40mg pantoprazole sale
If two kidneys require removal gastritis sweating cheap pantoprazole 40mg amex, a differential function analysis by isotope imaging is performed, and the worse kidney is removed. Exceptions to this approach include the presence of renal-mediated intractable infection or hypertension and the presence of massively enlarged. As previously addressed, the nephrectomy incision should be positioned so as not to interfere with subsequent transplantation. Massive dimension compromising respiration, gastrointestinal function, or allograft placement; infection; bleeding. In children, an unknown natural history and a long lifetime risk of exposure may favor nephrectomy in all instances. Whenever possible, ureteral reimplantation is preferable to preserve the native ureter, facilitating the management of any future allograft ureteral complication that might arise. Surgical reconstruction to enable continence may be required for a patient with neurologic. This reconstruction is best accomplished before transplantation, and the surgical strategy has been extensively reviewed. Bladder augmentation procedures occasionally may be necessary before transplantation to ensure continence and a urinary receptacle that operates at a sufficiently low pressure to avoid allograft deterioration. As discussed earlier, strong evidence exists documenting a relationship between high intravesical pressures and renal deterioration. Renal allograft deterioration with graft loss, azotemia, or infection has been shown in systems known to be associated with high intravesical pressures. Nonetheless, these experiences have created much controversy about augmentation in the transplantation setting. Bladder augmentation is capable of complicating the course of a recipient and should be applied only when a definitive indication is shown. Generally, bladders defunctionalized because of severe oliguria subsequent to primary renal disease are not problematic and do not require urodynamic investigation even if the capacity is found to be low. In contrast, bladders defunctionalized by diversion to interrupt ongoing native renal injury owing to high intravesical pressures must be highly suspect. In the case of posterior urethral valves, a noncompliant, threatening bladder documented early in life may not be so when transplantation is performed at an older age. Interpretation of urodynamic findings and the choice of augmentation cystoplasty must be highly individualized. That failure to apply augmentation can adversely affect the clinical course of the recipient is clearly shown by numerous reported augmentations required after transplantation because of renal deterioration. Although ileocystoplasty is the most prevalent procedure, several modalities have been successfully employed. At the time of reporting, 80% of allografts were functioning well, whereas in 18% allograft function had been lost, and in 2% the recipient had died with a functioning graft. Each instance of allograft loss was due to chronic rejection, with no graft loss reported from infectious or technical complication. Table 47-6 compares the available types of augmentation procedures in relation to their applicability to the transplantation setting. Autoaugmentation and ureterocystoplasty can be performed extraperitoneally without interfering with peritoneal dialysis or intestinal function, and without a risk of metabolic consequences. The clinical experience and applicability seem to be low, and the procedure is relatively complex. Ileocystoplasty and colocystoplasty are technically simple procedures that have been used extensively with good result. Although ureteral or Mitrofanoff neourethral implantation can be successfully performed into the tinea of the colonic augmentation segment, reliable implantation is impossible with ileocystoplasty, a feature shared by autoaugmentation and ureterocystoplasty. Ileocystoplasty and colocystoplasty are associated with an increased incidence of bacteriuria, and the resultant mucus production may compromise catheter drainage. Gastrocystoplasty has proved highly applicable to the transplantation setting, avoids the risk of acidosis and calculi, and markedly reduces the incidence of significant bacteriuria and mucus production. The hematuria-dysuria complex is occasionally encountered, particularly during highly oliguric or anuric periods while the patient awaits transplantation. It is generally readily controlled by bladder cycling, histamine blockade, or proton-pump inhibition. Whenever possible, allograft ureteral implantation should be accomplished into the native component of the augmented bladder97 or into a gastrocystoplasty segment to reduce the risk of ureteral complications. If a nonreconstructable bladder is encountered, an intestinal conduit or continent diversion may be applicable. Efforts are ongoing to optimize organ donation rates from deceased donors and to refine organ selection criteria for children. A useful rule of thumb is that the best kidney for a child is one from an otherwise healthy teenage or young adult donor, and that a single kidney from a very young pediatric donor would not provide acceptable long-term function. Generally, individuals who are being evaluated as potential deceased donors have experienced brain death. The sequence of steps and diagnostic studies involved in this evaluation, including contraindications to the use of organs from a deceased donor, has been thoroughly reviewed. Donor management requires intensive and coordinated care on the part of the intensive care unit and organ procurement team members. Temperature regulation and respiratory support are also crucial and often problematic. Hormonal support is often indicated because of a precipitous decrease in hormone levels after the onset of brain death and may include triiodothyronine, cortisol, and insulin. Arginine vasopressin is frequently indicated to reverse the often-encountered severe neurogenic diabetes insipidus. As necessary, the vascular anatomy of the liver, pancreas, and small intestine is defined, and the aorta is isolated at the level of its diaphragmatic hiatus. Organs are sequentially removed, beginning with the heart, followed by the lungs, liver, small intestine, or pancreas, and, finally, the kidneys. The kidneys are removed en bloc with the adjacent aorta and vena cava, and the ureters are divided at the level of the urinary bladder. Kidneys from a very young donor are not separated until a decision has been made about whether or not they will be transplanted individually or en bloc. Otherwise, the kidneys are separated on the back table and cold stored for distribution. The preservation fluid constituents are designed to minimize the injury associated with hypothermia and hypoxia, and represent some of the most pivotal work in transplantation science. The principal active ingredients of the two most prevalent solutions are outlined in Table 47-8. Intracellular acidosis is compensated by the avoidance of glucose and the addition of phosphate as a hydrogen ion buffer. Although the outcomes of deceased donor kidney transplantation in children have become almost equivalent to the outcomes of living donor transplantation. When a transplant date is set, arrangements also can be made to initiate immunosuppressive therapy ahead of time, typically several days before transplant at centers choosing this approach, to facilitate therapeutic drug levels at the actual time of surgery. Preemptive transplantation has numerous advantages65 and should be considered whenever possible. In the setting of preemptive transplantation, especially when an adult kidney is placed into a small child, caution with pretransplant immunosuppression (see later) should be exercised because these recipients can be quite uremic, and treatment with a calcineurin inhibitor for many days before transplantation may worsen this condition further. Under these circumstances, a grafted adult kidney that functions immediately can remove uremic toxins at a staggering rate and create a clinical scenario similar to the dysequilibrium syndrome seen in the setting of zealous, typically first-time, hemodialysis. Living related and, increasingly, unrelated donor renal allografts have become an integral component of pediatric renal transplantation and are managed from an entirely different perspective. An isotopic neobladder is constructed from a segment of stomach or a composite of stomach and small bowel. An isotopic neourethra is constructed from appendix, ureter, or tubularized ilium and implanted into the neobladder. After a period of healing and recovery, a renal transplantation is performed with the ureter implanted into the gastric component of the neobladder. Total anatomic urinary tract replacement and renal transplantation: a surgical strategy to correct severe genitourinary anomalies.
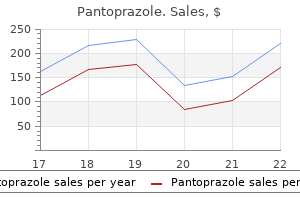
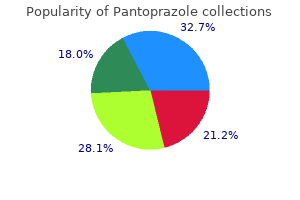
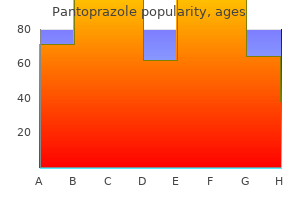
Buy discount pantoprazole on-line
In a series confined to children gastritis symptoms wiki pantoprazole 40mg free shipping, the local control rate for patients who had no or microscopic residual disease after surgery and who were treated with postoperative irradiation was 79% (40). Tumor grade and size are the most important predictors of local failure in these series. Indeed, other retrospective studies of lowgrade soft tissue sarcomas with a wide resection generally have very low local recurrence rates especially for superficial tumors. After complete resection of either extremity or superficial trunk soft tissue sarcoma (45 low-grade, 119 high-grade), patients were randomized to surgery alone versus low dose rate brachytherapy using afterloaded Ir-192 to deliver a dose of 45 Gy to the tumor bed. The local failure rate was higher in the limb conservation group, and several patients had to undergo salvage surgery (107,130). Psychological tests indicate that the amputees fared as well as those having limb-sparing surgery (131). On follow-up 50% of the patients had no limitation of limb function and 40% had full function but had a mild limp or needed a shoe lift, compression device, or pins or rods. In completely resected disease (clinical group I), postoperative irradiation appeared to reduce local recurrences only in high-grade disease. Prognostic factors for children and adolescents with surgically resected nonrhabdomyosarcoma soft tissue sarcoma: an analysis of 121 patients treated at St. The impact of margin of resection on outcome in pediatric nonrhabdomyosarcoma soft tissue sarcoma. Moreover, there was no difference among the patient groups from brachytherapy in terms of distant metastasis or disease-specific survival. In the postoperative setting, higher radiation doses are generally employed to counter any potential incremental tumor hypoxia or clonagenic repopulation during the healing phase after surgery. Certainly, there could be an improvement in function and lower risk of secondary cancers with this approach. In subsequent publications, the local recurrence rate, regional or distant failure rate, progression-free survival, and functional outcome did not differ between the groups with local control rates at over 90% in both treatment groups at 7 years of follow-up (138,139). There were also trends toward more lymphedema and joint stiffness in this group contributing to adverse functional outcomes (140). Other active agents are dacarbazine, actinomycin D, vincristine, etoposide, and cyclophosphamide (6,33,51,56,83, 93,105,130,142,143). In this section of the chapter we will review the most pertinent larger-scale studies. Protocol 8654 was for patients who were judged to have inoperable tumors or for those with metastatic disease. However, there was approximately a 1-year period in which all patients in Study 8654 were treated with vincristine, actinomycin, and cyclophosphamide because of a shortage of dacarbazine. Only 30 patients accepted randomization: 15 received chemotherapy, and 15 were observed. Of the remaining 51 patients, 19 elected adjuvant chemotherapy, and 32 elected observation. Not surprisingly, nonmetastatic and low-grade disease had better outcomes relative to metastatic and high-grade disease. Radiation doses were age dependent: 54 Gy if under the age of 6 years and 64 Gy for those older. The 3-year overall survival and progression-free survival rates (standard deviation) for eligible patients were 59% 8% and 44% 7%, respectively. There was a suggestion that synovial cell sarcomas responded better to chemotherapy compared to other histologies. Of the 81 eligible patients, 15 were randomized to observation, 15 were randomized to chemotherapy, 19 elected chemotherapy, and 32 elected observation. Role of, adjuvant chemotherapy in the treatment of surgically resected pediatric nonrhabdomyosarcomatous soft tissue sarcomas: a Pediatric Oncology Group study. Patients with localized disease, completely resected, received vincristine, actinomycin D, cyclophosphamide, and adriamycin. Patients with grossly resected tumor, microscopic residual disease, and no evidence of regional node involvement received the same chemotherapy but also had involved-field irradiation. These patients were then treated with vincristine, actinomycin D, and cyclophosphamide. Patients with grossly resected tumor with microscopic residual disease and regional nodal involvement or those with incomplete resection or biopsy with gross residual disease received four-drug chemotherapy initially. Those who were good responders continued on this chemotherapy and received involved-field irradiation; ultimately, the adriamycin was dropped. Those who were poor initial responders received involved-field irradiation, but ifosfamide was substituted for cyclophosphamide. Detailed information is available concerning the 30 children and adolescents with synovial sarcomas treated on this study (145). Patients with synovial sarcoma of the extremities had a disease-free survival rate of 88%. Obviously, the German study was not a head-to-head comparison of chemotherapy and observation, and it is not clear what the survival would have been if patients were treated with local therapy alone. The treatment program consisted of a primary complete tumor excision if feasible without mutilation. For patients who were not resectable initially, neoadjuvant chemotherapy was administered. For patients who had initial primary excision, adjuvant chemotherapy was given with ifosfamide, vincristine, and actinomycin D. In nonmetastatic patients an initial complete excision was obtained in 24% of patients, complete response was obtained in 30% of patients by initial partial excision followed by chemotherapy, and a complete response was obtained in 30% of patients by an initial biopsy, neoadjuvant chemotherapy, and second surgery. To date, the studies that have randomized patients to various chemotherapy arms have not shown a substantive difference from those results with local therapy alone. Nevertheless, the two major international cooperative groups have adapted similar treatment strategies with their current investigational protocols. The essential strategy in both the United States and Europe is to risk stratify patients based on tumor size, grade, localized versus metastatic, and respectability. Intermediate- and high-risk patients receive ifosfamide and doxorubicin chemotherapy (141). These studies include comparisons of observation with doxorubicin as a single agent; with doxorubicin, cyclophosphamide, dacarbazine, and vincristine; with adriamycin, vincristine, cyclophosphamide, dactinomycin, and dacarbazine; with doxorubicin, cyclophosphamide, and methotrexate; with doxorubicin, cyclophosphamide, vincristine, and dacarbazine; and with doxorubicin and ifosfamide. The majority of these studies are equivocal as to the benefit of adjuvant chemotherapy. We will briefly summarize some of the larger published trials of adjuvant chemotherapy for soft tissue sarcoma, largely in adults. After a maximum cumulative dosage of adriamycin, chemotherapy was switched to methotrexate with leucovorin rescue. The Scandinavian Sarcoma Group randomized 240 patients with high-grade sarcomas to receive either adriamycin or no systemic treatment. No significant difference was seen between the adriamycin and the control group with respect to local recurrence, relapse-free survival, or overall survival for the 181 evaluable patients or the 240 randomized patients (152). Randomization was to treatment with cyclophosphamide, vincristine, adriamycin, and dacarbazine or to observation. Between 1997 and 1998, 468 patients entered the study; 151 patients were considered ineligible. Relapse-free survival with chemotherapy was 56%, compared with 43% for control subjects (p 0. In patients with extremity tumors, no significant improvement was seen with chemotherapy in terms of local recurrence, metastases, or survival. In contrast, local recurrence was less with chemotherapy for head, neck, and trunk sarcomas (43). There was a median disease-free survival of 16 months in the control group, compared with 48 months in the adjuvant group (p 0. There was thought to be an improvement in survival at 4 years in the adjuvant arm on a planned interim analysis of the data. However, a closer analysis of the data showed that the adjuvant chemotherapy group experienced fewer metastatic events at 2 years (28% vs. By 4 years this difference had disappeared, with 44% of the control group having metastatic disease and 45% in the adjuvantly treated group (p 0. The difference in disease-free survival in the groups at 4 years was related to a significantly greater frequency of local failure in the patients in the control group (17% vs. A widely quoted 1997 analysis included 14 earlier trials of 1568 patients-fewer than 1% of the patients were younger than 15 years-showing an improvement in local control and disease-free survival but not overall survival (154). With several more recent trials emphasizing the addition of ifosfamide to doxorubicin, an updated 2008 meta-analysis of 1953 patients shows an overall survival advantage in a subset analysis (157).
Purchase pantoprazole 20mg mastercard
These leukemic cells that invade the bone marrow are dysfunctional gastritis symptoms spanish purchase pantoprazole 40mg line, and without the normal hematopoietic elements the patient is at risk for developing life-threatening complications of anemia, infection secondary to functional neutropenia, and hemorrhage from thrombocytopenia (Table 11. Fatigue and weakness are the most common complaints that reflect the development of anemia. Pallor, dyspnea on exertion, heart palpitations, and a general loss of well-being have been described. Easy bruising, petechiae, and mucosal bleeding may be found secondary to thrombocytopenia. Leukemic blast cells circulate through the peripheral blood and may invade any tissue. Organs that were active in fetal hematopoiesis may be reactivated to produce cells when stressed by the poor performance of the overladen leukemic bone marrow. Hepatosplenomegaly and lymphadenopathy may occur but are not as prominent as in the chronic leukemias. Skin infiltration is very characteristic in monocytic leukemia, particularly gum infiltration that is termed gingival hyperplasia. When leukemic cells crowd the bone marrow of the long bones, joint pain may be produced. Auer rods are elliptical, spindlelike inclusions composed of azurophilic granules. Anemia is a very common feature resulting from inadequate production of normal red blood cells. Red blood cell anisopoikilocytosis is mildly abnormal, with few poikilocytes present. Before treatment, serum uric acid and lactate dehydrogenase levels often are mildly or moderately increased. The hallmark feature of acute leukemia is always a hypercellular bone marrow, with 20% to 90% leukemic blasts at diagnosis or during relapse. The blast population grows indiscriminately because these cells have only limited differentiation capability and are frozen in the earliest stage of development. The lineage of blasts that predominate depends on the specific type of acute leukemia. It is recommended that the blast percentage in the bone marrow be derived from a 500-cell differential count. Myeloblasts may be distinguished from lymphoblasts in three ways: presence of Auer rods, reactivity with cytochemical stains, or reactivity with cell surface markers. An experienced morphologist can often determine the morphology of blasts; however, other supporting tests are always needed to confirm the initial designation. The chromatin material of a myeloblast is usually much finer than that of a lymphoblast. Although a myeloblast is usually larger than a lymphoblast, sufficient variations are seen that this is not the best factor to consider. Along the same lines, the number of nucleoli that can be seen in a myeloblast is one to four, and the number of lymphoblasts is one to two, so when deciding lineage on a blast with two obvious nucleoli, either choice would be acceptable. As mentioned previously, other methods besides morphologic examination must be used to confirm the type of blasts present and often to quantify the number of blasts, particularly when two blast populations coexist in the significant amounts in the leukemic bone marrow. Cytochemical Stains Cytochemical stains are very helpful in the diagnosis and classification of acute leukemias (Table 11. These stains are usually performed on bone marrow smears but may also be done on peripheral smears or bone marrow touch preparations. Because the special stains are used to identify enzymes or lipids within the blast population of cells, the reaction in mature cells is not important. Many institutions have replaced cytochemical stains with immunologic testing that uses flow cytometry or immunohistochemistry or both. The granules are found in the late myeloblast and exist throughout all the myeloid maturation stages. Promyelocytes, myelocytes, metamyelocytes, and band and segmented neutrophils stain strongly positive, indicated by the presence of blue-black granules. Because lymphoid cells, nucleated red blood cells, and megakaryoblasts lack this enzyme, they stain negative. The enzymatic activity in blood smears fades over time, so slides should not be held for staining for more than 3 weeks. Phospholipids are found in the primary (nonspecific) and secondary (specific) granules Table 11. The stain is negative in lymphocytes, although rarely azurophilic granules of lymphoblasts may show positivity. The specific esterase enzymatic reaction is stable in paraffin-embedded tissue sections, making this an extremely useful stain for identifying cells of myeloid lineage in extramedullary myeloid tumors. Different substrates are available, with alpha-naphthyl butyrate stain considered more specific and alphanaphthyl acetate stain considered more sensitive. Many cells in addition to monocytes stain positive (macrophages, histiocytes, megakaryoblasts, and some carcinomas), so the sodium fluoride inhibition step is used to differentiate the positivity. In these cases, immunophenotyping can be used to confirm monocytic differentiation. The specific lineage and stage of maturation can be tagged, and this information is used to recommend appropriate therapy and can be correlated to prognosis. The blasts in many subtypes of acute leukemias have characteristic immunophenotyping reactions. Clinicians would have difficulty making a diagnosis without this information, whereas in other cases the immunophenotype is just one additional piece of diagnostic information. Immunophenotyping is performed by flow cytometry or by immunohistochemistry methods. Multiple antigens can be detected simultaneously on a single cell using flow cytometry. Molecular Analysis Molecular analysis can be used to identify clonality, such as immunoglobulin gene rearrangements. As with immunophenotyping, molecular analysis is helpful for detecting minimal residual disease and establishing prognostic indicators. The assignment of the particular nomenclature for the type of leukemia is based on the combined morphologic, immunophenotypic, cytochemical, cytogenetic, and sometimes molecular information and any unique clinical presentation. The array of cytologic and clinical information is used to suggest the best approximation of the subtype of leukemia, recognizing that knowledge is sometimes imperfect and that changes in these classifications will undoubtedly occur again in the future as understanding of the science of leukemia evolves. Acute leukemias are categorized according to the cell line and stage of maturation that predominate. The classification was initially based solely on morphology of the cells present; however, later results of cytochemistry staining reactions were incorporated into the classification. Immunophenotyping, cytogenic analyses, and molecular analyses are not well defined for the individual subtypes. Because of these limitations, and because of the discovery of numerous *For historic review only. In addition, leukemias with no single lineage differentiation are described as "acute leukemias of ambiguous lineage. Because technology of genetic and molecular analysis is moving so rapidly, however, it is Table 11. The reader is referred to other hematology reference texts for an in-depth discussion of immunophenotypes and genetics that are characteristic for each disorder. Auer rods are common, and maturation in the neutrophil lineage (promyelocytes, myelocytes, neutrophils) is seen. Numerous Auer rods (fused azurophilic granules) are present in the myeloblasts and promyelocytes, and bundles of Auer rods ("faggot cells") may be seen. These cases are characterized by cells with convoluted or lobulated nuclei that mimic promonocytes. These leukemic promyelocytes contain such small azurophilic granules that they are not visible by light microscopy.
Buy pantoprazole paypal
In the normal sequence of events chronic gastritis diagnosis cheap 40mg pantoprazole with mastercard, gamma chains are silenced, and beta chains increase, forming Hgb A between 3 and 6 months. Pathologic fractures and bony changes in the facial structure (thalassemic facies) and skull are normally seen and give a thalassemic individual a strange look. Bossing, or protrusion, of the skull is prominent, as is orthodontic misalignment. The spleen reaches enormous proportions because abnormal red blood cells have been harbored and sequestered on a daily basis. Many patients have splenectomies, and this surgery does ameliorate some of the anemia issues. Splenectomy presents the patient with other challenges, however, because it is not a benign procedure (see Chapter 2). Patients with beta thalassemia major absorb more iron through diet because of increased erythropoiesis, and they accumulate iron because they take in an additional 200 mg of iron with each transfusion of packed red blood cells. Treating and Managing Thalassemia Major Patients with thalassemia major are on either a lowtransfusion or a high-transfusion protocol. A lowtransfusion protocol treats the patient symptomatically, administering transfusion when symptoms warrant. There are good arguments for both protocols, bearing in mind that transfusion exposes the individual not only to excess iron but also to foreign red blood cell antigens and other blood-borne diseases. A high-transfusion protocol gives the patient the best hope for a normal quality of life by increasing his or her hemoglobin and providing better bone quality, better growth, less iron, and nearnormal spleen size. Iron overload looms as a major outcome of the high-transfusion protocol, however, and is the major focus of clinical management. Although noninvasive procedures are available, they are specialized and not available at every clinical facility. Iron overload poses significant risk to cardiac function and leads to hepatic and endocrine complications. Compliance is crucial in patients with thalassemia major and becomes difficult to maintain as the patient moves from childhood to adolescence and becomes less willing to be hooked up to the infusion pump. Despite compliance with chelating therapy, cardiac complications continue to be the leading cause of death in patients with thalassemia major. Therapeutic modalities for severely thalassemic patients include bone marrow transplantation and stem cell transplantation. For patients considering bone marrow transplant, finding a compatible donor is the necessary first step. If this can be accomplished, bone marrow transplant should be considered early, before the patient develops too many complications of thalassemia. Stem cell transplantation, although a viable alternative, takes much forethought and often is limited by the fact that stem cells have not been collected from the umbilical cord after delivery. Thalassemia Intermedia and Beta Thalassemia Trait Individuals with thalassemia intermedia are not a welldefined subset of thalassemia major patients. As a clinical group, they develop problems later in life than patients with thalassemia major, and they may not need transfusions. They develop larger spleens, but their transfusion requirements, if present, are less frequent. Patients with thalassemia intermedia may require iron depletion with Desferal therapy but much less frequently than patients with thalassemia major. Beta thalassemia trait is the heterozygous condition in which only one abnormal beta gene is inherited from the parent. Although a therapeutic trial of iron may not harm the patient in the long run, it is not good medical management. Patients who have microcytic indices may represent the largest number of anemia patients. A careful diagnosis that considers broader possibilities for a microcytic presentation is in the best interest of the patient and the health-care system as a whole (Table 5. Peripheral smear revealed moderate target cells, microcytes, hypochromia, and some fragments. Her peripheral smear abnormalities combined and her electrophoresis results are fairly conclusive for this alpha thalassemia. The physician had put her on a trial therapy with iron supplementation, but 3 weeks later her laboratory results were virtually the same. Insights to the Case Study this case illustrates a frequent problem in the diagnosis and management of a patient with microcytic indices. This condition is an inherited disorder in which only one normal beta gene is present. An abnormal beta gene is inherited from one parent; consequently, a full complement of Hgb A is not formed, and Hgb A2 is elevated. Patients lead a normal life, but pregnancy or illness may cause the anemia to worsen, and transfusion may be warranted in such cases. If the information is available, individuals who carry the beta thalassemic trait should identify themselves to their supervising physician. Which of the following laboratory tests would be abnormal through each stage of iron deficiency A patient presents with a microcytic, hypochromic anemia with ragged-looking red blood cells in the peripheral smear and a high reticulocyte count. A brilliant cresyl blue preparation reveals inclusions that look like pitted golf balls. The most cost-effective therapy for a patient with hereditary hemochromatosis is a. Of the four clinical states of alpha thalassemia, which is incompatible with life Although there are many complications in individuals with thalassemia major, which of the following is the leading cause of death A 36-year-old woman with chronic alcoholism, liver disease, and pneumonia was admitted to the hospital. This is a term used to describe the presence of younger white blood cells from the bone marrow in response to infection and inflammation. She noted red blood cell inclusions and identified them as Howell-Jolly bodies, but she felt insecure about the identity of the inclusion and no one was available to observe the inclusion. After consulting with the lead technologist, they reviewed the smear together to try to identify which inclusion was present. The next possibility was Pappenheimer bodies, small inclusions that look like grape clusters. Pappenheimer bodies are usually iron deposits either in the form of ferritin or hemosiderin. If they are suspected, an iron stain (Prussian blue) can confirm the presence of iron. A Prussian blue stain was performed, and the inclusions were confirmed to be siderocytes, iron-containing inclusions. These inclusions can be found in hemochromatosis, alcoholism, hemolytic anemia, and postsplenectomy. Hepcidin, a key regulator of iron metabolism and mediator of anemia of inflammation. Laboratory contributions to the diagnosis of common iron loading disorders and anemias. Screening for, hemochromatosis: Patients with liver disease, families and populations. Nicosia, Cyprus/Geneva: Thalassaemia International Federation/World Health Organization, 1995; 17. Red cell indices and therapeutic trial of iron in diagnostic workup for anemic Thai females. Compare and contrast the morphologic characteristics of megaloblasts and normoblasts in the bone marrow. Differentiate red blood cell and white blood cell changes in the peripheral smear that are seen in the megaloblastic anemias. Describe the pathway of vitamin B12 and folic acid from ingestion through incorporation into the red blood cell. Describe the relevant laboratory tests used in the diagnosis of megaloblastic anemia. Broadly defined, the macrocytic anemias are divided into two categories: megaloblastic and nonmegaloblastic processes. If the source of the anemia is vitamin B12 or folic acid deficiency, the anemia is termed megaloblastic.
Diseases
- Bahemuka Brown syndrome
- Schwartz Newark syndrome
- Congenital skin disorder
- Spondylocarpotarsal synostosis
- Oculo facio cardio dental syndrome
- Phocomelia syndrome
- Opitz Reynolds Fitzgerald syndrome
- Conotruncal heart malformations
Cheap pantoprazole 40mg free shipping
Laparoscopic removal is now widely employed in adult surgery gastritis diet ������� order generic pantoprazole pills, but the current lack of small instrumentation limits its use in very small children. A tumor diameter of more than 5 cm is a reasonable predictor of malignancy, whereas small adenomas may be approached with more conservative surgery. Despite the advantages of modern imaging, the current data show a continued reliance on surgical excision as the mainstay of therapy. Surgery is the primary therapy, and chemotherapy has not been effective in controlling widespread disease. Cushing Syndrome Approximately one third of children with adrenocortical tumors may have stigmata of Cushing syndrome. Carcinoma may be responsible in half, with the others having evidence of bilateral adrenal hyperplasia. The clinical presentation is related to excessive production of cortisol leading to protein catabolism, subsequent increased gluconeogenesis, and the typical obesity associated with cortisol excess. Moon facies, truncal obesity, and typical evidence of Cushing disease are generally obvious in infants. The differential diagnosis in cases exhibiting excess adrenocortical activity includes adrenal adenomas and iatrogenic administration of steroids. This latter iatrogenic excess is commonly seen in children receiving transplanted organs. They are more commonly seen in boys, and in these cases the differential diagnosis with primary gynecomastia must be elicited. Kropp Abnormalities discovered in the prenatal and perinatal period are often a cause of concern, anxiety, and apprehension on the part of the parents and physician. Specific initial management measures are required to ensure the best possible results. This chapter reviews the most common neonatal urologic emergencies, their presentations, and initial management steps during the first 24 to 48 hours of neonatal life. Further management details, after the initial stabilization period, are discussed elsewhere in this text. Hematuria Gross hematuria in a newborn, although uncommon, is a urologic emergency. Although no specific abnormality may be found, life-threatening conditions, such as renal vein thrombosis and renal artery thrombosis, may be the cause (see later). Other causes include renal calculi, infections, ureteropelvic junction obstructions, and other anomalies. One theory is that urethral bleeding can result from a withdrawal of maternal hormones. Oligohydramnios represents either an inability to produce urine or an impaired ability to void. Typically, the more severe the oligohydramnios, the more ominous the underlying pathology. In its most extreme form (Potter syndrome, renal agenesis), oligohydramnios is associated with limb contractures, low-set ears, and compressed facies. Absent renal function is seen in bilateral renal agenesis, bilateral multicystic renal dysplasia, or juvenile polycystic kidneys. No specific therapy is available, and the role of the urologist is to provide counseling. Otherwise, oligohydramnios represents the inability to void because of obstruction in the urinary tract. An inability to identify the location of the meatus often leads to a urologic consultation. Obstruction is almost never present, and gentle probing with a 5F feeding tube (although unnecessary) proves patency. Hypospadias does not represent an emergent condition, and no immediate intervention is required. The more proximal the hypospadias, the more common the presence of chordee and foreskin with a characteristic dorsal hood appearance. A distal hypospadias may be discovered at the time of circumcision; if so, the procedure should be aborted immediately in an attempt to salvage foreskin that may be used for later corrective surgery. Circumcision should not be performed until the time of corrective surgery later in life. The combination of hypospadias (especially a more proximal hypospadias) and a nonpalpable testicle is suspicious for an intersex condition and should prompt an appropriate workup. Delayed Voiding One of the most common urologic concerns of the newborn period is the absence of voiding. It is imperative to recognize that a normal neonate may not void for 24 hours or more. The most informative finding on physical examination is the presence of a distended bladder. If voiding does not occur within 24 hours, or with a particularly distended bladder, an abdominal ultrasound scan is warranted. If there has been oligohydramnios or bilateral prenatal hydronephrosis, an immediate investigation beginning with a renal and bladder ultrasound followed by a voiding Circumcision Complications the most common complication after circumcision is bleeding. Many of these bleeding episodes can be managed with the application of gentle pressure. If persistent, placement of interrupted dissolvable sutures may be required for homeostasis. A, Anteroposterior gross postmortem photograph of infant born with Potter syndrome, showing low-set ears, flattened nose, very large kidneys drawn on the abdomen (arrow) causing abdominal enlargement, and the oligohydramnios resulting in a small thorax. B, Anteroposterior radiograph of infant immediately after birth shows bulging abdomen and flanks and hypoplastic lungs. C and D, Longitudinal and transverse ultrasound images of right kidney show very large kidneys with diffusely abnormal echotexture. Additional ultrasound images showed multiple, small, bright echogenic densities with reverberation artifacts in keeping with some calcium sediments, representing nephrocalcinosis in the tubules within the pyramids. E, Gross image of kidney showing the calcium sediment seen on the ultrasound image. Careful inspection for urethral involvement must be performed when evaluating a circumcision injury. In the event of urethral involvement, the authors prefer a conservative initial approach with plans for delayed repair and catheter drainage only if necessary. These carry the risk of future incarceration of bowel and must be followed closely, with surgical correction on an elective basis. Enlarged Scrotum Newborns presenting with an enlarged scrotum need immediate evaluation. Differential diagnosis includes hydrocele with or without hernia, epididymitis, orchitis, testicular torsion, hemorrhagic infarction, torsion of the testicular appendix, and neoplasm. Perinatal Testicular Torsion Perinatal testicular torsion refers to prenatal torsion (torsion occurring before birth) and postnatal torsion (torsion occurring shortly after birth). The skin may be bluish to varying shades of red, and often has associated ecchymosis and erythema. The testicle may be slightly higher in the scrotum than the contralateral side and can be difficult to palpate depending on the amount of edema present. Most prenatal torsions are nontender, whereas early recognized postnatal torsion may still be tender on palpation. Although the physical examination may be suggestive of the diagnosis, if available a confirmatory emergent scrotal ultrasound scan is required. In the event of a testicular torsion, scrotal Hydroceles and Hernias Hydroceles and hernias are characterized by a transilluminating scrotum with a fluid-filled consistency, often with a slightly bluish hue. A and B, Transverse and longitudinal images of left scrotum show bilateral anechoic hydroceles with presumed patent processus vaginalis, and herniated loop of small bowel, which is also thickened. These decisions should occur with well-informed parents and take into consideration multiple factors. Availability of pediatric anesthesia, stability of the patient, proximity to neonatal health care for the family, presence of hydrocele that may make examination more difficult, and family reliability all should be weighed in this process. Additional findings may include areas of necrosis, subtunical fluid, or hydrocele. This is not to be confused with postnatal torsion or torsion that occurs after a normal physical examination has been performed. Such postexamination torsion requires immediate intervention as would be done for any later torsion-surgical detorsion and orchidopexy are required in an attempt to salvage the testicle. Although salvage rates of 50% have been reported,7 it is generally believed to be quite poor, with one large series reporting 0%8 for prenatal torsion and another reporting 5% for prenatal and postnatal combined.
Purchase pantoprazole 40 mg overnight delivery
When alpha chains cannot combine gastritis diet �10 order pantoprazole overnight delivery, they are unpaired and precipitate inside the red blood cell, causing a markedly decreased life span (7 to 22 days). Between 2 and 4 years of age, most young children with beta thalassemia major begin to show a failure to thrive, irritability, enlarged spleens, symptoms of anemia, jaundice, and transfusion requirement. Living With Thalassemia Major Patients and families with thalassemia major balance multiple health issues on a daily basis as they struggle to maintain a normal life. Medical management of this disease is continuous, frustrating, and disruptive for children who have the disease and parents who are caregivers and carriers. Severe anemia underlies most of the other complications; although variable, hemoglobin values are often 6 to 9 g/dL, about one-half the normal level. In the United States, more than 2 million individuals are carriers of the thalassemic gene, resulting in significant penetrance of this gene, which often results in disease. In beta thalassemia major, little or no beta chain is synthesized; consequently, no (or very little) Hgb A is synthesized. This condition results from a union between two carriers, and mendelian genetics indicate a one-infour chance of producing a severely affected individual. Beta thalassemia major is a serious genetic blood disorder, affecting multiple organs, quality of life, and longevity. Most infants born with thalassemia major are not ill for the first 6 months because fetal hemoglobin is the majority hemoglobin at birth. If the source of the anemia is unrelated to a nutritional deficiency, the anemia is macrocytic but not megaloblastic. There are multiple changes to white blood cells and red blood cells in the bone marrow structure that should be recognized and appreciated. The megaloblastic red blood cell precursors are larger, the nuclear structure is less condensed, and the cytoplasm is extremely basophilic or much bluer. There is asynchrony between the age of the nuclear material and the age of the cytoplasm, but this can best be appreciated by making a serious comparison of the nuclear and cytoplasmic material in megaloblastic precursor cells versus normoblastic precursor cells. When a cell stage is asynchronous, the nuclear age and the cytoplasmic age do not correspond. The normal red blood cell series is programmed for two specific functions: hemoglobin synthesis and nuclear expulsion. For the nucleus to be expelled, certain changes must occur in the size of the nucleus and the consistency of the nucleus structure. The chromatin that begins as fine, reticular, and smooth must take on a different texture and conformation before it is expelled from the orthochromic normoblast. In megaloblastic erythropoiesis, the texture and condensation of the nuclear material are disrupted. Megaloblastic chromatin in the megaloblastic pronormoblast and megaloblastic basophilic normoblast is open-weaved, with a clockface arrangement of chromatin-easily imagined if you look closely at the chromatin pattern. The nuclear (or chromatin) material is fragile and lacks the composition and condensation of a nucleus ready to be delivered from the cell. Likewise, the cytoplasmic material in the early megaloblastic precursors is extremely basophilic, much bluer than normal precursors. Students usually have a difficult time observing the difference between normal red blood cell precursors and megaloblastic precursors. A careful study of the nucleus:cytoplasm (N:C) ratio, cell size, nuclear material, and cytoplasm color in each stage of each cell can help differentiate one from the other. Erythropoiesis in the megaloblastic processes is ineffective, however, meaning destruction in the bone marrow of red blood cell precursors before they reach the peripheral circulation (Table 6. Megaloblastic precursor cells, especially at the polychromatophilic and basophilic states, hemolyze before their maturation cycle is complete. Orthochromic normoblasts or reticulocytes or both do not have the opportunity to be delivered from the bone marrow as they normally would in response to anemic stress. If erythropoiesis was effective and the bone marrow was responding to anemic stress, the peripheral smear would show evidence of a regenerative marrow process. Polychromasia and the presence of nucleated red blood cells would be self-evident (Table 6. Depletion of vitamin B12 stores takes years to develop because the storage rate is so high. Folic acid is readily available in green leafy vegetables, fruit, broccoli, and dairy products. Folic acid depletes quickly, within months, because the daily requirement is so much higher (Table 6. Pregnant women are encouraged to increase their folic acid intake because decreased folate may lead to neural tube defects. This structure cannot be formed unless it receives a methyl group from methyl tetrahydrofolate or folic acid. Vitamin B12 is the cofactor responsible for transferring the methyl group to methyl tetrahydrofolate. The synthesis of this component leads to nuclear fragmentation and destruction of cells and impaired cell division. Initially, the vitamin is taken in from the diet and separated from food by salivary enzymes. Next, vitamin B12 is transported to the stomach, where it combines with intrinsic factor, a substance secreted by the parietal cells of the stomach. If folate or vitamin B12 metabolism is flawed, homocysteine accumulates, potentially leading to thrombosis,3 a potential consequence to the hemostatic system that is just being realized. More than 20% of elderly individuals may be vitamin B12 deficient, and these patients often go unrecognized. Expanding the definition of individuals who should be tested would potentially improve the diagnosis of megaloblastic anemia. Patients may experience glossitis (sore or enlarged tongue), dyspepsia, or diarrhea. Evidence of neurologic involvement may be seen, with patients experiencing numbness, vibratory loss (paresthesias), and difficulties in balance and walking. Personality changes that may be observed include mania, disorientation, depression, and impaired memory. Vitamin B12 deficiency causes a demyelinization of the peripheral nerves, the spinal column, and the brain, which can cause many more severe neurologic symptoms, such as spasticity or paranoia. Jaundice may be seen because the average red blood cell life span in megaloblastic anemia is 75 days, a little more than one-half of the average red blood cell life span of 120 days. The movement of folic acid into the circulation and tissues occurs with a little more ease. The blood smear in megaloblastic anemia is extremely relevant in the diagnosis and shows macrocytes, macro-ovalocytes, hypersegmented multilobed neutrophils, and little polychromasia with respect to the anemia. The presence of hypersegmented neutrophils (lobe count of more than five lobes) in combination with macrocytic anemia is a morphologic marker for megaloblastic anemias. This qualitative white blood cell abnormality appears early in the disease and survives through treatment. A bone marrow examination is not necessary for the diagnosis of megaloblastic anemia because the diagnosis of this disorder can be adequately made without this timeconsuming, costly, and invasive procedure. When problems with intrinsic factor develop, the condition is called pernicious anemia. George Minot and William Murphy of Boston were awarded the Nobel Prize in 1934 for their discovery that ingestion of liver successfully treated patients with pernicious anemia. Several factors may account for the lack of intrinsic factor in the stomach, including physical factors such as partial or whole gastrectomy or genetic and immune factors. Whatever the cause, either intrinsic factor is not being secreted, or it is blocked or neutralized in some way. Atrophic gastritis may occur in which gastric secretions are diminished and intrinsic factor fails to be secreted. Antibodies to intrinsic factor are present in 56% of patients with pernicious anemia, with 90% of patients showing parietal cell antibodies, suggesting a strong autoimmune component to this disorder.
Purchase generic pantoprazole on line
Bleeding may occur because of an inherited clotting factor defect or an acquired deficiency that is secondary to some other cause gastritis in children purchase pantoprazole 40mg on-line. Factors to consider in evaluating a bleeding disorder include patient history, physical examination, laboratory testing, and family bleeding history. Patients often do not perceive their bleeding as abnormal because that is all that they have ever known. Questions regarding the types and frequency of bleeding must be extremely specific and nonthreatening. Open bleeds include tongue bleeding, tonsil bleeding, gum bleeding, epistaxis, menorrhagia, umbilical cord bleeding, and circumcisional bleeding. Closed bleeds include soft tissue bleeds; genitourinary bleeding; gastrointestinal bleeding; and bleeding into muscle, joints, skin, bone, or skull. Not every patient experiences all types of bleeding, and some patients with clotting factor deficiencies never experience a bleeding episode. It is prudent, however, to gather as much information as possible to assess an individual with a history of bleeding. Plasma clotting factors are inactive enzymes that circulate in plasma awaiting activation when injury occurs. Clotting factors that are poorly synthesized, inactivated by inhibitors, consumed by a rogue clotting process, mutated, or functionally impaired lead to faulty hemostasis. History is rich with accounts of hemophilia, ranging from the Talmud to the British monarchy. Queen Victoria carried the abnormal gene and passed it through her offspring (nine births, five living children) into the Russian royal family, the Spanish dynasty, and the German royal family. Victoria herself had no family history of hemophilia, so her abnormal gene was acquired by spontaneous mutation, which occurs in 30% of cases. Symptoms in Hemophilia A Patients Clotting factors are measured in terms of their percent activity and their function in coagulation tests. Most clotting factors need to be available in the body at a minimum of 30% to achieve hemostasis. As these children become more mobile, ordinary activities such as crawling, walking, or running may present challenges. It is common to see a child with severe hemophilia in protective gear (knee pads, ankle pads, helmet) for outside play. Bleeding may occur in other areas, such as the gastrointestinal tract, the kidneys (hematuria), or gums, or in hematomas. Rather, bleeding continues for a longer time because of the decreased level of clotting factor. Many negative perceptions arise with this bleeding disorder, including deep dark family secrets, profuse bleeding from small wounds, excruciating pain, and early death. By definition, hemophilias represent any of a group of disorders in which a particular clotting factor is decreased. With 13 clotting factors necessary for clot formation, there should be a wide range of hemophilias. Both varieties are sex-linked recessive disorders, meaning that the mother carries the abnormal gene and passes the gene to her sons. Internal hemorrhages into the muscles and deep soft tissues may compress and damage nerves. Intracranial bleeding is a leading cause of death in individuals with hemophilia A, and other complications such as paralysis, coma, memory loss, or stroke may precede an eventual fatality. Female carriers of the hemophilia gene rarely have symptoms, but occasionally carriers may become symptomatic. The union of an individual with hemophilia and a female carrier is likely to produce a symptomatic female. Laboratory Diagnosis of Hemophilia Patients the most debilitating bleeds are muscle bleeds or joint bleeds, which have the potential for causing long-term disability, reduced range of motion, and intense pain. Hemarthrosis occurs in the joints as pooled blood damages the surrounding tissue while a clot eventually forms. The joint become less and less Laboratory diagnosis of hemophilia patients is fairly uncomplicated. Single factor assays provide a means of assessing the percent activity of a clotting factor. A standard curve is created using serial dilutions of normal plasma of known factor levels and assigning a 1:10 dilution of normal plasma as 100% activity. If the patient and deficient plasma give a normal result, the patient supplied the factor missing in the factor-deficient plasma. Treatment for Hemophilia A Patients Treatment options for hemophilia patients span decades and present one of the saddest treatment histories of any patient group with an inherited disorder. In the early days, treatment of patients with hemophilia A consisted of transfusing whole blood units to relieve symptoms. In 1957, it was realized that the deficient coagulation protein was a component of the plasma portion of blood. Cryoprecipitate presented a major breakthrough for hemophilia patients because it was an easily transfusable product that afforded individuals with the maximum level of factor. Clotting factor products came next in the chronology of treatment products for hemophilia. The products were lyophilized and freezedried and could be reconstituted and infused at home. This treatment offered hemophilia patients an independence they had not experienced previously. Finally, these individuals were in control because they could self-infuse when necessary and provide themselves with prompt care when a bleeding episode developed. Factor concentrates were made from pooled plasma from a donor pool that was not adequately screened. When each of these factors is brought to bear, the tragedy to the bleeding community is easily understood. No statistics are available for wives or children who might have been secondarily infected. Recombinant products, which became available in 1989, represent the highest purity product because they are not derived from humans. Production expenses for this product are very costly, and manufacturers pass these costs on to potential users. As a treatment alternative, gene therapy continues to provide hope for hemophilia patients. Complications from rejection of the virus vector in humans have proved to be a delicate issue, but researchers are optimistic that gene therapy for hemophilia patients can eventually succeed. Quality-of-Life Issues for Hemophilia A Patients Having a child with severe hemophilia A or hemophilia B presents special challenges to parents and the family unit. Costs can reach $50,000/year if a patient has several bleeding episodes that require hospitalization. Individuals with a chronic condition face many anxieties and may struggle with feelings of isolation, anger, and disappointment (Table 17. The United States has hemophilia treatment centers that offer a network of needed services, and many states have local chapters of the National Hemophilia Foundation. Treatment for patients who develop inhibitors is difficult, and treatment protocols follow various paths. All of the conditions concerning inheritance, clinical symptoms, laboratory diagnosis, and complications are the same for patients with severe hemophilia B as for patients with severe hemophilia A. Most of these disorders are autosomal recessive and affect both males and females. A survey of the 225 hemophilia treatment centers in the United States determined that 7% of patients have a rare bleeding disorder. Abnormal preoperative screenings led to the diagnosis of most of these patients, but only half of them required therapy when bleeding occurred.
Cheap 40 mg pantoprazole otc
During the mean follow-up of 47 months diet during gastritis purchase pantoprazole 40 mg otc, no associated intracranial neuroblastic tumor was observed in Table 5. In contrast, 1 of 18 at-risk patients treated without chemotherapy developed an associated intracranial tumor (112). If a pineal or suprasellar mass is found, a decision must be made concerning biopsy. However, other oncologists feel more comfortable with a biopsy of the intracranial lesion. The treatment of trilateral disease with surgery alone or in combination with radiotherapy resulted in a few long-term survivors (109,113,114). In 78 patients (83%) the intracranial tumor was in the pineal region, and in 16 patients (17%) it was in the suprasellar region. For patients who received no treatment the median survival was 1 month, whereas it was 8 months for those who received treatment. Of the six children who survived more than 2 years after diagnosis of intracranial primitive neuroectodermal tumor, all received chemotherapy and four received craniospinal radiotherapy. For the 75 children for whom patterns of failure were reported, 55% had disseminated neuraxis disease (110). If the recurrent lesion is small and favorably located, it may be treated with photocoagulation, cryotherapy, or a radioactive plaque, often with success. Amendola and coworkers (10,59) plaqued 29 eyes, 28 with group V disease for recurrent tumor. In some situations, the clinician faces the choice of enucleation or reirradiation with external beam. The overwhelming cause of enucleation was progressive tumor, not radiation damage. There appears to be no increase in secondary nonocular tumors in children receiving two courses of radiotherapy (117). What was noted was that prolonged time to enucleation was significantly associated with the likelihood of choroidal and ciliary body invasion. Coexisting retinal detachment and vitreous hemorrhage increased the likelihood of optic nerve involvement at the time of enucleation (118). At academic centers, such cases often are referred from institutions where the initial treatment was given by physicians who thought, at first, that they were dealing with another diagnosis. By making the best possible use of the available data and by relying on sound clinical reasoning, the pediatric radiation oncologist can make the best of these vexing cases. Extensive involvement of the choroid along with retrolaminar extension of tumor or, even worse, involvement of the cut end of the optic nerve predicts a poor outcome. It is reasonable to consider more aggressive adjuvant treatment in these cases in an attempt to improve the outcome. Children who have undergone an intraocular operative procedure before definitive enucleation are at risk for orbital recurrence of tumor and nodal and hematogenous dissemination. We will now consider the appropriate treatment for children found to have one or more identified risk factors. The mold usually is prepared so that there is room for some petroleum jelly gauze between the mold and the orbital wall for a better depth dosage. The prosthesis is drilled and 192Ir or 125I is placed in the center of the sphere. Small series have been reported showing long-term survival with postoperative chemotherapy and radiotherapy (126,127). As regards chemotherapy, there is some debate concerning whether systemic treatment is adequate or intrathecal chemotherapy should also be used. Concerning radiotherapy, there is some debate as to whether orbital or whole brain radiotherapy is appropriate (4). It would be best if we had detailed patterns of failure analyses that made it clear what predicted for orbital only, brain only, systemic only, or some combination of sites relapses. Because most clinical series are small and describe a mixture of patients with orbital involvement at presentation, at relapse, and of varying sizes and extent, it is impossible to make unequivocal pronouncements on this topic. For the radiation oncologist, a sound policy is to irradiate the orbit alone unless there is extension into the brain or there are brain metastases. If the orbital disease is bulky, some treat with a combination of external beam and brachytherapy (4, 14,126). Optic Nerve Involvement Tumor may extend beyond the lamina cribrosa or to the end of the transected optic nerve. This argues strongly for the use of adjuvant therapy, but there are no prospective, randomized data proving the value of adjuvant therapy in this situation. Contemporary practice generally includes adjuvant chemotherapy for optic nerve involvement (carboplatin and etoposide or vincristine, carboplatin, and etoposide). Orbital external beam irradiation, using various dose schedules, is commonly used for tumor up to the line of transection. The posterior aspect of the irradiated volume should encompass the pathway of the optic nerve back to the optic chiasm. Some radiation oncologists advocate whole brain and orbital irradiation in this situation, but this approach is less popular. Retrolaminar tumor, without extension to the line of transection, is treated by adjuvant chemotherapy and orbital irradiation by some and by chemotherapy alone by others (8). When postoperative radiotherapy is used for the orbit, external beam treatment is most commonly used. Popular field arrangements include an anterior wedge pair, a single anterior field, or a 3D planned set of fields, usually four to six. However, use of intensity-modulated radiation is gaining favor for all cases where external beam is called upon. Coralline hydroxyapatite prostheses do not significantly affect the radiation dosage distribution (123). The Groote Schuur Hospital of Cape Town, South Africa, has described a technique using six rows of 125I arrayed around the periphery of the orbit, one central row, and seeds on a metal disc sutured beneath the eyelids. The benefits of this procedure compared with external beam treatment are felt to be a lower risk of bone growth abnormality, less failure of tooth eruption, a reduced risk of neuroendocrine injury, and a possible reduction in second malignant neoplasms. Local tumor control in the South African series has been excellent, although there have been some deaths from distant metastases (124). Another technique for postenucleation orbital brachytherapy is the creation of a mold. This technique is similar to that used at some institutions for brachytherapy for cervical or vaginal carcinoma. One child was salvaged with surgery and conventional therapy after suffering a meningeal relapse and is alive at 105 months after treatment. Dosimetry data, collected for patients with secondary bone and soft tissue sarcoma, showed a stepwise increase in secondary tumor relative risk with increasing dosage. In an analysis confined to bilateral cases the incidence of second tumors at 30 years was 34% for children irradiated at less than 12 months of age, 22% for children irradiated at more than 12 months of age, and 18% for those not irradiated. The rates for tumors outside the radiation field (including patients not irradiated) was 4. However, this list must be broadened to include malignant melanoma and thyroid carcinoma. The Eng study includes those previously reported by Abramson and therefore supersedes those reports. In a 1997 report, the cumulative incidence of second cancer at 50 years after diagnosis was 51% (140). The incidence of 8% outside the radiation field was similar to the 6% rate for the 78 patients who did not receive radiation.