600 mg myambutol mastercard
Women diagnosed with this condition should be counseled regarding which of the following Risk factors for developing this condition include all of the following except: a antibiotics questions cheap myambutol line. Assuming that additional testing was performed, which of the following results would you most likely expect to find Diagnostic testing is not reliable and treatment should be based on clinical suspicion 3. She recently tried an over-the-counter antifungal treatment A answers Vignette 1 Question 4 Answer C: Because of the high rate of concomitant Trichomonas infections in sexual partners, all partners should be treated to prevent reinfection. This is likely due to the high efficacy of nitroimidazole drugs, with a 90% to 95% cure rate. Empiric treatment for chlamydial infection is not recommended with the diagnosis of Trichomonas infections. Vignette 1 Question 5 Answer B: Metronidazole 500 mg orally twice a day for 7 days is recommended for cases of metronidazole single-dose treatment failure. Treatment with tinidazole 2 g orally daily for 5 days is recommended after treatment failure with both the single-dose and the multidose metronidazole regimens. Consultation with infectious disease specialist is recommended only for refractory cases after multiple treatment failures. Nitroimidazoles are the only class of drugs useful for the treatment of Trichomonas infections. Pap smears should begin at 21 years of age regardless of age at first intercourse. A pelvic ultrasound is not indicated based on lack of current symptoms and physical examination findings. A diagnosis of chlamydial infection or gonorrhea should be made prior to treatment. Vaginal cultures are typically not a useful diagnostic tool because they are nonspecific. Vaginal cultures can be useful if yeast or trichomoniasis is suspected and microscopy is normal. The sensitivity of Gram stain to the diagnosis of chlamydial infection or gonorrhea is low. In addition, the patient Vignette 1 Question 1 Answer D: the symptoms and findings are most consistent with Trichomonas. Symptomatic patients report a frothy vaginal discharge that may be yellow, gray, or green. The classical cervical findings include erythematous, punctate epithelial papillae, or "strawberry" appearance. Symptoms include vaginal burning, pruritus, and increased thick, white, curdy vaginal discharge. Multinucleated giant cells can be seen on Tzanck smear preparation of herpetic lesions. Vignette 1 Question 2 Answer C: Trichomoniasis is caused by Trichomonas vaginalis. Vignette 1 Question 3 Answer A: A single-dose regimen with metronidazole or tinidazole is the mainstay treatment of trichomoniasis. An alternative multidose regimen is metronidazole 500 mg orally twice daily for 7 days. Clindamycin can be used as an alternative regimen for the treatment of bacterial vaginosis. Metronidazole gel is considerable less efficacious for the treatment of trichomoniasis. The use of topical antimicrobial preparation is unlikely to achieve therapeutic levels in the perivaginal glands and is not recommended. Finally, the diagnosis of genital herpes should not be based on clinical suspicion. Up to 20% of at-risk women with findings compatible with herpetic lesions will not have genital herpes. Vignette 3 Question 3 Answer C: For primary genital herpes infections, acyclovir 200 mg orally five times daily for 7 to 10 days is recommended to reduce the length of infection and the length of time a patient has viral shedding. Other options include a 7 to 10 day oral treatment with acyclovir 400 mg three times per day, famciclovir 250 mg three times per day, or valacyclovir 1 g twice per day. Extended regimens of doxycycline can be used to treat lymphogranuloma venereum caused by C. Vignette 3 Question 4 Answer D: Viral shedding can occur both with and without genital herpes symptoms. It is important to counsel patients that they can transmit the virus even if they are asymptomatic. Subclinical viral shedding appears to be highest in the first 6 months following acquisition and is more common immediately before and after a clinical outbreak. Condom use can reduce the risk of transmission of genital herpes, but will not prevent the transmission. Both symptomatic and asymptomatic viral shedding can occur in genital areas not covered or protected by a condom. Recurrent outbreaks can be reduced through the use of daily suppressive antiviral drugs. Cesarean delivery is recommended only for those pregnant patients with active genital lesions or prodromal symptoms. With this shift in vaginal flora, there is an accompanied decrease in lactobacilli. Patients usually complain of an increased vaginal discharge that often has a malodorous fishy amine odor. Alternatives include clindamycin 300 mg twice a day for 7 days or topical formulations of these antibiotics. Azithromycin 1 g orally once is also the correct treatment option for chlamydial infection. Unless chlamydial co-infection has been ruled out, patients diagnosed with gonorrhea should be empirically treated for chlamydial infection with ceftriaxone and azithromycin. Doxycycline 100 mg orally twice daily for 7 days is the correct treatment for chlamydial infection. Because of increasing resistance, fluoroquinolones are no longer recommended in the United States for the treatment of gonorrhea. Vignette 3 Question 1 Answer B: Genital herpes classically presents with painful clusters of small vesicles and ulcers. Moreover, primary infections usually begin with flulike symptoms including malaise, myalgias, nausea, diarrhea, and fever. Primary syphilis is characterized by a nontender, red, round, firm ulcer approximately 1 cm in size with raised edges, known as a chancre. The vesicles described in this case are different than that typically seen in primary syphilis. The lesion presents initially as an erythematous papule, which evolves to a pustule and ulcer. The ulcer is painful with an erythematous base and irregular, well-demarcated borders. Vignette 3 Question 2 Answer D: A definitive diagnosis of genital herpes should be made through viral or serology testing. On the other hand, empiric treatment of chlamydial infection is recommended in patients infected with N. It is often a polymicrobial infection with a variety of pathogens, including skin and gastrointestinal flora in addition to the usual flora colonizing the lower reproductive tract. Mycobacterium tuberculosis is a rare cause of chronic endometritis in developed countries but is a leading cause of infertility in endemic countries. Chronic endometritis can be suspected in patients with chronic irregular bleeding, discharge, and pelvic pain. The diagnosis can be made in a nonpuerperal patient with endometrial biopsy showing plasma cells. Although defenses such as ciliary movement creating flow and cervical mucus exist, there is essentially an open tract between the vagina, the pelvis, and abdomen. This can lead to ascending infections of the uterus, fallopian tubes, adnexa, pelvis, and abdomen.
Basking Shark Liver Oil (Shark Liver Oil). Myambutol.
- Are there safety concerns?
- Leukemia and other cancers, side effects of cancer treatment, common cold, flu, skin problems, and other conditions.
- How does Shark Liver Oil work?
- Dosing considerations for Shark Liver Oil.
- What is Shark Liver Oil?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96919
Order discount myambutol online
Ampicillin can also be added to this regimen to increase coverage for grampositive bacteria bacteria candida purchase myambutol on line. Ampicillin can also be added to this regimen to increase coverage for gram-positive bacteria. Vignette 4 Question 4 Answer A: this patient has a clinical picture concerning for a ruptured tubo-ovarian abscess. Consulting infectious disease specialist is not appropriate in a potentially unstable patient. Doxycycline 100 mg orally twice daily for 14 days is the treatment regimen for chronic endometritis. For those patients with a cephalosporin allergy, clindamycin can be used with gentamicin. Invasive procedures including artificial rupture of membranes and use of fetal scalp electrodes should be avoided. Women with a viral load greater than 1,000 copies/mL should be offered and recommended a cesarean section. Damage to any one of these structures can potentially result in a weakening or loss of support to the pelvic organs. Damage to the anterior vaginal wall pubocervical fascia can result in herniation of the bladder (cystocele) and/or urethra (urethrocele) into the vaginal lumen. Injuries to the endopelvic fascia of the rectovaginal septum in the posterior vaginal wall can result in herniation of the rectum (rectocele) into the vaginal lumen. Injury or stretching of the uterosacral and cardinal ligaments can result in descensus, or prolapse, of the uterus (uterine prolapse). Pelvic organ prolapse presents with a variety of symptoms including pelvic pressure and discomfort, dyspareunia, difficulty evacuating the bowels and bladder, and low back discomfort. These clinical symptoms are often associated with a visible or palpable bulge in the vagina. This increase is attributed to decreased endogenous estrogen, the effects of gravity over time, and normal aging in the setting of previous pregnancy and vaginal delivery. Atrophy is associated with compromised elasticity, diminished vascular support, and laxity in structural elements. Tissues become less resilient to forces of gravity and increased intraabdominal pressure, and accumulative stresses on the pelvic support system take effect. The reported prevalence of pelvic organ prolapse in population-based surveys ranges from 2. Population-based surgical intervention studies report a higher prevalence of symptomatic prolapse quoting an 11% to 19% lifetime risk for undergoing surgery. Previous studies have asserted that lower rates of prolapse are seen in African American women compared to Caucasian women, but this has not been consistently demonstrated in the literature. Obstructed defecation Constipation Painful defecation Incomplete defecation Splintinga a Placing fingers in or around the vagina/perineum to aid in defecation. The incidence of pelvic relaxation increases four- and eightfold with the first two vaginal deliveries, respectively. Obstructed labor and traumatic delivery are also risk factors for pelvic organ prolapse as are conditions that result in chronically elevated intra-abdominal pressure. Additionally, a surgical history of hysterectomy is associated with an increase in apical prolapse. Some patients perform a maneuver known as "splinting" to aid in evacuation of stool. This refers to the application of manual pressure (usually by a finger) to the perineum or posterior vaginal wall. Although dyspareunia and pelvic pain are usually not attributable to prolapse per se, sexual dysfunction can occur as a consequence of embarrassment or fear of discomfort. These symptoms can impact daily activities, and can have a detrimental impact on body image and sexuality. With small degrees of pelvic relaxation, patients are often asymptomatic; however, prolapse severity and symptoms are not always well-correlated. When symptomatic, patients often complain of pelvic pressure, heaviness in the lower abdomen, or a vaginal bulge that may worsen at night or become aggravated by prolonged standing, vigorous activity, or lifting heavy objects. Women with prolapse often experience concurrent urinary dysfunction with complaints ranging from incomplete bladder emptying and obstructed voiding to overactive bladder. Paradoxically, stress incontinence can appear to "improve" as the prolapse worsens. As the support for the anterior vaginal wall weakens and the bladder descends, a kink is introduced Pelvic relaxation is best observed by separating the labia and viewing the vagina while the patient strains or coughs. A splitspeculum examination should be performed by using a Sims speculum or the lower half of a Grave speculum to provide better visualization of the anterior vaginal wall, posterior vaginal wall, and apex individually. Using this method, the speculum is used to retract the posterior vaginal wall and a cystocele may cause a downward movement of the anterior vaginal wall when the patient strains. Similarly, rectoceles and enteroceles result in an upward bulging of the posterior vaginal wall when the patient strains with the split speculum placed upside down retracting the anterior vaginal wall. This laxity in the rectovaginal wall can also be demonstrated on rectal examination. A prolapsed uterus can also be viewed on split-speculum examination or by bimanual pelvic examination. Complete procidentia refers to complete eversion of the vagina with the entire uterus prolapsing outside the vagina (Color Plate 11). The examination is conducted with the patient straining in order to record maximum descent. It provides a standardized means for documenting, comparing, and communicating clinical findings of pelvic organ prolapse that focuses on the physical extent of the vaginal wall prolapse, and not on which organ is presumed to be prolapsing within that defect. It is usually caused by an acquired defect in the anterior endopelvic fascial anatomy. Other tools that may be useful in the diagnosis and preoperative evaluation of cystoceles and urethroceles include urine cultures, cystoscopy, urethroscopy, and urodynamic studies, if indicated. When a rectocele is suspected from a history of chronic constipation and difficulty passing stool, obstructive lesions should be ruled out using anoscopy or sigmoidoscopy. A defecography study (similar to a barium enema) may also help to show a rectocele or enterocele but is not essential to diagnosis. Many clinicians formerly use the Baden-Walker Halfway Scoring System for quantifying pelvic organ prolapse. It is usually caused by an acquired defect in the posterior endopelvic fascial anatomy. In general, grade 1 is given to a defect that descends at least half-way to the hymenal ring. When a rectocele is suspected, obstructive lesions of the colon and rectum (lipomas, fibromas, sarcomas) should be investigated. Cervical elongation, prolapsed cervical polyp, prolapsed uterine fibroid, and prolapsed cervical and endometrial tumors may be mistaken for uterine prolapse as can lower uterine segment fibroids. Thus, asymptomatic prolapse can be monitored but does not require any further treatment and expectant management is acceptable. For those patients who have significant bother from her prolapse symptoms, intervention is appropriate. Regardless of the etiology, symptomatic pelvic organ prolapse is essentially a structural problem and therefore requires therapies that reinforce the lost support to the pelvis. Conservative modalities begin with exercises to strengthen the pelvic floor musculature (Kegel exercises). Mechanical support devices (pessaries) may be used to manage prolapse and the associated symptoms, or the defect may be repaired surgically. In postmenopausal women, low-dose vaginal estrogen can be an important supplemental treatment, improving tissue tone and facilitating reversal of atrophic changes in the vaginal mucosa. In motivated patients with mild symptoms, a first-line therapy involves the use of Kegel exercises to strengthen the pelvic musculature. These exercises involve the tightening and releasing of the levator ani muscles repeatedly to strengthen the muscles and improve pelvic support. Although these may play a protective role in the prevention of prolapse, the available literature does not support the notion that these measures reverse or treat existing symptomatic prolapse. Pessaries act as mechanical support devices to replace the lost structural integrity of the pelvis and to diffuse the forces of descent over a wider area.
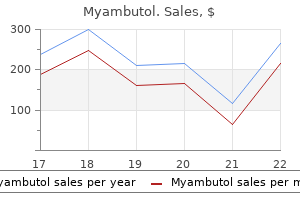
Myambutol 600 mg with mastercard
Arthroplasty should be available in the physiologically older and lower-demand patient antibiotic resistant germs order myambutol with visa, with a view to converting the decision to an acute arthroplasty if the osteosynthesis potential is tenuous. Careful dissection of the nerve from the cubital tunnel restraints will allow freedom to move the nerve without risking traction injury during the remainder of the procedure. During a tendon-splitting approach, the distal triceps tendon should be split within the structure of the tendon and should not involve the muscular belly. Inspection A thorough inspection of the ulna and radial articular surface should be performed to investigate the possibility of a hemiarthroplasty replacement in the appropriately selected younger patient. The surgeon should observe the state of the ulnar nerve and muscles around the elbow (especially triceps and brachialis); this will help to explain altered nerve function in the former, and weakness and possible myositis ossificans and stiffness in the latter. Bone preparation Implantation If the humeral columns are intact, then an attempt at preservation should be made, with their extensor and flexor mass attachments, during a total elbow replacement. When planning length and implantation, the surgeon should pay careful attention to the tension and lever arms of the main motor drivers; the brachialis and triceps need some tension to function well, but if over-tensioned the elbow will be stiff and if under-tensioned the elbow will be weak. Drains should not be used because of the superficial nature of the elbow and the risk of deep infection. However, the surgeon should pay close attention to hemostasis, and for the first 12 hours a moderately tight bandage should be used to avoid hematoma formation. With triceps reattachment, the surgeon should be cautious to avoid overzealous rehabilitation for fear of compromising triceps healing, with subsequent avulsions or extension weakness. The arm is elevated on pillows or with a Bradford sling overnight to prevent edema. Nonsteroidal anti-inflammatories are avoided because of their detrimental effects on tissue healing (bone to tendon and bone to bone). On the second day after surgery the dressing is removed and the compliant patient should commence gentle active antigravity flexion, with passive gravity-assisted extension. Graduated and targeted motion is prescribed, with greater than 90 degrees of elbow flexion attempted after 5 weeks. This allows sufficient time for the triceps to adhere and heal (incompletely) to the ulna. Always, at each patient interaction, the surgeon should reiterate the restrictions of use with an elbow arthroplasty: limited internal (varus) and external (valgus) rotatory torques, 2-pound repetitive and 10-pound single-event lifting. Ray et al14 reported 5 excellent and 2 good functional results in a group of patients with an average age of 81 years at 2 to 4 years of follow-up. Gambirasio et al5 reported excellent functional results in a cohort of 10 elderly patients with osteoporotic intra-articular fractures. All 12 acute primary elbow replacements achieved excellent (n 11) or good (n 1) results. Lee et al10 reported seven acute elbow replacements for distal humeral fractures in patients with an average age of 73 years. Total elbow arthroplasty as primary treatment for distal humeral fractures in elderly patients. A comparison of open reduction and internal fixation and primary total elbow arthroplasty in the treatment of intraarticular fractures of the distal humerus in women older than 65 years. A comparison of open reduction and internal fixation and primary total elbow arthroplasty in the treatment of intraarticular distal humerus fractures in women older than age 65. Total elbow replacement for complex fractures of the distal humerus: an option for the elderly patient. Untreated median-nerve entrapment in bone after fracture of the distal end of the humerus: postmortem findings after forty-seven years. The results of open reduction and internal fixation in elderly patients with severe fractures of the distal humerus: a critical analysis of the results. Distal humeral fractures treated with noncustom total elbow replacement: surgical technique. Results of total elbow arthroplasty in the treatment of distal humerus fractures in elderly Asian patients. Operative treatment of type C intercondylar fractures of the distal humerus: results after a mean followup of 2 years in a series of 18 patients. Elbow hemiarthroplasty for acute and salvage reconstruction of intra-articular distal humerus fractures. Surgical treatment of comminuted intraarticular fractures of the distal humerus with double tension band osteosynthesis. Chapter 47 Management of Primary Degenerative Arthritis of the Elbow: Linkable Total Elbow Replacement Bassem Elhassan, Matthew L. These changes in the radiohumeral and ulnohumeral joints lead to the loss and fragmentation of the cartilaginous joint surfaces with distortion, cyst formation, and bone sclerosis. Suvarna and Stanley30 reported on the progressive fibrosis of the local marrow, increased thickness of all the bony components of the olecranon fossa, and increases in anterior and posterior fibrous tissues. Characteristic manifestations of primary degenerative arthritis of the elbow are well described. It is generally believed that overuse plays a key role in the onset of the disease process. However, younger patients with this disease often have predisposing conditions such as osteochondritis dissecans. The anterior and posterior involvement of this joint is usually manifested by fibrosis of the anterior capsule in the form of a cord-like band and hypertrophy of the olecranon. Osteophytes are seen over the olecranon, especially medially, the coronoid process, and the coronoid fossa. Ulnar neuropathy Medial joint pain in patients with advanced osteoarthritis of the elbow might be the first manifestation of ulnar neuropathy. Up to 20% of patients with primary osteoarthritis of the elbow have some degree of ulnar neuropathy. The expansion of the capsule as a result of synovitis and the presence of osteophytes in that area of the joint result in direct compression and ischemia of the ulnar nerve. Acute onset of cubital tunnel syndrome in patients with osteoarthritis of the elbow might be also the first manifestation of a medial elbow ganglion. This could lead to disability in this patient population as well in the older laborers who extensively use their upper extremity. Involvement of the proximal radioulnar and radiohumeral joint later in the disease process may limit forearm rotation. Forced motion at the extremes of flexion and extension will often cause pain, particularly in extension. A cubital tunnel view is obtained if there is ulnar nerve irritation to look for impinging osteophytes or loose bodies. Range of motion the flexion-extension arc will demonstrate loss of extension greater than flexion and will average about 30 to 120 degrees. Anteroposterior and lateral views of a right osteoarthritic elbow show narrowing of the joint line and subchondral sclerosis, with formation of osteophytes in the coronoid, capitellar, and olecranon fossae. Computed tomography of the elbow demonstrating marginal osteophytes on the ulna and olecranon fossa. Three-dimensional reconstructions provide additional detail on osteophytic deformity and facilitate preoperative planning of removal. Early in the course of the disease, treatment by nonsurgical measures should be followed. Contraindications to arthroscopic treatment include altered neurovascular anatomy, limited surgical expertise, and advanced involvement of the ulnohumeral joint. Several surgical options exist for the management of primary degenerative arthritis of the elbow. Surgery is directed toward addressing the pathology contributing to the predominant complaints of the patient.
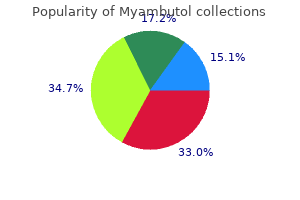
600 mg myambutol with mastercard
This is usually only reserved for workup of infertility or to confirm tubal occlusion following permanent sterilization antibiotic lock protocol 400 mg myambutol with visa. Vignette 2 Question 2 Answer E: Opioid agonists are narcotic medications used to treat pain. These have no role in the treatment of heavy bleeding in women with uterine fibroids. Nonsteroidal anti-inflammatory drugs reduce levels of prostaglandin, which are produced by the uterus during menses and cause uterine contractions that augment pain from the fibroids. These are commonly used to treat dysmenorrhea associated with menses in women with and without uterine fibroids. Vignette 2 Question 3 Answer A: Several mechanisms of fibroid induced menorrhagia have been described. It is well-known that submucosal fibroids can mechanically distort the endometrial lining, prohibiting it from building an organized endometrial layer. Other effects could be related to altered vascular growth due to expression of angiogenic growth factors by the fibroids themselves. Intramural fibroids involve the myometrial layer of the uterus and the most common symptom is dysmenorrhea. Subserosal fibroids are on the surface of the uterus and typically are asymptomatic. Parasitic fibroids are pedunculated off of the uterine serosa and grow within the peritoneal cavity. They recruit additional blood supply from nearby organs, but do not directly affect endometrial blood flow. All of the different types of fibroids can cause pressure and pain symptoms if their sizes are significantly increased and result in mass effect in the pelvis. Vignette 2 Question 4 Answer B: Uterine fibroids are more commonly associated with nulliparity. Other known risk factors include African American heritage, nonsmoking status, early menarche, increased alcohol use, and hypertension. Generally, low-dose oral contraceptive pills do not cause growth of fibroids and depot-medroxyprogesterone acetate (Depo-Provera) is protective against fibroid formation. Many uterine anomalies require no treatment unless there is a concern for significant future pregnancy complication or if the patient is symptomatic, for example, from bleeding into a noncommunicating uterine horn or nonpatent vaginal septum. Vignette 1 Question 4 Answer A: Uterine septa can vary in thickness and are composed of collagen fibers and often lack an adequate blood supply to facilitate and support placental growth. For this reason, recurrent pregnancy loss is the most common complication for these patients. Once a pregnancy is successful beyond the first trimester in these women, they usually do not have further complications. Placental abruption, second-trimester fetal loss and premature rupture of membranes occurs more often in patients with bicornuate or unicornuate uteri. Simple and complex refer to glandular crowding of cytologically normal cells, and atypia describes the cytologically abnormal cells in more severe endometrial hyperplasia. Simple hyperplasia without atypia is the simplest form of hyperplasia, less than 1% of these lesions progress to carcinoma. Complex hyperplasia without atypia consists of abnormal proliferation of the glandular endometrial elements without proliferation of the stromal elements. The glands are crowded in a back-to-back fashion and are of varying shapes and sizes. Simple hyperplasia with atypia involves cellular atypia and mitotic figures in addition to glandular crowding and complexity and progresses to carcinoma in about 10% of cases if untreated. As many as 17% to 52% of patients with complex hyperplasia with atypia have coexistent cancer at the time of diagnosis. Functional ovarian cysts are classically asymptomatic, unilateral, and arise after failure of a follicle to rupture during the follicular maturation phase of the menstrual cycle. Ectopic pregnancies are often tender to palpation, and her menstrual history suggests that she may not be pregnant with the recent menstrual cycle; however, a pregnancy test is still indicated for this patient who is sexually active and not using any contraception. Implantation or first-trimester bleeding in pregnancy can sometimes be mistaken for a "light" menstrual cycle. Her asymptomatic menstrual history does not suggest endometriosis because she does not report dysmenorrhea. An ultrasound will aid in diagnosis of the cyst appearance and internal components. Vignette 4 Question 2 Answer D: When cysts reach a size of greater than 4 cm, they are at risk for torsion. This is somewhat determined by the contents of the cyst, with mature teratomas having a slight higher risk of torsion if solid internal components are present to act as a leading edge of the fulcrum for torsion. Acute pain in a gynecologic situation could also be caused by ruptured hemorrhagic corpus luteum cyst, a torsed ovary, or a ruptured follicular cyst. Emergent evaluation of this patient is recommended as she is at risk for ovarian necrosis if torsion is present. It is also important to counsel your patients who have a large ovarian cysts of this risk and to encourage early evaluation if pain arises. These medications provide steady estrogen levels (as opposed to the fluctuating levels in a patient who is not on these medications). Therefore, the immature follicles never develop, there is no ovulation and the probability of a functional cyst is decreased. Vignette 3 Question 1 Answer A: A transvaginal ultrasound is the initial best imaging test for postmenopausal bleeding. This will discern if there are any uterine leiomyomas, potential masses or polyps, and evaluate the thickness of the endometrium. This has lower specificity in regards to diagnosing polyps when compared to hysteroscopy (direct visualization of the endometrial cavity), but hysteroscopy is more invasive and may need to be performed in the operating room. Hysterosalpingogram is used to assess the shape and contour of the endometrial cavity. Radiopaque contrast medium is injected through the cervical canal and fluoroscopy is used to image the uterine cavity and fallopian tubes. This test will not evaluate the myometrium or endometrial thickness, and is not used for postmenopausal vaginal bleeding. Vignette 3 Question 2 Answer B: It is prudent that you consider endometrial polyps, hyperplasia, and endometrial carcinoma in the differential diagnosis of patients presenting with abnormal menstrual bleeding, including those older than 45 years, but especially in postmenopausal women with any bleeding. It is up to 95% accurate and should be performed in all postmenopausal women with a thickened endometrial stripe (. A cystourethroscopy will not aid in determination of the cause of her vaginal bleeding at this time because it evaluates the bladder and urethra. Given her age of greater than 50, she does need a colonoscopy for routine colo-rectal cancer screening however, this is not used in the initial gynecologic workup for postmenopausal bleeding. Diagnostic laparoscopy is an invasive test and will not help to determine the pathologic nature of her endometrial cavity, which is causing the heavy bleeding. Vignette 3 Question 3 Answer C: Nulliparity (instead of multiparity) is a known risk factor for endometrial hyperplasia.
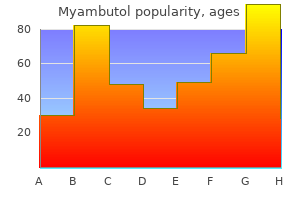
Discount 800mg myambutol with mastercard
Insertion site of this ligament has two attachments antibiotics for sinus infection how long to work order myambutol 600 mg line, one to the glenoid labrum and the other directly to the anterior neck of the glenoid. With the arm at the side, both the anterior and the posterior bands pass through a 90-degree arc and insert on the humerus. Levator Scapula and Serratus Anterior the levator scapula and the serratus anterior are often discussed together because of their close relationship anatomically and functionally. The levator scapula takes origin from the posterior tubercles of the transverse process from C1 through C3 and sometimes C4. Inserts on the superior angle of the scapula Acts to elevate the superior angle of the scapula In conjunction with the serratus anterior, produces upward rotation of the scapula Innervation is from the deep branches of C3 and C4. Serratus anterior takes origin from the ribs on the anterior lateral wall of the thoracic cage. Bounded medially by the ribs and intercostal muscles and laterally by the axillary space Protracts the scapula and participates in upward rotation of the scapula More active in flexion than in abduction because straight abduction requires some retraction of the scapula Absence of serratus activity, usually because of paralysis, produces a winging of the scapula with forward flexion of the arm and loss of strength in that motion. Blood supply is from the lateral thoracic artery, with a large contribution from the thoracodorsal artery. Labrum Surrounds the periphery of the glenoid and is a site of attachment of the capsuloligamentous structures It is composed of dense fibrous connective tissue, with a small fibrocartilaginous transition zone at the anteroinferior attachment of the osseous glenoid rim. The labrum acts as a load-bearing structure for the humeral head and serves to increase the surface area of the glenoid. Howell and Galinat showed that the labrum deepened the glenoid socket by nearly 50%. Triangular cross-section of the labrum allows it to act as a chock-block to help prevent subluxation. Supraspinatus Lies on the superior portion of the scapula It takes origin from the supraspinatus fossa and overlying fascia and inserts into the greater tuberosity. Nerve comes through the suprascapular notch and is bound above by the transverse scapular ligament. The deltoid is supplied by the axillary nerve (C5 and C6), which enters the posterior portion of the shoulder through the quadrilateral space and innervates the teres minor in this position. Nerves to the posterior third of the deltoid enter the muscle very close to their exit from the quadrilateral space, traveling in the deltoid muscle along the medial and inferior borders of the posterior deltoid. Branch of the axillary nerve that supplies the anterior two thirds of the deltoid ascends superiorly and then travels anteriorly, about 2 inches inferior to the rim of the acromion. Vascular supply to the deltoid is largely derived from the posterior humeral circumflex artery, which travels with the axillary nerve through the quadrilateral space of the deep surface of the muscle. Infraspinatus Second most active rotator cuff muscle Its tendinous insertion is in common with the supraspinatus anterosuperiorly and the teres minor inferiorly at the greater tuberosity. One of the two main external rotators of the humerus and accounts for as much as 60% of external rotation force Also functions as a depressor of the humeral head Even in a passive state, it is an important stabilizer against posterior subluxation. Innervated by the suprascapular nerve Blood supply is from two large branches of the suprascapular artery. Teres Minor One of the few external rotators of the humerus It provides up to 45% of the external rotation force. Innervated by the posterior branch of the axillary nerve (C5 and C6) Blood supply is derived from several vessels in the area, especially the posterior humeral scapular circumflex artery. Subscapularis Makes up the anterior portion of the rotator cuff Takes origin from the subscapularis fossa, which covers most of the anterior surface of the scapula Its upper 60% inserts through a cartilaginous tendon into the lesser tuberosity of the humerus, and its lower 40% has a fleshy insertion into the humerus below the lesser tuberosity cupping the head and neck. Functions as an internal rotator and passive stabilizer to anterior subluxation and serves in its lower fibers to depress the humeral head Innervation usually supplied by two sources: Upper subscapular nerve (C5) and lower subscapular nerves (C5 and C6) Upper subscapular nerves usually come off the posterior cord. Middle portion takes origin from the manubrium and upper two thirds of the body of the sternum and ribs 2 through 4. It inserts directly behind the clavicular portion and maintains a parallel fiber arrangement. Inferior portion of the pectoralis major takes origin from the distal body of the sternum, the fifth and sixth ribs, and the external oblique muscle fascia. Action Clavicular portion participates somewhat in flexion with the anterior portion of the deltoid while the lower fibers are antagonistic. Is active in internal rotation against resistance and will extend the shoulder from flexion until the neutral position is reached Powerful adductor of the glenohumeral joint Innervation is supplied by two sources: Lateral pectoral nerve (C5, C6, and C7) innervates the clavicular portion of the muscle. Loop contribution from the lateral to the medial pectoral nerve carrying C7 fibers into the upper sternal portion Major blood supply derives from two sources: the deltoid branch of the thoracoacromial artery supplies the clavicular portion and the pectoral artery supplies the sternocostal portion of the muscle. Teres Major Takes origin from the posterior surface of the scapula along the inferior portion of the lateral border It has a muscular origin and a common tendinous insertion with the latissimus dorsi into the humerus along the medial lip of the bicipital groove. In their course, both the latissimus dorsi and the teres major undergo a 180-degree spiral; thus, the formerly posterior surface of the muscle is represented by fibers on the anterior surface of the tendon. Latissimus Dorsi Takes origin by the large and broad aponeurosis from the dorsal spines of T7 through L5, a portion of the sacrum, and the crest of the ilium Wraps around the teres major and inserts into the medial crest and floor of the bicipital or intertubercular groove Actions are inward rotation and abduction of the humerus, shoulder extension, and indirectly through its pull on the humerus downward rotation of the scapula. Biceps Brachii There are two origins of the biceps muscle in the shoulder: the long head takes origin from the bicipital tubercle at the superior rim of the glenoid. Has two distal tendinous insertions: Lateral insertion is to the posterior part of the tuberosity of the radius Medial insertion is aponeurotic (lacertus fibrosus), passing medially across and into the deep fascia of the muscles of the volar forearm. Loss of the long head attachment expresses itself mainly as loss of supination strength (20%), with a smaller loss (8%) of elbow flexion strength. Blood supply derives from a single large bicipital artery from the brachial artery (35%), multiple very small arteries (40%), or combination of two types. Coracobrachialis Originates from the coracoid process, in common with and medial to the short head of the biceps, and inserts onto the anteromedial surface in the midportion of the humerus Action is flexion and adduction of the glenohumeral joint. Arterial supply is derived mainly from the profunda brachial artery and the superior ulnar collateral artery. The dorsal scapular nerve comes off C5 with some C4 fibers and penetrates the scalenus medius and the levator scapulae, sometimes contributing with C4 fibers to the latter. The dorsal scapular nerve accompanies the deep branch of the transverse cervical artery or the dorsal scapular artery on the undersurface of the rhomboids and innervates them. Rootlets of the nerves C5, C6, and C7 immediately adjacent to the intravertebral foramina contribute to the formation of the long thoracic nerve, which immediately passes between the middle and posterior scalene muscles or penetrates the middle scalene. Trunks, Divisions, and Cords the roots combine to form trunks: C5 and C6 form the superior trunk; C7 forms the middle trunk; and C8 and T1 form the inferior trunk. The posterior divisions combine to form the posterior cord, the anterior division of the inferior trunk forms the medial cord, and the anterior division of the superior and middle trunks forms the lateral cord. These cords give off the remaining largest number of the terminal nerves of the brachial plexus, and roots from the lateral and medial cords come together to form the median nerve. The brachial plexus leaves the cervical spine and progresses into the arm through the interval between the anterior and middle scalene muscles. Divided into three portions in relation to the insertion of the scalenus anterior muscle Vertebral artery takes origin in the first portion, and the costocervical trunk and thyrocervical trunk take origin in the second portion. Two vessels encountered more frequently by the shoulder surgeon are the transverse cervical artery and the suprascapular artery. Come off the thyrocervical trunk in 70% of dissections In the remaining cases, they come off directly, or in common from the subclavian artery. Trochlea Hyperbolic, pulley-like surface that articulates with the semilunar notch of the ulna, covered by articular cartilage over an arc of 300 degrees Medial margin is large and projects more distally than does the lateral margin. The prominent medial and lateral margins are separated by a groove that courses in a helical manner from an anterolateral to the posteromedial direction. Capitellum Capitellum is almost spheroidal in shape and is covered with hyaline cartilage, which is about 2 mm thick anteriorly. A groove separates the capitellum from the trochlea, and the rim of the radial head articulates with this groove throughout the arc of flexion and during pronation and supination. Axillary Is the continuation of the subclavian artery It begins at the lateral border of the first rib and continues along the inferior border of the latissimus dorsi, at which point it becomes the brachial artery. This artery is traditionally divided into three portions: First portion is above the superior border of the pectoralis minor. Usual number of branches for each of the three sections corresponds to the name of the section: one branch in the first portion, two in the second, and three in the third. Second portion gives off the thoracoacromial artery and the lateral thoracic artery. Third portion gives off the following: Largest branch is the subscapular artery, and this is the largest branch of the axillary. Next branch is the posterior humeral circumflex artery, and the third branch is the anterior humeral circumflex artery. Anterior humeral circumflex artery is an important surgical landmark because it travels laterally at the inferior border of the subscapularis tendon, marking the border between the upper tendinous insertion of the subscapularis and the lower muscular insertion. The center of the concentric arc formed by the trochlea and capitellum is on a line that is coplanar with the anterior and distal cortex of the humerus.
Purchase myambutol with paypal
An incision is made about 5 cm proximal to the elbow crease on the lateral margin of the biceps tendon antimicrobial boxers buy myambutol 600 mg on line. It extends transversely across the joint line and curves distally over the medial aspect of the forearm. The interval between the brachioradialis and brachialis proximally and the biceps tendon and pronator teres in the distal portion of the wound is identified. The supinator muscle is released from the anterior aspect of the radius, which is fully supinated. The radial recurrent branches of the radial artery and its muscular branches are identified and sacrificed if more extensive exposure is required. This interval may now be developed to expose the anterior aspect of the elbow joint. A B Fascia Fascia Biceps Radial nerve Brachialis Brachioradialis Sensory branch of radial nerve Interosseous branch of radial nerve Capsule Incision in capsule opened Brachioradialis Biceps Radial nerve Brachialis Capitellum Annular ligament Supinator reflected Biceps tendon Biceps tendon Radial artery Radial artery Radius Periosteum reflected Pronator teres C Supinator Incision D Chapter 3 Bankart Repair and Inferior Capsular Shift Theodore A. The static stabilizers of the glenohumeral joint include the glenohumeral ligaments of the capsule (C), and the glenoid labrum (D), which deepens the socket and serves as an attachment for the glenohumeral ligaments and biceps tendon. Contact athletes (football players and wrestlers) have the highest incidence of shoulder dislocations as compared to other sports. The "essential anatomical defect," or Bankart lesion, was first described by a British pathologist, A. The "essential" nature of the Bankart lesion has been challenged, since a simulated Bankart lesion without capsular stretching does not lead to significant increases in glenohumeral translation. Biomechanical studies of this ligament have demonstrated that failure typically occurs at the glenoid insertion (40%), followed by the ligament substance (35%) and the humeral attachment (25%). Arm dominance, sport, position, and level of competition should be noted, as well as associated factors, including other sporting activities, training modalities, and past history of injuries. Traumatic causes of instability should be determined, as these are more likely to be associated with Bankart lesions. Any prior treatments (physical therapy, training modifications, medication, and surgery) should be noted. Palpation is performed to identify point tenderness; anterior joint line tenderness may be present in acute anterior dislocations; subacromial tenderness may be present with impingement secondary to subtle instability. Active and passive motion tests are an important part of the instability examination. Significant variations in motion are encountered in throwing athletes, with increased external rotation and decreased internal rotation common in the affected shoulder. Provocative testing is perhaps the most important aspect in the clinical evaluation of shoulder instability. Anterior translation and posterior translation are similarly graded with the patient supine and with an anterior or posterior load and shift test, although this test is performed only in the anesthetized patient. The apprehension test is routinely performed with the arm abducted, extended, and externally rotated. A sensation of impending subluxation or dislocation in the patient is diagnostic of instability. Pain is less specific and may instead indicate internal impingement of the articular surface of the rotator cuff or functional impingement of the bursal side of the rotator cuff on a prominent coracoacromial ligament. A posterior-directed force on the arm by the examiner that relieves the apprehension in this position (Jobe relocation test) suggests an unstable shoulder. Subscapularis integrity and strength should be evaluated in patients with glenohumeral instability. Inability to press the hand to the belly is a positive result of the belly press test and indicates subscapularis muscle weakness or tear. Inability to lift the hand from the back is a positive result in the lift-off test and indicates subscapularis muscle weakness or tear. The duration of immobilization has been controversial, but 3 to 6 weeks is recommended. However, many patients will not tolerate this position, and a position of adduction and internal rotation therefore is more commonly used. For treatment of acute injuries, rotational and scapular strengthening exercises of the affected shoulder are started after the initial immobilization period. The program is progressed toward normalization of strength and motion through increased resistance training. Return to sports is allowed when the patient has a full and pain-free range of motion, normal strength, and little or no apprehension. Resistive exercises of the rotator cuff are begun with the arm in neutral below 90 degrees and are progressed gradually. The axillary view is particularly important for assessing anterior glenoid rim defects. In young patients participating in high-risk activities (eg, military cadets), the rate of redislocation is as high as 92%. Nonanatomic procedures (Putti-Platt, Magnuson-Stack) are aimed at tightening the anterior structures and preventing atrisk arm positions (ie, abduction and external rotation). These procedures have largely been abandoned after it was discovered that overtightening the anterior structures could lead to posterior subluxation and glenohumeral arthritis. Coracoid transfer procedures are other nonanatomic procedures where the coracoid process, with its attached short head of the biceps and coracobrachialis tendons, is transferred to the anterior glenoid rim and secured with screws. Although several authors have achieved excellent success with these procedures, the concern for hardware migration and late resorption of the bone block have made these procedures less popular than the anatomic procedures. They are used mainly for revision procedures and in cases where there is deficient glenoid bone stock. Anatomic reconstruction procedures have been aimed at reconstructing the anterior labrum using sutures, staples, or tacks. The Bankart repair and inferior capsular shift procedures are the most commonly used anatomic reconstruction procedures. Although recurrence rates for arthroscopic Bankart repair and capsular shift were initially higher than open procedures, these rates have become comparable to open as the arthroscopic techniques have evolved. Noncompliance with the postoperative restrictions will increase the risk of redislocation after surgical repair. It is important to assess mental status and any secondary gain issues in patients with multidirectional instability. Patients with voluntary dislocations and malingering (Munchausen syndrome) patients have a high rate of failure and should be identified before surgery. It is important to identify before surgery any glenoid bony deficiency that may require bony augmentation via coracoid transfer or allograft reconstruction. Positioning Interscalene block anesthesia is preferred because of the excellent muscle relaxation and postoperative pain relief it offers. If an adequate block cannot be performed, however, general anesthesia can also be used. The patient should be moved to the edge of the table or the shoulder cut-out removed to allow access to the anterior and posterior shoulder as required. The concealed axillary incision is made from below the coracoid process toward the axillary fold. The miniincision is made in line with the deltopectoral interval and is centered one-third above and two-thirds below the coracoid process. Approach the bony landmarks of the shoulder are identified, including the acromion, clavicle, and coracoid process. Approaches to the shoulder that may be used include the deltopectoral, the concealed axillary incision, and the miniincision approach. A 7- to 15-cm incision is made lateral to the coracoid process beginning below the clavicle and extending toward the anterior humeral shaft at the deltoid insertion. This incision is cosmetically appealing and is useful in patients where cosmesis is important. The location of this incision is important to achieve direct access to the glenoid without extending the incision: one third of the incision should be above and two thirds below the coracoid process. The cephalic vein is taken laterally with the deltoid muscle, and the clavipectoral fascia overlying the subscapularis tendon and strap muscles is exposed. When additional exposure is needed, it is helpful to incise and tag with a suture the upper third of the pectoralis major insertion into the humerus. Great care should be taken not to injure the biceps tendon, which lies just underneath the pectoralis major insertion. The clavipectoral fascia is incised lateral to the strap muscles, and a retractor is placed between them to expose the subscapularis muscle and tendon.
Syndromes
- Arterial blood gas
- A weakened cervix that begins to open (dilate) early, also called cervical incompetence
- Citric acid urine test
- Other creams include benzyl benzoate, sulfur in petrolatum, and crotamiton.
- Night sweats or unexplained weight loss
- Amount swallowed
- Can the person remember events from further in the past (is there impaired long-term memory)?
- A (BMI) of 40 or more. This usually means that men are 100 pounds overweight and women are 80 pounds over their ideal weight.
- Constipation
- Leucine aminopeptidase - urine
Buy cheap myambutol
About 4 mm of redundant capsule is removed from the inverted-L portion of the capsulotomy to help reduce and advance the sesamoids upon closure antibiotic 2 purchase generic myambutol on-line. With larger deformities, more capsule may need to be removed to reduce the tibial sesamoid position adequately. To correct pronation of the hallux, the towel clip can be rotated to correct the deformity, and a double simple suture is placed to maintain the correction. The clamp is placed medially at the first metatarsal head and laterally around the second metatarsal head. Placing a sponge in the first interspace while closing the capsule will splint the toe in the corrected position. Place a soft toe spica dressing by dividing a sponge in thirds and wrapping lateral to medial around the hallux to maintain correction. Use caution to prevent aggressive splinting, which can cause overcorrection and potential hallux varus. Placing a varus stress on the hallux will expose redundant capsular tissue that can be incorporated within the L portion of the capsulotomy and can be adequately removed. The proximal portion of the osteotomy should be at least 1 cm distal from the first tarsometatarsal joint. This will also prevent placement of the osteotomy within the first tarsometatarsal joint. The saw blade is kept parallel to the weight-bearing surface of the foot to prevent unwanted dorsal angulation of the first metatarsal head after completion of the osteotomy. To maintain complete control of the osteotomy, a guidewire for the cannulated screw can be placed perpendicular in the completed proximal portion of the osteotomy. The osteotomy can be completed dorsal-distally without fear of losing the orientation. Placing a screw too distal may cause fracture of the dorsal portion of the osteotomy site. Allow adequate space between the screws and the distal aspect of the osteotomy to prevent fracture. If encountered, the fist tarsometatarsal joint may be temporarily pinned and permanent fixation placed. The pin across the first tarsometatarsal joint can be removed 4 to 6 weeks postoperatively. Two weeks after surgery the sutures are removed and the patient is fully weight bearing in a surgical shoe. The Mau is a stable osteotomy due to the dorsal shelf to help reduce dorsal displacement forces and broad bony apposition to facilitate twoscrew fixation. The authors performed a follow-up study comparing the Mau and crescentic osteotomies. Complications included dorsal malunion, placement of screws within the tarsometatarsal joint, and nonunion. This may be due to selection of the inappropriate procedure to correct the moderate to severe bunion deformity or intraoperative failure to obtain an adequate alignment to correct the deformity. It occurs as a result of overcorrection of the deformity and is much more difficult to correct. Other complications include shortening, dorsal malunion, and transfer lesions, which can occur with all proximal osteotomies. Mechanical comparison of cyclic loading in five different first metatarsal shaft osteotomies. Early results of the Mau osteotomy for correction of moderate to severe hallux valgus. Relationship of hallux abductus angle and first metatarsal angle to severity of pronation. Conclusions drawn from a comparative study of the feet of barefooted and shoe-wearing peoples. Hallux valgus repair utilizing a distal soft tissue procedure and proximal metatarsal osteotomy: a long-term follow-up. The relationship of abnormal foot pronation to hallux abducto valgus, a pilot study. A study of the correlation between neutral calcaneal stance position and relaxed calcaneal stance position in the development of hallux abducto valgus. Pins provide little inherent stability and have been associated with postoperative infections. Getting excellent fixation of screws can be a problem in cases in which there is poor bone quality. Recently, the use of locking plates and locking screws has been increasing in the orthopaedic world. The locking plates provide a fixed-angle device, which allows for a potentially stronger method of fixation. Advantages for the surgeon are that it is possible to do any osteotomy for the first metatarsal and that excellent and secure fixation is obtained. Although many different configurations of the osteotomy can be used, the proximal chevron osteotomy permits a greater degree of correction compared with distal osteotomies. It does this through both an angular and translational displacement of the distal portion of the first metatarsal. A dorsomedial incision is made in the capsule parallel to the first metatarsal, creating a plantarly based capsular flap with exposure of the medial eminence. First use a blunt Freer elevator to develop some room and then cut the capsular tissue with a sharp no. The proximal first metatarsal is subsequently exposed both dorsally and plantarly. A plantar and proximally based capsular flap is created, and the capsule is released with a Freer elevator. A proximally based chevron osteotomy is created at an angle of about 60 degrees using a microsagittal saw. The proximal fragment is grasped with a towel clamp, and the distal fragment angulated laterally. The prominent proximal fragment is cleaned of periosteum and removed flush with the distal fragment. The opening created by plantar flexing the metatarsal creates a gap into which the removed bone may be impacted. During the approach, dissect thick tissue flaps to allow for improved wound healing. Pay particular attention to keeping the saw in the same plane while performing the proximal chevron osteotomy to ensure good bony apposition at the site of fixation. If the plate requires contouring, do not bend the plate through the locking holes or the screws will not seat properly in the plate. By removing redundant medial capsule during the approach, the capsule repair can be accomplished more efficiently at the conclusion of the procedure. The great toe should be positioned in slight varus, about 2 degrees, to allow healing of the capsular tissues in a good position. Do not overtighten the capsule, because this will overcorrect the toe position and result in varus malalignment. Capsular imbrication also can be used to correct pronation deformity of the hallux. Heel weight bearing can be allowed immediately postoperatively, with advancement to weight bearing as tolerated in a regular shoe at 6 weeks postoperatively. Prospective, randomized comparison of proximal crescentic and proximal chevron osteotomies for correction of hallux valgus deformity. Bunion surgery using locking-plate fixation of proximal metatarsal chevron osteotomies.
Purchase myambutol with a visa
The head is slightly higher than the tuberosities antibiotic resistance food safety cheap myambutol master card, slightly medial and posterior to the humeral shaft, retroverted 30 degrees. Axial load transmitted to the humerus may cause impacted fracture in osteoporotic bone. Violent muscle contractures, as in grand mal seizures and electric shock, are associated with posterior dislocation due to overpowering internal rotators and adductors. Pathologic causes include tumor, multiple myeloma, and metastatic or metabolic disorders. Osteoporosis is associated with fractures of the proximal humerus (more than any other fracture). In a three-part fracture with intact greater tuberosity, the humeral head is pulled by the supraspinatus and infraspinatus tendons; if the tendons are intact, the humeral head is externally rotated. Rotator cuff tears Neurovascular injury: axillary nerve, brachial plexus Avascular necrosis of the humeral head often results from disruption of the arcuate artery. The axillary artery also may be damaged, but less commonly, in fracture-dislocations. In patients younger than 50 years of age, violent trauma, contact sports, and falls from heights are responsible for fractures. Acute, recurrent, or chronic dislocation without major Indications Two-part proximal humerus fracture Three-part proximal humerus fracture Certain four-part proximal humerus fractures Prerequisites Shoulder table, image intensification, and experienced radiology technician Be aware of the learning curve (do not attempt nailing of a four-part fracture before acquiring adequate experience with two- and three-part fractures). The muscular attachments of the greater and lesser tuberosities will cause abduction, external rotation, and internal rotation, respectively. A bolster is used to elevate the shoulder from the table and to allow shoulder extension. Extension of the shoulder is necessary to expose the entry site in the humeral head. Flexion of the shoulder will result in the acromion overlying the center of the humeral head in the sagittal plane, obscuring the entry site or errantly directing an entry angle. Anterior cutout of the nail in the head fragment can easily occur in an osteoporotic humeral head with an associated greater tuberosity fracture. Contraindication: head-splitting, comminuted displaced humeral head fragment devoid of soft tissue attachment Preoperative Planning Successful intramedullary nailing of the proximal humerus fracture depends on consistent integration between image intensification and the surgical steps. Patient positioning on a radiolucent table will allow the surgeon to use a minimally invasive approach. Any error on the entry site will cause inevitable problems with the rest of the procedure. Positioning Positioning on the table must allow orthogonal and overhead axillary views. Intramedullary nailing for isolated surgical neck fractures may be performed completely percutaneously using most of the techniques described in the following paragraphs. However, when tuberosity reduction and fixation are required, a wider approach often is necessary. The timing of the open approach depends on the sequencing of head, shaft, and tuberosity fixation. Alternatively, an open approach with tuberosity reduction and fixation can be performed before nail insertion. Significant rotator cuff defect is not created with this approach, as confirmed in cadaver dissection. The wires should be separated by enough distance to allow insertion of the nail between them (1. The K-wires should be directed in the longest axis of the humeral head in the axial plane. Confirmation of the correct placement in the axial plane is done by the overhead axillary view. Then the C-arm is positioned to view the advancement of the pins in the coronal plane projection. Unfortunately, with internal rotation, extension also occurs in the humerus and the humeral head, depending on the soft tissue attachments. This initial pin will serve to orient the humeral head, specifically the desired degree of retroversion. Image intensification can be used to place a K-wire through the head in line with intramedullary axis of the humerus. To achieve fracture reduction, the joysticks in the proximal fragment must be used to rotate the head while simultaneously rotating the distal shaft manually to obtain true orthogonal views of the head in reference to the shaft. Combining rotation of the head fragment (K-wires) with the shaft (arm) is used to assist in fracture reduction. Manipulation of the fracture fragments with the K-wires allows disimpaction of the fracture, improving the varus or valgus alignment. The anterior edge may be difficult to palpate and to differentiate from the humeral head because of edema and hematoma from the fracture. Therefore, it is helpful to locate the anterior edge of the angle of the acromion under image intensification with a K-wire where it intersects the longitudinal axis of the humerus. Manipulation of the proximal fragment has been the only reliable way to identify correct placement. This is easily accomplished in the coronal plane, but it is more difficult in the sagittal plane. The reamer is inserted over the guidewire, and the soft tissues are retracted and protected. The reamer is advanced through the rotator cuff in "reverse" until bone contact, then on "forward" through the humeral head. The guidewire that was used to initiate the entry site is removed, and a longer guidewire is passed to the shaft fragment. On some occasions, even external fixator placement from the scapular spine to the distal humerus is necessary. The external fixator is applied and distraction accomplished with manipulation of the proximal aspect of the shaft; guidewire passage usually is simple. Usually, impaction of the distal fragment by blows against the olecranon, while supporting the proximal humeral head indirectly through the soft tissues, is adequate. The goal of this screw is to attach the head to the shaft before fixation of the tuberosities. Careful blunt dissection to bone, drilling within the sheath, and placing the screw within the confines of the sheath are necessary. Drilling should be done very carefully, although it certainly does not completely negate the risk of drilling through the humeral head. It is occasionally helpful to remove the drill and then use a blunt guidewire and assure good humeral head subchondral bone contact before further drilling or screw placement. This step should flow very smoothly if the initial K-wires have been placed in the correct axial plane alignment. Errant placement or acceptance of poorly positioned K-wires will result only in further deviation. However, patients with osteoporosis do have a risk of the fracture fragment settling. Overdrilling to countersink the more proximal screw usually is necessary to avoid impingement. With very displaced tuberosity fractures, if shaft-to-head fixation is performed initially with the tuberosities displaced, the guide will perforate the cuff and pin the cuff in a nonanatomic position, resulting in inability to perform reduction of the tuberosities. Therefore, if tuberosity fixation is going to be aided with the nail, the tuberosity alignment must be performed before nailing. Another sequence involves fixation of the head and shaft followed by later fixation of the tuberosity. Anchors can be passed through the nail with sutures used later to fix the tuberosities. The sequence of fixation should involve passing sutures through the musculotendinous junction of the subscapularis, infraspinatus, and supraspinatus. Sutures passed over the superior aspect of the head from the infraspinatus and subscapularis and sutures passed laterally around the head provide helpful, reliable fixation points. Plan B: for complex fractures, obtain consent for a hemiarthroplasty and have an implant available.
Buy cheapest myambutol
One pin should enter lateral to the biceps in a primarily anterior-to-posterior direction antibiotics omnicef purchase cheapest myambutol and myambutol. Another pin should enter further laterally in a primarily lateral-to-medial direction. Stability should be checked under fluoroscopic imaging with live, gentle internal and external rotation. The starting point for the pins is approximately 5 to 6 cm distal to the surgical neck fracture line. Often a posterior vector must be applied to the shaft or an instrument can be introduced through the reduction portal to lever the head back onto the shaft. Retrograde pins are introduced several centimeters below the level of the surgical neck fracture into the head. The pins should be placed in different directions to provide stability to the construct. The pins should be cut below the skin after insertion to prevent pin site infection. They are easily removed a couple of weeks later with a small procedure in the office or operating room. Any suggestion of instability or motion at the fracture is an indication for open reduction and plate fixation at that point. The rotator cuff pulls the tuberosity medially (to a certain extent) and posteriorly. Posterior displacement and rotation often are underappreciated and must be considered. The guidewire is passed through the tuberosity, across the surgical neck fracture, and engages the medial cortex of the proximal humeral shaft. A small incision is made over the greater tuberosity, and a cannulated screw is used for fixation. The guidewire is aimed to engage the greater tuberosity fragment as well as the medial cortex to provide compression. Over-tightening should be avoided to prevent fracture of the greater tuberosity fragment. If the greater tuberosity fragment is large enough, a second cancellous screw is directed through the tuberosity fragment, engaging cancellous bone of the humeral head. This fracture configuration results in a low incidence of avascular necrosis compared to that of other fourpart fractures, because the medial periosteal hinge of soft tissues is intact along the medial and posterior anatomic neck, preserving the blood supply provided by the posterior humeral circumflex artery and its ascending vessels. The reduction maneuver for this fracture requires raising the humeral head back into its anatomic position. The instrument passes through the surgical neck fracture and through the fracture line between the tuberosities, which reliably exists 0. The surgical neck fractures and tuberosity fractures are then fixed using the techniques described earlier. Valgus impacted proximal humerus fractures are reduced using a small bone tamp or other blunt-tipped instrument. The instrument is inserted through the fracture line between the greater tuberosity and the lesser tuberosity, which lies posterior to the biceps groove. The bone tamp is impacted in a superior direction, bringing the humeral head into a reduced position. The greater and lesser tuberosities fall naturally into a reduced position after this reduction maneuver. In some cases, there may be significant medial displacement of the lesser tuberosity. In these cases, the lesser tuberosity is reduced using the hook through the reduction portal and fixed with a screw placed in the anterior-to-posterior direction through the tuberosity into the head. In most cases, minimal medial displacement of the lesser tuberosity is well tolerated and no fixation is required. Criteria include good bone stock, minimal to no comminution at the greater tuberosity fragment, minimal to no comminution at the medial calcar and proximal shaft, and patient compliance. Contraindications include poor bone stock that will not hold pins, comminution of greater tuberosity or proximal shaft fragments, and a noncompliant patient with poor follow-up potential. Positioning Reduction technique the patient must be lateral enough on the table to obtain unencumbered access to the shoulder and clear fluoroscopic images. The location of the reduction portal is critical for maximizing its usefulness during the procedure. The surgeon must have a thorough understanding of three-dimensional anatomy, as well as interpretation and application of two-dimensional fluoroscopic images. Pin placement Pins should engage the humerus distal to the axillary nerve, but proximal to the deltoid insertion to avoid nerve injury. The angle of insertion is steep to enter the humeral head and avoid cutting out posteriorly. At least two fluoroscopic images in different planes are necessary to confirm successful pin placement. Screw placement the deltoid should be spread bluntly and a drill guide used to prevent injury to the axillary nerve in this location. In most cases, insertion will be proximal to the nerve, but precautionary measures should be taken. Overtightening the screw with a washer may result in fracture of the greater tuberosity. Engaging medial cortex of the proximal shaft gives stability to the screw construct. Intraoperative assessment of stability the arm should be internally and externally rotated gently under continuous fluoroscopic imagery after completion of hardware placement. Any motion or suggestion of instability is an indication for open reduction and fixation. Pins are removed as a short procedure in the office or operating room about 3 to 4 weeks postoperatively or when early signs of healing are evident radiographically. Pendulum exercises are initiated 2 to 3 weeks postoperatively, and passive stretching (forward elevation in scapular plane), external rotation, and internal rotation (all in supine position) is initiated when pins are removed. Ideally, pins should be out and motion started no later than 4 weeks postoperatively. There were 29 surgical neck, 3 anatomic neck, 8 three-part, and 5 four-part fractures. Keener et al5 reported a multicenter study of 35 patients- 7 two-part, 8 three-part, and 12 valgus impacted fractures. Four patients had some residual malunion, and four developed posttraumatic arthritis. In published studies, patients are not randomized to percutaneous pinning, but, rather, careful patient selection is left to the treating surgeon. Therefore, it can be concluded that this is an appropriate technique in certain patients who meet the outlined criteria. This classification system involves four segments: the articular surface, the greater tuberosity, the lesser tuberosity, and the humeral shaft. Fracture fragments displaced 1 cm or angulated 45 degrees are considered displaced. The subscapularis inserts onto the lesser tuberosity, whereas the supraspinatus, infraspinatus, and teres minor insert onto the greater tuberosity. Knowledge of deforming forces associated with humerus fracture allows the surgeon to better treat proximal humerus fractures by both operative and nonoperative means. In a two-part surgical neck fracture, the pectoralis major pulls the humeral shaft anteromedial. In a two-part greater tuberosity fracture, the pull of the supraspinatus, infraspinatus, and teres minor tendons displaces the greater tuberosity superiorly and/or posteriorly. Three-part fractures involving the greater tuberosity result in unopposed subscapularis function, and the humeral articular surface rotates posteriorly. Four-part fractures result in displacement of the shaft and both tuberosities, leaving a free head fragment with little soft tissue attachment. An understanding of the vascular anatomy is crucial to treat fractures of the proximal humerus effectively. The main blood supply to the humeral head is the anterolateral ascending branch of the anterior circumflex artery.
Best purchase myambutol
However antibiotic quick reference purchase myambutol no prescription, a mass that continues to grow, causing pain and nerve dysfunction, may need to be resected. Surgical exposure begins with an open carpal tunnel release to identify the transition zone between normal and abnormal nerve. Painful expanding soft tissue mass along the common digital nerve to the third web space. Low-intensity normal nerve fascicles are seen coursing through the high-intensity fatty mass. At surgery, normal fascicles cannot be distinguished from the fibrofatty proliferation. Anticipation allows for appropriate preoperative planning and discussions with the patient. Watch for signs of malignancy, including increasing nerve dysfunction, rapid growth, and pain. Masses should be resected through an extensile approach; avoid transverse incisions. Loupe magnification and microinstruments facilitate enucleation of a tumor (schwannoma). A microscope should be available should microdissection or nerve resection and reconstruction become necessary (neurofibroma). If necessary, the end range of motion may be avoided for up to 1 month to protect nerve repairs or reconstructions. When axons have been injured, a hand therapist may assist with desensitization or sensory re-education. A Tinel sign may be followed for renervation along the course of the affected nerve. Permanent neurologic deficits follow en bloc resection of a neurofibroma, thus limiting the surgical indications for this procedure. Microdissection preserves nerve function11 but likely has an increased risk of recurrence. Resection of a lipofibromatous hamartoma of the median nerve (including partial excision or interfascicular dissection) often results in permanent nerve deficits. Unicameral bone cysts are benign endothelial-lined fluid-filled cavities arising in metaphyseal bone; they are occasionally seen in the distal radius and rarely seen in the hand. Giant cell tumor of bone is an uncommon benign neoplasm of bone, which is locally aggressive and can metastasize. While its histology suggests a benign process, is behaves as a lowgrade malignancy. Enchondroma and unicameral bone cysts may be associated with bone development and growth. Enchondroma, unicameral bone cyst, and giant cell tumor of bone can weaken the bone and predispose the patient to pathologic fracture. Enchondromas causing substantial fracture risk and those presenting after pathologic fracture can be treated surgically with a low risk of recurrence. Unicameral bone cysts with a low risk of fracture may be observed with activity modification. Suspected unicameral bone cysts in the bones of the hand are sufficiently rare that strong consideration should be given to biopsy when this lesion is suspected. It can be seen in metaphyseal and epiphyseal regions and is typically confined to the bone. Unicameral bone cysts are typically confined to bone and pathologic fracture may be seen. Giant cell tumor of bone most commonly arises in the epiphyseal region except in the skeletally immature patient, in whom it may arise in the metaphysis. Giant cell tumor of bone metastasizes 2% to 10% of the time, with metastasis more frequently seen with distal radius and hand lesions. Patients with giant cell tumor of bone require systemic staging, treatment, and long-term surveillance, as recurrence may be seen late. Giant cell tumor of bone may cause swelling, pain, tenderness, and a sense of weakness. Grade 2 lesions distend the cortex but do not extend into the surrounding soft tissues. The rare risk of malignant degeneration of enchondromas should be considered and discussed with the patient. Radiation is associated with a risk of subsequent true malignant degeneration to a highly malignant giant cell tumor of bone. Precautions to prevent donor-site cross-contamination must be considered and reviewed with the operating room team. The surgeon must determine the anticipated need for frozen section and discuss this with the pathologist and review radiographs before any anticipated frozen section. Positioning Surgery is typically done in the supine position with the arm extended on a radiolucent armboard. Distal radius lesions may be approached at the tubercle of Lister or at the interval between the radial border of the pronator quadratus and the first dorsal compartment, proximal to the radial styloid. Proximal humerus lesions are best approached just lateral to the deltopectoral interval. It must be done in a way that does not compromise the potential need for a subsequent limb-sparing procedure. Obtain plain radiographs in the operating room to confirm complete excision and appropriate grafting. A branch of the superficial radial nerve may be encountered and should be retracted and protected. Wide exteriorization of the lesion with a window roughly two-thirds the maximum dimension of the lesion is needed to ensure adequate visualization. The right radius is approached from the palmar radial aspect between the first dorsal compartment and the radial artery. The radial border of the pronator quadratus is exposed to gain access to the lesion for creation of the bone window. Finger extensors are released from the retinaculum while wrist extensors and often thumb extensors or abductors may need to be sacrificed. Dissect the flexor pollicis longus and the radial artery away from the tumor-bearing segment. Dorsal exposure of the distal radius and ulna with transection of the radius and ulna proximally. The radius and ulna are everted into the dorsal wound to allow palmar exposure and dissection of palmar soft tissues. A lateral approach to phalanx lesions provides more rapid return to normal motion and a better appearance. A volar radial approach for distal radius grade 1 and 2 giant cell tumors of bone allows excellent visualization and limits local contamination risk. The dorsal approach for large grade 3 giant cell tumor distal radius lesions is best when wide excision and reconstruction or arthrodesis is anticipated. Monitoring Surveillance monitoring is mandatory, particularly for giant cell tumor of bone, which can recur late and metastasize. Curettage, cryosurgery, and cementation of distal radius giant cell tumor of bone Dressings are changed 10 days postoperatively. Activities are gradually increased, with high-risk activities being restricted for up to 2 years due to cryonecrosis of bone caused by cryosurgery. Wide en bloc extra-articular distal radius resection Patients are dressed in a bulky compressive dressing, most commonly with a volar splint. Elevation is encouraged for the first 48 hours and digit range of motion is encouraged. When not exercising, patients are asked to use a protective splint for an additional month. Surveillance for local recurrence should continue for 5 years for benign lesions and 10 years for giant cell tumor of bone. When recurrence is seen, the question of malignant transformation should be considered. Intralesional treatment (curettage) is best reserved for lesions without soft tissue extension (grade 1 and 2 lesions). Isolated curettage without the use of adjuvants cannot be advocated in this setting. There are several successful examples of curettage cryosurgery and cementation of giant cell tumor of the small bones of the hand.