Proven ivermectin 3mg
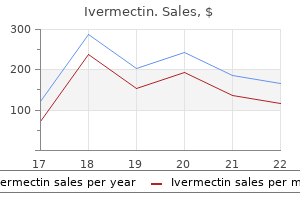
If a transfusion is indicated usp 51 antimicrobial effectiveness test buy ivermectin online pills, irradiated leukocyte-reduced red cells are preferred. In patients with newly diagnosed myeloma, induction chemotherapy is often associated with a prompt improvement in hemoglobin levels, so it is better to avoid the use of erythropoietin. Erythropoietin (Epogen) should be seriously considered in relapsed patients receiving chemotherapy who have a persistent, symptomatic hemoglobin level of 10 g/dL or less. Erythropoietin reduces the transfusion requirement and increases hemoglobin concentration in more than half of patients. Most physicians proceed with a trial of erythropoietin 150 U/kg three times weekly, or 40,000 U once a week. Darbepoetin, a long-lasting erythropoietin (Aranesp), may be given weekly or biweekly. Skeletal Lesions Bone lesions manifested by pain and fractures are a major problem. A skeletal radiographic survey should be repeated at 6-month intervals, or sooner if pain develops. Daratumumab has a response rate of approximately 30% in heavily pretreated patients. Ixazomib Ixazomib (Ninlaro) is an oral proteasome inhibitor approved for the treatment of relapsed myeloma. Other New Drugs New drugs that are in clinical trials include new proteasome inhibitors (marizomib5, oprozomib5, and dinaciclib5). Supportive Therapy Radiotherapy Palliative radiation in a dose of 20 to 30 Gy should be limited to patients who have disabling pain and a well-defined focal process that has not responded to chemotherapy. This approach is preferred to local radiation because pain often occurs at another site, and local radiation does not benefit the patient with systemic disease. In addition, the myelosuppressive effects of radiotherapy and chemotherapy are cumulative and can restrict future therapy. Infections Bacterial infections are more common in patients with myeloma than in the general population. All patients should receive pneumococcal and influenza immunizations despite their suboptimal antibody response. Substantial fever is an indication for appropriate cultures, chest radiography, and consideration of antibiotic therapy. The greatest risk for infection is during the first 3 months after chemotherapy is initiated and prophylactic antibiotics (levofloxacin [Levaquin] or co-trimoxazole [Bactrim]) should be considered during this period. Antiviral prophylaxis (acyclovir [Zovirax] 400 mg twice daily or valacyclovir [Valtrex] 500 mg once daily) should be given to all patients receiving bortezomib because of the increased risk of herpes zoster. Hyperviscosity Syndrome Symptoms of hyperviscosity can include oronasal bleeding, gastrointestinal bleeding, blurred vision, neurologic symptoms, or congestive heart failure. Most patients have symptoms when the serum viscosity measurement is more than 4 cP, but the relationship between serum viscosity and clinical manifestations is not precise. The decision to perform plasmapheresis, which promptly relieves the symptoms of hyperviscosity, should be made on clinical grounds rather than serum viscosity levels. Hyperviscosity is more common in immunoglobulin (IgA) myeloma than in IgG myeloma. Raje N, Terpos E, Willenbacher W, et al: Denosumab versus zoledronic acid in bone disease treatment of newly diagnosed multiple myeloma: an international, doubleblind, double-dummy, randomised, controlled, phase 3 study, Lancet Oncol Feb 8. San Miguel J, Weisel K, Moreau P, et al: Pomalidomide plus low-dose dexamethasone versus high-dose dexamethasone alone for patients with relapsed and refractory References 425 Multiple Myeloma demineralization of the skeleton. Fixation of long bone fractures or impending fractures with an intramedullary rod and methyl methacrylate gives excellent results. Pamidronate (Aredia) 90 mg intravenously over 2 hours every 4 weeks or zoledronic acid (Zometa) 4 mg intravenously over 15 minutes every 4 weeks are equally efficacious. Because renal insufficiency or nephrotic-range proteinuria can occur, serum creatinine and 24-hour urine protein monitoring is necessary. Bisphosphonates should be resumed upon relapse with newonset skeletal-related events. Although the relationship is unclear, it is essential to obtain a complete dental evaluation and perform preventive dental treatment before beginning bisphosphonates. Invasive procedures (especially dental extractions) should be avoided during bisphosphonate therapy. Vertebroplasty or kyphoplasty may be helpful for patients with an acute compression fracture of the spine. Results appear to be better when the procedure is performed shortly after the compression fracture. A choice between vertebroplasty and kyphoplasty depends on the expertise of the physician performing the procedure. Extradural Myeloma (Cord Compression) the possibility of cord compression must be considered if weakness of the legs or difficulty in voiding or defecating occurs. The sudden onset of severe radicular pain or severe back pain with neurologic symptoms suggests compression of the spinal cord. Radiation therapy in a dose of approximately 30 Gy is beneficial in about one half of patients. Dexamethasone (Decadron)1 should be administered in addition to radiation therapy. Surgical decompression is necessary only if the neurologic deficit does not improve. Venous Thromboembolism Patients with multiple myeloma have an increased risk of venous thromboembolism. This is due to the malignancy itself as well as therapy with lenalidomide, thalidomide, or pomalidomide. Emotional Support All patients with multiple myeloma need substantial and continuing emotional support. It is vital that the physician caring for patients with multiple myeloma has the interest and capacity for dealing with incurable disease over the span of years with assurance, sympathy, and resourcefulness. A thorough history and physical examination should be performed on every patient with one or more peripheral blood cytopenias, along with basic laboratory tests such as iron studies, vitamin B12, and folic acid levels. However, many disorders can cause pancytopenia; therefore consideration for a hematology referral should be entertained for the evaluation of pancytopenia or persistent otherwise-unexplained cytopenias, in which case a bone marrow biopsy may be necessary. These mutations involve genes encoding for splicing factors, epigenetic modifiers, and transcription factors among others. These processes include excessive apoptosis of myeloid progenitors, abnormal responses to cytokines and growth factors, epigenetic aberrations resulting in gene silencing, chromosomal abnormalities, and a defective bone marrow microenvironment. Those with significant neutropenia and thrombocytopenia can present with infections or bleeding. Systemic symptoms are less common but, when present, can herald disease progression. These include mycophenolate mofetil (Cellcept), ganciclovir (Cytovene), lead, and excess zinc. The treating physician should consider the ultimate goal of therapy and whether it is intended to cure, extend survival, or merely palliate symptoms. Clinical trials evaluating novel agents are being conducted to help identify effective agents for patients who have relapsed or failed to respond to standard therapies. Immunomodulatory Drugs the novel class of immunomodulatory drugs includes thalidomide (Thalomid)1 and lenalidomide (Revlimid). Thalidomide was investigated initially with some success in patients with low-risk disease. It has been shown for the first time that treatment with 5-azacitidine was reported to result in prolongation of survival in patients with Int-2 and high-risk. The recent introduction of reducedintensity conditioning regimens and nonmyeloablative transplants has resulted in expanding the age limit for performing the procedure, reducing transplant-related complications and mortality. Because stem cell transplantation is associated with a high rate of treatment-related death-estimated at 39% at 1 year-and the development of acute and chronic graft versus host disease, such treatment is recommended to patients with high-risk disease. It is curable only by allogeneic stem cell transplantation, which is feasible in only a small subset of patients.
Purchase ivermectin 3mg otc
An otorhinolaryngology consultation may be helpful in determining which surgical approaches may be most beneficial for the individual bacteria phylum purchase ivermectin american express. Assessment and appropriate counseling for weight loss, cardiovascular risk factors, and driving while untreated (or extreme caution) should be part of a treatment plan. Weight loss may reduce soft tissue in the neck, making the oropharynx less compressible. The improvement in lung volumes accompanied by weight loss also favor enhancement of longitudinal traction on the upper airway, the so-called "tracheal tug. The patient wears a snug-fitting T-shirt with a pocket sewn onto the back between the shoulder blades with two or three tennis or wiffle balls inserted into it to discourage the patient from turning onto the back during sleep. A correctional device for positional sleep apnea is also approved in the European Union. Unfortunately, shoulder or hip pain often limits the application of positional therapy, especially in elderly persons, and long-term adherence or compliance remains poor, with only about one-third of patients able to perpetuate positional therapy strategies in long-term follow-up. Nasal pillows, a type of cannula that provides a tight seal within the nares, and a newer tube-like frame that sits in front of and not within the nares are most effective at lower treatment pressures; they may be favored by many patients with claustrophobia but may dislodge at higher pressures or with frequent nocturnal movement. Nasal masks of various types are used in many patients, but if mouth breathing and consequent leak are a problem, a chin strap may be added, or an oronasal face mask may be substituted. They provide a means of advancing the mandible that pull the tongue base forward slightly, opening the oropharyngeal airway to some degree and obviating some apnea and hypopnea events. There is as yet limited experience with the device; however, this may be an option for some patients who are averse to or intolerant of other therapies. Central Sleep Apnea Syndrome Central sleep apnea syndrome results from an unstable ventilatory drive during sleep, resulting in periods of insufficient ventilation and compromise of gas exchange despite a patent oropharyngeal airway. Central sleep apnea has a heterogeneous pathophysiology and may be idiopathic or due to high-altitude-induced periodic breathing, due to Cheyne-Stokes breathing, or narcotic-induced. Neurologic causes-such as brainstem infarction or neurodegenerative disorders, including multiple system atrophy-may also cause central apnea. In heart failure, the presence of central sleep apnea syndrome or Cheyne-Stokes breathing imparts a poor prognosis. Treatment-Emergent Central Sleep Apnea Syndrome Treatment-emergent central sleep apnea syndrome is a subtype of central sleep apnea wherein patients have significant obstructive/ anatomical problems with ventilation, but also have unstable ventilatory patterns noted in patients with central sleep apnea syndromes. Some patients clearly continue to manifest frequent central sleep apneic events more than five times per hour, leading to the suboptimal outcomes of persisting clinical complaints of hypersomnia and medical risk. Sleep-Related Hypoventilation the causes of hypoventilation during sleep include primary pulmonary parenchymal disorders, neuromuscular conditions affecting bellows musculature, or restrictive physiology of the chest wall accompanying kyphoscoliotic disorders or morbid obesity. Failure to treat significant nocturnal hypoventilation may result in the development of sequelae of hypoxemia such as polycythemia, pulmonary hypertension, and right heart failure, or of hypercapnic respiratory failure. These therapies are best titrated in the context of a supervised overnight laboratory polysomnogram under the direction of a sleep or pulmonary medicine specialist. Cataplexy is a distinctive and highly specific symptom characterized by emotionally provoked muscle atonia intruding into wakefulness that is seen in a minority of patients overall and may precede but more often follows onset of the main symptom of hypersomnia. In addition to sleepiness and cataplexy, the full clinical pentad of narcolepsy also includes symptoms of sleep paralysis (the inability to move the body upon awakening), hypnogogic hallucinations (the intrusion of dream imagery and mentation into conscious awareness following awakening), and sleep-maintenance insomnia (with frequent nocturnal arousals and difficulty maintaining sleep). However, narcolepsy is most frequently monosymptomatic, with the sole symptom being pervasive, enduring sleepiness and decreased vigilance with a tendency toward dozing off inadvertently in permissive settings and the overwhelming desire to nap during the daytime, especially in the afternoons. Naps are most often highly refreshing; scheduled naps can be utilized to therapeutic advantage or indeed, in rare patients, as the sole treatment for those bent on avoiding stimulant pharmacotherapy. Narcolepsy is relatively uncommon, affecting approximately 1:2000 of the general population. While the etiology of narcolepsy remains unknown, most experts continue to favor a long hypothesized autoimmune cause. Within the last few years, epidemic narcolepsy-cataplexy following H1N1 vaccination in Narcolepsy and Central Disorders of Hypersomnolence Europe and Asia also provided further support for the autoimmune hypothesis of narcolepsy. Unfortunately, these tantalizing discoveries have not yet yielded clear insight into pathogenic mechanisms nor more specific therapies for patients, and the mainstay of treatment for the condition remains the use of older stimulant and wake-promoting medications, or prescribed therapeutic napping, as naps are most often highly refreshing and restorative in narcolepsy patients. Idiopathic hypersomnia is a closely related condition often difficult to distinguish from narcolepsy without cataplexy, although a few nuanced clinical features tend to distinguish it from narcolepsy, chiefly a characteristically reported unrefreshing nocturnal sleep and nap quality. Idiopathic hypersomnia has previously been further subclassified as variants with or without prolonged sleep period, although these phenotypes are overlapping and current diagnostic standards have eliminated this distinction. Hypersomnia is also commonly associated with as many as 50% of those with myotonic dystrophy type 1. The mainstay of treatment for each of these conditions is stimulant and wake-promoting agent therapy, with the goal of improved vigilance and psychomotor functioning. Stimulants and wakepromoting agents range in intensity from lower to higher intensity and efficacy/tolerability options, from modafinil (Provigil) and armodafinil (Nuvigil) on the milder end of the spectrum-although selected narcolepsy patients respond quite well to these drugs-to methylphenidate (Ritalin), and to the amphetamine/dextroamphetamine (Adderall). Relevant clinical pharmacology of the stimulant medications commonly used in clinical practice are summarized in Table 4. Pitolisant (Wakix), a selective H3 subtype histamine inverse agonist/antagonist proven effective as a wake promoting agent for narcolepsy, recently received European Medicines Agency marketing authorization but is currently unavailable in the United States. Patients with uncontrolled hypersomnias should be cautioned against driving, operating dangerous machinery, or engaging in other similarly dangerous activities or hobbies while they are drowsy, as they may be prone to sudden and unpredictable sleep attacks. Circadian Rhythm Sleep Wake Disorders Circadian rhythm sleep disorders result in misalignment of the timing of the sleep period relative to the desired bed and rise times, resulting in concurrent insomnia and hypersomnia symptoms despite normal total sleep time. The most common circadian rhythm disturbances are actually exogenous influences on the patient and his/her circadian axis, which in these cases is functioning normally but is unable to adjust rapidly enough to the required new temporal milieu. Jet lag disorder results when an individual crosses across several transmeridian time zones in a single day. Crossing one or two time zones is usually not too difficult for the traveler to accommodate, but crossing three time zones typically causes symptoms of jet lag. Flying eastward is generally much more difficult than flying westward, as patients more easily accommodate phase delay then phase advancing, or "loss" of time. Also critical is attempting to rapidly adapt to the new time zone, such as by seeking regular sunlight exposure during the daytime and avoiding light exposure in the evening. Shift-work sleep disorder results from workers who must constantly and regularly alter or rotate their work schedules between different shifts (so-called "swing shifts") or workers who must accommodate a regularly scheduled second or third shift. Shift workers often have difficulty adapting and shifting their sleep-wake schedules and develop symptoms of 7 Available as a dietary supplement. Shift workers must be educated to prioritize regularly obtaining a sufficient quantity of sleep, regardless of their work circumstances. Swing shift workers should also be counseled to avoid working more than five night shifts in a row, as night shift work frequently leads to a greater degree of sleep deprivation over time. Shift workers should also be counseled to avoid rotating swing shifts whenever possible, to strictly avoid scheduling overtime duty, and to avoid long commutes (and to exercise special caution to avoid drowsy driving). Judicious use of caffeinated beverages, or prescribed stimulant therapy with modafinil may be helpful for enhancing vigilance in some patients, but should be used with caution as they might interfere with sleep initiation. Adolescent and young adult patients present with profound intractable initial insomnia due to their inability to fall asleep at a conventional bedtime as required for school or most daytime occupations, and profound daytime hypersomnia due to their inability to arise and function in the morning hours. Diagnosis is easily recognized by clinical history and sleep diaries, with or without adjunctive actigraphy to objectively verify the pattern of consistent delayed 731 Sleep Disorders 732 sleep-phase periods. The presentation can mimic depression, whose hallmark biological sign is often noted to be an early morning awakening; care should be taken to carefully distinguish between these two diagnoses. Treatment of each is difficult; options include specifically timed bright light therapy, with or without light restriction, and timed administration of low dose melatonin. Bright light therapy is administered at approximately 2500 lx intensity for at least 30 minutes. However, the efficacy of blue light restriction currently lacks explicit evidence from large clinical trials. As a last resort, the measure of chronotherapy, a progressive delay of bedtime every few days, is prescribed, with the bed and rise times being progressively and successively delayed until the desired bed and rise times are achieved. Attempts to then entrain the patient on this schedule with the aforementioned measures are again attempted with scheduled bright light and prescribed timed melatonin dosing. Parasomnias and Other Nocturnal Events Parasomnias are nocturnal events that disrupt sleep but usually do not appreciably disturb sleep quality. Consequent clinical manifestations are surprisingly heterogeneous and often age related, with specific syndromes such as sleep terrors (also called night terrors) in children, sleep walking and confusional arousals seen in children and adults, and sleep-related eating behavior seen almost exclusively in adults, especially those receiving zolpidem or other newer prescribed hypnotics. As such, pediatric parasomnias are frequently outgrown; however, in some patients, they do endure throughout life. Nightmares are undesirable, disturbing dreams that lead to sudden arousal from sleep with heightened autonomic sequelae of sweating, hypervigilance, tachycardia, and tachypnea.
Discount ivermectin online amex
The destruction of liver tissue leads to decreased production of coagulation and fibrinolytic proteins such that a new Plasma 388 balance is established antimicrobial needleless connectors purchase cheapest ivermectin and ivermectin. Patients with end-stage liver disease have been shown to have normal levels of circulating thrombin and reduced levels of certain anticoagulant proteins. Thus the prophylactic use of plasma to correct a mildly prolonged laboratory value in the absence of bleeding is not indicated. It will lead to unnecessary plasma infusion, and the risk of volume overload and transfusion reactions outweighs the benefit in these patients. In trauma patients, patients with ruptured aortic aneurysms, and patients with other arterial bleeding, massive transfusion may be necessary. The basic principles of such a scenario include taking steps early into the resuscitation to prevent the patient from becoming too cold, acidotic, or coagulopathic to reverse the situation. Some plasma (and cryoprecipitate, if the fibrinogen is very low) should be infused early into the resuscitation to help prevent coagulopathy. Hemophilia A, hemophilia B, and von Willebrand disease are no longer treated by plasma but can require factor concentrates to prevent bleeding. Systemic administration of heparin must be reversed by protamine, if fast reversal is desired. Reversal of anticoagulation in the setting of intracranial hemorrhage or life-threatening bleeding depends on the anticoagulant. Inquire with a transfusion medicine physician or hematologist to determine whether such a protocol exists in your facility. Supplement with plasma or prothrombin complex concentrate depending on urgency of correction. If the product has been pooled in plasma before freezing, then one unit will increase fibrinogen by 7 to 8 mg/dL; a six-unit pool will increase fibrinogen by 45 mg/dL. Check with the transfusion service laboratory regarding which product is available and the expected increment. Reactions to transfusion are relatively common; life-threatening reactions are rare (Tables 3 and 4). The infusion of product should cease, at least until the laboratory results are known and the patient has responded to treatment. The main point of the laboratory investigation is to evaluate the plasma for abnormal (usually red) color in an effort to detect intravascular hemolysis as quickly as possible. If the hemolysis, clerical, and direct antiglobulin test checks are negative, one might consider restarting the transfusion with careful surveillance of the patient. A direct antiglobulin test is also performed to detect the presence of antibody coating red blood cells in circulation; a positive result could indicate extravascular hemolysis, which is not as dangerous as intravascular hemolysis. Hypertension, tachypnea, and transient decrease in oxygen saturation can also occur until the symptoms are treated. Cytokines produced by white blood cells present in cellular blood components (red blood cell and platelet units) are responsible for the clinical presentation. Platelets also secrete cytokines; thus leukoreduction of platelet units might not be successful in preventing the reaction. These include obstetric bleeding, trauma involving head injury or crush injury, and sepsis. Clinical events that can lead to an isolated decrease in serum fibrinogen concentration include administration of L-asparaginase (Elspar) and surgeries that disrupt bladder or salivary gland endothelium. Fibrinogen concentrates are available for patients who will not accept cryoprecipitate. Transfusion Triggers Transfusion is appropriate in patients with low serum fibrinogen, typically less than 100 mg/dL. In cases of massive transfusion, a trigger of 150 mg/dL is considered practical, so that the patient becomes less coagulopathic in the time that it takes to draw and review new laboratory values. New evidence indicates that a fibrinogen level of less than 300 mg/dL predicts severe postpartum hemorrhage, as a normal postpartum fibrinogen level is in the 600 mg/ dL range. Because component therapy aims to replete coagulation factors to hemostatic (rather than completely normal) levels, consensus guidelines suggest maintaining a fibrinogen level greater than 200 mg/dL during a postpartum hemorrhage. Administration of an antipyretic is the routine treatment; meperidine (Demerol)1 may be required to address severe rigors. Ordering leukoreduced red blood cells and platelets (if the hospital inventory is not entirely composed of leukoreduced components) is also a preventive measure. For recurring reactions with platelets, volume reduction of the component can reduce the incidence. Allergic reactions are immunoglobulin (Ig)Emediated reactions against some allergen in the donor plasma. Because all blood components have some amount of plasma, it is possible to experience an allergic reaction with any blood product. For patients with recurrent reactions, transfusing the blood product more slowly (maximum of transfusion over 4 hours), or premedication with antihistamines will reduce the incidence. The patient has respiratory distress, typically during the transfusion, and increase in blood pressure unless cardiac decompensation occurs. Radiographic findings include pleural effusions, perihilar edema, and increased vascular pedicle width. Slowing the infusion rate with a maximum time of transfusion over 4 hours can prevent the reaction. Red blood cells have proteins and carbohydrates on the cell surface that are antigenic. These epitopes are categorized into blood groups based on structure and sharing of a parent protein. A patient who lacks particular epitopes can develop antibodies through pregnancy or transfusion. Such red blood cell alloantibodies can then lyse transfused red blood cells that possess the cognate antigen. When time allows for pretransfusion testing, the antibodies are identified, and antigen-negative units are provided. In a patient with absolute IgA deficiency, naturally occurring anti-IgA can precipitate this reaction on binding IgA in the plasma. Airway and blood pressure support should be provided with the patient recumbent and the lower extremities elevated. The treatment of choice is epinephrine (Adrenalin) 1 mg/ mL, also labeled as 1:1000 or 0. If symptoms persist, the dose may be repeated every 5 to 15 minutes for a maximum of three times, unless palpitations, tremors, or extreme anxiousness occurs. Bronchodilators such as albuterol can be given as adjunctive treatment for bronchospasm that does not appear to respond to epinephrine. For patients on -blockers, the addition of intravenous glucagon1 (GlucaGen) 1 to 5 mg administered over 5 minutes, followed by infusion of 5 to 15 g/minute, may be required. The addition of glucocorticoids can help prevent the biphasic reaction that occurs in some patients. Steroids may be administered, although their effectiveness has not been confirmed through controlled trials. The most-common presentation includes fever and rigors, nausea and vomiting, and possible onset of moderate hypotension during or after a platelet transfusion. Rarely, presentation includes signs of overt septic shock, including marked hypotension, typically early into the transfusion of a red blood cell or platelet component. The most-common organisms to contaminate a platelet product are gram-positive organisms such as Staphylococcus epidermidis. These organisms are thought to be introduced into the collection bag via a skin plug that results from phlebotomy using a large-gauge needle when sterilization of the phlebotomy site has been ineffective. The most common organisms to contaminate a red blood cell unit are gram-negative, endotoxin-producing organisms such as Yersinia enterocolitica. This organism is introduced into the blood product as a result of asymptomatic bacteremia in the donor, from sources such as the gastrointestinal tract. The donor-screening questionnaire and vital sign assessment at the time of donation help to make collection from such a donor a very rare event. Transfusion of a bacterially contaminated red blood cell unit is most often a fatal event.
Order 3mg ivermectin with mastercard
Oral carbonic anhydrase inhibitors are not commonly used today because effective topical medications are available antibiotics for acne bactrim cheap 3 mg ivermectin with amex. Side effects can include aplastic anemia, kidney stones, bitter taste, indigestion, paresthesia of the extremities, tinnitus, and polyuria. Clinicians need to consider the possibility of hypokalemia when patients take other diuretics to control blood pressure (Table 2). Laser Trabeculoplasty Argon or selective laser trabeculoplasty can be used to increase aqueous outflow. Laser trabeculoplasty is noninvasive and safe, Mechanism of Acute Angle Closure: Pupillary Block After aqueous is produced in the ciliary body in the posterior chamber, it travels through the pupil and exits the anterior chamber through the trabecular meshwork located between the iris and the cornea. Pupillary block occurs when the iris comes in contact with the lens and obstructs the flow of aqueous through the pupil. Increased posterior chamber pressure displaces the iris anteriorly against the trabecular meshwork and stops aqueous outflow. These patients have smaller eyes, allowing the lens to contact the iris to initiate papillary block. The distance between the iris and the lens is the shortest when the pupil is mid-dilated. They are administered once at bedtime but may be administered once at any time during the day to promote adherence. Side effects are primarily local and include increased conjunctival hyperemia, increased lash growth, and possible irreversible increase in periocular and iris pigmentation. Timolol (Betimol, Istalol, Timoptic), levobunolol (Betagan), and betaxolol (Betoptic) are color-coded by yellow caps. Physicians need to be aware that a topical -blocker is a potential cause of acute changes in cardiovascular or pulmonary status. There are several reported incidents of death following the use of topical -blockers mostly due to exacerbation of asthma. Brimonidine (Alphagan) and apraclonidine (Iopidine) belong to the class of selective 2 receptor agonists, and brimonidine is more commonly prescribed; it is color-coded by purple caps. Dorzolamide (Trusopt) and brinzolamide (Azopt) are color-coded by orange caps and are sulfabased medications. However, some patients complain about transient stinging and a bitter taste in the mouth after administration. Timolol and dorzolamide (Cosopt) and timolol and brimonidine (Combigan) are color-coded by blue caps. Combined medications decrease exposure to preservatives and can decrease irritation and problems with dry eyes. It is ineffective or less effective in some patients with light trabecular meshwork pigmentation. The effect of laser decreases over time but may be repeated in the case of selective laser trabeculoplasty. Surgery the most commonly performed glaucoma surgeries are trabeculectomy, tube shunt, and cyclodestruction. Trabeculectomy and tube shunt are procedures that create an opening in the sclera to increase aqueous outflow. The procedure can be transscleral or endoscopic; the endoscopic method is typically done at the time of cataract surgery. Alternative surgical methods such as deep sclerectomy, Trabectome, canaloplasty, iStent and Cypass are performed at the time of cataract surgery to minimize the invasiveness and potential complications associated with traditional glaucoma surgery however these have lower efficacy. Visual Impairment and Blindness Patients who are visually impaired (Snellen vision of less than 20/ 40) or legally blind (Snellen vision of less than 20/200 or visual field of less than 20 degrees) may have significantly decreased mobility and ability to function. Continued glaucoma treatment is still important in these patients because even maintenance of countfinger vision can allow the patients some degree of independence. Low-vision devices and services, including high-contrast video magnifiers, audiobooks, eccentric viewers, and mobility training, can allow patients maximal use of their residual vision and improve their confidence and quality of life. Acute Angle Closure Glaucoma Pupillary block in susceptible patients blocks aqueous drainage and leads to sudden and extreme rise of intraocular pressure. Acute angle closure can damage the optic nerve, resulting in acute angle closure glaucoma. History can include hyperopia, onset after exposure to a dim environment, or taking anticholinergic medications. Acute angle closure is sometimes misdiagnosed as migraines or gastrointestinal illness. Patients with conjunctivitis, keratitis, uveitis, and corneal abrasion can also present with the same symptoms. Treatment If acute angle closure is suspected, an emergent referral to ophthalmology is indicated. The maximum dose of oral or intravenous carbonic anhydrase inhibitor is given: acetazolamide 500 mg or methazolamide 50 mg (see Table 2). If there is no improvement after another 30 minutes, a hyperosmotic, oral glycerin1 1 g/kg or intravenous mannitol (Osmitrol) 1 g/kg over 30 minutes, is administered. Once the pressure is controlled, it is important to perform an iridotomy in both eyes to prevent future episodes. Patients who have undergone procedures that cause acute loss of vestibular function often have vertigo for a while after the surgery; the vertigo improves more quickly with vestibular rehabilitative therapy. One drop of topical aqueous suppressant-blocker, selective 2 agonist, or carbonic anhydrase inhibitor-should be administered (timolol, brimonidine, dorzolamide) (see Table 1). The patient is placed in the supine position to allow the lens and iris to fall posteriorly. The patient is reassessed in 30 minutes, and if the condition is not improved, topical drops are repeated. Hyperosmotics may be contraindicated in patients with congestive heart failure, and glycerin can cause severe hyperglycemia in diabetic patients. Possible reasons for this periodic swelling of the endolymph compartment include mechanical obstruction of endolymph flow or at least dysregulation of the electrochemical membrane potential between endolymph and perilymph compartments. Vertigo usually lasts 1 to 6 hours but can last as little as 30 minutes or as long as all day. Patients prone to motion sickness often report that their dizziness lasts longer because the aftereffect of vertigo lingers longer in those who are motion sensitive. The hearing loss is usually unilateral, and patients might notice fluctuation in hearing accompanied by ear fullness and a low-pitched roaring tinnitus either before or coincident with the vertigo. These spells, referred to as otolithic crises of Tumarkin, can lead to serious injury and should prompt aggressive treatment. The mechanism is presumed to be related to sudden mechanical deformation or sudden neural discharges related to the otolith structures of the inner ear. Meanwhile, with each vertigo attack, some vestibular function is lost, and so as vertigo attacks continue, vestibular loss ensues, often paralleling the hearing loss. Patients might report less severe dizziness or just a vague feeling of unsteadiness. Surgical treatment of both sides is also problematic because it could leave the patient with bilateral hearing loss, vestibular loss, or both. Acoustic neuroma (vestibular schwannoma) typically leads to slowly progressive unilateral sensorineural hearing loss, but vertigo is infrequently a prominent feature because patients compensate gradually as their vestibular function wanes due to compressive effects of the tumor. Fluctuating unilateral hearing loss, ear fullness, and tinnitus can occur without vertigo and is referred to as cochlear hydrops. When a patient has very frequent vertigo attacks and is disabled, more-aggressive treatment may be considered sooner. The average person consumes about 4000 mg daily, and the maximum recommended daily intake of sodium is 2300 mg. Because more than 70% of the daily sodium comes from processed foods, this dietary restriction generally requires more than simply stopping the use of table salt, which generally accounts for only about 10% of daily sodium intake for most people. The most commonly prescribed diuretic is hydrochlorothiazide 25 mg combined with triamterene 37. Acetazolamide (Diamox)1 125 to 250 mg bid or furosemide (Lasix)1 10 to 20 mg daily are also options. Patients with severe sulfa allergy can use low-dose ethacrynic acid (Edecrin)1 12. Scopolamine in patch form (Transderm-Scp)1 is too slow to be useful because o it takes hours to be absorbed transdermally.
Buy ivermectin pills in toronto
Speech therapy referral for a swallow evaluation should be performed if there is concern for dysphagia antimicrobial herbs and spices purchase 3 mg ivermectin with visa. When used as a maintenance therapy, 1 to 2 exchanges are typically performed, at variable intervals, as frequently as weekly. Hypotension may occur because of citrate-induced hypovolemia, and it may be associated with hypocalcemia. It is dosed 325 mg/m2 weekly for 4 weeks, although it can also be dosed 1 g/m2 with a second dose 2 weeks later. Side effects include infusion-related symptoms including pruritis, headache, hypotension, nausea, and chills. Infusion-related symptoms can be pretreated with acetaminophen and diphenhydramine. It is dosed at 900 mg weekly for 4 weeks, followed by 1200 mg for the fifth week and thereafter 1200 mg every 2 weeks. Generally only mild infusion reactions are reported, typically managed by pretreatment acetaminophen and diphenhydramine, although there is risk for severe meningococcal infection. Cyclophosphamide (Cytoxan)1 is typically reserved for treatment-refractory patients. Periodic laboratory monitoring is required with use of immunomodulatory medications, which may vary depending on the specific medication used. Myasthenic crisis may be seen in up to 20% of patients at some point in disease course. It is important to recognize that new respiratory or swallowing complaints can quickly escalate, and patients with these complaints should be quickly assessed. One can assess diaphragm strength by the force of a strong sniff or cough; patients should be able to count to 20 after a deep breath. Pathophysiology Most optic neuritis occurs as a result of inflammation causing demyelination of the ganglion cell axons that compose the optic nerve. The natural history of clinically isolated optic neuritis includes resolution of pain 3 to 5 days after onset and nadir of vision 7 to 14 days after onset. Myasthenic crisis is most commonly encountered in the setting of concomitant illness, change in medications, or early in the disease course because maximum weakness occurs in the first year of the disease in 66% of patients. Respiratory failure can result from respiratory muscle weakness, oropharyngeal weakness, or a combination of both. Staccato speech or dyspnea that precludes speaking in full sentences is of high concern for myasthenic crisis. Spirometry with forced vital capacity <2 L or negative inspiratory force of <40 cm H2O should be sent to the hospital for further evaluation. Assessment of swallowing function by speech therapy and possible modified barium swallow should be considered in the context of dysphagia for solids and liquids. Though it typically affects women in their fourth decade of life, 1 in 4 patients are male, and patients have been reported ranging from the first to seventh decades of life. A typical optic neuritis patient experiences acute or subacute loss of vision characterized by decreased visual acuity, visual field loss, and/or color vision loss, accompanied or preceded by pain in the affected eye that is worse with eye movements. Other signs include a relative afferent papillary defect in cases where one eye is affected and a mildly swollen optic nerve head in approximately one-third of patients. Spontaneous improvement in vision is typically evident within 3 weeks, and almost 70% of affected patients recover 20/20 visual acuity even in the absence of treatment. Long-term side effects of steroid treatment for this condition are rare owing to the brief period of treatment. Differential Diagnosis Other diagnostic considerations in a patient with unilateral painful vision loss without explanatory pathology evident on ophthalmic examination include other optic neuropathies such as those due to sarcoidosis, lupus, vasculitis, neoplastic, vascular, and infectious causes. Treatment with low-dose oral prednisone alone (1 mg/kg/day for 14 days) was associated with an increased risk of relapse compared with placebo treatment. The 15-year follow-up results, published in 2008, demonstrated persistence of visual recovery. Therefore it is important to screen for historical and current neurologic impairment through history and examination. This should be considered in patients with severe vision loss, bilateral involvement, or history of prior optic neuritis or transverse myelitis. Testing for this is commercially available with a published sensitivity and specificity of 63% and 99%, respectively. Complications Though more than 70% of patients with optic neuritis recover objectively normal visual acuity, many have residual subjective visual disturbances. Complications of steroid therapy include insomnia, agitation, and stomach irritation. Atypical features for optic neuritis such as systemic symptoms, history of cancer, pain that persists beyond 2 weeks, progressive vision loss beyond 14 days, no spontaneous improvement in vision, retinal hemorrhages, cotton-wool spots, or macular exudates should prompt diagnostic evaluation for etiologies other than optic neuritis. Regardless of the decision to treat or not with steroids, all patients should be monitored closely. The average age of onset is in the seventh decade of life, but onset is before age 40 in 3% to 5% of cases. Ninety percent of cases are considered to be sporadic or idiopathic, whereas approximately 10% are inherited. Other proposed risk factors include exposure to pesticides, herbicides, solvents, and well water. Cigarette smoking, coffee consumption, regular exercise, and elevated uric acid levels may be protective. Loss of dexterity with fine motor tasks, micrographia (small handwriting), hypophonia (soft speech), masked facies (diminished facial expression and reduced blinking), shortened strides, and decreased arm swing while walking are all potential manifestations of bradykinesia. This symptom can lead a patient to explore musculoskeletal causes, such as seeking out a specialist in sports medicine, before realizing it has a neurologic basis. In addition, patients with essential tremor can exhibit cogwheeling without underlying rigidity. Parkinsonian tremor most classically starts in one hand, although it can be seen in the jaw and lower extremity as well. It has a slow frequency (4-6 Hz) and is visualized with the affected body part at rest. It is often enhanced by distraction (conversation, having the patient perform calculations or name the months backward) and can be temporarily alleviated by concentration or repositioning. This is referred to as "reemergent rest tremor" and differs from essential tremor, which is typically present immediately on extending the arms. Early gait changes can include bent posture and shuffling or dragging of the feet, often initially on one side of the body. Later gait changes can include freezing (hesitancy and difficulty initiating a stride with a sensation of feeling stuck to the floor) and festination (a series of small, rapid steps with a sensation of being propelled forward and unable to stop). Postural instability is assessed with the "pull test," in which the examiner stands behind the patient and tugs back firmly on his or her shoulders. An abnormal response is defined by taking two or more steps backward or, in severe cases, by complete lack of response, leading to the examiner catching the patient as he or she falls back. This leads to degeneration of dopamine-producing neurons in the substantia nigra pars compacta, setting off a chain of altered signaling in the basal ganglia and ultimately reduced activation of the motor cortex. However, Lewy body deposition and neurodegeneration also occurs in other brain regions, perhaps well before the degeneration of the substantia nigra. Unfortunately, the pathophysiological process that leads to Lewy body formation is not well understood at this time, and several different mechanisms have been proposed.
Buy generic ivermectin on line
However infection 8 weeks after birth ivermectin 3 mg with mastercard, authorities warn that these statistics considerably underestimate (owing to underreporting) the true magnitude of epidemics, which field studies estimate as 50 times greater. A frightening prospect associated with failing mosquito control in urban habitats is the potential reemergence of yellow fever similar to the recent rapid resurgence of dengue, which is also transmitted by the vector A. Experts contend that one of the most profound mysteries of tropical medicine is that this dangerous virus has not emerged more frequently where a susceptible, unimmunized human population and the vector density coexist. However, since the 1980s, a resurgence of yellow fever has been seen across South America and Africa, which augurs potential risk for the United States. While yellow fever outbreaks remain unlikely in the Unites States, travelrelated cases should be expected, as well as the possibility of brief urban cycle transmission in the American Southeast. A large urban outbreak in Angola, which began in December 2015 and subsequently spread to the Democratic Republic of the Congo, resulted in 962 confirmed cases and 393 deaths and included multiple travel-related cases appearing in nonendemic areas internationally such as China. The outbreak in Brazil was first recognized in December 2016, with more than 1828 confirmed cases and 560 deaths noted as of April 24, 2018, including two dozen travel-related cases. This upsurge of human cases, which is the highest observed in the Americas for decades, reflects the spread into densely populated metropolitan areas, such as Rio de Janeiro and Sao Paulo, which in the past were not considered at risk for transmission. This outbreak has impacted not only Brazil but six other American countries: Bolivia, Colombia, Ecuador, French Guiana, Peru, and Suriname. In the current outbreak, all human cases have been linked only to Haemagogus and Sabethes mosquitoes. Yellow fever remains the most dangerous arbovirus ever to inhabit the Western Hemisphere. Despite ongoing vaccination and mosquito control efforts in endemic areas, sylvatic and intermediate transmission cycles persist and appear to be expanding toward urban spread. Public health leaders encourage clinicians to utilize heightened suspicion and awareness for the virus, especially among travelers to tropical areas. Recent yellow fever outbreaks underscore boldly the potential threat this disease poses for the international community. In jungle (sylvatic) yellow fever, the virus is transmitted by various forest canopy mosquitoes that acquire it from wild primates and then disseminate it to humans who are visiting or working in the jungle. Incidence of the disease is highest during months of peak temperature, rainfall, and humidity in South America and during the late rainy and early dry seasons in Africa. In the intermediate (savannah) cycle, which is most common in Africa, transmission of the virus to humans results from humans living or working in jungle border areas, with the virus spread from monkey to human or from human to human by mosquitoes. Humans infected with the virus are infectious to mosquitoes (what is termed being "viremic") shortly before the onset of illness and up to 5 days after onset. Yellow fever is a mosquito-borne infection that can be prevented by mosquito avoidance and vaccination. Mosquito control is an essential component of any strategy to prevent the spread of yellow fever. Before the development of the vaccine and after the mosquito was proven as the vector, eliminating mosquito-breeding sites and decreasing exposure to A. During jungle outbreaks, mosquito elimination is impractical and evacuation is essential until individuals are immunized and mosquitoes controlled. To prevent further mosquito transmission during outbreaks, infected patients should be isolated in well-screened rooms sprayed with insecticides. Immunization is the most effective and reliable way to prevent yellow fever in areas in which it is endemic. A single dose of vaccine gives greater than or equal to 99% protection and confers lifelong immunity. The typically well-tolerated vaccine is contraindicated in pregnant women, in individuals with concurrent febrile illness or compromised immunity, and in infants younger than 6 months. If infants aged 6 to 8 months cannot avoid travel to a high-risk location, parents should discuss immunization with their physician, since the vaccine is usually not offered until the age of 9 months. The International Certificate of Vaccination is valid for 10 years from 10 days after immunization or immediately after reimmunization. After the 2016 outbreaks depleted global vaccine supplies, experts suggested as a dose-sparing strategy the utilization of a fractional dose of the vaccine among children 2 years of age or older and among nonpregnant adults. In the 2018 outbreaks, mass vaccination campaigns have utilized primarily fractional dosing. With an incubation period lasting 3 to 6 days, the illness is typically biphasic, with a two-stage course during which the pulse slows and kidney involvement occurs along with bleeding disorders. In those cases recognized, the pulse is usually rapid initially but by the second day becomes slow for the degree of fever (Faget sign). In most cases, this initial period of mild infection resolves after 1 to 3 days, occasionally longer, and the illness concludes with rapid recovery and no sequelae. However, approximately 15% of those infected progress further into the moderate to severe phases. In these cases, the falling fever and remission of symptoms 2 to 5 days after onset are only transitory, and a deadly phase soon begins with renewal of malignant symptoms. This stage of the illness, called intoxication, is marked by the fever returning, and although the pulse remains slow, the blood pressure drops, with resultant renal failure. There may be oliguria, albuminuria, disseminated intravascular coagulopathy, backache, dizziness, ecchymoses, myocarditis, agitated delirium, intractable hiccups, seizures, coma, and multiple organ failure. In terminal cases, death usually transpires within 7 days of onset and is rare beyond 10 days of illness. In patients with intoxication (malignant yellow fever), a 20% to 60% mortality may be seen, with survival depending on the quality of supportive management. At autopsy, the kidneys, liver, heart, and spleen appear to be the organs most impacted by the disease. Complete blood count, urinalysis, liver function tests, coagulation studies, viral blood cultures, and serologic tests should be done. Leukopenia with relative neutropenia is common, as are thrombocytopenia, prolonged clotting, and increased prothrombin time. Bilirubin and aminotransferase levels may be elevated acutely and for several months. Diagnosis is confirmed by viral culture, serology, the identification of viral antigens and virus-specific immunoglobulin M (IgM) and neutralizing antibodies in serum by several rapid diagnostic methods, or detecting characteristic midzonal hepatocyte necrosis at autopsy. Needle biopsy of the liver during illness is contraindicated because of high risk of hemorrhage. Mild yellow fever appears clinically like a broad expanse of other infections presenting with similar symptoms, including dengue, viral hepatitis, malaria, typhus, Q fever, typhoid, Rift Valley fever, Yellow Fever leptospirosis, drug-induced syndromes, and toxic causes. Yellow fever may be distinguished from malaria by the findings of conjunctival suffusion or relative bradycardia. As well, a proton pump inhibitor, H2 blocker, and sucralfate (Carafate)1 can be helpful as prophylaxis for gastrointestinal bleeding and should be considered in all hospitalized patients. Avoidance of sedatives and drugs metabolized hepatically is prudent, and medication dosing should be adjusted in the face of declining renal function. Owing to the increased risk of bleeding, avoidance of aspirin and other nonsteroidal antiinflammatory drugs, such as naproxen and ibuprofen, is recommended. The mortality rates in tropical America range from 45% to 75%, compared with less than 30% in Africa. The convalescence of a yellow fever patient is usually prolonged and varies from patient to patient. Pertussis, or whooping cough, is an acute infectious disease caused by the bacterium Bordetella pertussis. Outbreaks of pertussis were first described in the 16th century, and the organism was first isolated in 1906. In 1932, an outbreak of whooping cough hit Atlanta, Georgia, and a pediatrician by the name of Leila Denmark began her study of the disease. In partnership with Emory University and Eli Lilly & Company, she developed the first pertussis vaccine. Despite generally high coverage with childhood pertussis vaccines, pertussis is one of the leading causes of vaccinepreventable deaths worldwide.
Diseases
- Sideroblastic anemia, autosomal
- Kozlowski Ouvrier syndrome
- Microgastria short stature diabetes
- Lymphosarcoma
- Hemangioma, capillary infantile
- Neuritis with brachial predilection
- Toxic conjunctivitis
- Keloids
Order ivermectin 3 mg free shipping
For example antibiotics for uti azithromycin purchase ivermectin 3 mg on-line, newborns tend to have high neutrophil count for several days, which then falls into the normal adult range by the first weeks of life. Some persons of African or Middle Eastern descent may typically have a neutrophil count <1000/mm3 with no apparent increased risk of infection. The most common cause of neutropenia in pediatric patients is viral infection; however, neutropenia in infants less than 6 months of age is often caused by autoimmune mechanisms. Persistent neutropenia found in children 1 year of age or more is often idiopathic but could represent an underlying genetic disorder. If a patient is otherwise asymptomatic, observation over a period of weeks with intermittent interrogation of neutrophil count is the preferred management, prior to embarking on a more extensive evaluation. Many drugs, particularly chemotherapy drugs, can cause myelosuppression, leading to neutropenia of variable severity and duration. Radiation exposure, either therapeutic or accidental, can also cause delayed reactions, but neutropenia and reversibility is related to dose and surface area exposed. A number of pharmaceutical agents are associated with idiopathic neutropenia, presumably immune related. Rare congenital disorders can be associated with long-term neutropenia, and most of these are identifiable at an early age. Neutropenia can also be caused by primary hematologic disorders such as leukemia, lymphoma, and myelodysplasia, where the etiology of neutropenia is caused either by ineffective myelopoiesis or infiltration by a malignant clone. Widely metastatic cancer, such as prostate or breast, can occasionally present with neutropenia due to extensive marrow replacement. Finally, splenomegaly from variable causes can produce neutropenia through sequestration. Important items include general questions regarding age and recent health including fevers, weight loss, and night sweats. The duration of these symptoms is critical, as neutropenia persisting over several months is likely to be pathological. Lightheadedness or dizziness or decreased exercise tolerance may indicate associated anemia. It is also valuable to ask about the existence of relatives with neutropenia or other blood disorder Interrogation regarding exposure to recent or remote infectious agents, various drugs, including both over-the-counter and prescription, and supplements is essential, as is inquiring about any previous history of neutropenia. Patients should be asked about any past medical history of cancer, or cancer chemotherapy and radiation therapy and previous surgery, particularly involving the gastrointestinal tract. Physical Examination Most patients with neutropenia will have a normal physical exam at the time their low counts are documented. However, certain patients may present with fever and weight loss, or other constitutional symptoms. The presence of pallor, bruising, and petechiae likely indicates a patient with pancytopenia. Patients should be asked about bowel habits and any rectal pain, discomfort, or discharge that could be related to perirectal abscess. Patients should be asked about any past similar or recurrent episodes and family history of any blood disorders. A detailed history of any drug exposures, including any chemotherapy agents, should be elicited. For patients on systemic anticancer therapy, it is useful to inquire if they have had similar problems and the severity of previous infections, including hospitalizations. Localized or systemic rash may suggest a viral exanthem, drug-mediated rash, or collagen vascular disease. The finding of adenopathy and splenomegaly may suggest an underlying hematologic disorder. It is important to recognize that neutropenic patients may be unable to form abscesses due to the fact that pus is composed of neutrophils. Laboratory examinations should include a complete blood count with a blood smear, the latter preferably reviewed by a hematologist or pathologist. Additional testing may be appropriate, including flow cytometry to look for abnormal lymphocytes, mutational analysis, and even bone marrow biopsy and aspirate. Antibiotic prophylaxis may also be considered in some of the congenital syndromes associated with prolonged neutropenia (see below). Because the simultaneous use of steroids in patients who are profoundly neutropenic significantly increases the risk of invasive fungal infections, any prolonged exposure to systemic corticosteroids should be avoided. Alternatively, patients with chronic neutropenia who must receive steroids are candidates for fungal prophylaxis. Patients presenting with signs of impending or current sepsis, such as fever, unexplained hypotension, and/or tachycardia, should be immediately evaluated, and appropriate interventions including blood and urine cultures and the institution of broadspectrum antibiotics must commence quickly to avoid serious complications. Studies have consistently shown that in this group of patients delay of institution of antibiotics is associated with an increased risk of mortality. The utility of tests such as procalcitonin in neutropenic patients to rule out infection is debatable. Aggressive management of the unstable neutropenic patient can truly be lifesaving. The routine use of growth factors for treatment of neutropenia with infection or sepsis is controversial and is not recommended. However, the prophylactic use of filgrastim or sargramostim (Leukine)1 in high-risk populations to maintain an adequate neutrophil count should be considered for some patients with chemotherapy- and other drug-induced neutropenia, as well as with high-risk cyclic neutropenia patients. Etiology Acquired Causes of Neutropenia Infectious Agents Infections are a common cause of transient neutropenia, particularly in children. In children, acute parvovirus B19 infection may cause neutropenia, although the classic presentation in adults is that of red cell aplasia. Bacterial pathogens are less likely to be associated with significant neutropenia, with the exception of mycobacteria, Rickettsia, and Brucella infections. Overwhelming bacterial sepsis can be associated with profound neutropenia, particularly in children and the elderly, and this is associated with a poor prognosis. The routine introduction of colony-stimulating factors while a patient is acutely ill is of unclear benefit. Drug-Induced Neutropenia One of the most common causes of neutropenia, particularly in adults, is drugs. Drug associated neutropenia seems to increase in incidence with aging, with most reported cases in patients over 65 years, and with a slight female predominance. The mechanism by which drugs cause neutropenia varies, and includes myelosuppression, hypersensitivity or autoimmune reactions, and specific suppression of neutrophil production. Some drugs such as penicillins or cephalosporins can cause neutropenia by acting as haptens. Neutropenia related to rituximab can be quite delayed and long lasting, persisting for weeks to months. Although assays to detect anti-neutrophil antibodies associated with drug exposure exist, their variable specificity and turnaround time limit their utility in making treatment decisions, and they are often expensive. Furthermore, there is a lack of consensus as to the appropriate assay that should be used. Patients with drug-related neutropenia can present with lymphadenopathy, mucocutaneous rash, and fever. The optimal management of such patients includes cessation of the suspecting agent, watching for recovery over days to weeks, and at times rechallenging to verify the association. Neutropenia related to anthracyclines or alkylating agents is caused by bone marrow suppression and therefore is often accompanied by anemia and thrombocytopenia. Among the many oral chemotherapy agents in common use that can be associated with neutropenia are capecitabine (Xeloda), sunitinib (Sutent), sorafenib (Nexavar), and lenalidomide (Revlimid). Several antiviral agents routinely cause neutropenia, including ganciclovir (Cytovene) and valganciclovir (Valcyte). Antipsychotic and anticonvulsant drugs rarely produce neutropenia, but patients receiving these agents should be periodically monitored. Clozapine (Clozaril) is one drug most often cited with neutropenia or agranulocytosis and therefore carries a black box warning. Neutropenia associated with fever has been seen in patients receiving valproic acid (Depakene).
Purchase genuine ivermectin line
Oral decongestants such as pseudoephedrine (Sudafed) have minimal effect on nasal congestion antibiotics you can give a cat generic ivermectin 3mg mastercard, and can result in systemic hypertension, anxiety, and difficulty sleeping. Nasal sprays containing vasoconstricting agents such as oxymetazoline (Afrin) can result in mild temporary relief of nasal obstruction. However, the use of these compounds for more than 3 or 4 days can result in rebound vasodilation and paradoxically increased rhinorrhea. Side effects of histamine use, primarily sedation and dry mouth, are commonly encountered. Antihistamines have also been found to be ineffective in relief of cough during colds. Rhinoviruses are the most commonly identified etiologic agents and cause illness year-round. Other common causative agents during winter months include influenza viruses and respiratory syncytial virus, and enteroviruses predominate in summer months. The parainfluenza viruses also commonly cause respiratory infection, particularly in autumn (type 1) and late spring or summer (type 3). Coronaviruses, metapneumoviruses, adenoviruses, and other agents are identified less often. Although each of these agents can cause a common cold, some viral infections are associated with characteristic patterns of respiratory disease. Influenza-Like Illness Common Colds Colds are the most common of the viral respiratory illnesses. Pharyngitis is usually the earliest sign of a cold, beginning a few days the influenza syndrome is defined as the abrupt onset of fever, headache, and striking degrees of malaise and prostration, often with intense myalgia. The principal cause is, of course, influenza virus, although infection with many other viruses can cause similar (although not as intense) symptoms. Influenza virus infection and influenza-like illness are best treated symptomatically, relying on rest, adequate intake of fluids and calories, and appropriate analgesic therapy. Positive outcomes from therapy with these agents are observed only when therapy is instituted within 48 hours after the onset of symptoms, and benefits are not striking. In recent years, resistance to M2 inhibitors has been commonly observed among circulating epidemic strains of influenza virus. Nasal congestion and clear or slightly cloudy rhinorrhea usually follow within 24 to 48 hours. Treatment with antibiotics is ineffective before this time, and they are ineffective especially in the absence of other clinical signs of ear and sinus infections. The most appropriate approach to treatment therefore entails rest, with adequate nutrition and hydration. They are effective in reducing fever and, perhaps more importantly in most colds, reducing malaise, headache, and pharyngitis. Vasoconstrictors have therefore been used extensively to attempt to reverse these symptoms. The propensity for these compounds to cause cardiac arrhythmias in the very young child has led to recommendations against their use in the first year or two of life. The release of histamine itself is not associated with fever, cough, or malaise, so effects on these symptoms would not be expected. Furthermore, nasal congestion and discharge may be more related to the release of kinins, and not histamine. Indeed, the administration of antihistamines in adults and, particularly, in children has not demonstrated strikingly positive results. Cough during colds is principally caused by secretions entering the airway (postnasal drip) and not by inflammation of the airway itself. Therefore, it is not surprising that cough suppressants, especially codeine, have little effect on cough induced by colds. Infants and young children can sustain six to eight such infections annually, and adults have an average of nearly two such infections per year. Respiratory symptoms can occur concurrently, but they might not be prominent features. The illness is generally self-limited, and most symptoms resolve over 4 or 5 days. Compounds referred to as M2 inhibitors such as amantadine (Symmetrel) and rimantadine (Flumadine) have been approved for therapy. More recently, inhibitors of the activity of influenza viral neuraminidase have been used in treatment and prevention of influenza Viral Respiratory Infections virus infection in adults and children. The first such compound released, zanamivir (Relenza), was administered by inhalation but was unpopular because of its irritating effects on the airway. An oral compound, oseltamivir (TamiFlu), has been used to prevent and to treat influenza virus infection. As with M2 inhibitors, it is believed that treatment should be started within the first 48 hours of symptoms and that prophylaxis should be instituted within 48 hours of exposure. Treatment with oseltamivir shortens the duration of subsequent illness by only about 24 hours. Treatment can prevent some of the complications of influenza infection, including pneumonia. The drug may be more effective as a therapeutic agent, because it may be up to 90% effective in preventing culture-positive symptomatic influenza illness. In children, the appropriate dose based on body weight is 30 mg twice daily for children weighing less than 15 kg, 45 mg twice daily for children weighing 15 to 23 kg, 60 mg twice daily for children weighing 23 to 40 kg, and 75 mg twice daily for children weighing more than 40 kg. The principal side effect is nausea, which can be reduced by taking the drug with food. At the time of this writing, both this epidemic H1N1 strain as well as the seasonal influenza A/H3N2 and type B strains continue to circulate in the world. The considerable majority of these epidemic and seasonal strains continue to show sensitivity to oseltamivir, while most are resistant to M2 inhibitors. Contrasting with asthma, obstruction of the airway in bronchiolitis is a result of plugging of bronchioles with detached epithelium and inflammatory cells. Also in contrast with asthma is the absence of a sustained response to bronchodilators and corticosteroids among infants with bronchiolitis. Therapy of bronchiolitis primarily consists of administration of supplemental oxygen and replacement of fluid deficits as needed. The compound is quite expensive and must be delivered via a special aerosol generator. Infants who may be considered candidates for therapy include those with chronic lung disease, those born prematurely, and those with hemodynamically significant congenital heart disease. Airway obstruction in croup is caused by constriction in the subglottic area, often noted on radiographs by a steeple-shaped narrowing of the air column in this region. Parainfluenza virus type 1 is the primary cause of croup, although infection with many different viruses can produce this illness, and influenza virus can cause a particularly severe form of croup. Bacterial secondary infection occurs uncommonly, but it can result in fever and severe obstruction of the airway. Croup Bronchiolitis Bronchiolitis represents the most common cause for hospitalization of infants in developed countries. Infants present with a history of several days of upper respiratory symptoms, followed by the rapid onset of wheezing and labored breathing. Older studies have implicated Klebsiella pneumoniae, although recent data have not borne this out. Recent data from the National Health and Nutrition Examination Survey have estimated the prevalence of axial spondyloarthritis to occur in more than one percent of the U. This pain is classically characterized as a dull pain in the low back or in the buttocks and hips that begins before the age of 40 years, has an insidious onset, and lasts longer than 3 months. This limitation of motion is initially the result of axial inflammation and muscle spasm but is contributed to over time by ossification of the ligamentous structures and ultimately bony fusion of the sacroiliac joints, apophyseal joints, and the outer fibers of the annulus fibrosis of the intervertebral disks.
Cheap 3mg ivermectin visa
Doxycycline combined with rifampin1 for a full 6-week course is a commonly used therapy recommended by the World Health Organization infection vre order ivermectin once a day. It is considered the most effective regimen, particularly when combined with an aminoglycoside. In patients with spondylitis or sacroiliitis, doxycycline plus streptomycin is an effective combination. For pediatric patients older than 8 years, doxycycline plus gentamicin1 is the recommended therapy. Once brucellosis is diagnosed, immediate therapy is critical because it can alleviate symptoms and also prevent the development of complications. Depending on the severity or complications of the illness and the treatment time applied, the recovery time can last from several weeks to several months. Because relapse is indicated by the recurrence of a positive blood culture result during the post-therapy period or signs and symptoms of brucellosis infection, routine examination of the patient includes serum culture for Brucella organism and assessment for brucellosis symptoms after the treatment phase. Generally, brucellosis patients should be followed up clinically for up to 2 years to detect relapse. IgG antibody should be checked by serum agglutination test for levels that remain in the diagnostic range for more than 2 years. Centers for Disease Control and Prevention: Sexually Transmitted Diseases Treatment Guidelines, 2010: Epididymitis, 2012. Spondylitis caused by brucellae is characterized by joint inflammation between the vertebrae bones of the spine or between the spine and pelvis. Young patients tend to have cutaneous, hematologic, and respiratory complications. In addition to monitoring brucellosis symptoms, both doctors and patients should monitor any adverse effects of medication. In these regards, education is beneficial for preventing infection by this pathogen. People who handle animals or animal products should wear personal protective equipment, including glasses, rubber gloves, and clothing to protect skin and eyes from exposure or direct contact. Animal immunization programs must be maintained all over the world to cut off the transmission chain from livestock to humans. In addition, primary care physicians should be familiar with the clinical and laboratory findings of brucellosis symptoms and complications. References Complications 526 Brucellae are transported into the lymphatic system and can replicate in spleen, liver, kidney, breast tissue, and joints to cause both localized and systemic infections. Owing to the low virulence, low toxicity, and multiple mechanisms to protect them from the immune system, brucellae can survive and reproduce in nearly any tissues or organs. At 1 year after infection, the disease can develop into chronic brucellosis that can further cause one or multiple complications in one organ or the whole body. Middle-aged patients tend to develop genitourinary, neurologic, and gastrointestinal complications. Prevention Maintaining hygienic habits is very important for avoiding Brucella infection. Like Yersinia, Campylobacter infection can mimic acute appendicitis (ileocecitis), especially if this occurs in the absence of significant diarrhea. Computed tomography or ultrasound scanning in bacterial pseudoappendicitis usually documents mesenteric adenitis, and surgery can be avoided. In young children, seizures can occur before the onset of diarrhea and fever, and dysenteric illness (50%) is more common. Epidemiology Campylobacter enteritis is one of the most common forms of bacterial diarrhea in the world and the most common food-related illness in North America. Most cases (95%) are caused by Campylobacter jejuni, a commensal gram-negative bacteria found in the gut of animals, particularly poultry. The related Campylobacter coli causes a clinically identical but much less common (5%) infection. Foodborne outbreaks affect adults in developed counties, as well as travelers to developing nations. Most infections are due to crosscontamination of food with raw poultry (unwashed cutting boards) or from drinking unpasteurized milk or contaminated water. After recovery, the bacteria are excreted in the feces for several weeks and may be transmitted by improper hand washing, although person-to-person transmission is unusual. Diagnosis Most cases are diagnosed by stool culture in the setting of acute diarrhea and crampy abdominal pain. On microscopic examination, C jejuni is a gram-negative, spiral-shaped rod with a single polar flagellum at one or both ends. It can be isolated in culture media containing cephalothin, to which it is usually resistant. Darkfield microscopic stool examination is occasionally attempted for early diagnosis, but this is not very sensitive. Polymerase chain reaction analysis of stool samples is a very promising diagnostic approach, although it is not yet available in many laboratories. Later diagnosis, subsequent to resolution of diarrhea, requires serologic testing. Differential Diagnosis Campylobacter infections are clinically indistinguishable from other bacterial enteritides such as salmonellosis and shigellosis. However, Campylobacter colitis is more likely to mimic inflammatory bowel disease and appendicitis and later to cause Guillain-Barr e syndrome. Most cases of Campylobacter infection are mild and self-limited, and antibiotics are not required. If antibiotics are to be used, they are most effective if given early to high-risk patients, because delayed treatment. First-line choices include macrolides, such as azithromycin (<5% resistance), or fluoroquinolones, such as ciprofloxacin (Cipro). Azithromycin has supplanted erythromycin (Ery-Tab)1 because it is better tolerated and has fewer gastrointestinal side effects. Rarely, intravenous aminoglycosides or carbapenems are necessary in very ill patients unable to take oral medication. The widespread practice of using antibiotics, especially fluoroquinolones (enrofloxacin [Baytril]),2 as additives to chicken feed has resulted in increasing quinolone resistance in Campylobacter strains found in poultry, the major source of infection. A newer strategy involves supplementing poultry feed with bacteriocins, nontoxic antimicrobial peptides, to reduce Campylobacter colonization. One or two doses of antibiotics are usually sufficient to abort symptoms, and prolonged treatment is usually unnecessary. Loperamide (Imodium) might help control diarrhea in adults, but it should be avoided in dysenteric illness and in young children. Improperly cooked poultry or food contaminated by raw poultry is the most common source. A 17-state outbreak of multidrug-resistant Campylobacter was linked to pet store puppies in 2017. Elderly, immunocompromised, or very young patients are at additional risk for prolonged symptoms, invasive disease, and hospitalization. Proton-pump inhibitors, by reducing protective stomach acid, appear to increase the risk of campylobacteriosis and other bacterial enteritides. Symptoms can begin with enteritis (profuse watery stools) or with frank colitis (bloody stools). Inflammatory bowel disease may be excluded by colon biopsies, which demonstrate acute but not chronic inflammatory change.
Buy ivermectin with a mastercard
Official statistics suggest the incidence of yellow fever fluctuates antibiotic resistance is caused by buy discount ivermectin 3mg on-line, with 90% of the 200,000 annual cases reported in Africa. Most deaths occur in infants who are either unvaccinated or incompletely vaccinated. The year 2012 was the peak year in which there were more than 48,000 reported cases in the United States, which drew the attention of the public health community. The other viral hemorrhagic fevers, which include dengue, Lassa fever, Marburg disease, Ebola, Crimean-Congo hemorrhagic fever, and Bolivian and Argentine hemorrhagic fevers, usually present without jaundice. As well, albuminuria is a reliable hallmark of yellow fever that allows its differentiation from other causes of viral hepatitis. Transfusions of blood, fresh-frozen plasma, and vitamin K1 may be utilized with hemorrhagic symptoms. Antibiotic therapy for secondary bacterial sepsis is often necessary during the recovery period. This difference suggests genetic factors play a role in the course of the illness, as well as the viral strain. Although uncommon, late death (weeks after the acute illness) can occur as a result of cardiac complications or renal failure. Profound asthenia and fatigue usually last for 1 to 2 weeks, but in some cases can last many months. Jaundice and the elevation of liver enzymes have been known to last an extended period (several months) during convalescence. In the 20th century, pertussis was one of the most common childhood diseases and a major cause of childhood mortality in the United States. Before the availability of the pertussis vaccine in the 1940s, more than 200,000 cases of pertussis were reported annually. Since widespread use of the vaccine began, incidence has decreased more than 80% compared with the prevaccine era. References Worldwide, it is estimated that there are about 16 million pertussis (whooping cough) cases and about 195,000 pertussis deaths in children per year. Transmission most commonly occurs by the respiratory route through aerosolized respiratory droplets or by direct contact with airborne droplets of respiratory secretions. Transmission occurs less frequently by contact with freshly contaminated articles of an infected person as the bacteria cannot not survive long outside of the reservoir. Persons with pertussis are most infectious during the catarrhal period and the first 2 weeks after cough onset. These products are responsible for the clinical features of pertussis disease, and an immune response to one or more produces immunity following infection. During the first 1 or 2 weeks of this stage, the attacks increase in frequency and severity, remain at the same level for 2 to 3 weeks, and then gradually decrease. The paroxysmal stage usually lasts 1 to 6 weeks but may persist for up to 10 weeks. However, paroxysms often recur with subsequent respiratory infections for many months. The bacteria attach to the cilia of the respiratory epithelial cells, causing inflammation, and produce toxins that paralyze the cilia, which interferes with the clearing of pulmonary secretions. Filamentous Hemagglutinin* this large surface protein can participate in the interaction of B. Fimbriae* these surface appendages, similar to those in other bacteria, function as adhesins and make up several of the agglutinogens, which are used for Bordetella serotyping. Tracheal Cytotoxin the cytotoxin kills respiratory epithelial cells by a mechanism involving intracellular interleukin-1 and nitric oxide. Complications the most common complication and the cause of most pertussisrelated deaths is secondary bacterial pneumonia. Young infants are at highest risk for acquiring pertussis-associated complications. Neurologic complications such as seizures and encephalopathy may occur as a result of hypoxia or possibly from the toxin itself. Other less serious complications of pertussis include otitis media, anorexia, and dehydration. Complications resulting from pressure effects of severe paroxysms include pneumothorax, epistaxis, subdural hematomas, hernias, and rectal prolapse. Prognosis Most healthy older children and adults fully recover, but those with comorbid conditions have a higher risk of morbidity and mortality. First-year infants are also more likely to develop complications, such as pneumonia (20%), encephalopathy (0. Diagnosis Clinical Features the whole clinical course of the illness can typically last from 30 to 90 days and is divided into three stages. The incubation period of pertussis is commonly 7 to 10 days but can range anywhere from 4 to 21 days. The first stage, the catarrhal stage, is similar to the symptoms of the common cold, which makes early diagnosis difficult. It is characterized by sneezing, low-grade fever, rhinitis, and a mild, occasional cough. This cough gradually becomes more severe over 1 to 2 weeks, which transitions to the second, or paroxysmal, stage. It is during the paroxysmal stage that the diagnosis of pertussis is usually suspected. Due to the length and force of the paroxysm, a long deep inspiratory effort is usually accompanied by a distinguishing high-pitched "whoop. An elevated white blood cell count with a lymphocytosis is usually present in classical disease of infants. Chest radiographs may show peribronchial consolidation, interstitial edema, or variable atelectasis, all of which are non-specific. Culture is considered the gold standard laboratory test and is the most specific of the laboratory tests for pertussis. As with any sample, the yield of culture can be affected by specimen collection, transportation, and isolation techniques. Successful culture rates are highest during the first 2 weeks of illness (catarrhal and early paroxysmal stages). Since adolescents and adults have often been coughing for several weeks before they seek medical attention, it is often too late for culture to be useful. Results should be interpreted along with the clinical symptoms and epidemiologic information. If treatment for pertussis is started early in the course of illness, during the first 1 to 2 weeks before coughing paroxysms occur, symptoms may be Whooping Cough (Pertussis) lessened. Clinicians should strongly consider treating prior to receiving test results if clinical history is strongly suggestive or the patient is at risk for severe or complicated disease. If the patient is diagnosed late, antibiotics will likely not alter the course of the illness, but they will help to eradicate the organism from secretions, thereby decreasing communicability. In 1947, researchers at the East African Research Institute in Entebbe, Uganda, were studying yellow fever and placed a caged rhesus macaque in the nearby Zika Forest. The monkey developed a fever and from its serum was isolated a transmissible agent that was first described as Zika virus in 1952. Millennia ago, North African villagers began storing water in their dwellings, giving arboreal A. Now, thousands of years later, the worst effects of this evolutionary cascade are being seen in the repeated emergence of arboviruses in human ecosystems. There is insufficient evidence to determine the effectiveness of antibiotics in those who have been exposed but are without symptoms. Preventive antibiotics, however, are still frequently used in those who have been exposed and are at high risk of severe disease (such as infants). Atkinson W: Pertussis epidemiology and prevention of vaccine-preventable diseases. Initially, Zika virus, borne by arboreal mosquitoes such as Aedes africanus, infected wild primates and rarely infected humans, even in highly enzootic areas. From its discovery until 2007, there were only 14 confirmed human cases of Zika virus infection, the vertebrate life cycle primarily involving monkey-mosquito-monkey, with rare spread to humans. The Zika virus appears to have mutated in character while expanding its geographical range, transforming from a localized endemic, mosquitoborne infection producing only a mild illness to a disease causing explosive outbreaks linked with neurological disorders including Guillain-Barr syndrome and microcephaly.