Discount tadora generic
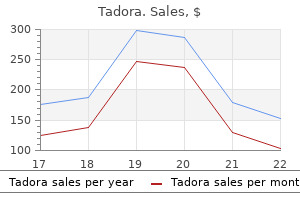
Diagnosis Aortic regurgitation is recognized clinically by its characteristic diastolic murmur testosterone associations with erectile dysfunction diabetes and the metabolic syndrome discount 20mg tadora visa, heard best along the right sternal border, and peripheral signs of a hyperdynamic circulation, including a widened pulse pressure, decreased diastolic blood pressure, and bounding pulses. In addition to the typical murmur of aortic regurgitation, there may be a low-pitched diastolic rumble (Austin-Flint murmur) that results from fluttering of the mitral valve caused by the regurgitant jet. As with mitral regurgitation, symptoms of aortic regurgitation may not appear until left ventricular dysfunction is present. Symptoms at this stage are manifestations of left ventricular failure (dyspnea, orthopnea, fatigue) and coronary ischemia. Common causes of leaflet abnormalities are infective endocarditis, rheumatic fever, bicuspid aortic valve, and the use of anorexigenic drugs. The operative mortality for isolated aortic valve replacement is approximately 4%. It is higher if there is concomitant aortic root replacement or coronary artery bypass grafting or if there are substantial comorbidities. The mortality rate of asymptomatic patients with normal left ventricular size and function is less than 0. In contrast, symptomatic patients have a mortality rate greater than 10% per year. In acute aortic regurgitation, immediate surgical intervention is necessary, because the acute volume overload results in heart failure. Alternatives to aortic valve replacement with a prosthetic valve include a pulmonic valve autograft (Ross procedure) and aortic valve reconstruction. Medical treatment of aortic regurgitation is designed to decrease systolic hypertension and left ventricular wall stress and improve left ventricular function. Intravenous infusion of a vasodilator such as nitroprusside and an inotropic drug such as dobutamine may be useful for improving left ventricular stroke volume and reducing regurgitant volume. Long-term therapy with nifedipine or hydralazine can be beneficial and may delay the need for surgery in asymptomatic patients with good left ventricular function. Decreased diastolic time (myocardial perfusion time), diastolic aortic pressure, and effective stroke volume reduce myocardial O2 supply. The heart rate must be kept above 80 beats per minute because bradycardia, by increasing the duration of diastole and thereby the time for regurgitation, produces acute left ventricular volume overload. An abrupt increase in systemic vascular resistance can also precipitate left ventricular failure. The compensations for aortic regurgitation may be tenuous, and anesthetic-induced myocardial depression may upset this delicate balance. If left ventricular failure occurs, it is treated with a vasodilator to reduce afterload and an inotrope to increase contractility. Overall, modest increases in heart rate and modest decreases in systemic vascular resistance are reasonable hemodynamic goals during anesthesia. Echocardiography will reveal any anatomic abnormalities of the aortic valve, including leaflet perforation or prolapse, and will identify any abnormalities in the aortic root and aortic annulus. Left ventricular size, volume, and ejection fraction can be measured, and Doppler examination can be used to identify the presence and severity of aortic regurgitation. These include regurgitant jet width as a percentage of overall left ventricular outflow tract width, pressure half-time, and diastolic flow reversal in the descending aorta. Cardiac catheterization and cardiac magnetic resonance imaging may be useful for grading aortic regurgitation if echocardiography is insufficient. Induction of anesthesia in the presence of aortic regurgitation can be achieved with an inhaled anesthetic or an intravenous induction drug. Ideally the induction drug should not decrease the heart rate or increase systemic vascular resistance. The increase in heart rate, decrease in systemic vascular resistance, and minimal myocardial depression associated with isoflurane, desflurane, and sevoflurane make these drugs excellent choices in patients with aortic regurgitation. In patients with severe left ventricular dysfunction, high-dose opioid anesthesia may be preferred. Bradycardia and myocardial depression from concomitant use of nitrous oxide or a benzodiazepine are risks of the high-dose narcotic technique. Neuromuscular blockers with minimal or no effect on blood pressure and heart rate are typically used, although the modest increase in heart rate associated with pancuronium administration could be helpful in patients with aortic regurgitation. Mechanical ventilation should be adjusted to maintain normal oxygenation and carbon dioxide elimination and provide adequate time for venous return. Intravascular fluid volume should be maintained at normal levels to provide for adequate preload. Bradycardia and junctional rhythm require prompt treatment with intravenous atropine. Management of Anesthesia Management of anesthesia in patients with tricuspid regurgitation includes maintenance of intravascular fluid volume and central venous pressure in the high-normal range to facilitate adequate right ventricular preload and left ventricular filling. Positive pressure ventilation and vasodilating drugs may be particularly deleterious if they significantly reduce venous return. Events known to increase pulmonary artery pressure, such as hypoxemia and hypercarbia, must also be avoided. A specific anesthetic drug combination or technique cannot be recommended for management of patients with tricuspid regurgitation. Agents that produce some pulmonary vasodilation and those that maintain venous return are best. Nitrous oxide can be a weak pulmonary artery vasoconstrictor and could increase the degree of tricuspid regurgitation, so it is best avoided. Intraoperative monitoring should include measurement of right atrial pressure to guide intravenous fluid replacement and to detect changes in the amount of tricuspid regurgitation in response to administration of anesthetic drugs. With high right atrial pressures, the possibility of right-to-left intracardiac shunting through a patent foramen ovale must be considered. Taking meticulous care to avoid infusion of air through intravenous fluid systems can reduce the risk of a systemic air embolism. Surgery in patients with asymptomatic aortic regurgitation may not require invasive monitoring. Standard monitors should be adequate to detect rhythm disturbances or myocardial ischemia. In the presence of severe aortic regurgitation, monitoring with a pulmonary artery catheter or transesophageal echocardiography is helpful for detecting myocardial depression, for facilitating intravascular volume replacement, and for measuring the response to administration of a vasodilating drug. The most common cause in adults is rheumatic heart disease with co-existing tricuspid regurgitation and often mitral or aortic valve disease. Carcinoid syndrome and endomyocardial fibrosis are even rarer causes of tricuspid stenosis. Tricuspid stenosis increases right atrial pressure and increases the pressure gradient between the right atrium and right ventricle. Right atrial dimensions are increased, but the right ventricular dimensions are determined by the degree of volume overload from concomitant tricuspid regurgitation. Evaluation by echocardiography and color flow Doppler imaging helps estimate the severity of the stenosis. Mild tricuspid regurgitation can be a normal finding at any age and is very commonly seen in highly trained athletes. Pathophysiology the basic hemodynamic consequence of tricuspid regurgitation is right atrial volume overload. The high compliance of the right atrium and vena cava result in only a minimal increase in right atrial pressure even in the presence of a large regurgitant volume. Signs of tricuspid regurgitation include jugular venous distention, hepatomegaly, ascites, and peripheral edema. The treatment of functional tricuspid regurgitation is aimed at the cause of the lesion, that is, at improving lung function, relieving left-sided heart failure, or reducing pulmonary hypertension. Other causes include connective tissue diseases, carcinoid syndrome, infective endocarditis, and rheumatic heart disease. An acquired form can be due to rheumatic fever, carcinoid syndrome, infective endocarditis, or previous surgery or other interventions. Significant obstruction can cause syncope, angina, right ventricular hypertrophy, and right ventricular failure. Aortic valve replacement has traditionally been accomplished via open heart surgery and the use of cardiopulmonary bypass. Patients who are deemed to be at very high risk or even inoperable because of age and multiple comorbid conditions have been treated medically or by balloon aortic valvotomy. This treatment might provide shortterm relief of symptoms but does not alter the natural history of severe aortic stenosis. The need for alternative treatment options for this population of patients with valvular heart disease is now being addressed.
Pygeum. Tadora.
- Low urine flow, nighttime urinating, and other symptoms of an enlarged prostate (benign prostatic hyperplasia or BPH).
- Are there safety concerns?
- What is Pygeum?
- Dosing considerations for Pygeum.
- How does Pygeum work?
- Inflammation, kidney disease, malaria, stomachache, fever, madness, sexual dysfunction, and other conditions.
- What other names is Pygeum known by?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96402
Purchase genuine tadora on line
Preoperative preparation is directed at treating active pulmonary infection and determining whether any significant organ inversion is present erectile dysfunction tips discount 20 mg tadora with mastercard. Inversion of the great vessels is a reason to select the left internal jugular vein for central venous cannulation. Uterine displacement in parturient women is logically to the right in these patients. Should a double-lumen endobronchial tube be considered, it is necessary to appreciate the altered anatomy introduced by pulmonary inversion. In view of the high incidence of sinusitis, nasopharyngeal airways should be avoided. These patients must use accessory muscles of respiration during all phases of the breathing cycle and must breathe slowly. After surgical exposure, the distal normal trachea is opened and a sterile cuffed tube is inserted and attached to the anesthetic circuit. Maintenance of anesthesia with volatile anesthetics is useful for ensuring maximum inspired concentrations of oxygen. Anesthesia for tracheal resection may be facilitated by the addition of helium to the inspired gases. This decreases the density of the gases and may improve flow through the area of tracheal narrowing. Bronchiolitis Obliterans Bronchiolitis is a disease of childhood and is most often the result of infection with respiratory syncytial virus. Treatment of bronchiolitis obliterans is usually ineffective, although corticosteroids may be administered in an attempt to suppress inflammation involving the bronchioles. Tracheal mucosal ischemia that may progress to destruction of cartilaginous rings and subsequent circumferential constricting scar formation is minimized by the use of high-volume, low-pressure cuffs on endotracheal tubes. Infection and hypotension may also contribute to events that culminate in tracheal stenosis. Symptoms may not develop until several weeks after tracheal Pulmonary edema is due to leakage of intravascular fluid into the interstitium of the lungs and into the alveoli. Acute pulmonary edema can be caused by increased capillary pressure (hydrostatic or cardiogenic pulmonary edema) or by increased capillary permeability. Pulmonary edema typically manifests as bilateral symmetrical opacities on chest radiography. However, this pattern of lung opacity is more commonly seen with increased capillary pressure than with increased capillary permeability. The presence of air bronchograms on chest radiography suggests increased-permeability pulmonary edema. Cardiogenic pulmonary edema is characterized by extreme dyspnea, tachypnea, and signs of sympathetic nervous system activation (hypertension, tachycardia, diaphoresis) that may be more pronounced than in patients with increased-permeability pulmonary edema. Pulmonary edema caused by increased capillary permeability is characterized by a high concentration of protein and secretory products in the edema fluid. As a result, there is atelectasis and leakage of intravascular fluid into the lungs, producing capillary permeability pulmonary edema. In addition, there may be tachypnea, bronchospasm, and acute pulmonary hypertension. Chest radiographs may not demonstrate evidence of aspiration pneumonitis for 6 to 12 hours after the event. Evidence of aspiration, when it does appear, is most likely to be in the right lower lobe if the patient aspirated while in the supine position. Measurement of gastric fluid pH is useful since it reflects the pH of the aspirated fluid. Measurement of tracheal aspirate pH is of no value because the aspirated gastric fluid is rapidly diluted by airway secretions. The aspirated gastric fluid is also rapidly distributed to peripheral lung regions, so lung lavage is not useful unless there has been aspiration of particulate material. There is no evidence that prophylactic antibiotics decrease the incidence of pulmonary infection or alter outcome. Despite the absence of confirmatory evidence that corticosteroids are beneficial, some practitioners treat aspiration pneumonitis with very large dosages of methylprednisolone or dexamethasone. Typically, this form of pulmonary edema occurs minutes to hours after central nervous system injury and may manifest during the perioperative period. Presumably, increased pulmonary capillary pressure leads to transudation of fluid into the interstitium and alveoli. Pulmonary hypertension and hypervolemia can also injure blood vessels in the lungs. The association of pulmonary edema with a recent central nervous system injury should suggest the diagnosis of neurogenic pulmonary edema. Unlike neurogenic pulmonary edema, chemical pneumonitis resulting from aspiration frequently persists longer and is often complicated by secondary bacterial infection. High-permeability pulmonary edema is suggested by high protein concentrations in the pulmonary edema fluid. Cocaine can also cause pulmonary vasoconstriction, acute myocardial ischemia, and myocardial infarction. There is no evidence that administration of naloxone speeds resolution of opioid-induced pulmonary edema. Treatment of patients who develop drug-induced pulmonary edema is supportive and may include tracheal intubation for airway protection and mechanical ventilation. The onset of symptoms is often gradual but typically occurs within 48 to 72 hours at high altitude. Fulminant pulmonary edema may be preceded by the less severe symptoms of acute mountain sickness. The cause of this highpermeability pulmonary edema is presumed to be hypoxic pulmonary vasoconstriction, which increases pulmonary vascular pressures. Treatment includes administration of oxygen and prompt descent from the high altitude. The time to onset of pulmonary edema after relief of airway obstruction ranges from a few minutes to as long as 2 to 3 hours. Tachypnea, cough, and failure to maintain oxygen saturation above 95% are common presenting signs and may be confused with pulmonary aspiration or pulmonary embolism. It is possible that many cases of postoperative oxygen desaturation are due to unrecognized negativepressure pulmonary edema. The pathogenesis of negative-pressure pulmonary edema is related to the development of high negative intrapleural pressure by vigorous inspiratory efforts against an obstructed upper airway. High negative intrapleural pressure decreases the interstitial hydrostatic pressure, increases venous return, and increases left ventricular afterload. In addition, such negative pressure leads to intense sympathetic nervous system activation, hypertension, and central displacement of blood volume. Together these factors produce acute pulmonary edema by increasing the transcapillary pressure gradient. Maintenance of a patent upper airway and administration of supplemental oxygen are sufficient treatment, because this form of pulmonary edema is typically transient and selflimited. Radiographic evidence of this form of pulmonary edema resolves within 12 to 24 hours. Hemodynamic monitoring may be useful in both the assessment and treatment of pulmonary edema. Intraoperative management should be a continuation of critical care management and include a plan for intraoperative ventilator management. The best way to ventilate patients with acute respiratory failure and restrictive lung disease has not been determined. However, because the pathophysiology is similar to that of acute lung injury and because there is the risk of hemodynamic compromise and barotrauma with the use of large tidal volumes and high airway pressures, it is reasonable to ventilate with low tidal volumes. Patients with restrictive lung disease typically breathe rapidly and shallowly, so tachypnea is likely during the weaning process and Intraoperative Rapid expansion of a collapsed lung may lead to pulmonary edema in that lung. The risk of reexpansion pulmonary edema after relief of a pneumothorax or pleural effusion is related to the amount of air or liquid that was present in the pleural space (>1 L increases the risk), the duration of collapse (>24 hours increases the risk), and the rapidity of reexpansion. High protein concentrations in the edema fluid suggest that enhanced capillary membrane permeability is important in the development of this form of pulmonary edema. Chronic Intrinsic Restrictive Lung Disease (Interstitial Lung Disease) Interstitial disease is characterized by changes in the intrinsic properties of the lungs, most often caused by pulmonary fibrosis. Pulmonary hypertension and cor pulmonale develop as progressive pulmonary fibrosis results in the loss of pulmonary vasculature.
Cheap tadora 20mg
A disadvantage of volume-cycled ventilation is the inability of these devices to compensate for leaks in the delivery system impotent rage definition generic tadora 20mg with amex. In the control mode, a preset respiratory rate ensures that a patient receives a predetermined number of mechanically delivered breaths even if there are no inspiratory efforts. In the assist mode, however, if Controlled ventilation the patient can create some negative airway pressure, a breath at the preset tidal volume will be delivered. Pressure-cycled ventilation provides gas flow into the lungs until a preset airway pressure is reached. Critically ill patients who require mechanical ventilation may benefit from continuous infusion of sedative drugs to treat anxiety and agitation and to facilitate coordination with ventilator-delivered breaths. Inadequate sedation or agitation can lead to life-threatening problems such as selfextubation, acute deterioration in gas exchange, and barotrauma. However, when acceptable sedation without hemodynamic compromise cannot be achieved, it may be necessary to produce skeletal muscle paralysis to ensure appropriate ventilation and oxygenation. Benzodiazepines, propofol, and narcotics are the drugs most commonly administered to decrease anxiety, produce amnesia, increase patient comfort, and provide analgesia during mechanical ventilation. Newer approaches to mechanical ventilation involving the use of permissive hypercapnia (Paco2 may reach 50 mm Hg) can cause substantial discomfort and necessitate deep sedation. Continuous infusion of drugs rather than intermittent injection provides a more constant and desirable level of sedative effect. Daily interruption of sedative infusions to allow the patient to "awaken" may facilitate evaluation of mental status and ultimately shorten the period of mechanical ventilation. Continuous infusion of propofol is uniquely attractive for this purpose, because the brief context-sensitive half-life of this drug is not influenced by the duration of the infusion, and rapid awakening is predictable. Prompt recovery from the effects of a remifentanil infusion also is not affected by the duration of the intravenous drug infusion. When sedation is inadequate or hypotension accompanies the administration of drugs used for sedation, the use of nondepolarizing neuromuscular blocking drugs to produce skeletal muscle relaxation may be necessary to permit optimal mechanical ventilation. Arrows indicate initiation of a spontaneous breath by the patient, who triggers the ventilator to deliver a mechanically assisted breath. It is better to use intermittent rather than continuous skeletal muscle paralysis to allow periodic assessment of the adequacy of sedation and the need for ongoing paralysis. Monitoring of neuromuscular blockade and titration of muscle relaxant doses so that a twitch response remains present is prudent. A risk of prolonged drug-induced skeletal muscle paralysis is accentuation of the diffuse polyneuropathy that may accompany critical illness. These examples of extraalveolar air almost always reflect dissection or passage of air from overdistended and ruptured alveoli. Infection increases the risk of barotrauma, presumably by weakening pulmonary tissue. Tension pneumothorax is the most common life-threatening manifestation of ventilator-induced barotrauma. Hypotension, worsening hypoxemia, and increased airway pressure suggest the presence of a tension pneumothorax. Atelectasis is a common cause of hypoxemia that develops during mechanical ventilation. Migration of the tracheal tube into the left or right main bronchus or development of mucus plugs should be considered when abrupt worsening of oxygenation occurs in the absence of hypotension. Arterial hypoxemia resulting from atelectasis is not responsive to an increase in Fio2. Other causes of sudden hypoxemia in mechanically ventilated patients include tension pneumothorax and pulmonary embolism, but in contrast to atelectasis, these are usually accompanied by hypotension. Bronchoscopy may be necessary to remove mucus plugs responsible for persistent atelectasis. Patients who undergo mechanical ventilation for treatment of acute respiratory failure are at risk of neuromuscular weakness that persists long after the cause of the respiratory failure has resolved. A common cause of diffuse skeletal muscle weakness is polyneuropathy of critical illness, an axonal disorder that occurs in the presence of sepsis and multiple organ system failure. Prolonged administration of nondepolarizing neuromuscular blocking drugs may contribute to the development of an acute myopathy, particularly in patients who undergo concomitant therapy with corticosteroids. The duration of drug-induced paralysis rather than the specific neuromuscular blocker used seems to be more important in the development of persistent weakness. Decreased clearance of active metabolites of nondepolarizing neuromuscular blocking drugs resulting from renal and/or hepatic dysfunction is also a consideration when persistent weakness follows prolonged administration of these drugs. The major pathogenic mechanism is microaspiration of contaminated secretions around the tracheal tube cuff. Diagnosis of pneumonia in the presence of acute respiratory failure may be difficult, since fever and pulmonary infiltrates may already be present in association with the cause of the acute respiratory failure. Treatment of nosocomial sinusitis includes administration of antibiotics, replacement of nasal tubes with oral tubes, and use of decongestants and head elevation to facilitate sinus drainage. Alveolar overdistention resulting from large tidal volumes (10 to 12 mL/kg) and high airway pressures (>50 cm H2O) may result in alveolar rupture and alveolar hemorrhage. These alveoli may collapse and reopen repeatedly, and this could be responsible for ventilator-induced lung injury. However, use of this form of ventilation may require acceptance of some degree of hypercarbia and respiratory acidosis and often a Pao2 of less than 60 mm Hg. Permissive hypercapnia or controlled hypoventilation may accompany the reduction in tidal volume and airway pressure designed to minimize or prevent alveolar overdistention. The increased respiratory drive associated with permissive hypercapnia causes discomfort, which makes deep sedation, skeletal muscle paralysis, or both necessary. Permissive hypercapnia is not recommended in patients with increased intracranial pressure, cardiac dysrhythmias, or pulmonary hypertension. Barotrauma may present as subcutaneous emphysema, pneumomediastinum, pulmonary interstitial emphysema, pneumoperitoneum, pneumopericardium, arterial gas embolism, Barotrauma Alveolar Overdistention Monitoring the progress of the treatment of acute respiratory failure includes evaluation of pulmonary gas exchange (arterial and venous blood gases, pHa) and cardiac function (cardiac output, cardiac filling pressures, intrapulmonary shunt). Mechanical ventilatory support can be withdrawn when a patient can maintain oxygenation and carbon dioxide elimination without assistance. Some of the guidelines that have been proposed for indicating the feasibility of discontinuing mechanical ventilation include (1) vital capacity of more than 15 mL/kg, (2) alveolar-arterial oxygen difference of less than 350 cm H2O while breathing 100% oxygen, (3) Pao2 of more than 60 mm Hg with Fio2 of less than 0. Breathing at rapid rates and with low tidal volumes usually signifies an inability to tolerate extubation. Ultimately, the decision to attempt withdrawal of mechanical ventilation is individualized and considers not only pulmonary function but also the presence of co-existing abnormalities. When a patient is ready for a trial of withdrawal from mechanical support of ventilation, three options may be considered: (1) synchronized intermittent mandatory ventilation, which allows spontaneous breathing amid progressively fewer mandatory breaths per minute until the patient is breathing unassisted; (2) intermittent trials of total removal of mechanical support and breathing through a T-piece; and (3) use of decreasing levels of pressure-support ventilation. Overall, correcting the underlying condition responsible for the need for mechanical support of ventilation seems to be more important for successful extubation than the weaning method. Deterioration in oxygenation after withdrawal of mechanical ventilation may reflect progressive alveolar collapse, which can be responsive to treatment with continuous positive airway pressure rather than reinstitution of mechanical ventilation. Several things may interfere with successful withdrawal from mechanical ventilation and extubation. Excessive workload on the respiratory muscles imposed by hyperinflation, copious secretions, bronchospasm, increased lung water, or increased carbon dioxide production from fever or parenteral nutrition greatly decreases the likelihood of successful tracheal extubation. Use of noninvasive ventilation as a bridge to discontinuation of mechanical ventilation may occasionally be considered. This involves early extubation with immediate application of a form of noninvasive ventilation. However, noninvasive ventilation may impair the ability to clear airway secretions if the patient does not have a good cough, and there may be inadequate control of minute ventilation. Tracheal extubation should be considered when patients tolerate 30 minutes of spontaneous breathing with a continuous positive airway pressure of 5 cm H2O without deterioration in arterial blood gas concentrations, mental status, or cardiac function. Likewise, the Paco2 should remain less than 50 mm Hg, and the pHa should remain above 7. Patients should be alert with active laryngeal reflexes and the ability to generate an effective cough and clear secretions. Protective glottic closure function may be impaired following tracheal extubation, which results in an increased risk of aspiration. Weaning from supplemental oxygen is accomplished by gradually decreasing the inspired concentration of oxygen, as guided by measurements of Pao2 and monitoring of oxygen saturation by pulse oximetry.
Order tadora 20 mg overnight delivery
In both groups zma erectile dysfunction purchase tadora 20mg without a prescription, there was an increase in urinary albumin excretion during pregnancy (592 versus 119 mg/24 hr, respectively; P =. Rossing and colleagues66 evaluated the effect of pregnancy on deterioration of renal function in 93 women older than 20 years of age. They compared groups of never-pregnant and ever-pregnant women who received similar medical therapy and who had similar degrees of renal function at the start of the study. About 60% of births are premature, often because of uncontrollable hypertension, renal failure, or fetal growth failure. Among the 20% to 25% of pregnancies ending in live births, 40% of babies are severely growth restricted. A major practical problem with achieving a successful pregnancy outcome while on hemodialysis is proper maintenance of maternal vascular volume. Dialysis teams are accustomed to removing significant vascular volume at each session. This volume augmentation is required to maintain uteroplacental perfusion and fetal growth. The poor prognosis associated with hemodialysis combined with other considerations has prompted increased interest in continuous ambulatory peritoneal dialysis. Although fluid and chemical balance is constant and heparinization is not necessary, intrauterine deaths, abruption, prematurity, hypertension, and fetal distress still occur. The best strategy for most diabetic women on dialysis who desire pregnancy is to undergo kidney transplantation. Renal Transplantation and Diabetic Pregnancy Successful pregnancy after renal transplantation is now a reality. Deshpande and colleagues performed a systematic review and meta-analysis of articles published between 2000 and 2010 consisting of 50 studies with 4706 pregnancies in 3570 transplant recipients. Outcomes were more favorable in those pregnancies with lower mean maternal age, and obstetric complications were more frequent with a shorter mean interval between transplantation and pregnancy. In composite studies of all types of diabetic pregnancies, the incidence of hypertensive disorders during pregnancy varied from 15% to 30%, with the rate of hypertension increased fourfold over that for the nondiabetic population. In women with pregestational diabetes, the prevalence of chronic hypertension increases with duration of diabetes and is closely associated with nephropathy. The diagnosis is strengthened if the mean blood pressure fails to decline normally in the late second trimester, the blood urea nitrogen level is greater than 10 mg/dL, the serum creatinine concentration is greater than 1 mg/dL, creatinine clearance is less than 100 mL/min, or a combination of these factors is present. Preeclampsia Preeclampsia occurs two to four times as frequently in women with pregestational diabetes as in those without diabetes. The risk of developing preeclampsia is proportional to the duration of diabetes before pregnancy, the preexistence of nephropathy and hypertension, and the level of glycemic control when the pregnancy began. Heart Disease Although it is uncommon, atherosclerotic heart disease may afflict diabetic patients in the later reproductive years. For diabetic women with cardiac involvement, pregnancy outcome is dismal, with a maternal mortality rate of 50% or higher and perinatal loss rates approaching 30%. Compromised cardiac function may also be difficult to detect in patients who are restricted to bed rest for hypertension or poor fetal growth. With intensive monitoring, successful pregnancy is possible, albeit hazardous, for women with significant cardiac disease. Precipitating factors for ketoacidosis include pulmonary, urinary, or soft tissue infections; poor compliance; and unrecognized new onset of diabetes. Fetal well-being in particular is in jeopardy until maternal metabolic homeostasis is reestablished. This leads to increased hepatic glucose release but decreased or absent tissue disposal of glucose. Glucose-lacking tissues release ketone bodies, and vascular hyperglycemia promotes osmotic diuresis. Over time, the diuresis causes profound vascular volume depletion and loss of electrolytes. Left unchecked, this cycle of dehydration, tissue hypoglycemia, and electrolyte depletion can lead to multisystem collapse, coma, and death. If hyperglycemia is not corrected, diuresis, dehydration, and hyperosmolality follow. Pregnant women in the early stages of ketoacidosis respond quickly to appropriate treatment of the initiating cause. A serum bicarbonate level lower than 18 mg/dL or an anion gap exceeding 10 to 15 mEq/L should prompt performance of an arterial blood gas analysis. Typical initiators include pyelonephritis and pulmonary or gastrointestinal viral infections. The patient will continue to generate vascular volume deficits until her glucose levels and acidosis are largely resolved. Potassium chloride should be added to the infusate when the plasma potassium level nears the lower limit of normal. Although intermittent injections may be used, a continuous infusion of regular or short-acting insulin. However, even if the fetal status is questionable during the phase of therapeutic volume and plasma glucose correction, emergency cesarean delivery should be avoided. Usually, correction of the maternal metabolic disorder is effective in normalizing fetal status. Nevertheless, if a reasonable effort has been expended in correcting the maternal metabolic disorder and the fetal status remains a concern, delivery should not be delayed if the maternal condition is stable. Nevertheless, the perinatal mortality rates reported for diabetic women remain approximately three times those observed in the nondiabetic population, with congenital malformations, respiratory distress syndrome, and extreme prematurity accounting for the majority. Recognizing these risks, many experts have recommended early delivery (at 37 to 38 weeks) to optimize fetal outcome. Even among women with excellent glycemic control, delivery at term increases the risk of fetal demise, fetal macrosomia, and birth injury. Miscarriage Studies of miscarriage rates from several decades ago indicated an increased incidence of spontaneous abortion among women with pregestational diabetes, especially those with poor glucose control during the periconceptional period. Given the welldocumented association between congenital anomalies and hyperglycemia, such a finding is not surprising. They found an increasing rate among patients with more advanced classes of diabetes: Rates for White classes C, D, and F were 25%, 44%, and 22%, respectively, compared with a 15% expected rate in the nondiabetic population. Later studies of populations with better preconceptional glycemic control reported miscarriage rates similar to those in the nondiabetic population, indicating that diabetic women with excellent glycemic control have a risk of miscarriage equivalent to that in women without diabetes. Patients who present in early pregnancy with normal glycohemoglobin values can be reassured that the overall elevation in risk of miscarriage is modest. However, for patients with glycohemoglobin values 2 to 3 standard deviations above the norm, intense early pregnancy surveillance is indicated. Congenital Anomalies Among women with overt diabetes before conception, the risk of a structural anomaly in the fetus is increased threefold to eightfold, compared with the 1% to 2% risk for the general population. A classic report by Miller and associates83 compared the frequency of congenital anomalies in patients with normal or high first-trimester maternal glycohemoglobin levels and found only a 3. Bell and coworkers studied 1677 pregnant women with diabetes and more than 400,000 controls. The typical congenital anomalies observed in diabetic pregnancies and their frequency of occurrence are listed in Table 59-6. The mechanism by which hyperglycemia disturbs embryonic development is multifactorial. Diabetic teratogenesis has been associated with oxidative stress,86 enhanced lipid peroxidation,87 decreased antioxidative defense capacity,88 and sorbitol accumulation. Because the critical time for teratogenesis is during the period 3 to 6 weeks after conception, nutritional and metabolic intervention must be instituted preconceptionally to be effective. Several clinical trials of preconceptional metabolic care have demonstrated that malformation rates equivalent to those in the general population can be achieved with meticulous glycemic control. Wahabi and colleagues analyzed 12 cohort studies with low or medium risk of bias involving 2502 women with diabetes who did or did not participate in preconception care. In these studies, preconception care lowered Hb A1C in the first trimester of pregnancy by an average of 2. These results demonstrated that periconceptional folic acid use was related to a reduction of approximately 20% in the prevalence of any congenital heart defect. This association suggests that uteroplacental vasculopathy may promote restricted fetal growth in these patients. Fetal Macrosomia Macrosomia has been defined using various criteria, such as birth weight greater than the 90th percentile for gestational age, gender, and race; birth weight greater than 4000 g; and estimates of neonatal adiposity based on body composition measures.
Purchase tadora 20mg otc
Magnetic Resonance Imaging Magnetic resonance imaging can be safely used during pregnancy to evaluate adnexal masses even without the use of gadolinium-based contrast erectile dysfunction late 20s cheap tadora 20 mg on line. This phenomenon and the rapid return of these structures to their normal anatomic location after parturition increases the risk for torsion of adnexal masses in pregnancy, particularly at the beginning of the second trimester and during postpartum involution. Ultrasonographic criteria can successfully stratify the risk by identifying the few masses with suspect complex features that warrant surgical management. Most masses have a benign ultrasonographic appearance, and they are suitable for conservative (expectant) management. Surgery Surgical management of adnexal masses during the first trimester should be limited to lesions with complications. Persistence of adnexal pathology during the second and third trimester may warrant intervention if there is a strong suspicion of malignancy or large size (>6 cm), or if there are symptomatic complaints. A large size may signal increased risk for torsion, rupture, or obstruction during labor. Before undergoing surgical removal, patients should be appropriately counseled about the possibility of an underlying malignancy and be prepared for possible ovarian cancer staging and related evaluation of tumor serum markers. Although the risks to mother and fetus have been substantially reduced with the improvement of anesthesia, intraoperative and postoperative care, and prenatal care, surgery during pregnancy requires a trained team of surgeons and anesthesiologists and close monitoring postoperatively. Laparoscopy offers clear advantages to exploratory laparotomy for surgical management of adnexal masses, including less invasive surgical management and a shorter postoperative course with fewer complications. Sound clinical judgment is critical for patient selection, and caution is strongly advised when considering laparoscopic management of possible ovarian cancer. Although many case series proposed aspiration of simple unilocular cysts to avoid the need for major surgery, to provide symptomatic relief, or to allow these masses to fit into endoscopic bags, aspiration of a complex ovarian cyst runs the potential risk for malignant fluid spillage, which is associated with decreased survival. Whether by laparoscopy or laparotomy, consideration can be given to ovarian cystectomy if the imaging criteria for a benign mass are met. Delaying surgery because of fear about the risks of the operation may lead to increased fetal and maternal complications. Adverse fetal outcomes associated with abdominal surgery are most commonly the result of an abdominal catastrophe, such as ovarian torsion or rupture as indications for the surgery. In elective surgical cases, there seems to be no association between surgery and adverse perinatal outcome. Hess and colleagues71 reported that patients who underwent emergency surgery because of adnexal torsion or hemorrhage had a greater incidence of abortion and preterm delivery than patients who underwent elective laparotomy. Elective surgical intervention is preferably timed for the second trimester, when the risk for fetal loss is minimal. Laparotomy in the third trimester was associated with a 50% risk for preterm delivery. The effectiveness of tocolytics for suppression of preterm delivery associated with adnexal surgery is similar to that of tocolysis administered for preterm labor. Whitecar and coworkers61 reported that tocolytics were administered to 13 patients who had operations in the second and third trimesters; 6 of 13 had 69 Benign Gynecologic Conditions in Pregnancy 1165 preterm deliveries, although only two delivered within 2 weeks of laparotomy. Uterine malformations result in an abnormal uterine cavity, which is thought to impair reproductive performance, increasing the incidence of early and late abortions, preterm deliveries, and obstetric complications. Other factors may be associated with the anatomic anomalies and may have the potential to affect pregnancy outcomes. Such factors may explain why even a minor uterine anomaly, such as arcuate uterus, has been found by some investigators to result in an excess of spontaneous abortions, second-trimester losses, and preterm deliveries. Accurate identification of the type of uterine malformation is important because each type is associated with different rates of obstetric complications. Traditionally, diagnosis rested on hysteroscopy, hysterosalpingography, or sonohysterography for visualization of the uterine cavity, and on laparoscopy or laparotomy for intraabdominal views. Three-dimensional ultrasound and saline contrast sonohysterography appear promising for reliable diagnosis and classification of congenital uterine anomalies in a noninvasive way. When a recent study compared the accuracy of three-dimensional ultrasound with hysterosalpingography for diagnosing congenital uterine anomalies, 30 of 30 were correctly identified by three-dimensional sonography, but only 10 of 30 by hysterosalpingography. Septate uterus has been associated with the poorest reproductive outcome, mainly because of an association with a high rate of spontaneous abortion. The risk for uterine rupture should be considered in the presence of asymmetric uterine malformations or uterine anomalies of unclear types. Identification of fetal growth restriction and of postural deformities can be achieved by serial sonographic assessments during pregnancy. Fetal presentation during labor should be verified with ultrasonography in doubtful cases. Leach K, Khatain L, Tocce K: First trimester myomectomy as an alternative to termination of pregnancy in a woman with a symptomatic uterine leiomyoma: a case report, J Med Case Reports 5:571, 2011. Condous G, Khalid A, Okaro E, et al: Should we be examining the ovaries in pregnancy Bromley B, Benacerraf B: Adnexal masses during pregnancy: accuracy of sonographic 42.
Generic tadora 20 mg fast delivery
Occlusion of specific arteries distal to the circle of Willis results in predictable clinical neurologic deficits (Table 10-5) impotence jelqing cheap tadora 20mg with mastercard. Acute Ischemic Stroke Patients who experience the sudden onset of neurologic dysfunction or describe neurologic signs and symptoms evolving over minutes to hours are most likely experiencing a stroke. A transient ischemic attack is a sudden vascular-related focal neurologic deficit that resolves promptly (within 24 hours). A transient ischemic attack is not considered a separate entity but rather evidence of an impending ischemic stroke. Stroke represents a medical emergency, and the prognosis depends on the time elapsed from the onset of symptoms to thrombolytic intervention if thrombosis is the cause of the symptoms. Patients who receive early treatment to restore cerebral perfusion have better outcomes. Systemic hypertension is the most significant risk factor for acute ischemic stroke, and long-term treatment of systolic or diastolic hypertension dramatically reduces the risk of a first stroke. Cigarette smoking, hyperlipidemia, diabetes mellitus, excessive alcohol consumption, and increased serum homocysteine concentrations are also associated with increased risk of acute ischemic stroke. This distinction is important, because treatment of hemorrhagic stroke is substantially different from treatment of ischemic stroke. Alternatively, transcranial Doppler ultrasonography can provide indirect evidence of major vascular occlusion and offers the advantage of real-time bedside monitoring in patients undergoing thrombolytic therapy. Acute ischemic stroke most likely reflects embolism occurring as a result of a cardiac cause, for example, atrial fibrillation, ventricular akinesis following myocardial infarction, dilated cardiomyopathy, valvular heart disease, large vessel atherothromboembolism (from atherosclerotic narrowing, especially at major arterial branch points such as the carotid bifurcation), or small vessel occlusive disease (lacunar infarction). Patients with long-standing diabetes mellitus or systemic hypertension are most likely to experience acute ischemic stroke resulting from small vessel occlusive disease. Echocardiography is useful for evaluating the presence of anatomic or vascular anomalies that could result in embolization. Intravenous recombinant tissue plasminogen activator is used in patients who meet specific eligibility requirements and in whom treatment can be initiated within 3 hours of the onset of acute symptoms. Despite advances in the treatment of acute ischemic stroke, most patients will have residual neurologic dysfunction. The initial stroke severity is a strong predictor of outcome, and early evidence of recovery is a good prognostic sign. Management of the airway, oxygenation, ventilation, systemic blood pressure, blood glucose concentration, and body temperature are part of the overall medical management of acute ischemic stroke. The expanding infarction may cause focal or diffuse mass effects that typically peak 2 to 5 days following stroke onset. Large hemispheric strokes may be characterized by malignant middle cerebral artery syndrome, in which the edematous infarcted tissue causes compression of the anterior and posterior cerebral arteries and results in secondary infarctions. Similarly, infarction of the cerebellum may result in basilar artery compression and brainstem ischemia. Mortality rates for both middle cerebral artery syndrome and infarction of the cerebellum approach 80%. Craniotomy with cerebellar resection is a lifesaving intervention for acute cerebellar stroke because it prevents secondary brainstem and vascular compression. Malignant middle cerebral artery syndrome may be amenable to treatment with hemicraniectomy. Ventilatory drive is usually intact except after medullary or massive hemispheric infarction. The ability to protect the lungs against aspiration may be impaired in the acute setting, so that endotracheal intubation is necessary. In most patients, however, supplemental oxygen administration without endotracheal intubation is sufficient to maintain arterial oxygen saturation at more than 95%. Hypertension often gradually decreases during the first few days following an acute stroke. Antihypertensive drug therapy such as small intravenous doses of labetalol may be used when necessary to maintain the systemic blood pressure at less than 185/110 mm Hg in an attempt to lessen myocardial work and irritability. Appropriate intravascular volume replacement in patients with acute stroke improves cardiac output and cerebral perfusion. Hyperglycemia appears to parallel poor outcomes in patients experiencing acute ischemic stroke. During periods of cellular hypoxia or anoxia, as occur with stroke, glucose is metabolized to lactic acid, which results in tissue acidosis and increased tissue injury. Normalization of blood glucose concentration is recommended, using insulin when appropriate. Based on animal data, hypothermia may improve outcome following acute ischemic stroke as a result of its ability to decrease neuronal oxygen demands, cerebral edema, and neurotransmitter toxicity. There are few human studies evaluating the effectiveness of hypothermia for the reduction of morbidity and mortality from acute stroke. Normothermia should be maintained in acute ischemic stroke patients using antipyretics or cooling blankets as necessary. Prophylaxis to prevent deep vein thrombosis is initiated early in the treatment of patients experiencing acute ischemic stroke. Patients with acute hemorrhage who cannot be given heparin are treated with pneumatic compression stockings. Acute Hemorrhagic Stroke Acute hemorrhagic stroke results from either intracerebral hemorrhage or subarachnoid hemorrhage. Acute hemorrhagic stroke cannot be reliably distinguished from ischemic stroke based on clinical criteria alone. The estimated volume of extravasated blood and the level of consciousness are the two most reliable predictors of outcome. Patients with intracerebral hemorrhage often deteriorate clinically as cerebral edema worsens during the first 24 to 48 hours following the acute bleed. The efficacy of earlier surgical evacuation of a hematoma to decrease ischemic injury and edema to the surrounding tissue remains unclear. Prompt ventricular drainage should be performed to treat any signs of hydrocephalus. Sedation (with propofol infusion, barbiturates, or benzodiazepines), with or without drug-induced skeletal muscle paralysis, is often helpful in managing patients who require endotracheal intubation. Various pathologic conditions such as hypertension, coarctation of the aorta, polycystic kidney disease, fibromuscular dysplasia, and the occurrence of cerebral aneurysms in first-degree relatives are associated with the presence of cerebral aneurysms. The risk of aneurysm rupture depends on the size of the aneurysm, with a 6% risk of rupture during the first year in aneurysms of at least 25 mm in diameter. Other risk factors for rupture include hypertension, cigarette smoking, cocaine abuse, female sex, and use of oral contraceptives. A common presentation of an unruptured aneurysm is the development of a new focal neurologic deficit. The cause of this new deficit may be either a mass effect from an expanding aneurysm that compresses normal neurologic structures or small emboli to the distal cerebral circulation from a thrombus contained within the aneurysm. New-onset seizures can indicate an unruptured aneurysm and are thought to result from the formation of a glial scar (gliosis) in brain parenchyma adjacent to the aneurysm. Unruptured aneurysms may also be identified incidentally on cerebral imaging performed for unrelated reasons. For aneurysms smaller than 10 mm in diameter, the annual risk of rupture is approximately 0. Aneurysm diameter is not static; thus, although smaller aneurysms may be followed with serial imaging, larger aneurysms are often considered for surgery. In addition to severe headache, the rapid onset of photophobia, stiff neck, decreased level of consciousness, and focal neurologic changes suggest subarachnoid hemorrhage. Prompt establishment of the diagnosis followed by treatment of the aneurysm can decrease morbidity and mortality. Two of the most common methods used to grade the severity of subarachnoid hemorrhage are the Hunt and Hess classification and the World Federation of Neurologic Surgeons grading system (Table 10-6). These grading systems are useful because they help predict severity and outcome and can be used as metrics to evaluate the efficacy of various therapies. This same catecholamine release may result in cardiac dysrhythmias and may also be responsible for producing pulmonary edema. Echocardiography has demonstrated temporary depression of myocardial contractility, independent of coronary artery disease, in patients with subarachnoid hemorrhage. Of note, apical cardiac function may be preserved, a phenomenon attributed to the paucity of sympathetic innervation at the cardiac apex. Treatment of subarachnoid hemorrhage involves localizing the aneurysm with conventional or magnetic resonance angiography and surgically excluding the aneurysmal sac from the intracranial circulation while preserving its parent artery.
Syndromes
- Surgery to prevent the buildup or return of fluid to the chest (pleurodesis)
- Chlorothiazide (Diuril, Diurigen)
- Infection (a slight risk any time the skin is broken)
- Cancer
- Confusion or change in ability to think clearly
- Histamine H2 receptor blockers
Discount tadora 20mg on line
The prevalence of sinus node dysfunction may be as high as 1 in 600 patients older than 65 years of age erectile dysfunction treatment yoga discount tadora online. Many patients with sick sinus syndrome are asymptomatic; others experience syncope or palpitations. In patients with ischemic heart disease, periods of bradycardia may contribute to the development of congestive heart failure, whereas periods of tachycardia can contribute to the development of hypertension and angina pectoris. There is normally a pause in electrical activity before a secondary slower pacemaker begins to fire. However, these patients should be monitored for worsening bradycardia or hemodynamic deterioration. In mildly symptomatic patients, any potential contributing factors such as excess vagal tone or drugs should be eliminated. In severely symptomatic patients-that is, those with chest pain or syncope-immediate transcutaneous or transvenous pacing is indicated. In the event that cardiac pacing is delayed or pacing capabilities are limited, an epinephrine or dopamine infusion may be titrated to response while cardiac pacing is awaited. If atropine is ineffective, glucagon may be useful if the bradycardia is due to -blocker or calcium channel blocker overdose. Suggested dosing of glucagon is 50 to 70 mcg/kg (3 to 5 mg in a 70-kg patient) every 3 to 5 minutes until clinical response is achieved or a total dose of 10 mg is reached. To maintain clinical effect, this should be followed with a continuous infusion at 2 to 10 mg/hr. Bradycardia or asystole may develop suddenly (within seconds or minutes) in a patient with a previously normal or even increased heart rate, or the heart rate slowing may be progressive. Bradycardia can occur at any time during neuraxial blockade but most often occurs approximately an hour after anesthetic administration. The risk of bradycardia and asystole may persist into the postoperative period even after the sensory and motor blockade has diminished. Approximately half of patients who experience arrest during neuraxial anesthesia complain of shortness of breath, nausea, restlessness, light-headedness, or tingling of the fingers and manifest deterioration in mental status before arrest. The exact mechanism responsible for bradycardia and asystole during spinal and epidural anesthesia is not known. This is a paradoxical reflex-induced bradycardia resulting from decreased venous return and activation of vagal reflex arcs mediated by baroreceptors and stretch receptors. Another possible mechanism is the unopposed parasympathetic nervous system activity that results from the anesthetic-induced sympathectomy. Bradydysrhythmias associated with spinal or epidural anesthesia should be treated aggressively. Bradycardia can occur despite prophylactic therapy with atropine and/ or intravenous fluids. Secondary factors such as hypovolemia, opioid administration, sedation, hypercarbia, concurrent medical illnesses, and long-term use of medications that slow the heart rate can contribute to the development of bradycardia. Junctional pacemakers usually have an intrinsic rate of 40 to 60 beats per minute. The impulse initiated by a junctional pacemaker travels to the ventricles along the normal conduction pathway but can also be conducted retrograde into the atria. Junctional rhythm can be suspected if on physical examination the jugular venous pulsation shows cannon a waves. Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Junctional tachycardia is a narrow-complex tachycardia at a rate usually lower than 120 beats per minute. This can result in symptoms such as fatigue, generalized weakness, angina pectoris, impaired cardiac output, congestive heart failure, pulmonary edema, and hypotension. Junctional tachycardia can result from increased automaticity of junctional tissues in the setting of digitalis toxicity or cardiac ischemia. Junctional rhythm that occurs in association with myocarditis, myocardial ischemia, or digitalis toxicity should be managed by treating the underlying disorder. Junctional rhythms are not uncommon during general anesthesia using halogenated anesthetic vapors and, in this setting, require no treatment. Even in the setting of acute myocardial infarction, junctional rhythms are usually considered benign and require no treatment. The Framingham Heart Study followed long-term outcomes of individuals with first-degree heart block, and the results suggested an increased risk of atrial fibrillation in this population. However, in patients with significant heart disease, the increase in heart rate produced by atropine may contribute to myocardial ischemia. In patients with risk factors such as coronary ischemia and systemic infection, these clinical conditions should be treated and medically optimized before surgery. Digoxin levels should be checked before surgery, and serum potassium should be maintained at normal levels in patients receiving digoxin. An intact cardiac conduction system normally ensures conduction of each sinus impulse from the atria to the ventricles. Abnormalities of the conduction system can disrupt this process and lead to heart block. Assessing the site of the conduction abnormality and the risk of progression to complete heart block are core issues in treating a patient with heart block. These include acute myocardial infarction (especially in the distribution of the right coronary artery), digitalis toxicity, excessive -blockade or calcium channel blockade, myocarditis, rheumatic fever, mononucleosis, Lyme disease, and infiltrative diseases such as sarcoidosis and amyloidosis. Mobitz type I block does not require treatment unless the decreased ventricular rate results in signs of hypoperfusion. It can also be associated with the use of certain drugs such as calcium channel blockers, -blockers, digoxin, and sympatholytic drugs. This is because anatomically the posterior fascicle usually has a dual blood supply, whereas the anterior fascicle does not. Pacing capability should be available in the event of progression to complete heart block. A theoretical concern in patients with bifascicular heart block is that perioperative events (changes in blood pressure, arterial oxygenation, serum electrolyte concentrations) might compromise impulse conduction in the remaining fascicle and lead to third-degree heart block. There is no evidence, however, that surgery performed with general or regional anesthesia predisposes patients with preexisting bifascicular heart block to the development of third-degree heart block. The heart rate in Mobitz type I block is usually good and rarely does it progress to third-degree heart block. In the presence of an acceptable ventricular rate and an adequate cardiac output, no treatment is needed. Bundle Branch Blocks Conduction disturbances at various levels of the His-Purkinje system are called bundle branch blocks or intraventricular conduction defects. Intraventricular conduction disturbances are usually associated with significant structural heart disease, especially dilated cardiomyopathies. They are a marker of poor prognosis, both in terms of heart failure and increased mortality. It does not always imply cardiac disease and is often of no clinical significance. Preoperative placement of a transvenous pacemaker or the availability of transcutaneous cardiac pacing is necessary before an anesthetic is administered for insertion of a permanent cardiac pacemaker. Isoproterenol may be needed to maintain an acceptable heart rate and act as a "chemical pacemaker" until a permanent pacemaker is implanted and functional. Continued activity of the ventricles is due to impulses from an ectopic pacemaker distal to the site of the conduction block. Approximately 8% of patients with acute inferior wall myocardial infarction develop complete heart block. A syncopal episode caused by third-degree heart block is called a Stokes-Adams attack. These drugs act by altering various electrophysiologic characteristics of myocardial cells. The majority of antidysrhythmia drugs work by one of three mechanisms: (1) suppressing automaticity in pacemaker cells by decreasing the slope of phase 4 depolarization, (2) prolonging the effective refractory period to eliminate reentry circuits, or (3) facilitating impulse conduction along normal conduction pathways to prevent conduction over a reentrant pathway. Abnormal physiologic parameters should be corrected before initiating antidysrhythmic drug therapy or inserting a cardiac pacemaker. Establishment of physiologic acid-base values, normalization of serum electrolyte concentrations, and stabilization of autonomic nervous system activity are important and maximize the possibility of reestablishing normal sinus rhythm. Sixty percent of patients respond at a dose of 6 mg, and an additional 32% of patients respond at a dose of 12 mg.
Cheap tadora uk
This list reflects the importance of multidisciplinary input for optimal management of patients with congenital malformations erectile dysfunction homeopathic drugs discount tadora 20 mg without a prescription. Patients typically are best delivered in a setting where experienced delivery room attendants are available. If needed consultative services or equipment is not readily available, arrangement should be made for prompt transfer to a tertiary care center. For example, prompt notification of the delivery of an infant with gastroschisis ensures that the delivering hospital can provide adequate intravenous hydration and protection of exposed viscera, and it alerts the referral center to prepare for immediate pediatric surgery intervention on arrival. In settings of premature, preterm, or prolonged rupture of the membranes and premature labor, mothers are frequently treated with antibiotics and tocolytic agents. Maternal medications administered during pregnancy for non-obstetric diseases can have a significant impact on the neonate. A common challenge in many centers evolved from the treatment of opiateaddicted mothers with methadone or buprenorphine. Many infants appear neurologically normal at delivery, only to exhibit symptoms on the first, second, or even third day of postnatal life. Infants with neonatal abstinence syndrome typically demonstrate irritability, poor feeding, loose and frequent stools, and in severe cases, seizures. Treatment options for neonatal abstinence syndrome include nonpharmacologic interventions. These infants often require hospitalization for many days or weeks until their irritability is under sufficient control to allow care in a home setting. There is clinical evidence that neonates may exhibit similar symptoms after withdrawal from antenatal nicotine exposure. Maternal cocaine abuse has been associated with obstetric complications such as placental abruption. Vascular compromise may predispose neonates to cerebral infarcts and bowel injury. Developmental delay and behavioral problems are observed, and associated factors such as poverty, lack of prenatal care, and low socioeconomic status also contribute. Rh hemolytic disease has become uncommon, but it still must be considered as a cause of unexplained hydrops, anemia, or heart failure in infants born to Rh-negative mothers, especially if there is a possibility of maternal sensitization. The responsible isohemagglutinins have a weak affinity for blood group antigens, and the degree of hemolysis and subsequent jaundice varies from patient to patient. Indirect immunoglobulin (Coombs) testing has limited value in predicting clinically significant jaundice. The neonatal morbidity is typically restricted to hyperbilirubinemia requiring treatment with phototherapy. Complications of Prematurity the mean duration of a spontaneous singleton pregnancy is 282 days or 40 menstrual weeks (38 postconceptional weeks). Beyond the increased mortality risk, prematurity is associated with increased risk of morbidity in almost every major organ system. Between 1983 and 2004, the rate of preterm birth increased in the United States by 30%, from 9. Three major causes have been identified to explain the rise (see Chapter 40): improved gestational dating associated with increased use of early ultrasound,21 a substantial rise in multifetal gestations associated with assisted reproductive technology, and an increase in indicated preterm births. The risk of death before hospital discharge doubles when the gestational age decreases from 27. Delaying delivery for even a few days may substantially improve outcome, especially before 32 weeks, assuming that the intrauterine environment is safe to support the fetus. However, in some clinical situations with a high potential for preterm delivery, it is difficult to assess the quality of the intrauterine environment. In each case, prolonging gestation to allow continued fetal growth and maturation in utero is accompanied by an uncertain risk of rapid change in maternal status with a corresponding increased risk of fetal compromise. Tests of fetal well-being are discussed in Chapter 32, and clinical decision making in obstetrics is addressed in Chapters 34, 38, 40, 42, 46, 47, and 48. Obstetric decisions about the timing of delivery in the setting of uncertain in utero risk significantly contribute to the increase in late preterm births occurring after 32 to 34 weeks. Although perinatal mortality continues to decrease, in part due to a decline in stillbirths (see Chapter 45),22 interest in understanding the extent of morbidity associated with late preterm deliveries has intensified because of the large number of these late preterm infants and the potential for avoiding morbidities such as temperature instability, feeding problems, hyperbilirubinemia requiring treatment, suspected sepsis, and respiratory distress. For example, brain growth and development proceeds rapidly during the third trimester and continues for the first several years of life. Studies demonstrate an association between late preterm delivery and long-term neurodevelopmental problems, including learning disabilities and attention deficit disorders. Late preterm infants experience excess infant mortality (death before 12 months) compared with their full-term counterparts. Table 72-3 compares estimates of complication rates between preterm and late preterm infants. Even uncommon complications in the later preterm population may represent a significant health care burden. The duration of gestation decreased by 1 week during that decade, from 40 weeks to 39 weeks. B, the risk of intrauterine fetal demise increases with increasing gestational age, especially beyond 40 weeks. At 22 weeks (22 0/7 days to 22 6/7 days), survival is rare and typically is not included in studies of survival or long-term outcome. Seventeen percent survived to hospital discharge40 Whereas mortality rates fall for each 1-week increase in gestational age at delivery, long-term neurodevelopmental outcomes do not improve proportionately. Higher weights within gestational age categories and female sex consistently show a survival advantage and better neurodevelopmental outcomes. Maternal transfer to a tertiary center and administration of corticosteroids (see Chapter 34) are the only antenatal interventions that have been significantly and consistently related to improved neonatal neurodevelopmental outcomes. Planning for Delivery at the Limits of Viability Ideally, discussion between physicians and parents should begin before the birth in a non-emergent situation and should include obstetric and neonatal care providers. Even during active labor, communication with the family should be initiated as a foundation for postnatal discussions. The family should understand that plans made before delivery are influenced by maternal and fetal considerations and based are on limited information. The neonatologist can assist families in making decisions regarding a birth plan for their infant by providing general information about the prognosis, the hospital course, potential complications, survival, and general health and well-being of infants delivered at a similar gestational age. When time does not permit such discussions, careful evaluation of gestational age and response to resuscitation are instrumental in assisting families in making decisions regarding viability or nonviability of an extremely premature infant. The presence of an experienced pediatrician at delivery is recommended to assess weight, gestational age, and fetal status and to provide medical leadership in decisions to be made jointly with families. Health care providers tend to be more pessimistic when considering outcomes based solely on experience and subjective reasoning. Decisions concerning resuscitation should be individualized to the case and the family but should begin with parameters for care that are based on global reviews of the medical and ethical literature and expertise. If the prognosis is more uncertain and survival is borderline with a high rate of morbidity. Decisions regarding the care of extremely preterm infants are always difficult for everyone involved. Parental involvement, active listening, and accurate information are critical to an optimal outcome for infants and their families. Although parents are considered the best surrogate for their infant, health care professionals have a legal and ethical obligation to provide appropriate care for the infant based on medical information. If agreement with the family cannot be reached, it may be appropriate to consult the hospital ethics committee or legal counsel. In a normal term infant, the lungs expand with air, pulmonary vascular resistance rapidly decreases, and vigorous, consistent respiratory effort ensues within a minute of separation from the placenta. The process depends on crucial physiologic mechanisms, including production of functional surfactant, dilatation of high-resistance pulmonary arterioles, bulk transfer of fluid from airspaces, and physiologic closure of the ductus arteriosus and foramen ovale. Complications such as prematurity, infection, neuromuscular disorders, developmental defects, and complications of labor may interfere with neonatal respiratory function. This is the most common respiratory cause of admission to the special care nursery. During the last trimester, a series of physiologic events leads to changes in the hormonal milieu of the fetus and the mother to facilitate neonatal transition. The bulk of this fluid clearance is mediated by transepithelial sodium reabsorption through amiloride-sensitive sodium channels in the respiratory epithelial cells. Traditional explanations based on Starling forces and vaginal squeeze for fluid clearance account for only a fraction of the fluid absorbed.
Order tadora with visa
Dialysis Patients and Pregnancy End-stage renal disease in women of childbearing age is often accompanied by menstrual disturbances impotence causes buy 20 mg tadora free shipping, anovulation, sexual dysfunction, and infertility. However, despite these many disturbances, 57 Renal Disorders 959 successful conception and delivery have been described in patients on chronic hemodialysis or on peritoneal dialysis. The frequency of pregnancies in women of childbearing age who are on dialysis is reportedly on the rise, increasing from a historic low of less than 1%, to 7% or even greater in recent reports from across the globe. For individuals on dialysis who desire and are considering pregnancy, the risks of such a decision should be explained. The conversation with the patient should include discussion about the increased risk for polyhydramnios, intrauterine growth restriction, preterm labor, and preeclampsia (Table 57-3). In the absence of a potential donor, however, many women do not have the option of a transplantion during their fertile years, and the management of pregnancy in the dialysis patient continues to remain relevant. Surprisingly, some investigators have reported that fetal outcomes were better in the presence of polyhydramnios, possibly because this condition is evidence of adequate placental function. Successful outcomes demand meticulous attention to ensure dialysis adequacy, fluid balance, blood pressure control, and optimal nutrition. This is best achieved using a multidisciplinary approach involving an experienced nephrologist, an obstetrician familiar with high-risk patients, a dialysis nurse, and a nutritionist (Table 57-4). For example, one group used nocturnal home hemodialysis to provide intensified clearance after conception. Six live births after seven pregnancies (one pregnancy was electively terminated) were documented, with a mean gestational age of 36. Nevertheless, vigilant efforts to avoid both hypovolemia and hypotension are warranted, as both can be damaging to the fetus. Because the pregnant dialysis patient will undergo frequent dialysis, the clinician should perform frequent physical examinations to evaluate for the presence of excess fluid unrelated to the pregnancy. Thus, erythropoietin dosages should be adjusted to maintain the physiologic anemia of pregnancy (10 to 11 g/L). Careful follow-up of complete blood count and iron stores can guide both intravenous erythropoietin and iron supplementation. Exacerbation of hypertension is common, although the incidence of preeclampsia in dialysis patients is difficult to ascertain because of the inability to apply standard diagnostic criteria. In the absence of urine output revealing proteinuria, the diagnosis of preeclampsia relies on the assessment of worsening blood pressure. For example, because amino acids are lost during dialysis, protein intake recommendations can increase to 1 to 1. Because several water-soluble vitamins are also lost during dialysis and dialysis regimens are intensified overall during pregnancy, some suggest standard vitamin and supplement dosages should increase: for example, 1 to 5 mg folate per day and double the prescribed dosage of daily multivitamin. Preterm delivery, premature rupture of membranes, and stillbirths have also been documented to occur secondary to acute peritonitis in women who are undergoing peritoneal dialysis. Renal Transplant and Pregnancy End-stage renal disease causes hypothalamic-gonadal dysfunction that leaves most affected women of childbearing age infertile. This section reviews the issues related to kidney donors, renal transplantation, and pregnancy, including the associated risks to the mother and fetus, strategies to increase the likelihood of a successful pregnancy while minimizing risk to the mother and renal allograft, management of the common immunosuppressant medications during and after pregnancy, management of acute allograft rejection, and issues related to labor and the subsequent neonatal period. Similarly, pregnancy after kidney donation was associated with higher risk for gestational diabetes, gestational hypertension, proteinuria, and preeclampsia. For example, a retrospective cohort study from the European Dialysis and Transplant Association compared 53 women (the cases) who had successful pregnancies, with a cohort of persons who had not been pregnant matched with regard to date of transplant and renal disease leading to transplant (the controls). Over 24 to 36 months of follow-up, the study found renal function unchanged in 67% of case-control pairs, and worse in both groups in 9% of pairs. This group therefore concluded that pregnancy had no adverse effect on graft function. Another matched cohort series published in 2006 matched each of 39 women who had had one or more pregnancies with functioning renal allografts (total number of live births = 55) with three controls who had not been pregnant but matched with regard to 12 factors known to affect graft survival. These authors concluded that pregnancy did not adversely affect long-term graft or patient survival. Only one retrospective cohort series has suggested that pregnancy adversely affects allograft function. After 10 years of follow-up, graft survival was 100% in the control group and 69% in the group with pregnancies (P <. The difficulty of generalizing from this single study lies in the rarity of centers with a 10-year graft survival of 100%, as was observed in the control group. Thus, the preponderance of the evidence indicates that the risk for irreversible loss of renal allograft function is minimal when the creatinine level is less than 1. National Transplantation Pregnancy Registry, the European Dialysis and Transplant Association Registry, and the U. Transplant Pregnancy Registry have collected data on pregnancy outcomes for more than 2000 pregnancies in women with solid-organ transplants. Approximately 22% of pregnancies among renal transplant recipients end in the first trimester, 13% resulting from miscarriage and the remaining from elective termination. For pregnancies that continue beyond the first trimester, more than 90% result in a successful maternal and fetal outcome. However, there is a substantial risk for low birth weight (25% to 50%) or preterm delivery (30% to 50%). Vaginal delivery is safe in this population and should be the default method of delivery, with cesarean section performed only for routine obstetric indications. Pregnancy within the first 6 to 12 months after transplantation is not recommended for the following important reasons: the risk for acute allograft rejection is relatively high, immunosuppressant medications are administered at higher dosages, and the risk for infection is greatest. The American Society of Transplantation currently recommends that conception could be safely considered as early as 1 year after transplant if (1) graft function is adequate and stable. Allograft function should be serially assessed and biopsy performed if there is a concern for acute rejection. The most common complication of pregnancy in transplant recipients is hypertension, which affects 30% to 75% of patients. The American Society of Transplantation recommends that hypertension in pregnant renal transplant recipients should be managed aggressively, with target blood pressure close to normal-a goal that differs from somewhat higher blood pressure goals in women with hypertension in pregnancy in the absence of a transplant. Cesarean delivery can therefore reduce the risk for neonatal transmission in women with active lesions. Nevertheless, a significant amount of published data can inform decisions about the use of some of these agents safely in pregnancy (see Table 57-6). Cyclosporine (or tacrolimus, although data for it are more limited) and steroids, with or without azathioprine, form the basis of immunosuppression during pregnancy. Given the chronic adrenal suppression associated with long-term steroid use, stress-dosage steroids are needed at the time of delivery and for 24 to 48 postpartum hours. For azathioprine to become active, it must be converted to 6-mercaptopurine by the enzyme inosinate pyrophosphorylase, which the immature fetal liver lacks. Hence, close monitoring of serum levels with dosage adjustment is required to maintain optimal levels. It should be discontinued 57 Renal Disorders 963 preemptively in women of childbearing age who are not using contraception. The diagnosis of acute rejection can be difficult, but it should be considered if fever, oliguria, graft tenderness, or deterioration in renal function is observed. Allograft biopsy is necessary for confirmation of the diagnosis before the initiation of therapy. High-dosage steroids have been the mainstay of treatment for acute allograft rejection during pregnancy. Yes, with increased risk for preterm premature rupture of membranes at higher dosages Safe in Breastfeeding Yes, but breastfeeding is not encouraged if receiving >60 mg prednisolone daily Yes Azathioprine Mycophenolate mofetil Yes Tacrolimus Yes Slightly increased risk for congenital malformations, specifically ventricular and atrial septal defects208 Hypoplastic nails, shortened fifth fingers, diaphragmatic hernia, microtia (ear deformity), micrognathia, cleft lip and palate, and congenital heart defects214 No Fetal growth restriction, and dosage-related myelosuppression in the neonate208 Yes Yes No. Exceptional circumstance: with no other effective agent, continue treatment but counsel about teratogenicity. No Hyperkalemia and renal impairment Cyclophosphamide Cyclosporine Yes (animal data) Yes Yes No Chromosomal abnormalities and cytopenia Transient immune alterations Sirolimus Not known Not reported None reported Intravenous immunoglobulin Rituximab Yes Yes (from 16 weeks of gestation) No Not reported None reported Yes. May need up to 40% increase in pre-pregnancy dosage because of increased clearance. Stop 12 weeks before conception214 and switch to a safer agent (until more data regarding safety in pregnancy available). With regard to contraception, intrauterine devices are more likely to fail in women on immunosuppressive drugs because their efficacy depends on intact immunologic function. In this population, the risk of developing an adverse fetal outcome (preterm delivery, neonatal or fetal death, low birth weight) has been shown to be at least two times higher than in normal healthy pregnant women.
Buy 20 mg tadora visa
The site of delivery should be chosen based on optimizing the availability of appropriate expertise erectile dysfunction doctors in navi mumbai purchase generic tadora canada. The neonatologist can facilitate appropriate delivery coverage and ensure availability of appropriate equipment, medications, and personnel. Management considerations include availability of expertise and equipment needed for optimal management. This condition is classically seen in infants delivered near term, especially after cesarean birth before the onset of spontaneous labor. The chest radiograph usually shows prominent perihilar streakings that represent engorged pulmonary lymphatics and blood vessels. Other rare diagnoses are pulmonary hypertension, meconium aspiration, and polycythemia. Chest radiographs typically demonstrate mild pulmonary congestion with hazy lung fields. Small accumulations of extrapleural fluid, especially in the minor fissure on the right side, may be seen. Supplemental oxygen is provided to keep the oxygen saturation level greater than 90%. Infants are usually given intravenous fluids and not fed orally until their tachypnea resolves. Pulmonary Hypoplasia Lung development begins during the first trimester when the ventral foregut endoderm projects into adjacent splanchnic mesoderm (see Chapter 15). Branching morphogenesis, epithelial differentiation, and acquisition of a functional interface for gas exchange ensue through the remainder of gestation and are not completed until the second or third year of postnatal life. Clinical conditions associated with pulmonary hypoplasia and approaches to prevention and treatment are discussed in this section. Perturbation of lung development at any time during gestation may lead to clinically significant pulmonary hypoplasia. Two general pathophysiologic mechanisms contribute to pulmonary hypoplasia: extrinsic compression and neuromuscular dysfunction. Oligohydramnios, whether caused by premature rupture of membranes or diminished fetal urine production, can lead to pulmonary hypoplasia. The reduction in branching morphogenesis and surface area for gas exchange may be lethal or clinically imperceptible. Clinical studies link the degree of pulmonary hypoplasia to the duration and severity of the oligohydramnios. Similarly, pulmonary hypoplasia is a hallmark of congenital diaphragmatic hernia and is caused by extrinsic compression of the developing fetal lung by the herniated abdominal contents. The degree of pulmonary hypoplasia in congenital diaphragmatic hernia is directly related to the extent of herniation. Diffuse, ground-glass infiltrates along with air bronchograms make the cardiothymic silhouette indistinct. However, the remaining infants did well and were discharged with apparently normal pulmonary function. Prenatal diagnosis and treatment of pulmonary hypoplasia are discussed in Chapter 35. Some infants with profound hypoplasia have insufficient surface area for effective gas exchange. These patients typically display profound hypoxemia, respiratory acidosis, pneumothorax, and pulmonary interstitial emphysema. At the other end of the spectrum, some infants have no clinical evidence of pulmonary insufficiency at birth but have diminished reserves when stressed. In between is a cohort of patients with respiratory insufficiency that is responsive to mechanical ventilation and pharmacologic support. Typically, these patients have adequate oxygenation and ventilation, suggesting adequate gas exchange capacity. The pathophysiologic sequence begins with limited cross-sectional area of resistance arterioles, followed by smooth muscle hyperplasia in these same vessels. Early use of pulmonary vasodilators such as nitric oxide is the mainstay of management for increased pulmonary vasoreactivity. Optimizing pulmonary blood flow reduces the potential for hypoxemia that is thought to stimulate pathologic medial hyperplasia. In many cases, the process is lengthy, requiring mechanical ventilation and treatment with pulmonary vasodilators such as sildenafil, bosentan, or prostacyclin for weeks to months. Just as prenatal prognosis is difficult to assess, predicting outcome for patients with pulmonary hypoplasia managed in the neonatal intensive care unit is hampered by limited data. Factors that negatively affect surfactant synthesis include maternal diabetes, perinatal asphyxia, cesarean section without labor, and genetic factors. Prenatal assessment of fetal lung maturity and treatment to induce fetal lung maturity are discussed in detail in Chapter 34. Symptoms, which are typically evident in the delivery room or shortly thereafter, include tachypnea, nasal flaring, subcostal and intercostal retractions, cyanosis, and expiratory grunting. The characteristic expiratory grunt results from expiration through a partially closed glottis, providing continuous distending airway pressure to maintain functional residual capacity and thereby prevent alveolar collapse. Progressive worsening of symptoms in the first 2 to 3 days, followed by recovery, characterizes the typical clinical course. This timeline (curve) is modified by administration of exogenous surfactant with a more rapid recovery. Classic radiographic findings include low-volume lungs with a diffuse reticulogranular pattern and air bronchograms. The diagnosis can be established chemically by measuring surfactant activity in tracheal or gastric aspirates, but this is not routinely done. Infants are managed in an incubator or under a radiant warmer in a neutral thermal environment to minimize oxygen requirement and consumption. Arterial oxygen tension (Pao2) is maintained between 50 and 80 mm Hg, with saturations between 88% and 96%. Heart rate, blood pressure, respiratory rate, and peripheral perfusion are monitored closely. Because sepsis cannot be excluded, screening blood culture and complete blood counts with differential are performed, and infants are started on broad-spectrum antibiotics for 48 hours, until culture results are available. Surfactant replacement is one of the safest and most effective interventions in neonatology. The advantages of prophylactic administration include a better distribution of surfactant when instilled into a partially fluid-filled lung and the potential to decrease trauma related to resuscitation. Avoiding treatment of unaffected infants and related cost savings are the advantages of rescue therapy. Biologically active surfactant can be prepared from bovine, porcine, human, or synthetic sources. Rarely, the increased transthoracic pressure leads to progressive decrease in venous return and decreased cardiac output. The goal of mechanical ventilation is to limit volutrauma and barotrauma without causing progressive atelectasis while maintaining adequate oxygenation and gas exchange. Acute complications include pneumothorax, pneumomediastinum, pneumopericardium, and pulmonary interstitial emphysema. The incidence of these complications has decreased significantly with surfactant treatment. Incidence of these complications is inversely related to decreasing birth weight and gestation. These infants were larger, late preterm infants with lung changes attributed to mechanical ventilation and oxygen toxicity. These changes lead to ventilation-perfusion mismatching and increased work of breathing. Results of two large, randomized trials enrolling preterm infants have suggested that the use of supplemental oxygen to maintain higher saturations resulted in worsening pulmonary outcomes. Blended oxygen or, if not available, room air is recommended for initial resuscitation of preterm infants in the delivery room, along with continuous monitoring by pulse oximetry.