Cheap terazosin 2 mg line
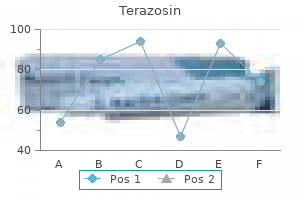
Thus blood pressure check discount terazosin 5 mg, orthopaedic surgeons need to understand the complex biology of fracture healing and the factors that can inhibit or promote this process. After trauma, bone heals by a direct intramembranous or an indirect fracture healing process, which consists of intramembranous and endochondral bone formation. The most common pathway is secondary healing, which occurs if instability and micromotion exist at the fracture site. The most important response occurs in the periosteum and neighboring soft tissues. Committed osteoprogenitor cells and undifferentiated mesenchymal cells derived from the periosteum contribute to the healing process through intramembranous bone formation that occurs on either side of the fracture. The endochondral response also depends on the periosteum, but the cells in the neighboring soft tissues primarily contribute to this process. Endochondral ossification is located adjacent to the fracture site and initially manifests as a cartilage anlage that develops from undifferentiated mesenchymal cells in the peripheral soft tissues. These cells are recruited, proliferate, and differentiate into cartilage-forming cells. The inflammatory phase of fracture healing initiates this process of neovascular invasion. Most fractures heal by a combination of intramembranous and endochondral ossification. These two processes demonstrate a series of distinct stages that comprise four temporally defined phases of repair: inflammatory, early callus, mature callus, and remodeling. Inflammatory Phase this phase begins irmnediately after fracture, with the formation of the hematoma. The formation of the hematoma is accompanied by the invasion of macrophages, polymorphonuclear leukocytes, and lymphocytic cells. These cytokines and signaling molecules are involved in the processes of chemotaxis and angiogenesis and regulate cell proliferation and the differentiation of the cells that have migrated to the site of the fracture. This leads to activation of the endochondral healing response and intramembranous ossification. The inflammatory phase is characterized by neovascularixation and the ingrowth of proliferative blood vessels. Fibronectin has been found in the fracture hematoma within the first 3 days following fracture. Its production by cells associated with the callus appears to be greatest in the earliest stages of fracture healing. U with rigid stability, which occurs only after open reduc- tion and internal fixation, substantially limiting the overall strain at the fracture site. When such conditions are achieved, however, the direct healing cascade allows the bone structure to immediately regenerate anatomic lamellar bone and the haversian systems without any intervening remodeling steps. Gap healing takes place within these interstices, initially by the ingrowth of blood vessels. Mesenchymal cells differentiate into osteoblasts, which begin to lay down osteoid on the exposed fracture gap surfaces. The edges of necrotic bone and preliminary callus within the gap undergo resorption. Primary cortical healing takes place to reestablish cortical continuity with the aid of the so-called "cutting cones. These remodeling osteoclasts resorb cortical bone, thereby permitting angiogenesis. The new blood vessels are accompanied by stem cell deposition at the fracture site. Progenitor cells differentiate into osteoblasts that secrete matrix and bridge the fracture gap, and the callous is replaced by new osteons. The process of frac- ture healing requires that areas of absolute contact and rigidity provide stabilization for gap healing to proceed. Unlike indirect fracture healing, this process enlists minimal participation from the peri- Direct bone healing requires an anatomic reduction by the T cells. Stress fracture healing is very similar to gap healing in that these fractures unite by intramembranous ossification. These actions may include additional cellar attachments, dictate cellular movement, cellular death, or differentiation. The actual attachment of the cells takes place through the formation of cell adhesion complexes, which consist of integrins and a number of cytoplasmic proteins, such as alpha-actinin. Arachidonic Acid Metabolism Arachidonic acid metabolism exerts complex control over many bodily systems, mainly those involved in inflammation and immunity. Two families of enzymes catalyze the fatty acid oxygenation of arachidonic acid and produce prostaglandin or leukotriene factors; the actions of both factors can affect the inflammatory phase of healing. These actions include a direct role in the stimulation of platelet aggregation and vasoconstriction; both are important for the activation and degranulation of platelets. They have a chemotactic effect on migrating neutrophils and other cellular constituents and, as such, help to bring the necessary cells to the tissue. Black arrows show numerous multinucleate giant cell osteoclasts resorbing dead hone spicules. When triggered, integrins activate chemical pathways to the interior of the cell in a process called signal transduction. In addition, signal transduction may upregulate the production of new receptors added to the cell membrane. Together with signals arising from the receptors for soluble growth factors such El 2. Section 1: Principles of flrthopaedics a powerful effect in increasing vascular permeability and stimulate proinflammatory activities such as endothelial cell adherence and chemokine production by mast cells. This effect on mast cells stimulates additional phagocytosis, edema production, and interstitial fluid accumulation. U the Wnt signaling pathway involves families of secreted growth factors that are involved in a wide range of cellular processes. These proteins bind to the cell membrane receptors and transdnce signals to the interior of the cell. These Wilt protein complexes help to regulate cell-to-cell interactions and tissue homeostasis. This bound receptor then passes the biologic signal to the protein "disheveled" inside the cell. Of the three identified Writ pathways, the one most pertinent to this phase of fracture healing is the canonical Writ pathway. This conversion takes place under the influence of inductive factors during the inflammatory phase of fracture healing. E Induction of the Wnt signaling pathway promotes bone formation, whereas inactivation of the pathway leads to osteope- nic states. Potential therapeutic approaches may help stimulate the Wnt signaling pathway by upregulation of intracellular mediators of the "Writ signaling cascade and inhibition of endogenous antagonists of the pathway. The residual necrotic bone is resorbed and replaced by fibrous tissue and new vessel ingrowth. White arrows depict fibrous tissue undergoing early remodeling to early callus by osteolysis and orderly osteoblastic lining of the early collagen. Black arrow shows osteoclast multinucleate giant cells in a receding osseous trabecula. A have demonstrated promising results in promoting bone formation and increased callus size. Improved fracture healing rates are equivocal, and more studies are needed in this regard. An antibody for sclerostin, antisclerostin antibody, is available and is in early clinical trials. The formation of a cartilage callus provides immediate mechanical stability and delivers a specific three-dimensional architecture, which is crucial to the establishment of sites of attachment for additional cells and the facilitating of new bone formation. At the periphery of the fracture, the cartilage cells have developed prominent nuclear and cytoplasmic vacuoles and appear as hypertrophic chondrocytes. The matrix between these swollen cells becomes calcified as the chondrocytes release calcium into the extracellular matrix. This process forms a zone of provisional preliminary calcification white arrows. Note the vascular channels black arrows] in this area of peripheral endochondral ossification. A critical mass of cartilage callus must develop before calcification; that goal is achieved by the presence of proteoglycans, which prevent mineralisation.
Cheap terazosin online american express
An electrocardiogram should also be performed in anyone complaining of palpitations arrhythmia update 2014 cheapest generic terazosin uk. This patient needs admission and immediate referral to the on-call psychiatrist for stabilisation with psychotropic medications or in some cases even sedation. She will also need an urgent referral to the Mother and Baby Psychiatric Unit for further specialist assessment and management. Accurate and timely diagnosis and management are essential to avoid harm to both the mother and the baby. For those with thoughts of harm to self or others who do not consent to treatment, involuntary admission and treatment under the Mental Health Act or Mental Capacity Act may be required. Urgent transfer to a Mother and Baby Unit will help provide the supervision and support that is required in such cases. He told the triage nurse that it came on suddenly last night, and this was the first time it has happened. The triage nurse has performed some vital signs, prescribed simple analgesia and prioritised him for a chest radiograph. Examination Vital signs are as follows: respiratory rate of 22/min, blood pressure of 125/65, O2 saturation of 96% on air, temperature of 36. There are reduced breath sounds on the left side of the chest with hyper-resonance on percussion. You assess him with your Registrar who has asked you to consent him for needle thoracentesis and to get the necessary kit ready. The General Medical Council has formal guidance on obtaining informed consent and outlines the responsibilities of the treating doctor. The guidance states that you should clearly explain the diagnosis and the options available for treatment to the patient. You should have a good working knowledge of the treatment options with the ability to explain potential risks, complications and the failure to achieve the desired end-point. Ideally, you should be able to perform the procedure or treatment option being offered to the patient. The patient should be of sound mind, be able to retain this information long enough to arrive at a balanced decision and be able to communicate this. When explaining risks, complications and outcomes, language should be in terms that the patient may understand. An independent native language interpreter should be used if necessary, and if the patient has any questions, these should be answered in full prior to the procedure. Risks of a thoracentesis include the following: unable to locate space, discomfort, infection, bleeding, neurovascular injury, lung injury and the failure to reach the desired end-point (persistent pneumothorax, recurrence). You should also inform the patient that you may need to proceed to an intercostal drain and discuss this separately. Consent may be implied (such as rolling up a sleeve for blood pressure measurement), verbal or written. This should be witnessed and documented in the patient record along with any discussions regarding risks and complications. Although it is infrequently done, best practice would be to obtain written consent for an elective needle thoracocentesis/proceed to intercostal drain. Some specialties and trusts have generated standardised patient consent forms for common procedures, and these should be used if available. The legal process of capacity and consent to treatment in adolescents and children is different. In general, one needs to have the permission of their parent or those with parental responsibility for anyone under 18 years. The law assumes that the mother has parental responsibility, but this must be checked. For example, 16- and 17-year-olds are presumed by law to be able to consent to medical treatment. Refusal of treatment, however, may be overturned by the parent or court of law in certain circumstances. This refers to case law whereby a child demonstrated capacity to consent for oral contraceptive pill treatment against the wishes of her parents. There is no lower limit to Gillick competence, although in children of 13 years and under, parental consent is usually sought for all treatment. In terms of best practice, consent in all patients under 18 years should be taken jointly with the parents and the young person and in line with the principles outlined for adults. Any additional discussions and decisions should be documented in the patient record. Most hospitals do have a 24-hour legal team that may be able to help with complex queries, and this should be escalated via senior medical staff as soon as possible. In life-threatening emergencies, medical professionals are able to carry out interventions in the best interests of the patient. He was brought to the Emergency Department by his mother, and a radiograph of the wrist was performed. They were told that the wrist was sprained and was discharged home with the advice to come back if the pain did not settle. Examination There is isolated pain over the distal radius with some associated soft tissue swelling. There is full range of motion of the wrist and the hand, but flexion and extension are painful. Once identified, you should check the radiograph carefully to see if the injury extends to the growth plate and for any other associated injuries. Your first steps should be to explain your findings to the patient and his mother. Most parents are relieved when a diagnosis is reached and they have clear guidance on treatment and prognosis. In this case, the injury is managed non-operatively in either a splint, or more commonly in a plaster of Paris backslab with follow-up in fracture clinic. The next question for most parents is why was the fracture missed and what can be done to prevent it from happening again The Consultant will also take on the responsibility for investigating the incident. Once completed, the form generates a report and is assigned to the most appropriate person for investigation, risk classification and review. Once the form is assigned to an investigator, steps can be taken to unravel why this incident happened and steps put in place to stop it from happening again. Was it a case of simple error or does the attending doctor require additional training This serves as an additional reminder to the attending practitioner that there is an abnormality present. However, it should not be relied on as a sole indicator and queries escalated to senior medical staff in real time. With electronic systems, reporting radiologists and radiographers can check that appropriate follow-up or actions have been taken. They form an important bridge for the patient, parent and the staff involved, and their ability to listen and understand the patient or parent concerns helps to focus the investigative process and provide an outcome for all involved within formally agreed timelines. Her carers have brought in her medication in a dosset box that includes metformin, gliclazide, bumetanide, aspirin and simvastatin. As the department is busy, the nurse asks the doctor to co-sign the infusion and starts the pump. The assessing doctor correctly recognised that this patient was hyperkalaemic from an acute kidney injury and prescribed an insulin/dextrose infusion.
Best purchase terazosin
Extrapolating the data to all hospital admissions in the United States prehypertension stress purchase terazosin 5 mg on line, the authors estimated that preventable deaths occur at a yearly rate of between 210,000 and 400,000. American Academy of Urthopacdic Surgeons Chapter 3: Patient Safety and Core Competencies obesity (body mass index:40, and rheumatoid arthritis conferred an increased infection risk. Proper skin preparation, laminar flow rooms, limited operating room traffic, and various skin closure techniques lower the risk of infection. Most importantly, proper preoperative antibiotic administration is key to minimizing infection. This article is a consensus paper on optimal perioperative skin preparation and perioperative hand washing from experts in the field. American Academy of Urthopaedic Surgeons: Preventing Venous Thromboetnftoiic Disease in Pntients Undergoing Elective Hip and Knee Arthroplasty. In addition, age older than 30 years, a history of cardiac disease, and hypertension requiring medications were found to be risk factors for a cardiac complication. Knowing the precise time that an event is likely to occur can increase the suspicion for that event to be diagnosed after spinal surgery. American Academy of Urthopaedic Surgeons Urthopaedic Knowledge Update 12 sjgpaedoqug u! Devin C], Lee D5, Armaghani 5], et al: Approach to pain management in chronic opioid users undergoing orthopaedic surgery. African-American, Native American, and Alaskan American race was associ- 1: Principles in Grthopaedics 3. Widowed marital status or Medicaid insurance coverage also increased the risk of readmission. These risk factors should be managed to avoid potential preventable complications. An increased likelihood of readmission was found in patients with coronary artery disease, diabetes, a long length of hospital stay, underweight status, obesity, and Medicare coverage, as well as in those older than 30 years or younger than 50 years. The authors of this study found no statistically significant difference among subspecialties. Although readmission rates have declined over the past 10 years, the authors found a higher rate among Medicare patients, patients who are obese, those with hospital stays of a long length, older patients, and those with increased American Society of Anesthesiologists scores. Desmeules F, Hall J, Woodhouse L]: Prehabilitation improves physical function of individuals with severe disability from hip or knee osteoarthritis. In addition, self-paced walking scores and stair performance improved before surgery. A culture of safety is necessary to improve quality and patient outcomes while avoiding mistakes. Mattson M, Hellgren], Coransson 5: Leader communication approaches and patient safety: An integrated model. American Academy of Urthopaedic Surgeons Chapter 3: Patient Safety and Core Competencies this study asserts that communication by the leader of a medical team is critical in increasing organizational and patient safety and that various communication approaches positively affect different employee safety behaviors. Implementation was associated with reductions in medical errors and improved communication without a decrease in workflow. It showed that a high percentage of orthopaedic surgeons possess attitudes and behaviors indicative of mistake or collision tie, medical error]. Foundation for Health Care Quality: Surgicai Ciinicai Outcomes and Assessment Program. Potential pitfalls in administer- ing medications such as confusing and similar labels are highlighted. Advice is offered that can help anesthesiologists avoid mistakes while caring for surgical patients. Jamsen E, Nevalainen P, Eskelinen A, Huotari K, Kalliovalkama J, Moilanen T: Dbesity, diabetes, and preoperative hyperglycemia as predictors of periprosthetic joint infection. American Academy of Orthopaedic Surgeons: Consistency for Safety in Orthopaedic Surgery. American Academy of Drthopaedic Surgeons: Information Statement: Surgeon and Surgicai Team Concentration. Three themes were established that represent a culture of safety and teamwork: building shared under- srandings through open communication, managing contextual stressors in a hierarchical environment, and limiting high turnover in the team, which can influence team performance. The device application and approval processes depend on the class of the device and whether a predicate device exists. Surgeons also must understand that, although reporting of adverse events is optional. The medical device approval process in the United States has been evolving over the past four decades. This law includes regulations and requires site visits to ensure that the manufacturer is in compliance with the current good manufacturing practices specified States, although it will be subjected to the general controls Act. An approved premarket in the requirements for devices in part 820 of the Quality Systems Regulation 21 Code of Federal Regulations. Braun, Medtronic, and Panoramic; has received research or institutional support from AesculapiB. Goodman or an immediate family member serves as a paid consultant to lntegra Life Sciences; serves as an unpaid consultant to Acceiaiox and Biomimedica; has stoclc or stock options held in Acceiaiox, Bioimimedica, and StemCor Systems; has received research or institutional support from Baxter and Di Grthopedlcs; and serves as a board member, owner; officer; or committee member of the American Academy of Orthopaedic Surgeons, and the Society for Bioma teriais. Sale nor any immediate family member has received anything of value from or has stocir or stock options held in a commercial company or institution related directly or indirectly to the subject of this chapter: Drthopaedie Knowledge Update 12. American Academy of Drthopaedic Surgeons Chapter 4: Regulation of Drthopaedic Products commercially on or after May 23, 1976. Custom Devices Often, a customised device or implant is needed to attain of the Federal Food, Drug, and Cosmetic Act. Posta- 2012 Food and Drug Administration Safety and Innovation Act, and the manufacturer must determine whether the requirements are satisfied before proceeding with the request for exemption. Although not well known, a compassionate-use request can be helpful in many circumstances that do not meet all the criteria for a custom device exemption. Follow-up information about the use of the compassionate-use device should be submitted in a report after patients have been treated. A preamendment device is one that was in commercial distribution before May 23, 19%, the date of enactment of the Medical Device Regulation Act or the Medical Device Amendments of 1976. Custom Device Use Changes to the custom device provision set the number of devices for which a manufacturer could use the custom device pathway at five per year. Thus, if a patient requires bilateral custom implants, the manufacturer can count this request as one rather than two requests. The physician must find a manufacturer willing to supply the custom device and start the application process using that manufacturer. Such a supplement should include the protocol to be followed or identify deviations from the approved clinical protocol. The patients should be monitored to detect any possible problems arising from the use of the device. This exemption can be applied to devices used to treat conditions affecting 4,000 or fewer patients in the United States annually. Depending on institutional review board procedures, approval may be needed for each patient or may be granted for all patients of that physician or for all uses of the device. In many cases, institutional review board applications for a humanitarian device exemption can be expedited. A separate consent procedure that ensures the patient understands the humanitarian-use status of the device is required. All orthopaedic surgeons need to be aware of the pathways available to obtain the devices needed for patients in unusual circumstances. For example, the study of a total hip arthroplasty device labeled for use in adults older than 55 years with a body mass index Drthopaedic Knowledge Update 12. Inclusion of groups in the study population that are not part of the labeled population would increase the duration and cost of the study without adding value for the sponsor. Testing standards are defined to permit the performance comparison of similar products. The American Society for Testing and Materials International and the International Organization for Standardisation create most of the standards applicable to orthopaedic surgery. For example, testing is done under idealized conditions before implantation of the device and before important changes may have occurred. In addition, in vivo processes may not be understood completely, and, therefore, existing tests may not be designed adequately to anticipate critical factors such as alternative modes of wear. Patient characteristics also may influence device behavior following initial implantation.
Purchase generic terazosin canada
However blood pressure meaning terazosin 5mg for sale, this issue is confounded by multiple factors such as the increased rate of infertility among women undergoing bariatricsurgery, which has been found to be as high as 41. It is clear that more extensive prospective studies must be performed before a definitive conclusion can be made as to whether bariatric surgery will exacerbate or improve infertility, especially as compared to obese comparison cohorts and community rates. SurgerytoConception Interval Considering the favorable improvement in fertility status among postbariatric patients, there is substantial interest in determining an ideal time for conception following surgery. This advice is related to concerns over potential micronutrient deficiencies and adverse perinatal outcomes associated with rapid weight loss. In another study of 104 women that conceived within one year of surgery and 385 that conceived after the first year following surgery, a shortened surgerytoconception interval was not correlated with adverse events in pregnancy (77). These studies, along with a growing body of evidence, suggest that the ideal surgeryto conception interval may not be as critical as previously thought (79). Nevertheless, although patients who conceive during the first postoperative year have comparable shortterm perinatal outcomes compared with patients who conceive after the first postoperative year, it seems reasonable to advise women to delay pregnancy for one year until consensus is reached within the obstetric community. If a pregnancy, however, occurs in a shorter interval, the existing Contraception There is evidence that the effectiveness of oral contraceptives may be affected by post bariatric status, as effectiveness of oral contraceptives relies on sufficient absorption (70,71). In one systematic review examining drug absorption following bariatric surgery, conflicting evidence was found with regard to the effect of postbariatric surgery status on absorption of oral contraceptives. The theoretical mechanism of reduced absorption is related to the metabolism of oral contraceptives, including reduced drug disintegration and dissolution; delayed gastric emptying; bypass of large portions of the small intestines, which may be important for drug absorption; and the reliance of oral contraceptives on firstpass metabolism and enterohepatic recirculation (72). Pregnancy, Perinatal, and Fertility Outcomes Following Bariatric Surgery 233 data should help the caregiver in advising these patients. Following bariatric surgery, practitioners should provide patients with the relevant information and tailor an appropriate reproductive timeline suited to their needs. Miscarriage No studies have comprehensively evaluated the relationship between bariatric surgery and miscarriage. Another study found decreased miscarriage rates among postbariatric patients; however, the study was underpowered (80). Additionally, it is important to recognize that patients who come to bariatric surgery may do so in an attempt to restore fecundity following multiple miscarriages. However, since the number of studies is insufficient and the sample sizes are small, definitive conclusions may not be drawn. Hypertensive Disorders of Pregnancy Obesity has long been associated with increased rates of hypertension and hypertensive disorders of pregnancy (5), which pose risks for the fetus and the mother during pregnancy (65,84). As such, it is imperative to determine whether the weight loss associated with bariatric procedures lowers the likelihood of hypertensive disorders in pregnancy. On the whole, postbariatric status seems to be associated with a lower risk of developing hypertensive disorders during pregnancy; this decrease in risk is found both when patients are compared with their own preoperative status and as compared to an obese cohort (15,50,52,84). Some studies have not found any significant difference in the rates of hypertension among postbariatric surgery patients and obese cohorts (86,87). Several studies have focused on determining the risk of preeclampsia following bariatric surgery. Reducing the rate of preterm deliveries is a key component of reducing maternal/fetal risks, and as such it is of interest to examine the impact of bariatric surgery on this outcome. In one large Swedish cohort, pregnancies of patients following bariatric surgery were associated with shorter gestation (273. Even when obese patients manage to attain adequate glycemic control, there is still a two to threefold increased risk of pregnancy complications as compared to the nonobese cohort (93). Initial studies have pointed toward a potential benefit from bariatric surgery, not only due to the resulting weight loss, but also because of potential associated neuroendocrine changes (94). In another recent study, including parturients from the Swedish Medical Birth Register, 670 singleton pregnancies occurred in women who had previously undergone bariatric surgery and for whom presurgery weight was documented. Cesarean Section Some studies have found that the rate of cesarean section is no higher than community rates (37), while others have documented higher rates of cesarean section following bariatric surgery (15,67). For example, one large prospective study recently found that rates of prior Csection are high among patients who elect for bariatric surgery, highlighting the role that history of prior Csection may play in confounding postoperative rates (88). This same study found that rates of emergent Csection were lower among postoperative patients compared to controls (88). Pregnancy, Perinatal, and Fertility Outcomes Following Bariatric Surgery 235 Fetal Outcomes Given the favorable obstetric risk profile in postbariatric patients as compared to their obese counterparts, it is logical to reflect on whether postbariatric patients can also expect improved perinatal and fetal outcomes. Specifically, no meaningful variations in rates of perinatal complications such as perinatal mortality, meconiumstained amniotic fluid, and low Apgar scores at 1 and 5 minutes were reported between the groups. In another study comparing rates of perinatal complications between postbariatric surgery pregnancies and those of non operated obese patients, no significant differences were found, even though both had higher rates of complications as compared to nonobese counterparts (79). The theoretical reason for concern is related to possible maternal micronutrient deficiencies and the resulting effect on the intrauterine environment (100). Even with the strong body of evidence, healthcare providers should continue to check for maternal micronutrient deficiencies and fetal malformations and provide medically appropriate treatments. This is especially vital in postoperative patients whose obesity persists following surgery, since obesity is an independent risk factor for 236 A Practical Manual of Diabetes in Pregnancy neural tube defects (100). Summary Given the large body of evidence documented in the literature so far, several general conclusions can be made about the impact of bariatric surgery on reproductive health outcomes. The first is that fertility may improve following bariatric surgery, but further studies are needed. Following bariatric surgery, patients are advised to wait one year before conception, although large, populationbased studies have not found significant differences between pregnancies within or after the one year period. Therefore, if patients wish to postpone or prevent pregnancy, clinicians should recommend a nonoral contraceptive as there is a theoretical risk of decreased absorption and effectiveness of oral contraceptives, and no conclusive studies have been performed. Future Directions Further studies are needed to determine the effects, if any, of bariatric surgery on rates of preterm delivery and miscarriage. Additionally, studies examining the efficacy of oral contraceptives following bariatric surgery are imperative to establish appropriate contraceptive guidelines. Finally, additional large populationbased trials and randomized controlled trials should address the possible ramifications of micronutrient deficiencies on the developing fetus. MultipleChoice Questions 1 A G3P2 woman comes to your office in her first trimester. She underwent bariatric surgery three years ago and is concerned about problems she may have during pregnancy because of the bariatric surgery. A Due to her postbariatric status, this woman is at an extremely high risk of preterm labor. She should have postponed her bariatric surgery until she was sure she no longer wanted to have children. B this woman has a very high risk of miscarriage due to her history of bariatric surgery. Pregnancy, Perinatal, and Fertility Outcomes Following Bariatric Surgery 237 2 A woman in her early twenties comes to your office and tells you that she is considering bariatric surgery. A In order to ensure the best maternal and fetal outcome, the best time for this woman to become pregnant is in the first year following bariatric surgery. B After bariatric surgery, oral contraceptives are the most effective form of birth control and are preferred over other birth control methods. D the effectiveness of oral contraceptives is questionable following bariatric surgery, especially in the setting of rapid weight loss. She has come to your office in order to confirm the test and is very excited about this muchwanted pregnancy. C the risk of gestational diabetes and pregnancyinduced hypertension is elevated in this patient because of the recent timing of the bariatric surgery. The short and longterm implications or maternal obesity on the mother and her offspring. Prepregnancy body mass index and gestational weight gain 238 A Practical Manual of Diabetes in Pregnancy 8 9 10 11 12 13 14 15 16 17 with the outcome of pregnancy: a 13year study of 292,568 cases in China.
Proven terazosin 5 mg
What are the potential advantages and disadvantages of bariatric surgery in this clinical context Introduction Diabetes and obesity are both becoming more common on a worldwide basis blood pressure zanidip terazosin 5 mg otc, with increased prevalence in high, middle, and lower income countries (1). Compounding these "twin epidemics," women are choosing to have children at later ages, particularly in many developed countries. These factors have led to an increasing prevalence of gestational and preexisting diabetes mellitus in pregnancy (2). Maternal diabetes and maternal obesity are both associated with a similar range of preg nancy complications (3). This article aims to consider these risks both separately and in combination to outline their epidemiology, prevalence, and contribution to overall risk of adverse pregnancy outcomes from several perspectives: (1) a clinical case discussion; (2) underlying physiology and pathophysiology; (3) epidemiology; (4) the current evidence base for treatments, emphasizing the results of randomized controlled trials; and (5) the importance of these pregnancy factors for later offspring health. It is widely recognized that the hormonal changes of pregnancy can convert some normo glycemic women to varying degrees of hyper glycemia. Physiology and Pathophysiology In early pregnancy, maternal metabolism is anabolic and results in maternal fat deposi tion. In healthy pregnancy, maternal insulin resistance increases throughout the second trimester with a peak in the third trimester due to secretion of placental hormones. In normal women, insulin sensitivity decreases by 50 to 60% from prepregnancy to late pregnancy (12). This decrease in insulin sen sitivity (or increase in insulin resistance) is usually overcome by increased insulin secre tion, ensuring relative normoglycemia. Increasing insulin resistance shifts maternal metabolism from an anabolic to a catabolic state. In the catabolic state, maternal metabo lism becomes more reliant on lipids and ketones. Insulin sensitivity is inversely correlated to maternal plasma free fatty acid levels (13). In addition to an increase in free fatty acid levels, other aspects of mater nal lipid metabolism are also altered during pregnancy. Fat oxidation is significantly higher, and a marked hyperlipidemia occurs in late gestation. For many obese women, the additional rise in insulin resist ance can be counterbalanced by increased insulin secretion. Other women with a reduced insulin secretory potential, for example those with a genetic predisposi tion to glucose intolerance. The transduction of insulin signaling, espe cially in mediating the metabolic effects in its target tissues, is critically dependent on the insulin receptor substrates, with insulin receptor substrate 1 being the main substrate in skeletal muscle and adipose tissue and insulin receptor substrate 2 in the liver (22). While the substrates have overlapping func tions, they also regulate specific processes and therefore cannot fully compensate for each other (22). This included genes encoding proteins involved in fatty acid uptake and intracellular transport, triglyceride synthesis, lipogenesis, and lipolysis. In late pregnancy, inhibition of lipolysis by insulin through inhibition of hor monesensitive lipase is less effective. The placenta synthesizes and secretes a large array of hormones, cytokines, and metabolic signaling molecules. In obese pregnancy, the placenta and the adipose tissue both regulate maternal metabolism, although their regulation is not coordinated. White adipose tissue is not only a reposi tory for lipids but also an active endocrine organ, secreting a wide variety of adipokines and cytokines. Pregnancy is also a state of lowgrade "meta"inflammation with the expression of proinflammatory cytokines from the pla centa and the uterine epithelium (27). As normal pregnancy progresses, the balance between proinflammatory and antiinflammatory cytokines shifts toward the antiinflammatory cytokines (30). Separation of their associations is difficult, especially as the two conditions frequently coexist and obesity commonly lies on the causal pathway toward hyperglycemia. Furthermore, heterogeneity in study population, screening, treatment, and analysis complicates the interpretation of studies. In view of this, the relative "importance" of these factors is heavily influenced by the potential costs and benefits of preventative or treatment strategies. A study (40) regarding 9835 women from Southern California with a high prevalence of overweight (32%) and obesity (28%) reported that, on a population basis, over weight and obesity accounted for 21. Essentially, these studies aimed to limit weight gain in overweight and obese pregnant women through lifestyle interven tion. Obesity and Diabetes in Pregnancy 95 There have been numerous small rand omized controlled trials of (usually intensive) lifestyle and other interventions in over weight and obese women that have demon strated reduced weight gain in pregnancy, and some have demonstrated reduced neonatal weight. To date, the benefits seen in these small studies were not replicated when translated in practical interventions that are affordable at a population level (46). At present, it would appear that diagnosing and treating gestational diabetes in overweight and obese women have the best evidence with regard to limiting weight gain, preventing maternal adverse outcomes, and preventing neonatal adverse outcomes. However, it is important to note that the longterm impacts of any of these interventions on the health of adult offspring are as yet unproven and will need to be carefully examined. Macrosomia can occur even when maternal glucose con trol appears satisfactory and may be due to increased maternal triglycerides and other lipids (14,20). Maternal obesity is a predictor for higher fetal fat mass (53) and is associated with fetal insulin resistance (54). These results suggest that maternal obesity specifi cally affects fetal adiposity rather than overall fetal growth. Birthweight and fetal fatfree mass are both correlated with maternal insulin sensitivity in late gestation (12). Maternal obesity doubles the risk for child hood obesity (56,57) and is associated with metabolic syndrome in the offspring (58). In glucosetolerant Pima Indian mothers who are genetically predisposed to developing type 2 diabetes, maternal glucose levels in the third trimester were strongly associated with increased risk of type 2 diabetes in the offspring (60). These increased risks in the offspring may largely be determined by a genetic back ground predisposing to obesity as well as by the postnatal environment related to the fam ily lifestyle. Animal models have dem onstrated altered epigenetic regulation in many regulatory and metabolic organs in the offspring, including brain, liver, pancreas (61), and adrenals, in response to maternal obesity and hyperglycemia in pregnancy and lactation. In humans, longterm effects of the intrauterine environment have been reported with maternal undernutrition in the Dutch hunger winter study (62). The intrauterine environment may therefore affect the health of the offspring long beyond the immediate perinatal period. These increased risks are especially pronounced in women who were obese prior to pregnancy (59). Other Effects on Offspring Beyond excessive intrauterine growth, other significant complications may affect infants born to women with diabetes mellitus and women with obesity. There are similarities 96 A Practical Manual of Diabetes in Pregnancy and differences in these risks, and the mater nal conditions of diabetes mellitus and obe sity are synergistic in their effects on the infant. Infant of Diabetic Mother Congenital Malformations Effects on Neonatal Complications the association of maternal pregestational diabetes with increased rates of congenital malformations has long been recognized. This risk is clearly related to glycemic control around the time of conception and during organogenesis. In metaanalysis, the relative risk of major congenital malformations is increased in women with pregestational diabetes mellitus by 2. Recent population registry studies show persistent increased rates of congenital malformations in women with type 1 diabetes, which are increased further in women with type 2 diabetes (64). Infant of Obese Mother Congenital Malformations Maternal obesity is itself associated with increased rates of congenital malforma tions. A recent systematic review demon strated a positive association between increasing maternal obesity and congenital heart defects. An analysis of the Florida Birth Defects Registry showed an increase in prevalence of birth defects in liveborn infants, increas ing from 3. Additionally, maternal obesity decreases the chance of detecting congenital anomalies antenatally by 23% in obese women (67). Adiposity assessment using anthropometric measures and total body electrical conductivity demonstrated a marginal increase in birthweight, no change in lean body mass, but a significant increase in percent body fat from 9.
Buy discount terazosin 5 mg
As described in early studies in the Pima Indian population heart attack 6 hours buy terazosin online from canada, it appears clear that offspring of mothers with type 2 diabetes have an increase in adiposity and altered glucose tolerance (37,38), and similar effects are observed in offspring of mothers with type 1 diabetes (39,40), supporting the notion that programming effects are occurring. As a further development, it is suggested not only that clinical outcomes should be improved by detection and treatment of gestational diabetes, but also that diagnostic and intervention programs should be shown to be costeffective (24). Diagnosis in the First Trimester A further important area is the potential for diagnosis of hyperglycemic states in early pregnancy. Systematic review of the literature around the same time (2008) found no randomized controlled trials of screening and treatment earlier than 24 weeks (46). Broadly, higher glucose by a variety of measures would appear predictive of adverse outcomes. Taken together, these data give a sense that earlier treatment may be advantageous, but they are far from determining what the best marker (glucose or HbA1c) or threshold might be and have all of the caveats usually applied to observational data. The dramatic secular increase in type 2 diabetes and obesity should not be forgotten, and it seems clear that it will be necessary to define a group of women with very high glucose who are at particularly high risk of adverse maternal fetal outcomes and who require particular Diagnostic Criteria for Hyperglycemia in Pregnancy 69 supervision. This group currently most closely conforms to the category of overt diabetes in pregnancy and reflect diabetes not detected before pregnancy. Below this category is a much larger group of women who benefit in terms of fetal growth from the detection and management of hyperglycemia in later pregnancy. The exact lower boundaries of this group are clearly still disputed, as is whether the goal will be purely clinical or governed by health economics. This will be refined and may become different in different healthcare settings (26). Particularly for those with the mildest abnormalities of glu- cose tolerance, there are legitimate concerns over the potential for "medicalizing" pregnancy (51), but the beneficial effects on fetal growth and indeed preeclampsia from a fairly unintrusive healthcare intervention in many women should also be emphasized. As others have written, the term gestational diabetes is possibly unhelpful (28) if these women are viewed not as having a defined disease in pregnancy but rather as a group with one of several risk factors. MultipleChoice Questions 1 Overt diabetes in pregnancy or diabetes mellitus in pregnancy can be diagnosed at or above a fasting plasma glucose level of: A 5. Studies of abnormal carbohydrate metabolism in pregnancy; the significance of impaired glucose tolerance. American Diabetes Association Workshop Conference on gestational diabetes: summary and recommendations. Definition, Diagnosis and Classification of Diabetes Mellitus and its Complications. Screening for hyperglycaemia in pregnancy: a rapid update for the National Screening Committee. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diagnostic Criteria and Classification of Hyperglycaemia First Detected in Pregnancy. Association between hyperglycaemia and adverse perinatal outcomes in south Asian and Diagnostic Criteria for Hyperglycemia in Pregnancy 71 26 27 28 29 30 31 32 33 white British women: analysis of data from the Born in Bradford cohort. Toward universal criteria for gestational diabetes: the 75gram glucose tolerance test in pregnancy. Lesser than diabetes hyperglycemia in pregnancy is related to perinatal mortality: a cohort study in Brazil. Interventions for pregnant women with hyperglycaemia not meeting gestational diabetes and type 2 diabetes diagnostic criteria. Impact of increasing carbohydrate intolerance on maternalfetal outcomes in 3637 women without gestational diabetes. Excessive obesity in offspring of Pima Indian women with diabetes during pregnancy. Programming of adiposity in offspring of mothers with type 1 diabetes at age 7 years. Screening for 47 48 49 50 51 gestational diabetes mellitus: a systematic review for the U. Early diagnosis of gestational diabetes mellitus and prevention of diabetesrelated complications. Overweight and obesity affect about 50% of women entering pregnancy in developed countries. Obesity increases the risk of gestational diabetes, preeclampsia, preterm birth, stillbirth, and macrosomia. Lifestyle intervention trials in pregnancy have been shown to reduce gestational weight gain and improve quality of diet. Lifestyle intervention trials have only had a limited impact on clinical pregnancy and neonatal outcomes. Followup in the offspring of mothers participating in lifestyle intervention trials in pregnancy are important to demonstrate impact and safety on longterm outcomes. Early maternal metabolic conditions program placenta function and gene expression from the time of conception. Future intervention trials in prepregnant obese women are needed to examine the effect on maternal and neonatal outcomes in a subsequent pregnancy. At gestational week 28, an oral glucose tolerance test is performed with a 2 h glucose level of 8. Due to glucosuria, an oral glucose tolerance test is done at gestational week 24, and Linda is now diagnosed with gestational diabetes and referred to a program with a diabetes nurse, a dietician, obstetricians, and endocrinologists. By the time of diagnosis, she has gained 5 kg, and with the intervention initiated she restricts the total gestational weight gain to 8 kg. From gestational week 35, insulin treatment is added, and the delivery is induced 4 weeks later due to rapid increase in abdominal circumference of the baby. Birthweight is 4650 g, and the delivery is complicated with a grade 3 anal sphincter injury. Both developed and developing countries have experienced a rapid increase in the prevalence of obesity (1), and this global epidemic poses a significant burden to public health and clinical practice (2,3). Pregnancy has been considered "a window of opportunity" in terms of changing behavior and improving awareness of healthy living. Furthermore, pregnant women are easily reached because of frequent contacts with healthcare professionals during pregnancy. This article highlights different lifestyle intervention trials in obese women and discusses reasons why targeting pregnancy as a time to treat obesity is challenging. Lifestyle Intervention in Obese Pregnant Women Pregnancy offers the opportunity to manage or prevent obesity as many women are concerned with the health of their babies during pregnancy and also are in frequent contact with their healthcare professionals. A few studies have also looked at maternal metabolic parameters such as hyperglycemia, insulin, and lipid profile (10,11). Only one study so far has published detailed childhood followup data in the offspring (12). Lifestyle intervention comprised dietary advice, individual diet plans, and encouragement to exercise. Lifestyle Treatment 75 the behavioral strategies were provided by a research dietician during a facetoface visit after inclusion and in gestational weeks 28 and 36, and followed up by three personal phone calls at 22, 24, and 32 weeks gestation. Women allocated to the intervention group had an individual interview with a health trainer, followed by weekly sessions for 8 weeks (control theory and elements of social cognitive therapy). Based on a 3day food diary during each trimester, the intervention group had a significantly lower energy intake and a reduced intake of food with high glycemic index. No differences in birthweight (primary outcome), length, or neonatal abdominal circumference were seen. Women in the intervention group received four individual diet counseling sessions during pregnancy and an exercise program consisting of aerobic classes (1 h weekly), free fitness club membership during pregnancy, and exercisemotivating initiatives. The study measured a number of metabolic outcomes throughout pregnancy and found that the lifestyle intervention resulted in attenuation of the physiologic pregnancy induced insulin resistance (10). The intervention had no effect on duration of breastfeeding or postpartum weight retention (19). The study is the first pregnancy intervention trial to publish detailed followup in the offspring, showing no anthropometric or metabolic effects at 2.
Diseases
- Cleft palate lateral synechia syndrome
- Hepatic venoocclusive disease
- Astigmatism
- Mayer Rokitanski Kuster syndrome
- Minoxidil antenatal infection
- Sarcosinemia
Terazosin 2mg visa
Closed reduction for acute posterior dislocations was successful in 72% of the patients heart attack jokes discount 1mg terazosin with mastercard. Kirschner wire or pin fixation was associated with a small but significant risk of catastrophic complications. In contrast; multiple high-level studies support the primary fixation of displaced midshaft fractures of the clavicle in select patients. Little evidence exists regarding advantages of specific techniques or implants for the treatment of most fractures of the humerus and shoulder; and the limited high-level evidence available shows no major differences. Despite the lack of high-level evidence; several absolute and relative surgical indications exist for each specific fracture type. American Academy of Drthopacdic Surgeons Chapter 23: Humerus and Shoulder: Fractures and Honunions mated Referen 1. Mao Z, Zhang L, Zhang L, et al: Operative versus nonoperative treatment in complex proximal humeral fractures. The authors reported a 124% increase in the number of were associated with the care of these patients. Substantial costs this meta-analysis compared surgical and nonsurgical treatment in complex proximal humerus fractures and found no important outcomes benefit to surgical treatment. Li Y, Zhao L, Zhu L, Li J, Chen A: Internal fixation versus nonoperative treatment for displaced 3-part or 4-part proximal humeral fractures in elderlyF patients: A meta-analysis of randomised controlled trials. Hertel R, Hempfing A, Stiehler M, Leunig M: Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. Krappinger D, Bizzotto N, Riedmann S, Kammerlander C, Hengg C, Kralinger F5: Predicting failure after surgical fixation of proximal humerus fractures. No substantial between-group differences in complications or outcomes were found, and the outcomes in both patient groups generally were excellent. Buecking B, Mohr J, Bockmann B, Zettl R, Ruchholtz S: Deltoid-split or deltopectoral approaches for the treatment of displaced proximal humeral fractures Osteoporosis, displaced varus fracture, medial comminution, and insufficient medial support were independent risk factors for reduction loss. Medline this randomized study of 120 patients compared the standard deltopectoral approach with a minimally invasive deltoid-split approach for treating displaced fractures of the proximal humerus. Boileau P, Winter M, Cikes A, et al: Can surgeons predict what makes a good hemiarthroplasty for fracture Uutcomes and tuberosity healing were substantially better with the use of a fracture-specific stem. Multivariate logistic regression analysis confirmed that the restoration of medial cortical support was the most reliable factor for preventing bone- and fracture-related complications. No substantial differences in complications or outcomes were found, and the outcomes in both patient groups generally were excellent. Zafra M, Uceda P, Flores M, Carpintero P: Reverse total shoulder replacement for nonunion of a fracture of the proximal humerus. The authors of this study included 13 randomiaed controlled trials with a total of 443 patients. The use of intramedulla ry nailing was associated with an increased risk of shoulder morbidity, intraoperative fracture comminution, a higher incidence of implant failure, and increased risk of revision surgery. It was concluded that compression plating may be superior to intramedullary nailing in the treatment of humeral shaft fractures. Medline not this retrospective review of humeral shaft fractures com- pared 91 nonsurgically treated patients with 95 surgically treated patients. No substantial differences in the rate of delayed union or radial nerve palsy were reported between the two groups. Ali E, Griffiths D, Obi N, Tytherleigh-Strong G, Van Reusburg L: Nonoperative treatment of humeral shaft fractures 43. Cosens T, Speigner B, Minekus J: Fracture of the scapular body: Functional outcome after conservative treatment. Functional outcomes were best with fixation of both the clavicle and the scapular neck. Borkurt M, Can F, Kirdemir V, Erden Z, Demirkale I, Basboxkurt M: Conservative treatment of scapular neck fracture: the effect of stability and glenopolar angle on clinical outcome. Canadian Urthopaedic Trauma Society: Multicenter randomized clinical trial of nonoperative versus operative treatment of acute acromio-clavicular joint dislocation. There were no substantial between-group differences, but patients who were Urthopaedic Knowledge Update 12. American Academy of Urthopaedic Surgeons Chapter 23: Humerus and Shoulder: Fractures and Honunions nonsurgically treated had better early outcomes. Similar between-group union rates were reported with a substantially higher complication rate in those treated with a hook plate. Tauber M, Gordon K, Koller H, Fox M, Resch H: Semi- clavicular ligament procedures using a cortical fixation button or tendon graft, a 2 Canadian Clrthopaedic Trauma Society: Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures: A multicenter, randomized clinical trial. Virtanen K], Remes V, Pajarinen], Savolainen V, Bjorkenheim 1M, Paavola M: Sling compared with plate osteosynthesis for treatment of displaced midshaft clavicular fractures: A randomized clinical trial. Surgical treatment resulted in substantially lower rates of nonunion and better functional outcomes. In a retrospective review of 19 patients treated with a locking plate for distal clavicle fracture, a 100% union rate was reported, along with an excellent return of function. Section 3: Upper Extremity clavicular fractures: A meta-analysis of randomized clinical trials. Xu J, Xu L, Xu W, Cu Y, Xu J: Clperative versus nonoperative treatment in the management of midshaft clavicular fractures: A meta-analysis of randomised controlled trials. Plate fixation resulted in superior outcomes with lower rates of nonunion, fewer total complications, and fewer symptomatic malunions. No substantial between-group differences were reported, with the exception of faster recovery in patients treated with plate fixation. Bak K, Fogh K: Reconstruction of the chronic anterior unstable sternoclavicular joint using a tendon autograft: Medium-term to long-term follow-up results. This randomized study of 59 patients compared plate fixa- tion with elastic intramedullary nail fixation for displaced fractures of the midshaft clavicle. Lazarides S, Zafiropoulos G: Conservative treatment of fractures at the middle third of the clavicle: the relevance of shortening and clinical outcome. American Academy of Cirthopaedic Surgeons Chapter 24 Shoulder Arthritis Neal Chen. Reverse shoulder arthroplasty can be used to address abnormal glenoid morphology, glenoid bone loss, and revision problems. Propionibacteriam acnes is conunonly isolated from cultures obtained during revision shoulder surgery. Keywords: shoulder arthritis: shoulder arthroplasty; reverse shoulder arthroplasty; Propionibacterium aches: viscosupplementation: arthropathy. Traditional treatment options consist of conservative management, nonarthroplasty surgery, and arthroplasty. Evidence of the effectiveness of these modalities is limited and their overall utility is unclear. Patients receiving viscosupplementation reported a significant decrease in pain levels at 26 weeks compared to a control group receiving saline injections. Autumn; Jaddn 1E Section 3: Upper Extremity Biologic Resurfacing of the Glenoid With Hemiarthroplasty There was great potential for treatment of the young patient with arthritis using a resurfacing arthroplasty or hemiarthroplasty of the humerus coupled with resurfacing of the glenoid using allograft fascia lata or lateral meniscus. Because of currently weak evidence, biologic resurfacing of the glenoid remains a topic of controversy. Many manufacturers have short, miniastemmed, or even stemless shoulder replacement components. Glenoid Component Understanding of the factors that affect glenoid component loosening is improving. Superior tilt of the glenoid, preoperative posterior humeral head subluxation, and reaming that violated the subchondral bone were associated with glenoid component subsidence. Moreover, retroversion of the glenoid of more than 10" was associated with loosening. A study of 23 patients who underwent hemiarthroplasty demonstrated that patients with concentric glenoid wear reported significantly greater Modified Neer and EuroQol scores than those patients with Orthopaedic Knowledge Update 12 El 2M American Academy of Orthopaedic Surgeons Chapter 14: Shoulder Arthritis ogy in osteoarthritis:4 is classified in Table 1. However, two had subsequent revision arthroplasty and two additional patients had broken screws on radiographs.
Generic 2 mg terazosin with amex
This is consistent with previous reports in that pseudarthrosis is the most common postoperative complication requiring revision in the neuromuscular scoliosis population hypertension benign essential 4011 cheap terazosin 2 mg without prescription, and with clear 25. A recent metaanalysis of complications in neuromuscular spinal deformity surgery included 7,612 patients and found an overall implant complication rate of 12. A study of 74 neuromuscular patients who underwent spinal fusion reported 6 cases of broken rods, yet 4 were asymptomatic and did not require revision surgery. A pseudarthrosis can result from several causes including insufficient stability or infection and often presents in the form of pain, deformity progression, or failed instrumentation. Although these new techniques have been shown to be powerful in the correction and maintenance of pelvic obliquity, they also have introduced new modes of failure. Iliac screws became popular with proponents citing diminished implant failure and lower pseudarthrosis rates; however, complications related to rod disengagement from screws and connectors were reported. In the case of implant failure in Galveston rods, revision to modern screw-based constructs is commonly used if fusion is not present. Revision of screw-based constructs commonly consists of additional or longer screw placement with deformity correction and debridement and bone grafting of pseudarthrosis, if present. Longer screws have been shown to improve implant stability if they reach anterior to the caudal extension of the middle osteoligamentous column. One patient in the S2-alar group required revision for sacral joint pain, which improved with longer screw placement, and one patient in the traditional group required revision for failure of fixation and pain at implant site. Myung et al retrospectively looked at 41 patients with neuromuscular scoliosis who underwent posterior spinal fusion to the pelvis with iliac screws in 31 patients and S2-iliac screws in 10 patients. Despite this, only 2 patients required revision surgery, both in the iliac screw group for failed pelvic anchors. They noted that no failure occurred in patients in whom there were 6 or more screws in L5 and below. They concluded that more robust distal pelvic anchorage was protective against implant failure and this was easier to achieve with S2iliac screws. In neuromuscular spinal deformity, there are considerable forces the implant must withstand to prevent complications and achieve a successfully outcome. Each technique has cited advantages and disadvantages, and understanding several is necessary to manage a revision surgery for failed spinal or sacropelvic instrumentation. Preoperative hyperkyphoses greater than 50-degree and greater than 10-degree intraoperative reduction of thoracic kyphosis have both been identified as a risk factor for junctional kyphosis as significant intraoperative correction of kyphosis can concentrate this stress at the ends of the fusion. Also a more rigid construct using all pedicle screws, especially at the transition between instrumented and uninstrumented vertebrae, has been found to have a higher incidence of junctional kyphosis compared to less rigid constructs using all-hook or hybrid fixation. Minimizing soft-tissue dissection and preserving the facet joints, interspinous, and supraspinous ligaments near the ends of the construct are commonly recommended to preserve the posterior tension band near transitions. An anterior approach is generally unnecessary as the kyphosis can be managed posteriorly. If there is associated neuroforaminal or central stenosis, decompression may be a necessary addition as well. Osteotomies are sometimes a necessary addition for correction of the junctional deformity along with proximal extension of the fusion. However, the goal in revision surgery for junctional kyphosis should be a moderate correction. If too much correction is attempted, the kyphotic deforming forces can be translated into the new end vertebra and a compensatory curve can even develop. Patient had to undergo a revision due to decompensation in the coronal and sagittal plane. Once corrected, rod-to-rod connectors are used to attach the new rods to the existing ones. Both of these were successfully treated by extending the posterior fusion several levels superiorly. Although revisions are uncommon, both of these studies highlight the fact that revision spine surgery for junctional kyphosis in the neuromuscular patient is technically demanding, but successful outcomes are possible with careful planning. The authors concluded that cervical deformity correction should be offered to patients with Duchenne muscular dystrophy with significant neck deformities at the same time as undergoing thoracolumbar curve correction as these patients are vulnerable to repeat anesthesia and surgery. All patients had stable arthrodesis with significant clinical improvement in posture and were able to maintain horizontal gaze compensatory postures through 10. Although the technique of Giannini does not typically use instrumentation, posteriorly based instrumentation and extension to the occiput has been described with success in addition to posterior releases and bone graft in the treatment of these rare and challenging deformities. This muscle imbalance, especially in the setting of remaining growth, leads to poor head control in extension and often to progressive cervical lordosis and fixed hyperextension contractures. Giannini et al described a technique to address cervical spine hyperextension that has been successfully applied to patients with various underlying myopathies. Next the interspinous spaces are freed using a rongeur, as they are typically very narrow, and then the neck is then forward flexed, correcting the deformity. Finally, wedge-shaped autograft bone without instrumentation is placed between the spinous processes posteriorly to maintain the correction and facilitate arthrodesis. This technique was applied to seven patients with Duchenne muscular dystrophy with rigid neck hyperextension or poor head control in extension in addition to a significant thoracolumbar spinal deformity. Both deformities were corrected in the same operative setting with the cervical extension deformity addressed by the Giannini technique after posterior fusion from T1 to sacrum was complete. All of the patients achieved significant deformity correction, improved posture, and head References [1] Sarwark J, Sarwahi V. Spinal fusion augmented by Luque-rod segmental instrumentation for neuromuscular scoliosis. Results and complications after spinal fusion for neuromuscular scoliosis in cerebral palsy and static encephalopathy using Luque Galveston instrumentation: experience in 93 patients. Maintenance of sagittal plane alignment after surgical correction of spinal deformity in patients with cerebral palsy. Results and morbidity in a consecutive series of patients undergoing spinal fusion with iliac screws for neuromuscular scoliosis. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Evaluation of proximal junctional kyphosis in adolescent idiopathic scoliosis following pedicle screw, hook, or hybrid instrumentation. Proximal junctional kyphosis in adolescent idiopathic scoliosis after 3 different types of posterior segmental spinal instrumentation and fusions: incidence and risk factor analysis of 410 cases. Proximal junctional kyphosis in adolescent idiopathic scoliosis following segmental posterior spinal instrumentation and fusion: minimum 5-year follow-up. Risk factor analysis of proximal junctional kyphosis after posterior fusion in patients with idiopathic scoliosis. Complications of the Luque-Galveston scoliosis correction technique in paediatric cerebral palsy. Proximal junctional kyphosis following spinal deformity surgery in the pediatric patient. Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Mechanisms of curve progression following sublaminar (Luque) spinal instrumentation. Nontraumatic proximal junctional kyphosis with catastrophic neurologic deficits after instrumented arthrodesis in an adolescent with cerebral palsy: case report and review of the literature. Surgical treatment of neck hyperextension in Duchenne muscular dystrophy by posterior interspinous fusion. The development of validated disease-specific metrics for neuromuscular scoliosis and their use in prospective studies will further help guide decision-making to maximize patient quality of life. Keywords: cerebral palsy, Duchenne muscular dystrophy, flaccid neuromuscular disease, health-related quality of life, myelomeningocele, neuromuscular scoliosis, spinal cord injury, spinal muscular atrophy. However, such motor disorders are often accompanied by disturbances of sensation, perception, cognition, and communication. Despite the static nature of the original insult, patients may also go on to develop secondary musculoskeletal problems, which may be progressive throughout life. Hip displacement usually precedes the onset of scoliosis, but this is not always the case.
Buy cheap terazosin 5 mg on line
The degree to which this balance is shifted in favor of the desirable effect and the certainty with which this balance is established will ultimately dictate the recommendation strength heart attack kush buy terazosin 1 mg with visa. Additional extensions are forthcoming: for those and for up-to-date references relevant to this ch ecltlist. These standards include transparency, management of conflicts of interest, for rating evidence, articulation of guidelines, external review, and requirements for updating guidelines. Give the rationale for the choice of cases and a: D (b) Cohort study-For matched studies, give matching criteria and number of exposed and unexposed Case-control study-For matched studies, give matching criteria and the number of controls per case. Describe comparability of assessment methods if there is more than one group Describe any efforts to address potential sources of bias Explain how the study size was arrived at Explain how quantitative variables were handled in the analyses. If applicable, describe which groupings were chosen and why (a) Describe all statistical methods, including those used to control for confounding (b) Describe any methods used to examine subgroups and interactions (c) Explain how missing data were addressed (d) Cohort study-If applicable, explain how loss to follow-up was addressed Case-control study-If applicable, explain how matching of cases and controls was addressed Cross-sectionai study-If applicable, describe analytical methods taking account of sampling strategy ell Describe any sensitivity analyses 9 1! Note: An Explanation and Elaboration article discusses each checklist item and gives methodological background and published examples of transparent reporting. Case-controi study-Report numbers in each exposure category, or summary measures of exposure Cross-sectionai study-Report numbers of outcome events or summary measures Main results 16 a Give unadjusted estimates and, if applicable, confounder-adjusted estimates and their precision [for instance, 95% confidence interval. Report other analyses done-such as analyses of subgroups and interactions, and sensitivity analyses 13 19 Summarize key results with reference to study objectives Discuss limitations of the study, taking into account sources of potential bias or imprecision Discuss both direction and magnitude of any potential bias Interpretation Generalizability other information Funding 20 21 Give a cautious overall interpretation of results considering objectives, limitations, multiplicity of analyses, results from similar studies, and other relevant evidence Discuss the generalizability external validity of the study results 22 Give the source of funding and the role of the funders for the present study and, if applicable, for the original study on which the present article is based. A Note: An Explanation and Elaboration article discusses each checklist item and gives methodological background and published examples of Remaining Challenges the quality of the evidence is not the only factor that can influence clinical decision making. American Academy of Drthopaedic Surgeons Chapter 2: Levels of Evidence and Grades of Recommendation if the treatments are inconsistent, painful, toxic, or associ- Another factor is uncertainty, which pervades the work orthopaedic surgeons do. For many important clinical problems that physicians treat daily, high-quality evidence is lacking. Several tools can help an orthopaedic surgeon in the face of uncertainty; decision analysis is one such tool. Although it is methods-intensive, decision analysis can provide helpful, real-world-applicablc conclusions. High-quality decision analyses have been performed comparing surgical with nonsurgical treatments of Achilles tendon rupture," direct-exchange versus two-stage treatment of the infected arthroplasty,14 and other treatmentsdi! Some recent and high-quality guidelines include those on management of osteoarthritis, hip fractures in the elderly, carpal tunnel syndrome, and distal radius fractures. In addition to the quality of the evidence in support of a treatment, physicians must consider patients" preferences and values. The fact that a treatment is available and potentially indicated, such as aggressive chemotherapy for a particular tumor, or elective joint surgery, does not mean that every patient will opt to pursue it, particularly ated with complications. Shared decision-making tools are emerging as a means to help physicians understand the value systems of each patient and help patients learn what they need to know to help guide care. Key Study Points - Even when the evidence base for decision making helping each patient make the best possible choices ments of shared decision making. U this studyr sought to estimate the effect of patient requests for specific types of pain medications on physician prescribing behavior: the authors found that requests for particular brand-name drugs made it more likely that physicians who otherwise did not use those medications as much would prescribe those drugs. Begg C, Gho M, Eastwood S, et al: Improving the quality of reporting of randomized controlled trials. Bishop J, Ring D: Management of radial nerve palsy associated with humeral shaft fracture: A decision analysis model. Hannon M, Mannin R, Dorney K, Mooney D, Hennelly K: Pediatric cervical spine injury evaluation after blunt trauma: A clinical decision analysis. American Academy of Urthopaedic Surgeons: EvidenceBased Ciinicai Practice Gnideiines. National Academy of Sciences: Standards for Deeeioping Trustworthy Ciinicai Practice Gnideiines. Surgeon leadersh ip a nd safety knowledge are key to the implementation and maintenance of surgical safety progra ms. Such programs shoul d be put into place to prevent adverse surgical events and improve surgica l outcomes in all orthopaed ic patients. It is important for the orthopaedic surgeon to be knowledgeable about the core competencies of surgical safet y fo r surgeons, surgical patients, surgical teams, and surgical facilities. The regu lar systematic use of these core competencies is essential for the delivery of safe surgical care. Surgical safety requires committed surgeon eaeler hip supporting surgical team behav iors re uir. Several nontechnical competencies of orthopaedic care are needed to balance technical competencies Dr. Robb Ill or an immediate fam ily member has received royalties from lnnomed; has stock or stock options held in Stryker; and serves as a boar d member, owner, officer, or committee member of the American Academy of Orthopaedic Surgeons and t he Orthopaedic Research and Education Foundation. Waddell nor any immedia the family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this chapter. In 1999, the Institute of Medicine, in the document To Err is Human: Building a Sa fer Hea lth System, ra ised important safety concerns. Despite improvements in health care including advances in surgica l tech niques and equipment, medica l errors caused as many as 98,000 deaths each year. As a result, physicians and researchers intensified efforts to identify deficiencie within health system that could be corrected to improve patient safety. The surgeon and all other healthcare professionals (anesthesiologist, the operating room nurse, physician assistant, nurse practitioner, surgical technician, any medical student directly in contact with the surgical patient during the surgical event. E wrong-site surgery that was promoted to all hospitals and operating rooms in the United States. The program recommended that before every surgery, the surgeon patient chart, [2 check and display patient radiographs, 3 confirm that a correct consent has been obtained, and 1] confirm the correct surgical information in the and categories of sentinel events. In 2004, the Joint Commission introduced a new surgical safety standard, the Universal Protocol, which required regular use for hospital accreditation. Joint Commission Efforts to Improve Surgical Safety In 1996, the Joint Commission initiated a program of voluntary self-reporting of adverse safety events, termed sentinel events and defined as events contributing to or causing severe temporary or permanent patient harm, injury, or death. Among 21 defined sentinel events cat- egories, 2 are surgical: an invasive procedure or surgery on the wrong patient, at the wrong site, or using the wrong unintended procedure and unintended reten- tion of a foreign object after an invasive procedure or surgery. Two other categories are often associated with surgery: infection-related events and medical or surgical equipment-related events. To maintain facility accreditation, all sentinel events require immediate hospital review, appropriate corrective actions, and voluntary reporting to a confidential Joint Commission Sentinel Events database. Because reporting is voluntary, the database likely represents an underreported number of events National Quality Forum Initiatives In 2001, the National Quality Forum introduced the term "never events" to describe egregious medical events, such as wrong-site surgery, that caused harm to the patient The National Quality Forum adopted evidence-based recommendations to make patient care safer, improye health outcomes, and contain healthcare system costs. In 2002, the National Quality Forum defined a set of serious reportable events designed to better protect patients from harm. In 2014, the serious reportable events for surgical and invasive procedures wrong patient; the wrong surgical procedure; unintended retention of a foreign object in a patient during surgery; and intraoperatiye or immediate postoperative were updated to include surgery on the wrong side or death of a patient categorized as American Society of Anesthesiologists physical classification class 1. American Academy of Drthopaedic Surgeons Chapter 3: Patient Safety and Core Competencies Table 2 Table 3 Joint Commission Universal Protocol Requirements Standardized Preprocedure Verification Process Correct surgical site, procedure, and patient Availability and proper functioning of needed surgical equipment Availability of needed surgical documentation! Leapfrog Group Established in 2003, the Leapfrog Group is composed of 150 public and private healthcare organizations representing 34 million healthcare consumers in the United States. Of the 23 safety and quality measures, 19 are direct or indirect surgical safety or quality improvement measures Table 4. The Leapfrog scoring methodology has been validated as confirmation of hospital safety and quality performance. Section 1: Principles in firthopaedics Table 4 Table 5 Leapfrog Safety and Quality Measures Directly Related to Surgery Leadership structures and systems Culture measurement. E E Eu In 1: U surgeon and team safety knowledge, as these skills historically are not taught or used during surgical residency training or in hospital surgical departments. Surgical Site Infection 55] is defined by the Centers for Disease Control and Prevention as an infection at a surgical site occurring within 30 days of a surgical procedure or within 1 year that involves a surgical procedure with a nonbiologic device hardware or implant. Proper use of such nontechnical skills often requires additional in surgical technical skills; however, new focus is on use of surgical procedure, patient factors, and facility or system factors. For most outpatient or surgery center surgeries, infections are uncommon, at less than 0. For commonly performed elective hospital-based orthopaedic procedures such as total hip replacement or total knee replacement, infections rates are reported to be 1. American Academy of Clrthopaeclic Surgeons Chapter 3: Patient Safety and Core Competencies preparation, appropriate preoperative antibiotics, glycemic control in diabetic. Optimal skin preparation begins the night before surgery with local cleansing of the surgical site and adjacent limb or body area using a chlorhexidine gluconate or antibacterial soap.
Buy terazosin 5 mg lowest price
Using this method blood pressure machine name purchase line terazosin, value-based purchasing models can recognise innovations in quality, efficiency, and cost savings. At the same time, poor performance is discouraged through the withholding of reimbursements and the assessment of penalties for preventable hospital readmissions and hospital-acquired conditions. Those funds are used to reward hospitals that achieve the lowest rates of poor-performance events. Although defining the term quality beyond hospital-based process measures is often elusive, a great clinical practice guidelines, and applying peer-reviewed appropriate use criteria. These initiatives will remain a focal point for advocacy in the changing landscape of government regulation. Bundled Payments Bundled payments represent a form of reimbursement based on a predefined episode of care. If bundled payments are not appropriately risk stratified for case complexity and expected resource utilization, treating only the healthiest and easiest patients cherry picking and denying care to sicker, more complex patients. Patient-Centered Medical Home Model the patient-centered medical home model is a healthcare delivery model with a central healthcare provider leading a group of medical professionals with the goal of coordinating care in a multidisciplinary manner to improve healthcare outcomes through synergistic use of resources. Care is facilitated by registries, information technology, health information exchange, and other means to ensure that patients get the indicated care when and where they need it and want it in an appropriate manner. American Academy of Drthopaedic Surgeons Chapter 6: Health Policy nisation of the care delivery process. The purpose of these new models is to assist the transition from the fee-for-service reimbursement systems to systems that incentiviae high-value care for patients. Owing to the enormous societal effect of these policies, understanding their history is increasingly important in the day-to-day practice of medicine. The shift away from traditional fee-for-service reimbursement, which rewards providers solely on the volume of units of care, toward more value-based principles, which place emphasis on the quality of coordinated care, is a central theme in the current healthcare environment. Mastering these concepts will enable individual providers of care to be successful in the new medical marketplace. Current Medicare eligibility has expanded to include specific subsets of Americans younger than 65 years. In 1 922, Congress expanded the eligibility to include younger Americans who have permanent disabilities or blindness and are eligible for Social Security Disability Insurance or those with end-stage renal disease. In 2001, coverage again was extended by Congress to include Americans with amyotrophic lateral sclerosis. In this model, traditional fee-for-service payment is preserved but, going forward, 4% to 9% of the payment will be adjusted based on the performance of quality and outcome measures. Beginning on January 1, 2019, the following four performance categories will be assessed: quality, resource use, use of electronic health records, and the establishment of clinical practice improvement activities. I the Social Security Amendments of 1965 created the Medicare and Medicaid entitlement programs in the United States, which drastically changed the health insurance landscape in the country. I Rapidly increasing healthcare costs have led to 2010, which sought to reform insurance coverage to protect children and patients with preexisting conditions, expand Medicaid eligibility, and incentivise healthy patients to participate in insurance programs. U Although most Medicare beneficiaries are covered by traditional Medicare, a growing number of individuals have enrolled in Medicare Advantage plans. The percentage of beneficiaries enrolled in these plans has grown from 13% in 2004 to 31% in 2016. Medicare pays the administrators of these plans a capitation fee per beneficiary to cover all Part A and Part B benefits and provides a separate payment if the plan provides Part D benefits. The standard Medicare Part D drug benefit contained a coverage gap (known as the donut hole] whereby beneficiaries were required to pay the full cost of their medications, even while they continue to pay premiums. In 2014, when the ont-of-pocket drug costs of Medicare beneficiaries exceed 152,35 0, they enter this coverage gap until costs total $4,550. Medicaid covers economic disadvantaged Americans and individuals with substantial disabilities. Medicaid is financed by the federal and state governments, with federal matching of state funding varying from state to state. In 2016, it is estimated that nearly $600 billion will be spent on healthcare services provided to Medicaid beneficiaries. A list of all participating healthcare facilities and the details of models and episodes is available at this Website. Gainsharing with physicians and other providers can be an effective way to drive care redesign. This extra 50% fee for a procedure with no additional overhead or other costs creates a powerful incentive for improvement. These areas are counties associated with a core urban area that has a population of at least 50,000. The pro- pensity score was defined as the conditional probability of sustaining a fracture based on preoperative comorbid conditions. The American College of Surgeons National Surgical lQuality Improvement Program database was used to analyse in-hospital and 30-day postoperative clini- cal outcomes. The analysis showed that compared with patients with osteoarthritis, patients with femoral neck fractures sustained more complications, had longer hos- pital stays, were more likely discharged to a skilled care facility, and had higher rates of unplanned hospital readmissions. The authors concluded that these data show that resource utilization for fracture patients is substantially higher than for patients with osteoarthritis. The two competing approaches to value-based reimbursement-capitation and bundled payments-are discussed. The authors believe that capitation is not the correct long-term solution and support the use of the bundled payments approach. Medicare Physician Payment Reform: Implications and Dpiions for Physicians and Hospitals. Quality Payment Program: Modernizing Medicare to provide better care and smarter spending for a healthier America. A timeline for eligible Part B Medicare providers is provided, beginning in January 201. American Academy of Urthopaedic Surgeons Drthopaedic Knowledge Update 12 Chapter 7 Medical and Surgical Risk Factors Mouhanad IvI. A com- prehensive understanding of these comorbidities would lead to proper perioperative medical management, which, if done thoroughly and appropriately, would positively affect postoperative outcomes and reduce resource utilization. This goal can be achieved through appropriate management of all the medical comorbidities, risk factors, and biopsychosocial factors that might affect the perioperative course. When needed, orthopaedic surgeons should consult specialised providers including but not limited to subspecialiaed internists, psychiatrists, physiatrists, physical therapists, and social workers to optimise the postoperative outcomes. Keywords: medical clearance; risk factors; comorbidities: perioperative management Emphasizing quality-driven care and patient satisfac- tion and preventing provider-associated perioperative conditions have the potential to positively affect federal and private insurance reimbursement rates substantially. These goals inevitably make physicians accountable for patient comorbidities that affect surgical outcomes, posing a dilemma for the orthopaedic surgeon providing care for this high-risk patient population. Therefore, surgeons should be implementing a collaborative, team-based approach to optimize preoperative medical clearance in patients scheduled for surgery as a crucial step to improve postoperative outcomes. Cardiovascular Risk Assessment and Optimization Cardiovascular disease is the leading cause of death in the United States. Neither of the foiiowing authors nor any immediate famiiy member has received anything of vaiue from or has stock or stock options heid in a commerciai company or institution reiated directiy or indirectiy to the subject of this chapter: Or. In cases of urgent surgery needed after a recent myocardial infarction, such as surgery for a femoral neck fracture in a geriatric patient, the surgeon should weigh the benefits of the procedure against the bleeding risk and the risk for cardiac events. The advantage of coronary revasculariaation also should be taken into consideration. If it proves to be absolutely beneficial, a combined coronary artery bypass grafting might be considered at the time of the urgent orthopaedic surgery. E Coronary Artery Disease Cardiac functional capacity is expressed in metabolic equivalents. The American College of Cardiology and the American Heart Association guidelines recommend that cardiac testing should be reserved for patients with high clinical predictors for cardiovascular complications or for those unable to meet a functional capacity of 4 metabolic equivalents during daily activities. Hip arthroplasty, knee arthroplasty, and hip fracture are the procedures associated with the highest risk. One of the challenges in using pharmacologic agents is balancing the benefit of anticoagulation against the risk of bleeding complications. Pharmacologic thromboprophylaxis is not recommended for orthopaedic patients with fractures in areas other than the hip or those with soft-tissue injuries, nor for arthroscopy patients. Unfractionated heparin should be considered for bridging in patients with substantial renal impairment (creatinine clearance <30 mLfmin) who are at high risk for thromboembolism. Continue aspirin therapy while holding clopidogrel 5-1fl days before surgery in patients at moderate or high risk for cardiovascular events.