Order cefdinir once a day
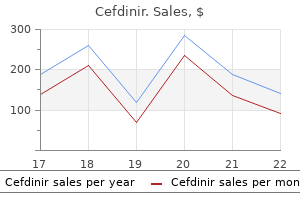
This diagnosis should be confirmed at a centre with experienced haematopathologists antibiotics vs virus order genuine cefdinir on line. Practically, these classifications allow better prognostication of expected responses to therapy and the determination of whether patients should proceed to consolidation with an allogeneic transplant or high-dose chemotherapy once they have reached a complete remission after induction chemotherapy. This cell, relatively resistant to the effects of chemotherapy, gives birth to the abnormal clone of myeloblasts that cannot differentiate, but can proliferate. In recent years, it has become apparent that this model should be expanded, as many mutations have been discovered in genes that encode epigenetic modifications that activate or suppress gene transcription. This is evident in routine clinical evaluations, as the percentage of myeloblasts does not always correlate with the degree of cytopenia. Hyperuricaemia is common, and allopurinol-or in patients presenting with severe renal failure, at least a single dose of recombinant urate oxidase (rasburicase)-should be prescribed [75]. Dyspnoea and stupor, ischaemic symptoms of heart, kidneys, distal extremities, or priapism, in the absence of alternative aetiology, may suggest hyperleukocytosis and leukopheresis should be considered [76]. Extramedullary leukaemic infiltration may exist but no routine evaluation or imaging is required. Brain imaging and lumbar puncture are indicated only when clinical symptoms are suspicious for central nervous system involvement [77]. It may also be justified in patients presenting with very high counts, but should be delayed until blasts are eradicated from peripheral blood. Of all cancers, acute leukaemias are particularly recognized for a very rapid progression from diagnosis to initiation of therapy. In contrast, those arising after exposure to the epipodophyllotoxins and anthracyclines usually have a shorter latency period, no period of myelodysplasia, and monocytic morphology. In recent years, multiple ways of intensifying the traditional protocol of three daily doses of anthracycline and a week-long continuous infusion of cytarabine (3 + 7) have been tested. However, intensifying induction by administering 50 mg/m2 of daunorubicin for five days failed to improve patient outcome [80]. It may well be that achievement of high peak plasma levels is more important than the total daunorubicin administrated dose. Several double induction protocols exist but only few have been compared to a regular 3 + 7 protocol. The effect of exposure to low levels of radiation over a lifetime, from medical radiological imaging, radon, and frequent travel in airplanes, is unknown [67, 68]. Active infection and occult bleeding should be ruled out and chest radiography, complete blood count, blood chemistry studies and coagulation panel, including fibrinogen, are indicated. Adequate hydration to maintain high urinary flow and rapid response to any signs or symptoms of infection are mandatory. Virtually identical survival curves from major co-operative groups, despite varying treatment regimens, population size, and countries. Similarly, with high daunorubicin doses the median survival of patients with favourable or intermediate cytogenetic profile has been significantly improved (from 20. Considering the dismal prognosis of patients who experience induction failure, early identification of resistant disease is warranted. Such a difference could not be demonstrated, in smaller numbers, among patients with unfavourable cytogenetics (B). Unfortunately, partly due to the inability to deliver maximal post-remission therapy, relapse rates are higher in older patients and only a small portion of patients can be cured. The following data should guide physicians in their judgement and must be carefully explained to patients. Mortality rate during the first month following intensive induction protocol is 10% in patients over 60 years, compared to 5% in younger patients. This is intuitively understandable when death is due to hyperleukocytosis or tumour lysis syndrome, but is also true in cases of fatal infections or bleeding which have similar prevalence among patients treated with palliative care only [90]. Comorbidities and performance status-but not age alone-are predictive parameters for early death [90]. In older adults, intensifying induction with high daunorubicin dose of 90 mg/m2 is safe, induces more remissions, and may also provide a survival advantage for some patients over 60 [91]. However, there is no reason to believe that the same results could not have been achieved using a higher anthracycline dose. Low-intensity induction protocols may have fewer side effects but are much less effective in inducing complete remission [93]. Data from Swedish and Swiss registries suggest that older patients, even those with poorer performance status, do better with intensive induction than with best supportive care only [90] (Table 51. Early death is the mortality rate from all causes within the first 30 days of therapy. Only 63 (56%) patients were randomized to best supportive care and the number of patients randomized to low-dose cytarabine and intensive chemotherapy was also small. For patients randomized to not receive decitabine, low-dose cytarabine was offered to 88% and only 12% of patients were assigned to supportive care. Therefore, azacitidine or decitabine, though they may prolong survival of some patients, should not be a substitute for intensive chemotherapy in patients who can tolerate it (Table 51. The non-treatment control arm was terminated due to a significantly shorter remissions and higher relapse rates [101]. The addition of daily 20 mg/m2 cytarabine subcutaneously for 14 days to clofarabine improved remission rate to 63%, but with a price of increased induction mortality [95]. There were several attempts to further improve long-term results using different consolidation protocols. With the growing number of Post-remission therapy in older patients Unlike in younger adults, there is no unequivocal evidence that any form of post-remission therapy changes the long-term outcome in older patients [105]. Nevertheless, virtually every major study in older adults includes some form of post-remission therapy. The reported results of comparable long-term outcome with either one or three consolidation cycles following double induction should be carefully interpreted. In addition, the toxicity and mortality with each consolidation cycle is age-dependent. Thus, the cumulative mortality risk related to the administration of three to four cycles can reach 5% in younger and 30% in older adults. However, only in young adults do the benefits of repetitive consolidations outweigh toxicity. There is no agreement regarding the number, drug combination, or doses of consolidation cycles. The common practice of administrating multiple courses is based on retrospective data and, except for patients with favourable cytogenetics, a considerable relapse risk should be expected [112]. Such clinical scenarios are common, especially in older patients where unfavourable genetics are frequent and the probabilities for transplant-related complications are high. Two main paths of therapy exist in such conditions but it must be recognized that they are directed at different goals. The study was stopped due to slow accrual but results from randomization of 195 patients were recently published [135]. Since ultimate relapse is predicted, the main goal of such therapy is prolonging life with the best quality. A large Japanese study demonstrated that for patients receiving three intensive consolidation courses, the addition of maintenance improved outcome no better than a shorter Table 51. It seems that this modality has not been adequately studied in large prospective trials, including maintenance for young adults after intensive chemotherapy, autologous transplant, or even allogeneic transplant. However, such factors became relevant only with uniform treatment strategies and larger patient numbers from prospective multicentre trials. These prognostic factors, still used in most studies, were later extended to immunophenotypes, cytogenetic and genetic alterations [155, 156]. The aim of evaluating prognostic factors in acute lymphoblastic leukaemia is to stratify patients into good- and poor-risk groups and to adapt different treatment strategies accordingly. There are principally two phases where prognostic factors are evaluated; the first is the patient characteristics at diagnosis and the second is the response to treatment.
Order cefdinir overnight
They occur equally in both sexes infection epsom salt order cefdinir toronto, and are rare under the age of 30 years; their prevalence increasing with age. The majority are benign adenomas, with the majority of the rest comprising adrenal carcinomas, phaeochromocytomas, and secondary metastases. Surgical excision is the treatment of choice while the role of radiotherapy has not been clearly defined. Increasing data suggest that many apparent non-secretory adrenal adenomas do in fact show low-grade cortisol secretion, which may have metabolic effects, but whether all should then be removed is controversial. In the case of an adrenal mass which has been deemed hormonally non-secretory, the possibility of primary or metastatic malignancy must be excluded. Attempts to separate benign from malignant lesions on the basis of size (greatest diameter) criteria have been shown to be of limited value [62]. Furthermore, suspected malignant adrenal tumours should not undergo biopsy because of the risk of dissemination. Adrenocortical scintigraphy 131I-6-iodomethylnorcholesterol has been used but now is mainly of historical interest [63, 81]. Adrenal tumours may increase in size, develop overt or subclinical hormone secretion or feature malignant transformation. Therefore, radiological and hormonal follow-up should be recommended to the patients. More investigations are needed for the establishment of long-term follow-up protocols [77, 79]. They present a heterogeneous group of chromaffin cell neoplasms with different ages of onset, secretory profiles, locations, and potential for malignancy according to underlying genetic mutations [83]. Epidemiology Phaeochromocytomas are rare tumours, showing no sexual predominance, occurring at any age, although most commonly in the third and fourth decades. A significant number of phaeochromocytomas (>50%) are found at autopsy having escaped diagnosis in life [87]. Tumours account for less than 1% of cases of hypertension, but importance of diagnostics is in potential lethal consequences if unrecognized and untreated [64, 65, 83]. Aetiology and pathogenesis Phaeochromocytomas and sympathetic paragangliomas usually produce catecholamines or their metabolites. Significant intra-tumour metabolism of catecholamines occurs in large tumours; conversely, small lesions can be disproportionally symptomatic because of high concentrations of catecholamines [64]. Phaeochromocytomas may produce vasoactive peptides that reduce vascular responsiveness; thus, some patients with high catecholamine levels can be completely asymptomatic, while in others adrenoceptor blockade is ineffective in controlling hypertension [64]. Adrenomedullary tumours Phaeochromocytomas and paragangliomas Neuroendocrine tumours originated from chromaffin adrenal cells are called phaechromocytomas, while those arising in extra-adrenal sympathetic and parasympathetic paraganglia are called paragangliomas. Raised urinary dopamine and high levels of 3-methoxytyramine may indicate malignancy, the latter being typically raised in paragangliomas [82, 83]. After biochemical diagnosis confirmation, anatomical localization is necessary due to the variable location of these tumours. Signs of capsular invasion and vascular penetration are not proof of malignancy, which is clear if metastatic lesions to the bone, liver, lungs, and within the tumour bed are present. Diagnosis and staging Patients with phaeochromocytomas present with a diversity of symptoms, due to secreted catecholamines and other active substances. The classic triad of severe headache, diaphoresis, and palpitations carries a high degree of specificity (94%) and sensitivity (91%) for phaeochromocytoma in the hypertensive population. Other symptoms in acute attack include tremor, pallor, weakness, nausea, and panic attacks. Orthostatic hypotension can occur because of hypovolaemia and impaired arterial and venous constriction responses. Hypertensive crises with induction of anaesthesia, hypertensive encephalopathy, or spells suggestive of seizure disorder should all evoke suspicion of an underlying phaeochromocytoma. Cardiovascular and cerebrovascular complications can occur, including sudden left ventricular failure, pulmonary oedema, dysrhythmias, circulatory shock, myocardial infarction, dilated cardiomyopathy, cerebral infarction, and intracranial haemorrhage. Less specific signs and symptoms such as heat intolerance, weight loss, carbohydrate intolerance, pyrexia of unknown origin, and constipation mimicking pseudo-obstruction and paralytic ileus, have been described. Certain drugs can precipitate a hypertensive crisis in the presence of a phaeochromocytoma, which include tricyclic antidepressants, anti-dopaminergic agents (such as sulpiride and metoclopramide), and naloxone. Biochemical testing should be performed in symptomatic patients, in patients with adrenal incidentalomas, or those in an increased hereditary risk [82]. Initial testing should include measurement of urinary or plasma metanephrines, or both if available. Measurement of plasma-free and urinary metanephrines show similarly high specificity, but overall plasma levels offer higher sensitivity [83]. If plasma metanephrines are more than four-fold above the upper reference limit there is a close to 100% probability of a tumour. Levels above the normal range but less than this can be seen in patients with acute, debilitating, non-endocrine illness [66], Management Laparoscopic surgery is first choice technique for resection of adrenal and extra-adrenal tumours. The possibility of cortical-sparing surgery in hereditary syndromes with frequent bilateral disease, in order to avoid medical adrenal replacement therapy, remains controversial because of possible disease recurrence. Preoperatively, all patients should be given adequate alpha-blockade to achieve expansion of the intravascular volume and a reduction the frequency and severity of intraoperative pressor episodes. At least two weeks prior to surgery patients are started with oral phenoxybenzamine, usually at a dose of 1 mg/kg. Alternatives include calcium channel blockers and selective 1-adrenoreceptor blocking agents such as doxazocin or terazosin. However, significant elevations of blood pressure can still be seen during surgical manipulation of the tumour and thus nitroprusside should be available during operation. Beta-adrenoreceptor blockade may be used for control of tachyarrhythmias and angina, but always after prior -adrenoceptor blockade, otherwise unopposed catecholamine induced vasoconstriction can result in dangerous blood pressure elevations. Patients with phaeochromocytomas have a high volume requirement both during and after surgery and plasma expanders may be necessary. Perioperatively, the use of morphine or phenothiazines should be avoided as these agents can precipitate hypertensive crises or hypotension. Enflurane and isoflurane are the anaesthetics preferentially used as they do not sensitize the myocardium to catecholamines and minimize the risk of arrhythmias. Post-operatively, the blood pressure may remain elevated for a few weeks and around 75% of patients become normotensive. Surgical mortality is now extremely low with adequate preparation and thus complete cure is the rule in patients undergoing elective procedures. Post-operative follow-up is necessary, not only for patients with identified mutations of disease causing genes, but for all patients because there is currently no reliable pathological technique which can rule out the potential for malignancy or recurrence. Malignant phaeochromocytomas Malignancy is diagnosed in terms of metastatic spread, which may occur years (median 5. There is a greater tendency to malignancy with paragangliomas, tumours in young people, female sex, large, familial lesions, and those associated with other endocrine or neoplastic disorders. These tumours are usually associated with increased dopamine and methoxytyramine secretion. There have also been a number of reports of treating inoperable primary and metastatic lesions with technically challenging embolization [67]. The five-year survival of patients with malignant phaeochromocytomas is 20%; however, there are patients who have survived for 20 years or longer [83]. Pituitary tumours Pituitary tumours account for approximately 10% of clinically apparent intracranial neoplasms. Significant advances have improved the diagnosis and management of these tumours, including imaging of the pituitary by nuclear magnetic resonance, radioimmunoassay of circulating pituitary hormones, the advent of microsurgical techniques, immunocytochemistry, refinement of techniques for administering external pituitary irradiation, and new drug therapies. The term pituitary carcinoma should not be used unless metastases within the nervous system or spinal cord separate from the primary tumour (or outside the neuroaxis) are found, and this is very rare.
Diseases
- 8p23.1 duplication syndrome
- Prostate cancer, familial
- Cleft palate heart disease polydactyly absent tibia
- Engelhard Yatziv syndrome
- Endocarditis
- Pseudoachondroplastic dysplasia
Buy cefdinir 300mg without a prescription
Subtype-specific genomic alterations define new targets for soft-tissue sarcoma therapy antibiotics over the counter cvs buy cheap cefdinir 300 mg. Sarcoma: concordance between initial diagnosis and centralized expert review in a population-based study within three European regions. The effect of the anatomic setting on the results of surgical procedures for soft parts sarcoma of the thigh. Status of surgical margins and prognosis in adult soft tissue sarcomas of the extremities: a series of patients treated at a single institution. Surgical margins, local recurrence and metastasis in soft tissue sarcomas: 599 surgically-treated patients from the Scandinavian Sarcoma Group register. Surgical margins and re-excision in the management of patients with soft tissue sarcoma using conservative surgery and radiation therapy. Retroperitoneal soft-tissue sarcoma: analysis of 500 patients treated and followed at a single institution. Prognostic factors in retroperitoneal sarcoma: a multivariate analysis of a series of 165 patients of the French Cancer Center Federation Sarcoma Group. Operative management of primary retroperitoneal sarcomas: a reappraisal of an institutional experience. Primary and locally recurrent retroperitoneal soft-tissue sarcoma: local control and survival. Clinical outcomes of deep atypical lipomas (well-differentiated lipoma-like liposarcomas) of the extremities. Prognostic impact of dedifferentiation in retroperitoneal liposarcoma: a series of patients surgically treated at a single institution. Myxoid/round cell and pleomorphic liposarcoma: prognostic factors and survival in a series of patients treated at a single institution. Localized and metastatic myxoid/round cell liposarcoma: clinical and molecular observations. Radiosensitivity translates into excellent local control in extremity myxoid liposarcoma: a comparison with other soft tissue sarcomas. Extensive adipocytic maturation can be seen in myxoid liposarcomas treated with neoadjuvant doxorubicin and ifosfamide and pre-operative radiation therapy. Dermatofibrosarcoma protuberans treated at a single institution: a surgical disease with a high cure rate. Dermatofibrosarcoma protuberans: clinical diagnoses and treatment results of 260 cases in China. Leiomyosarcoma and sarcoma with myogenic differentiation: two different entities or two faces of the same disease Primary leiomyosarcomas of the gastrointestinal tract in the post-gastrointestinal stromal tumor era. Surgical technique, morbidity, and outcome of primary retroperitoneal sarcoma involving inferior vena cava. Outcomes and prognostic factors for a consecutive case series of 115 patients with somatic leiomyosarcoma. Clinicopathologic re-evaluation of 100 malignant fibrous histiocytomas: prognostic relevance of subclassification. Indistinguishable genomic profiles and shared prognostic markers in undifferentiated pleomorphic sarcoma and leiomyosarcoma: different sides of a single coin A synovial sarcoma-specific preoperative nomogram supports a survival benefit to ifosfamide-based chemotherapy and improves risk stratification for patients. Synovial sarcoma: a retrospective analysis of 271 patients of all ages treated at a single institution. Myxofibrosarcoma: prognostic factors and survival in a series of patients treated at a single institution. Recurrence patterns and survival for patients with intermediate- and high-grade myxofibrosarcoma. Malignant peripheral nerve sheath tumors: prognostic factors and survival in a series of patients treated at a single institution. Internal hemipelvectomy of musculoskeletal tumors-indications and options for reconstruction. Survival, local recurrence, and function after pelvic limb salvage at 23 to 38 years of followup. Dedifferentiated chondrosarcoma: prognostic factors and outcome from a European group. Chordoma of the Mobile Spine and Sacrum: A Retrospective Analysis of a Series of Patients Surgically Treated at Two Referral Centers. Malignant peripheral nerve sheath tumors: prognostic impact of rhabdomyoblastic differentiation (malignant triton tumors), neurofibromatosis 1 status and location. Localised angiosarcomas: the identification of prognostic factors and analysis of treatment impact. Angiosarcomas, a heterogeneous group of sarcomas with specific behavior depending on primary site: a retrospective study of 161 cases. A 14-year retrospective review of angiosarcoma: clinical characteristics, prognostic factors, and treatment outcomes with surgery and chemotherapy. Epithelioid sarcoma and unclassified sarcoma with epithelioid features: clinicopathological variables, molecular markers, and a new experimental model. Epithelioid sarcoma: prognostic factors and survival in a series of patients treated at a single institution. Clear cell sarcoma (malignant melanoma) of soft parts: a clinicopathologic study of 52 cases. Sentinel node biopsy in soft tissue sarcoma subtypes with a high propensity for regional lymphatic spread-results of a large prospective trial. Do radiation-associated soft tissue sarcomas have the same prognosis as sporadic soft tissue sarcomas Osteoarticular and intercalary allograft transplantation in the management of malignant tumors of bone. Massive resection and allograft transplantation in the treatment of malignant bone tumors. Radiotherapeutic factors in the management of cervical-basal chordomas and chondrosarcomas. Long-term results of a prospective randomized trial of adjuvant brachytherapy in soft tissue sarcoma. Randomized prospective study of the benefit of adjuvant radiation therapy in the treatment of soft tissue sarcomas of the extremity. Preoperative versus postoperative radiotherapy in soft-tissue sarcoma of the limbs: a randomised trial. Long-term results of two prospective trials of preoperative external beam radiotherapy for localized intermediate- or high-grade retroperitoneal soft tissue sarcoma. Locoregional recurrence after preoperative radiation therapy for retroperitoneal sarcoma: adverse impact of multifocal disease and potential implications of dose escalation. Proton radiotherapy: the biological effect of treating alternating subsets of fields for different treatment fractions. Clinical outcome of sacral chordoma with carbon ion radiotherapy compared with surgery. Doxorubicin alone versus intensified doxorubicin plus ifosfamide for first-line treatment of advanced or metastatic soft-tissue sarcoma: a randomised controlled phase 3 trial. High-dose ifosfamide: circumvention of resistance to standard-dose ifosfamide in advanced soft tissue sarcomas. Prolonged 14-day continuous infusion of high-dose ifosfamide with an external portable pump: feasibility and efficacy in refractory pediatric sarcoma. Histology- and non-histology-driven therapy for treatment of soft tissue sarcomas. Gemcitabine in advanced angiosarcoma: a retrospective case series analysis from the Italian Rare Cancer Network. Dermatofibrosarcoma protuberans-derived fibrosarcoma: clinical history, biological profile and sensitivity to imatinib.
Order cefdinir pills in toronto
A small minority of oligodendrogliomas present as intraventricular or extra-axial masses antibiotics for staph discount cefdinir 300 mg otc. Pilocytic astrocytomas are rare in adults compared to children and the anatomical distribution differs with supratentorial lesions outnumbering the cerebellar and brainstem lesions more commonly encountered in children. Pilocytic astrocytoma in the cerebrum can resemble various other tumours including oligodendroglioma, glioblastoma, ganglioglioma, and pleomorphic xanthroastrocytoma. Optic nerve gliomas are usually pilocytic astrocytomas but are usually infiltrative, leading to fusiform enlargement of the optic nerve, often extending to the chiasm and beyond. Contrast enhancement is also more variable in optic pathways pilocytic astrocytomas and is occasionally absent. To maximize the extent of resection, a craniotomy is performed with the patient awake under local anaesthesia or asleep for the initial craniotomy and then awake after the dura is opened. With the patient awake, intraoperative electrostimulation is now considered the gold standard. Eloquent cortical and subcortical white fibre tracts (motor, somatosensory, optic radiation, language, and spatial cognition) are stimulated to define their relationship to the tumour and preserve them during tumour resection [123]. This has resulted in reduction in neurological deficit from up to 28% (without awake mapping) to less than 2% with more evidence pointing towards functional mapping-guided resection rather than image-guided resection. An aggressive surgical approach also results in improvement in quality of life, especially with reduction in seizures. Pilocytic astrocytomas are grade 1 benign tumours and carry an excellent prognosis. Therefore, the aim of surgery is a complete resection without producing a deficit. In children and young adults the cerebellum is a common site and the tumour presents as a cyst with enhancing mural nodule. The cyst wall is non-neoplastic and need not be removed unless it enhances as well. Invasion of brainstem or involvement of cranial nerves or blood vessels may limit resection. Resection is indicated for tumours with a dorsal exophytic component in the fourth ventricle or the cerebellopontine angle as these are generally benign and amenable to radical subtotal resection [127]. Subependymomas of the fourth ventricle are approached through a suboccipital craniotomy and telovelar approach and should be resected as fully and safely as possible. Surgery reduces the tumour burden and re-establishes the flow of cerebrospinal fluid [128]. The majority of intracranial ependymomas arise in the wall of the fourth ventricle and these tumours often fill the ventricle and extend through one or more of its outflow foramina into the cisterna magna leading to obstructive hydrocephalus. Supratentorial ependymomas are usually much larger than fourth ventricular tumours at the time of presentation and most are within the brain parenchyma rather than intraventricular. It is rarely possible to make a prospective radiological diagnosis of a supratentorial ependymoma since their imaging features overlap significantly with those of a number of other lesions including glioblastoma, ganglioglioma, and pleomorphic xanthroastrocytoma. There is no clear evidence that prophylactic spinal irradiation prevents isolated spinal metastases, particularly if the primary tumour remains uncontrolled. The consensus view is that ependymomas should be treated with local irradiation to the site of the tumour and the appropriate margin, regardless of tumour grade and site. The technique and doses used are the same as those employed for other low-grade gliomas (54 Gy in 1. The prognosis is related to the histological grade, the extent of surgical resection, patient age, and performance status [136]. The presence of three or more risk factors determines a higher risk group with a median survival of three years. Glial tumours may involve any of the structures from the thalamus and hypothalamus through the midbrain to the pons and medulla. Just under 10% of cases are focal tectal glioma, often presenting with hydrocephalus, and prognosis exceeds ten years without irradiation [135]. Patients with medulloblastoma may present with raised intracranial pressure (usually due to hydrocephalus), cerebellar signs, and occasionally brainstem cranial nerve palsies. Medulloblastomas are usually solid, well-circumscribed intra-axial lesions of the cerebellum. Contrast enhancement is variable with some tumours enhancing avidly and relatively uniformly while some show only patchy enhancement and a small minority show no enhancement at all. Subarachnoid dissemination in the intracranial and spinal canal is a frequent finding. A medulloblastoma is approached by posterior fossa craniotomy and usually removal of the posterior arch of C1. The approach depends on the anatomical location of the tumour but the telovelar approach is the best choice for tumours in the fourth ventricle and avoids post-operative mutism [138]. In adults, 75% of ependymomas arise within the spinal canal, and up to 10% of patients have spinal metastases. Patients are classified according to extent of disease using the Modified Chang criteria [147]. The use of adjuvant chemotherapy in paediatric medulloblastoma has been extensively tested in sequential intergroup studies; however, there have been no trials in adults. As the natural history of adult medulloblastoma is similar to that in children, similar indications for chemotherapy could be accepted. The extent of disease defined by the Modified Chang criteria, age, completeness of resection, histological subtype, and genetic markers are prognostic indicators [150]. Stem cell transplant results in a disease-free survival in 24% of patients at ten years [152]. Tumours arising from the pineal gland can be germ cell tumours, pineal cell tumours, and gliomas (see Table 56. Due to their location, obstruction of the cerebral aqueduct with obstructive hydrocephalus is a common complication. Other features reflect the involvement of adjacent structures, such as the midbrain, hypothalamus, and the brainstem. Pineal germ cell tumours, like their systemic testicular counterparts, may secrete alpha-fetoprotein and human chorionic gonadotrophin into the cerebrospinal fluid and systemic circulation. Patients who need a surgical resection can undergo four possible surgical approaches: (a) transcallosal interforniceal, (b) transventricular, (c) occipital transtentorial, and (d) infratentorial supracerebellar. For benign or low-grade tumours a complete surgical resection results in excellent long-term recurrence-free survival [157, 158]. Intravascular lymphoma is a systemic non-Hodgkin lymphoma which causes systemic symptoms such as night sweats, hepatosplenomegaly, or pancytopaenia [166]. As well as ophthalmic examination and bone marrow histology for all patients, elderly males should undergo testicular ultrasound. In view of the morbidity of treatment, neuropsychological baseline testing should be considered. Avid uniform contrast enhancement and prominent surrounding vasogenic oedema are characteristic. Treatment with corticosteroids should therefore be avoided before attempting a tissue diagnosis. The mainstay of treatment is chemotherapy; therefore, a craniotomy and tumour resection is not warranted [170]. Tissue diagnosis is required prior to starting treatment and a stereotactic biopsy (framebased or frameless) is an excellent means of obtaining tissue. Such treatment morbidity of an aggressive approach [159, 160] although, a recent meta-analysis showed a graded increase in five-year survival with increasing degrees of resection (84% for gross total, 53% subtotal, and 29% debulking for pineoblastoma) [161]. Lymphoma infiltrates the white matter tracts to produce an array of symptoms including focal weakness or language deficits, cognitive, and behavioural changes.
Cheap cefdinir express
In addition to an epithelial component resembling acinar cell carcinoma antibiotic resistance lab report purchase 300mg cefdinir with mastercard, pancreatoblastomas contain squamoid bodies and eventually neuroendocrine or primitive-appearing small cell areas [51]. The overall survival is 50%, with a highly unfavourable outcome in non-resectable patients [51]. Solid pseudopapillary neoplasms display solid-appearing cell-rich areas containing thick-walled capillaries. These low-grade malignant neoplasms predominantly affect young females and have a good prognosis even in cases with liver metastasis [50, 51]. Neuroendocrine tumours/ carcinomas express neuroendocrine markers (Chromogranin A, Synaptophysin) and show similar growth patterns to acinar cell carcinomas [50]. Proliferation activity (mitotic count, Ki67) is essential for tumour classification [51]. In serous cystic neoplasms, malignancy, as defined by metastases, is exceedingly rare [51]. Variants of pancreatic ductal adenocarcinoma Pancreatic ductal adenocarcinoma may contain substantial areas of mixed squamous, neuroendocrine and/or acinar differentiation. Although they are highly aggressive neoplasms, long-term survivors were observed Role of frozen section Frozen section is primarily useful to examine the pancreatic transection margin. Secondly, preoperatively unclear masses and cystic lesions can be diagnosed by frozen sections, helping to plan the extent of operations. Unfortunately, about 80% of patients present with an advanced often metastasized disease with surgery not being the primary treatment option [75, 76]. Histological confirmation of pancreatic adenocarcinoma is contraindicated in patients with resectable and borderline resectable disease if primary surgical resection is planned, due to prolonged waiting time for surgery and risk of tumour cell dissemination and the missing of a therapeutic consequence [77]. According to current consensus on definitions, these are defined as follows [77, 85]. The main question that needs to be answered is whether the primary tumour is resectable. Pancreatic cancers can be categorized into localized and systemically metastasized disease. The group of patients presenting with systemic disease is treated with systemic chemotherapy, palliative surgery, endoscopic intervention, and best supportive care [77]. Patients in the localized pancreatic cancer group should be divided into resectable, borderline-resectable, and unresectable cases. Treatment will follow a standardized algorithm; patients with resectable tumours will undergo exploration laparotomy and resection of the tumour with the goal of R0 status with curative intent. In case of a borderline-resectable cancer, neoadjuvant therapy should be contemplated. Patients primarily categorized as locally unresectable should undergo neoadjuvant (radio)chemotherapy for local downsizing followed by laparotomy with the goal of curative R0 resection [77, 78]. If the intraoperative judgement is that an R0 resection is not possible and/or systemic disease exists (distant metastases, peritoneal seeding), palliation surgery may be performed in the same session, for example by a double bypass (gastro-enterostomy and bilodigestive anastomosis). Resectable Tumours recognized as being locally resectable will present without any signs of distant metastases (including para-aortic lymph node metastases). Borderline resectable Borderline resectable tumours present without any signs of distant metastases (including para-aortic lymph node metastases). Venous involvement has to be with sufficient clear venous vessel allowing for safe venous resection and reconstruction. Borderline resectable tumours may present with gastroduodenal artery encasement up to the hepatic artery (including short segment encasement of the hepatic artery), but without any involvement of the celiac trunk. Unresectable Any pancreatic adenocarcinoma presenting in the stage of systemic disease (distant metastases). Members of this expert team include surgical oncologists and/or pancreatic surgeons, radiologists, medical oncologists, radiation oncologists, and endoscopy experts [77, 78, 84]. The pancreas will then be cut above the portal vein via sharp dissection, and pancreas and bile duct resection margins will be sent to immediate histopathological analysis via frozen section to confirm clear resection margins. The most important part of the reconstruction phase is the pancreatic anastomosis. This can be either performed via a pancreaticojejunostomy or pancreaticogastrostomy. Both techniques can be regarded as equal, as long as a tension-free anastomosis in well-perfused tissue without obstruction is performed [102]. The biliodigestive anastomosis is performed as an end-to-end anastomosis approximately 15 cm arborally from the pancreatic anastomosis. Antecolic reconstruction has been shown to reduce the incidence of delayed gastric emptying [103]. Drainage placement has not been shown to improve surgical outcome; however, many surgeons still use drains for two to three days post-operatively to measure enzyme activity [104]. The classical Whipple procedure is similar to the modified version with the difference that the distal 1/3 of the stomach is resected and gastrointestinal continuity is reestablished via an antecolic gastrojejunostomy. Operative technique Surgery should be performed in specialized high-volume pancreatic cancer centres [79, 80]. The goal of every potentially curative pancreatic resection should be a R0 resection with complete removal of the tumour and a standardized lymphatic dissection with a safe reconstruction technique. History of pancreatic surgery the first documented pancreatic resection has been attributed to Friedrich Trendelenburg, who performed a distal pancreatectomy and splenectomy in a patient with a sarcoma originating from the tail of the pancreas in 1882, more than a century ago [86]. The first modern pancreaticoduodenectomy has been credited to Walther Carl Eduard Kausch, who described a two-staged pancreaticoduodenectomy, which he performed in Berlin, Germany in 1909 [87]. A one-stage pancreaticoduodenectomy had been performed in 1912 by Georg Hirschel of Heidelberg, Germany [88]. In 1935 a landmark article was published by Allen Oldfather Whipple describing his surgical experience in three cases of pancreatic ampullary carcinoma, linking his name to the procedure of pancreaticoduodenectomy [89]. Current studies have shown the superiority of this modification with respect to operation time and intraoperative blood loss, while maintaining equal morbidity and short- and long-term mortality rates [96]. Any suspicious areas will be biopsied and analysed by a pathologist via frozen sections to exclude systemic disease. The next step is the mobilization of the right colonic flexure, the duodenum, and pancreatic head by a Kocher manoeuvre. After dissection of the gastrocolic ligament or the greater omentum from the transverse colon, access to the lesser sac is obtained. Careful preparation of the hepatoduodenal ligament will provide details about potential arterial involvement and any potential accessory hepatic arteries. Left resection (pancreatic tail resection) Resection of the pancreatic tail will be performed in tumours of the left side and pancreatic corpus. The lower resection rate in this type of surgery results from the usually more advanced disease in left-sided pancreatic cancer, as symptoms usually only appear in a very late (unresectable) stage of disease. In most cases a splenectomy with resection of the splenic vessels will be performed simultaneously to achieve R0 status. After transection of the splenic artery and vein the pancreatic tail can then be removed together with the spleen; care should be taken to obtain a negative retroperitoneal resection margin. A recent trial has compared closure with a stapling device compare to hand suture and found no significant difference with regard to the fistula rate [92]. Total pancreatectomy If a clear resection margin cannot be achieved with a Whipple procedure or for multifocal tumours in the pancreas, a total pancreatectomy might be indicated if R0 resection status can then be achieved. En bloc venous resections can be performed with equal perioperative mortality and morbidity rates as standard resections.
Syndromes
- Lack of head control
- Skin biopsy
- Fever
- Sleep apnea
- Name of product (as well as the ingredients and strength, if known)
- Sore throat

Order cefdinir 300mg line
Internal fixation of long bones is desirable to minimize pain antibiotic horror cheapest cefdinir, speed mobilization, and avoid non-union. Bones at risk of pathological fracture identified on imaging should have pre-emptive internal fixation. Patient information and psychological support Patients should be given information about their disease and advised of the steps to take in the event of disease- or treatment-related adverse events, such as neutropenic sepsis, drug reactions, or new symptoms of disease. A multidisciplinary approach to the whole patient and appropriate referrals to psychological and palliative care support are important. Anaemia the aetiology of anaemia in myeloma is multifactorial, resulting from the combined effects of bone marrow infiltration, renal failure, the blunting of the erythropoietin response by cytokines and the effects of chemotherapy. Adequate specific therapy will usually correct the anaemia in patients responding to treatment and transfusions will maintain adequate control in others. Relapse Despite improvements in myeloma therapy with the advent of novel agents, disease relapse inevitably occurs in most patients. With progressive relapses, the disease becomes more difficult to treat and progression-free periods between treatments shorten [164]. Monitoring during treatment Myeloma patients are generally monitored regularly in a specialist haematology clinic, at two- to three-monthly intervals after disease remission. In the latter case, treatment should be started in the absence of symptoms to prevent rapid clinical deterioration. More recently, with the advent of new drugs which modify the disease natural history, there has been a tendency to start treatment earlier as soon as clinical relapse can be predicted. Prevention of infection Recurrent bacterial infections are a major cause of morbidity and mortality in patients with myeloma. The risk of infection is highest in the first few months after diagnosis and decreases with response to therapy [156] but still remains the major contributor to early deaths [57]. Aminoglycosides are avoided because of the likely additive impact on renal function. Patients are offered vaccination against seasonal influenza, Streptococcus pneumonia, and Haemophilus influenza, but the vaccination may not produce an effective Investigations at relapse Relapse should be confirmed by repeating the bone marrow biopsy and imaging. As treatments become available to target specific genetic lesions this will be of even greater importance. The molecular events acquired as myeloma progresses are not acquired in a linear fashion but in branching non-linear pathways resulting in different clonal populations with different molecular characteristics, a concept termed intraclonal heterogeneity. These clones compete for dominance and at each relapse the dominant clone may have different features. This suggests that the sequence in which treatments with different mechanisms of action are used may affect clonal selection and, therefore, clinical outcomes. It also has an impact on the development of targeted treatments, as a treatment targeting a lesion found in only a minor subclone will not successfully eradicate the whole population. Treatment with bortezomib is unaffected by prior lenalidomide [167, 168] and vice versa [169]. Importantly, even if response duration has been short in a relapsed patient with no other therapeutic options, high dose melphalan supported by stem cells may be acceptable. Other options include combinations of novel agents, such as lenalidomide and bortezomib [173], the new proteasome inhibitor carfilzomib (which has efficacy even in patients with bortezomib-refractory disease) [174], or older agents such as bendamustine (see Box 53. There have been particularly promising results for antibody-targeted therapies. In addition, trials are ongoing for oral proteasome inhibitors, epigenetic therapies including histone deacetylase inhibitors, and molecularly-targeted treatment strategies. Assessment of relapse the age and performance status of the patient at the time of relapse will help determine what type of agents may be tolerable. Side effects often accumulate with therapy and should be carefully assessed, including the presence of neuropathy, risk factors for venous thromboembolism, and the remaining bone marrow reserve. This includes patients who have stable disease on all therapies and those who have progressive disease having never responded. Relapse Relapse is defined as patients who have had a period of time (at least 60 days) off therapy and have disease progression requiring treatment. Prospective studies are required to investigate whether a lower cut-off would be more valid as even a few circulating plasma cells may indicate a highly proliferative and aggressive process. Patients often present with a high tumour burden and aggressive, rapidly developing clinical symptoms including anaemia, bleeding due to thrombocytopenia, and hypercalcaemia. Extramedullary disease is common and should be investigated with whole-body imaging techniques. The assessment of disease response to relapse treatment should also be considered differently from induction treatment. Especially in later stages of disease, it becomes more important to maintain a stable disease state rather than aim for complete response. If a thalidomide-based treatment has been used first-line then bortezomib is generally preferred at relapse, with lenalidomide reserved for subsequent relapse. Symptomatic improvement is often slow but continues over time and has been seen up to three years following treatment. The goals of treatment are to rapidly control disease to minimize the risk of early death and to achieve complete responses if possible. Intensive chemotherapy regimens combining novel drugs, including bortezomib with different classes of chemotherapy and steroids, are often used. In younger patients, myeloablative or reduced intensity allografts and tandem autografts have also been used if they are in deep stable responses. Amyloidosis Amyloidosis is a condition characterized by the deposition of insoluble, fibrillar protein in the extracellular space leading to organ dysfunction. Protein deposition can occur in virtually all organs but predominantly symptoms result from cardiac (70%), renal (70%), liver (17%), neurological (15%), or gastrointestinal (10%) involvement [191]. Amyloidosis may also be associated with coagulopathy due to factor X deficiency, as a result of vitamin K-dependent clotting factors binding to amyloid deposits [192]. Demonstration of amyloid deposition in the tissue is performed by Congo red staining, but further characterization of the amyloid type is also necessary to guide the correct treatment and requires the use of mass spectrometry proteomics. Following diagnosis, each organ system should be fully evaluated and investigations to look for clonal plasma cells, if their presence is not already known, should be undertaken. Treatment for amyloid is aimed at rapidly reducing the abnormal light-chain production by targeting the plasma cell clone. In addition to their prognostic role, cardiac biomarkers are also important in determining appropriate therapy. Patients at high risk need gentler, but rapidly acting regimens; bortezomib is often used. It is characterized by the presence of Polyneuropathy, Organomegaly, Endocrinopathy, Monoclonal plasma cell disorder, and Skin changes. It may also include other features including papilloedema, fluid overload, sclerotic bone lesions, and elevated red blood cells or platelets [183, 184]. It should be considered in cases of myeloma where the symptoms are not typical, for example when neuropathy, endocrine abnormalities and volume overload predominate over bone pain. If there is evidence of a clonal plasma cell population on bone marrow biopsy or other evidence of disseminated disease then radiotherapy is not expected to be curative and treatment with systemic chemotherapy should be initiated even if the plasma cell percentage is very small. Patients may have a poor pulmonary reserve as a result of neuromuscular impairment and a reduction in lung diffusion capacity. There is also a relatively high incidence of engraftment syndrome [189]; treatment-related morbidity and mortality can be reduced by actively monitoring and treatment with corticosteroids. Intermediate-risk patients are commonly given melphalan and dexamethasone, which induces good responses [196] although newer agents are being investigated. Haematologic and cardiac response is assessed frequently to enable therapy to be switched to a different agent and prevent progression of target organ damage if there is not a good response. To meet diagnostic criteria there must be <10% plasma cells on bone marrow biopsy, a single area of disease, and no related organ or tissue impairment. The key to successful treatment is to accurately rule out the presence of disease elsewhere as truly isolated lesions can be treated with radiotherapy alone with the expectation of cure. These cases are often marginal zone lymphomas with plasma-cell differentiation and can be cured with surgical resection (although this is often technically impossible due to the location of disease) or radiotherapy. Gender disparities in the tumor genetics and clinical outcome of multiple myeloma.
Discount 300 mg cefdinir mastercard
Fortunately infection 2 strategy 300mg cefdinir for sale, there is little danger that this type of cancer will spread, or metastasize, to other areas of the body. Squamous cell carcinoma develops from cells immediately superficial to the stratum basale. Normally, these cells undergo little or no cell division, but in squamous cell carcinoma, the cells continue to divide as they produce keratin. The typical result is a nodular, keratinized tumor confined to the epidermis (figure 5. As the body ages, the skin is more easily damaged because the epidermis thins and the amount of collagen in the dermis decreases. A decrease in the number of elastic fibers in the dermis and loss of adipose tissue from the subcutaneous tissue cause the skin to sag and wrinkle. A decrease in the activity of sweat glands and in the blood supply to the dermis results in reduced ability to regulate body temperature. The number of melanocytes generally decreases, but in some areas the number of melanocytes increases to produce age spots. Note that age spots are different from freckles, which are caused by increased melanin production. Gray or white hair also results because of a decrease in or a lack of melanin production. Skin that is exposed to sunlight shows signs of aging more rapidly than nonexposed skin, so avoiding overexposure to sunlight and using sunscreen is advisable. We also know that the amount of melanin produced is determined by several natural factors, including our genes. We can assume that Mia and landon naturally have darker skin than Christine because they each possess genes that allow them to produce more melanin when exposed to ultraviolet light. Other functions include sensation, vitamin D production, temperature regulation, and excretion of small amounts of waste products. Keratinization is the transformation of stratum basale cells into stratum corneum cells. Collagen and elastic fibers provide structural strength, and the blood vessels of the papillae supply the epidermis with nutrients. Melanin production is determined genetically but can be modified by exposure to ultraviolet light and by hormones. Carotene, a plant pigment ingested as a source of vitamin A, can cause the skin to appear yellowish. Increased blood flow produces a red skin color, whereas decreased blood flow causes a pale skin color. Ultraviolet light stimulates the production of a precursor molecule in the skin that is modified by the liver and kidneys into vitamin D. Through dilation and constriction of blood vessels, the skin controls heat loss from the body. The subcutaneous tissue, which is not part of the skin, is loose connective tissue that attaches the skin to underlying tissues. Each hair consists of a shaft (above the skin), a root (below the skin), and a hair bulb (site of hair cell formation). Contraction of the arrector pili, which are smooth muscles, causes hair to "stand on end" and produces a "goose bump. Apocrine sweat glands produce an organic secretion that causes body odor when broken down by bacteria. Partial-thickness burns damage only the epidermis (first-degree burn) or the epidermis and the dermis (second-degree burn). Full-thickness burns (third-degree burns) destroy the epidermis, the dermis, and usually underlying tissues. The nail matrix produces the nail, which is composed of stratum corneum cells containing hard keratin. Basal cell carcinoma involves the cells of the stratum basale and is readily treatable. Squamous cell carcinoma involves the cells immediately superficial to the stratum basale and can metastasize. Protection the skin reduces water loss, prevents the entry of microorganisms, and provides protection against abrasion and ultraviolet light; hair and nails also perform protective functions. Blood flow to the skin is reduced, the skin becomes thinner, and elasticity is lost. Sweat and sebaceous glands are less active, and the number of melanocytes decreases. What structural changes does keratinization produce to make the skin resistant to abrasion and water loss Where are the cells that make up the nail produced, and what kind of cells make up a nail A woman has stretch marks on her abdomen, yet she states that she has never been pregnant. After the match, he discovers that a blister has formed beneath an old callus on his foot and the callus has fallen off. A mucous membrane covers the lips internally, and the skin of the face covers them externally. The red part of the lips (called the vermillion border) is covered by keratinized epithelium that is a transition between the epithelium of the mucous membrane and the facial skin. The vermillion border can become chapped (dry and cracked), whereas the mucous membrane and the facial skin do not. Propose as many reasons as you can to explain why the vermillion border is more prone to drying than the mucous membrane or the facial skin. Given what you know about the cause of acne, propose some ways to prevent or treat it. Consider the following statement: Dark-skinned children are more susceptible to rickets (insufficient calcium in the bones) than lightskinned children. What color would you expect his skin to be (a) after going outside and just before starting to run, (b) during the run, and (c) 5 minutes after the run Roberta Rutledge had worked together for almost two decades, and Roberta knew something was bothering Thomas. She noticed him wincing in pain whenever he bent down to retrieve something from a bottom shelf, and he was shorttempered rather than his usual happy self. Also, using your knowledge of vertebral anatomy, predict the region of the injury and explain why this region of the vertebral column is more prone to this type of injury than other regions. Sitting, standing, walking, picking up a pencil, and taking a breath all involve the skeletal system. Without the skeletal system, there would be no rigid framework to support the soft tissues of the body and no system of joints and levers to allow the body to move. Rather, the skeletal system consists of dynamic, living tissues that are able to grow, detect pain stimuli, adapt to stress, and undergo repair after injury. Many joints are movable, although some of them allow only 110 limited movement; others allow no apparent movement. Although the skeleton is usually thought of as the framework of the body, the skeletal system has many other functions in addition to support. Rigid, strong bone is well suited for bearing weight and is the major supporting tissue of the body. Cartilage provides firm yet flexible support within certain structures, such as the nose, external ear, thoracic cage, and trachea. Ligaments are strong bands of fibrous connective tissue that attach to bones and hold them together. For example, the skull encloses and protects the brain, and the vertebrae surround the spinal cord. Skeletal System: Bones and Joints 111 Skull Clavicle Sternum Ribs Vertebral column Pelvis Radius Ulna Humerus Femur Tibia Fibula molecules, as well as water and minerals. But the types and quantities of these substances differ in each type of connective tissue. Collagen (kol la-jen; koila, glue + -gen, producing) is a tough, ropelike protein.
Purchase cefdinir 300mg without prescription
Additional factors related to the leukaemogenic potential of residual cells antibiotics for strep viridans uti buy line cefdinir, and immune or microenvironmental factors may determine risk of relapse. Several preclinical and clinical studies addressing these questions are already underway. The clinical course is variable with an indolent, minimally symptomatic course in many patients for many years. The remainder present with various symptoms including constitutional symptoms, such as fatigue, weight loss, and fever. Sometimes, enlarged lymph nodes, with the development of an infection is the initial manifestation of disease. Bacterial infections, such as pneumonia, are more common in patients who present with advanced stage disease. Infections secondary to opportunistic organisms, particularly Herpes zoster, may occur. Leptomeningeal leukaemia is rare and, if present, is usually seen in patients with refractory disease. The pathologic features of the lymph node are those of a small lymphocytic lymphoma. The blood lymphocyte count must be charted at diagnosis and at each follow-up to determine the doubling time. Molecular changes leading to the pathogenesis of the disease are still poorly understood. Patients with 17p or 11q deletion generally have more advanced disease with frequent splenomegaly, mediastinal, and abdominal lymphadenopathy and more extensive peripheral lymphadenopathy. Chlorambucil is still indicated for use in the low-risk patient and elderly patients who have a poor performance status. The drug also suppresses both T and B lymphocytes with resultant increase in bacterial, viral and opportunistic infections [142, 143]. Treatment options are: (i) chlorambucil, (ii) fludarabine, (iii) fludarabine + cyclophosphamide, or (iv) observation. Selecting the best treatment for an individual patient is sometimes difficult and challenging. Patients either relapsing rapidly or not responding to first-line chlorambucil should be considered for fludarabine-containing regimens. The majority of patients treated with these agents and combinations have a partial response. Three randomized trials have shown the superiority of this combination over fludarabine alone. Even though the combination produces more myelosuppression, infection rates and mortality due infection have not been found to be increased. However, grade 3 and 4 neutropaenia have been reported in 51% patients [151, 152]. Grade 3/4 neutropaenia was significantly more common in the three-drug regimen [153, 154]. Combination of rituximab with purine analogues and/or alkylating agents significantly adds to activity and potency [152, 154, 156]. Rituximab administration can be associated with significant infusion toxicities including rigors, anaphylactic reactions, and hypotension. As a rule, premedication with steroids and antihistaminics should be given to all patients and the infusion should be initiated slowly under careful monitoring of vital parameters. The initial approval of the drug was for patients who were refractory to fludarabine [159] but recently it has been approved for first-line use also. There are some reports suggesting that alemtuzumab may have significantly more activity than standard treatment in high-risk patients who have 17p and 11q deletions [160, 162]. The drug has shown encouraging activity when combined with fludarabine [163, 164] and chlorambucil [162]. Subcutaneous administration of the drug is effective and is being tested in clinical trials [165, 166]. Management of the relapse/refractory chronic lymphocytic leukaemia patient the most important consideration in the choice of therapy for the patient who relapses is the initial treatment and the duration of response to the same. The drug is indicated either alone or in combination with fludarabine or rituximab. Rituximab in combination with purine analogues is being tested in relapsed patients. Infiltration in the spleen occurs exclusively in the red pulp with sparing of the white pulp, liver involvement is restricted to sinusoids, and lymph node infiltration is rare [187]. The fibrosis seen in the involved tissues is thought to be due to the secretion of fibronectin by the hairy cells, which is an extracellular matrix ligand for a4b. Lenalidomide (Revlimid) is presently approved for use in multiple myeloma and in patients of myelodysplastic syndrome with 5q deletion. About a quarter of patients present either with easy fatigability, infections, incidental splenomegaly, or abnormal blood counts. Though peripheral lymphadenopathy is uncommon (10%), abdominal lymphadenopathy at presentation is found in 17% and in 75% at autopsy. However, certain unusual organisms like atypical mycobacteria, Pneumocystis jirovecii, Legionella, Listeria, and fungi occur more frequently than in other lymphoproliferative disorders. Presentation is often non-specific with symptoms of fever, malaise, weight loss, arthralgias, and palpable purpura. The reason for this association is hypothesized to be antigenic cross reaction between hairy cell antigens and epitopes on endothelial cells as well as defective immune complex clearance by the functionally impaired immune mechanisms [192]. Most patients have variable degree of cytopaenias and more than half have pancytopaenia [189]. These hairy cells are so-called because of their circumferential fine hairy-like cytoplasmic projections. Other haematopoietic elements may or may not be adequately represented in the biopsy specimens. Immunohistochemistry on trephine is often not done in the era of immunophenotyping. One needs to be aware of the immunophenotypic variations that can be seen in up to 35% of the cases. Symptomatic cytopaenias, organomegaly, constitutional symptoms interfering in the activities of daily living of the patient are common indications for treatment. It is important to intervene if there is a rapid worsening of blood counts, as treatment itself entails a further risk of worsening the cytopaenias [196]. Major long-term studies have not shown a plateau in relapse-free survival curves even with current therapies, suggesting disease control but not cure [208]. The results with these two new agents were so remarkable that the response criteria were redefined. Following their discovery, many case series were published using pentostatin and cladribine. However, there is no clinical difference in outcomes when used as either first- or second-line therapy. To overcome the inconvenience of seven-day continuous infusion, alternative dosing schedules were designed: daily intravenous pulse of 0. All these regimens were found to have equivalent efficacy, toxicity, and outcomes [201]. In the absence of randomized control trials, the choice between cladribine and pentostatin rests with the physician and the patient.
Purchase cefdinir 300mg with visa
Prospective study of early detection of hepatocellular carcinoma in patients with cirrhosis infection with red line buy cefdinir 300 mg otc. European Association for the Study of the L, European Organisation for R, Treatment of C. Prognosis of hepatocellular carcinoma: comparison of 7 staging systems in an American cohort. Meta-analysis: surveillance with ultrasound for early-stage hepatocellular carcinoma in patients with cirrhosis. Model for end-stage liver disease and Child-Turcotte-Pugh score as predictors of pretransplantation disease severity, posttransplantation outcome, and resource utilization in United Network for Organ Sharing status 2A patients. Elective liver transplant mortality: development of a United Kingdom end-stage liver disease score. Prognostic impact of hepatectomy for patients with non-hepatitis B, non-hepatitis C hepatocellular carcinoma. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. Liver transplantation for hepatocellular carcinoma: expansion of the tumor size limits does not adversely impact survival. Recommendations for liver transplantation for hepatocellular carcinoma: an international consensus conference report. A novel model measuring the harm of transplanting hepatocellular carcinoma exceeding Milan criteria. Transcatheter arterial chemoembolization combined with radiofrequency ablation for the treatment of hepatocellular carcinoma. Survival analysis of high-intensity focused ultrasound therapy versus radiofrequency ablation in the treatment of recurrent hepatocellular carcinoma. Irreversible electroporation therapy in the liver: longitudinal efficacy studies in a rat model of hepatocellular carcinoma. Contrast-enhanced ultrasound for the differentiation of benign and malignant focal liver lesions: a meta-analysis. Transcatheter arterial chemoembolization for unresectable hepatocellular carcinoma: recent progression and perspective. A prospective randomized controlled trial of preoperative whole-liver chemolipiodolization for hepatocellular carcinoma. Patient selection and activity planning guide for selective internal radiotherapy with yttrium-90 resin microspheres. Chemosaturation with percutaneous hepatic perfusion for unresectable isolated hepatic metastases from sarcoma. Tivantinib, a new option for second-line treatment of advanced hepatocellular carcinoma Phase 2 study of erlotinib in patients with unresectable hepatocellular carcinoma. Phase I study investigating everolimus combined with sorafenib in patients with advanced hepatocellular carcinoma. Doxorubicin plus sorafenib vs doxorubicin alone in patients with advanced hepatocellular carcinoma: a randomized trial. Hepatitis B reactivation in patients with hepatocellular carcinoma undergoing systemic chemotherapy. Operative microwave ablation for hepatocellular carcinoma: complications, recurrence, and long-term outcomes. Ablation of perivascular hepatic malignant tumors with irreversible electroporation. Complete pathological remission is possible with systemic combination chemotherapy for inoperable hepatocellular carcinoma. Unresectable hepatocellular carcinoma: a prospective controlled trial with tamoxifen. Tamoxifen in treatment of hepatocellular carcinoma: a randomised controlled trial. Treatment of advanced hepatocellular carcinoma with tamoxifen and the correlation with expression of hormone receptors: a prospective randomized study. Lamivudine for the prevention of hepatitis B virus reactivation in hepatitis B s-antigen seropositive cancer patients undergoing cytotoxic chemotherapy. Jaundice predicts advanced disease and early mortality in patients with gallbladder cancer. Management of carcinoma of the gallbladder: a single-institution experience in 16 years. An aggressive surgical approach leads to improved survival in patients with gallbladder cancer: a 12-year study at a North American Center. Treatment outcomes associated with surgery for gallbladder cancer: a 20-year experience. Impact of integrated positron emission tomography and computed tomography on staging and management of gallbladder cancer and cholangiocarcinoma. Positron-emission tomography with fluorine-18-fluoro-2-deoxy-D-glucose for gallbladder cancer diagnosis. Regional and para-aortic lymphadenectomy in radical surgery for advanced gallbladder carcinoma. Surgical treatment of primary carcinoma of the gallbladder based on the histologic analysis of 48 surgical specimens. Incidence of finding residual disease for incidental gallbladder carcinoma: implications for re-resection. Cholecystectomy, liver resection, and pylorus-preserving pancreaticoduodenectomy for gallbladder cancer: report of five cases. Combined pancreaticoduodenectomy and hepatectomy for patients with locally advanced gallbladder carcinoma: long term results. Prognostic significance of the number of positive lymph nodes in gallbladder cancer. What prognostic factors are important for resected intrahepatic cholangiocarcinoma Intrahepatic peripheral cholangiocarcinoma: mode of spread and choice of surgical treatment. Outpatient chemotherapy with gemcitabine and oxaliplatin in patients with biliary tract cancer. Gemcitabine and oxaliplatin combination chemotherapy in advanced biliary tract cancers. Adjuvant external beam radiation therapy with concurrent chemotherapy in the management of gallbladder carcinoma. Intrahepatic biliary enteric bypass provides effective palliation in selected patients with malignant obstruction at the hepatic duct confluence. The role of chemotherapy and radiation in the management of biliary cancer: a review of the literature. Long-term survival and prognostic factors in the surgical treatment of mass-forming type cholangiocarcinoma. Indications for surgical treatment of intrahepatic cholangiocarcinoma with lymph node metastases. Number of lymph node metastases is a prognostic factor in intrahepatic cholangiocarcinoma. Mesothelioma may involve the pleura, less frequently the peritoneum, and rarely, the pericardium and tunica vaginalis testes. In the past, peritoneal mesothelioma was a rapidly fatal peritoneal surface malignancy with a median survival of less than one year [1, 2]. It represents about one-fifth to one-third of all forms of mesothelioma; there are approximately 400 new cases in the United States each year [3].
Cheap cefdinir master card
Late side effects of the skin include atrophy antibiotic kinetics cefdinir 300mg without prescription, telangiectasia, fibrosis, and pigmentary changes. The combination of lymph node dissection and radiotherapy has an increased risk for chronic lymphoedema. A Cochrane analysis between radiochemotherapy (primary or neoadjuvant) and primary surgery did not show a significant difference in overall survival or treatment-related side effects [143]. Side effects are similar to adjuvant radiotherapy and primary radiotherapy of vaginal cancer. Ovarian cancer Surgery and adjuvant chemotherapy are the cornerstones in primary treatment of ovarian cancer. Radiotherapy is currently not part of the primary treatment concept in the majority of cases. However, radiotherapy is mainly applied in palliative intent for metastatic disease such as bone or brain metastasis and especially for inoperable isolated pelvic recurrences. Medical management Cervical cancer this entity shows high sensitivity for radiotherapy. Combined radiochemotherapy with weekly 40 mg cisplatin in addition to radiotherapy led to an improved survival and apart from systemic effect chemotherapy is mainly considered as a radiosensitizer in this setting [107]. Neoadjuvant chemotherapy is an option in bulky disease with the aim of shrinkage of advanced disease. Neoadjuvant chemotherapy with dose dense weekly paclitaxel and carboplatin followed by standard combined radiochemotherapy is a feasible approach and is associated with a high response rate (67%) in locally advanced cervical cancer [144]. Another small study with neoadjuvant platinum-taxane based chemotherapy showed a response rate of 78. In consequence, radiochemotherapy may be used for improving resectability or as single treatment. At first external beam radiotherapy is performed following the same principle as for adjuvant treatment. For further chemotherapy lines, monotherapies with anthracyclines or taxane are recommended. Vulvar cancer Vulvar cancer is a rare disease, usually diagnosed in a stage still amenable to potentially curative treatments, including surgery and/or radiotherapy with or without chemotherapy. Prognosis of metastatic or recurrent disease not amenable to salvage surgery or radiotherapy is very poor. Evidence about the efficacy of chemotherapy in this setting is limited and its role still remains unclear. Combined radiochemotherapy with cisplatin can be used in the adjuvant setting as well as in the neoadjuvant setting in locally advanced tumours [66]. At present, patients with advanced vulvar carcinomas and patients with metastatic disease are usually treated with schedules adopted for chemoradiation or extrapolated from cervical cancer [160]. Criteria for the indication and performance of chemo/radiotherapy of the vulva, groins, and pelvis are still not fully established and vary between different countries and institutions due to the low level of evidence. Often an individualized therapeutic approach aside from guidelines is necessary to treat these patients adequately [66]. Endometrial cancer Endometrial cancer shows the highest incidence in gynaecologic malignancies. Low-risk early stage endometrial cancer needs surgical treatment only and no adjuvant chemotherapy. Chemotherapy has evolved into an important modality in high-risk early stage and advanced stage disease and in recurrent endometrial cancer. Multi-institutional trials are in progress to better define optimal adjuvant treatment for subsets of patients [151]. For patients able to tolerate aggressive therapy, multiagent chemotherapy produces higher response rates than single-agent therapy. A significant 5-year survival increase of 13% for patients was present for patients who got chemotherapy relative to the radiotherapy arm [152]. Meta-analysis of nine prospective, randomized trials with 2197 patients showed that adjuvant chemotherapy in high-risk endometrial carcinoma can decrease lethality by 25% [153]. The most favourable benefit/risk profile seems to have carboplatin/paclitaxel, but platinum/anthracycline and platinum/anthracycline/taxane combinations are effective also [154]. Hormonal therapy is standard treatment in metastatic hormonal receptor positive endometrial cancers, but not in the adjuvant setting. Hormonal therapy, primarily with progestins, is less toxic than chemotherapy and 20% response rates are seen in properly selected patients [155]. Control hysteroscopy and curettage is necessary and recommendation of hysterectomy and oophorectomy after childbearing [157]. For distant metastases chemotherapy schedules similar to cervical cancer are applicable. These data provide robust evidence for the important role of bevacizumab in ovarian cancer treatment. Data from European clinical trials of dose-dense regimen with paclitaxel weekly could not confirm a survival benefit in comparison to standard treatment [170]. Neoadjuvant platinum/taxane-based chemotherapy in ovarian cancer is recommended only within clinical trials. Despite higher complete resection rates after neoadjuvant treatment, no improved survival was present and the documented extent of surgical management within this trial was very questionable [98]. If neoadjuvant chemotherapy was initiated because of contraindication for immediate radical surgery, interval debulking surgery should be performed after a maximum of two to three cycles because of the development of resistance mechanisms in case of later surgery [171]. A very mild toxicity profile was documented for maintenance therapy with olaparib [172]. The management of the very rare, but very aggressive small-cell carcinomas of the gynaecologic tract (cervix, ovary, uterus, vulva, and vagina) requires systemic chemotherapy with cisplatin and etoposide, both in the setting of early and advanced stage disease [173]. General and surgical management A biopsy was performed and histology showed invasive squamous cell carcinoma, grade 2. Cystoscopy showed an intact urinary bladder mucosa and thus did not confirm bladder wall invasion. After laparoscopic lymph node staging, 0 of 23 removed lymph nodes (12 pelvic, 11 para-aortic) showed malignant cells indicating a pN0 status. Radiotherapy management the patient was referred to the Department of Radiotherapy for initiation of primary radiochemotherapy consisting of external beam radiotherapy, concomitant chemotherapy, and image-guided adaptive brachytherapy. The clinical tumour-related target volume included the whole uterus, the upper third of the vagina, the whole parametria and the (regional) lymph node areas up to the aortic bifurcation, internal/external/common iliac areas, para-rectal, and pre-sacral areas. The fifth cycle of chemotherapy had to be delivered in reduced dosage due to impaired renal function. In week six, the first brachytherapy application was performed in an operation theatre under spinal anaesthesia. Case report 1 A 45-year-old patient presented at the Department of Gynaecology with dyspareunia, vaginal bleeding, and persisting vaginal discharge for approximately three months. C, D: At the time of brachytherapy after 45 Gy of external beam radiotherapy and five cycles of chemotherapy: 5. The surrounding organs at risk (rectum, urinary bladder, sigmoid colon, and bowel) were delineated. Follow-up the patient achieved complete remission as assessed three months after completion of radiochemotherapy. Gynaecologic examination shows no evidence of disease and some vaginal shortening and narrowing in the upper third (G2). Rectosigmoidoscopy shows telangiectasia in the proximal anterior rectal wall but without any sign for bleeding. Discussion According to international and institutional guidelines based on clinical level 1 evidence this patient was treated with primary radiochemotherapy. Before initiation of radiochemotherapy laparoscopic lymph node staging was performed. However, precise assessment of lymph node status is crucial for the definition of the lymph node target volume (pelvic vs pelvic + para-aortic).