading hypothesis, variceal hemorrhage Given the alcohol history, the volume of the bleed, and the lack of previous abdominal symptoms, bleeding from esophageal varices is highest on the differential diagnosis, and empiric therapy is begun with octreotide and antibiotics. Alternative Diagnosis: Peptic Ulcer Disease the details of peptic ulcer disease are discussed in Chapter 32, Unintentional Weight Loss. Bleeding occurs when an ulcer erodes into a vessel in the stomach or duodenal wall. Biopsy during endoscopy allows for exclusion of malignancy and H pylori infection as a cause of the ulcer. Other endoscopic findings associated with high risk are ulcer size > 2 cm and arterial bleeding. Clinical factors such as transfusion requirements, age, comorbid conditions, and hemodynamic stability must also be taken into account. Early endoscopy achieves hemostasis in > 94% of patients and decreases length of hospital stay. For patients with a high-risk lesion, endoscopic intervention such as clipping, thermocoagulation, or sclerotherapy is warranted. Patients found to be at high risk for rebleeding (Table 19-6) on endoscopy should continue this therapy for 72 hours. All patients who are discharged should be taking proton pump inhibitors (as well as H pylori therapy, if warranted) to ensure ulcer healing. Patients who have rebleeding that cannot be controlled endoscopically can either undergo embolization or surgical therapy. Alternative Diagnosis: Mallory-Weiss Tear Textbook Presentation Mallory-Weiss tear is typically seen in patients with vomiting of any cause in whom hematemesis develops acutely. In fact, a history of retching preceding hematemesis is present in about 33% of cases. Although there was no clinically significant rebleeding, other complications developed. He remained intubated for 5 days for presumed aspiration pneumonia, experienced alcohol withdrawal symptoms, and developed mild encephalopathy. During the hospitalization he was found to have Child-Turcotte-Pugh grade B cirrhosis. Follow-up in an outpatient alcohol program and the hepatology practice was scheduled. His bleeding was controlled with a combination of medical and endoscopic management. The complicated hospital course is not surprising given the comorbid conditions frequently present in patients with varices. On review of systems, she notes that she occasionally passes bright red blood per rectum. It is bleeding in a young patient without "red flags" for serious disease such as anemia, change in bowel habits, weight loss, or diarrhea. The goal is to diagnose these patients appropriately without missing occasional serious lesions and without subjecting excessive numbers of patients to unpleasant evaluation. Anal fissures are usually painful so hemorrhoids are the more likely diagnosis in this case. S reports no recent change in bowel habits, no weight loss, and says she feels well. She does report that although the bleeding has never been associated with pain, it is sometimes associated with constipation. Leading Hypothesis: Hemorrhoidal Bleeding Textbook Presentation Hemorrhoidal bleeding typically presents with severe rectal pain and bleeding. Present either as painless bleeding or with engorged, painful, swollen perianal tissue; or with thrombosis. Both internal and external hemorrhoids will be most symptomatic with sitting, straining, and constipation. An important question is "When does benign sounding anorectal bleeding need a more extensive evaluation than an anal exam with or without anoscopy One study looked at 201 patients whose review of symptoms revealed rectal bleeding. Factors associated with risk of serious disease were age, short duration of bleeding, and blood mixed with stool. Another study found only 10 polyps among 314 patients under 40 with rectal bleeding compared with 27 polyps and 1 case of cancer among 256 patients between the ages of 40 and 50. In general, if a young patient (under age 40) with rectal bleeding does not have a clear anorectal source or if the bleeding continues despite treatment of the anorectal source, a more complete evaluation (with colonoscopy) should be done. Although serious disease is rare among young people with rectal bleeding, it does occur. Most hemorrhoids and anal fissures can be treated conservatively with general recommendations for perianal well being. Analgesia with acetaminophen, topical creams, or short-term topical corticosteroids.
Order cheap orlistat on-line
She smoked 1 pack of cigarettes per day for 10 years and quit when she was 28 years old weight loss jars purchase cheap orlistat online. She has no pivotal clues that can help limit the differential diagnosis (fever, pleuritic chest pain, or other chest pain. On physical exam, the patient appears comfortable at rest but becomes markedly dyspneic with ambulation. In such cases, it is particularly important to systematically review the differential diagnosis in order to arrive at the correct diagnosis (Table 15-2). Each item on the list should be reviewed in light of the history and physical to determine whether it remains in the differential and should be explored further, or whether the existing information makes it highly unlikely. Pneumonia is highly unlikely given the normal chest film and the lack of fever and cough. Asthma remains a possibility although this is not particularly suggested by the history or physical exam. A significant pleural effusion and pneumothorax are ruled out by the normal chest radiograph, which also makes interstitial disease unlikely (although not impossible). A methodical approach to the differential diagnosis is vital whenever the leading diagnosis is unclear or when the leading hypothesis cannot be confirmed. The history and normal pulmonary function tests with methacholine challenge make asthma very unlikely. Pathophysiology: Most commonly occurs when a lower extremity venous thrombosis embolizes to the lung. Protein C or S deficiency (rare) (1) Protein C and S are naturally occurring anticoagulants (2) Deficiency is associated with hypercoagulability. Lower respiratory tract infection (increased sputum, purulence, fever, cold or sore throat) b. Clinical presentation: the diagnosis of pulmonary emboli is complicated because patients may present in a variety of ways and signs and symptoms are neither sensitive nor specific. Although dyspnea and chest pain are the most common symptoms, neither is sufficiently sensitive to rule out the diagnosis when absent nor sufficiently specific to rule in pulmonary emboli when present. Makes alternative diagnosis in 25% of patients (lymphadenopathy, tumor, aortic dissection) 4. Duplex ultrasonography (1) Ultrasonography may visualize the whole leg or be limited to the proximal leg. Other options include venography (invasive) and magnetic resonance direct thrombus imaging (accurate but costly). Options include anticoagulation (with a variety of agents) or thrombolytic therapy. Thrombolytic therapy is rarely used but recommended in hemodynamically unstable patients in whom the benefits outweigh the risks. If such patients have contraindications to thrombolysis, surgical embolectomy is recommended. Research is ongoing to determine optimal therapy and the choice of anticoagulants is likely to evolve rapidly. Work-up for thrombophilia: Guidelines for routine testing have not been determined. At particularly high risk are patients undergoing hip fracture surgery, hip or knee replacement, and those with spinal cord injury. Options include compression stockings, pneumatic compression devices (particularly useful in patients who have active bleeding or are at high risk), and anticoagulation. N-terminal pro-B-type natriuretic peptide predicts the burden of pulmonary embolism. Role of cardiovascular magnetic resonance as a gatekeeper to invasive coronary angiography in patients presenting with heart failure of unknown etiology. Accuracy of B-type natriuretic peptide tests to exclude congestive heart failure: systematic review of test accuracy studies. Usefulness of handcarried ultrasound to predict elevated left ventricular filling pressure. Meta-analysis: the value of clinical assessment in the diagnosis of deep venous thrombosis. Comparison of hand-carried ultrasound assessment of the inferior vena cava and N-terminal pro-brain natriuretic peptide for predicting readmission after hospitalization for acute decompensated heart failure. A systolic murmur is a common presentation of aortic regurgitation detected by echocardiography. Association between phonocardiographic third and fourth heart sounds and objective measures of left ventricular function. Limited value of patient history and physical examination in diagnosing deep vein thrombosis in primary care. A joint report of the American College of Radiology Appropriateness Criteria Committee and the American College of Cardiology Foundation Appropriate Use Criteria Task Force. Bedside hand-carried ultrasound by internal medicine residents versus traditional clinical assessment for the identification of systolic dysfunction in patients admitted with decompensated heart failure. Management of venous thromboembolism: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Pulmonary embolism in patients with unexplained exacerbation of chronic obstructive pulmonary disease: prevalence and risk factors. History and physical examination in acute pulmonary embolism in patients without preexisting cardiac or pulmonary disease. Does this dyspneic patient in the emergency department have congestive heart failure Antithrombotic therapy for valvular disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. When considering this symptom, pivotal points are history and physical exam findings that suggest more serious or complicated etiologies. Important historical features include vaginal or penile discharge, flank pain, rectal/perineal pain, nausea or vomiting, fever, hematuria, urinary hesitancy, urinary urgency, nocturia, and urinary frequency. A prostate exam should be performed in any man in whom cystitis is suspected, especially those with symptoms of nocturia, hesitancy, or rectal pain. When approaching the differential diagnosis for dysuria, an anatomic approach to the genitourinary tract is helpful for organization. Complicated (men or patients with any of the following: urinary obstruction; pregnancy; neurogenic bladder; concurrent kidney stone; immunosuppression; indwelling Foley catheter; systemic infection, such as bacteremia or sepsis) 2. She denies flank pain, fever or chills, nausea or vomiting, vaginal discharge, genital rash, or hematuria. Her last menstrual period ended 5 days ago, and she takes an oral contraceptive pill regularly for contraception. The pivotal points in this case are the absence of flank pain, vaginal discharge, nausea, vomiting, or fever. Vaginitis is a common disease that can cause similar symptoms, and pyelonephritis is a must not miss diagnosis. These diagnoses must be explored as part of the limited differential diagnosis (Table 16-1). Leading Hypothesis: Cystitis Textbook Presentation Cystitis typically presents with dysuria or suprapubic pain or both. Gram positives: Staphylococcus saprophyticus, Enterococcus faecalis, and group B streptococcus. Elderly patients often have atypical presentations of cystitis; many have chronic symptoms of frequency and incontinence. Delirium, functional decline, or acute confusion may be the presenting symptoms of cystitis in elderly patients. The probability of cystitis is over 90% in women with dysuria and frequency without vaginal discharge or irritation.
Purchase orlistat 120 mg free shipping
As a cusp becomes contracted weight loss 411 purchase orlistat online now, the tissue near its free end retracts, resulting in a pattern with some chordae tendineae attaching directly to the free edge of the cusp. The involved commissures are held in a nearly closed position by the other changes responsible for mitral stenosis. If both commissures are calcified, the mitral valve is converted into a fixed structure that is open throughout the cardiac cycle. The aggravation of mitral insufficiency by left atrial enlargement depends primarily on the anatomic phenomenon of the left atrial wall and mitral cusps being one continuous structure. Enlargement of the left atrium is constant, and the degree of enlargement is usually greater than in mitral stenosis. The secondary effects on the esophagus, tracheal bifurcation, right ventricle, and pulmonary vascular bed are similar to those described for mitral stenosis. The interventional cardiologist uses a clip device to mimic the surgical procedure (Alfieri) that creates a double orifice of the mitral valve resembling a bowtie. The mitral valve clip is unlikely to replace the usual mitral valve surgery, but in nonsurgical candidates who still require a procedure, the clip may provide an alternative therapy. The cardiac surgeon must determine which procedure can be performed using criteria determined by transesophageal ultrasound and direct visualization of the valve apparatus at surgery. Patients who undergo mitral valve repair must remember that they do not have an anatomically normal valve, and that endocarditis prophylaxis must be considered when certain noncardiac procedures are performed. Left atrium Left ventricle 2D echocardiogram showing normal configuration of mitral valve leaflets in systole Normal systole mitral valves coapt on ventricular side of mitral valve. If mitral insufficiency results from prolapse, physical examination reveals that the regurgitation is in late systole and is often preceded by a midsystolic click (late systolic murmur). In the normal heart during systole, when the mitral valve closes, the coaptation of the valves occur on the ventricular side of the mitral valve below the plane of the mitral valve annulus. In an aortic valve, various residua of rheumatic inflammation reduce the valve orifice (see Plate 6-43). The simplest type of stenosis is characterized by fusion of two of the cusps at one commissure. The second way that rheumatic inflammation leads to aortic stenosis is through the inflammatory process, which operates indirectly by first establishing an acquired bicuspid valve, which in turn may become calcified. This process may become established on the acquired bicuspid valve or may represent a complication of a congenital bicuspid valve (see Plate 6-43). A congenital bicuspid valve becomes a likely candidate for calcific aortic stenosis. Also, some patients with calcific aortic stenosis have a malformation associated with a high incidence of congenital bicuspid valve, such as coarctation of the aorta. In patients with aortic stenosis, coronary artery disease may be present to the same extent as seen in the general population. In an occasional case, coronary arterial narrowing results from embolism, the source of which may be calcific material in the diseased aortic valve or emboli from infective endocarditis of the aortic valve. As each cusp is shortened, some of its "extra length," which makes the valve competent, is lost. The incompetent orifice of the valve is then represented by a triangular opening bounded by the affected cusps (see Plate 6-44). Secondary signs of aortic regurgitation include widening or dilatation of the ascending aorta and alterations in the left ventricle. Along with thickening of the wall, the cavity becomes enlarged in both lateral and downward directions. This tends to change the axis of the papillary muscles and the chordae tendineae from a near-vertical position, with respect to the long axis of the left ventricle, to an axis prone to an orientation toward the horizontal position. The right ventricular hypertrophy accompanying aortic stenosis or aortic insufficiency may be derived similar to the right ventricular hypertrophy of mitral stenosis. A systolic murmur is usually audible, related to the large volume of blood flowing across a diseased valve in systole (see Plate 6-45). Currently, two devices are available in the United States (more in Europe) for implantation in appropriate patients: a self-expanding trileaflet porcine pericardial valve mounted on a metal frame (CoreValve, Medtronic) and a trileaflet valve of bovine pericardium mounted on a metal stent with expandable balloon (Sapien, Edwards Laboratories). The valve must be positioned precisely and oriented correctly to avoid interference with the coronary artery orifices. Either valve is generally used in high-risk patients with severe aortic stenosis, and except for a higher incidence of stroke than with surgical aortic valve replacement, outcome results are comparable over the short term. In high-risk patients with severe aortic stenosis, transcatheter and surgical procedures for aortic valve replacement have similar rates of survival at 1 year, although there are important differences in risks associated with the procedure. The transcatheter procedure was associated with a higher risk of stroke than the surgical replacement (5. With a dilated annulus and incompetent orfice Dilated ascending aorta Prolapsed leaflets of mitral valve cyStic meDial necroSiS of aorta Cystic medial necrosis (also called Erdheim disease) of the aorta is another cause of aortic regurgitation. In some patients the aortic valve may be competent, while other manifestations, such as mitral regurgitation or dissection of the aorta, may occur. Cystic medial necrosis is seen in elastic arteries and is characterized histologically by deposits within the media of amorphous basophilic accumulations, or microcysts, and accounting for the "cystic" necrosis. Initially tiny isolated lesions, the microcysts tend to coalesce and in extreme cases replace broad areas of the media. In the presence of coalesced microcysts, however, the elastic laminae in a given area are interrupted, and such fibers then recoil. The histologic effect is that multiple areas of the media are devoid of elastic fibers. In some this is normal, and the enlargement of the aorta is called idiopathic dilatation of the aorta. These patients characteristically are unusually tall and have correspondingly long bones of the arms, legs, feet, and hands. These patients also have a higharched palate, dislocation of the optic lenses, and a tendency toward emphysema. Aortic segment showing cystic medial necrosis the aortic valve effect is a common manifestation and results in aortic regurgitation. This functional abnormality may develop in several ways, most simply through extensive dilatation of the aortic root, including each sinus of Valsalva. Some patients show extreme enlargement with prolapse of the aortic cusps, which compounds the effect of aortic dilatation in causing aortic regurgitation. Regardless of whether a localized dissection or an intramural hematoma is present, the ascending aorta dilated by cystic medial necrosis may cause some alteration in the shape of the heart on chest radiographs. Characteristically, the valve substance between the insertion of the chordae tendineae tends to balloon up toward the atrium (myxomatous degeneration, mitral valve prolapse), and there may also be elongation of the chordae. Medical management of Marfan aortic disease consists of beta-adrenergic blockade to decrease the force and velocity of contraction of the left ventricle on the proximal aorta. Completed aortic graft Surgical Management of Abdominal and Thoracic Aortic Dissection and Aneurysms Surgical management of other types of aortic dissections and aneurysms are typically deferred until risk of rupture outweighs the risk of repair. Currently, endovascular therapy of dissection or aneurysm repair is often used by vascular surgeons or cardiac surgeons to treat an abdominal or thoracic aortic aneurysm or dissection. The primary affected site is the media of the thoracic aorta, which shows many microscopic foci where tissue has been lost and replaced by delicate stellate scars. This change has led investigators to determine whether the medial change of syphilis is an effect of direct infection of the media or a result of faulty aortic nutrition, secondary to the alterations in the vasa vasorum. Certain gross characteristics are displayed by the aorta, which is the end organ in syphilitic disease. The combination of two features of syphilitic heart disease-widening of the affected portion of the aorta and localization to the thoracic portion of the vessel- results in a characteristic appearance of the syphilitic aorta. In the classic example, widening extends to the level of the diaphragm, where because of a lack of dilatation of the abdominal portion, the descending aorta assumes a funnel shape as it becomes continuous with the abdominal segment. Grossly, another feature usually becomes apparent: a strong tendency for the involved portion to show diffuse atherosclerosis.
Purchase orlistat australia
Therefore 5 weight loss pills order orlistat online from canada, serial fetal ultrasonography in the third trimester is warranted to follow the appearance of the bowel. Progressive worsening of these findings could lead to future complications and may be an indication for early delivery. The evaluation of other life-threatening anomalies, which are rare, may delay surgery. Damp, warm gauze sponges or a damp, warm roll of gauze is wrapped around the intestine. The infant should be in a warming isolette or under an overhead radiant warmer to help maintain normothermia. Eventually, almost all infants with gastroschisis will require central venous access. A nasogastric tube placed at the time of birth is necessary for gastrointestinal decompression because of the bowel inflammation and resulting ileus. Thus, before surgery, the infant with gastroschisis should be normothermic, hemodynamically stable, and have normal serum electrolytes following adequate fluid resuscitation. After the induction of general anesthesia, the dressing previously placed over the herniated contents should be removed. The antiseptic solution must be warm to the touch in an effort to minimize heat loss. After gently washing the bowel and the anterior and lateral abdominal wall, drapes are appropriately placed and the herniated contents are laid on the drapes. The choice of anesthetic agents should be made by the anesthetist, but two points should be emphasized: first, muscle paralysis is useful in optimizing the chances for complete reduction of the herniated bowel and primary abdominal wall closure, and second, nitrous oxide should not be used as it diffuses into the lumen of the bowel causing distension and 4 It is sometimes necessary to extend the abdominal wall defect to facilitate reduction of the herniated bowel. Extending the incision caudally is not recommended because the urinary bladder is in close proximity to the inferior aspect of the abdominal wall defect. Although gentle stretching of the anterior abdominal wall can be useful, the authors are opposed to vigorous stretching. If it can be closed without undue tension, 3/0 absorbable, monofilament sutures are used. When all the sutures have been placed, they are tied in sequence with a thin, malleable retractor initially underneath the fascia to prevent a loop of intestine from becoming entrapped under the sutures. It is best to avoid high intra-abdominal pressure and excessive suture line tension. This can result in abdominal compartment syndrome, possibly leading to intestinal necrosis, renal hypoperfusion, and difficulty in ventilation, as well as wound disruption. Intragastric and bladder pressure monitoring has been used by some pediatric surgeons to determine intra-abdominal pressure. These two measurements are used as a guide to monitor intra-abdominal pressure during primary or staged closure of gastroschisis. It is generally necessary to enlarge the fascial defect prior to suturing the Silastic sheet. However, extending the fascial opening too far inferiorly should be avoided as bladder injury may occur. The top of the sac is oversewn with a 3/0 monofilament suture placed in a running horizontal mattress fashion. The Silastic sac is covered with povidone-iodine ointment followed by dry roll gauze to act as a protective dressing and provide support to the Silastic sac at the fascial level. When the herniated bowel has been successfully reduced into the peritoneal cavity and the fascial edges brought to within 1 cm of each other, the infant is ready for removal of the sac and primary abdominal wall closure in the operating room under general anesthesia. This method involves bedside placement of a springloaded silo, followed by passive reduction of the herniated contents into the abdomen via gravity. The infant is kept paralyzed or sedated and intubated with assisted ventilation during the passive reduction. If this is the case, the fascial opening should be enlarged prior to silo placement to prevent this potential complication. A stoma can be created at the time of removal of the Silastic sac and primary abdominal wall closure. It is preferable to use the staged reduction approach when primary abdominal wall closure might result in excessive intra-abdominal pressure. The incidence of necrotizing enterocolitis in patients with gastroschisis has been reported to be as high as 20 percent. Finally, sepsis, resulting from intra-abdominal or wound infections, and central line infections are additional causes of morbidity in the patient with gastroschisis. Intestinal perforation can be managed in one of several ways, depending on the specific circumstances. The options at the time of birth include suture closure, resection of the site of perforation with oversewing of the two ends of the bowel. In this technique, the bowel is reduced in the usual fashion either primarily or after placement in a silo. However, instead of placing sutures to approximate the fascia, the defect is covered with the umbilical stump or a non-adherent dressing. Occlusive dressings are then placed over the site and the wound is allowed to granulate. Once granulation tissue covers the wound bed, the area is covered with dry dressings. In addition to the marked improvement in survival, the length of time to initiation of feedings and hospital discharge have been significantly shortened. Whereas hospitalization usually averaged approximately 6 weeks, the average is now around 4 weeks. Prenatal ultrasonographic gastrointestinal abnormalities in fetuses with gastroschisis do not correlate with postnatal outcomes. Bladder pressure monitoring significantly enhances care of infants with abdominal wall defects: a prospective clinical study. The development of necrotizing enterocolitis following repair of gastroschisis: a surprisingly high incidence. Staged reduction using a Silastic sac is the treatment of choice for large congenital abdominal wall defects. There is no exception to this, and because of the fulcrum, all internal movements are paradoxical. Moving an instrument to the right will result in the opposite movement inside the body. Principles of port placement 321 manipulating instruments in first-order paradox, this is not necessarily the case when it comes to positioning the assistant surgeons or nurses. Video Nurse Assistant the ergonomIcs oF Port Placement Surgeons intuitively place open surgical incisions close to the operative field to gain maximum extensile exposure to the surgical field. The closer the port is to the operation site, the less room there will be to maneuver. The optimum port position for laparoscopic surgery is one which provides direct access to the target organ, optimizing the volume of the internal space to allow the manipulation of instruments with minimal exaggerated movements. To overcome the problem with second-order paradox, the optimum position for the operating team is one which allows everyone to work with the camera pointed away. When operating in an extremely confined space, such as when repairing a duodenal atresia, it will be necessary to break some ergonomic rules in order to maximize the internal space available to allow for accurate suturing. The optimum port position is to have approximately the same length of instrument on the inside as you would on the outside. Position ports to allow you to manipulate instruments with your arms completely adducted by the side of your body, with shoulders in resting position, i. In practice, the optimum position is for the surgeon to be sitting down, and for both arms to be adducted and resting comfortably by the side of the body without elevating the shoulders. Laparoscopic intracorporeal suturing Video Video 323 a telescope and at least two other hand instruments, the surgeon should be able to navigate any instrument to the convergent point by using the other two instruments.
Buy orlistat visa
There is normally a small gradient favoring filtration out of the vascular space into the interstitium; the excess fluid is removed via the lymphatic system weight loss pills homemade purchase orlistat 120mg on-line. An increase in capillary hydrostatic pressure (for example, increased plasma volume due to renal sodium retention). Due to a systemic cause (with or without presacral edema, ascites, pleural effusion, pulmonary edema, periorbital edema) a. Hematologic: anemia the most common systemic causes of edema are cardiac, hepatic, and renal diseases. Lymphatic obstruction (lymphedema) (1) Primary (idiopathic, often bilateral) (a) Congenital (b) Lymphedema praecox (onset in puberty) or tarda (onset after age 20) (2) Secondary (more common; generally unilateral-see below) B. V was well until a couple of months ago when she began feeling a bit more tired than usual, despite continuing to sleep well. She has noted intermittent vague abdominal pain, not related to eating, position, or bowel movements. Over the last 2 weeks, she has noted swelling in her feet and lower legs and has not been able to wear her regular shoes. As she tells you this, you note that she is wearing house slippers, and that her socks have produced a significant indentation above her ankles. Her past medical history is notable for hypertension and diabetes, both well controlled. Her current medications include hydrochlorothiazide, lisinopril, pioglitazone, simvastatin, and aspirin. V, you can see that she has significant bilateral leg edema, a pivotal point in her presentation. Although there are some local diseases that can present with bilateral leg edema, the first step in such patients is always to look for systemic causes. While the history and physical are often not sensitive or specific enough to make a diagnosis, they are a good starting point for organizing the differential. V have any signs, symptoms, or risk factors pointing to a cardiac, hepatic, or renal cause of her edema She is certainly at risk for both heart and kidney disease because of her history of hypertension and diabetes. Medication should be considered as a cause, since pioglitazone frequently causes edema; hypothyroidism does not cause pitting edema, and so is not likely. Finally, although it is uncommon for obstruction to cause bilateral edema, you should think about ovarian cancer causing malignant ascites and venous obstruction if another cause is not found. Leading Hypothesis: Cirrhosis Textbook Presentation Patients with cirrhosis can be asymptomatic or have mild symptoms, such as fatigue. Some patients have the classic manifestations of portal hypertension: ascites, edema, variceal bleeding, encephalopathy, or hypersplenism. Genetic metabolic diseases (Wilson disease, alpha-1-antitrypsin deficiency, glycogen storage diseases, porphyria) d. Primary or secondary biliary cirrhosis the 2 most common causes of cirrhosis in the United States are alcoholic liver disease and chronic hepatitis C. Advanced fibrosis, or cirrhosis, causes architectural distortion of the hepatic vasculature, leading to shunting of the blood coming into the liver via the portal vein directly to the hepatic vein outflow system, which causes a. Renal vasoconstriction and hypoperfusion of the kidneys, causing salt and water retention d. Edema due to a combination of salt and water retention (increasing hydrostatic pressures) and hypoalbuminemia (decreasing intravascular oncotic pressure) C. Up to 60% of patients progress to decompensated cirrhosis, defined as worsening portal hypertension and decreased hepatic reserve, at 10 years after diagnosis. Rates of progression are quite variable and are related to the etiology of the cirrhosis, presence of other liver disease, available treatment (such as for chronic hepatitis B and C), and avoidance of hepatic toxins (such as alcohol). In patients with cirrhosis but no varices and no ascites, the 1-year mortality rate is 1%. In those with varices and ascites, the 1-year mortality rate is 20%; in those with variceal bleeding and ascites, the 1-year mortality is 57%. Cirrhosis is a pathologic diagnosis definitively made only by examining the entire liver at autopsy or after liver transplantation. Patients may have physical findings suggestive of chronic liver disease (see below), constitutional symptoms, asymptomatic liver enzyme or radiologic abnormalities, manifestations of portal hypertension (see below), or no symptoms at all. Cirrhosis is sometimes diagnosed at autopsy in patients in whom the disease never manifested. Physical findings may increase the likelihood that a patient with liver disease has cirrhosis, but rarely rule out cirrhosis (Table 17-2). Physical exam findings for the diagnosis of cirrhosis in patients with liver disease. Patients who show manifestations of portal hypertension (see below) are assumed to have cirrhosis. A low platelet count in a patient with liver disease increases the probability of cirrhosis. Useful for distinguishing mild fibrosis from cirrhosis, but less accurate in identifying moderate fibrosis. FibroScan is an imaging method that measures liver stiffness, which correlates with cirrhosis. Treatment Once it has been determined that the patient probably or definitively has cirrhosis, it is important to determine the specific cause of the cirrhosis (see Chapter 26, Jaundice & Abnormal Liver Enzymes) and to determine whether the patient has manifestations of portal hypertension: variceal bleeding, ascites, hepatic encephalopathy, and hypersplenism. Treatments for selected causes of cirrhosis are discussed in Chapter 26, Jaundice & Abnormal Liver Enzymes. Ascites Textbook Presentation the patient complains of an inability to fasten her pants due to increasing abdominal girth, sometimes accompanied by dyspnea and edema. Incidence in patients with cirrhosis and ascites is 18% at 1 year and 39% at 5 years. Overgrowth of intestinal bacterial and increased intestinal permeability lead to movement of bacteria into mesenteric lymph nodes; the bacteria can then enter the systemic circulation and colonize the ascitic fluid. The 3 most common isolates are Escherichia coli, Klebsiella pneumoniae, and pneumococci. Consider secondary peritonitis if more than 1 organism is cultured from the ascitic fluid. Serum-ascites albumin gradient is used to distinguish ascites due to portal hypertension from ascites due to other causes. In portal hypertension, ascites occurs due to transudation, without changes in permeability that would allow albumin to leak into the ascitic fluid. This is in contrast to exudative types of ascites, such as ascites from infection or malignancy, in which albumin can leak into the ascitic fluid. Spironolactone is the diuretic of choice to treat the aldosterone driven salt and water retention seen in cirrhosis. Furosemide or other loop diuretics can be added in patients who do not respond to spironolactone alone; 90% of patients respond to sodiumrestricted diets, spironolactone, and loop diuretics. In order to avoid hypovolemia and renal impairment, the rate of weight loss should not exceed 0. Large volume paracentesis with volume expansion (dextran or albumin) is done in patients unresponsive to diuretics. Creates a shunt between the high-pressure portal vein and the lowpressure hepatic vein, leading to improved hemodynamics and a decrease in ascites. Grade 2 (moderate) and grade 3 (severe) ascites are generally treated due to patient discomfort and respiratory compromise. Hepatic Encephalopathy Textbook Presentation the classic presentation of hepatic encephalopathy is a patient with known cirrhosis who has mental status changes or is in a coma. A spectrum of reversible neuropsychiatric abnormalities seen in patients with cirrhosis B.